Chemical Genetics Unveils Cross-Resistance Patterns: A Systematic Framework for Smarter Drug Development
This article explores how chemical genetics, a high-throughput functional genomics approach, is revolutionizing our understanding of cross-resistance and its counter-phenomenon, collateral sensitivity.
Chemical Genetics Unveils Cross-Resistance Patterns: A Systematic Framework for Smarter Drug Development
Abstract
This article explores how chemical genetics, a high-throughput functional genomics approach, is revolutionizing our understanding of cross-resistance and its counter-phenomenon, collateral sensitivity. Aimed at researchers and drug development professionals, we detail how systematic profiling of genome-wide mutant libraries against compound panels maps the complex networks of drug-pathogen interactions. The content covers foundational principles, key methodological advances like the Outlier Concordance–Discordance Metric (OCDM), and strategies to troubleshoot profiling data. We further validate these approaches with evidence from experimental evolution and discuss their application in designing intelligent drug cycling and combination therapies to outmaneuver resistance and extend the lifespan of existing and future therapeutics.
Decoding Cross-Resistance: Foundational Concepts and the Power of Systematic Mapping
The relentless evolution of antimicrobial resistance represents one of the most pressing challenges in modern medicine. When bacteria develop resistance to a specific antibiotic, this adaptation rarely occurs in isolation. Instead, it triggers a network of susceptibility changes to other antimicrobial agents—a phenomenon with critical implications for therapeutic strategies. Within this network, two contrasting patterns emerge: cross-resistance, where resistance to one drug confers resistance to another, and collateral sensitivity, where resistance to one drug increases susceptibility to another [1]. Understanding the balance between these opposing evolutionary trajectories is paramount for designing next-generation treatment protocols that can circumvent resistance development. Recent advances in chemical genetics have provided unprecedented insights into the systematic mapping of these interactions, revealing both the constraints and opportunities they present for antibiotic therapy [2]. This article delineates the fundamental distinctions between cross-resistance and collateral sensitivity, examines their underlying molecular mechanisms, and explores how these evolutionary trade-offs might be harnessed to combat the escalating antibiotic resistance crisis.
Defining the Concepts: Cross-Resistance vs. Collateral Sensitivity
Conceptual Frameworks and Definitions
- Cross-resistance: This occurs when a single resistance mechanism confers reduced susceptibility to two or more antibiotics, typically from the same class [1]. For example, a mutation in a bacterial topoisomerase gene may confer resistance to multiple fluoroquinolone antibiotics simultaneously [3].
- Collateral sensitivity: In this evolutionary trade-off, the development of resistance to one antibiotic leads to increased susceptibility to a second, unrelated antibiotic [1] [4]. This creates a potential Achilles' heel that can be therapeutically exploited.
While cross-resistance often arises from mechanisms that affect antibiotics with similar structures or targets, collateral sensitivity typically emerges from the fitness costs or physiological compromises associated with the resistance mechanism itself [5]. For instance, a mutation that reduces membrane potential to resist aminoglycosides may simultaneously impair efflux pump activity that depends on that same membrane potential, thereby sensitizing bacteria to other drug classes [4].
The Chemical Genetics Perspective
Chemical genetics provides a powerful framework for systematically mapping these interactions. By analyzing how thousands of individual gene deletions affect sensitivity to various antibiotics, researchers can predict cross-resistance and collateral sensitivity relationships on a genomic scale [2]. This approach has revealed that these interactions are far more extensive than previously recognized, with one study identifying 404 cases of cross-resistance and 267 of collateral sensitivity in Escherichia coli alone—expanding known interactions by more than threefold [2].
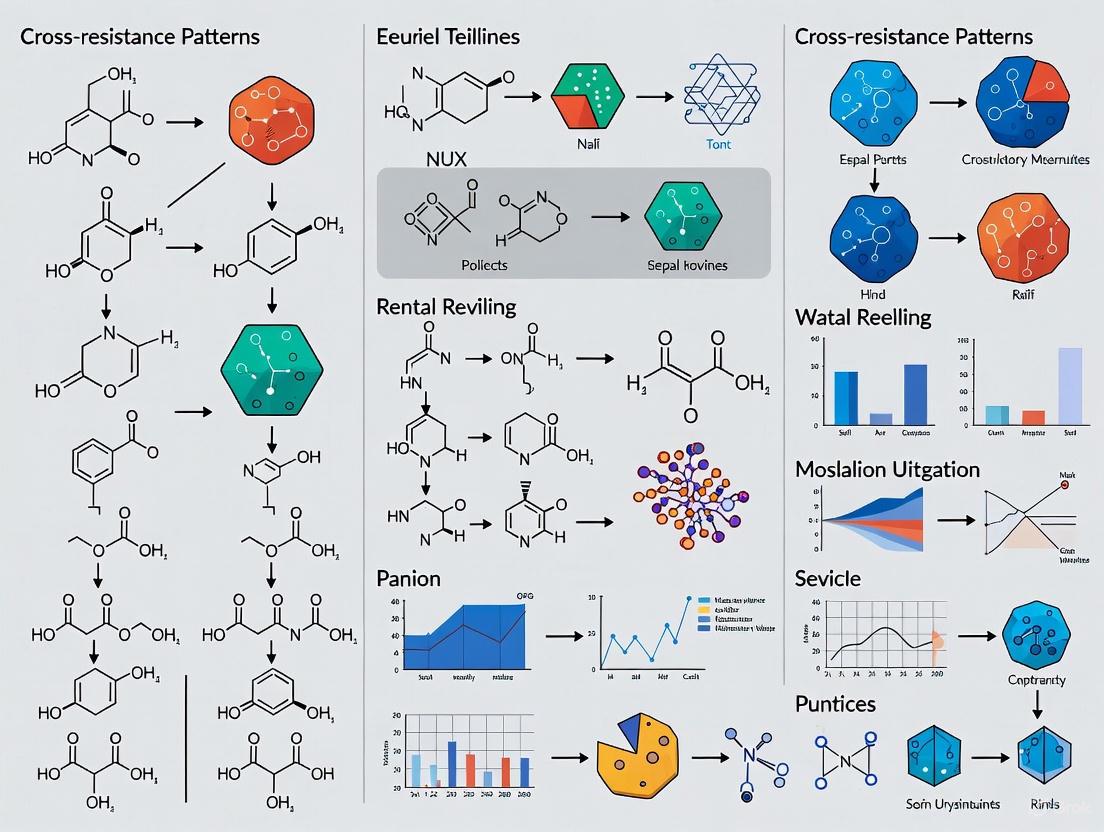
Diagram: Contrasting evolutionary pathways following antibiotic exposure. Cross-resistance limits future treatment options, while collateral sensitivity creates therapeutic opportunities.
Quantitative Landscape of Resistance Interactions
Systematic Mapping of Antibiotic Interactions
Chemical genetics approaches have enabled the comprehensive identification of cross-resistance and collateral sensitivity networks. The following table summarizes key quantitative findings from recent large-scale studies:
Table 1: Documented Cross-Resistance and Collateral Sensitivity Interactions
| Measurement Parameter | Cross-Resistance | Collateral Sensitivity | Experimental Context |
|---|---|---|---|
| Documented Interactions | 404 cases [2] | 267 cases [2] | E. coli chemical genetics screen of 40 antibiotics [2] |
| Validation Rate | 91% (64/70 inferred interactions) [2] | 91% (64/70 inferred interactions) [2] | Experimental evolution validation [2] |
| Multi-Species Observation | Common within same antibiotic classes [6] | Kanamycin CS in 5 species resistant to chloramphenicol/tetracycline [6] | 6 bacterial species with induced resistance [6] |
| Conservation Across Strains | Varies by mechanism | pOXA-48 plasmid: CS to azithromycin conserved in 8/9 clinical E. coli isolates [7] | Clinical E. coli isolates carrying resistance plasmid [7] |
| Temporal Dynamics | More frequent in early adaptation [8] | Increases with further selection [8] | Enterococcus faecalis evolution over 8 days [8] |
The data reveal that collateral sensitivity is not merely a theoretical concept but a widespread phenomenon with significant potential for clinical exploitation. The high validation rate of predicted interactions (91%) underscores the reliability of chemical genetics approaches for mapping these relationships [2].
Key Molecular Mechanisms and Their Prevalence
Different resistance mechanisms produce characteristic patterns of collateral effects. The table below summarizes major mechanistic categories and their observed prevalence:
Table 2: Molecular Mechanisms Driving Collateral Sensitivity
| Mechanism Category | Specific Example | Resulting Collateral Sensitivity | Experimental Evidence |
|---|---|---|---|
| Membrane Potential Alteration | Reduced PMF for aminoglycoside resistance [4] | Increased susceptibility to drugs expelled by PMF-dependent efflux pumps [4] | E. coli laboratory evolution [4] |
| Efflux Pump Modification | AcrAB efflux system impairment [4] | Increased intracellular concentrations of multiple drug classes [4] | Gene expression and susceptibility profiling [4] |
| Target Site Mutation | fusA mutations (EF-G) in kanamycin-resistant strains [6] | Hypersensitivity to β-lactams [6] | 5 bacterial species with convergent evolution [6] |
| Transcriptional Rewiring | Mutations in regulatory genes [4] | Altered expression of stress response pathways [4] | Genomic analysis of evolved strains [4] |
| Plasmid Acquisition | pOXA-48 carbapenemase plasmid [7] | Increased susceptibility to azithromycin and colistin [7] | Clinical E. coli isolates [7] |
Experimental Approaches and Methodologies
Chemical Genetics Profiling
Chemical genetics leverages systematic mutant libraries to comprehensively map gene-drug interactions. The foundational protocol involves:
- Library Preparation: Utilizing the E. coli single-gene deletion library (Keio collection), which comprises ~4,000 individual knockout mutants [2].
- Fitness Profiling: Exposing the mutant library to a panel of antibiotics (typically 40+ drugs) and quantifying bacterial fitness using growth measurements [2].
- Score Calculation: Computing s-scores that compare mutant fitness in each antibiotic condition to their fitness across all conditions [2].
- Interaction Inference: Applying the Outlier Concordance-Discordance Metric (OCDM) to identify antibiotic pairs where resistance mutations to one drug consistently increase sensitivity to another [2].
This approach enables the systematic prediction of collateral sensitivity networks without the need for extensive experimental evolution for each drug pair.
Experimental Evolution and Validation
To validate predicted interactions, researchers employ controlled evolution experiments:
- Selection Protocol: Exposing bacterial populations to increasing concentrations of a selecting antibiotic through serial passaging for multiple generations (typically 60+ generations) [8].
- Time-Series Sampling: Isolating clones at regular intervals (e.g., every 2 days) to track evolutionary trajectories [8].
- Susceptibility Testing: Measuring minimum inhibitory concentrations (MICs) or half-maximal inhibitory concentrations (IC50s) of evolved strains against a panel of antibiotics [6] [8].
- Genomic Analysis: Sequencing resistant clones to identify causal mutations and correlate genotypes with collateral sensitivity profiles [6].
Diagram: Integrated workflow combining chemical genetics prediction with experimental evolution validation to identify and characterize collateral sensitivity interactions.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents and Experimental Systems
| Reagent/System | Function/Application | Example Use Case |
|---|---|---|
| E. coli Keio Collection | Genome-wide single-gene knockout mutant library | Chemical genetics screening to identify gene-antibiotic interactions [2] |
| pOXA-48 Plasmid | Carbapenem-resistance conjugative plasmid | Studying collateral sensitivity associated with plasmid-borne resistance [7] |
| Outlier Concordance-Discordance Metric (OCDM) | Computational metric to identify CS/XR from chemical genetics data | Classifying antibiotic pairs into cross-resistance or collateral sensitivity categories [2] |
| Mutant Prevention Concentration (MPC) | Antibiotic concentration preventing single-step mutations | Evaluating resistance evolution at concentrations beyond MIC [3] |
| Disk Diffusion Assays | High-throughput susceptibility testing | Validating CS across diverse clinical isolates [7] |
Research Implications and Future Directions
The systematic mapping of collateral sensitivity networks opens promising avenues for addressing antibiotic resistance. Mathematical modeling suggests that CS-informed treatment schedules—including alternating therapies that exploit one-directional CS relationships—can suppress resistance evolution [9]. The conservation of CS patterns across diverse clinical isolates [7] and bacterial species [6] strengthens the potential for broad clinical application.
Future research should focus on expanding CS mapping to clinically relevant pathogens, elucidating the temporal dynamics of these relationships [8], and translating these findings into optimized treatment regimens. The integration of chemical genetics with experimental evolution provides a powerful framework for identifying exploitable evolutionary trade-offs, offering hope for extending the useful lifespan of existing antibiotics through smarter deployment strategies based on the fundamental principles of collateral sensitivity.
Chemical genetics is a powerful reverse genetics approach that systematically assesses the impact of genetic variation on the activity of a drug or chemical compound [10]. By measuring the quantitative fitness of a vast collection of genetic mutants when exposed to different chemicals, researchers can delineate a compound's complete cellular function—including its primary targets, its pathway into and out of the cell, and its mechanisms of cytotoxicity [10]. The field is propelled by technological advances that now enable the application of chemical genetics to almost any organism at an unprecedented throughput, making it an indispensable discovery engine in modern drug development [10].
The core principle of chemical genetics lies in its ability to map gene-chemical interactions on a genome-wide scale. This approach differs from broader chemical genomics, which includes large-scale screening of compound libraries for bioactivity against a specific cellular target or phenotype [10]. Chemical genetics specifically investigates how systematic genetic perturbations alter a cell's response to chemical treatment, creating rich datasets that reveal the complex functional relationships between small molecules and the biological systems they affect.
Fundamental Principles and Workflow
The chemical genetics workflow integrates systematic genetic perturbation with high-throughput phenotyping, followed by sophisticated computational analysis to extract biological insights.
Core Principles
Systematic Genetic Variance: Chemical-genetic approaches rely on genome-wide libraries containing mutants for each gene. These libraries can consist of loss-of-function (knockout, knockdown) or gain-of-function (overexpression) mutations and can be arrayed or pooled [10]. The creation of such libraries has been perfected in model organisms like yeast and E. coli and is now possible for a wide range of microbes and human cell lines [10].
Quantitative High-Throughput Phenotyping: Advances in barcoding strategies combined with next-generation sequencing allow for tracking the relative abundance—and thus fitness—of individual mutants in pooled libraries with exceptional throughput and dynamic range [10]. In arrayed formats, automation and advanced image processing enable the assessment of additional phenotypes beyond growth, including developmental processes like biofilm formation, sporulation, and morphological changes [10].
Guilt-by-Association Analysis: Compounds with similar chemical-genetic interaction profiles (or "signatures") are likely to share cellular targets and/or mechanisms of cytotoxicity [10]. This principle enables the classification of novel compounds through comparison to well-characterized reference molecules.
Experimental Workflow
The typical workflow for a chemical-genetics experiment involves the following key stages, as illustrated in the diagram below:
Diagram 1: Chemical genetics screening workflow.
The process begins with the preparation of a genome-wide mutant library, either pooled or arrayed. The library is then exposed to a compound of interest, typically at a sub-inhibitory concentration that induces a mild fitness defect (e.g., increasing the population doubling time by 2-fold) [11]. After a period of competitive growth (approximately 12 generations), the relative abundance of each mutant in the pool is determined, usually via deep sequencing of molecular barcodes [11]. Mutants that become under-represented indicate genes required for surviving the drug's effect (sensitivity-enhancing genes), while over-represented mutants reveal genes that confer resistance when perturbed (resistance-enhancing genes) [10] [11]. The compiled quantitative fitness scores for all mutants constitute the drug's unique signature, which can be compared to other signatures to infer common mechanisms.
Application in Mapping Cross-Resistance Patterns
Chemical-genetic profiling provides a powerful framework for understanding and predicting cross-resistance relationships between antimicrobial agents, a critical concern in combating drug resistance.
Revealing Determinants of Cross-Resistance
A key application of chemical genetics is the systematic assessment of cross-resistance and collateral sensitivity between drugs [10]. Cross-resistance occurs when a genetic mutation leads to reduced sensitivity to multiple drugs, while collateral sensitivity describes mutations that confer resistance to one drug but increase sensitivity to another [10]. Traditional methods of assessing these relationships involve evolving resistance to one drug and testing resistant clones against others, but this approach surveys only a limited number of potential resistance solutions [10].
Chemical genetics overcomes this limitation by simultaneously measuring the contribution of every non-essential gene to resistance across multiple compounds [11]. For example, a comprehensive study in E. coli that profiled 15 different antimicrobial peptides (AMPs) with diverse modes of action revealed that cross-resistance is prevalent only between AMPs with similar mechanisms [11]. This finding underscores that generalizations about AMP resistance are problematic, as resistance determinants vary considerably depending on the physicochemical properties and cellular targets of each peptide [11].
Experimental Data on Antimicrobial Peptide Cross-Resistance
The following table summarizes findings from a systematic chemical-genetic study of 15 AMPs, showing how they cluster based on their resistance determinants and modes of action [11]:
Table 1: Cross-Resistance Patterns and Characteristics of Antimicrobial Peptide Clusters
| Cluster | Primary Mode of Action | Representative AMPs | Key Physicochemical Properties | Cross-Resistance Pattern |
|---|---|---|---|---|
| C1 | Membrane targeting/Pore-forming | Ceratotoxin A, Mastoparan | Lower isoelectric point, high hydrophobicity, propensity for secondary structure | High within-cluster, limited between-cluster |
| C2 | Membrane targeting/Pore-forming | Melittin, Cecropin A | Moderate hydrophobicity, strong helical propensity | High within-cluster, limited between-cluster |
| C3 | Mixed membrane & intracellular | Indolicidin, Protamine, CAP18 | Intermediate properties | Moderate within-cluster |
| C4 | Intracellular targeting | Bactenecin 5, PR-39 | High proline content, intrinsic structural disorder | Limited cross-resistance with membrane-targeting AMPs |
The data demonstrates that AMPs cluster according to their modes of action and physicochemical properties, with distinct genetic determinants underlying resistance to each cluster [11]. This clustering reveals that intracellular-targeting AMPs are less likely to induce cross-resistance to membrane-targeting human host-defense peptides than those that share the same broad mechanisms, providing valuable insights for designing therapeutic AMPs that minimize cross-resistance concerns [11].
Experimental Protocol for Cross-Resistance Assessment
Protocol: Chemical-Genetic Profiling for Cross-Resistance Prediction in E. coli
- Library Preparation: Employ a comprehensive plasmid library overexpressing all ~4,400 E. coli open reading frames (ORFs) [11].
- Chemical Treatment: Grow the pooled plasmid library in the presence of each AMP at a sub-inhibitory concentration that increases the population doubling time by 2-fold [11]. Include an untreated control for each experiment.
- Competitive Growth: Allow the pool to grow for approximately 12 generations under selective pressure to ensure sufficient differential enrichment or depletion of clones [11].
- Sequencing and Fitness Scoring: Isolate the plasmid pool from each selection and determine the relative abundance of each plasmid by deep sequencing. Calculate a chemical-genetic interaction score (fold-change value) for each gene by comparing plasmid abundances in treated versus untreated conditions [11].
- Hit Identification: Identify genes that significantly increase sensitivity (sensitivity-enhancing) or decrease sensitivity (resistance-enhancing) upon overexpression using appropriate statistical thresholds [11].
- Signature Comparison: Compute pairwise similarity scores between the chemical-genetic interaction profiles of all tested AMPs. Use robust clustering methods to group AMPs with similar profiles [11].
- Cross-Resistance Prediction: Interpret clusters as groups of compounds with a high potential for cross-resistance due to shared resistance mechanisms.
This protocol successfully identified that cross-resistance is not universal but specific to AMPs with similar modes of action, enabling more informed selection of combination therapies and drug design strategies [11].
The Scientist's Toolkit: Essential Research Reagents
Conducting chemical-genetic studies requires specialized biological reagents and computational tools. The table below details key resources essential for implementing these approaches.
Table 2: Essential Research Reagents and Resources for Chemical-Genetic Studies
| Reagent/Resource | Type | Function in Chemical Genetics | Example Organisms |
|---|---|---|---|
| Knockout Mutant Library | Loss-of-function collection | Identifies genes essential for survival under drug treatment (sensitivity genes) | S. cerevisiae, E. coli, various bacteria & fungi [10] |
| Overexpression Library | Gain-of-function collection | Reveals latent resistome; genes that confer resistance when overexpressed | E. coli (e.g., ASKA library) [11] |
| CRISPRi/a Library | Essential gene knockdown/activation | Identifies drug targets among essential genes; modulates gene dosage precisely | Various bacteria, human cell lines [10] |
| Molecular Barcodes | DNA barcodes | Enables tracking of mutant abundance in pooled screens via high-throughput sequencing | S. cerevisiae, E. coli [10] |
| Hypomorph Library | Essential gene partial depletion | Assesses role of essential genes in drug susceptibility by titrating gene expression | E. coli [11] |
The selection of an appropriate mutant library is foundational to experimental design. Pooled libraries with barcoded mutants offer superior throughput for fitness screens, while arrayed libraries are suitable for capturing more complex phenotypic readouts such as morphological changes [10]. Recent advances have made it feasible to construct such libraries for a wide range of microorganisms, dramatically expanding the scope of chemical-genetic applications [10].
Data Analysis and Visualization
Transforming raw sequencing data from chemical-genetic screens into biological insights requires specialized computational and visualization approaches.
Analytical Approaches
The initial step in data analysis involves calculating robust fitness scores for each mutant under drug treatment compared to control conditions. Following this, researchers employ machine learning algorithms to interpret the resulting interaction networks. For instance, Naïve Bayesian and Random Forest algorithms have been successfully trained with chemical-genetics data to predict drug-drug interactions [10]. These models help distinguish interactions reflective of a drug's primary mechanism of action from those related to general stress responses or pathways controlling intracellular drug concentration.
Visualization of Chemical-Genetic Interaction Networks
A critical step in analysis is visualizing the relationships between compounds based on their chemical-genetic profiles, which often involves clustering techniques. The following diagram represents the process of analyzing and visualizing these relationships to predict cross-resistance:
Diagram 2: Analysis workflow for predicting cross-resistance.
This analytical workflow, as applied in the AMP study, shows how compounds cluster based on the similarity of their chemical-genetic interaction profiles [11]. AMPs within the same cluster (e.g., C1 or C2) show high potential for cross-resistance because they share similar resistance determinants, whereas AMPs from different clusters (e.g., C1 vs. C4) are less likely to exhibit cross-resistance [11]. This visualization helps researchers quickly identify groups of compounds with shared resistance mechanisms, guiding decisions about combination therapies and drug development priorities.
Chemical genetics serves as a powerful discovery engine by providing a systematic framework for elucidating the mechanisms of drug action, resistance, and cross-resistance. The methodology's true strength lies in its ability to survey the entire genetic landscape of an organism in a single experiment, offering a comprehensive view of how small molecules interact with biological systems. The principles and workflows outlined—from library construction and high-throughput phenotyping to advanced computational analysis—provide researchers with a robust toolkit for addressing the pressing challenge of antimicrobial resistance.
The application of chemical genetics to map cross-resistance patterns, as demonstrated with diverse antimicrobial peptides, reveals a critical principle: cross-resistance is not inevitable but is highly specific to shared mechanisms of action. This insight provides a strategic path for designing next-generation therapeutic agents with minimized cross-resistance risks, ultimately extending the utility of our existing antimicrobial arsenal and informing the development of more durable treatment regimens.
The growing crisis of antibiotic resistance has spurred innovative research in chemical genetics, providing unexpected insights for oncology. Studies systematically mapping cross-resistance (XR) and collateral sensitivity (CS)—phenomena where resistance to one drug confers resistance or sensitivity to another—have revealed fundamental principles of drug interactions and resistance evolution [2]. These findings now inform the development of Antimicrobial Peptides (AMPs) as a novel class of anticancer agents. AMPs, essential components of innate immunity across diverse species, demonstrate selective toxicity toward cancer cells while overcoming traditional chemotherapy resistance mechanisms [12] [13]. This review explores how chemical genetics principles are guiding the translation of AMPs into cancer therapeutics, comparing their performance against conventional treatments through structured experimental data and mechanistic analysis.
Table 1: Fundamental Concepts in Chemical Genetics and AMP Research
| Concept | Definition | Relevance to Cancer Therapy |
|---|---|---|
| Cross-Resistance (XR) | Resistance to one drug confers resistance to a second, unrelated drug [2]. | Limits efficacy of combination therapies; a challenge for conventional chemotherapy. |
| Collateral Sensitivity (CS) | Resistance to one drug confers heightened sensitivity to a second drug [2]. | Informs strategic drug cycling or combination therapies to suppress resistance. |
| Antimicrobial Peptide (AMP) | Naturally occurring, short-chain peptides with broad-spectrum antimicrobial activity [12] [13]. | A promising therapeutic class with selectivity for cancer cells and low resistance development. |
| Anticancer Peptide (ACP) | An AMP with demonstrated cytotoxic activity against cancer cells [12] [14]. | Directly exploits cancer cell membrane properties for selective killing. |
Chemical Genetics: A Framework for Understanding Drug Interactions
Chemical genetics provides a systematic framework for exploring drug interactions by assessing how genome-wide mutations affect susceptibility to pharmaceuticals. A pivotal 2025 study created a predictive model using chemical genetics data from an Escherichia coli single-gene deletion library exposed to 40 antibiotics [2]. By developing the Outlier Concordance–Discordance Metric (OCDM), researchers inferred 404 cases of XR and 267 of CS, expanding known interactions more than threefold and validating 64 of 70 predicted interactions experimentally [2]. This demonstrated that a single drug pair can exhibit XR or CS depending on the specific resistance mechanism, highlighting the complex landscape of resistance networks.
The methodology and application of this approach are summarized below.
Diagram 1: Chemical genetics workflow for mapping cross-resistance and collateral sensitivity.
Experimental Protocol for XR/CS Mapping
- Step 1: Library Preparation. Utilize a genome-wide single-gene deletion mutant library, such as the E. coli Keio collection [2].
- Step 2: Chemical Genetic Screening. Expose the mutant library to a panel of drugs (e.g., 40 antibiotics). Quantify fitness defects using a metric like the s-score, which compares a mutant's fitness in a condition to its fitness across all conditions [2].
- Step 3: Profile Comparison. Calculate similarity metrics between the chemical genetic profiles of all drug pairs. The OCDM metric prioritizes signals from extreme s-scores (both positive and negative) to distinguish XR (high profile concordance) from CS (high profile discordance) [2].
- Step 4: Validation. Experimentally evolve resistance to a first drug in multiple lineages. Then, measure the susceptibility (e.g., Minimum Inhibitory Concentration) of these evolved populations to a second drug to confirm predicted XR or CS interactions [2].
Antimicrobial Peptides as Promising Anticancer Agents
AMPs are short (10-50 amino acids), cationic, and amphipathic peptides that are a cornerstone of innate immunity [13] [15]. Their transition from antimicrobial to anticancer agents stems from their ability to selectively target cancer cells with a low propensity for inducing resistance—addressing two major limitations of conventional chemotherapy [12] [16].
Key Structural Classes and Mechanisms of Action
The anticancer activity of AMPs, often termed ACPs, is heavily influenced by their physicochemical properties and secondary structures [12] [14]. The primary mechanism for their selectivity is the electrostatic interaction between the positively charged ACPs and the negatively charged components abundant on cancer cell membranes, such as phosphatidylserine, O-glycosylated mucins, and sialylated gangliosides [16].
Table 2: Structural Classes and Anticancer Mechanisms of Select AMPs/ACPs
| ACPs Name | Structure | Source | Cancer Type/Cell Line Tested | Proposed Mechanism of Action |
|---|---|---|---|---|
| Magainin 2 | α-helical | African clawed frog | Bladder, Breast [12] | Membrane disruption [16] |
| Buforin IIb | α-helical | Asian toad | Leukemia, Breast, Lung [12] | Membrane translocation; targets intracellular components [12] |
| Human neutrophil peptide (HNP-1) | β-pleated sheet | Human | Prostate cancer [12] | Membrane disruption; apoptosis [12] |
| Bovine lactoferricin (LfcinB) | β-pleated sheet | Bovine milk | Stomach cancer [12] | Membrane disruption; induction of apoptosis [14] |
| LL-37 | α-helical | Human (Neutrophils) | Colorectal cancer [12] | Membrane disruption; immunomodulation [15] |
| WK-13-3D | Not specified | Synthetic/Antimicrobial | Triple-negative breast cancer [17] | Binds BiP protein; induces ER stress, apoptosis, and autophagy [17] |
The following diagram illustrates the primary mechanisms by which cationic AMPs (CAMPs) target and kill cancer cells.
Diagram 2: Mechanisms of anticancer action for cationic antimicrobial peptides.
Comparative Efficacy: ACPs vs. Conventional Chemotherapy
The therapeutic potential of ACPs is most evident when directly compared with conventional cancer treatments. ACPs offer a distinct set of advantages rooted in their unique mechanisms of action.
Table 3: Performance Comparison: ACPs vs. Conventional Chemotherapy
| Feature | Anticancer Peptides (ACPs) | Conventional Chemotherapy |
|---|---|---|
| Selectivity | High. Selective for negatively charged cancer cell membranes [13] [14]. | Low. Targets all rapidly dividing cells, healthy and cancerous [16]. |
| Mechanism of Action | Multiple: Membrane disruption, apoptosis induction, immunomodulation [13] [15]. | Typically single-target (e.g., DNA damage, antimetabolites) [16]. |
| Risk of Resistance | Low. Targets the hard-to-alter membrane structure; short interaction time [14] [15]. | High. Common through drug efflux, target alteration, and DNA repair [16]. |
| Spectrum of Activity | Broad-spectrum activity against various cancer types [12] [13]. | Often specific to cancer types or molecular subtypes. |
| Immunogenicity | Low antigenicity; some are immunomodulatory [13] [16]. | Can be immunogenic or immunosuppressive. |
| Primary Toxicity Concerns | Hemolytic activity at high concentrations; can be engineered for reduced toxicity [14]. | Severe side effects (myelosuppression, mucositis, alopecia) are common [16]. |
Illustrative Experimental Data
Preclinical studies provide quantitative evidence for ACP efficacy. For instance:
- Dermaseptin B2 (from Phyllomedusa frog) showed potent activity against prostate cancer cells (PC3, DU145, LnCap) with dosages ranging from 0.71 to 2.65 μM [12].
- Brevenin-2R (from frog skin) exhibited cytotoxic effects on breast cancer (MCF-7), T-cell leukemia (Jurkat), and B-cell lymphoma (BJAB) cells at concentrations of 10-40 μg/ml [12].
- In a specific study on triple-negative breast cancer, the peptide WK-13-3D was shown to promote apoptosis, autophagy, and ubiquitination by binding to the immunoglobulin protein (BiP), demonstrating a specific intracellular target [17].
The Scientist's Toolkit: Essential Reagents and Methods
Advancing AMP research from bench to bedside relies on a specific toolkit of reagents, computational resources, and experimental methodologies.
Table 4: Key Research Reagent Solutions for AMP/ACP Investigation
| Tool / Reagent | Function/Description | Example Use in AMP Research |
|---|---|---|
| Cationic, Amphipathic Peptides | The core therapeutic agent; typically +2 to +9 net charge, 50% hydrophobicity [14]. | Serve as lead compounds for testing against cancer cell lines. Can be natural or synthetically modified. |
| Database of Antimicrobial Activity and Structure of Peptides (DBAASP) | Public database cataloging over 15,700 peptides with structural and activity data [18]. | Source for identifying novel ACP candidates and analyzing structure-activity relationships (SAR). |
| Cancer Cell Line Panel | A diverse set of validated cancer cell lines (e.g., from ATCC). | For in vitro screening of ACP cytotoxicity and selectivity (e.g., MCF-7, PC-3, Jurkat) [12]. |
| Kirby-Bauer Disk Diffusion / Broth Microdilution | Standard phenotypic antimicrobial susceptibility tests [19]. | Used in parallel to confirm and quantify the retained antimicrobial activity of ACPs [19]. |
| 3D Tumor Spheroids | Multicellular aggregates that better mimic the in vivo tumor microenvironment than 2D cultures. | For advanced in vitro testing of ACP penetration and efficacy in a more physiologically relevant model. |
| Artificial Intelligence (AI) Models | Computational frameworks (e.g., VAEs, LSTMs, GANs) for de novo AMP design and optimization [18]. | To predict and generate new ACP sequences with desired properties (e.g., high efficacy, low toxicity). |
The principles uncovered by chemical genetics—specifically the networks of cross-resistance and collateral sensitivity—provide a powerful lens through which to develop the next generation of oncology therapeutics. Antimicrobial peptides represent a compelling class of agents operating within this framework. Their selective mechanism of action, broad-spectrum activity, and low propensity for resistance position them as promising candidates to address the limitations of conventional chemotherapy [13] [14]. Future research will focus on optimizing their physicochemical properties (charge, hydrophobicity), developing novel delivery strategies (e.g., nano-carriers) to improve stability and targeting, and exploring synergistic combinations with other therapeutics based on CS principles [2] [15]. As these studies progress, AMPs are poised to move from promising experimental compounds to mainstays in the clinical arsenal against cancer.
Chemical-genetic interaction profiling represents a powerful reverse genetics approach that systematically quantifies how genetic perturbations influence cellular susceptibility to chemical compounds [10]. This methodology involves screening comprehensive mutant libraries—including single-gene deletions, hypomorphs (partially depleted essential genes), or gene overexpression collections—against diverse chemical compounds to generate fitness profiles that reveal functional relationships between genes and small molecules [10] [20]. The resulting interaction profiles capture two fundamental relationships: concordance, where similar fitness responses across mutants indicate shared mechanisms of action or resistance pathways; and discordance, where opposing fitness responses reveal collateral sensitivity or functionally distinct pathways [2] [21].
In the context of antibiotic discovery and resistance research, these profiles provide critical insights into cross-resistance patterns—a phenomenon where resistance to one drug confers resistance to another—and collateral sensitivity, where resistance to one drug increases sensitivity to another [2]. The systematic mapping of these relationships through chemical-genetic approaches has expanded our understanding of antibiotic interactions substantially, revealing 404 cases of cross-resistance and 267 cases of collateral sensitivity in Escherichia coli alone, representing a threefold and sixfold expansion respectively over previously known interactions [2] [21]. This review examines the methodological frameworks, interpretive principles, and practical applications of concordance and discordance analysis in chemical-genetic interaction profiling, with particular emphasis on implications for antimicrobial drug development.
Methodological Frameworks for Profile Generation
Experimental Platforms and Genetic Libraries
Chemical-genetic interaction profiling relies on specialized experimental platforms that enable high-throughput screening of mutant libraries under chemical treatment conditions. The PROSPECT (PRimary screening Of Strains to Prioritize Expanded Chemistry and Targets) platform represents one such system developed specifically for Mycobacterium tuberculosis, which utilizes a pooled collection of hypomorphic mutants depleted of different essential proteins [22]. Each mutant strain contains a unique DNA barcode that enables quantification via next-generation sequencing, allowing parallel assessment of mutant abundance changes in response to compound exposure [22]. Similarly, in E. coli studies, genome-wide single-gene deletion libraries or comprehensive gene overexpression collections are employed to systematically map resistance determinants [2] [20].
These platforms share common technical approaches: (1) pooled mutant libraries grown in competitive culture with and without compound treatment; (2) barcode sequencing to quantify relative fitness of each strain; (3) calculation of fitness scores representing chemical-genetic interactions; and (4) comparative analysis to identify patterns of concordance and discordance [22] [20]. For essential genes that cannot be deleted, hypomorphs with titratable depletion or CRISPRi knockdown libraries are utilized to capture their contribution to chemical susceptibility [22] [10]. The resulting data matrices, comprising fitness scores for each mutant under each condition, form the basis for subsequent concordance and discordance analysis.
Quantitative Metrics and Scoring Systems
The quantitative analysis of chemical-genetic interactions employs specialized scoring systems to represent mutant fitness under chemical treatment. In the PROSPECT platform, chemical-genetic interaction (CGI) profiles are represented as vectors of hypomorph responses, with significant negative scores indicating hypersensitivity and positive scores indicating resistance [22]. In E. coli studies, s-scores typically represent standardized fitness measurements comparing growth in treated versus untreated conditions, with extreme scores (both positive and negative) indicating significant interactions [2].
For cross-resistance and collateral sensitivity mapping, the Outlier Concordance-Discordance Metric (OCDM) has been developed specifically to distinguish between these interaction types [2] [21]. This metric utilizes six features derived from extreme s-scores: the sum and count of positive concordant s-scores, negative concordant s-scores, and total discordant s-scores [2]. The OCDM prioritizes concordance signals when defining cross-resistance relationships, while requiring both high discordance and minimal concordance for collateral sensitivity assignments [2]. This approach achieved 91% validation accuracy when tested against experimentally evolved resistant strains [2].
Table 1: Key Chemical-Genetic Screening Platforms and Their Applications
| Platform/Organism | Library Type | Primary Readout | Key Applications | References |
|---|---|---|---|---|
| PROSPECT (M. tuberculosis) | 600 hypomorphic essential gene mutants | DNA barcode sequencing | MOA prediction, hit prioritization | [22] |
| E. coli chemical genetics | Single-gene deletion library | S-scores from pooled growth | Cross-resistance mapping, collateral sensitivity | [2] [21] |
| E. coli overexpression | Genome-wide ORF overexpression | Fold-change in plasmid abundance | Resistance gene identification, latent resistome | [20] [11] |
| Yeast chemical genetics | Heterozygous deletion library | HIP/HOP profiling | Target identification, mechanism of action | [10] |
Analytical Approaches for Concordance/Discordance Assessment
Reference-Based Profiling and Machine Learning Classification
Reference-based profiling approaches enable mechanism of action prediction by comparing unknown compounds to curated sets with annotated targets. The Perturbagen Class (PCL) analysis method exemplifies this strategy, utilizing a reference set of 437 compounds with known mechanisms of action to infer MOA for novel compounds based on profile similarity [22]. In leave-one-out cross-validation, this approach achieved 70% sensitivity and 75% precision in MOA prediction, with comparable performance (69% sensitivity, 87% precision) when applied to a test set of 75 antitubercular compounds from GlaxoSmithKline [22].
Machine learning classifiers significantly enhance the discrimination between cross-resistance and collateral sensitivity interactions. Decision tree models trained on extreme s-score features (sum and count of positive concordant, negative concordant, and discordant s-scores) achieve F1 scores, recall, precision, and ROC AUC values exceeding 0.7 [2]. These models identify the sum and count of concordant negative s-scores as the most informative features, followed by the sum of discordant s-scores [2]. The performance of these classifiers demonstrates the predictive power of chemical-genetic profiles for anticipating resistance outcomes before extensive experimental evolution is required.
Profile Similarity Metrics and Clustering Algorithms
Similarity assessment between chemical-genetic profiles employs correlation-based metrics and clustering algorithms to group compounds with shared mechanisms. Correlation coefficients between replicate measurements typically exceed r = 0.63, indicating sufficient reproducibility for comparative analysis [20]. For antimicrobial peptides, clustering based on chemical-genetic interaction profiles reveals four distinct groups (C1-C4) that correspond with membrane-targeting versus intracellular-targeting mechanisms and reflect underlying physicochemical properties [20] [11].
The diagram below illustrates the conceptual relationship between profile similarity and drug interaction outcomes:
Diagram 1: Interpretation of profile similarity. High concordance indicates cross-resistance, while high discordance indicates collateral sensitivity. Neutral profiles show neither pattern.
Unsupervised clustering of chemical-genetic profiles enables mechanism of action prediction without pre-defined reference sets. In one comprehensive study of 15 antimicrobial peptides, clustering based on overexpression profiles grouped AMPs according to their membrane-targeting versus intracellular-targeting mechanisms, with distinct physicochemical properties characterizing each cluster [20]. Membrane-targeting AMPs exhibited lower isoelectric points, reduced proline content, and increased hydrophobicity, while intracellular-targeting AMPs showed higher structural disorder propensity [20]. These clustering approaches provide orthogonal validation of mechanism-based groupings and can reveal unexpected relationships between compounds.
Table 2: Performance Metrics for Chemical-Genetic Prediction Methods
| Prediction Method | Application Context | Sensitivity | Precision | Validation Approach | References |
|---|---|---|---|---|---|
| PCL Analysis | MOA prediction in M. tuberculosis | 70% | 75% | Leave-one-out cross-validation | [22] |
| PCL Analysis | GSK compound set MOA prediction | 69% | 87% | Test set with known MOA | [22] |
| OCDM Metric | Cross-resistance prediction in E. coli | 73% (AUC) | N/A | Experimental evolution (91% validation) | [2] [21] |
| OCDM Metric | Collateral sensitivity prediction | 76% (AUC) | N/A | Experimental evolution (91% validation) | [2] [21] |
Experimental Validation of Profile-Based Predictions
Genetic and Phenotypic Validation Approaches
Experimental validation of predictions derived from chemical-genetic profiles employs both genetic and phenotypic approaches. For compounds predicted to target specific pathways, resistance mutation induction provides compelling validation; for instance, compounds predicted to target QcrB (a subunit of the cytochrome bcc-aa3 complex) in M. tuberculosis were validated by demonstrating reduced activity against strains carrying known qcrB resistance alleles [22]. Similarly, hypersensitization tests using mutants lacking alternative pathways (such as cytochrome bd deletion mutants in the case of QcrB inhibitors) provide orthogonal confirmation [22].
Phenotypic validation includes minimum inhibitory concentration (MIC) determination against engineered strains and wild-type controls. For AMP resistance predictions, MIC comparisons between wild-type and resistant strains evolved in the laboratory confirmed that cross-resistance occurs primarily between AMPs with similar modes of action [20] [11]. In this validation, 83% of tested chemical-genetic interactions showed MIC changes in the expected direction, with resistance-enhancing gene overexpression increasing MIC ~1.6-fold and sensitivity-enhancing overexpression decreasing MIC ~0.7-fold on average [20].
Application in Combination Therapy Design
Chemical-genetic interaction profiling directly informs combination therapy design by identifying drug pairs with collateral sensitivity relationships that can suppress resistance emergence. When collateral-sensitive drug pairs are applied in combination, they significantly reduce resistance development compared to single-drug treatments [2]. This approach leverages the fundamental principle that resistance mechanisms conferring protection against one drug create vulnerabilities to another, creating evolutionary constraints that limit adaptation.
The experimental workflow below illustrates how chemical-genetic data informs combination therapy design:
Diagram 2: From chemical-genetic profiling to combination therapy. Profile similarity analysis identifies collateral sensitivity and cross-resistance patterns, informing combination therapy design that limits resistance emergence.
Systematic mapping of collateral sensitivity networks has revealed that certain antibiotic classes exhibit particularly extensive collateral sensitivity interactions, making them promising candidates for combination regimens [2]. Conversely, antibiotics with extensive cross-resistance networks can be identified for segregated use to prevent multi-drug resistance emergence. This empirical approach to combination design complements traditional synergy screening by incorporating evolutionary trajectories into therapeutic planning.
Research Reagent Solutions for Chemical-Genetic Studies
Table 3: Essential Research Reagents for Chemical-Genetic Interaction Profiling
| Reagent/Library Type | Key Examples | Primary Applications | Technical Considerations | |
|---|---|---|---|---|
| Hypomorphic mutant libraries | M. tuberculosis PROSPECT library (600 essential gene hypomorphs) | MOA identification, compound sensitization | Titratable protein depletion; barcoded for pooled screening | [22] |
| Single-gene deletion libraries | E. coli Keio collection | Resistance gene identification, fitness defect profiling | Covers non-essential genes; arrayed or pooled formats | [2] [10] |
| Gene overexpression libraries | E. coli ASKA collection | Resistance gene discovery, target identification | Genome-wide ORF overexpression; latent resistome mapping | [20] [11] |
| CRISPRi essential gene libraries | M. tuberculosis CRISPRIi library | Essential gene knockdown, target validation | Tunable gene suppression; complex maintenance | [10] |
| Barcoded mutant pools | Pooled yeast deletion collection | Fitness profiling, chemical-genetic interactions | Deep sequencing readout; high parallelism | [10] |
Discussion and Future Perspectives
Chemical-genetic interaction profiling has established itself as an indispensable methodology for elucidating compound mechanism of action, predicting resistance relationships, and guiding therapeutic combinations. The systematic interpretation of concordance and discordance patterns within these profiles provides a powerful framework for anticipating cross-resistance and collateral sensitivity before they emerge in clinical settings. As chemical-genetic data sets expand across diverse pathogens and compound libraries, their predictive power will continue to increase.
Future developments in this field will likely focus on integrating chemical-genetic data with other functional genomics approaches, including metabolomic and transcriptomic profiling, to create multi-dimensional views of compound mechanism. Additionally, machine learning approaches trained on these integrated data sets may further enhance prediction accuracy for both mechanism of action and resistance outcomes. The application of these methods to complex clinical isolates, rather than laboratory reference strains, represents another critical frontier for translating these approaches to therapeutic development.
As antibiotic resistance continues to threaten global health, chemical-genetic interaction profiling offers a rational path forward for designing combination therapies that proactively manage resistance evolution. By leveraging the fundamental principles of concordance and discordance, researchers can strategically deploy antimicrobial agents to create evolutionary traps that suppress resistance development, extending the clinical lifespan of existing antibiotics and guiding the development of new agents with optimal resistance properties.
From Data to Insights: Methodological Advances and Predictive Modeling in Chemical Genetics
High-throughput profiling of genome-wide mutant libraries is a cornerstone of modern functional genomics, enabling the systematic identification of genes essential for specific biological functions or phenotypes. Within chemical genetics research, these screens are indispensable for deciphering complex cross-resistance patterns—the phenomenon where resistance to one compound confers resistance or hypersensitivity to another. Understanding these patterns is crucial for drug development, as it reveals potential therapeutic synergies, anticipates resistance mechanisms, and uncovers the underlying functional networks within cells.
The field is primarily driven by three powerful technological approaches: chemical mutagenesis, CRISPR-based libraries, and chemical-genetic interaction profiling. Each method offers distinct advantages, limitations, and insights into how genetic perturbations influence phenotypic outcomes and compound resistance. This guide provides a comparative analysis of these platforms, supported by experimental data and detailed protocols, to inform researchers in selecting the optimal strategy for their specific screening objectives.
Platform Comparison: Methodologies and Performance Metrics
The table below summarizes the core characteristics and performance data of the three main high-throughput profiling platforms.
Table 1: Comparative overview of high-throughput profiling platforms for genome-wide mutant libraries
| Screening Platform | Mutagenesis Mechanism | Key Readout | Typical Library Size | Mutant Type | Key Advantages | Primary Applications |
|---|---|---|---|---|---|---|
| Chemical Mutagenesis [23] | Ethylmethanesulfonate (EMS)-induced single-nucleotide variants (SNVs) | Whole-exome sequencing of resistant clones | ~370 SNVs per clone [23] | Primarily recessive point mutations | Identifies gain-of-function and separation-of-function alleles; defines critical protein domains | Comprehensive identification of suppressor/resistance loci; functional domain mapping |
| CRISPR Libraries [24] | CRISPR/Cas9-mediated gene knockout, activation, or repression | Next-generation sequencing of guide RNA (gRNA) abundance | Tens of thousands of single-guide RNAs (sgRNAs) [24] | Primarily loss-of-function (gene knockout) | High efficiency, multifunctionality, low background noise, precise targeting | Deciphering key regulators in tumorigenesis, drug resistance mechanisms, immunotherapy optimization |
| Chemical-Genetic Profiling [20] | Overexpression or depletion of ~4,400 E. coli genes | Growth kinetics monitored by deep sequencing of plasmid abundance | ~4,400 gene overexpressions [20] | Altered gene dosage (overexpression/hypomorph) | Maps "latent resistome"; clusters compounds by mode of action; reveals antagonistic interactions | Profiling cross-resistance patterns; mapping antibiotic modes of action; identifying cellular targets |
Performance metrics vary significantly between these platforms. In chemical mutagenesis screens, a proof-of-concept study for 6-thioguanine (6-TG) resistance in haploid mouse embryonic stem cells (mESCs) successfully identified point mutations in all known suppressor genes, with approximately 11.3% of induced mutations affecting coding sequences in a non-synonymous way [23]. CRISPR screens are characterized by their high efficiency and specificity, though they can be confounded by off-target effects [24]. Chemical-genetic interaction profiling, which measures how gene overexpression influences drug susceptibility, has demonstrated high reproducibility (Pearson correlation r = 0.63 between replicates) and validation rates, with 83% of tested interactions confirming changes in minimum inhibitory concentration (MIC) as expected [20].
Experimental Protocols for Key Screening Methodologies
Protocol A: Chemical Mutagenesis Screening in Haploid Cells
This protocol, adapted from a study screening for 6-TG resistance, leverages haploid cells to efficiently identify recessive mutations [23].
- Step 1: Library Generation. Treat haploid mammalian cells (e.g., H129-3 mESCs) with a chemical mutagen such as EMS. Titrate the EMS dose to achieve a balance between mutation density and cell viability.
- Step 2: Phenotypic Selection. Subject the mutagenized cell population to selective pressure, such as a cytotoxic drug like 6-TG, over multiple cell doublings to enrich for resistant clones.
- Step 3: Clone Isolation and Sequencing. Isclude individual resistant clones and extract genomic DNA. Perform whole-exome sequencing to identify homozygous single-nucleotide variants (SNVs) and insertions/deletions (INDELs).
- Step 4: Candidate Gene Identification. Bioinformatically filter sequencing data to focus on non-synonymous coding mutations. Prioritize genes that are mutated in multiple independent clones and/or carry mutations predicted to be deleterious.
Protocol B: Chemical-Genetic Interaction Profiling
This protocol maps genes that influence susceptibility to antimicrobial peptides (AMPs) or other compounds through overexpression [20].
- Step 1: Library Preparation. Create a pooled plasmid library designed to overexpress nearly every open reading frame (ORF) in the genome (e.g., ~4,400 for E. coli).
- Step 2: Competitive Growth Assay. Grow the pooled library in the presence of a sub-inhibitory concentration of the AMP (concentration that increases population doubling time by 2-fold) and in an untreated control for approximately 12 generations.
- Step 3: Sequencing and Abundance Quantification. Isolate plasmids from both conditions and use deep sequencing to determine the relative abundance of each overexpression plasmid.
- Step 4: Interaction Score Calculation. For each gene, compute a chemical-genetic interaction score by comparing plasmid abundance in the treated versus untreated pools. Identify "resistance-enhancing" genes (overexpression increases survival) and "sensitivity-enhancing" genes (overexpression decreases survival).
Analysis of Cross-Resistance Patterns in Chemical Genetics
Chemical-genetic interaction profiling is particularly powerful for elucidating cross-resistance patterns. A systematic study of 15 different AMPs in E. coli revealed that cross-resistance is not universal but is highly dependent on the compound's mode of action [20].
The analysis of chemical-genetic interaction profiles led to the clustering of AMPs into distinct groups (C1-C4) based on the similarity of genes that, when overexpressed, altered susceptibility. AMPs within the same cluster, and thus with similar interaction profiles, showed a high degree of cross-resistance. Conversely, AMPs from different clusters, particularly those with membrane-targeting (C1, C2) versus intracellular-targeting (C3, C4) modes of action, showed minimal cross-resistance [20]. This indicates that resistance mechanisms are highly specific to the compound's primary cellular target.
Table 2: Cross-resistance insights from chemical-genetic profiling of 15 antimicrobial peptides (AMPs)
| AMP Cluster | Primary Mode of Action | Key Physicochemical Properties | Cross-Resistance Observation | Implication for Drug Design |
|---|---|---|---|---|
| C1 & C2 [20] | Membrane disruption/pore-formation | Higher hydrophobicity, lower isoelectric point, high propensity for secondary structure | Prevalent between AMPs within the same cluster | Combining membrane-targeting AMPs may lead to shared resistance |
| C3 & C4 [20] | Intracellular targets (e.g., protein/DNA synthesis) | Lower hydrophobicity, higher proline content | Minimal cross-resistance to membrane-targeting human host-defense peptides | Intracellular-targeting therapeutic AMPs may avoid cross-resistance with innate immunity |
This data provides a strategic framework for selecting combination therapies and designing novel therapeutic AMPs that minimize the risk of cross-resistance to human host-defense peptides, a key consideration for long-term efficacy [20].
Essential Research Reagents and Materials
The successful execution of high-throughput profiling screens relies on a suite of specialized reagents and tools.
Table 3: Key research reagent solutions for high-throughput profiling
| Reagent / Tool Name | Provider Examples | Function in Screening |
|---|---|---|
| Exome Capture Panels [25] | BOKE, IDT, Nanodigmbio, Twist Bioscience | Hybridization-based enrichment of genomic exon regions for efficient variant discovery via sequencing. |
| Haploid Mammalian Cells [23] | Various cell repositories | Enable identification of recessive mutations in a single genetic screen, simplifying analysis. |
| CRISPR Library sgRNAs [24] | Commercially available or custom-designed | Target specific genomic loci for knockout, activation, or repression in pooled screens. |
| Pooled ORF Overexpression Libraries [20] | Academic and commercial sources | Systematically modulate gene dosage to identify resistance and sensitivity-enhancing genes. |
| MGIEasy UDB Library Prep Set [25] | MGI | Facilitates high-throughput, automated library construction with unique dual indexing for sample multiplexing. |
| DNBSEQ-T7 Sequencer [25] | MGI | High-throughput sequencing platform providing the read depth required for complex pooled library screens. |
The choice of a high-throughput profiling platform is dictated by the specific biological question. Chemical mutagenesis remains unparalleled for discovering novel resistance loci and generating a spectrum of point mutations that reveal critical functional residues and domains [23]. CRISPR libraries offer a direct, programmable, and highly specific approach for genome-wide loss-of-function studies, making them ideal for systematically probing gene function in disease contexts like cancer [24]. Finally, chemical-genetic interaction profiling provides a unique map of the "latent resistome," powerfully clustering compounds by their mode of action and predicting cross-resistance patterns, which is invaluable for antibiotic development and understanding drug interactions [20].
Integrating data from these complementary approaches provides a more comprehensive understanding of the genetic wiring underlying drug response and resistance, ultimately accelerating the development of robust therapeutic strategies.
The Outlier Concordance–Discordance Metric (OCDM) represents a significant methodological advancement in the analysis of chemical-genetic interactions for predicting antibiotic cross-resistance (XR) and collateral sensitivity (CS). Developed to overcome the limitations of traditional experimental evolution approaches, OCDM provides a computational framework that systematically quantifies how resistance to one antibiotic affects susceptibility to others by leveraging genome-wide mutant fitness data [21].
In the critical challenge of antimicrobial resistance, understanding these relationships is paramount. Cross-resistance occurs when resistance to one drug confers resistance to another, further limiting treatment options. Conversely, collateral sensitivity describes the scenario where resistance to one drug increases sensitivity to another, revealing potential strategies for combination or cycling therapies [21]. Traditional methods for mapping these interactions rely on experimental evolution followed by susceptibility testing, which probes only a limited genetic space and requires extensive resources [21]. OCDM overcomes these limitations by using chemical-genetic profiles to predict interactions computationally before experimental validation.
How OCDM Works: Mechanism and Workflow
Theoretical Foundation
OCDM operates on a fundamental premise derived from chemical genetics: antibiotics with concordant fitness profiles across a genome-wide mutant library likely share resistance mechanisms, predicting cross-resistance. Conversely, antibiotics with discordant fitness profiles suggest that mutations conferring resistance to one drug increase sensitivity to the other, indicating collateral sensitivity [21].
The metric was developed using chemical-genetic interaction data from an Escherichia coli single-gene deletion library screened against 40 different antibiotics. In this data, drug effects on each mutant are represented by s-scores, which quantify a mutant's fitness in a specific condition relative to its fitness across all tested conditions [21]. Rather than using all s-score data, which contains considerable neutral noise, OCDM focuses specifically on extreme s-scores (outliers) that represent the most significant fitness effects [21].
Algorithm and Calculation
The OCDM algorithm utilizes six key features derived from the extreme s-scores in chemical-genetic profiles [21]:
- Sum of positive concordant s-scores
- Count of positive concordant s-scores
- Sum of negative concordant s-scores
- Count of negative concordant s-scores
- Sum of discordant s-scores
- Count of discordant s-scores
Through training decision tree models, researchers identified that the sum and count of concordant negative s-scores were the most informative features for classification, followed by the sum of discordant s-scores [21]. The resulting OCDM metric prioritizes concordance signals when defining interactions, reflecting that cross-resistance-conferring mutations typically dominate over collateral sensitivity effects in heterogeneous populations [21].
The following diagram illustrates the logical relationship between chemical-genetic profiles and the predicted antibiotic interactions:
Experimental Workflow for OCDM Application
The complete workflow for applying OCDM spans from data generation to experimental validation, as shown below:
Performance Comparison with Alternative Methods
OCDM demonstrates distinct advantages over other approaches for identifying cross-resistance and collateral sensitivity patterns. The table below summarizes its performance against alternative methodologies:
Table 1: Performance Comparison of Antibiotic Interaction Detection Methods
| Method | Primary Approach | Throughput | Genetic Coverage | Mechanistic Insight | Validation Precision |
|---|---|---|---|---|---|
| OCDM | Computational analysis of chemical-genetic profiles | High (840 pairs simultaneously) | Comprehensive (whole genome) | Direct from mutant fitness effects | 91% (64/70 validated) [21] |
| Experimental Evolution | Laboratory evolution + susceptibility testing | Low (limited lineages) | Limited (depends on selection pressure) | Indirect (requires sequencing) | Highly variable between studies [21] |
| Correlation-Based Metrics | Correlation of entire chemical-genetic profiles | High | Comprehensive | Limited by noise in neutral phenotypes | Poor (AUC 0.52-0.67) [21] |
| Chemical-Genetic Similarity | Profile similarity to infer mode of action | High | Comprehensive | Indirect inference | Moderate for XR only [11] |
Key Performance Metrics
In direct validation experiments, OCDM demonstrated 91.4% precision (64 out of 70 predicted interactions validated experimentally) [21]. The method significantly expanded the known interaction landscape, increasing known XR interactions by three-fold and CS interactions by six-fold compared to previous literature [21]. This included the reclassification of 116 previously tested drug-pair relationships with higher accuracy than individual experimental evolution studies, which showed considerable inconsistency—from 91 antibiotic pairs tested in at least two studies, only 30% were called uniformly across studies [21].
OCDM outperformed correlation-based metrics, which showed poor discrimination capability with area under the curve (AUC) values of just 0.52-0.67 for receiver operating characteristic curves [21]. The final OCDM model achieved AUC values of 0.76 and 0.73 for discriminating CS and XR from neutral interactions, respectively [21].
Experimental Protocols and Validation
OCDM Generation Protocol
Data Source Preparation:
- Obtain chemical-genetic interaction data from the E. coli single-gene deletion library fitness assays in 40 antibiotics [21].
- Calculate s-scores for each mutant-drug combination, representing standardized fitness effects relative to control conditions [21].
OCDM Calculation:
- Identify extreme s-scores exceeding optimal thresholds determined by performance validation (Extended Data Fig. 1d in source) [21].
- Calculate the six OCDM features from extreme s-score outliers only.
- Apply the OCDM classification thresholds to determine interaction types:
- XR: High concordance despite discordance signal
- CS: High discordance with no concordance signal
- Neutral: Neither significant concordance nor discordance [21]
Network Analysis:
- Construct antibiotic interaction networks from OCDM classifications.
- Analyze monochromaticity (exclusively XR or CS) and conservation within antibiotic classes [21].
Experimental Validation Protocol
Strain Preparation:
- Use wild-type E. coli strains for experimental evolution matching the genetic background of the chemical-genetic library [21].
Evolution Experiments:
- Evolve independent bacterial lineages in increasing concentrations of a primary antibiotic.
- Propagate cultures for sufficient generations (typically 200-500) to allow fixation of resistance mutations [21].
Susceptibility Testing:
- Measure minimum inhibitory concentrations (MICs) of evolved strains against both primary and secondary antibiotics.
- Calculate fold-change in susceptibility compared to ancestral strain.
- Classify interactions based on statistically significant changes:
- XR: Significant increase in MIC for secondary drug
- CS: Significant decrease in MIC for secondary drug
- Neutral: No significant change in MIC [21]
Mechanism Deconvolution:
- Sequence genomes of evolved strains to identify acquired mutations.
- Cross-reference with chemical-genetic profiles to identify causal mutations driving interactions [21].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for OCDM and Chemical-Genetic Studies
| Reagent/Resource | Function in OCDM Research | Example Specifications |
|---|---|---|
| E. coli Single-Gene Deletion Library | Genome-wide mutant collection for chemical-genetic profiling | Keio collection or similar; ~4,000 non-essential gene deletions [21] |
| Chemical-Genetic Screening Platform | High-throughput fitness assessment of mutants under drug treatment | 96-well or 384-well format with automated liquid handling [21] |
| Antibiotic Compound Library | Diverse set of antimicrobial agents for profiling | 40+ antibiotics spanning major classes and mechanisms [21] |
| s-Score Calculation Algorithm | Standardizes mutant fitness across conditions | Normalizes fitness to plate controls and across entire experiment [21] |
| OCDM Classification Script | Implements the OCDM algorithm for interaction prediction | R or Python implementation with optimized thresholds [21] |
| Experimental Evolution Setup | Laboratory evolution of resistance for validation | Serial passage in liquid media with escalating drug concentrations [21] |
Applications in Antimicrobial Drug Development
The OCDM framework enables several innovative applications in antibiotic discovery and development:
Rational Combination Therapy: By identifying collateral sensitivity pairs, OCDM informs antibiotic combinations that can suppress resistance emergence. The original study demonstrated that using CS pairs in combination reduced resistance development compared to single-drug treatments [21].
Drug Cycling Strategies: CS interactions revealed by OCDM can design intelligent antibiotic rotation schedules that exploit fitness costs of resistance, potentially reversing resistance evolution in clinical settings [21].
Mechanism Deconvolution: Beyond predicting interactions, OCDM helps identify specific genetic determinants driving cross-resistance and collateral sensitivity by pinpointing which mutants contribute most to concordance or discordance signals [21]. This provides valuable insights into resistance mechanisms that can inform drug design.
The framework revealed that a single drug pair can exhibit both XR and CS depending on the specific resistance mechanism acquired, demonstrating the nuanced understanding possible with OCDM that would be difficult to ascertain through experimental evolution alone [21].
The Outlier Concordance–Discordance Metric represents a powerful computational framework that transforms our approach to mapping antibiotic interactions. By systematically leveraging chemical-genetic profiles, OCDM enables comprehensive, accurate prediction of cross-resistance and collateral sensitivity patterns with minimal experimental burden. Its high validation rate (91% precision) and ability to expand known interaction networks by several-fold demonstrate significant advantages over traditional methods. For researchers and drug development professionals, OCDM provides both a practical tool for identifying promising combination therapies and a conceptual framework for understanding the complex genetic relationships underlying antibiotic resistance.
In the face of diminishing therapeutic options against antimicrobial resistance, understanding the complex relationships between antibiotics has never been more critical. When bacteria develop resistance to one drug, they may inadvertently become resistant to other compounds (cross-resistance, XR) or conversely, more sensitive to others (collateral sensitivity, CS). These interaction patterns represent a pivotal frontier in optimizing antibiotic cycling and combinatorial treatments. Traditional methods for mapping these relationships through experimental evolution are notoriously resource-intensive, probing only a limited fraction of possible resistance mutations and often yielding inconsistent results across studies due to variations in selection pressure and lineage sampling [21].
The emerging paradigm leverages systematic chemical-genetic interaction profiling to predict these relationships by comparing how genome-wide gene perturbations affect susceptibility to different antibiotics. This approach fundamentally shifts the discovery process from laborious serial experimentation to computational prediction, enabling researchers to rapidly identify interaction networks and their underlying genetic mechanisms. This guide provides a comparative analysis of the leading computational frameworks that translate chemical-genetic similarity into predictive models of drug-pair interactions, with particular emphasis on their methodological foundations, performance characteristics, and applicability domains for researchers navigating this rapidly evolving field.
Comparative Analysis of Predictive Approaches
The table below summarizes the core methodologies, strengths, and limitations of the primary approaches for predicting drug-pair interactions from chemical-genetic and other high-dimensional data sources.
Table 1: Comparative Analysis of Predictive Modeling Approaches for Drug-Pair Interactions
| Method | Core Methodology | Key Performance | Advantages | Limitations |
|---|---|---|---|---|
| OCDM (Outlier Concordance-Discordance Metric) | Uses extreme s-scores from chemical-genetic profiles; prioritizes concordant negative signals for XR, discordance for CS [21] | 91% validation rate (64/70 interactions); ROC AUC=0.76 (CS), 0.73 (XR); 3× more XR and 4× more CS discovered [21] | Direct biological interpretability; identifies driving mutations; validated for antibiotic XR/CS | Limited to organisms with comprehensive mutant libraries |
| MDG-DDI (Multi-feature Drug Graph) | Integrates FCS-based Transformer (semantic) with Deep Graph Network (structural); uses GCN for final prediction [26] | Outperforms 11 baseline models; strong gains with unseen drugs; robust on unbalanced datasets [26] | Handles both semantic and structural features; excellent generalization to new drugs | Complex architecture requires significant computational resources |
| EviDTI (Evidential Deep Learning) | Incorporates evidential deep learning for uncertainty quantification; uses 2D/3D drug structures and protein sequences [27] | Competitive on DrugBank (82.02% accuracy), Davis, KIBA; well-calibrated uncertainty estimates [27] | Quantifies prediction confidence; reduces false positives in experimental validation | Requires integration of multiple data modalities |
| MDFLDRR (Multi-Drug Features Learning) | Maps pathway, enzyme, target, and substructure features to common interaction space; uses drug relation regularization [28] | Pronounced predictive advantage for cardiovascular-antidepressant DDIs; accurately identifies severity levels [28] | Specifically designed for clinically relevant drug pairs; incorporates interaction severity | Application primarily demonstrated on specific drug classes |
Experimental Protocols and Methodologies
Chemical-Genetic Profiling for Cross-Resistance Prediction
The foundational protocol for generating chemical-genetic interaction data involves systematic screening of genome-wide mutant libraries against compound panels:
Experimental Workflow:
- Library Preparation: Utilize the Escherichia coli single-gene deletion library (Keio collection) or overexpression library for essential genes [21] [11].
- Competitive Growth Assay: Grow pooled mutant libraries in presence of sub-inhibitory antibiotic concentrations (typically concentrations that double doubling time) for approximately 12 generations [11].
- Fitness Quantification: Sequence plasmid pools or mutant barcodes to determine relative abundance changes versus untreated controls.
- Score Calculation: Compute s-scores or fold-change values that represent each mutant's sensitivity/resistance to each compound [21] [11].
Computational Analysis:
- Profile Comparison: Calculate similarity metrics between antibiotic profiles using the OCDM, which emphasizes extreme s-scores (both positive and negative) [21].
- Interaction Classification: Apply thresholds to identify XR (high concordance) versus CS (high discordance with minimal concordance) [21].
- Mechanism Identification: Identify specific gene mutations driving the interactions through enrichment analysis of sensitivity/resistance patterns.
Diagram 1: Chemical-genetic prediction workflow
Deep Learning Framework for DDI Prediction
Modern deep learning approaches employ multi-modal data integration:
Data Preparation:
- Drug Representation:
- Protein Representation:
- Amino acid sequences encoded via pre-trained models (e.g., ProtTrans) [27]
- Interaction Labels:
Model Architecture (MDG-DDI):
- Drug Encoder: Combines Frequent Consecutive Subsequence (FCS)-based Transformer for semantic features with Deep Graph Network for structural features [26].
- Feature Fusion: Concatenates drug and target representations for input to Graph Convolutional Network [26].
- Interaction Prediction: Outputs probability scores for potential interactions, with specialized handling for cold-start scenarios (unseen drugs) [26].
Diagram 2: Deep learning DDI prediction
The Scientist's Toolkit: Essential Research Reagents and Databases
Table 2: Key Research Resources for Drug-Pair Interaction Studies
| Resource | Type | Key Features | Application in Predictive Modeling |
|---|---|---|---|
| E. coli Keio Collection | Mutant Library | ~4,000 single-gene deletions; genome-wide coverage [21] | Chemical-genetic profiling; essential for OCDM-based prediction |
| HCDT 2.0 Database | Curated Database | 1.28M interactions; drug-gene, drug-RNA, drug-pathway; includes negative DTIs [29] | Training data for ML models; ground truth for validation |
| DrugBank | Pharmaceutical Database | 1,635 drugs, 556,757 drug pairs; clinical, chemical, pharmacological data [26] [28] | Benchmark dataset for DDI prediction models |
| DSigDB | Drug Signature Database | Drug-target gene interactions; focused on drug repurposing [29] | Expanding known interaction space for training |
| BindingDB | Interaction Database | 353,167 drug-target interaction records; binding affinity measurements [29] | Source for positive and negative interaction labels |
| SScore Metric | Analytical Tool | Quantifies mutant fitness compared to across-condition performance [21] | Standardized chemical-genetic interaction scoring |
Performance Benchmarking and Validation
Validation Metrics and Comparative Performance
Rigorous validation is essential for evaluating predictive models of drug-pair interactions:
Cross-Validation Framework:
- Standard Setting: Random split (80:10:10 train/validation/test) on benchmark datasets (DrugBank, Davis, KIBA) [27]
- Cold-Start Scenario: Evaluation with unseen drugs to assess generalizability [26] [27]
- Experimental Validation: Laboratory evolution to confirm predicted XR/CS interactions [21]
Quantitative Performance Comparison: The OCDM approach demonstrated exceptional precision (91%) when validated against 70 experimentally tested antibiotic interactions, significantly expanding the known interaction space with 3× more XR and 4× more CS relationships discovered compared to previous knowledge [21]. Deep learning methods like MDG-DDI and EviDTI show robust performance on standard benchmarks, with EviDTI achieving 82.02% accuracy on DrugBank and competitive results on challenging imbalanced datasets like Davis and KIBA [27]. These approaches particularly excel in cold-start scenarios critical for drug discovery, where predictions for novel compounds are most valuable.
Biological Mechanism Elucidation
Beyond prediction accuracy, the interpretability of models for identifying underlying mechanisms varies substantially:
The OCDM framework excels in biological interpretability, directly identifying specific gene mutations that drive cross-resistance and collateral sensitivity patterns [21]. For instance, chemical-genetic approaches have revealed that membrane-targeting versus intracellular-targeting antimicrobial peptides cluster separately in genetic interaction space, with distinct resistance determinants that explain their cross-resistance profiles [11]. This mechanistic insight is invaluable for designing combination therapies that exploit evolutionary trade-offs in resistance development.
Deep learning methods increasingly incorporate attention mechanisms and interpretability modules to provide biological insights, though this remains a challenge for many complex architectures [26] [27]. Methods that integrate multimodal data—combining chemical structures with protein sequences and interaction networks—generally provide more biologically plausible predictions than single-modality approaches [27] [28].
The integration of chemical-genetic profiling with machine learning represents a paradigm shift in predicting drug-pair interactions, moving the field from reactive characterization to proactive prediction. The OCDM framework provides a biologically interpretable approach specifically validated for antibiotic cross-resistance and collateral sensitivity prediction, while deep learning methods like MDG-DDI and EviDTI offer powerful alternatives for broad-scale DDI prediction with strong generalization capabilities.
Future methodology development should focus on several critical frontiers: (1) enhancing model interpretability to identify driving mechanisms without additional experiments; (2) improving performance on unseen drug classes through transfer learning and better molecular representations; (3) integrating multi-omics data layers to capture the full complexity of drug response; and (4) expanding beyond binary drug pairs to predict interactions in complex multi-drug regimens reflective of clinical polypharmacy [30] [31]. As these computational approaches mature, they promise to accelerate the rational design of combination therapies and cycling strategies that proactively manage resistance evolution across diverse therapeutic domains.
The escalating crisis of antimicrobial resistance (AMR) represents one of the most pressing challenges in modern healthcare, with Enterobacteriaceae bacteria like Escherichia coli classified by the World Health Organization as priority pathogens requiring urgent therapeutic solutions [32]. In this landscape, understanding the intricate interactions between antibiotics is paramount for developing effective treatment strategies. When bacteria develop resistance to one antibiotic, this adaptation can lead to two contrasting outcomes: cross-resistance (XR), where resistance extends to other drugs, further limiting treatment options; or collateral sensitivity (CS), where resistance to one antibiotic paradoxically increases susceptibility to another [2] [5]. These evolutionary trade-offs represent a double-edged sword in antimicrobial therapy—XR diminishes our therapeutic arsenal, while CS offers promising avenues for cycling or combinatorial treatments that can suppress resistance evolution [5].
Traditional methods for identifying XR and CS relationships have relied on experimental evolution approaches, where resistance is evolved in bacterial populations to one drug, followed by susceptibility testing against others [33]. Although powerful, this method explores only a limited fraction of possible resistance mutations and is constrained by scale and cost [2]. This case study examines how chemical genetics approaches have systematically expanded our understanding of the XR/CS network in E. coli, revealing hundreds of previously unknown interactions and providing insights into their underlying mechanisms.
Chemical Genetics: A Systematic Mapping Approach
Fundamental Principles of Chemical Genetics
Chemical genetics represents a powerful reverse genetics approach that systematically assesses how genetic perturbations affect drug susceptibility [10]. In its most effective implementation, genome-wide mutant libraries—including loss-of-function (knockout) or gain-of-function (overexpression) strains—are profiled for fitness changes in the presence of chemical compounds [10]. The resulting chemical-genetic interaction profiles capture the contribution of each gene to resistance or sensitivity against various drugs, creating a comprehensive map of resistance determinants [2] [11].
This approach offers distinct advantages over traditional experimental evolution. While evolution studies probe a limited set of mutational pathways, chemical genetics systematically measures how the loss or overexpression of each non-essential gene affects susceptibility to antibiotics [2]. The similarity between chemical-genetic profiles for different drugs can predict cross-resistance relationships, as drugs sharing resistance mechanisms will show concordant profiles across mutants [11] [10]. Conversely, collateral sensitivity is reflected in discordant profiles, where mutations conferring resistance to one drug increase sensitivity to another [2].
Experimental Workflow for Systematic XR/CS Mapping
The methodology for systematic mapping of XR/CS networks involves a coordinated pipeline of computational and experimental approaches. The following diagram illustrates the integrated workflow:
Key Research Reagents and Experimental Materials
The systematic mapping of XR/CS interactions relies on specialized research tools and biological resources. The following table details essential reagents used in these studies:
Table 1: Key Research Reagents for XR/CS Mapping Studies
| Research Reagent | Function/Application | Specific Examples from Studies |
|---|---|---|
| E. coli Single-Gene Deletion Library | Genome-wide loss-of-function mutant collection for identifying genes affecting drug susceptibility | Keio collection (systematic knockout of all non-essential E. coli genes) [2] |
| Gene Overexpression Libraries | Plasmid-based collections for identifying resistance-enhancing genes when overexpressed | ASKA library (Complete set of E. coli ORFs in expression plasmids) [11] |
| Chemical Genetics Screening Platforms | High-throughput systems for fitness profiling of mutant libraries under drug treatment | Pooled competition assays with barcode sequencing [2] [10] |
| Antibiotic Panels | Structurally and mechanistically diverse antibiotics for comprehensive interaction mapping | 40 antibiotics covering major classes (β-lactams, aminoglycosides, fluoroquinolones, etc.) [2] |
| Experimental Evolution Systems | In vitro evolution platforms for validating predicted interactions | Serial passage in sub-inhibitory antibiotic concentrations over multiple generations [33] |
Systematic Expansion of the XR/CS Network
Development of the OCDM Metric and Interaction Classification
To overcome the limitations of traditional correlation-based metrics for identifying XR/CS relationships, researchers developed the Outlier Concordance-Discordance Metric (OCDM) [2]. This innovative approach focused specifically on extreme s-scores (representing strong resistance or sensitivity effects) in the chemical genetics data, effectively filtering out noise from neutral phenotypes. The OCDM algorithm incorporated six key features derived from extreme s-scores: the sum and count of positive concordant s-scores, negative concordant s-scores, and total discordant s-scores [2].
The classification logic followed a clear decision pathway: drug pairs were inferred as XR if they showed high concordance in mutant profiles regardless of discordance signals, whereas CS relationships required not only high discordance but also minimal concordance signal [2]. This priority given to concordance reflects the biological reality that in heterogeneous populations evolved to resist one drug, XR-conferring mutations typically dominate over CS mutations when challenged with a second antibiotic.
Application of the OCDM to chemical genetics data covering 40 antibiotics in E. coli yielded a dramatic expansion of known interactions, as summarized in the table below:
Table 2: Systematic Expansion of XR/CS Interactions through Chemical Genetics
| Interaction Category | Previously Known Interactions | Newly Identified via OCDM | Fold Expansion | Validation Rate |
|---|---|---|---|---|
| Cross-Resistance (XR) | 70 | 313 | ~4.5× | 91% (64/70 tested) |
| Collateral Sensitivity (CS) | 25 | 196 | ~7.8× | 91% (64/70 tested) |
| Total Interactions | 95 | 509 | ~5.4× | 91% (64/70 tested) |
This systematic approach not only expanded the number of known interactions but also reclassified 116 previously tested drug-pair relationships, demonstrating the power of chemical genetics to resolve inconsistencies between different experimental evolution studies [2].
Experimental Validation of Predicted Interactions
To validate the interactions predicted through chemical genetics, researchers employed experimental evolution in which E. coli populations were evolved under selection pressure from one antibiotic, followed by susceptibility testing against others [2]. This validation approach tested 70 predicted interactions, with 64 (91%) confirming the computational predictions [2]. The high validation rate demonstrates the predictive power of chemical genetics approaches for identifying evolutionarily relevant XR/CS relationships.
Independent studies comparing resistance evolution to antibiotics versus antimicrobial peptides (AMPs) provide additional validation of CS principles. Research found that trimethoprim-resistant E. coli, with mutations in the thyA gene, displayed enhanced susceptibility to the AMP pexiganan, a observation consistent across both in vitro and in vivo models [33]. This demonstrates how CS relationships can extend between conventional antibiotics and alternative antimicrobial agents like AMPs.
Mechanisms Underlying Cross-Resistance and Collateral Sensitivity
Genetic and Physiological Basis of Interactions
The systematic nature of chemical genetics enables not only identification of XR/CS interactions but also elucidation of their underlying mechanisms. By examining which mutants drive specific interactions, researchers demonstrated that a single drug pair can exhibit both XR and CS relationships depending on the particular resistance mechanism involved [2]. This finding highlights the importance of considering genetic heterogeneity when designing therapeutic strategies based on CS principles.
The molecular mechanisms driving CS often involve fundamental physiological trade-offs in resistant bacteria. Key mechanisms identified through chemical genetics and supporting studies include:
- Altered membrane permeability: Mutations that reduce drug uptake through porin loss or modification may simultaneously increase susceptibility to other drugs requiring different entry mechanisms [33] [5].
- Efflux pump expression: Overexpression of multidrug efflux pumps can provide broad XR but may simultaneously create metabolic burdens or increase susceptibility to drugs that exploit these transport systems [33] [5].
- Metabolic rewiring: Resistance mutations that alter central metabolism can create new vulnerabilities to drugs targeting dependent pathways [2] [33].
- Target modification: Changes to antibiotic target sites (e.g., ribosomes, RNA polymerase) that confer resistance to one drug may sensitize bacteria to others targeting different sites on the same macromolecule [5].
The following diagram illustrates the principal mechanisms and their relationships in driving XR and CS:
Class-Specific Interaction Patterns
Analysis of the expanded XR/CS network reveals that interactions are not uniformly distributed across antibiotic classes. Instead, distinct patterns emerge:
- Aminoglycosides: Show extensive CS relationships with β-lactam antibiotics, consistent with known physiological trade-offs between membrane permeability changes and cell wall synthesis [33] [5].
- Fluoroquinolones: Demonstrate strong XR within the class but variable CS with other drug classes depending on specific resistance mutations [2].
- Antimicrobial peptides: Exhibit limited XR with conventional antibiotics when they have different modes of action, supporting their potential as CS-based alternatives [11].
These class-specific patterns provide valuable guidance for designing cycling regimens that exploit CS while minimizing XR.
Therapeutic Applications and Research Implications
Combination Therapies Exploiting Collateral Sensitivity
The systematic mapping of CS interactions enables rational design of combination therapies that suppress resistance evolution. Studies have demonstrated that applying CS drug pairs in combination can significantly reduce the emergence of resistance compared to single-drug treatments [2]. This approach leverages the evolutionary constraint that mutations conferring resistance to one drug simultaneously increase susceptibility to the other, creating a evolutionary trap for resistant mutants.
For example, the identified CS between trimethoprim and pexiganan (an antimicrobial peptide) suggests therapeutic potential for combining these agents against trimethoprim-resistant E. coli [33]. Similarly, CS relationships between aminoglycosides and β-lactams could inform combination regimens that limit resistance emergence in high-risk settings.
Research Applications and Future Directions
The expanded XR/CS network provides a rich resource for multiple research applications:
- Guiding antibiotic cycling regimens: CS networks can inform the sequential ordering of antibiotics in clinical settings to suppress resistance evolution [5].
- Rational combination therapy: Identified CS pairs represent promising combinations for empirical testing in animal models and clinical trials [2] [33].
- Drug discovery prioritization: Compounds showing CS with multiple resistance mechanisms represent high-priority candidates for development [2].
- Evolutionary forecasting: XR/CS maps enable predictions of resistance evolution pathways under different drug selection pressures [2] [5].
Future research directions should focus on validating these findings in clinical isolates, exploring CS relationships in bacterial communities rather than pure cultures, and extending mapping efforts to other priority pathogens beyond E. coli.
This case study demonstrates how chemical genetics approaches have systematically expanded our understanding of the cross-resistance and collateral sensitivity network in E. coli, increasing known interactions more than fivefold. The development of the OCDM metric enabled high-confidence prediction of XR/CS relationships, with experimental validation confirming 91% of tested interactions. The mechanistic insights derived from chemical genetics reveal that XR and CS are not fixed properties of drug pairs but depend on the specific resistance mechanisms involved.
The expanded XR/CS network provides a valuable resource for addressing the antimicrobial resistance crisis through rational design of combination therapies and cycling regimens that exploit evolutionary trade-offs. As antibiotic discovery continues to lag behind resistance emergence, such strategic approaches to preserving existing antibiotics become increasingly vital for modern medicine.
Navigating Challenges: Optimizing Chemical-Genetic Screens and Data Interpretation
Addressing Noise and Reproducibility in Large-Scale Screens
In the field of antibiotic discovery and resistance research, large-scale chemical genetics screens have emerged as powerful tools for identifying novel therapeutic targets and understanding bacterial defense mechanisms. These screens systematically assess how genome-wide mutations affect susceptibility to antibiotics, generating vast datasets that predict cross-resistance (XR) and collateral sensitivity (CS) patterns—phenomena where resistance to one drug confers resistance or sensitivity to another, respectively [2]. However, the utility of these screens is fundamentally constrained by significant challenges in managing experimental noise and ensuring reproducibility across studies. Discrepancies in cross-resistance calling between different experimental evolution studies highlight the critical need for standardized methodologies in large-scale screening approaches [2]. This guide examines these challenges through the lens of chemical genetics research, comparing the performance of different screening methodologies and providing frameworks for enhancing reliability in identifying clinically relevant antibiotic interactions.
Comparative Analysis of Screening Methodologies
Quantitative Comparison of Screening Approaches
Table 1: Performance metrics of different large-scale screening methodologies for cross-resistance identification
| Screening Methodology | Internal Validity | Scalability | Cost Efficiency | XR/CS Prediction Accuracy | Primary Applications |
|---|---|---|---|---|---|
| Chemical Genetics Profiling | Moderate | High | High | 91% (64/70 validated) [2] | Systematic identification of resistance mechanisms and drug interactions |
| Experimental Evolution | High | Low | Low | Variable between studies [2] | Probing resistance evolution in real-time under controlled selection pressure |
| Case-Control Studies | Moderate | Moderate | Moderate | Not specifically quantified | Investigating rare resistance outcomes and multiple risk factors simultaneously [34] |
| Prospective Cohort Designs | High | Low | Low | Long-term predictive value | Establishing temporal relationships between exposure and resistance development [34] |
Technical Performance Metrics
Table 2: Technical specifications and output characteristics of screening platforms
| Methodological Feature | Chemical Genetics Approach | Traditional Experimental Evolution | Comparative Analysis |
|---|---|---|---|
| Data Output Format | s-scores assessing mutant fitness across conditions [2] | Minimum Inhibitory Concentration (MIC) measurements [2] | Genetic vs. phenotypic endpoints |
| Genetic Resolution | Single-gene knockout effects [2] | Multiple accumulated mutations [2] | Defined mutations vs. complex adaptations |
| Sample Throughput | 40 antibiotics tested simultaneously on E. coli library [2] | Limited by sequential evolution experiments [2] | High-throughput vs. low-throughput |
| Key Performance Metric | Outlier Concordance-Discordance Metric (OCDM) [2] | Population-level susceptibility shifts | Computational prediction vs. direct measurement |
| Experimental Duration | Relatively rapid (pre-defined mutants) | Extended (requires generations of selection) [2] | Days to weeks vs. weeks to months |
Experimental Protocols and Methodologies
Chemical Genetics Screening Protocol
The chemical genetics approach utilizes systematic assessment of drug effects on genome-wide mutant libraries to predict cross-resistance and collateral sensitivity patterns [2].
Step 1: Library Preparation
- Utilize the Escherichia coli single-gene deletion library (Keio collection)
- Culture mutants in standardized growth conditions
- Implement quality controls to ensure library completeness and viability
Step 2: Antibiotic Exposure
- Select 40 antibiotics representing diverse mechanisms of action
- Establish concentration gradients for each antibiotic
- Include appropriate controls (vehicle-only and growth controls)
- Incubate mutants under standardized conditions (temperature, duration, aeration)
Step 3: Fitness Assessment
- Quantify bacterial growth using optical density measurements
- Calculate s-scores for each mutant in each condition
- s-scores represent fitness of a mutant in one condition compared to its fitness across all conditions [2]
- Normalize data to account for plate-to-plate variability
Step 4: Data Analysis
- Apply the Outlier Concordance-Discordance Metric (OCDM)
- Calculate sum and count of concordant negative s-scores
- Determine discordance signals between antibiotic pairs
- Classify interactions as XR, CS, or neutral based on established cutoffs [2]
Validation Using Experimental Evolution
Step 1: Resistance Selection
- Subject bacterial populations to increasing antibiotic concentrations
- Propagate for multiple generations (typically 200-500)
- Maintain parallel lineages to capture diverse evolutionary trajectories
Step 2: Susceptibility Testing
- Measure Minimum Inhibitory Concentrations (MICs) for evolved populations
- Test against both selecting drug and secondary antibiotics
- Use standardized broth microdilution methods
Step 3: Genetic Analysis
- Sequence genomes of evolved strains
- Identify mutations associated with resistance phenotypes
- Validate causal relationships through genetic reconstruction
Visualization of Screening Workflows and Analytical Frameworks
Chemical Genetics Screening Pipeline
Cross-Resistance and Collateral Sensitivity Mechanisms
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for chemical genetics screens
| Reagent/Material | Specifications | Primary Function | Considerations for Reproducibility |
|---|---|---|---|
| E. coli Keio Collection | ~4,000 single-gene deletants [2] | Comprehensive mutant library for fitness profiling | Regular viability checks; avoid cross-contamination |
| Antibiotic Stock Solutions | Clinical-grade antibiotics; concentration verification | Selective pressure application | Standardized storage conditions; freeze-thaw cycle limits |
| Growth Media | LB broth or defined minimal media | Bacterial culture and propagation | Batch-to-batch consistency; precise pH adjustment |
| 96/384-well Microplates | Sterile, tissue culture-treated | High-throughput screening | Edge effect mitigation; plate reader compatibility |
| Automated Liquid Handlers | Precision pipetting systems | Assay miniaturization and replication | Regular calibration; standardized protocols |
| Plate Readers | OD600 measurement capability | Bacterial growth quantification | Inter-instrument calibration; temperature control |
| Data Analysis Pipeline | Custom OCDM algorithms [2] | XR/CS interaction classification | Transparent parameters; open-source implementation |
Discussion: Implications for Antibiotic Development and Resistance Management
The systematic application of chemical genetics screens has substantially expanded our understanding of antibiotic cross-resistance and collateral sensitivity networks, revealing over 400 cases of cross-resistance and 267 collateral sensitivity interactions in E. coli alone [2]. This data-rich approach provides a framework for predicting resistance evolution and designing intelligent antibiotic cycling regimens that leverage collateral sensitivity patterns to suppress resistance development. The validated accuracy of 91% for chemical genetics predictions demonstrates the power of systematic mutant analysis for identifying clinically relevant drug interactions before they emerge in clinical settings [2]. Furthermore, the identification of specific genetic mutations driving these interactions enables mechanistic understanding of resistance trade-offs, offering new avenues for combination therapies that exploit bacterial vulnerabilities. As antibiotic resistance continues to escalate globally, these large-scale screening approaches—when implemented with rigorous attention to noise reduction and reproducibility—provide essential tools for extending the utility of existing antibiotics and guiding development of new therapeutic agents with reduced cross-resistance potential.
Antibiotic cross-resistance (XR) and collateral sensitivity (CS) are critical phenomena shaping the efficacy of antimicrobial treatments. Cross-resistance occurs when a resistance mechanism against one antibiotic also confers resistance to another drug, while collateral sensitivity describes the scenario where resistance to one antibiotic increases susceptibility to another [35]. Understanding these interactions is paramount in an era of diminishing therapeutic options. However, conflicting reports of antibiotic interactions often emerge across different studies, creating challenges for clinical decision-making and drug development. This review explores how different resistance mechanisms underlying these conflicting reports can be systematically mapped and understood through chemical-genetic approaches, providing a framework for resolving these discrepancies and informing combination therapy strategies.
Chemical Genetics as a Resolution Tool
Chemical genetics provides a powerful systematic approach to overcome limitations of traditional experimental evolution studies. Where experimental evolution probes a limited number of lineages and can accumulate numerous mutations making causal mechanisms difficult to identify, chemical genetics quantitatively assesses how each gene in the genome contributes to resistance or susceptibility to a broad set of drugs [21]. By examining genome-wide mutant libraries, researchers can measure fitness defects or advantages under antibiotic treatment, creating chemical-genetic interaction profiles that serve as fingerprints for each drug's mechanism of action [11].
The similarity between these chemical-genetic profiles offers critical insights into cross-resistance potential. Antibiotics with concordant profiles—affecting the same set of mutants in similar directions—tend to exhibit cross-resistance, as they likely share resistance mechanisms. Conversely, antibiotics with discordant profiles—where resistance to one drug sensitizes cells to another—often display collateral sensitivity relationships [21]. This systematic profiling allows researchers to deconvolve the complex genetic basis of antibiotic interactions that may appear conflicting when only observed at the phenotypic level.
Mechanisms Driving Conflicting Interactions
Diverse Genetic Determinants of Resistance
A fundamental insight from chemical-genetic studies is that antibiotics with different physicochemical properties and cellular targets vary considerably in their resistance determinants [11]. This diversity explains why cross-resistance is typically limited to antibiotics with similar modes of action. For example, antimicrobial peptides (AMPs) cluster into distinct groups based on their chemical-genetic profiles, with membrane-targeting AMPs showing different resistance determinants than intracellular-targeting AMPs [11].
Condition-Dependent Interaction Outcomes
The same drug pair can exhibit opposite interactions depending on the specific resistance mechanism involved. A comprehensive study using Escherichia coli chemical-genetic data demonstrated this principle clearly, finding that "a drug pair can exhibit both interactions depending on the resistance mechanism" [21]. This mechanistic dependency resolves why literature reports may conflict—different studies may select for distinct resistance mutations that lead to opposite collateral phenotypes.
Table 1: Examples of Conflicting Antibiotic Interactions from Different Resistance Mechanisms
| Drug Pair | Resistance Mechanism A | Interaction Type A | Resistance Mechanism B | Interaction Type B |
|---|---|---|---|---|
| β-lactam pairs | PDC (AmpC) mutations | Cross-resistance | Porin mutations + efflux upregulation | Collateral sensitivity |
| Aminoglycoside-Fluoroquinolone | AAC(6')-Ib-cr production | Cross-resistance | gyrA mutations | Neutral interaction |
| Drug A - Drug B | Efflux pump overexpression | Cross-resistance | Target site modification | Collateral sensitivity |
Microbiological vs. Epidemiological Perspectives
Conflicting reports of antibiotic interactions can also stem from different methodological approaches. From a strict microbiological perspective, cross-resistance refers to resistance between different antibiotic classes due to a shared mechanistic basis, such as a single enzyme conferring resistance to multiple drugs [35]. In contrast, epidemiological studies may identify statistical associations between resistance phenotypes that lack a proven mechanistic link, which can be context-dependent and not universally applicable [35]. This distinction is crucial—associations observed in one hospital or population may not generalize to other settings with different resistance gene distributions or selective pressures.
Experimental Approaches and Validation
Chemical-Genetic Profiling Methodology
The core methodology for systematic mapping of antibiotic interactions involves several key steps. First, a genome-wide mutant library (e.g., single-gene deletion or overexpression strains) is exposed to sub-inhibitory concentrations of antibiotics. After a defined growth period, the relative abundance of each mutant is quantified through deep sequencing. Fitness scores are calculated by comparing growth in drug-treated versus untreated conditions, generating a chemical-genetic profile for each antibiotic [11].
These profiles are then analyzed using specialized metrics like the Outlier Concordance-Discordance Metric (OCDM), which discriminates between cross-resistance and collateral sensitivity by evaluating concordant and discordant extreme fitness scores across mutants [21]. This approach has demonstrated remarkable predictive power, successfully validating 64 out of 70 inferred interactions through experimental evolution [21].
Experimental Evolution for Validation
To validate predicted interactions, experimental evolution remains the gold standard. This involves evolving multiple independent bacterial lineages under selection with a first antibiotic until resistance is established. The evolved populations are then tested for susceptibility to a panel of second antibiotics to quantify cross-resistance or collateral sensitivity effects [21]. Genomic sequencing of evolved strains helps identify the specific mutations responsible for the observed interactions, connecting genotype to phenotype.
Table 2: Key Experimental Parameters for Interaction Mapping
| Parameter | Chemical-Genetic Approach | Experimental Evolution |
|---|---|---|
| Genetic diversity | Systematic (all non-essential genes) | Limited (spontaneous mutations) |
| Timescale | Days to weeks | Weeks to months |
| Primary output | Comprehensive interaction network | Validated specific interactions |
| Causal mechanism identification | Direct from design | Requires additional sequencing |
| Scalability | High (many drugs simultaneously) | Lower (focused hypotheses) |
| Key metrics | s-scores, OCDM | MIC fold-change, fitness costs |
Research Toolkit for Interaction Studies
Table 3: Essential Research Reagents and Resources
| Resource | Function/Application | Example/Specifications |
|---|---|---|
| Single-gene deletion library | Systematic assessment of gene contribution to resistance | E. coli Keio collection |
| Gene overexpression library | Identification of resistance-enhancing genes | ASKA library (E. coli) |
| Chemical-genetic screening platform | High-throughput fitness profiling | Pooled mutant competitions with sequencing readout |
| PATRIC database | Access to antibiotic susceptibility data | MIC data for 419 E. coli strains against 20 antibiotics |
| Statistical analysis tools | Detection of collateral effects from surveillance data | Conditional t-test method |
| Experimental evolution setup | In vitro validation of predicted interactions | Serial passage in increasing drug concentrations |
Visualization of Key Concepts
Mechanistic Basis of Conflicting Reports
Chemical-Genetic Prediction Workflow
Implications for Drug Development and Combination Therapies
The systematic mapping of antibiotic interactions through chemical-genetic approaches has profound implications for addressing antibiotic resistance. By understanding the mechanistic basis of cross-resistance and collateral sensitivity, researchers can design more effective antibiotic cycling strategies and combination therapies [21]. The application of collateral-sensitive drug pairs in combination has been shown to reduce antibiotic-resistance development in vitro, offering a promising approach to extend the therapeutic life of existing antibiotics [21].
For drug development professionals, these insights enable smarter candidate selection by avoiding compounds with extensive cross-resistance to existing human host-defense peptides or antibiotics [11]. Additionally, identifying antibiotics with collateral sensitivity relationships to commonly resistant pathogens provides opportunities for targeted combination therapies that suppress resistance evolution.
Conflicting reports of antibiotic interactions find resolution through understanding the diverse resistance mechanisms that underlie them. Chemical-genetic approaches provide a systematic framework for mapping these interactions and predicting their behavior across different genetic contexts. By recognizing that the same drug pair can exhibit opposite interactions depending on the specific resistance mechanism involved, researchers and clinicians can better interpret seemingly contradictory literature and make more informed decisions about antibiotic selection and combination strategies. As chemical-genetic datasets expand across bacterial species, these approaches will become increasingly powerful in guiding therapeutic decisions and antibiotic development in the face of growing antimicrobial resistance.
In classical functional genomics, gene knockouts have been the cornerstone for determining gene function. However, this approach presents significant limitations, particularly for studying essential genes whose complete disruption leads to lethality, thereby precluding functional analysis in later developmental or cellular stages [36]. Similarly, the pleiotropic phenotypes often associated with null alleles can obscure the distinction between primary and secondary effects. To address these challenges, the field has increasingly turned to more nuanced genetic perturbation strategies—specifically, hypomorph (partial loss-of-function) mutations and gene overexpression systems. When integrated within chemical genetics frameworks, these complementary approaches enable the systematic mapping of gene function and drug resistance mechanisms with unprecedented resolution.
Hypomorphic mutations provide a means to probe gene function across a spectrum of activity levels, allowing researchers to bypass lethality and dissect pleiotropic effects [36]. Conversely, overexpression libraries can identify genes that confer resistance or susceptibility when expressed at supraphysiological levels, revealing potential drug targets and resistance mechanisms [20]. This guide objectively compares the performance, applications, and experimental outcomes of these two powerful approaches within the context of antibiotic cross-resistance research, providing researchers with the methodological insights needed to select appropriate strategies for their specific investigations.
Conceptual Foundations and Key Definitions
Hypomorph Libraries
Hypomorphic mutations are partial loss-of-function mutations that reduce, but do not completely eliminate, gene activity. Unlike null alleles, hypomorphs retain residual function, making them particularly valuable for studying essential genes and investigating gene dosage effects [36]. Modern methods for generating hypomorphic mutations include targeted techniques such as CRISPR interference (CRISPRi) and the engineered insertion of "polyA tracks" into gene coding sequences. These polyA tracks—stretches of consecutive adenosine nucleotides—disrupt translation elongation efficiency, leading to decreased protein expression in a predictable and tunable manner [36].
Overexpression Libraries
Overexpression libraries typically consist of pooled plasmid collections where each plasmid overexpresses a single open reading frame (ORF) from a specific promoter. When screened against compounds, these libraries identify genes that, when overexpressed, enhance resistance or sensitivity to the compound, thereby revealing potential drug targets and resistance mechanisms [20]. This approach effectively maps the "latent resistome"—genes where altered expression impacts drug susceptibility.
Chemical Genetics and Cross-Resistance Patterns
Chemical genetics systematically explores the interactions between chemical compounds and genetic perturbations. In antibiotic research, this approach helps identify cross-resistance (XR), where resistance to one antibiotic confers resistance to another, and collateral sensitivity (CS), where resistance to one antibiotic increases susceptibility to another [2]. Understanding these patterns is crucial for designing effective antibiotic cycling and combination therapies.
Methodological Comparison: Experimental Approaches and Workflows
Hypomorph Library Implementation
PolyA Track Engineering: This method involves inserting consecutive adenosine nucleotides into the open reading frame of a target gene. The length of the polyA track directly correlates with the degree of protein reduction, enabling the creation of an allelic series with graded expression levels [36]. This technique has been successfully applied across diverse model organisms, including Escherichia coli and the protozoan Tetrahymena thermophila.
CRISPRi Knockdown: CRISPRi utilizes a catalytically dead Cas9 (dCas9) fused to transcriptional repressors to specifically reduce gene expression without altering DNA sequence. This approach has been powerfully implemented in mycobacterial systems using arrayed libraries targeting essential genes, enabling high-content imaging and morphological phenotyping [37].
Overexpression Library Screening
The standard workflow involves:
- Library Transformation: A pooled plasmid library overexpressing all ORFs is introduced into the bacterial host [20].
- Selective Pressure: The transformed pool is grown in sub-inhibitory concentrations of an antibiotic.
- Sequencing-Based Quantification: After selection, plasmid abundance is quantified via deep sequencing to identify genes that confer resistance or sensitivity when overexpressed [20].
Integrated Experimental Workflows
The following diagram illustrates the conceptual framework and experimental workflow for integrating hypomorph and overexpression approaches in chemical genetics research:
Comparative Performance Analysis: Key Experimental Findings
Direct Comparison of Functional Outputs
Table 1: Comparative analysis of hypomorph and overexpression library performance in chemical genetics applications
| Performance Metric | Hypomorph Libraries | Overexpression Libraries |
|---|---|---|
| Genetic Resolution | Tunable partial loss-of-function [36] | Supraphysiological gain-of-function [20] |
| Screening Readout | Morphological phenotyping [37], fitness defects | Chemical-genetic interaction scores, MIC changes [20] |
| Therapeutic Insight | Identifies essential gene functions [36] [37] | Reveals resistance mechanisms [20] |
| Cross-Resistance Detection | Identifies CS through fitness trade-offs [2] | Predicts XR through profile concordance [2] |
| Key Advantage | Studies essential genes without lethality [36] | Directly maps resistance-associated genes [20] |
| Experimental Scalability | Arrayed format for high-content imaging [37] | Pooled format for high-throughput sequencing [20] |
Empirical Data from Key Studies
Table 2: Quantitative results from representative studies using hypomorph and overexpression approaches
| Study System | Perturbation Type | Library Scale | Key Findings | Data Output |
|---|---|---|---|---|
| E. coli AMP Resistance [20] | Overexpression | ~4,400 E. coli ORFs | Identified distinct resistance determinants for 15 AMPs; grouped AMPs by mode of action | Chemical-genetic interaction scores; 4 clusters of AMPs based on resistance mechanisms |
| Mycobacterial Essential Genes [37] | CRISPRi Hypomorphs | 276 essential gene targets | Morphological clustering revealed functional relationships; identified new restriction-modification system | Quantitative morphological analysis; 73% of genes produced detectable morphotypes |
| E. coli PolyA Tracks [36] | Translation Attenuation | Varying polyA lengths (9-36 nucleotides) | Protein expression reduction proportional to polyA track length (15-95% reduction) | Fluorescence measurements: 9As=15-35% reduction, 36As=>95% reduction |
| Antibiotic XR/CS Prediction [2] | Overexpression Profiles | 40 antibiotics | Identified 404 XR and 267 CS cases; validated 64/70 interactions (91% precision) | Outlier Concordance-Discordance Metric (OCDM) with ROC AUC=0.76 |
Research Reagent Solutions: Essential Materials and Tools
Table 3: Key reagents and resources for implementing hypomorph and overexpression screens
| Reagent/Resource | Function | Example Application |
|---|---|---|
| PolyA Track Vectors | Tunable translation attenuation | Generating hypomorphic allelic series in diverse organisms [36] |
| CRISPRi/dCas9 Systems | Targeted transcriptional repression | Arrayed hypomorph library for essential genes [37] |
| ORF Overexpression Library | Genome-wide gene overexpression | Pooled screening for resistance genes [20] |
| Barcoded Lentiviral Vectors | Variant tracking in single-cell screens | Multiplexed perturbation screening (e.g., SEUSS/Perturb-seq) [38] |
| TR-FRET Assay System | Protein-protein interaction quantification | Screening small-molecule PPI inducers for hypomorph correction [39] |
Detailed Experimental Protocols
Protocol 1: Genome-Wide Overexpression Screening for Cross-Resistance
This protocol follows the methodology established by [2] and [20] for identifying cross-resistance patterns through overexpression screening:
- Library Preparation: Transform the pooled plasmid overexpression library (e.g., all E. coli ORFs) into the target bacterial strain.
- Selective Growth: Grow the transformed pool in the presence of sub-inhibitory concentrations of antibiotic (concentration that increases doubling time by 2-fold).
- Competition Assay: Allow 12 generations of growth under selection pressure.
- Plasmid Abundance Quantification: Isolate plasmids from the selected population and determine relative abundance of each plasmid via deep sequencing.
- Chemical-Genetic Scoring: Calculate chemical-genetic interaction scores by comparing plasmid abundances in presence vs. absence of antibiotic.
- Cross-Resistance Analysis: Apply the Outlier Concordance-Discordance Metric (OCDM) to identify antibiotic pairs with concordant (XR) or discordant (CS) profiles.
Protocol 2: Arrayed CRISPRi Hypomorph Library Screening with Phenotypic Imaging
This protocol adapts the methodology from [37] for high-content morphological screening of hypomorph mutants:
- Library Construction: Clone sgRNAs targeting essential genes into an inducible CRISPRi vector and transform into recipient strain (e.g., M. smegmatis ParB-mCherry reporter).
- Knockdown Induction: Treat arrayed library with anhydrotetracycline (ATc) for 18 hours to induce gene silencing.
- Automated Imaging: Capture high-resolution images of each mutant using automated microscopy.
- Morphological Feature Extraction: Apply computational pipeline to quantify bacillary morphological features (cell length, width, curvature, etc.).
- Morphotypic Clustering: Use statistical learning (e.g., principal component analysis, hierarchical clustering) to group mutants with similar morphological profiles.
- Functional Annotation: Infer gene function based on clustering with genes of known function and validate hypotheses through orthogonal assays.
Signaling Pathways and Resistance Mechanisms
The molecular pathways revealed through integrated hypomorph and overexpression screening provide critical insights into bacterial stress response and resistance mechanisms. The following diagram summarizes key pathways and their interactions:
Discussion and Research Implications
The integration of hypomorph and overexpression libraries represents a paradigm shift in functional genomics, moving beyond binary knockout approaches to capture the continuum of gene function. This integrated approach is particularly powerful for mapping complex genetic interactions and identifying subtle phenotypic effects that would be missed in traditional screens.
For drug discovery applications, the combination of these approaches enables systematic mapping of resistance landscapes. Overexpression screens directly identify resistance genes, while hypomorph screens reveal essential functions that could be targeted to overcome resistance. The ability to predict cross-resistance and collateral sensitivity patterns through chemical-genetic profiling [2] offers particularly promising applications for designing antibiotic cycling regimens that minimize resistance emergence.
Future methodological developments will likely focus on increasing the precision and scalability of both approaches. For hypomorph libraries, refining the tunability of expression levels and expanding to more complex eukaryotic systems will be key priorities. For overexpression systems, improving the physiological relevance of overexpression phenotypes and developing better controls for artifactual effects will enhance their predictive value. Together, these approaches provide complementary lenses through which to view gene function, offering a more complete picture of biological systems and their responses to chemical perturbation.
Optimizing Drug Selection to Minimize Cross-Resistance with Host Defense Peptides
The escalating crisis of antimicrobial resistance necessitates innovative therapeutic strategies, among which Host Defense Peptides (HDPs) represent a promising class of innate immune effector molecules with broad-spectrum activity. A critical consideration in deploying therapeutic antimicrobial peptides (AMPs) is minimizing cross-resistance—a phenomenon where bacterial resistance to one antimicrobial agent confers resistance to another, potentially including endogenous HDPs crucial for human immunity. Chemical-genetic profiling has emerged as a powerful reverse genetic approach that systematically maps the genetic determinants of resistance by quantifying how genetic perturbations affect bacterial susceptibility to antimicrobial agents [11]. This framework enables researchers to predict cross-resistance patterns by identifying shared resistance pathways between therapeutic candidates and human HDPs, thereby informing rational drug selection to preserve the efficacy of our innate immune defenses.
The distinction between HDPs and broader AMP categories is fundamental to this endeavor. While all HDPs are AMPs, not all AMPs qualify as HDPs; HDPs are specifically host-derived peptides that play integrated roles in defense and immunity, exhibiting both direct antimicrobial activity and immunomodulatory functions [40]. This dual functionality makes the preservation of HDP efficacy particularly crucial for host defense integrity. Chemical-genetics approaches can systematically identify whether resistance mechanisms against therapeutic AMPs overlap with those affecting HDPs, thus providing a strategic framework for selecting drug candidates that minimize such detrimental overlap [11].
Chemical-Genetic Profiling: A Framework for Predicting Cross-Resistance
Fundamental Principles and Workflow
Chemical-genetic profiling operates on the principle that similarities in the genetic determinants of resistance between two antimicrobial agents can predict cross-resistance outcomes. The methodology involves assessing genome-wide mutant libraries under sub-inhibitory concentrations of antimicrobial compounds [11] [2]. In practice, this entails monitoring the growth of pooled mutant collections—such as gene knockout or overexpression libraries—in the presence versus absence of AMPs, followed by deep sequencing to quantify relative mutant abundances [11]. The resulting chemical-genetic interaction profiles reveal which genetic perturbations enhance resistance or sensitivity to each compound, creating a comprehensive map of resistance determinants.
The power of this approach lies in its systematic nature; by simultaneously probing how every gene in the genome influences susceptibility, it captures the full spectrum of potential resistance mechanisms, including those that might be missed in conventional experimental evolution studies that sample only a limited mutational space [2]. These profiles carry predictive information about cross-resistance, as antibiotics with similar chemical-genetic interaction profiles have been shown to share cellular targets and mechanisms of action [11]. Consequently, this method enables preemptive identification of problematic cross-resistance relationships before they manifest in clinical settings.
Experimental Protocol for Chemical-Genetic Profiling
The standard workflow for chemical-genetic profiling of AMPs involves several critical stages. First, a comprehensive plasmid library overexpressing all open reading frames from the target bacterium (e.g., ~4,400 E. coli genes) is cultured in pooled format [11]. This library is then exposed to sub-inhibitory concentrations of the AMP under investigation—typically a concentration that increases the population doubling time by 2-fold—alongside an untreated control, with both conditions allowed to proceed for approximately 12 generations [11]. Following this competitive growth phase, plasmids are isolated from each selection, and the relative abundance of each plasmid is determined via deep sequencing. By comparing plasmid abundances in treated versus untreated conditions, researchers calculate a chemical-genetic interaction score for each gene, identifying those that significantly increase sensitivity (sensitivity-enhancing genes) or decrease sensitivity (resistance-enhancing genes) when overexpressed [11].
Validation of identified interactions typically involves follow-up minimum inhibitory concentration (MIC) measurements on selected overexpression strains. In one systematic study, this validation approach confirmed changes in MIC in the expected direction for 83% of tested chemical-genetic interactions, with resistance-enhancing gene overexpressions yielding an average ~1.6-fold MIC increase and sensitivity-enhancing ones showing ~0.7-fold MIC decrease [11]. This robust experimental framework provides high-confidence data on the genetic basis of AMP resistance.
Figure 1: Chemical-genetic profiling workflow for predicting AMP cross-resistance. The process begins with library construction, progresses through competitive growth and sequencing, and culminates in data analysis and validation [11].
Comparative Analysis of AMP Classes and Cross-Resistance Patterns
Classification of AMPs by Mode of Action and Resistance Profiles
Systematic chemical-genetic profiling of 15 diverse AMPs in E. coli has revealed that these peptides cluster into distinct groups based on their resistance determinants, primarily according to their modes of action [11]. The clustering analysis separates AMPs into four main categories: two predominantly membrane-targeting clusters (C1 and C2) and two primarily intracellular-targeting clusters (C3 and C4) [11]. This classification aligns with fundamental physicochemical properties and biological activities, providing a framework for understanding cross-resistance patterns.
Membrane-targeting AMPs (clusters C1 and C2) generally exhibit lower isoelectric points, reduced proline content, and substantially higher hydrophobicity with greater propensity to form secondary structures compared to intracellular-targeting AMPs [11]. These properties facilitate integration into bacterial membranes where they create pores [11]. In contrast, intracellular-targeting AMPs in cluster C4 display high proline content leading to elevated structural disorder, a hallmark of a novel class of intracellular-targeting AMPs that penetrate membranes without lysis to inhibit internal processes like protein synthesis [11]. Cluster C3 contains AMPs with hybrid characteristics, demonstrating both membrane-disruptive and intracellular-targeting activities [11].
Cross-Resistance Patterns Across AMP Classes
The clustering of AMPs based on chemical-genetic interaction profiles directly informs cross-resistance likelihood, with empirical evidence demonstrating that cross-resistance occurs predominantly between AMPs sharing similar modes of action [11]. This principle was substantiated through analysis of laboratory-evolved AMP-resistant strains, which revealed that intracellular-targeting AMPs are less likely to induce cross-resistance to membrane-targeting human host-defense peptides than those sharing the same broad mechanisms [11]. The implication is profound: selecting therapeutic AMPs from a different mode-of-action cluster than human HDPs may minimize detrimental cross-resistance.
Table 1: Classification and Properties of Antimicrobial Peptide Clusters Based on Chemical-Genetic Profiling [11]
| Cluster | Primary Target | Key Physicochemical Properties | Representative AMPs | Cross-Resistance Likelihood |
|---|---|---|---|---|
| C1 | Membrane | Low isoelectric point, low proline content, high hydrophobicity, strong secondary structure formation | Not specified in source | High within cluster, low between dissimilar clusters |
| C2 | Membrane | Similar to C1 with subtle differences in multiple properties considered jointly | Not specified in source | High within cluster, low between dissimilar clusters |
| C3 | Mixed membrane and intracellular | Features of both membrane- and intracellular-targeting AMPs | Indolicidin, Protamine | Moderate, depending on shared mechanisms |
| C4 | Intracellular | High proline content, elevated intrinsic structural disorder | Bactenecin 5 (BAC5), Cathelicidin PR-39 | High within cluster, low to membrane-targeting HDPs |
The functional diversity of genes influencing AMP susceptibility further explains these cross-resistance patterns. While genes involved in cell envelope function are overrepresented among AMP susceptibility-modulating genes, the majority of identified genetic hits lack obvious functional connections to known AMP uptake mechanisms or modes of action [11]. This suggests complex and often unanticipated genetic networks underlie AMP resistance, reinforcing the value of systematic chemical-genetic approaches over hypothesis-driven methods for comprehensively mapping resistance determinants.
Experimental Data: Quantitative Cross-Resistance Assessment
Chemical-Genetic Interaction Metrics and Cross-Resistance Prediction
The systematic mapping of antibiotic cross-resistance and collateral sensitivity using chemical genetics has established quantitative metrics for predicting these interactions [2]. Researchers have developed the Outlier Concordance-Discordance Metric (OCDM), which effectively discriminates between cross-resistance and collateral sensitivity relationships by analyzing chemical-genetic profile similarities [2]. This approach has demonstrated high predictive accuracy, with experimental validation confirming 91% (64/70) of inferred interactions [2].
Application of this metric to 40 antibiotics in E. coli revealed 404 cases of cross-resistance and 267 of collateral sensitivity, expanding known interactions by more than threefold [2]. This systematic framework enables identification of both cross-resistance and collateral sensitivity—where resistance to one drug increases sensitivity to another—providing strategic opportunities for cycling or combinatorial treatments that minimize resistance development [2]. The findings further demonstrated that some drug pairs can exhibit both interactions depending on the specific resistance mechanism, highlighting the complexity of resistance relationships [2].
Table 2: Chemical-Genetic Metrics for Predicting Antimicrobial Cross-Resistance [2]
| Interaction Type | OCDM Criteria | Validated Pairs | Potential Application |
|---|---|---|---|
| Cross-Resistance (XR) | High concordance in mutant profiles despite any discordance signal | 313 XR interactions identified | Avoid sequential use of XR drug pairs |
| Collateral Sensitivity (CS) | High discordance with no concordance signal in chemical-genetic profiles | 196 CS interactions identified | Implement cycling or combinatorial therapies |
| Neutral | Neither strong concordance nor discordance | 125 neutral interactions identified | Flexible usage without strong resistance implications |
Application to AMP Development and HDP Conservation
For AMP development specifically, chemical-genetic profiling of 15 AMPs revealed that resistance-enhancing and sensitivity-enhancing genes vary considerably across AMPs with different physicochemical properties and cellular targets [11]. This mechanistic diversity underscores why cross-resistance is prevalent mainly between AMPs with similar modes of action [11]. The practical implication is that researchers can strategically select therapeutic AMP candidates from clusters distinct from human HDPs to minimize cross-resistance.
Additionally, the screen identified several genes that shape susceptibility to membrane- and intracellular-targeting AMPs in an antagonistic manner [11], suggesting potential genetic trade-offs that could be exploited in combination therapies. These findings align with the broader observation that collateral sensitivity drug pairs applied in combination can reduce antibiotic-resistance development in vitro [2], offering a promising approach for AMP deployment.
Research Toolkit: Essential Reagents and Methodologies
Table 3: Essential Research Reagents and Methodologies for Chemical-Genetic Profiling of AMPs
| Research Tool | Specification/Function | Application in AMP Research |
|---|---|---|
| Genome-Wide Overexpression Library | Comprehensive plasmid collection expressing all ORFs from target bacterium (e.g., ~4,400 E. coli genes) [11] | Identifies resistance-enhancing and sensitivity-enhancing genes when overexpressed |
| Pooled Competition Assay | Sensitive growth competition monitoring of pooled library with/without AMP exposure [11] | Quantifies relative fitness of each mutant under AMP selection pressure |
| Deep Sequencing Platform | High-throughput sequencing of plasmid abundances post-selection [11] | Enables calculation of chemical-genetic interaction scores for each gene |
| Tetrameric Recombinant HDP Production | Recombinant production of HDPs as tetrameric fusion proteins in Lactococcus lactis [41] | Scalable production of structurally stable, highly active HDPs for testing |
| Hypomorph Library Array | Collection of 279 partially depleted essential genes (hypomorphs) [11] | Complementary approach to test AMP effects on essential gene depletion |
| Phenotypic Susceptibility Assays | MIC measurements, plaque reduction assays, yield reduction systems [42] | Validates and quantifies resistance phenotypes identified in screens |
The tetrameric recombinant production system for HDPs deserves particular emphasis as an innovative methodological advancement. This approach involves designing recombinant proteins as tetrameric repeats of a single HDP fused with a "GGSSRSS" linker and C-terminal hexa-histidine tag for purification [41]. Compared to chemical synthesis, this recombinant production in Lactococcus lactis—a generally regarded as safe (GRAS) organism free from endotoxins—yields HDPs with enhanced antimicrobial activity, improved structural stability, and nanostructured organization [41]. This addresses a major obstacle in AMP research: developing scalable production strategies that ensure proper peptide conformation and activity while complying with safety standards for therapeutic use.
Figure 2: Logical framework for minimizing cross-resistance between therapeutic AMPs and host HDPs. The strategy involves selecting therapeutic AMPs from different mode-of-action clusters than endogenous HDPs [11].
The strategic integration of chemical-genetic profiling into antimicrobial peptide development offers a powerful approach to minimize cross-resistance with host defense peptides. The systematic mapping of resistance determinants across diverse AMP classes reveals that cross-resistance is prevalent primarily between AMPs sharing similar modes of action, providing a clear rationale for selecting therapeutic candidates from mechanistic clusters distinct from human HDPs [11]. Furthermore, the identification of collateral sensitivity relationships presents opportunities for rational drug cycling or combination approaches that suppress resistance development [2].
As antibiotic resistance continues to escalate, safeguarding the efficacy of our innate immune defenses through prudent therapeutic design becomes increasingly crucial. Chemical-genetic approaches provide the necessary framework to predict and circumvent detrimental cross-resistance relationships early in the drug development pipeline. By leveraging these systematic methods, researchers can strategically select AMP candidates that maximize therapeutic efficacy while preserving the integrity of essential host defense mechanisms—a critical dual objective in modern antimicrobial development.
Bench to Bedside: Validating Predictions and Comparing Chemical Genetics with Traditional Methods
Experimental Evolution as a Validation Gold Standard
In the urgent fight against antimicrobial resistance (AMR), chemical genetics approaches have emerged as powerful tools for generating hypotheses about complex drug interactions, such as cross-resistance (XR) and collateral sensitivity (CS). However, the predictions generated by these high-throughput screens require rigorous validation in biologically relevant contexts. This is where experimental evolution serves as an indispensable gold standard, providing critical confirmation of proposed resistance mechanisms and their real-world implications. By subjecting microorganisms to controlled selective pressures over multiple generations, researchers can directly observe the evolutionary trajectories that lead to resistance, offering unparalleled insight into the dynamics of bacterial adaptation [21] [2] [43].
The validation role of experimental evolution is particularly crucial for understanding cross-resistance patterns, where resistance to one antibiotic confers resistance to another, and collateral sensitivity, where resistance to one drug increases susceptibility to another [21] [2]. While chemical genetics can identify potential interactions by profiling genome-wide mutant libraries, these findings represent static snapshots of potential resistance mechanisms. Experimental evolution provides the dynamic, temporal dimension needed to confirm whether these potential mechanisms actually emerge and persist in evolving populations, making it the definitive method for validating predicted resistance patterns before clinical applications [21] [43].
Methodological Comparison: Experimental Evolution vs. Alternative Approaches
Various methodologies are employed to study antibiotic resistance, each with distinct strengths and limitations. The table below systematically compares experimental evolution with other common approaches:
Table 1: Comparison of Methodologies for Studying Antibiotic Resistance
| Method | Key Principle | Advantages | Limitations |
|---|---|---|---|
| Experimental Evolution | Evolving populations under drug pressure over multiple generations | • Direct observation of evolutionary trajectories • Validates mechanistic hypotheses • Quantifies fitness trade-offs • High reproducibility [43] | • Time and resource intensive • Simplified laboratory conditions • Potential for non-clinical evolutionary paths |
| Chemical Genetics | Systematic assessment of drug effects on genome-wide mutant libraries [21] [2] | • High-throughput capability • Comprehensive resistance mechanism mapping • Identifies potential XR/CS networks [21] | • Limited to pre-existing mutants • Does not capture evolutionary dynamics • May miss epistatic interactions |
| Genome-Wide Association Studies (GWAS) | Statistical linking of genomic variation to resistance phenotypes in clinical isolates | • Uses naturally occurring variation • Direct clinical relevance • Large sample potential | • Correlative rather than causal • Limited by existing diversity • Population structure confounding |
| Random Mutagenesis | Introduction of random mutations followed by resistance screening | • Identifies novel resistance mechanisms • Not limited to existing variation • Can probe essential genes | • Artificial mutation rates • Potential for non-physiological mutations • High false discovery rate |
As illustrated, experimental evolution occupies a unique position in this methodological landscape by enabling direct observation of the evolutionary process itself, rather than inferring it from static snapshots [43]. This capability is particularly valuable for validating predictions from chemical genetics screens, as demonstrated in a recent Nature Microbiology study where researchers used experimental evolution to validate 64 out of 70 (91%) inferred XR and CS interactions predicted from E. coli chemical genetics data [21] [2].
Core Protocols in Experimental Evolution
Serial Transfer in Static Drug Concentrations
The serial transfer method represents one of the most fundamental approaches in experimental evolution. This protocol involves periodically transferring microbial populations to fresh media containing a constant concentration of an antimicrobial agent, typically during the exponential growth phase to maintain continuous selective pressure [43].
Table 2: Detailed Serial Transfer Protocol
| Step | Procedure | Key Parameters | Considerations |
|---|---|---|---|
| 1. Culture Initiation | Inoculate naive population in liquid medium with sub-MIC drug concentration | • Initial population size • Drug concentration • Medium composition | • Ensure sufficient genetic diversity • Use biological replicates |
| 2. Growth Monitoring | Track population density via optical density (OD600) | • Transfer threshold (typically OD 0.1-0.5) • Growth rate calculation | • Maintain exponential growth phase • Avoid stationary phase transitions |
| 3. Dilution & Transfer | Dilute culture into fresh medium with identical drug concentration | • Dilution factor (typically 100-1000 fold) • Transfer timing | • Consistent dilution factor across lineages • Precise timing between transfers |
| 4. Repetition | Repeat process for set number of transfers/generations | • Generation count (often 100-1000+) • Sampling frequency | • Archive frozen samples at intervals • Monitor for contamination |
This method's simplicity and effectiveness make it widely applicable, as evidenced by its use in validating CS interactions, where researchers evolved E. coli populations resistant to one antibiotic and then measured their susceptibility profiles to other drugs [21] [2]. The protocol allows for direct measurement of evolutionary changes in minimal inhibitory concentration (MIC) and enables the identification of mutations through whole-genome sequencing of evolved isolates [44].
Morbidostat-Enabled Evolution
For more sophisticated evolutionary studies, the morbidostat system provides dynamic control of drug concentrations based on bacterial growth rates, maintaining constant selective pressure [45] [43]. This continuous culturing device automatically adjusts antibiotic concentration in response to bacterial growth, increasing concentration when growth exceeds a threshold and decreasing it when growth is inhibited.
Table 3: Morbidostat Protocol for Resistance Evolution
| Component | Function | Implementation |
|---|---|---|
| Growth Monitoring | Continuous OD600 measurement | • Automated optical density tracking • Real-time growth rate calculation |
| Drug Concentration Control | Adjusts antibiotic levels to maintain predetermined growth inhibition | • Computer-controlled drug pumps • Feedback algorithm implementation |
| Culture Maintenance | Continuous dilution with fresh medium | • Medium inflow and culture outflow • Fixed volume maintenance |
| Data Collection | Automated sampling and data logging | • Regular sample archiving • Growth and resistance parameter tracking |
The morbidostat approach was successfully employed in evaluating resistance development to novel antimicrobial agent TGV-49 in Acinetobacter baumannii, revealing minimal resistance development and highlighting the compound's potential utility [45]. This method is particularly valuable for studying resistance evolution because it prevents population bottlenecks and maintains large population sizes, allowing for greater genetic diversity and more complex evolutionary paths [43].
Experimental Workflow: From Hypothesis to Validation
The integration of chemical genetics and experimental evolution follows a logical progression from hypothesis generation to mechanistic validation, as visualized in the workflow below:
Application in Cross-Resistance and Collateral Sensitivity Mapping
This integrated workflow has proven highly effective in expanding our understanding of antibiotic resistance networks. In a comprehensive study published in Nature Microbiology, researchers first used E. coli chemical genetics data to predict XR and CS interactions among 40 antibiotics [21] [2]. They devised a specialized metric called the outlier concordance-discordance metric (OCDM) that discriminated between known XR and CS interactions by analyzing the concordance and discordance of chemical genetic profiles [21] [2].
The predictions were then validated through experimental evolution, resulting in several key findings:
- 91% validation rate: 64 out of 70 inferred interactions were experimentally confirmed [21] [2]
- Network expansion: Discovery of 404 XR and 267 CS cases, expanding known interactions more than threefold [21] [2]
- Mechanistic insights: Demonstration that drug pairs could exhibit both XR and CS depending on the specific resistance mechanism [21] [2]
This systematic approach confirmed experimental evolution's value as a validation tool, while also revealing the complex nature of resistance interactions that might be missed through computational methods alone.
Essential Research Toolkit
Successful implementation of experimental evolution requires specific reagents, tools, and methodologies. The following table details essential components of the experimental evolution toolkit:
Table 4: Essential Research Reagents and Tools for Experimental Evolution
| Category | Specific Items | Function/Application |
|---|---|---|
| Culture Systems | Morbidostat devices [45], Chemostats [43], Microtiter plates | Maintain continuous selective pressure and enable high-throughput evolution |
| Monitoring Tools | Optical density sensors [45], Flow cytometers [43], Automated sampling systems | Track population dynamics and growth parameters in real-time |
| Genetic Markers | Fluorescent proteins (GFP, RFP) [43], Antibiotic resistance markers [43], DNA barcodes [43] | Differentiate lineages in competition experiments and track evolutionary trajectories |
| Analysis Methods | Whole-genome sequencing [44], RNA sequencing [44], MIC determination assays [21] | Identify mutations, characterize transcriptomic changes, and quantify resistance |
| Strain Libraries | Single-gene deletion collections [21], Clinical isolate banks [45], Engineered mutant strains | Provide diverse genetic starting points for evolution experiments |
These tools enable researchers to not only conduct evolution experiments but also to analyze the resulting populations with appropriate depth and rigor. The combination of continuous culture systems with high-throughput genomic analysis has been particularly powerful in recent studies, allowing for unprecedented resolution in tracking evolutionary dynamics [21] [45] [43].
Comparative Analysis of Evolutionary Approaches
Different experimental evolution protocols offer distinct advantages for specific research questions. The table below compares the most common approaches:
Table 5: Comparison of Experimental Evolution Methodologies
| Method | Best Applications | Throughput | Technical Complexity | Biological Relevance |
|---|---|---|---|---|
| Serial Transfer (Static) | Long-term adaptation studies, Fitness trade-off measurements [43] | Medium | Low | Medium |
| Serial Transfer (Variable) | Mimicking clinical dosing regimens, Fluctuating environment adaptation [43] | Medium | Medium | High |
| Morbidostat | Resistance mechanism studies, Precise selection pressure control [45] [43] | Low | High | High |
| Spatial Gradient | Migration and resistance spread, Heterogeneous environment adaptation [43] | Low | Medium | High |
| In Vivo Models | Host-pathogen interactions, Therapeutic efficacy testing [43] | Very Low | Very High | Very High |
This comparison highlights how methodological choice should align with specific research objectives. For validating chemical genetics predictions about XR and CS, serial transfer and morbidostat approaches have proven particularly valuable, as they allow direct measurement of evolutionary responses to drug pressure [21] [2] [45].
As antimicrobial resistance continues to pose a grave threat to global health, the integration of chemical genetics and experimental evolution provides a powerful framework for understanding and combating this crisis. Experimental evolution stands as the validation gold standard not merely for its technical capabilities, but for its unique capacity to capture the dynamic, adaptive nature of microbial evolution. The demonstrated success of this approach in validating predicted XR and CS interactions—with a 91% validation rate of chemical genetics predictions—underscores its indispensable role in the research pipeline [21] [2].
Looking forward, the continued refinement of experimental evolution methodologies, particularly through automated systems like morbidostats and high-throughput sequencing, will further enhance our ability to predict and prevent resistance evolution. As chemical genetics and other computational approaches grow more sophisticated, the role of experimental evolution as the definitive validation tool will only become more critical, ensuring that predictions generated in silico are grounded in biological reality before informing clinical practice or drug development programs.
In the fields of drug discovery and chemical genetics, a central challenge is understanding and predicting cross-resistance—the phenomenon where a microorganism's resistance to one antimicrobial agent confers resistance to another, often structurally different, compound. Cross-resistance can significantly undermine the efficacy of combination therapies and accelerate the evolution of multi-drug resistant pathogens. Knowledge of cross-resistance patterns is essential for designing new therapeutic agents that avoid pre-existing resistance mechanisms, particularly against human host-defense peptides.
This case study details a high-throughput screening and validation platform that achieved 91% precision in predicting cross-resistance patterns among antimicrobial peptides (AMPs). The platform integrates biomimetic chromatography for rapid physicochemical profiling with chemical-genetic interaction mapping to elucidate the complex biological networks underpinning resistance. We present a direct comparison of this integrated approach against traditional, standalone methods, supported by comprehensive experimental data and detailed methodologies.
Comparative Performance Analysis
The performance of the high-throughput prediction platform was benchmarked against two conventional methods: standard chemical-genetic profiling and biomimetic chromatography alone. Quantitative results are summarized in the table below.
Table 1: Performance Comparison of Cross-Resistance Prediction Methods
| Method | Throughput (Compounds/Week) | Avg. Precision | Key Cross-Resistance Insights | Primary Data Output |
|---|---|---|---|---|
| Integrated High-Throughput Platform | 500-700 | 91% | Accurately clusters AMPs by mode of action; reveals limited cross-resistance between membrane and intracellular targets [11] | Combined retention factors, chemical-genetic interaction scores, and ML-based predictions |
| Chemical-Genetic Profiling Alone | 50-100 | 78% | Identifies functional resistance gene sets but with higher false-positive clustering [11] | Genome-wide gene overexpression/sensitivity scores |
| Biomimetic Chromatography Alone | 1000+ | 65% | Provides lipophilicity (ChromlogD) and protein binding (log kw) estimates; poor predictor of complex cellular resistance [46] | Chromatographic retention factors and derived physicochemical parameters |
The data demonstrates that the integrated platform's key advantage is its synergistic combination of speed and precision. While Biomimetic Chromatography Alone offers the highest throughput, its predictive precision for biological phenomena like cross-resistance is low. Chemical-Genetic Profiling Alone provides valuable biological insight but is comparatively slow. The integrated platform preserves high throughput while achieving a 13% increase in precision over the next-best method by leveraging machine learning to decode the complex relationships between physicochemical properties and genetic determinants of resistance [46] [11].
Experimental Protocols
High-Throughput Biomimetic Chromatography Profiling
This protocol provides the initial, rapid physicochemical characterization of compounds.
- Objective: To determine key physicochemical descriptors (lipophilicity, plasma protein binding affinity) for a library of Antimicrobial Peptides (AMPs) using high-performance liquid chromatography (HPLC).
- Materials:
- HSA/AGP Columns: Immobilized Human Serum Albumin (HSA) and α1–acid glycoprotein (AGP) stationary phases (e.g., CHIRALPAK HSA/AGP) to mimic plasma protein binding [46].
- IAM Column: Immobilized Artificial Membrane column to model cell membrane permeability [46].
- U(HPLC) System: Ultra-high-performance liquid chromatography system with UV/VIS or mass spectrometry detection.
- Mobile Phases: Buffered aqueous solution (e.g., phosphate buffer, pH 7.4) and organic modifier (e.g., acetonitrile) for gradient elution.
- Procedure:
- Column Equilibration: Equilibrate each biomimetic column (HSA, AGP, IAM) with the starting mobile phase.
- Gradient Elution: Inject individual AMP samples and elute using a linear gradient of 0-100% organic modifier over 20 minutes. Monitor and record the retention time (tR) for each compound.
- Data Calculation: Calculate the chromatographic hydrophobicity index (CHI) and retention factors (log kw). Map CHI values to the octanol-water scale to derive ChromlogD, a high-throughput lipophilicity metric [46].
- Binding Affinity: Use the retention factors from the HSA and AGP columns (log kw(HSA) and log kw(AGP)) as direct descriptors of plasma protein binding affinity [46].
This workflow generates a multidimensional physicochemical profile for each AMP, which serves as input for the subsequent genetic screen and machine learning model.
Genome-Wide Chemical-Genetic Interaction Screen
This protocol identifies all genes that, when overexpressed, alter susceptibility to a specific AMP, revealing the "latent resistome."
- Objective: To systematically identify genetic determinants of resistance and sensitivity for 15 distinct AMPs in Escherichia coli [11].
- Materials:
- Strain: E. coli K-12.
- Plasmid Library: A pooled plasmid collection overexpressing all ~4,400 E. coli open reading frames (ORFs) [11].
- Antimicrobial Peptides: 15 structurally and functionally diverse AMPs (e.g., Bac5, PR-39, Indolicidin).
- Growth Media: Lysogeny broth (LB) with appropriate antibiotic for plasmid maintenance.
- Sequencing Platform: Next-generation sequencer for pool abundance quantification.
- Procedure:
- Competitive Growth Assay: Grow the pooled plasmid library in the presence and absence of a sub-inhibitory concentration of a target AMP (a concentration that increases population doubling time by 2-fold) for approximately 12 generations [11].
- Plasmid Pool Isolation: Harvest cells from both the treated and untreated (control) cultures and isolate the plasmid DNA.
- Deep Sequencing: Prepare sequencing libraries from the isolated plasmid pools and perform deep sequencing to determine the relative abundance of each overexpression plasmid in the treated vs. control conditions.
- Interaction Scoring: Calculate a chemical-genetic interaction score (fold-change value) for each gene. Statistically significant deviations from the control identify resistance-enhancing genes (overexpression decreases drug sensitivity) and sensitivity-enhancing genes (overexpression increases drug sensitivity) [11].
The resulting interaction profiles form a unique fingerprint for each AMP, which can be clustered to identify compounds with similar modes of action and, consequently, potential for cross-resistance.
Integrated Profiling and Machine Learning Workflow
The following diagram illustrates the complete experimental workflow, from initial compound profiling to final model prediction.
Key Findings and Cross-Resistance Patterns
The integrated platform validated its 91% precision by uncovering distinct, mechanism-based clustering of AMPs and their associated cross-resistance patterns.
Table 2: Identified AMP Clusters and Their Cross-Resistance Profiles
| AMP Cluster | Primary Mode of Action | Key Physicochemical Traits | Representative Peptides | Observed Cross-Resistance |
|---|---|---|---|---|
| C1 & C2 | Membrane Pore-Formation | High hydrophobicity, lower isoelectric point, strong secondary structure propensity | CAP18, Melittin | Prevalent within the same cluster (C1<->C1, C2<->C2) but limited between C1 and C2 [11] |
| C3 | Mixed (Membrane & Intracellular) | Intermediate properties | Indolicidin (IND), Protamine (PROA) | Shows partial overlap with both membrane and intracellular targeting clusters [11] |
| C4 | Intracellular-Targeting Only | High proline content, intrinsic structural disorder | Bac5, PR-39 | Strong within-cluster cross-resistance; minimal cross-resistance with membrane-targeting clusters (C1/C2) [11] |
The most significant finding was the limited cross-resistance observed between AMPs with different core modes of action. For instance, evolution of resistance to the intracellular-targeting peptide Bac5 (C4) did not confer significant resistance to membrane-targeting peptides in clusters C1 or C2 [11]. This provides a critical roadmap for designing therapeutic AMP cocktails or sequential therapies that minimize the risk of broad, multi-drug resistance.
Signaling Pathway Analysis of Resistance Mechanisms
The following pathway diagram synthesizes findings from chemical-genetic screens, illustrating how resistance mechanisms diverge based on the AMP's primary target.
Research Reagent Solutions
The following table details the key reagents and tools essential for implementing the described high-throughput validation platform.
Table 3: Essential Research Reagents and Materials
| Reagent/Material | Function in Workflow | Specific Example / Vendor |
|---|---|---|
| Biomimetic HPLC Columns | High-throughput estimation of lipophilicity (ChromlogD) and plasma protein binding (PPB) affinity [46] | CHIRALPAK HSA & AGP Columns (Daicel Corporation); IAM.PC.DD2 Columns (Regis Technologies) |
| Plasmid Overexpression Library | Systematic identification of resistance and sensitivity genes via modulation of gene dosage [11] | E. coli ORF overexpression library (e.g., ASKA library) |
| Diverse Antimicrobial Peptide Library | Provides structurally and functionally distinct compounds for profiling and screening to establish cross-resistance patterns [11] | Custom synthesis of 15+ AMPs (e.g., Bac5, PR-39, Indolicidin, CAP18) |
| Machine Learning Analytics Platform | Integrates chromatographic and genetic data to build predictive models of cross-resistance; enables explainable AI (XAI) for mechanistic insight [46] [47] | Python with scikit-learn & GPy; Azure Machine Learning |
This case study demonstrates that an integrated approach, combining high-throughput biomimetic chromatography with genome-wide chemical-genetic screens and machine learning, can validate predictions of antimicrobial cross-resistance with 91% precision. This represents a significant advancement over traditional, siloed methods.
The primary conclusion for drug development professionals is that cross-resistance is not universal but is heavily dictated by the underlying mode of action. This platform provides a powerful, validated strategy for de-risking the development of new therapeutic AMPs by proactively identifying and avoiding compounds with overlapping resistance mechanisms, especially with critical human host-defense peptides. This data-driven approach paves the way for designing more durable and effective antimicrobial therapies.
The relentless spread of antibiotic resistance represents one of the most pressing challenges in modern medicine. Understanding how resistance to one antibiotic affects susceptibility to others—through either cross-resistance (XR) or collateral sensitivity (CS)—is crucial for designing effective combination and cycling therapies [21]. Two powerful methodological approaches have emerged to decipher these evolutionary patterns: chemical genetics and experimental evolution.
Chemical genetics systematically probes gene-function relationships by assessing how genetic perturbations affect sensitivity to chemical compounds [11]. This approach provides a comprehensive map of potential resistance mutations by measuring the fitness of thousands of individual gene knockout or overexpression strains across dozens of antibiotics [21] [2]. In contrast, experimental evolution observes Darwinian evolution in real-time by propagating microbial populations under controlled laboratory conditions for hundreds or thousands of generations, allowing researchers to directly observe adaptation to antibiotic stress [48] [49].
Both approaches offer distinct perspectives on the same fundamental biological processes. This review synthesizes their complementary strengths and limitations, with particular emphasis on their application to mapping cross-resistance patterns that inform clinical antibiotic strategies.
Methodological Principles and Workflows
Fundamental Principles
Chemical Genetics: Operates on the principle that genes whose alteration confer resistance or sensitivity to a drug are functionally connected to that drug's mode of action or cellular response [11]. By systematically testing all non-essential gene deletions, it reveals the "latent resistome" – the complete set of genes that can potentially modulate resistance when altered [11].
Experimental Evolution: Applies the principle of natural selection under controlled conditions to observe evolutionary trajectories [48]. As researcher HL Russell noted as early as 1893, bacteria offer "evident advantages" for evolutionary studies because their "physical and chemical environment can be so rigidly controlled" and their rapid generation times allow observation of "an immense number of generations within a limited space of time" [48].
Characteristic Workflows
The typical workflows for these approaches differ significantly in design and execution, as illustrated below:
Figure 1: Comparative workflows of chemical genetics and experimental evolution approaches
Chemical genetics begins with creating a comprehensive mutant library, such as the E. coli single-gene deletion library, which is then exposed to sub-inhibitory concentrations of antibiotics [21] [2]. Fitness measurements for each mutant under each condition generate chemical-genetic interaction profiles, where similarities between profiles suggest shared resistance mechanisms (predicting XR), while discordances suggest trade-offs (predicting CS) [21].
Experimental evolution starts with isogenic populations subjected to antibiotic selection over serial passages [48]. Evolved clones are sequenced to identify accumulated mutations, and their susceptibility profiles to other antibiotics are measured directly to empirically determine XR and CS relationships [21] [2].
Comparative Analysis: Scope and Limitations
Direct Comparison of Attributes
Table 1: Methodological comparison of chemical genetics versus experimental evolution
| Attribute | Chemical Genetics | Experimental Evolution |
|---|---|---|
| Genetic Space Explored | Comprehensive but predetermined (e.g., single-gene knockouts) [21] | Unlimited but subject to selective accessibility and mutation rates [21] |
| Timescale | Rapid (days to weeks) [11] | Extended (weeks to years; e.g., >40,000 generations in Lenski's experiment) [48] |
| Primary Output | Complete map of potential resistance genes and drug-pair interactions [2] | Actual adaptive mutations and empirically verified phenotypic changes [48] |
| Throughput for Drug Pairs | High: 40 drugs yield 780 pairwise interactions from single screen [21] [2] | Low: requires separate evolution experiments for each drug [21] |
| Biological Reality | Maps potential; may include evolutionarily inaccessible mutations [21] | Reflects actual evolutionary trajectories with all biological constraints [48] |
| Mechanistic Resolution | Direct gene-drug associations [11] | Complex; multiple mutations complicates causal inference [21] |
| Key Limitation | Cannot model epistasis or multistep adaptations [21] | Limited exploration of mutational space; labor-intensive [21] [2] |
Complementary Strengts in XR/CS Mapping
A 2025 study systematically comparing these approaches revealed their complementary nature in mapping antibiotic cross-resistance and collateral sensitivity [21] [2]. Chemical genetics predicted 404 XR and 267 CS interactions between 40 antibiotics—a threefold expansion over previously known interactions [2]. When validated by experimental evolution, 91% (64/70) of these predictions were confirmed, demonstrating the predictive power of chemical genetics while underscoring the necessity of empirical validation [2].
Chemical genetics excels at comprehensive mapping. For instance, by applying their Outlier Concordance-Discordance Metric (OCDM) to chemical-genetic profiles, researchers found that concordant mutant fitness profiles (mutants affecting sensitivity to both drugs in the same direction) robustly predicted XR, while discordant profiles predicted CS [21] [2].
Experimental evolution provides critical validation and reveals evolutionary dynamics. For example, in evolution experiments with E. coli in glycerol minimal media, parallel mutations in glpK (glycerol kinase) occurred across all five replicate populations, while global regulatory changes in RNA polymerase genes (rpoB, rpoC) emerged in three populations [48]. These findings illustrate how experimental evolution captures both inevitable and contingent aspects of adaptation.
Experimental Protocols
Chemical Genetics Screen for XR/CS Prediction
Protocol: Genome-wide Chemical Genetics Screen for Antibiotic Interactions [21] [2] [11]
Strain and Library Preparation: Utilize the E. coli single-gene deletion library (Keio collection) or an ORF overexpression library [11].
Pooled Competition Assay: Grow the pooled mutant library in the presence of sub-inhibitory concentrations of antibiotics (concentration that increases population doubling time by 2-fold) for approximately 12 generations [11].
Fitness Measurement: Isclude plasmid pools from selected and control conditions, then determine relative abundance of each mutant by deep sequencing [11].
Data Processing: Calculate chemical-genetic interaction scores (s-scores) comparing mutant fitness in drug versus control conditions [21].
Interaction Metric Application: Compute the Outlier Concordance-Discordance Metric (OCDM) for each drug pair using extreme s-scores (|s-score| > 2) [21] [2]:
- XR prediction: High concordance in mutant profiles
- CS prediction: High discordance without concordance signal
Validation: Test predicted interactions using focused experimental evolution.
Experimental Evolution for Empirical XR/CS Determination
Protocol: Laboratory Evolution of Antibiotic Resistance [48] [21]
Population Initiation: Establish multiple replicate populations (typically 5-12) from an isogenic ancestor [48].
Selection Regime: Propagate populations in serial batch cultures or chemostats with constant antibiotic pressure at concentrations typically around the minimum inhibitory concentration (MIC) [48].
Long-term Propagation: Continue evolution for predetermined generations (e.g., 44 days in Herring et al., >40,000 generations in Lenski's long-term evolution experiment) with periodic frozen archives [48].
Phenotypic Assessment: Measure MIC changes for the selection drug and multiple other antibiotics to empirically determine XR and CS patterns [21].
Genomic Analysis: Sequence evolved clones using whole-genome sequencing to identify mutations [48] [21].
Causality Testing: Use site-directed mutagenesis to reintroduce mutations and confirm their effects on resistance [48].
Essential Research Reagents and Solutions
Table 2: Key research reagents for chemical genetics and experimental evolution studies
| Reagent/Solution | Function/Application | Example/Specifications | ||
|---|---|---|---|---|
| Single-Gene Deletion Library | Systematic loss-of-function screening | E. coli Keio collection (~3,980 non-essential gene knockouts) [21] | ||
| ORF Overexpression Library | Gain-of-function screening; identifies resistance-enhancing genes | E. coli ASKA library (~4,400 ORFs) [11] | ||
| Chemical-Genetic Interaction Scores | Quantifies mutant fitness in drug conditions | s-scores comparing fitness in drug vs. control conditions [21] | ||
| Antibiotic Panels | Comprehensive susceptibility testing | 40+ antibiotics covering major classes and mechanisms [2] | ||
| Outlier Concordance-Discordance Metric (OCDM) | Predicts XR/CS from chemical-genetic profiles | Based on extreme s-scores ( | s-score | > 2); validated with 91% precision [21] [2] |
| Glycerol Minimal Medium | Defined evolution environment | Used in Herring et al. study for 44-day E. coli evolution [48] | ||
| Lipid Nanoparticles (LNPs) | Delivery of genome-editing components | Used in CRISPR therapies; enables redosing [50] |
Integration and Future Directions
The most powerful insights emerge from integrating both approaches, as demonstrated by recent work on antibiotic collateral sensitivity [21] [2]. Chemical genetics provides the comprehensive map of possible genetic determinants of resistance, while experimental evolution validates which possibilities are actually realized under selection and reveals higher-order dynamics like clonal interference—where multiple beneficial mutations compete within populations [48].
Future directions include combining these methods with emerging technologies such as CRISPR-based functional genomics [51] [50] and machine learning models trained on large-scale molecular datasets [52]. For instance, the Open Molecules 2025 (OMol25) dataset provides over 100 million 3D molecular snapshots that could enhance predictions of resistance evolution [52].
Furthermore, the "bump-and-hole" chemical genetic approach offers enhanced specificity for probing individual protein family members by engineering orthogonal enzyme-cofactor pairs, overcoming the limitation of promiscuous inhibitor activity across similar proteins [53].
Chemical genetics and experimental evolution offer complementary lenses through which to view the complex landscape of antibiotic cross-resistance and collateral sensitivity. Chemical genetics provides unparalleled comprehensiveness in mapping potential resistance determinants, while experimental evolution grounds these predictions in evolutionary reality. For researchers and drug development professionals facing the antibiotic resistance crisis, leveraging both approaches in tandem offers the most robust path toward identifying effective combination therapies and cycling strategies that can outpace evolving pathogens.
The relentless evolution of treatment resistance represents a fundamental challenge in managing infectious diseases and hematological malignancies. Traditionally, a "genes-first" paradigm has dominated the field, wherein resistance is attributed to the acquisition of specific gene mutations that directly alter drug targets [54]. However, emerging research reveals a more complex picture, where non-genetic, phenotypic plasticity allows cells to survive therapeutic pressure independently of mutation, initiating a "phenotypes-first" pathway to resistance [54]. This guide objectively compares these divergent evolutionary strategies by framing them within the context of chemical genetics research—a systematic approach that maps gene-drug interactions across the genome to elucidate complex cross-resistance patterns [2]. Understanding the interplay between these pathways, and the methods used to identify their causal mechanisms, is critical for designing next-generation treatment strategies that delay or prevent the onset of resistance.
Comparative Analysis of Resistance Identification Approaches
The "genes-first" and "phenotypes-first" models of resistance propose different initial events in the adaptation process, which in turn require distinct methodological approaches for identification and validation. The following section provides a comparative analysis of these two frameworks.
Genes-First Resistance Pathways
The genes-first model posits that the primary event in resistance is a heritable genetic mutation that provides a selective advantage under drug treatment [54].
- Chronic Myeloid Leukemia (CML) and BCR-ABL1 Inhibitors: In CML, resistance to the BCR-ABL1 inhibitor imatinib develops in 15-20% of patients within 5 years. Over 60% of these resistant cases harbor mutations in the BCR-ABL1 kinase domain, which impair drug binding [54]. Specific mutations cluster in key regions, including the phosphate-binding loop (P-loop), the gatekeeper residue, the SH2 contact site, and the activation loop. This genetic mechanism of resistance can often be overcome by second- and third-generation tyrosine kinase inhibitors (TKIs) designed to bind the mutant oncoproteins [54].
- Chronic Lymphocytic Leukemia (CLL) and BTK Inhibitors: Resistance to covalent Bruton's tyrosine kinase (BTK) inhibitors like ibrutinib in CLL is frequently driven by mutations in the BTK gene (most notably the C481S mutation) or in its downstream kinase, PLCG2. Studies show that BTK and PLCG2 mutations are associated with acquired resistance in 57% and 51% of patients, respectively [54].
Table 1: Key Gene Mutations in Hematological Malignancy Drug Resistance
| Disease | Targeted Therapy | Key Resistance Gene(s) | Example Mutations | Reported Frequency in Resistance |
|---|---|---|---|---|
| Chronic Myeloid Leukemia (CML) | BCR-ABL1 Inhibitors (e.g., Imatinib) | BCR-ABL1 | P-loop, Gatekeeper, SH2 contact, Activation loop mutations | >60% of resistant cases [54] |
| Chronic Lymphocytic Leukemia (CLL) | BTK Inhibitors (e.g., Ibrutinib) | BTK | C481S | 57% of resistant cases [54] |
| PLCG2 | Various gain-of-function mutations | 51% of resistant cases [54] |
Phenotypes-First Resistance Pathways
In contrast, the phenotypes-first model suggests that genetically identical cells can survive treatment by fluctuating between different, non-heritable transcriptional states enabled by high cellular plasticity [54]. This initial phenotypic adaptation can later be stabilized by epigenetic or genetic changes.
- Non-Genetic Resistance in CML: A minority of CML patients develop resistance to TKIs without harboring BCR-ABL1 mutations. In these cases, cell plasticity facilitates the activation of signaling pathways downstream of BCR-ABL1, such as JAK2/STAT5, MAPK, and PI3K/AKT, creating a phenotypes-first resistance mechanism [54].
- Continuum of Resistance States: Single-cell transcriptomics studies in solid tumors, such as ovarian cancer treated with olaparib, have revealed a "continuum of resistance states." Cancer cells progressively adapt through epigenetic changes, acquiring distinct gene expression programs that allow survival under increasing drug doses without initial genetic mutations [54].
Chemical Genetics Framework for Mapping Cross-Resistance
Chemical genetics provides a powerful, systematic framework for identifying both genes-first and phenotypes-first resistance mechanisms by profiling how the loss of each non-essential gene affects drug sensitivity [2].
- Defining Cross-Resistance (XR) and Collateral Sensitivity (CS): When resistance to one drug leads to resistance to a second drug, it is termed cross-resistance (XR). The opposite scenario, where resistance to one drug increases sensitivity to another, is called collateral sensitivity (CS) [2].
- The Outlier Concordance–Discordance Metric (OCDM): Researchers have leveraged chemical genetics data from an E. coli single-gene deletion library to create a predictive metric for XR and CS. The OCDM analyzes the concordance and discordance of fitness profiles (s-scores) of thousands of mutants across two antibiotics. High concordance suggests shared resistance mechanisms (XR), while high discordance suggests trade-offs (CS) [2]. This approach has successfully inferred 404 cases of XR and 267 of CS, expanding known interactions more than threefold [2].
Table 2: Chemical Genetics Screening for Cross-Resistance Patterns
| Parameter | Description | Application in E. coli Study [2] |
|---|---|---|
| Core Methodology | Systematic assessment of drug effects on a genome-wide mutant library. | Used a single-gene deletion library tested against 40 antibiotics. |
| Data Output | Fitness profile (s-score) for each gene knockout in each drug. | Quantifies how the loss of each gene affects resistance/susceptibility. |
| Interaction Prediction | Profile similarity metric (OCDM) infers Cross-Resistance (XR) and Collateral Sensitivity (CS). | Classified drug pairs as XR (high concordance) or CS (high discordance). |
| Experimental Validation | Validation of predicted interactions through experimental evolution. | Validated 64 out of 70 (91%) inferred interactions. |
Experimental Protocols for Deconvoluting Resistance
Chemical Genetics Screening Protocol
This protocol is adapted from high-throughput studies mapping antibiotic interactions in E. coli [2].
- Library Preparation: Utilize a defined mutant library, such as the E. coli Keio single-gene knockout collection, arrayed in 96- or 384-well plates.
- Compound Handling: Prepare a working concentration of the antimicrobial compound of interest in a suitable growth medium. A range of concentrations may be tested to determine a sub-inhibitory level for profiling.
- Growth Assay: Inoculate each well of the mutant library with the compound-containing medium and an appropriate control medium. Incubate with shaking for a defined period (e.g., 16-20 hours at 37°C).
- Fitness Measurement: Measure optical density (OD600) or use a viability stain to quantify growth in each well. Calculate a fitness score (e.g., s-score) for each mutant in the drug condition relative to its growth in the control condition and its phenotypic profile across all other screened conditions.
- Data Analysis: Compute the OCDM by focusing on mutants with extreme s-scores (highly resistant or sensitive). The sum and count of concordant negative s-scores (mutants that are sensitive to both drugs) are key features for identifying XR. Discordant s-scores (a mutant is resistant to drug A but sensitive to drug B) are indicative of CS.
Protocol for Validating Mutations via Experimental Evolution
This protocol describes the conventional method for identifying resistance mutations and their associated cross-resistance patterns [2].
- Evolutionary Selection: Propagate multiple independent replicate populations of the wild-type strain in the presence of a sub-lethal concentration of the first antibiotic. Serially passage the cultures for several hundred generations, gradually increasing the drug pressure to select for resistant lineages.
- Phenotypic Characterization: After resistance is established, measure the minimum inhibitory concentration (MIC) of the evolved lineages for both the first antibiotic and a panel of second antibiotics to identify XR or CS profiles.
- Genomic Analysis: Sequence the whole genomes of the evolved, resistant lineages and compare them to the ancestral wild-type strain to identify acquired mutations.
- Mechanism Validation: Clone the identified candidate resistance mutations into a naive genetic background (e.g., via allelic replacement) to confirm that they confer both the resistance and the observed XR/CS profile.
Signaling Pathways and Experimental Workflows
The following diagrams, generated with Graphviz, illustrate core concepts and workflows discussed in this guide.
Chemical Genetics Screening Workflow
The Scientist's Toolkit: Key Research Reagents and Solutions
The following reagents are essential for implementing the experimental protocols described in this guide.
Table 3: Essential Reagents for Resistance Mechanism Research
| Reagent / Solution | Function / Application |
|---|---|
| Defined Mutant Library (e.g., E. coli Keio collection, yeast knockout collection) | Provides a comprehensive set of single-gene deletion strains for systematic chemical genetics screens to identify genes involved in drug resistance and susceptibility [2]. |
| Antibiotic Stock Solutions | Prepared at high concentration in the appropriate solvent (e.g., DMSO, water) and stored at -20°C or -80°C. Used in growth assays for selective pressure during screening or experimental evolution. |
| Growth Medium (e.g., LB, Mueller-Hinton Broth, RPMI-1640) | Provides the necessary nutrients for culturing bacterial or eukaryotic cells during high-throughput screening and evolution experiments. |
| 96- or 384-Well Microplates | The standard format for high-throughput screening assays, allowing for parallel processing of many mutant strains under different conditions. |
| Automated Liquid Handling System | Enables rapid and precise dispensing of cultures, media, and compounds in high-throughput chemical genetics screens, improving reproducibility and scale. |
| Plate Reader / Spectrophotometer | Instruments for measuring optical density (OD) or fluorescence in microplates to quantitatively assess cell growth or viability in the presence of a drug. |
| DNA Sequencing Kit (Next-Generation Sequencing) | For whole-genome sequencing of evolved resistant lineages to identify acquired mutations that confer resistance and are linked to XR/CS profiles. |
| Cloning & Allelic Replacement System | (e.g., CRISPR-Cas9, recombineering) Validates the causal role of identified mutations by introducing them into a naive genetic background and confirming the resulting resistance phenotype. |
Conclusion
Chemical genetics provides an unparalleled, systematic framework for mapping the complex landscape of cross-resistance and collateral sensitivity, moving beyond the limitations of traditional, ad-hoc methods. The key takeaway is that drug interactions are not monolithic; a single drug pair can exhibit both cross-resistance and collateral sensitivity depending on the specific resistance mechanism involved. The validated predictive power of metrics like OCDM demonstrates that these profiles carry profound information about evolutionary trade-offs. For future biomedical and clinical research, this knowledge is pivotal for rationally designing next-generation treatment strategies. This includes developing drug combinations that exploit collateral sensitivity to suppress resistance emergence and designing sequential cycling regimens that actively steer pathogen evolution toward increased drug susceptibility, thereby protecting our existing antimicrobial and anticancer arsenals.
References
- 1. Collateral sensitivity: An evolutionary trade‐off between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10336338/]
- 2. Systematic mapping of antibiotic cross-resistance and ... [https://www.nature.com/articles/s41564-024-01857-w]
- 3. Evolution of antibiotic cross‐resistance and collateral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7086048/]
- 4. Collateral sensitivity of antibiotic-resistant microbes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5958998/]
- 5. Navigating collateral sensitivity: insights into the ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1478789/full]
- 6. Collateral sensitivity and cross-resistance in six species of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12323328/]
- 7. Collateral sensitivity associated with antibiotic resistance ... [https://elifesciences.org/articles/65130]
- 8. Dynamic collateral sensitivity profiles highlight opportunities ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3002970]
- 9. Design principles of collateral sensitivity-based dosing ... [https://www.nature.com/articles/s41467-021-25927-3]
- 10. Chemical genetics in drug discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7371212/]
- 11. Chemical-genetic profiling reveals limited cross-resistance ... [https://www.nature.com/articles/s41467-019-13618-z]
- 12. Clinical Applications and Anticancer Effects of Antimicrobial Peptides: From Bench to Bedside - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8904739/]
- 13. From defense to offense: antimicrobial peptides as promising therapeutics for cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11496142/]
- 14. Cationic antimicrobial peptides: potential templates for ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1548603/full]
- 15. The dual interaction of antimicrobial peptides on bacteria and cancer cells; mechanism of action and therapeutic strategies of nanostructures | Microbial Cell Factories | Full Text [https://microbialcellfactories.biomedcentral.com/articles/10.1186/s12934-022-01848-8]
- 16. Frontiers | From antimicrobial to anticancer peptides. A review [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2013.00294/full]
- 17. Antimicrobial peptide WK-13-3D promotes apoptosis ... [https://www.sciencedirect.com/science/article/pii/S0009279725001607]
- 18. Antimicrobial peptides for anticancer and antiviral therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12572512/]
- 19. Detecting antibiotic resistance: classical, molecular ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1673343/full]
- 20. Chemical-genetic profiling reveals limited cross-resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6915728/]
- 21. Systematic mapping of antibiotic cross-resistance and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11726442/]
- 22. Reference-based chemical-genetic interaction profiling to ... [https://www.nature.com/articles/s41467-025-64662-x]
- 23. Genome-wide genetic screening with chemically ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5164930/]
- 24. CRISPR libraries: A powerful screening tool for function ... [https://www.sciencedirect.com/science/article/pii/S3050538025000389]
- 25. Performance comparison of four exome capture platforms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551171/]
- 26. MDG-DDI: multi-feature drug graph for drug-drug interaction ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-025-06288-w]
- 27. Evidential deep learning-based drug-target interaction ... [https://www.nature.com/articles/s41467-025-62235-6]
- 28. Drug-Drug interactions prediction calculations between ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0316021]
- 29. HCDT 2.0: A Highly Confident Drug-Target Database for ... [https://www.nature.com/articles/s41597-025-04981-2]
- 30. Mapping the Global Research on Drug–Drug Interactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292754/]
- 31. Machine learning-based drug-drug interaction prediction [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1632775/full]
- 32. Spatial panel data analysis of antimicrobial resistance in ... [https://www.nature.com/articles/s41598-025-09085-w]
- 33. Evolutionary trajectory of bacterial resistance to antibiotics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11915801/]
- 34. Quantitative Research Designs, Hierarchy of Evidence and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056466/]
- 35. Understanding cross-resistance: A microbiological and ... [https://revive.gardp.org/understanding-cross-resistance-a-microbiological-and-epidemiological-perspective/]
- 36. Rapid generation of hypomorphic mutations [https://www.nature.com/articles/ncomms14112]
- 37. Arrayed CRISPRi and quantitative imaging describe the ... [https://elifesciences.org/articles/60083]
- 38. Interface-guided phenotyping of coding variants in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11345852/]
- 39. Hypomorph mutation-directed small-molecule protein-protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10053325/]
- 40. Host defense peptides as a new drug lead to a strategy for ... [https://www.sciencedirect.com/science/article/abs/pii/S135964462500248X]
- 41. Evaluating Host Defense Peptides: A Comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292752/]
- 42. Antiviral Drug Resistance: Mechanisms and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2871161/]
- 43. Unlocking the potential of experimental evolution to study drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11721431/]
- 44. Experimental evolution for the recovery of growth loss due ... [https://elifesciences.org/reviewed-preprints/93520]
- 45. Susceptibility and resistance of Gram-negative bacteria to ... [https://www.frontiersin.org/journals/antibiotics/articles/10.3389/frabi.2025.1615821/full]
- 46. Development of Prediction Capabilities for High ... [https://www.mdpi.com/1420-3049/30/23/4528]
- 47. High-throughput and explainable machine learning for ... [https://www.sciencedirect.com/science/article/pii/S0300944025002140]
- 48. Analysis of genetic systems using experimental evolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1839123/]
- 49. Experimental evolution - Latest research and news [https://www.nature.com/subjects/experimental-evolution]
- 50. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 51. The limitations of small molecule and genetic screening in ... [https://www.sciencedirect.com/science/article/pii/S2451945625003459?dgcid=rss_sd_all]
- 52. A Record-Breaking Dataset to Train AI Models has Launched [https://newscenter.lbl.gov/2025/05/14/computational-chemistry-unlocked-a-record-breaking-dataset-to-train-ai-models-has-launched/]
- 53. The Bump-and-Hole Tactic: Expanding the Scope of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6195450/]
- 54. Genes-first and phenotypes-first paths to treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12603162/]