Troubleshooting Heterogeneous Data Integration in Multi-Cohort Studies: A Practical Guide for Biomedical Researchers
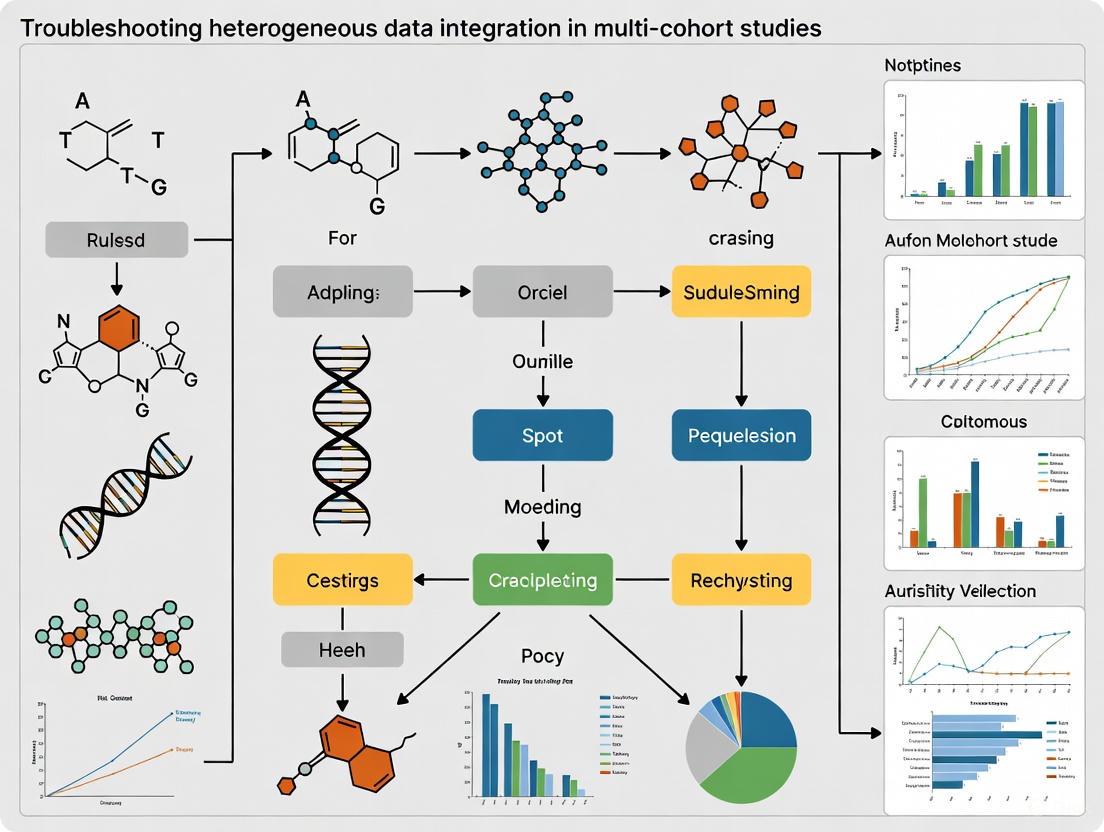
Integrating heterogeneous data from multiple cohort studies is crucial for enhancing statistical power and enabling novel discoveries in biomedical research, yet it presents significant challenges in data harmonization, technical variability,...
Troubleshooting Heterogeneous Data Integration in Multi-Cohort Studies: A Practical Guide for Biomedical Researchers
Abstract
Integrating heterogeneous data from multiple cohort studies is crucial for enhancing statistical power and enabling novel discoveries in biomedical research, yet it presents significant challenges in data harmonization, technical variability, and analytical methodology. This article provides a comprehensive framework for researchers and drug development professionals, covering foundational concepts, practical methodologies, common troubleshooting scenarios, and validation techniques. By addressing key intents from exploration to validation, it offers actionable strategies to overcome data inconsistency, implement robust integration pipelines, and build generalizable models, ultimately facilitating more reliable and impactful multi-cohort research.
Understanding the Landscape: Core Concepts and Challenges of Heterogeneous Data in Multi-Cohort Research
Frequently Asked Questions (FAQs)
Q1: What are the primary types of data formats encountered in biomedical research, and how do they differ? Biomedical data is categorized into three main formats, each with distinct characteristics [1]:
- Structured Data: Highly organized data that fits into predefined models and is easily searchable. Examples in healthcare include patient demographics in Electronic Health Records (EHRs), medical billing codes (CPT, ICD), and clinical trial data like patient enrollment and outcomes [1]. This data is typically stored in rows and columns within relational databases.
- Unstructured Data: Data that lacks a predefined format or structure. This constitutes the majority (approximately 80% or more) of healthcare data [2] [3] [4]. Examples include clinical notes, medical images (X-rays, MRIs), pathology reports, and doctors' audio dictations [1] [4]. Analyzing this data requires advanced techniques like Natural Language Processing (NLP) and image recognition.
- Semi-Structured Data: Data that does not conform to a rigid schema but contains tags or other markers to enforce a hierarchy of records and fields. Examples include HL7 FHIR resources, C-CDA documents for health information exchange, and JSON or XML files [1] [5]. It balances structure with flexibility, facilitating data exchange between disparate systems.
Q2: What are the most significant challenges when integrating these heterogeneous data types in multi-cohort studies? Integrating heterogeneous data presents a cascade of challenges [6], which can be categorized as follows:
- Technical and Semantic Heterogeneity: Data sources vary in structure, format, and content. Combining data from different hospitals, registries, and omics technologies often involves matching patient variables by hand due to a lack of common data standards, which is time and resource-intensive [7] [8].
- Data Complexity and Preprocessing: Unstructured and semi-structured data require significant preprocessing and feature extraction before they can be analyzed or integrated [9] [3]. This includes cleaning, normalizing, and transforming data, which is complicated by the high-dimensional nature of biomedical data where variables often far outnumber samples [6].
- Interoperability and Schema Evolution: The lack of fixed schema in semi-structured and unstructured data, along with the use of different terminology systems (e.g., SNOMED-CT, RxNorm), creates interoperability barriers [8]. Furthermore, schemas can evolve over time, complicating integration efforts [5].
- Regulatory and Privacy Concerns: Fusing data streams increases the risk of patient re-identification. Managing sensitive health data requires strict adherence to privacy laws like HIPAA and GDPR, which governs data de-identification, consent processes, and access control [8] [4].
Q3: What methodologies can be used to categorize and merge unstructured clinical data from different sources? One effective methodology involves semantic categorization and clustering [9]:
- Sub-category Identification: Begin with the existing titles or labels provided by dataset providers (e.g., "Diagnosis," "Differential Diagnosis").
- Semantic Similarity Computation: Extract semantic information from the unstructured text in these sub-categories. Use medical ontologies to identify terms and compute semantic similarity between sub-categories from different datasets. Techniques like hierarchical clustering and similarity measures such as Hausdorff distance can be employed.
- Cluster and Merge: Group semantically similar sub-categories (e.g., "Findings," "Observation," and "Diagnosis") into clusters. Based on the contents of the merged data elements, identify attributes for a new, integrated database schema. This approach has been shown to reduce the number of original sub-categories significantly, enabling the design of a unified schema [9].
Q4: How can Natural Language Processing (NLP) transform unstructured data for use in research? NLP uses several core processes to convert unstructured text into structured, analyzable information [4]:
- Tokenization: Breaking down text into smaller units like words or phrases.
- Named Entity Recognition (NER): Identifying and classifying key entities such as patient names, medications, and diseases.
- Sentiment Analysis: Assessing the tone or emotion in text, useful for analyzing patient feedback.
- Text Classification: Assigning categories or labels to text, such as flagging a clinical note as "urgent." These techniques allow for the extraction of clinical information from doctors' notes, automation of medical coding and billing, acceleration of drug discovery by scanning research papers, and improvement of clinical trial matching by analyzing patient records [4].
Q5: What are the common strategies for integrating multi-omics data, which is inherently heterogeneous? Multi-omics data integration strategies for vertical data (data from different omics layers) can be categorized into five types [6]:
- Early Integration: All omics datasets are concatenated into a single large matrix before analysis. This is simple but can result in a complex, high-dimensional matrix.
- Mixed Integration: Each dataset is separately transformed into a new representation and then combined, which helps reduce noise and dimensionality.
- Intermediate Integration: Datasets are integrated simultaneously to produce both common and omics-specific representations.
- Late Integration: Each omics dataset is analyzed separately, and the final predictions or results are combined. This does not capture inter-omics interactions well.
- Hierarchical Integration: Prior knowledge about regulatory relationships between different omics layers is incorporated, truly embodying the goal of trans-omics analysis, though this is a nascent field.
Troubleshooting Guides
Guide 1: Resolving Data Format and Schema Mismatches
Problem: Researchers encounter errors when trying to query or combine datasets due to incompatible structures or schemas (e.g., different date formats, missing fields, or varying code systems).
Investigation & Solution:
| Step | Action | Example/Details |
|---|---|---|
| 1. Profiling | Systematically analyze the structure, content, and quality of all source datasets. | Identify differences in data types (e.g., string vs. categorical), value formats (e.g., DD/MM/YYYY vs. MM-DD-YYYY), and the use of controlled terminologies (e.g., different ICD code versions) [7]. |
| 2. Standardization | Map data elements to common data models (CDMs) and standard terminologies. | Adopt models like OMOP CDM or use standards like FHIR for semi-structured data [1] [8]. Map local medication codes to a standard like RxNorm [8]. |
| 3. Schema Mapping | Define explicit rules to transform source schemas to a unified target schema. | Create a mapping table that defines how each source field (e.g., Pat_DOB, PatientBirthDate) corresponds to the target integrated field (e.g., birth_date). Tools with mapping engines can automate this for structured data [2]. |
| 4. Validation | Perform checks to ensure data integrity and accuracy after transformation. | Run queries to check for null values in critical fields, validate that value ranges are plausible, and spot-check mapped records against source data. |
Guide 2: Addressing High Preprocessing Burden for Unstructured Data
Problem: The effort required to clean, normalize, and extract features from unstructured data (like clinical notes) is prohibitive and delays analysis.
Investigation & Solution:
| Step | Action | Example/Details |
|---|---|---|
| 1. Tool Selection | Implement an NLP pipeline suited to the biomedical domain. | Use NLP libraries with pre-trained models for tasks like tokenization, Named Entity Recognition (NER), and sentiment analysis specifically tuned for clinical text [4]. |
| 2. Information Extraction | Apply the NLP pipeline to convert unstructured text into structured data. | Extract entities such as diagnoses, medications, and symptoms from clinical notes and insert them into structured fields in a database [4]. |
| 3. Dimensionality Reduction | Apply techniques to manage the high number of features resulting from data integration. | When integrating diverse data, the resulting matrix can be highly dimensional. Use techniques like PCA or autoencoders to create efficient abstract representations of the data, reducing complexity for downstream analysis [8] [6]. |
| 4. Workflow Automation | Script the preprocessing steps into a reproducible workflow. | Use a data processing framework (e.g., based on Snowpark or similar) to create a reusable pipeline that handles data loading, transformation, and feature extraction, reducing manual effort for subsequent studies [1]. |
Guide 3: Managing Data Integration and Computational Workflows
Problem: Data integration workflows are computationally intensive, difficult to scale, and yield inconsistent results.
Investigation & Solution:
| Step | Action | Example/Details |
|---|---|---|
| 1. Architecture Choice | Select a data integration strategy aligned with your research question. | Choose between horizontal integration (combining data from different studies measuring the same entities) and vertical integration (combining data from different omics levels) and select a corresponding strategy (early, intermediate, or late integration) [6]. |
| 2. Parallel Processing | Leverage distributed computing frameworks to handle large data volumes. | Use platforms like Snowflake or Apache Spark that support parallel processing to distribute the computational workload, significantly improving processing time for complex queries on large, semi-structured, and unstructured datasets [1] [5]. |
| 3. Provenance Tracking | Implement systems to track the origin and processing history of all data. | Maintain metadata about data sources, transformation steps, and algorithm parameters. This is crucial for reproducibility, auditability, and debugging in complex, multi-step integration pipelines [8]. |
Table 1: Comparison of Data Formats in Biomedical Research
| Aspect | Structured Data | Semi-Structured Data | Unstructured Data |
|---|---|---|---|
| Definition | Data with fixed attributes, types, and formats in a predefined schema [5]. | Data with some structure (tags, metadata) but no rigid data model [5]. | Data not in a pre-defined structure, requiring substantial preprocessing [3]. |
| Prevalence in Healthcare | Makes up a smaller proportion; ~50% of clinical trial data can be structured [2]. | Not explicitly quantified, but used in key interoperability standards. | Majority of data; estimates of 80% or more [2] [3] [4]. |
| Examples | EHR demographic fields, lab results, billing codes [1]. | FHIR resources, C-CDA documents, JSON, XML [1] [5]. | Clinical notes, medical images, pathology reports [1] [4]. |
| Ease of Analysis | Easy to search and analyze with traditional tools and SQL [1]. | Requires specific query languages (XQuery, SPARQL) or processing [1] [5]. | Requires advanced techniques (NLP, machine learning, image recognition) [1] [4]. |
| Primary Challenge | Limited view of patient context [4]. | Schema evolution, query efficiency [5]. | High volume, complexity, and preprocessing needs [3] [4]. |
Table 2: Multi-Omics Data Integration Strategies for Vertical Data [6]
| Integration Strategy | Description | Advantages | Disadvantages |
|---|---|---|---|
| Early Integration | Concatenates all datasets into a single matrix before analysis. | Simple and easy to implement. | Creates a complex, noisy, high-dimensional matrix; discounts data distribution differences. |
| Mixed Integration | Transforms each dataset separately before combining. | Reduces noise, dimensionality, and dataset heterogeneities. | Requires careful transformation. |
| Intermediate Integration | Integrates datasets simultaneously to output common and specific representations. | Captures interactions between datatypes. | Requires robust pre-processing due to data heterogeneity. |
| Late Integration | Analyzes each dataset separately and combines the final predictions. | Avoids challenges of assembling different datatypes. | Does not capture inter-omics interactions. |
| Hierarchical Integration | Incorporates prior knowledge of regulatory relationships between omics layers. | Truly embodies trans-omics analysis; reveals interactions across layers. | Nascent field; methods are often less generalizable. |
Experimental Protocols & Workflows
Protocol 1: Semantic Categorization and Merging of Clinical Data
This methodology is designed to integrate unstructured clinical data from different sources by leveraging semantic similarity [9].
Detailed Methodology:
- Data Acquisition and Sub-category Identification: Collect clinical data from multiple heterogeneous sources (e.g., public medical datasets like EURORAD, MIRC RSNA). Identify the existing sub-categories provided within these datasets, which are titles describing the information type (e.g., "History," "Diagnosis," "Imaging Findings").
- Semantic Information Extraction: For each sub-category, process the underlying unstructured text data (clinical cases) to extract semantic information. This involves using medical ontologies to identify and standardize key terms and concepts.
- Similarity Computation and Clustering: Compute the semantic similarity between all pairs of sub-categories from different datasets. Use a measure like Hausdorff distance. Employ a hierarchical clustering algorithm to group sub-categories based on their semantic similarity. A predetermined confidence threshold (e.g., empirically set based on cluster analysis) is used to determine which sub-categories are sufficiently similar.
- Cluster Merging and Schema Design: Merge the clustered sub-categories to form new, unified super-categories (e.g., merging "Findings," "Observation," and "Diagnosis" into one category). Analyze the content of the merged data elements to identify the necessary attributes. Use these attributes to design a final, integrated database schema.
Diagram Title: Workflow for Semantic Data Integration
Protocol 2: NLP-Powered Transformation of Clinical Notes
This protocol details the process of converting unstructured clinical notes into a structured, analyzable format using a standard NLP pipeline [4].
Detailed Methodology:
- Data Collection: Source raw, unstructured text from clinical narratives, such as doctors' notes, discharge summaries, or radiology reports stored in EHRs.
- NLP Preprocessing:
- Tokenization: Break the text into individual words, phrases, or sentences (tokens).
- Dependency Parsing: Analyze the grammatical structure of sentences to understand how words relate to each other, capturing context and nuance.
- Information Extraction:
- Named Entity Recognition (NER): Identify and classify relevant clinical entities within the tokenized text. This includes extracting mentions of diseases, medications, procedures, symptoms, and anatomical sites.
- Text Classification: Categorize entire documents or sections of text into predefined classes (e.g., "urgent" vs. "routine," or by medical specialty).
- Post-processing and Storage: Validate and normalize the extracted entities (e.g., mapping medication names to standard codes). Insert the structured output into designated fields in a database or EHR for further analysis, reporting, or use in clinical decision support systems.
Diagram Title: NLP Pipeline for Unstructured Text
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Heterogeneous Data Integration
| Tool / Solution | Function | Application Context |
|---|---|---|
| OMOP Common Data Model (CDM) | A standardized data model that allows for the systematic analysis of disparate observational databases by transforming data into a common format [1]. | Enables large-scale analytics across multiple institutions and structured EHR data. |
| FHIR (Fast Healthcare Interoperability Resources) | A standard for exchanging healthcare information electronically using RESTful APIs and resources in JSON or XML format [1] [8]. | Facilitates the exchange of semi-structured data between EHRs, medical devices, and research applications. |
| NLP Libraries (e.g., CLAMP, cTAKES) | Software toolkits with pre-trained models for processing clinical text. Perform tasks like tokenization, NER, and concept mapping [4]. | Essential for extracting structured information from unstructured clinical notes and reports. |
| Snowflake / Distributed Computing Platforms | A cloud data platform that supports processing and analyzing structured and semi-structured data (JSON, XML) at scale, leveraging parallel computing [1]. | Handles large-volume data integration and transformation workloads, including for healthcare interoperability standards. |
| i2b2 (Informatics for Integrating Biology & the Bedside) | An open-source analytics platform designed to create and query integrated clinical data repositories for translational research [8]. | Used for cohort discovery and data integration in clinical research networks. |
| HYFTs Framework (MindWalk) | A proprietary framework that tokenizes biological sequences into a common data language, enabling one-click normalization and integration of multi-omics data [6]. | Aims to simplify the integration of heterogeneous public and proprietary omics data for researchers. |
Understanding Core Data Structures and Integration Types
What is the fundamental difference between horizontal and vertical data integration?
The terms "horizontal" and "vertical" describe how multi-omics datasets are organized and integrated, corresponding to the complexity and heterogeneity of the data [6].
Horizontal integration (also called homogeneous integration) involves combining data from across different studies, cohorts, or labs that measure the same omics entities [6]. For example, combining gene expression data from multiple independent studies on the same disease [10] [11]. This approach typically deals with data generated from one or two technologies for a specific research question across a diverse population, representing a high degree of real-world biological and technical heterogeneity [6].
Vertical integration (also called heterogeneous integration) involves analyzing multiple types of omics data collected from the same subjects [12] [11]. This includes data generated using multiple technologies probing different aspects of the research question, traversing various omics layers including genome, metabolome, transcriptome, epigenome, proteome, and microbiome [6]. A typical example would be collectively analyzing gene expression data along with their regulators (such as mutations, DNA methylation, and miRNAs) from the same patient cohort [11].
Table: Comparison of Horizontal vs. Vertical Integration Approaches
| Feature | Horizontal Integration | Vertical Integration |
|---|---|---|
| Data Source | Multiple studies/cohorts measuring same variables [6] | Multiple omics layers from same subjects [12] |
| Primary Goal | Increase sample size, validate findings across populations [13] | Understand regulatory relationships across molecular layers [12] |
| Data Heterogeneity | Technical and biological variation across cohorts [6] | Different omics modalities with distinct distributions [6] |
| Complexity | Cohort coordination, data harmonization [13] | Computational integration of diverse data types [12] |
| Typical Methods | Meta-analysis, cross-study validation [10] | Multi-omics factor analysis, similarity network fusion [12] |
What are the main technical challenges researchers face with each integration type?
Horizontal Integration Challenges:
- Data harmonization complexity: Different cohorts often use varied data capture methods, representations, and documentation standards, requiring extensive manual alignment of equivalent variables across studies [7].
- Administrative hurdles: Multi-cohort projects involve complicated management with many administrative obstacles, including obtaining relevant permits and ethics approvals from multiple governing bodies [13].
- Cohort heterogeneity: Different cohorts have specific purposes, focus areas, policies, and established methods of managing, collecting, and sharing data [13].
Vertical Integration Challenges:
- Data heterogeneity: Integrating completely different data distributions and types that require unique scaling, normalization, and transformation [6].
- High-dimension low sample size (HDLSS): Variables significantly outnumber samples, causing machine learning algorithms to overfit and decrease generalizability [6].
- Missing values: Omics datasets often contain missing values that hamper downstream integrative analyses, requiring additional imputation processes [6].
- Regulatory relationships: Effective integration must account for regulatory relationships between different omics layers to accurately reflect multidimensional data nature [6].
Integration Methodologies and Experimental Protocols
What methodologies are available for vertical integration of multi-omics data?
Five distinct integration strategies have been defined for vertical data integration in machine learning analysis [6]:
Table: Vertical Data Integration Strategies for Multi-Omics Analysis
| Strategy | Description | Advantages | Limitations |
|---|---|---|---|
| Early Integration | Concatenates all omics datasets into single matrix [6] | Simple implementation [6] | Creates complex, noisy, high-dimensional matrix; discounts dataset size differences [6] |
| Mixed Integration | Separately transforms each dataset then combines [6] | Reduces noise, dimensionality, and heterogeneities [6] | Requires careful transformation selection [6] |
| Intermediate Integration | Simultaneously integrates datasets to output multiple representations [6] | Creates common and omics-specific representations [6] | Requires robust pre-processing for data heterogeneity [6] |
| Late Integration | Analyzes each omics separately then combines predictions [6] | Circumvents challenges of assembling different datasets [6] | Does not capture inter-omics interactions [6] |
| Hierarchical Integration | Includes prior regulatory relationships between omics layers [6] | Embodies true trans-omics analysis intent [6] | Most methods focus on specific omics types, limiting generalizability [6] |
Can you provide a specific experimental workflow for integrative analysis?
The miodin R package provides a streamlined workflow-based syntax for multi-omics data analysis that can be adapted for both horizontal and vertical integration [12]. Below is a generalized workflow diagram for integrative analysis:
Detailed Workflow Steps:
Study Design Declaration: Use expressive vocabulary to declare all study design information, including samples, assays, experimental variables, sample groups, and statistical comparisons of interest [12]. The
MiodinStudyclass facilitates this through helper functions likestudySamplingPoints,studyFactor,studyGroup, andstudyContrast[12].Data Import and Validation: Import multi-omics data from different modalities (transcriptomics, genomics, epigenomics, proteomics) and experimental techniques (microarrays, sequencing, mass spectrometry) [12]. Automatically validate sample and assay tables against the declared study design to detect potential clerical errors [12].
Data Pre-processing: Address dataset-specific requirements including missing value imputation, normalization, scaling, and transformation to account for technical variations across platforms and batches [6].
Quality Control: Perform modality-specific quality control checks to identify outliers, technical artifacts, and data quality issues that might affect downstream integration and analysis.
Data Integration: Apply appropriate integration strategies (early, mixed, intermediate, late, or hierarchical) based on the research question and data characteristics [6]. Methods like Multi-Omics Factor Analysis (MOFA), similarity network fusion, or penalized clustering can be employed [12].
Statistical Analysis: Conduct both unsupervised (clustering, dimension reduction) and supervised (differential analysis, predictive modeling) analyses to extract biologically meaningful patterns [12] [11].
Biological Interpretation: Interpret results in context of existing biological knowledge, pathways, and regulatory networks to generate actionable insights into health and disease mechanisms [12].
Troubleshooting Common Integration Problems
How can researchers address missing data in multi-omics datasets?
Missing values are a common challenge in omics datasets that can hamper downstream integrative analyses [6]. Implementation strategies include:
- Imputation methods: Apply appropriate imputation techniques (mean/mode, k-nearest neighbors, matrix completion) to infer missing values before statistical analysis [6].
- Missing data mechanisms: Assess whether data is missing completely at random (MCAR), missing at random (MAR), or missing not at random (MNAR) to select appropriate handling methods.
- Algorithm selection: Choose integration methods that can handle missing data natively, such as MOFA, which can accommodate missing values across different omics modalities [12].
What strategies help manage the high-dimension low sample size (HDLSS) problem?
When variables significantly outnumber samples, machine learning algorithms tend to overfit, decreasing generalizability to new data [6]. Addressing strategies include:
- Dimension reduction: Apply principal component analysis, sparse PCA, or other dimension reduction techniques to reduce variable space while preserving biological signal [10].
- Feature selection: Use prior biological knowledge to prescreen genes or features [10]. For mental disorders analysis, focusing on relevant signaling pathways (ubiquitin-mediated proteolysis, tryptophan metabolism, neurotrophin signaling) has proven effective [10].
- Regularization methods: Employ penalized regression and regularization techniques (lasso, ridge, elastic net) that constrain model complexity to prevent overfitting [10].
How can researchers effectively coordinate multi-cohort studies?
Multi-cohort projects present significant administrative and coordination challenges [13]. The PGX-link project demonstrated a 6-step approach:
Key coordination strategies:
- Early engagement: Involve cohort collaborators during grant writing, not after funding approval, to ensure scientific questions are feasible and clearly defined [13].
- Unified protocols: Establish common data standards, collection methods, and sharing policies across cohorts to facilitate interoperability [13] [7].
- Realistic timelines: Allocate sufficient time (potentially up to one year) for the preparation phase involving ethics approvals, scientific board reviews, and administrative setup [13].
- Clear communication channels: Establish regular communication protocols between cohort representatives to address challenges and maintain project momentum [13].
What software tools are available for integrative multi-omics analysis?
Table: Key Software Tools for Multi-Omics Data Integration
| Tool/Platform | Functionality | Integration Type | Key Features |
|---|---|---|---|
| miodin R package [12] | Workflow-based multi-omics analysis | Vertical & Horizontal | Streamlined syntax, study design vocabulary, Bioconductor interoperability |
| MOFA [12] | Multi-Omics Factor Analysis | Vertical | Unsupervised integration, handles missing data, generalization of PCA |
| mixOmics [12] | Multivariate analysis | Vertical | PLS, CCA, generalization to multi-block data |
| Similarity Network Fusion [12] | Patient similarity networks | Vertical | Constructs fused multi-omics patient networks for clustering |
| MindWalk HYFT [6] | Biological data tokenization | Both | One-click normalization using HYFT framework |
What analytical techniques support horizontal integration of related disorders?
Horizontal integration of related mental disorders (e.g., bipolar disorder and schizophrenia) employs advanced statistical techniques [10]:
- Sparse principal component analysis: Identifies latent components that explain covariation patterns across disorders while selecting relevant features [10].
- Penalized regression methods: Incorporates regularization to identify robust biomarkers and patterns that generalize across related conditions [10].
- Pathway-based prescreening: Focuses analysis on biologically relevant signaling pathways (ubiquitin-mediated proteolysis, tryptophan metabolism, neurotrophin signaling) to improve reliability and reduce computational cost when sample size is limited [10].
The experimental protocol for such analysis involves:
- Data acquisition from repositories like Stanley Medical Research Institute Online Genomics Database
- Prescreening of genes based on prior biological knowledge from KEGG pathways
- Data matching across disorders and omics modalities
- Application of sparse modeling and regularization techniques
- Validation of findings through resampling and biological interpretation [10]
Implementation FAQs
When should researchers choose horizontal versus vertical integration?
Choose horizontal integration when:
- Your research question requires larger sample sizes than a single cohort can provide [13]
- You need to validate findings across diverse populations or study designs [10]
- You are investigating related disorders or conditions with potential shared mechanisms [10]
Choose vertical integration when:
- You want to understand regulatory relationships across different molecular layers [12] [11]
- Your research focuses on complex mechanisms that span multiple biological levels [12]
- You need to identify biomarkers or signatures that incorporate multiple types of omic measurements [11]
How can researchers assess the quality of integrated analysis results?
Quality assessment strategies include:
- Biological validation: Verify that findings align with established biological knowledge and pathways [10]
- Method consistency: Compare results across different integration methods and parameters to identify robust patterns [6]
- Predictive performance: Evaluate whether integrated models improve prediction accuracy compared to single-omics approaches [11]
- Reproducibility: Ensure analyses are reproducible through workflow tools like Nextflow and container technology like Docker [12]
What standards facilitate more effective data integration?
Implementation of standards is crucial for reducing integration challenges:
- Data standards: Use common data elements, ontologies, and formats during data collection to facilitate future integration [7]
- Metadata documentation: Comprehensively document sample processing, experimental conditions, and data transformations [7]
- Sharing policies: Establish clear data sharing agreements and access policies during project initiation [13]
- Workflow transparency: Use tools that promote transparent data analysis and reduce technical expertise requirements [12]
FAQs on Data Heterogeneity
What are the main types of heterogeneity in multi-database studies? In multi-database studies, statistical heterogeneity arises from two primary sources: methodological diversity and true clinical variation. Methodological diversity includes differences in study design, database selection, variable measurement, and analysis methods, which can introduce varying degrees of bias to a study's internal validity. In contrast, true clinical variation reflects genuine differences in population characteristics and healthcare system features across different countries or settings, meaning the exposure-outcome association truly differs between populations [14].
How can I systematically investigate sources of heterogeneity in my study? A structured framework can be used to explore heterogeneity systematically [14]:
- Conceptualize the Heterogeneity: Distinguish whether observed differences are due to methodological diversity or true clinical variation.
- Explore Methodological Diversity: Use a checklist to compare differences in eligibility criteria, database structures, coding practices, confounder adjustment, and outcome ascertainment across study sites.
- Generate Hypotheses on True Variation: After accounting for methodological differences, remaining heterogeneity may be attributed to genuine variations in patient populations, clinical practices, or healthcare systems.
What is an example of how data source structure creates heterogeneity? The intended purpose and structure of a database directly influence the data it contains and can introduce significant heterogeneity [15]:
- Spontaneous Reporting Systems (e.g., FAERS): Rely on voluntary reports, which can lead to underreporting or overreporting of specific events, influenced by factors like media attention or how long a drug has been on the market.
- Electronic Health Records (EHRs): Designed for clinical care, not research. Data can be incomplete due to patients moving between health systems, and medication use (especially over-the-counter) is often inconsistently documented.
- Claims Databases: Contain structured billing data across providers but often lose patients to follow-up when they change insurance providers.
The table below summarizes the impact of different database purposes and structures.
| Database Type | Primary Purpose | Key Structural Limitations Introducing Heterogeneity |
|---|---|---|
| Spontaneous Reporting Systems (e.g., FAERS) | Collect voluntary adverse event reports | Underreporting/overreporting; reporting bias; variable data quality [15] |
| Electronic Health Records (EHR) | Patient care delivery & administration | Inconsistent medication/adherence data; loss to follow-up between systems; unstructured clinical notes [15] |
| Claims Data | Insurance & billing processing | Loss to follow-up with insurer changes; contains only coded billing information [15] |
Troubleshooting Guide: Data Heterogeneity
Challenge: Schema and format variations across data sources.
Different sources often use different schemas and formats, making it difficult to map fields consistently. For example, a field might be named user_id in one source and userId in another, or dates might be stored as strings in a CSV file but as datetime objects in a SQL database [16].
- Solution: Use automated ETL (Extract, Transform, Load) frameworks or schema mapping tools to transform data into a common structure. Implement careful manual oversight to handle edge cases and ensure alignment [16].
Challenge: Integrating data from disparate systems. Combining data from relational databases, NoSQL stores, and flat files introduces integration hurdles. For instance, merging relational customer data with semi-structured application logs requires resolving different data models. Differences in time zones or date formats further complicate this process [16].
- Solution: Develop robust transformation logic that accounts for discrepancies like time zones and units. For real-time data integration, implement buffering or windowing strategies to align streaming data with batch reports [16].
Challenge: Varying data quality and consistency. Heterogeneous sources often have different data quality standards, leading to missing values, duplicates, or conflicting entries (e.g., a patient's age differing between sources) [16].
- Solution: Establish validation pipelines with defined rules for anomaly detection. For regulated data, incorporate anonymization or filtering steps to comply with standards like HIPAA or GDPR during the extraction process [16].
FAQs on Missing Data
What are the different mechanisms of missing data? Missing data can be categorized into three mechanisms [17]:
- Missing Completely at Random (MCAR): The probability of data being missing is unrelated to any observed or unobserved variables.
- Missing at Random (MAR): The probability of data being missing may depend on observed variables but not on the unobserved missing data itself.
- Missing Not at Random (MNAR): The probability of data being missing depends on the unobserved missing values themselves.
When is a complete-case analysis valid? A complete-case analysis (excluding subjects with any missing data) can be valid only when the data is Missing Completely at Random (MCAR). In some specific situations, it may also be valid for data that is Missing at Random (MAR), but in most real-world research scenarios, this approach leads to biased estimates and reduced statistical power [17]. Its use should be justified with great caution.
What is the recommended approach for handling missing data? Multiple Imputation (MI) is a widely recommended and robust approach for handling missing data, particularly when the Missing at Random (MAR) assumption is reasonable. With MI, multiple plausible values are imputed for each missing datum, creating several complete datasets. The desired statistical analysis is performed on each dataset, and the results are pooled, accounting for the uncertainty introduced by the imputation process [18] [19]. It is highly advised over single imputation methods like mean imputation [17].
Troubleshooting Guide: Missing Data with Multiple Imputation
Protocol: Implementing Multiple Imputation This protocol outlines the key steps for performing Multiple Imputation, using the example of developing a model to predict 1-year mortality in patients hospitalized with heart failure [18] [19].
- Step 1: Develop the Imputation Model. Decide on the variables to include in the imputation model. It is good practice to include all variables that will be used in the final analysis, as well as auxiliary variables that are related to the missingness or the missing values themselves [18].
- Step 2: Create Multiple Imputed Datasets. Generate
Mcompleted datasets (common choices forMrange from 5 to 20, or higher depending on the fraction of missing information). This reflects the uncertainty about the imputed values [18] [19]. - Step 3: Perform Statistical Analysis. Run the same statistical model (e.g., a logistic regression for 1-year mortality) separately on each of the
Mimputed datasets [18]. - Step 4: Pool the Results. Combine the parameter estimates (e.g., regression coefficients) and their standard errors from the
Manalyses into a single set of results using Rubin's rules. These rules account for both the within-imputation variance and the between-imputation variance, producing valid confidence intervals [18] [19].
FAQs on High-Dimension Low Sample Size (HDLSS)
What defines an HDLSS problem?
HDLSS, or "High-Dimension Low Sample Size," refers to datasets where the number of features or variables (p) is vastly larger than the number of available samples or observations (n). This imbalance is common in fields like genomics, proteomics, and medical imaging, where a study might involve expression levels of tens of thousands of genes from only a few dozen patients [20].
What are the primary challenges when working with HDLSS data? HDLSS data presents several key challenges [20]:
- Overfitting: Models can fit the training data perfectly but fail to generalize to new, unseen data because they learn noise and spurious patterns specific to the small sample.
- Curse of Dimensionality: In high-dimensional spaces, traditional distance-based measures become less meaningful, and data points can appear equally distant from each other, weakening algorithms that rely on these measures.
- Feature Selection and Statistical Significance: It is difficult to identify which features are truly relevant, and achieving statistical significance is harder due to the small sample size relative to the vast number of tests performed.
Are there specific machine learning techniques for HDLSS classification? Yes, specialized methods have been developed. For example, one state-of-the-art approach involves using a Random Forest Kernel with Support Vector Machines (RFSVM). This method uses the similarity measure learned by a Random Forest as a precomputed kernel for an SVM. This learned kernel is particularly suited for capturing complex relationships in HDLSS data and has been shown to outperform other methods on many HDLSS problems [21].
Troubleshooting Guide: The HDLSS Problem
Challenge: Model overfitting and poor generalizability. With thousands of variables and only a small sample, models are prone to overfitting [20].
- Solution: Employ regularization techniques like Lasso (L1) or Ridge (L2) regression, which penalize model complexity. Dimensionality reduction methods like Principal Component Analysis (PCA) can project data into a lower-dimensional space. Cross-validation and bootstrapping are essential for validating model performance and assessing generalizability [20].
Challenge: Identifying meaningful features among thousands. Many variables in an HDLSS dataset may be irrelevant or redundant [20].
- Solution: Use feature selection algorithms to narrow down the variable set. In genomics, this can involve focusing on biologically relevant pathways. Regularized models like Lasso inherently perform feature selection by driving some coefficients to zero. Combining domain knowledge with algorithmic selection is often the most effective strategy [20].
Strategy: Improve generalizability by embracing cohort heterogeneity. Models trained on a single, homogeneous cohort may not perform well in new settings due to population or operational heterogeneity [22].
- Solution: Train models on data from multiple cohorts. While this introduces more heterogeneity into the training data, it dilutes cohort-specific patterns and helps the model learn more general, disease-specific predictors. This approach has been shown to produce models with better external performance than models trained on the same amount of data from a single cohort [22]. Note that model calibration should be carefully checked after training on mixed cohorts.
The Scientist's Toolkit: Research Reagent Solutions
| Tool / Method | Function | Application Context |
|---|---|---|
| Multiple Imputation | A statistical technique that handles missing data by creating multiple plausible datasets, analyzing them separately, and pooling results. | Handling missing data in clinical research datasets under the MAR assumption [18] [17]. |
| Regularization (L1/Lasso, L2/Ridge) | Prevents overfitting in high-dimensional models by adding a penalty term to the model's loss function, shrinking coefficient estimates. | Building predictive models with HDLSS data to improve generalizability [20]. |
| Dimensionality Reduction (PCA, t-SNE) | Reduces the number of random variables under consideration by obtaining a set of principal components or low-dimensional embeddings. | Visualizing and pre-processing HDLSS data (e.g., genomic, proteomic) for analysis [20]. |
| Random Forest Kernel (RFSVM) | A learned similarity measure from a Random Forest used as a kernel in a Support Vector Machine, designed for complex, high-dimensional data. | HDLSS classification tasks where traditional algorithms fail [21]. |
| Heterogeneity Assessment Checklist | A systematic tool for identifying differences in study design, data source, and analysis that may contribute to variation in results. | Planning and interpreting multi-database or multi-cohort studies [14]. |
| Cross-Validation / Bootstrapping | Resampling techniques used to assess how the results of a statistical model will generalize to an independent dataset and to estimate its accuracy. | Model validation and selection, especially in HDLSS contexts to avoid overfitting [20]. |
FAQs and Troubleshooting Guides
What are variable encoding differences and how do they disrupt my multi-cohort analysis?
Variable encoding differences occur when the same conceptual data is represented using different formats, structures, or coding schemes across various cohort studies. This creates significant semantic barriers that can disrupt integrated analysis.
Problem Example: In a harmonization project between the LIFE (Jamaica) and CAP3 (United States) cohorts, researchers encountered variables collecting the same data but with different coding formats [23]. For instance, a "smoking status" variable might be coded as:
- Study A:
0=Non-smoker,1=Current smoker,2=Former smoker - Study B:
1=Never,2=Past,3=Present
Impact: If merged directly, these encoding differences would misclassify participants, leading to incorrect prevalence estimates and flawed statistical conclusions about smoking-related health risks.
Troubleshooting Protocol:
- Create a Data Dictionary Map: Document all variable encodings from each source study.
- Define a Common Model: Establish a unified coding scheme for the integrated dataset.
- Develop a Mapping Table: Implement a transformation logic to convert all source values to the common model. The LIFE-CAP3 project used a user-defined mapping table for this recoding process [23].
Table: Example Mapping Table for Smoking Status Variable
| Source Study | Source Code | Source Label | Target Code | Target Label |
|---|---|---|---|---|
| Study A | 0 | Non-smoker | 1 | Never |
| Study B | 1 | Never | 1 | Never |
| Study A | 2 | Former smoker | 2 | Past |
| Study B | 2 | Past | 2 | Past |
| Study A | 1 | Current smoker | 3 | Present |
| Study B | 3 | Present | 3 | Present |
What is schema drift and how can I prevent it from invalidating my research results?
Schema drift refers to unexpected or unintentional changes to the structure of a database—such as adding, removing, or modifying tables, columns, or data types—that create inconsistencies across different environments or over time [24].
Problem Example: A new column like "Patient Type" is added to a production database to support a new business need but is not replicated in the development or testing environments. Applications or researchers expecting the old schema structure will encounter failures or corrupted data [24].
Impact: Schema drift can lead to data integrity issues, application downtime, increased maintenance costs, and compliance or security concerns [24].
Troubleshooting Protocol:
- Detection: Use automated schema monitoring and comparison tools to track changes and alert teams to unexpected modifications [24].
- Version Control: Implement version control for database schemas, similar to software code, to track and synchronize changes across environments [24].
- Automated Validation: Incorporate schema validation into continuous integration/continuous delivery (CI/CD) pipelines to detect drift early [24].
- Regular Audits: Perform routine audits of database schemas to identify and address drift before it causes operational problems [24].
Table: Common Causes and Impacts of Schema Drift
| Cause of Schema Drift | Potential Impact on Research | Prevention Strategy |
|---|---|---|
| Evolving business requirements (e.g., new variables) | Incomplete data, failed analyses | Comprehensive documentation and communication |
| Multiple development teams working independently | Inconsistent data models, pipeline failures | Version control systems (e.g., Git) |
| Frequent updates to production databases | Mismatch between development and production data | Automated testing and CI/CD pipelines |
| Changes in external data sources or APIs (Source Schema Drift) [24] | Disrupted data pipelines, analytics errors | Proactive monitoring of source systems |
What is the step-by-step methodology for prospectively harmonizing active cohort studies?
Prospective harmonization occurs before or during data collection and is a powerful strategy for reducing future integration costs. The established ETL (Extract, Transform, Load) process provides a structured framework [23].
Experimental Protocol: The LIFE and CAP3 harmonization project followed this methodology [23]:
Extract
- Objective: Collect raw data from source cohort studies.
- Action: Use secure Application Programming Interfaces (APIs) to routinely download data from each study's data management platform (e.g., REDCap). Automate this process with server-side jobs.
Transform
- Objective: Convert and map source variables to a common, unified structure.
- Action:
- Variable Mapping: Identify shared data elements across studies. Create a mapping table that defines the relationship between each source variable and its corresponding target variable in the integrated dataset [23].
- Recoding: Apply logic to handle different data types and coding schemes, using the mapping table to recode values for consistency [23].
- Data Cleaning: Address missing values and ensure data quality.
Load
- Objective: Insert the transformed data into a single, integrated database.
- Action: Upload the harmonized data to a central project. Implement automated, weekly cycles to keep the integrated database synchronized with source studies [23].
Quality Assurance: Conduct routine quality checks. Pull a random sample from the integrated database and cross-check it against the source data. Correct any errors at the source to maintain integrity [23].
How do I manage the integration of highly heterogeneous data (structured, semi-structured, unstructured)?
Integrating heterogeneous data—which includes structured tables, semi-structured JSON/XML, and unstructured text or images—requires a robust architectural approach to handle varying formats, structures, and semantics [25].
Problem Example: A multi-omics study might need to combine structured clinical data (e.g., from a REDCap database), semi-structured genomic annotations (e.g., in JSON format), and unstructured text from pathology reports [6].
Troubleshooting Protocol:
- Unified Ingestion Layer: Use tools that can collect, process, and deliver diverse data types from various sources, supporting both batch and real-time ingestion patterns [25].
- Transformation and Normalization Engines: Apply specialized processing for different data types. This includes scaling, normalization, encoding categorical data, and preprocessing text or images to make them suitable for analysis [25].
- Centralized Metadata Management: Produce standardized metadata from all sources. Use common standards and tools to create an integrated, accessible metadata system that improves data governance and simplifies querying [25].
- Unified Storage Abstraction: Implement a software layer that provides a standard interface for interacting with diverse underlying storage systems, simplifying development and enabling centralized management [25].
Table: Components of a Heterogeneous Data Architecture
| Architectural Layer | Function | Example Tools/Techniques |
|---|---|---|
| Ingestion Layer | Collects mixed-format data from diverse sources | Hybrid patterns (batch/real-time), Schema-on-read |
| Transformation Engine | Prepares raw data for analysis; handles scaling, encoding, etc. | Min-max scaling, Z-score standardization, NLP for text |
| Metadata Management | Creates standardized, integrated metadata for governance | Metadata management tools, Semantic annotations (DCAT-AP, ISO19115) |
| Storage Abstraction | Provides a unified interface to access different storage systems | Data lake architectures, Pluggable frameworks |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Tools for Heterogeneous Data Integration
| Tool / Solution | Function | Application Context |
|---|---|---|
| REDCap API [23] | Enables secure, automated data extraction and exchange from the REDCap platform. | Extracting data from multiple clinical cohort studies for central pooling. |
| Schema Migration Tools (e.g., Flyway, Liquibase) [24] | Automate and version-control the application of schema changes across environments. | Preventing schema drift by ensuring consistent database structures in development, testing, and production. |
| Mapping Tables | User-defined tables that define the logic for recoding variables from a source format to a target format [23]. | Resolving variable encoding differences during the "Transform" stage of the ETL process. |
| Data Observability Platform (e.g., Acceldata) [24] | Monitors pipeline health, automatically detects schema changes, data quality errors, and data source changes. | Providing end-to-end visibility into data health, crucial for managing complex, multi-source pipelines. |
| HYFTs Framework (MindWalk Platform) [6] | Tokenizes all biological data (sequences, text) into a common set of building blocks ("HYFTs"). | Enabling one-click normalization and integration of highly heterogeneous multi-omics and non-omics data. |
Frequently Asked Questions (FAQs)
Q1: What are the most critical data privacy regulations affecting multi-cohort studies in 2025? A complex maze of global regulations now exists. The EU's GDPR remains foundational, while in the US, researchers must comply with a patchwork of laws including the California Consumer Privacy Act (CCPA), Texas Data Privacy and Security Act (TDPSA), and the health-specific HIPAA [26]. Brazil's LGPD and India's Personal Data Protection Bill also impact international studies. Non-compliance can lead to fines and loss of consumer trust, with data breach costs averaging $10.22 million in the US as of 2025 [27].
Q2: How can we handle Data Subject Access Requests (DSARs) efficiently across pooled datasets? Regulations like GDPR and CCPA give individuals rights to access, rectify, or erase their data. To manage these requests, you need deep visibility into your data landscape. Implement processes and tools for comprehensive data mapping and inventory to quickly identify, retrieve, and modify personal data across all source systems and storage locations [26]. A centralized data catalog can be instrumental in streamlining the DSAR process.
Q3: Our data sources have different variable encodings for the same concept. How can we harmonize them? This is a common challenge in heterogeneous data integration. One robust solution is to use an automated harmonization algorithm like SONAR (Semantic and Distribution-Based Harmonization). This method uses machine learning to create embedding vectors for each variable by learning from both variable descriptions (semantic learning) and the underlying participant data (distribution learning), achieving accurate concept-level matching across cohorts [28].
Q4: What is the best way to structure a data integration workflow for active, ongoing cohort studies? A prospective harmonization approach, using a structured ETL (Extract, Transform, Load) process, is highly effective. This involves mapping variables across projects before or during data collection. A proven method is to use a platform like REDCap, which supports APIs for automated data pooling. Researchers create a mapping table to direct the integration, and a custom application can routinely download and upload data from all studies into a single, integrated project on a scheduled basis [23].
Q5: How can we prevent costly mistakes when scaling our data integration architecture? Avoid three common strategic errors: 1) Betting everything on cloud-only tools in a hybrid reality, which can create compliance risks and visibility gaps; 2) Treating scale and performance as future problems, which causes latency and failed data jobs under AI workloads; and 3) Locking your future to today's architecture with vendor-specific APIs, which leads to costly "migration tax" later. The solution is to plan for hybrid, elastic, and portable data integration from the start [29].
Troubleshooting Guides
Issue 1: Data Silos and Incompatible Systems
Problem: Data is trapped in a patchwork of legacy systems, modern cloud tools, and niche applications, preventing a unified view.
Solution:
- Action 1: Adopt a flexible integration platform with pre-built connectors for common applications (e.g., CRMs, ERPs) to reduce integration time [30].
- Action 2: Implement a data fabric architecture, which acts as a unified framework for managing and integrating different data types across various systems, simplifying access and sharing [30].
- Action 3: For semantic inconsistencies, use an ontology-based data integration approach. This provides a joint knowledge base that acts as a common reference point, solving heterogeneity at the semantic level [31].
Issue 2: Poor Data Quality and Integrity
Problem: Integrated data is inconsistent, inaccurate, or contains duplicates, undermining trust in analytics.
Solution:
- Action 1: Use AI-driven validation and cleansing tools to automate data quality assurance. These tools can be built into your integration platform to ensure integrity throughout the data pipeline [30].
- Action 2: Implement a Data Quality Management System to proactively validate data at the point of entry, preventing bad data from contaminating systems [32].
- Action 3: Track data lineage to trace where duplicates or errors originate. Encourage a culture of collaboration where teams share updates openly to prevent redundant records [32].
Issue 3: Real-Time Data Integration Failures
Problem: Batch processing is too slow for time-sensitive decisions in fields like finance or healthcare, leading to missed opportunities.
Solution:
- Action 1: Build event-driven architectures that trigger integration workflows the moment new data arrives [32].
- Action 2: Use stream processing technologies like Apache Kafka for real-time data handling and continuous ingestion [32].
- Action 3: Ensure your integration platform supports real-time data streaming and synchronization to keep critical systems updated instantly [30].
Issue 4: Managing Data Privacy and Security During Integration
Problem: Sensitive data is exposed during integration, creating compliance risks and vulnerability to breaches.
Solution:
- Action 1: Embed compliance protocols directly into data integration workflows. This includes using encryption (for data in transit and at rest), role-based access controls, and maintaining detailed audit trails [30].
- Action 2: Develop a Data Compliance Framework with core components like data mapping/inventory, risk management tools, and monitoring processes. This framework ensures personal data is handled responsibly per legal requirements [26].
- Action 3: For AI-driven projects, prioritize transparency in how models use personal data and implement safeguards against bias to prepare for upcoming AI-specific regulations [26].
Table 1: Key Global Data Privacy Regulations (2025)
| Regulation/Region | Scope & Key Requirements | Potential Fines & Penalties |
|---|---|---|
| GDPR (EU) | Protects personal data of EU citizens; mandates rights to access, erasure, and data portability. | Up to €20 million or 4% of global annual turnover [26]. |
| US State Laws (CCPA, TDPSA, etc.) | A patchwork of laws granting consumers rights over their personal data; requirements vary by state. | Significant financial penalties; brand damage and loss of customer trust [26]. |
| HIPAA (US) | Safeguards protected health information (PHI) for covered entities and business associates. | Civil penalties up to $1.5 million per violation per year [26]. |
Table 2: Data Integration Strategies for Multi-Cohort Studies
| Integration Strategy | Description | Best Used For |
|---|---|---|
| Prospective Harmonization | Variables are mapped and standardized before or during data collection [23]. | Active, ongoing cohort studies where data collection instruments can be aligned. |
| Retrospective Harmonization | Data is integrated after collection from completed or independent studies [23]. | Leveraging existing datasets where the study design cannot be changed. |
| ETL (Extract, Transform, Load) | Data is extracted from sources, transformed into a unified format, and loaded into a target system [31]. | Creating a physically integrated, analysis-ready dataset (e.g., a data warehouse). |
| Virtual/Federated Integration | A mediator layer allows querying of disparate sources without physical data consolidation [31]. | Scenarios requiring real-time data from source systems with minimal storage costs. |
| SONAR (Automated Harmonization) | An ensemble ML method that uses semantic and distribution learning to match variables across cohorts [28]. | Large-scale studies with numerous variables where manual curation is infeasible. |
Experimental Protocols & Workflows
Protocol 1: Prospective Data Harmonization for Active Cohorts
This protocol is based on a successful implementation integrating cohort studies in Jamaica and the United States [23].
- Variable Mapping: Hold working group sessions with epidemiologists, domain experts, and research assistants to identify shared data elements. Group items into domains (e.g., demographics, medical history).
- Create Mapping Table: Develop a mapping table (e.g., within a REDCap project) that links source variables from each cohort to a common destination variable. Include metadata for recoding values if data types differ.
- Automate ETL Process: Develop a custom application (e.g., in Java) that uses APIs (like REDCap's API) to routinely download data from all cohort studies.
- Transform and Load: The application uses the mapping table to recode and transform the data, then uploads it to a central, integrated project on a scheduled basis (e.g., weekly).
- Quality Assurance: Implement routine checks. Pull a random sample from the integrated database weekly and cross-check it against the source data. Correct any errors at the source.
Protocol 2: Automated Variable Harmonization Using SONAR
This protocol uses the SONAR method for accurate variable matching within and between cohort studies [28].
- Data Extraction: Gather variable documentation (name, description, accession ID) and patient-level data from all cohort studies (e.g., from dbGaP).
- Preprocessing: Filter for the data type of interest (e.g., continuous variables). Remove temporal information (e.g., "at baseline," "visit 2") from variable descriptions to focus on the core concept.
- Model Training: Apply the SONAR algorithm, which learns an embedding vector for each variable by combining:
- Semantic Learning: Infers meaning from the variable description strings.
- Distribution Learning: Analyzes the underlying patient-level data patterns for each variable.
- Similarity Scoring: Calculate pairwise cosine similarity scores between all variable embeddings to identify matches.
- Validation: Evaluate harmonization performance against a manually curated gold standard using metrics like area under the curve (AUC) and top-k accuracy.
Workflow Diagrams
Diagram 1: Prospective Harmonization & ETL Workflow
Prospective Harmonization ETL Flow
Diagram 2: Data Privacy & Security Compliance Framework
Data Privacy Compliance Framework
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Solutions for Data Integration and Privacy
| Tool / Solution | Function / Purpose |
|---|---|
| REDCap (Research Electronic Data Capture) | A secure, HIPAA-compliant web application for building and managing data collection surveys and databases; its APIs enable automated data pooling for harmonization [23]. |
| Data Catalog | A centralized tool that provides a view of all data sources, storage locations, and lineage. Essential for tagging, mapping, and governing data for specific regulatory requirements (e.g., DSARs) [26]. |
| Data Fabric Architecture | A unified framework that connects structured and unstructured data from diverse sources, simplifying access, sharing, and management of complex datasets across the organization [30]. |
| Encryption & Role-Based Access Controls (RBAC) | Security measures to protect data in transit and at rest (encryption) and to restrict data access to authorized users based on their role (RBAC) [32] [30]. |
| AI-Driven Data Validation & Cleansing Tools | Automated tools that identify and correct data quality issues (e.g., duplicates, inaccuracies) within integration pipelines, ensuring the reliability of pooled data [30]. |
| SONAR Algorithm | An ensemble machine learning method for automated variable harmonization across cohorts, using both semantic (descriptions) and distribution (patient data) learning [28]. |
Building Robust Integration Pipelines: Methodologies and Real-World Applications
Troubleshooting Guide: Common ETL Harmonization Challenges
Data Mapping and Variable Alignment
| Challenge | Symptom | Solution | Prevention |
|---|---|---|---|
| Semantic Heterogeneity | Same variable names measure different concepts (e.g., different age ranges for "young adults") [33] | Create detailed data dictionaries; implement crosswalk tables for value recoding [23] | Prospective: Establish common ontologies during study design [34] |
| Structural Incompatibility | Dataset formats conflict (event data vs. panel data); routing errors during integration [33] | Use intermediate transformation layer; implement syntactic validation checks [35] | Adopt standardized data collection platforms like REDCap across studies [23] |
| Variable Coverage Gaps | Incomplete mapping—only 74% of forms achieve >50% variable harmonization [34] | Prioritize core variable sets; accept partial integration where appropriate [7] | Prospective harmonization of core instruments before data collection [34] |
Technical Implementation and Quality Assurance
| Challenge | Symptom | Solution | Prevention |
|---|---|---|---|
| Missing Data Patterns | Systematic missingness in key variables hampers pooled analysis [6] | Implement multiple imputation techniques; document missingness patterns [36] | Standardize data capture procedures; implement real-time validation [23] |
| High-Dimensionality | Variables significantly outnumber samples (HDLSS problem); algorithm overfitting [6] | Apply dimensionality reduction; use mixed integration approaches [6] | Plan variable selection strategically; avoid unnecessary data collection [34] |
| Cohort Heterogeneity | Statistical power diminished due to clinical/methodological differences [7] | Apply covariate adjustment; stratified analysis; random effects models [7] | Characterize cohort differences early; document protocols thoroughly [13] |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between prospective and retrospective harmonization, and when should I choose each approach?
A: Prospective harmonization occurs before or during data collection, with studies designed specifically for integration, while retrospective harmonization occurs after data collection is complete, requiring alignment of existing datasets [36].
- Choose prospective harmonization when designing new multi-cohort studies: it achieves higher variable coverage (74% of forms harmonized >50% of variables in the LIFE/CAP3 integration) [34] and reduces costs long-term.
- Choose retrospective harmonization when working with legacy datasets: it enables resource leveraging from completed studies but requires manual variable alignment and complex mapping [7].
Q2: Our multi-cohort project is experiencing significant delays in ethics approvals and data sharing agreements. What strategies can help accelerate this process?
A: Multi-cohort projects typically require ≥1 year for preparation phase alone [13]. Effective strategies include:
- Establish communication channels early with all cohort governance bodies (scientific boards, foundation boards) [13]
- Develop a unified protocol that addresses all cohorts' requirements simultaneously rather than sequentially
- Leverage existing cohort relationships - cohorts with prior collaboration history experience fewer administrative hurdles [13]
- Engage ethics committees early with clear documentation on data protection measures (HIPAA/GDPR compliance through platforms like REDCap) [23]
Q3: What are the most effective ETL tools for cohort harmonization, particularly for research teams with limited programming expertise?
A: Tool selection depends on technical capacity and harmonization scope:
- REDCap with APIs provides secure, web-based data collection with built-in harmonization features, ideal for multi-site studies with varying technical expertise [23]
- BIcenter offers visual, drag-and-drop ETL interfaces that reduce dependency on programming support, successfully applied to harmonize 6,669 Alzheimer's disease subjects [35]
- Custom Python implementations (like CMToolkit) provide flexibility for complex transformations but require more technical resources [37]
- OHDSI Common Data Model enables standardized schema migration for observational data, though it requires initial technical investment [37]
Q4: How can we effectively handle the "high-dimension, low sample size" (HDLSS) problem in multi-omics data integration?
A: The HDLSS problem, where variables drastically outnumber samples, causes machine learning algorithms to overfit [6]. Effective strategies include:
- Mixed Integration: Separately transform each omics dataset before combination, reducing noise and dimensionality [6]
- Early Integration: Concatenate datasets into a single matrix but apply rigorous variable selection to minimize dimensionality [6]
- Hierarchical Integration: Incorporate prior knowledge of regulatory relationships between omics layers to guide analysis [6]
- Feature Selection: Prioritize biologically relevant variables rather than attempting to integrate all available omics data [6]
Experimental Protocols: Successful Harmonization Methodologies
Protocol 1: Prospective ETL Harmonization for Active Cohorts
Based on the successful integration of LIFE (Jamaica) and CAP3 (Philadelphia) cohorts [34]:
Key Implementation Details:
- Variable Mapping Algorithm: Direct mapping for identical variables; user-defined mapping tables for differently coded variables [23]
- Technical Infrastructure: REDCap APIs with custom Java applications for automated weekly data pooling [23]
- Quality Assurance: Random sampling with cross-referencing against source data; error correction at source level [23]
- Coverage Validation: Quantitative assessment of variable completeness across all integrated forms [34]
Protocol 2: Retrospective Harmonization of Legacy Datasets
Based on the MASTERPLANS consortium experience with Systemic Lupus Erythematosus trials [7]:
Key Implementation Details:
- Manual Variable Alignment: Required when standards weren't implemented at source; matching equivalent patient variables across studies [7]
- Research-Driven Process: Focus on specific research questions to make harmonization feasible within realistic timelines [7]
- Flexible Approach: Accept inferential equivalence rather than insisting on identical measures [33]
- Systematic Preparation: Comprehensive data cleaning and organization before integration attempts [7]
The Scientist's Toolkit: Essential Research Reagents and Solutions
ETL Platforms and Data Integration Tools
| Tool | Function | Use Case | Key Features |
|---|---|---|---|
| REDCap with APIs [23] | Secure data collection and harmonization platform | Multi-site cohort studies with varying technical capacity | HIPAA/GDPR compliant, role-based security, automated ETL capabilities |
| BIcenter | Visual ETL tool with drag-and-drop interface | Complex medical concept harmonization (e.g., Alzheimer's disease) | No programming expertise required, collaborative web platform [35] |
| CMToolkit (Python) [37] | Programmatic cohort harmonization | Large-scale data migration to common data models | OHDSI CDM support, open-source (MIT license) |
| OHDSI Common Data Model | Standardized schema for observational data | Integrating electronic health records with research data | Enables systematic analysis across disparate datasets [37] |
Integration Strategy Framework
| Strategy | Approach | Best For | Limitations |
|---|---|---|---|
| Early Integration | Concatenate all datasets into single matrix | Simple, quick implementation | Increases dimensionality, noisy, discounts data distribution differences [6] |
| Mixed Integration | Transform datasets separately before combination | Noisy, heterogeneous data | Requires careful transformation design [6] |
| Intermediate Integration | Simultaneous integration with multiple representations | Capturing common and dataset-specific variance | Requires robust pre-processing for heterogeneous data [6] |
| Late Integration | Analyze separately, combine final predictions | Preserving dataset integrity | Doesn't capture inter-dataset interactions [6] |
| Hierarchical Integration | Incorporate regulatory relationships between layers | Multi-omics data with known biological pathways | Less generalizable, nascent methodology [6] |
Key Lessons from Active Implementations
Prospective Harmonization Success Factors
The LIFE/CAP3 integration demonstrated that 74% of questionnaire forms can achieve >50% variable harmonization when studies implement prospective design [34]. Critical success factors included:
- Cross-disciplinary working groups during variable selection (epidemiologists, psychologists, laboratory scientists) [23]
- Leveraging existing platforms with built-in security compliance (REDCap with HIPAA/GDPR) [23]
- Automated ETL processes with weekly synchronization and quality checks [23]
Retrospective Harmonization Realities
The MASTERPLANS consortium experience with Lupus trials revealed that retrospective harmonization remains possible without source standards, but requires [7]:
- Substantial manual effort for variable alignment
- Focus on specific research questions to make the process manageable
- Flexibility in accepting inferentially equivalent rather than identical measures
- Systematic preparation and data cleaning before integration
Effective ETL processes for cohort harmonization—whether prospective or retrospective—require careful planning, appropriate tool selection, and acknowledgment that some challenges require pragmatic compromises rather than perfect solutions.
Frequently Asked Questions (FAQs)
1. What is vertical integration in the context of multi-omics data? Vertical integration, or cross-omics integration, involves combining multiple types of omics data (e.g., genomics, transcriptomics, proteomics, metabolomics) collected from the same set of samples to gain a comprehensive understanding of biological systems and disease mechanisms [11] [38] [39].
2. What are the main challenges of heterogeneous data integration in multi-cohort studies? Key challenges include:
- High Dimensionality and Low Sample Size (HDLSS): Variables vastly outnumber samples, leading to a "lack of information" and risk of overfitting in machine learning models [11] [38] [6].
- Data Heterogeneity: Omics datasets differ in scale, distribution, and data type, making integration difficult [38] [6].
- Technical Noise and Batch Effects: Unwanted variations introduced across different platforms, labs, or batches can confound true biological signals [39].
- Missing Data: Omics datasets often contain missing values that can hamper downstream integrative analysis [38] [6].
3. How do I choose the right vertical integration strategy for my study? The choice depends on your research question and data structure. Early Integration is simple but struggles with highly dimensional data. Late Integration is flexible but may miss inter-omics interactions. Intermediate and Mixed Integration are powerful for capturing complex relationships but can be computationally intensive. Hierarchical Integration is ideal for leveraging known biological prior knowledge [38] [6].
4. What are some best practices for ensuring data quality before integration? Implement rigorous quality control (QC) for each omics dataset individually before integration. Using multi-omics reference materials, such as those from the Quartet Project, provides a built-in ground truth for assessing data quality and integration performance. Employing a ratio-based profiling approach, which scales feature values of a study sample against a common reference sample, can also improve reproducibility and data comparability across batches and platforms [39].
Troubleshooting Guides
Issue 1: Poor Model Performance or Overfitting After Early Integration
Problem: After concatenating all omics datasets into a single matrix (Early Integration), your machine learning model performs poorly on validation data, likely due to the "curse of dimensionality" [38] [6].
Solution:
- Apply Dimensionality Reduction: Before concatenation, use methods like Principal Component Analysis (PCA) on each omics block to create lower-dimensional representations. Then, concatenate the reduced components [38].
- Switch to a Mixed Integration Strategy: Transform each omics dataset independently into a new representation (e.g., using autoencoders) to reduce noise and dimensionality before combining them for analysis [38] [6].
- Use Regularization Techniques: Implement machine learning models with built-in regularization (e.g., Lasso, Ridge Regression) to penalize model complexity and reduce overfitting.
Issue 2: Failure to Capture Interactions Between Omics Layers
Problem: Your analysis results seem to reflect only the strongest single-omics signals and fail to reveal novel, interconnected biological pathways across omics layers.
Solution:
- Adopt an Intermediate Integration Strategy: Use methods like Multiple Kernel Learning or Joint Matrix Factorization that simultaneously integrate raw datasets to output both common and omics-specific representations. This forces the model to learn shared and interacting factors [38].
- Implement Network-Based Integration: Construct multi-layered molecular networks to reveal the interconnections and regulatory relationships between features from different omics datasets [40].
- Consider Hierarchical Integration: If prior knowledge of regulatory relationships exists (e.g., genomic variants influencing transcriptome), use hierarchical methods that base the integration on this biological hierarchy [38] [6].
Issue 3: Inconsistent Results Across Different Cohorts or Batches
Problem: A integration model trained on one cohort fails to generalize to another, likely due to strong batch effects or cohort-specific technical artifacts [39].
Solution:
- Employ Ratio-Based Profiling with Reference Materials: Scale the absolute feature values of your study samples relative to those of a concurrently measured common reference sample (e.g., from the Quartet Project). This minimizes batch effects and improves reproducibility [39].
- Apply Batch Effect Correction: Before vertical integration, use horizontal integration methods (within-omics) to correct for batch effects across different cohorts or studies for each omics type individually [39].
- Validate with Built-in Truth: Use study designs with built-in truth, such as family-based cohorts (e.g., parents and twins), to objectively evaluate the reliability of your integration method's ability to classify samples or identify feature relationships [39].
Comparison of Vertical Integration Strategies
The table below summarizes the core methodologies, typical applications, and key considerations for the five vertical integration strategies.
Table 1: Overview of Vertical Integration Strategies for Multi-Omics Data
| Strategy | Description | Common Methods | Advantages | Disadvantages |
|---|---|---|---|---|
| Early Integration | Concatenates all omics datasets into a single input matrix [38] [6]. | Support Vector Machines, Random Forests, Regularized Regression on concatenated data [38]. | Simple to implement; Model can capture all interactions at once [38]. | Highly dimensional and complex; Noisy; Model may struggle to learn (curse of dimensionality) [38] [6]. |
| Mixed Integration | Transforms each omics dataset independently before combining them [38] [6]. | PCA, Autoencoders, or other dimensionality reduction on each dataset, followed by concatenation and analysis [38]. | Reduces noise and dimensionality; Handles dataset heterogeneity well [38] [6]. | Risk of losing important information during transformation; May not fully capture inter-omics interactions [38]. |
| Intermediate Integration | Simultaneously integrates raw datasets to find a joint representation [38] [6]. | Multiple Kernel Learning, Joint Matrix Factorization, Deep Learning (e.g., multimodal autoencoders) [38]. | Effectively captures complex inter-omics interactions; Powerful for pattern discovery [38]. | Computationally intensive; Requires robust pre-processing; Complex to implement and tune [38] [6]. |
| Late Integration | Analyzes each omics dataset separately and combines the final results or predictions [38] [6]. | Ensemble methods, Model stacking, Majority voting on predictions from single-omics models [38]. | Flexible; Uses state-of-the-art single-omics models; Avoids data heterogeneity issues [38] [6]. | Does not capture inter-omics interactions; May lead to suboptimal performance if interactions are strong [38] [6]. |
| Hierarchical Integration | Bases integration on prior knowledge of regulatory relationships between omics layers [38] [6]. | Bayesian networks, Pathway-based integration methods [38]. | Biologically driven; Can reveal causal relationships; Embodies true trans-omics analysis intent [38] [6]. | Requires high-quality prior knowledge; Less generalizable if prior knowledge is incomplete or incorrect [38] [6]. |
Experimental Protocol for Benchmarking Integration Strategies
Objective: To systematically evaluate and compare the performance of different vertical integration strategies for sample classification in a multi-cohort study.
1. Data Preparation and QC
- Acquire Datasets: Obtain multi-omics data (e.g., genome, transcriptome, methylome) from at least two independent cohorts with matched sample phenotypes (e.g., disease subtypes).
- Pre-processing: Independently pre-process each omics dataset according to best practices for that data type (normalization, scaling, etc.) [38].
- Quality Control: Perform stringent QC on each dataset. Remove low-quality samples and features. Recommended Reagent: Integrate data from the Quartet Project reference materials to serve as a quality benchmark and built-in truth for evaluating integration accuracy [39].
- Handle Missing Data: Impute missing values using appropriate methods (e.g., k-nearest neighbors) [38].
- Batch Effect Correction: Apply horizontal integration/batch correction methods (e.g., ComBat) to each omics type across the different cohorts to remove technical artifacts [39].
2. Implementation of Integration Strategies
- Early Integration: Concatenate the processed and batch-corrected omics matrices from all cohorts into a single matrix.
- Mixed Integration: Apply PCA to each omics type to generate top principal components. Concatenate these components across omics types.
- Intermediate Integration: Apply a joint matrix factorization method (e.g., JIVE) or a multiple kernel learning algorithm to the raw omics matrices.
- Late Integration: Train a separate classifier (e.g., SVM) on each omics type. Combine the predictions via a meta-classifier (e.g., logistic regression).
- Hierarchical Integration: Construct a Bayesian network where the structure is defined by known regulatory relationships (e.g., genetic variants -> methylation -> gene expression).
3. Model Training and Evaluation
- Uniform Classifier: For Early, Mixed, and Intermediate integration, use a single classifier (e.g., Random Forest) on the integrated output.
- Cross-Validation: Implement a nested cross-validation scheme to tune hyperparameters and evaluate model performance, ensuring cohorts are kept separate during training to test generalizability.
- Performance Metrics: Evaluate each strategy using metrics such as classification accuracy, F1-score, and Area Under the ROC Curve (AUC). The most robust strategy will maintain high performance across independent cohorts.
The following workflow diagram illustrates the benchmarking protocol.
Research Reagent Solutions
The table below lists key reagents and resources essential for conducting robust multi-omics integration studies.
Table 2: Essential Research Reagents and Resources for Multi-Omics Integration
| Item Name | Function/Application | Key Features / Examples |
|---|---|---|
| Quartet Project Reference Materials | Provides multi-omics ground truth for quality control and benchmarking of integration methods [39]. | Comprises matched DNA, RNA, protein, and metabolites from a family quartet (parents, monozygotic twins). Offers built-in truth for Mendelian consistency and central dogma information flow [39]. |
| Reference-Based Data Profiling Pipeline | Enables reproducible and comparable data across labs and platforms, mitigating batch effects [39]. | A ratio-based approach that scales absolute feature values of a study sample against a common reference sample (e.g., one Quartet sample) measured concurrently [39]. |
| Multi-Omics Data Portals | Centralized access to processed, large-scale multi-omics datasets for method development and testing. | Examples include The Cancer Genome Atlas (TCGA) and the Quartet Data Portal, which provide comprehensive, multi-layered molecular data [11] [39]. |
| Batch Effect Correction Algorithms | Corrects for unwanted technical variation within a single omics type across different batches or cohorts. | Methods such as ComBat or limma's removeBatchEffect are crucial pre-processing steps before vertical integration [39]. |
Frequently Asked Questions (FAQs)
What is SONAR and what problem does it solve? SONAR (Semantic and Distribution-Based Harmonization) is an ensemble machine learning method designed to automate the harmonization of variables across different cohort studies. It addresses the critical challenge of combining datasets where the same clinical concept is recorded using different variable names, encodings, or measurement units, a common and labor-intensive obstacle in multi-cohort research [28].
What are the main data sources SONAR was validated on? The SONAR method was developed and validated using three major National Institutes of Health (NIH) cohorts:
- Cardiovascular Health Study (CHS): A longitudinal study of cardiovascular disease risk factors in adults aged 65 and older [28].
- Multi-Ethnic Study of Atherosclerosis (MESA): A prospective study of subclinical cardiovascular disease in a diverse, population-based sample [28].
- Women’s Health Initiative (WHI): A long-term national health study focusing on prevention strategies in postmenopausal women [28].
What type of data is SONAR best suited for? SONAR is primarily focused on the harmonization of continuous variables at the conceptual level. This means it identifies variables that represent the same underlying notion (e.g., "C-reactive protein"), independent of the specific measurement unit or the time point of collection [28].
How does SONAR differ from other data integration strategies? SONAR uniquely integrates two complementary learning approaches, whereas other common strategies have different focuses:
- SONAR: Combines semantic learning (from variable descriptions) and distribution learning (from participant-level data) [28].
- Early Integration: Simply concatenates all datasets into one large matrix, which can lead to high dimensionality and noise [6].
- Late Integration: Analyzes each dataset separately and combines the results at the end, which may fail to capture important inter-dataset interactions [6].
Troubleshooting Guides
Problem: Poor Harmonization Accuracy for Specific Concepts
Symptoms
- The model consistently fails to match variables representing the same clinical concept across cohorts.
- Performance metrics (e.g., Top-k accuracy) are low for certain families of variables.
Investigation and Resolution
- Verify Data Preprocessing: Confirm that temporal information (e.g., "from visit 1") and unit descriptors have been properly removed from variable descriptions to ensure the model focuses on the core concept [28].
- Check Data Distributions: Analyze the distribution of participant-level data for the problematic variables in each cohort. Significant distribution shifts between cohorts for the same concept can hinder matching.
- Review Subgroup Data: SONAR filters variables that have no patient data in any of the 16 predefined patient subgroups (based on age, race, and sex). Ensure your variables have adequate data coverage across these subgroups [28].
- Inspect Semantic Descriptions: Manually review the variable names and descriptions for the failed matches. Ambiguous or overly technical language in the source data may require curating a custom fine-tuning set for the embedding model.
Problem: Handling of Heterogeneous and Complex Data
Symptoms
- Challenges integrating datasets with different underlying structures (e.g., horizontal vs. vertical integration).
- Performance degradation when integrating omics data with non-omics (clinical, epidemiological) data.
Investigation and Resolution
- Classify Your Data Structure:
- Horizontal Datasets: Come from one or two technologies for a specific research question. SONAR's cohort-based approach is well-suited for this [6].
- Vertical Datasets: Generated using multiple technologies probing different omics layers (genome, proteome, etc.). This presents a greater integration challenge [6].
- Consider Preprocessing for High-Dimensional Data: For omics data, which often has many more variables than samples (HDLSS problem), consider additional dimensionality reduction techniques prior to harmonization to prevent overfitting [6].
- Address Missing Data: Omics and clinical datasets often contain missing values. Implement an appropriate imputation process for your data before applying SONAR's distribution learning [6].
Experimental Protocols & Validation
SONAR Methodology Workflow
The following diagram illustrates the core workflow of the SONAR harmonization process.
Key Experiment: Performance Validation on NIH Cohorts
Objective To evaluate the intracohort and intercohort variable harmonization performance of SONAR against existing benchmark methods using manually curated gold standard labels [28].
Protocol
- Data Acquisition: Variable metadata and participant-level data were extracted for continuous variables from the CHS, MESA, and WHI studies via the Database of Genotypes and Phenotypes (dbGaP) [28].
- Gold Standard Preparation: Manually curated labels defining true variable matches across the cohorts were used as the ground truth for training and evaluation.
- Model Training: The supervised SONAR model was trained to learn an embedding vector for each variable by combining:
- Semantic Inputs: Variable description strings, preprocessed to remove temporal information.
- Distributional Inputs: Patient-level data, filtered to include only variables with data available across all defined patient subgroups (age, race, sex) [28].
- Evaluation: Model performance was assessed using:
- Area Under the Curve (AUC)
- Top-k Accuracy
Results Summary The supervised SONAR method outperformed existing benchmark methods for almost all intracohort and intercohort comparisons [28]. The table below summarizes the key validation contexts.
| Validation Type | Cohorts Involved | Key Performance Metrics | Reported Outcome |
|---|---|---|---|
| Intracohort | Within individual cohorts (CHS, MESA, WHI) | AUC, Top-k Accuracy | Outperformed benchmarks [28] |
| Intercohort | Between different cohorts (e.g., CHS->MESA) | AUC, Top-k Accuracy | Outperformed benchmarks for most comparisons [28] |
| Concept Difficulty | Across all cohorts | Accuracy on difficult concepts | Significantly improved harmonization of concepts that were problematic for semantic-only methods [28] |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Components for Implementing a SONAR-like Harmonization Framework
| Item / Reagent | Function & Explanation |
|---|---|
| Cohort Data with Metadata | Source data from studies like CHS, MESA, and WHI. Must include variable descriptions and participant-level data. Provides the raw material for both semantic and distributional learning [28]. |
| dbGaP (Database of Genotypes and Phenotypes) | A repository for accessing variable metadata (accession, name, description) and associated patient data. Serves as a practical data source for this type of research [28]. |
| Pre-trained Language Model (e.g., BERT) | A foundational model used to generate initial semantic embeddings from variable description text. This is the base for semantic learning [28] [41]. |
| Embedding Vectors | Numerical representations of variables in a high-dimensional space. SONAR learns these vectors by combining information from text descriptions and data distributions, enabling similarity calculation [28]. |
| Cosine Similarity Metric | A mathematical measure used to calculate the similarity between two embedding vectors. It is the final step for scoring and identifying potential variable matches [28]. |
| Gold Standard Labels | A manually curated set of known correct variable matches. Used to fine-tune the model in a supervised manner and to evaluate its performance objectively [28]. |
| OMOP Common Data Model (CDM) | An alternative or complementary approach for standardizing data representation across cohorts. It facilitates data harmonization by providing a standardized structure, though it may have limitations with cohort-specific fields [42]. |
Troubleshooting Common Flexynesis Implementation Issues
Installation and Environment Setup
Problem: Installation fails due to Python version incompatibility. Solution: Flexynesis requires Python 3.11 or newer [43]. Create a fresh environment using conda/mamba before pip installation:
Verification: Test your installation with the provided example dataset to confirm all dependencies are correctly resolved [44].
Problem: "Module not found" errors during execution. Solution: This typically indicates incomplete dependency installation. Reinstall Flexynesis via pip, ensuring your environment has adequate internet access and privileges. The pip installation method automatically handles core dependencies including PyTorch and Captum for interpretability features [43].
Data Formatting and Input Structure
Problem: Runtime errors stating sample/feature mismatches between train and test sets. Solution: Ensure your directory structure follows Flexynesis requirements [44]:
Critical checks:
- Corresponding omics files in train/test splits must contain overlapping feature names
clin.csvfiles must contain matching clinical variables between splits- Sample identifiers in omics files must overlap with those in
clin.csv
Problem: Training fails with dimension mismatches in multi-omics data.
Solution: For Graph Neural Network (GNN) architectures, ensure features across modalities share identical naming conventions (e.g., all gene-based). Use --fusion intermediate instead of early fusion when data modalities have different feature spaces [44].
Frequently Asked Questions (FAQs)
Data Integration Challenges
Q: How does Flexynesis handle heterogeneous data integration from multiple cohorts? A: Flexynesis provides multiple fusion strategies to address cohort heterogeneity [44]:
- Early fusion: Concatenates all omics datasets into a single matrix
- Intermediate fusion: Processes each modality separately before combining embeddings
- Model recommendation: Start with intermediate fusion (
--fusion intermediate) for heterogeneous data as it better handles technical variability across studies.
Q: Can Flexynesis integrate non-omics (clinical) data with molecular profiling? A: While primarily designed for bulk multi-omics, clinical variables can be incorporated as target variables or through custom preprocessing to matrix format compatible with the omics input structure [44].
Model Selection and Performance
Q: Which model architecture should I choose for my specific task? A: Refer to the model selection guide below:
Table: Flexynesis Model Selection Guide
| Research Task | Recommended Model | Key Considerations |
|---|---|---|
| Standard prediction (classification/regression) | DirectPred |
Default choice for most supervised tasks |
| Multi-task learning | DirectPred with multiple target variables |
Supports mixed regression/classification/survival |
| Unsupervised representation learning | supervised_vae |
No target variables needed |
| Cross-modality translation | CrossModalPred |
Learn embeddings that translate between modalities |
| Gene network-informed analysis | GNN |
Requires gene-based features and prior biological networks |
Q: How can I improve poor performance on my dataset? A: Implement the following troubleshooting protocol:
- Feature selection: Use
--features_top_percentile 5to reduce dimensionality - Hyperparameter optimization: Increase
--hpo_iterfrom default (≥20 for production models) - Fusion strategy: Experiment with early vs. intermediate fusion based on data heterogeneity
- Data modality assessment: Evaluate individual modality performance before integration
Survival Analysis Specific Issues
Q: What format should survival data follow?
A: Survival analysis requires two separate variables in your clin.csv [44]:
- Event variable: Binary (0/1) where 1 indicates occurrence of the event (death, progression)
- Time variable: Continuous values indicating time to event or last follow-up
Command structure:
--surv_event_var OS_STATUS --surv_time_var OS_MONTHS
Q: How is survival model performance evaluated? A: Flexynesis uses the concordance index (C-index) similar to established multi-omics survival methodologies, with values closer to 1.0 indicating better predictive performance [45].
Data Integration Workflow and System Requirements
Experimental Protocol for Multi-Cohort Integration
For researchers handling heterogeneous multi-cohort data, follow this validated workflow:
Table: Multi-Cohort Integration Protocol
| Step | Procedure | Quality Control Check |
|---|---|---|
| 1. Data harmonization | Standardize variable names and formats across cohorts | Verify consistent clinical variable definitions |
| 2. Input preparation | Create train/test splits preserving cohort heterogeneity | Ensure feature overlap between splits |
| 3. Feature selection | Apply --features_top_percentile to reduce dimensionality |
Confirm retained biologically relevant features |
| 4. Model configuration | Select --fusion intermediate for heterogeneous cohorts |
Validate architecture supports mixed data types |
| 5. Hyperparameter optimization | Set --hpo_iter ≥20 for final models |
Check performance stability across iterations |
Computational Requirements and Research Reagents
Table: Essential Research Reagents and Computational Resources
| Resource Type | Specification | Purpose/Function |
|---|---|---|
| Minimum system requirements | Python 3.11+, 8GB RAM | Basic installation and small dataset operation |
| Production requirements | 16+ GB RAM, GPU recommended | Large-scale multi-omics integration |
| Input data formats | CSV matrices (samples × features) | Compatible with Flexynesis input parsers |
| Biological networks | STRING database (for GNN models) | Prior knowledge integration for graph-based models |
| Benchmark datasets | TCGA, CCLE, GDSC2 | Model validation and performance benchmarking [46] |
Advanced Configuration and Optimization
Model Architecture Decision Framework
Performance Optimization Guide
For large-scale multi-cohort studies:
- Feature selection: Always use
--features_top_percentileto manage high-dimensionality challenges common in multi-omics data [46] - Hyperparameter optimization: Allocate sufficient iterations (
--hpo_iter) as computational resources allow - Fusion strategy selection: Choose early fusion for homogeneous data, intermediate fusion for technically heterogeneous cohorts
- Interpretability: Leverage integrated Captum gradients for biomarker discovery in heterogeneous populations
Troubleshooting performance bottlenecks:
- Memory issues: Reduce feature percentile or use data chunking
- Training instability: Adjust learning rate or switch fusion strategy
- Poor convergence: Verify data preprocessing and normalize input matrices
- Overfitting: Increase regularization or reduce model complexity
This technical support framework addresses the most common implementation challenges while providing systematic guidance for optimizing Flexynesis in heterogeneous multi-cohort research environments.
Troubleshooting Guides & FAQs for Heterogeneous Data Integration
Frequently Asked Questions (FAQs)
Q1: What are the most common data integration challenges in multi-cohort studies? The most common challenges stem from data heterogeneity, which includes discrepancies in how variables are documented and measured across different cohort studies [28]. You will often encounter issues with missing values, high-dimensionality where variables significantly outnumber samples (the HDLSS problem), and the sheer technical complexity of combining datasets with different distributions, formats, and scales [6].
Q2: How can I handle missing data in my multi-omics dataset before integration? An additional imputation process is typically required to infer the missing values in these incomplete datasets before statistical analyses can be applied [6]. The specific methodology depends on the nature of your data, but this step is crucial to prevent hampering downstream integrative bioinformatics analyses.
Q3: Our team is struggling with integrating clinical (non-omics) data with high-throughput omics data. What is the best strategy? The large-scale integration of non-omics data with omics data is extremely limited due to heterogeneity and the presence of subphenotypes [6]. A promising strategy is to use semantic and distribution-based harmonization methods, like the SONAR approach, which learns from both variable descriptions and patient-level data to create a unified view [28].
Q4: What is the difference between "horizontal" and "vertical" data integration? This is a fundamental concept for structuring your integration project [6]:
- Horizontal Integration involves combining data from different studies, cohorts, or labs that measure the same omics entities. It often deals with technical and biological heterogeneity from diverse populations.
- Vertical Integration involves combining datasets from different omics levels (e.g., genome, transcriptome, proteome) measured using different technologies. This is essential for a holistic, trans-omics view of biological systems.
Troubleshooting Common Experimental Issues
Problem: Low Accuracy in Variable Harmonization
- Symptoms: Models fail to generalize, inconsistent findings when replicating analysis on another cohort.
- Solution: Implement an ensemble harmonization algorithm like SONAR (Semantic and Distribution-Based Harmonization) that uses both semantic learning (from variable descriptions) and distribution learning (from participant data) to create robust embedding vectors for each variable [28].
- Protocol:
- Data Extraction: Gather variable documentation (accession, name, description) and corresponding patient-level data from all cohorts (e.g., via dbGaP) [28].
- Preprocessing: Filter for your data type of interest (e.g., continuous variables). Remove temporal information (e.g., "visit 1") from variable descriptions to focus on the core concept [28].
- Embedding & Scoring: Use a model to learn an embedding vector for each variable and calculate pairwise cosine similarity to score variable similarity [28].
- Validation: Evaluate harmonization performance using manually curated gold standard labels and metrics like area under the curve (AUC) and top-k accuracy [28].
Problem: Inability to Capture Inter-omics Interactions
- Symptoms: The integrated model provides a static view and misses crucial regulatory relationships between different molecular layers.
- Solution: Move beyond simple "early integration" (dataset concatenation) and adopt an "intermediate" or "hierarchical" integration strategy. These methods are designed to capture interactions across omics layers, truly embodying the intent of trans-omics analysis [6].
- Protocol (Hierarchical Integration):
- Define Prior Knowledge: Incorporate established regulatory relationships between different omics layers (e.g., known transcription factor-gene interactions) into your model structure [6].
- Model Training: Use a framework that can integrate these hierarchical constraints during analysis.
- Validation: Assess if the model outputs reveal biologically plausible interactions across the different data layers.
Table 1: Performance Metrics of SONAR Data Harmonization Method
| Evaluation Metric | Cohort Comparison | Performance Result |
|---|---|---|
| Area Under the Curve (AUC) [28] | Intracohort & Intercohort | Outperformed existing benchmark methods |
| Top-k Accuracy [28] | Intracohort & Intercohort | Outperformed existing benchmark methods |
| Application: Multimodal Fusion in Oncology | ||
| Prediction of Anti-HER2 Therapy Response [47] | Oncology (Multimodal) | AUC = 0.91 |
| Application: Digital Biomarkers in Parkinson's Disease | ||
| Gait Analysis for Fall Risk Prediction [48] | Parkinson's Disease | 89% Accuracy |
| Data Capture Completion Rate (Passive Sensing) [48] | Parkinson's Disease | >95% |
Table 2: Clinical Research Technology Impact
| Technology | Application / Metric | Impact / Result |
|---|---|---|
| eSource Systems [48] | Data Entry Error Rate | Reduced from 15-20% to <2% |
| eConsent Platforms [48] | Participant Comprehension & Enrollment | 23% higher comprehension, 31% faster enrollment |
| Decentralized Clinical Trials (DCTs) [48] | Trial Timelines | Reduction of up to 60% |
| Wearable Devices (Apple Heart Study) [48] | Participant Enrollment | 420,000+ participants enrolled remotely |
Experimental Protocols
Protocol 1: SONAR for Automated Variable Harmonization This protocol is designed for harmonizing variables across cohort studies to facilitate multicohort studies [28].
- Ethical Considerations: Secure IRB approval for access to retrospective, de-identified data from all cohort studies.
- Data Sources: Obtain data from established cohort studies (e.g., Cardiovascular Health Study, Multi-Ethnic Study of Atherosclerosis, Women's Health Initiative).
- Data Extraction:
- Source variable metadata (accession, name, description) from dbGaP.
- Extract corresponding patient-level data for the variables.
- Filter data to focus on a specific type (e.g., continuous variables).
- Data Preprocessing:
- Remove temporal phrases from variable descriptions.
- Filter out variables with incomplete patient data or uniformly zero values.
- Model Implementation (SONAR):
- Learn an embedding vector for each variable by combining semantic learning (from descriptions) and distribution learning (from patient data).
- Use pairwise cosine similarity to score variable similarity.
- Refine embeddings using gold standard labels in a supervised manner.
- Validation: Evaluate intracohort and intercohort harmonization performance against manually curated gold standards using AUC and top-k accuracy metrics [28].
Protocol 2: Multimodal Integration for Oncology Tumor Characterization This protocol uses multimodal data for enhanced tumor characterization and personalized treatment planning [47].
- Data Collection: Gather multimodal patient data, including pathological images, genomic/transcriptomic data (e.g., from RNA sequencing), and clinical information from EHRs.
- Feature Extraction:
- Use a trained convolutional neural network (CNN) to capture deep features from pathological images.
- Use a trained deep neural network to extract features from genomic and other omics data.
- Data Fusion: Integrate the extracted multimodal features using a fusion model.
- Model Application: Apply the fused model to achieve accurate prediction of molecular subtypes, therapy response (e.g., to anti-HER2 therapy), or patient prognosis [47].
Protocol 3: Developing Digital Biomarkers for Parkinson's Disease This protocol outlines the use of wearable devices and smartphones for continuous monitoring and digital biomarker development [48].
- Device Selection: Equip participants with consumer-grade wearable devices (e.g., smartwatches with accelerometers) and/or smartphones.
- Data Capture: Collect continuous, passive data on movement (gait), voice, and activity levels in the participants' daily living environment.
- Data Processing: Process the raw sensor data to extract digital biomarkers (objective health measures), such as gait analysis metrics from smartphone accelerometers or voice features from smartphone-based analysis.
- Model Validation: Correlate the digital biomarkers with traditional clinical rating scales and validate their accuracy for detecting disease progression or predicting events like falls [48].
Workflow and Signaling Pathway Diagrams
Multi-Cohort Data Harmonization with SONAR
Oncology Multi-Modal Data Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Heterogeneous Data Integration
| Tool / Resource | Type | Primary Function in Integration |
|---|---|---|
| SONAR Algorithm [28] | Software/Method | Harmonizes variables across cohorts by combining semantic and distribution learning. |
| dbGaP (Database of Genotypes and Phenotypes) [28] | Data Repository | Provides access to cohort study data and variable metadata for extraction. |
| Convolutional Neural Network (CNN) [47] | AI Model | Extracts deep features from unstructured data like pathological images. |
| Deep Neural Network (DNN) [47] | AI Model | Extracts features from structured omics data (e.g., genomic, transcriptomic). |
| Wearable Devices (e.g., Smartwatches) [48] | Hardware/Sensor | Captures continuous, real-world digital biomarker data (e.g., for Parkinson's gait analysis). |
| eSource/eConsent Platforms [48] | Clinical Trial Software | Digitizes data capture at the point of collection and improves participant engagement and understanding. |
| Trusted Research Environments [48] | Data Platform | Provides secure, cloud-based foundations for multi-site collaboration on sensitive data. |
Solving Common Integration Challenges: Practical Troubleshooting and Optimization Strategies
Troubleshooting Guide: FAQs on Data Quality in Multi-Cohort Studies
FAQ 1: What are the most effective methods for handling missing data in combined cohort datasets?
Missing data is a common issue that can reduce statistical power and introduce bias if not handled properly [49]. The approach depends on the type of missingness. The table below summarizes the primary methods:
Table 1: Methods for Handling Missing Values
| Method | Description | Best Use Case | Advantages & Limitations |
|---|---|---|---|
| Complete Case Analysis | Removes any row with a missing value [49]. | Data Missing Completely At Random (MCAR); small amount of missing data. | Advantage: Simple to implement.Limitation: Reduces sample size and can introduce bias [49]. |
| Imputation Analysis | Replaces missing values with substituted estimates [49]. | Data Missing At Random (MAR); to preserve sample size. | Advantage: Retains dataset size and statistical power.Limitation: Can distort data relationships if done incorrectly. |
| Mean/Median/Mode Imputation | Replaces missing values with the variable's mean (numeric) or mode (categorical) [50]. | Simple, quick method for numeric data. | Advantage: Very simple.Limitation: Can reduce variance and distort distributions [50]. |
| Regression Imputation | Uses a regression model to predict missing values based on other variables [50]. | Data with strong correlations between variables. | Advantage: Can be more accurate than mean imputation.Limitation: Assumes linear relationships and can underestimate variance [50]. |
| Multiple Imputation | Creates several plausible versions of the complete dataset and pools results [50]. | High-stakes analysis requiring robust handling of uncertainty. | Advantage: Gold standard; accounts for uncertainty in imputation.Limitation: Computationally intensive and complex to implement [50]. |
FAQ 2: How can I identify and manage outliers in my integrated research data?
Outliers are extreme values that deviate from the overall data pattern and can significantly distort statistical estimates [49]. A combined approach of visual inspection and statistical methods is most effective.
Table 2: Techniques for Identifying and Treating Outliers
| Category | Technique | Description | Application |
|---|---|---|---|
| Identification | Visual Inspection (Box Plots) | Graphical display using quartiles to identify data points outside the "whiskers" [50] [49]. | Quick, univariate outlier detection. |
| Identification | Statistical Methods (Z-Score/IQR) | Z-Score: Flags points >3 standard deviations from mean. IQR (Tukey's Method): Flags points below Q1-1.5IQR or above Q3+1.5IQR [50]. | Robust, rule-based univariate detection. IQR is less sensitive to extreme outliers than Z-Score. |
| Treatment | Removal (Trimming) | Completely removing outlier records from the dataset [49]. | Outliers caused by clear data entry errors; can introduce bias if overused. |
| Treatment | Winsorization | Replacing extreme values with the nearest value within the acceptable range (e.g., the 95th percentile value) [50] [49]. | Retains data points while reducing the undue influence of extreme values. |
| Treatment | Robust Estimation | Using statistical models and estimators that are inherently less sensitive to outliers [49]. | When the underlying population distribution is known and robust models are available. |
FAQ 3: What strategies ensure data consistency when harmonizing heterogeneous cohorts?
Inconsistency arises when the same information is represented differently across sources (e.g., formats, units, or codes) [51]. A proactive, rule-based strategy is key.
- Standardization: Transform data into a consistent format [50]. This includes:
- Data Validation Rules: Implement automated checks to flag inconsistencies [50] [52]. Rules can check for permissible value ranges, valid formats, and logical relationships between fields (e.g., discharge date cannot be before admission date) [50] [52].
- Dynamic, Rule-Based Validation Frameworks: For complex integrations, use frameworks like AIDAVA that employ SHACL (Shapes Constraint Language) rules within a knowledge graph. This allows for continuous validation of data consistency and completeness throughout the data lifecycle, not just as a one-time check [52].
Experimental Protocol: Data Harmonization Workflow for Multi-Cohort Studies
This protocol outlines a methodology for harmonizing data from multiple active cohort studies, based on established ETL (Extraction, Transform, and Load) processes [23] [37].
1. Objective: To integrate and harmonize data from disparate cohort studies (e.g., LIFE project, Jamaica; CAP3, USA) into a single, analysis-ready dataset while managing data quality issues [23].
2. Materials and Reagents:
Table 3: Research Reagent Solutions for Data Harmonization
| Item Name | Function/Description | Example/Note |
|---|---|---|
| REDCap (Research Electronic Data Capture) | A secure web application for building and managing online surveys and databases [23]. | Used as the primary data collection and management platform; supports HIPAA compliance and APIs for automation [23]. |
| SHACL (Shapes Constraint Language) | A language for validating RDF knowledge graphs against a set of conditions [52]. | Used in frameworks like AIDAVA to define and check data consistency rules (e.g., diagnosis codes align with patient sex) [52]. |
| OHDSI OMOP CDM (Common Data Model) | A standardized data model for observational health research data [37]. | Serves as a target schema for harmonizing different clinical cohorts, enabling large-scale analytics. |
| Python/Java Application | Custom scripts or applications to automate the ETL process [23]. | Used to call REDCap APIs, perform data transformations, and load data into the harmonized database [23]. |
3. Methodology:
The entire harmonization and quality assurance workflow is illustrated below.
Data Harmonization and Quality Control Workflow
Step-by-Step Instructions:
- Variable Mapping and Prospective Harmonization:
- Action: Conduct working group sessions with domain experts (e.g., epidemiologists, lab scientists) to identify shared data elements across cohorts [23].
- Process: Map source variables from all cohorts to a common set of destination variables that represent the same construct. Create a mapping table that includes recoding logic for variables with different schemas [23].
- Data Extraction:
- Data Transformation:
- Data Loading:
- Action: Load the transformed data into a centralized, integrated database.
- Process: The automated script uploads the processed data to the harmonized project, typically on a scheduled basis (e.g., weekly) [23].
- Quality Assurance and Dynamic Validation:
- Action: Implement a continuous quality control loop.
- Process:
- Run automated checks for completeness, consistency, and plausibility [52].
- Perform routine spot checks by comparing a random sample from the integrated database against the source data [23].
- Use a framework like AIDAVA to apply SHACL validation rules dynamically during integration, flagging logical inconsistencies (e.g., a diagnosis of prostate cancer for a female patient) [52].
- When errors are found, correct them in the source cohort database. The corrections will then propagate to the harmonized database during the next ETL cycle, ensuring ongoing data integrity [23].
In multi-cohort studies, researchers often face significant technical bottlenecks when attempting to integrate heterogeneous datasets from diverse sources. These challenges stem from inconsistent data formats, varying collection protocols, and incompatible infrastructure systems that hinder scalable analysis. The process of combining data from multiple clinical trials and patient registries presents particular difficulties due to the inherent complexity and heterogeneity of both the disease data and the technological frameworks used to manage it [7]. These technical hurdles can consume substantial research time and resources, potentially compromising the validity and generalizability of findings if not properly addressed.
Within life course research and systemic disease studies, multi-cohort approaches are essential for improving estimation precision, enhancing confidence in findings' replicability, and investigating interrelated questions within broader theoretical models [53]. However, the sheer heterogeneity of omics data comprising varied datasets from different modalities with completely different distributions presents a cascade of technical challenges involving unique scaling, normalization, and transformation requirements for each dataset [6]. Without effective infrastructure management and troubleshooting protocols, researchers risk creating resource-intensive workflows that fail to deliver proportional gains in analytical productivity or biological insight.
Troubleshooting Guide: Common Technical Issues in Data Integration
The following table outlines frequent technical problems encountered during heterogeneous data integration in multi-cohort studies, their potential causes, and evidence-based solutions.
Table 1: Troubleshooting Guide for Data Integration in Multi-Cohort Studies
| Error/Issue | Potential Cause | Solution |
|---|---|---|
| Missing values in combined datasets | Inconsistent data collection protocols across cohorts; technical variations in omics measurements [6] | Implement systematic imputation processes; apply statistical methods to infer missing values while accounting for uncertainty [6] |
| High-dimension, low sample size (HDLSS) problems | Numerous variables significantly outnumbering samples in pooled data [6] | Apply dimensionality reduction techniques; utilize regularization methods in machine learning algorithms to prevent overfitting [6] |
| Incompatible data formats and structures | Lack of standardized data capture, recording, and representation across different studies [7] | Implement data harmonization protocols; use standardized data transformation pipelines; establish common data models before integration [7] |
| Performance degradation after data pooling | Inefficient resource allocation; insufficient computing power for expanded datasets [54] | Implement proactive monitoring systems; optimize resource utilization; scale infrastructure through cloud solutions or virtualization [54] [55] |
| Unable to replicate findings across cohorts | Unaccounted technical batch effects; uncontrolled biological heterogeneity [53] | Apply batch effect correction algorithms; implement robust cross-validation strategies; utilize statistical methods designed for multi-study replication [53] |
Infrastructure Management Framework for Scalable Research
Core IT Infrastructure Management Components
Effective IT infrastructure management provides the foundation for overcoming technical bottlenecks in multi-cohort research. A well-managed research IT ecosystem encompasses physical hardware, software applications, networks, and data centers that collectively support data-intensive operations [54]. The primary objectives of such infrastructure management include maximizing uptime, ensuring application reliability, optimizing resource utilization, and implementing robust security measures to protect sensitive research data [54].
Key infrastructure management activities specifically relevant to multi-cohort research include:
- Asset Management: Tracking and managing hardware and software assets across distributed research environments, including servers, network devices, storage systems, and software licenses [55].
- Configuration Management: Maintaining and controlling configuration of infrastructure components to ensure consistency, stability, and compliance across research computing environments [55].
- Performance Monitoring: Continuously monitoring and analyzing infrastructure performance to identify bottlenecks, optimize resource utilization, and ensure optimal performance for computational workflows [55].
- Capacity Planning: Assessing and forecasting future computational and storage requirements to ensure infrastructure can meet evolving research needs as cohort datasets expand [55].
Strategic Approaches to Infrastructure Scaling
Several strategic approaches enable research infrastructure to scale effectively with the demands of multi-cohort data integration:
Virtualization: This transformative technology allows a single physical server to function as multiple virtual machines, enabling more efficient utilization of hardware resources [54]. For research institutions, virtualization enables workload consolidation onto fewer physical servers, maximizing resource utilization while reducing physical footprint, energy costs, and hardware expenses [54].
Cloud Computing: Cloud solutions offer on-demand, scalable resources that can adapt as research projects evolve [54]. The scalability of cloud computing is particularly valuable for multi-cohort research, allowing teams to quickly modify their IT infrastructure to accommodate fluctuating computational workloads and data storage demands [54].
Automation: Implementing automation for repetitive infrastructure management tasks streamlines operations and reduces human error [54]. Automated monitoring tools can continuously track system health and performance, enabling proactive issue identification before they disrupt research activities [54].
Software-Defined Networking (SDN): SDN offers significant advantages over traditional networking through centralized control and management, typically backed with an API to enable programmability [56]. This enables faster deployment and provisioning, enhanced automation and orchestration, improved network visibility and analytics, and better security and threat detection [56].
Diagram: Multi-Cohort Data Integration Workflow
Frequently Asked Questions (FAQs)
What are the most significant technical challenges when integrating heterogeneous data from multiple cohorts? The primary challenges include data heterogeneity with varying formats and structures, missing values resulting from inconsistent collection protocols, high-dimensionality with relatively small sample sizes (HDLSS problem), and computational infrastructure limitations when processing large combined datasets [7] [6]. Additionally, technical batch effects and uncontrolled biological heterogeneity can compromise the replicability of findings across different cohorts [53].
How can we effectively handle missing data in integrated multi-cohort datasets? Effective handling requires a multi-pronged approach: First, implement systematic imputation processes to infer missing values in incomplete datasets before statistical analysis [6]. Second, apply sensitivity analyses to understand the potential impact of missingness on results. Third, where possible, leverage the increased sample size of pooled data to use more robust missing data techniques that require larger sample sizes. Documentation of all missing data handling procedures is essential for transparency.
What infrastructure specifications are needed for scalable multi-cohort data integration? A scalable infrastructure should include: (1) Virtualization capabilities to maximize hardware resource utilization [54]; (2) Cloud computing resources for on-demand scaling [54]; (3) Automated monitoring and provisioning systems to maintain performance [54]; (4) Software-defined networking for flexible, programmable network management [56]; and (5) Robust security measures including encryption and access controls to protect sensitive research data [55].
What are the key differences between horizontal and vertical data integration approaches? Horizontal integration involves combining data from across different studies, cohorts, or labs that measure the same omics entities, typically generated from one or two technologies for a specific research question from a diverse population [6]. Vertical integration involves combining multi-cohort datasets from different omics levels (genome, transcriptome, proteome, etc.) measured using different technologies and platforms [6]. The techniques for one approach generally cannot be applied to the other, requiring specific methodological considerations.
How can we ensure the security of sensitive research data in integrated environments? Security requires a comprehensive approach including: implementation of robust security protocols and procedures such as user access controls and data encryption [54]; regular vulnerability assessments and security audits [55]; establishment of clear security policies and incident response processes [55]; and maintenance of comprehensive documentation of security protocols and compliance measures [55].
Essential Research Reagents and Computational Tools
Table 2: Research Reagent Solutions for Data Integration and Analysis
| Tool/Category | Primary Function | Application in Multi-Cohort Studies |
|---|---|---|
| Configuration Management Tools | Automate server, software, and network device configuration and provisioning [54] | Ensure consistency across research computing environments; simplify deployment and maintenance processes [54] |
| Monitoring Tools | Provide continuous visibility into performance and health of IT infrastructure components [55] | Proactively identify performance issues; track resource utilization; generate real-time alerts for computational workflow problems [55] |
| HYFT Framework | Tokenization of biological data to a common omics language through identification of atomic units of biological information [6] | Enable normalization and integration of diverse omics data sources; facilitate one-click integration of omics and non-omics data [6] |
| Cloud Monitoring Tools (Amazon CloudWatch, Azure Monitor) | Monitor performance and availability of cloud-based resources and applications [55] | Track utilization of cloud resources; optimize scaling parameters; manage costs in cloud-based research environments [55] |
| Security Monitoring Tools (Splunk Enterprise Security, IBM QRadar) | Monitor security events, detect vulnerabilities, and prevent unauthorized access [55] | Protect sensitive research data; ensure compliance with data governance policies; monitor for potential security breaches [55] |
| Data Harmonization Tools | Align and standardize heterogeneous data elements across different studies [7] | Match equivalent patient variables across different studies; clean, organize and combine diverse datasets into analysis-ready formats [7] |
Successful management of technical bottlenecks in multi-cohort research requires both robust infrastructure management practices and systematic troubleshooting methodologies. The complexity of heterogeneous data integration necessitates intentional approaches to system design, incorporating virtualization, cloud resources, automation, and software-defined networking to create scalable, adaptable research environments [54] [56]. Furthermore, researchers must acknowledge that data harmonization across studies remains complex and resource-intensive, highlighting the critical importance of implementing standards for data capture, recording, and representation from the initial study design phase [7].
While technical challenges will continue to evolve with advancing multi-omics technologies and expanding cohort sizes, the frameworks outlined in this technical support center provide researchers with actionable strategies for overcoming immediate bottlenecks while building infrastructure capable of supporting future research demands. By adopting these structured approaches to troubleshooting and infrastructure management, research teams can dedicate more time to scientific discovery rather than computational problem-solving, ultimately accelerating the pace of insights from multi-cohort studies.
Troubleshooting Guides
Guide 1: Resolving Variable Schema Mismatches Across Cohorts
Problem: Inconsistent variable names, formats, or units prevent merging datasets from different cohort studies. For example, one study uses "BMI" and another uses "BodyMassIndex," or blood pressure is recorded in different units.
Solution: Implement a systematic harmonization protocol.
Create a Data Dictionary Crosswalk: Manually map all variables from each source dataset to a common set of target variables [7] [13].
- Action: Develop a spreadsheet listing source variable names, descriptions, and formats from each cohort alongside the unified target variable.
- Example:
Target Variable Cohort A Source Variable Cohort B Source Variable Transformation Needed height_cmheight_inheightConvert inches to cm for Cohort A diabetes_status|diab_flag (0/1)t2d (YES/NO)Map both to standard (YES/NO) Automate Mapping with Advanced Tools: For large-scale projects, use tools that leverage semantic and distribution-based learning to suggest variable mappings [28].
- Action: Platforms like the SONAR algorithm use variable descriptions and patient-level data distributions to find similar concepts across cohorts [28].
Execute Schema Transformation: Use ETL (Extract, Transform, Load) scripts or data pipeline tools to apply the mappings and transformations, converting all data into the unified schema [57] [58].
Guide 2: Addressing Missing and Incomplete Data
Problem: Required data fields are sporadically missing or entire patient subgroups are unrepresented, compromising dataset completeness and statistical power [13] [59].
Solution: Apply completeness validation and imputation techniques.
Run Completeness Tests: Systematically check for null or empty values in mandatory fields [57] [60] [58].
- Action: Use automated data quality tools to profile datasets and report on the percentage of missing values per critical variable [60].
Analyze Missingness Pattern: Determine if data is missing completely at random, or if there is a bias (e.g., data is missing for a specific patient subgroup) [13].
- Action: Cross-tabulate missingness against anchor variables like age, sex, and recruitment site.
Implement a Handling Strategy:
- For a small amount of missing data: Consider complete-case analysis.
- For non-critical missing data: Use imputation methods (e.g., mean/median imputation for continuous variables, model-based imputation for complex patterns) [6]. Document all imputation procedures.
Guide 3: Correcting Data Format and Validity Errors
Problem: Data values are in the wrong format (e.g., text in numeric fields), violate business rules, or are duplicates, leading to processing failures and analytical errors.
Solution: Establish data validation checkpoints at every stage of the integration pipeline [58].
At Ingestion (Raw Data): Perform initial checks.
During Transformation (Cleaning & Mapping): Perform integrity checks.
Before Loading (Final Output): Perform reconciliation.
Data Validation Checkpoints in Pipeline
Frequently Asked Questions (FAQs)
Q1: What are the most critical data quality dimensions to check in multi-cohort studies?
The most critical dimensions are Completeness (all required data is present), Consistency (uniform representation across systems), Accuracy (data correctly represents real-world values), and Validity (data conforms to predefined syntax and formats) [57] [60] [58]. Focusing on these first prevents major analytical roadblocks.
Q2: Our team spent months manually harmonizing variables. Are there tools to automate this?
Yes. While manual curation is common, new automated and semi-automated tools are emerging. These include:
- Semantic Mapping Tools: These use natural language processing on variable descriptions to suggest matches [28].
- Data Quality Platforms: Tools like Great Expectations or Talend allow you to codify validation rules and run them automatically on new datasets [60] [58].
- Specialized Biomedical Platforms: Platforms like Polly use ontologies to standardize biological metadata, automating part of the harmonization process [59].
Q3: How can we ensure our harmonized data is reusable and compliant with FAIR principles?
Adopt community-driven data models and standards from the start. Using standardized formats like SDTM for clinical data or MIAME for microarray data ensures metadata is structured and discoverable [59]. Annotating metadata with ontology-backed terms (e.g., for disease, tissue type) is fundamental for making data Findable, Interoperable, and Reusable [59].
Q4: What is a realistic timeline for setting up a data quality framework for a new multi-cohort project?
Allocate a significant preparatory phase. Evidence from real projects suggests that just the process of obtaining approvals, achieving cohort consensus, and finalizing the study protocol can take a year or more before data processing even begins [13]. Building the quality framework is an integral part of this setup.
The Scientist's Toolkit: Essential Reagents for Data Harmonization
| Tool Category | Example / Solution | Primary Function in Harmonization |
|---|---|---|
| Data Quality Testing Frameworks | Great Expectations [58], dbt [60] | Codify and automate data validation rules (e.g., checks for nulls, duplicates, valid ranges). |
| Ontologies & Standardized Vocabularies | SNOMED CT, HUGO Gene Nomenclature | Provide standardized terms for metadata fields (e.g., disease, tissue), enabling consistent annotation and searchability [59]. |
| Semantic Harmonization Algorithms | SONAR (Semantic and Distribution-Based Harmonization) [28] | Use machine learning on variable descriptions and data distributions to automatically suggest mappings between cohort variables. |
| Biomedical Data Harmonization Platforms | Polly [59] | A platform that ingests, processes, and quality-controls biomedical data from diverse sources into a consistent, analysis-ready schema. |
| Pipeline Orchestration & Checkpoints | Apache Airflow, Prefect | Manage and automate the multi-step data validation and harmonization workflow, ensuring checks are executed in sequence [58]. |
| Checkpoint | Key Checks to Perform | Common Tools / Methods |
|---|---|---|
| Data Ingestion | Schema validation, Data type check, File/record count validation [58]. | Manual inspection, Great Expectations [58], Data profiling. |
| Data Staging | Field-level validation (format, range), Business rule compliance, Data completeness [58]. | SQL queries, Custom scripts, Open-source data quality tools [60]. |
| Data Transformation | Referential integrity, Transformation validation, Data consistency check [58]. | ETL/ELT tools (e.g., dbt [60]), Data reconciliation scripts. |
| Data Loading | Load validation (row counts), Target schema validation, Data reconciliation [58]. | Database constraints (UNIQUE, NOT NULL), Automated reconciliation reports. |
Data Quality Framework Lifecycle
Frequently Asked Questions
Q: My data processing job is failing due to insufficient memory. What steps can I take to resolve this? A: Out-of-memory errors are common with large datasets. You can:
- Increase Chunk Size: Process data in smaller, more manageable chunks rather than loading entire datasets into memory at once.
- Optimize Data Types: Convert data to more memory-efficient types (e.g., from 64-bit to 32-bit floating-point numbers).
- Utilize Disk-Based Processing: Use tools that spill excess data to disk rather than holding everything in RAM.
- Scale Hardware: If possible, allocate more RAM to your computational nodes or processing environment.
Q: How can I improve the execution speed of my long-running data analysis workflow? A: To enhance performance, consider the following strategies:
- Parallelize Code: Identify independent tasks and run them concurrently across multiple CPU cores.
- Leverage Distributed Computing: Use frameworks like Apache Spark to distribute workloads across a cluster of machines.
- Profile Code: Use profiling tools to pinpoint specific bottlenecks in your code, such as inefficient loops or functions.
Q: My workflow involves integrating multiple heterogeneous datasets, which often leads to format and schema inconsistencies. How can I manage this? A: Heterogeneous data integration requires a systematic approach:
- Establish Data Contracts: Define expected formats, schemas, and metadata requirements for all incoming data streams.
- Implement a Standardized Preprocessing Pipeline: Create a robust extraction, transformation, and loading (ETL) process that can handle various formats and validate data upon ingestion.
- Use Ontologies: Adopt or build domain-specific ontologies to create a common semantic framework for data from different sources, ensuring consistent interpretation.
Troubleshooting Guides
Problem: Job Fails with "MemoryError" This error occurs when a process requests more memory than the system can allocate.
- Diagnosis Steps:
- Check the error log to confirm the exception type (
MemoryError). - Use system monitoring tools (e.g.,
htop,top) to observe memory usage in real-time. - Review your code for operations that load large datasets entirely into memory.
- Check the error log to confirm the exception type (
- Solution Steps:
- Refactor for Sequential Chunking: Read and process data in chunks. For example, when using pandas, specify a
chunksizeinread_csv(). - Use Efficient Data Structures: Replace default data types with more efficient ones (e.g.,
int32instead ofint64if the value range allows). - Explicit Garbage Collection: Manually trigger the garbage collector to free up unused objects after large variables are no longer needed.
- Refactor for Sequential Chunking: Read and process data in chunks. For example, when using pandas, specify a
Problem: Workflow Execution is Unacceptably Slow Slow performance often stems from computational bottlenecks or inefficient resource use.
- Diagnosis Steps:
- Code Profiling: Run a code profiler to identify functions or lines of code with the longest execution times.
- Resource Monitoring: Check if CPU usage is consistently at 100% on a single core, indicating a lack of parallelization.
- Solution Steps:
- Implement Parallel Processing: Use libraries like
multiprocessingin Python or theparallelpackage in R to execute independent tasks simultaneously. - Optimize Algorithms: Replace inefficient algorithms (e.g., nested loops) with vectorized operations or more efficient alternatives.
- Utilize Caching: Cache the results of expensive function calls that are called with the same arguments to avoid recomputation.
- Implement Parallel Processing: Use libraries like
Problem: Data Integration Causes Schema Mismatches This occurs when merging datasets with different structures, column names, or data types.
- Diagnosis Steps:
- Profile each dataset individually to document its schema, including column names, data types, and value ranges.
- Identify specific points of failure, such as missing columns or type conversion errors.
- Solution Steps:
- Create a Data Mapping Schema: Develop a definitive mapping that aligns columns and formats from all source datasets to a unified master schema.
- Build a Flexible Ingestion Layer: Design your data ingestion code to handle schema variations gracefully, using data mapping for transformations.
- Validate and Log: After integration, run checks to ensure data consistency and completeness, and log any anomalies for review.
Experimental Protocols & Methodologies
Protocol 1: Resource Utilization Benchmarking This protocol measures the computational efficiency of a data processing workflow.
- Objective: To quantify the memory footprint and execution time of a data analysis pipeline under a standard workload.
- Materials: Standard dataset (e.g., a 50GB multi-cohort genomic association dataset), computing node with 64GB RAM and 16 CPU cores, resource monitoring software (e.g.,
time,psrecord). - Procedure:
- Step 1: Instrument the data processing script to log its start and end times.
- Step 2: Launch the resource monitoring tool to track the process's CPU and memory usage at one-second intervals.
- Step 3: Execute the data processing workflow on the standard dataset.
- Step 4: Terminate monitoring upon workflow completion.
- Data Analysis: Calculate total runtime, peak memory usage, and average CPU utilization from the monitoring logs. The goal is to identify if the workflow operates within the 64GB memory limit and utilizes available CPU cores effectively.
Protocol 2: Data Integration Fidelity Testing This protocol validates the success of a heterogeneous data integration process.
- Objective: To ensure that the integrated dataset preserves all critical information from the source cohorts without introducing errors.
- Materials: Source datasets (Cohort A, B, C), data integration pipeline, validation framework script.
- Procedure:
- Step 1: Run the source datasets through the integration pipeline to produce a unified master dataset.
- Step 2: Execute a row-count check: the sum of unique keys from source datasets should match the count in the master dataset.
- Step 3: Perform statistical fidelity checks: compare the summary statistics (mean, standard deviation) of key numerical variables in each source cohort against the same cohort's data within the master dataset.
- Data Analysis: A successful integration is confirmed if the row counts match and the summary statistics for each cohort pre- and post-integration are identical, indicating no data loss or corruption.
The following table summarizes key performance metrics from resource benchmarking experiments on three different data processing strategies.
Table 1: Performance Comparison of Data Processing Strategies
| Processing Strategy | Average Execution Time (min) | Peak Memory Usage (GB) | CPU Utilization (%) | Data Integrity Score (%) |
|---|---|---|---|---|
| In-Memory (Single Machine) | 45.2 | 58.1 | 98 | 100 |
| Chunked Sequential Processing | 68.5 | 12.3 | 65 | 100 |
| Distributed Computing (4 nodes) | 18.7 | 16.5 (per node) | 92 | 100 |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools for Large-Scale Data Processing
| Item | Function |
|---|---|
| Workflow Management System (e.g., Nextflow, Snakemake) | Orchestrates complex, multi-step data analysis pipelines, ensuring reproducibility and managing software dependencies. |
| Distributed Data Framework (e.g., Apache Spark, Dask) | Enables parallel processing of massive datasets that are too large for a single machine by distributing data and computations across a cluster. |
| Containerization Platform (e.g., Docker, Singularity) | Packages analysis code, dependencies, and runtime environment into a single, portable unit, guaranteeing consistent execution across different computing environments. |
| High-Performance Computing (HPC) Scheduler (e.g., SLURM, PBS Pro) | Manages and allocates computational resources (CPUs, memory) across multiple users and jobs in a shared cluster environment. |
| In-Memory Data Store (e.g., Redis) | Provides a ultra-fast caching layer for frequently accessed data or intermediate results, significantly speeding up iterative computations. |
Workflow and Signaling Diagrams
The following diagrams, generated with Graphviz, illustrate core concepts and workflows described in this article.
Data Processing Strategy Comparison
Heterogeneous Data Integration
Resource Troubleshooting Logic
Troubleshooting Guide: Common Data Integration Errors
This guide addresses specific issues researchers encounter when integrating heterogeneous data from multi-cohort studies and provides step-by-step solutions.
Variable Mapping and Join Errors
Problem: Unable to join datasets from different cohorts due to column name mismatches or structural differences.
Error Message Examples:
'job_code' column not found in rhs, cannot join[62]- Data misalignment after concatenating DataFrames, with unexpected
NaNvalues [63]
Diagnosis Steps:
- Verify column names exist in both datasets using
names()in R or.columnsin Python. [62] [64] - Check for case sensitivity differences (e.g.,
JOB_CODEvs.job_code). [62] - Inspect data types and structures using
str()ordtypeto ensure compatibility. [63] - Confirm the joining key (e.g.,
job_code) is correctly specified in the function call. [62]
Resolution Protocol:
- For case sensitivity or naming differences: Use a named vector in the join function. For example, in R:
by = c("JOB_CODE" = "job_code"). [62] - For data type mismatches: Convert columns to consistent types before joining (e.g., using
pd.to_numeric()oras.character()). [64] - For structural misalignment when appending data: Ensure DataFrames have identical column names when using
append()orconcat(). Explicitly set column names after reading data if they are not defined in the source file. [63]
Data Quality and Consistency Errors
Problem: Integrated data shows inconsistencies, missing values, or failed validation checks, compromising analysis validity.
Error Message Examples:
- Validation errors in the target system due to bad or missing source data. [65]
- Hidden
NULLvalues or placeholder codes (e.g.,-999) from source cohorts propagating to the integrated dataset.
Diagnosis Steps:
- Profile data to identify missing values, outliers, and invalid entries using
summary()orisnull().sum(). [66] - Run cross-tabulations or frequency counts on key categorical variables to spot inconsistencies. [23]
- Check for systematic coding differences (e.g., "M/F" vs. "1/2" for sex) across cohorts. [23]
Resolution Protocol:
- Implement proactive data validation: Check for errors or inconsistencies immediately after data collection, before integration. [66]
- Create a data quality management plan: Define and implement rules for handling missing data, outliers, and value transformations. [66]
- Use a mapping table: For variables collecting the same data but with different coding schemes, use a user-defined mapping table to recode values to a consistent standard. [23]
- Establish data governance policies: Implement clear guidelines for data entry, storage, and management in source systems to prevent quality issues at the origin. [66]
Semantic Heterogeneity Errors
Problem: Datasets appear to integrate successfully, but underlying differences in data meaning or collection methods lead to erroneous results.
Error Message Examples:
- No direct error message, but statistical models fail or produce nonsensical effect estimates.
- Incorrect analysis results due to subtle differences in how questions were phrased or measurements were taken across cohorts.
Diagnosis Steps:
- Carefully compare the source data dictionaries and study protocols for all cohorts. [23]
- Conduct a pilot analysis on a subset of harmonized variables to check for face validity. [23]
- Use visualization (e.g., histograms, scatter plots) to compare distributions of key variables across cohorts before and after integration.
Resolution Protocol:
- Prospective harmonization: Before data collection, align variable definitions, measurement units, and questionnaire items across participating studies. [23]
- Define a common data model: Create a target schema that all source data is mapped to, specifying allowed values, formats, and meanings. [23]
- Involve domain experts: Epidemiologists, psychologists, and other subject matter experts should be involved in working groups to select questions and ensure measured constructs are equivalent. [23]
- Document everything: Maintain detailed metadata describing all original sources, transformations applied, and any assumptions made during the harmonization process. [67]
Frequently Asked Questions (FAQs)
1. What are the first steps in creating a data governance framework for multi-cohort research?
Begin by establishing data governance and data stewardship policies. This involves creating a common data language for consistent interpretation and use across teams. Assign data stewards to guide strategy, implement policies, and connect IT teams with business planners to ensure compliance with standards [66]. For multi-cohort studies, this also involves prospective variable mapping and defining a core set of shared data elements before data collection begins [23].
2. Our team uses different column names for the same variable. How can we fix this during integration?
This is a common challenge. The solution involves:
- Creating a data mapping table: Document the source variable from each cohort and its corresponding destination variable in the integrated dataset [23].
- Using explicit syntax in joins: When using tools like R's dplyr, specify the relationship with a named vector:
by = c("SourceColumn" = "TargetColumn")[62]. - Implementing ETL (Extract, Transform, Load) processes: Use these processes to systematically rename and transform columns into a consistent format during the integration workflow [23] [66].
3. How can we effectively track and manage changes in data structure over time (schema drift)?
Schema drift is a major challenge in heterogeneous data management [25]. Mitigate it by:
- Using adaptive integration solutions: Choose tools that are flexible and scalable to handle changes in source systems [66].
- Implementing robust metadata management: Track metadata from various sources and use common standards to integrate it in a central system [25].
- Regular monitoring and ecosystem verification: Continuously check the reliability and performance of data integration tools and workflows [66].
- Establishing a change management protocol: Define a clear process for communicating and implementing schema changes across all participating cohorts.
4. What is the most effective way to handle data from different formats (CSV, JSON, databases) in one analysis?
Adopt a unified access and storage abstraction layer. This software layer provides a standard interface for interacting with diverse underlying storage systems and access methods, regardless of their complexity or location [25]. Furthermore, leverage transformation and normalization engines that can prepare raw data from various formats for modeling, addressing issues like outlier handling and encoding categorical data [25].
5. How do we ensure data security and privacy when integrating sensitive cohort data?
- Protect sensitive data: Apply security measures like encryption, pseudonymization, and access controls to prevent unauthorized access [66].
- Use secure platforms: Utilize data management platforms compliant with regulations like HIPAA and GDPR, and leverage their built-in, role-based security features [23].
- Governance frameworks for compliance: Implement governance frameworks that work with access restrictions, metadata libraries, and policy engines to ensure data is used ethically and safely [25].
Heterogeneous Data Integration Workflow
The diagram below outlines the core workflow for integrating data from multiple cohort studies, from initial mapping to final quality assurance.
Research Reagent Solutions: Data Integration Tools
The table below lists essential tools and methodologies for managing heterogeneous data integration in research environments.
| Tool/Methodology | Primary Function | Key Application in Multi-Cohort Studies |
|---|---|---|
| ETL Tools [23] [66] | Extract, Transform, and Load data from disparate sources. | Implements the core harmonization process; transforms cohort-specific data formats and codes into a unified structure. |
| REDCap API [23] | Application Programming Interface for REDCap data management platform. | Enables secure, automated data extraction and pooling from multiple REDCap-based cohort studies into an integrated database. |
| Data Mapping Tools [66] | Visualize data structure and relationships between source and target systems. | Aids in understanding and documenting how variables from different cohorts correspond to each other, reducing mapping errors. |
| Data Quality Management Systems [66] | Automate data cleansing, standardization, and validation. | Identifies and rectifies errors and discrepancies (e.g., outliers, missing patterns) in the integrated dataset before analysis. |
| Centralized Data Storage [66] | A consolidated system (e.g., data warehouse) for storing integrated data. | Simplifies access and management of the final harmonized dataset, ensuring all analysts work from a single source of truth. |
Conclusion
Successful integration of heterogeneous data across multiple cohorts requires a systematic approach that addresses foundational challenges, implements robust methodologies, proactively troubleshoots issues, and rigorously validates outcomes. The future of multi-cohort research lies in developing more automated harmonization tools, adopting standardized data models, and creating flexible frameworks that can adapt to evolving data types and research questions. By mastering these integration principles, researchers can unlock the full potential of collaborative studies, accelerating discoveries in precision medicine and therapeutic development while ensuring scientific rigor and reproducibility across diverse populations.
References
- 1. Working with Semi-Structured & Unstructured Data in ... [https://hakkoda.io/resources/unstructured-data-in-healthcare/]
- 2. How structured data is used in clinical trials [https://ignitedata.com/how-structured-data-is-used-in-clinical-trials/]
- 3. Challenges and best practices for digital unstructured data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10566734/]
- 4. Unstructured data | Fast Data Science [https://fastdatascience.com/natural-language-processing/unstructured-data/]
- 5. Semistructured Data - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/computer-science/semistructured-data]
- 6. Challenges in multi-omics data integration [https://www.mindwalkai.com/blog/challenges-in-multi-omics-data-integration]
- 7. Heterogeneity and Complexity in Clinical Trials and Patient ... [https://pubmed.ncbi.nlm.nih.gov/32580708/]
- 8. Merging heterogeneous clinical data to enable knowledge ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6447393/]
- 9. Biomedical heterogeneous data categorization and ... [https://www.frontiersin.org/journals/big-data/articles/10.3389/fdata.2023.1173038/full]
- 10. Horizontal and vertical integrative analysis methods for ... [https://www.nature.com/articles/s41598-019-49718-5]
- 11. Vertical integration methods for gene expression data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8138889/]
- 12. Vertical and horizontal integration of multi-omics data with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6902525/]
- 13. Collaborative Challenges of Multi-Cohort Projects in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9562084/]
- 14. A Case Study Using EXACOS-CV Studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12176119/]
- 15. Opportunities and Challenges of Using Big Data to Detect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6617974/]
- 16. Extracting data from heterogeneous sources ... [https://milvus.io/ai-quick-reference/what-challenges-arise-when-extracting-data-from-heterogeneous-sources]
- 17. Handling missing data in clinical research [https://pubmed.ncbi.nlm.nih.gov/36150546/]
- 18. Missing Data in Clinical Research: A Tutorial on Multiple ... [https://pubmed.ncbi.nlm.nih.gov/33276049/]
- 19. Missing Data in Clinical Research: A Tutorial on Multiple ... [https://www.sciencedirect.com/science/article/pii/S0828282X20311119]
- 20. What is HDLSS?. High-dimensional low-sample size… | by [https://vtiya.medium.com/what-is-hdlss-c6663c28d484]
- 21. Random Forest Kernel for High-Dimension Low Sample ... [https://arxiv.org/abs/2310.14710]
- 22. Embracing cohort heterogeneity in clinical machine ... [https://www.nature.com/articles/s41598-023-35557-y]
- 23. Harmonization and integration of data from prospective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109133/]
- 24. Understanding Schema Drift | Causes, Impact & Solutions [https://www.acceldata.io/blog/schema-drift]
- 25. Heterogeneous Data: Use Cases, Tools & Best Practices [https://lakefs.io/blog/heterogeneous-data/]
- 26. Data Privacy in 2025: 7 Trends Every CDO Needs to ... [https://www.alation.com/blog/data-privacy-in-2025-trends/]
- 27. 65+ Data Privacy Statistics 2025 | Key Breaches & Insights [https://data.folio3.com/blog/data-privacy-stats/]
- 28. Robust Automated Harmonization of Heterogeneous Data ... [https://medinform.jmir.org/2025/1/e54133]
- 29. Avoid 3 data integration mistakes that cost millions [https://www.ibm.com/think/insights/avoid-3-data-integration-mistakes-that-cost-millions]
- 30. Top 9 Data Integration Problems and Solutions in 2025 [https://www.rapidionline.com/blog/data-integration-problems]
- 31. Heterogeneous data integration: Challenges and opportunities [https://pmc.ncbi.nlm.nih.gov/articles/PMC11402636/]
- 32. Top 12 Data Integration Challenges & Solutions in 2025- ... [https://www.ksolves.com/blog/big-data/data-integration-challenges-and-solutions]
- 33. A General Primer for Data Harmonization | Scientific Data [https://www.nature.com/articles/s41597-024-02956-3]
- 34. and integration of data from Harmonization ... prospective cohort [https://pubmed.ncbi.nlm.nih.gov/40433195/]
- 35. BIcenter-AD: Harmonising Alzheimer's Disease cohorts ... [https://www.sciencedirect.com/science/article/pii/S2352914822002702]
- 36. Learning Hub | Retrospective vs prospective harmonisation [https://learning.closer.ac.uk/learning-modules/data-harmonisation/retrospective-vs-prospective-harmonisation/]
- 37. A methodology for cohort harmonisation in multicentre ... [https://www.sciencedirect.com/science/article/pii/S2352914821002343]
- 38. Integration strategies of multi-omics data for machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8258788/]
- 39. Multi-omics data integration using ratio-based quantitative ... [https://www.nature.com/articles/s41587-023-01934-1]
- 40. Integrating Multi-Omics Data: Methods and Applications in ... [https://www.sciencedirect.com/science/article/pii/S2215017X25000657]
- 41. An Introduction to Semantic Matching Techniques in NLP ... [https://medium.com/georgian-impact-blog/an-introduction-to-semantic-matching-techniques-in-nlp-and-computer-vision-c22bf3cee8e9]
- 42. Data harmonization and federated learning for multi-cohort ... [https://www.sciencedirect.com/science/article/pii/S1532046424000790]
- 43. BIMSBbioinfo/flexynesis: A deep-learning based multi- ... [https://github.com/BIMSBbioinfo/flexynesis]
- 44. Getting Started - Flexynesis Documentation [https://bimsbstatic.mdc-berlin.de/akalin/buyar/flexynesis/site/getting_started/]
- 45. Adaptive multi-omics integration framework for breast ... [https://www.nature.com/articles/s41598-025-22202-z]
- 46. Flexynesis: A deep learning toolkit for bulk multi-omics data ... [https://www.nature.com/articles/s41467-025-63688-5]
- 47. Multimodal Integration in Health Care - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12370271/]
- 48. Clinical Research Technology: 10 Powerful Innovations in ... [https://lifebit.ai/blog/clinical-research-technology/]
- 49. Statistical data preparation: management of missing values ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5548942/]
- 50. Mastering Data Cleaning Techniques: Handling Missing ... [https://medium.com/@nikhilmalkari18/mastering-data-cleaning-techniques-handling-missing-values-outliers-and-inconsistencies-a0581a949829]
- 51. 14 Most Common Data Quality Issues and How to Fix Them [https://lakefs.io/data-quality/data-quality-issues/]
- 52. Assessing Data Quality in Heterogeneous Health Care ... [https://medinform.jmir.org/2025/1/e75275]
- 53. Advancing life course research through multi-cohort ... [https://www.sciencedirect.com/science/article/pii/S1040260822000399]
- 54. What Is IT Infrastructure Management? [https://www.atlassian.com/itsm/it-operations/it-infrastructure-management]
- 55. IT Infrastructure Management: Streamlining Operations ... [https://www.scalecomputing.com/resources/it-infrastructure-management]
- 56. Advanced managed services for scalable IT infrastructure [https://whitespider.com/it-infrastructure-services/]
- 57. Data Quality Testing: Key Techniques & Best Practices [2025] [https://atlan.com/data-quality-testing/]
- 58. Data Integrity in a Data Pipeline: Best Practices and ... [https://medium.com/@georgemichaeldagogomaynard/data-integrity-in-a-data-pipeline-best-practices-and-strategies-for-data-quality-checks-dim-71af7a3bf21e]
- 59. Data Quality in Early-Stage Drug Development [https://www.elucidata.io/blog/data-quality-in-early-stage-drug-development]
- 60. The Ultimate Guide to Data Quality Testing: Ensure ... [https://www.6sigma.us/six-sigma-in-focus/data-quality-testing/]
- 61. The Best 10 Data Validation Best Practices in 2025 [https://numerous.ai/blog/data-validation-best-practices]
- 62. Error with R dplyr left_join [https://stackoverflow.com/questions/40536953/error-with-r-dplyr-left-join]
- 63. Python Pandas Data not aligned correctly [https://stackoverflow.com/questions/62123237/python-pandas-data-not-aligned-correctly]
- 64. Common Pandas Errors [https://medium.com/@whyamit404/common-pandas-errors-6b7883dc744c]
- 65. How to handle data integration errors [https://www.rapidionline.com/blog/data-integration-error]
- 66. 11+ Most Common Data Integration Challenges & Solutions [https://estuary.dev/blog/data-integration-challenges/]
- 67. Heterogeneous data integration: Challenges and ... [https://www.sciencedirect.com/science/article/pii/S2352340924008175]