Harnessing Directed Evolution and Whole-Genome Sequencing to Decode Antimicrobial Resistance
This article provides a comprehensive overview for researchers, scientists, and drug development professionals on the synergistic application of directed evolution and whole-genome sequencing (WGS) to identify and characterize antimicrobial resistance...
Harnessing Directed Evolution and Whole-Genome Sequencing to Decode Antimicrobial Resistance
Abstract
This article provides a comprehensive overview for researchers, scientists, and drug development professionals on the synergistic application of directed evolution and whole-genome sequencing (WGS) to identify and characterize antimicrobial resistance (AMR) genes. It covers the foundational principles of mimicking natural evolution in the lab and leveraging high-throughput sequencing technologies. The scope extends to detailed methodological pipelines, from library generation and in vivo mutagenesis to bioinformatic analysis using tools like CARD and ResFinder. It further addresses troubleshooting for experimental and computational challenges and offers a comparative analysis against traditional phenotypic methods. The goal is to equip professionals with the knowledge to accelerate the discovery of resistance mechanisms and inform the development of novel therapeutics.
The Evolutionary Engine: Principles of Directed Evolution and WGS for AMR Discovery
Directed evolution is a powerful protein engineering method that mimics the process of natural selection in a laboratory setting to steer proteins or nucleic acids toward user-defined goals [1]. This approach harnesses natural evolutionary principles but operates on a much shorter timescale, enabling the rapid selection of biomolecule variants with properties that make them more suitable for specific applications [2]. Since the first in vitro evolution experiments performed by Sol Spiegelman in 1967, a wide range of techniques have been developed to tackle the two main steps of directed evolution: genetic diversification (library generation) and isolation of variants of interest [2] [1]. The development of directed evolution methods was recognized with the awarding of the 2018 Nobel Prize in Chemistry to Frances Arnold for the evolution of enzymes, and to George Smith and Gregory Winter for phage display [1].
Directed evolution functions through iterative rounds of mutagenesis (creating a library of variants), selection (expressing those variants and isolating members with the desired function), and amplification (generating a template for the next round) [1]. This process can be performed in vivo (in living organisms) or in vitro (in cells or free in solution) [1]. The fundamental requirement for evolution—variation between replicators, fitness differences upon which selection acts, and heritable variation—is maintained throughout these iterative cycles [1]. The likelihood of success in a directed evolution experiment is directly related to the total library size, as evaluating more mutants increases the chances of finding one with the desired properties [1].
Core Principles and Methodologies
The Directed Evolution Workflow
The directed evolution cycle consists of three fundamental steps that are repeated iteratively: diversification, selection, and amplification. This systematic approach enables researchers to navigate vast sequence spaces efficiently to identify variants with improved or novel functions.
Library Creation Methods
The first step in directed evolution involves creating genetic diversity through various mutagenesis techniques. The choice of method depends on the specific engineering goals, available structural information, and desired library size.
Table 1: Common Genetic Diversification Methods in Directed Evolution
| Method | Mechanism | Advantages | Disadvantages | Typical Applications |
|---|---|---|---|---|
| Error-prone PCR | Random point mutations via low-fidelity PCR | Easy to perform; no prior knowledge needed | Reduced sampling of mutagenesis space; mutagenesis bias | Subtilisin E, Glycolyl-CoA carboxylase [2] |
| DNA Shuffling | Random sequence recombination of parental genes | Recombination advantages; accesses new combinations | High homology between parental sequences required | Thymidine kinase, Non-canonical esterase [2] |
| Site-Saturation Mutagenesis | Focused mutagenesis of specific positions | In-depth exploration of chosen positions; smart libraries reduce size | Libraries can become very large; only a few positions mutated | Widely applied to enzyme evolution [2] |
| RAISE | Insertion of random short insertions and deletions | Enables random indels across sequence | Introduces frameshifts | β-Lactamase evolution [2] |
| Gene Shuffling | Fragmentation and recombination of related sequences | Combines beneficial mutations from different parents | Requires multiple parent sequences | Antibody engineering [3] |
Selection and Screening Strategies
After generating variant libraries, the critical challenge lies in identifying the rare improved variants from the vast majority of neutral or deleterious mutations. The selection strategy is typically determined by the availability of high-throughput assays and the specific property being engineered.
Table 2: Selection and Screening Methods in Directed Evolution
| Method | Principle | Throughput | Advantages | Limitations |
|---|---|---|---|---|
| Display Techniques (Phage, Yeast) | Physical linkage of genotype to phenotype | Very High (10^7-10^11) | Extremely high throughput; direct selection | Limited to binding properties; not ideal for enzymes [2] [1] |
| FACS-based Methods | Fluorescence-activated cell sorting | High (10^7-10^9) | Very high throughput; quantitative | Requires fluorescence coupling [2] [4] |
| Colorimetric/Fluorimetric Assays | Colony-based screening with chromogenic substrates | Medium (10^3-10^6) | Simple, inexpensive; direct activity measurement | Limited to specific spectral properties [2] |
| In vivo Selection | Coupling desired function to cell survival | Ultra High (Limited by transformation efficiency) | Extremely high throughput; minimal equipment | Difficult to engineer; prone to artifacts [1] |
| MS-based Methods | Mass spectrometry for product detection | Medium (10^3-10^4) | Does not rely on specific substrate properties | Requires specialized equipment [2] |
Experimental Protocols
Protocol 1: Error-Prone PCR for Random Mutagenesis
Purpose: To introduce random point mutations throughout a target gene sequence for creating diverse variant libraries.
Materials:
- Target DNA template (10-100 ng)
- Taq DNA polymerase or other low-fidelity polymerase
- dNTP mixture (standard concentration)
- PCR primers specific to target gene
- MgCl₂ (additional may be required)
- MnCl₂ (optional, to increase error rate)
Procedure:
- Prepare Reaction Mix:
- Combine in a PCR tube: 10-100 ng DNA template, 1× PCR buffer, 0.2 mM each dNTP, 0.5 μM each primer, 5-7 mM MgCl₂, 0.1-0.5 mM MnCl₂ (optional), and 2.5 U Taq polymerase.
- Adjust total volume to 50 μL with nuclease-free water.
PCR Amplification:
- Initial denaturation: 94°C for 3 minutes
- 25-30 cycles of:
- Denaturation: 94°C for 30 seconds
- Annealing: 45-65°C (primer-specific) for 30 seconds
- Extension: 72°C for 1 minute per kb of template
- Final extension: 72°C for 7 minutes
Purification and Cloning:
- Purify PCR product using standard methods
- Clone into appropriate expression vector
- Transform into competent cells for library generation
Notes: Error rate can be modulated by adjusting Mg²⁺ concentration, adding Mn²⁺, using unequal dNTP concentrations, or increasing template concentration [3]. The mutation rate should be optimized to typically 1-5 amino acid substitutions per gene.
Protocol 2: Phage Display for Binding Selection
Purpose: To select protein variants (e.g., antibodies, peptides) with enhanced binding properties from large libraries.
Materials:
- Phage display library (10^9-10^11 diversity)
- Target antigen for selection
- Immunotubes or microtiter plates
- Washing buffers (PBS with 0.1% Tween-20)
- Elution buffer (0.1 M glycine-HCl, pH 2.2)
- Neutralization buffer (1 M Tris-HCl, pH 9.0)
- E. coli host strain for phage amplification
Procedure:
- Panning Round:
- Coat immunotube with 10-100 μg/mL target antigen in PBS overnight at 4°C
- Block with 2% milk-PBS for 2 hours at room temperature
- Add phage library (10^11-10^12 phage) in 2% milk-PBS, incubate 1-2 hours with rotation
- Wash 10-20 times with PBS-0.1% Tween-20, then with PBS alone
Elution and Amplification:
- Elute bound phage with 1 mL glycine buffer (10 minutes, room temperature)
- Neutralize with 0.5 mL Tris buffer
- Infect log-phase E. coli with eluted phage for amplification
- Precipitate amplified phage with PEG/NaCl for next panning round
Iterative Selection:
- Repeat panning for 3-5 rounds with increasing stringency
- After final round, plate infected bacteria for individual clone analysis
- Screen individual clones for binding specificity and affinity
Notes: Selection stringency can be increased by reducing antigen concentration, increasing wash number, or adding competitors in later rounds [1]. The diversity of the output library should be monitored to avoid selection of overly dominant clones.
Research Reagent Solutions
Successful directed evolution campaigns require specialized reagents and tools for creating diversity, expressing variants, and measuring improved functions.
Table 3: Essential Research Reagents for Directed Evolution
| Reagent/Tool | Function | Application Examples | Considerations |
|---|---|---|---|
| Taq Polymerase | Low-fidelity PCR for random mutagenesis | Error-prone PCR for library generation | Naturally lower fidelity than high-fidelity polymerases [3] |
| NNK Degenerate Primers | Saturation mutagenesis of specific codons | Targeted diversification of active sites | NNK codons encode all 20 amino acids with only one stop codon [5] |
| Yeast Display System | Surface display for eukaryotic protein expression | Antibody engineering, protein stability | Allows for eukaryotic post-translational modifications [3] |
| Phage Display Vectors | Surface display on bacteriophage | Peptide and antibody selection | High diversity libraries (10^9-10^11 variants) [1] |
| Fluorescence-Activated Cell Sorter (FACS) | High-throughput screening based on fluorescence | Enzyme engineering with coupled assays | Can screen >10^7 variants per hour [2] [4] |
| Comprehensive Antibiotic Resistance Database (CARD) | Reference database for resistance genes | Analysis of evolved antibiotic resistance | Uses Resistance Gene Identifier (RGI) for prediction [6] |
Integration with Whole-Genome Sequencing for Resistance Gene Identification
The integration of directed evolution with whole-genome sequencing (WGS) has created powerful synergies for understanding and engineering resistance mechanisms. WGS enables comprehensive analysis of evolved variants, moving beyond single-gene studies to organism-level resistance profiling.
Directed evolution experiments have demonstrated that resistance to extended-spectrum β-lactams in Gram-negative bacteria can be accurately predicted from WGS data. In one study, WGS predictions showed sensitivity of 0.87, specificity of 0.98, positive predictive value of 0.97, and negative predictive value of 0.91 for identifying resistance to β-lactams used in treating neutropenic fever [7]. This approach successfully identified 133 putative instances of resistance, 65% of which would not have been detected by typical PCR-based methods targeting only β-lactamase genes [7].
Bioinformatics tools and databases play a crucial role in analyzing WGS data for resistance gene identification:
- CARD (Comprehensive Antibiotic Resistance Database): A rigorously curated resource using the Antibiotic Resistance Ontology (ARO) for classification [6]
- ResFinder/PointFinder: Specialized tools for identifying acquired AMR genes and chromosomal point mutations [6]
- DeepARG: Machine learning-based tool for identifying novel or low-abundance ARGs [6]
Benchmarking datasets have been developed to standardize AMR gene detection from WGS data, containing 174 bacterial genomes representing 22 species with curated resistance profiles [8]. These resources enable robust comparison of different computational approaches for resistance gene identification.
Advanced Applications and Future Directions
Machine Learning-Enhanced Directed Evolution
Recent advances have integrated machine learning with directed evolution to overcome limitations of traditional approaches. Active Learning-assisted Directed Evolution (ALDE) represents a cutting-edge development that uses uncertainty quantification to explore protein sequence space more efficiently [5].
In the ALDE workflow:
- A combinatorial design space on k residues is defined (20^k possible variants)
- Initial sequence-fitness data is collected through wet-lab screening
- Machine learning models predict fitness across sequence space
- Acquisition functions balance exploration and exploitation to select next variants
- Iterative cycles continue until fitness is optimized [5]
This approach has demonstrated remarkable efficiency in challenging engineering landscapes. In one application, ALDE optimized five epistatic residues in a protoglobin active site for a non-native cyclopropanation reaction, improving yield from 12% to 93% in just three rounds while exploring only ~0.01% of the design space [5].
High-Throughput Measurement Technologies
The effectiveness of directed evolution campaigns increasingly depends on high-throughput measurement (HTM) technologies that can quantitatively characterize genotype-phenotype relationships. Recent innovations include:
- Sort-seq: Combining fluorescence-activated cell sorting with deep sequencing [4]
- Deep mutational scanning: Comprehensive assessment of mutation effects [4]
- Repurposed sequencing flow cells: For in vitro characterization of binding kinetics [4]
These approaches enable quantitative characterization of up to 10^6 protein variants, providing rich datasets that fuel machine learning predictions and expand engineering capabilities [4]. The integration of HTMs with laboratory automation through biofoundries further accelerates the design-build-test-learn cycle in directed evolution [4].
Directed evolution has matured from a specialized protein engineering technique to a robust methodology that mimics natural selection in laboratory settings. The integration of whole-genome sequencing provides comprehensive analysis of evolved variants, while machine learning approaches like ALDE offer promising directions for navigating complex fitness landscapes more efficiently. As high-throughput measurement technologies continue to advance, directed evolution will remain an essential tool for engineering biological systems with precise specifications, from therapeutic antibodies to environmentally-friendly biocatalysts. The continued development of standardized protocols, benchmarking datasets, and computational resources will further enhance the reproducibility and impact of directed evolution across basic research and applied biotechnology.
The evolution of DNA sequencing technologies, from the Sanger chain-termination method to modern massively parallel next-generation sequencing (NGS) platforms, has fundamentally transformed biological research and clinical applications. This technological shift has been particularly impactful in the field of directed evolution and antimicrobial resistance (AMR) research, enabling comprehensive analysis of entire genomes with unprecedented speed and resolution. Where Sanger sequencing once provided a reliable but narrow snapshot of genetic information, whole-genome sequencing (WGS) now offers researchers a powerful tool to observe genetic changes across entire organisms, track the emergence of resistance mechanisms, and engineer improved biomolecules through directed evolution approaches.
The transition between these sequencing eras represents more than just incremental improvement—it constitutes a paradigm shift in experimental capabilities. While Sanger sequencing remains suitable for interrogating single genes or small genomic regions, NGS technologies empower scientists to sequence hundreds to thousands of genes simultaneously, providing the comprehensive genetic landscape necessary for identifying novel resistance genes, understanding complex evolutionary pathways, and accelerating drug discovery pipelines [9] [10].
Technological Evolution: From Sanger to Next-Generation Sequencing
Fundamental Principles and Historical Context
First developed in 1977 by Frederick Sanger and colleagues, the chain-termination method formed the foundation of DNA sequencing for decades [10]. This technique relies on DNA polymerase to synthesize complementary strands to a single-stranded DNA template, with the incorporation of fluorescently-labeled dideoxynucleotides (ddNTPs) randomly terminating strand elongation. The resulting fragments are separated by capillary electrophoresis, generating a sequence readout based on their terminal ddNTPs [9]. Automated Sanger sequencing significantly advanced the field, enabling milestone projects like the first complete bacterial genome sequencing of Haemophilus influenzae in 1995, which required substantial time and resources [10].
The critical distinction of NGS technologies lies in their massively parallel sequencing approach. While Sanger sequencing processes a single DNA fragment per run, NGS simultaneously sequences millions of fragments, dramatically increasing throughput and reducing costs [9]. This parallelization enables researchers to sequence entire genomes in hours rather than years, at a fraction of the previous cost [10]. The underlying biochemistry varies across NGS platforms, with Illumina employing sequencing-by-synthesis with reversible dye terminators, Pacific Biosciences utilizing single-molecule real-time sequencing, and Oxford Nanopore relying on electronic signal detection as DNA passes through protein nanopores [10] [11].
Comparative Analysis of Sequencing Technologies
Table 1: Key Technical Specifications and Performance Metrics of Sequencing Platforms
| Technology/Platform | Read Length | Time per Run | Output per Run | Primary Applications |
|---|---|---|---|---|
| Sanger Sequencing | 500-1,000 bp | ~7 hours | 0.44 Mbp | Validation of genetic variants, small-target sequencing [10] |
| Illumina (Short-read) | 56-300 bp | 56 hours - 14 days | 15-600 Gbp | Whole-genome sequencing, transcriptomics, targeted sequencing [9] [10] |
| Ion Torrent | 200-400 bp | ~4 hours | 200 Mbp - 2.5 Gbp | Microbial sequencing, targeted panels [10] |
| Pacific Biosciences (Long-read) | 10->50 kb | 0.5-4 hours | 0.5-1 Gbp | De novo assembly, complex genomic regions [10] |
| Oxford Nanopore (Long-read) | 0.5->50 kb | 0.5-2 hours | 15-30 Gbp | Real-time sequencing, metagenomics, field sequencing [10] [11] |
Table 2: Advantages and Limitations of Sequencing Approaches for Directed Evolution and AMR Research
| Sequencing Method | Key Advantages | Key Limitations | Optimal Use Cases |
|---|---|---|---|
| Sanger Sequencing | • High accuracy for single targets• Established, familiar workflow• Cost-effective for 1-20 targets | • Low throughput• Limited discovery power• Sensitivity ~15-20% [9] | • Validation of NGS findings• Confirming specific mutations• Small-scale projects |
| Short-read NGS (Illumina, Ion Torrent) | • High sequencing depth/sensitivity• Cost-effective for large target numbers• Detection of low-frequency variants (down to 1%)• High accuracy [9] [10] | • Limited read length challenges assembly• Difficulties with repetitive regions• GC bias [10] | • Variant detection across many samples• Resistance gene identification• Microbial genomics |
| Long-read NGS (PacBio, Oxford Nanopore) | • Resolves complex genomic regions• Epigenetic modification detection• Real-time sequencing (Nanopore)• Improved de novo assembly [10] [11] | • Higher error rates (mitigated by consensus)• Higher DNA input requirements• Lower throughput than short-read [11] | • Complete genome assembly• Structural variant detection• Hybrid sequencing approaches |
The dramatic reduction in sequencing costs has been a pivotal driver of WGS adoption. The cost per million bases of DNA sequence has dropped from over $5,000 in 2001 to approximately $0.006 in 2022, while the cost to sequence an entire human genome has fallen from over $95 million to about $525 during the same period [10]. This cost reduction has made large-scale genomic studies feasible and enabled researchers to design more ambitious directed evolution experiments with comprehensive sequencing at multiple time points.
Whole-Genome Sequencing for Resistance Gene Identification
Mechanisms of Antimicrobial Resistance
Antimicrobial resistance arises through diverse molecular mechanisms that WGS can comprehensively detect. These include: (1) point mutations in genes encoding drug targets (e.g., gyrA mutations conferring fluoroquinolone resistance); (2) acquired resistance genes encoding enzymes that inactivate antibiotics (e.g., β-lactamases); (3) target modification or bypass mechanisms; (4) changes in membrane permeability; and (5) efflux pump overexpression [6] [12]. WGS provides the resolution to identify all these mechanisms in a single assay, from single nucleotide variants to large structural rearrangements and horizontal gene transfer events.
The power of WGS extends beyond merely cataloging known resistance determinants. By providing a complete view of the bacterial genome, researchers can discover novel resistance mechanisms and understand the complex genetic networks that regulate resistance expression. This comprehensive approach is particularly valuable for tracking the mobilization of resistance genes through plasmids, integrons, and transposons, which drive the dissemination of AMR across bacterial populations [13] [6].
Bioinformatics Approaches for Resistance Gene Detection
Table 3: Key Bioinformatics Resources for Antibiotic Resistance Gene Identification
| Resource Name | Type | Primary Function | Key Features | Considerations |
|---|---|---|---|---|
| CARD [6] | Manually curated database | Comprehensive AMR detection | • Antibiotic Resistance Ontology (ARO)• Resistance Gene Identifier (RGI) tool• CARD*Shark curation algorithm | • Requires experimental validation• Manual curation delays updates |
| ResFinder/PointFinder [6] [12] | Specialized detection tool | Identifies acquired AMR genes and chromosomal mutations | • K-mer-based alignment for rapid analysis• Integrated platform for genes and mutations• Phenotype prediction tables | • Focuses on known determinants• Limited novel gene discovery |
| DeepARG [6] | Machine learning tool | Predicts novel and low-abundance ARGs | • Deep learning model trained on known ARGs• Identifies distant ARG homologs• Suitable for metagenomic data | • Computational resource-intensive• Potential false positives |
| ARGMiner [6] | Consolidated database | Integrates multiple ARG resources | • Broad coverage from multiple sources• Text mining for literature curation• Regular updates | • Potential redundancy• Variable curation standards |
| MEGARes [6] | Manually curated database | AMR reference for metagenomics | • Hierarchical structure for precision• Comprehensive resistance mechanism coverage• Compatible with various analysis tools | • Focused on acquired resistance genes• Limited chromosomal mutation data |
Bioinformatics pipelines for resistance gene identification typically follow two main approaches: assembly-based methods, which reconstruct complete genomes or large contigs before ARG identification, and read-based methods, which identify ARGs directly from sequencing reads [6]. Assembly-based approaches generally offer higher accuracy, especially for complex or low-abundance resistance determinants, while read-based methods are faster and suitable for rapid screening. The selection of appropriate bioinformatics tools and databases depends on the research objectives, with considerations for database curation standards, annotation depth, and coverage of relevant resistance mechanisms [6].
Experimental Protocol: WGS for Antimicrobial Resistance Profiling
Protocol: Whole-Genome Sequencing and Analysis of Bacterial Isolates for Antibiotic Resistance Gene Identification
I. DNA Extraction and Quality Control
- Extract genomic DNA using validated kits (e.g., DNeasy Blood & Tissue Kit, Qiagen; Maxwell RSC Cell DNA purification kit, Promega) [12].
- Assess DNA concentration using fluorometric methods (e.g., Qubit Fluorometer) and purity via spectrophotometry (A260/A280 ratio ~1.8-2.0).
- Verify DNA integrity by agarose gel electrophoresis, ensuring high molecular weight bands without degradation.
II. Library Preparation and Sequencing
- For Illumina platforms: Fragment 500 ng genomic DNA to ~550 bp insert size using enzymatic (e.g., NEBNext Ultra II FS module) or mechanical shearing [12].
- Prepare sequencing libraries using kits such as KAPA HyperPlus (Roche) with platform-specific adapters.
- For NovaSeq 6000: Perform size selection with Pippin Prep (Sage Science) using CDF1510 1.5% agarose dye-free cassette [12].
- Quantify libraries by qPCR and pool equimolarly. Include 1% PhiX control library to enhance sequence diversity.
- Sequence on Illumina platforms (MiSeq, NextSeq, or NovaSeq 6000) using appropriate reagent kits (e.g., v2/v3 for MiSeq, SP for NovaSeq) to generate 2×250 bp or 2×300 bp paired-end reads [12].
III. Bioinformatic Analysis
- Assess raw read quality with FastQC (v0.11.4+) and perform adapter trimming and quality filtering with Trimmomatic or Cutadapt.
- Perform de novo assembly using SPAdes genome assembler with appropriate k-mer sizes [12].
- Assess assembly quality using QUAST, evaluating contiguity (N50), completeness, and potential contamination.
- Annotate resistance genes using a combination of tools:
- Determine sequence types (STs) using MLST schemes appropriate for the bacterial species (e.g., Achtman scheme for E. coli) [12].
IV. Validation and Phenotypic Correlation
- Compare genotypic predictions with phenotypic susceptibility testing using broth microdilution according to EUCAST standards [12].
- Calculate categorical agreement, major errors (resistant genotype/susceptible phenotype), and very major errors (susceptible genotype/resistant phenotype).
- Resolve discrepancies by manual inspection of sequencing coverage, assembly quality, and potential novel resistance mechanisms.
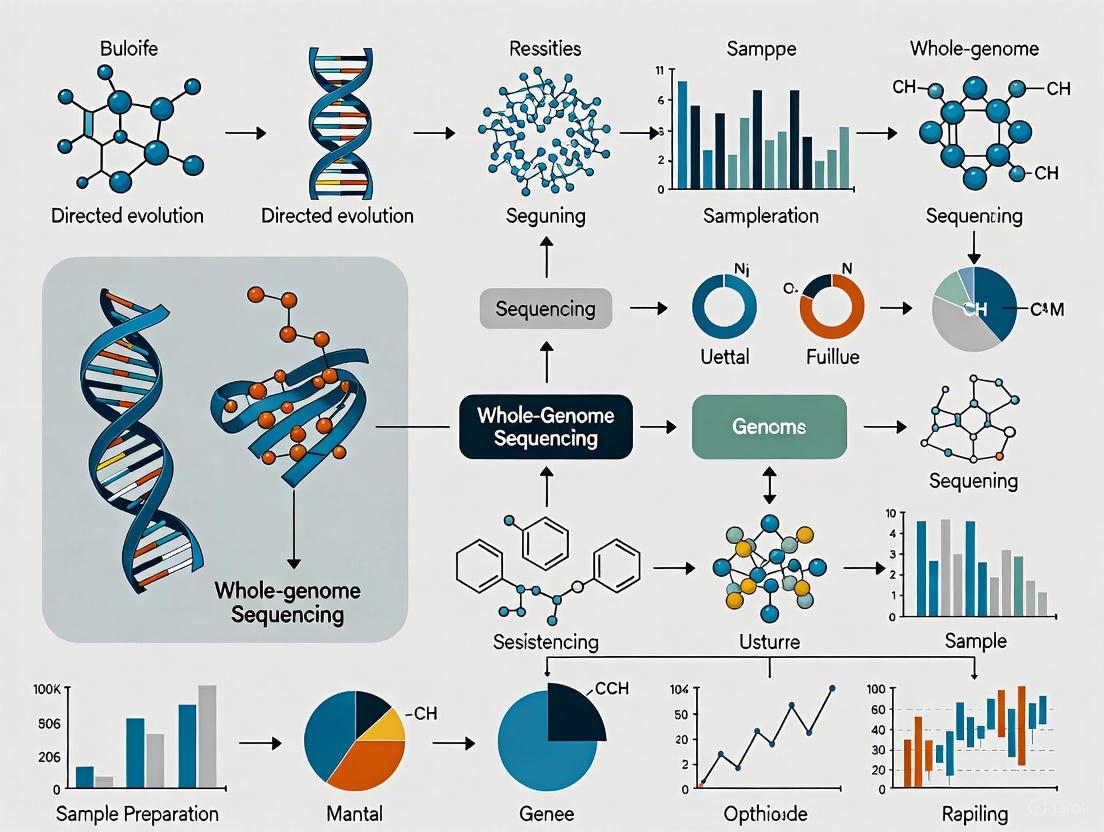
Figure 1: Comprehensive Workflow for Whole-Genome Sequencing and Analysis of Antibiotic Resistance Genes
Directed Evolution and Whole-Genome Sequencing
Directed Evolution Methodology
Directed evolution mimics natural selection in laboratory settings to engineer biomolecules with improved or novel functions. This powerful approach has become indispensable for developing enzymes with enhanced stability, activity, and specificity for industrial and therapeutic applications [2]. The process involves two fundamental steps: (1) generating genetic diversity in a target gene to create variant libraries, and (2) screening or selecting for variants with desired properties [2] [14].
Key techniques for generating genetic diversity include:
- Error-prone PCR: Randomly introduces point mutations throughout the target sequence through imperfect PCR conditions [2].
- DNA shuffling: Recombines sequences from related genes to create chimeric variants with beneficial mutations [2].
- Site-saturation mutagenesis: Systematically targets specific residues to explore all possible amino acid substitutions [2].
- RAISE (Random Insertion/Deletion Strategy): Creates random short insertions and deletions to explore more diverse sequence space [2].
- Orthogonal replication systems: Utilizes specialized DNA polymerases with inherent mutagenic properties for in vivo continuous evolution [2].
Following library generation, high-throughput screening methods identify improved variants. These include fluorescence-activated cell sorting (FACS) for binding or enzymatic activity, microplate-based assays, and display technologies such as phage display that physically link genotype to phenotype [2].
Integration of WGS in Directed Evolution Workflows
Whole-genome sequencing has become an invaluable tool in directed evolution campaigns, enabling researchers to move beyond simply identifying improved variants to understanding the genetic basis of those improvements. By sequencing populations throughout the evolution process, researchers can:
- Track the trajectory of beneficial mutations across generations
- Identify synergistic mutations that contribute to improved function
- Detect compensatory mutations that alleviate fitness costs
- Uncover mutational hotspots that tolerate or benefit from variation
- Guide subsequent library design based on empirical mutation data
In pharmaceutical applications, directed evolution coupled with WGS has enabled engineering of enzymes for improved drug synthesis, therapeutic proteins with enhanced pharmacokinetics, and antibodies with increased affinity and specificity [14]. The combination of these approaches accelerates the development of biocatalysts for industrial processes and biotherapeutics for clinical use.
Experimental Protocol: Directed Evolution with WGS Analysis
Protocol: Directed Evolution of Enzymes with Whole-Genome Sequencing Analysis
I. Library Generation through Mutagenesis
- For error-prone PCR: Use mutagenic conditions (e.g., unbalanced dNTP concentrations, Mn2+ supplementation, error-prone polymerases) to achieve 1-10 mutations per gene [2].
- For DNA shuffling: Fragment related genes with DNase I, reassemble through primerless PCR, then amplify full-length chimeras with flanking primers [2].
- For site-saturation mutagenesis: Design primers containing NNK degeneracy at target codons to cover all 20 amino acids, then amplify using high-fidelity polymerase [2].
- Clone variant libraries into appropriate expression vectors using Gibson assembly or restriction enzyme-based methods.
II. High-Throughput Screening/Selection
- Transform library into expression host (e.g., E. coli, yeast) to achieve >10x library coverage.
- For enzymatic activity: Implement fluorescence-activated cell sorting (FACS) with fluorogenic substrates or product entrapment strategies [2].
- For binding affinity: Utilize display technologies (phage, yeast, or ribosome display) with iterative rounds of panning/selection [2].
- For antibiotic resistance: Plate transformed cells on gradient antibiotic plates to select for enhanced resistance determinants [2].
- Isolate top-performing variants for further analysis and sequencing.
III. Whole-Genome Sequencing of Evolved Variants
- Prepare sequencing libraries from selected variants using kits such as KAPA HyperPrep or Nextera XT.
- For population dynamics analysis, include barcodes to multiplex multiple variants in a single sequencing run [11].
- Sequence on appropriate platform: Illumina for high accuracy, PacBio for complete gene assembly, or Nanopore for real-time monitoring.
- Ensure sufficient coverage (>50x for clonal isolates, >100x for population sequencing).
IV. Bioinformatics Analysis of Evolved Sequences
- Map sequencing reads to parental sequence using BWA or Bowtie2.
- Call variants with GATK or LoFreq, applying appropriate quality filters.
- Identify consensus mutations in improved variants and examine mutation frequencies across populations.
- For structural context, map mutations to protein structures using PyMOL or ChimeraX.
- Design next-generation libraries focusing on beneficial mutation combinations.
Figure 2: Directed Evolution Workflow Integrated with Whole-Genome Sequencing Analysis
Research Reagent Solutions
Table 4: Essential Research Reagents and Kits for Whole-Genome Sequencing and Directed Evolution
| Product Category | Specific Examples | Primary Function | Key Features |
|---|---|---|---|
| DNA Extraction Kits | DNeasy Blood & Tissue Kit (Qiagen), Maxwell RSC Cell DNA Purification Kit (Promega) | High-quality genomic DNA isolation from bacterial cultures | • Removal of inhibitors• High molecular weight DNA• Reproducible yields [12] |
| NGS Library Prep Kits | KAPA HyperPrep Kit (Roche), NEBNext Ultra II FS Module | Fragment DNA and add sequencing adapters | • Efficient library construction• Low bias• Compatible with automation [12] [14] |
| Target Enrichment | KAPA HyperCapture, Illumina Nextera Flex | Enrich specific genomic regions of interest | • Customizable target panels• Uniform coverage• High on-target rates |
| High-Fidelity Polymerases | KAPA HiFi DNA Polymerase (Roche) | Accurate amplification for library construction | • Engineered via directed evolution• Ultra-high fidelity• Robust performance [14] |
| Mutagenesis Kits | GeneMorph II Random Mutagenesis Kit (Agilent), commercial site-directed mutagenesis kits | Introduce genetic diversity for directed evolution | • Controllable mutation rates• Even mutation distribution• High efficiency [2] |
| Bioinformatics Tools | CARD RGI, ResFinder, DeepARG, SPAdes | Analyze sequencing data and identify resistance genes | • Curated databases• User-friendly interfaces• Regular updates [6] [12] |
Applications in Drug Discovery and Development
The integration of WGS into drug discovery pipelines has revolutionized multiple aspects of pharmaceutical development, from target identification to companion diagnostic development. In antimicrobial drug discovery, WGS enables comprehensive resistance profiling of clinical isolates, identification of novel resistance mechanisms, and tracking of resistance transmission in healthcare settings [10] [12]. This information guides the development of new antibiotics that circumvent existing resistance mechanisms and informs stewardship programs to preserve antibiotic efficacy.
In oncology, WGS facilitates comprehensive genomic profiling of tumors, identifying driver mutations, resistance mechanisms, and biomarkers for targeted therapy [15]. The ability to sequence circulating tumor DNA (ctDNA) provides a non-invasive method for monitoring treatment response and detecting emergent resistance mutations during therapy [15]. For rare diseases, WGS can identify previously unknown genetic determinants, enabling development of targeted therapies for patient populations with specific genetic profiles [16].
The pharmaceutical industry increasingly utilizes WGS across the entire drug development pipeline:
- Target identification: Uncovering novel therapeutic targets through association of genetic variants with disease states [15]
- Preclinical development: Validating targets in disease models and assessing potential resistance mechanisms [15]
- Clinical trials: Stratifying patients based on genetic biomarkers and monitoring molecular responses [15] [16]
- Post-market surveillance: Tracking resistance development and understanding variable treatment responses [13]
The journey from Sanger sequencing to modern NGS platforms has unleashed transformative potential in biological research and therapeutic development. The power of whole-genome sequencing lies not only in its comprehensive scope but also in its integration with sophisticated bioinformatics tools and experimental approaches like directed evolution. For researchers focused on antimicrobial resistance, WGS provides an unparalleled tool for deciphering resistance mechanisms, tracking transmission pathways, and guiding the development of countermeasures against resistant pathogens.
As sequencing technologies continue to evolve, with improvements in read length, accuracy, and accessibility, their applications in drug discovery and resistance research will expand correspondingly. The convergence of WGS with directed evolution creates a powerful synergy—where sequencing reveals nature's solutions to chemical challenges, and directed evolution optimizes those solutions for human benefit. This integrated approach promises to accelerate the development of novel therapeutics and diagnostic tools, ultimately enhancing our ability to combat antimicrobial resistance and address unmet medical needs across diverse disease areas.
A central challenge in modern therapeutic development is the predictable and rapid emergence of drug resistance. Traditional laboratory evolution methods explore only a fraction of possible genetic sequences, often failing to identify rare resistance mutations and combinations thereof [17]. This application note details how the integration of directed evolution with whole-genome sequencing creates a powerful framework for definitively linking genetic diversity to resistance phenotypes. By moving beyond observational studies to actively generating and mapping genetic variation, researchers can systematically identify resistance mechanisms and predict their evolution, ultimately informing the development of more durable treatments. This document provides a detailed protocol for implementing Directed Evolution with Random Genomic Mutations (DIvERGE) and its application in both microbial and human cell systems.
Key Concepts and Quantitative Foundations
Resistance arises through two primary evolutionary pathways, each with distinct implications for drug development and monitoring.
- Genes-First Pathway: This classical model posits that a new gene mutation appears first and provides a reproductive advantage, leading to its spread in the population. This pathway is often driven by single-point mutations in the drug target [18].
- Phenotypes-First Pathway: An alternative model suggests that genetically identical cells can fluctuate between different, non-heritable cell states due to phenotypic plasticity. These transient states can later become stabilized by subsequent genetic or epigenetic changes, accelerating adaptation to therapeutic pressures [18].
The following table summarizes the core differences between these pathways, which can coexist within a single patient.
Table 1: Comparing Genes-First and Phenotypes-First Resistance Pathways
| Feature | Genes-First Pathway | Phenotypes-First Pathway |
|---|---|---|
| Initial Event | New gene mutation (e.g., in drug target) | Phenotypic variability and plasticity in isogenic cells |
| Stability | Heritable from onset | Initially transient, may stabilize later |
| Primary Driver | DNA-level events | Cell-intrinsic plasticity & microenvironmental signals |
| Detection Method | Genome sequencing | Single-cell transcriptomics, functional assays |
| Exemplary Context | BCR-ABL1 mutations in CML [18] | Ovarian cancer adaptation to Olaparib [18] |
Quantitative data from a meta-analysis of HIV-1 further illustrates the practical output of such research, demonstrating the prevalence of drug resistance mutations (DRMs) across different drug classes.
Table 2: Quantitative Analysis of HIV-1 Drug Resistance Mutations in East Africa (2025 Data)
| Antiretroviral Drug Class | Prevalence of DRMs | Most Frequent Mutations |
|---|---|---|
| Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTI) | 36.5% | K103N |
| Nucleoside Reverse Transcriptase Inhibitors (NRTI) | 25.5% | M184V |
| Integrase Strand Transfer Inhibitors (INSTI) | 3.7% | - |
Data derived from 7,614 HIV-1 pol gene sequences. INSTI resistance, while currently low, warrants ongoing monitoring due to its clinical significance [19].
Experimental Protocols
Protocol A: DIvERGE in Bacterial Systems
Purpose: To rapidly generate and select for antibiotic resistance mutations in predefined genomic loci of bacterial species. Principle: This method uses pools of soft-randomized single-stranded DNA (ssDNA) oligonucleotides that fully cover the target locus. These oligos are incorporated into the genome via recombineering, introducing random mutations with a tunable rate and a uniform spectrum [17].
Procedure:
- Oligo Library Design and Synthesis:
- Design 90-nt ssDNA oligos complementary to the target genomic region, with oligos aligned in a partially overlapping pattern.
- Synthesize the oligo pool using a soft-randomization protocol. Spiking with a defined ratio (e.g., 2-5%) of mismatching nucleotides during synthesis ensures each possible mutation is represented while maintaining sufficient similarity to the wild-type sequence for efficient incorporation [17].
- Bacterial Preparation and Transformation:
- Grow the bacterial strain (e.g., E. coli K-12 MG1655) to mid-log phase.
- Induce the expression of recombineering proteins (e.g., using the pORTMAGE system) to make the cells competent for ssDNA incorporation [17].
- Electroporate the synthesized oligo pool into the competent cells.
- Mutagenesis and Selection:
- Allow for oligo incorporation and mutant outgrowth. This constitutes one DIvERGE cycle.
- Perform multiple iterative cycles (e.g., 5 cycles) to increase genetic diversity.
- Plate the mutagenized population on agar containing the antibiotic of interest at a concentration that inhibits wild-type growth.
- Isolate resistant colonies for downstream analysis [17].
- Analysis and Validation:
- Prepare genomic DNA from resistant clones.
- Sequence the targeted genomic regions using Illumina high-throughput sequencing to identify the precise resistance-conferring mutations [17].
Protocol B: In Vitro Evolution in Haploid Human Cells (IVIEWGA)
Purpose: To study chemotherapy drug resistance and identify resistance genes or drug targets in an isogenic human background. Principle: A near-haploid human cell line (HAP1) is subjected to increasing sublethal concentrations of a drug over multiple generations. Resistant clones are sequenced to identify de novo variants that confer the resistance phenotype [20].
Procedure:
- Cell Line and Compound Selection:
- Culture the HAP1 cell line, a near-haploid line derived from chronic myelogenous leukemia (CML).
- Select compounds with potent growth inhibition (EC50 < 1 µM is ideal). Validate efficacy using a 48-hour dose-response assay (e.g., with CellTiterGlo) [20].
- Cloning and Selection for Resistance:
- Clone the parent HAP1 cells by limiting dilution to ensure an isogenic starting population.
- Initiate independent selection series from different parent clones.
- For each series, expose cells to a sublethal concentration of the drug (e.g., doxorubicin, gemcitabine).
- Once cells recover, apply a lethal challenge (~3-5 × EC50). Alternatively, use a stepwise selection method, increasing the drug concentration by 5-10% every 5 days.
- Continue selection for several weeks to months until resistant populations emerge [20].
- Phenotypic Validation and Sequencing:
- Isolate clones from the resistant populations.
- Confirm stable resistance by re-testing the EC50 after culturing without drug pressure for 8 weeks.
- Perform whole-genome or exome paired-end sequencing on resistant clones and their matched, drug-sensitive parent clones [20].
- Bioinformatic Analysis:
- Develop a pipeline to compare resistant and sensitive genomes.
- Filter for high-frequency alleles that change protein sequence.
- Prioritize alleles that appear in the same gene across multiple independent selections with the same compound, as this provides high statistical confidence [20].
Visualizing Workflows and Pathways
The following diagrams, generated using Graphviz DOT language, illustrate the core experimental workflow and the conceptual models of resistance emergence.
Diagram 1: DIvERGE Experimental Workflow
Diagram 2: Resistance Evolution Pathways
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and resources essential for implementing the described protocols.
Table 3: Essential Research Reagents and Resources
| Reagent / Resource | Function / Application | Key Characteristics |
|---|---|---|
| Soft-Randomized ssDNA Oligo Pools [17] | Induce random, tunable mutations in long, predefined genomic targets during DIvERGE. | Overlapping design; spiking with mismatching nucleotides (2-5%); 90-nt length. |
| pORTMAGE System [17] | Enables highly efficient allelic replacement in E. coli without off-target effects for DIvERGE. | Plasmid-based system for expressing recombineering proteins. |
| HAP1 Cell Line [20] | Near-haploid human cell line for IVIEWGA, simplifying the identification of resistance-conferring variants. | Haploid for all chromosomes except a fragment of chr15; exposes mutated phenotypes. |
| Stanford HIV Drug Resistance Database (HIVDB) [19] | Online tool for identifying and interpreting HIV-1 drug resistance mutations in sequenced isolates. | Curated public database; uses sequence data to predict resistance to ARV drugs. |
| Genotyping-by-Sequencing (GBS) [21] | High-throughput method for discovering and genotyping SNPs in diverse germplasm, e.g., plant collections. | Identifies 100,000+ SNPs; used for population structure and GWAS. |
The fields of directed evolution and resistance gene identification represent pillars of modern biotechnology and therapeutic development. These disciplines, though seemingly distinct, share a common historical foundation built upon the pioneering work of Sol Spiegelman and his contemporaries in nucleic acid research. This application note traces the critical path from these early molecular experiments to the sophisticated high-throughput screening (HTS) technologies available today. By examining key milestones and methodologies, we provide researchers with both a historical framework and practical protocols to advance their work in engineering biomolecules and identifying genetic determinants of resistance. The integration of directed evolution with whole-genome sequencing has created a powerful paradigm for interrogating biological function, accelerating the development of novel enzymes, therapeutics, and diagnostic tools.
Historical Timeline and Key Developments
The following table summarizes the pivotal milestones that have shaped directed evolution and screening technologies since Spiegelman's foundational experiments.
Table 1: Key Historical Milestones in Directed Evolution and Screening
| Year | Milestone | Key Researchers/Group | Significance |
|---|---|---|---|
| 1960 | Invention of DNA-RNA Hybridization | Hall and Spiegelman [22] | Provided first direct evidence of RNA as a DNA transcript; enabled detection of specific genetic sequences. |
| 1965 | Spiegelman's Monster Experiment | Spiegelman et al. [23] | Demonstrated first in vitro Darwinian evolution of RNA; showed selective pressure (replication speed) drives evolution of minimal replicons (218 nucleotides). |
| 1967 | Pioneering in vitro Evolution | Spiegelman [2] | Established foundational principles for all subsequent directed evolution work. |
| 1975 | De novo RNA Generation | Sumper and Luce [23] | Showed Qβ replicase could spontaneously generate self-replicating RNA, bridging prebiotic chemistry and early evolution. |
| 1980s-1990s | Phage Display Development | Smith et al. [2] | Provided first application-driven directed evolution platform for selecting binding peptides and antibodies. |
| 1990s-2000s | Automation & Miniaturization | Various (Industry & Academia) [2] [24] | Enabled High-Throughput Screening (HTS), dramatically increasing testing capacity to >100,000 compounds per day [24]. |
| 2000s-Present | Advanced Recombination Methods | Various [2] | Development of DNA shuffling, StEP, and other methods to overcome limitations of point mutagenesis. |
| 2025 | AI-Powered RNA Structure Prediction | Kihara Lab (NuFold) [25] | End-to-end deep learning approach for predicting RNA 3D structure from sequence, accelerating RNA-targeted drug discovery. |
The progression from these foundational discoveries to modern applications illustrates a consistent trend toward greater throughput, miniaturization, and computational integration. Spiegelman's work established the core principle that evolutionary pressures could be applied in a controlled laboratory environment to select for desired molecular traits. This principle now underpins sophisticated campaigns to identify resistance genes and engineer novel biocatalysts.
Detailed Experimental Protocols
Protocol 1: In Vitro RNA Evolution (Based on Spiegelman's Experiment)
This protocol outlines the core procedure for the Darwinian evolution of RNA molecules in a cell-free system, replicating the essential elements of Spiegelman's work [23].
1. Reagent Preparation:
- Qβ Bacteriophage RNA: The initial template (~4500 nucleotides).
- Qβ Replicase: RNA-dependent RNA polymerase from the Qβ bacteriophage.
- Nucleotide Mixture: Contains ATP, GTP, CTP, and UTP.
- Replication Buffer: Provides optimal ionic strength and pH for Qβ replicase activity.
- Dilution Buffer: Fresh replication buffer for serial transfers.
2. Procedure: 1. Initial Reaction Setup: In a microcentrifuge tube, combine the following: - 1 µg Qβ RNA - 10 U Qβ Replicase - 1 mM each NTP - 1X Replication Buffer - Bring to a final volume of 100 µL with nuclease-free water. 2. Incubation: Incubate the reaction at 37°C for 20 minutes to allow for RNA replication. 3. Serial Transfer: Take a 10 µL aliquot from the initial reaction and transfer it to a new tube containing 90 µL of fresh, pre-warmed Replication Buffer with NTPs and Qβ Replicase. 4. Repetition: Repeat the serial transfer process (Step 3) every 20 minutes. This constitutes one "generation." 5. Monitoring: Continue the serial transfers for 74 or more generations. Monitor the reaction products periodically by denaturing gel electrophoresis (e.g., 8% polyacrylamide/7 M urea gel).
3. Analysis:
- Gel Electrophoresis: Analyze the RNA products from different generations. A progressive shift toward faster-migrating (shorter) RNA species over time will be visually evident.
- Sequencing: Extract the dominant RNA band from the final generations and subject it to RNA sequencing to confirm the emergence of a minimal replicon (~218 nucleotides) [23].
4. Key Considerations:
- Aseptic Technique: Maintain RNase-free conditions throughout the procedure to prevent RNA degradation.
- Control Reactions: Include a control without Qβ replicase to confirm that replication is enzyme-dependent.
- Selection Pressure: The dilution factor and fixed incubation time create the selective pressure for faster-replicating (and consequently shorter) RNA molecules.
Protocol 2: A Modern High-Throughput Screening Workflow for Enzyme Variants
This protocol describes a generic, cell-based HTS workflow suitable for identifying enzyme variants with improved properties (e.g., activity, stability) from a library generated by directed evolution [2] [24] [26].
1. Reagent Preparation:
- Variant Library: A library of clones (e.g., in E. coli) expressing different enzyme variants.
- Assay Plates: 384-well or 1536-well microplates.
- Growth Medium: Appropriate sterile liquid medium with selective antibiotic.
- Substrate: A fluorogenic or chromogenic substrate that yields a detectable signal upon enzyme activity.
- Lysis Buffer: (If needed) A buffer to permeabilize cells and release the enzyme.
- Stop Solution: A reagent to quench the reaction at the endpoint.
2. Procedure: 1. Cell Dispensing: Using a liquid handler, dispense a suspension of each variant clone into individual wells of the assay plate. Include positive (wild-type enzyme) and negative (empty vector) controls in designated wells. 2. Cell Growth: Incubate the assay plates at the appropriate temperature with shaking to allow for cell growth and enzyme expression. 3. Assay Initiation: Add the substrate solution to all wells, either manually or via automated dispensing. 4. Signal Incubation: Incubate the plates for a predetermined time to allow the enzymatic reaction to proceed. 5. Signal Detection: Read the plate using a microplate reader configured for absorbance, fluorescence, or luminescence detection.
3. Analysis: 1. Data Normalization: Normalize the raw signal from each well against the positive and negative controls on the same plate. A common metric is the Z'-factor, which assesses the quality of the assay based on the separation between positive and negative controls [26]. 2. Hit Identification: Variants that produce a signal statistically significantly above a set threshold (e.g., 3 standard deviations above the mean of the negative control) are designated as "hits" [26]. 3. Validation: The hits from the primary screen are re-tested in a secondary, more quantitative screen (e.g., to determine IC50 or Ki values) to confirm the desired activity.
4. Key Considerations:
- Assay Robustness: The assay must be optimized for minimal variability and a high Z'-factor (>0.5 is excellent) before screening the entire library.
- Automation: The entire process is typically automated using robotic systems for plate handling, liquid dispensing, and incubation to achieve high throughput [26].
- Miniaturization: Using 1536-well plates and low (µL) volumes reduces reagent costs and enables ultra-high-throughput screening (uHTS) [24].
The logical flow of this HTS protocol, from library preparation to hit validation, is depicted below.
Diagram 1: HTS Workflow for Enzyme Variants
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of directed evolution and HTS campaigns relies on a suite of specialized reagents and tools. The following table details key components for building and screening genetic libraries.
Table 2: Key Research Reagent Solutions for Directed Evolution and HTS
| Reagent/Material | Function | Application Example |
|---|---|---|
| Qβ Replicase | RNA-dependent RNA polymerase that catalyzes RNA replication. | In vitro evolution of RNA molecules (e.g., Spiegelman's Monster) [23]. |
| Error-Prone PCR Kit | Introduces random point mutations into a gene of interest during amplification. | Generating genetic diversity for the first step of a directed evolution campaign [2]. |
| DNA Shuffling Kit | Recombines fragments of homologous genes to create chimeric libraries. | Accelerating evolution by combining beneficial mutations from different parent genes [2]. |
| KAPA HiFi DNA Polymerase | A high-fidelity polymerase engineered via directed evolution for ultra-high accuracy in PCR. | High-fidelity amplification of NGS libraries to avoid introducing errors during preparation [14]. |
| 384/1536-Well Microplates | Miniaturized assay plates that enable high-density, low-volume reactions. | Conducting HTS assays to screen hundreds of thousands of compounds or enzyme variants [24] [26]. |
| Fluorogenic/Chromogenic Substrates | Compounds that produce a measurable signal (fluorescence/color) upon enzyme activity. | Detecting and quantifying enzyme activity in a high-throughput format [26]. |
| NuFold Algorithm | A deep learning-based computational tool for predicting RNA 3D structure from sequence. | Accelerating RNA-targeted drug discovery by providing structural models where experimental data is lacking [25]. |
The strategic selection of these reagents is critical for experimental success. For instance, the choice of DNA polymerase can directly impact the quality and diversity of a mutant library, while the selection of an appropriate substrate is paramount for developing a robust HTS assay.
Integrated Data Analysis and Interpretation
The massive datasets generated by HTS require robust analytical methods for quality control and hit selection. Key metrics include the Z-factor, which evaluates the quality and separation band of an assay, and the Strictly Standardized Mean Difference (SSMD), which is a more powerful statistic for assessing the size of effects and data quality [26]. For hit selection in screens without replicates, the z-score method is often employed, whereas screens with replicates benefit from the use of t-statistics or SSMD, which can directly estimate variability for each compound [26].
The integration of whole-genome sequencing with HTS data is a cornerstone of resistance gene identification. After an HTS campaign identifies a clone with a desired phenotype (e.g., drug resistance), its genome is sequenced and compared to the parent strain. Single-nucleotide polymorphisms (SNPs), insertions, deletions, and gene amplifications are identified. The causal mutation is then confirmed by reintroducing it into a naive background and re-assaying the phenotype. This closed-loop workflow powerfully links genotype to phenotype.
The logical progression from a phenotypic screen to the identification of a causal gene is summarized in the following diagram.
Diagram 2: Resistance Gene Identification Workflow
The journey from Spiegelman's simple test tube containing a "monster" RNA to the automated, AI-enhanced laboratories of today underscores a remarkable trajectory in biotechnology. The core principle remains unchanged: the application of selective pressure to populations of biomolecules drives the evolution of desired traits. However, the tools available to the researcher have been transformed. Modern directed evolution leverages high-throughput methodologies that allow for the screening of library sizes unimaginable just decades ago. Furthermore, the integration of whole-genome sequencing provides an unambiguous link between selected phenotype and underlying genotype, making the identification of resistance genes and beneficial mutations a systematic process. As computational tools like NuFold [25] continue to mature and merge with experimental screening, the cycle of design-build-test-learn will only accelerate, opening new frontiers in enzyme engineering, drug discovery, and fundamental biological research.
Application Notes
The relentless evolution of bacterial pathogens and the escalating crisis of antimicrobial resistance (AMR) demand a new generation of precise and adaptable countermeasures. The integration of directed evolution with advanced whole-genome sequencing (WGS) technologies is creating a powerful paradigm shift in how we identify resistance genes and engineer novel biological agents to combat pathogens. This approach moves beyond static solutions, allowing researchers to rapidly optimize biomolecules and therapies in direct response to the genetic mechanisms of resistance. The following application notes illustrate the breadth of this expanding scope, showcasing how these technologies are being deployed to develop new antimicrobials, gene therapies, and pathogen control strategies.
Application Note 1: Engineering Host-Defense Peptides as Non-Resistance-Inducing Antimicrobials
- Challenge: Conventional antibiotics increasingly fail due to resistance, and the pharmaceutical pipeline for novel antibiotics is limited. There is a critical need for new classes of antimicrobials that attack bacteria via mechanisms for which resistance is difficult to develop.
- Solution & Technology: Recent research has re-examined human chemokines, a class of immune signaling molecules known to have secondary antimicrobial properties. Using structure-function studies guided by mechanistic insights, researchers are engineering these peptides to enhance their direct killing power.
- Key Experimental Data: Investigations revealed that specific chemokines, such as CCL20, kill bacteria by binding to negatively charged phospholipids (cardiolipin and phosphatidylglycerol) in the bacterial cell membrane and disrupting its integrity [27]. Crucially, unlike conventional antibiotics, repeated exposure to CCL20 did not lead to increased bacterial resistance, even after multiple generations [27].
- Insight: This approach leverages a fundamental vulnerability—the bacterial membrane—which is less mutable than the protein targets of many antibiotics. Directed evolution campaigns can now be designed to optimize chemokine variants for enhanced binding to these phospholipids, creating a promising new class of resistance-resistant therapeutics.
Table 1: Quantitative Analysis of Antimicrobial Chemokine Activity
| Chemokine/Peptide | Target Bacteria | Key Mechanism | Resistance Development? |
|---|---|---|---|
| CCL20 | E. coli | Binds cardiolipin & phosphatidylglycerol, disrupting cell membrane | No resistance observed after multiple exposures [27] |
| Beta-defensin 3 (Comparison) | E. coli | Antimicrobial peptide activity | Not specified in study [27] |
Application Note 2: Directed Evolution of Bridge Recombinases for Universal Gene Replacement Therapies
- Challenge: Correcting large or diverse genetic mutations in monogenic diseases is inefficient with CRISPR-based tools, which rely on error-prone DNA repair and struggle with inserting full-length genes.
- Solution & Technology: Bridge recombinases are a novel class of genome-editing enzymes that use a bridge RNA (bRNA) to precisely insert large DNA donor fragments into a genome without creating double-stranded breaks [28]. To enhance their efficiency and specificity for therapeutic use, researchers are applying directed evolution.
- Key Experimental Data: A proof-of-concept project targeting Alpha-1 Antitrypsin Deficiency (A1ATD) has established a complete workflow. This includes:
- Identification of target sites in the SERPINA1 gene.
- Use of deep mutational learning (DML), a machine-learning method, to screen thousands of recombinase variants [28].
- Implementation of two directed evolution systems: E. coli Orthogonal Replicon (EcORep) and Phage-Assisted Continuous Evolution (PACE) to select for recombinases with improved activity [28].
- Insight: The goal is a universal therapy where a single evolved bridge recombinase can insert a healthy gene copy to treat all patients with a disease, regardless of their specific mutation. This demonstrates how WGS identifies pathogenic mutations, and directed evolution creates the tools to correct them.
Application Note 3: Expanding Phage Host Range to Target Multidrug-Resistant Infections
- Challenge: Bacteriophage (phage) therapy is a promising alternative to antibiotics, but naturally occurring phages often have a narrow host range, limiting their utility against diverse clinical isolates of a pathogen like Klebsiella pneumoniae.
- Solution & Technology: The Appelmans protocol (in vitro directed evolution) was used to train a cocktail of five myophages against a panel of 11 bacterial strains, including phage-resistant clinical isolates [29].
- Key Experimental Data: After multiple passages, evolved phage variants were isolated and sequenced. The study found:
- Host Range Shift: Some variants gained the ability to lyse previously resistant strains while losing activity against formerly susceptible ones.
- Host Range Expansion: Several variants demonstrated broadly expanded activity [29].
- Genetic Basis: Whole-genome sequencing identified that mutations and recombination events in tail fiber genes were likely responsible for the altered host tropism [29].
- Insight: Directed evolution is a powerful method to generate phages with tailored host ranges for therapeutic cocktails, overcoming a major limitation of phage therapy and providing a dynamic strategy to combat evolving multidrug-resistant pathogens.
Table 2: Outcomes of Phage Host Range Expansion via Directed Evolution
| Phage Variant Type | Change in Host Range | Primary Genetic Mechanism | Therapeutic Potential |
|---|---|---|---|
| Variant A | Expanded to include previously resistant strains | Mutations in tail fiber genes [29] | High; improves cocktail coverage |
| Variant B | Shifted from old hosts to new resistant hosts | Recombination events in tail fiber genes [29] | Moderate; requires careful cocktail design |
Experimental Protocols
The following protocols provide detailed methodologies for key experiments cited in the application notes, enabling researchers to replicate and build upon these advanced techniques.
Protocol 1: In Vitro Directed Evolution of Phages Using the Appelmans Protocol
Purpose: To isolate bacteriophage variants with expanded or altered host ranges for therapeutic use against multidrug-resistant bacterial strains [29].
Materials:
- Bacterial Strains: A panel of target bacterial strains, including a permissive host and clinical phage-resistant isolates.
- Parental Phages: A mixture of phages with complementary initial host ranges.
- Growth Media: Appropriate liquid broth (e.g., LB) and soft agar for plaque assays.
- Equipment: Sterile culture flasks/tubes, incubator, centrifuge, filtration units (0.22 µm).
Procedure:
- Preparation: Mix the parental phage cocktail and a portion of the bacterial panel (excluding the permissive host) in a flask containing growth medium.
- Co-culture Incubation: Incubate the culture with shaking until visible lysis is observed or for a predetermined period (e.g., 24 hours).
- Harvesting: Centrifuge the culture to remove bacterial debris. Filter the supernatant through a 0.22 µm filter to obtain a phage lysate containing progeny from the initial round.
- Repassaging: Use a small volume of the filtered lysate to infect a fresh batch of the bacterial panel. Repeat steps 2-4 for multiple serial passages (e.g., 10-20 rounds).
- Plaque Isolation & Screening: After the final passage, perform plaque assays on both the permissive host and the previously resistant strains. Isplicate individual plaques from plates showing lysis.
- Characterization: Amplify the isolated phage variants and characterize their new host ranges against a comprehensive diversity panel of bacterial strains. Confirm genomic changes through whole-genome sequencing [29].
Protocol 2: Quantitative Microbial Risk Assessment (QMRA) Integrating ARG Mobility from Metagenomic Data
Purpose: To move beyond simple abundance counts of Antibiotic Resistance Genes (ARGs) and incorporate their mobility potential, as a proxy for dissemination risk, into environmental surveillance risk models [30].
Materials:
- Environmental Samples: (e.g., water, sediment, wastewater).
- DNA Extraction Kit: Suitable for complex environmental samples.
- Sequencing Platform: Illumina, Oxford Nanopore, or PacBio for metagenomic sequencing.
- Bioinformatics Tools: ARG databases (CARD, ResFinder), MGE databases, metagenomic assembly tools (SPAdes, metaSPAdes), and contig binning software.
Procedure:
- Sample Collection & DNA Extraction: Collect environmental samples in triplicate. Extract high-molecular-weight genomic DNA.
- Metagenomic Sequencing: Prepare sequencing libraries and perform whole-community shotgun sequencing using short-read (Illumina) and/or long-read (Nanopore, PacBio) technologies to facilitate better assembly [30].
- Bioinformatic Analysis:
- Assembly & Binning: Assemble quality-filtered reads into contigs. Bin contigs into Metagenome-Assembled Genomes (MAGs) to infer bacterial hosts.
- ARG & MGE Annotation: Annotate contigs using ARG and MGE databases to identify resistance determinants and mobile genetic elements (plasmids, integrons, transposons).
- Mobility Linkage: Analyze co-localization of ARGs and MGEs on the same contig or within the same MAG. This physical linkage is a strong indicator of mobility potential [30].
- Risk Integration: Calculate a risk score that incorporates both the abundance of high-risk ARGs (e.g., those ranked by clinical relevance) and their association with MGEs. Integrate this score into a QMRA framework for hazard identification and exposure assessment [30].
Protocol 3: Engineering a Chimeric Peptidoglycan Hydrolase for Enhanced Anti-Listerial Activity
Purpose: To improve the efficacy and specificity of a novel M23 peptidase (StM23) against Listeria monocytogenes by creating a chimeric enzyme fused with a high-affinity cell wall-targeting domain [31].
Materials:
- Gene Fragments: DNA encoding the catalytic domain of StM23 and the cell wall-targeting domain (CWT) from Staphylococcus pettenkoferi (SpM23B).
- Expression Vector & Host: Plasmid (e.g., pET series) and E. coli expression strain (e.g., BL21(DE3)).
- Chromatography Systems: Equipment for protein purification (e.g., Ni-NTA affinity chromatography).
- Bacterial Strains: Target strains (e.g., L. monocytogenes, Bacillus subtilis) and safety evaluation models (zebrafish, moth larvae, human cell lines).
Procedure:
- Gene Design & Synthesis: Design a synthetic gene encoding the StM23 catalytic domain fused via a flexible linker to the SpM23B CWT domain. The construct is codon-optimized for the expression host.
- Cloning & Expression: Clone the chimeric gene (StM23_CWT) into an expression vector. Transform into the expression host and induce protein production with IPTG.
- Protein Purification: Lyse the cells and purify the chimeric enzyme using affinity chromatography based on an engineered tag (e.g., His-tag).
- Enzyme Characterization:
- Activity Assay: Measure bacteriolytic activity against planktonic cultures of L. monocytogenes and other Gram-positive bacteria. Compare the chimeric enzyme's efficacy to the EAD-alone construct.
- Biofilm Disruption: Test the ability of StM23_CWT to disrupt pre-formed biofilms on relevant surfaces (glass, stainless steel, silicone).
- Environmental Tolerance: Assess enzymatic activity under varying pH and salt conditions to determine industrial applicability [31].
- Safety Evaluation: Conduct toxicity assessments using zebrafish embryos, moth larvae, and human cell culture models to confirm a non-toxic profile [31].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and tools essential for research in directed evolution and antimicrobial discovery.
Table 3: Essential Research Reagents for Directed Evolution and Pathogen Combatting
| Research Reagent / Tool | Function & Application | Example Use Case |
|---|---|---|
| Phage-Assisted Continuous Evolution (PACE) | Links target protein activity to phage replication, enabling continuous directed evolution without intervention [28]. | Evolving bridge recombinases for improved gene insertion efficiency [28]. |
| Comprehensive Antibiotic Resistance Database (CARD) | A manually curated resource and ontology for identifying AMR genes and mutations from genomic data [6]. | Annotating and predicting ARGs from whole-genome or metagenome sequences in surveillance studies [6]. |
| Bridge Recombinase System | An RNA-guided system for precise insertion of large DNA fragments without double-strand breaks [28]. | Developing universal gene replacement therapies for monogenic diseases like Alpha-1 Antitrypsin Deficiency [28]. |
| High-Throughput qPCR (HT-qPCR) | Allows simultaneous quantification of hundreds of ARGs and MGEs from environmental or clinical DNA extracts [32]. | Profiling the abundance and diversity of resistance genes in wastewater to assess environmental impact [32]. |
| Antibiotic Resistance Gene Index (ARGI) | A standardized metric to compare overall AMR levels across different samples or studies [32]. | Benchmarking the performance of wastewater treatment plants in reducing AMR load [32]. |
From Mutation to Data: A Step-by-Step Pipeline for Resistance Gene Identification
Directed evolution stands as a powerful protein engineering methodology that mimics natural evolution in laboratory settings, enabling the development of biomolecules with enhanced or novel properties for therapeutic, industrial, and research applications [2]. This approach has revolutionized our ability to optimize enzymes, antibodies, and other proteins without requiring comprehensive prior knowledge of structure-function relationships [33]. The fundamental process of directed evolution consists of two critical phases: (1) the creation of genetic diversity (library generation), and (2) the screening or selection of variants with desired traits [2]. Library generation techniques form the foundation of this process, determining the nature and quality of diversity available for selection. Within the specific context of resistance gene identification research, these methodologies enable the systematic investigation of molecular adaptation mechanisms and the identification of critical genetic determinants conferring resistance phenotypes [6] [20]. This article provides detailed application notes and protocols for three key library generation techniques—Error-Prone PCR, DNA Shuffling, and RAISE—framed within directed evolution and whole-genome sequencing for resistance gene identification.
Comparative Analysis of Techniques
Table 1: Comparison of Key Library Generation Techniques
| Technique | Primary Mechanism | Diversity Type | Key Advantages | Key Limitations | Ideal Applications |
|---|---|---|---|---|---|
| Error-Prone PCR | Random point mutations during PCR amplification | Point mutations throughout sequence | • Does not require prior structural knowledge• Technically straightforward to perform• Wide accessibility [33] | • Biased mutation spectrum• Limited amino acid substitutions due to codon bias [33]• Reduced sampling of mutagenesis space [2] | • Initial exploration of sequence-function relationships• Stability engineering• Activity optimization |
| DNA Shuffling | Fragmentation and recombination of homologous sequences | Recombination of existing diversity | • Combines beneficial mutations• Can remove deleterious mutations [33]• Mimics natural evolutionary process | • Requires high sequence homology between parents [2]• Can introduce unwanted neutral mutations | • Family shuffling of homologous genes• Directed evolution of multi-domain proteins• Pathway engineering |
| RAISE | Random insertion and deletion of short sequences | Insertions and deletions (indels) | • Generates random indels across sequence• Accesses distinct mutational space compared to point mutations [2] | • Can introduce frameshifts• Limited to small insertions/deletions | • Exploring structural flexibility• Loop engineering• Domain linking optimization |
Method Selection Guidelines
Choosing the appropriate library generation method depends on several factors, including the starting genetic material, desired diversity type, and screening capabilities. Error-prone PCR serves as an excellent starting point for novel targets with limited structural information, providing broad mutational coverage across the entire gene [33]. DNA shuffling demonstrates particular utility when multiple parent sequences with beneficial mutations are available, enabling the combination of advantageous traits [33] [2]. RAISE offers unique capabilities for exploring structural conformations and access to distinct sequence space through indel mutations, which are underrepresented in other methods [2]. For comprehensive resistance gene studies, iterative approaches combining these techniques often yield superior results, allowing researchers to explore diverse mutational landscapes and identify non-obvious resistance mechanisms.
Error-Prone PCR: Application Notes and Protocols
Principle and Applications in Resistance Research
Error-prone PCR (epPCR) introduces random point mutations throughout a DNA sequence by reducing the fidelity of DNA polymerase during amplification [33]. This technique has become one of the most accessible and widely used methods for generating initial diversity in directed evolution experiments, particularly for investigating resistance mechanisms [33] [34]. In resistance gene identification, epPCR enables researchers to explore how random mutations throughout a gene sequence affect drug binding, efflux, or metabolic bypass mechanisms. The method's advantage lies in its ability to identify unexpected resistance mutations outside of known functional domains, potentially revealing novel resistance mechanisms [20].
Detailed Experimental Protocol
Table 2: Error-Prone PCR Reaction Setup
| Component | Standard PCR | Error-Prone PCR | Purpose |
|---|---|---|---|
| Template DNA | 1-10 ng | 1-10 ng | Target gene for mutagenesis |
| Primers | 0.2-0.5 μM each | 0.2-0.5 μM each | Gene-specific amplification |
| dNTPs | 200 μM each | Unequal concentrations (e.g., 0.2 mM dGTP, 1 mM dTTP) [33] | Increased misincorporation |
| MgCl₂ | 1.5-2.0 mM | 2.5-7.0 mM | Reduced fidelity, enhanced processivity |
| Additional Cations | None | 0.1-0.5 mM MnCl₂ [33] | Significant reduction in polymerase fidelity |
| Polymerase | High-fidelity Taq | Standard Taq or error-prone variants | DNA amplification |
| Buffer | Manufacturer's recommendation | Manufacturer's recommendation | Optimal enzyme activity |
Procedure:
- Reaction Setup: Prepare the error-prone PCR reaction mixture according to Table 2 components in a total volume of 50 μL. MnCl₂ should be added after other components as it can precipitate in PCR buffer.
- Thermal Cycling:
- Initial denaturation: 95°C for 2-5 minutes
- 25-35 cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing: 55-65°C (gene-specific) for 30 seconds
- Extension: 72°C for 1 minute/kb
- Final extension: 72°C for 5-10 minutes
- Mutation Rate Control: Modulate mutation frequency by adjusting Mn²⁺ concentration (0.1-0.5 mM) and number of PCR cycles [33]. Higher Mn²⁺ and more cycles increase mutation rates.
- Product Purification: Purify PCR products using standard gel extraction or PCR purification kits.
- Library Construction: Clone purified fragments into appropriate expression vectors using restriction enzyme digestion and ligation or recombination-based cloning [35].
- Transformation: Transform competent cells (e.g., E. coli) with the constructed library for expression and screening.
Technical Considerations and Optimization
The mutation rate in epPCR typically ranges from 1-20 mutations per kb, with optimal results often achieved at 1-5 mutations per gene to balance diversity and protein functionality [33]. Several factors influence mutation spectrum and rate: Mn²⁺ concentration dramatically increases error rates, while unbalanced dNTP pools bias mutations toward specific transitions [33]. Different DNA polymerases exhibit distinct error profiles—Taq polymerase shows AT→GC bias, while Mutazyme II provides more balanced mutations [33] [2]. Recent innovations include inosine-containing epPCR, which introduces targeted GC-biased mutations beneficial for aptamer development and stability engineering [36]. For resistance studies, we recommend using multiple epPCR conditions with different mutational biases to maximize sequence space coverage and enhance the probability of identifying novel resistance determinants.
DNA Shuffling: Application Notes and Protocols
Principle and Applications in Resistance Research
DNA shuffling accelerates directed evolution by in vitro recombination of homologous sequences, mimicking natural sexual recombination [33] [2]. This technique enables researchers to combine beneficial mutations from different parent sequences while eliminating deleterious mutations, effectively exploring combinatorial fitness landscapes [33]. In resistance research, DNA shuffling proves particularly valuable for studying multi-gene resistance families or evolving broad-spectrum resistance against drug cocktails. By recombining sequences from various resistant isolates, researchers can identify synergistic mutations and epistatic interactions that contribute to resistance phenotypes [20].
Detailed Experimental Protocol
Procedure:
- Template Preparation: Combine 1-10 μg of parent DNA sequences (70-99% homologous) in equimolar ratios. Parent sequences can include naturally occurring homologs or previously evolved variants.
- Fragmentation: Digest DNA with DNase I (0.1-0.2 units/μg DNA) in 10 mM Tris-HCl (pH 7.4), 10 mM MnCl₂ at 15-25°C for 10-30 minutes. Monitor fragmentation by agarose gel electrophoresis to achieve optimal fragment sizes of 50-200 bp.
- Purification: Purify fragments using silica membrane columns or gel extraction to remove DNase I and buffer components.
- Reassembly PCR: Set up reassembly without primers:
- Fragments: 0.5-2 μg
- dNTPs: 0.2-0.4 mM each
- Taq polymerase buffer with 1.5-2.5 mM MgCl₂
- Taq polymerase: 2-5 units/100 μL reaction
- Thermal cycling:
- 94°C for 2 minutes
- 40-60 cycles: 94°C for 30-60 seconds, 50-60°C for 30-60 seconds, 72°C for 30-60 seconds (no primers)
- Amplification: Add gene-specific primers (0.2-0.5 μM) to 1-5 μL of reassembly product and perform standard PCR (25-35 cycles) to amplify full-length chimeric genes.
- Cloning and Screening: Clone products into expression vectors and transform host cells for functional screening.
Technical Considerations and Optimization
The efficiency of DNA shuffling depends heavily on sequence homology between parent genes—higher homology (>80%) yields more crossovers and viable recombinants [2]. Fragment size significantly affects recombination frequency, with 50-100 bp fragments typically optimal. For genes with low natural homology, family shuffling incorporating multiple homologous sequences from nature expands diversity [33]. Alternative recombination methods like StEP (Staggered Extension Process) offer simplified approaches by performing priming and extension in short cycles, gradually switching templates [2]. In resistance mechanism studies, DNA shuffling of resistant and sensitive alleles can pinpoint minimal mutational sets required for resistance, informing drug design strategies to overcome resistance.
RAISE: Application Notes and Protocols
Principle and Applications in Resistance Research
RAISE (Random Insertion/Deletion Strand Exchange Mutagenesis) generates diversity through random short insertions and deletions (indels) throughout the target sequence [2]. Unlike point mutagenesis methods, RAISE accesses distinct sequence space by altering protein length and potentially creating novel structural motifs. In resistance research, this technique helps identify structural plasticity and alternative conformations that enable escape from inhibitory compounds. RAISE proves particularly valuable for investigating resistance mechanisms involving loop rearrangements, domain shuffling, or altered substrate access channels [2].
Detailed Experimental Protocol
Procedure:
- Template Preparation: Prepare linearized plasmid DNA (2-5 μg) containing the target gene using restriction enzymes that cut outside the coding region.
- Transposon Integration: Perform in vitro transposition reaction using commercial transposon systems (e.g., ThermoFisher Scientific kit):
- Linearized DNA: 1 μg
- Transposon: 100 ng
- Transposase: 1 unit
- Reaction buffer: as recommended
- Incubate at 37°C for 1-2 hours
- Heat-inactivate at 70°C for 10 minutes
- Library Transformation: Transform 1-5 μL reaction into E. coli, plate on selective media, and incubate overnight.
- Colony PCR: Screen colonies by PCR to identify clones with insertions in the target region using gene-specific primers.
- Deletion Generation (optional): For deletion libraries, subject insertion library to partial digestion with specific nucleases or additional transposition steps.
- Curing: Remove selection marker through restriction digestion or site-specific recombination if needed for functional studies.
- Functional Screening: Screen library for desired phenotypes (e.g., drug resistance) under selective conditions.
Technical Considerations and Optimization
RAISE typically generates indels of 1-15 amino acids, with smaller indels (<5 aa) having higher probability of maintaining protein fold and function [2]. Transposon systems can be engineered to incorporate additional features such as protease sites, affinity tags, or additional diversity at insertion sites. Frameshift mutations occur frequently with RAISE, which can be minimized using engineered transposons that maintain reading frame [2] [37]. For resistance studies, we recommend combining RAISE with high-throughput sequencing to comprehensively map permissive insertion sites that tolerate structural rearrangement while maintaining or enhancing resistance phenotypes.
Integration with Whole-Genome Sequencing for Resistance Gene Identification
Synergistic Workflow for Resistance Mechanism Elucidation
Table 3: Sequencing Strategies for Library Analysis
| Sequencing Approach | Application Context | Key Advantages | Considerations |
|---|---|---|---|
| Whole-Genome Sequencing | Comprehensive variant identification in evolved clones [20] | • Identifies mutations throughout genome• Reveals structural variants• Detects off-target mutations | • Higher cost• Computational complexity• Requires high-quality DNA |
| Targeted Amplicon Sequencing | High-depth variant frequency analysis [38] | • Ultra-high sequencing depth• Cost-effective for multiple samples• Sensitive for rare variants | • Limited to predefined regions• Primer design critical |
| Long-Read Sequencing | Structural variant detection | • Resolves complex rearrangements• Phases mutations• Maps insertion sites precisely | • Higher error rate• Lower throughput• Higher cost per base |
The combination of library generation techniques with next-generation sequencing creates a powerful pipeline for resistance gene identification and mechanism elucidation [6] [20]. This integrated approach enables researchers to move beyond correlation to establish causal relationships between genetic variations and resistance phenotypes. In practice, this involves generating diverse mutant libraries, applying selective pressure (e.g., antibiotic treatment), and sequencing resistant clones to identify enriched mutations [20]. Advanced bioinformatic tools like CARD and ResFinder facilitate the annotation and interpretation of resistance-conferring mutations [6]. For comprehensive resistance gene identification, we recommend iterative cycles of library generation, selection, and sequencing, progressively refining understanding of resistance mechanisms and identifying key genetic determinants.
Data Analysis and Interpretation
Analysis of sequencing data from directed evolution experiments requires specialized bioinformatic approaches. For whole-genome sequencing of resistant clones, the bioinformatic pipeline typically includes: (1) quality control and preprocessing of raw sequencing data; (2) alignment to reference genome; (3) variant calling and annotation; (4) filtering for high-frequency alleles predicted to change protein sequence; and (5) identification of genes that repeatedly acquire mutations across independent selections [20]. This approach successfully identifies known resistance genes (e.g., TOP1, TOP2A, DCK) and novel candidates when applied to drug-resistant cell lines [20]. For large libraries, tracking variant frequency before and after selection through amplicon sequencing identifies enriched mutations, with molecular barcoding methods like SPIDER-seq enabling high-sensitivity detection of rare variants [38].
Research Reagent Solutions
Table 4: Essential Research Reagents for Library Generation
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Error-Prone PCR Kits | Diversify PCR Random Mutagenesis Kit (Clontech), GeneMorph System (Stratagene) [33] | Controlled introduction of random mutations | • Different kits offer distinct mutational biases• Useful for novice researchers |
| Transposition Systems | Commercial transposon kits (ThermoFisher Scientific) [37] | Random insertion mutagenesis | • Engineered transposons maintain reading frame• Enable customization of inserted sequences |
| Gateway Cloning System | pDONR vectors, LR Clonase II enzyme mix [35] | High-efficiency library cloning | • Near 100% cloning efficiency• Streamlines subcloning between vectors |
| High-Fidelity Polymerases | KAPA HiFi, Q5, Phusion | Accurate amplification for library construction | • Essential for DNA shuffling reassembly• Minimizes background mutations |
| Specialized Polymerases | Phi29 DNA polymerase [39] | Rolling circle amplification for mutagenesis | • Enables whole-plasmid mutagenesis• Strong strand displacement activity |
| Mutator Strains | XL1-Red (Stratagene) [33] [37] | In vivo random mutagenesis | • Deficient in DNA repair pathways• Simple system for continuous mutagenesis |
Workflow Diagram
Directed Evolution Workflow for Resistance Gene Identification
This workflow illustrates the integrated process of library generation, selection, and analysis for resistance gene identification. The pathway begins with target gene selection, followed by parallel library generation using Error-Prone PCR, DNA Shuffling, or RAISE methodologies. Libraries then undergo either selective pressure (e.g., antibiotic treatment) or high-throughput screening to isolate variants with enhanced resistance phenotypes. Selected clones proceed to whole-genome sequencing and bioinformatic analysis, culminating in resistance gene identification. The iterative nature of directed evolution enables refinement through multiple cycles, progressively enhancing resistance phenotypes and elucidating underlying genetic mechanisms.
Advanced selection methods are pivotal in modern biotechnology for identifying rare, functionally improved protein variants from vast genetic libraries. This document details two powerful, complementary approaches: FACS-Based Functional Screening using microfluidic co-encapsulation and In Vivo Growth-Coupling Strategies. When integrated with directed evolution frameworks and validated by whole-genome sequencing (WGS), these methods significantly accelerate the engineering of biocatalysts, therapeutics, and other proteins of industrial and pharmaceutical relevance [40] [41] [42].
FACS-based screening enables ultra-high-throughput, functional analysis of library variants by linking a desired cellular function to a fluorescent readout. Concurrently, in vivo growth-coupling provides a powerful selection pressure by directly linking the metabolic activity of a desired enzyme to host cell survival and growth [41] [42]. These methodologies move beyond simple binding assays, enabling the direct selection of variants based on phenotypic activity, which is especially critical for developing novel biopharmaceuticals and enzymes with tailored functions [40] [2].
FACS-Based Functional Screening via Microfluidic Co-encapsulation
Principle and Workflow
This method establishes a genotype-phenotype linkage by co-encapsulating individual yeast cells (secreting a protein variant) and mammalian reporter cells within picoliter-scale agarose microdroplets. The secreted protein accumulates within the droplet, acting on the reporter cell. A functional protein induces a specific response (e.g., GFP expression) in the reporter, which is detected by FACS to isolate the microbead containing the desired yeast variant [40].
The core advantage of this system is its compatibility with standard FACS instruments, bypassing the need for complex custom microfluidic sorters. The use of agarose hydrogel solidification allows for the transfer of droplets from an oil phase to an aqueous buffer for sorting, avoiding the need for detergents that can compromise mammalian cell viability [40].
A general workflow for a directed evolution campaign integrating this screening method is outlined below [40] [42]:
Detailed Experimental Protocol: Model Study with mIL-3
The following protocol is adapted from a model study selecting for functional murine Interleukin-3 (mIL-3) and serves as a template for other biologics [40].
Step 1: Reporter Cell Line Engineering and Validation
- Objective: Generate a mammalian reporter cell line that responds to the target protein with a fluorescent signal.
- Protocol:
- Utilize a murine Ba/F3 progenitor cell line.
- Stably transduce with a construct containing the GFP gene under the control of a promoter responsive to the cytokine of interest (e.g., via the CIS promoter for mIL-3).
- Validate reporter functionality by treating with a concentration gradient of recombinant mIL-3 (e.g., 0.01–40 ng/mL) for 24 hours.
- Analyze by flow cytometry to confirm a dose-dependent increase in GFP fluorescence. Ensure clear separation between non-activated and weakly-activated cell populations for effective FACS gating [40].
Step 2: Secretor Yeast Strain Preparation
- Objective: Engineer yeast cells to secrete the protein library, with an intracellular fluorescent marker correlating to expression levels.
- Protocol:
- Clone the gene of interest (e.g., mIL-3) into a yeast expression vector. Fuse it to a secretion signal (e.g., app831) and link it via a T2A ribosomal skipping sequence to an intracellular fluorescent protein (e.g., mCherry) under a shared inducible promoter (e.g., GAL1) [40].
- Transform the library into an appropriate S. cerevisiae strain (e.g., EBY100).
- Induce protein expression in a suitable induction medium. For co-culture with mammalian cells, test mammalian media (e.g., RPMI) for yeast compatibility, potentially requiring additives and temperature adjustment (30°C) [40].
Step 3: Microfluidic Co-encapsulation in Agarose Microdroplets
- Objective: Pairwise encapsulate yeast secretor cells and mammalian reporter cells in monodisperse, agarose-containing microdroplets.
- Protocol:
- Prepare cell suspensions: Induced yeast cells and mammalian reporter cells, resuspended in warm, liquid low-melting-point agarose solution (e.g., 1-2% in PBS).
- Load the aqueous cell-agarose suspension and an inert carrier oil (e.g., fluorinated oil with surfactant) into a microfluidic droplet generation device.
- Generate water-in-oil (w/o) emulsion droplets with a target diameter of ~40-80 µm, ensuring a high probability of single yeast and single mammalian cell co-encapsulation based on Poisson statistics.
- Collect droplets off-chip and cool to solidify the agarose, forming stable microbeads.
- Prior to FACS, break the emulsion and transfer the agarose microbeads into an aqueous PBS buffer [40].
Step 4: FACS Analysis and Enrichment
- Objective: Identify and sort microbeads containing yeast cells secreting functional proteins.
- Protocol:
- Use a standard FACS sorter equipped with lasers suitable for GFP (e.g., 488 nm) and mCherry (e.g., 561 nm).
- Establish sorting gates based on control samples:
- Negative Control: Beads with reporter cells and yeast secreting a non-functional protein (e.g., mIL-3 E49G mutant).
- Positive Control: Beads with reporter cells and yeast secreting the functional protein (e.g., mIL-3 wt).
- Gate on microbeads that are double-positive for high GFP (reporter activation) and mCherry (successful yeast encapsulation and expression).
- Sort the positive bead population into recovery medium.
- After sorting, dissociate the agarose matrix (e.g., enzymatically or by melting) to recover the yeast cells for regrowth and analysis [40].
Table 1: Key Reagents and Materials for FACS-Based Screening
| Item | Function/Description | Example/Target |
|---|---|---|
| Reporter Cell Line | Produces fluorescent signal upon activation by target protein. | mIL-3-inducible Ba/F3-CIS-d2EGFP cells [40]. |
| Secretor Yeast Strain | Secretes protein variant library; contains expression fluorescence. | S. cerevisiae EBY100 with pYEX-mIL-3-T2A-mCherry [40]. |
| Microfluidic Device | Generates monodisperse water-in-oil emulsion droplets. | PDMS or glass chip with flow-focusing geometry [40]. |
| Low-Melt Agarose | Hydrogel polymer for cell encapsulation and bead stability. | 1-2% in PBS, enables phase transfer for FACS [40]. |
| FACS Instrument | Analyzes and sorts microbeads based on multiplexed fluorescence. | Standard commercial sorter (e.g., BD FACS Aria) [40] [43]. |
Key Performance Data from Model Study
Table 2: Enrichment Data for Functional mIL-3 Selection
| Selection Round | Input Ratio (mIL-3 wt : mIL-3 E49G) | Output / Enrichment | Key Parameter |
|---|---|---|---|
| Starting Library | 1 : 10,000 | Baseline | Robust GFP signal vs. control [40]. |
| FACS Sort 1 | Not specified | Positive population collected | Gating on GFP+/mCherry+ beads [40]. |
| FACS Sort 2 | Not specified | Successful enrichment achieved | Two rounds of co-encapsulation/FACS [40]. |
In Vivo Growth-Coupling for Enzyme Selection
Principle of Enzyme Selection Systems (ESS)
Enzyme Selection Systems (ESS) are engineered chassis cells designed to have a severe, growth-limiting metabolic chokepoint that can only be alleviated by the activity of a desired enzyme. This creates a direct, selectable link between the enzyme's catalytic function and the host's metabolic activity and growth, enabling direct selection for improved enzyme variants from large libraries without the need for external screening [41].
The design principle is to couple the target enzyme's activity to the overall microbial metabolic activity, not just the synthesis of a single biomass precursor. Computational workflows, such as constraint-based metabolic modeling, are used to identify and design these coupling strategies in organisms like E. coli [41].
Protocol for Implementing an ESS
Step 1: Computational Design of the ESS
- Objective: Identify gene knockouts or metabolic perturbations that create a conditional essentiality for the target enzyme's reaction.
- Protocol:
- Use a genome-scale metabolic model (e.g., of E. coli).
- Apply a computational workflow (e.g., using the CobraPy toolbox) to simulate gene deletions that render cell growth dependent on the flux through the reaction catalyzed by the target enzyme.
- Calculate the Growth-Coupling Strength (GCS) to rank designs. Select a design with suboptimal but sufficient coupling strength to avoid non-viable ESS strains [41].
Step 2: Chassis Strain Construction
- Objective: Genetically engineer the host strain to implement the designed metabolic chokepoint.
- Protocol:
- Using the computational design as a blueprint, perform precise gene knockouts in the chosen host organism (e.g., E. coli) using techniques like CRISPR-Cas or lambda Red recombination.
- Validate the engineered chassis by confirming its auxotrophy or severe growth defect under non-permissive conditions (e.g., in a defined minimal medium without the necessary metabolite). Growth should be restored upon expression of a functional version of the target enzyme [41].
Step 3: Library Selection and Variant Isolation
- Objective: Isolate improved enzyme variants by growing the library in the ESS under selective pressure.
- Protocol:
- Transform the engineered ESS strain with the plasmid library encoding the enzyme variants.
- Plate the transformed cells on solid minimal medium or inoculate into liquid minimal medium to impose the selection pressure. Only cells expressing enzyme variants that sufficiently overcome the metabolic chokepoint will grow.
- Isolate individual colonies that appear after an appropriate incubation time. Larger, faster-growing colonies often harbor the most active enzyme variants.
- Re-streak isolates to confirm phenotype and sequence the enzyme gene to identify beneficial mutations [41].
Table 3: Key Resources for In Vivo Growth-Coupling
| Item | Function/Description | Example/Source |
|---|---|---|
| Metabolic Model | In silico platform for predicting growth-coupling strategies. | E. coli GEM (e.g., iJO1366) [41]. |
| ESS Design Database | Repository of pre-computed strain designs. | Publicly accessible database with 25,505 E. coli ESS designs [41]. |
| Chassis Organism | Host for implementing the metabolic chokepoint. | Escherichia coli K-12 MG1655 [41]. |
| Genetic Toolset | For precise genome editing in the chassis organism. | CRISPR-Cas9 or Lambda Red Recombinase System [41]. |
Integration with Whole-Genome Sequencing and Directed Evolution
The Directed Evolution Cycle
Directed evolution mimics natural selection in the laboratory to optimize protein functions. The general cycle involves iterative rounds of diversity generation, selection/screening, and amplification [2] [42]. The advanced methods described herein are primarily applied in the selection/screening phase.
Table 4: Core Steps in a Directed Evolution Campaign
| Step | Description | Common Methodologies |
|---|---|---|
| 1. Diversity Generation | Creating a large library of gene variants. | Error-prone PCR, DNA shuffling, site-saturation mutagenesis [2] [42]. |
| 2. Selection/Screening | Identifying variants with desired properties. | FACS-based screening (Sect. 2) or In vivo growth-coupling (Sect. 3) [40] [41]. |
| 3. Gene Amplification | Recovering and amplifying genes of best hits. | PCR from sorted cells/selected colonies [42]. |
Role of Whole-Genome Sequencing (WGS)
WGS is a critical tool for validating directed evolution outcomes and understanding resistance mechanisms.
- Resistance Gene Identification: WGS provides comprehensive data on acquired resistance genes and chromosomal mutations conferring antibiotic resistance in pathogens, allowing for genotype-phenotype comparisons [44] [12].
- Validation of Selected Variants: After selection cycles, WGS of evolved clones identifies all accumulated mutations, revealing the genetic basis for improved function and potential off-target effects [44].
- Strain Quality Control: WGS ensures that the genetic background of engineered ESS chassis strains is correct and identifies any unintended mutations that may have arisen during construction [12].
Table 5: Example WGS Agreement with Phenotypic Resistance in E. coli
| Antibiotic | Categorical Agreement (Genotype vs. Phenotype) | Discrepancy Notes |
|---|---|---|
| Meropenem | 100% | No resistance observed in the study [12]. |
| Gentamicin | 100% | High predictive value [12]. |
| Amikacin | >95% | High predictive value [12]. |
| Ciprofloxacin | <95% | Lower agreement; complex resistance mechanisms [12]. |
Research Reagent Solutions
Table 6: Essential Materials and Reagents for Advanced Selection Methods
| Category | Specific Item | Function in Experiment | Example Product/System |
|---|---|---|---|
| Library Creation | Error-Prone PCR Kit | Introduces random mutations across the gene of interest. | KAPA2G Fast Multiplex PCR Kit [42]. |
| Cell Culture & Engineering | Yeast Expression System | Host for secreting protein variant libraries. | S. cerevisiae EBY100 & pYEX vectors [40]. |
| Mammalian Cell Line | Engineered reporter cell for functional response. | Ba/F3-CIS-d2EGFP [40]. | |
| Microfluidics & Encapsulation | Droplet Generation Chip | Creates monodisperse water-in-oil emulsions. | Microfluidic PDMS chip (Flow-focusing) [40]. |
| Low-Melting-Point Agarose | Forms hydrogel microbeads for cell encapsulation. | Standard molecular biology grade [40]. | |
| Analysis & Sorting | High-Throughput Flow Cytometer | Analyzes and sorts samples at high speed (~40 wells/min). | IntelliCyt HTFC Screening System [43]. |
| Sequencing & Validation | Next-Generation Sequencer | Provides whole-genome data for variant/resistance analysis. | Illumina MiSeq/NovaSeq [12]. |
| DNA Extraction & Library Prep Kit | Prepares high-quality sequencing libraries. | KAPA HyperPlus Kit [12]. |
In the field of directed evolution and whole-genome sequencing for resistance gene identification, the choice of sequencing technology is paramount. Next-generation sequencing (NGS) has revolutionized genomics research by enabling the rapid sequencing of millions of DNA fragments simultaneously, providing comprehensive insights into genome structure, genetic variations, and gene expression profiles [45]. Researchers now face a critical decision between short-read and long-read sequencing technologies, each with distinct advantages and limitations for specific applications in resistance gene characterization.
This application note provides a detailed comparison of these technologies, offering experimental protocols and strategic guidance tailored for scientists investigating antimicrobial resistance mechanisms and conducting directed evolution studies. The massive parallelization offered by NGS has transformed previously laborious sequencing tasks into high-throughput operations, making it possible to sequence an entire human genome in hours instead of years and at a fraction of the cost [46]. For researchers focused on resistance mechanisms, this technological advancement enables unprecedented insights into the genetic basis of drug resistance across diverse pathogens.
Technology Comparison: Short-Read vs. Long-Read Sequencing
Fundamental Differences and Technical Specifications
Short-read sequencing (typically 50-600 base pairs) employs massively parallel sequencing of small DNA fragments, with Illumina's sequencing-by-synthesis (SBS) technology representing the dominant platform in this category [45] [47]. This approach offers ultra-high throughput and exceptional base-level accuracy, exceeding 99.9% per base [46]. Short-read platforms excel at detecting single nucleotide polymorphisms (SNPs) and small insertions/deletions (indels) with high confidence, making them ideal for variant calling and quantitative applications [45].
Long-read sequencing, also known as third-generation sequencing, generates reads tens of thousands of bases long through technologies such as Pacific Biosciences (PacBio) Single-Molecule Real-Time (SMRT) sequencing and Oxford Nanopore Technologies (ONT) [45] [47]. These platforms sequence individual DNA molecules without amplification, preserving epigenetic information and capturing structural variations often missed by short-read technologies [46]. While historically characterized by higher error rates, recent advancements have substantially improved accuracy, particularly through PacBio's HiFi mode which combines long reads with high accuracy through circular consensus sequencing [48].
Table 1: Comparative Analysis of Short-Read and Long-Read Sequencing Technologies
| Parameter | Short-Read Sequencing | Long-Read Sequencing |
|---|---|---|
| Read Length | 50-600 bp [47] | 10,000-30,000+ bp [45] |
| Primary Platforms | Illumina, Ion Torrent | PacBio SMRT, Oxford Nanopore |
| Accuracy | >99.9% per base [46] | Variable; ~97% raw, >99.9% with HiFi [48] |
| Throughput | High to ultra-high | Moderate to high |
| Cost perGb | Lower | Higher |
| DNA Input | Low (can be amplified) | Higher (often requires high molecular weight DNA) |
| Best Applications | Variant detection, expression profiling, targeted sequencing | De novo assembly, structural variant detection, haplotype phasing |
| Limitations | Struggles with repetitive regions, complex structural variants | Higher cost per sample, potentially lower base-level accuracy for some applications |
Performance in Resistance Gene Identification
For researchers investigating resistance mechanisms, each technology offers distinct advantages. Short-read sequencing demonstrates excellent performance for comprehensive single nucleotide variant detection and quantification of allele frequencies in mixed populations [49]. This makes it particularly valuable for tracking the emergence of resistance-conferring point mutations in directed evolution experiments.
Long-read sequencing excels in resolving complex genomic regions rich in repetitive elements, which are frequently associated with resistance mechanisms in pathogens like Mycobacterium tuberculosis [50]. The PE/PPE gene families in M. tuberculosis, which constitute approximately 10% of the genome and contain GC-rich repetitive elements, are challenging to sequence with short-read technology but are effectively characterized with long-read approaches [50]. A comparative study demonstrated that long-read and hybrid approaches achieved optimal coverage in these difficult regions, whereas short-read sequencing showed significantly lower performance [50].
In microbial epidemiology and resistance gene characterization, long-read sequencing provides more complete information about the genomic context of resistance genes, including their location on plasmids, chromosomes, or other mobile genetic elements [51]. This structural information is crucial for understanding the transmission dynamics of resistance mechanisms in hospital and community settings.
Experimental Protocols
Protocol 1: Short-Read Whole Genome Sequencing for Resistance Variant Detection
Application: Identification of single nucleotide polymorphisms and small indels associated with drug resistance in bacterial populations from directed evolution experiments.
Workflow Steps:
- DNA Extraction: Use standardized kits (e.g., Promega Maxwell, Qiagen DNeasy) to extract genomic DNA from bacterial cultures. Verify DNA quality and quantity using fluorometric methods (Qubit) and fragment analysis (TapeStation) [51].
- Library Preparation: Employ Illumina Nextera DNA Flex Library Prep Kit or similar:
- Fragment DNA to target size (350-800 bp) via enzymatic or mechanical shearing
- Perform end repair, A-tailing, and adapter ligation with dual indexing
- Amplify library with 8-10 PCR cycles using high-fidelity polymerase [49]
- Quality Control: Assess library size distribution (TapeStation 4150), quantify (Qubit Fluorometer), and validate absence of primer dimers [49].
- Sequencing: Dilute library to appropriate concentration (100-200 pM for iSeq100; 12 pM for MiSeq) and sequence with 2×150 bp paired-end configuration using Illumina platforms. Include 1% PhiX control for quality monitoring [51] [49].
- Data Analysis:
Key Considerations: This protocol is optimized for detection of minority variants present at frequencies as low as 5-10%, enabling identification of emerging resistance mutations in heterogeneous populations [49].
Protocol 2: Long-Read Sequencing for Structural Variation Analysis in Resistance Genomes
Application: Comprehensive characterization of structural variations, repetitive regions, and complex resistance loci in bacterial genomes.
Workflow Steps:
- High Molecular Weight DNA Extraction: Use specialized kits (Zymo Genomic DNA Clean & Concentrator) to preserve long DNA fragments. Verify DNA integrity via pulsed-field gel electrophoresis or Genomic DNA ScreenTape analysis [50].
- Library Preparation for Nanopore Sequencing:
- Quality Control: Assess library quantity with Qubit HS DNA assay and fragment size distribution with Genomic DNA ScreenTape.
- Sequencing: Load library at optimal concentration (1 pM) onto MinION flow cells (FLO-MIN106D). Sequence for 24-72 hours using MinKNOW software with base calling enabled [50].
- Data Analysis:
- Perform base calling with Guppy or Dorado
- Conduct quality assessment with NanoPlot
- Assemble genomes using Flye or Canu assemblers
- Polish assemblies with Medaka or using Illumina short reads
- Annotate resistance genes using ABL DeepChek or ARG-ANNOT databases [49]
Key Considerations: This protocol enables complete assembly of resistance plasmids and characterization of insertion sequences and repetitive elements that may harbor resistance genes [50] [51].
Protocol 3: Hybrid Approach for Complete Resistance Genome Resolution
Application: Maximum accuracy variant calling combined with structural variant detection for comprehensive resistance profiling.
Workflow Steps:
- Parallel Library Preparation: Prepare both short-read (Illumina) and long-read (Nanopore) libraries from the same DNA extraction as described in Protocols 1 and 2 [50].
- Sequencing: Run both libraries on their respective platforms using standardized conditions.
- Data Integration and Analysis:
- Correct long reads with high-accuracy short reads using Ratatosk or similar hybrid correction tools [50]
- Perform genome assembly using hybrid assemblers such as Unicycler or SPAdes
- Call variants using pipelines optimized for hybrid data (customized MTBseq) [50]
- Annotate resistance-associated variants and structural changes using pathogen-specific databases
Key Considerations: The hybrid approach leverages the accuracy of short reads with the contiguity of long reads, providing the most comprehensive view of resistance genomes. This method has demonstrated superior performance in comparative studies, particularly for challenging genomic regions associated with drug resistance [50].
Diagram 1: Comprehensive workflow for resistance gene identification integrating short-read and long-read technologies. The hybrid approach maximizes the advantages of both platforms.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for Resistance Gene Sequencing
| Reagent/Platform | Function | Application Notes |
|---|---|---|
| DeepChek Whole Genome HIV-1 Assay | Amplification of HIV-1 genome for resistance mutation detection | Enables detection of minority variants (<20%) in protease, reverse transcriptase, and integrase regions [48] |
| Nextera DNA Flex Library Prep Kit | Library preparation for Illumina platforms | Optimized for bacterial genomes; suitable for low-input samples [51] |
| SQK-LSK109 Ligation Sequencing Kit | Library preparation for Nanopore sequencing | Preserves long DNA fragments; compatible with barcoding for multiplexing [50] |
| MagNA Pure 24 System | Automated nucleic acid extraction | Ensures consistent yield and purity; critical for reproducible results [49] |
| MTBseq Pipeline | Bioinformatic analysis of bacterial sequencing data | Customizable for inclusion of repetitive regions; optimized for resistance variant calling [50] |
| ABL DeepChek Software | Comprehensive analysis of resistance mutations | Compatible with multiple sequencing platforms; maintains extensive resistance database [49] |
| Oxford Nanopore MinION Mk1B | Portable long-read sequencing | Enables real-time sequencing analysis; suitable for rapid resistance profiling [51] |
| Illumina iSeq 100 System | Benchtop short-read sequencing | Cost-effective for targeted resistance gene sequencing; fast turnaround [51] |
Strategic Implementation Guide
Technology Selection Framework
Choosing between short-read and long-read technologies requires careful consideration of research goals, sample types, and resource constraints. The following framework supports informed decision-making:
Select Short-Read Sequencing When:
- Primary focus is on single nucleotide variants and small indels associated with resistance
- Studying large sample sets requiring high throughput and cost-effectiveness
- Working with low-quality or degraded DNA samples
- Research questions involve quantitative assessment of allele frequencies in mixed populations [48] [49]
Select Long-Read Sequencing When:
- Investigating complex genomic regions with repeats or low complexity
- Characterizing structural variations, insertions, or deletions larger than 50 bp
- Performing de novo genome assembly of resistant strains
- Resolving haplotype phasing to understand linkage of resistance mutations [50] [51]
Implement Hybrid Approaches When:
- Pursuing complete genome resolution with maximum accuracy
- Studying particularly challenging genomes with high repetition or GC content
- Resources permit comprehensive analysis using both technologies
- Research requires both variant accuracy and structural context [50]
Emerging Trends and Future Directions
The field of resistance gene sequencing continues to evolve rapidly. Promising developments include:
Improved Long-Read Accuracy: New sequencing chemistries and analysis algorithms are substantially enhancing the accuracy of long-read technologies. PacBio's HiFi sequencing now delivers >99.9% accuracy with read lengths of 10-20 kb, bridging the accuracy gap between short and long-read platforms [48].
Hybrid Analysis Pipelines: Advanced bioinformatic tools that intelligently integrate short and long-read data are becoming more sophisticated and user-friendly. Tools like Ratatosk and Unicycler enable researchers to leverage the complementary strengths of both technologies [50].
Portable Sequencing Solutions: The miniaturization of sequencing technology, particularly Nanopore devices, enables real-time resistance profiling in clinical or field settings. This facilitates rapid intervention and containment of resistant outbreaks [51].
AI-Assisted Resistance Prediction: Machine learning approaches are increasingly being applied to predict resistance phenotypes from genotypic data, helping to address the challenge of imperfect genotype-phenotype correlations [52].
The strategic selection between short-read and long-read sequencing technologies is fundamental to successful resistance gene identification in directed evolution studies. Short-read platforms offer unparalleled accuracy for variant detection, while long-read technologies provide unique insights into structural variations and complex genomic regions. For the most comprehensive resistance profiling, hybrid approaches that integrate both technologies deliver superior genome resolution.
As sequencing technologies continue to advance and costs decrease, the implementation of these methods will become increasingly accessible, empowering researchers to tackle the growing challenge of antimicrobial resistance with unprecedented precision and efficiency. The protocols and strategic guidance provided herein offer a foundation for optimizing sequencing approaches to address specific research questions in resistance gene characterization.
Antimicrobial resistance (AMR) presents a critical global health threat, with estimates attributing 1.27 million deaths directly to AMR worldwide and projections suggesting this number could rise to 10 million annually by 2050 [53]. The advent of affordable whole-genome sequencing (WGS) has revolutionized AMR research, enabling scientists to identify resistance determinants directly from bacterial genomes and complex metagenomic samples [6] [44]. Within the specific research context of directed evolution and whole-genome sequencing for resistance gene identification, bioinformatic databases play an indispensable role in annotating and characterizing the genetic basis of resistance [20].
This application note provides a detailed overview of three primary antibiotic resistance gene (ARG) databases—CARD, ResFinder, and MEGARes—focusing on their practical application in experimental workflows for identifying resistance mechanisms discovered through directed evolution studies and WGS. We present structured comparisons, standardized protocols for database utilization, and visualization tools to assist researchers in selecting appropriate resources for resistance gene identification and characterization.
Comprehensive Antibiotic Resistance Database (CARD)
CARD is a rigorously curated bioinformatic database that employs the Antibiotic Resistance Ontology (ARO) to organize resistance genes, their products, and associated phenotypes [54]. Its ontology-driven structure classifies resistance determinants, mechanisms, and antibiotic molecules into a logical framework that supports sophisticated computational analysis [6]. CARD's curation standards require that included sequences be deposited in GenBank, demonstrate an experimentally validated increase in Minimal Inhibitory Concentration (MIC), and be published in peer-reviewed literature [6].
The database includes several specialized features and modules:
- CARD-R (Resistomes & Variants): Computer-generated resistome predictions for 414 important pathogens, including sequence variants beyond those reported in scientific literature [54]
- FungAMR: A specialized component for investigating fungal mutations associated with AMR [54]
- TB Mutations: A curated list of Mycobacterium tuberculosis mutations from ReSeqTB, CRyPTIC, and WHO catalogs [54]
- CARD:Live: A pilot project that collects pathogen identification, MLST, and AMR gene data from submissions to the RGI online platform [54]
CARD's analytical capabilities are centered around the Resistance Gene Identifier (RGI) software, which predicts resistomes based on homology and SNP models [54]. The database also provides BLAST functionality and a bait capture platform for targeted metagenomic detection of resistance determinants [54].
ResFinder and PointFinder
ResFinder is a specialized database and tool for identifying acquired antimicrobial resistance genes in fully or partially sequenced bacterial isolates [53] [55]. Initially based on the Lahey Clinic β-Lactamase Database and ARDB, it has expanded through extensive literature review and now covers a broad spectrum of acquired resistance genes categorized by antimicrobial classes and resistance mechanisms [6].
PointFinder specializes in detecting chromosomal point mutations conferring resistance in specific bacterial species [6]. The integration of ResFinder and PointFinder under the ResFinder 4.0 project has created a unified framework for detecting both acquired genes and chromosomal mutations, complete with phenotype prediction tables that link genetic information to potential resistance traits [6].
A key technical feature of ResFinder is its use of a K-mer-based alignment algorithm, which enables rapid analysis directly from raw sequencing reads without requiring de novo assembly [6]. This makes it particularly valuable for clinical settings where turnaround time is critical.
MEGARes
MEGARes is a comprehensive AMR database that incorporates data from multiple sources, including CARD, ARG-ANNOT, and ResFinder, while addressing sequence redundancy to create a non-redundant resource optimized for high-throughput sequencing analysis [53] [55]. Its structure is designed specifically for metagenomic analysis, making it particularly suitable for environmental resistome studies where multiple organisms contribute to the resistance gene pool.
The database employs a hierarchical annotation structure that categorizes resistance genes into four levels: mechanism, class, group, and gene. This multi-level classification system enables researchers to analyze AMR data at different resolutions, from broad mechanistic overviews to specific gene variants [53].
Comparative Database Analysis
Table 1: Quantitative comparison of major ARG databases
| Database | Last Update | Primary Focus | Gene Count | Mutation Data | Metagenomic Support | Analysis Tools |
|---|---|---|---|---|---|---|
| CARD | 2025 [54] | Comprehensive resistance ontology | 6,442 reference sequences [54] | Yes (TB Mutations, SNP models) [54] | Yes (RGI, bait capture) [54] | RGI, BLAST, CARD:Live [54] |
| ResFinder/PointFinder | 2021 [53] | Acquired genes & point mutations | Not specified in sources | Yes (PointFinder) [6] | Limited | K-mer based alignment [6] |
| MEGARes | 2019 [53] | Non-redundant reference for high-throughput analysis | Combined from multiple sources [55] | Limited | Optimized for metagenomics | Compatible with various tools [53] |
Table 2: Database content and structural comparison
| Feature | CARD | ResFinder | MEGARes |
|---|---|---|---|
| Curation Method | Manual expert curation with experimental validation [6] | Literature review & specialized curation [6] | Integration of multiple databases with redundancy removal [53] |
| Ontology Structure | ARO with three branches: determinants, mechanisms, antibiotics [6] | Categorized by antimicrobial class & mechanism [6] | Hierarchical: mechanism→class→group→gene [53] |
| Mobile Genetic Elements | Included when associated with ARGs | Limited focus | Included |
| Strengths | Detailed mechanism information, phenotype prediction, regular updates [54] [6] | Rapid analysis, mutation detection, integrated genotype-phenotype tables [6] | Non-redundant, metagenomics-optimized, hierarchical annotation [53] |
| Limitations | Dependent on manual curation pace [6] | Less comprehensive for non-acquired resistance | Less frequently updated [53] |
Application in Directed Evolution and Whole-Genome Sequencing
Database Integration in Resistance Identification Workflow
In vitro evolution and whole genome analysis (IVIEWGA) has emerged as a powerful methodology for studying resistance mechanisms in haploid human cells and microbial pathogens [20]. This approach involves exposing clonal populations to sublethal antibiotic concentrations, selecting for resistant clones, and comparing their genomes to susceptible ancestors using next-generation sequencing [20]. ARG databases are essential for annotating the genetic variants that emerge during these experimental evolution studies.
The following workflow diagram illustrates the integrated role of ARG databases in a typical directed evolution study for resistance gene identification:
Diagram 1: ARG Database Integration in Directed Evolution Workflow (76 characters)
Database Selection Guidelines for Different Research Scenarios
The choice of ARG database significantly impacts research outcomes, and selection should be guided by specific experimental goals:
- For comprehensive resistance mechanism studies: CARD's detailed ontology and inclusion of both acquired and mutational resistance make it ideal for understanding complete resistance landscapes [6].
- For clinical isolate screening and rapid diagnostics: ResFinder's K-mer based approach and PointFinder's mutation detection provide fast, clinically actionable results [6].
- For environmental metagenomics and resistome analysis: MEGARes's non-redundant structure and hierarchical classification optimize it for complex microbial community data [53].
- For directed evolution experiments: CARD and ResFinder/PointFinder combined offer complementary coverage for detecting both acquired genes and chromosomal mutations that emerge under selective pressure [20].
Recent research on Listeria monocytogenes demonstrates the value of multi-database approaches, where studies simultaneously utilized CARD, ResFinder, and MEGARes to identify recurrent resistance determinants across diverse sample types and geographies [56].
Experimental Protocols and Methodologies
Standardized Protocol for ARG Annotation from Whole-Genome Data
This protocol describes a comprehensive workflow for identifying antibiotic resistance genes from bacterial whole-genome sequencing data, optimized for use in directed evolution studies.
Input Data Requirements
- Sequence data: Illumina paired-end reads (2×150 bp or 2×250 bp) or long-read data (Oxford Nanopore, PacBio)
- Quality control: FastQC report with Q-score >30 for Illumina data
- Minimum coverage: 50× for reliable variant detection in evolved clones [20]
Bioinformatics Processing Steps
Step 1: Quality Control and Preprocessing
Step 2: Genome Assembly
Step 3: Parallel ARG Annotation Using Multiple Databases
Step 4: Results Integration and Visualization
- Compile results from all databases into a unified table
- Filter hits based on identity (>80%) and coverage (>90%) thresholds [56]
- Cross-reference with phenotype data when available
Quality Control and Validation
- Positive controls: Include reference strains with known resistance profiles
- Phenotypic correlation: Compare genotypic predictions with MIC measurements when possible [56]
- Manual inspection: Verify ambiguous hits by checking adjacent genetic context for mobile elements
Protocol for Detecting Emerging Resistance in Directed Evolution Studies
Directed evolution experiments applying selective pressure with subinhibitory antibiotic concentrations generate unique requirements for resistance detection:
Experimental Design Considerations:
- Time-series sampling: Collect samples at regular intervals during evolution experiment
- Independent replicates: Perform at least 3 independent selection lines to distinguish adaptive mutations from random drift [20]
- Selective pressure: Use concentrations at 3-5× EC50 values for lethal selections or stepwise increases for gradual adaptation [20]
Bioinformatic Analysis of Evolved Clones:
Validation of Candidate Resistance Mutations:
- Gene knockout/complementation: Confirm causality by introducing mutations into naive backgrounds [20]
- Transcriptional analysis: Assess expression changes in resistance genes and efflux pumps
- Dose-response curves: Compare EC50 values between evolved and ancestral clones [20]
Table 3: Key research reagents and computational tools for ARG analysis
| Category | Item/Resource | Specification/Function | Application in Directed Evolution |
|---|---|---|---|
| Wet-Lab Reagents | Antimicrobial compounds | Clinical-grade antibiotics for selective pressure | Creating evolution environments [20] |
| Culture media | Mueller-Hinton broth/agar for AST | Standardized phenotypic resistance testing [56] | |
| DNA extraction kits | High-molecular weight DNA isolation | Preparing sequencing libraries | |
| Reference Materials | Control strains | ATCC strains with known resistance profiles | Method validation and quality control [56] |
| Breakpoint standards | CLSI/EUCAST guidelines | Interpreting phenotypic resistance [57] | |
| Bioinformatics Tools | RGI (CARD) | Resistance Gene Identifier software | Comprehensive ARG annotation [54] |
| ResFinder | K-mer based gene detection | Rapid screening of acquired ARGs [6] | |
| AMRFinderPlus | NCBI's resistance finder | Detecting genes and point mutations [57] | |
| Abricate | Wrapper for multiple databases | Multi-database screening [56] | |
| Computational Resources | BV-BRC database | Bacterial & Viral Bioinformatics Resource Center | Access to genomic and phenotype data [57] |
| CARD:Live | Dynamic resistome database | Real-time tracking of emerging ARGs [54] |
The strategic selection and application of ARG databases—CARD, ResFinder, and MEGARes—provide complementary strengths for identifying and characterizing antibiotic resistance mechanisms in directed evolution and whole-genome sequencing studies. CARD offers unparalleled mechanistic depth through its ontology-driven structure, ResFinder delivers rapid detection of acquired resistance, and MEGARes provides optimized resources for metagenomic analysis. As antimicrobial resistance continues to evolve, these bioinformatic resources will play an increasingly critical role in tracking emerging resistance threats and developing novel therapeutic strategies. The standardized protocols and comparative analyses presented here offer researchers practical guidance for implementing these databases in resistance gene identification workflows.
Tuberculosis and Klebsiella pneumoniae co-infections represent a significant clinical challenge in infectious disease management, particularly in regions with high TB burden. These co-infections are characterized by complex host-pathogen interactions and worsened patient outcomes due to several synergistic factors. Pulmonary TB creates an immunocompromised environment through destructive alterations of lung parenchyma, bronchiectasis, and scarring, which impair normal pulmonary function and reduce protective immunity [58]. This immunodysfunction significantly increases susceptibility to opportunistic pathogens like K. pneumoniae [59]. The convergence of these two pathogens is particularly concerning given the rising incidence of multidrug-resistant (MDR) strains in both organisms, which complicates therapeutic interventions and increases mortality risk [58] [60].
The epidemiological significance of TB and K. pneumoniae co-infections is substantial. Research indicates that among pulmonary TB patients with bacterial co-infections, K. pneumoniae is one of the most common coexisting pathogens [58] [59]. A study conducted at a tertiary teaching hospital in China found that 31.4% of pulmonary TB patients had bacterial co-infections, with K. pneumoniae being a predominant organism [58]. Another surveillance study identified K. pneumoniae as the main pathogen associated with healthcare-associated infections, with carbapenem-resistant K. pneumoniae (CRKP) widely distributed across multiple regions [61]. Understanding the genomic and evolutionary mechanisms driving resistance in these co-infections is paramount for developing effective diagnostic and therapeutic strategies.
Clinical Case Studies: Manifestations and Therapeutic Challenges
Case Series: Clinical Presentations and Outcomes
Analysis of clinical cases reveals distinctive patterns in TB and K. pneumoniae co-infections. The table below summarizes findings from recent case studies and clinical series:
Table 1: Clinical Characteristics of TB and K. pneumoniae Co-infection Cases
| Case Source | Patient Demographics | TB Diagnosis | K. pneumoniae Strain Characteristics | Clinical Management | Outcome |
|---|---|---|---|---|---|
| Retrospective Study (n=76) [58] | Median age 56.8 years; 81.6% male | 48.7% primary TB; 51.3% retreated TB | 36.3% ESBL-producing; 8.8% carbapenem-resistant | Varies; MDR-group required more respiratory support | MDR-group had more pronounced inflammatory responses |
| Miliary TB Case Report [60] | 47-year-old male, low socioeconomic status | Miliary, rifampicin-resistant | CRKP (resistant to cephalosporins, imipenem, carbapenem) | Piperacillin-tazobactam + MDR-TB regimen + steroids | Improved by day 18; stable at 8-month follow-up |
| Nanopore Sequencing Study (n=23) [62] | Median age 58 years; 52.17% female | 20 MTB cases; 3 NTM cases | Identified as common co-pathogen with MTB | Tailored regimens based on sequencing results | Variable; sequencing guided targeted therapy |
A particularly illustrative case involved a 47-year-old male with miliary TB who developed co-infection with carbapenem-resistant K. pneumoniae [60]. Despite initiating a standard MDR-TB regimen, the patient's oxygen saturation dropped to 85% by day 9, requiring intravenous steroids and ventilatory support. The therapeutic challenge intensified when bronchoscopy revealed K. pneumoniae resistant to third-generation cephalosporins, imipenem, and carbapenem, but sensitive to piperacillin. The combination of piperacillin-tazobactam with continued MDR-TB regimen and corticosteroids eventually led to clinical improvement, highlighting the necessity of comprehensive antimicrobial susceptibility testing in co-infected patients [60].
Comparative Analysis of Resistance Patterns
The resistance profiles of K. pneumoniae in TB co-infections present significant treatment challenges. In a study of 80 isolates from TB patients, 29 (36.3%) were extended-spectrum β-lactamase (ESBL)-producing strains, and 7 (8.8%) were carbapenem-resistant Enterobacteriaceae (CRE) [58]. Genomic analysis revealed diverse sequence types, with ST23 (15%), ST15 (12.5%), and ST273 (7.5%) being most prevalent. Notably, 26.25% of strains were classically hypervirulent K1/K2 K. pneumoniae, all carrying salmochelin and rmpA virulence genes [58]. Patients infected with MDR K. pneumoniae strains required more respiratory support (40.6% vs. 18.2%) and exhibited higher inflammatory markers, including elevated C-reactive protein (62.6% vs. 41.8%) and lower hemoglobin levels (87.5% vs. 47.7%) compared to those with non-MDR strains [58].
Genomic Methodologies for Resistance Gene Identification
Whole-Genome Sequencing Protocols
Comprehensive genomic analysis of TB and K. pneumoniae co-infections requires standardized methodologies for pathogen identification and resistance gene detection. The following workflow outlines the core process:
Figure 1: Comprehensive workflow for genomic analysis of TB and K. pneumoniae co-infections.
Sample Processing and DNA Extraction
Clinical samples (sputum, bronchoalveolar lavage, or biopsy tissue) undergo processing for simultaneous isolation of mycobacterial and bacterial pathogens. For K. pneumoniae, DNA extraction uses commercial kits such as the QIAamp DNA Kit (Qiagen) following manufacturer's instructions [61]. For M. tuberculosis, due to its complex cell wall, additional mechanical or enzymatic lysis steps are incorporated. DNA quality and quantity should be assessed using fluorometric methods (e.g., Qubit fluorometer) with minimum concentration thresholds of 20 ng/μL and purity ratios (A260/A280) between 1.8-2.0 [61].
Library Preparation and Sequencing
Tagmentation-based library preparation kits (e.g., Illumina Nextera) are recommended for efficient fragmentation and adapter ligation. For comprehensive resistance profiling, both short-read (Illumina MiniSeq, NovaSeq) and long-read (Oxford Nanopore GridION) platforms should be employed in a complementary approach [61] [62]. The Nanopore sequencing protocol, as implemented in recent studies, enables real-time analysis and rapid turnaround, which is crucial for clinical decision-making in co-infection cases [62].
Genomic Analysis Pipeline
Quality Control and Assembly
Raw sequencing reads require rigorous quality assessment and preprocessing. The following steps are critical:
- Quality Control: FastQC for initial quality assessment, followed by adapter trimming and quality filtering using Trimmomatic (parameters: LEADING:3, TRAILING:3, SLIDINGWINDOW:4:15, MINLEN:36) [61].
- Genome Assembly: De novo assembly using SPAdes assembler v.3.15.5 with k-mer ranges from 21-71 for optimal contiguity [61]. For reference-guided assembly, RagTag v.2.1.0 can improve draft genomes using reference strains (e.g., K. pneumoniae HS11286, M. tuberculosis H37Rv).
- Assembly Quality Assessment: QUAST v.5.0.5 evaluates assembly metrics (N50, contig number, total length), with exclusion of contigs <200 bp [61].
Resistance Gene Identification
Comprehensive antimicrobial resistance profiling requires multiple bioinformatic tools:
- AMRFinderPlus: NCBI's tool for identifying AMR genes, resistance-associated point mutations, and other resistance mechanisms using curated Reference Gene Database [63].
- RGI (Resistance Gene Identifier): CARD-based analysis for predicting resistomes from protein or nucleotide data using homology and SNP models [64].
- Kleborate: Specifically designed for K. pneumoniae genomic analysis, profiling resistance genes, virulence factors, and capsule typing [58] [61].
- ResFinder: Detection of acquired antimicrobial resistance genes in M. tuberculosis with integration of WHO mutation catalog for standardized reporting [61].
Table 2: Essential Research Reagents and Computational Tools for Genomic Analysis
| Category | Specific Tool/Reagent | Application/Function | Key Features |
|---|---|---|---|
| Wet Lab Reagents | QIAamp DNA Kit | Nucleic acid extraction | Efficient extraction from Gram-negative and acid-fast bacteria |
| Illumina DNA Prep Kits | Library preparation | Tagmentation-based approach for efficient library construction | |
| Oxford Nanopore Ligation Kits | Long-read library prep | Enables real-time sequencing and structural variant detection | |
| Bioinformatic Tools | SPAdes | Genome assembly | De novo assembler optimized for bacterial genomes |
| AMRFinderPlus | Resistance gene detection | NCBI-curated database with comprehensive resistance markers | |
| Kleborate | K. pneumoniae genotyping | MLST, resistance, and virulence profiling in one tool | |
| RGI (CARD) | Resistance analysis | Homology-based detection with curated significance thresholds | |
| Reference Databases | CARD | Antibiotic resistance | Curated repository of resistance genes, variants, and mechanisms |
| NCBI Pathogen Detection | Genomic epidemiology | Platform for comparing clinical isolates across outbreaks | |
| SRA | Raw sequence data | Public repository for benchmarking and comparative analysis |
Directed Evolution Insights from Resistance Mechanisms
Molecular Mechanisms of Antibiotic Resistance
The evolutionary pathways to drug resistance in TB and K. pneumoniae co-infections follow distinct but complementary mechanisms. For M. tuberculosis, resistance is primarily chromosomal and arises through spontaneous mutations in drug targets, activator enzymes, or efflux pump regulators [65]. Key resistance mechanisms include:
- Target-based mutations: rpoB (rifampicin), inhA (isoniazid, ethionamide), gyrA/B (fluoroquinolones), atpE (bedaquiline) [65].
- Drug activator mutations: katG (isoniazid), pncA (pyrazinamide), fbiA/B/C, fgd1, ddn (delamanid/pretomanid) [65].
- Efflux pump regulation: Rv0678 (bedaquiline, clofazimine) [65].
For K. pneumoniae, resistance mechanisms are more diverse and often plasmid-mediated:
- Enzyme production: ESBLs (CTX-M, TEM, SHV), carbapenemases (KPC, NDM, VIM, OXA-48-like) [61].
- Membrane permeability: Porin mutations (ompK35, ompK36) combined with efflux pump overexpression [61].
- Target modification: Alterations in penicillin-binding proteins, DNA gyrase, and ribosomal targets [61].
Experimental Protocol for Directed Evolution Studies
Understanding resistance development requires experimental models of evolutionary pressure. The following protocol adapts directed evolution approaches for studying resistance emergence:
In Vitro Evolution of β-lactamase Under Antibiotic Selection
This protocol is modified from Feiler et al. (2013) who studied M. tuberculosis β-lactamase evolution [66]:
Library Construction:
- Amplify blaC gene (M. tuberculosis β-lactamase) or blaCTX-M (common in K. pneumoniae) with error-prone PCR conditions (0.1 mM MnCl₂, unbalanced dNTP ratios).
- Clone mutated genes into expression vector (pET28a) with antibiotic selection marker.
- Transform into suitable expression host (e.g., E. coli BL21 for initial screening).
Selection and Screening:
- Plate transformed libraries on LB agar containing gradient concentrations of target β-lactam (ampicillin, ceftriaxone, or meropenem).
- Incubate at 37°C for 16-24 hours and identify colonies growing at highest antibiotic concentrations.
- Isplicate resistant colonies for sequence analysis and resistance validation.
Characterization of Evolved Mutants:
- Purify mutant β-lactamases using affinity chromatography.
- Determine kinetic parameters (Km, kcat) against multiple β-lactam substrates.
- Assess thermal stability and minimum inhibitory concentrations (MICs).
- Perform structural modeling to understand mutation effects on active site architecture.
This approach identified gatekeeper residues like I105 in BlaC that when mutated (e.g., I105F) widened active site access by 3.6 Å and increased catalytic efficiency 3-fold, conferring 5-fold greater antibiotic resistance [66].
Integration of Genomic Data for Clinical Applications
Diagnostic Implementation Framework
The translation of genomic data into clinical practice requires standardized workflows and interpretation guidelines. The integration pathway for clinical decision support is visualized below:
Figure 2: Integration framework for genomic data in clinical decision support.
Case Study: Nanopore Sequencing in Clinical Co-infection Management
A recent study demonstrated the clinical utility of nanopore sequencing for managing complex co-infections [62]. Researchers applied metagenomic nanopore sequencing to respiratory samples from 23 patients with MTB and other pathogen co-infections. The methodology successfully identified MTB in 86.96% of cases, outperforming traditional culture (39.13%), AFB staining (27.27%), and Xpert MTB/RIF (53.84%) [62]. Notably, the approach detected co-infections with Candida albicans, K. pneumoniae, and Mycobacterium abscessus, enabling tailored therapeutic regimens.
In one case, a 21-year-old female with extensively drug-resistant tuberculosis (XDR-TB) showed recurrent symptoms during treatment [62]. Nanopore sequencing not only confirmed MTB with specific resistance mutations (rrs, rpoB, katG, gyrA, pncA, rpsL) but also guided successful regimen adjustment to bedaquiline, linezolid, cycloserine, protionamide, and ethambutol. This case highlights how comprehensive genomic profiling can direct personalized therapy in complex co-infections.
The integration of whole-genome sequencing and directed evolution principles provides a powerful framework for understanding and addressing the complex challenge of TB and K. pneumoniae co-infections. Clinical outcomes in these cases are significantly worsened by the convergence of resistance mechanisms and virulence factors, necessitating sophisticated diagnostic approaches that can detect complex resistance patterns and guide targeted therapeutic interventions.
Future directions in this field should focus on several key areas:
- Development of integrated databases that correlate genomic markers with clinical outcomes in co-infected patients
- Implementation of machine learning approaches to predict resistance evolution based on mutational patterns
- Expansion of rapid sequencing technologies in clinical settings to enable real-time treatment adjustment
- Exploration of evolutionary trade-offs between resistance and virulence that could inform novel therapeutic strategies
The protocols and case studies presented here provide a foundation for researchers and clinicians to implement genomic approaches in both investigative and clinical settings. As antimicrobial resistance continues to evolve, these methodologies will become increasingly essential for managing complex infectious disease scenarios and preserving the efficacy of existing antimicrobial agents.
Navigating the Challenges: Strategies for Optimizing Directed Evolution and WGS Workflows
In the field of directed evolution and resistance gene identification, the construction of mutant libraries serves as the foundational step for uncovering novel biological mechanisms and therapeutic targets. Library bias refers to the non-random distribution of mutations introduced by various mutagenesis techniques, which can significantly skew experimental outcomes and limit the diversity of identifiable resistance mechanisms. Different mutagenesis methods exhibit distinct preferences in the types and locations of mutations they generate, directly impacting the scope and reliability of your functional screens. For researchers using whole-genome sequencing to identify resistance genes, understanding and mitigating these biases is paramount to ensuring comprehensive coverage of potential mechanisms, including point mutations, insertions/deletions, and copy number variations that might otherwise be missed by biased approaches.
The strategic selection of mutagenesis methods enables researchers to either broadly explore the entire genomic landscape or deeply investigate specific functional regions. Chemical mutagenesis, for instance, excels at generating genome-wide point mutations with minimal sequence context bias, making it ideal for identifying novel resistance-conferring single nucleotide variants [67]. In contrast, modern oligonucleotide-based and CRISPR-Cas methods offer precise targeting but may introduce their own biases related to delivery efficiency and repair outcomes [68]. This Application Note provides a structured framework for selecting appropriate mutagenesis strategies to overcome library bias in resistance gene identification studies.
Comparative Analysis of Mutagenesis Methods
Quantitative Comparison of Mutagenesis Techniques
Table 1: Characteristics of Major Mutagenesis Methods for Resistance Gene Identification
| Method | Mutation Type | Coverage | Bias Profile | Best Applications in Resistance Research |
|---|---|---|---|---|
| Chemical Mutagenesis (ENU/EMS) | Primarily point mutations (96% base substitutions) [67] | Genome-wide saturation [67] | Minimal sequence context bias; under-represents C>G transversions (3% of substitutions) [67] | Identification of novel point mutation-mediated resistance mechanisms; unbiased forward genetic screens [67] |
| Error-Prone PCR | Point mutations (base substitutions) [69] | Single gene to pathways | Significant mutational preference; limited to amplified regions; inefficient for insertions/deletions [69] | Rapid diversification of specific genes or domains; when structural data is unavailable [69] |
| Oligonucleotide Pool Synthesis | Designed substitutions, insertions, deletions [69] | Precisely targeted sites | Synthesis errors; chimera formation during assembly [69] | Saturation mutagenesis of protein domains; deep mutational scanning [70] |
| CRISPR-Cas Systems | Indels via NHEJ; precise edits via HDR [71] | Targetable sites limited by PAM requirements | PAM restriction; efficiency varies by target sequence; delivery-dependent bias [71] | Functional validation of candidate resistance genes; pathway-focused screens [68] |
Bias Profiles and Artifact Mitigation
Each mutagenesis method introduces characteristic artifacts that researchers must account for in experimental design and data interpretation. In chemical mutagenesis screens, mathematical approaches like non-negative matrix factorization can extract mutational signatures specific to the mutagen (e.g., "Signature A" for ENU) from background processes, enabling more accurate identification of true resistance mutations [67]. For oligonucleotide-based methods, synthesis errors and chimeric sequence formation during PCR assembly represent major sources of bias that can be mitigated by using high-fidelity DNA polymerases like KAPA HiFi HotStart or Platinum SuperFi II [69].
In CRISPR-Cas systems, the requirement for specific PAM sequences adjacent to target sites fundamentally restricts mutagenesis coverage, while variations in sgRNA activity and cellular repair preferences can introduce additional biases [71]. Recent approaches combining multiple methods have shown promise in overcoming individual technique limitations—for example, using chemical mutagenesis for broad mutation generation followed by CRISPR-Cas validation to establish causal relationships [68].
Method Selection Framework
Decision Matrix for Mutagenesis Method Selection
Table 2: Method Selection Guide Based on Research Objectives
| Research Goal | Recommended Primary Method | Complementary Methods | Bias Mitigation Strategies |
|---|---|---|---|
| Unbiased discovery of novel resistance mechanisms | Chemical mutagenesis (ENU/EMS) [67] | Whole-genome sequencing; computational enrichment analysis [67] | Use mathematical extraction of mutagen-specific signatures; combine MSS and MSI cell models [67] |
| Comprehensive analysis of specific protein domains | Oligonucleotide pool synthesis with high-throughput assembly [70] | Cellular abundance assays (aPCA); protein language models [70] | Implement quality control via NGS; use high-fidelity polymerases to reduce chimeras [69] |
| Functional validation of candidate resistance pathways | CRISPR-Cas9 with homology-directed repair [71] | Allelic replacement; protein stability assays [72] | Utilize multiple sgRNAs per target; validate with orthogonal methods [68] |
| Rapid diversification without structural information | Error-prone PCR [69] | FACS screening; selection under drug pressure | Acknowledge limited mutation spectrum; use complementary methods for indels [69] |
Experimental Design Considerations
The scale of your resistance study should significantly influence method selection. For genome-wide screens, chemical mutagenesis provides exceptional coverage, with studies demonstrating successful identification of all known resistance mutations to therapeutics like Cetuximab while simultaneously uncovering novel clinically relevant mutations [67]. The high mutation density achievable with ENU (approximately 470 novel mutations per exome) enables detection of even rare resistance mechanisms [67].
For focused studies on specific gene families or protein domains, large-scale saturation mutagenesis offers unprecedented resolution. Recent work with 500 human protein domains demonstrated the feasibility of assaying over 500,000 missense variants in a single experimental framework, providing rich datasets for clinical variant interpretation [70]. In microbial systems, coupling chemical mutagenesis with drug selection successfully identified resistance mechanisms in parasites like Leishmania, highlighting the cross-species applicability of these approaches [72].
Detailed Protocols
Protocol 1: Genome-Wide Chemical Mutagenesis Screen for Drug Resistance
Principle: Chemical mutagens like N-ethyl-N-nitrosourea (ENU) efficiently generate random point mutations throughout the genome, enabling identification of resistance mutations without prior knowledge of potential mechanisms [67].
Reagents and Equipment:
- Cell line of interest (e.g., CCK-81 or NCI-H508 for colorectal cancer studies) [67]
- ENU (N-ethyl-N-nitrosourea) stock solution
- Target therapeutic agent (e.g., Cetuximab for EGFR inhibition) [67]
- Cell culture reagents and equipment
- Whole-exome sequencing platform
Procedure:
- ENU Dose Optimization:
- Expose cells to ENU concentration range (e.g., 0.01-1 mg/mL) for 24 hours
- Determine concentration that yields minimal viability impact while maximizing mutation diversity (typically 0.1 mg/mL for many cell lines) [67]
- Validate mutation spectrum meets expected distribution across all six base substitution types
Mutagenesis and Selection:
- Treat cells with optimized ENU concentration for 24 hours
- Allow recovery for 48-72 hours to fix mutations
- Apply therapeutic selection pressure (e.g., 10 µg/mL Cetuximab) for 8 consecutive weeks [67]
- Include non-mutagenized controls to establish baseline resistance frequency
Resistant Clone Isolation and Validation:
- Isolate and expand individual resistant colonies
- Confirm stable resistance phenotype through clonogenic survival assays [67]
- Prepare 72+ clones for whole-exome sequencing to ensure statistical power
Sequencing and Analysis:
- Perform whole-exome sequencing on resistant clones and parental line
- Detect novel mutations and estimate ENU-associated mutations per Mb
- Use computational approaches to identify mutations enriched in resistant populations
- Apply mutational signature analysis to distinguish ENU-induced mutations from background
Troubleshooting:
- If insufficient resistant colonies form, optimize ENU concentration and increase selection stringency gradually
- If mutation burden is too high, reduce ENU concentration or exposure time
- Validate candidate mutations through orthogonal methods like CRISPR-Cas9 editing
Protocol 2: High-Throughput Oligonucleotide-Based Saturation Mutagenesis
Principle: Array-synthesized oligonucleotide pools enable systematic mutagenesis of every position in a target gene to all possible amino acid substitutions, providing comprehensive coverage of mutational space [70].
Reagents and Equipment:
- Designed oligonucleotide pool (e.g., GenTitan Oligo Pool)
- High-fidelity DNA polymerase (KAPA HiFi HotStart, Platinum SuperFi II, or Hot-Start Pfu) [69]
- Gibson assembly reagents
- Selection system (e.g., abundance protein fragment complementation assay for stability measurements) [70]
- High-throughput sequencing platform
Procedure:
- Library Design:
- Divide target gene into sub-libraries covering 24 amino acids (72 bp) each [69]
- Design oligonucleotides with 16-19 bp homologous arms for recombination
- Include all 19 possible amino acid substitutions at each position
- Order pooled oligonucleotides via commercial synthesis service
Library Construction:
- Amplify variant oligonucleotides using high-fidelity polymerase to minimize chimeras
- Assemble full-length genes via Gibson assembly using homologous recombination
- Clone into appropriate expression vector
- Transform into host cells at high efficiency to maintain library diversity
Functional Selection:
- Apply relevant selection pressure (e.g., drug resistance, protein stability)
- Use abundance protein fragment complementation assay (aPCA) for quantitative stability measurements [70]
- Collect input and output populations for sequencing
- Perform 3+ biological replicates to ensure reproducibility
Sequencing and Data Analysis:
- Sequence pre- and post-selection populations with deep coverage
- Calculate enrichment scores for each variant based on frequency changes
- Correlate abundance measurements with independent stability data
- Identify functional sites by comparing stability effects with evolutionary fitness
Troubleshooting:
- If library coverage is incomplete, optimize assembly conditions and increase transformation scale
- If chimeric sequences are prevalent, use different high-fidelity polymerase or adjust PCR conditions
- If selection dynamic range is limited, adjust stringency or use alternative selection system
Research Reagent Solutions
Table 3: Essential Reagents for Mutagenesis Studies
| Reagent/Category | Specific Examples | Function and Application |
|---|---|---|
| Chemical Mutagens | N-Ethyl-N-nitrosourea (ENU), Ethyl methanesulfonate (EMS) [67] [72] | Induce random point mutations throughout genome; ideal for unbiased resistance screens [67] |
| High-Fidelity DNA Polymerases | KAPA HiFi HotStart, Platinum SuperFi II, Hot-Start Pfu DNA Polymerase [69] | Amplify oligonucleotide pools with minimal errors and reduced chimeras during library construction [69] |
| CRISPR-Cas Systems | Cas9 nuclease, sgRNA libraries [71] | Targeted gene disruption via NHEJ (indels) or precise editing via HDR; functional validation [68] |
| Selection Assays | Abundance protein fragment complementation assay (aPCA) [70] | Quantifies effects of variants on protein abundance in cells; connects stability to resistance [70] |
| Whole-Genome Sequencing Platforms | Illumina NovaSeq, MiSeq [44] | Identify mutations in resistant clones; monitor evolution of resistance in real-time [44] |
Workflow Visualization
Method Selection Decision Pathway
Chemical Mutagenesis Experimental Workflow
The strategic selection of mutagenesis methods based on their characteristic biases is fundamental to successful resistance gene identification in directed evolution studies. Chemical mutagenesis approaches provide exceptional breadth for discovering novel point mutation-mediated resistance, while oligonucleotide-based methods offer unparalleled depth for investigating specific protein domains. CRISPR-Cas systems enable precise functional validation, and emerging machine learning approaches continue to enhance our ability to predict and interpret mutational effects. By understanding and leveraging the complementary strengths of these methods while implementing appropriate bias mitigation strategies, researchers can construct more comprehensive mutant libraries and accelerate the identification of clinically relevant resistance mechanisms. The protocols and frameworks presented here provide a practical foundation for designing mutagenesis screens that maximize coverage while minimizing blind spots in resistance gene discovery.
In directed evolution, a local fitness optimum represents a state where a biological system (e.g., an enzyme, microbial strain, or phage) achieves a peak performance level in its immediate genetic neighborhood. While this state represents an improvement, it is suboptimal globally and can trap evolutionary processes, halting progress toward the true fitness maximum. Such scenarios are evolutionary dead ends, where incremental, stochastic mutagenesis and selection can no longer drive improvement. The problem is particularly acute in applied research, such as developing therapeutic biocatalysts or overcoming antimicrobial resistance (AMR), where maximal performance is critical. This Application Note details practical strategies and protocols to identify and escape these local optima, contextualized within resistance gene identification and manipulation research. The concepts of evolutionary traps also apply at a planetary scale, where societal innovations can lead humanity into global sustainability dead ends, underscoring the universality of the challenge [73] [74].
Key Concepts and Definitions
- Local Fitness Optimum: A genotype from which any small mutational step leads to a decrease in fitness, despite more beneficial genotypes existing elsewhere in the fitness landscape. It represents a "peak" in the immediate vicinity but not the highest peak in the landscape.
- Evolutionary Dead End: A trajectory in phenotypic or genotypic space that leads to a state from which escape via gradual, cumulative mutations is highly improbable, effectively terminating adaptive progress.
- Fitness Landscape: A conceptual representation of the relationship between genotypes (or phenotypes) and reproductive success (fitness). The landscape features peaks (high fitness), valleys (low fitness), and ridges (neutral paths).
- Directed Evolution: A biomimetic laboratory method that applies selective pressure to a library of gene variants to evolve proteins or RNAs with desired properties. It faces the inherent risk of stalling at local optima.
- Antibiotic Resistance Gene (ARG): A gene that enables a bacterium to survive exposure to an antibiotic. The evolution and spread of ARGs are a major global health threat, and their identification is crucial for surveillance and developing countermeasures [6] [75].
Table 1: Common Evolutionary Dead Ends and Their Prevalence in Key Research Areas
| Research Area | Type of Local Optimum | Key Challenge | Quantitative Impact/Prevalence |
|---|---|---|---|
| Antimicrobial Resistance (AMR) | Multi-drug resistant (MDR) pathogens [29] | Limited treatment options lead to ~1.27 million annual deaths directly attributable to AMR [6]. | |
| Wastewater Treatment Plants (WWTPs) | ARGs in activated sludge [76] | WWTPs are hotspots for ARG dissemination; a core set of 20 ARGs was found in 100% of 142 global WWTPs, accounting for 83.8% of total ARG abundance [76]. | |
| Phage Therapy | Narrow host range of therapeutic phages [29] | Phages evolved to overcome resistance in Klebsiella pneumoniae sometimes lost activity against originally susceptible strains, a trade-off indicative of a local optimum [29]. | |
| Protein Engineering | Specialized enzyme with high activity for a specific substrate but inability to catalyze related reactions. | Stalled optimization campaigns despite large mutant library screens, requiring radical sequence re-design. |
Research Reagent Solutions
Table 2: Essential Research Reagents and Resources for Overcoming Evolutionary Dead Ends
| Reagent/Resource | Function/Description | Application Example |
|---|---|---|
| Bridge Recombinase System [28] | A novel genome editing system combining a recombinase protein with a bridge RNA (bRNA) for precise, cut-free insertion of large DNA fragments. | Targeted gene replacement therapies (e.g., for Alpha-1 Antitrypsin Deficiency) to avoid the dead ends of double-strand break repair [28]. |
| Protein Language Models (ProtBert-BFD, ESM-1b) [77] | Deep learning models that convert protein sequences into numerical embeddings, capturing structural and functional information for predicting new protein functions. | Identifying novel or divergent Antibiotic Resistance Genes (ARGs) beyond the limits of homology-based searches [77]. |
| Phage-Assisted Continuous Evolution (PACE) [28] | A continuous evolution system that links the desired activity of a protein or RNA to the life cycle of a bacteriophage, enabling rapid exploration of sequence space. | Evolving bridge recombinases with enhanced activity and specificity; expanding phage host range [28] [29]. |
| Comprehensive Antibiotic Resistance Database (CARD) [6] | A manually curated resource containing information on ARGs, their mechanisms, and associated metadata, based on the Antibiotic Resistance Ontology (ARO). | Reference database for identifying and annotating resistance genes from genomic and metagenomic data [6]. |
| Deep Mutational Learning (DML) [28] | A method that uses machine learning on mutational library data to map fitness landscapes and identify optimal evolutionary paths. | Predicting beneficial combinations of mutations in bridge recombinases to escape local optima [28]. |
| E.coli Orthogonal Replicon (EcORep) [28] | A synthetic, high-mutation-rate DNA replicon system in E. coli for continuous in vivo mutagenesis and enrichment of improved variants. | Continuous directed evolution of enzymes within a bacterial host [28]. |
Core Experimental Protocols
Protocol 1: Phage Host Range Expansion Using Directed Evolution (Appelmans Protocol)
Application Note: This protocol is designed to escape the local optimum of a narrow host range in therapeutic phages, a major limitation in phage therapy [29].
Materials:
- Bacterial Strains: A panel of 11 target strains, including a permissive host and clinically isolated, phage-resistant variants of Klebsiella pneumoniae.
- Parental Phages: A cocktail of five myophages (e.g., genus Jiaodavirus) with complementary initial host ranges.
- Growth Media: Standard liquid and agar media suitable for the host bacteria.
- Buffers: SM Buffer or similar for phage storage and dilution.
Procedure:
- Preparation: Mix the five parental phages to create an initial evolutionary cocktail.
- Training Passage: a. Infect a fresh, high-density culture of the first target bacterial strain (a resistant clinical isolate) with the phage cocktail at a high multiplicity of infection (MOI). b. Allow co-incubation for a predetermined period (e.g., 6-18 hours) to permit lytic infection and phage replication. c. Centrifuge the culture and filter the supernatant through a 0.22 µm filter to obtain a lysate containing phage progeny.
- Iterative Evolution: a. Use the filtered lysate from the previous step to infect the next target bacterial strain in the panel. b. Repeat the passage cycle through the entire panel of 11 bacterial strains. This constitutes one full "training" round. c. Perform multiple (e.g., 10-20) rounds of training to impose strong selective pressure for host range expansion.
- Plaque Assay and Isolation: a. After the final round, plaque-purify individual phage variants on the original permissive host and on initially resistant target strains. b. Isolate phage clones that form clear plaques on previously resistant hosts.
- Characterization: a. Screen isolated variants against a large diversity panel (e.g., 100 strains) to assess changes in host range. b. Sequence the genomes of evolved phages and align to parental sequences to identify mutations (e.g., in tail fiber genes) responsible for altered tropism.
Troubleshooting:
- No Phage Recovery: If a phage population goes extinct during passage on a highly resistant strain, return to an earlier lysate and passage through a less restrictive intermediate strain.
- Loss of Original Activity: Some variants will trade original host range for new one. Maintain a diverse population and screen multiple clones.
Protocol 2: Predicting ARGs with Protein Language Models to Overcome Database Limits
Application Note: This protocol uses deep learning to escape the local optimum of homology-based ARG detection, which fails to identify novel or highly divergent resistance genes [77].
Materials:
- Hardware: Computer with a high-performance GPU (e.g., NVIDIA Tesla V100, A100) for model training and inference.
- Software: Python environment with PyTorch/TensorFlow, HuggingFace
transformerslibrary, and custom scripts. - Data: Dataset of protein sequences labeled as ARGs or non-ARGs (e.g., from DeepARG, CARD).
Procedure:
- Feature Extraction: a. Input protein sequences (as amino acid strings) into two pre-trained protein language models: ProtBert-BFD and ESM-1b. b. For each sequence, ProtBert-BFD will output a 30,720-dimensional feature vector, and ESM-1b will output a 1,310,720-dimensional vector [77]. c. Save these embeddings as the numerical representation of each protein.
- Data Augmentation: a. To handle imbalanced data (rare ARG classes), use a cross-referencing method. b. For a protein from a rare class, use Principal Component Analysis (PCA) to reduce the high-dimensional ESM-1b embedding to 32 dimensions. c. Concatenate these features with the ProtBert-BFD features to create a novel, augmented data sample for the underrepresented class [77].
- Model Training: a. Build a classification model using a Long Short-Term Memory (LSTM) network, optionally with a Multi-Head (MH) attention mechanism. b. Train separate LSTM models on the feature datasets from ProtBert-BFD and ESM-1b. c. The model learns to classify the vector representations into one of several ARG classes (e.g., 16 groups) or as non-ARG.
- Prediction and Integration: a. For a new, uncharacterized protein sequence, process it through steps 1a-b to get its feature vectors. b. Run the vectors through the two trained LSTM models to get two independent predictions. c. Integrate the results via an ensemble method (e.g., selecting the class with the maximum combined probability) to produce the final ARG prediction [77].
Troubleshooting:
- Low Prediction Accuracy: Ensure the training dataset is representative and the data augmentation step is correctly implemented for imbalanced classes.
- High Computational Load: Use feature dimensionality reduction (like PCA) before training the LSTM if resources are limited.
Workflow Visualization
Integrated Strategy to Escape Evolutionary Dead Ends
Experimental Workflow for Phage Host Range Expansion
Computational Workflow for Novel ARG Discovery
In the context of directed evolution and whole-genome sequencing for resistance gene identification, the accuracy of bioinformatics analysis is fundamentally constrained by the completeness of reference databases and the precision of annotation tools. Antimicrobial resistance (AMR) research exemplifies this challenge, where inconsistent annotations across tools and databases directly impact the reliability of predictive models and the discovery of novel resistance mechanisms [57]. Current databases exhibit significant variations in gene content and curation rules, while annotation tools differ in supported inputs, search algorithms, and output formats, leading to substantial inconsistencies in analysis results [57]. This application note details standardized protocols and analytical frameworks designed to quantify and address these bioinformatics limitations, enabling more accurate identification of antimicrobial resistance genes (ARGs) and directing evolutionary research toward areas where knowledge gaps are most pronounced.
Quantitative Assessment of Annotation Tools and Databases
Performance Comparison of AMR Annotation Tools
A comparative assessment of eight commonly used annotation tools applied to Klebsiella pneumoniae genomes reveals critical differences in their operational characteristics and output [57]. These tools were evaluated based on their database dependencies, analysis capabilities, and specific strengths or limitations relevant to resistance gene identification.
Table 1: Comparative Analysis of AMR Annotation Tools
| Tool Name | Primary Database | Analysis Approach | Key Capabilities | Notable Limitations |
|---|---|---|---|---|
| Kleborate | Species-specific | K. pneumoniae-focused | Catalogues variation in K. pneumoniae; virulence gene hits can be excluded | Limited to specific bacterial species [57] |
| AMRFinderPlus | NCBI Reference Gene Catalog | Comprehensive AMR detection | Detects presence of AMR genes and point mutations; wide coverage [57] | Requires careful parameterization [57] |
| ResFinder | ResFinder | Gene-to-antibiotic/class relationships | Annotates samples against default database settings [57] | May not cover all resistance mechanisms [57] |
| DeepARG | DeepARG | Confidence-based prediction | Includes variants predicted to impact phenotype with high confidence [57] | May include less validated predictions [57] |
| RGI | CARD | Protein homolog/variant models | Leverages CARD's comprehensive ontology; precise resistance mechanism annotation [78] | Specificity can be lower, requiring filtering of results [78] |
| Abricate | CARD (default) | Rapid screening | Quick analysis of assembled genomes | Cannot detect point mutations; covers only a subset of AMRFinderPlus content [57] |
| SraX | CARD | Custom implementation | Alternative approach to CARD database utilization | Performance characteristics less documented [57] |
| StarAMR | ResFinder | Integrated analysis | Works with ResFinder database for consolidated reporting | Dependent on ResFinder's update cycle [57] |
"Minimal Model" Approach for Identifying Knowledge Gaps
The "minimal model" concept provides a methodological framework for identifying antibiotics where known resistance mechanisms inadequately explain observed phenotypic resistance [57]. This approach utilizes only known resistance determinants from curated databases to build parsimonious machine learning models that predict binary resistance phenotypes.
Protocol: Implementing Minimal Models for Gap Analysis
Data Collection and Curation: Obtain whole-genome sequences and corresponding antibiotic susceptibility testing data for target pathogens. For K. pneumoniae, the Bacterial and Viral Bioinformatics Resource Centre (BV-BRC) provides quality-controlled assemblies with phenotypic data for numerous antibiotics [57].
Genome Annotation: Annotate all samples using multiple annotation tools (Table 1) to generate comprehensive feature sets of known AMR determinants. Format positive identifications as binary presence/absence matrices (Xₚ×ₙ ∈ {0,1}), where p represents samples and n represents unique AMR features [57].
Feature Subset Selection: Create minimal gene subsets for each antibiotic using stringent database ontologies (e.g., CARD) that document gene-to-antibiotic and mutation-to-antibiotic relationships with experimental evidence [57].
Model Training and Validation: Implement machine learning algorithms (e.g., logistic regression with Elastic Net regularization or XGBoost) using minimal feature subsets. Employ standard train-test splits (70-30%) with cross-validation to assess prediction accuracy [57].
Performance Gap Analysis: Identify antibiotics where minimal models show significantly suboptimal performance (e.g., low accuracy, precision, or recall), indicating substantial knowledge gaps in known resistance mechanisms [57].
Standardized Bioinformatics Practices for Clinical-Grade Analysis
Consensus Recommendations for Clinical Bioinformatics
The Nordic Alliance for Clinical Genomics (NACG) has established consensus recommendations to ensure accuracy, reproducibility, and comparability in clinical bioinformatics operations [79]. These standards are particularly relevant for directed evolution studies requiring clinical validation.
Table 2: Essential Standards for Clinical Bioinformatics Pipelines
| Category | Recommendation | Implementation Example |
|---|---|---|
| Reference Standards | Adopt hg38 genome build as primary reference [79] | Use hg38 for all human genome alignments in WGS analysis |
| Variant Analysis | Implement multiple tools for structural variant (SV) calling [79] | Combine Manta, Delly, and LUMPY for comprehensive SV detection |
| Quality Control | Filter variants using tool-specific matched in-house datasets [79] | Maintain site-specific background variant databases for common artifacts |
| Computational Environment | Utilize reliable air-gapped clinical-grade HPC and IT systems [79] | Deploy ISO 15189-compliant computing infrastructure |
| Data Integrity | Verify data integrity using file hashing (e.g., MD5, SHA1) [79] | Implement checksum verification at all data transfer points |
| Reproducibility | Encapsulate software in containers or Conda environments [79] | Use Docker or Singularity containers for all analytical components |
| Sample Identity | Verify sample identity via inference of identifying traits and relatedness checks [79] | Implement genetic fingerprinting with sex and ancestry markers |
Integrated Workflow for Simultaneous Pathogen and AMR Detection
The CZ ID AMR module represents an integrated approach for concurrent detection of microbes and antimicrobial resistance genes from both metagenomic next-generation sequencing (mNGS) and single-isolate whole-genome sequencing (WGS) data [78].
Protocol: Integrated Pathogen and Resistome Profiling
Sample Processing and Host Depletion: Accept raw FASTQ files from Illumina platforms (up to 75 million single-end or 150 million paired-end reads per sample). Remove low-quality and low-complexity reads using fastp, followed by host read depletion with Bowtie2 and HISAT2 alignments against reference genomes [78].
Data Normalization: Filter duplicate reads using CZID-dedup, then subsample to 1 million single-end or 2 million paired-end reads to limit computational resources for downstream alignment. For targeted mNGS protocols, duplicate reads are added back prior to further processing to maintain sensitivity for low-abundance AMR genes [78].
Parallel AMR Detection:
- Contig Approach: Assemble quality-filtered reads into contigs using SPAdes, then analyze contigs with Resistance Gene Identifier (RGI) software using "rgi main -a BLAST" command for AMR gene detection based on sequence similarity and mutation mapping [78].
- Read Approach: Directly analyze quality-filtered reads with RGI using "rgi bwt -a kma" command for read mapping by KMA to Comprehensive Antibiotic Resistance Database (CARD) reference sequences [78].
Pathogen-of-Origin Prediction: Submit contigs or reads containing AMR genes to RGI with "rgi kmer_query" command to predict pathogen origin using k-mers uniquely associated with AMR alleles of specific pathogens or plasmids [78].
Result Interpretation: Filter AMR hits using metrics such as gene coverage, percent identity, and depth of coverage to improve specificity. The platform provides an interactive table sorted by Gene, Gene Family, Drug Class, Mechanism, and detection model [78].
Integrated Pathogen & AMR Detection Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools
| Item | Function/Application | Implementation Notes |
|---|---|---|
| CARD Database | Comprehensive AMR gene reference | Provides antibiotic resistance ontology; links genes to mechanisms and drug classes [78] |
| Resistance Gene Identifier (RGI) | AMR detection from sequences | Works with CARD; detects genes and specific mutations; enables pathogen-of-origin prediction [78] |
| AMRFinderPlus | Bacterial AMR gene detection | NCBI tool; detects presence of AMR genes and point mutations; wide coverage [57] |
| Kleborate | Species-specific annotation | Specialized for K. pneumoniae; catalogues resistance and virulence variation [57] |
| Evo Genomic Language Model | AI-generated functional sequences | Enables semantic design of novel genes; uses genomic context for function-guided generation [80] |
| CZ ID AMR Module | Cloud-based AMR analysis | Open-access platform integrating pathogen detection and AMR profiling from mNGS/WGS data [78] |
| Directed Evolution Systems | Enzyme engineering | EcORep and PACE systems enable continuous evolution of proteins like bridge recombinases [28] |
| Bridge Recombinases | Precise gene replacement | RNA-guided enzymes for inserting large DNA fragments without double-strand breaks [28] |
| CRISPR-Directed Evolution | Targeted mutagenesis | Combines CRISPR precision with directed evolution for complex gene evolution [81] |
Advanced Methodologies for Addressing Database Limitations
Incorporating Mobility Potential into AMR Risk Assessment
Current AMR risk assessment frameworks frequently overestimate epidemiological risk by assuming worst-case historical genetic contexts without considering the actual mobility potential of resistance genes in environmental samples [30]. Integrating mobility information provides more accurate risk prioritization.
Protocol: Assessing ARG Mobility Potential
Sample Collection and Metagenomic Sequencing: Collect environmental or clinical samples and perform metagenomic sequencing using both short-read (Illumina) and long-read (Oxford Nanopore, PacBio) technologies to enhance assembly quality and mobile genetic element (MGE) reconstruction [30].
Contig-Based Analysis: Reconstruct metagenome-assembled genomes (MAGs) and identify associations between ARGs and MGEs (plasmids, integrons, transposons) through contig co-localization analysis [30] [82].
MGE Detection and Typing: Implement specialized tools for plasmid prediction (PlasmidFinder, mlplasmids), integron detection (IntegronFinder), and phage identification (Phaster, VirSorter) to characterize the mobility context of identified ARGs [82].
Horizontal Gene Transfer Potential Assessment: Quantify ARG mobility risk using frameworks that consider:
- Circulation: Is the ARG shared between different One Health settings with increased abundances due to human activities? [30]
- Mobility: Has the ARG been identified on MGEs that increase transfer likelihood to pathogens? [30]
- Pathogenicity: Has the ARG been found in human or animal pathogens? [30]
- Clinical Relevance: Has the ARG been linked to worsened treatment outcomes? [30]
Quantitative Microbial Risk Assessment (QMRA) Integration: Incorporate mobility data into QMRA frameworks that include hazard identification, exposure assessment, dose-response analysis, and risk characterization to quantify health risks more accurately [30].
Semantic Design for Accessing Novel Functional Sequences
Generative genomic models like Evo can design novel functional sequences beyond natural evolutionary landscapes, addressing database gaps through AI-generated content [80]. The "semantic design" approach leverages the genomic context of known functions to generate novel sequences with related activities.
Protocol: Semantic Design of Novel Genes
Prompt Engineering: Curate genomic sequence prompts based on functional context, including:
- Known gene sequences (e.g., toxin genes) and their reverse complements
- Upstream or downstream genomic contexts of functional loci
- Operonic structures with functionally related genes [80]
Sequence Generation: Use Evo 1.5 model (131K context length) to generate novel sequences conditioned on the curated prompts, leveraging the model's understanding of prokaryotic genomic semantics [80].
In Silico Filtering: Apply computational filters to select promising generated sequences based on:
- Predicted protein-protein interactions for multi-component systems
- Sequence novelty requirements (e.g., <70% identity to known proteins)
- Structural feasibility and conservation of functional domains [80]
Experimental Validation: Test generated sequences using appropriate functional assays:
- Growth inhibition assays for toxin-antitoxin systems
- Phage inhibition assays for anti-CRISPR proteins
- Antibiotic susceptibility testing for novel resistance genes [80]
Semantic Design Workflow for Novel Genes
The protocols and analytical frameworks presented herein provide a systematic approach for identifying, quantifying, and addressing critical gaps in bioinformatics databases and annotation tools. By implementing the minimal model approach, researchers can prioritize directed evolution efforts toward antibiotics and resistance mechanisms where knowledge is most limited. Standardized clinical bioinformatics practices ensure reproducibility, while integrated pathogen-AMR detection workflows enable comprehensive resistome profiling. Finally, emerging methodologies incorporating mobility potential and semantic design offer promising avenues for advancing beyond current database limitations, ultimately enhancing the accuracy of resistance gene identification in directed evolution and whole-genome sequencing research.
The Role of AI and Machine Learning in Predictive Modeling and Variant Calling
The convergence of artificial intelligence (AI) with genomics is revolutionizing our capacity to decipher the genetic underpinnings of antimicrobial resistance (AMR). Within directed evolution studies and whole-genome sequencing (WGS) projects aimed at identifying resistance genes, AI-driven tools are dramatically accelerating the pace of discovery. These technologies are moving beyond traditional statistical methods, offering superior accuracy in pinpointing genetic variants and predicting resistance phenotypes from sequence data [83] [84]. The application of AI in this domain is not merely an incremental improvement but a paradigm shift, enabling researchers to process vast genomic datasets with a speed and precision previously unattainable [85]. This document provides detailed application notes and protocols for leveraging AI in predictive modeling and variant calling, specifically framed within resistance gene identification research.
AI in Predictive Modeling for Antimicrobial Resistance
Predictive modeling using AI integrates diverse data types to forecast AMR, a critical capability for public health. In 2019, AMR was associated with an estimated 4.95 million deaths globally, a figure projected to rise to 10 million annually by 2050 if left unchecked [84]. AI models are uniquely suited to combat this crisis by learning complex patterns from large-scale genomic and clinical datasets.
Key AI Methodologies and Applications
Clinical Diagnostics and Sepsis Prediction: AI models significantly improve the speed and accuracy of diagnosing bacterial infections. For sepsis, a life-threatening condition where each hour of delay in antibiotic treatment increases mortality risk by 9%, AI tools like COMPOSER (COnformal Multidimensional Prediction Of SEpsis Risk) have been developed. COMPOSER uses a deep learning architecture that achieves AUROC scores of 0.953 in intensive care units and 0.945 in emergency departments. Its implementation in the UC San Diego Hospital System led to a 17% relative decrease in in-hospital mortality [84]. Another model, which employs a Bidirectional Long Short-Term Memory (BiLSTM) network on data from ~180,000 patient records, achieved an AUC of 0.94 for sepsis risk prediction [84].
Antibiotic Discovery: AI is accelerating the discovery of new antibacterial agents to combat resistant bacteria. Machine learning (ML) and deep learning (DL) models can screen vast chemical libraries to identify novel compounds. Methods include:
- Support Vector Machines (SVM) and Random Forests (RF): Used to classify molecules based on biological activity or predict their activity quantitatively [86].
- Deep Neural Networks (DNNs) and Graph Neural Networks (GNNs): These process molecular structures as graphs, where atoms are nodes and chemical bonds are edges, to predict molecular properties and interactions effectively [86].
- Generative Models: Variational Autoencoders (VAEs) can generate novel molecular structures with desired antibacterial properties by exploring a learned chemical space [86].
AI for Antibiotic Resistance Gene (ARG) Identification
The identification of ARGs from whole genome and metagenome sequencing datasets relies on specialized bioinformatics tools and databases. AI-enhanced tools are particularly adept at detecting novel or low-abundance ARGs that might be missed by traditional homology-based methods [6].
Table 1: Key Databases for Antibiotic Resistance Gene Identification
| Database Name | Type | Primary Focus | Strengths | Weaknesses/Limitations |
|---|---|---|---|---|
| CARD [6] | Manually Curated | Comprehensive AMR data (genes, mutations, mechanisms) | Rigorous curation via Antibiotic Resistance Ontology (ARO); includes RGI analysis tool | Relies on published validation; manual curation can delay updates |
| ResFinder/PointFinder [6] | Manually Curated | Acquired ARGs (ResFinder) & chromosomal point mutations (PointFinder) | Integrated K-mer-based alignment for rapid analysis from raw reads; phenotype prediction | Limited to predefined targets and specific bacterial species for mutations |
| DeepARG [6] | AI-Based | ARG prediction from sequence data | Detects novel/low-abundance ARGs using machine learning models | Performance depends on training data; may have higher false positives for distant homologs |
Table 2: Select Computational Tools for ARG Identification
| Tool Name | Underlying Algorithm | Input Data | Key Features | Suitability |
|---|---|---|---|---|
| AMRFinderPlus [6] | BLAST-based homology search | Assembled genomes/contigs | Identifies acquired genes, point mutations, and variant sequences | Routine surveillance of known resistance determinants |
| DeepARG [6] | Deep Learning (DL) | Raw reads or assembled contigs | Predicts novel ARGs; models optimized for metagenomic data | Exploratory studies, environments with unknown resistomes |
| HMD-ARG [6] | Machine Learning (ML) | Metagenomic data | Designed to identify complex or low-abundance ARGs in diverse samples | Detection of emerging resistance threats in complex microbiomes |
AI-Driven Variant Calling for Resistance Mutation Detection
Variant calling—the process of identifying single nucleotide polymorphisms (SNPs), insertions/deletions (InDels), and structural variants from sequencing data—is a foundational step in genomics. AI-based callers have surpassed traditional statistical methods by using deep learning models to reduce false positives and navigate complex genomic regions [83].
State-of-the-Art AI-Based Variant Callers
- DeepVariant: Developed by Google Health, this open-source tool uses a deep convolutional neural network (CNN) that analyzes sequencing data converted into pileup image tensors. It supports both short-read (Illumina) and long-read (PacBio HiFi, Oxford Nanopore) technologies. A key strength is its ability to automatically produce filtered variants, eliminating the need for separate refinement steps. It has demonstrated high accuracy in large-scale studies like the UK Biobank WES consortium but can be computationally intensive [83] [87].
- DeepTrio: An extension of DeepVariant, also from Google Health, DeepTrio is specialized for analyzing family trios (child and parents). Its CNN leverages familial context to improve variant detection accuracy, especially for de novo mutations and in challenging genomic regions, outperforming methods like GATK and Strelka [83].
- Clair/Clair3: These DL-based callers build upon their predecessor, Clairvoyante, using CNNs for variant detection from both short and long-read data. Clair3 is noted for its high speed and performance, particularly at lower sequencing coverages which are traditionally prone to errors [83].
- DNAscope: Developed by Sentieon, DNAscope combines the mechanics of GATK’s HaplotypeCaller with a machine learning-based genotyping model. It is optimized for computational speed and efficiency, achieving high accuracy for SNPs and small InDels without requiring manual filtering thresholds or GPU acceleration [83].
Performance and Application in Hybrid Sequencing
Emerging approaches leverage the complementary strengths of different sequencing technologies. A 2025 study highlighted that a hybrid DeepVariant model, which jointly processes Illumina short-read and Nanopore long-read data, can match or surpass the germline variant detection accuracy of single-technology methods. This "shallow hybrid" strategy can reduce overall sequencing costs while improving detection, a significant advantage for large-scale clinical screening of resistance variants [87].
Table 3: Comparison of AI-Based Variant Calling Tools
| Variant Caller | Core Technology | Supported Reads | Key Strengths | Key Limitations |
|---|---|---|---|---|
| DeepVariant [83] [87] | Deep CNN (Images) | Short (Illumina), Long (PacBio, ONT) | High accuracy; automatic filtering; supports hybrid data | High computational cost |
| DeepTrio [83] | Deep CNN (Trio) | Short, Long | Superior accuracy for trios; better in complex regions | Requires trio data; computationally intensive |
| Clair3 [83] | Deep CNN | Short, Long | Fast runtime; high accuracy at low coverage | - |
| DNAscope [83] | Machine Learning | Short, Long (PacHiFi, ONT) | High speed & efficiency; reduced memory overhead | ML-based, not a deep learning architecture |
Integrated Experimental Protocols
The following protocols outline a cohesive workflow for identifying resistance genes and mutations using WGS and AI-driven analysis, directly applicable to directed evolution experiments.
Protocol 1: Whole-Genome Sequencing and Analysis of Mycobacterium tuberculosis for Resistance and Transmission
This protocol is adapted from a 2025 study characterizing the molecular epidemiology of M. tuberculosis (MTB) in a low-incidence setting [88].
1. Sample Collection and DNA Extraction
- Sample Collection: Collect sputum samples from patients and culture on Lowenstein-Jensen (L-J) medium.
- DNA Extraction: Extract genomic DNA from MTB colonies using a commercial kit (e.g., Mag-MK Bacterial Genomic DNA Extraction Kit). Quantify DNA concentration using a fluorometer (e.g., Qubit 2.0).
2. Library Preparation and Whole-Genome Sequencing
- Library Prep: Construct 150 bp paired-end libraries from the extracted genomic DNA.
- Sequencing: Sequence the libraries on an Illumina NovaSeq 6000 platform, targeting a minimum depth of 200x coverage.
3. Bioinformatic Processing and Quality Control
- Read Classification: Use Kraken v1.1.1 to ensure >90% of reads map to the MTB complex.
- Quality Control & Trimming: Assess FASTQ quality with fastp v0.23, trimming low-quality regions to ensure an average read quality ≥ Q20.
- Alignment: Map filtered reads to the MTB reference genome H37Rv using BWA-MEM. Perform base recalibration and realignment with GATK [88] [6].
4. Variant Calling and Resistance Profiling
- Variant Calling: Call SNPs using SAMtools/BCFtools, applying a frequency threshold of ≥90% and a minimum of five supporting reads [88].
- Lineage & Resistance Assignment: Use TB-Profiler to determine MTB lineage and identify mutations associated with resistance to anti-tuberculosis drugs (e.g., isoniazid, rifampin) [88].
5. Phylogenetic and Cluster Analysis
- Phylogenetic Tree Construction: Extract high-quality, concatenated SNPs, excluding PE/PPE genes and drug resistance loci. Build a maximum-likelihood phylogenetic tree using IQ-Tree v2.2.2, rooted with an outgroup (e.g., Mycobacterium canettii).
- Transmission Clustering: Calculate pairwise SNP distances between all isolates. Define transmission clusters as groups of isolates with ≤12 SNP differences, indicating recent transmission [88].
Protocol 2: AI-Driven Variant Calling for Detecting Resistance Mutations
This protocol details the use of a state-of-the-art AI variant caller, such as DeepVariant, for highly accurate detection of SNPs and InDels.
1. Input Data Preparation
- Input: A sorted BAM file from Protocol 1 (Step 3) and the corresponding reference genome (FASTA format).
- Note: DeepVariant can be run on data from a single technology (Illumina or Nanopore) or on hybrid data combining both [87].
2. Running DeepVariant
- Model Selection: Choose the appropriate pre-trained DeepVariant model that matches your sequencing technology (e.g., "WGS" for Illumina whole-genome, "PACBIO" for PacBio data, "HYBRIDPACBIOILLUMINA" for combined data).
- Execution: Run DeepVariant using the following core command structure. The tool is compatible with both CPU and GPU, though GPU acceleration is recommended for speed.
- Output: DeepVariant produces a VCF file containing the called variants. A key feature is that these calls are already filtered, so no additional hard filtering is required [83].
3. Validation and Comparison (Optional)
- For critical applications, validate AI-called variants against those from a traditional caller (e.g., GATK) or a different AI caller (e.g., Clair3).
- Use hap.py or similar benchmarking tools for a precise comparison of performance metrics like precision and recall.
Workflow Visualization
The following diagram illustrates the integrated bioinformatics workflow for resistance gene identification, from sample preparation to AI-driven analysis.
Integrated Workflow for Resistance Gene Identification
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for WGS and AI-Driven Analysis
| Item | Function/Application | Example Product/Resource |
|---|---|---|
| DNA Extraction Kit | Isolation of high-quality genomic DNA from bacterial cultures for sequencing. | Mag-MK Bacterial Genomic DNA Extraction Kit [88] |
| Sequencing Platform | Generating high-throughput short-read or long-read genomic data. | Illumina NovaSeq 6000 [88] |
| Reference Genome | A standardized genomic sequence for aligning sequencing reads and calling variants. | M. tuberculosis H37Rv (GenBank: NC000962.3) [88] |
| AI Variant Calling Software | Accurate detection of SNPs and InDels from aligned sequencing data using deep learning. | DeepVariant, Clair3, DNAscope [83] |
| Resistance Database | A curated resource of known resistance genes and mutations for annotating and predicting AMR. | CARD, ResFinder/PointFinder [6] |
| Metagenomic Analysis Tool | Identification of ARGs directly from complex microbial communities (metagenomes). | DeepARG, HMD-ARG [6] |
Weighing the Evidence: Validating Results and Comparing Genotypic vs. Phenotypic Methods
In the relentless battle against antimicrobial resistance (AMR), the accuracy of laboratory susceptibility testing is a critical determinant of therapeutic success. This document delineates the foundational principles and practical protocols for establishing the correlation between the disk diffusion method and the reference minimum inhibitory concentration (MIC) determination, the gold standard for antimicrobial susceptibility testing (AST) [89]. Within a broader research framework utilizing directed evolution and whole-genome sequencing (WGS) to identify novel resistance genes, the validation of phenotypic assays is paramount. These correlated methods are indispensable for confirming the resistance phenotypes of evolved microbial strains, thereby bridging the gap between genotypic predictions and phenotypic expression. As the World Health Organization reports a surge in resistance, with over 40% of pathogen-antibiotic combinations showing increased resistance between 2018 and 2023, the imperative for precise, reliable AST has never been greater [90] [91].
Core Principles of Method Correlation
Antimicrobial susceptibility testing operates on the principle of quantifying the effect of an antibacterial agent on a bacterial isolate. The MIC method provides a quantitative measure, defining the lowest concentration of an antimicrobial that inhibits visible growth of a microorganism [89]. The disk diffusion method, in contrast, is a qualitative approach where the diameter of the zone of inhibition around an antibiotic-impregnated disk correlates with the susceptibility of the isolate [89]. The correlation between these methods is established by plotting zone diameters against their corresponding MIC values for a large number of bacterial isolates, generating a scattergram that enables the determination of interpretive criteria (breakpoints) that minimize discrepancies between the methods [92] [89]. These breakpoints are codified by standards organizations such as the Clinical and Laboratory Standards Institute (CLSI) and are recognized by regulatory bodies like the U.S. Food and Drug Administration (FDA) [93].
Quantitative Correlation Data
Comparative Method Performance forNeisseria gonorrhoeae
A study comparing two disk diffusion methods (CLSI and AGSP) with MIC determination via E-test for 100 Neisseria gonorrhoeae isolates demonstrated variable levels of agreement across different antibiotic classes [94].
Table 1: Agreement Between AST Methods for N. gonorrhoeae (n=100)
| Antibiotic | CLSI vs. MIC Agreement | AGSP vs. MIC Agreement | Key Findings |
|---|---|---|---|
| Ciprofloxacin | 100% (Kappa=1) | 100% (Kappa=1) | 99% resistance (QRNG) by all methods [94]. |
| Ceftriaxone | 100% (Kappa=1) | 100% (Kappa=1) | All isolates susceptible by three methods [94]. |
| Spectinomycin | 100% (Kappa=1) | 100% (Kappa=1) | All isolates susceptible by three methods [94]. |
| Penicillin | Moderate (Kappa=0.83) | Moderate | 8 isolates categorized as less susceptible by CLSI/MIC but resistant by AGSP [94]. |
Error Rate Analysis for Ceftazidime-Avibactam
A multi-laboratory study assessing ceftazidime-avibactam against 112 Enterobacterales isolates, many with MIC values near the breakpoints, validated current CLSI disk diffusion breakpoints [92].
Table 2: Discrepancy Analysis for Ceftazidime-Avibactam Testing
| Parameter | Finding | Recommendation |
|---|---|---|
| Optimal Disk Breakpoint | ≥21 mm (Sensitive) / ≤20 mm (Resistant) | Confirmatory MIC testing for zones of 20-22 mm [92]. |
| Error Rates | Lowest with current CLSI breakpoints | Adherence to CLSI M100 guidelines is critical [92]. |
| QC Strains Used | E. coli ATCC 25922, P. aeruginosa ATCC 27853, etc. | Essential for ensuring testing conditions and reagent quality [92]. |
Integrated Experimental Protocols
Workflow for Correlating Disk Diffusion with MIC
The following diagram illustrates the integrated workflow for performing disk diffusion and MIC assays and correlating their results, which is vital for AST method validation and surveillance of resistance patterns.
Protocol: Broth Microdilution for MIC Determination
Principle: A standardized inoculum is introduced into a panel containing serial two-fold dilutions of an antimicrobial agent. The Minimum Inhibitory Concentration (MIC) is the lowest concentration that completely inhibits visible growth after incubation [89].
Materials:
- Cation-adjusted Mueller-Hinton Broth (CAMHB)
- Sterile water or saline for suspension
- McFarland 0.5 standard
- MIC panel with serial antibiotic dilutions
- Incubator at 35°±2°C
Procedure:
- Inoculum Preparation: From an overnight culture, select 3-5 well-isolated colonies. Prepare a suspension in saline or broth, adjusting the turbidity to match a 0.5 McFarland standard (approximately 1-2 x 10^8 CFU/mL) [89].
- Inoculum Dilution: Within 15 minutes, dilute the standardized suspension 1:20 in sterile water or saline to achieve a working inoculum of ~5 x 10^6 CFU/mL [89].
- Panel Inoculation: Transfer the diluted inoculum to the MIC panel tray. Use panel prongs to deliver a precise volume (~0.1 mL) to each well, resulting in a final target concentration of 5 x 10^5 CFU/mL per well [89].
- Incubation: Seal the panel to prevent evaporation and incubate at 35°±2°C for 16-20 hours in an ambient atmosphere [89].
- Reading Results: Examine each well for turbidity. The MIC is the lowest antibiotic concentration that shows no visible growth. Compare the MIC value to established clinical breakpoints (e.g., CLSI M100) to categorize the isolate as Susceptible (S), Intermediate (I), or Resistant (R) [89].
Protocol: Kirby-Bauer Disk Diffusion
Principle: Antibiotic-impregnated disks are placed on an agar plate seeded with a test organism. The antibiotic diffuses into the agar, creating a concentration gradient. After incubation, the diameter of the zone of inhibition is measured and correlated with susceptibility [89].
Materials:
- Mueller-Hinton Agar (MHA) plates, 4-5 mm deep
- Antibiotic disks of specified potencies
- Sterile cotton swabs or replicating device
- McFarland 0.5 standard
- Caliper or automated zone scanner
- Incubator at 35°±2°C
Procedure:
- Inoculum Preparation: Prepare a bacterial suspension adjusted to a 0.5 McFarland standard as described in section 4.2 [89].
- Plate Inoculation: Within 15 minutes, dip a sterile swab into the suspension, remove excess fluid by pressing against the tube wall, and swab the entire surface of the MHA plate in three directions (rotating ~60° each time) for a uniform lawn [89].
- Disk Application: Allow the plate surface to dry for a few minutes. Using sterile forceps or an automated dispenser, place antibiotic disks firmly onto the agar surface, ensuring adequate spacing (e.g., 24 mm center-to-center for a 150 mm plate) to prevent overlapping zones [89].
- Incubation: Invert plates and incubate at 35°±2°C for 16-18 hours [89].
- Reading Results: Measure the diameter of each complete zone of inhibition (including the disk diameter) to the nearest millimeter using a caliper under reflected light. Interpret the zone diameter using the appropriate standards (e.g., CLSI M100) to assign an S, I, or R category [89].
The Scientist's Toolkit: Essential Research Reagents
For researchers employing directed evolution and WGS, correlating genotypic findings with phenotypic resistance requires a suite of validated reagents and tools.
Table 3: Key Research Reagent Solutions for AST Correlation Studies
| Reagent / Material | Function & Importance in Correlation Studies |
|---|---|
| Mueller-Hinton Agar/Broth | The standardized, reproducible growth medium specified by CLSI for AST, ensuring consistent antibiotic diffusion and bacterial growth [94] [89]. |
| Antibiotic Disks (CLSI Potency) | Pre-dosed, quality-controlled disks are essential for generating accurate, reproducible zone diameters in diffusion assays [94] [89]. |
| MIC Panels (Customizable) | Pre-made or custom panels with serial antibiotic dilutions for precise, high-throughput MIC determination, the gold standard for comparison [89]. |
| QC Strains (e.g., E. coli ATCC 25922) | Essential for daily quality control, verifying that media, reagents, and test conditions perform within established limits [92] [89]. |
| Whole-Genome Sequencing Kits | To identify genetic mutations (SNPs, CNVs) underlying resistance phenotypes observed in directed evolution experiments, linking genotype to phenotype [44] [20]. |
Integration with Directed Evolution & WGS Workflows
The correlation of MIC and disk diffusion assays forms a critical phenotypic validation node within a larger research pipeline for resistance gene identification. In a typical directed evolution experiment, bacterial populations are subjected to sublethal, escalating antibiotic pressure to select for resistant mutants [20]. The correlated AST methods described herein are then used to:
- Phenotypically Confirm Resistance: Quantify the level of resistance (e.g., fold-increase in MIC) in evolved clones compared to the ancestral strain [20].
- Guide Strain Selection: Identify clones with clinically relevant or novel resistance patterns for further genomic analysis.
- Validate Genomic Findings: After whole-genome sequencing of resistant clones, the identified genetic variants (e.g., mutations in efflux pumps, target enzymes) can be linked to the specific resistance profile observed in the AST [44] [20]. This integrated approach, often called In Vitro Evolution and Whole Genome Analysis (IVIEWGA), provides powerful statistical confidence that a discovered allele confers resistance [20]. WGS can also elucidate complex resistance mechanisms, such as the mutational upregulation of efflux pumps leading to cross-resistance, which might manifest as a specific, correlated phenotype in both MIC and disk diffusion assays against multiple drug classes [44].
The rigorous correlation of disk diffusion with the gold standard MIC method provides a robust, reliable, and accessible framework for antimicrobial susceptibility testing. For researchers engaged in directed evolution and WGS, these validated phenotypic assays are not merely endpoints but are integral to a discovery feedback loop. They confirm the functional consequences of genetic mutations, guide the selection of clones for deep sequencing, and ultimately bridge computational predictions with biological reality. As the AMR crisis escalates, the synergy of classical microbiology—exemplified by these correlated AST methods—with modern genomic technologies will be paramount in accelerating the identification of new resistance mechanisms and informing the development of next-generation therapeutics.
Antimicrobial resistance (AMR) represents one of the most severe threats to modern healthcare, with drug-resistant infections contributing significantly to global morbidity and mortality [95]. The accurate and timely detection of resistant pathogens is fundamental to effective treatment and antimicrobial stewardship. For decades, conventional antimicrobial susceptibility testing (AST) methods have served as the cornerstone of clinical microbiology, guiding therapeutic decisions by measuring bacterial response to antibiotics in vitro [95] [96]. However, the emergence of whole-genome sequencing (WGS) promises a transformative shift, offering the potential to predict resistance from a single, comprehensive assay by identifying known resistance genes and mutations [44] [97].
This application note provides a direct comparison of WGS-based and traditional phenotypic AST methodologies. Framed within the context of directed evolution and resistance gene identification research, we delineate the operational workflows, performance characteristics, and optimal applications of each approach. The content is structured to assist researchers, scientists, and drug development professionals in selecting and implementing the most appropriate methodology for their specific objectives, whether for fundamental resistance mechanism discovery, routine clinical diagnostics, or global AMR surveillance.
Performance Comparison: Quantitative Data Analysis
The evaluation of WGS against traditional AST reveals a complex performance profile, where genotypic predictions excel in some areas but face challenges in others. The table below summarizes key performance metrics from comparative studies.
Table 1: Direct Performance Comparison of WGS and Traditional AST
| Antibiotic Class / Metric | Categorical Agreement (WGS vs. AST) | Major Errors (ME) | Very Major Errors (VME) | Notable Findings |
|---|---|---|---|---|
| β-lactams (Pneumococci) | >94% [98] | <1% [98] | <1% [98] | Excellent performance despite complexity of predicting β-lactam resistance. |
| Erythromycin | AREScloud: >93%; Pathogenwatch: ~88% [98] | N/R | AREScloud: 14.3%; Pathogenwatch: 53.6% [98] | High VME rates indicate need for optimization for non-β-lactams. |
| Tetracycline | AREScloud: >93%; Pathogenwatch: ~88% [98] | N/R | AREScloud: 19.1%; Pathogenwatch: 47.0% [98] | Tool-dependent variation in performance. |
| Trimethoprim-Sulfamethoxazole | <86% for both tools [98] | N/R | N/R | Lower agreement highlights challenges with certain drug classes. |
| Gram-negative β-lactams | Sensitivity: 0.87; Specificity: 0.98 [7] | N/R | N/R | WGS outperformed some commercial phenotypic methods (PPV: 0.97 vs. 0.92). |
| Hidden Plasmid-mediated Resistance | Case Study: Detected low-abundance blaKPC-14 [99] | N/A | N/A | Phenotypic methods failed to detect this resistance, impacting treatment efficacy. |
Abbreviations: N/R: Not Reported; N/A: Not Applicable; PPV: Positive Predictive Value.
The data demonstrates that WGS can achieve high categorical agreement with phenotypic AST for specific drug-bug combinations, particularly for β-lactam antibiotics in pneumococci [98] and Gram-negative bacteria [7]. However, the technology's performance is not uniform. Notably, high very major error rates (a false-susceptible result) for antibiotics like erythromycin and tetracycline underscore that current genomic predictions require further refinement for reliable application across all antibiotic classes [98]. The ability of WGS to detect "hidden" resistance, such as low-abundance plasmid-encoded genes that phenotypic methods miss, represents a significant strategic advantage in complex infections and for studying directed evolution [99].
Methodological Protocols
Protocol for Traditional Broth Microdilution AST
Broth microdilution is a reference phenotypic method for determining the Minimum Inhibitory Concentration (MIC), the lowest concentration of an antimicrobial that prevents visible growth of a microorganism [95].
Key Reagents and Materials:
- Cation-adjusted Mueller-Hinton Broth (for most non-fastidious bacteria)
- Sterile, multi-well microdilution trays
- Standardized bacterial inoculum (e.g., 0.5 McFarland standard)
- Antibiotic stock solutions at defined concentrations
- Incubator at 35±2°C
Procedure:
- Inoculum Preparation: Suspend 3-5 isolated colonies from an overnight agar plate in a broth medium. Adjust the turbidity to a 0.5 McFarland standard, equating to approximately 1-2 x 10^8 CFU/mL.
- Dilution: Further dilute the bacterial suspension in broth to achieve a final concentration of about 5 x 10^5 CFU/mL in the test well.
- Tray Inoculation: Dispense the diluted inoculum into the wells of a microdilution tray containing serial two-fold dilutions of the antibiotics of interest. Include growth control and sterility control wells.
- Incubation: Incubate the trays under appropriate conditions (temperature, atmosphere, duration) for the specific organism (e.g., 16-20 hours for most aerobes).
- MIC Determination: Read the MIC as the lowest antibiotic concentration that completely inhibits visible growth. Compare MIC values to established clinical breakpoints (e.g., from EUCAST or CLSI) to categorize the isolate as Susceptible, Intermediate, or Resistant [95].
Protocol for WGS-Based Genomic AST
This protocol outlines the process for predicting antimicrobial susceptibility from bacterial whole-genome sequences, utilizing tools like the Comprehensive Antibiotic Resistance Database (CARD) and ResFinder [6].
Key Reagents and Materials:
- High-quality genomic DNA from a pure bacterial isolate.
- Next-generation sequencing platform (e.g., Illumina, Oxford Nanopore Technologies).
- Computational resources (high-performance computing cluster or cloud-based services).
- Bioinformatic tools and curated AMR databases (e.g., CARD, ResFinder, AREScloud, Pathogenwatch).
Procedure:
- DNA Extraction and Sequencing: Extract genomic DNA using a method suitable for the sequencing technology. Prepare sequencing libraries according to the manufacturer's instructions. Sequence the genome to achieve sufficient coverage (e.g., >50x for Illumina).
- Bioinformatic Processing:
- Quality Control: Assess raw sequencing reads for quality using tools like FastQC. Trim adapters and low-quality bases.
- Genome Assembly: De novo assemble the quality-filtered reads into contigs using assemblers like SPAdes or Velvet [100].
- Species Identification: Confirm the bacterial species through tools like MLST or average nucleotide identity.
- AMR Gene Detection:
- Database Interrogation: Use a tool like the Resistance Gene Identifier (RGI) from CARD or ResFinder to align the assembled contigs or reads against a curated database of known AMR genes and resistance-conferring mutations [6].
- Analysis Parameters: Employ strict thresholds for sequence identity and coverage (e.g., >90% identity and >90% coverage) to minimize false positives.
- Phenotype Prediction: Interpret the presence of AMR determinants to predict the susceptibility profile. For instance, the detection of blaKPC predicts resistance to carbapenems, and specific mutations in gyrA predict fluoroquinolone resistance [99] [6]. The predictions from tools like AREScloud and Pathogenwatch can include inferred MICs [98].
Diagram 1: WGS-based AST workflow
Successful implementation of AST methodologies, both phenotypic and genotypic, relies on a suite of critical reagents and computational resources.
Table 2: Key Research Reagent Solutions for AST and WGS
| Item | Function/Application | Examples / Key Features |
|---|---|---|
| Mueller-Hinton Broth | Standardized medium for broth microdilution AST. | Ensures reproducible ion content for accurate antibiotic activity. |
| MIC Panels & Gradient Strips | Phenotypic MIC determination. | Customizable panels; Etest strips provide a simple gradient. |
| Automated AST Systems | High-throughput phenotypic testing. | VITEK 2 (bioMérieux), Phoenix (Becton Dickinson). |
| DNA Extraction Kits | Preparation of high-quality genomic DNA for WGS. | Must be compatible with sequencing technology (e.g., Illumina, ONT). |
| NGS Platforms | Generating whole-genome sequence data. | Illumina (high accuracy), Oxford Nanopore (long reads, portability). |
| Curated AMR Databases | Reference for identifying AMR genes from WGS data. | CARD [6], ResFinder/PointFinder [6], NDARO. |
| Bioinformatic Tools | Analysis of WGS data for AMR detection. | RGI [6], AMRFinderPlus [101], ARIBA. |
Comparative Analysis: Strengths and Limitations
The choice between WGS and traditional AST is not a simple substitution but a strategic decision based on the research or clinical question. The following diagram and analysis outline the core strengths and limitations of each approach.
Diagram 2: Strengths and limitations of WGS vs. traditional AST
WGS Strengths: WGS provides unparalleled resolution, identifying not just resistance but the specific genes and mutations responsible (e.g., blaKPC-2 vs. blaKPC-14), which is invaluable for studying directed evolution and transmission dynamics [44] [99]. It can detect resistance determinants present at low abundance that are missed by phenotypic assays, a critical advantage in complex infections and for early resistance emergence studies [99]. Its speed and portability, especially with nanopore sequencing, enable rapid diagnostics and real-time surveillance [99].
WGS Limitations: The primary limitation is that it predicts resistance potential based on genetic markers, not the expressed phenotype. A detected resistance gene may not be expressed, or resistance may arise from an unknown mechanism, leading to discrepancies [101] [97]. The field also faces challenges with standardization, database curation, and the requirement for significant bioinformatic infrastructure and expertise [100] [97].
Traditional AST Strengths: The foremost strength of phenotypic AST is its direct measurement of the bacterial response to an antibiotic, providing a functional result that has historically guided effective therapy [95]. These methods are well-standardized, widely available, and relatively low-cost, forming a reliable bedrock for clinical microbiology [95].
Traditional AST Limitations: The major drawback is turnaround time, often requiring 24-48 hours after initial culture, which can delay optimal treatment [95]. They are unable to detect the genetic basis of resistance, provide no early warning for emerging resistance, and can fail to detect resistance in heteroresistant populations [99].
Both WGS and traditional AST are indispensable tools in the fight against antimicrobial resistance, yet they serve complementary roles. Traditional AST remains the proven method for functional, phenotypic confirmation of susceptibility that directly informs patient treatment. In contrast, WGS is a powerful discovery and surveillance tool that offers rapid results, high-resolution mechanism insight, and the ability to track the evolution and spread of resistance genes. For research focused on directed evolution, WGS is unmatched in its capacity to identify novel resistance mutations and understand evolutionary pathways.
The future of AST lies not in choosing one method over the other, but in their integrated application. Using WGS for rapid prediction and mechanistic insight, followed by targeted phenotypic confirmation for complex or discrepant results, creates a powerful synergistic workflow. This combined approach will accelerate both fundamental resistance research and the implementation of precision antimicrobial therapy.
The rapid emergence of antimicrobial resistance (AMR) represents a critical global health threat, often described as a silent pandemic [102]. Within this landscape, directed evolution studies and whole-genome sequencing have become indispensable for identifying resistance mechanisms and understanding bacterial adaptation under selective pressure. The accurate identification of antibiotic resistance genes (ARGs) from genomic data is foundational to this research, relying heavily on robust bioinformatics tools. This review provides a detailed evaluation of three prominent tools—AMRFinderPlus, DeepARG, and the Resistance Gene Identifier (RGI)—framed within the context of resistance gene identification research. We assess their underlying algorithms, database structures, and performance characteristics to guide researchers in selecting appropriate resources for investigating the genomic links among AMR, stress response, and virulence [103].
Core Characteristics and Underlying Methodologies
The three tools employ distinct strategies for ARG detection, each with unique strengths for different research scenarios.
AMRFinderPlus, developed by the National Center for Biotechnology Information (NCBI), uses a comprehensive Reference Gene Catalog that includes not only core AMR genes but also those conferring resistance to biocides, metals, and stress, alongside virulence factors [103]. It can identify both acquired genes and chromosomal point mutations from nucleotide or protein sequences, utilizing a combination of BLAST and HMMER with manually curated cutoffs [103]. Its database is rigorously curated, with genes classified by function and supported by evidence from the literature.
DeepARG leverages a deep learning model, specifically a convolutional neural network (CNN), to predict ARGs from sequence data [104] [105]. This alignment-free approach allows it to detect ARGs with low sequence similarity to known references, making it particularly powerful for discovering novel or divergent resistance genes in metagenomic studies [6] [105]. It reports genes and their probability scores across different resistance classes.
RGI (Resistance Gene Identifier) is the analysis tool for the Comprehensive Antibiotic Resistance Database (CARD) [6]. CARD is built around the Antibiotic Resistance Ontology (ARO), which provides a structured, hierarchical classification of resistance determinants, mechanisms, and antibiotics [6]. RGI primarily relies on protein-level homology (BLASTP) with predefined, curated bit-score thresholds to ensure high-quality annotations [6].
Performance and Application Comparison
A comparative assessment of annotation tools reveals significant differences in their outputs and performance, influenced by their underlying databases and algorithms [106]. The following table summarizes the key features and recommended use cases for each tool.
Table 1: Key Features and Use Cases for AMRFinderPlus, DeepARG, and RGI
| Feature | AMRFinderPlus | DeepARG | RGI (CARD) |
|---|---|---|---|
| Primary Method | BLAST & HMMER | Deep Learning (CNN) | Homology (BLASTP) & ARO |
| Database Scope | AMR, stress, virulence, point mutations [103] | ARGs from multiple sources [104] | ARO-curated AMR genes & variants [6] |
| Key Strength | Detects point mutations; integrated NCBI tool | Finds novel/divergent ARGs | Detailed ontology & mechanistic classification |
| Ideal For | Comprehensive pathogen characterization; regulatory analysis | Exploratory metagenomics; novel gene discovery | Mechanistic studies; linking genotype to phenotype |
Quantitative performance evaluations indicate that machine learning-based tools like DeepARG can achieve higher recall, especially for ARGs with lower sequence similarity, compared to strict alignment-based methods [105]. However, tools like AMRFinderPlus and RGI, with their manually curated databases, are noted for high precision in identifying well-characterized resistance mechanisms [106] [103]. The choice of tool can substantially impact the outcome of a study, as differences in database curation, annotation standards, and underlying algorithms lead to variations in the ARGs detected [6] [106].
Integrated Analysis Workflow for Directed Evolution Studies
Investigating resistance evolution requires a pipeline that integrates multiple tools to leverage their complementary strengths. The following workflow diagram outlines a robust protocol for a comprehensive resistome analysis.
Diagram 1: Comprehensive ARG Analysis Workflow. This workflow integrates multiple tools and standardization steps for robust resistance gene identification.
Detailed Protocol for Tool Execution and Analysis
This protocol provides a step-by-step guide for running the core tools and integrating their results, suitable for individual genomes or metagenome-assembled genomes (MAGs).
Input Data Preparation and ORF Prediction
- Input Data: The process can begin with either raw sequencing reads or pre-assembled contigs. For raw reads, use a assembler like SPAdes to generate contigs [107].
- ORF Prediction: Identify protein-coding sequences using prediction tools. Prokka or Bakta provide rapid whole-genome annotation, while Prodigal or Pyrodigal (a faster, more resource-optimized alternative) are stand-alone options specifically for ORF calling [108]. The output is a protein sequence file (FASTA) for each sample, which serves as the primary input for subsequent ARG screening.
Parallel ARG Detection with Multiple Tools
Execute the three tools on the predicted protein sequences (or contigs, if required) to ensure comprehensive detection.
Running AMRFinderPlus:
- Command Example:
amrfinder --protein input.faa --output amrfinder_results.txt --plus - The
--plusflag instructs the tool to include stress response and virulence genes in its analysis, providing a more holistic view of the genome's adaptive features [103]. - The output includes detailed information on the gene name, its predicted function, the class of antibiotic it confers resistance to, and any detected point mutations.
- Command Example:
Running DeepARG:
- Command Example:
deeparg predict --type proteins --input input.faa --output deeparg_results.json --format json - DeepARG can also process short reads directly (
--type reads), which is advantageous for metagenomic studies without an assembly step [104]. - The output includes a probability score for each predicted ARG, allowing researchers to filter results based on confidence.
- Command Example:
Running RGI:
- Command Example:
rgi main --input_sequence input.faa --output_file rgi_results --input_type protein --alignment_tool BLAST - RGI uses the CARD ontology to classify genes. The output can be parsed to understand not just the presence of a gene, but also its mechanism of action and the antibiotic molecule it targets [6].
- Command Example:
Results Standardization and Normalization
A significant challenge in comparing outputs from different tools is their use of inconsistent nomenclature and categorization for ARGs [109]. This is addressed in two steps:
Step 1: Standardization with hAMRonization: Use the
hamronizetool to parse the native outputs of AMRFinderPlus, DeepARG, and RGI into a single, unified data specification format [110].- Command Example:
hamronize amrfinderplus amrfinder_results.txt --format tsv > amrfinder_standardized.tsv
- Command Example:
Step 2: Normalization with argNorm: Feed the standardized outputs into
argNorm, which maps all gene names to unique identifiers from the Antibiotic Resistance Ontology (ARO) in CARD [109]. This resolves issues where the same gene has different names in different databases or where the same name refers to different genes.- Command Example:
argnorm --input amrfinder_standardized.tsv --output amrfinder_normalized.tsv --format tsv
- Command Example:
This two-step process ensures that results are directly comparable across tools, enabling a more reliable and integrated analysis.
Successful in silico prediction of ARGs relies on a suite of computational tools and curated databases. The following table details key resources for constructing a robust analysis pipeline.
Table 2: Key Research Reagents and Computational Resources for ARG Analysis
| Resource Name | Type | Primary Function | Relevance to Directed Evolution |
|---|---|---|---|
| nf-core/funcscan [108] | Workflow | Integrated pipeline for screening (meta)genomes for ARGs, AMPs, and BGCs. | Automates and standardizes functional annotation, ensuring reproducibility in longitudinal evolution studies. |
| hAMRonization [110] | Parser | Standardizes the output formats of >17 AMR detection tools into a unified specification. | Enables direct comparison of results from different tools, crucial for tracking the emergence of new resistance variants. |
| argNorm [109] | Normalization Tool | Maps ARG annotations from different tools to the CARD ARO for consistent nomenclature. | Resolves database conflicts in gene naming, allowing accurate profiling of resistance shifts over time. |
| CARD & ARO [6] | Curated Database & Ontology | Provides a structured, hierarchical classification of resistance determinants and mechanisms. | Essential for interpreting the functional consequence and evolutionary context of identified ARGs. |
| Reference Gene Catalog [103] | Curated Database | NCBI's catalog of AMR, stress, virulence, and point mutations used by AMRFinderPlus. | Provides a comprehensive set of known markers for correlating resistance with other adaptive traits. |
Discussion and Future Perspectives
The integration of tools like AMRFinderPlus, DeepARG, and RGI provides a powerful, multi-faceted approach for profiling antibiotic resistomes. While AMRFinderPlus offers exceptional breadth and curation for known pathogens, DeepARG excels at uncovering the "dark matter" of resistance in complex metagenomes. RGI, grounded in the ARO, delivers deep mechanistic insights. Future directions in the field point towards dynamic evolutionary models. For instance, the proposed Evolutionary Mixture of Experts (Evo-MoE) framework aims to embed predictive models within genetic algorithms to simulate the evolutionary trajectories of resistance development under selective pressure [102]. Such approaches, which move beyond static genomic snapshots to model dynamic adaptation, will be critical for anticipating resistance evolution and guiding the development of next-generation therapeutics and stewardship strategies. For researchers engaged in directed evolution, employing a consolidated workflow that leverages the strengths of each tool—coupled with standardization and normalization steps—will yield the most comprehensive and reliable insights into the complex landscape of antimicrobial resistance.
In the fields of microbiology and drug development, the independent use of genotypic or phenotypic data has historically provided an incomplete picture of complex biological mechanisms, particularly in the study of antimicrobial and drug resistance. The integration of these datasets, however, creates a powerful synergy that reveals a comprehensive view of resistance mechanisms, enabling more effective therapeutic interventions. This approach is particularly vital for addressing the growing threat of antimicrobial resistance (AMR), a major global health challenge characterized by complexities where correlation between genetic markers and observable resistance is not always straightforward [111] [44]. Framed within the context of directed evolution and whole-genome sequencing for resistance gene identification, this application note details how the deliberate combination of phenotypic drug susceptibility testing (DST) with advanced genotypic methods like whole-genome sequencing (WGS) provides researchers with an unprecedented capacity to identify, understand, and surveil resistance mechanisms. The technical and operational complexities of traditional phenotypic DST alone, which remains the "gold standard" but is technically difficult, time-consuming, and can expose laboratory workers to potential infection, create a pressing need for complementary genotypic approaches [111]. Meanwhile, genotypic methods, while rapid, can produce data with undetermined clinical significance if not correlated with phenotypic outcomes [112]. This document provides detailed methodologies and data integration protocols to bridge this gap, offering researchers a validated framework to harness the complete power of combined data for accelerating therapeutic development and combating resistance.
Applications in Research and Drug Development
Elucidating Resistance Mechanisms and Accelerating Antibiotic Discovery
The integration of genotypic and phenotypic data has become an indispensable tool in the pipeline of novel antibiotic development, particularly for challenging pathogens like Mycobacterium tuberculosis. Whole-genome sequencing (WGS) enables the rapid identification of resistance mechanisms during drug development. A seminal example was the first use of 454 pyrosequencing to identify the F0 subunit of the ATP synthase as the target of bedaquiline, which subsequently became the first representative of a novel class of anti-tuberculosis agents approved in 40 years [44]. This genotypic information allows researchers to sequence target genes across phylogenetically diverse reference collections to ensure conservation across pathogen lineages, an important step since drug candidates are typically only tested against a small number of isolates during early development phases [44]. Furthermore, the early elucidation of resistance mechanisms using WGS directly influences clinical trial design. When resistance mechanisms are discovered that only result in marginally increased minimal inhibitory concentrations (MICs), developers can employ more frequent dosing or higher doses in clinical trials to overcome this level of resistance [44]. WGS also plays a crucial role in distinguishing exogenous reinfection from relapse of the primary infection during clinical trials, which is vital for accurately assessing the efficacy of the drug or regimens under investigation [44].
Predicting Resistance Phenotypes from Genomic Data
A critical application of integrated data is the development of bioinformatic platforms that can accurately predict antibiotic resistance phenotypes directly from genomic sequences. The abritAMR platform serves as a prime example—an ISO-certified bioinformatics pipeline for genomics-based bacterial AMR gene detection that utilizes NCBI's AMRFinderPlus while adding features to classify AMR determinants into antibiotic classes and provide customized reports [112]. The validation of this pipeline demonstrates the power of integrated data, showing 99.9% accuracy, 97.9% sensitivity and 100% specificity when compared to PCR or reference genomes, representing 1500 different bacteria and 415 resistance alleles [112]. For Salmonella spp., genomic predictions of phenotype showed 98.9% accuracy when compared against agar dilution results [112]. The implementation of such pipelines in professional settings results in streamlined bioinformatics and reporting pathways, making genomic AMR prediction a practical reality for clinical and public health microbiology.
Table 1: Performance Metrics of the abritAMR Platform in Predicting AMR from Genomic Data
| Validation Method | Accuracy (%) | Sensitivity (%) | Specificity (%) | Details |
|---|---|---|---|---|
| Compared to PCR & Sanger Sequencing | 99.6 | 99.6 | 99.4 | 1179/1184 resistance genes correctly detected |
| Compared to Synthetic Read Data | 99.9 | 97.5 | 100 | 415 AMR genes across 321 genomes |
| Inferred Phenotype for Salmonella spp. | 98.9 | - | - | Compared to agar dilution results |
Studying Chemotherapy Drug Resistance in Human Cells
The integrated approach extends beyond infectious diseases to cancer research, where in vitro evolution and whole genome analysis (IVIEWGA) provides powerful methods for studying chemotherapy drug resistance. Using a near-haploid human cell line (HAP1), researchers have evolved resistance to five different anticancer drugs (doxorubicin, gemcitabine, etoposide, topotecan, and paclitaxel) and then analyzed the genomes of the drug-resistant clones [20]. This approach involves a bioinformatic pipeline that filters for high-frequency alleles predicted to change protein sequence, or alleles which appear in the same gene for multiple independent selections with the same compound [20]. When applied to sequences from 28 drug-resistant clones, this method identified a set of 21 genes strongly enriched for known resistance genes or known drug targets (TOP1, TOP2A, DCK), demonstrating that the same drug resistance mechanisms found in diverse clinical samples can be evolved, discovered, and studied in an isogenic background [20]. The resistance phenotypes were stable, persisting even after drug pressure was removed for 8 weeks (approximately 56 generations) [20].
Integrated Experimental Protocols
Protocol for In Vitro Evolution and Whole-Genome Analysis (IVIEWGA) in Human Cells
This protocol details the process of evolving drug-resistant human cell lines and identifying resistance-conferring genetic variants through whole-genome sequencing, adapted from established methods in haploid human cells [20].
Materials and Reagents:
- Near-haploid human cell line (e.g., HAP1, a chronic myelogenous leukemia-derived cell line)
- Anticancer drugs of interest (e.g., doxorubicin, gemcitabine, etoposide, topotecan, paclitaxel)
- Tissue culture plates and flasks, poly-L-lysine treated 96-well plates
- Cell culture media and supplements appropriate for the cell line
- CellTiter-Glo ATP assay kit for viability assessment
- DNA extraction kit (high-quality, suitable for whole-genome sequencing)
- Next-generation sequencing library preparation kit
Procedure:
- Clone Cells: Dilute HAP1 cells to an average density of ~0.5 cells per well in a poly-L-lysine treated 96-well plate. Pick clones from wells that contain single colonies to establish isogenic parent lines.
- Establish Baseline EC50: For each drug, perform a 48-hour dose-response assay using ATP levels (CellTiter-Glo) as the endpoint to determine the baseline EC50 values for the parent clones.
- Initiate Selection: Start multiple independent selection series for each drug using different parent clones to establish biological replicates.
- Apply Selection Pressure: Use one of two methods:
- Lethal Challenge: For most drugs (e.g., DOX, GEM, TPT, PTX), grow cells to 60-80% confluence with sublethal drug concentrations, then apply a lethal concentration (~3-5 × EC50 value). Remove treatment until cells recover, then reapply drug at ~EC95 value.
- Stepwise Selection: For challenging drugs (e.g., ETP), repeatedly expose cells to concentrations that kill approximately 50% of the population. Increase drug concentration by 5-10% every 5 days while maintaining growth rate at 50% of untreated culture.
- Isolate Resistant Clones: Once resistance emerges in batch culture (typically 7-30 weeks), isolate clones from drug-selected cultures.
- Validate Stable Resistance: Measure drug sensitivity of clones compared to isogenic parent clones. Remove drug pressure for 8 weeks and retest to confirm stability of resistance.
- Sequence and Analyze: Perform whole-genome and exome paired-end read sequencing on drug-resistant clones and their matched drug-sensitive parent clones. Use a bioinformatic pipeline to identify putative resistance variants by filtering for:
- High-frequency alleles predicted to change protein sequence
- Alleles appearing in the same gene across multiple independent selections with the same compound
Protocol for Validated Genomic Detection of AMR Determinants
This protocol describes the implementation of a validated, ISO-certifiable bioinformatics workflow for detecting antimicrobial resistance determinants from bacterial whole-genome sequencing data, based on the abritAMR platform [112].
Materials and Reagents:
- Bacterial isolates with known or unknown AMR profiles
- DNA extraction kit suitable for whole-genome sequencing
- Whole-genome sequencing platform (e.g., Illumina, PacBio)
- High-performance computing cluster or server
- abritAMR software (publicly available)
- NCBI AMRFinderPlus database
- Validation datasets (publicly available from abritAMR publication)
Procedure:
- DNA Extraction and Sequencing: Extract high-quality DNA from bacterial isolates. Perform whole-genome sequencing with minimum 40X coverage (as validated by abritAMR developers).
- Quality Control: Assess sequence quality using FastQC or similar tools. Ensure average sequencing depth ≥40X for reliable AMR gene detection.
- Run abritAMR Pipeline: Execute the abritAMR pipeline, which:
- Performs de novo genome assembly using Shovill (based on SPAdes)
- Runs AMRFinderPlus to identify AMR determinants
- Further classifies AMR mechanisms by antimicrobial class and/or mechanism
- Filters results according to configurable reporting requirements
- Generate Reports: Utilize abritAMR's customized reporting features to create outputs suitable for clinical and public health microbiology, including inferred susceptibility results for specific pathogens (e.g., Salmonella spp.).
- Validation and Quality Assurance: For laboratory accreditation, perform validation against:
- PCR results for key AMR genes
- Synthetic read data from reference genomes
- Phenotypic data for relevant bacterial species
- Precision Assessment: Confirm repeatability and reproducibility through replicate sequencing runs, expecting 100% concordance as demonstrated in validation studies.
Workflow and Data Integration Diagrams
Integrated Genotypic-Phenotypic Analysis Workflow
The following diagram illustrates the comprehensive workflow for integrating phenotypic drug susceptibility testing with genotypic whole-genome sequencing data to identify and validate resistance mechanisms:
Bioinformatics Pipeline for AMR Detection
This diagram details the bioinformatics workflow for processing whole-genome sequencing data to identify antimicrobial resistance determinants, based on the validated abritAMR platform:
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful integration of genotypic and phenotypic data requires specialized reagents and platforms. The following table details key solutions for implementing the protocols described in this application note.
Table 2: Essential Research Reagents and Platforms for Integrated Resistance Studies
| Category | Specific Product/Platform | Function/Application | Key Features |
|---|---|---|---|
| Directed Evolution Systems | EcORep (E. coli Orthogonal Replicon) | Continuous mutagenesis and enrichment of improved enzyme variants | Special DNA replicon with high mutation rate; enables continuous evolution [28] |
| PACE (Phage-assisted Continuous Evolution) | Evolution of biomolecules with improved function | Links enzyme function directly to bacteriophage propagation [28] | |
| High-Fidelity Polymerases | KAPA HiFi DNA Polymerase | NGS library preparation and amplification | Engineered using directed evolution for ultra-high fidelity and robustness [14] |
| Bioinformatics Platforms | abritAMR | Detection of AMR determinants from WGS data | ISO-certified wrapper for NCBI AMRFinderPlus; customized reporting [112] |
| TBDR (Tuberculosis Drug Resistance Database) | Integration of mutation and DST data across studies | Captures structure from multiple studies; enables cross-study querying [111] | |
| Single-Cell Multiomics | SDR-seq (Single-cell DNA–RNA Sequencing) | Functional phenotyping of genomic variants | Simultaneously profiles genomic DNA loci and genes in thousands of single cells [113] |
| Cell Lines | HAP1 (Near-haploid human cell line) | In vitro evolution of drug resistance | Haploid except for 30 Mb fragment of chromosome 15; exposes mutated phenotypes [20] |
In the field of directed evolution and resistance gene identification, next-generation sequencing (NGS) has become a foundational technology. The cost-benefit analysis of genomic research hinges on three critical performance metrics: throughput (the total amount of data generated), speed (how rapidly sequencing is completed), and clinical applicability (the translation of data into actionable diagnostic or therapeutic insights) [114] [45]. For researchers and drug development professionals, optimizing these parameters is essential for efficient experimental design and resource allocation, particularly when tracking the emergence of resistance mutations or conducting large-scale mutagenesis studies.
The cost of whole-genome sequencing has plummeted from approximately $100 million in 2001 to just over $500 in 2023, with some centers reporting costs as low as $350 in 2024 [115]. This dramatic reduction has democratized access to genomic technologies, enabling more extensive directed evolution experiments and comprehensive resistance gene profiling. However, true cost-benefit analysis must extend beyond mere sequencing costs to encompass data quality, analytical throughput, and ultimately, the clinical utility of the generated data [116] [115].
Quantitative Analysis of Sequencing Platforms
Selecting the appropriate sequencing technology requires careful consideration of performance specifications relative to experimental goals. The table below summarizes key metrics for current sequencing platforms relevant to directed evolution and resistance gene studies.
Table 1: Performance Metrics of Sequencing Technologies for Genomic Research
| Platform | Technology Type | Read Length (bp) | Throughput | Key Strengths | Limitations |
|---|---|---|---|---|---|
| Illumina NovaSeq X | Short-read sequencing-by-synthesis | 36-300 | Very high | High accuracy, cost-effective for large volumes | Short reads may challenge complex region assembly |
| PacBio SMRT | Long-read sequencing-by-synthesis | 10,000-25,000 (average) | Moderate | Excellent for resolving repetitive regions, structural variants | Higher cost per gigabase, lower throughput |
| Oxford Nanopore | Long-read electrical impedance detection | 10,000-30,000 (average) | Variable | Real-time sequencing, portability | Higher error rate (~15%) requiring computational correction |
| Ion Torrent | Semiconductor sequencing | 200-400 | Moderate | Rapid turnaround time | Homopolymer sequence errors |
Data synthesized from [114] [45]
The choice between these platforms involves trade-offs. Short-read technologies like Illumina offer high accuracy and throughput at lower costs, making them ideal for variant calling in directed evolution experiments where single-nucleotide changes must be detected [45]. Long-read platforms from PacBio and Oxford Nanopore facilitate complete genome assembly and can identify structural variations and resistance genes in complex genomic regions, but at a higher cost and with generally lower throughput [45].
Table 2: Cost-Benefit Considerations for Research Applications
| Application | Recommended Platform | Data Requirements | Clinical/Research Utility |
|---|---|---|---|
| Resistance gene identification in bacterial populations | Illumina (cost-effective screening) PacBio/Nanopore (complex loci) | 30-50x coverage for variants | High: Direct diagnostic and surveillance applications |
| Directed evolution mutant library screening | Illumina | 50-100x coverage | High: Identifies beneficial mutations and evolutionary trajectories |
| Comprehensive genome assembly for novel organisms | PacBio/Nanopore | 20-30x coverage with long reads | Medium: Foundational for downstream analyses |
| Rapid genomic surveillance | Oxford Nanopore | 20-30x coverage | High: Real-time monitoring of resistance emergence |
Data synthesized from [45] [115] [117]
Experimental Protocols for Resistance Gene Studies
Sample Preparation and Quality Control
Protocol: DNA Extraction for Resistance Gene Sequencing
- Sample Lysis: Use mechanical disruption (bead beating) for bacterial cells, followed by enzymatic lysis with lysozyme (20 mg/mL) and proteinase K (100 µg/mL) at 56°C for 2 hours.
- Nucleic Acid Purification: Employ silica membrane-based columns or magnetic bead purification systems. For long-read technologies, prioritize gentle extraction methods to preserve high molecular weight DNA.
- Quality Assessment:
- Quantify DNA using fluorometric methods (Qubit) rather than spectrophotometry for accuracy.
- Assess integrity via pulsed-field gel electrophoresis for long-read sequencing or bioanalyzer for short-read sequencing.
- Ensure minimum DNA quantities: 100 ng for Illumina, 1-3 µg for PacBio, 400 ng for Nanopore.
Critical Considerations: DNA integrity directly impacts library complexity and sequencing efficiency. Degraded samples yield biased variant calling and incomplete resistance gene detection [45].
Library Preparation and Sequencing
Protocol: Whole Genome Sequencing Library Construction
- DNA Fragmentation: For short-read platforms, use acoustic shearing to generate 300-500 bp fragments. For long-read technologies, minimize fragmentation to maintain read length.
- Library Preparation:
- Illumina: Utilize manufacturer's kits for end-repair, A-tailing, and adapter ligation. Include dual index barcodes for sample multiplexing.
- PacBio: Prepare SMRTbell libraries with hairpin adapters for continuous sequencing.
- Nanopore: Use native ligation kits without PCR amplification to preserve modification detection.
- Quality Control: Validate library size distribution using bioanalyzer or fragment analyzer, and quantify via qPCR for accurate loading.
Sequencing Parameters: For resistance gene studies, aim for minimum 30x coverage across the genome. Increase to 50-100x for detecting low-frequency mutations in heterogeneous populations [117].
Data Analysis Workflow
The following diagram illustrates the core bioinformatics pipeline for analyzing sequencing data from directed evolution and resistance gene studies:
Diagram 1: Genomic Data Analysis Workflow
Implementation Protocol
Protocol: Bioinformatics Analysis for Resistance Gene Detection
Quality Control:
- Use FastQC for initial quality assessment.
- Perform adapter trimming and quality filtering with Trimmomatic or Cutadapt.
- Remove host DNA contamination using mapping-based approaches.
Genome Assembly:
- For reference-based alignment: Use BWA-MEM or Bowtie2 for short reads, Minimap2 for long reads.
- For de novo assembly: Utilize SPAdes for short reads, Flye or Canu for long reads.
- Hybrid assembly approaches often yield optimal results for complex samples.
Variant Calling and Annotation:
- Identify SNPs and indels using GATK or FreeBayes.
- Animate variants with SnpEff or VEP to predict functional consequences.
- For directed evolution studies, quantify mutation frequencies across time points.
Resistance Gene Identification:
- Screen against curated resistance databases (CARD, ResFinder, MEGARes).
- Contextualize resistance mutations within evolutionary frameworks.
- Correlate genotypic resistance with phenotypic predictions.
Computational Requirements: Cloud computing platforms (AWS, Google Cloud) provide scalable infrastructure for large-scale genomic analyses, with specialized workflows available in Terra, Galaxy, and Nextflow [114].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Platforms for Genomic Studies
| Category | Specific Products/Platforms | Function in Research |
|---|---|---|
| Sequencing Platforms | Illumina NovaSeq X, PacBio Revio, Oxford Nanopore PromethION | Generate raw sequencing data with different read length/accuracy trade-offs |
| Library Prep Kits | Illumina DNA Prep, PacBio SMRTbell Prep, Nanopore Ligation Sequencing | Prepare DNA fragments for sequencing with platform-specific compatibility |
| DNA Extraction | QIAamp DNA Mini Kit, MagAttract HMW DNA Kit, Quick-DNA HMW MagBead | Isolate high-quality, high-molecular-weight DNA suitable for sequencing |
| Quality Control | Agilent Bioanalyzer, Qubit Fluorometer, Nanodrop Spectrophotometer | Assess DNA quantity, quality, and integrity before library preparation |
| Bioinformatics Tools | FastQC, Trimmomatic, BWA, SPAdes, GATK, SnpEff, CARD | Process, analyze, and interpret sequencing data to extract biological insights |
| Cloud Platforms | AWS Genomics, Google Cloud Genomics, DNAnexus | Provide scalable computational resources for data storage and analysis |
Data synthesized from [114] [45]
Clinical Applicability Assessment
Translating genomic findings into clinical applications requires rigorous validation and context-specific interpretation. The convergence of genomic technologies with artificial intelligence is accelerating this translation, particularly in personalized oncology where genomic profiling guides targeted therapy selection [117].
Protocol: Validating Clinical Relevance of Resistance Mutations
- Association Studies: Correlate identified mutations with phenotypic resistance data using statistical models that account for population structure.
- Functional Validation: Employ CRISPR-based gene editing to introduce candidate resistance mutations into naive backgrounds and test for resistance phenotypes.
- Clinical Correlation: For human pathogens, integrate genomic data with patient outcomes and treatment histories to establish clinical breakpoints.
- Reporting: Generate clinically actionable reports that highlight validated resistance mechanisms and, where appropriate, suggest alternative therapeutic strategies.
Studies demonstrate that comprehensive genomic profiling directly influences treatment decisions in approximately 17.3% of cases, with higher impact in metastatic diseases (OR=2.73) [117]. The clinical utility is further enhanced when genomic data is integrated with multi-omics approaches, providing a systems-level understanding of resistance mechanisms.
Cost-benefit analysis in genomics extends beyond financial considerations to encompass throughput, speed, and clinical applicability. As sequencing costs continue to decline and technologies evolve, researchers must strategically select platforms and methodologies that align with their specific experimental goals. The integration of automated workflows, cloud computing, and AI-assisted analysis is accelerating the translation of genomic data into clinically actionable insights, particularly in the critical areas of directed evolution and antimicrobial resistance research. By adopting the standardized protocols and analytical frameworks outlined in this document, researchers can optimize resource allocation and maximize the scientific and clinical impact of their genomic investigations.
Conclusion
The integration of directed evolution and whole-genome sequencing presents a formidable strategy for proactively addressing the global AMR crisis. This powerful combination allows researchers to not only identify known resistance genes with high precision but also to discover novel and emerging mechanisms by artificially evolving resistance in a controlled laboratory setting. The key takeaway is that a synergistic approach, which combines the exploratory power of directed evolution with the comprehensive analytical capacity of WGS and robust bioinformatics, is essential for staying ahead of pathogen evolution. Future directions will be shaped by the increasing use of long-read sequencing technologies, the integration of AI and multi-omics data for predictive insights, and the ongoing challenge of translating these sophisticated research tools into rapid, routine clinical diagnostics to guide precision antimicrobial therapy.
References
- 1. Directed evolution [https://en.wikipedia.org/wiki/Directed_evolution]
- 2. A primer to directed evolution: current methodologies and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10074555/]
- 3. Antibodies 101: Antibody Engineering and Directed Evolution [https://blog.addgene.org/antibodies-101-antibody-engineering-and-directed-evolution]
- 4. Measurements drive progress in directed evolution for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8489032/]
- 5. Active learning-assisted directed evolution [https://www.nature.com/articles/s41467-025-55987-8]
- 6. Identification of antibiotic resistance genes from whole ... [https://onehealthadv.biomedcentral.com/articles/10.1186/s44280-025-00079-x]
- 7. Whole-Genome Sequencing Accurately Identifies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5850535/]
- 8. Datasets for benchmarking antimicrobial resistance genes ... [https://www.nature.com/articles/s41597-022-01463-7]
- 9. NGS vs Sanger Sequencing [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-sanger.html]
- 10. Whole Genome Sequencing: Applications in Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11221363/]
- 11. Comparing Gold-Standard Sanger Sequencing with Two ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11631799/]
- 12. Genotypic resistance determined by whole genome ... [https://www.nature.com/articles/s41598-023-27723-z]
- 13. Integrating Whole-Genome Sequencing Data Into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6558386/]
- 14. Directed Evolution Technology for Engineering Enzymes in ... [https://sequencing.roche.com/us/en/article-listing/directed-evolution.html]
- 15. NGS for Drug Development [https://www.illumina.com/areas-of-interest/genomics-in-drug-development/ngs-for-drug-development.html]
- 16. How Whole Genome Sequencing Analysis Facilitates Drug ... [https://danteomics.com/2023/08/21/unleashing-new-frontiers-how-whole-genome-sequencing-analysis-facilitates-drug-discovery-for-rare-diseases/]
- 17. Directed evolution of multiple genomic loci allows the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6016788/]
- 18. Genes-first and phenotypes-first paths to treatment ... [https://www.nature.com/articles/s41419-025-08127-5]
- 19. The Genetic Diversity and Drug Resistance Patterns of HIV‐1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539661/]
- 20. In vitro evolution and whole genome analysis to study ... [https://www.nature.com/articles/s41598-024-63943-7]
- 21. Evaluation of genetic , agronomic traits, and anthracnose... diversity [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-020-6489-0]
- 22. The invention of DNA–RNA hybridization and its outcome [https://www.sciencedirect.com/science/article/abs/pii/S1369848615001004]
- 23. Spiegelman's Monster [https://en.wikipedia.org/wiki/Spiegelman%27s_Monster]
- 24. Adaptation of High-Throughput Screening in Drug Discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3269696/]
- 25. Researchers advance RNA medical discovery decades ... [https://www.sciencedaily.com/releases/2025/02/250224175709.htm]
- 26. High-throughput screening [https://en.wikipedia.org/wiki/High-throughput_screening]
- 27. A Promising New Tool to Combat Antibiotic-Resistant ... [https://irp.nih.gov/blog/post/2025/08/a-promising-new-tool-to-combat-antibiotic-resistant-bacteria]
- 28. iDEC 2025 | Evolution Suisse 2025 [https://idec-teams.github.io/2025_Evolution_Suisse_2025/]
- 29. Phage Host Range Expansion Through Directed Evolution ... [https://pubmed.ncbi.nlm.nih.gov/40806726/]
- 30. Towards the integration of antibiotic resistance gene ... [https://www.nature.com/articles/s44259-025-00154-8]
- 31. engineering a novel M23 peptidase to combat Listeria ... [https://www.nature.com/articles/s41598-025-99141-2]
- 32. High-throughput qPCR profiling of antimicrobial resistance ... [https://www.sciencedirect.com/science/article/pii/S0269749125004695]
- 33. library construction methods for directed evolution [https://pmc.ncbi.nlm.nih.gov/articles/PMC390300/]
- 34. Live culture-based qPCR screening of Taq DNA ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1624735/full]
- 35. One-step generation of error-prone PCR libraries using ... [https://microbialcellfactories.biomedcentral.com/articles/10.1186/1475-2859-11-14]
- 36. Rediscovering Inosine-EpPCR to Create Starting Libraries for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293787/]
- 37. Random Mutagenesis: 8 Approaches for Success [https://bitesizebio.com/252/8-approaches-to-random-mutagenesis/]
- 38. Correcting errors in PCR-derived libraries for rare allele ... [https://www.nature.com/articles/s42003-025-08537-3]
- 39. Development of simple random mutagenesis protocol for the ... [https://biotechnologyforbiofuels.biomedcentral.com/articles/10.1186/s13068-016-0613-z]
- 40. FACS-Based Functional Protein Screening via Microfluidic ... [https://www.nature.com/articles/s41598-020-66927-5]
- 41. Metabolic growth-coupling strategies for in vivo enzyme ... [https://www.sciencedirect.com/science/article/pii/S221403012500001X]
- 42. Directed Evolution [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/protein-biology/protein-expression/directed-evolution?srsltid=AfmBOoqd_XyjjUkmZvMNTaYne0sWOnzWhgAjufXRWA9mJ6SK7HCr4sss]
- 43. Cell-Based Screening Using High-Throughput Flow Cytometry [https://pmc.ncbi.nlm.nih.gov/articles/PMC3045571/]
- 44. Whole-genome sequencing to control antimicrobial resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC4156311/]
- 45. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 46. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 47. Long-Read Sequencing Technology | For challenging ... [https://www.illumina.com/science/technology/next-generation-sequencing/long-read-sequencing.html]
- 48. Comparison of short-read and long-read next-generation ... [https://pubmed.ncbi.nlm.nih.gov/39387352/]
- 49. Advancing Drug Resistance Detection: Comparative ... [https://www.mdpi.com/2813-9038/2/3/14]
- 50. Advantages of long- and short-reads sequencing for the ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1104456/full]
- 51. Comparative Analysis of Short- and Long-Read ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2022.857801/full]
- 52. Application of next-generation sequencing in the detection ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898125003997]
- 53. Review and Comparison of Antimicrobial Resistance Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8944830/]
- 54. The Comprehensive Antibiotic Resistance Database [https://card.mcmaster.ca/]
- 55. ARGs: Detection, Database, and Bioinformatics Tools [https://www.cd-genomics.com/microbioseq/resource-args-detection-database-bioinformatics-tools.html]
- 56. Predicting Antibiotic Resistance in Listeria monocytogenes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563061/]
- 57. Comparative assessment of annotation tools reveals ... [https://www.nature.com/articles/s41598-025-24333-9]
- 58. Clinical and Microbiological Characteristics of Klebsiella ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10640825/]
- 59. A global trend on tuberculosis co-infection with ... [https://japsonline.com/abstract.php?article_id=4576&sts=2]
- 60. Miliary Tuberculosis Associated with Klebsiella pneumonia [https://e-trd.org/journal/view.php?doi=10.4046/trd.2024.0105]
- 61. Whole-genome sequencing of Klebsiella pneumoniae MDR ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10835-9]
- 62. A case series of co-infection in Mycobacterium tuberculosis ... [https://ejb.springeropen.com/articles/10.1186/s43168-024-00270-5]
- 63. AMRFinderPlus - Pathogen Detection - NCBI - NIH [https://www.ncbi.nlm.nih.gov/pathogens/antimicrobial-resistance/AMRFinder/]
- 64. RGI Resistance Gene Identifier [https://card.mcmaster.ca/analyze/rgi]
- 65. Evolution of Mycobacterium tuberculosis drug resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9585206/]
- 66. Directed evolution of Mycobacterium tuberculosis β ... [https://pubmed.ncbi.nlm.nih.gov/24023821/]
- 67. Genome-wide chemical mutagenesis screens allow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5378179/]
- 68. Mutagenesis techniques for evolutionary engineering of ... [https://www.sciencedirect.com/science/article/pii/S0966842X24000465]
- 69. A Rapid, High-Throughput Method for the Construction of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12649946/]
- 70. Site-saturation mutagenesis of 500 human protein domains [https://www.nature.com/articles/s41586-024-08370-4]
- 71. 机器学习方法在CRISPR/Cas9系统中的应用 - 遗传 [http://www.chinagene.cn/article/2018/0253-9772/0253-9772-40-9-704.shtml]
- 72. Coupling chemical mutagenesis to next generation ... [https://www.nature.com/articles/s41467-019-13344-6]
- 73. New research maps 14 potential evolutionary dead ends ... [https://www.stockholmresilience.org/research/research-news/2023-11-13-new-research-maps-14-potential-evolutionary-dead-ends-for-humanity-and-ways-to-avoid-them.html]
- 74. New research maps 14 potential evolutionary dead ends ... [https://www.sciencedaily.com/releases/2023/11/231113111803.htm]
- 75. Antimicrobial resistant bacteria and genes move freely ... [https://www.sanger.ac.uk/news_item/antimicrobial-resistant-bacteria-and-genes-move-freely-between-people-animals-and-the-environment/]
- 76. Global diversity and distribution of antibiotic resistance ... [https://www.nature.com/articles/s41467-025-59019-3]
- 77. Predicting antibiotic resistance genes and bacterial ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1628952/full]
- 78. Simultaneous detection of pathogens and antimicrobial ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01480-2]
- 79. Recommendations for bioinformatics in clinical practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535132/]
- 80. Semantic design of functional de novo genes from a ... [https://www.nature.com/articles/s41586-025-09749-7]
- 81. Advanced research and exploration of CRISPR technology ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975025001193]
- 82. Metagenomics as a Transformative Tool for Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11939754/]
- 83. Artificial intelligence in variant calling: a review [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1574359/full]
- 84. How AI can help us beat AMR | npj Antimicrobials and ... [https://www.nature.com/articles/s44259-025-00085-4]
- 85. The 2025 Bioinformatics Toolkit: From Sample Prep to AI- ... [https://blog.omni-inc.com/blog/the-2025-bioinformatics-toolkit-from-sample-prep-to-ai-driven-analysis]
- 86. Recent Applications of Artificial Intelligence in Discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11624680/]
- 87. Joint processing of long- and short-read sequencing data ... [https://www.sciencedirect.com/science/article/pii/S2667237525001432]
- 88. Whole genome sequencing to characterize the molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595642/]
- 89. Antimicrobial Susceptibility Testing - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK539714/]
- 90. WHO warns of widespread resistance to common ... [https://www.who.int/news/item/13-10-2025-who-warns-of-widespread-resistance-to-common-antibiotics-worldwide]
- 91. Antibiotic resistance surges globally, UN health agency warns [https://news.un.org/en/story/2025/10/1166087]
- 92. Correlation between Broth Microdilution and Disk Diffusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7098758/]
- 93. Antibacterial Susceptibility Test Interpretive Criteria [https://www.fda.gov/drugs/development-resources/antibacterial-susceptibility-test-interpretive-criteria]
- 94. Comparison of Two Disc Diffusion Methods with Minimum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4071750/]
- 95. Antimicrobial Susceptibility Testing: A Comprehensive Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9024665/]
- 96. Microbiological methodologies: Comparative evaluation of ... [https://www.sciencedirect.com/science/article/pii/S0717345825000053]
- 97. The role of whole genome sequencing in antimicrobial ... [https://www.sciencedirect.com/science/article/pii/S1198743X16305687]
- 98. a direct comparison of two genomic tools to conventional ... [https://pubmed.ncbi.nlm.nih.gov/39745445/]
- 99. Detection of hidden antibiotic resistance through real-time ... [https://www.nature.com/articles/s41467-024-49851-4]
- 100. Next generation sequencing as a panacea for antibiotic ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1650925/full]
- 101. Limitations of current techniques in clinical antimicrobial ... [https://www.nature.com/articles/s44259-024-00033-8]
- 102. AMR-MoEGA: Antimicrobial Resistance Prediction using ... [https://arxiv.org/html/2511.12223v1]
- 103. and the Reference AMRFinderPlus Catalog facilitate... Gene [https://www.nature.com/articles/s41598-021-91456-0?error=cookies_not_supported]
- 104. PLM-ARG: antibiotic resistance gene identification using a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10676515/]
- 105. an alignment-free explainable approach to annotate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12403478/]
- 106. Comparative assessment of annotation tools reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627748/]
- 107. Combining Functional Genomics and Whole ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8070361/]
- 108. (Meta-) genome screening for functional and natural product gene ... [https://nf-co.re/funcscan/2.0.0/docs/output/]
- 109. argNorm: normalization of antibiotic resistance annotations to... gene [https://pmc.ncbi.nlm.nih.gov/articles/PMC12064170/]
- 110. pha4ge/hAMRonization: Parse multiple Antimicrobial Resistance ... [https://github.com/pha4ge/hAMRonization]
- 111. Integration of Published Information Into a Resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4366577/]
- 112. An ISO-certified genomics workflow for identification and ... [https://www.nature.com/articles/s41467-022-35713-4]
- 113. Functional phenotyping of genomic variants using joint ... [https://www.nature.com/articles/s41592-025-02805-0]
- 114. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 115. Measuring Genome Sequencing Costs and its Health Impact [https://www.wipo.int/en/web/global-health/w/news/2025/measuring-genome-sequencing-costs-and-its-health-impact]
- 116. Cost–effectiveness analysis - Health system efficiency - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK436886/]
- 117. Advances in personalized medicine: translating genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106117/]