Ensuring Phenotypic Data Quality: A Guide to Multi-Parameter Gating for Robust Biomedical Research
This article provides a comprehensive guide for researchers and drug development professionals on establishing high-quality multi-parameter gating for phenotypic data.
Ensuring Phenotypic Data Quality: A Guide to Multi-Parameter Gating for Robust Biomedical Research
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on establishing high-quality multi-parameter gating for phenotypic data. It covers the foundational principles of immunophenotyping and the critical challenges of manual analysis, explores cutting-edge computational and automated methods, details strategies for troubleshooting and optimizing gating performance, and finally, outlines robust frameworks for validating and comparing gating strategies to ensure data reproducibility and reliability in clinical and research settings.
The Critical Foundation: Understanding Phenotypic Diversity and the Imperative for Rigorous Gating
Defining Immunophenotyping and Its Role in Disease Diagnosis and Monitoring
Immunophenotyping is a foundational technique in clinical and research laboratories that identifies and classifies cells, particularly those of the immune system, based on the specific proteins (antigens) they express on their surface or intracellularly [1] [2]. This process is most commonly performed using flow cytometry, a laser-based technology that can analyze thousands of cells per second in a high-throughput manner [3] [4]. By detecting combinations of these markers, researchers and clinicians can define specific immune cell subsets, identify aberrant cell populations, and track how these populations shift in response to disease, treatment, or other experimental conditions [3]. The ability to profile the immune system at the single-cell level makes immunophenotyping an indispensable tool for diagnosis, prognosis, and monitoring of a wide range of diseases, from immunodeficiencies to cancers like leukemia and multiple myeloma [1] [5].
FAQs and Troubleshooting Guides
This section addresses common challenges encountered during immunophenotyping experiments, providing evidence-based solutions to ensure data quality and reproducibility.
Troubleshooting Common Immunophenotyping Issues
| Problem Area | Common Issue | Potential Cause | Recommended Solution |
|---|---|---|---|
| Sample & Staining | High background noise/non-specific binding | Dead cells in sample; antibody concentration too high [3] [6] | Use a viability dye (e.g., 7-AAD) to gate out dead cells; titrate antibodies to find optimal separating concentration [3] [6]. |
| Data Acquisition | Unstable signal or acquisition interruptions | Air bubbles, cell clumps, or clogs in the fluidic system [7] | Use a time gate (SSC/FSC vs. time) to identify and gate on regions of stable signal; check sample filtration and fluidics [7]. |
| Gating Strategy | Inability to resolve dim populations or define positive/negative boundaries | Poor voltage optimization; spillover spreading; lack of proper controls [6] | Perform a voltage walk to determine Minimum Voltage Requirement (MVR); use FMO controls to accurately set gates for dim markers [6]. |
| Population Analysis | Doublets misidentified as single cells | Two or more cells stuck together and analyzed as one event [8] | Use pulse geometry gating (FSC-H vs. FSC-A or FSC-W vs. FSC-H) to exclude doublets and cell clumps [8] [7]. |
| Panel Design | Excessive spillover spreading compromising data | Poor fluorophore selection; bright dyes paired with highly expressed antigens [6] | Pair bright fluorophores with low-abundance markers and dim fluorophores with highly expressed antigens [6]. |
Frequently Asked Questions (FAQs)
Q1: What are the most critical controls for a multicolor immunophenotyping panel? The essential controls are:
- Unstained cells: To set background autofluorescence levels.
- Single-stained controls: For calculating compensation due to spectral overlap between fluorochromes.
- Fluorescence Minus One (FMO) controls: Tubes containing all antibodies except one. These are critical for accurately setting gates, especially for dimly expressed markers or when markers are expressed on a continuum [3] [6].
- Viability dye control: To distinguish and exclude dead cells that bind antibodies non-specifically [3] [6].
Q2: How do I determine the correct gate boundaries for a mixed or smeared cell population? Do not rely on arbitrary gates. Use FMO controls to define where "negative" ends and "positive" begins for each marker in the context of your full panel. This control accounts for the spillover spreading from all other fluorochromes into the channel of interest, allowing for confident and reproducible gating [6].
Q3: My experiment requires analyzing a very rare cell population. What should I consider? The number of cells that need to be collected depends on the rarity of the population. To ensure statistically significant results, you must acquire a sufficiently large total number of events. Furthermore, use a "loose" initial gate around your target population on FSC/SSC plots to avoid losing rare cells early in the gating strategy [7].
Q4: What is the limitation of manual gating, and are there alternatives? Manual gating is subjective, can be influenced by user expertise, and becomes time-consuming for high-parameter screens. Computational and automated gating methods (e.g., in FlowJo, SPADE, viSNE) offer a fast, reliable, and reproducible way to analyze samples and can even identify new cellular subpopulations that may be missed by a pre-defined manual strategy [7].
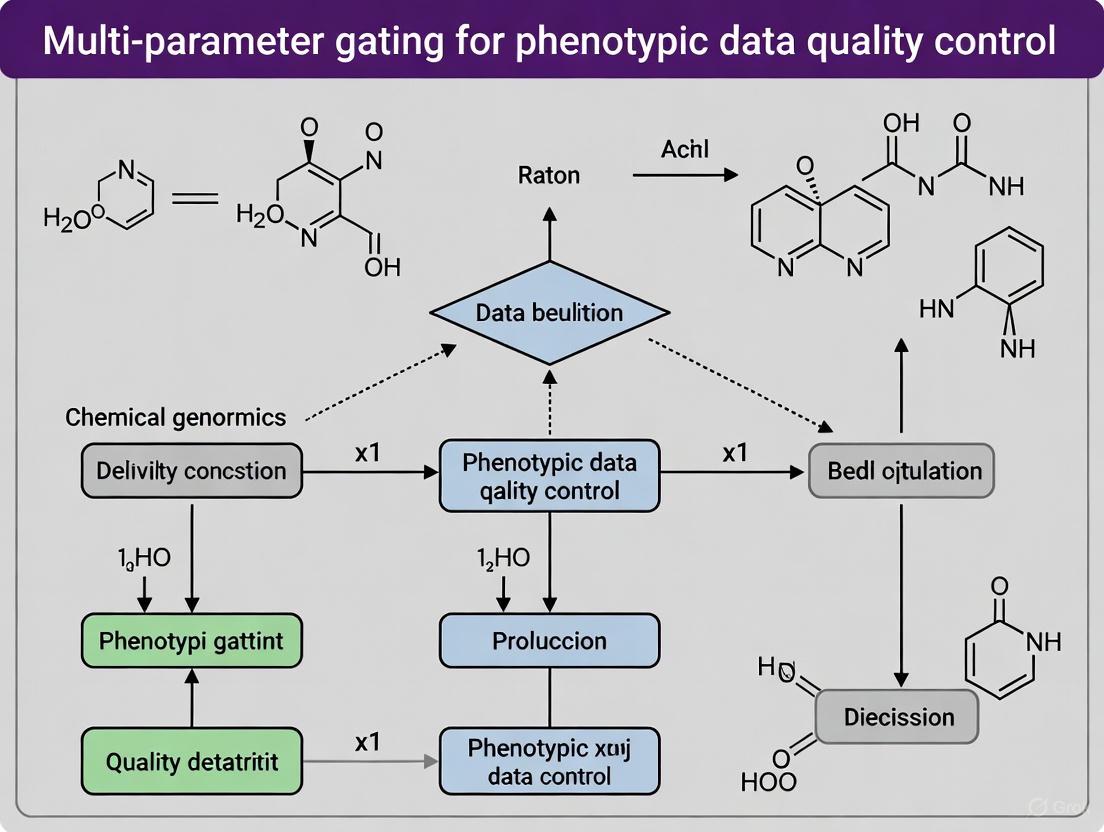
Core Experimental Workflow and Visualization
A standardized workflow is fundamental to generating high-quality, reproducible immunophenotyping data. The following diagram and protocol outline the key stages.
Immunophenotyping Workflow for Data Quality
Detailed Methodology for Multi-Parameter Flow Cytometry
Sample Preparation and Staining:
- Collect samples in appropriate anticoagulants (e.g., EDTA or heparin) [1].
- Create a single-cell suspension. For tissues, mechanical or enzymatic dissociation may be required.
- Wash cells with a buffer (e.g., PBS) containing a detergent like Triton X-100 to reduce non-specific binding [1].
- Incubate with a viability dye to mark dead cells.
- Stain with titrated, fluorophore-conjugated antibodies targeting specific surface and/or intracellular markers. Incubate in the dark, then wash to remove unbound antibody [1] [6].
Data Acquisition on Flow Cytometer:
- Use the fluidics system to transport cells single-file past a laser [8].
- As cells intercept the laser, light is scattered (Forward Scatter - FSC, Side Scatter - SSC) and fluorophores are excited, emitting light at specific wavelengths [8].
- Detectors (photodiodes and photomultiplier tubes) convert these light signals into electronic data for each cell [8].
Data Pre-processing & Multi-Parameter Gating:
- Exclude doublets: Plot FSC-H vs. FSC-A to gate on single cells [8] [7].
- Exclude dead cells: Gate on viability dye-negative cells [3].
- Apply compensation: Use single-stained controls to correct for spectral overlap [6].
- Sequential gating: Use a stepwise strategy to isolate the population of interest. A classic example for identifying human regulatory T cells (Tregs) is [3]:
- Gate on single cells -> Gate on live cells -> Gate on CD45+ leukocytes -> Gate on CD3+ T cells -> Gate on CD4+ T cells -> Identify Tregs as CD25high, FoxP3+, and optionally CD127low.
The Scientist's Toolkit: Essential Research Reagents
| Item | Function / Application |
|---|---|
| Fluorophore-conjugated Antibodies | Probes that bind with high specificity to target cell antigens (e.g., CD4, CD8, CD19); allow for detection and classification of cell types [3] [4]. |
| Viability Dyes | Amine-reactive dyes (e.g., 7-AAD, PI) that permeate dead cells; essential for excluding these cells from analysis to reduce background noise [3] [6]. |
| FMO Controls | A cocktail of all fluorophore-conjugated antibodies in a panel except one; critical for accurately defining positive and negative populations during gating [3] [6]. |
| Compensation Beads | Uniform beads that bind antibodies; used with single-color stains to create consistent and accurate compensation matrices for spectral overlap correction [6]. |
| Lymphocyte Isolation Kits | Reagents for density gradient centrifugation or negative selection to enrich for lymphocytes from peripheral blood mononuclear cells (PBMCs), reducing sample complexity. |
FAQs: Addressing Core Experimental Challenges
Q1: What are the primary sources of phenotypic heterogeneity in Acute Myeloid Leukemia (AML) that can confound multiparameter gating?
A1: Phenotypic heterogeneity in AML stems from several sources that can create subpopulations with distinct marker expressions, challenging clear gating strategies.
- Genetic and Clonal Evolution: AML is not a single clone but often consists of multiple subclones with distinct genetic mutations (e.g., in FLT3, NPM1, IDH1/2). These subclones can evolve, especially under treatment pressure, leading to shifts in the phenotypic landscape detectable by flow cytometry [9].
- Epigenetic Regulation: Even within genetically identical cells, epigenetic heterogeneity can drive diverse gene expression profiles and cell states, influencing surface protein expression [9].
- Cell of Origin and Differentiation State: The disease arises from hematopoietic stem cells, and the phenotypic makeup can reflect varying degrees of differentiation block, resulting in mixtures of progenitor-like and more differentiated blast populations [10] [9].
Q2: In Multiple Myeloma (MM), how does the bone marrow microenvironment contribute to phenotypic heterogeneity and drug response variability?
A2: The bone marrow microenvironment is a critical contributor to MM heterogeneity, acting as a protective niche and influencing drug sensitivity.
- Protective Niche Interactions: Myeloma cells interact with immune cells, stromal cells, osteoclasts, and osteoblasts. These interactions provide survival and proliferative signals (e.g., via cytokines like TNF-α and IL-6) that can alter the phenotype and drug resistance of the malignant plasma cells [11].
- Inflammation and Treatment Stage: Ex vivo drug sensitivity in MM has been globally associated with bone marrow microenvironmental signatures that reflect the patient's treatment stage, clonality, and inflammation status [11].
- Non-Cell-Autonomous Resistance: The microenvironment can confer innate resistance to therapies, meaning that measuring myeloma cell phenotype alone is insufficient; the surrounding cellular context must also be considered in the analysis [11].
Q3: What advanced analytical techniques can help deconvolute complex, heterogeneous cell populations in these malignancies?
A3: Moving beyond traditional two-dimensional gating, several high-dimensional techniques are now essential.
- High-Parameter Flow and Mass Cytometry: Technologies like spectral flow cytometry (measuring full emission spectra) and mass cytometry (CyTOF) allow for the simultaneous measurement of 40+ parameters on a single-cell level. This dramatically increases the resolution to identify rare subpopulations and new cell phenotypes without significant signal spillover [12].
- Single-Cell RNA Sequencing (scRNA-seq): This technique allows for the inference of gene regulatory networks (GRNs) at a single-cell resolution. It can capture patient-specific signatures of gene regulation that perfectly discriminate between AML and control cells, revealing heterogeneity that is masked in bulk analyses [10].
- Multiplexed Immunofluorescence and Deep Learning: Automated microscopy combined with deep-learning-based single-cell phenotyping can classify millions of cells from a bone marrow sample. Convolutional neural networks (CNNs) can identify latent phenotypic features and reliably distinguish malignant cells (e.g., large myeloma cells) from their benign counterparts based on size and marker expression [11].
Experimental Protocols for Investigating Heterogeneity
Protocol 1: Single-Cell Gene Regulatory Network (GRN) Analysis in AML
Methodology: This protocol outlines the process for using single-cell RNA sequencing data to infer patient-specific GRNs, capturing regulatory heterogeneity [10].
- Sample Preparation & Sequencing: Obtain bone marrow samples from AML patients and healthy controls. Perform single-cell RNA sequencing (scRNA-seq) on sorted progenitor, monocyte, and dendritic cells.
- Data Preprocessing: Quality control, normalization, and filtering of the scRNA-seq count data.
- Network Inference: Infer gene regulatory networks using a consensus approach from multiple algorithms (e.g., ARACNE, CLR, MRNET, GENIE3) to build a robust consensus network.
- Single-Sample Network Construction: Apply the LIONESS (Linear Interpolation to Obtain Network Estimates for Single Samples) method to reconstruct a unique GRN for each individual patient and cell type.
- Downstream Analysis:
- Perform dimensionality reduction (e.g., PCA, t-SNE) on network statistics or adjacency matrices.
- Use classification models (e.g., random forests) to test the predictive power of the single-cell GRNs.
- Conduct pathway enrichment analysis on highly connected and predictive genes.
Protocol 2: Image-Based Ex Vivo Drug Sensitivity Profiling in Multiple Myeloma
Methodology: This protocol, known as pharmacoscopy, details an image-based high-throughput screen to assess heterogeneous drug responses in MM patient samples [11].
- Sample Acquisition: Collect bone marrow aspirates from MM patients across different disease stages.
- Ex Vivo Drug Treatment: Plate bone marrow mononuclear cells (BMNCs) in multi-well plates. Treat with a panel of therapeutic agents (e.g., proteasome inhibitors, immunomodulatory drugs, monoclonal antibodies) across a range of concentrations.
- Multiplexed Immunofluorescence and Imaging: Stain cells with fluorescent antibodies targeting key markers (e.g., CD138, CD319, CD3, CD14). Use automated high-throughput microscopy to image millions of cells per sample.
- Deep-Learning-Based Single-Cell Phenotyping:
- Train a Convolutional Neural Network (CNN) to classify every imaged cell into categories: CD138+/CD319+ plasma cells, CD3+ T cells, CD14+ monocytes, and "other" cells.
- A second neural network is used to identify "large" plasma cell-marker-positive cells as the putative myeloma cell population for analysis.
- Quantitative Analysis: For each drug condition, quantify the abundance and viability of the defined myeloma cell population. Integrate this ex vivo sensitivity data with matched genetic, proteomic, and clinical data to map molecular regulators of drug response.
Summarized Quantitative Data
Table 1: Technological Platforms for Multiparametric Cell Analysis
| Technology | Key Principle | Max Parameters | Advantages | Key Challenge |
|---|---|---|---|---|
| Conventional Flow Cytometry [12] | Fluorescent labels detected by lasers and PMTs/APDs | ~30 | High throughput, well-established | Fluorescence spillover complicates panel design |
| Spectral Flow Cytometry [12] | Full spectrum measurement; mathematical deconvolution | 40+ | Reduced spillover, flexible panel design | Sensitive to spectral changes in fluorescent labels |
| Mass Cytometry (CyTOF) [12] | Metal isotope labels; detection by time-of-flight mass spectrometry | 100+ | Minimal signal spillover, deep phenotyping | Lower throughput, destructive to cells, costly reagents |
| Image-Based Deep Learning [11] | Automated microscopy & CNN-based cell classification | Morphological + molecular | Provides spatial context, latent feature discovery | Computationally intensive, requires large datasets |
Table 2: Molecular and Phenotypic Heterogeneity in Case Studies
| Disease | Source of Heterogeneity | Experimental Evidence | Impact on Data Quality & Gating |
|---|---|---|---|
| Acute Myeloid Leukemia (AML) [10] [9] | - Multiple genetic subclones- Epigenetic states- Cell of origin | - scRNA-seq GRNs enable 100% classification accuracy [10]- Mouse models require multiple mutations for disease [9] | Gating strategies based on limited markers may miss rare, resistant subclones that drive relapse. |
| Multiple Myeloma (MM) [13] [11] | - Familial predisposition [13]- Tumor microenvironment signals- Treatment-induced evolution | - Deep learning identifies phenotypically distinct "large" myeloma cells [11]- Ex vivo drug response correlates with clinical outcome [11] | Standard plasma cell gating (CD138+) may include non-malignant cells; size and multi-marker verification are critical. |
Visualized Workflows and Signaling Pathways
Diagram 1: Single-Cell GRN Analysis Workflow
Diagram 2: Key Signaling Pathways in AML Pathogenesis
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Biological Role | Application in Featured Experiments |
|---|---|---|
| Fluorochrome Conjugated Antibodies [12] | Tag specific cell surface/intracellular proteins for detection by flow cytometry. | Panel design for high-content screening to identify multiple cell subsets simultaneously. |
| Stable Lanthanide Isotopes [12] | Metal tags for antibodies in mass cytometry; detected by time-of-flight. | Allows for >40-parameter detection with minimal spillover for deep immunophenotyping. |
| Single-Cell RNA Barcoding Kits [10] | Uniquely label mRNA from individual cells for sequencing. | Enables generation of single-cell RNA-seq data for gene regulatory network inference. |
| Recombinant Cytokines (e.g., IL-6, TNF-α) [11] | Mimic bone marrow microenvironment signals in ex vivo cultures. | Used in functional assays to study their role in myeloma cell survival and drug resistance. |
| Targeted Inhibitors (e.g., Bortezomib, Venetoclax) [11] | Pharmacological probes to perturb specific pathways in cancer cells. | Applied in ex vivo drug screens to profile patient-specific sensitivity and resistance patterns. |
Frequently Asked Questions (FAQs)
1. What are the primary pitfalls of manual gating? Manual gating, the traditional method for analyzing cytometry data, suffers from three major pitfalls:
- Subjectivity: The process depends highly on the investigator's knowledge and is prone to human bias, leading to inconsistent results [14] [15].
- Time Consumption: It is a labor-intensive and slow process, with analysis of a single sample potentially taking 30 minutes to 1.5 hours [15] [16].
- Inter-Operator Variability: When multiple users analyze the same data, technical variability can be as high as 25-78% due to difficulties in reproducing the exact gating strategy [15] [16].
2. Why does increasing the number of parameters measured make manual gating unsustainable? The number of pairwise plots required for analysis increases quadratically with the number of measured parameters, an issue known as "dimensionality explosion" [14]. While instruments can now measure 40-50 parameters and are moving toward 100 dimensions, the 2D computer screen forces analysts to slice data into a series of 2D projections, a process that becomes unmanageable for large, high-dimensional datasets [14] [15].
3. Can automated methods truly replicate the expertise of a manual analyst? Yes, and they offer additional benefits. Automated gating methods, including unsupervised clustering and supervised auto-gating, are not only designed to reproduce expert manual gating but also to perform this task in a rapid, robust, and reproducible manner [14] [17]. Furthermore, some computational methods can act as "discovery" tools by identifying new, biologically relevant cellular populations that were not initially considered by the researcher, as they use mathematical algorithms to detect trends within the entire dataset [16].
4. What is the performance of automated tools compared to manual gating? Comprehensive evaluations have shown that several automated tools perform well. A 2024 study comparing 23 unsupervised clustering tools found that several, including PAC-MAN, CCAST, FlowSOM, flowClust, and DEPECHE, generally demonstrated strong performance in accurately identifying cell populations compared to manual gating as a truth standard [17]. Supervised approaches, which use pre-defined cell-type marker tables, can attain close to 100% accuracy compared to manual analysis [15].
5. How do automated methods improve reproducibility in multi-operator or multi-site studies? Automated methods are unbiased and based on unsupervised clustering or supervised algorithms, which apply the same mathematical rules to every dataset [14]. This eliminates the subjectivity inherent in manual human assessment, ensuring that the same input data will yield the same output populations regardless of who runs the analysis or where it is performed, thereby significantly enhancing reproducibility [16] [18].
Troubleshooting Guides
Issue 1: High Inter-Operator Variability in Population Identification
Problem: Different scientists are gating the same samples differently, leading to inconsistent results and difficulties reproducing findings.
Solution: Implement automated gating algorithms to standardize analysis.
- Step 1: Choose an Analysis Approach. Select from two main categories of computer-aided methods [17]:
- Unsupervised Clustering: Cells are grouped into clusters based solely on marker intensities without human intervention. The resulting clusters require annotation by the researcher. Tools include FlowSOM and SPADE [14] [19].
- Supervised Auto-gating: The algorithm groups cells and also assigns cell-type labels based on a pre-specified marker table, requiring an initial training phase [17].
- Step 2: Apply the Chosen Tool. Use the selected software to analyze all samples within the study with an identical, predefined configuration.
- Step 3: Validate Results. Compare the automated output with manual gating on a small subset to ensure biological relevance. A strong correlation (e.g., r > 0.9) across key lymphocyte subsets has been demonstrated with validated AI tools [20].
Prevention: Establish a standard operating procedure (SOP) for data analysis that incorporates automated gating tools from the start of a project, especially for multi-operator or longitudinal studies [18].
Issue 2: Overwhelming Data Volume and Analysis Time
Problem: The massive data volumes from high-throughput or high-dimensional cytometry experiments make manual analysis too slow, creating a bottleneck.
Solution: Leverage computational tools for efficiency.
- Step 1: Utilize Dimensionality Reduction for Exploration. Use non-linear dimensionality reduction techniques like t-SNE or UMAP to visualize high-dimensional data in 2D or 3D plots. This allows for rapid exploratory analysis and identification of cellular heterogeneity with fewer plots [14] [19].
- Step 2: Employ Clustering for Population Identification. Apply clustering algorithms to simultaneously analyze multiple parameters across millions of cells. These algorithms can characterize and categorize diverse cell populations much faster than sequential manual gating [15].
- Step 3: Implement Automated Gating Pipelines. For routine analysis, use autogating pipelines that can be customized to robustly reproduce existing gating hierarchies. Once designed, the pipeline automatically adjusts gates for each sample, drastically reducing hands-on time [15].
Example Workflow: A clinical study using an AI-assisted workflow (DeepFlow) reduced the analysis time for each flow cytometry case to under 5 minutes, compared to the 10-20 minutes required for manual analysis [20].
Quantitative Comparison of Manual vs. Automated Gating
The table below summarizes key differences based on recent literature:
| Feature | Manual Gating | Automated Gating |
|---|---|---|
| Inherent Bias | High, depends on operator's knowledge [14] | Unbiased, based on mathematical algorithms [14] |
| Inter-Operator Variability | Can be as high as 25-78% [15] [16] | Minimal to none when the same parameters are used [16] |
| Analysis Time per Sample | 30 minutes to 1.5 hours [15] | Under 5 minutes for supervised AI tools [20] |
| Scalability with Dimensions | Poor; requires multiple biaxial plots, complexity increases quadratically [14] | Excellent; can efficiently visualize every marker simultaneously [14] |
| Discovery of Novel Populations | Limited by pre-defined gating strategy [16] | Enabled; can detect unexpected trends in the data [16] |
| Reproducibility | Low, difficult to replicate exactly [18] | High, analysis is fully objective and reproducible [18] |
Experimental Protocol: Validating an Automated Gating Tool
This protocol is adapted from a clinical validation study for an AI-assisted workflow [20].
Objective: To validate the performance of an automated gating algorithm against manual gating by expert hematopathologists as the gold standard.
Materials and Reagents:
- Biological Sample: Whole blood collected in EDTA tubes from 379 clinical cases.
- Staining Panel: A 3-tube, 10-color flow panel with 21 antibodies for immunodeficiency diseases (e.g., including CD3, CD4, CD8, CD19, CD45, TCRαβ, IgD).
- Key Equipment and Software:
- Navios flow cytometer (or equivalent) for data acquisition.
- Kaluza software (or equivalent) for manual gating and analysis.
- DeepFlow software (or other AI-based gating tool) for automated analysis.
Methodology:
- Sample Preparation:
- Process whole blood within 24 hours of collection.
- Lyse red blood cells using a lysing solution (e.g., from BD BioSciences).
- After centrifugation, resuspend the leukocyte pellet and divide it into three staining tubes.
- Incubate cells with fluorochrome-conjugated antibody panels for 15 minutes in the dark at room temperature.
- Acquire data on the flow cytometer, collecting a minimum of 100,000 events per tube.
Data Analysis - Manual Gating (Gold Standard):
- Transfer the raw data files (e.g., LMD files) to analysis software.
- A technologist performs manual gating to identify lymphocyte subsets (T-cells, B-cells, NK cells, and relevant subpopulations) following a standard laboratory procedure.
- The manual gating results are reviewed and confirmed by a hematopathologist. These final percentages for each cell subset are used as the ground truth.
Data Analysis - Automated Gating:
- Process the same raw data files using the automated gating software (e.g., DeepFlow).
- The software automatically imports the files, performs clustering, and generates a report with cell counts and percentages for all defined immune cell subsets.
Validation and Statistical Comparison:
- Divide the 379 cases into training, validation, and testing sets chronologically.
- Train the AI model on the training set using the manual gating results as labels.
- Compare the automated results from the testing set against the manual gating gold standard.
- Calculate the correlation coefficient (e.g., Pearson's r) for each major lymphocyte subset to quantify the agreement between the two methods. A strong correlation (r > 0.9) indicates successful validation.
Visualization of Analysis Workflows
The diagram below illustrates the key differences in steps and outcomes between manual and automated gating workflows.
Research Reagent Solutions
The table below lists essential materials and software tools used in automated gating experiments, as cited in the literature.
| Item | Function in Experiment | Example Tools / Reagents |
|---|---|---|
| Clustering Algorithm | Identifies groups of phenotypically similar cells in an unsupervised manner, defining cell populations without prior bias. | FlowSOM [17] [19], SPADE [14] [19], flowEMMi [18] |
| Dimensionality Reduction Tool | Reduces high-dimensional data to 2D/3D for visualization and exploratory analysis, helping to reveal cellular heterogeneity. | t-SNE, UMAP [14] [19], viSNE [19] |
| Supervised Auto-gating Software | Uses pre-gated data to train a model that automatically identifies and labels cell populations in new datasets, improving consistency. | DeepFlow [20], Cytobank Automatic Gating [19] |
| Panel Design Tool | Assists in designing multicolor antibody panels by minimizing spectral overlap and matching fluorophore brightness to antigen density. | FluoroFinder's panel tool [7] |
| Viability Dye | Distinguishes live from dead cells during gating to exclude artifacts caused by non-specific antibody binding to dead cells. | Amine-based live/dead dyes [7] |
The Impact of Data Quality on Downstream Analysis and Clinical Decision-Making
Data Quality Fundamentals for Researchers
What is the tangible impact of data quality on clinical decision support systems (CDSS)?
Poor data quality directly compromises the accuracy of clinical decision support systems. Since these systems rely on patient data to provide guidance, inaccuracies or incomplete information can lead to incorrect medical recommendations.
- Accuracy and Completeness Rates: Studies have shown that data accuracy in medical registries can be as low as 67%, while completeness rates can plummet to 30.7% [21].
- Impact on System Output: The effect of poor data quality is not always straightforward. In some cases, incorrect data (e.g., a male patient coded as a female under 50) may still lead to the same clinical output as correct data, but it follows an erroneous decision path. This makes errors in clinical logic harder to detect than a simple wrong output [21].
The table below summarizes how different data quality dimensions affect clinical and research analyses [21] [22]:
| Data Quality Dimension | Impact on Downstream Analysis & Clinical Decision-Making |
|---|---|
| Accuracy | Incorrect data can lead to false positives/negatives in cell population identification and erroneous clinical guidance [21] [22]. |
| Completeness | Missing data can prevent comprehensive analysis of cell subsets and skew patient stratification and treatment decisions [21] [22]. |
| Consistency | Inconsistent data entry (e.g., "Street" vs. "St") hampers data integration and matching, crucial for multi-center research and patient record reconciliation [22]. |
| Uniqueness | Duplicate patient records can lead to incorrect cohort definitions in research and misidentification of patients in clinical care, risking patient safety [22]. |
What are the core components of a data quality assessment framework?
A systematic, business-driven approach to data quality assessment is essential for ensuring data is "fit for purpose." This involves defining and measuring quality against specific dimensions [22].
- Fitness for Purpose: Data quality is assessed against the needs of specific business processes. For example, a dataset may be incomplete if it lacks the attributes needed to run an effective record-matching algorithm [22].
- Targets and Thresholds: Organizations should define the desired state (target) and the minimum acceptable level of quality (threshold) for each data attribute and dimension [22].
- Stakeholder Engagement: Data quality is a business responsibility, not just an IT function. Representatives from across the patient lifecycle must be engaged to define requirements and targets [22].
The following table provides an example of how targets and thresholds can be defined for a data quality assessment [22]:
| Dimension | Definition | Threshold | Target |
|---|---|---|---|
| Accuracy | Affinity of data with original intent; veracity as compared to an authoritative source. | 85% | 100% |
| Conformity | Alignment of data with the required standard. | 75% | 99.9% |
| Uniqueness | Unambiguous records in the data set. | 80% | 98% |
Troubleshooting Guides & FAQs for Experimental Data Quality
This section addresses common data quality issues encountered during experimental research, particularly in fields utilizing multi-parameter analysis like flow cytometry.
FAQ: During flow cytometry analysis, I am observing a weak fluorescence signal. What could be the cause?
A weak signal can stem from various issues in your sample preparation, panel design, or instrument setup [23].
- Potential Source: The antibody titer may be too dilute for your specific experimental conditions, even if it is validated for flow cytometry [23].
- Troubleshooting Steps:
- Titrate Antibodies: Perform a titration to determine the optimal concentration for your cell type and conditions [23].
- Match Fluorochrome to Antigen Density: Use bright fluorochromes for low-abundance (rare) proteins [23].
- Check Instrument Configuration: Verify that the correct laser and filter sets are used for your fluorochrome and that all lasers are properly aligned [23].
- Prevent Photobleaching: Protect samples from excessive light exposure, which can degrade fluorochromes, especially tandem dyes [23].
FAQ: My flow cytometry data shows high background fluorescence. How can I reduce it?
High background can obscure your true signal and is often related to sample viability, staining specificity, or compensation [23].
- Potential Source: Non-specific binding from dead cells or binding of the antibody's Fc region to Fc-receptors on cells [23].
- Troubleshooting Steps:
- Use Viability Dyes: Always include a viability dye (e.g., PI, 7-AAD) to identify and gate out dead cells, which bind antibodies non-specifically [23].
- Fc Receptor Blocking: Use an Fc receptor blocking reagent to prevent non-specific antibody binding [23].
- Increase Washes: Increase the volume, number, or duration of washes, particularly when using unconjugated primary antibodies [23].
- Review Compensation: Verify that compensation controls are brighter than the sample signal and that spillover spreading is not causing high background in adjacent channels [23].
FAQ: What are the best practices for gating in flow cytometry to ensure data quality?
Gating is a critical step that directly impacts the quality of your downstream analysis. A robust strategy is key to identifying a homogeneous cell population of interest [7].
- Start with Biology: Have a deep understanding of the expected cell size, granularity, and marker expression before you begin analysis [7].
- Use Appropriate Controls:
- Gating Strategy:
- Time Gate: Plot FSC or SSC against time to identify and exclude regions with acquisition problems like clogs or air bubbles [7].
- Singlets Gate: Use pulse geometry (e.g., FSC-H vs FSC-A) to exclude cell doublets and clumps [7].
- Loose Morphology Gate: Draw a relatively loose gate on FSC/SSC to isolate your main population of interest (e.g., lymphocytes) without unnecessarily excluding cells [7].
- Subset Gating: Use specific markers to further isolate the target cell population [7].
Experimental Protocols for Ensuring Phenotypic Data Quality
Protocol: A Standardized Workflow for High-Dimensional Phenotypic Data Analysis
This protocol outlines a methodology for analyzing highly multiplexed, single-cell-resolved tissue data, as implemented by tools like the multiplex image cytometry analysis toolbox (miCAT) [24]. This workflow ensures data quality from image processing through to the quantitative analysis of cell phenotypes and interactions.
- Principle: To comprehensively explore individual cell phenotypes, cell-to-cell interactions, and microenvironments within intact tissues by integrating image-based spatial information with high-dimensional molecular measurements [24].
- Applications: Defining molecular and spatial signatures in tissue biology, identifying clinically relevant features in disease, and investigating cellular "social networks" [24].
Step-by-Step Methodology:
Data Acquisition & Single-Cell Segmentation:
- Acquire highly multiplexed images of the tissue using a technology such as Imaging Mass Cytometry (IMC) or multiplexed immunofluorescence [24].
- Apply a segmentation mask to identify individual cells within the images. This process extracts for each cell:
- The abundance of all measured markers.
- Spatial features (e.g., cell size, shape).
- Environmental information (e.g., neighboring cells) [24].
Data Compilation & Integration:
- Compile the extracted single-cell data into a standard flow cytometry file format (.fcs). This allows for the use of both image analysis and high-dimensional cytometry analysis tools in a "round-trip" fashion [24].
- Link all single-cell information back to its spatial coordinates in the original image for parallel visualization and analysis [24].
Cell Phenotype Characterization:
- Supervised Analysis: Use dimensionality reduction tools like t-SNE to project the multi-marker data into two dimensions. Manually gate and annotate cell populations based on marker expression visualized on the t-SNE map [24].
- Unsupervised Analysis: Apply clustering algorithms (e.g., PhenoGraph) to identify distinct cell phenotypes without prior bias. This reveals shared phenotype clusters across images and clinical subgroups [24].
Spatial Interaction Analysis:
- User-Guided Neighborhood Analysis: Select a population of interest (e.g., CD68+ macrophages) and retrieve all cells that are touching or are proximal to it for further analysis [24].
- Unbiased Neighborhood Analysis: Use a permutation-based algorithm to systematically compare all observed cell-to-cell interactions in a tissue against a randomized control. This identifies interactions that occur more or less frequently than expected by chance, revealing significant cellular organization [24].
- Visualize significant interactions as heatmaps or "social networks" of cells specific to conditions like tumor grade [24].
Protocol: Automated Quality Control for Phenotypic Datasets Using PhenoQC
For large-scale genomic and phenotypic research, robust computational quality control is necessary. This protocol uses the PhenoQC toolkit to automate the process of making phenotypic datasets analysis-ready [25].
- Principle: To provide a high-throughput, configuration-driven workflow that unifies data validation, ontology alignment, and missing-data imputation [25].
- Applications: Preparing phenotypic data for reliable genotype-phenotype correlation studies in genomic research, saving manual curation time [25].
Step-by-Step Methodology:
Schema Validation:
Ontology-Based Semantic Alignment:
Missing-Data Imputation:
- Apply user-defined or state-of-the-art imputation methods to handle missing data. Available methods include:
- Traditional: Mean/Median/Mode.
- Machine Learning-based: K-Nearest Neighbors (KNN), Multiple Imputation by Chained Equations (MICE), Iterative SVD [25].
- The toolkit uses chunk-based parallelism for efficient processing of large datasets (up to 100,000 records) [25].
- Apply user-defined or state-of-the-art imputation methods to handle missing data. Available methods include:
Bias Quantification:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and tools used in the featured experiments and fields to ensure high-quality phenotypic data [23] [26] [24].
| Tool/Reagent | Function |
|---|---|
| Viability Dyes (e.g., PI, 7-AAD) | Distinguish live cells from dead cells to reduce non-specific background staining and false positives in flow cytometry [23] [7]. |
| Fc Receptor Blockers | Prevent non-specific binding of antibodies via Fc receptors, thereby reducing high background staining [23]. |
| Fluorescence-Minus-One (FMO) Controls | Critical controls for accurate gating in multicolor flow cytometry; help define positive and negative populations [23] [7]. |
| Panel Design Software (e.g., Spectra Viewer) | Tools to design multicolor panels by visualizing excitation/emission spectra, minimizing spillover spreading, and matching fluorochrome brightness to antigen density [23] [7]. |
| Human Phenotype Ontology (HPO) | A standardized vocabulary for phenotypic abnormalities, allowing consistent annotation and sharing of clinical data in resources like the Genome-Phenome Analysis Platform (GPAP) [26]. |
| Metal-Isotope Labeled Antibodies | Enable highly multiplexed protein measurement (40+ parameters) in tissues via mass cytometry (e.g., CyTOF) and Imaging Mass Cytometry (IMC) [12] [24]. |
| PhenoQC Toolkit | An open-source computational toolkit for automated quality control of phenotypic data, performing schema validation, ontology alignment, and missing-data imputation [25]. |
| miCAT Toolbox | An open-source computational platform for the interactive, quantitative exploration of single-cell phenotypes and cell-to-cell interactions in multiplexed tissue images [24]. |
Frequently Asked Questions (FAQs)
Q1: What is a LAIP, and why is it fundamental to immunophenotypic MRD assessment? A Leukemia-Associated Immunophenotype (LAIP) is a patient-specific aberrant phenotype used to identify and track residual leukemic cells. It is characterized by one or more of the following features [27]:
- Asynchronous antigenic expression: Co-expression of immaturity and maturity biomarkers (e.g., CD34/CD117 with CD15/CD11b).
- Aberrant lineage antigen expression: Expression of lymphoid antigens on myeloid cells (e.g., CD19, CD7, CD56).
- Antigen overexpression, reduction, or loss: Abnormal expression levels of antigens like CD123, CD33, CD13, or HLA-DR [27]. LAIPs are fundamental because they allow for the detection of one leukemic cell in 10,000 normal cells, providing a highly sensitive method for Measurable Residual Disease (MRD) monitoring in Acute Myeloid Leukemia (AML) [27] [28].
Q2: What is the difference between the "LAIP-method" and the "LAIP-based DfN-method"? These are two analytical approaches for MultiParameter Flow Cytometry (MFC)-MRD assessment [27]:
- The LAIP-method involves counting all cells within a patient-specific template created at diagnosis without further gating. It is specific but may not account for immunophenotypic shifts in the leukemic clone after therapy.
- The LAIP-based Different-from-Normal (DfN)-method involves further selecting only the cells that are positive for the LAIP-specific aberrant markers. This approach improves accuracy and comparability with molecular MRD techniques like RT-qPCR for NPM1 mutations [27]. The European LeukemiaNet (ELN) recommends using a combination of both approaches to leverage their respective advantages [27].
Q3: My gating strategy seems correct, but the MRD result is inconsistent with clinical findings. What could be wrong? Inconsistencies can arise from several sources related to LAIP quality and gating hierarchy [27]:
- Partial LAIP Expression: The most specific aberrant markers are often only partially expressed by the leukemic clone at diagnosis. Relying solely on these may miss a subset of residual cells.
- LAIP Instability: The immunophenotype of leukemic cells can shift between diagnosis and follow-up, causing the original LAIP template to become less effective.
- Operator Variability: Manual gating is subjective; differences in gate placement and strategy between operators or centers can lead to significantly different MRD results [28]. It is recommended to review your backgating hierarchy to visualize the population of interest within the context of its parent populations and confirm the gating logic [29].
Troubleshooting Guides
Issue 1: Low Specificity in MRD Detection
Problem: A high background of normal cells is obscuring the true MRD signal, leading to potential false positives.
Solution:
- Refine the LAIP: Focus on incorporating high-specificity aberrant markers, particularly aberrant lineage antigen expression (e.g., CD7, CD56), which are more robust for distinguishing leukemic cells from normal hematopoietic stem cells [27] [28].
- Employ the DfN Approach: Use the LAIP-based DfN-method, which actively selects for aberrant marker positivity, to improve the signal-to-noise ratio [27].
- Leverage Computational Tools: Consider machine learning algorithms (e.g., FlowSOM, CellCnn) that can perform high-dimensional, objective analysis to highlight rare, suspect leukemic clusters that might be missed manually [28].
Issue 2: High Variability in Manual Gating Results
Problem: MRD levels quantified by manual gating differ significantly between trained operators or repeated analyses.
Solution:
- Standardize the Gating Hierarchy: Implement a pre-defined, step-wise gating strategy that is consistently applied across all samples. The following table summarizes a generalized protocol [28]:
Table 1: Standardized Gating Protocol for AML MRD Assessment
| Step | Gating Action | Purpose | Key Markers (Example) |
|---|---|---|---|
| 1 | Select single cells | Remove doublets and cell aggregates | FSC-A vs. FSC-H |
| 2 | Identify viable nucleated cells | Remove debris and dead cells | Viability dye (e.g., DAPI-) |
| 3 | Gate blast population | Identify the lineage of interest | CD45 dim, SSC low |
| 4 | Apply patient-specific LAIP | Identify residual leukemic cells | Based on diagnostic aberrancies (e.g., CD34+/CD7+) |
- Implement a "Cluster-with-Normal" Pipeline: Use computational tools like FlowSOM to cluster cells and then compare follow-up samples to a reference of normal bone marrow. This objectifies the identification of aberrant populations [28].
- Review with Backgating: Use the backgating hierarchy view to visually explore your final gated population within its ancestral populations, ensuring the gates are logically and correctly placed [29].
Issue 3: Handling Samples with Complex Phenotypes or Rare Events
Problem: The leukemic population is phenotypically heterogeneous or present at a very low frequency, challenging the limits of detection.
Solution:
- Utilize High-Parameter Cytometry: If available, use spectral flow cytometry or mass cytometry (CyTOF). These technologies can measure 40+ parameters, allowing for a more granular dissection of complex phenotypes and better separation of rare cell populations from background [30].
- Apply Supervised Machine Learning: If a diagnostic sample is available, train a supervised classifier (e.g., k-Nearest Neighbors, Random Forest) on the diagnostic LAIP. This model can then be used to automatically find and classify phenotypically identical cells in follow-up samples, even at very low frequencies [28].
Experimental Protocols
Protocol: Validating MFC-MRD Results Against a Molecular Marker (NPM1 mutation)
This protocol outlines a method to validate and refine MFC-MRD assessment by comparing it with RT-qPCR for NPM1 mutations, a highly sensitive molecular benchmark [27].
1. Sample Collection and Preparation
- Collect bone marrow samples at diagnosis and post-treatment follow-up time points.
- Prepare mononuclear cells using standard Ficoll density gradient centrifugation.
- Split the sample for parallel analysis by MFC and RT-qPCR.
2. Multiparameter Flow Cytometry Analysis
- Staining: Stain ~1x10^6 cells with a pre-designed 8-color antibody panel. Include antibodies for standard blast identification (e.g., CD45, CD34) and a range of markers for LAIP identification (e.g., CD117, CD33, CD13, HLA-DR, CD7, CD56, CD4, CD15, CD123).
- Acquisition: Acquire a minimum of 500,000 events per sample on a flow cytometer to ensure sufficient sensitivity for rare event detection.
- Gating and Analysis: Perform sequential manual gating to identify the blast population. Apply both the LAIP-method and the LAIP-based DfN-method to quantify MRD.
3. Molecular MRD Assessment by RT-qPCR
- RNA Extraction and cDNA Synthesis: Extract total RNA from the parallel sample and synthesize cDNA.
- qPCR Amplification: Perform RT-qPCR using primers specific for the NPM1 mutation type identified at diagnosis.
- Quantification: Use a standard curve to quantify the copy number of the mutant NPM1 transcript, normalized to a control gene (e.g., ABL1). Report results as a percentage.
4. Data Correlation and Cut-off Determination
- Compare the MRD percentages obtained by the two MFC methods against the RT-qPCR results across all patient samples.
- Use statistical methods like Receiver Operating Characteristic (ROC) analysis to determine the optimal MFC-MRD cut-off that best discriminates between positive and negative molecular MRD results. Note that these cut-offs may differ based on therapy (e.g., 0.034% for intensive chemotherapy vs. 0.095% for hypomethylating agents) [27].
Diagram 1: MRD validation workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for MFC-MRD Assays
| Item | Function/Description | Example/Note |
|---|---|---|
| Multicolor Antibody Panels | To simultaneously detect multiple cell surface and intracellular antigens for LAIP identification. | Panels typically include CD45, CD34, CD117, CD33, CD13, HLA-DR, and a suite of lymphoid markers (CD7, CD56, CD19, etc.) [27] [28]. |
| Viability Dye | To distinguish and exclude dead cells during analysis, which can cause non-specific antibody binding. | e.g., DAPI, Propidium Iodide (PI), or fixable viability dyes. |
| Flow Cytometer | Instrument for acquiring multiparametric data from single cells in suspension. | Conventional (up to 60 parameters) or spectral flow cytometers (e.g., Cytek Aurora, Sony ID7000) offer enhanced parameter resolution [30]. |
| Normal Bone Marrow Controls | To establish a "different-from-normal" (DfN) baseline and understand the immunophenotype of regenerating marrow. | Essential for distinguishing true MRD from background hematopoietic progenitors, especially post-therapy [27]. |
| Computational Analysis Software | For automated, high-dimensional data analysis to reduce subjectivity and identify rare cell populations. | Tools include FlowSOM (clustering), UMAP/t-SNE (visualization), and supervised classifiers (e.g., kNN, Random Forest) [28]. |
Diagram 2: MFC-MRD core concepts
From Manual to Automated: A Landscape of Modern Gating Methodologies and Tools
FAQs and Troubleshooting Guides
Algorithm Selection and Performance
Q1: My cell classification model has high accuracy on training data but poor performance on new samples. What is the cause and how can I fix it?
A: This is a classic sign of overfitting.
- For k-Nearest Neighbors (kNN): This occurs when the value of
Kis too small (e.g., K=1). A model with K=1 considers only its nearest neighbor, making it highly sensitive to noise and outliers in your training data [31].- Solution: Use a validation set to find the optimal
K. Plot the validation error rate for different K values; the K with the lowest error is optimal. Typically, higher values of K create a smoother decision boundary and reduce overfitting [31].
- Solution: Use a validation set to find the optimal
- For Support Vector Machines (SVM): Overfitting can occur if the regularization parameter
Cis too high. A highCvalue tells the model to prioritize correctly classifying every training point, even if it requires creating a highly complex, wiggly decision boundary that may not generalize [32].
Q2: How do I handle high-dimensional mass cytometry data where the number of markers (features) far exceeds the number of cells (samples)?
A: This is a common challenge in immune monitoring studies.
- SVM is particularly well-suited for this scenario. Its effectiveness depends on the support vectors and the margin, not the dimensionality of the input space, making it robust against the "curse of dimensionality" [32]. It can achieve high accuracy even when the number of features is greater than the number of samples [32].
- kNN, conversely, often performs worse with high-dimensional data. In high-dimensional space, the concept of "nearest neighbors" can become less meaningful as the distance between all points becomes more similar, a phenomenon known as the "distance concentration" problem [34].
Q3: My dataset has significant batch effects from multiple experimental runs. How can I prevent my classifier from learning these artifacts?
A: Batch effects are a major confounder in large-scale studies.
- Data Preprocessing is Critical: Implement a robust data preprocessing pipeline to correct for batch effects before training your classifier. This includes normalization and batch correction algorithms. For cytometry data, tools and packages like
CytoNormare specifically designed for this purpose [35]. - Confounder-Correcting SVM (ccSVM): A specialized approach involves using a confounder-correcting SVM (ccSVM). This method modifies the standard SVM objective function to minimize the statistical dependence (e.g., using Hilbert-Schmidt Independence Criterion - HSIC) between the classifier's predictions and the confounding variables (like batch ID). This forces the model to base its predictions on features independent of the confounder [36].
Data Preprocessing and Experimental Design
Q4: Why is my kNN model's performance so poor, even after choosing a seemingly good K value?
A: kNN is a distance-based algorithm and is highly sensitive to the scale of your features [34].
- Cause: If the markers in your mass cytometry data are on different scales (e.g., CD3 expression ranging from 0-1000 vs. CD4 ranging from 0-50), the marker with the larger scale will dominate the distance calculation, and the model will be biased towards that feature.
- Solution: Always standardize your data before using kNN. Apply either Standard Scaler (which transforms data to have zero mean and unit variance) or Min-Max Normalization (which scales data to a fixed range, e.g., [0, 1]) [34]. This ensures all markers contribute equally to the distance metric.
Q5: How can I ensure my functional variant assay results are reliable and not due to clonal variation or experimental artifacts?
A: Employ a well-controlled experimental design like CRISPR-Select. This method uses an internal, neutral control mutation (WT') knocked into the same cell population as the variant of interest [37].
- Protocol: The frequencies of the variant and the WT' control are tracked relative to each other over time, space, or cell state. By using this paired, internal control, the method effectively dilutes out confounding effects from clonal variation, CRISPR off-target effects, and other experimental variables. The key is to calculate the absolute numbers of knock-in alleles to ensure results are based on a sufficient number of cells for statistical power [37].
Table 1: Comparison of kNN and SVM for Cell Classification Tasks
| Aspect | k-Nearest Neighbors (kNN) | Support Vector Machine (SVM) |
|---|---|---|
| Key Principle | Instance-based learning; class is determined by majority vote of the K nearest data points [34] [31] | Finds the optimal hyperplane that maximizes the margin between classes [36] [32] |
| Performance with High Dimensions | Poor; suffers from the curse of dimensionality [34] | Excellent; effective when features > samples [32] |
| Handling Noisy Data | Sensitive to irrelevant features and noise; requires careful feature selection and scaling [34] | Robust to noise due to margin maximization, but performance can degrade with significant noise [32] |
| Data Scaling Requirement | Critical; sensitive to feature scale, requires standardization [34] | Critical; performance improves with feature scaling [32] |
| Computational Load | High prediction time; must store entire dataset and compute distances to all points for prediction [34] [38] | High training time, especially for large datasets; but fast prediction [32] |
| Key Parameters to Tune | Number of neighbors (K), Distance metric (e.g., Euclidean, Manhattan), Weighting (uniform, distance) [31] [38] | Regularization (C), Kernel type (linear, RBF, etc.), Gamma (for RBF kernel) [32] [33] |
| Best Suited For | Smaller datasets, multi-class problems, data with low dimensionality after preprocessing [34] [31] | High-dimensional data (e.g., mass cytometry), data with clear margin of separation, complex non-linear problems (with kernel trick) [36] [32] |
Table 2: Troubleshooting Common Cell Classification Issues
| Problem | Potential Causes | Solutions |
|---|---|---|
| Poor Generalization (Overfitting) | kNN: K value too low [31].SVM: C parameter too high, leading to a complex model [32]. | Tune K and C using validation curves and cross-validation. For kNN, increase K. For SVM, decrease C. |
| Slow Model Training | kNN: N/A (training is trivial) [34].SVM: Dataset is too large; algorithm complexity is high [32]. | For SVM, use stochastic gradient descent solvers. For large datasets, consider linear SVMs or other algorithms. |
| Model Bias Towards Majority Cell Populations | Imbalanced class distribution in the training data [32]. | Use resampling techniques (oversampling minority classes, undersampling majority classes). Apply class weights in the SVM or kNN algorithm. |
| Inconsistent Results Across Batches | Strong batch effects confounding the model [36] [35]. | Apply batch effect correction (e.g., CytoNorm [35]). Use confounder-correcting algorithms like ccSVM [36]. |
Experimental Protocols
Protocol 1: kNN-Based Cell Population Classification from Mass Cytometry Data
This protocol details the steps for using kNN to classify cell populations in a standardized mass cytometry dataset.
Data Preprocessing and Normalization:
- Bead-Based Normalization: Use a tool like
CATALYSTto correct for instrument noise and signal drift over time [35]. - Transformations: Apply an arcsinh transformation with a cofactor of 5 to stabilize the variance of the cytometry data.
- Standardization: Standardize all marker expression values using Z-score normalization (Standard Scaler) to ensure no single marker dominates the distance calculation [34].
- Bead-Based Normalization: Use a tool like
Dimensionality Reduction and Feature Selection (Optional but Recommended):
- To mitigate the curse of dimensionality for kNN, reduce the number of features.
- Perform manual gating or use automated tools (
flowClean,flowDensity) to remove debris and dead cells [35]. - Use expert knowledge to select the most biologically relevant markers for the cell populations of interest.
Model Training and Hyperparameter Tuning:
- Split the preprocessed data into training (e.g., 70%) and test (e.g., 30%) sets, using stratification to maintain class distribution.
- Initiate the
KNeighborsClassifier. UseGridSearchCVwith 5-fold cross-validation on the training set to find the optimalK(e.g., range 1-25), the bestdistance metric(e.g., Euclidean, Manhattan), andweightingscheme (uniform or distance-based) [38].
Model Evaluation:
- Use the optimized model to make predictions on the held-out test set.
- Evaluate performance using accuracy, F1-score, and a confusion matrix. For a visual assessment, project the test set into a 2D space using UMAP and plot the decision boundaries.
Protocol 2: SVM for High-Dimensional Phenotypic Classification with Batch Effect Correction
This protocol leverages SVM's strength in high-dimensional spaces and incorporates steps to mitigate batch effects.
Data Preprocessing and Batch Integration:
- Follow the same initial preprocessing and normalization steps as in Protocol 1.
- Critical Step - Batch Correction: If the data comes from multiple batches or days, apply a batch correction algorithm like
CytoNormto align the distributions of the different batches [35].
Model Training with Confounder Correction:
- Split the batch-corrected data into training and test sets.
- Option A - Standard SVM: Use
GridSearchCVto tune theCparameter and, if using an RBF kernel, thegammaparameter [33]. - Option B - Confounder-Correcting SVM (ccSVM): If batch effects persist, consider a ccSVM implementation. This involves formulating the SVM optimization to include a term that minimizes the dependence between the learned model and the batch information, effectively forcing the model to ignore batch-related variance [36].
Validation and Interpretation:
- Validate the final model on the test set.
- For linear SVMs, you can examine the weight vector
wto determine which markers (features) were most influential in the classification. Techniques like Recursive Feature Elimination with SVM (SVM-RFE) can also be used to rank feature importance [33].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Cell Classification Experiments
| Item / Reagent | Function / Application in Context |
|---|---|
| CRISPR-Select Cassette | A set of reagents (CRISPR-Cas9, ssODN with variant, ssODN with WT' control) for performing highly controlled functional assays to determine the phenotypic impact of genetic variants (e.g., on cell state or proliferation) in their proper genomic context [37]. |
| Mass Cytometry Panel (Antibodies) | A panel of metal-tagged antibodies targeting specific cell surface and intracellular markers. These are the primary features used for cell classification and phenotyping in mass cytometry experiments [35]. |
| Normalization Beads | Beads impregnated with a known concentration of heavy metals. They are run alongside cell samples and are used to correct for instrument noise and signal drift during acquisition, which is a critical first step in data preprocessing [35]. |
| CATALYST R Package | An R package for the pre-processing of mass cytometry data. Its functions include bead-based normalization and sample debarcoding, which are essential for ensuring data quality before analysis [35]. |
| CytoNorm R Package | An R package designed specifically for batch effect normalization in cytometry data. It is crucial for integrating data from large-scale, multicenter, or multibatch studies [35]. |
| FlowSOM & UMAP | Dimensionality reduction and clustering tools. FlowSOM is used for high-speed clustering of cells, while UMAP provides a 2D visualization of high-dimensional data, both aiding in data exploration and analysis [35]. |
Workflow and Signaling Pathway Diagrams
kNN vs SVM Cell Classification Workflow
This diagram illustrates the logical flow and key decision points for choosing and applying kNN or SVM to a cell classification problem.
High-Dimensional Data Analysis Pipeline
This diagram details the specific workflow for processing high-dimensional cytometry data, highlighting critical quality control and batch correction steps.
Frequently Asked Questions (FAQs)
Q1: What are the primary strengths of FlowSOM and PhenoGraph? FlowSOM is renowned for its speed, scalability, and stability with large sample sizes. It performs well in internal and external evaluations and is relatively stable as sample size increases, making it suitable for high-throughput analysis [39] [40]. PhenoGraph is particularly powerful at identifying refined sub-populations and is highly effective at detecting rare cell types due to its graph-based approach [40].
Q2: How do I decide whether to use FlowSOM or PhenoGraph for my dataset? Your choice should balance the need for resolution, computational resources, and data size. The following table summarizes key decision factors:
| Consideration | FlowSOM | PhenoGraph |
|---|---|---|
| Primary Strength | Speed, stability, and handling of large datasets [40] | Identification of fine-grained and rare populations [40] |
| Clustering Resolution | Tends to group similar cells into meta-clusters; user-directed resolution [40] | Tends to split biologically similar cells; can over-cluster [41] [40] |
| Impact of Sample Size | Performance is relatively stable as sample size increases [40] | Performance and number of clusters identified can be impacted by increased sample size [40] |
| Best Use Case | Standardized, reproducible analysis pipelines; large datasets (>100,000 cells) [39] | Discovering novel or rare cell populations; datasets of at least 100,000 cells [41] |
Q3: Should I downsample my data before clustering? It is generally recommended to avoid downsampling whenever possible, as it can lead to the loss of rare cell populations [42]. If you must downsample, ensure you use a sufficient number of events (e.g., 100,000 cells) to maintain population diversity [41]. For large datasets, FlowSOM is a preferable choice as it can handle millions of events without requiring downsampling [42].
Q4: Is over-clustering or under-clustering better? Many experts recommend a strategy of intentional over-clustering, followed by manual merging of related clusters post-analysis. This is preferable to under-clustering, which can cause distinct populations to be grouped together and missed [42].
Q5: Why are my clustering results different each time I run PhenoGraph? PhenoGraph results can be highly sensitive to the number of input cells and the random seed used. For reproducible results with Rphenograph, always set a fixed random seed before running the analysis. The FastPG implementation, while faster, may not be fully deterministic and can produce variable results even with a fixed seed [41].
Troubleshooting Guides
Common FlowSOM Issues
Problem: FlowSOM analysis fails or runs very slowly. This is often due to the dataset exceeding memory limits.
- Solution: Check the event and channel limits on your platform (e.g., Cytobank). If you see a "data approaching memory limits" warning, try the following [43] [44]:
- Reduce the number of input events by sampling.
- Pre-gate your data to a population of interest (e.g., CD45+ cells) using the "Split Files by Population" feature to create a smaller, focused experiment [43].
- Ensure you are only selecting relevant phenotyping markers as clustering channels, excluding scatter, viability, and DNA content channels [44].
Problem: FlowSOM results contain too many very small clusters.
- Solution: The granularity of FlowSOM clusters is controlled by the
xdimandydimparameters (which define the grid size of the self-organizing map) and the final number of meta-clusters. Start with a smaller grid (e.g., 10x10) and a lower number of meta-clusters, then increase gradually to achieve the desired resolution [39] [44].
Problem: Unstable or unreliable clusters.
- Solution: This can occur if the Self-Organizing Map (SOM) is not sufficiently trained. Increase the
rlenparameter, which controls the number of training iterations. A higherrlen(e.g., 50-100) leads to more stable and reliable clustering outcomes [39].
Common PhenoGraph Issues
Problem: The number of clusters identified by PhenoGraph seems arbitrary and changes with settings.
The number of clusters (K) in PhenoGraph is highly dependent on the k parameter (nearest neighbors) and the total number of cells analyzed.
- Solution [42] [41]:
- Do not use a fixed
kvalue across all analyses. Optimize it for your specific dataset. - Use a sufficient number of cells as input (at least 100,000 is recommended).
- Use a strategy of over-clustering and then manually merge related clusters based on biological knowledge and marker expression patterns.
- Do not use a fixed
Problem: PhenoGraph splits a homogeneous population into multiple clusters.
- Solution: This is a known behavior of PhenoGraph. If a single biological population (e.g., naive T cells) appears as multiple clusters on a t-SNE plot, it is often appropriate to manually merge these clusters into one for downstream analysis [41].
Problem: PhenoGraph analysis takes too long.
- Solution: For large datasets, consider using the FastPG implementation, which offers a significant speed improvement. Be aware that FastPG may be less deterministic than the original Rphenograph [41].
General Clustering Issues
Problem: Algorithm fails (for FlowSOM, PhenoGraph, SPADE, viSNE).
- Solution [43]:
- Check file size: Files that are too large (in events or channels) are a common cause of failure. Reduce file size by pre-gating and using "Split Files by Population".
- Check FCS file keywords: Files not written with standard keywords can cause errors. Try re-writing the FCS files within your analysis platform.
- Check scaling: For algorithms like viSNE, ensure your data is transformed using arcsinh and not log scale.
Experimental Protocols & Workflows
Standardized Clustering Workflow for High-Dimensional Cytometry Data
The following diagram outlines a robust, generalized workflow for applying FlowSOM and PhenoGraph to mass or spectral flow cytometry data, ensuring data quality and analytical rigor.
Key Parameter Optimization
Optimal clustering requires careful parameter tuning. The table below summarizes critical parameters for FlowSOM and PhenoGraph, with guidelines for optimization based on your data and goals [39] [42] [41].
| Algorithm | Parameter | Function & Impact | Optimization Guideline |
|---|---|---|---|
| FlowSOM | xdim / ydim |
Controls the number of nodes in the primary SOM grid; influences granularity. | Start with 10x10. Increase (e.g., to 14x14) for finer resolution on complex datasets [39]. |
rlen |
Number of iterations for SOM training; impacts stability. | Default is 10. Increase to 50-100 for more stable, reliable clusters [39]. | |
Meta-cluster Number (k) |
Final number of consolidated cell populations. | Use a number that reflects biological expectation. Start low and increase, or over-cluster and merge [42]. | |
| PhenoGraph | k (nearest neighbors) |
Size of the neighborhood graph; dramatically affects cluster number and size. | Test values (e.g., 30, 50, 100). Use a higher k for larger datasets. Aim to over-cluster [42] [41]. |
| Random Seed | Ensures computational reproducibility. | Always set a fixed random seed before analysis for reproducible results [41]. | |
| Input Cell Number | The total number of cells analyzed. | Use at least 100,000 cells for stable results. Avoid downsampling when possible [41]. |
The following table details key computational tools and resources essential for implementing unsupervised clustering workflows in high-dimensional cytometry.
| Tool / Resource | Function | Role in Phenotypic Data Quality |
|---|---|---|
| Cytobank Platform | Web-based platform for cytometry data analysis. | Provides integrated environments to run FlowSOM, viSNE, and CITRUS, often with guided workflows and troubleshooting support [43] [44]. |
| R Programming Language | Open-source environment for statistical computing. | The primary platform for running algorithms like Rphenograph and FlowSOM via specific packages, enabling customizable and reproducible analysis pipelines [45] [39]. |
| FastPG | A high-speed implementation of the PhenoGraph algorithm. | Drastically reduces computation time for large datasets, though users should be aware of potential variability in results compared to the original algorithm [41]. |
| t-SNE & UMAP | Dimensionality reduction algorithms. | Not clustering methods themselves, but essential for visualizing the high-dimensional relationships and cluster structures identified by FlowSOM and PhenoGraph [45] [46]. |
| ConsensusClusterPlus | An R package for determining the stability of cluster assignments. | Often used in the meta-clustering step of FlowSOM to help determine a robust number of final meta-clusters [42]. |
This technical support center provides troubleshooting and guidance for researchers using BD ElastiGate Software, an automated gating tool for flow cytometry data analysis. ElastiGate addresses a key challenge in multi-parameter gating for phenotypic data quality research by using elastic image registration to adapt gates to biological and technical variability across samples [47] [48]. This document assists scientists in leveraging this technology to improve the consistency, objectivity, and efficiency of their flow cytometry workflows.
FAQ: Understanding BD ElastiGate
1. What is the core technology behind BD ElastiGate? BD ElastiGate uses a visual pattern recognition approach. It converts flow cytometry plots and histograms into images and then employs an elastic B-spline image registration algorithm. This technique warps a pre-gated training plot image to match a new, ungated target plot image. The same transformation is then applied to the gate vertices, allowing them to follow local shifts in the data [47] [49].
2. How does ElastiGate improve upon existing automated gating methods? Unlike clustering- or density-based algorithms (e.g., flowDensity), ElastiGate does not make assumptions about population shapes or rely on peak finding. It is designed to mimic how an expert analyst visually adjusts gates, making it particularly effective for highly variable data or continuously expressed markers where batch processing often fails [47] [48].
3. What are the main applications and performance metrics of ElastiGate? ElastiGate has been validated across various biologically relevant datasets, including CAR-T cell manufacturing, immunophenotyping, and cytotoxicity assays. Its accuracy, measured by the F1 score when compared to manual gating, consistently averages >0.9 across all gates, demonstrating performance similar to expert manual analysis [47] [50].
4. Where can I access and how do I install the BD ElastiGate plugin? The ElastiGate plugin is available for FlowJo v10 software. Installation involves downloading the plugin from the official FlowJo website, extracting the JAR file, and placing it in the FlowJo plugins folder. After restarting FlowJo, the plugin becomes available under the "Workspace > Plugins" menu [49].
5. Can ElastiGate handle all types of gates? ElastiGate supports polygon gates and linear gates for histograms. However, it converts ellipses into polygons and does not support Boolean gates [49].
Troubleshooting Guide
Common Issues and Solutions
| Problem Category | Specific Issue | Proposed Solution |
|---|---|---|
| Installation & Setup | Plugin not appearing in FlowJo. | Ensure the JAR file is in the correct plugins folder and rescan for plugins via FlowJo > Preferences > Diagnostics [49]. |
| Error when selecting target samples. | Confirm that target samples have the same parameters as the training files. Training files are automatically ignored as targets [49]. | |
| Gate Performance | Poor gate adjustment on sparse plots. | Lower the "Density mode" setting (e.g., to 0 or 1) to improve performance in low-density areas [49]. |
| Gate movement is too rigid. | Enable the "Interpolate gate vertices" option. This adds more vertices, allowing the gate to curve and follow data shifts more flexibly [49]. | |
| Gating fails when a population is missing in a target file. | Check the "Ignore non-matching populations" option. This uses a mask to focus registration only on populations present in both images [49]. | |
| Data Interpretation | High variability in gating results for a specific population. | Consult the validation data; populations with low event counts (e.g., intermediate monocytes) naturally have more variability. Manually review and adjust these gates if necessary [47]. |
Optimization Parameters Guide
The ElastiGate plugin offers several options to fine-tune performance for your specific data [49]:
- Density Mode (0-3): Use lower values (0,1) for sparse plots or when gate placement is determined by sparse areas. Use higher values (2,3) for dense populations.
- Interpolate Gate Vertices: Enable this for complex gate shapes to allow for more elastic deformation.
- Preserve Gate Type: Keep this checked to maintain rectangles and quad gates as their original type. Uncheck to convert them to more flexible polygons.
- Ignore Non-matching Populations: Essential for experiments where not all cell populations are present in every sample (e.g., FMO controls).
Experimental Protocols & Validation
The following table summarizes the experimental contexts in which BD ElastiGate has been rigorously validated, providing a benchmark for your own research.
| Experiment / Assay | Sample Type | Key Performance Metric (vs. Manual Gating) | Reference |
|---|---|---|---|
| Lysed Whole-Blood Scatter Gating | 31 blood-derived samples | Median F1 scores: Granulocytes (0.979), Lymphocytes (0.944), Monocytes (0.841) [47]. | [47] |
| Monocyte Subset Analysis | 20 blood samples | Median F1 scores >0.93 for most gates [47]. | [47] |
| Stem Cell Enumeration (SCE) | 128 samples (Bone Marrow, Cord Blood, Apheresis) | Median F1 scores >0.93, comparable to manual analysts [50]. | [50] |
| Lymphoid Screening Tube (LST) | 80 Peripheral Blood, 28 Bone Marrow | Median F1 scores >0.945 for most populations [50]. | [50] |
Detailed Protocol: Implementing ElastiGate for a Cell Therapy QC Assay
This protocol outlines the steps to use ElastiGate for quality control in cell therapy manufacturing, a common application cited in validation studies [47].
1. Training Sample Selection:
- Select one or more representative FCS files that have been meticulously gated by an expert according to your established gating strategy.
- Ensure the training files cover expected biological variability (e.g., different donors, processing conditions).
2. Plugin Setup in FlowJo:
- Open your workspace in FlowJo v10. Right-click on a fully gated training sample.
- Navigate to Workspace > Plugins > BD ElastiGate Plugin.
- In the dialog box, select all relevant training samples and the target (ungated) samples.
3. Gate and Parameter Selection:
- In the "Select the gates to export" section, choose the gates from your hierarchy that you wish to apply automatically.
- The plugin will display the parameters for the selected gate; verify they match the parameters in your target files.
4. Option Configuration for QC Data:
- Density Mode: Start with a setting of 2, as cell therapy products often form dense populations.
- Interpolate Gate Vertices: Enable this for non-rectangular gates to improve adaptability.
- Preserve gate type: Check this if you require final gates to be specific types (e.g., rectangles for reporting).
5. Execution and Result Verification:
- Click "Start" to run the plugin. The newly created gates will appear on your target files.
- Crucially, review all generated gates. While ElastiGate is highly accurate, manual confirmation is recommended, especially for critical QC thresholds. Gates can be manually adjusted as needed.
Visual Workflows
ElastiGate Gating Workflow
The diagram below illustrates the core automated gating process of the BD ElastiGate algorithm.
Gating Strategy for Cell Phenotyping
This diagram outlines a simplified, generalized gating hierarchy for deep cell phenotyping, a context where ElastiGate is frequently applied.
The Scientist's Toolkit: Essential Research Reagent Solutions
For researchers implementing high-parameter flow cytometry panels for phenotypic analysis, the following reagent and instrument portfolio is essential. This table details key solutions that integrate with the ElastiGate ecosystem.
| Tool / Reagent Category | Key Examples | Function in Phenotypic Data Quality Research |
|---|---|---|
| Flow Cytometry Instrumentation | BD FACSDiscover S8 Cell Sorter, BD FACSLyric Systems | Generates high-parameter data; BD FACSLyric systems can integrate ElastiGate for standardized, automated analysis [51]. |
| Analysis Software | FlowJo Software, BD FACSuite Application | The primary platform for data analysis; hosts the ElastiGate plugin and provides advanced computational tools [51]. |
| Reagent Portfolio | BD Horizon Brilliant, RealYellow, RealBlue Dyes, BD OptiBuild | A broad portfolio of over 9,000 reagents enables complex panel design. Fluorochromes are engineered for reduced spillover, optimizing resolution and data quality [51]. |
| Single-Cell Multiomics | BD Rhapsody HT System, BD AbSeq Assays | Allows simultaneous analysis of protein and mRNA from single cells, providing deeper insights into cell function and phenotype [51]. |
Technical Support Center
Troubleshooting Guides & FAQs
Model Training & Convergence
Q: My deep learning model is training very slowly. What could be the cause and how can I improve it?
A: Slow training can arise from several factors. Solutions include using Mini-batch Gradient Descent to speed up the process, parallelizing the training across multiple GPUs, and employing distributed training across multiple machines [52]. Furthermore, advanced optimizers like Adam, which combines the benefits of momentum and adaptive learning rates, can lead to faster convergence [53].
Q: During training, my model's loss becomes NaN (Not a Number). What is the typical cause and how can I fix it?
A: This is a common sign of numerical instability [54]. It can often be traced back to using an exponent, log, or division operation in your code [54]. To mitigate this, use built-in functions from your deep learning framework (e.g., TensorFlow, PyTorch) for these operations, as they are typically numerically stable [54]. Additionally, normalizing your inputs (e.g., scaling pixel values to [0,1]) can help stabilize training [54].
Q: What is a fundamental debugging step to ensure my model implementation is correct?
A: A highly effective heuristic is to overfit a single batch of data [54]. This involves trying to drive the training error on a very small batch (e.g., 2-4 examples) arbitrarily close to zero. If your model cannot overfit this small batch, it is a strong indicator of a bug in your model, such as an incorrect loss function or data preprocessing error [54].
Data Quality & Preprocessing
Q: My model performs well on training data but poorly on unseen validation data. What is happening?
A: This is a classic sign of overfitting [52]. Your model has learned the training data too well, including its noise, and fails to generalize. To address this:
- Apply regularization: Use L1 or L2 regularization to penalize large weights in the model [52].
- Use Dropout: Randomly "drop out" a proportion of neurons during training to prevent the network from becoming overly reliant on any single neuron [52].
- Implement Early Stopping: Halt the training process when the validation loss stops improving for a predetermined number of epochs [52].
- Apply Data Augmentation: Artificially increase the size and diversity of your training set by creating modified versions of your existing data through transformations like rotation, scaling, and flipping [52].
Q: How does the quality and size of my dataset impact model performance?
A: Data is critical, and common mistakes include using low-quality or improperly sized datasets [55].
- Low-Quality Data: Data with missing values, significant noise (outliers), or that is not representative of the real-world problem will lead to poor and unreliable models [55]. It is imperative to invest time in data cleaning and exploration.
- Dataset Size: A dataset that is too small can lead to overfitting, while one that is excessively large relative to model complexity can lead to underfitting [55]. There is a "sweet spot" where the dataset is large enough for the model to learn from but not so large that it becomes computationally infeasible to train [55].
Model Selection & Architecture
Q: For a new problem, what is a recommended strategy for selecting a model architecture?
A: When starting on a new problem, it is best to start with a simple architecture [54].
- For image-like data, begin with a simple Convolutional Neural Network (CNN) like LeNet [54].
- For sequence data, start with a single-layer LSTM or temporal convolutions [54].
- For other tasks, a fully-connected network with one hidden layer is a good starting point [54]. This approach allows for faster implementation and debugging. You can later transition to more complex, proven architectures (e.g., ResNet for images, Transformers for sequences) as your project matures [54].
Q: Should I use the same model for every task and dataset?
A: No. Using a single model repeatedly is a common mistake [55]. Training multiple model variations on different datasets provides statistically significant data and valuable insights. Different models may capture different patterns, and this variety can lead to more robust and generalizable findings [55].
Optimizer Comparison Table
The table below summarizes common optimizers used in deep learning to minimize the loss function. Choosing the right one depends on your specific problem, data, and resources.
| Optimizer | Key Advantages | Common Disadvantages |
|---|---|---|
| SGD | Simple and easy to implement [53] | Slow convergence; requires careful tuning of learning rate [53] |
| Mini-Batch SGD | Faster training than SGD [53] | Computationally expensive; can get stuck in local minima [53] |
| SGD with Momentum | Faster convergence; reduces gradient oscillations and noise [53] | Requires tuning of the momentum coefficient (β) [53] |
| AdaGrad | Adapts learning rate for each parameter, good for sparse features [53] | Learning rate can decay too aggressively, slowing convergence [53] |
| RMSProp | Prevents the rapid decay of learning rates seen in AdaGrad [53] | Computationally expensive due to an additional parameter [53] |
| Adam | Fast convergence; combines benefits of Momentum and RMSProp [53] | Memory-intensive; computationally expensive [53] |
The Scientist's Toolkit: Research Reagent Solutions
This table details key computational "reagents" and their functions for experiments involving CellCnn and Transformer models on high-dimensional phenotypic data.
| Item | Function / Explanation |
|---|---|
| CellCnn | A representation learning approach based on convolutional neural networks to identify rare disease-associated cell subsets from high-dimensional single-cell data (e.g., mass cytometry) [56]. |
| Transformer Model | A neural network architecture based on a multi-head self-attention mechanism. It processes entire sequences in parallel, effectively capturing long-range dependencies, and is the foundation for modern large language models [57] [58]. |
| Multi-Head Self-Attention | The core mechanism of the Transformer. It allows the model to weigh the importance of different parts of the input sequence when processing a specific element, capturing diverse contextual relationships [57] [58]. |
| PIXANT | A multi-phenotype imputation method using a mixed fast random forest algorithm. It accurately imputes missing phenotypic values in large biobank datasets (e.g., UK Biobank) by leveraging correlations between traits, thereby enhancing the power of downstream GWAS [59]. |
| Rule-Based Phenotyping Algorithms | Carefully crafted rules (e.g., using ICD codes, medications, lab values) to define disease cohorts from Electronic Health Records (EHR). High-complexity algorithms that integrate multiple data domains improve the accuracy of GWAS cohorts and results [60]. |
Experimental Protocols & Workflows
Detailed Protocol: Identifying Rare Cell Subsets with CellCnn
CellCnn is designed to detect rare cell populations associated with a phenotype from high-dimensional single-cell data [56].
- Input Preparation: The input is a set of multi-cell populations (e.g., patient blood samples), where each sample is associated with a phenotype (e.g., disease status, survival time). Each cell is measured across multiple markers (e.g., 20+ proteins via mass cytometry) [56].
- Convolutional Filtering: The model uses a convolutional neural network adapted for unordered sets of cells. It learns molecular profile "filters" that strongly respond to phenotype-associated cells [56].
- Pooling (Max or Mean): The network uses a pooling layer (max or mean) for each filter. Max-pooling measures the presence of cells with high filter response, while mean-pooling approximates the frequency of the responsive cell subset [56].
- Output Prediction: The pooling layer is connected to an output layer that predicts the sample-associated phenotype. Network training optimizes the filter weights to match the true phenotypes [56].
- Post-hoc Analysis: After training, cells with high response to a filter can be clustered (e.g., density-based clustering) to identify distinct cell types. Marker importance is determined by comparing the abundance distribution between the selected cells and the whole population [56].
Detailed Protocol: Transformer Model for Sequence Data
Transformers process sequential data using a self-attention mechanism [57] [58].
- Embedding: The input text is tokenized and converted into vector embeddings. Positional encodings are added to these embeddings to provide information about the order of tokens [57].
- Transformer Block Processing: The embedded sequence is processed through a stack of Transformer blocks. Each block contains:
- Multi-Head Self-Attention: The input is projected into Queries, Keys, and Values. The self-attention mechanism calculates a weighted sum of Values for each token, where the weights are based on the compatibility between its Query and all Keys. Multiple heads allow the model to focus on different representation subspaces [57].
- Multi-Layer Perceptron (MLP): A feed-forward network is applied independently to each token to further refine its representation [57].
- Output Generation: The final output from the Transformer blocks is passed through a linear layer and a softmax function to produce a probability distribution over the vocabulary for the next token [57].
Workflow & Architecture Visualizations
CellCnn Analysis Workflow
Simplified Transformer Architecture
Frequently Asked Questions (FAQs)
Q1: What is the fundamental purpose of gating in flow cytometry? Gating is a data reduction technique that involves selecting a specific subset of events from all data collected for further analysis [61]. It is used to isolate target cell populations based on characteristics like size, granularity, and marker expression, while excluding unwanted events such as debris, dead cells, or cell clumps [62] [63]. This process is essential for cleaning data and accurately identifying the cells of interest.
Q2: In what order should I apply gates to my data? A logical, hierarchical sequence is recommended for robust and reproducible analysis [63]. A widely accepted strategy involves these steps [61]:
- Flow stability gating: Remove data collected while the instrument's flow was unstable.
- Pulse geometry gating: Exclude doublets or cell clumps to ensure single-cell analysis.
- Forward and side scatter gating: Remove debris and non-cellular events based on size and complexity.
- Subsetting gating: Use fluorescence markers, viability dyes, and "dump" channels to define the target cell population.
- Backgating: Visualize the final gated population on previous plots (like FSC vs. SSC) to validate that no desired cells were unintentionally excluded.
Q3: What are the most common errors in gating, and how can I avoid them? Common pitfalls include over-gating, fluorescence spillover, and missing doublets. The table below summarizes these issues and their solutions.
Table: Common Gating Errors and Solutions
| Common Error | Impact on Data | Recommended Solution |
|---|---|---|
| Over-gating | Loss of legitimate cell events, skewed results [63] | Use backgating to verify population distribution; keep initial scatter gates generous [61] [63] |
| Fluorescence Spillover | False-positive signals, inaccurate population definitions [63] | Recalibrate compensation using single-stained controls; use Fluorescence Minus One (FMO) controls [61] [63] |
| Incomplete Doublet Removal | Distorted fluorescence intensity and population statistics [61] [63] | Strictly apply pulse geometry gating (e.g., FSC-A vs. FSC-W or FSC-H) [62] [63] |
| Inconsistent Gating | Poor reproducibility and unreliable data across samples [63] | Use standardized FMO controls and align gates using biological references [63] |
Q4: How do I define positive and negative populations for a marker, especially in complex panels? Using appropriate controls is non-negotiable. Fluorescence Minus One (FMO) controls are critical for this [61] [63]. An FMO control contains all the fluorochromes in your panel except one, helping you determine the spread of signal in a specific channel due to spillover from all other dyes. This allows you to set accurate, unbiased gates for positive and negative populations, particularly for dimly expressed markers or in high-parameter panels [61].
Q5: How is modern technology like AI and mass cytometry changing gating strategies? New technologies are making gating more automated, reproducible, and high-dimensional.
- AI-Powered Gating: Machine learning platforms (e.g., in FlowJo, OMIQ, Cytobank) can be trained on expertly gated samples to automatically replicate the gating strategy on new datasets, drastically reducing analysis time and subjective variability [64]. Deep learning models like GateNet can gate millions of events in seconds with human-level accuracy [64].
- Mass Cytometry (CyTOF): This technology uses metal-tagged antibodies and time-of-flight mass spectrometry, virtually eliminating spectral spillover [12]. This allows for the simultaneous measurement of over 40 parameters without compensation concerns, enabling deep phenotyping of complex cell populations that would be challenging with conventional flow cytometry [12] [24]. Analysis then heavily relies on automated clustering algorithms (e.g., PhenoGraph, FlowSOM) to identify cell populations in the high-dimensional space [24].
Troubleshooting Guides
Problem 1: Poor Separation Between Positive and Negative Populations
Potential Causes and Step-by-Step Solutions:
Check Panel Design and Antibody Titration:
- Cause: Inadequate antibody concentration or excessive spectral overlap due to suboptimal fluorochrome pairing.
- Solution: Re-titrate antibodies to achieve optimal staining index. Re-evaluate your panel design using tools like FluoroFinder to ensure fluorochromes are matched to marker abundance and instrument capabilities [62].
Verify Compensation:
- Cause: Uncorrected fluorescence spillover is spreading the negative population into the positive channel.
- Solution: Generate fresh single-stained compensation controls using beads or cells. Ensure compensation matrices are correctly calculated and applied in your analysis software [63]. Algorithms like AutoSpill can automate this process [64].
Employ FMO Controls:
Assess Instrument Performance:
- Cause: Poor laser alignment or PMT sensitivity.
- Solution: Run calibration beads regularly to ensure instrument optics and fluidics are performing optimally. Fine-tune PMT voltages to place the negative population correctly on the axis [63].
Problem 2: High Background or "Sticky" Cells
Potential Causes and Step-by-Step Solutions:
Increase Viability Staining Stringency:
Implement a "Dump" Channel:
- Cause: Unwanted cell types are contributing to non-specific background.
- Solution: In a complex mixture like PBMCs, use a channel to "dump" or exclude cells not of interest. For a T-cell analysis, you could combine antibodies for CD19 (B cells), CD14 (monocytes), and CD56 (NK cells) into a single, bright channel and exclude these cells from your analysis [61].
Optimize Staining Protocol:
- Cause: Non-specific antibody binding.
- Solution: Include an Fc receptor blocking step. Titrate antibodies to use the minimum required concentration. Wash cells thoroughly with a buffered solution containing protein (e.g., BSA) after staining.
Problem 3: Low Cell Yield After Gating
Potential Causes and Step-by-Step Solutions:
Apply Backgating:
Revisit Doublet Discrimination:
- Cause: The singlets gate is too narrow, excluding genuine single cells.
- Solution: Check the FSC-A vs. FSC-H/W plot and adjust the gate to encompass the main diagonal population where single cells reside, ensuring you are not unnecessarily excluding events [62].
Check for Sample Preparation Issues:
- Cause: Excessive cell death or mechanical damage during processing.
- Solution: Standardize your tissue dissociation or cell isolation protocol to minimize stress and ensure high cell viability from the start.
Experimental Protocols for Data Quality
Protocol 1: Hierarchical Gating for Immunophenotyping
Objective: To identify and quantify specific immune cell subsets (e.g., CD4+ T cells) from peripheral blood mononuclear cells (PBMCs) with high data quality.
Table: Essential Reagents for Immunophenotyping
| Reagent | Function | Example |
|---|---|---|
| Viability Dye | Distinguishes live from dead cells to reduce background. | Propidium Iodide (PI), 7-AAD [63] |
| Lineage Marker Antibodies | Identifies major cell lineages for population isolation. | CD3 (T cells), CD19 (B cells), CD14 (Monocytes) [63] |
| Subset Marker Antibodies | Defines specific functional subsets within a lineage. | CD4 (Helper T cells), CD8 (Cytotoxic T cells) [63] |
| "Dump" Channel | Combines markers for unwanted lineages into one bright channel to exclude them. | CD14, CD19, CD56 combined in one fluorochrome [61] |
| FMO Controls | Determines positive/negative boundaries for each marker. | All antibodies minus one, for each marker [61] |
Methodology:
- Acquisition: Run samples on the flow cytometer and collect at least 100,000 events per sample for meaningful statistics.
- Gating Hierarchy:
- Step 1: Cells of Interest. On an FSC-A vs. SSC-A plot, draw a gate (P1) around the lymphocyte population based on size and granularity [62].
- Step 2: Single Cells. On an FSC-A vs. FSC-H plot, draw a gate (P2) on the diagonal population to exclude cell doublets [62] [61].
- Step 3: Live Cells. From P2, plot the viability dye vs. SSC-A. Gate on the viability dye-negative population (P3) to select live cells [62] [63].
- Step 4: Leukocytes. From P3, plot CD45 vs. SSC-A. Gate on CD45-positive events (P4) to isolate all nucleated hematopoietic cells [63].
- Step 5: Lineage and Subset. From P4, use a series of fluorescence plots to progressively narrow down the population:
The following workflow diagram illustrates this sequential gating strategy:
Protocol 2: Automated Gating and Clustering for High-Dimensional Data
Objective: To analyze complex, high-parameter (e.g., >15-color) flow or mass cytometry data in an unbiased, reproducible manner using computational tools.
Methodology:
- Data Preprocessing: Export your data in Flow Cytometry Standard (FCS) format. Use automated algorithms like FlowAI or FlowClean to perform quality control, flagging and removing anomalies from the data [64].
- Dimensionality Reduction: Transform the high-dimensional data into a 2-dimensional map for visualization. Common algorithms are:
- Unsupervised Clustering: Apply algorithms to automatically identify cell populations without manual gating.
- Validation and Annotation: Manually review the resulting clusters by assessing their marker expression profiles. Annotate clusters based on known biology (e.g., "CD4+ T cells," "B cells," "monocytes"). The relationship between raw data, analysis, and validation is shown below:
The Scientist's Toolkit
Table: Key Research Reagent Solutions and Materials
| Item | Function in Gating Strategy | Specific Example |
|---|---|---|
| Viability Dyes | Critical for excluding dead cells that cause nonspecific binding and background noise [63]. | Propidium Iodide (PI), 7-AAD [63] |
| Compensation Controls | Essential for calculating spillover matrix to ensure signal purity in each detector [63]. | Single-stained beads or cells for each fluorochrome in the panel. |
| FMO Controls | Gold standard for accurately setting positive/negative gates, especially for dim markers or in crowded spectral areas [61] [63]. | Sample stained with all antibodies except one. |
| Ultra-compense Antibodies | Designed for complex panels, they minimize spontaneous fluorescence and offer bright, clean signals for better population separation. | Multiple commercial suppliers offer "super bright" or "ultra-compense" conjugates. |
| Automated Gating Software | Provides reproducible, high-throughput analysis by applying machine-learned or pre-defined gating templates, reducing inter-operator variability [64]. | OMIQ, Cytobank, FlowJo Plugins [64]. |
| Clustering Algorithms | Enable unbiased discovery of novel cell populations in high-dimensional data without manual gating [24]. | PhenoGraph, FlowSOM [64] [24]. |
Optimizing Your Pipeline: Troubleshooting Common Gating Challenges and Improving Performance
Frequently Asked Questions
Why is a clearly defined research question even more critical for high-dimensional cytometry? High-dimensional panels allow the measurement of many parameters, which can lead to the temptation to include as many markers as possible without a clear purpose. A poorly defined question can result in noisy data, the inability to set boundaries for what constitutes a "real" cell population, and difficulty in determining significant differences between test groups. A specific research question guides appropriate experimental design and analysis, ensuring data quality and relevance [65].
My traditional serial gating strategy is becoming unmanageable. What's the alternative? High-dimensional cytometry requires a shift in analysis thinking. Manually gating through more than 40 parameters is impractical. Instead, researchers are encouraged to use computational tools that group similar cells together based on all markers simultaneously. Techniques like clustering and dimensionality reduction (e.g., t-SNE) allow for a global, unbiased view of cell populations and their relationships [65].
How can I validate my gating strategy when moving to a high-dimensional panel? Even with high-dimensional data, incorporating biological knowledge through a preliminary gating strategy is essential. To study a specific population, you should have a fool-proof way to define what it is and what it is not. Furthermore, using Fluorescence Minus One (FMO) controls in multicolor experiments is critical to resolve ambiguous populations and accurately set positive/negative boundaries for markers [66].
A major challenge is the technical variance between samples. How can this be managed? Technical and biological variance can cause cell populations to shift location and shape between samples, making consistent automated analysis difficult. Computational frameworks like UNITO are being developed to address this. By transforming protein expression data into bivariate density maps and using image-based segmentation, these tools can learn gating patterns from human annotations and robustly apply them to new data, adapting to this inherent variance [67].
What are the best visualization methods for understanding high-dimensional data? Since we cannot easily visualize beyond three dimensions, several plot types are commonly used to explore high-dimensional cytometry data:
- Parallel Coordinates Plots: Show how each variable contributes to the data and help detect trends across parameters [68].
- Trellis Charts (Faceting): Display smaller plots in a grid to visualize the structure of complex data across different conditions or cell types [68].
- t-SNE and UMAP: These are dimensionality reduction techniques that project high-dimensional data into a 2D or 3D map where distances between points reflect their phenotypic similarity [65].
Troubleshooting Common Experimental Issues
| Problem | Possible Cause | Solution |
|---|---|---|
| Poor population resolution in fluorescence plots | Spectral overlap (spillover) between fluorochromes not properly compensated [66]. | - Use single-stained controls (e.g., capture beads or cells) for each fluorophore [69].- Recalibrate compensation matrix on the flow cytometer software [66]. |
| High background or false positives | Overlap in fluorescence emission spectra; overly broad antibody panels without proper controls [65] [66]. | - Implement FMO controls to set accurate boundaries for positive signals [66].- Re-titrate antibodies to optimize signal-to-noise ratio [65]. |
| Inconsistent gating across samples | Technical variance from sample prep or instrument changes shifting population locations [67]; manual gating bias. | - Use automated gating tools (e.g., FlowSOM, UNITO) for objective, reproducible analysis [67] [70].- Align gates using stable biological reference populations (e.g., lymphocytes in blood) [66]. |
| Inability to identify known cell populations | Panel design does not include key lineage markers for clear population definition [65]. | - Incorporate well-validated, high-quality lineage markers in the panel to create a "fool-proof" initial gating strategy [65].- Use backgating to confirm that gated populations align with expected physical parameters (FSC/SSC) [66]. |
| Low cell yield after sequential gating | Over-gating, leading to excessive exclusion of events [66]. | - Use backgating to verify population distribution and ensure gates are not overly restrictive [66].- Review the gating hierarchy to ensure debris and doublets are effectively removed early on [66]. |
Experimental Protocols for Robust Panel Design and Validation
Protocol 1: Panel Design and Antibody Conjugation This protocol outlines the initial steps for building a high-dimensional panel, from marker selection to antibody preparation.
- Define Research Question & Preliminary Gating: Start with a specific biological question. Plan a serial gating or selection strategy that directs the analysis toward the answer. This includes defining key lineage markers for inclusion and exclusion of cell types [65].
- Fluorophore Selection: Choose fluorophores matched to your instrument's lasers and filters. Prioritize bright fluorophores for low-abundance antigens and dim fluorophores for highly expressed markers. Maximize the use of spatially separated lasers to minimize spectral overlap [69].
- Antibody Titration: For each antibody, perform a titration experiment using target cells to determine the concentration that provides the best signal-to-noise ratio. Avoid using excess antibody, which can increase background [65].
- Single-Stained Control Preparation:
- Completely resuspend compensation capture beads and negative beads by vortexing [69].
- Add one drop of capture beads to a series of tubes [69].
- Add a pre-titrated amount of each conjugated antibody to its respective tube, ensuring the antibody is mixed directly into the bead suspension [69].
- Incubate for 15 minutes at room temperature, protected from light [69].
- Wash beads by adding 3 mL of PBS, centrifuging, and decanting the supernatant. Resuspend in 0.5 mL of PBS [69].
- Add one drop of negative beads to each tube and vortex before analysis [69].
Protocol 2: Staining, Fixation, and Permeabilization for Surface and Intracellular Markers This detailed methodology is adapted from a 10-color immunophenotyping protocol for mouse splenocytes [69].
- Cell Preparation: Pipette 100 μL (approximately 1 x 10^6 cells) of thoroughly mixed splenocytes into a conical tube [69].
- Surface Staining: Add antibodies against surface antigens to the cell pellet as per manufacturer's instructions. Mix gently and incubate for 15 minutes at room temperature (22 ± 3°C) in the dark [69].
- Wash: Centrifuge tubes for 5 minutes at 300 x g. Carefully remove the supernatant [69].
- Fixation and Permeabilization: Resuspend the cells in 100 μL of PBS or sheath fluid. Add 1 mL of 1X Fixation/Permeabilization solution (e.g., from a Foxp3/Transcription Factor Staining Buffer Kit) and vortex briefly. Incubate for 30–60 minutes at room temperature or 4°C [69].
- Wash: Add 2 mL of 1X Permeabilization Wash Buffer, vortex, centrifuge, and decant the supernatant [69].
- Intracellular Staining: Resuspend the cell pellet in 100 μL of 1X Wash Buffer. Add the antibody specific to the intracellular target (e.g., Foxp3), vortex, and incubate for 30–60 minutes at 4°C [69].
- Final Wash: Add 2 mL of 1X Wash Buffer, vortex, centrifuge, and decant the supernatant [69].
- Resuspension and Acquisition: Resuspend the final cell pellet in an appropriate volume of flow cytometry staining buffer (e.g., PBS with 1% BSA). Acquire data on the flow cytometer, collecting a preferred number of events (e.g., 10,000) [69].
Protocol 3: Automated Gating Validation with UNITO Framework This protocol describes how to use a modern computational framework for automated, human-level gating.
- Training Data Preparation: Manually gate 30–40 cytometry samples to establish a robust ground truth. Define the hierarchical gating structure for all cell populations of interest [67].
- Data Preprocessing: Normalize protein expression values to a fixed range (e.g., [0, 100]). Convert the normalized expression data for each pair of markers into a 2D density plot [67].
- Mask Generation: Use the manual gate annotations to generate a binary mask overlay for each density plot, representing the "ground truth" cell population. Apply convex hull processing to fill any empty spaces within the mask [67].
- Model Training: Feed the pairs of density plots and binary masks into the UNITO model. The model learns the pattern of gating for each specific cell population in the hierarchy [67].
- Inference on New Data: For new, unseen samples, UNITO processes the density plots and outputs a predicted binary mask for each gate. The framework then translates this mask back into single-cell classification results [67].
- Validation: Compare UNITO's results to a consensus of manual gates from multiple experts. The framework has been shown to deviate from human consensus by no more than any individual human expert [67].
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function |
|---|---|
| Flow Cytometer with Multiple Lasers | Instrument platform for detection; configurations with 4 lasers and 16 detection channels enable complex 10+-color immunophenotyping [69]. |
| Metal-Labeled Antibodies (Mass Cytometry) | Antibodies conjugated to stable elemental isotopes; allow for measurement of >40 parameters with minimal signal spillover [65]. |
| Fluorophore-Labeled Antibodies | Antibodies conjugated to fluorescent dyes (e.g., FITC, PE, APC); used for antigen detection in flow cytometry. Brightness and laser compatibility are key selection factors [69]. |
| Viability Dye (e.g., PI, 7-AAD) | Distinguishes live cells from dead cells; dead cells with compromised membranes are permeable to the dye and exhibit high fluorescence [66]. |
| Fixation/Permeabilization Buffer Kit | Chemical solutions that preserve (fix) cells and make the membrane permeable, allowing staining of intracellular (e.g., cytokines) and nuclear (e.g., transcription factors) proteins [69]. |
| Compensation Beads | Uniform particles that bind antibodies; used with single-color stains to create controls for accurately calculating and correcting for spectral overlap between fluorochromes [69]. |
| FMO Controls | Control samples stained with all antibodies in a panel except one; critical for correctly setting positive/negative boundaries and resolving ambiguous populations in multicolor experiments [66]. |
Experimental Workflow and Data Analysis Diagrams
The following diagrams illustrate the core workflows for managing multi-parameter panels, from experimental setup to computational analysis.
High-Dimensional Cytometry Analysis Workflow
Hierarchical Gating Strategy for Immunophenotyping
Within the framework of multiparameter gating for phenotypic data quality research, the reliable detection of rare cell populations presents a significant challenge. Techniques such as high-parameter flow cytometry and advanced computational methods are essential for identifying these low-abundance cells, which are critical in fields like oncology and immunology. This technical support center provides troubleshooting guides and detailed methodologies to help you overcome the specific issues associated with low event counts, ensuring the integrity and quality of your phenotypic data.
FAQs & Troubleshooting Guides
1. What are the primary causes of weak or absent fluorescent signals when staining rare populations, and how can I resolve them?
Weak signals can be particularly detrimental when trying to resolve rare events from background noise. The table below summarizes common causes and solutions.
| Possible Cause | Solution |
|---|---|
| Low antibody concentration or degradation | Titrate antibodies to find optimal concentration; ensure proper storage and check expiration dates [71]. |
| Low epitope/antigen expression | Use bright fluorochromes (e.g., PE, APC) for weak antigens; check literature for expression levels; use fresh cells when possible [71]. |
| Inadequate instrument settings | Ensure PMT voltages are optimized and correct laser settings are loaded for the fluorochrome used [71]. |
| Inaccessible intracellular antigen | Optimize cell permeabilization protocols to ensure antibody can reach the target [71]. |
2. How can I reduce high background or non-specific staining that obscures rare events?
High background can mask the faint signals from rare cells. Key solutions include:
- Fc Receptor Blocking: Use Fc blockers, BSA, or FBS prior to antibody incubation to prevent non-specific antibody binding [71].
- Include Appropriate Controls: Always use an unstained control to quantify and subtract autofluorescence, and an isotype control to account for non-specific Fc binding [71].
- Thorough Washing: Include additional washing steps after antibody incubation to remove excess, unbound antibodies [71].
- Remove Dead Cells: Use viability dyes (e.g., PI, 7-AAD) to gate out dead cells, which contribute to autofluorescence and non-specific staining [71].
3. My event rate is abnormal during acquisition. What should I check?
An abnormal event rate can lead to an unrepresentative analysis of the cell population.
- Low Event Rate: This is often due to a low cell concentration or sample clumping. Ensure the cell count is around 1x10^6/mL and sieve the cells before acquisition to remove debris [71].
- No Events: This may indicate a clogged sample injection tube. Follow the instrument manufacturer's instructions to unclog the system, often by running a 10% bleach solution followed by dH₂O [71].
- High Event Rate: This can be caused by an overly concentrated sample or air in the flow cell. Dilute the sample to the correct concentration and refer to the instrument manual to address air bubbles [71].
4. What are the key considerations for panel design in multicolor flow cytometry to detect rare cells?
Panel design is critical for successfully resolving multiple parameters on rare populations.
- Fluorochrome Brightness: Pair bright fluorochromes (e.g., PE, APC) with weakly expressed antigens, and dimmer fluorochromes (e.g., FITC) with highly expressed antigens [71].
- Spectral Overlap: In conventional flow cytometry, careful panel design is required to manage fluorescence spillover. Spectral flow cytometry can overcome this by deconvoluting the full fluorescence spectrum of each cell [12].
- Technology Choice: Spectral flow cytometers can deconvolute over 40 fluorescent signals, offering greater flexibility, while mass cytometry fundamentally avoids fluorescence spillover by using metal isotopes, allowing for the measurement of over 100 parameters [12].
Key Experimental Protocols
Protocol for Isolating Low-Abundant Cells from Drosophila Visual System using FACS
This protocol, optimized for isolating fewer than 100 cells per brain, demonstrates key principles for maximizing yield and viability when sorting very rare populations [72].
1. Planning and Pilot Experiments
- Confirm Specificity: Use immunohistochemistry to confirm that genetic markers label only the desired cells within the optic lobe.
- Pilot FACS: Perform a pilot sort to assess the purity of the isolatable population and determine the number of cells of interest per brain.
- Calculate Scale: Based on pilot data, calculate the number of flies needed. This protocol consistently recovers ~25% of fluorescently labeled cells, and high-quality RNA-seq data can be obtained from as few as 1,000 FACS-purified cells [72].
2. Fly Work and Staging
- Set Crosses: Set a large number of crosses (100-200) to obtain sufficient biological material.
- Include Negative Control: Use a genotype that has the reporter (e.g., UAS-GFP) but not the driver to set appropriate FACS gating.
- Stage Pupae Precisely: Stage pupae in a 1-hour window to ensure developmental synchrony and minimize gene expression variability.
3. Sample Preparation and Dissociation
- Shorten Protocol: The total length of the dissociation protocol is minimized to maximize cellular health.
- Reduce Mechanical Stress: Gentle mechanical disruption is applied to the dissected tissue to preserve cell integrity.
- Use Optimized Buffers: Improved dissection and dissociation buffers are used to maintain cell health during the process.
4. FACS and Replication
- Sort Directly: Perform FACS directly after cell dissociation (~40 minutes after dissection begins).
- Perform Biological Replicates: Conduct at least three independent biological replicates to ensure robust results.
Unsupervised Computational Detection of Rare Events in Liquid Biopsy Images
For assays where physical sorting is not feasible, an unsupervised computational approach called the Rare Event Detection (RED) algorithm can be used to identify rare analytes, such as circulating tumor cells (CTCs), in immunofluorescence (IF) images [73] [74].
1. Image Tiling
- A single four-channel IF image is divided into approximately 2.5 million tiles, each sized at 32x32 pixels. This size is chosen so that each tile contains, on average, up to 4 cellular events [73] [74].
2. Denoising Autoencoder (DAE) Training
- Uncorrelated Gaussian noise is added to each tile.
- Pairs of clean and noisy tiles are used to train a DAE. The DAE learns to reconstruct the original data from its noisy version [73] [74].
- The reconstruction error of the DAE approximates the magnitude of the score function (∇log(p)) of the probability density. This value is large in low-density (rare) regions and small in high-density (common) regions, making it an effective metric for rarity [73] [74].
3. Ranking and Artifact Removal
- Each tile is passed through the trained DAE, and a weighted sum of the reconstruction errors across all IF channels is calculated to produce a single rarity metric for each tile [73] [74].
- All tiles are ranked from most rare (highest error) to least rare (lowest error).
- An algorithm is applied to remove tiles containing imaging artifacts, which are then replaced with the next highest-ranked rare tiles [73] [74].
4. Outcome
- The RED algorithm can reduce the initial 2.5 million tiles to a cohort of about 2,500 tiles (a thousand-fold reduction) that are highly enriched for biologically relevant rare events, enabling feasible downstream manual or automated analysis [73] [74].
Workflow Visualization
Traditional Gating Workflow for Rare Cells
Unsupervised Computational Detection Workflow
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials essential for experiments focused on detecting rare cell populations.
| Item | Function |
|---|---|
| Viability Dyes (PI, 7-AAD) | Used to gate out dead cells during flow cytometry, reducing background and non-specific signals that can obscure rare events [71]. |
| Fc Receptor Blockers | Critical for blocking non-specific antibody binding to Fc receptors on immune cells, thereby lowering background staining [71]. |
| Bright Fluorochromes (PE, APC) | Essential for detecting weakly expressed antigens on rare cells, as they provide a strong signal above background noise [71]. |
| Proteolytic Enzyme Blend | Used in tissue dissociation protocols to break down extracellular matrix and create single-cell suspensions for FACS, crucial for maintaining cell health and yield [72]. |
| Four-Channel IF Markers | In liquid biopsy assays, a panel (e.g., DAPI, Cytokeratins, Vimentin, CD45/CD31) is used to stain different cell types, providing the multidimensional data needed for rare event detection [73] [74]. |
| Stable Isotope Labels (Lanthanides) | Used in mass cytometry (CyTOF) as tags for antibodies. They virtually eliminate spectral spillover, allowing for the simultaneous measurement of 40+ parameters on single cells [12]. |
| Spectral Reference Controls | Critical for spectral flow cytometry. These single-stain controls are used to create a reference spectral library for accurate deconvolution of multicolor experimental data [12]. |
Managing Batch Effects and Technical Variability Across Samples and Instruments
Frequently Asked Questions (FAQs)
1. What are batch effects and why are they a problem in phenotypic research? Batch effects are systematic technical variations in data introduced when samples are processed in different groups (batches). These variations can be caused by factors such as different reagent lots, personnel, instruments, or processing dates [75]. In multi-parameter gating for phenotypic data quality research, batch effects are problematic because they can confound true biological signals, leading to spurious findings, reduced statistical power, and irreproducible results [75] [76]. If uncorrected, they can make technical groups appear as distinct biological populations, severely compromising data interpretation.
2. How can I detect batch effects in my flow or mass cytometry data? Several visual and statistical methods can help detect batch effects:
- Visual Inspection: Use PCA or t-SNE plots to see if samples cluster by batch rather than biological condition [75] [77]. For example, a t-SNE plot built on activation markers showing clear segregation by batch indicates a batch effect [77].
- Statistical Tests: Utilize tests like the Cross-Entropy test to quantify the divergence between samples from different batches [77].
- Quality Control Metrics: Compare correlation of samples within and between batches, and assess the correlation of peptides or markers within and between proteins [78].
3. My study has a confounded design where biological groups are processed in separate batches. Can I still correct for batch effects? This is a challenging scenario. When biological groups (e.g., cases and controls) are completely processed in separate batches, the biological variable is said to be "fully confounded" with the batch variable [75] [79]. In such cases, it becomes difficult or impossible to statistically disentangle true biological signals from technical effects [75]. One Bioconductor community discussion highlights that with a confounded design, there is no guaranteed statistical fix, and any correction requires assumptions that may not be warranted [79]. The best solution is preventive: a balanced experimental design where biological groups are evenly distributed across batches [75] [78].
4. What are some common batch effect correction methods? Multiple computational methods exist for batch effect correction. The choice often depends on your data type and experimental design.
Table 1: Common Batch Effect Correction Methods
| Method Name | Typical Application | Key Characteristics |
|---|---|---|
| ComBat | Omics data (e.g., transcriptomics) | Empirical Bayes framework; adjusts for location and scale batch effects [75]. |
limma's removeBatchEffect |
Omics data (e.g., microarray, RNA-seq) | Linear model to remove batch effects [75]. |
| Harmony | Single-cell data (e.g., scRNA-seq) | Iterative process that removes batch effects while preserving biological variability [80]. |
| Mutual Nearest Neighbors (MNN) | Single-cell data | Identifies mutual nearest neighbors across batches to correct the data [80]. |
| Seurat Integration | Single-cell data | Uses canonical correlation analysis (CCA) and mutual nearest neighbors to integrate datasets [80]. |
| NPmatch | Omics data (in Omics Playground) | A newer method using sample matching & pairing; reported to have superior performance [75]. |
5. How can I prevent batch effects during experimental design? Prevention is the most effective strategy. Key steps include:
- Randomization: Randomly assign samples from all biological groups across processing batches [78] [76].
- Replication: Include technical replicates and control samples. For large studies, regularly inject a pooled sample mixture (e.g., every 10-15 samples) to monitor technical variation [78].
- Standardization: Use the same reagent lots, protocols, and equipment for the entire study where possible [80] [77].
- Metadata Collection: Meticulously record all technical factors, both planned and unexpected [78].
- Overnight Staining: In cytometry, overnight staining can lead to a stable staining equilibrium, making results more consistent across batches and forgiving minor pipetting errors [77].
Troubleshooting Guides
Problem: Inconsistent Cell Population Clustering Across Batches in Cytometry
Symptoms: When analyzing data from multiple batches, cells from the same biological population cluster separately in t-SNE or UMAP plots based on their batch of origin rather than their phenotype [77].
Solutions:
- Assess the Effect: First, visualize the data without correction. Coloring the dimensionality reduction plot by batch will reveal the extent of the batch effect [75] [77].
- Apply Batch Correction: Use a suitable batch correction algorithm like Harmony or Seurat Integration, which are designed for high-dimensional single-cell data [80].
- Re-cluster: After correction, perform clustering again on the integrated data. The goal is for cells of the same type to cluster together regardless of batch.
- Validate: Check if known biological populations are now well-defined and if batch-specific clustering has been reduced. Use statistical tests like the Cross-Entropy test to quantify the improvement [77].
Problem: Drifting Signal Intensities in a Large-Scale Proteomics Study
Symptoms: Signal intensities for the same proteins show a systematic upward or downward drift over the course of a long mass spectrometry run involving hundreds of samples [78].
Solutions:
- Initial Assessment: Check sample intensity distributions and correlations between sample pairs to identify batch-specific biases [78].
- Normalization: Apply a normalization procedure (e.g., quantile normalization) to align the distribution of measured quantities across samples [78].
- Batch Effect Correction: Apply a feature-level batch correction method such as ComBat or limma. The
proBatchR package offers a specialized workflow for proteomic data [78]. - Quality Control: Post-correction, compare the correlation of samples within and between batches again. Pay special attention to replicate correlations to ensure they have improved [78].
Problem: Confounded Batch and Biological Variable in a Longitudinal Study
Symptoms: In a study with repeated measures from the same individuals over time, samples from different visits were processed in different batches. It is now impossible to distinguish whether variability between visits is due to true biological changes or batch effects [79].
Solutions: This is a severe problem with no perfect solution, but some approaches can be attempted:
- Use Housekeeping Features: If available, use a set of stable "housekeeping" miRNAs, proteins, or genes that are not expected to change biologically. Methods like
RUVgfrom theRUVSeqpackage can use these to estimate and remove unwanted variation [79]. - Subset the Data: If the data is ample, analyze a subset where repeated measures for the same individual were processed within the same batch. This allows for a clean analysis of biological variability, albeit with a potentially smaller sample size [79].
- Model with Covariates: In subsequent modeling (e.g., a GLM), you can include the batch as a covariate. However, this is often inadequate when batch and the variable of interest are perfectly confounded [79].
Experimental Protocols
Protocol 1: Assessing Batch Effects Using Principal Component Analysis (PCA)
Purpose: To visually determine if technical batch has a stronger influence on data structure than biological group.
Materials:
- Normalized data matrix (samples x features)
- Metadata file specifying batch and biological group for each sample
- Statistical software (e.g., R, Python)
Methodology:
- Data Input: Load your normalized data matrix and the associated metadata.
- Perform PCA: Conduct Principal Component Analysis on the normalized data. This reduces the dimensionality of your data to key components that explain the most variance.
- Visualize Results: Create a scatter plot of the first two principal components (PC1 vs. PC2).
- Color by Batch: Color the data points in the plot based on their batch ID. Examine if samples cluster primarily by their batch.
- Color by Biology: Overlay or create a new plot coloring points by the biological condition (e.g., healthy vs. disease). Compare the strength of clustering by batch versus biology.
- Interpretation: If samples form distinct clusters based on batch, it indicates a strong batch effect that must be addressed before biological conclusions can be drawn [75] [76].
Protocol 2: Correcting Batch Effects in Single-Cell Data Using Harmony
Purpose: To integrate multiple single-cell datasets from different batches, enabling joint analysis without technical artifacts.
Materials:
- A combined data object (e.g., a Seurat object in R) containing normalized count data from all batches.
- A defined list of highly variable features.
Methodology:
- Preprocessing: Normalize the data for each batch independently and identify highly variable features.
- Scale and PCA: Scale the data and run PCA on the combined dataset.
- Run Harmony: Input the PCA embedding and batch metadata into the Harmony algorithm. Harmony iteratively corrects the embeddings so that data aligns across batches.
- Use Corrected Embeddings: Retrieve the Harmony-corrected PCA embeddings. Use these for downstream clustering and UMAP/t-SNE visualization instead of the original PCA results.
- Validation: Visualize a new UMAP generated from the Harmony-corrected space. Cells should now mix between batches but separate by biologically distinct populations [80].
Workflow and Relationship Diagrams
Diagram 1: Overall batch effect management workflow, showing progression from prevention to correction.
Diagram 2: Problematic confounded design, where batch is entangled with biology.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for Managing Batch Effects
| Item | Function | Considerations for Batch Effect Reduction |
|---|---|---|
| Antibody Panels | Tagging cell surface and intracellular markers for phenotyping. | Use the same vendor and product lot for an entire study. Be wary of custom conjugates from suppliers, as these can have higher lot-to-lot variability [77]. |
| Control Samples | (e.g., pooled patient samples, reference standards, spike-ins). | Run in every batch to monitor technical variation and enable normalization. In proteomics, a sample mix injected regularly serves as a control [78]. |
| Viability Dye | Distinguishing live cells from dead cells. | Consistent use of the same dye and concentration across batches improves gating consistency and reduces background signal. |
| Cell Staining Buffer | Medium for antibody incubation. | Using the same buffer formulation and lot ensures consistent pH and ion strength, which affect antibody binding [77]. |
| Instrument Calibration Beads | Standardizing cytometer settings across runs. | Daily calibration with the same bead lot ensures data is comparable over time and between instruments. |
Frequently Asked Questions & Troubleshooting Guides
FAQ 1: What is the core challenge of multi-parameter optimization in phenotypic research?
The primary challenge is balancing multiple, often conflicting, objectives simultaneously. In phenotypic data quality research, you may need to optimize for parameters like treatment effectiveness, energy efficiency, processing time, and model accuracy all at once. For example, in electromagnetic vibration treatment for seed phenotypes, optimizing for germination rate might conflict with energy consumption goals [81]. Multi-parameter optimization (MPO) provides a computational framework to quantitatively balance these competing design goals, replacing cognitive biases with data-driven decisions [82] [83].
FAQ 2: Which hyperparameter optimization (HPO) method should I choose for my phenotypic dataset?
Your choice depends on your dataset size, computational resources, and the types of hyperparameters you need to tune. The table below summarizes methods from recent studies:
Table: Comparison of Hyperparameter Optimization Methods
| Method | Best For | Key Advantage | Validation Performance (AUC) |
|---|---|---|---|
| FedPop | Federated Learning with distributed phenotypic data | Online "tuning-while-training"; optimizes client & server HPs [84] | New SOTA on FL benchmarks [84] |
| Bayesian Optimization | Medium-sized datasets with limited features | Efficient search with surrogate models [85] | ~0.84 (from 0.82 baseline) [85] |
| Evolutionary Algorithms | Complex search spaces with multiple HP types | Population-based approach; broad exploration [84] | Substantial gains in complex tasks [84] |
| Random Search | Initial exploration of HP space | Simple implementation; good baseline [85] | ~0.84 (comparable to other methods) [85] |
For large datasets with strong signal-to-noise ratio, most HPO methods perform similarly, but for federated or distributed phenotypic data, FedPop shows particular promise [85] [84].
FAQ 3: How do I handle dataset shift between training and production populations in phenotypic studies?
Implement a robust validation strategy that includes both internal and temporal external validation. In clinical predictive modeling, studies show that models with adequate HPO maintain performance on temporal independent datasets when they have large sample sizes and strong signal-to-noise ratios [85]. For phenotypic data, consider:
- Federated Population-based Tuning (FedPop-L): Optimizes hyperparameters for local client updates based on local validation performance [84]
- Cumulative Environmental Modeling: As demonstrated in tomato quality prediction, track how environmental factors cumulatively affect phenotypes over time [86]
- Multi-objective Validation: Validate not just accuracy but also calibration and feature importance stability [85]
FAQ 4: Why does my model perform well during tuning but poorly on new phenotypic batches?
This often indicates overfitting to specific batch characteristics or insufficient diversity in your tuning dataset. Recent research on corn seed phenotype prediction emphasizes the importance of adaptive parameter optimization strategies that maintain robust performance across different seed batches [81]. Solutions include:
- Expanding HP Search Space: Use methods like FedPop that enable broader exploration beyond pre-defined narrow spaces [84]
- Incorporating Batch Effect Parameters: Explicitly model batch-to-batch variation as an additional parameter in your optimization framework
- Transfer Learning: Leverage patterns learned from one phenotypic population to accelerate tuning for new populations
Experimental Protocols & Methodologies
Protocol 1: Multi-objective Optimization for Electromagnetic Vibration Parameters
This protocol adapts methodology from corn seed phenotype prediction research for general phenotypic data quality applications [81].
Table: Core Parameter Ranges and Optimization Objectives
| Parameter | Operational Range | Theoretical Foundation | Primary Impact |
|---|---|---|---|
| Magnetic Field Strength (B₀) | 0.5-5.0 mT | Cellular membrane integrity preservation [81] | Treatment penetration depth |
| Vibration Frequency (f) | 10-1000 Hz | Seed tissue resonance characteristics [81] | Cellular component selectivity |
| Treatment Duration (T) | 1-30 minutes | Thermal damage prevention vs. physiological activation [81] | Cumulative effect magnitude |
| Phase Angle (φ) | 0-360 degrees | Wave interference patterns [81] | Signal superposition control |
Workflow Overview: The following diagram illustrates the adaptive optimization process for tuning electromagnetic vibration parameters:
Step-by-Step Methodology:
Establish Multi-modal Data Acquisition
- Integrate electromagnetic vibration sensors with high-resolution imaging devices
- Collect temporal data across the entire treatment and response cycle
- Implement quality control using box-plot method for outlier detection: upper bound (Q3 + 1.5 × IQR) and lower bound (Q1 - 1.5 × IQR) [86]
Develop Hybrid Deep Learning Architecture
- Apply CNN for spatial feature extraction from imaging data:
- Utilize LSTM networks for processing sequential electromagnetic vibration data
- Implement simultaneous prediction of multiple phenotype characteristics
Implement Multi-objective Optimization
- Apply integrated Genetic Algorithms with Particle Swarm Optimization (GA-PSO)
- Define objective function incorporating:
- Treatment effectiveness (e.g., germination rate, phenotype quality)
- Energy efficiency constraints
- Processing time limitations
- Use Pareto-optimal solution identification for balanced compromises
Validate with Experimental Framework
- Test optimized parameters on held-out population batches
- Measure key performance indicators: accuracy, recall, physiological improvements
- For corn seeds, researchers achieved 93.7% prediction accuracy with 91.2% recall [81]
Protocol 2: Image-Based Phenotype Quality Prediction with Limited Hardware
This protocol adapts tomato quality prediction methodology for general phenotypic applications where expensive instrumentation is unavailable [86].
Table: Phenotypic Prediction Model Configuration
| Model Component | Architecture | Performance (R²) | Primary Function |
|---|---|---|---|
| Environmental Predictor | LSTM Network | >0.9559 [86] | Cumulative environmental effects |
| Maturity Prediction | GRU with Attention Mechanism | >0.86 (color ratio) [86] | Dynamic phenotype progression |
| Quality Evaluation | Deep Neural Network | >0.811 (LYC, FI, SSC) [86] | Internal quality parameter mapping |
Workflow Overview: The following diagram illustrates the image-based phenotypic quality prediction workflow:
Step-by-Step Methodology:
Temporal Data Collection Protocol
- Deploy multi-parameter environment loggers for temperature, humidity, and light intensity
- Capture sequential RGB images throughout phenotype development cycle
- For tomato studies, researchers collected 1,606 images at 3024×3024 resolution [86]
- Implement missing data handling:
- ≤5 consecutive missing points: linear interpolation
- >5 consecutive missing points: historical data from nearest timestamp with matching conditions [86]
Deep Learning Model Training
- LSTM Environmental Predictor:
- Input: cumulative environmental factors (light, temperature, humidity)
- Output: predicted environmental progression patterns
- GRU with Attention Mechanism (GRU-AT):
- Processes dynamic color ratio changes from RGB images
- Attention mechanism identifies critical temporal points in phenotype development
- DNN Quality Evaluation:
- Establishes nonlinear mapping between color features and internal quality parameters
- Simultaneously predicts multiple quality indicators (e.g., firmness, composition)
- LSTM Environmental Predictor:
Model Integration and Validation
- Fuse outputs from all three model components
- Establish three-dimensional environment-phenotype-quality relationships
- Validate prediction accuracy against destructive testing methods (HPLC, spectrophotometry)
- Achieve non-destructive monitoring with significantly reduced hardware costs
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Multi-parameter Phenotypic Research
| Research Material | Function/Application | Example Specifications |
|---|---|---|
| Electromagnetic Vibration System | Controlled phenotype treatment | Field strength: 0.5-5.0 mT, Frequency: 10-1000 Hz [81] |
| Multi-parameter Environment Logger | Monitoring cumulative environmental effects | Temperature, humidity, solar radiation sensors [86] |
| High-Resolution Industrial Camera | Phenotype image acquisition | 3024×3024 resolution, sequential capture capability [86] |
| Hybrid CNN-LSTM Network | Multi-modal data processing | Spatial feature extraction + temporal dependency modeling [81] |
| Evolutionary Optimization Algorithms | Multi-parameter tuning | Population-based methods (GA, PSO) for HP optimization [81] [84] |
| Federated Learning Framework | Distributed phenotype analysis | FedPop for hyperparameter tuning across decentralized data [84] |
In multi-parameter gating for phenotypic data quality research, the integrity of the final analysis is entirely dependent on the quality control (QC) and pre-processing steps performed before a single gate is drawn. Errors introduced during sample preparation or instrument setup propagate through the entire analytical workflow, compromising phenotypic identification and quantification. This guide provides researchers, scientists, and drug development professionals with a systematic framework for troubleshooting common pre-gating issues and implementing robust QC protocols to ensure data reliability.
Core Concepts: Foundational Principles of Flow Cytometry QC
Effective quality control is built upon several non-negotiable principles. Understanding the instrument's optical configuration—including the number and type of lasers, the number of detectors, and the specific filter sets—is the first critical step in panel design and is essential for anticipating and managing spectral overlap [87]. Furthermore, the fundamental rule of pairing bright fluorochromes (such as PE or APC) with low-density antigens and dimmer fluorochromes (like FITC or Pacific Blue) with highly expressed antigens is crucial for achieving optimal signal-to-noise ratio [87] [88].
Troubleshooting Guides
Table 1: Troubleshooting Fluorescence Signal Issues
| Possible Cause | Solution | Relevant Control |
|---|---|---|
| Weak or No Signal | ||
| Antibody degraded or concentration too low [88] | Titrate antibodies; ensure proper storage; use fresh aliquots. | Positive control |
| Low antigen expression [88] | Use bright fluorochromes (PE, APC); check literature for expression; use fresh cells. | Biological positive control |
| Inaccessible intracellular antigen [88] | Optimize permeabilization protocol; use Golgi blocker (e.g., Brefeldin A). | Intracellular staining control |
| Incompatible laser/PMT settings [88] | Ensure instrument settings match fluorochrome; adjust PMT voltage. | Negative & positive control |
| Saturated or Excess Signal | ||
| Antibody concentration too high [88] | Titrate antibody to find optimal concentration. | Positive control |
| High antigen paired with bright fluorochrome [88] | Re-panel with a dimmer fluorochrome (e.g., FITC, Pacific Blue). | Positive control |
| PMT voltage too high [88] | Adjust instrument settings for the specific channel. | Negative & positive control |
| High Background/Non-Specific Staining | ||
| Unbound antibodies present [88] | Increase washing steps after antibody incubation. | Unstained control |
| Fc receptor-mediated binding [88] | Block Fc receptors prior to antibody incubation. | Isotype control |
| High autofluorescence [88] | Use fluorochromes in the red channel (e.g., APC); use viability dye. | Unstained control |
| Presence of dead cells [88] | Include a viability dye (e.g., PI, 7-AAD) to gate out dead cells. | Viability control |
Table 2: Troubleshooting Sample and Instrument Issues
| Possible Cause | Solution | Relevant Control |
|---|---|---|
| Abnormal Scatter Profile | ||
| Cells are lysed or damaged [88] | Optimize preparation; avoid vortexing/high-speed centrifugation. | Fresh, healthy cells |
| Presence of un-lysed RBCs [88] | Ensure complete RBC lysis; use fresh lysis buffer. | Microscopic inspection |
| Presence of dead cells or debris [88] | Sieve cells before acquisition; use viability dye. | Viability control |
| Abnormal Event Rate | ||
| Low event rate due to clog [88] | Unclog sample injection tube (e.g., run 10% bleach, then dH2O). | Sheath fluid pressure check |
| Low event rate due to clumping [88] | Sieve cells; mix sample gently before running. | Visual inspection |
| Event rate too high [88] | Dilute sample to recommended concentration (~1x10^6 cells/mL). | Cell count |
Frequently Asked Questions (FAQs)
My single-stained controls look perfect, but my fully stained tube has compensation errors. What is the most likely cause?
This is a classic scenario where the compensation controls did not follow the critical rules for setup. The two most common causes are:
- Brightness Mismatch: The single-stained control must be as bright or brighter than the fully stained sample for the same fluorophore. If the fully stained sample is brighter, the calculated compensation will be incorrect [89].
- Fluorophore Mismatch: The exact same fluorophore must be used to stain the control and the fully stained sample. Using a FITC control to compensate for GFP, or compensation beads to compensate for a viability dye in cells, will lead to errors due to potential differences in emission spectra [89].
How can I minimize spectral overlap in my multicolor panel from the start?
Strategic panel design is key to minimizing spillover. Follow these steps:
- Know Your Cytometer: Understand the specific lasers and filters available on your instrument [87].
- Consult Spectra Viewers: Use online tools to choose fluorophores with minimal emission spectrum overlap [87].
- Spread Fluorophores Across Lasers: Where possible, assign fluorophores to different laser lines to avoid spillover entirely.
- Avoid Bad Combinations: Some combinations, like APC and PE-Cy5, have a high degree of overlap and should be avoided unless properly accounted for [87]. The EuroFlow consortium, for example, conducted extensive evaluations to select optimal 8-color fluorochrome combinations to minimize this issue [90].
What are the essential experimental controls for a rigorous flow cytometry experiment?
To ensure your data is interpretable and reproducible, a complete experiment should include:
- Unstained Control: Cells without any fluorescent antibodies to assess autofluorescence [88].
- Fluorescence Minus One (FMO) Controls: Tubes containing all antibodies except one, used to set boundaries for positive staining and to detect spread error due to compensation in that channel.
- Isotype Control: Antibodies of the same isotype but irrelevant specificity, helping to identify non-specific Fc receptor binding [88].
- Viability Control: A dye to mark dead cells, which should be excluded from analysis as they often bind antibodies non-specifically [88].
- Compensation Controls: Single-stained samples for each fluorophore in your panel, used to calculate the spectral overlap matrix [87] [89].
- Biological Positive/Negative Controls: Known positive and negative cell samples or populations to confirm antibody functionality.
My data looks noisy and populations are poorly resolved, but my staining protocol was followed. What should I check?
This is often related to sample quality. First, confirm the health and viability of your cells. An excess of dead cells and debris will dramatically increase background and autofluorescence [88]. Always use a viability dye. Second, check for clumps by sieving your cells gently before acquisition, as clogs and clumps can cause abnormal flow rates and scatter profiles [88]. Finally, ensure all buffers and reagents are fresh and that cells were handled gently to prevent lysis during preparation.
Experimental Protocols for Standardization
EuroFlow Instrument Standardization and Setup
The EuroFlow Consortium established a highly reproducible SOP for instrument setup to ensure maximal comparability of results across different laboratories [90].
- Daily Quality Control: Run standardized fluorescent beads to check laser delays and photomultiplier tube (PMT) voltages, ensuring the instrument is performing within specified parameters.
- Optical Configuration: Use a pre-defined set of fluorochromes and antibody clones that have been experimentally validated for compatibility and performance on specific cytometer models with blue (488 nm), red (633/635 nm), and violet (405/407 nm) lasers [90].
- Compensation Setup: Calculate compensation using single-stained controls that are brighter than the experimental samples and treated with the same fixatives (if any) to account for any spectrum shifts [89] [90].
Workflow for Pre-processing and Gating Standardization
The International Society for the Advancement of Cytometry (ISAC) has developed data standards to make FCM data analysis reproducible and exchangeable [91]. A standardized pre-processing workflow can be captured using these standards:
- Data Acquisition: Raw data is stored in the Flow Cytometry Standard (FCS) file format [91].
- Pre-processing: This critical step includes applying a compensation matrix and removing debris and dead cells. This can be performed in software like FlowJo or using the
flowCorepackage in R/Bioconductor [91]. - Standardized Data Export: The pre-processed FCS files, along with the gating definitions (exported in the Gating-ML standard format) and cell population assignments (in the Classification Results (CLR) format), can be bundled into an Archival Cytometry Standard (ACS) container [91]. This creates a complete, reproducible record of the entire analytical pipeline.
The following diagram illustrates this standardized workflow and the role of data standards in ensuring reproducibility.
Protocol: Identifying and Resolving Compensation Errors
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents for Flow Cytometry QC
| Item | Function | Example/Note |
|---|---|---|
| Viability Dyes (e.g., PI, 7-AAD) | Distinguishes live cells from dead cells for exclusion during gating, reducing non-specific background [88]. | Critical for all assays involving processed cells (frozen, cultured, treated). |
| Fc Receptor Blocking Reagent | Blocks non-specific antibody binding via Fc receptors on immune cells, reducing false positives [88]. | Essential for staining immune cells like monocytes and macrophages. |
| Compensation Beads | Uniformly coated particles used to create consistent single-stained controls for calculating compensation [87]. | Useful when a cell type lacks a universally expressed antigen. |
| Bright Fluorochromes (PE, APC) | Provides high signal-to-noise ratio for detecting low-density antigens or rare cell populations [87] [88]. | PE is one of the brightest available fluorophores. |
| Dim Fluorochromes (FITC, Pacific Blue) | Ideal for labeling highly expressed antigens to avoid signal saturation and reduce spillover [87] [88]. | Helps balance panel and manage spillover. |
| Polymer Stain Buffer | Prevents non-specific aggregation ("sticking") of polymer-based dyes (e.g., Brilliant Violet series) when used together [89]. | Must be used when more than one polymer dye is in a panel. |
| Standardized Antibody Panels (e.g., EuroFlow) | Pre-validated combinations of antibody clones and fluorochromes designed for specific applications and instruments [90]. | Maximizes reproducibility and minimizes panel design effort. |
| Data Standard Files (Gating-ML, CLR) | Computable file formats for exchanging gating definitions and classification results, ensuring analytical reproducibility [91]. | Supported by software like FlowJo and the R/Bioconductor package flowCore. |
Benchmarking for Reliability: Validating Gating Strategies and Comparative Performance Analysis
Frequently Asked Questions (FAQs)
1. What is "ground truth" in the context of phenotypic analysis, and why is it critical? In phenotypic analysis, particularly in cytometry, "ground truth" refers to the accurate and definitive identification of cell populations, which serves as a reference standard against which automated algorithms or new methods are validated [67]. Manual gating by experts is traditionally considered the gold standard [67]. Establishing a robust ground truth is fundamental for ensuring the quality and reliability of your data, as inaccuracies here will propagate through all downstream analyses, leading to reduced power and diluted effect sizes in studies such as Genome-Wide Association Studies (GWAS) [60].
2. Why is a consensus from multiple experts preferred over a single expert's opinion for defining ground truth? Relying on a single expert's gating can be subjective and sensitive to individual choices [67]. Building a consensus from multiple annotators provides a more robust and defensible ground truth [92]. This approach minimizes individual bias and variability, creating a more reliable standard. This is especially important for regulatory-defensible protocols and for training automated gating systems like UNITO, which are validated against such consensus standards [67].
3. What are the practical methods for achieving expert consensus? There are several established methods for building consensus, offering different trade-offs between cost, speed, and regulatory risk [92]. The following table summarizes three common approaches:
| Consensus Method | Description | When to Use |
|---|---|---|
| Three Asynchronous Reads → Automated Consensus [92] | Three readers work independently. Consensus (e.g., 2-of-3 majority vote for cell labels, median for measurements, STAPLE algorithm for segmentation masks) is established automatically without meetings. | A balanced approach for speed, budget, and regulatory risk. |
| Three Asynchronous Reads → Manual Consensus [92] | Three readers work independently. Only cases with discordant results are brought to a synchronous consensus meeting for a final decision. | Ideal when the lowest possible regulatory risk is a priority over cost and speed. |
| Two Readers → Third Adjudicator [92] | Two readers perform independent reads. If they disagree, a third, blinded adjudicator reviews the case and issues the final label. | Most budget-friendly, but may be slower and potentially raise more questions from regulatory bodies. |
4. My automated gating tool is producing unexpected results. How should I troubleshoot this? Unexpected results from automated gating often stem from issues with the input data or the ground truth used for training. Follow this systematic approach:
- Verify Your Single-Cell Suspension: Re-examine your sample preparation protocol. Issues like cell clumping, debris, or excessive dead cells can severely impact pre-gating and all subsequent analysis [93]. Ensure you have created a high-quality single-cell suspension and used appropriate concentration methods [93].
- Check for Technical Variance: Technical variations from sample preparation or instrument settings can cause population shapes and locations to shift between samples [67]. Check that your staining panels are carefully titrated to avoid signal saturation and that compensation has been performed correctly to account for spectral overlap [93].
- Audit Your Ground Truth: The performance of any supervised automated method is limited by the quality of the ground truth it was trained on [67]. Revisit the expert consensus data used to train or validate the algorithm. Inconsistent manual gating will lead to a poorly performing model.
- Confirm Gating Hierarchy: Ensure that the automated tool is configured to respect the biological hierarchy of immune cell differentiation, where gates are set in a tree-like structure [67]. An error in an early, pre-gating step (like singlet selection) will affect all downstream populations.
5. When should objective diagnoses be prioritized over expert consensus? Whenever available, objective, definitive findings should be used as the primary reference standard [92]. This includes results from histopathology, operative findings, polysomnography (PSG), or structured chart review. This practice removes the chance of high inter-reader variability, which can make a device or algorithm perform worse on paper than it truly is [92].
Troubleshooting Guide: Common Gating Issues
Here is a guide to diagnosing and resolving frequent problems encountered during manual gating and consensus building.
| Error / Symptom | Potential Cause | Solution |
|---|---|---|
| High disagreement between expert gaters. | Unclear gating protocol; high technical variance in data; ambiguous cell population boundaries. | Develop a Standard Operating Procedure (SOP) for gating. Pre-calibrate readers using a training set. Use the "Three Asynchronous Reads → Manual Consensus" method for discordant cases [92]. |
| Automated gating fails to identify a known rare population. | Insufficient examples of the rare population in the training data; the population is consistently gated out during pre-gating. | Manually review the pre-gating steps. Ensure the training set for the algorithm is enriched with enough representative events from the rare population. |
| Cell population appears in an unexpected location on the bivariate plot. | Major technical variance; improper compensation or staining; instrument fluctuation [67]. | Check your single-stained controls and re-run compensation [93]. Verify that all staining protocols were followed and reagents were titrated properly [93]. |
| Poor performance of a trained automated gating model on new data. | "Batch effects" or significant technical variance between the training data and new data; panel design changes. | Retrain the model on a new set of 30-40 manually gated samples from the new batch or with the updated panel to ensure performance aligns with human expectations [67]. |
Experimental Protocols for Validation
Protocol 1: Establishing a Consensus Ground Truth for a Gating Hierarchy
This protocol outlines a method for creating a robust ground truth by leveraging independent expert analysis.
1. Objective: To generate a reliable, consensus-based ground truth for a predefined gating hierarchy (e.g., singlets → lymphocytes → CD4+ T cells) to be used for validating automated gating algorithms.
2. Materials:
- Cytometry data files (e.g., .fcs files)
- At least three experienced immunologists or cell biologists
- Gating software (e.g., FlowJo, FACS Diva)
- A secure platform for sharing data and annotations
3. Methodology:
- Step 1: Pre-calibration. Hold a session with all experts to review and agree upon the gating hierarchy and the specific criteria for drawing boundaries for each cell population.
- Step 2: Independent, Blinded Gating. Each expert independently analyzes the same set of files (recommended 30-40 samples) without consulting the others [67]. They apply the agreed-upon hierarchy and save their gating results.
- Step 3: Consensus Generation. Use one of the structured methods described in the FAQs:
- For Automated Consensus: Collect all gating results and compute a consensus mask for segmentation tasks using the STAPLE algorithm, or use a 2-of-3 majority vote for case-level labels (e.g., "population present/absent") [92].
- For Manual Consensus: Identify all cases where the experts' calls disagree. Convene a consensus meeting where these specific cases are reviewed and a final, unanimous label is assigned [92].
4. Output: A single, consensus gating label for every cell in the dataset, which becomes the ground truth for downstream validation.
Protocol 2: Validating an Automated Gating Framework Against Ground Truth
This protocol describes how to test the performance of an automated tool like UNITO against the consensus ground truth.
1. Objective: To quantitatively evaluate the performance of an automated gating framework in reproducing expert-defined cell populations.
2. Materials:
- Consensus ground truth from Protocol 1.
- Automated gating software (e.g., UNITO, FlowSOM, DeepCyTOF).
- Computing environment capable of running the software.
3. Methodology:
- Step 1: Data Partitioning. Split the dataset with consensus labels into a training set (e.g., ~70% of samples) and a held-out validation set (e.g., ~30%).
- Step 2: Model Training. Train the automated gating model on the training set. For a framework like UNITO, this involves feeding the bivariate density plots and consensus masks into the model to learn the gating pattern for each hierarchy level [67].
- Step 3: Prediction and Comparison. Run the trained model on the held-out validation set. Compare the model's cell-type predictions against the consensus ground truth labels.
- Step 4: Performance Metrics. Calculate metrics such as F-measure, precision, and recall for each cell population. The benchmark for success is that the automated method "deviates from human consensus by no more than any individual [expert] does" [67].
Workflow Visualization
The following diagram illustrates the integrated workflow of expert consensus building and automated gating validation.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table lists key materials and computational tools essential for experiments in high-parameter phenotypic gating and ground truth establishment.
| Item / Reagent | Function / Application |
|---|---|
| Heavy Metal-labeled Antibodies | Used in mass cytometry to tag specific cell surface and intracellular proteins, allowing for the simultaneous measurement of dozens of parameters with minimal signal spillover [93]. |
| Fluorophore-labeled Antibodies | Used in flow cytometry to tag proteins of interest. Require careful panel design to manage spectral overlap and necessitate compensation [93]. |
| DNA Intercalator (e.g., Iridium) | A cell viability dye that stains DNA in fixed cells; a critical channel for identifying intact, nucleated cells and for singlet gating in mass cytometry [93] [67]. |
| Permeabilization Reagent (e.g., Saponin) | Allows antibodies to cross the cell membrane and stain intracellular proteins (e.g., FoxP3) and transcription factors [93]. |
| UNITO Framework | An automated gating framework that transforms protein expression data into bivariate density maps and uses image segmentation to perform gating, achieving human-level performance [67]. |
| STAPLE Algorithm | A computational tool used to combine multiple expert segmentations (e.g., gating masks) into a single, probabilistic consensus segmentation, automating the ground truth process [92]. |
Frequently Asked Questions (FAQs)
Q1: What are precision and recall, and how do they differ in the context of phenotypic data validation?
A: Precision and recall are core metrics for evaluating classification performance, crucial for ensuring high-quality phenotypic cohorts in research.
- Precision answers: "Of all the cells or samples my gating strategy classified as positive, how many were truly positive?" It is calculated as True Positives / (True Positives + False Positives). High precision indicates a low rate of false positives, meaning your target population is pure and not contaminated by off-target cells [94] [95].
- Recall (also known as Sensitivity) answers: "Of all the truly positive cells or samples present, how many did my strategy correctly identify?" It is calculated as True Positives / (True Positives + False Negatives). High recall indicates you are missing very few of the cells you aim to study, which is critical for comprehensive population analysis [94] [95].
In multi-parameter gating, a high-precision, low-recall strategy might yield a very pure but potentially rare cell population. Conversely, a high-recall, low-precision strategy might capture most of the target cells but include many others, leading to a heterogeneous and potentially misleading population.
Q2: What is the F1 Score, and when should I use it to evaluate my gating strategy?
A: The F1 Score is the harmonic mean of precision and recall, providing a single metric to balance the trade-off between them [96]. It is calculated as 2 * (Precision * Recall) / (Precision + Recall).
The F1 Score is most valuable when you need to find an equilibrium between false positives and false negatives [96]. It is particularly useful when:
- Your cell population of interest is rare (an imbalanced dataset) [96].
- There is no clear, dominant priority between avoiding contamination (false positives) and ensuring comprehensive capture (false negatives).
If your experiment demands prioritizing one metric over the other (e.g., maximizing recall to ensure no target cell is missed for downstream single-cell sequencing), the F1 score may be less informative than the individual metrics.
Q3: How do specificity and sensitivity relate to precision and recall?
A: The terminology differs between data science and medical fields, but the underlying calculations are the same. This table clarifies the relationship:
| Data Science Metric | Medical / Biological Metric | Formula | Focus |
|---|---|---|---|
| Recall | Sensitivity | TP / (TP + FN) | Ability to identify all true positives [95]. |
| Not directly equivalent | Specificity | TN / (TN + FP) | Ability to correctly identify true negatives [94] [95]. |
| Precision | Positive Predictive Value (PPV) | TP / (TP + FP) | Accuracy of a positive classification [94]. |
Q4: Which F1 Score variant should I use for multi-class immunophenotyping?
A: When moving beyond a simple positive/negative gate to classify multiple cell types (e.g., T cells, B cells, NK cells), you need to use F1 score variants. The choice depends on your biological question.
| Scenario | Recommended Variant | Explanation |
|---|---|---|
| Equal importance for all cell types | Macro-F1 | Calculates F1 for each class independently and then takes the average. It treats all classes equally, regardless of abundance [96]. |
| Overall performance across all cells | Micro-F1 | Aggregates all TP, FP, and FN across all classes to compute one overall F1 score. It is dominated by the most frequent classes [96]. |
| Account for class imbalance | Weighted-F1 | Calculates a Macro-F1 but weights each class's contribution by its support (the number of true instances). This is often the most pragmatic choice for immunophenotyping [96]. |
Troubleshooting Guides
Problem: My gating strategy yields a high recall but low precision.
Symptoms: Your final population contains most of the target cells (good recall) but is contaminated with other cell types, leading to high background and impure populations for downstream analysis.
Potential Causes and Solutions:
Cause: Poorly optimized fluorescence thresholds.
Cause: Inadequate exclusion of dead cells or doublets.
- Solution: Strictly apply sequential gating for viability and singlets.
- Viability: Use a viability dye (e.g., Propidium Iodide, 7-AAD) and gate to exclude positive (dead) cells [98] [97].
- Singlets: Plot Forward Scatter-Area (FSC-A) vs. Forward Scatter-Height (FSC-H) or -Width (FSC-W). Gate on the diagonal population to exclude cell doublets and aggregates that can cause false positive signals [98] [97].
- Solution: Strictly apply sequential gating for viability and singlets.
Problem: My gating strategy yields high precision but low recall.
Symptoms: The gated population is very pure but misses a significant portion of the target cells, potentially leading to a loss of biological information and statistical power.
Potential Causes and Solutions:
Cause: Overly conservative gating.
- Solution: Use back-gating to validate your strategy. Overlay your final gated population onto earlier plots (like FSC vs. SSC) to see if you are unintentionally excluding a subset of your target cells based on their physical characteristics. Adjust gates to be more inclusive while monitoring precision [7].
Cause: Antibody concentration or staining is suboptimal.
- Solution: Titrate antibodies to find the optimal concentration that provides the best signal-to-noise ratio. Weak staining can cause dim populations to be incorrectly excluded from the positive gate, lowering recall.
Interpretation of Metric Combinations
This table helps diagnose the performance profile of your phenotyping or gating algorithm based on the combination of metrics [95].
| Metric Profile | Precision | Recall | Specificity | Interpretation |
|---|---|---|---|---|
| Inclusive Screener | Low | High | High | Trust negative predictions; positive predictions are unreliable. Good for initial screening to avoid missing positives. |
| Critical Detector | High | High | Low | Fails to identify true negatives. Effectively finds all positives but with many false alarms. |
| Conservative Confirmer | High | Low | High | Positive predictions are very reliable, but many true positives are missed. Ideal when false positives are costly. |
F1 Score Variants and Their Formulas
| Variant | Formula | Use-Case |
|---|---|---|
| Macro-F1 | Calculate F1 for each of ( N ) classes, then average: ( \text{Macro-F1} = \frac{1}{N} \sum{i=1}^{N} F1i ) | All cell types are equally important. |
| Micro-F1 | Compute a global F1 from total counts: ( \text{Micro-F1} = \frac{2 \times \sum TP}{\sum (2 \times TP + FP + FN)} ) | Overall performance across all cells is the goal. |
| Weighted-F1 | Compute Macro-F1, but weight each class's F1 by its support: ( \text{Weighted-F1} = \sum{i=1}^{N} wi \times F1_i ) | To account for class imbalance (common in phenotyping). |
Experimental Protocols
Detailed Methodology: Validating a Phenotyping Algorithm Using Quantitative Metrics
This protocol outlines steps to quantitatively assess the performance of a rule-based phenotyping algorithm, such as one used to define a disease cohort from Electronic Health Records (EHR), mirroring best practices from genomic studies [60].
1. Objective: To evaluate the accuracy, power, and functional relevance of a phenotyping algorithm for defining case cohorts for a genome-wide association study (GWAS).
2. Materials and Input Data:
- EHR Data: Structured data in domains such as conditions (e.g., ICD codes), medications, procedures, laboratory measurements, and observations [60].
- Phenotyping Algorithms: The rules to be compared (e.g., simple code-based vs. complex multi-domain rules) [60].
- Validation Tool: A method like PheValuator to estimate the Positive Predictive Value (PPV) and Negative Predictive Value (NPV) of the algorithms, which directly influence GWAS power [60].
3. Procedure:
a. Cohort Construction: Apply each phenotyping algorithm to the EHR database to create distinct case and control cohorts [60].
b. Sample QC: Perform standard genetic quality control on the cohorts to remove related individuals and those with poor-quality genetic data [60].
c. Metric Estimation: Use a validation tool to estimate PPV (precision) and NPV for each algorithm. The effective sample size for GWAS is adjusted by a dilution factor calculated as PPV + NPV - 1 [60].
d. GWAS Execution: Conduct a GWAS for each cohort, using standard covariates (age, sex, genetic principal components) [60].
e. Downstream Analysis:
* Power & Heritability: Calculate statistical power and SNP-based heritability (using LDSC) for each GWAS [60].
* Functional Enrichment: Assess the number of significant hits (hits) located in coding or functional genomic regions [60].
* Replicability & PRS: Evaluate the replicability of findings and the accuracy of derived Polygenic Risk Scores (PRS) [60].
4. Expected Outcome: Studies show that high-complexity phenotyping algorithms (integrating multiple data domains) generally yield GWAS with greater power, more functional hits, and improved co-localization with expression quantitative trait loci (eQTLs), without compromising replicability or PRS accuracy [60].
Diagrams and Workflows
Diagram 1: The Precision-Recall Relationship
Diagram Title: Relationship Between Precision and Recall
Diagram 2: Hierarchical Gating for High-Quality Phenotyping
Diagram Title: Sequential Gating Strategy Flowchart
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function |
|---|---|
| Viability Dyes (e.g., PI, 7-AAD) | Distinguish live from dead cells based on membrane integrity; crucial for eliminating false positives from non-specifically staining dead cells [98] [97]. |
| Fluorescence Minus One (FMO) Controls | Define positive/negative boundaries for each marker in a multi-color panel; essential for accurate gating and maximizing precision [7]. |
| Isotype Controls | Help identify and account for non-specific antibody binding, though FMO controls are generally preferred for setting gates in complex panels. |
| Back-gating | A validation technique, not a reagent. Overlaying a gated population on previous plots (e.g., FSC/SSC) to ensure the gating strategy aligns with the expected physical characteristics of the cells [7]. |
| Panel Design Tools | Software (e.g., FluoroFinder) that assists in designing multi-color panels by minimizing spectral overlap and assigning fluorophores based on antigen density and instrument configuration [7]. |
Technical Support Center
This guide provides troubleshooting and FAQs for issues encountered when benchmarking automated flow cytometry gating tools.
Troubleshooting Guides
Problem: Inconsistent Performance Across Samples Automated tools perform well on some samples but poorly on others with merged or skewed populations.
| Troubleshooting Step | Action & Rationale |
|---|---|
| Check Cluster Separation | Visually inspect 2D plots for overlapping populations. Tools struggle when Separation Index (SI) falls below zero [99]. |
| Verify Data Distribution | Assess if populations have non-normal (skewed) distributions. Skewed clusters can reduce accuracy, especially for model-based algorithms like SWIFT [99]. |
| Re-evaluate Tool Selection | If clusters are merged, avoid Flock2 or flowMeans. For skewed data, prefer FlowSOM, PhenoGraph, or SPADE3 [99]. |
Problem: Discrepancy Between Automated and Manual Gating Results Cell population statistics from an automated tool do not match the manual "gold standard."
| Troubleshooting Step | Action & Rationale |
|---|---|
| Review Ground Truth | Manually re-inspect the discordant population. The manual gate itself may be subjective or suboptimal [100]. |
| Use F1 Score for Validation | Quantify agreement between manual and automated gating. An F1 score >0.9 indicates strong agreement [48] [100]. |
| Inspect Rare Populations | Scrutinize gates on small cell populations. Both manual and automated gating have higher variance with low event counts [100]. |
Problem: Compensation Errors in Data Analysis Unexpected spreading or shifting of populations in fluorescence channels.
| Troubleshooting Step | Action & Rationale |
|---|---|
| Identify Error Scope | Determine if errors appear only in fully stained tubes or also in single-stained controls. This dictates the solution path [89]. |
| Inspect Single Stains | If errors are in both, recalibrate compensation using single-stained controls, ensuring gates capture the positive population correctly [89]. |
| Check Fluorophore Matching | If errors are only in full stains, verify that the same fluorophore was used for both the control and the experimental sample [89]. |
Frequently Asked Questions (FAQs)
Q1: What is the most important metric for comparing automated gating to manual gating? The F1 score is a key metric. It is the harmonic mean of precision and recall, providing a single value (between 0 and 1) that measures the per-event agreement between two gating strategies. A score of 1 represents perfect agreement [100]. In validation studies, tools like ElastiGate and flowDensity have demonstrated average F1 scores >0.9 when compared to expert manual gating [48] [100].
Q2: My data has rare cell populations. Which automated gating method should I use? The best method depends on the population characteristics. ElastiGate can be configured with a lower "density level" setting to better capture populations with low cell counts [48]. For discovery-based workflows, Exhaustive Projection Pursuit (EPP) is designed to automatically find all statistically supported phenotypes, including rare ones [101]. Benchmarking with your specific data is recommended.
Q3: How can I objectively validate an automated gating tool for use in a regulated environment? Incorporate synthetic flow cytometry datasets into your validation pipeline. These datasets contain known population characteristics (ground truth) and allow you to systematically test tool performance against factors like population separation and distribution skewness, providing objective evidence of accuracy [99].
Q4: Why does my automated analysis work well in FlowJo but fail when I run it programmatically in R? This often stems from differences in data pre-processing. Ensure that the following steps are consistent between environments:
- Transformation: The same logicle or arcsinh transform and parameters are applied.
- Compensation: The compensation matrix is identical.
- Initial Gating: The same parent population is used as the starting point for analysis.
Performance Benchmarking Data
The table below summarizes the performance of various automated gating tools as reported in recent studies.
| Tool / Algorithm | Type | Key Performance Metric (vs. Manual Gating) | Reported F1 Score (Median/Average) |
|---|---|---|---|
| BD ElastiGate [48] | Supervised | High accuracy across complex datasets | > 0.9 (average) |
| flowDensity [100] | Supervised | Robust for sequential bivariate gating | > 0.9 (median for most pops) |
| FlowGM [102] | Unsupervised (GMM) | Improved gating of "hard-to-gate" monocyte/DC subsets | Par or superior to manual (CV) |
| Exhaustive Projection Pursuit (EPP) [101] | Unsupervised | Automatically identifies all statistically supported phenotypes | Comparable to published phenotypes |
| FlowSOM [99] | Unsupervised (Clustering) | Robust performance on skewed data | Accuracy deteriorates with low SI |
Experimental Protocols
Protocol 1: Benchmarking an Automated Gating Tool Using Synthetic Data This protocol uses synthetic data with known "ground truth" to objectively assess tool performance [99].
- Dataset Generation: Use the R
clusterGenerationpackage to create synthetic datasets.- Set parameters: number of clusters (2-3), events per cluster (e.g., 1000), and a range of Separation Index (SI) values from -0.3 (merged) to +0.3 (well-separated).
- For skewness tests, use the R
snpackage to generate clusters with controlled asymmetry.
- Data Export: Convert the synthetic data matrices to FCS files using the
flowCoreR package. - Tool Execution: Run the automated gating tool(s) on the synthetic FCS files.
- Accuracy Calculation: Compare the tool's output to the known cluster labels to calculate accuracy metrics (e.g., F1 score).
Protocol 2: Validating Against Manual Gating with Biological Data This protocol validates an automated tool against the current manual gating standard [48] [100].
- Training Set Selection: Manually gate a small, representative subset of samples (e.g., 3-5 files) to create a "gold standard" training set.
- Template Application: If using a supervised tool (e.g., ElastiGate, flowDensity), apply the gating template from the training set to a larger target dataset. For unsupervised tools, run the algorithm on the entire dataset.
- Result Comparison: For each cell population of interest, calculate the F1 score by comparing the events assigned by the automated tool to those identified by manual gating.
- Statistical Analysis: Aggregate F1 scores across all populations and samples. Report median and distribution of scores. A median F1 > 0.9 is typically considered successful validation.
The Scientist's Toolkit
| Research Reagent / Material | Function in Gating & Analysis |
|---|---|
| Fluorescence Quantitation Beads | Used to calibrate fluorescence scales and quantify antigen density; a good test case for automated gating of multiple, closely-spaced populations [48]. |
| Viability Dye (e.g., PI, 7-AAD) | Critical for identifying and excluding dead cells during initial gating steps, which reduces background and improves analysis accuracy [103]. |
| Single-Stained Compensation Controls | Beads or cells stained with a single fluorophore, essential for calculating a compensation matrix to correct for spectral overlap [89]. |
| FMO Controls | Controls used in multicolor panels to accurately set positive gates and resolve ambiguous populations, especially for markers with continuous expression [103]. |
| Synthetic Datasets | Computer-generated data with known population truths; used for objective benchmarking and validation of automated gating algorithms [99]. |
Workflow and Decision Diagrams
Automated Gating Tool Selection Workflow
Troubleshooting Gating Discrepancies
Performance Comparison & Quantitative Results
This section provides a quantitative comparison of the gating performance for ElastiGate, flowDensity, and Cytobank across multiple biological applications. Performance was evaluated against manual gating by expert analysts using F1 scores (the harmonic mean of precision and recall), where a score of 1 indicates perfect agreement with manual gating [48].
Table 1: Performance Comparison (F1 Scores) Across Different Biological Assays
| Biological Application | ElastiGate | flowDensity | Cytobank | Notes on Dataset |
|---|---|---|---|---|
| Lysed Whole-Blood Scatter Gating (31 samples) | Lymphocytes: 0.944Monocytes: 0.841Granulocytes: 0.979 [48] | Information missing | Information missing | High variability from RBC lysis protocol [48] |
| Multilevel Fluorescence Beads (21 samples) | Median: 0.991 [48] | Information missing | Information missing | Used for antigen density quantification [48] |
| Monocyte Subset Analysis (20 samples) | Median: >0.93 [48] | Information missing | Information missing | Complex subsets (classical, intermediate, non-classical) [48] |
| Cell Therapy QC & TIL Immunophenotyping (>500 files) | Average: >0.9 [48] | Underperforms with highly-variable or continuously-expressed markers [48] | Underperforms with highly-variable or continuously-expressed markers [48] | CAR-T manufacturing and tumor infiltrate datasets [48] |
Key Performance Insights:
- ElastiGate consistently achieved high accuracy across all tested datasets, with average F1 scores exceeding 0.9. It was specifically noted to outperform existing solutions in handling highly-variable or continuously-expressed markers [48].
- flowDensity is identified as a leading tool but may require computational expertise for optimization and can underperform in scenarios where ElastiGate excels [48].
- Cytobank Automatic Gating was used as a comparator in one dataset, but detailed performance metrics were not included in the available search results [48].
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Our flow cytometry data shows high technical and biological variability from patient samples. Which tool is most robust for this situation? A: ElastiGate was specifically designed for this challenge. Its elastic image registration algorithm automatically adjusts gates to capture local variability, recapitulating the visual process of an expert analyst. It has been validated on highly variable datasets, such as lysed whole-blood samples, where it maintained high F1 scores [48]. flowDensity, which often relies on percentile thresholds, can underperform in such conditions [48].
Q2: We need to automate a quality control (QC) pipeline for cell therapy manufacturing according to an SOP. How can ElastiGate help? A: ElastiGate is accessible as a plugin in FlowJo software, allowing you to define a gating template on a pre-gated training file and then batch-apply it to subsequent target files (e.g., from different patients or manufacturing batches). The software automatically adjusts the gates for each file, ensuring consistency and objectivity while following the intended SOP strategy. This has been successfully tested on CAR-T cell incoming leukapheresis and final product release samples [48].
Q3: When applying the ElastiGate plugin in FlowJo, what does the "Density Mode" parameter do, and how should I set it? A: The "Density Mode" (an integer from 0 to 3) changes parameters for image normalization before registration. Use lower values (0-1) for sparse plots or when gate placement is determined by sparse areas of the plot. Use higher values (2-3) for denser populations or if gate placement is determined by dense areas of the plot [49].
Q4: We are computational biologists comfortable with R. Is there still an advantage to using the ElastiGate plugin over a scripted solution like flowDensity? A: Yes, for speed and ease of implementation. The study noted that ElastiGate outperformed flowDensity in F1 scores and was easier to implement. ElastiGate provides a high-accuracy, GUI-driven workflow that does not require the installation and configuration of R, potentially saving time and standardizing analysis across team members with varying computational skills [48] [49].
Common Error Messages and Resolutions
| Issue / Error | Probable Cause | Solution |
|---|---|---|
| Boolean gates are not supported. | Attempting to use a Boolean (AND, OR, NOT) gate in the ElastiGate plugin. | Convert the Boolean gate into a standard polygon or rectangle gate before using it as a training gate [49]. |
| Poor gating results on a sparse population. | The "Density Mode" may be set too high for the data. | Re-run the analysis with a lower "Density Mode" setting (e.g., 0 or 1) [49]. |
| Gate does not flexibly adapt to a shifted population. | The "Interpolate gate vertices" option may be disabled, or "Preserve gate type" may be restricting deformation. | Enable the "Interpolate gate vertices" option. For rectangles/quadrilaterals, uncheck "Preserve gate type" to allow them to become more flexible polygon gates [49]. |
Experimental Protocols & Workflows
Protocol 1: Benchmarking Automated Gating Tools Against Manual Analysis
This protocol outlines the methodology used to generate the performance data in this case study [48].
1. Objective: To evaluate the accuracy and consistency of an automated gating tool (e.g., ElastiGate) compared to manual gating by multiple expert analysts.
2. Materials and Reagents:
- Biological Samples: Relevant primary cells (e.g., lysed whole blood, monocyte subsets, CAR-T cells).
- Staining Panels: Antibody panels designed for the target immunophenotypes.
- Flow Cytometer: Calibrated instrument.
- Software: FlowJo with ElastiGate plugin; R for flowDensity; Cytobank.
3. Procedure:
- Step 1: Data Acquisition. Acquire flow cytometry data files (.fcs) for all samples.
- Step 2: Manual Gating (Ground Truth). Have multiple expert analysts manually gate the same set of training files to establish a consensus "ground truth." Resolve major discrepancies through discussion.
- Step 3: Template Creation. Select one manually gated file to serve as the training template for ElastiGate.
- Step 4: Automated Gating. Apply the automated gating tool (trained on the template) to the entire set of target files.
- Step 5: Statistical Comparison. For each gate and each sample, calculate the F1 score by comparing the automated gate to the manual ground truth.
- F1 Score = 2 × (Precision × Recall) / (Precision + Recall)
- Precision = True Positives / (True Positives + False Positives)
- Recall = True Positives / (True Positives + False Negatives)
4. Data Analysis:
- Aggregate F1 scores across all gates and samples to calculate median and average performance.
- Use statistical tests (e.g., Wilcoxon signed-rank test) to determine if performance differences between tools are significant.
Diagram 1: Tool benchmarking workflow.
Protocol 2: Implementing ElastiGate in a FlowJo QC Pipeline
This protocol details the steps to set up and run the BD ElastiGate plugin within FlowJo for automated analysis [49].
1. Software Installation and Setup:
- Step 1: Ensure you have FlowJo v10 installed.
- Step 2: Download the ElastiGate plugin .jar file from the FlowJo website.
- Step 3: Place the .jar file in the FlowJo "plugins" folder on your workstation.
- Step 4: In FlowJo, go to
FlowJo > Preferences > Diagnostics, click "Scan for plugins," select the plugins folder, and restart FlowJo.
2. Running ElastiGate:
- Step 1: In your FlowJo workspace, gate a sample according to your desired strategy. This will be your training file.
- Step 2: Click on this gated file, go to the
Workspacetab, and underPlugins, selectElastiGate. - Step 3: In the dialog box:
- Select Training Samples: Choose the pre-gated file(s).
- Select Target Samples: Choose the ungated files you wish to analyze.
- Select Gates to Export: Choose which gates from the hierarchy to apply.
- Step 4: Set Options:
Density Mode: Adjust based on plot density (0-1 for sparse, 2-3 for dense).Interpolate gate vertices: Enable for flexible gate deformation.Preserve gate type: Uncheck to allow rectangles/quads to become polygons.
- Step 5: Click "Start." The plugin will create the adjusted gates on your target files.
Diagram 2: ElastiGate plugin setup and workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Software for Automated Gating Experiments
| Item Name | Function / Description | Example / Specification |
|---|---|---|
| Lysed Whole-Blood Samples | Biologically relevant sample matrix with high technical variability, ideal for testing algorithm robustness [48]. | Prepared using RBC lysis protocol [48]. |
| Fluorescence Quantitation Beads | Calibrate cytometer and quantify antigen density; multiple distinct populations test linear gating accuracy [48]. | Bead populations bound to known numbers of fluorescent molecules [48]. |
| CAR-T Cell & TIL Samples | Complex primary cell samples used for validation in immunophenotyping and cell therapy QC applications [48]. | From leukapheresis or final cell therapy products [48]. |
| BD ElastiGate Software | Automated gating tool that uses elastic image registration to adapt gates to local data variability [48]. | Accessible as a FlowJo plugin or in BD FACSuite Software [48] [49]. |
| FlowJo Software | Industry-standard flow cytometry data analysis platform used to host and run the ElastiGate plugin [49]. | Version 10 or higher [49]. |
| R Statistical Environment | Open-source software environment required to run the flowDensity package and other computational tools [48]. |
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Common Gating Issues and Solutions
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| High variability in reported % of positive cells across labs [104] | Use of different, subjective gating strategies and gate placement [104]. | Implement a pre-defined, consensus gating strategy for all analyses [104]. |
| High background or false positives | Inclusion of dead cells or cell doublets; fluorescence spillover [105] [106]. | Use a viability dye to exclude dead cells; apply doublet exclusion (FSC-A vs. FSC-W); properly compensate for spectral overlap [6] [105]. |
| Low signal or loss of dim populations | Incorrect photomultiplier tube (PMT) voltage; antibody under-titration; over-gating [6] [105]. | Perform a voltage walk to determine optimal PMT settings; titrate all antibodies; use "loose" initial gates to avoid losing populations of interest [6] [7]. |
| Inconsistent results across instruments or batches | Instrument-specific settings; lot-to-lot variation of reagents; signal drift over time [107]. | Use standardized beads for instrument harmonization; implement batch correction scripts; use dried antibody formats for stability [107]. |
Frequently Asked Questions
Q: Why is gating strategy so critical for reproducible research in multi-parameter flow cytometry?
A: Gating is the foundation of data interpretation. A study involving 110 laboratories revealed that when they used 110 different gating approaches on the same data files, the reported percentage of cytokine-positive cells was highly variable. This variability was dramatically reduced when all labs used the same, harmonized gating strategy [104]. Consistent gating is therefore essential for generating robust, comparable results within a single center and across multiple institutions, a cornerstone of reproducible science [104] [107].
Q: What are the essential controls needed for accurate gating in a multicolor panel?
A: Beyond unstained cells, several critical controls are required:
- Viability Dye: To identify and exclude dead cells that nonspecifically bind antibodies [6] [105].
- Fluorescence Minus One (FMO) Controls: These contain all fluorophores except one and are crucial for accurately setting positive gates and resolving dim or smeared populations [6] [7].
- Compensation Controls: Single-stained samples are necessary to correct for spectral overlap between fluorophores [6].
Q: How can we reduce subjectivity and improve consistency in gating?
A: Several approaches can mitigate subjectivity:
- Establish Standard Operating Procedures (SOPs): Define and consistently use a fixed gating hierarchy and gate placement rules [104].
- Leverage Automated Gating Algorithms: Supervised machine learning algorithms or other automated gating tools provide a fast, reliable, and reproducible method for analyzing samples, reducing human bias [107] [7].
- Use Consensus Guidelines: Adopt community-driven recommendations for gate placement, doublet discrimination, and scaling adjustments [104].
Q: Our multi-center study uses different flow cytometers. How can we harmonize the data?
A: A proven procedure involves:
- Instrument Harmonization: Using standardized beads to adjust instrument settings so they all yield similar MFI values for the same sample [107].
- Longitudinal Normalization: Applying an R script to normalize daily quality control (QC) data against initial harmonization targets, correcting for any signal drift over time [107].
- Centralized Analysis: Using automated, supervised gating pipelines to analyze all data uniformly, regardless of the source instrument [107].
Experimental Protocols for Standardization
Protocol 1: Harmonized Gating for Intracellular Cytokine Staining (ICS)
This protocol is adapted from a large-scale gating proficiency panel that successfully reduced inter-laboratory variability [104].
1. Objective: To accurately identify and quantify cytokine-producing CD4+ and CD8+ T cells using a standardized gating strategy.
2. Key Materials:
- Flow cytometry data files (FCS format) from stimulated PBMCs.
- A pre-defined gating strategy document (consensus-based).
3. Methodology:
- Data Acquisition: Download identical, shared FCS files to ensure all analysts are working from the same primary data [104].
- Gating Hierarchy: Adhere strictly to the following sequential gating steps, drafted by expert consensus [104]:
- Lymphocyte Gate: Place a gate on the population based on FSC-A vs. SSC-A to exclude debris and monocytes.
- Singlets Gate: Exclude cell doublets and aggregates by plotting FSC-A vs. FSC-W and gating on the linear population.
- Live Cells Gate: Exclude dead cells using a viability dye.
- CD3+ T Cell Gate: Gate on CD3+ lymphocytes.
- CD4+ and CD8+ Subsets: From the CD3+ population, create separate gates for CD4+ and CD8+ T cells. Pay special attention to excluding CD4+CD8+ double-positive T cells as per guidelines [104].
- Cytokine-Positive Gate: For the final cytokine (e.g., IFN-γ) gate, place it based on FMO controls. A key recommendation is to ensure proximity of the cytokine gate to the negative population to minimize false positives and negatives [104].
4. Quantitative Data Output: The analysis should report the following metrics for each sample [104]:
- Percentage of lymphocytes in the initial "lymphocyte gate"
- Percentage of CD3+CD8+ cells
- Percentage of CD3+CD4+ cells
- Percentage of CD8+ cytokine-positive cells
- Percentage of CD4+ cytokine-positive cells
Protocol 2: Multicenter Flow Cytometry Data Harmonization
This protocol outlines the steps for standardizing data across multiple instruments in a long-term prospective study [107].
1. Objective: To generate comparable flow cytometry data (frequencies, absolute counts, and MFI) across multiple centers and different instrument models over a multi-year period.
2. Key Materials:
- Multiple flow cytometers from various manufacturers.
- VersaComp Capture Beads (or equivalent) for initial harmonization.
- 8-peak beads for daily quality control (QC).
- Dried antibody panels (e.g., DuraClone) for reagent stability.
- R and Python scripts for normalization and batch correction.
3. Methodology:
- Step 1: Initial Instrument Harmonization: Use capture beads to adjust all cytometers to generate matching MFIs for identical samples. Target an inter-instrument coefficient of variation (CV) of less than 5% [107].
- Step 2: Longitudinal Intra-Center Normalization: Run 8-peak beads daily as QC. Use a custom R script to regress the daily QC MFIs back to the targets set during the initial harmonization. Apply the resulting transformation parameters to all experimental data files from that day [107].
- Step 3: Centralized "Manual" Compensation: Have a single, experienced operator review and adjust the compensation matrices for all standardized files to ensure consistency [107].
- Step 4: Automated Gating with Supervised Machine Learning: Develop and apply a supervised machine learning-based gating pipeline. The pipeline should be trained on manually gated datasets and deployed to automatically extract population data from all files, ensuring analysis consistency [107].
- Step 5: Intra-Center Data Correction: Use a Python script to correct for remaining "center effects" and lot-to-lot variation of antibodies identified after large-scale data analysis [107].
4. Validation: Compare the results of the automated gating (Step 4) against traditional manual gating on a subset of hundreds of patients. A high correlation for frequencies, absolute counts, and MFIs validates the automated pipeline [107].
Workflow Visualization
Diagram: Multicenter Flow Cytometry Harmonization
Diagram: Hierarchical Gating Strategy for ICS
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function | Importance for Standardization |
|---|---|---|
| Dried Antibody Panels (e.g., DuraClone) [107] | Pre-mixed, lyophilized antibodies in a single tube. | Provides exceptional lot-to-lot consistency and reduces pipetting errors, crucial for long-term and multi-center studies [107]. |
| Standardized Beads (8-Peak & Capture Beads) [107] | Particles with defined fluorescence intensity used for instrument setup and tracking. | Enables initial harmonization of different cytometers and daily monitoring of instrument performance (signal drift) [107]. |
| Viability Dye (e.g., PI, 7-AAD) [105] | Fluorescent dye that enters dead cells with compromised membranes. | Critical for excluding dead cells, which are a major source of non-specific binding and background noise [6] [105]. |
| FMO Controls [6] | Control sample containing all fluorophores in a panel except one. | Essential for accurately defining positive populations and setting gates, especially for dim markers or in complex multicolor panels [6] [7]. |
| Automated Gating Algorithms [107] [7] | Software that uses computational methods (e.g., supervised machine learning) for cell population identification. | Removes analyst subjectivity, ensures reproducibility, and enables efficient analysis of large, high-parameter datasets [107] [7]. |
Conclusion
The evolution from subjective manual gating to sophisticated, automated computational methods is pivotal for ensuring the quality, reproducibility, and scalability of phenotypic data analysis. This synthesis of foundational knowledge, modern methodologies, optimization techniques, and rigorous validation frameworks underscores that robust multi-parameter gating is no longer a technical nicety but a fundamental requirement for advancing biomedical research and clinical diagnostics. Future directions will be shaped by the increasing adoption of artificial intelligence, the development of standardized, harmonized protocols to minimize inter-laboratory variability, and the deeper integration of these tools into routine clinical workflows. This progression will ultimately empower researchers and clinicians to derive more reliable biological insights, accelerate drug development, and improve patient outcomes through precise and objective cellular characterization.
References
- 1. Immunophenotyping - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK558927/]
- 2. What Is Immunophenotyping? Purpose, Testing & Results [https://my.clevelandclinic.org/health/diagnostics/immunophenotyping]
- 3. Immunophenotyping by flow cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/immunophenotyping-by-flow-cytometry]
- 4. Immunophenotyping [https://en.wikipedia.org/wiki/Immunophenotyping]
- 5. Dissecting immunophenotypic diversity in multiple ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1642609/full]
- 6. Best Practices for Multiparametric Flow Cytometry [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-79/best-practices-multiparametric-flow-cytometry.html]
- 7. Newsletter: Gating Strategies [https://fluorofinder.com/newsletter-gating-strategies/]
- 8. Flow Cytometry Gating: Everything You Need to Know [https://nanocellect.com/blog/flow-cytometry-gating-everything-you-need-to-know/]
- 9. Dissecting the Genetic and Non-Genetic Heterogeneity of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9103951/]
- 10. Heterogeneity of acute myeloid leukemia patients explored ... [https://www.sciencedirect.com/science/article/pii/S1874939925000446]
- 11. Ex vivo drug response heterogeneity reveals personalized ... [https://www.nature.com/articles/s43018-023-00544-9]
- 12. Mapping Cell Phenomics with Multiparametric Flow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9590532/]
- 13. Phenotypic heterogeneity in multiple myeloma families [https://pubmed.ncbi.nlm.nih.gov/15681516/]
- 14. Meeting the Challenges of High-Dimensional Single-Cell Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6634245/]
- 15. Challenges of Transforming Raw Flow Cytometry Data Into ... [https://www.dotmatics.com/blog/flow-cytometry-data-actionable-insights]
- 16. An Introduction to Automated Flow Cytometry Gating Tools ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4515551/]
- 17. manual gating, unsupervised clustering, and auto-gating - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11630031/]
- 18. Automatic, fast, hierarchical, and non-overlapping gating of ... [https://www.sciencedirect.com/science/article/pii/S200103702200527X]
- 19. Introduction to the machine learning tools in the Cytobank ... [https://support.cytobank.org/hc/en-us/articles/4405135671707-Introduction-to-the-machine-learning-tools-in-the-Cytobank-platform]
- 20. Validation of Artificial Intelligence (AI)-Assisted Flow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10888253/]
- 21. Analyzing the Effect of Data Quality on the Accuracy of Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1839724/]
- 22. Data Quality Assessment [https://www.healthit.gov/playbook/pddq-framework/data-quality/data-quality-assessment/]
- 23. Flow Cytometry Troubleshooting Guide [https://www.bio-techne.com/applications/flow-cytometry/flow-cytometry-troubleshooting-guide]
- 24. A toolbox for analysis of cell phenotypes and interactions in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5617107/]
- 25. An integrated toolkit for quality control of phenotypic data in ... [https://www.sciencedirect.com/science/article/pii/S2352914825000826]
- 26. FAQ: Genome-Phenome Analysis Platform [https://rd-connect.eu/what-we-do/omics/gpap/faq-2/]
- 27. Validation Study of Analytical Methods for Multiparameter ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12110934/]
- 28. Applications of machine learning for immunophenotypic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12093103/]
- 29. View Your Backgating Hierarchy in Figure [https://help.omiq.ai/hc/en-us/articles/28963381869972-View-Your-Backgating-Hierarchy-in-Figure]
- 30. Mapping Cell Phenomics with Multiparametric Flow ... [https://link.springer.com/article/10.1007/s43657-021-00031-0]
- 31. to Guide - K ( Nearest ) Algorithm [ Neighbors Edition] KNN 2025 [https://www.analyticsvidhya.com/blog/2018/03/introduction-k-neighbours-algorithm-clustering/]
- 32. 10 Pros & Cons of Support Vector Machines [2025] [https://digitaldefynd.com/IQ/pros-cons-of-support-vector-machines/]
- 33. Step-wise support vector machines for classification of ... [https://www.sciencedirect.com/science/article/abs/pii/S0925231214016993]
- 34. - K ( Nearest ) Algorithm - Neighbors KNN 2025 [https://machinelearningprojects.net/k-nearest-neighbors/]
- 35. Data processing workflow for large-scale immune ... [https://www.sciencedirect.com/science/article/pii/S2001037021002130]
- 36. ccSVM: correcting Support Vector Machines for confounding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3117385/]
- 37. Multiparametric and accurate functional analysis of genetic ... [https://www.nature.com/articles/s41588-022-01224-7]
- 38. How to use k - Nearest ( Neighbors ) with Python... - JC Chouinard KNN [https://www.jcchouinard.com/k-nearest-neighbors/]
- 39. Parameter optimization for stable clustering using FlowSOM [https://pmc.ncbi.nlm.nih.gov/articles/PMC11497637/]
- 40. A comparison framework and guideline of clustering methods ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1917-7]
- 41. The peculiarities of Phenograph [https://www.colibri-cytometry.com/post/the-peculiarities-of-phenograph]
- 42. Settings for clustering arbitrary? (Phenograph/FlowSOM) [https://cytoforum.stanford.edu/viewtopic.php?f=1&t=1844]
- 43. Common Troubleshooting - Cytobank Support [https://support.cytobank.org/hc/en-us/articles/360044794011-Common-Troubleshooting]
- 44. How to Configure and Run a FlowSOM Analysis [https://support.cytobank.org/hc/en-us/articles/360015918512-How-to-Configure-and-Run-a-FlowSOM-Analysis]
- 45. A Beginner's Guide To Analyzing and Visualizing Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5765874/]
- 46. Advances in Multiparametric Flow Cytometry and Data ... [https://www.labx.com/resources/advances-in-multiparametric-flow-cytometry-and-data-analysis-software/5522]
- 47. Automation of flow cytometry data analysis with elastic ... image [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081842/]
- 48. Automation of flow cytometry data analysis with elastic ... [https://www.nature.com/articles/s41598-025-99118-1]
- 49. BD ElastiGate Plugin [https://docs.flowjo.com/flowjo/plugins-2/plugin-demonstration-videos/bd-elastigate-plugin/]
- 50. Automated analysis of flow cytometry data with minimal ... [https://pubmed.ncbi.nlm.nih.gov/39417216/]
- 51. CAR-T and Cell Therapy Research & Development [https://www.bdbiosciences.com/en-us/solutions/translational-research/car-t-and-cell-therapy-research-development]
- 52. Common Problems When Training Deep Learning Models ... [https://medium.com/@lostandfound2654/common-problems-when-training-deep-learning-models-and-how-to-overcome-them-e37d0ac0a13b]
- 53. Optimization Rule in Deep Neural Networks [https://www.geeksforgeeks.org/deep-learning/optimization-rule-in-deep-neural-networks/]
- 54. Lecture 7: Troubleshooting Deep Neural Networks [https://fullstackdeeplearning.com/spring2021/lecture-7/]
- 55. 7 Machine Learning and Deep Learning Mistakes ... [https://www.exxactcorp.com/blog/Deep-Learning/7-Common-Machine-Learning-and-Deep-Learning-Mistakes-and-Limitations-to-Avoid]
- 56. Sensitive detection of rare disease-associated cell subsets ... [https://www.nature.com/articles/ncomms14825]
- 57. LLM Transformer Model Visually Explained [https://poloclub.github.io/transformer-explainer/]
- 58. Transformer (deep learning) [https://en.wikipedia.org/wiki/Transformer_(deep_learning)]
- 59. Rapid and accurate multi-phenotype imputation for millions ... [https://www.nature.com/articles/s41467-024-55496-0]
- 60. Multi-domain rule-based phenotyping algorithms enable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318046/]
- 61. 5 Gating Strategies To Get Your Flow Cytometry Data ... [https://expertcytometry.com/gating-strategies-get-your-flow-cytometry-data-published/]
- 62. Flow Cytometry Gating for Beginners [https://www.ptglab.com/news/blog/flow-cytometry-gating-for-beginners/?srsltid=AfmBOooqdtjH3Dt0CUPG0mDuI89DfELiqHOiwjGM3LPUg9Rn4WuIBY_I]
- 63. Comprehensive Guide to Gating Strategies in Flow Cytometry [https://www.bosterbio.com/blog/post/comprehensive-guide-to-gating-strategies-in-flow-cytometry?srsltid=AfmBOopV93ka-BGYlxbQy9AOLd8kZP0wznT_P05jk1UY6a3gWjaUli64]
- 64. Transforming Flow Cytometry with AI: Automating Gating ... [https://sababiomedicals.com/transforming-flow-cytometry-with-ai-automating-gating-and-simplifying-analysis/]
- 65. Making the most of high‐dimensional cytometry data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8453896/]
- 66. Comprehensive Guide to Gating Strategies in Flow Cytometry [https://www.bosterbio.com/blog/post/comprehensive-guide-to-gating-strategies-in-flow-cytometry?srsltid=AfmBOop2d8UjKywAfZcgyznHkMNV9m015M_Ck8G3R9g2WN1oPA99qt39]
- 67. Automated cytometric gating with human-level ... [https://www.nature.com/articles/s41467-025-56622-2]
- 68. 5 Basic questions and answers about high dimensional data [https://www.thinkingondata.com/5-basic-questions-and-answers-about-high-dimensional-data/]
- 69. Multiparameter Analysis of Murine Regulatory T Cells and ... [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/flow-cytometry/flow-cytometry-learning-center/flow-cytometry-resource-library/flow-cytometry-application-notes/multiparameter-analysis-murine-regulatory-t-cells-dendritic-cells-attune-nxt-flow-cytometer.html]
- 70. A computational approach for phenotypic comparisons of ... [https://www.sciencedirect.com/science/article/pii/S1046202317300452]
- 71. Troubleshooting Flow Cytometry Issues [https://www.bosterbio.com/protocol-and-troubleshooting/flow-cytometry-troubleshooting?srsltid=AfmBOorh6yvQS_MvSyvqIel1eNYfJGSec-5bCxGOCo_F8AoIm7Hq3jjn]
- 72. Purification of Low - abundant in the Drosophila Visual System Cells [https://www.jove.com/t/58474/purification-of-low-abundant-cells-in-the-drosophila-visual-system]
- 73. Unsupervised detection of rare events in liquid biopsy assays [https://www.nature.com/articles/s41698-025-01015-3]
- 74. Unsupervised Detection of Rare Events in Liquid Biopsy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11838382/]
- 75. Correction: What are Batch in Omics Data and How to... Batch Effects [https://bigomics.ch/blog/the-tricky-problem-of-batch-effects-in-biological-data/]
- 76. Assessing and mitigating batch in large-scale omics studies effects [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03401-9]
- 77. Doing more with less: reducing batch effects [https://www.colibri-cytometry.com/post/doing-more-with-less-reducing-batch-effects]
- 78. Diagnostics and correction of batch in large‐scale proteomic... effects [https://pmc.ncbi.nlm.nih.gov/articles/PMC8447595/]
- 79. controling for batch while preserving variation within repeated... effect [https://support.bioconductor.org/p/9154981/]
- 80. Correction | 10x Genomics Batch Effect [https://www.10xgenomics.com/analysis-guides/introduction-batch-effect-correction]
- 81. Multi-objective optimization of electromagnetic vibration ... [https://www.nature.com/articles/s41598-025-20846-5]
- 82. 15-MINUTE FACTS: Multi-parameter optimization [https://events.malvernpanalytical.com/W221130_multi-parameter-optimization]
- 83. Finding balance in drug discovery through multi-parameter ... [https://optibrium.com/webinars/finding-balance-in-drug-discovery-through-multi-parameter-optimisation/]
- 84. Federated Population-based Hyperparameter Tuning [https://arxiv.org/html/2308.08634]
- 85. Comparison of methods for tuning machine learning model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12083160/]
- 86. Research on Tomato Quality Prediction Models Based ... [https://www.mdpi.com/2223-7747/14/23/3569]
- 87. Designing a multicolor flow cytometry protocol [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/designing-a-multicolor-protocol]
- 88. Troubleshooting Flow Cytometry Issues [https://www.bosterbio.com/protocol-and-troubleshooting/flow-cytometry-troubleshooting?srsltid=AfmBOoryLzrMgdgkBB1bXH2XpMgR0sQD9RTIckDiekVQaq2K1EgrpawB]
- 89. How to Fix Flow Cytometry Compensation Errors (and ... [https://voices.uchicago.edu/ucflow/2021/08/09/how-to-fix-compensation-errors-and-unmixing-errors-bad-data-part-4/]
- 90. EuroFlow standardization of flow cytometer instrument ... [https://www.nature.com/articles/leu2012122]
- 91. Flow cytometry data standards - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3060130/]
- 92. Definitive Guide to AI/ML SaMD Ground Truthing [https://innolitics.com/articles/adjudication-strategies/]
- 93. Imaging flow cytometry: a primer - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10468826/]
- 94. On evaluation metrics for medical applications of artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8993826/]
- 95. Data Science in Medicine: Precision & Recall or Specificity ... [https://www.analyticsvidhya.com/blog/2024/06/data-science-in-medicine/]
- 96. F1 Score: Balancing Precision and Recall in AI Evaluation [https://galileo.ai/blog/f1-score-ai-evaluation-precision-recall]
- 97. Flow Cytometry Gating for Beginners [https://www.ptglab.com/news/blog/flow-cytometry-gating-for-beginners/?srsltid=AfmBOorufRg-N0E_C-t9FC2ZKA0_3TQ0yaFKLgJzuSytAHgEn06SSMot]
- 98. Comprehensive Guide to Gating Strategies in Flow Cytometry [https://www.bosterbio.com/blog/post/comprehensive-guide-to-gating-strategies-in-flow-cytometry?srsltid=AfmBOoqkyPig43ByvvCOUenaABUHZrf1EeXtCyHPaZAqDSBF721CjBM0]
- 99. Assessment of Automated Flow Cytometry Data Analysis ... [https://www.mdpi.com/1422-0067/23/6/3224]
- 100. Improving the Rigor and Reproducibility of Flow Cytometry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8043840/]
- 101. Automatic phenotyping using exhaustive projection pursuit [https://www.nature.com/articles/s42003-025-08581-z]
- 102. Automated flow cytometric analysis across large numbers ... [https://www.sciencedirect.com/science/article/pii/S1521661614002873]
- 103. Comprehensive Guide to Gating Strategies in Flow Cytometry [https://www.bosterbio.com/blog/post/comprehensive-guide-to-gating-strategies-in-flow-cytometry?srsltid=AfmBOoqUKXnBewkMHwOfs_tkrUzzpdziDHCoRlY4s2GUrI8dW5Yrg7bx]
- 104. A Harmonized Approach to Intracellular Cytokine Staining ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4443815/]
- 105. Comprehensive Guide to Gating Strategies in Flow Cytometry [https://www.bosterbio.com/blog/post/comprehensive-guide-to-gating-strategies-in-flow-cytometry?srsltid=AfmBOoq-cyGBvrdAAASzdVAi34aldcYSI12szjSuOml05ekyRnxYZK1H]
- 106. Flow Cytometry Troubleshooting Guide [https://fluorofinder.com/flow-cytometry-troubleshooting/]
- 107. Standardization procedure for flow cytometry data ... [https://www.nature.com/articles/s41598-020-68468-3]