Chemical Biology Platforms: The Engine of Modern Drug Discovery and Translational Physiology
This article explores the integral role of chemical biology platforms in bridging the gap between basic research and clinical application in drug discovery.
Chemical Biology Platforms: The Engine of Modern Drug Discovery and Translational Physiology
Abstract
This article explores the integral role of chemical biology platforms in bridging the gap between basic research and clinical application in drug discovery. Aimed at researchers, scientists, and drug development professionals, it provides a comprehensive examination of the field—from its foundational principles and key historical shifts to the latest methodological tools like chemoproteomics and AI. The scope extends to practical strategies for troubleshooting optimization challenges, contemporary validation techniques for assessing clinical potential, and a comparative analysis of platform efficiencies. By synthesizing insights across the translational continuum, this article serves as a strategic guide for leveraging chemical biology to enhance the efficacy and speed of therapeutic development.
From Potent Compounds to Clinical Benefit: The Evolution of a Discipline
The chemical biology platform represents an organizational and strategic framework within pharmaceutical research and development that is fundamentally rooted in a multidisciplinary, mechanism-based approach. Its evolution marks a significant departure from traditional, empirical drug discovery methods, driven by the critical need to demonstrate clear clinical benefit for highly potent, target-specific compounds [1]. This platform is defined by its systematic integration of knowledge across chemistry, biology, and physiology to optimize drug target identification and validation, thereby improving the safety and efficacy profiles of biopharmaceuticals [1].
The core philosophy of the chemical biology platform is its emphasis on understanding underlying biological processes and leveraging knowledge gained from the action of similar molecules on these processes [1]. It connects a series of strategic steps to determine whether a newly developed compound could translate into clinical benefit through the lens of translational physiology, which examines biological functions across multiple levels—from molecular interactions to population-wide effects [1]. This approach has become a critical component in modern drug development, fostering a mechanism-based pathway to clinical advancement that persists in both academic and industry-focused research environments [1].
Core Principles and Strategic Framework
Foundational Concepts and Definitions
At its essence, chemical biology involves the study and modulation of biological systems and the creation of biological response profiles through the use of small molecules that are selected or designed based on current knowledge of the structure, function, or physiology of biological targets [1]. Unlike traditional approaches that relied primarily on trial-and-error methods, even when using high-throughput technologies, chemical biology focuses on selecting target families and incorporates systems biology approaches to understand how protein networks integrate [1].
The chemical biology platform achieves its objectives through several defining characteristics:
- Multidisciplinary Teamwork: It relies on collaborative teams that accumulate knowledge and solve problems, often using parallel processes to accelerate timelines and reduce costs associated with bringing new drugs to patients [1].
- Targeted Selection: It emphasizes rational target selection over random screening approaches [1].
- Integration of Omics Technologies: It leverages systems biology techniques, including transcriptomics, proteomics, metabolomics, and network analyses, to comprehensively understand protein network interactions [1].
- Physiological Context: Physiology forms the core of the platform by providing essential biological context in which chemical tools and principles are applied to understand and influence living systems [1].
The Four-Step Translational Framework
A critical historical development in the chemical biology platform was the establishment of a systematic four-step framework, based on Koch's postulates, to indicate potential clinical benefits of new therapeutic agents [1]:
- Identify a disease parameter (biomarker)
- Show that the drug modifies that parameter in an animal model
- Show that the drug modifies the parameter in a human disease model
- Demonstrate a dose-dependent clinical benefit that correlates with similar change in direction of the biomarker
This framework was first operationalized through the creation of Clinical Biology departments in pharmaceutical companies, which were tasked with bridging the gap between preclinical findings and clinical outcomes [1]. This approach represented the first organized effort in the industry to focus on translational physiology, examining biological functions across levels spanning from molecules to cells to organs to populations [1].
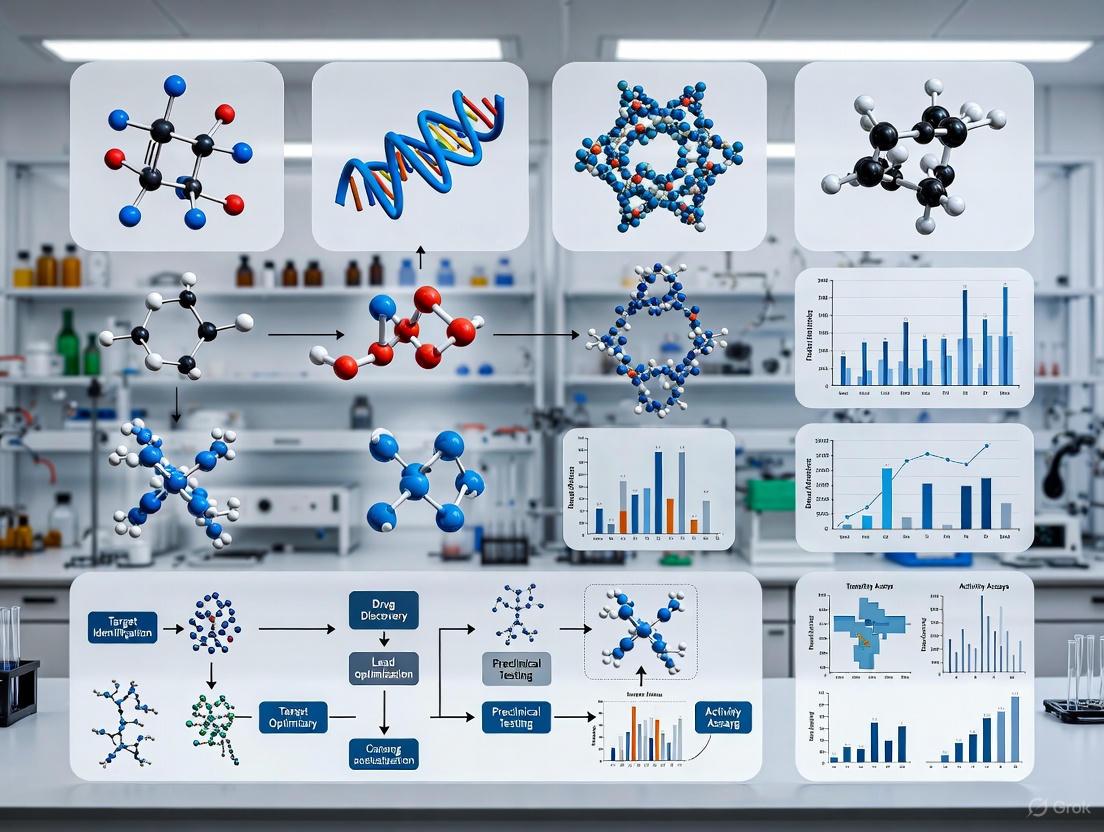
Figure 1: The Four-Step Translational Framework for validating clinical benefit of new therapeutic agents, adapted from the approach developed in Clinical Biology departments [1].
Key Methodologies and Experimental Approaches
Integrative Workflow for Target Validation
The chemical biology platform employs a sophisticated, integrated workflow that connects various technological and methodological approaches to validate therapeutic targets. This workflow synthesizes knowledge from diverse disciplines and technologies to establish a robust, mechanism-based understanding of drug-target interactions and their physiological consequences.
Figure 2: Integrated workflow of the chemical biology platform, synthesizing multiple technological approaches for target validation and lead optimization [1].
Advanced Cellular Assay Technologies
The platform incorporates sophisticated cellular assay technologies that enable multiparametric analysis of cellular events. These include:
- High-content multiparametric analysis using automated microscopy and image analysis to quantify cell viability, apoptosis, cell cycle analysis, protein translocation, and phenotypic profiling [1].
- Reporter gene assays to assess signal activation in response to ligand-receptor engagement [1].
- Ion channel activity assessment using voltage-sensitive dyes or patch-clamp techniques to screen neurological and cardiovascular drug targets [1].
These advanced cellular assays, often coupled with genetic manipulation capabilities, provide the functional data necessary to validate targets and optimize lead compounds within a physiological context [1].
Objective Assessment of Chemical Probes
A critical methodological advancement within the chemical biology platform is the development of objective, quantitative, data-driven assessment of chemical probes. Tools such as Probe Miner capitalize on public medicinal chemistry data to empower systematic evaluation of chemical probes across multiple parameters [2]. This approach involves:
- Systematic analysis of chemical probes to uncover new insights and limitations
- Novel data-driven scoring methodologies that enable objective assessment
- Public, regularly updated resources that equip researchers to evaluate probes
- Integration with expert curation to provide a powerful resource for probe selection
This quantitative framework addresses the critical need for high-quality chemical tools in biomedical research, particularly for target validation and understanding biological systems [2].
Quantitative Data in Chemical Biology Research
Key Performance Metrics and Standards
Quantitative assessment is fundamental to the chemical biology platform, with rigorous standards applied to evaluate compound suitability, assay performance, and experimental accuracy. The platform employs various statistical measures to ensure data quality and reproducibility.
Table 1: Key Quantitative Metrics for Experimental Assessment in Chemical Biology
| Metric | Calculation Formula | Application in Chemical Biology | Acceptance Criteria | ||
|---|---|---|---|---|---|
| Percent Error | `% error = | (measured value - expected value) / expected value | × 100` | Assessment of equipment accuracy (balances, pipettes) and experimental precision [3]. | Varies by application; lower values indicate greater accuracy. |
| Average Measured Mass | Average = (Mass1 + Mass2 + Mass3) / 3 |
Determination of mean values from replicate measurements to establish reliable baseline data [3]. | Replicates should show low variability. | ||
| Z-factor | `Z-factor = 1 - (3×(σsample + σcontrol) / | μsample - μcontrol | )` | Quality metric for high-throughput screening assays; measures assay signal dynamic range and data variation [1]. | Z' > 0.5 indicates excellent assay; Z' > 0.4 acceptable. |
| Coefficient of Variation (CV) | CV = (Standard Deviation / Mean) × 100% |
Measurement of precision and reproducibility in biochemical and cellular assays [1]. | Typically <20% for biological assays; <10% for analytical methods. |
Historical Distribution of Drug Targets
The implementation of the chemical biology platform in the pharmaceutical industry circa 2000 focused on approximately 500 targets across specific protein families, with the following distribution [1]:
Table 2: Historical Distribution of Drug Targets in Pharmaceutical Research (c. 2000)
| Target Class | Percentage of Industry Focus | Representative Therapeutic Areas |
|---|---|---|
| G-protein Coupled Receptors (GPCRs) | 45% | Cardiovascular, neurological, metabolic diseases |
| Enzymes | 25% | Oncology, inflammatory diseases, infectious diseases |
| Ion Channels | 15% | Neurological disorders, cardiovascular diseases |
| Nuclear Receptors | ~2% | Metabolic diseases, endocrine disorders |
| Other Targets | ~13% | Various therapeutic areas |
This targeted distribution reflects the mechanism-based approach of chemical biology, focusing on target families with well-characterized physiological functions and therapeutic potential [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
The experimental implementation of the chemical biology platform relies on a carefully selected set of research reagents and tools that enable the precise manipulation and analysis of biological systems.
Table 3: Essential Research Reagent Solutions for Chemical Biology Investigations
| Reagent/Tool Category | Specific Examples | Function in Chemical Biology Research |
|---|---|---|
| Chemical Probes | Selective kinase inhibitors, GPCR modulators, epigenetic probes | Tool compounds for perturbing and understanding specific biological targets and pathways; essential for target validation [2]. |
| Cellular Assay Systems | Reporter gene assays, voltage-sensitive dyes, high-content screening assays | Functional assessment of compound effects in cellular contexts; provides physiological relevance to molecular interactions [1]. |
| Biomarker Detection Reagents | Selective antibodies, molecular probes, binding agents | Identification and quantification of disease parameters and target engagement in both animal models and human disease models [1]. |
| Characterized Biological Models | Genetically engineered cell lines, animal models of disease, human disease models | Systems for evaluating compound effects across translational continuum from in vitro to in vivo contexts [1]. |
| Analytical Standards | Internal standards, reference compounds, quality control materials | Ensuring accuracy, precision, and reproducibility of quantitative measurements across experimental systems [3]. |
Implementation in Drug Discovery and Development
Integrated Discovery Workflow
The chemical biology platform operates through an integrated workflow that spans from initial target identification to clinical proof-of-concept, with decision points that determine progression of compounds through the development pipeline.
Figure 3: Implementation workflow of the chemical biology platform in pharmaceutical R&D, showing the critical role of Clinical Biology in bridging preclinical and clinical development [1].
Impact on Translational Physiology
The chemical biology platform has profoundly influenced translational physiology by providing a systematic framework for examining biological functions across multiple levels of organization. This integration has enabled researchers to:
- Bridge molecular and systems biology by connecting precise molecular interventions with organism-level physiological responses [1].
- Identify and validate targets within their physiological context, ensuring therapeutic relevance [1].
- Develop tools for directed application that are biologically meaningful, relevant, and translatable to real-world health and disease contexts [1].
- Discover drugs for therapeutic use through mechanism-based approaches that prioritize understanding of physiological systems [1].
The platform's emphasis on physiology as its core ensures that chemical tools and insights maintain biological relevance throughout the drug discovery and development process [1].
The chemical biology platform continues to evolve, incorporating new technologies and methodologies that enhance its mechanism-based, multidisciplinary approach. The integration of objective, quantitative assessment tools for chemical probes represents a significant advancement in ensuring the quality and reliability of research tools used in the platform [2]. Furthermore, the growing emphasis on precision medicine aligns perfectly with the platform's foundational principles of targeted, mechanism-based therapeutic development [1].
The continued influence of the chemical biology platform in both academic research and pharmaceutical innovation underscores its value as a framework for advancing clinical medicine through rigorous, physiology-informed science. As the platform incorporates emerging technologies such as artificial intelligence and advanced data analytics, its capacity to bridge the gap between basic chemical biology and clinical application will only strengthen, further solidifying its role as a critical component in modern drug development and translational research.
For researchers implementing this platform, understanding its historical development, integrative nature, and foundation in translational physiology is essential for designing experimental studies that effectively connect molecular interventions with physiological outcomes and, ultimately, clinical benefit [1].
The pharmaceutical research landscape of the late 20th century faced a fundamental crisis: the inability to translate potent, mechanism-specific compounds into demonstrated clinical benefit. This efficacy challenge catalyzed a paradigm shift from traditional trial-and-error approaches to integrated research models centered on chemical biology and translational physiology. This whitepaper examines the historical evolution of this pivot, detailing how the strategic integration of multidisciplinary teams, biomarker validation, and systems biology technologies addressed critical translational gaps. For today's researchers and drug development professionals, understanding this historical transition provides foundational insights for designing modern experimental studies that effectively bridge laboratory discovery and clinical application.
The final decades of the 20th century marked a pivotal period in pharmaceutical research. While advances in chemistry and molecular biology enabled the production of highly potent compounds targeting specific biological mechanisms, the industry confronted a formidable obstacle: demonstrating meaningful clinical benefit in patients [1]. This efficacy challenge emerged as the primary bottleneck in the drug development pipeline, where promising laboratory results consistently failed to translate into successful human therapeutics.
The traditional drug development approach relied heavily on trial-and-error methodologies, including high-throughput screening campaigns that often prioritized quantity over biological relevance [1]. This model generated numerous potent compounds but provided insufficient understanding of their interaction with complex physiological systems. The fundamental gap between mechanistic potency and clinical efficacy exposed systemic limitations in the prevailing research paradigm, necessitating a fundamental restructuring of pharmaceutical R&D strategy.
Regulatory changes further intensified this crisis. The 1962 Kefauver-Harris Amendment, enacted in response to the thalidomide tragedy, mandated proof of efficacy from "adequate and well-controlled clinical trials" [1]. This requirement bifurcated Phase II clinical evaluation into distinct components: Phase IIa for identifying potential disease targets and Phase IIb/III for demonstrating statistical proof of efficacy and safety. This regulatory landscape demanded more sophisticated approaches to establishing drug efficacy earlier in the development process.
The Rise of Translational Physiology and Clinical Biology
Foundational Concepts and Definitions
The response to the efficacy challenge emerged through the formalization of translational physiology, defined as "the examination of biological functions across levels spanning from molecules to cells to organs to populations" [1]. This discipline provided the conceptual framework for integrating knowledge across biological scales, fundamentally shifting how researchers approached the efficacy gap.
A critical institutional development in this transition was the establishment of the Translational Physiology Interest Group within the American Physiological Society in 2010, signaling formal recognition of this emerging discipline [1]. This organizational endorsement reflected a growing consensus that understanding physiological integration across multiple levels was essential for predicting clinical efficacy.
The Clinical Biology Department: An Organizational Innovation
The strategic organizational response to the efficacy challenge materialized in 1984 with the creation of the Clinical Biology department at Ciba (now Novartis) [1]. This innovative structure was specifically designed to bridge the critical gap between preclinical findings and clinical outcomes by fostering direct collaboration between preclinical physiologists, pharmacologists, and clinical pharmacologists.
The Clinical Biology team was tasked with identifying human disease models and biomarkers that could demonstrate drug effects before progressing to costly Phase IIb and III trials [1]. This approach encompassed Phases I and IIa of clinical development, focusing on establishing proof-of-concept in select disease subsets through:
- Identification of appropriate biomarkers of target engagement
- Development of human disease models with clinically monitorable symptoms
- Demonstration of relationship between biomarker modulation and clinical symptoms
The Four-Step Framework for Clinical Benefit Assessment
The Clinical Biology department implemented a systematic four-step framework, adapted from Koch's postulates, to evaluate potential clinical benefit of new therapeutic agents [1]:
- Identification of a specific disease parameter (biomarker)
- Demonstration that the drug modifies this parameter in animal models
- Verification that the drug modifies the parameter in human disease models
- Correlation of dose-dependent clinical benefit with biomarker changes
This framework's utility was demonstrated through its application to CGS 13080, a thromboxane synthase inhibitor. The approach revealed critical limitations in the compound's pharmacokinetic profile—specifically a short 73-minute half-life and lack of feasible oral formulation—leading to early termination of development before substantial resources were expended on later-phase trials [1]. This case exemplified how the Clinical Biology model could efficiently identify fundamental efficacy barriers.
Table 1: Evolution of Key Organizational Structures in Pharmaceutical R&D
| Time Period | Dominant Model | Primary Focus | Key Limitations |
|---|---|---|---|
| Pre-1980s | Separate Chemistry & Pharmacology | Compound screening; Animal models | Limited clinical translation; Trial-and-error approach |
| 1984 onward | Clinical Biology Department | Biomarker identification; Human disease models | Early-phase focus; Limited impact on late-stage development |
| 2000 onward | Chemical Biology Platform | Target validation; Systems biology | Integration complexity; Data interpretation challenges |
The Chemical Biology Platform: An Integrative Framework
Conceptual Foundation and Definition
The formalization of the chemical biology platform around the year 2000 represented the maturation of translational approaches into a comprehensive organizational framework [1]. Chemical biology is defined as "the study and modulation of biological systems, and the creation of biological response profiles through the use of small molecules" selected or designed based on knowledge of biological target structure, function, or physiology [1].
This platform emerged synergistically with several technological advancements, including:
- Completion of the Human Genome Project and expansion of genomic information
- Advances in combinatorial chemistry for compound library generation
- Improvements in structural biology methods, particularly for membrane-bound receptors
- Sophisticated cellular assays with genetic manipulation capabilities
Strategic Implementation and Target Focus
The chemical biology platform fundamentally shifted screening strategies from indiscriminate testing to targeted selection based on biological understanding. By 2000, the pharmaceutical industry was focusing on approximately 500 targets across key protein families [1]:
- G-protein coupled receptors (45%)
- Enzymes (25%)
- Ion channels (15%)
- Nuclear receptors (~2%)
This target distribution reflected a prioritization of target classes with established druggability and physiological significance, enabling more efficient resource allocation.
Enabling Technologies and Methodologies
The chemical biology platform incorporated advanced experimental systems that provided multidimensional data on compound activity [1]:
- High-content multiparametric analysis using automated microscopy and image analysis to quantify cell viability, apoptosis, cell cycle analysis, protein translocation, and phenotypic profiling
- Reporter gene assays for assessing signal activation in response to ligand-receptor engagement
- Ion channel activity assessment using voltage-sensitive dyes or patch-clamp techniques for neurological and cardiovascular targets
These technologies enabled the generation of biological response profiles that contextualized compound activity within broader physiological systems rather than isolated molecular targets.
Modern Research Methodologies and Experimental Protocols
Biomarker Validation Framework
The historical emphasis on biomarker development established through the Clinical Biology model has evolved into sophisticated validation protocols. The contemporary biomarker validation workflow integrates computational and experimental approaches:
Diagram 1: Biomarker validation workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
Modern chemical biology research relies on integrated technology platforms and reagent systems that enable comprehensive compound profiling:
Table 2: Essential Research Reagent Solutions for Chemical Biology
| Reagent/Platform Category | Specific Examples | Research Application |
|---|---|---|
| Multi-omics Analysis Platforms | Proteomics, Metabolomics, Transcriptomics | Understanding protein network interactions and systems biology [1] |
| Advanced Cellular Assay Systems | High-content multiparametric analysis, Reporter gene assays, Patch-clamp techniques | Quantifying cell viability, apoptosis, protein translocation, signal activation [1] |
| Specialized Compound Libraries | DNA-encoded libraries, Diversity-oriented synthesis | Expanding chemical space exploration for bioactive compounds [4] [5] |
| Bioorthogonal Chemistry Reagents | Tetrazine ligations, Strained alkynes, Light-activated systems | Selective molecular tagging in biological systems for imaging and drug delivery [4] |
| Computational Chemistry Databases | QDπ dataset, Machine Learning Potentials (MLPs) | Training universal MLP models for molecular simulations in drug discovery [6] |
AI-Enhanced Methodologies for Predictive Compound Profiling
Contemporary chemical biology increasingly incorporates artificial intelligence and machine learning to accelerate compound optimization:
Diagram 2: AI-enhanced compound profiling
The QDπ dataset exemplifies modern data resources, incorporating 1.6 million molecular structures with energies and forces calculated at the ωB97M-D3(BJ)/def2-TZVPPD theory level to enable accurate machine learning potential development [6]. This dataset employs active learning strategies to maximize chemical diversity while minimizing computational expense through query-by-committee approaches that identify structures introducing significant new information [6].
Quantitative Impact Assessment
Historical Efficiency Metrics
The transition to chemical biology platforms has generated measurable impacts on pharmaceutical R&D efficiency. Analysis of development timelines reveals significant acceleration in specific therapeutic areas:
Table 3: Drug Development Timeline Acceleration Across Therapeutic Areas
| Therapeutic Area | Traditional Timeline (Years) | Accelerated Timeline (Years) | Key Accelerating Technologies |
|---|---|---|---|
| Oncology | 7-10 | 2-3 | AI-powered modeling, Adaptive trial designs, Platform-based clinical operations [7] |
| Infectious Disease | 7-10 | <1 (COVID-19 vaccines) | Real-time data sharing, Rolling regulatory reviews [7] |
| Rare Diseases | 7-10 | 3-5 | High-throughput omics strategies, Patient-derived organoids [8] [7] |
The economic implications of these accelerated timelines are substantial, with median R&D costs for novel drugs approximating $150 million, though complex therapeutics can exceed $1.3 billion [7]. The orphan drug market, a key focus of targeted therapeutic development, is projected to surpass $394.7 billion by 2030, reflecting the economic viability of the precision medicine model [7].
Success Metrics in Contemporary Drug Discovery
Analysis of screening efficiency demonstrates the impact of integrated chemical biology approaches. Research comparing virtual screening libraries of 99 million versus 1.7 billion molecules revealed that the larger library produced improved hit rates, enhanced compound potency, and an increased number of scaffolds [5]. This scaling effect underscores the value of comprehensive chemical space exploration enabled by modern computational infrastructure.
The integration of New Approach Methodologies (NAMs) further enhances predictive capability. These include:
- Organ-on-a-chip systems that provide human-specific biology inaccessible through animal models
- AI and machine learning models that predict safety, immunogenicity, and pharmacokinetics
- 3D organoid models for oncology preclinical screening [8]
These platforms address fundamental limitations of traditional animal models, particularly concerning the genetic homogeneity of laboratory animals versus human population diversity [8].
Future Directions and Emerging Opportunities
Technology Convergence Trends
The continued evolution of chemical biology platforms reflects increasing integration of complementary technologies:
- Bioorthogonal chemistry advances enabling selective reactions in living systems for in vivo imaging and drug delivery [4]
- Chemoenzymatic strategies combining enzymatic and chemical steps for complex molecule synthesis [4]
- Foundation models trained on massive biological datasets to uncover fundamental biological principles [9]
- AI agents that automate bioinformatics tasks and lower barriers to advanced data analysis [9]
Addressing Persistent Challenges
Despite significant advances, chemical biology continues to confront methodological challenges:
- Limited enzyme catalysis scope for novel non-natural transformations [4]
- Bioorthogonal translation hurdles from model systems to human clinical applications [4]
- NAM validation requirements for regulatory acceptance [8]
- Systemic complexity in replicating multi-organ interactions [8]
The historical pivot from efficacy challenge to integrated R&D model established a foundation for addressing these challenges through multidisciplinary collaboration and technological innovation. As the field progresses, the continued refinement of this framework promises to further enhance the efficiency and success of therapeutic development.
The historical pivot from traditional drug development to integrated chemical biology platforms represents a foundational transformation in pharmaceutical R&D. Triggered by the critical challenge of demonstrating clinical efficacy for mechanism-based compounds, this shift established translational physiology as the conceptual core bridging basic research and clinical application. The organizational innovation of Clinical Biology departments in the 1980s provided the initial structural framework, which evolved into comprehensive chemical biology platforms incorporating systems biology, biomarker validation, and multidisciplinary team science.
For contemporary researchers and drug development professionals, understanding this historical transition provides critical insights for designing experimental studies that effectively navigate the complex pathway from molecular discovery to clinical implementation. The continued integration of emerging technologies—including AI-driven discovery, organ-on-a-chip systems, and bioorthogonal chemistry—within this established conceptual framework promises to further enhance the efficiency and success of therapeutic development in the precision medicine era.
The convergence of translational physiology and systems biology represents a paradigm shift in modern drug discovery and development. This integration, often orchestrated within a chemical biology platform, provides a powerful, holistic framework for understanding disease mechanisms and predicting clinical outcomes. By bridging the gap between molecular insights and whole-organism physiology, this synergy enables a more mechanistic approach to therapeutic development. This whitepaper explores the core conceptual, methodological, and computational pillars of this integration, providing technical guidance and protocols for its implementation. The discussion is framed within the context of advancing precision medicine, highlighting how these disciplines collectively enhance target validation, candidate selection, and the overall efficacy and safety of biopharmaceuticals.
The contemporary pharmaceutical research landscape has evolved from traditional, empirical methods to a more predictive, mechanism-based approach. Central to this evolution is the chemical biology platform, an organizational strategy that optimizes drug target identification and validation by emphasizing a deep understanding of underlying biological processes [1]. This platform achieves its goals through the strategic integration of two powerful disciplines:
- Translational Physiology: Defined as the examination of biological functions across multiple levels of organization, from molecules and cells to organs and populations [1]. It provides the essential biological context for understanding function in a living system.
- Systems Biology: A holistic, interdisciplinary approach that combines experimental and computational strategies to integrate information from different biological scales to unravel pathophysiological mechanisms [10]. It leverages high-throughput technologies to generate massive multi-omics datasets (genomics, transcriptomics, proteomics, metabolomics).
Individually, each field offers valuable insights; however, their integration creates a synergistic effect that is transformative. Translational physiology ensures that molecular discoveries are grounded in biological reality and clinical relevance, while systems biology provides the comprehensive, data-rich maps of biological networks and interactions. Together, they form the core of a robust framework for identifying and validating therapeutic targets, understanding drug actions and toxicities, and ultimately, delivering more effective and precise medicines to patients [1] [11].
Pillar 1: Foundational Concepts and Workflow Integration
The first pillar involves the strategic merging of the fundamental principles and workflows of translational physiology and systems biology into a cohesive, iterative process for drug discovery.
The Role of the Chemical Biology Platform
The chemical biology platform acts as the organizing principle that connects a series of strategic steps to determine whether a newly developed compound will translate into clinical benefit [1]. Unlike traditional trial-and-error methods, it leverages systems biology techniques—such as proteomics, metabolomics, and transcriptomics—to prioritize targeted selection [1] [12]. This platform is inherently multidisciplinary, relying on parallel processes to accelerate timelines and reduce the costs of bringing new drugs to patients [1].
A historical precedent for this integration was the establishment of Clinical Biology departments in the 1980s, which were early organized efforts to bridge preclinical and clinical research [1]. This approach was formalized using a four-step process, analogous to Koch's postulates, to gauge clinical benefit:
- Identify a disease parameter (biomarker).
- Show that the drug modifies that parameter in an animal model.
- Show that the drug modifies the parameter in a human disease model.
- Demonstrate a dose-dependent clinical benefit that correlates with a similar change in the direction of the biomarker [1].
This logical, step-wise approach, which seamlessly connects molecular data (biomarkers) with physiological and clinical outcomes, is the direct precursor to modern integrated workflows.
The Integrated Workflow
The following diagram illustrates the modern, iterative workflow for drug discovery that integrates systems biology and translational physiology, guided by the chemical biology platform.
Pillar 2: Methodological and Technical Approaches
The second pillar encompasses the specific experimental and analytical methodologies that enable the practical integration of systems biology and translational physiology.
Multi-omics Integration Strategies
Systems biology provides a suite of high-throughput technologies for generating multi-omics data. The integration of these datasets is crucial for gaining a holistic view of biological systems and disease pathologies [10]. The predominant data-driven integration strategies can be categorized as follows:
Table 1: Data-Driven Multi-Omics Integration Approaches
| Category | Description | Common Tools & Methods | Primary Application |
|---|---|---|---|
| Statistical & Correlation-Based | Quantifies the degree and significance of relationships between variables across omics datasets. | Pearson’s/Spearman’s correlation, RV coefficient, Procrustes analysis [10]. | Identifying coordinated changes (e.g., transcript-to-protein correlations), assessing dataset similarity. |
| Multivariate Methods | Reduces data dimensionality and identifies latent structures that explain variance across multiple omics datasets. | Partial Least Squares (PLS), Principal Component Analysis (PCA) [10]. | Identifying combined molecular patterns that differentiate patient groups or phenotypes. |
| Network Analysis | Transforms pairwise associations into graphical models to identify highly interconnected functional modules. | Weighted Gene Correlation Network Analysis (WGCNA), xMWAS [10]. | Discovering clusters of co-expressed genes/proteins/metabolites and linking modules to clinical traits. |
| Machine Learning (ML) & Artificial Intelligence (AI) | Uses algorithms to learn complex, non-linear patterns from integrated omics data for prediction and classification. | Classification models, regression models, feature selection algorithms [10]. | Identifying complex biomarker signatures, predicting patient response, classifying disease subtypes. |
A 2025 review of 64 research papers indicated that statistical and correlation-based approaches were the most prevalent, followed by multivariate methods and ML/AI techniques [10]. The choice of method depends on the specific biological question, data quality, and the desired outcome (e.g., biomarker discovery vs. pathway elucidation).
Experimental Protocols for Integrated Workflows
The following is a generalized protocol for a typical integrated study, such as investigating a disease mechanism or drug response.
Protocol: An Integrated Multi-Omics and Physiological Workflow
Sample Collection and Preparation:
- Collect relevant biological samples (e.g., tissue, blood, primary cells) from well-characterized in vivo models (e.g., spontaneously hypertensive rat [1]) or human cohorts. Patient samples should be stratified and well-annotated [13].
- Divide samples for subsequent multi-omics analyses and functional/physiological assays.
Multi-Omics Profiling:
- Perform genomic, transcriptomic, proteomic, and metabolomic profiling on the same sample set using appropriate high-throughput platforms (e.g., NGS for genomics/transcriptomics, LC-MS for proteomics/metabolomics).
- Key Consideration: Ensure data quality control, including handling missing values, normalization, and batch effect correction [10].
Functional Phenotypic Assessment:
- In parallel, conduct physiological or phenotypic assays relevant to the disease or drug target. This leverages translational physiology tools.
- Examples include high-content multiparametric analysis of cellular events (cell viability, apoptosis, protein translocation [1]), reporter gene assays, ion channel activity measurements using patch-clamp techniques [1], and using automated platforms for standardized 3D cell culture to improve reproducibility [14].
Data Integration and Analysis:
- Apply one or more integration strategies from Table 1 (e.g., WGCNA, xMWAS, ML) to the multi-omics data.
- The goal is to identify molecular networks, key drivers, and biomarker candidates associated with the physiological or phenotypic changes observed in Step 3.
Model Validation and Iteration:
- Validate key findings using orthogonal methods (e.g., qPCR, immunoblotting) in an independent sample set.
- Use genetic (e.g., CRISPR) or pharmacological interventions in relevant in vitro or in vivo models to perturb identified targets and confirm their functional role in the phenotype. This closes the loop between systems-level observation and physiological causation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Integrated Studies
| Item | Function in Integrated Workflows |
|---|---|
| Well-Annotated Patient Biospecimens | Provides clinically relevant biological material for omics profiling and model development. Essential for ensuring translational relevance [13]. |
| Human-Relevant Cell Models (e.g., 3D Organoids) | Offers a more physiologically accurate in vitro system for high-content screening and toxicity assessment, reducing reliance on animal models [14]. |
| DNA-Encoded Libraries (DELs) | Large collections of small molecules used for high-throughput screening against protein targets to identify potential drug leads [15]. |
| Antibodies for Immunoblotting | Enables relative quantitation of protein abundance for target validation and confirmation of omics findings [1]. |
| Reporter Gene Assay Kits | Used to assess signal activation in response to ligand-receptor engagement, linking molecular events to cellular responses [1]. |
| Voltage-Sensitive Dyes / Patch-Clamp Equipment | Critical for functional screening of neurological and cardiovascular drug targets, connecting molecular target engagement to cellular physiology [1]. |
| Automated Liquid Handlers (e.g., Tecan Veya) | Ensures consistency, reproducibility, and throughput in sample preparation and assay execution, reducing human variation [14]. |
Pillar 3: Computational Modeling and Data Analysis
The third pillar involves the computational infrastructure and modeling approaches required to synthesize data from systems biology and translational physiology into actionable, predictive insights.
The Role of AI, Machine Learning, and Data Management
The volume and complexity of data generated by integrated workflows necessitate robust computational strategies.
- Artificial Intelligence and Machine Learning: AI/ML is increasingly used to uncover complex, non-linear patterns from integrated omics and physiological data. Applications include de novo design of novel chemical compounds [15], identification of biomarker signatures from imaging and multi-omics data [14], and prediction of patient responses. A critical success factor is grounding AI in biological reality through close collaboration with experimentalists to prevent model "hallucination" [15].
- Quantitative Systems Pharmacology (QSP): QSP is a modeling discipline that leverages systems biology to simulate drug behaviors, predict patient responses, and optimize drug development strategies [11]. QSP models integrate knowledge of biological pathways, drug properties, and disease mechanisms to create virtual patient populations, enabling more informed decisions in clinical trial design.
- Data Traceability and Management: The effectiveness of AI and QSP is contingent on data quality and metadata completeness. There is a growing industry focus on capturing every condition and state of an experiment to provide quality data for models to learn from [14]. This requires software platforms that connect data, instruments, and processes to break down data silos [14].
Pathway and Workflow Visualization
The following diagram maps the logical flow of data and knowledge from initial multi-omics data generation to final clinical application, highlighting the computational integration points.
Current Applications and Future Outlook
The integration of translational physiology and systems biology is already driving innovation across the drug development spectrum.
- Precision Medicine: The integrated approach is fundamental to precision medicine. By understanding disease subtypes through multi-omics and linking them to clinical outcomes via translational physiology, therapies can be targeted to specific patient populations [1] [11].
- Biomarker Discovery: The combined power of multi-omics integration and physiological validation accelerates the identification of robust diagnostic, prognostic, and predictive biomarkers [10]. For example, foundation models applied to histopathology and multiplex imaging data are being used to identify new biomarkers and link them to clinical outcomes [14].
- Educational Evolution: To sustain this progress, cultivating a skilled workforce is essential. Successful industry-academia partnerships are crucial for developing MSc and PhD programs that equip the next generation of scientists with the necessary blend of biological, computational, and mathematical skills [11]. Examples include specialized programs at the University of Manchester, Imperial College, and the University of Delaware [11].
The future of this integrated field will be characterized by a tighter feedback loop between computational prediction and experimental validation, increased use of human-relevant models like automated 3D organoids [14], and the continued maturation of AI as a grounded, practical tool for accelerating the journey from bench to bedside.
The evolution of drug discovery from a discipline rooted in clinical biology to one powered by the genomic revolution represents a fundamental paradigm shift in biomedical science. This transition has been orchestrated within the context of the chemical biology platform, an organizational approach designed to optimize drug target identification and validation while improving the safety and efficacy of biopharmaceuticals [1]. This platform achieves its goals through a multidisciplinary emphasis on understanding underlying biological processes and leveraging knowledge gained from the action of similar molecules on these systems [1]. The integration of translational physiology—which examines biological functions across multiple levels from molecules to populations—has been deeply influenced by this evolution, creating a robust framework for modern therapeutic development [1]. This whitepaper traces the critical milestones in this journey, providing technical guidance for researchers navigating the contemporary drug discovery landscape.
The Foundation: Clinical Biology and Early Translational Models
The Emergence of Clinical Biology
The period from the 1950s to the 1980s witnessed the emergence of clinical biology as a response to regulatory changes and the limitations of traditional drug development approaches. The Kefauver-Harris Amendment of 1962 mandated proof of efficacy from well-controlled clinical trials, fundamentally changing pharmaceutical development strategies [1]. This regulatory shift necessitated more sophisticated approaches to bridge preclinical findings and clinical outcomes, leading to the establishment of Clinical Biology departments within pharmaceutical companies by the mid-1980s [1].
The clinical biology approach introduced a systematic framework for evaluating potential therapeutic agents, embodied in a four-step process adapted from Koch's postulates:
- Identification of a disease parameter (biomarker)
- Demonstration that the drug modifies that parameter in an animal model
- Verification that the drug modifies the parameter in a human disease model
- Confirmation of a dose-dependent clinical benefit that correlates with similar changes in the biomarker direction [1]
This methodology represented an early form of translational physiology, focusing on identifying human disease models and biomarkers that could more easily demonstrate drug effects before progressing to costly Phase IIb and III trials [1].
Pioneering Animal Models in Drug Development
The development of standardized animal models provided critical tools for evaluating therapeutic efficacy and safety. Key milestones in model development include:
Table: Historic Breakthroughs in Research Animal Models
| Year | Model | Significance | Application in Drug Discovery |
|---|---|---|---|
| 1906 | Wistar Rat [16] | First pure strain animal model for medical research | Standardized therapeutic testing |
| 1962 | Nude Mouse [16] | Major model for cancer progression and therapeutic intervention | Oncology drug development |
| 1974 | First transgenic mouse (SV40 DNA) [16] | First successful transfer of foreign DNA into a drug discovery animal model | Proof of concept for genetic manipulation |
| 1989 | First knockout mouse [16] | Technology for suppressing normal gene function to study gene function and disease | Functional genomics and target validation |
These models enabled researchers to replicate human diseases in systems that possessed biomarkers of interest, exhibited clinically monitorable symptoms, and demonstrated relationships between biomarker concentration and clinical conditions [1]. The spontaneously hypertensive rat for evaluating blood pressure control compounds and the rat tail-flick test for assessing pain reduction compounds represent classic examples of physiological screening systems that synergized with emerging mechanism-based approaches [1].
The Molecular Biology Revolution: Tools for Targeted Discovery
Key Technological Developments
The 1970s-1990s witnessed transformative advances in molecular biology that enabled precise targeting of DNA, RNA, and proteins involved in disease processes. Critical methodologies emerged during this period that became fundamental to modern drug discovery:
- Immunoblotting (late 1970s-early 1980s): Enabled relative quantitation of protein abundance, facilitating target validation [1]
- Monoclonal Antibody Technology (1975): Developed by Köhler and Milstein, enabling production of identical antibodies recognizing a single antigen, revolutionizing diagnostics and targeted therapies [17]
- Recombinant DNA Technology (1973): Pioneered by Cohen and Boyer, allowing DNA from different species to be combined and replicated in bacteria, launching the biotechnology industry [17]
- Polymerase Chain Reaction (1983): Developed by Kary Mullis, enabling exponential amplification of specific DNA sequences, transforming molecular analysis [16]
- DNA Sequencing (1977): Sanger's chain termination method enabled deciphering of genetic sequences, beginning with the bacteriophage Phi X 174 genome [17]
The Rise of High-Throughput Screening
By the 1990s, pharmaceutical research had shifted from traditional trial-and-error approaches to targeted selection strategies. The industry began focusing on specific target classes, with G-protein coupled receptors (45%), enzymes (25%), ion channels (15%), and nuclear receptors (~2%) comprising the majority of drug targets in the year 2000 [1]. This target-focused approach synergized with gains in high-throughput screening and combinatorial chemistry, enabled by several critical cellular assays:
- High-content multiparametric analysis using automated microscopy and image analysis to quantify cell viability, apoptosis, cell cycle analysis, protein translocation, and phenotypic profiling [1]
- Reporter gene assays to assess signal activation in response to ligand-receptor engagement [1]
- Ion channel activity screening using voltage-sensitive dyes or patch-clamp techniques for neurological and cardiovascular drug targets [1]
The Genomic Revolution: Decoding the Blueprint of Life
Foundational Milestones in Genomics
The genomic revolution represents one of the most significant transformations in biomedical science, originating from foundational discoveries and culminating in comprehensive mapping of human genetics.
Table: Key Milestones Powering the Genome Sequencing Revolution
| Era | Breakthrough | Key Scientists/Projects | Impact on Drug Discovery |
|---|---|---|---|
| 1953 | Discovery of DNA double helix structure [18] | Watson, Crick, Franklin, Wilkins | Revealed molecular basis of heredity |
| 1977 | First genome sequenced (bacteriophage ΦX174) [18] | Frederick Sanger | Established methodology for genome sequencing |
| 1980s-1990s | Next-generation sequencing [18] | Various institutions | Enabled faster, cheaper genome data production |
| 2003 | Human Genome Project completion [19] | International consortium | Mapped entire human genetic code for target identification |
Technological Advances in Sequencing
The evolution of sequencing technologies dramatically reduced the cost and time required for genomic analysis, making large-scale projects feasible:
- Sanger Sequencing (1977): The first generation of DNA sequencing technology, requiring significant time and resources [18]
- Next-Generation Sequencing (2000s): Automated sequencing performing many reactions simultaneously, offering "ultra-high throughput, scalability and speed" [18]
- Nanopore Sequencing (2010s): Enabled real-time analysis of long DNA or RNA fragments by monitoring electrical current changes as molecules pass through protein pores [18]
- Portable Sequencing (2010s): Miniaturized devices like the MinION sequencer allowed "point-of-care testing" at patient bedsides rather than central laboratories [18]
These technological advances facilitated the transition from reading genomes to writing and editing them, with CRISPR and synthetic biology enabling precise genetic modifications that were previously unimaginable [17].
The Chemical Biology Platform: Integrating Disciplines for Translational Success
Conceptual Framework and Implementation
The chemical biology platform emerged in approximately 2000 as an organizational response to leverage genomic information, combinatorial chemistry, improvements in structural biology, high-throughput screening, and genetically manipulable cellular assays [1]. This platform connects a series of strategic steps to determine whether newly developed compounds could translate into clinical benefit using translational physiology [1].
Chemical biology is defined as "the study and modulation of biological systems, and the creation of biological response profiles through the use of small molecules that are often selected or designed based on current knowledge of the structure, function, or physiology of biological targets" [1]. Unlike traditional approaches that relied on trial-and-error, even when using high-throughput technologies, chemical biology focuses on selecting target families and incorporates systems biology approaches—including transcriptomics, proteomics, metabolomics, and network analyses—to understand how protein networks integrate [1].
The platform's main advantage lies in its use of multidisciplinary teams to accumulate knowledge and solve problems, often relying on parallel processes to accelerate timelines and reduce costs for bringing new drugs to patients [1]. This approach represents a mechanism-based means to advance clinical medicine that persists in both academic and industry-focused research [1].
The Chemical Biology-Medicinal Chemistry Continuum
The integration of chemical biology with medicinal chemistry has created a powerful continuum for drug discovery [20]. Chemical biology, "sitting at the interface of many disciplines," has emerged as a major contributor to understanding biological systems and has become an integral part of drug discovery [20]. The blurring of boundaries between disciplines has created new opportunities to probe and understand biology, with both fields playing key roles in driving innovation toward transformative medicines [20].
This continuum leverages the design and synthesis of novel compounds from medicinal chemistry with the biological systems expertise of chemical biology, creating a synergistic relationship that enhances target identification, validation, and therapeutic development.
Modern Experimental Approaches and Protocols
Contemporary Translational Research Workflows
Modern translational research integrates multiple approaches to bridge basic discoveries with clinical applications, exemplified by several contemporary research programs:
Digestive Physiology Research Protocol
Mark Donowitz's research on diarrheal diseases demonstrates a progressive translational workflow:
- Initial Clinical Observation: Sodium absorption identified as critical in gut function [21]
- Animal Model Studies: Investigation using mouse and rabbit models [21]
- Cellular Studies: Transition to cell-based systems [21]
- Human Organoid Systems: Application of human intestinal cell culture models to understand pathophysiology and potential treatments [21]
- Therapeutic Development: Generation of two promising therapies—a drug entering human trials and a peptide to enhance sodium absorption [21]
Comparative Physiology Research Protocol
Lara do Amaral-Silva's approach to studying stress tolerance adaptations:
- Identification of Animal Adaptations: Focus on species with unique abilities to overcome stressors that cause human health issues (e.g., bullfrogs, birds, Tegu lizards tolerating prolonged hypoxia) [21]
- Mechanistic Studies: Investigation of physiological mechanisms (e.g., NMDA receptors in maintaining brain health during hypoxia) [21]
- Comparative Analysis: Examination of physiologically comparable traits (e.g., birds with high glucose and insulin resistance resembling human type 2 diabetes) [21]
- Therapeutic Insight Translation: Application of mechanistic understanding to human treatment approaches [21]
Advanced Methodologies in Modern Drug Discovery
Artificial Intelligence-Accelerated Virtual Screening
Recent advances in computational approaches have revolutionized early drug discovery:
- Platform Architecture: Development of open-source artificial intelligence-accelerated virtual screening platforms integrating active learning techniques for efficient compound triage [22]
- Screening Scale: Capability to screen multi-billion compound libraries against unrelated targets (e.g., ubiquitin ligase KLHDC2 and human voltage-gated sodium channel NaV1.7) [22]
- Performance Metrics: High hit rates (14% for KLHDC2, 44% for NaV1.7) with single-digit micromolar binding affinities [22]
- Time Efficiency: Screening completion in less than seven days using high-performance computing clusters [22]
- Validation: Experimental confirmation via high-resolution X-ray crystallography validating predicted docking poses [22]
Functional Genomics and Spatial Transcriptomics
Contemporary approaches leverage genomic technologies for enhanced target identification:
- Functional Genomics: Examination of how differences in genomes influence disease, providing crucial information for developing new diagnosis methods and therapies [18]
- Spatial Transcriptomics: Development of high-resolution ex vivo drug discovery platforms using precision-cut tissue samples (e.g., lung samples from healthy and idiopathic pulmonary fibrosis patients) to build reliable, predictive models for drug development [23]
- Remote Sampling Protocols: Creation of home-based collection methods with RNA preservation reagents (e.g., for human milk) to enable large-scale transcriptome studies without immediate ultra-cold storage requirements [23]
Research Reagent Solutions for Translational Studies
Table: Essential Research Reagents and Their Applications
| Reagent/Technology | Function | Application Example |
|---|---|---|
| Human Organoids [21] | Cell culture models from normal human tissues | Study digestive physiology and pathophysiology |
| Reporter Gene Assays [1] | Assess signal activation from ligand-receptor engagement | Screen potential therapeutic compounds |
| Voltage-Sensitive Dyes [1] | Measure ion channel activity | Neurological and cardiovascular drug target screening |
| Monoclonal Antibodies [16] | Recognize single antigens with high specificity | Diagnostics, research, and targeted cancer therapies |
| RNA Preservation Reagents [23] | Stabilize RNA in remote collection protocols | Large-scale transcriptome sequencing studies |
| Precision-Cut Tissue Slices [23] | Ex vivo modeling of disease states | Drug testing in living human tissue samples (e.g., IPF) |
| Knockout Mouse Models [16] | Study gene function and disease progression | Target validation and disease mechanism studies |
The journey from clinical biology to the genomic revolution represents a fundamental transformation in how researchers approach therapeutic development. The integration of chemical biology platforms with translational physiology has created a robust framework for modern drug discovery, enabling more efficient target identification, validation, and clinical translation [1]. This convergence of disciplines—spanning molecular biology, genomics, computational science, and systems biology—has accelerated the pace of therapeutic innovation while addressing the challenges of demonstrating clinical benefit [1].
The continued evolution of these approaches, particularly through artificial intelligence-accelerated screening [22], functional genomics [18], and sophisticated model systems [21] [23], promises to further enhance our ability to translate basic biological insights into transformative medicines. For researchers and drug development professionals, understanding this historical trajectory and the current technological landscape is essential for navigating the future of therapeutic innovation and addressing the complex health challenges of tomorrow.
The central dogma of molecular biology, first articulated by Francis Crick in 1958, establishes the fundamental framework for information flow in biological systems. In its original form, it posits that sequential information can be transferred from nucleic acid to nucleic acid, or from nucleic acid to protein, but once information has passed into protein, it cannot flow back to nucleic acid [24]. This principle governs the core operations of molecular biology: DNA replication, transcription of DNA to RNA, and translation of RNA into protein. While often simplified to "DNA makes RNA, and RNA makes protein," Crick's original formulation specifically emphasized the unidirectional nature of information transfer from nucleic acids to proteins [24].
For chemical biologists and drug discovery scientists, this framework provides the essential molecular context for understanding how genetic information manifests as physiological function and dysfunction. The field of chemical biology operates precisely at this interface, using small molecules and chemical tools to study and modulate biological systems [1]. By understanding the detailed mechanisms governing information flow, researchers can design targeted interventions that correct pathological information transfer errors responsible for disease states. This mechanistic understanding forms the foundation of modern drug development, particularly in the era of precision medicine, where therapies are designed to target specific molecular pathways in defined patient populations [1].
Recent research has continued to refine our understanding of the central dogma, revealing unexpected complexities in how genetic information flows through biological systems. For instance, the discovery of DNA polymerase θ (Polθ) in human cells, which possesses robust reverse transcriptase activity, demonstrates that RNA-templated DNA repair occurs in mammalian systems, expanding the traditional boundaries of information flow [25]. Similarly, work on group II self-splicing introns by Dr. Anna Pyle's laboratory has illuminated the three-dimensional molecular architecture and catalytic mechanisms that enable these "genetic parasites" to excise themselves from RNA transcripts without protein assistance [26]. These advances not only deepen our fundamental knowledge but also create new opportunities for therapeutic intervention through chemical biology approaches.
The Molecular Machinery of Information Flow: Key Processes and Experimental Methodologies
DNA Replication and Transcription
DNA replication represents the fundamental process of duplicating genetic information to provide for the progeny of any cell. This process is executed by a complex group of proteins called the replisome, which performs the replication of information from the parent strand to the complementary daughter strand [24]. The fidelity of this process is essential for maintaining genetic integrity across cell generations.
Transcription entails the transfer of information from DNA to RNA, wherein a section of DNA serves as a template for assembling a new piece of messenger RNA (mRNA). This process requires sophisticated molecular machinery, including RNA polymerase and transcription factors [24]. In eukaryotic cells, the initial product is pre-mRNA, which must undergo processing—including addition of a 5' cap, poly-A tail, and splicing—to become mature mRNA. Alternative splicing mechanisms significantly expand the diversity of proteins that can be produced from a single mRNA molecule, adding a layer of complexity to information flow [24].
Table 1: Key Experimental Techniques for Studying DNA Replication and Transcription
| Technique | Application | Key Insights Provided |
|---|---|---|
| X-ray Crystallography | Determining 3D structure of replication/transcription complexes | Reveals atomic-level architecture of polymerases, transcription factors, and nucleic acid complexes [26] |
| Photo-cross-linking | Mapping molecular interactions in transcription complexes | Identifies interaction networks between distant domains in RNA structures [26] |
| Nucleotide Analog Interference Mapping/Suppression (NAIM/NAIS) | Identifying functionally critical atoms in RNA | Maps atoms essential for splicing and catalytic activity in self-splicing introns [26] |
| Reporter Gene Assays | Assessing signal activation in response to ligand-receptor engagement | Measures transcriptional activity and signal transduction pathways in live cells [1] |
Translation and Protein Synthesis
Translation represents the final step of information transfer from nucleic acid to protein, wherein the genetic code is converted into functional polypeptides. The ribosome reads mRNA triplet codons, typically beginning with an AUG initiator methionine codon. Initiation and elongation factors facilitate the bringing of aminoacylated transfer RNAs (tRNAs) into the ribosome-mRNA complex, matching the codon in the mRNA to the anti-codon on the tRNA [24]. Each tRNA carries the appropriate amino acid residue to add to the growing polypeptide chain.
The complexity of protein formation extends far beyond the simple translation of nucleotide sequences. As amino acids incorporate into the growing peptide chain, the chain begins folding into its correct three-dimensional conformation—a process critical for biological function. Translation terminates at stop codons (UAA, UGA, or UAG), after which the nascent polypeptide chain typically requires additional processing to achieve functional maturity [24]. This includes chaperone-assisted folding, excision of internal segments (inteins), cleavage into multiple sections, cross-linking, and attachment of cofactors such as haem (heme) [24].
Table 2: Advanced Methodologies for Studying and Engineering Translation
| Methodology | Principle | Research/Drug Discovery Application |
|---|---|---|
| Flexizyme System | Artificial ribozyme that charges tRNA with diverse amino/hydroxy acids | Genetic code reprogramming for incorporation of non-natural amino acids [26] |
| Backbone-Cyclized Peptide Synthesis | In vitro translation of linear precursors that self-arrange into cyclic structures | Production of peptides with enhanced rigidity, proteolytic stability, and membrane permeability [26] |
| High-Content Multiparametric Cellular Analysis | Automated microscopy and image analysis to quantify multiple cellular events | Assessment of cell viability, apoptosis, cell cycle, protein translocation, and phenotypic profiling [1] |
| Patch-Clamp Techniques & Voltage-Sensitive Dyes | Direct measurement of ion channel activity | Screening neurological and cardiovascular drug targets [1] |
Chemical Biology Approaches to Manipulate Information Flow
Expanding the Genetic Code
Chemical biology has developed sophisticated approaches to reprogram the central dogma for both basic research and therapeutic applications. Dr. Hiroaki Suga's work on genetic code reprogramming demonstrates how the standard translational machinery can be engineered to incorporate non-natural amino acids—structurally modified amino acids with novel physicochemical and biological properties [26]. This approach reassigns codons for natural amino acids to non-natural amino acids using a flexizyme-based in vitro translation system.
The experimental workflow for genetic code reprogramming involves several key steps. First, natural aminoacyl-tRNA synthetases (ARSs) are removed from a reconstituted, cell-free translation system derived from Escherichia coli, leaving their cognate tRNAs uncharged. These uncharged tRNAs, called vacant codons, are then reassigned to desired non-natural amino acids using the flexizyme ribozyme, which charges tRNA with amino or hydroxy acids esterified with a 3,5-dinitrobenzyle (DBE) group [26]. A notable advantage of this system is that the aminoacylation reaction is virtually independent of the amino acid side chain, allowing virtually any amino acid to be charged onto any desired tRNA.
To maximize the variety of incorporatable amino acids, researchers artificially divide the codon box by exploiting redundancy in the genetic code. For example, while the codons GUU, GUC, GUA, and GUG all normally encode valine, GUU and GUC can be reprogrammed for p-methoxyphenyllactic acid (mFlac), while GUA and GUG triplets remain assigned to valine [26]. This approach enables the ribosomal synthesis of diverse non-natural peptides and even polyesters, expanding the chemical space available for drug discovery and biomaterial development.
Diagram 1: Genetic code reprogramming workflow
Engineering Novel Protein Architectures
The ability to reprogram the genetic code enables the synthesis of proteins with novel architectures and enhanced therapeutic properties. One notable application is the synthesis of backbone-cyclized peptides, which demonstrate enhanced structural rigidity, proteolytic stability, and membrane permeability compared to their linear counterparts [26]. The experimental protocol involves designing a DNA template that encodes a linear precursor peptide composed of a cysteine-protein dipeptide sequence followed by a glycolic acid sequence (C-P-HOG). When this template is transcribed and translated in vitro, expression of the linear peptide bearing the C-P-HOG sequence results in spontaneous self-rearrangement into a C-terminal diketopiperadine-thioester, generating a cyclized peptide non-enzymatically.
Remarkably, this entire process—including transcription of the DNA template, translation of the peptide, and peptide cyclization—occurs in a single reaction tube, streamlining production [26]. This methodology has enabled the construction of comprehensive libraries of backbone-cyclized peptides for rapid screening of inhibitors against functionally important enzymes. Such approaches exemplify how chemical biology leverages understanding of the central dogma to create powerful platforms for drug discovery, particularly for targets that have proven difficult to address with conventional small molecules or biologics.
Physiological Context: Integrating Molecular Information into Biological Systems
From Molecular Information to Physiological Function
Physiology provides the essential biological context in which chemical tools and principles are applied to understand and influence living systems. The chemical biology platform recognizes that molecular-level information gains functional meaning only when integrated across multiple biological levels—from molecules to cells to organs to populations [1]. This integrative perspective forms the core of translational physiology, which examines biological functions across these multiple levels to bridge laboratory discoveries with clinical applications.
The critical importance of physiological context becomes evident when considering drug development failures. Many compounds that show potent activity against isolated molecular targets fail to demonstrate clinical benefit in patients because of the complex physiological environments in which they must operate [1]. The chemical biology platform addresses this challenge through a multidisciplinary approach that accumulates knowledge and solves problems using parallel processes to accelerate the translation of basic discoveries into clinical applications. This approach has evolved significantly since the 1960s, when the Kefauver-Harris Amendment mandated proof of efficacy from adequate and well-controlled clinical trials, fundamentally changing drug development paradigms [1].
Physiological Validation in Drug Discovery
The chemical biology platform incorporates physiological validation at multiple stages of drug development. Douglas's adaptation of Koch's postulates for drug development outlines a four-step framework for establishing clinical relevance: (1) identify a disease parameter (biomarker); (2) demonstrate that the drug modifies that parameter in an animal model; (3) show that the drug modifies the parameter in a human disease model; and (4) demonstrate dose-dependent clinical benefit that correlates with similar changes in the biomarker [1]. This systematic approach bridges the gap between preclinical findings and clinical outcomes, increasing the efficiency of decision-making before progressing to costly Phase IIb and III trials.
The emergence of Clinical Biology departments in pharmaceutical companies during the 1980s represented an early organized effort to focus on translational physiology [1]. These interdisciplinary teams brought together preclinical physiologists, pharmacologists, and clinical pharmacologists to identify human disease models and biomarkers that could more easily demonstrate drug effects before advancing to large-scale trials. Effective disease models must possess the biomarker of interest, have clinically monitorable symptoms, and demonstrate a relationship between biomarker concentration and clinical manifestations of the condition [1].
Diagram 2: Physiological validation framework in drug discovery
The Scientist's Toolkit: Essential Research Reagents and Platforms
The experimental approaches discussed require specialized research reagents and platform technologies. The following table details key solutions essential for investigating and manipulating the central dogma.
Table 3: Research Reagent Solutions for Central Dogma Investigation
| Research Reagent | Composition/Principle | Function in Experimental Workflow |
|---|---|---|
| Reconstituted Cell-Free Translation System | E. coli extract with removed aminoacyl-tRNA synthetases | Enables genetic code reprogramming by providing translational machinery without native charging activity [26] |
| Flexizyme Ribozyme | Artificial ribozyme that charges tRNA with diverse amino/hydroxy acids esterified with DBE group | Facilitates charging of tRNAs with non-natural amino acids independent of side chain type [26] |
| High-Throughput Screening Assays | Combinatorial chemistry libraries combined with automated cellular or biochemical assays | Enables rapid screening of compound libraries against therapeutic targets [1] |
| Multiparametric Cellular Analysis Systems | Automated microscopy combined with image analysis algorithms | Quantifies multiple cellular events (viability, apoptosis, protein translocation) in response to perturbations [1] |
| Group II Intron Ribozymes | Self-splicing ribozymes purified from organisms like Oceanobacillus iheyensis | Provides model system for studying RNA structure, catalysis, and potential gene therapy vectors [26] |
| Backbone-Cyclized Peptide Libraries | DNA templates encoding C-P-HOG sequences that cyclize post-translationally | Generates diverse peptide libraries with enhanced stability for inhibitor screening [26] |
The central dogma of molecular biology continues to provide an essential framework for understanding information flow in biological systems, while chemical biology approaches offer powerful methods to manipulate this flow for therapeutic purposes. Recent discoveries, such as the reverse transcriptase activity of human Polθ and the development of flexizyme systems for genetic code reprogramming, have expanded our understanding of how genetic information can be stored, transferred, and manipulated [26] [25]. These advances create new opportunities for therapeutic intervention through chemical biology approaches that target specific steps in information flow.
The integration of physiological context remains paramount for successful translation of these discoveries into clinical benefits. The chemical biology platform, with its emphasis on multidisciplinary teamwork and systematic validation across biological scales, provides an organizational framework for bridging the gap between molecular insights and patient care [1]. As our understanding of the central dogma continues to evolve, so too will our ability to design precisely targeted interventions that correct pathological information flow in disease states, ultimately advancing the goals of precision medicine and improving therapeutic outcomes for patients.
The Modern Toolset: From Chemical Probes to AI-Driven Discovery
Targeted protein degradation (TPD) represents a paradigm shift in chemical biology and drug discovery, moving beyond traditional binding-based inhibition toward active removal of disease-driving proteins [27]. This approach has unlocked therapeutic possibilities for previously “undruggable” targets, including transcription factors like MYC and STAT3, mutant oncoproteins such as KRAS G12C, and scaffolding molecules lacking conventional binding pockets [27]. Among TPD strategies, proteolysis-targeting chimeras (PROTACs) have emerged as a leading platform, with the first molecule entering clinical trials in 2019 and progression to Phase III completion by 2024 [27].
The significance of PROTAC technology lies in its fundamental reimagining of pharmacological intervention. Traditional small-molecule inhibitors operate through occupancy-driven pharmacology, requiring sustained high drug concentrations to maintain target inhibition [28]. By contrast, PROTACs function through event-driven pharmacology, catalytically inducing protein degradation and allowing for sub-stoichiometric activity [28]. This mechanistic difference provides unique advantages in overcoming drug resistance, targeting proteins lacking functional pockets, and achieving prolonged pharmacological effects despite shorter exposure times [29] [28].
PROTACs have expanded the toolbox available to chemical biologists, enabling not only therapeutic development but also functional studies of complex biological systems. These heterobifunctional molecules serve as chemical probes to dissect protein function, validate targets, and manipulate cellular pathways with temporal precision, especially when combined with emerging pro-PROTAC strategies that offer spatial and temporal control over protein degradation [29] [30].
PROTAC Design and Mechanism of Action
Core Structural Components
PROTACs are trimeric small molecules consisting of three essential components [29]:
- Target Protein Ligand: A specific binder of the Protein of Interest (POI)
- E3 Ligase Ligand: A recruiter of ubiquitin ligase machinery
- Linker: A suitably flexible connector that spatially optimizes the ternary complex
The formation of a productive POI-PROTAC-E3 ternary complex enables the E3 ligase to ubiquitinate surface lysine residues of the POI, marking it for recognition and destruction by the ubiquitin-proteasome system (UPS) [29]. The catalytic nature of this process means that a single PROTAC molecule can mediate multiple rounds of degradation, offering significant potency advantages over traditional inhibitors [28].
Mechanistic Pathway of Targeted Degradation
The following diagram illustrates the sequential mechanism of PROTAC-induced protein degradation:
This mechanism highlights the catalytic cycle where the PROTAC molecule is released after each degradation event to engage additional target proteins [27] [28]. The efficiency of this process depends critically on the formation of a productive ternary complex with appropriate spatial orientation between the target protein and E3 ligase [27].
Comparative Analysis: PROTACs vs. Traditional Therapeutics
Table 1: Pharmacological comparison of PROTACs and traditional therapeutic modalities
| Feature/Capability | Small Molecule Inhibitors | Monoclonal Antibodies | PROTAC Protein Degraders |
|---|---|---|---|
| Mechanism of Action | Occupancy-driven inhibition | Occupancy-driven blocking | Event-driven degradation |
| Target Scope | Limited to proteins with defined pockets | Extracellular and membrane proteins | Broad, including "undruggable" targets |
| Resistance Management | Vulnerable to mutations and overexpression | Limited by target accessibility | Overcomes many resistance mechanisms |
| Dosing Requirements | Sustained high concentrations needed | Periodic administration | Catalytic, sub-stoichiometric activity |
| Selectivity Potential | Dependent on binding pocket specificity | High for extracellular targets | Enhanced through ternary complex formation |
| Therapeutic Duration | Short-lived (protein function returns) | Variable | Prolonged (requires new protein synthesis) |
The comparative advantages outlined in Table 1 demonstrate why PROTAC technology has generated substantial excitement across drug discovery and chemical biology research. Unlike traditional approaches that merely inhibit protein function, PROTACs achieve a more complete pharmacological effect by physically removing the target protein from the cellular environment [27] [28]. This is particularly valuable for targeting multifunctional proteins and scaffold proteins that can maintain partial function even when inhibited.
Advanced PROTAC Technologies and Clinical Applications
Pro-PROTAC Strategies for Controlled Activation
Recent advances have focused on developing PROTAC prodrugs (pro-PROTACs) that remain inactive until specific physiological or experimental conditions trigger their activation [29]. This latentiation strategy serves multiple purposes:
- Selective targeting of pathological tissues to reduce on-target off-tissue effects
- Prolonged biological action through controlled release kinetics
- Precise investigation of protein signaling pathways in vitro [29]
Photocaged PROTACs (opto-PROTACs) represent one of the most innovative pro-PROTAC approaches. These molecules are protected with photolabile groups such as 4,5-dimethoxy-2-nitrobenzyl (DMNB) moiety that prevent critical hydrogen-bond interactions with the corresponding E3 ligase [29]. Installation of caging groups can be achieved on the glutarimide NH of Cereblon (CRBN) ligands, the hydroxyl group of Von Hippel-Lindau (VHL) ligands, or directly on the target protein ligand [29]. Upon irradiation with specific wavelengths (typically UV light at 365 nm), the caging group is removed, releasing the active PROTAC and enabling spatiotemporal control of protein degradation [29].
Clinical Translation and Key Targets
Table 2: Clinically advanced PROTAC candidates and their targets
| PROTAC Candidate | Target | Indication | Development Stage |
|---|---|---|---|
| ARV-110 | Androgen Receptor (AR) | Prostate Cancer | Phase III |
| ARV-471 | Estrogen Receptor (ER) | Breast Cancer | Phase III |
| BTK Degraders | Bruton's Tyrosine Kinase | Hematologic Cancers | Phase II |
| STAT3 Targeting | Signal Transducer and Activator of Transcription 3 | Various Cancers | Phase I/II |
| IRAK4 Targeting | Interleukin-1 Receptor-Associated Kinase 4 | Inflammation, Cancer | Phase I |
The clinical landscape for PROTACs has expanded rapidly, with current data indicating 19 PROTACs in Phase I, 12 in Phase II, and 3 in Phase III clinical trials as of 2025 [29] [27]. These candidates target diverse proteins including nuclear receptors, kinases, and transcription factors implicated in cancer, neurodegenerative disorders, and immune system diseases [29].
Experimental Protocols for PROTAC Development
Protocol 1: Design and Synthesis of Photocaged PROTACs
Objective: To develop light-activatable PROTACs for spatiotemporal control of protein degradation [29].
Materials and Reagents:
- Parent PROTAC with known degradation activity
- Photolabile protecting groups (DMNB, NPOM, or DEACM)
- Anhydrous dimethylformamide (DMF) or dimethyl sulfoxide (DMSO)
- Diisopropylethylamine (DIPEA) as base
- Dichloromethane (DCM) for extraction
- Flash chromatography system for purification
Procedure:
- Identify caging site: Analyze ternary complex structure to determine optimal caging position that disrupts critical interactions with E3 ligase or target protein. The glutarimide NH of CRBN ligands and hydroxyproline moiety of VHL ligands are common sites [29].
- Synthesize caged building block: React the E3 ligase ligand (e.g., pomalidomide for CRBN) with the photolabile group (e.g., DMNB-chloroformate) in anhydrous DMF with DIPEA as base. Stir under nitrogen atmosphere for 12 hours at room temperature [29].
- Conjugate to target ligand: Connect the caged E3 ligase ligand to the target protein ligand using appropriate linker chemistry. This typically involves amide coupling or click chemistry reactions.
- Purify and characterize: Isulate the final caged PROTAC using flash chromatography and verify structure by mass spectrometry and NMR spectroscopy.
- Validate photoactivation: Test PROTAC inactivity in cellular models, then irradiate with 365 nm UV light (5-20 J/cm²) and confirm restoration of degradation activity via immunoblotting [29].
Protocol 2: Cellular Evaluation of PROTAC Activity
Objective: To assess target protein degradation efficiency and selectivity in cellular models.
Materials and Reagents:
- Appropriate cell line expressing target protein
- PROTAC compounds (serial dilutions in DMSO)
- Positive control inhibitor (if available)
- Lysis buffer (RIPA buffer with protease inhibitors)
- Immunoblotting equipment and antibodies
- Quantitative PCR system
- Cell viability assay reagents (MTT, CCK-8)
Procedure:
- Cell treatment: Plate cells in 6-well or 12-well plates and allow to adhere overnight. Treat with PROTAC concentrations (typically 1 nM - 10 µM) for predetermined time points (usually 4-24 hours).
- Protein extraction: Lyse cells in RIPA buffer, quantify protein concentration, and prepare samples for immunoblotting.
- Degradation assessment: Perform immunoblotting for target protein and loading controls. Calculate DC₅₀ (concentration causing 50% degradation) and Dmax (maximum degradation achieved) using densitometric analysis [30].
- Selectivity profiling: Evaluate related proteins and potential off-targets by immunoblotting or proteomic analysis to confirm degradation selectivity.
- Functional consequences: Assess downstream phenotypic effects through viability assays, cell cycle analysis, or apoptosis assays to link degradation to functional outcomes.
Research Reagent Solutions for Protein Degradation Studies
Table 3: Essential research tools for PROTAC development and evaluation
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| E3 Ligase Ligands | VHL ligands, CRBN ligands (thalidomide, lenalidomide), MDM2 ligands, IAP ligands | Recruit endogenous ubiquitin machinery to target protein |
| Target Protein Binders | Kinase inhibitors, BET inhibitors, AR/ER antagonists, transcription factor binders | Provide binding moiety for protein of interest |
| Linker Systems | PEG chains, alkyl chains, piperazine derivatives | Spatially connect E3 ligand and target binder |
| Photolabile Groups | DMNB, NPOM, DEACM | Enable spatiotemporal control of PROTAC activation |
| Protac Control Compounds | Inactive analogs with mismatched ligase ligands | Establish mechanism-specific effects |
| Ubiquitin-Proteasome Reagents | Proteasome inhibitors (MG132), ubiquitination assay kits | Validate mechanistic pathway |
The PROTAC field continues to evolve with several emerging trends shaping its future trajectory. Multitargeted degraders that simultaneously address multiple disease-associated proteins offer promise for tackling complex pathologies driven by interconnected molecular networks [31]. Artificial intelligence and machine learning are increasingly being applied to PROTAC design through predictive modeling of ternary complex formation, virtual screening of degrader candidates, and generative design of optimized linkers [29] [32]. Tools such as AIMLinker and DeepPROTACs exemplify how AI is revolutionizing rational degrader design [29].
Integration of PROTACs with advanced delivery platforms represents another frontier. Antibody-PROTAC conjugates leverage the targeting precision of antibodies to deliver PROTAC payloads specifically to diseased tissues, as demonstrated by BMS-986497 which uses an anti-CD33 antibody to deliver a GSPT1-targeting PROTAC into CD33-positive tumor cells [30]. Such approaches address the pharmacokinetic challenges of conventional PROTACs while maintaining their catalytic degradation efficiency.
In conclusion, PROTAC technology has established itself as an essential component of the chemical biology toolkit, providing researchers and drug developers with unprecedented capability to target previously inaccessible proteins. The continued innovation in pro-PROTAC strategies, combined with advanced computational design and selective delivery approaches, promises to expand the therapeutic application of targeted protein degradation across diverse disease contexts. As the field matures, these chemical tools will undoubtedly yield new fundamental insights into protein function while delivering transformative therapies for challenging diseases.
Within the modern chemical biology platform, target identification and validation represent the critical foundation upon which successful drug discovery and translational physiology research are built. This process aims to pinpoint the specific biomolecules—typically proteins—through which a small molecule exerts its therapeutic effect, and to provide robust evidence that modulating this target will yield a clinical benefit [33] [1]. The profound challenge of demonstrating clinical efficacy and managing safety concerns has historically resulted in a success rate of less than 10% for new drug development programs [34]. Overcoming this challenge necessitates a mechanism-based approach, deeply integrated with translational physiology, which examines biological functions across all levels, from molecular interactions to population-wide effects [1]. The emergence of powerful functional genomics and chemoproteomic technologies has created an unprecedented opportunity to systematically identify and validate drug targets, thereby de-risking the pipeline and accelerating the development of new therapies for conditions such as cardiovascular disease, the leading global cause of mortality [34].
The Functional Genomics Toolkit: RNAi and CRISPR
2.1 Core Principles and Workflows Chemical-genetic strategies are founded on the central tenet that a cell's sensitivity to a small molecule is directly influenced by the expression level of its molecular target [33]. Early work in yeast established that reducing the dosage of a drug's target gene (haploinsufficiency) confers hypersensitivity, while overexpressing the target often confers resistance [33]. These foundational principles have been successfully translated to mammalian systems using two primary technologies: RNA interference (RNAi) and CRISPR-Cas.
- RNA Interference (RNAi): This method uses short-hairpin RNAs (shRNAs) introduced into cells via lentiviral transduction to mediate the degradation of complementary target mRNAs, thereby reducing gene expression [33]. In a pooled screen, a library of shRNA expression constructs is introduced into a cell population, and the change in abundance of each shRNA after drug treatment is quantified by next-generation sequencing, revealing which gene knockdowns affect drug sensitivity [33].
- CRISPR-Cas Systems: The CRISPR-Cas system utilizes a Cas9 nuclease programmed with a single-guide RNA (sgRNA) to introduce double-strand breaks at specific DNA loci. Error-prone repair via non-homologous end-joining (NHEJ) often results in frameshift mutations and gene knockout [33] [35]. Catalytically inactive "dead" Cas9 (dCas9) can also be used as a programmable DNA-binding protein to recruit transcription factors for gene repression or activation without altering the DNA sequence [33].
Table 1: Comparison of Functional Genomics Screening Technologies
| Feature | RNAi (shRNA) | CRISPR Knockout (CRISPRn) | CRISPR Interference/Activation (CRISPRi/a) |
|---|---|---|---|
| Mechanism of Action | Degradation of target mRNA | Introduction of frameshift mutations via NHEJ | Programmable recruitment of repressors/activators via dCas9 |
| Type of Perturbation | Transcriptional knockdown | Complete gene knockout | Transcriptional knockdown or overexpression |
| Key Readout | Hypersensitivity to drug (for target ID) | Hypersensitivity or resistance to drug | Hypersensitivity or resistance to drug |
| Primary Application in Target ID | Loss-of-function (LOF) screens [36] | LOF screens; generation of drug-resistant variants [35] | LOF & gain-of-function (GOF) screens [33] |
| Main Advantage | Established, compatible with HTS [36] | Highly effective at removing gene expression [36] | Precise modulation without DNA damage; reversible |
The following diagram illustrates the core workflow for a pooled CRISPR knockout screen to identify a small molecule's target:
Diagram 1: Pooled CRISPR screen workflow.
2.2 Advanced CRISPR Applications: CRISPRres Beyond standard knockout screens, advanced CRISPR methodologies have been developed specifically for target identification. The CRISPRres (CRISPR-induced resistance) approach exploits Cas9-induced NHEJ repair to generate a wide variety of in-frame mutations at a specific locus [35]. When performed under drug selection, this method enriches for functional, drug-resistant protein variants, directly nominating the drug's molecular target. The process involves:
- Designing sgRNA Tiling Libraries: sgRNAs are designed to target exonic regions, particularly functional domains, of multiple essential genes suspected to be potential drug targets [35].
- Transient Expression and Selection: The sgRNA library is transiently expressed with SpCas9 in cells, which are then treated with the drug of interest [35].
- Resistant Colony Formation: Drug-resistant colonies emerge due to mutations that disrupt drug-target binding while preserving protein function [35].
- Mutation Identification: Sequencing of the targeted loci in resistant pools or clones reveals specific resistance-conferring mutations, thereby identifying the drug's target [35].
This method was successfully validated with known drug-target pairs (e.g., XPO1-selinexor, KIF11-ispinesib) and applied to identify NAMPT as the target of the anticancer agent KPT-9274 [35].
Chemoproteomic and Genoproteomic Strategies
3.1 Affinity-Based Chemoproteomics Affinity-based biochemical methods represent a complementary, direct approach to target deconvolution. These strategies involve immobilizing the small molecule of interest on a solid support to create "affinity beads," which are then used to capture interacting proteins from complex biological lysates [33]. The bound proteins are subsequently identified using advanced mass spectrometry (MS). This methodology is a cornerstone of the integrated service portfolio offered by research infrastructures like EU-OPENSCREEN, which provides open access to high-throughput screening and chemoproteomics platforms [37].
3.2 A Translational Genoproteomic Framework The integration of human genetics with high-throughput proteomics—genoproteomics—provides a powerful, hypothesis-free framework for identifying and prioritizing causal drug targets before a compound is even developed [34]. This translational framework bridges the genome, proteome, and phenome through four key stages:
- Causal Biomarker Screen: A proteome-wide Mendelian randomization (ProMR) analysis is performed to pinpoint circulating proteins (biomarkers) that are causally associated with a disease of interest. This mimics the therapeutic effect of modulating the biomarker [34].
- Drug-Targeting Protein Discovery: The specific proteins underlying the causal biomarker are identified using cis-acting protein quantitative trait loci (cis-pQTLs) as instrumental variables. This step pinpoints the actionable drug-targeting protein [34].
- On-Target and Off-Target Effect Exploration: The potential for unintended on-target side effects is investigated by testing the genetic association between the drug-targeting protein and a wide range of other clinical phenotypes [34].
- Pragmatic Target Trial: The final stage involves designing and implementing pragmatic trials, such as Mendelian randomization studies, to predict the long-term efficacy and safety of the proposed therapeutic intervention [34].
This framework has been successfully applied to validate known lipid-lowering drug targets (e.g., PCSK9, LDLR) and provides a robust, genetics-backed pipeline for prioritizing new targets [34].
Diagram 2: Genoproteomic translational framework.
Experimental Protocols for Core Methodologies
4.1 Protocol: Pooled CRISPR Knockout Screen for Target Identification This protocol outlines the key steps for identifying genes essential for small molecule activity [33] [35].
- Library Design and Production: Select a genome-wide sgRNA library (e.g., Brunello, GeCKO). Amplify the library and clone it into a lentiviral transfer vector.
- Virus Production and Cell Transduction: Generate high-titer lentivirus in HEK293T cells. Transduce the target cell population (e.g., HAP1, HCT116) at a low Multiplicity of Infection (MOI ~0.3) to ensure most cells receive a single sgRNA. Select transduced cells with puromycin for 3-5 days.
- Drug Treatment and Selection: Split the cell population into two arms: a drug-treated group (exposed to the small molecule at IC50-IC90 concentration) and an untreated control group. Culture cells for 14-21 days, passaging them regularly to maintain representation of all sgRNAs.
- Sequencing and Hit Analysis: Harvest genomic DNA from both arms. Amplify the integrated sgRNA cassettes by PCR and subject them to next-generation sequencing. Bioinformatically compare sgRNA abundance between treated and control samples. Genes targeted by sgRNAs that are significantly depleted in the treated arm are strong candidates for being essential for the drug's mechanism of action.
4.2 Protocol: CRISPRres for Direct Target Deconvolution via Resistance This protocol uses focused mutagenesis to reveal the target directly [35].
- sgRNA Tiling Library Design: Design a custom sgRNA library that tiles across the exons of a pre-selected set of essential genes (e.g., a few hundred candidate targets).
- Transient Transfection and Selection: Co-transfect the target cells (e.g., HAP1) with plasmids expressing SpCas9 and the sgRNA tiling library. 24-48 hours post-transfection, plate the cells and apply the drug at a lethal concentration (e.g., 4x IC50).
- Outgrowth and Clone Isolation: Culture the cells for 2-3 weeks, allowing resistant colonies to form. Either pool all resistant colonies or pick individual clones for further analysis.
- Target Locus Sequencing and Validation: PCR-amplify and sequence the genomic regions targeted by the sgRNA library from the resistant pool or clones. The gene(s) harboring in-frame mutations (missense, insertions, deletions) in the resistant population is the direct target of the small molecule. Validate by recreating the specific mutation in naive cells via HDR and confirming drug resistance.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of the described methodologies relies on a suite of specialized reagents, instruments, and computational resources.
Table 2: Key Research Reagent Solutions and Platforms
| Item / Platform | Function / Description | Application in Target ID/Validation |
|---|---|---|
| Genome-Wide sgRNA/shRNA Libraries | Pooled constructs for targeting all human genes. | Enables hypothesis-free genetic screens to find genes modulating drug response [33] [36]. |
| Lentiviral Delivery Systems | Efficient system for stable integration of genetic constructs into diverse cell types. | Essential for creating stable, scalable cell populations for pooled CRISPR/RNAi screens [33]. |
| HAP1 Cell Line | Near-haploid human cell line derived from KBM7. | Simplifies the identification of recessive mutations and is ideal for CRISPRres screens [35]. |
| 384-well Nucleofector System | High-throughput electroporation instrument. | Enables efficient, automated delivery of CRISPR components into primary cells for functional screens [38]. |
| High-Content Imaging Systems | Automated microscopes with integrated image analysis software. | Provides multiparametric phenotypic data (cell viability, apoptosis, protein translocation) for assay readouts [1]. |
| EU-OPENSCREEN RI | European Research Infrastructure for chemical biology. | Provides open access to HTS, chemoproteomics, and medicinal chemistry expertise [37]. |
| ColorBrewer / Viz Palette | Online tools for designing accessible color palettes. | Ensures clarity and accessibility in data visualization for publications and presentations [39] [40]. |
The convergence of functional genomics (RNAi and CRISPR) and direct biochemical/genetic approaches (chemoproteomics and genoproteomics) creates a powerful, synergistic toolkit for target identification and validation within the chemical biology platform. While CRISPR-based screens offer a direct path to discovering genes involved in a drug's mechanism, genoproteomic frameworks provide human genetic evidence that significantly increases the probability of clinical success for a drug target [34]. The future of translational research lies in the intelligent integration of these complementary technologies. By systematically applying functional screens to nominate candidate targets, using chemoproteomics to confirm direct binding, and leveraging human genetic data to validate causal roles in disease, researchers can build an irrefutable chain of evidence. This multi-faceted, integrative approach, firmly grounded in translational physiology, is the key to de-risking drug discovery and delivering precise, effective new medicines to patients.
The landscape of drug discovery has been fundamentally shaped by two predominant screening philosophies: phenotypic-based drug discovery (PDD) and target-based drug discovery (TDD). The 2020s have witnessed a significant paradigm shift, moving away from viewing these approaches as mutually exclusive and toward a more integrated strategy that leverages the strengths of both. This evolution is driven by technological advancements and a growing recognition that complex diseases often require modulation of multiple biological pathways [41] [42].
The unparalleled progress in science over recent decades has brought a better understanding of disease mechanisms, initially promoting TDD approaches. However, despite high promises associated with TDD, a critical decrease in the number of first-in-class drugs has been observed, prompting a re-evaluation of strategies [41]. Meanwhile, modern phenotypic drug discovery has re-emerged as a powerful approach, combining the original concept of observing therapeutic effects on disease physiology with contemporary tools and strategies [43]. This whitepaper examines the current state of both methodologies within the framework of chemical biology platforms and translational physiology research, providing researchers with advanced protocols and comparative analyses to guide strategic implementation in modern drug development pipelines.
Philosophical and Strategic Foundations
Target-Based Drug Discovery: A Reductionist Approach
Target-based drug discovery operates on a reductionist principle, focusing on specific molecular targets believed to be central to disease pathology. This approach begins with the selection of a well-characterized molecular target—typically a protein, enzyme, or receptor—followed by screening compounds that selectively bind to or modulate this target [44]. The TDD paradigm dominated pharmaceutical research throughout the 1990s and early 2000s, fueled by advances in molecular biology and the sequencing of the human genome [45].
The key advantage of TDD lies in its mechanistic clarity. Researchers can design drugs based on well-defined molecular interactions, enabling high specificity and efficient structure-based drug design through computational modeling and crystallography [44]. This approach has produced many effective drugs in the modern pharmacopeia, including clinically transformative modalities like BCR-Abl, Hepatitis C polymerase, and TNFα inhibitors [46].
Phenotypic Drug Discovery: A Systems Biology Approach
Phenotypic drug discovery takes a holistic approach, identifying bioactive compounds based on their ability to alter a cell or organism's observable characteristics (phenotype) in a desired manner without requiring prior knowledge of a specific molecular target [44]. This strategy evaluates how a compound influences a biological system as a whole, enabling the discovery of novel mechanisms of action, particularly in diseases where molecular underpinnings remain unclear [43].
The fundamental strength of PDD is its capacity for unbiased discovery. By selecting compounds based on therapeutic effect rather than predefined molecular interactions, PDD allows for mechanistically novel drug discovery and can capture complex biological interactions that contribute to clinical efficacy, especially for complex diseases like neurodegenerative disorders [43] [44]. Historical accounts show that phenotypic screening played a crucial role in early drug discovery, exemplified by Alexander Fleming's discovery of penicillin through observing the phenotypic effect of Penicillium rubens on bacterial colonies [44].
Comparative Analysis: Strategic Positioning
Table 1: Fundamental Comparison Between Phenotypic and Target-Based Screening Approaches
| Parameter | Phenotypic Screening | Target-Based Screening |
|---|---|---|
| Discovery Bias | Unbiased, allows for novel target identification | Hypothesis-driven, limited to known pathways |
| Mechanism of Action | Often unknown at discovery, requiring later deconvolution | Defined from the outset |
| Therapeutic Translation | Better captures complex biology, improving likelihood of clinical efficacy | May fail to capture complex disease pathophysiology |
| Technical Requirements | Requires high-content imaging, functional genomics, and AI | Relies on structural biology, computational modeling, and enzyme assays |
| Throughput | Moderate to high (depending on model complexity) | Typically high |
| First-in-Class Potential | High (majority of first-in-class drugs originate from PDD) | Moderate |
Advanced Methodologies and Experimental Protocols
Contemporary Phenotypic Screening Workflows
Modern phenotypic screening leverages sophisticated model systems and readout technologies that bridge the gap between traditional cell culture and human physiology. The following protocol outlines a comprehensive phenotypic screening workflow utilizing advanced 3D culture systems.
Protocol 1: High-Content Phenotypic Screening Using 3D Organoid Models
Biological Model Selection and Validation
- Step 1: Establish physiologically relevant disease models. Patient-derived organoids, induced pluripotent stem cell (iPSC)-derived models, and organ-on-chip systems represent the current gold standard [43] [44]. For cystic fibrosis research, for instance, cell lines expressing wild-type or disease-associated CFTR variants enabled discovery of both potentiators (ivacaftor) and correctors (tezacaftor, elexacaftor) [43].
- Step 2: Characterize model systems through transcriptomic, proteomic, and functional analyses to ensure they recapitulate key disease phenotypes. Multi-omics integration provides a systems-level understanding of the model's biological relevance [45].
Compound Library Design and Application
- Step 3: Curate diverse chemical libraries with high structural heterogeneity to maximize novel target discovery. Include non-annotated compounds and known bioactive molecules for reference [44]. Modern libraries often exceed 100,000 compounds for primary screens.
- Step 4: Implement concentration-response formatting (e.g., 10-point, 1:3 serial dilution) to gather robust pharmacological data from initial screens. Typical screening concentrations range from 1 nM to 10 μM.
Phenotypic Readouts and High-Content Analysis
- Step 5: Employ high-content imaging platforms capturing multiple parameters simultaneously: cell morphology, viability, intracellular trafficking, and metabolic activity [43] [44]. Key parameters include:
- Nuclear morphology and count (Hoechst stain)
- Cytoskeletal organization (Phalloidin stain)
- Mitochondrial function (TMRE, JC-1 dyes)
- Lysosomal activity (LysoTracker)
- Metabolic activity (Alamar Blue, ATP luminescence)
- Step 6: Apply automated image analysis using machine learning algorithms for feature extraction and pattern recognition. Convolutional neural networks can identify subtle phenotypic changes indistinguishable to the human eye [47].
Hit Validation and Triaging
- Step 7: Conduct counter-screens against unrelated cell types to exclude nonspecific cytotoxic compounds. Implement orthogonal assays to confirm primary hits.
- Step 8: Perform structure-activity relationship (SAR) analysis on confirmed hits to prioritize compounds for further optimization.
Advanced Target-Based Screening Platforms
Modern target-based screening has evolved beyond simple enzyme inhibition assays to incorporate complex biology while maintaining target specificity.
Protocol 2: CRISPR-Enhanced Target Validation and Screening
Target Identification and Prioritization
- Step 1: Employ multi-omics data integration to identify potential therapeutic targets. Combine transcriptomics, proteomics, and chromatin accessibility data (ATAC-seq) to build gene regulatory networks [45].
- Step 2: Use CRISPR-based functional genomics to validate target-disease relationships. Pooled CRISPR screens enable systematic assessment of gene function across entire pathways [45].
Mechanistic Assay Development
- Step 3: Design assays that capture target function in physiological contexts. For kinase targets, this may include:
- Phosphorylation-specific antibodies for high-content imaging
- TR-FRET-based phosphorylation assays
- Conformational biosensors for real-time activation monitoring
- Step 4: Incorporate structural biology early in screening campaigns. Use X-ray crystallography or cryo-EM to guide compound design and understand binding modes.
High-Throughput Screening and Hit Identification
- Step 5: Implement automation-compatible assays in 1536-well format for primary screening. Typical assay volumes: 5-10 μL.
- Step 6: Apply machine learning approaches to identify promising chemical series early. Utilize existing structure-activity relationship (SAR) data to build predictive models.
Integrated Approaches: Bridging the Screening Divide
The most advanced screening paradigms strategically combine phenotypic and target-based approaches.
Protocol 3: Phenotypic-to-Target-Based Transition Screening
- Phase 1: Conduct primary screening in phenotypic systems to identify compounds with desired functional effects.
- Phase 2: Implement target deconvolution strategies for phenotypic hits, including:
- Chemical proteomics (affinity purification + mass spectrometry)
- Functional genomics (CRISPR knockout screens with resistance selection)
- Transcriptomic profiling (similarity to known bioactive compounds)
- Phase 3: Validate identified targets through mechanistic target-based assays.
- Phase 4: Optimize compounds using target-directed medicinal chemistry while maintaining periodic testing in original phenotypic systems.
Technological Enablers and Research Tools
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for Modern Screening Approaches
| Reagent/Technology | Function | Application Examples |
|---|---|---|
| Patient-derived organoids | Physiologically relevant 3D culture models that recapitulate disease heterogeneity | Cancer biology, inflammatory bowel disease, cystic fibrosis [43] |
| CRISPR-Cas9 gene editing | Precise genome manipulation for target validation and model generation | Functional genomics, gene knockout, knock-in mutations [45] |
| High-content imaging systems | Automated microscopy with multiparametric image analysis | Subcellular localization, morphological profiling, phenotypic fingerprinting [44] |
| DNA-encoded libraries | Ultra-large chemical libraries for screening against purified targets | Billions of compounds screened in single tubes against target proteins [48] |
| Proteomics platforms (AP-MS, thermal shift) | Target identification and engagement validation | Target deconvolution, mechanism of action studies [43] |
| AI/ML analysis platforms | Pattern recognition in complex datasets | Hit prediction, toxicity forecasting, chemical optimization [47] |
Visualization of Screening Workflows and Decision Pathways
The following diagrams illustrate key workflows and strategic relationships in modern screening approaches.
Diagram 1: Phenotypic Screening Workflow
Diagram 2: Target-Based Screening Workflow
Diagram 3: Integrated Screening Strategy
Emerging Concepts and Future Directions
Polypharmacology and Selective Targeters of Multiple Proteins (STaMPs)
The renewed appreciation for polypharmacology represents a significant evolution in screening philosophy. Rather than viewing drug promiscuity as a liability, modern approaches increasingly recognize that therapeutic efficacy for complex diseases often requires modulation of multiple targets [46] [43]. This has led to the conceptualization of Selective Targeters of Multiple Proteins (STaMPs)—single small molecules designed to engage 2-10 specific targets with nanomolar potency while maintaining favorable pharmaceutical properties (molecular weight <600) [46].
The STaMP framework represents a departure from the traditional "one-target-one-disease" paradigm that dominated drug design in the late 20th century. Modern antidegeneration STaMPs typically engage between 2 and 7 low nanomolar targets, strategically selected to disrupt pathological systems across multiple cell lineages involved in disease processes such as neuroinflammation [46]. Computational approaches for STaMP design leverage systems biology and multi-omics integration to identify synergistic target combinations that offer enhanced therapeutic efficacy when modulated concurrently [46].
Artificial Intelligence and Machine Learning Integration
AI and machine learning have progressed from experimental curiosities to essential components of modern screening platforms. By mid-2025, AI-designed therapeutics were advancing through human trials across diverse therapeutic areas, with platforms demonstrating the ability to compress early-stage research and development timelines significantly [47]. Five distinct AI-driven discovery paradigms have emerged:
- Generative chemistry platforms that design novel molecular structures
- Phenomics-first systems that prioritize biological effects
- Integrated target-to-design pipelines that streamline the discovery process
- Knowledge-graph repurposing that identifies new indications for existing compounds
- Physics-plus-ML design that combines molecular simulations with machine learning [47]
Notably, companies like Exscientia have reported in silico design cycles approximately 70% faster than traditional approaches, requiring 10× fewer synthesized compounds [47]. The 2024 merger between Recursion and Exscientia created an integrated platform combining extensive phenomic screening with automated precision chemistry, representing a significant consolidation in the AI-driven drug discovery landscape [47].
Translational Physiology and Chemical Biology Platforms
The chemical biology platform represents an organizational approach that optimizes drug target identification and validation while improving the safety and efficacy of biopharmaceuticals [1]. This platform connects a series of strategic steps to determine whether a newly developed compound could translate into clinical benefit using translational physiology—the examination of biological functions across multiple levels, from molecular interactions to population-wide effects [1].
Unlike traditional trial-and-error methods, chemical biology emphasizes targeted selection and integrates systems biology approaches (transcriptomics, proteomics, metabolomics, network analyses) to understand protein network interactions [1]. Physiology forms the core of this platform by providing essential biological context, enabling researchers to understand function in a living context, identify and validate targets, bridge molecular and systems biology, and develop tools for directed application [1].
The evolution of screening strategies in the 2020s reflects a maturation in our approach to drug discovery. Rather than positioning phenotypic and target-based approaches as competitors, the field has moved toward strategic integration that leverages the unique strengths of each methodology. Phenotypic screening excels at identifying novel mechanisms and assessing complex biological systems, while target-based approaches provide mechanistic clarity and enable rational optimization [41] [43].
This integrated paradigm is further enhanced by advances in AI-driven design, complex model systems, and multi-omics technologies that bridge the historical gap between phenotypic observations and target identification. The resulting chemical biology platforms represent a holistic framework for drug discovery that incorporates translational physiology from the earliest stages, potentially increasing the efficiency of the drug discovery pipeline and improving clinical translation success rates [41] [1].
As these technologies continue to evolve, the distinction between phenotypic and target-based screening may further blur, giving rise to truly integrated platforms that simultaneously capture the complexity of biological systems while providing mechanistic insights into compound action. This synergistic approach promises to unlock new therapeutic avenues for diseases that have long eluded effective treatment, ultimately accelerating the delivery of transformative medicines to patients.
The chemical biology platform represents an organizational approach to drug discovery that emphasizes understanding underlying biological processes and leveraging knowledge from the action of similar molecules [1]. This platform connects strategic steps to determine whether a newly developed compound could translate into clinical benefit using translational physiology, which examines biological functions across multiple levels, from molecular interactions to population-wide effects [1]. Artificial intelligence (AI) and in silico technologies are now revolutionizing this framework by enabling the systematic exploration of chemical space and prediction of biological activity at unprecedented scales and speeds.
The traditional drug discovery process is notoriously lengthy and expensive, often requiring 10-15 years and over $4 billion to bring a new drug to market, with a failure rate exceeding 90% [49] [50]. This inefficiency stems largely from the trial-and-error nature of conventional methods and the challenges of demonstrating clinical benefit from highly potent compounds targeting specific biological mechanisms [1]. AI technologies, particularly machine learning (ML) and deep learning (DL), are disrupting this paradigm by providing data-driven insights that accelerate target identification, compound optimization, and clinical translation.
This technical guide examines how predictive modeling and virtual screening are transforming the chemical biology platform across the drug discovery pipeline. By integrating AI with systems biology approaches—including transcriptomics, proteomics, and metabolomics—researchers can now prioritize targeted selection and understand protein network interactions more effectively than ever before [1].
Foundational AI Technologies in Chemical Biology
Machine Learning and Deep Learning Architectures
AI in drug discovery encompasses multiple specialized architectures, each with distinct advantages for specific applications in the chemical biology workflow:
Generative Models: These include Variational Autoencoders (VAEs), Generative Adversarial Networks (GANs), and diffusion models that can propose novel molecular structures with desired properties [51]. VAEs offer a useful balance with rapid, parallelizable sampling, an interpretable latent space, and robust, scalable training that performs well even in low-data regimes [51].
Discriminative Models: These models, including random forests, support vector machines (SVMs), and gradient boosting methods like XGBoost, excel at classification and prediction tasks such as toxicity assessment or binding affinity prediction [52].
Graph Neural Networks (GNNs): GNNs effectively represent molecular structures as graphs, capturing complex topological features and enabling accurate prediction of molecular properties and interactions [52].
Transformers and Large Language Models: Adapted from natural language processing, these models treat molecular representations (e.g., SMILES) as sequences, allowing them to capture long-range dependencies and generate novel molecular structures [51].
Molecular Representations for AI
Effective molecular representation is crucial for AI applications in chemical biology. The table below summarizes the primary representation methods and their applications:
Table 1: Molecular Representations in AI-Driven Drug Discovery
| Representation Type | Format | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| SMILES | Text string | Generative AI, chemical language models | Simple, compact, human-readable | No explicit spatial information |
| Molecular Graphs | Node-edge structure | GNNs, property prediction | Explicit bond and atom representation | Complex preprocessing |
| 3D Structural | Atomic coordinates | Docking, molecular dynamics | Captures spatial relationships | Computationally intensive |
| Molecular Fingerprints | Binary vectors | Virtual screening, similarity search | Fast similarity calculations | Loss of structural details |
| Quantum Chemical | Electronic parameters | Quantum mechanics, QSAR | High accuracy for electronic properties | Extremely computationally expensive |
AI-Enabled Workflows in Target Identification and Validation
Enhancing Translational Physiology with Predictive Modeling
Translational physiology examines biological functions across levels from molecules to populations [1]. AI enhances this approach by creating multi-scale models that integrate data from diverse biological levels, enabling more accurate predictions of clinical efficacy during early discovery phases. Machine learning models can analyze transcriptomics, proteomics, and metabolomics data to identify novel disease targets and validate their therapeutic potential [1].
The introduction of clinical biology—using laboratory assessments to diagnose disease and monitor treatment efficacy—represented an early effort to bridge preclinical and clinical findings [1]. AI dramatically enhances this approach through:
- Biomarker Discovery: ML algorithms can identify complex biomarker signatures from high-dimensional omics data that correlate with clinical outcomes [49].
- Target-Disease Association: Network-based algorithms integrate diverse data sources to establish causal relationships between targets and disease pathophysiology [49] [50].
- Cross-Species Translation: AI models address the critical challenge of translating findings from model organisms to humans by learning conserved biological pathways and interspecies differences [1].
Research Reagent Solutions for AI-Enhanced Target Validation
Table 2: Essential Research Reagents for AI-Enhanced Target Validation
| Reagent Category | Specific Examples | Function in AI Workflow | Data Output for AI Models |
|---|---|---|---|
| Gene Editing Tools | CRISPR-Cas9 systems | Target perturbation | Validation of target-disease association |
| Antibodies | Phospho-specific antibodies | Protein detection and quantification | Protein expression and activation data |
| Cell-Based Assays | Reporter gene assays, HCS | High-content screening | Multiparametric cellular response data |
| Animal Models | Genetically engineered models | In vivo target validation | Translational physiology data |
| Proteomic Kits | Multiplex immunoassays | Protein profiling | Training data for predictive models |
Virtual Screening and Compound Design
Advanced Virtual Screening Methodologies
Virtual screening has evolved from simple similarity searching to sophisticated AI-driven approaches that can evaluate billions of compounds in silico. Modern virtual screening combines physics-based methods with data-driven approaches to achieve both accuracy and efficiency:
- Structure-Based Virtual Screening: Uses protein structures (experimental or predicted) to screen compound libraries through molecular docking [51]. AI enhances this through improved scoring functions and rapid pose prediction.
- Ligand-Based Virtual Screening: Leverages known active compounds to identify structurally or functionally similar molecules using AI-derived molecular representations [49].
- Hybrid Approaches: Combine both structure and ligand information to improve screening accuracy, especially when structural data is limited [51].
AI-powered virtual screening platforms like Atomwise use convolutional neural networks (CNNs) to predict molecular interactions and have identified drug candidates for diseases such as Ebola and multiple sclerosis in less than a day [49].
Generative AI for De Novo Molecular Design
Generative AI represents a paradigm shift from "design first then predict" to "describe first then design" [51]. These models learn underlying patterns in molecular datasets and generate novel compounds with tailored characteristics:
Fig. 1: Generative AI workflow for molecular design incorporating active learning feedback loops.
Successful implementations include generative models that created novel CDK2 inhibitors with nanomolar potency and novel scaffolds for KRAS inhibitors, addressing previously challenging drug targets [51]. The integration of active learning (AL) cycles—where AI models iteratively refine their predictions based on newly acquired data—significantly enhances the efficiency of generative workflows by maximizing information gain while minimizing resource use [51].
Predictive Modeling in Preclinical Development
AI-Enhanced ADMET and Toxicity Prediction
Predicting Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET) properties early in the discovery process is crucial for reducing late-stage failures. AI has dramatically improved these predictions:
- Physiologically-Based Pharmacokinetic (PBPK) Modeling: AI-enhanced PBPK models simulate drug concentration-time profiles in tissues, informing dosage regimens and potential drug-drug interactions [49].
- Toxicity Prediction: Machine learning models trained on large toxicology datasets can identify structural alerts and predict various toxicity endpoints with increasing accuracy [52].
- Bioavailability Optimization: AI models help optimize compounds for oral bioavailability by simultaneously balancing multiple parameters including solubility, permeability, and metabolic stability [53].
Research Reagent Solutions for Predictive Modeling
Table 3: Essential Research Materials for AI-Enhanced Predictive Modeling
| Material Category | Specific Examples | AI Application | Data Type Generated |
|---|---|---|---|
| In Vitro ADME Assays | Caco-2 permeability, microsomal stability | Model training for PK prediction | Quantitative ADME parameters |
| Toxicity Screening Panels | hERG assay, Ames test, hepatotoxicity | Toxicity prediction models | Binary and continuous toxicity endpoints |
| Biomimetic Systems | Artificial membranes, organ-on-chip | PBPK model refinement | Tissue-specific partitioning data |
| Proteomic Profiling | CYP450 inhibition assays | Drug-drug interaction prediction | Enzyme inhibition parameters |
| Tissue Biomarkers | Safety biomarker panels | Translational safety assessment | Biomarker-response relationships |
The Virtual Human: A Systems Pharmacology Approach
From Reductionist to Systemic Models
The current pharmaceutical development model often fails because it takes a reductionist approach, focusing on a new drug's effect on targeted genes in isolation [50]. This ignores the complex systemic interactions within the human body. The concept of a programmable virtual human uses AI to predict how new drugs will affect the entire body, not just a targeted protein [50].
This approach integrates physics-based models of biological, physiological, and clinical knowledge with machine-learning models trained on data demonstrating how different human systems work [50]. The resulting virtual human can be programmed to predict how a new drug will interact with the body, answering questions about side effects, toxicity, and effectiveness long before clinical phases [50].
Implementing Virtual Human Platforms
Fig. 2: Virtual human framework integrating multi-scale biological data for systemic drug response prediction.
This systemic approach is particularly valuable for complex diseases such as Alzheimer's disease or neurological disorders that affect systems rather than specific genes or proteins [50]. For these conditions, multiple genes work together in complex pathways that cannot be adequately addressed through single-target approaches.
Experimental Protocols for AI-Enhanced Drug Discovery
Protocol: Active Learning Framework for Generative Molecular Design
This protocol outlines the experimental workflow for implementing an active learning (AL) framework with generative AI for molecular design, based on validated methodologies [51]:
Data Preparation and Representation
- Collect target-specific compound data with associated binding affinities or activities
- Represent molecules as SMILES strings, tokenize, and convert to one-hot encoding vectors
- Split data into initial training set (general compounds) and target-specific training set
Initial Model Training
- Train Variational Autoencoder (VAE) on general training set to learn viable chemical space
- Fine-tune VAE on target-specific training set to enhance target engagement
- Validate model performance through reconstruction accuracy and novelty metrics
Nested Active Learning Cycles
Inner AL Cycles (Chemical Optimization):
- Sample VAE to generate new molecules
- Evaluate generated molecules for drug-likeness, synthetic accessibility, and novelty using chemoinformatic predictors
- Fine-tune VAE on molecules meeting threshold criteria
- Repeat for predetermined iterations (typically 3-5 cycles)
Outer AL Cycles (Affinity Optimization):
- Perform molecular docking simulations on accumulated molecules from inner cycles
- Transfer molecules meeting docking score thresholds to permanent-specific set
- Fine-tune VAE on permanent-specific set to prioritize high-affinity candidates
- Repeat nested AL process for multiple rounds (typically 2-3 outer cycles)
Candidate Selection and Validation
- Apply stringent filtration to identify promising candidates
- Perform advanced molecular modeling (e.g., PELE simulations) for binding interaction analysis
- Select top candidates for synthesis and experimental validation
This workflow successfully generated novel CDK2 inhibitors, with 8 of 9 synthesized molecules showing in vitro activity, including one with nanomolar potency [51].
Protocol: AI-Enhanced Peptide Drug Discovery
This protocol describes Gubra's integrated approach to AI-driven peptide discovery, which has produced novel GLP-1 receptor agonists with improved drug properties [53]:
Structure Prediction and Analysis
- Use AlphaFold for protein structure prediction of target receptors
- Analyze binding sites and structural features to inform design constraints
- Generate structural models of receptor-ligand complexes
De Novo Peptide Design
- Employ generative models (e.g., proteinMPNN) to design novel peptide sequences compatible with target 3D structure
- Generate diverse peptide candidates with variations in sequence and length
- Apply structural filters to ensure compatibility with binding site
Machine Learning-Guided Optimization
- Implement streaMLine platform for high-throughput in silico screening
- Optimize simultaneously for multiple properties: potency, selectivity, and stability
- Use predictive models to prioritize candidates with optimal drug-like properties
Experimental Validation and Iteration
- Synthesize top-ranking peptide candidates
- Validate receptor binding and functional activity through in vitro assays
- Assess selectivity against related receptors to minimize off-target effects
- Evaluate in vivo efficacy in relevant disease models (e.g., diet-induced obese mice)
- Use experimental results to refine AI models for subsequent optimization cycles
This approach has demonstrated success in developing novel GLP-1 receptor agonists based on a secretin backbone, with AI-driven substitutions improving GLP-1R affinity while reducing off-target effects [53].
Implementation Challenges and Future Directions
Addressing Current Limitations
Despite significant advances, several challenges remain in fully realizing AI's potential in drug discovery:
Data Quality and Quantity: AI models require large, high-quality datasets, which are often limited for specific targets or disease areas [49]. Transfer learning and data augmentation techniques are being developed to address this limitation.
Interpretability and Explainability: The "black box" nature of complex AI models raises concerns for regulatory approval and scientific understanding [49]. Explainable AI (XAI) methods are being integrated to provide insights into model decisions.
Regulatory and Ethical Considerations: Regulatory frameworks for AI-generated drug candidates are still evolving, requiring collaborative efforts to establish appropriate guidelines [49].
Integration with Existing Workflows: Successful implementation requires integrating AI tools with traditional medicinal chemistry expertise and experimental workflows [51].
Emerging Trends and Future Outlook
The field of AI in drug discovery continues to evolve rapidly, with several emerging trends shaping its future:
Foundation Models for Chemistry: Large-scale models pre-trained on extensive chemical databases are being developed, similar to GPT models in natural language processing, enabling transfer learning across multiple drug discovery tasks [54].
AI-Enabled Quantum Chemistry: Neural network wavefunction ansatz and AI-accelerated quantum Monte Carlo methods are improving the accuracy of molecular property predictions [54].
Integrated Multi-Scale Modeling: The combination of AI with physics-based simulations across quantum, molecular, and physiological scales promises more comprehensive predictive capabilities [50].
Automated Experimentation and Closed-Loop Systems: The integration of AI with laboratory automation enables closed-loop systems where AI designs experiments, interprets results, and iterates based on findings [54].
The continued advancement of AI in drug discovery promises to further reduce development timelines, decrease costs, and improve success rates, ultimately enhancing our ability to address unmet medical needs through the development of novel therapeutics.
Translational physiology represents a paradigm shift in biomedical research, moving beyond unidirectional "bench-to-bedside" models to embrace a dynamic, bidirectional workflow. This integrated approach systematically leverages clinical observations to inform basic research, which in turn generates new therapeutic strategies for clinical validation. Framed within the context of the chemical biology platform in drug discovery, this whitepaper delineates the core principles, methodologies, and practical frameworks essential for implementing successful bench-to-bedside-to-bench workflows. By emphasizing iterative learning across the molecular-to-population continuum, this guide provides researchers and drug development professionals with the strategic insights and technical protocols needed to accelerate the development of precision medicines and overcome the persistent challenges in translational science.
The concept of "Translational Research" (TR) has gained significant momentum in the biomedical domain as a proposed solution to bridge the perceived gap between knowledge produced at the lab bench and its application in clinical practice [55]. Initially conceived as a unidirectional process—moving discoveries from basic science to patient care—the concept has matured to recognize the critical importance of bidirectional feedback. The contemporary understanding of translational physiology acknowledges that clinical bedside observations must consistently inform and redirect fundamental bench research, creating a continuous cycle of refinement and discovery [1].
This evolution is partly rooted in historical precedent. The National Cancer Institute's Specialized Programs of Research Excellence (SPOREs), established in 1992, specifically encouraged TR that promoted a "bi-directional exchange between basic and clinical science" [55]. Today, this bidirectional workflow is recognized as fundamental to addressing the "valley of death" in drug development—the gap between promising laboratory discoveries and their successful clinical application [56]. The integration of a chemical biology platform, which applies chemical principles and tools to study and manipulate biological systems, provides a robust organizational framework for this process, optimizing drug target identification and validation while improving the safety and efficacy of biopharmaceuticals [1].
Core Principles of the Bidirectional Workflow
Deconstructing the Translational Continuum
The translational pathway is most effectively conceptualized as a multi-stage, recursive cycle rather than a linear sequence. Each phase has distinct objectives and feedback mechanisms.
T1: Basic Research to Clinical Application (Bench to Bedside): This initial phase involves translating fundamental scientific discoveries into potential clinical applications. Activities include identifying therapeutic targets based on disease mechanisms and developing novel drug compounds, therapies, or diagnostic tools [57]. The chemical biology platform is crucial here, employing small molecules to study and modulate biological systems and create biological response profiles [1].
T2: Clinical Implementation to Practice (Bedside to Guidelines): This stage shifts from controlled laboratory settings to real-world clinical trials, assessing safety and efficacy in diverse patient populations [58]. Success in T2 leads to the development of evidence-based clinical practice guidelines, ensuring treatments are used effectively and consistently [57].
T3: Practice to Population Impact (Guidelines to Public Health): The focus here is on disseminating proven interventions into healthcare systems and assessing their broader impact on public health. This includes long-term monitoring, analysis of health outcomes across populations, and influencing health policies [58].
T4: Population to Bench (Bedside to Bench): This critical, often overlooked phase completes the cycle. Observations from clinical practice, population-level data, and unresolved clinical questions are fed back to basic scientists. This informs new hypotheses, refines existing models, and identifies novel research avenues, ensuring that the laboratory work remains clinically relevant [59].
The Role of the Chemical Biology Platform
The chemical biology platform serves as the operational engine for the bidirectional workflow. It functions as an organizational approach that connects a series of strategic steps to determine whether a newly developed compound could translate into clinical benefit using translational physiology [1]. Its core functions include:
- Target Identification and Validation: Using chemical probes to understand the function of potential drug targets in physiologically relevant models.
- Lead Optimization: Applying principles of chemistry to improve the potency, selectivity, and drug-like properties of candidate molecules.
- Mechanism-of-Action Studies: Elucidating how compounds produce their biological effects at a molecular level.
- Biomarker Development: Identifying and validating measurable indicators of biological states or pharmacological responses to therapeutics.
Table 1: Key Dimensions of Translational Research as Defined in Scientific Discourse [55]
| Dimension | Description | Implication for Workflow |
|---|---|---|
| Construction of the Gap | How the disconnect between basic and clinical science is perceived. | Defines the specific problem the bidirectional workflow aims to solve. |
| Model of the Process | The conceptual framework of translation (e.g., linear vs. cyclical). | Directs the design of research programs and funding structures. |
| Attributed Cause | The perceived root cause of the translational gap (e.g., cultural, structural). | Determines where interventions and resources are focused. |
Implementing the Workflow: Methodologies and Protocols
Foundational Experimental Protocols for Translational Physiology
Implementing a successful bidirectional workflow requires adherence to rigorous, multi-level experimental protocols. The following methodology, adapted from the principles of clinical biology and the chemical biology platform, provides a framework for advancing a therapeutic candidate [1].
Protocol: Preclinical to Early-Clinical Translation for a Novel Therapeutic Agent
Objective: To establish a mechanistic link between a compound's activity in preclinical models and its potential clinical efficacy, enabling a robust "Go/No-Go" decision for Phase IIb/III trials.
Step 1: Identify and Qualify a Disease-Relevant Biomarker
- Methodology: Use multi-omic approaches (genomics, proteomics, metabolomics) on human diseased tissue and biofluids to identify a molecular parameter (biomarker) that is dysregulated in the disease state and plausibly linked to pathology.
- Validation: Confirm the biomarker is measurable, reproducible, and has a known range in healthy and diseased populations.
- Rationale: A qualified biomarker provides an objective, early measure of a drug's pharmacological activity in humans before clinical benefit can be observed [1].
Step 2: Demonstrate Target Engagement and Biomarker Modulation in an Animal Model
- Methodology:
- Select a pharmacologically relevant animal model (e.g., transgenic mouse, xenograft, or disease-induced model) that recapitulates the human biomarker.
- Administer the candidate compound at various doses.
- Collect tissue and biofluid samples at predetermined timepoints.
- Use targeted assays (e.g., immunoblotting, ELISA, LC-MS) to quantify biomarker levels and establish a dose-response relationship.
- Rationale: This confirms the compound can engage its intended target and produce the desired pharmacological effect in a complex living system [1].
Step 3: Establish Proof-of-Concept in a Human Model of Disease
- Methodology: Conduct a Phase IIa clinical trial in a small, well-characterized patient population. The trial should:
- Be designed to test if the drug modulates the biomarker in humans.
- Incorporate micro-dosing or Phase 0 studies with tracer compounds to confirm human pharmacokinetics and target engagement if possible.
- Monitor for early, albeit preliminary, signals of clinical efficacy alongside biomarker changes.
- Rationale: This step closes the loop between animal and human pharmacology, providing critical evidence that the mechanism of action is functional in patients [1] [60].
Step 4: Demonstrate Dose-Dependent Clinical Benefit
- Methodology: Design a larger trial (Phase IIb) to establish a correlation between the degree of biomarker modulation and a meaningful clinical outcome. The study must show that greater biomarker correction is associated with improved patient outcomes.
- Rationale: This confirms the biomarker is not just a surrogate of activity but is directly involved in the therapeutic pathway, validating the entire mechanistic hypothesis [1].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials central to conducting experiments within the translational physiology workflow.
Table 2: Research Reagent Solutions for Translational Workflows
| Reagent / Material | Function in Workflow | Specific Application Example |
|---|---|---|
| Chemical Probes | To selectively modulate and study the function of a specific protein or pathway in cells. | Investigating the phenotypic consequences of target inhibition in disease-relevant cell lines. |
| Validated Antibodies | For detection, quantification, and localization of specific proteins (antigens) in assays and tissues. | Immunoblotting or immunohistochemistry to measure biomarker levels in pre- and post-treatment tissue samples. |
| Biobanked Human Tissues | Provide physiologically relevant material for target and biomarker discovery/validation. | Genomic and proteomic analysis of diseased vs. healthy tissues to identify novel therapeutic targets. |
| Reporter Gene Assays | To assess signal activation in response to ligand-receptor engagement or pathway modulation. | Screening chemical libraries for activators or inhibitors of a specific signaling pathway of interest. |
| Human Organoids | 3D in vitro models that recapitulate human physiology and disease for drug testing. | Replacing traditional cell lines for more physiologically relevant assessment of drug efficacy and toxicity [61]. |
Visualization of Workflows and Signaling Pathways
The following diagrams, generated using Graphviz DOT language, illustrate the core logical relationships and workflows in bidirectional translational physiology.
The Bidirectional Translational Research Cycle
Diagram Title: Bidirectional Translational Cycle
Integrated Chemical Biology in Drug Discovery
Diagram Title: Chemical Biology Drug Discovery Workflow
Quantitative Frameworks and Data Analysis
The success of translational workflows depends on quantitative decision-making. The following table summarizes key quantitative data and timelines involved in the drug development process, highlighting opportunities for acceleration.
Table 3: Quantitative Benchmarks and Acceleration Strategies in Translational Research
| Metric | Traditional Timeline/Number | Accelerated Approaches | Data Source/Example |
|---|---|---|---|
| Bench to Bedside Timeline | 10-15 years [60] | Use of pragmatic trials, shared control groups, and global networks can reduce timeline. | The development of PCSK9 inhibitors unfolded over 10-15 years, considered "relatively fast" [60]. |
| Clinical Trial Participant Diversity | Historically limited | Global trials networks (e.g., STRIVE with 200+ sites across 40 countries) to expand pool and diversity [62]. | STRIVE network enrolls patients from six continents, enhancing generalizability and recruitment speed [62]. |
| FDA Drug Approvals (NME/BLA) | 22 approvals in 2016 [56] | Use of FDA designations (Fast Track, Breakthrough Therapy) to expedite review. | In 2016, 8 of 22 approved drugs were first-in-class, and 9 had Orphan Drug status [56]. |
| Phase II Trial Duration | Several years | "Learn as you go" adaptive trial designs and optimized statistical methods. | A Phase II study of selumetinib took 1-2 years for design/approval and 1-2 years for conduct [60]. |
Challenges and Future Directions
Despite its logical appeal, implementing a truly bidirectional workflow faces significant hurdles. A primary challenge is the knowledge deficit in translational chemical biology, particularly in academic settings, where discovered chemical probes often fail to advance due to a lack of medicinal chemistry expertise and translational medicine experience [56]. Furthermore, interdisciplinary collaboration remains difficult, requiring seamless integration between basic scientists, clinicians, bioinformaticians, and regulatory experts [57].
Future progress hinges on several key developments:
- Embracing Reverse Pharmacology: Learning from traditional medicine knowledge and natural products can provide validated starting points for drug discovery, reducing time and cost [56].
- Leveraging Artificial Intelligence and Big Data: AI will be critical for analyzing vast datasets from multi-omics studies to identify novel targets and biomarkers and predict patient responses [57].
- Adopting Innovative Trial Designs: Pragmatic trials embedded in clinical care and adaptive statistical designs are essential for improving efficiency and relevance [62].
- Fostering Continuous Education: Programs like genomic tumor boards for early-career researchers are vital for training scientists to understand the clinical context and communicate effectively with clinicians [59].
Integrating translational physiology through bidirectional bench-to-bedside-to-bench workflows is no longer a theoretical ideal but a practical necessity for advancing precision medicine. By leveraging the structured approach of the chemical biology platform and committing to iterative learning across the entire research continuum, the scientific community can systematically bridge the gap between laboratory discovery and clinical impact. This requires a cultural shift towards deeper collaboration, the adoption of innovative methodologies and trial designs, and a relentless focus on the feedback from the clinic to the bench. The frameworks, protocols, and visualizations provided in this whitepaper offer a roadmap for researchers and drug development professionals to navigate this complex but rewarding landscape, ultimately accelerating the delivery of effective therapies to patients.
Navigating Complexity: Strategies for Accelerating Hit-to-Lead and Beyond
Biomedical research is currently undergoing a paradigm shift, moving away from approaches heavily reliant on traditional animal models and toward strategies centered on human-specific biology. This transition is largely driven by the notoriously high failure rates of the current drug development process. Despite remarkable investments in research and development, the drug attrition rate recently reached an all-time high of 95% [63]. Most drugs fail in clinical stages despite proven efficacy and safety in animal models, revealing a significant translational gap between preclinical promise and clinical utility [64] [63]. This gap represents a critical roadblock in drug development, resulting in delayed treatments for patients, wasted investments, and reduced confidence in otherwise promising research avenues [64].
A major contributor to this challenge is the inherent limitation of conventional preclinical models. Animal models, while remaining the gold standard in basic research, often suffer from interspecies differences and poor prediction of human physiological and pathological conditions [63]. These discrepancies derive from different anatomical layouts, divergent receptor expression, immune responses, and distinct pathomech-anisms. Furthermore, animals are inbred and kept under standardized conditions, meaning they do not account for the genetic and ethnic diversity of human populations [63]. The consequences are twofold: potentially harmful or ineffective drugs proceed to clinical trials, while potentially effective drug candidates may be abandoned due to negative preclinical results in biologically irrelevant models [63].
This review explores an integrated strategy to bridge this translational gap, focusing on the synergistic application of advanced human disease models and robust biomarker validation frameworks within the context of chemical biology and translational physiology. By leveraging human-relevant models such as organoids, bioengineered tissues, and organs-on-chips, combined with multi-omics technologies and AI-driven analytics, researchers can improve the predictive validity of preclinical research and accelerate the path from biomarker discovery to clinical application [64] [63].
The Biomarker Challenge: From Discovery to Clinical Utility
The Biomarker Translational Pipeline
Biomarkers—defined as measurable indicators of biological processes, pathogenic processes, or pharmacological responses to therapeutic intervention—are fundamental to modern precision medicine. They encompass gene expression products, metabolites, polysaccharides, and other molecules such as circulating nucleic acids, single-nucleotide polymorphisms, and gene variants [65]. The ideal biomarker for diagnostic, prognostic, or drug development purposes demonstrates both high specificity and sensitivity [65].
Biomarkers can be categorized functionally into several types:
- Pharmacodynamic biomarkers indicate the outcome of the interaction between a drug and a target, including both therapeutic and adverse effects.
- Prognostic biomarkers suggest the likely course of a disease irrespective of treatment.
- Predictive biomarkers identify patients who are likely to respond to a particular treatment [65].
The journey of a biomarker from discovery to clinical application is long and arduous. Troublingly, less than 1% of published cancer biomarkers actually enter clinical practice [64]. This high failure rate results from multiple factors, including over-reliance on traditional animal models with poor human correlation, lack of robust validation frameworks, and inadequate reproducibility across cohorts [64]. Additionally, disease heterogeneity in human populations presents a significant challenge compared to the controlled conditions and uniformity of preclinical testing environments [64].
Key Pitfalls in Biomarker Translation
Several interpretative and practical issues must be understood and resolved before potential biomarkers can become clinically approved tests. The major pitfalls in the translation from biomarker discovery to clinical utility include:
- Inadequate Selection Criteria: Initiating the discovery phase without proper strategic selections regarding patient population, sample processing, and analytical methods.
- Deficient Validation Strategies: Lack of systematic biomarker characterization and validation strategies, including insufficient sample sizes and inadequate statistical power.
- Technical Limitations: Poor robustness of analysis techniques used in clinical trials, including lack of standardization across platforms [65].
The lack of agreed-upon protocols for biomarker validation presents a particular challenge. Without standardized methods to control variables or determine appropriate sample sizes, results can vary significantly between tests and laboratories, or fail to translate to wider patient populations [64]. Furthermore, different research teams may use varying evidence benchmarks for validation, making it difficult to accurately assess the reliability of newly identified biomarkers [64].
Table 1: Key Challenges in Biomarker Translation and Potential Solutions
| Challenge | Impact | Potential Solutions |
|---|---|---|
| Model Discrepancy | Poor correlation between animal model results and human clinical outcomes [64] | Implement human-relevant models (organoids, PDX, OoCs) [64] [63] |
| Validation Inconsistency | Low reproducibility across cohorts and laboratories [64] [65] | Establish standardized validation frameworks and protocols [65] |
| Disease Heterogeneity | Biomarkers fail in diverse patient populations [64] | Incorporate diverse patient-derived samples and multi-omics approaches [64] |
| Regulatory Complexity | Delayed approval and implementation [65] | Early engagement with regulatory agencies, companion diagnostic co-development [65] [66] |
Advanced Human Disease Models: Bridging the Preclinical-Clinical Divide
The Evolution of Disease Modeling
To address the limitations of traditional models, advanced human disease models with high clinical biomimicry are being developed. These models better recapitulate human physiology and pathology, offering improved predictive values for drug efficacy and safety testing [63]. The evolution from simple 2D cell cultures to complex 3D bioengineered systems represents a significant advancement in our ability to model human disease.
Two-dimensional (2D) cell cultures of patient-derived cells remain an invaluable tool for studying disease phenotypes and pathomechanisms, especially during early drug development phases. However, they have significant limitations, as cell responses and gene/protein expression patterns greatly differ between 2D and three-dimensional (3D) models [63]. For instance, 3D cultures of lung fibroblasts resemble in vivo tumor necrosis factor receptor expression and NF-κB activation patterns more closely than 2D cultures [63].
Bioengineered tissue models are primarily generated from human stem cells or primary cells seeded onto hydrogel or polymer-based scaffolds. These models emulate in vivo-like tissue conditions with maturated and differentiated states, achieving increased biomimicry of native human tissue compared to 2D systems [63]. This approach is particularly valuable for multi-layer or stratified tissues such as the gut, lungs, and skin [63].
Promising Model Systems
Organoids are self-organizing 3D structures generated from tissue-specific adult stem cells or induced pluripotent stem (iPS) cells [63]. These miniature organ-like structures retain key functional aspects of their source organs and demonstrate remarkable promise in biomarker research. Within organoids, particularly patient-derived organoids, the expression of characteristic biomarkers is more likely to be retained than in two-dimensional culture models [64]. They have been used effectively to predict therapeutic responses and guide the selection of personalized treatments, as well as in the identification of prognostic and diagnostic biomarkers [64].
Patient-derived xenograft (PDX) models, established by implanting human tumor tissue into immunodeficient mice, effectively recapitulate the characteristics of human cancer, including tumor progression and evolution [64]. PDX models have proven to be a more accurate platform for biomarker validation than conventional cell line-based models and have played key roles in investigating HER2 and BRAF biomarkers, among others [64]. Studies have demonstrated, for example, that KRAS mutant PDX models do not respond to cetuximab, suggesting that earlier use of these models could have expedited the discovery and validation of KRAS mutation as a marker of resistance [64].
Organs-on-chips (OoCs) are perfused microfluidic platforms containing bioengineered or miniaturized tissues or organs interconnected by 3D microchannels. These systems simulate in vivo functions, biomechanics, and pathophysiological responses of human organs [63]. Unlike organoids that form by self-organization, OoCs follow a reductionist engineering approach through targeted and pre-defined design of components. Multi-organ OoC systems enable the study of communication and interactions between several tissues simultaneously, potentially interconnecting at least 10 human organs to create a "human-on-a-chip" [63]. These systems currently constitute the most promising approach to emulate human diseases in vitro with high physiological relevance [63].
Table 2: Comparison of Advanced Human Disease Models
| Model Type | Key Features | Applications in Biomarker Research | Limitations |
|---|---|---|---|
| Organoids | Self-organizing 3D structures from stem cells; retain organ functionality [63] | Biomarker identification, personalized treatment prediction, drug response modeling [64] | Limited maturation (iPS-derived), protocol-dependent variability [63] |
| Patient-Derived Xenografts (PDX) | Human tumor tissue grown in immunodeficient mice [64] | Biomarker validation, studies of tumor evolution and drug resistance [64] | Costly, time-consuming, requires animal facilities [64] |
| Organs-on-Chips (OoCs) | Microfluidic devices with perfused, engineered tissues; multi-organ connectivity [63] | Tissue-specific responses, inter-tissue communication, pharmacokinetic studies [63] | Technical complexity, limited throughput, early development stage [63] |
| Bioengineered Tissue Models | Cells seeded on scaffolds; air-liquid interface capabilities [63] | Barrier function studies, host-pathogen interactions, toxicity testing [63] | Limited lifespan, cannot be cryopreserved, limited cell diversity [63] |
Integrated Methodologies: Combining Models and Biomarker Science
The Chemical Biology Platform Framework
The chemical biology platform represents an organizational approach to optimize drug target identification and validation while improving the safety and efficacy of biopharmaceuticals. This platform connects a series of strategic steps to determine whether a newly developed compound could translate into clinical benefit using translational physiology [1]. Unlike traditional trial-and-error methods, chemical biology emphasizes targeted selection and integrates systems biology approaches—including transcriptomics, proteomics, metabolomics, and network analyses—to understand protein network interactions [1].
The development of this platform occurred through several evolutionary steps. Initially, the bridging of disciplines between chemists and pharmacologists established foundational collaborations. The subsequent introduction of "clinical biology" further strengthened these connections by encouraging collaboration among preclinical physiologists, pharmacologists, and clinical pharmacologists [1]. Clinical biology focused on using laboratory assessments (later termed biomarkers) to diagnose disease, evaluate patient health, and monitor treatment efficacy, with interdisciplinary teams identifying human disease models and biomarkers that could more easily demonstrate drug effects before progressing to costly late-stage trials [1].
The modern chemical biology platform, introduced around 2000, leverages genomics information, combinatorial chemistry, improvements in structural biology, high-throughput screening, and various cellular assays [1]. These assays include high-content multiparametric analysis of cellular events using automated microscopy, reporter gene assays to assess signal activation, and ion channel activity screening using voltage-sensitive dyes or patch-clamp techniques [1].
Multi-Omics Integration and Longitudinal Validation
Advanced human disease models become particularly powerful when integrated with multi-omics strategies. Rather than focusing on single targets, multi-omic approaches leverage multiple technologies—including genomics, transcriptomics, and proteomics—to identify context-specific, clinically actionable biomarkers that might be missed with a single approach [64]. The depth of information obtained through these methods enables identification of potential biomarkers for early detection, prognosis, and treatment response, ultimately contributing to more effective clinical decision-making [64]. Recent studies have demonstrated that multi-omic approaches have helped identify circulating diagnostic biomarkers in gastric cancer and discover prognostic biomarkers across multiple cancers [64].
Longitudinal validation strategies represent another critical methodological advancement. While biomarker measurements at a single time-point offer a valuable snapshot of disease status, they cannot capture dynamic changes resulting from cancer progression or treatment [64]. Repeatedly measuring biomarkers over time provides a more comprehensive view, revealing subtle changes that may indicate cancer development or recurrence even before symptoms appear. This approach offers a more complete and robust picture than single, static measurements, significantly aiding translation to clinical settings [64].
Functional validation further strengthens biomarker development by confirming biological relevance. Traditional biomarker analysis often relies on the presence or quantity of specific biomarkers without confirming their direct role in disease processes or treatment responses. Functional assays complement traditional approaches by revealing more about a biomarker's activity and function, shifting from correlative to functional evidence that strengthens the case for real-world utility [64].
Experimental Protocol: Multi-Omic Biomarker Validation Using Patient-Derived Organoids
Purpose: To identify and validate clinically actionable biomarkers through integrated analysis of patient-derived organoids subjected to therapeutic compounds.
Materials and Requirements:
- Patient-derived organoids from relevant tissue (e.g., tumor biopsies)
- Matrigel or similar extracellular matrix scaffold
- Organoid culture media with tissue-specific growth factors
- Therapeutic compounds for screening
- Multi-omics platforms (NGS for genomics/transcriptomics, LC-MS/MS for proteomics, NMR/LC-MS for metabolomics)
- Automated imaging system for phenotypic analysis
- ELISA or MSD platforms for biomarker quantification
Methodology:
- Organoid Generation and Culture: Establish patient-derived organoids from primary tissue samples embedded in Matrigel domes and cultured with tissue-specific media [64] [63].
- Compound Screening: Treat organoids with therapeutic compounds across a concentration range (typically 5-8 points in duplicate) for 5-14 days, depending on doubling time.
- Phenotypic Response Assessment: Monitor viability, morphology, and functional readouts using automated imaging and ATP-based viability assays at multiple time points.
- Multi-Omic Profiling: At designated endpoints (e.g., 24h for transcriptomics, 72h for proteomics), harvest organoids for:
- Genomics/Transcriptomics: RNA/DNA extraction for NGS sequencing to identify differentially expressed genes and mutations.
- Proteomics: Protein extraction for LC-MS/MS to quantify protein expression and phosphorylation changes.
- Metabolomics: Metabolite extraction for NMR or LC-MS to assess metabolic pathway alterations.
- Data Integration: Use bioinformatics pipelines to integrate multi-omics datasets and identify candidate biomarkers correlated with treatment response.
- Biomarker Validation: Confirm candidate biomarkers using orthogonal methods (e.g., ELISA, immunohistochemistry) in original organoids and additional patient samples.
- Clinical Correlation: Compare biomarker findings with clinical response data when available to establish predictive value [64].
Visualization of Strategic Frameworks
The Translational Physiology Continuum
The following diagram illustrates the bi-directional nature of translational physiology, demonstrating how observations flow between basic science and clinical applications:
Integrated Biomarker Validation Workflow
This diagram outlines the comprehensive workflow for biomarker validation incorporating human disease models and multi-omics technologies:
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of the biomarker and human disease model strategy requires access to specialized reagents, platforms, and technologies. The following table details key solutions essential for research in this field:
Table 3: Research Reagent Solutions for Biomarker and Disease Modeling
| Tool/Category | Specific Examples | Function/Application |
|---|---|---|
| Stem Cell Sources | iPS cells, tissue-specific adult stem cells [63] | Generation of human disease models (organoids, tissue models) with patient-specific genetics |
| Extracellular Matrix | Matrigel, synthetic hydrogels, decellularized scaffolds [63] | 3D scaffolding for organoid and tissue model development |
| Multi-Omics Platforms | NGS systems, LC-MS/MS, spatial transcriptomics [64] | Comprehensive molecular profiling for biomarker discovery and validation |
| Microfluidic Systems | Organ-on-chip platforms, perfusion systems [63] | Physiologically relevant culture conditions with tissue-tissue interfaces |
| Specialized Assays | High-content screening, functional assays, AAV immunogenicity tests [64] [66] | Biomarker validation and functional characterization |
| AI/ML Analytics | Pattern recognition algorithms, multimodal data integration [64] [66] | Identification of biomarker signatures from complex datasets |
Emerging Technologies and Future Directions
Artificial Intelligence and Data Integration
Artificial intelligence has moved beyond hype to become an essential tool in biomarker discovery and validation. AI technologies, including deep learning and machine learning models, are revolutionizing biomarker discovery by identifying patterns in large datasets that could not be found using traditional manual means [64] [66]. These approaches are particularly valuable for integrating multimodal data from disparate sources, including different omics platforms, flow cytometry, and spatial biology [66].
The full potential of AI technologies relies on access to large, high-quality datasets that include comprehensive data from multiple sources [64]. This requires collaboration between all stakeholders to give research teams access to larger sample sizes and more diverse patient populations. As with all AI applications, maintaining scientific rigor is essential—researchers must verify AI-generated findings through traditional validation methods rather than accepting algorithmic outputs without question [66].
Companion Diagnostic Co-Development
Pharmaceutical companies are increasingly developing drugs and diagnostic tests simultaneously in a process referred to as drug-diagnostic co-development or companion diagnostic (CDx) development [65]. This approach better defines the appropriate patient population for treatment and offers several advantages, including reduced costs through pre-selected patient populations, improved chances of regulatory approval, significantly increased market uptake, and added value for core business operations [65].
The first drug introduced using the personalized medicine paradigm—Herceptin (Trastuzumab)—has now been on the market for more than a decade, yet the number of drugs marketed alongside CDx remains small [65]. Regulatory complexities present significant hurdles, particularly for smaller companies targeting rare diseases. Unlike off-the-shelf solutions, each gene therapy often requires bespoke assay development, validation, and commercialization planning—all before the first patient is dosed [66]. Success in this area requires early planning, parallel development of therapeutic and diagnostic programs, and partners capable of supporting both clinical and commercial phases.
Expansion Beyond Oncology
While oncology remains the established foundation for precision medicine, clear momentum is building in other therapeutic areas. Central nervous system (CNS) disorders, in particular, are showing promising parallels with oncology development pathways of 15-20 years ago [66]. Advances such as the recently FDA-cleared test from Fujirebio that measures phospho-Tau/B Amyloid 1-42 ratio now enable diagnosis in patients with cognitive symptoms without expensive PET scans [66]. This opens up the possibility of early treatment for dementia, much like oncology biomarkers revolutionized cancer care.
Other areas showing promise for biomarker-driven approaches include autoimmune and inflammatory diseases, where existing inflammatory biomarkers are being leveraged for new therapeutic applications; metabolic diseases, where GLP-1 drugs are creating demand for differentiation through biomarker profiles; and rare diseases, though these face headwinds due to small patient populations and high development costs [66].
The integration of advanced human disease models with comprehensive biomarker validation strategies represents a transformative approach to overcoming persistent translational hurdles in drug development. By leveraging human-relevant models such as organoids, PDX models, and organs-on-chips—combined with multi-omics technologies, longitudinal validation, and AI-driven analytics—researchers can significantly improve the predictive validity of preclinical research.
The chemical biology platform provides an organizational framework for implementing this strategy, emphasizing multidisciplinary collaboration and systematic approaches to target validation. As these technologies continue to evolve and demonstrate value across therapeutic areas beyond oncology, they offer the promise of accelerating the development of safer, more effective targeted therapies while reducing the high attrition rates that have plagued drug development.
Successful implementation requires addressing several ongoing challenges, including standardization of validation protocols, navigation of complex regulatory pathways, and development of robust companion diagnostics. By focusing on these integrated approaches, the biomedical research community can bridge the translational gap and more effectively deliver on the promise of precision medicine for patients worldwide.
Combinatorial optimization represents a paradigm shift in chemical biology and drug discovery, moving beyond traditional sequential trial-and-error approaches toward systematic, high-throughput methodologies. This technical guide examines the core principles, experimental protocols, and computational frameworks that enable efficient exploration of vast biological parameter spaces. Framed within the broader context of chemical biology platforms for translational physiology research, we detail how combinatorial strategies accelerate therapeutic development from target identification to clinical application. By integrating advanced computational algorithms with high-throughput experimental screening, researchers can now navigate complex multivariate optimization challenges in drug candidate selection, multi-gene pathway engineering, and combination therapy development with unprecedented efficiency and predictive power.
The evolution of pharmaceutical research has witnessed a fundamental transition from sequential optimization methods to integrated combinatorial approaches. This shift responds to the critical challenge of demonstrating clinical benefit for highly potent compounds targeting specific physiological mechanisms [1]. Traditional sequential optimization, which tests one variable or a small number of parts at a time, proves prohibitively time-consuming and expensive for complex biological systems with multidimensional parameter spaces [67]. The limitation is particularly acute in metabolic engineering, where successful pathway engineering typically requires simultaneous optimization of multiple variables rather than sequential adjustment of individual components [67].
Chemical biology platforms have emerged as organizational frameworks that leverage combinatorial optimization for drug target identification and validation. These platforms connect strategic steps to determine whether newly developed compounds will translate into clinical benefit through translational physiology, which examines biological functions across multiple levels from molecular interactions to population-wide effects [1]. The integration of combinatorial methods represents a cornerstone of modern precision medicine, enabling mechanism-based approaches to clinical advancement that fundamentally differ from traditional trial-and-error methodologies.
Table 1: Comparative Analysis of Optimization Approaches in Drug Discovery
| Feature | Sequential Trial-and-Error | Combinatorial Optimization |
|---|---|---|
| Experimental Throughput | Low (tests one variable at a time) | High (parallel testing of multiple variables) |
| Resource Requirements | High (time, labor, materials) | Reduced through automation and miniaturization |
| Systems-level Insight | Limited (focuses on individual components) | Comprehensive (captures emergent properties and interactions) |
| Success Rate in Complex Systems | Low due to oversight of interactions | High through systematic exploration |
| Applications in Drug Discovery | Traditional compound screening | Multi-target therapies, pathway engineering, synthetic biology |
Theoretical Foundations: From Mathematical Principles to Biological Applications
Computational Frameworks
Combinatorial optimization fundamentally involves finding an optimal object from a finite set of objects where the set of feasible solutions is discrete or can be reduced to a discrete set [68]. In biological contexts, this translates to identifying optimal combinations from a vast but finite array of possible biological configurations, such as gene expression levels, drug combinations, or protein engineering parameters.
The mathematical foundation recognizes that many combinatorial optimization problems are NP-complete, making exhaustive search computationally intractable for realistically-sized problems in drug discovery [68]. This computational complexity has driven the development of specialized algorithms that quickly rule out large parts of the search space or provide approximation solutions. For biological applications, these include:
- Greedy algorithms that make locally optimal choices at each stage
- Local search techniques that iteratively improve solutions
- Reverse greedy search that starts with a complete set and removes elements
- Branch-and-bound algorithms that systematically explore solution spaces
- Genetic algorithms that mimic natural selection processes
The performance of these algorithms varies by application context. For identifying c-optimal experimental designs with correlated observations, research has demonstrated that local and reverse greedy searches provide comparable performance, with the worst design outputs having variance less than 10% greater than the best design across a range of covariance structures [69].
The Supermodular Function Framework
A significant theoretical advancement for biological applications is the recognition that many optimization challenges in experimental design can be framed as monotone supermodular function minimization problems [69]. A function g is supermodular if:
$$g(d \cup {ej}) - g(d) \geq g(d' \cup {ej}) - g(d')$$
for all $d \subseteq d'$. This property indicates diminishing marginal reductions in the objective function with increasing design size, a characteristic common to many biological optimization problems where initial improvements diminish as systems approach their theoretical limits [69].
Experimental Platforms and Methodologies
High-Throughput Screening Systems
Combinatorial optimization in chemical biology relies on advanced laboratory platforms that enable high-throughput assessment of biological combinations. Conventional cell culture in well plates enables throughput of approximately 100 combinations tested per batch, but this proves insufficient for navigating the vast possibility space of drug combinations or genetic configurations [70]. For example, a mere 4-drug combination selected from a 100-drug library with three possible doses per drug generates approximately 3.2 × 10^9 possibilities [70].
Microfluidic technologies have dramatically enhanced screening capabilities by enabling massive miniaturization and parallelization. These systems can reduce reagent consumption to nanoliter volumes while increasing throughput to thousands of combinations per batch [70]. Advanced platforms such as mass-activated droplet sorting (MADS) enable high-throughput screening of enzymatic reactions at nanoliter scales, dramatically improving the efficiency of combinatorial space exploration [70].
Synthetic Biology and Metabolic Engineering Applications
In metabolic engineering, combinatorial optimization addresses the fundamental challenge of balancing multi-gene expression pathways without prior knowledge of optimal expression levels for each component [67]. Researchers have developed reusable combinatorial libraries with high diversity for efficient multi-gene expression optimization in Escherichia coli and other model systems [71]. These systems employ standardized genetic elements (promoters and 5' UTRs) with fluorescent reporters (e.g., eGFP, mCherry, TagBFP) to quantify expression variability, enabling rapid exploration of multi-gene expression landscapes [71].
The workflow typically involves:
- Engineering standardized genetic elements with fluorescent reporters
- Assembling libraries of single-, dual-, and tri-gene constructs via Golden Gate assembly
- Validating constructs through induction experiments
- Applying optimized configurations to metabolic pathways (e.g., lycopene biosynthesis)
- Quantitative analysis by qPCR to confirm uniformity of genetic components
This modular approach, featuring reusable libraries and dual-plasmid systems, offers a scalable tool for metabolic engineering and multi-enzyme co-expression [71].
Combinatorial Drug Therapy Optimization
Combinatorial drug therapy represents one of the most clinically significant applications of combinatorial optimization in chemical biology. The approach recognizes that multidrug combination therapies often show better results than single drug treatments (monotherapy) in combating complex diseases [70]. However, drug interactions are highly intricate and dose-dependent, creating a massive optimization landscape.
The phenotype-driven medicine concept associates combinatorial drug therapy with systems engineering and optimization theories, considering the biological system as an open system and optimizing drug combinations as system inputs based on phenotypic outputs [70]. This relationship is represented as:
$$X_{opt} = \underset{X}{\mathrm{argmax}}~E = \underset{X}{\mathrm{argmax}}~f(X)$$
where $X$ is the drug combination input, $E$ is the efficacy output (any measurable and quantifiable parameter), $f$ is the function relation between drug doses and efficacy, and $X_{opt}$ is the optimal combination [70].
Diagram 1: Drug Combination Optimization Workflow
Computational Strategies and Algorithmic Approaches
Classification of Optimization Methods
Combinatorial optimization strategies in synthetic biology and chemical biology can be broadly categorized into several distinct approaches:
- Combinatorial cloning methods generate multigene constructs from libraries of standardized basic genetic elements using one-pot assembly reactions [67]
- Multiplicative methods identify optimal weights to place on experimental units or design points, extending Elfving's Theorem to design spaces with correlated experimental units [69]
- Combinatorial optimization algorithms including local search, greedy search, and reverse greedy search that directly optimize discrete experimental designs [69]
- Advanced orthogonal regulators that enable precise control of gene expression timing and levels in various microorganisms [67]
Table 2: Performance Comparison of Combinatorial Optimization Algorithms for c-Optimal Experimental Designs
| Algorithm | Theoretical Guarantees | Practical Performance | Computational Complexity | Implementation Considerations |
|---|---|---|---|---|
| Local Search | Finds local minima | Worst-case variance <10% greater than best design | Polynomial time | Sensitive to initial solution; requires neighborhood definition |
| Greedy Search | Approximation bounds for supermodular functions | Competitive with multiplicative methods | Polynomial time | Simpler implementation; progressive solution building |
| Reverse Greedy Search | Performance guarantees for monotone functions | Comparable to local search | Polynomial time | Starts with full set; removes least valuable elements |
| Multiplicative Methods | Geometric characterization via Elfving's theorem | Effective for independent experimental units | Conic optimization required | Requires rounding to integer solutions; limited to certain correlation structures |
Biosensors and High-Throughput Screening
A significant innovation in combinatorial optimization is the integration of genetically encoded whole-cell biosensors with laser-based flow cytometry technologies [67]. These systems transduce chemical production into easily detectable fluorescence signals, enabling rapid screening of combinatorial libraries. This approach addresses the critical bottleneck in metabolic engineering where identifying optimal microbial strains from large libraries remains laborious due to time-consuming metabolite screening techniques [67].
Barcoding tools further enhance combinatorial optimization by facilitating diversity tracking at the DNA level, allowing researchers to correlate genotype with phenotype across vast combinatorial spaces [67]. When combined with biosensor approaches, these tools create powerful integrated systems for navigating complex biological design spaces.
Implementation Framework: A Three-Step Workflow for Drug Combination Optimization
Based on analysis of current methodologies, an effective combinatorial optimization workflow for chemical biology applications involves three integrated phases:
Phase 1: Literature Mining and Candidate Prioritization
Before conducting experiments, computational literature analysis and database mining can dramatically reduce the combinatorial search space. Research indicates that excluding just ten drugs from a 100-drug library reduces the number of quad-drug combinations by approximately one-third, while excluding fifty drugs reduces possibilities by over 95% [70]. This pre-screening phase leverages existing knowledge to eliminate unlikely candidates and focus resources on promising regions of the combinatorial landscape.
Phase 2: Iterative Experimental Optimization
The core optimization process employs iterative cycles of design, build, test, and learn:
- Design candidate combinations using computational models and prior results
- Build combinatorial libraries using high-throughput assembly methods
- Test libraries using automated screening platforms
- Learn from results to refine models and inform next design cycle
This iterative approach continuously narrows the search space toward optimal regions, dramatically improving efficiency compared to one-shot screening approaches.
Phase 3: Validation and Clinical Translation
The final phase focuses on validating optimized combinations in physiologically relevant models and designing clinical translation strategies. This includes assessing ADME (absorption, distribution, metabolism, and excretion) profiles, potential toxicities, and pharmacological interactions [1]. The translational physiology framework ensures that combinatorial optimization outcomes have genuine clinical relevance, bridging the gap between laboratory results and patient benefits.
Diagram 2: Three-Phase Combinatorial Optimization Workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Combinatorial Optimization
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| Standardized Genetic Parts (Promoters, UTRs, terminators) | Modular control of gene expression levels | Multi-gene pathway balancing in metabolic engineering [71] |
| Fluorescent Reporters (eGFP, mCherry, TagBFP) | Quantitative measurement of expression variability | Screening combinatorial libraries for optimal expression configurations [71] |
| Microfluidic Droplet Platforms | Miniaturized reaction environments for high-throughput screening | Assessing thousands of drug combinations or enzyme variants in parallel [70] |
| DNA Assembly Systems (Golden Gate, Gibson Assembly) | Modular construction of combinatorial genetic libraries | Building diverse genetic circuits and metabolic pathways [67] [71] |
| Whole-Cell Biosensors | Linking metabolite production to detectable signals | High-throughput screening of strain libraries for metabolic engineering [67] |
| Barcoding Systems | Tracking individual variants in pooled libraries | Monitoring population dynamics in combinatorial screens [67] |
| Advanced Orthogonal Regulators (CRISPR/dCas9, TALEs, ZFPs) | Precise control of gene expression timing and levels | Dynamic pathway regulation and optimization [67] |
Case Studies and Applications
Lycopene Biosynthesis Optimization
A practical implementation of combinatorial optimization demonstrated the balanced expression of three genes (crtE, crtI, and crtB) for lycopene biosynthesis in Escherichia coli [71]. Researchers created a high-throughput platform encompassing standardized genetic elements (promoters and 5' UTRs) with fluorescent reporters to quantify expression variability. Libraries of single-, dual-, and tri-gene constructs were assembled via Golden Gate assembly and validated by IPTG induction [71]. The optimized tri-gene library generated E. coli BL21(DE3) strains exhibiting variable levels of lycopene production, demonstrating the platform's capacity to balance multi-gene pathways without prior knowledge of optimal expression ratios.
c-Optimal Experimental Design with Correlated Observations
Combinatorial optimization algorithms have been successfully applied to identify c-optimal experimental designs when observations may be correlated within and between experimental units [69]. This approach assumes the data generating process can be described using generalized linear mixed models (GLMMs) and frames the c-optimal design criterion as a monotone supermodular function amenable to efficient minimization algorithms [69]. Experimental results demonstrate that local search and reverse greedy search algorithms perform competitively with multiplicative methods that generate weights to place on experimental units, providing a robust combinatorial approach to experimental design optimization.
Future Directions and Challenges
While combinatorial optimization has dramatically advanced chemical biology research, significant challenges remain. Biological systems exhibit nonlinearity, context-dependency, and evolutionary adaptation that complicate optimization efforts [67]. Current research focuses on integrating machine learning methods with combinatorial optimization to better predict biological system behavior from limited data [67]. Additional frontiers include the development of multi-objective optimization strategies that simultaneously balance efficacy, toxicity, manufacturability, and economic considerations in therapeutic development.
The integration of combinatorial optimization with translational physiology represents a particularly promising direction, creating closed-loop systems where computational predictions inform experimental design, and experimental results refine computational models. This iterative approach accelerates the translation of basic research findings into clinically beneficial therapies, ultimately fulfilling the promise of precision medicine through systematic, data-driven optimization of therapeutic interventions.
As combinatorial optimization methodologies continue to evolve, they will undoubtedly expand beyond their current applications in drug discovery and metabolic engineering to encompass broader challenges in chemical biology and translational physiology. The ongoing development of more sophisticated algorithms, higher-throughput experimental platforms, and more accurate biological models will further enhance our ability to navigate complex biological design spaces, moving ever further beyond the limitations of sequential trial-and-error approaches.
Drug development faces a critical challenge with high attrition rates, often stemming from a failure to demonstrate target engagement in physiologically relevant environments. This whitepaper examines the transformative role of the Cellular Thermal Shift Assay (CETSA) in addressing this challenge. As a label-free method that quantifies drug-target engagement directly in live cells and native tissues, CETSA provides a crucial bridge between in vitro screening and in vivo efficacy. We explore CETSA's mechanistic basis, methodological evolution, and implementation across the drug discovery pipeline, with specific technical guidance, quantitative data summaries, and resource specifications to empower researchers in deploying this critical technology.
The pharmaceutical industry confronts a persistent problem of late-stage clinical failures, where many drug candidates demonstrating promising in vitro activity prove ineffective in complex biological systems. A fundamental contributor to this attrition is the inability to confirm that a compound engages its intended target within the physiologically relevant context of living cells, tissues, or whole organisms [72] [73]. Traditional target engagement methods, such as affinity-based protein profiling, often require chemical modification of ligands, potentially altering their properties and providing misleading data [74].
The introduction of the Cellular Thermal Shift Assay (CETSA) in 2013 marked a paradigm shift by enabling direct, label-free measurement of drug-target engagement in native cellular environments [75] [76]. CETSA exploits the biophysical principle of ligand-induced thermal stabilization, wherein binding of a small molecule to its protein target reduces conformational flexibility, increasing the protein's resistance to heat-induced denaturation [74]. This stabilization is detectable by measuring the amount of soluble, non-denatured protein remaining after heat challenge. Unlike conventional thermal shift assays using purified proteins, CETSA operates within intact cells, preserving native physiology, including protein-protein interactions, post-translational modifications, and cellular compartmentalization [75] [76]. This capability makes CETSA uniquely powerful for verifying that compounds not only bind purified targets but also reach and engage their intended targets in the complex intracellular milieu.
CETSA Mechanistic Principle and Methodological Evolution
Fundamental Biophysical Basis
The core principle underlying CETSA is the thermodynamic stabilization of protein structure upon ligand binding. In their native state, proteins maintain a delicate equilibrium between folded and unfolded conformations. Applied thermal stress disrupts non-covalent bonds (e.g., hydrogen bonds, hydrophobic interactions), shifting this equilibrium toward unfolded states that typically aggregate and precipitate [76]. A ligand binding to its target's native state reduces the entropy of the unfolded system, effectively raising the energy barrier for denaturation. This manifests as an increased thermal stability threshold—a higher temperature is required to denature the ligand-bound protein compared to its unbound form [74] [75]. CETSA detects this stabilization by quantifying the amount of soluble protein surviving heat challenge, providing a direct readout of target engagement.
Evolution of CETSA Methodologies
Since its initial description, CETSA has evolved into a versatile platform with multiple formats tailored to different discovery objectives.
- Western Blot-based CETSA: The original format uses gel electrophoresis and Western blotting with target-specific antibodies to detect stabilized protein. While reliable, it offers low throughput and is limited by antibody availability and quality [74] [75].
- High-Throughput CETSA (CETSA HT): This format utilizes bead-based chemiluminescence or fluorescence detection in plate readers, enabling automation and screening of compound libraries against predefined targets [74] [75].
- Mass Spectrometry-based CETSA (CETSA MS): Also known as Thermal Proteome Profiling (TPP), this method couples the thermal shift principle with quantitative mass spectrometry, enabling unbiased proteome-wide screening for target deconvolution and off-target identification across thousands of proteins simultaneously [74] [75].
- Cellular Thermal Shift Assay with Parallel Imaging (CETSA PI): An emerging format allowing visualization of target engagement at single-cell resolution within complex co-cultures and tissue models [77].
Table 1: Comparison of Primary CETSA Formats
| Format | Detection Method | Primary Application | Throughput | Key Advantage |
|---|---|---|---|---|
| Western Blot CETSA | Gel electrophoresis & antibodies | Target validation | Low | Accessible; specific |
| CETSA HT | Bead-based chemiluminescence/fluorescence | Compound screening | High | Automated; quantitative |
| CETSA MS/TPP | Quantitative mass spectrometry | Target deconvolution, off-target profiling | Medium | Unbiased; proteome-wide |
| BiTSA | Split luciferase complementation | Lead optimization | High | Antibody-free; sensitive |
CETSA Applications Across the Drug Discovery Pipeline
Target Identification and Deconvolution
For compounds emerging from phenotypic screens, CETSA MS enables comprehensive target deconvolution by monitoring thermal stability shifts across the entire proteome. This approach has successfully identified novel targets for natural products and other bioactive molecules without requiring prior knowledge of their mechanism of action [74] [75]. Case studies demonstrate CETSA's effectiveness in uncovering mechanisms of action for various drugs, including the identification of unexpected protein targets that explain both therapeutic and off-target effects [74].
Hit Validation and Lead Optimization
CETSA provides critical data for Structure-Activity Relationship (SAR) studies by quantitatively measuring target engagement directly in cells. The Isothermal Dose-Response Fingerprint (ITDRF) format determines EC50 values—the concentration required for half-maximal stabilization—which often correlates with functional potency [75] [73]. This enables medicinal chemists to prioritize compounds based not only on biochemical potency but also on their ability to engage targets in physiologically relevant environments, a key factor in reducing attrition [77] [75].
Translational Studies and Biomarker Development
CETSA bridges the critical gap between in vitro assays and in vivo models by enabling target engagement validation in native tissues. Seminal work demonstrated quantitative measurement of RIPK1 inhibitor engagement in mouse peripheral blood mononuclear cells, spleen, and brain tissues following in vivo dosing [73]. This application provides unprecedented insight into drug distribution and target occupancy at disease sites, informing dose selection and regimen design for clinical trials. Optimized tissue homogenization protocols now enable TE monitoring in various biospecimens, potentially enabling patient stratification and pharmacodynamic biomarker development [73].
Table 2: Quantitative CETSA Data from RIPK1 Inhibitor Study [73]
| Parameter | Compound 25 | GSK-Compound 27 | Experimental Context |
|---|---|---|---|
| EC50 (ITDRF) | 4.9-5.0 nM | 640-1200 nM | HT-29 cells, 47°C, 8 min |
| 95% CI | 1.0-24 nM / 2.8-9.1 nM | 350-1200 nM / 810-1700 nM | Independent replicates |
| Tissue Engagement | Spleen and brain | Not reported | In vivo mouse model |
| Key Finding | Quantitative TE in CNS | Reversible binding demonstrated | Translational application |
Technical Implementation: Protocols and Reagent Solutions
Core Experimental Workflows
Melt Curve Generation:
- Treat cells with a saturating compound concentration or vehicle control
- Aliquot samples across a temperature gradient (e.g., 37-65°C)
- Heat challenge for 3-10 minutes (optimized per target)
- Lyse cells using freeze-thaw cycles (liquid nitrogen)
- Separate soluble protein via high-speed centrifugation
- Quantify remaining soluble target protein
- Plot percentage soluble protein versus temperature to determine Tm shift [75] [76]
Isothermal Dose-Response (ITDRF):
- Treat cells with serial compound dilutions
- Heat all samples at a single temperature (near Tm from melt curve)
- Process and quantify soluble protein as above
- Plot percentage soluble protein versus compound concentration to derive EC50 [75] [73]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for CETSA Implementation
| Reagent / Material | Function | Implementation Notes |
|---|---|---|
| Takara Dice Gradient PCR | Precise temperature control during heat challenge | Enables multiple temperatures in single 96-well plate [73] |
| High-Speed Refrigerated Centrifuge | Separation of soluble and aggregated protein | Critical for clean background in detection [73] |
| Liquid Handling Automation | Semi-automated washing and processing | Improves reproducibility; enables high-throughput [73] |
| Lysate Preparation Buffer | Maintains protein stability and interactions | Composition critical for lysate CETSA; may require cofactors [75] |
| Heat-Stable Loading Controls | Normalization reference | SOD1, APP-αCTF recommended for high stability [76] |
| Tandem Mass Tag (TMT) Reagents | Multiplexed quantitative proteomics | Enables CETSA MS with 10+ samples simultaneously [75] |
| Split Luciferase Systems (HiBiT/LgBiT) | Antibody-free detection | Enables BiTSA format for engineered cell lines [75] |
Troubleshooting and Methodological Considerations
Addressing Common Experimental Challenges
Successful CETSA implementation requires careful attention to potential pitfalls:
- Irregular Melt Curves: Can result from compound solubility issues, compound-dye interactions (in DSF), or incompatible buffer components. Always inspect raw fluorescence curves and include appropriate controls [76].
- Cell Membrane Permeability: In intact cell CETSA, absence of stabilization may indicate poor compound permeability rather than lack of binding. Parallel lysate CETSA can distinguish these possibilities [76].
- Compound-Mediated Quenching: Some compounds interfere with antibody-based detection, necessitating alternative detection methods or careful antibody selection [73].
- Buffer Considerations: Protein stability varies significantly with buffer composition. Physiological buffers maintain relevant biology, while specialized buffers may be needed for specific protein classes (e.g., kinases requiring ATP) [75] [76].
Quantitative Data Interpretation
A critical advancement in CETSA application is moving beyond qualitative stabilization observations to quantitative interpretation. The measured thermal shift depends not only on binding affinity but also on the thermodynamics of protein unfolding and experimental conditions [77]. Therefore, ITDRF-derived EC50 values provide more reliable potency metrics than melt curve Tm shifts alone. Furthermore, researchers should avoid direct comparison of CETSA data with functional readouts at 37°C without considering the assay's biophysical underpinnings [77].
CETSA represents a paradigm shift in target engagement assessment, directly addressing drug attrition by enabling confirmation of compound-target interactions in physiologically relevant contexts from in vitro models to native human tissues. Its integration into drug discovery pipelines provides critical decision-making data that bridges chemical biology, translational physiology, and clinical development.
Future methodology developments will likely focus on increasing spatial resolution through single-cell CETSA applications, enhancing proteome coverage and depth in CETSA MS, and improving computational frameworks for quantitative data interpretation. As these advancements mature, CETSA's role in de-risking drug discovery and illuminating complex biology will expand, ultimately contributing to more efficient development of therapeutics with validated mechanisms of action.
The development of modern therapeutics presents a critical challenge: the translation of highly potent, mechanism-targeting compounds into clinically beneficial treatments for patients. This challenge has catalyzed a fundamental shift in pharmaceutical research, driving the emergence of integrated, multidisciplinary approaches. The chemical biology platform represents a pivotal organizational strategy designed to optimize drug target identification and validation while improving the safety and efficacy of biopharmaceuticals. This approach achieves these goals through a fundamental emphasis on understanding underlying biological processes and leveraging knowledge gained from the action of similar molecules on these processes [1].
Traditionally, pharmaceutical research operated through disciplinary silos, where chemists, biologists, and clinicians worked sequentially with limited interaction. Chemists focused on synthesizing and scaling potential therapeutic agents, while pharmacologists and biologists used animal models and cellular systems to demonstrate potential therapeutic benefit and develop absorption, distribution, metabolism, and excretion (ADME) profiles. This division often created a significant gap between laboratory success and clinical efficacy, prompting a necessary re-evaluation of drug development strategies [1]. The evolution toward translational physiology and precision medicine has been deeply influenced by the advancement of the chemical biology platform, which connects a series of strategic steps to determine whether a newly developed compound could translate into clinical benefit [1].
Historical Evolution of Interdisciplinary Collaboration
The bridging of disciplines between chemists and pharmacologists marked the first critical step in this evolutionary process. The subsequent introduction of "Clinical Biology" departments in the 1980s, such as the one established at Ciba (now Novartis), was a pioneering effort to formally bridge the gap between preclinical findings and clinical outcomes. This model encouraged collaboration among preclinical physiologists, pharmacologists, and clinical pharmacologists, focusing on identifying human disease models and biomarkers that could more easily demonstrate drug effects before progressing to costly late-stage clinical trials [1].
A foundational framework, based on Koch's postulates, was developed to systematically evaluate potential clinical benefits of new agents. This framework involves four key steps [1]:
- Identify a disease parameter (biomarker)
- Show that the drug modifies that parameter in an animal model
- Show that the drug modifies the parameter in a human disease model
- Demonstrate a dose-dependent clinical benefit that correlates with similar change in direction of the biomarker
This approach enabled more efficient decision-making, allowing for early termination of programs with limited feasibility, such as the Ciba Geigy thromboxane synthase inhibitor CGS 13080, due to pharmacokinetic limitations identified in early-phase studies [1].
Table 1: Evolution of Interdisciplinary Platforms in Drug Discovery
| Era | Dominant Paradigm | Key Features | Limitations |
|---|---|---|---|
| Pre-1960s | Disciplinary Silos | Chemists and pharmacologists worked sequentially; limited interaction [1] | Gap between lab discovery and clinical application |
| 1980s | Clinical Biology | First organized effort to bridge preclinical and clinical research; used biomarkers and human disease models for early go/no-go decisions [1] | Still evolving integration of molecular biology tools |
| 2000s-Present | Chemical Biology Platform | Integrates genomics, combinatorial chemistry, structural biology, high-throughput screening, and cellular assays; multidisciplinary teams working in parallel [1] | Requires significant infrastructure and cultural shift toward team science |
Modern Chemical Biology Platforms and Collaborative Frameworks
The formal development of chemical biology platforms around the year 2000 marked a significant acceleration in collaborative science. This platform emerged to leverage advances in genomics information, combinatorial chemistry, structural biology, high-throughput screening, and genetically manipulable cellular assays [1]. Unlike traditional trial-and-error methods, chemical biology emphasizes targeted selection and integrates systems biology approaches—including transcriptomics, proteomics, metabolomics, and network analyses—to understand complex protein network interactions [1].
Modern collaborative frameworks, as exemplified by centers like the National Center for Advancing Translational Sciences (NCATS), provide specialized resources and expertise to bridge disciplinary gaps. These centers offer access to capabilities that individual research groups often lack, facilitating the entire translational pipeline [78].
Table 2: Key Collaborative Resources and Their Functions in Translational Science
| Resource/Capability | Function in Collaboration | Bridging Discipline(s) |
|---|---|---|
| High-Throughput Screening [78] | Identifies promising compounds that engage novel targets from large chemical libraries | Chemistry & Biology |
| Medicinal Chemistry [78] | Improves compound potency, selectivity, and pharmacokinetic properties to create pharmacological probes | Chemistry & Physiology/Biology |
| 3-D Tissue Bioprinting [78] | Creates tissue models that mimic organization and physiology of living organisms for drug screening | Biology, Engineering & Clinical Science |
| Stem Cell Translation Laboratory [78] | Provides human cell models for testing compound efficacy and toxicity using induced pluripotent stem cells | Biology & Clinical Medicine |
| Functional Genomics Lab [78] | Uses CRISPR and other technologies to validate novel drug targets and understand disease mechanisms | Biology, Chemistry & Clinical Science |
| Late-Stage Preclinical Development [78] | Advances promising therapeutic agents through IND-enabling studies toward clinical testing | Biology, Chemistry & Clinical Medicine |
The core facility model represents another powerful approach for fostering collaboration. As demonstrated by Professor Hening Lin's work at the University of Chicago, centralized facilities provide services for researchers lacking specialized resources to develop drug molecules, purifying proteins, understanding how different molecules bind to them, and designing, building, and testing the right compounds to manipulate their function [79]. Such facilities can dramatically accelerate the typically lengthy process of probe development from 2-3 years to less than six months, effectively promoting collaboration among clinical scientists, biologists, chemists, and engineers [79].
Figure 1: Collaborative Workflow in Modern Drug Discovery. This diagram illustrates the bidirectional flow of information and materials between basic scientists, chemical biology platforms, and clinicians, highlighting the iterative nature of modern therapeutic development.
Practical Methodologies for Effective Collaboration
Integrated Target Validation and Lead Optimization
A critical methodology for effective collaboration involves integrating knowledge across disciplines throughout the target validation and lead optimization process. This begins with biologists and clinicians identifying disease mechanisms and potential therapeutic targets, often through genetic approaches like knockout organisms that help determine gene function and relevance to disease phenotypes [80]. Once a target is identified, multidisciplinary teams employ parallel processes to accelerate development.
The workflow typically involves [1] [78]:
- Target Identification and Validation: Using functional genomics tools (e.g., CRISPR), cellular assays, and animal models to establish the target's role in disease.
- Assay Development and High-Throughput Screening: Developing robust biological assays compatible with automation and large-scale compound screening.
- Hit-to-Lead Optimization: Medicinal chemists design and synthesize analogs to improve potency and selectivity, while biologists assess functional effects in relevant cellular and animal models.
- Pharmacokinetic/Pharmacodynamic (PK/PD) Studies: Evaluating compound absorption, distribution, metabolism, excretion, and target engagement in physiological systems.
- Proof-of-Concept Studies in Disease Models: Testing optimized leads in clinically relevant models, including 3D tissue cultures, organoids, or animal models that recapitulate human disease.
Figure 2: The Four-Step Framework for Translational Validation. This workflow, adapted from Koch's postulates, provides a systematic approach for correlating biomarker modification with clinical benefit across model systems.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Collaborative Research
| Reagent/Platform | Function | Application in Collaboration |
|---|---|---|
| Chemical Libraries [1] | Collections of diverse small molecules for screening | Used by biologists to identify chemical probes; provides starting points for chemists |
| Pharmacological Probes [78] [79] | Optimized small molecules with defined potency and selectivity against specific targets | Enable biologists to modulate specific targets; used by clinicians to validate targets in disease models |
| Reporter Gene Assays [1] | Cellular systems that produce measurable signals upon pathway activation | Allow biologists and chemists to quantitatively assess compound effects on signaling pathways |
| Induced Pluripotent Stem Cells (iPSCs) [78] | Patient-derived cells that can be differentiated into relevant cell types | Provide clinicians and biologists with human-specific models; bridge genetic insights to cellular phenotypes |
| Voltage-Sensitive Dyes/Patch-Clamp [1] | Technologies for measuring ion channel activity | Enable neuroscientists and cardiologists to assess compound effects on electrophysiology |
| Proteomics/Transcriptomics Platforms [1] | Tools for comprehensive protein and gene expression analysis | Generate multidimensional data for biologists and chemists to understand compound mechanisms |
Case Studies in Successful Cross-Disciplinary Collaboration
Enzyme Research Translating to Therapeutic Candidates
The research on sirtuins, a group of enzymes involved in aging, metabolism, and inflammation, exemplifies successful cross-disciplinary collaboration. Basic scientific discovery revealed that these seven human enzymes do not all work the same way, with some removing completely different modifications from proteins [79]. This fundamental biological insight prompted chemists to develop small molecules that could selectively turn off different sirtuin enzymes, leading to the discovery of compounds with promising anti-cancer effects [79]. Further biological investigation revealed that inhibiting one of these enzymes also suppresses inflammation, opening potential applications for treating conditions like inflammatory bowel disease [79]. This progression from basic enzyme characterization to therapeutic candidate development demonstrates the power of integrating chemical and biological expertise.
Academic-Industrial Collaboration in Kidney Disease
The development of novel kidney disease treatments further illustrates effective collaboration. Clinical observations of patients with progressive kidney disease, particularly the frustration of limited treatment options, drove basic research into disease mechanisms [80]. This research identified how lipids contribute to kidney fibrosis, leading to the discovery of two drug candidates designed to reduce trapped lipids in kidney tissue [80]. One of these drugs, a sugar molecule called VAR 200, has been licensed by a biotechnology company and found safe in early trials, demonstrating potential to slow kidney disease progression [80]. This case highlights how clinician scientists can "close the loop" by bringing patient insights to the bench and developing new therapeutic approaches through integrated research.
Organizational Strategies and Best Practices
Fostering effective collaboration requires intentional organizational strategies that extend beyond scientific methodologies. Successful approaches include:
Co-Location and Shared Infrastructure: Physical proximity of chemistry, biology, and clinical facilities, as highlighted by Professor Lin's emphasis on having a top-ranked cancer program, medical school, and chemistry department within walking distance [79].
Dedicated Translational Cores: Establishing central facilities with specialized expertise and equipment that multiple research groups can access, such as the chemical biology and therapeutics core described previously [78] [79].
Integrated Training Programs: Developing educational initiatives that cross traditional disciplinary boundaries, such as the Medical Scientist Training Program (MSTP) that helps physician trainees combine medicine and research [80].
Academic Freedom with Strategic Direction: Allowing researchers the flexibility to pursue unexpected scientific leads while providing overarching strategic direction and resources in high-impact areas like neuroscience and aging [80].
Team Science Recognition: Creating promotion and tenure policies that value collaborative contributions alongside individual achievements, supported by administrative efforts to help researchers with career advancement and mentorship skills [80].
These strategies collectively create an ecosystem where interdisciplinary collaboration can flourish, accelerating the translation of basic discoveries into clinical applications that benefit patients.
The development of novel therapeutics presents a formidable challenge: the transition from identifying highly potent compounds to definitively demonstrating clinical benefit. This challenge has catalyzed the emergence of the chemical biology platform, an organizational approach designed to optimize drug target identification and validation, thereby improving the safety and efficacy of biopharmaceuticals [1]. At its core, this platform uses a multidisciplinary team to accumulate knowledge and solve problems, often relying on parallel processes to reduce the time and cost of bringing new drugs to patients [1]. A critical component of this platform is translational physiology, which examines biological functions across levels spanning from molecules to cells to organs to populations [1].
The integration of these disciplines creates a data-rich environment. However, the sheer volume and complexity of the data generated from modern techniques—including proteomics, metabolomics, and transcriptomics—can overwhelm traditional, siloed decision-making processes. This whitepaper outlines a framework for structuring these data streams into integrated workflows. By implementing systematic data collection and analysis protocols, research organizations can establish a robust foundation for confident, evidence-based Go/No-Go decisions throughout the drug development pipeline, from target identification to clinical proof-of-concept.
The Evolution of Decision-Making in Drug Development
The historical context of drug development reveals a necessary evolution toward more rigorous decision-making. The Kefauver-Harris Amendment of 1962 mandated proof of efficacy from adequate and well-controlled clinical trials, formally dividing Phase II into two distinct components: Phase IIa for finding a potential disease in which the drug would work, and Phase IIb/Phase III for demonstrating statistical proof of efficacy and safety [1]. This regulatory change highlighted the need for clearer, earlier indicators of potential success.
A pivotal advancement was the introduction of the Clinical Biology department, an early organized effort focused on translational physiology [1]. This approach, pioneered by companies like Ciba (now Novartis), was built on a four-step postulate to indicate potential clinical benefit [1]:
- Identify a disease parameter (biomarker).
- Show that the drug modifies that parameter in an animal model.
- Show that the drug modifies the parameter in a human disease model.
- Demonstrate a dose-dependent clinical benefit that correlates with a similar change in the direction of the biomarker.
This methodology emphasized early feasibility testing, allowing for the timely termination of programs with insurmountable obstacles, such as the Ciba Geigy thromboxane synthase inhibitor CGS 13080, which had a prohibitively short half-life [1]. The modern chemical biology platform, developed to leverage genomics, combinatorial chemistry, and high-throughput screening, is the direct descendant of this approach, providing the tools to generate the data necessary for these critical assessments [1].
Framework for a Data-Rich Workflow
A streamlined, data-rich pipeline integrates continuous data generation with structured decision points. The entire process, from target identification to clinical proof-of-concept, can be visualized as an integrated workflow with clear off-ramps for unpromising candidates.
The following diagram outlines the key stages and decision gates in this streamlined pipeline:
Key Decision Gates and Data Requirements
Each decision gate in the workflow relies on specific, quantitative data packages. The following table summarizes the core data requirements at each stage to inform a confident Go/No-Go call.
Table 1: Data Requirements for Key Go/No-Go Decision Gates
| Decision Gate | Primary Data Inputs | Quantitative Metrics for "Go" Decision |
|---|---|---|
| Go/No-Go 1:Target Validation & Biomarker Identification | - Genomic/proteomic data- High-content cellular assay data (viability, apoptosis, protein translocation) [1]- Reporter gene assays [1] | - Potency (IC50/EC50) in relevant cellular model- Biomarker modulation correlates with functional effect- High-confidence target-bioactivity link |
| Go/No-Go 2:Lead Efficacy & Safety | - Animal model efficacy data (e.g., SHR rat, tail-flick test) [1]- ADME-Tox profiles [1]- Multiparametric in vivo safety pharmacology | - Significant efficacy vs. control (p<0.05)- Acceptable therapeutic index- Favorable preliminary PK/PD profile |
| Go/No-Go 3:Clinical Proof-of-Concept | - Phase IIa human disease model data- Biomarker modulation in human subjects- Early clinical safety and tolerability | - Dose-dependent biomarker modulation- Statistically significant signal of clinical benefit- Positive benefit-risk profile in target population |
Experimental Protocols for Core Workflows
The following section provides detailed methodologies for key experiments that generate critical data for the decision gates outlined above.
Protocol: High-Content Multiparametric Cellular Assay for Target Validation
This protocol is designed to assess compound effects on multiple cellular phenotypes simultaneously, providing a rich dataset for early target validation and prioritization [1].
- Objective: To quantify the effects of lead compounds on cell viability, apoptosis, cell cycle distribution, and protein translocation in a single, automated assay.
- Materials:
- Cell line expressing the target of interest (e.g., engineered with a fluorescent tag for localization studies).
- Automated microscopy system with environmental control.
- Image analysis software capable of multiparametric quantification (e.g., CellProfiler or commercial equivalents).
- Fluorescent dyes: Hoechst 33342 (nuclei), Annexin V-FITC (apoptosis), MitoTracker Red (mitochondria), and antibodies for target protein immunofluorescence.
- Methodology:
- Cell Seeding & Treatment: Seed cells in 96-well or 384-well imaging plates. After 24 hours, treat with a dose-response range of test compounds (e.g., 0.1 nM - 10 µM), including positive and negative controls.
- Staining: At the assay endpoint (e.g., 24, 48, 72 hours), incubate cells with the panel of fluorescent dyes and antibodies according to established protocols.
- Image Acquisition: Using an automated microscope, acquire high-resolution images from multiple sites per well across all fluorescent channels.
- Image Analysis: Use the analysis software to identify cells and measure parameters including:
- Cell Count & Nuclear Morphology (from Hoechst channel) for viability and cell cycle analysis.
- Annexin V Intensity for apoptosis quantification.
- Fluorescent Protein Co-localization (e.g., target protein translocation from cytoplasm to nucleus).
- Data Analysis: Calculate Z-scores for each parameter relative to controls. Employ multivariate analysis (e.g., Principal Component Analysis) to cluster compound effects and identify promising leads based on their multiparametric profile.
Protocol: Establishing a Translational Physiology Bridge Using Biomarker Modulation
This protocol describes the critical step of demonstrating target engagement and biomarker modulation in a human disease model, a cornerstone of the Clinical Biology approach [1].
- Objective: To demonstrate that a drug candidate modifies a predefined disease biomarker in a validated human disease model, establishing a bridge between preclinical findings and potential clinical benefit.
- Materials:
- Validated human disease model (e.g., primary cell cultures, tissue biopsies, or well-characterized patient-derived xenografts).
- Specific and sensitive analytical method for biomarker quantification (e.g., ELISA, LC-MS/MS, immunoblotting) [1].
- The lead compound and appropriate vehicle control.
- Methodology:
- Model Characterization: Confirm that the human disease model expresses the biomarker of interest at a level that is dysregulated compared to healthy controls and is clinically relevant.
- Dosing Regimen: Treat the model with the lead compound across a range of doses predicted from preclinical PK/PD studies. Include a vehicle control and a standard-of-care control if available.
- Sample Collection: Collect samples (e.g., culture supernatant, tissue lysate) at multiple time points post-treatment to assess the kinetics of biomarker modulation.
- Biomarker Quantification: Analyze samples in a blinded manner using the validated analytical method. All samples from a single experiment should be run in the same assay to minimize inter-assay variability.
- Data Analysis:
- Determine the dose- and time-dependence of biomarker modulation.
- Establish the relationship between the extent of biomarker change and any concomitant functional or phenotypic readout in the model.
- The outcome of this experiment directly feeds into "Go/No-Go Decision 3", providing crucial evidence for proceeding to larger Phase IIb/III trials [1].
The Scientist's Toolkit: Essential Research Reagent Solutions
The execution of robust, data-rich workflows depends on high-quality, well-characterized reagents. The following table details key materials and their applications in the chemical biology platform.
Table 2: Key Research Reagent Solutions for Data-Rich Drug Discovery
| Reagent / Tool | Function / Application | Key Characteristics |
|---|---|---|
| Voltage-Sensitive Dyes | Screening ion channel activity for neurological and cardiovascular drug targets [1]. | Fast response kinetics, compatibility with high-throughput plate readers. |
| Reporter Gene Constructs | Assessing signal activation in response to ligand-receptor engagement (e.g., GPCR signaling) [1]. | Sensitive, amplifiable signal (e.g., luciferase), minimal background. |
| Genetic Code Expansion Systems | Enabling the incorporation of unnatural amino acids into proteins for novel functionality, such as creating antibody-protein conjugates [81]. | High fidelity, orthogonal tRNA/synthetase pairs, efficient in mammalian cells. |
| Activity-Based Protein Profiling (ABPP) Probes | Identifying and monitoring the functional state of enzyme families directly in complex biological systems. | Target-directed chemical structures with reporter tags (e.g., biotin, fluorophores). |
| Photoproximity Labeling Agents (e.g., µMap) | Mapping micro-scale proximity interactions for integrated phenotypic screening and target identification [81]. | Spatially restricted activation (e.g., via light), cleavable tags for purification. |
Visualizing Data Integration and the Decision Logic
The power of a data-rich workflow is fully realized only when disparate data streams are integrated into a unified view for decision-makers. The logic of synthesizing this information can be visualized as a flow from raw data to a strategic decision.
The following diagram illustrates the pathway from data generation to a final Go/No-Go decision, emphasizing the role of automated data consolidation and confidence scoring:
The integration of the chemical biology platform with structured, data-rich workflows represents a mature evolution in pharmaceutical research and development. By systematically applying the principles of translational physiology—building bridges from molecular findings to population-level outcomes—and leveraging the experimental protocols and tools outlined herein, organizations can transform decision-making from a reactive, siloed process into a proactive, evidence-driven strategy. This approach ensures that resources are channeled toward the most promising therapeutic candidates, ultimately accelerating the delivery of effective treatments to patients.
Establishing Efficacy: Validation Frameworks and Platform Impact
Within the modern drug development landscape, the chemical biology platform serves as a critical organizational strategy for optimizing drug target identification and validation. This whitepaper details the foundational four-step framework developed within Clinical Biology—a discipline designed to bridge preclinical research and clinical outcomes. We articulate a rigorous, mechanism-based approach for demonstrating clinical benefit, rooted in translational physiology. The document provides explicit methodologies for each step, supported by quantitative data tables, experimental protocols, and visual workflows, offering researchers and drug development professionals a structured pathway for transitioning from basic discovery to proof of concept in humans.
The challenge of translating potent, target-specific compounds into therapies with proven clinical benefit has long been a bottleneck in pharmaceutical research [1]. This challenge catalyzed the development of translational physiology and the formalization of the chemical biology platform, which uses small molecules and systems biology approaches to study and modulate biological systems [1]. A pivotal development in this evolution was the establishment of Clinical Biology departments within the industry, with the explicit goal of bridging the gap between preclinical findings and clinical outcomes [1].
Clinical Biology emerged as a strategic response to the Kefauver-Harris Amendment of 1962, which mandated proof of efficacy from adequate and well-controlled clinical trials [1]. It represents the first organized effort in the industry to focus on translational physiology, fostering collaboration among preclinical physiologists, pharmacologists, and clinical pharmacologists [1]. Its primary operational unit is a four-step framework, based on Koch's postulates, which provides a disciplined methodology for determining a new agent's potential for clinical success before committing to costly late-phase trials [1]. This framework ensures that decisions are grounded in a mechanistic understanding of both the drug and the disease, thereby de-risking the drug development process.
The Four-Step Framework: A Detailed Breakdown
The four-step framework provides a logical sequence for establishing a causal relationship between a drug's pharmacological activity and a meaningful clinical outcome [1]. The following table summarizes the core objectives and outputs for each step.
Table 1: The Clinical Biology Four-Step Framework for Demonstrating Benefit
| Step | Core Objective | Key Outputs & Decision Points |
|---|---|---|
| 1. Identify a Disease Parameter | To identify and validate a measurable biomarker that is intrinsically linked to the disease process. | - A quantified baseline of the biomarker in the target patient population.- Evidence establishing the biomarker's role in the disease pathophysiology. |
| 2. Modify Parameter in Animal Model | To demonstrate that the drug candidate effectively modulates the identified biomarker in a relevant animal model of the human disease. | - Pharmacodynamic (PD) data showing biomarker modulation.- Preliminary pharmacokinetic (PK) and dose-response relationship. |
| 3. Modify Parameter in Human Disease Model | To confirm that the drug modulates the biomarker in a controlled human model of the disease. | - Proof of mechanism in humans.- Data linking drug exposure to biomarker response.- Early signal of potential efficacy. |
| 4. Demonstrate Dose-Dependent Clinical Benefit | To establish a direct correlation between the degree of biomarker modulation and a meaningful, dose-dependent clinical improvement. | - Evidence for a exposure-response-efficacy relationship.- Robust rationale for proceeding to large-scale Phase IIb/III trials. |
Step 1: Identify a Disease Parameter (Biomarker)
The foundation of the framework is the identification of a quantifiable biomarker—a biological parameter that serves as a surrogate for a clinical endpoint of the disease.
- Methodology: The process begins with a comprehensive analysis of the disease pathophysiology. Researchers employ systems biology techniques—including proteomics, metabolomics, and transcriptomics—to identify and validate key molecular or physiological players [1]. The biomarker must be objectively measurable and exhibit a plausible, direct connection to the disease state.
- Protocol Details:
- Target Identification: Utilize high-content multiparametric analysis (e.g., automated microscopy) and genomic/proteomic databases to pinpoint potential targets [1].
- Assay Development: Develop robust in vitro assays (e.g., reporter gene assays, immunoblotting for protein quantification) to measure the biomarker [1].
- Validation: Establish the biomarker's baseline and variability in both healthy and diseased states using patient-derived samples or well-characterized cellular models.
Step 2: Show Drug Modifies Parameter in an Animal Model
This step transitions to demonstrating pharmacological activity in a complex, living system that replicates aspects of the human disease.
- Methodology: A relevant animal model is selected based on its ability to recapitulate both the biomarker and core clinical symptoms of the human condition [1]. The drug candidate is administered, and its effect on the biomarker is rigorously quantified.
- Protocol Details:
- Model Selection: Choose an established model (e.g., spontaneously hypertensive rat for hypertension) [1].
- Dosing and PK/PD Analysis: Administer a range of doses to establish a PK/PD relationship. Collect biological samples (e.g., blood, tissue) at multiple time points.
- Biomarker Analysis: Quantify biomarker levels using the assays developed in Step 1 (e.g., ELISA, mass spectrometry, functional enzymatic assays).
- Safety Monitoring: Conduct parallel toxicology studies to assess initial safety and define a therapeutic index.
Step 3: Show Drug Modifies Parameter in a Human Disease Model
This critical step provides the first evidence of activity in humans, moving from animal physiology to human translational physiology.
- Methodology: A human model of disease is identified. This model must possess the biomarker of interest and clinically relevant symptoms that can be easily monitored [1]. A small-scale, early-phase (Phase I or IIa) clinical study is conducted in a select patient population.
- Protocol Details:
- Study Design: Typically a small, open-label or single-blind proof-of-concept study.
- Participant Selection: Enroll a limited number of patients (dozens up to 100) with the well-defined disease and measurable biomarker levels [82].
- Intervention and Monitoring: Administer the drug and monitor biomarker response alongside clinical symptoms and safety parameters.
- Data Analysis: Evaluate the correlation between drug exposure, biomarker modulation, and any preliminary clinical signals.
Step 4: Demonstrate Dose-Dependent Clinical Benefit
The final step establishes the ultimate value of the drug by linking biomarker modulation to a tangible, dose-dependent improvement in patient health.
- Methodology: A larger, well-controlled clinical study (Phase IIb) is designed to specifically test for a correlation between the magnitude of biomarker change and the degree of clinical benefit [1]. The presence of a dose-response relationship is considered strong evidence of a true treatment effect.
- Protocol Details:
- Study Design: A randomized, controlled, and often double-blind trial comparing multiple doses of the drug against a placebo or standard of care.
- Endpoint Selection: Define a primary clinical efficacy endpoint (e.g., progression-free survival in oncology [83]) alongside continued biomarker measurement.
- Statistical Analysis: Pre-specify and test for a correlation between the level of biomarker modulation and the clinical outcome across different dose groups.
The logical progression and key decision points of this framework are visualized in the workflow below.
Quantitative Data and Trial Diversity in the Framework
The application of this framework generates critical quantitative data that informs go/no-go decisions. A key consideration in later stages is the diversity of clinical trial populations, which ensures the findings are broadly applicable. The following table synthesizes key quantitative aspects of clinical trial phases and a modern framework for evaluating diversity.
Table 2: Quantitative Benchmarks in Clinical Development and Diversity Assessment
| Parameter | Phase I (Early Clinical) | Phase II (Proof of Concept) | Phase III (Confirmation) | Diversity Rating (CDR Framework) |
|---|---|---|---|---|
| Typical Sample Size | 20-80 participants [82] | Dozens to 300 participants [82] | Hundreds to thousands of participants [82] | N/A |
| Primary Focus | Safety, Metabolism, Dosage [82] | Preliminary Efficacy, Short-term Side Effects [82] | Safety, Efficacy, Dosage Ranges [82] | Representativeness of Race, Sex, Age [84] |
| Typical Success Rate | ~70% pass [82] | ~33% pass [82] | 25-30% pass [82] | N/A |
| Key Benchmark | Maximum Tolerated Dose | Signal of Efficacy vs. Placebo/Standard of Care | Statistical Proof of Superiority/Efficacy | Comparison to Disease Prevalence in Population [84] |
The Clinical trial Diversity Rating (CDR) framework is a modern tool that aligns with the principles of rigorous clinical evaluation promoted by the four-step model. It provides an objective method to evaluate the representation of race/ethnicity, sex, and age in clinical trials against disease prevalence benchmarks, enhancing the generalizability and equity of research outcomes [84].
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing the four-step framework requires a suite of specialized reagents and tools. The following table details key materials essential for the experiments cited in this field.
Table 3: Essential Research Reagents for Clinical Biology Studies
| Reagent / Tool | Core Function | Application in the Framework |
|---|---|---|
| High-Content Screening (HCS) Assays | Multiparametric analysis of cellular events (viability, apoptosis, protein translocation) via automated microscopy [1]. | Step 1: Target and biomarker identification and validation in cellular models. |
| Reporter Gene Assays | Measure signal activation downstream of specific targets (e.g., ligand-receptor engagement) [1]. | Step 1: Functional validation of biomarker engagement and pathway modulation. |
| Animal Disease Models | In vivo systems (e.g., spontaneously hypertensive rat) that replicate human disease pathology [1]. | Step 2: Testing drug efficacy and biomarker modulation in a complex physiological context. |
| Immunoblotting (Western Blot) | Relative quantitation of specific protein abundance in complex biological samples [1]. | Steps 1 & 2: Measuring biomarker (protein) levels in cell lysates and animal tissues. |
| Combinatorial Chemistry Libraries | Large collections of diverse small molecules for high-throughput screening [1]. | Foundational: Provides the chemical starting points (leads) for the entire framework. |
| Voltage-Sensitive Dyes / Patch-Clamp | Functional screening of ion channel activity for neurological and cardiovascular targets [1]. | Step 1: Identifying and characterizing electrophysiological biomarkers. |
The four-step Clinical Biology framework is not an isolated process; it is the operational engine embedded within the broader chemical biology platform. This platform integrates multidisciplinary teams that leverage knowledge from chemical tools, systems biology, and structural biology to accumulate knowledge and solve problems in parallel, thereby accelerating the timeline from discovery to clinic [1]. The framework provides the critical "go/no-go" milestones for this platform, ensuring that only compounds with a clear, mechanism-based rationale and early evidence of human activity advance.
In conclusion, the four-step framework for demonstrating benefit is a pillar of translational physiology and modern precision medicine. By providing a disciplined, hypothesis-driven approach that moves sequentially from biomarker identification to dose-dependent clinical benefit, it introduces rigor and reproducibility into the high-stakes process of drug development [83] [1]. This framework empowers researchers to make data-driven decisions, ultimately increasing the likelihood of delivering safe and effective therapies to patients.
Within modern drug discovery, the integration of sophisticated chemical biology platforms with translational physiology research represents a paradigm shift towards data-driven decision-making. These platforms are pivotal for enhancing the efficiency of the discovery pipeline and reducing the high rates of compound attrition, particularly in the late, costly clinical stages. This whitepaper provides an in-depth technical analysis of how such platforms deliver measurable impact. We present quantitative case studies and detailed methodologies focused on applying Quantitative In Vitro to In Vivo Extrapolation (QIVIVE) and advanced Quantitative Structure-Activity Relationship (QSAR) modeling. These approaches are critical for translating in vitro bioactivity into predictive in vivo models, thereby de-risking the selection of chemical probes and drug candidates and objectively assessing their utility [85] [86] [2].
Core Platform Components and Impact Framework
A chemical biology platform designed for impact measurement is built upon several integrated, quantitative components. The synergy between these components creates a feedback loop that continuously refines predictions and improves decision-making.
Table 1: Core Components of an Integrated Chemical Biology Platform
| Platform Component | Primary Function | Key Impact Metric |
|---|---|---|
| In Vitro Mass Balance Modeling | Predicts free, biologically effective concentrations in assay media from nominal concentrations by accounting for distribution to lipids, proteins, and labware [85]. | Increased accuracy of in vitro to in vivo concordance. |
| Quantitative In Vitro to In Vivo Extrapolation (QIVIVE) | Uses in vitro bioactivity data and physiologically based kinetic (PBK) modeling to predict equivalent in vivo doses via reverse dosimetry [85]. | Reduction in false positive/negative predictions in early discovery. |
| QSAR for Virtual Screening | Predicts the bioactivity of new chemicals from structural data to enable the prioritization of compounds for experimental testing [86]. | Positive Predictive Value (PPV) and enrichment of true actives in top-ranked compounds. |
| Objective Chemical Probe Assessment | Provides a data-driven, quantitative scoring system to evaluate the suitability of chemical tools for target validation and biological research [2]. | Confident and standardized selection of high-quality chemical probes. |
The logical workflow of these components, from assay design to candidate nomination, is outlined below.
Diagram 1: Integrated platform workflow for efficiency and attrition reduction.
Case Study 1: Enhancing Predictive Accuracy with QIVIVE
Background and Protocol
A significant challenge in utilizing in vitro high-throughput screening (HTS) data is the discrepancy between the reported nominal concentration (total mass added to the medium) and the free concentration actually available for cellular uptake and effect [85]. This difference, caused by partitioning to media proteins, lipids, and labware plastic, leads to inaccurate in vitro to in vivo extrapolations. QIVIVE addresses this by using in vitro mass balance models to predict free concentrations, which are then used in physiologically based kinetic (PBK) modeling for reverse dosimetry [85].
Detailed Experimental Protocol: QIVIVE for In Vitro to In Vivo Concordance
- Input Parameter Collection: For the test chemical, gather key parameters: Molecular Weight (MW), octanol-water partition coefficient (KOW), acid dissociation constant (pKa), and solubility. Cell-related parameters (e.g., cell count, lipid volume) and media-related parameters (e.g., protein concentration) are also essential [85].
- Model Selection and Application: Apply one or more mass balance models (e.g., Armitage, Fischer). The Armitage model is often recommended as a first-line approach as it accounts for media, cells, labware, headspace, and media solubility, and is applicable to a broad range of chemicals [85].
- Prediction of Free Concentration: The model uses the nominal concentration and collected parameters to calculate the freely dissolved concentration in the assay media.
- Reverse Dosimetry: The predicted free media concentration is used as a target in vivo free plasma concentration. A PBK model then works in reverse to calculate the equivalent external in vivo dose that would produce this target plasma concentration.
- Concordance Analysis: Compare the in vivo points of departure (PODs) derived from this QIVIVE approach with regulatory in vivo PODs to assess the improvement in prediction accuracy.
Quantitative Impact and Results
A comparative analysis of four mass balance models evaluated their performance in predicting free media and cellular concentrations for a wide range of chemicals and test systems [85]. The findings are summarized in the table below.
Table 2: Performance Comparison of In Vitro Mass Balance Models for QIVIVE [85]
| Model Name | Key Features | Chemical Applicability | Overall Performance |
|---|---|---|---|
| Armitage et al. | Considers media, cells, labware, headspace, and media solubility. | Neutral and Ionizable Organic Chemicals | Slightly better performance overall; recommended as a first-line approach. |
| Fischer et al. | Considers media and cell compartments only. | Neutral and Ionizable Organic Chemicals | Simpler structure but may lack accuracy due to omitted compartments. |
| Fisher et al. | Includes media, cells, labware, headspace, and cellular metabolism. | Neutral and Ionizable Organic Chemicals | Time-dependent simulation; performance varies. |
| Zaldivar-Comenges et al. | Accounts for abiotic degradation and cell number variation. | Neutral Chemicals Only | Limited by applicability only to neutral chemicals. |
The study found that predictions of media concentrations were consistently more accurate than those for cellular concentrations [85]. Sensitivity analysis revealed that chemical property-related parameters (e.g., KOW) were the most influential for predicting media concentrations, while cell-related parameters were also critical for cellular predictions. When applied to a dataset of 15 chemicals, incorporating these in vitro bioavailability adjustments resulted in modest but valuable improvements to in vitro-in vivo concordance, directly contributing to attrition reduction by making early predictions more reliable [85].
Case Study 2: Revolutionizing Virtual Screening with PPV-Driven QSAR
Background and Protocol
The traditional paradigm for building binary classification QSAR models has prioritized Balanced Accuracy (BA), often achieved by balancing training datasets through down-sampling. This practice is ideal for lead optimization where the goal is to equally well-predict active and inactive compounds across an entire set [86]. However, for virtual screening of modern ultra-large chemical libraries (containing billions of compounds), the operational constraint is different: only a small, fixed number of top-ranked compounds (e.g., 128 for a single 1536-well plate) can be tested experimentally. In this context, the critical metric is Positive Predictive Value (PPV), or precision—the proportion of true actives among those predicted as active [86].
Detailed Experimental Protocol: Building a PPV-Optimized QSAR Model
- Dataset Curation: Collect a large HTS dataset, which is typically highly imbalanced (skewed heavily towards inactive compounds). Do not balance this dataset.
- Model Training: Train a binary classification QSAR model (e.g., using machine learning algorithms like Random Forest or Naive Bayes) directly on the imbalanced dataset.
- Model Validation and Selection: Instead of selecting the model with the highest Balanced Accuracy, select the model that demonstrates the highest PPV when applied to a held-out validation set. Critically, the PPV should be calculated specifically for the top N predictions (e.g., top 128), reflecting the real-world experimental throughput.
- Virtual Screening and Hit Nomination: Use the selected model to screen an ultra-large library. Rank all predicted actives by their prediction confidence and select the top N compounds (e.g., 128) for experimental validation.
Quantitative Impact and Results
A proof-of-concept study built QSAR models for five expansive HTS datasets, comparing the performance of models trained on balanced versus imbalanced datasets [86]. The results compellingly argue for a paradigm shift.
Table 3: Balanced vs. Imbalanced QSAR Models for Virtual Screening [86]
| Model Characteristic | Traditional Balanced Model | PPV-Optimized Imbalanced Model | Impact on Screening |
|---|---|---|---|
| Training Set | Artificially balanced 50:50 active:inactive ratio. | Original, imbalanced ratio (e.g., <1% actives). | Imbalanced models reflect the true distribution of chemical space. |
| Primary Selection Metric | Balanced Accuracy (BA). | Positive Predictive Value (PPV) in top N. | PPV directly measures the expected experimental hit rate. |
| Hit Rate in Top 128 | Lower hit rate (Baseline for comparison). | At least 30% higher hit rate than balanced models. | Dramatically increases efficiency and reduces cost per true active. |
| Utility | Best for lead optimization on small, focused sets. | Essential for hit identification from ultra-large libraries. | Aligns computational strategy with the practical experimental workflow. |
This study demonstrated that models trained on imbalanced datasets and selected for high PPV achieved a hit rate at least 30% higher than models using the traditional balanced approach [86]. This represents a direct and substantial increase in platform efficiency, ensuring that valuable experimental resources are devoted to testing compounds with a much higher probability of success.
The Scientist's Toolkit: Essential Research Reagent Solutions
The experimental protocols and case studies described rely on a foundation of specific reagents and materials. The following table details key solutions used in these advanced assessments.
Table 4: Essential Research Reagents for Chemical Biology and Translational Assessment
| Research Reagent | Technical Function | Application Context |
|---|---|---|
| High-Throughput Screening (HTS) Assays | Cell-based or biochemical assays configured in multi-well plates (e.g., 384, 1536-well) to generate dose-response data for thousands of compounds. | Generation of initial in vitro bioactivity data (nominal concentrations) for QIVIVE and QSAR modeling [85] [86]. |
| Ionizable and Neutral Organic Chemicals | Diverse chemical libraries with measured properties (logP, pKa, solubility) used for model training and validation. | Critical for developing and testing the applicability of mass balance and QSAR models across chemical space [85]. |
| Cell Culture Media with Defined Serum/Protein | Media with characterized concentrations of binding proteins like Bovine Serum Albumin (BSA). | Enables accurate modeling of chemical distribution in the media compartment; proprietary media can be a limiting factor [85]. |
| Induced Pluripotent Stem Cells (iPSCs) | Differentiated into relevant tissue-specific cells (e.g., hepatocytes, neurons) for more physiologically relevant in vitro assays. | Provides a human-relevant, translatable cell source for HTS, improving the biological relevance of the free concentration predictions [85]. |
| Public Bioactivity Databases (ChEMBL, PubChem) | Large-scale, curated repositories of chemical structures and associated bioactivity data. | Primary source for building robust, imbalanced training sets for PPV-optimized QSAR models [86]. |
| Objective Probe Assessment Resource (Probe Miner) | A data-driven resource that quantitatively scores compounds for their suitability as chemical probes based on public medicinal chemistry data. | Used alongside expert curation to select high-quality chemical tools for target validation, reducing the risk of using poor probes [2]. |
The integration of QIVIVE and PPV-driven QSAR modeling within a chemical biology platform provides a formidable strategy for measuring and improving efficiency while reducing attrition. By shifting from nominal to free concentration via mass balance models, researchers achieve a more physiologically relevant basis for predicting in vivo effects. By prioritizing Positive Predictive Value over Balanced Accuracy in virtual screening, research platforms align computational outputs with the practical constraints of experimental follow-up, dramatically increasing the yield of true actives. Together, these data-driven approaches enable translational physiology research to make more confident, quantitative decisions earlier in the drug discovery process, ultimately leading to a more efficient and successful pipeline.
The pharmaceutical research and development landscape is defined by a fundamental dichotomy between two distinct operational philosophies: the established, linear pathway of traditional drug discovery and the integrative, mechanism-oriented approach of the chemical biology platform. Traditional drug discovery, characterized by its sequential, target-centric, and often empirical nature, has long been the industry standard. In contrast, chemical biology represents a paradigm shift toward a multidisciplinary, knowledge-driven framework that strategically leverages small molecules as probes to elucidate biological systems, thereby bridging the critical gap between initial laboratory findings and clinical application within translational physiology research [1].
This analysis provides a comparative examination of these two workflows, emphasizing the core structural and philosophical differences that define their application in modern drug development. The integration of chemical biology is not merely an incremental improvement but a foundational change that addresses the persistent challenges of clinical attrition and the translational "valley of death" by fostering a deeper, more predictive understanding of drug action within complex physiological systems [1] [87].
Conceptual Foundations and Defining Characteristics
Traditional Drug Discovery Workflow
The traditional drug discovery pipeline is a linear and sequential process, where each stage operates in relative isolation. It is fundamentally a target-first approach, initiating with the identification of a single, often novel, molecular target such as a receptor or enzyme. The subsequent phases—screening, lead optimization, and preclinical testing—are primarily focused on refining a compound's interaction with this pre-selected target. This methodology relies heavily on high-throughput screening (HTS) of vast compound libraries, a process that is powerful but can be descriptive and lacks inherent mechanistic insight. The handoffs between stages are often discontinuous, leading to inefficiencies and a high risk of failure when compounds selected primarily for in vitro potency encounter the complexity of intact biological systems [88] [87].
Chemical Biology Platform Workflow
The chemical biology platform is an integrative and iterative organizational strategy. Its core objective is the systematic use of small molecules to investigate and modulate biological functions, thereby accumulating a knowledge base that informs the entire discovery process [1]. Unlike the target-first paradigm, chemical biology often employs a biology-first perspective, using phenotypic screening or systems biology data to observe compound effects in a physiologically relevant context before deconvoluting the specific molecular target(s) [89].
This platform is defined by its cross-disciplinary teams—spanning chemistry, physiology, pharmacology, and data science—and its use of parallel processes. A hallmark of this approach is the relentless focus on mechanistic understanding and target validation within living systems early in the discovery process. Technologies like Cellular Thermal Shift Assay (CETSA) are emblematic of this philosophy, enabling direct, quantitative measurement of drug-target engagement in intact cells and tissues, thus closing the gap between biochemical potency and cellular efficacy [90]. This workflow creates continuous feedback loops, where insights from later stages, including clinical observations, directly inform and refine earlier discovery and optimization efforts [1] [87].
Comparative Workflow Analysis: Stage-by-Stage Breakdown
The following table provides a direct, stage-by-stage comparison of the two methodologies, highlighting key differences in strategy, tools, and objectives.
Table 1: Stage-by-Stage Comparison of Traditional Drug Discovery and Chemical Biology Platforms
| Discovery Stage | Traditional Drug Discovery | Chemical Biology Platform |
|---|---|---|
| Core Philosophy | Linear, sequential, target-centric, and empirical [88]. | Integrative, iterative, systems-oriented, and knowledge-driven [1]. |
| Target Identification | Focus on a single, novel target (e.g., enzyme, receptor); often informed by genetic association [88]. | Investigation of target families and protein networks; uses systems biology (e.g., transcriptomics, proteomics) and phenotypic screening to identify functionally relevant targets [1] [89]. |
| Hit Identification | High-Throughput Screening (HTS) of massive compound libraries; "trial-and-error" with a focus on potency [88]. | Diverse strategies including fragment-based screening, DNA-encoded libraries (DEL) with high-throughput Surface Plasmon Resonance (HT-SPR) validation, and AI-driven de novo design [91] [87]. |
| Lead Optimization | Improve affinity, selectivity, and drug-like properties (ADMET) through sequential medicinal chemistry cycles [88]. | Accelerated by AI-guided retrosynthesis and high-throughput experimentation (HTE). Emphasizes functional relevance and confirmation of target engagement in cells (e.g., via CETSA) [90] [92]. |
| Preclinical Validation | Animal models to assess efficacy and safety; often poor predictors of human response [88] [87]. | Leverages physiologically relevant models (e.g., patient-derived cells, organ-on-a-chip) and direct ex vivo/in vivo target engagement studies in tissues for translational confidence [90] [88]. |
| Translational Bridge | Often weak; mechanistic uncertainty is a major cause of clinical failure [90]. | Strong; foundational to the platform. Uses clinical biology and biomarkers to connect preclinical findings with early-phase human trials (Phase I/IIa) [1]. |
Workflow Visualization
The fundamental logical difference between the two approaches is best understood through their overarching workflow structures, as illustrated below.
Quantitative Outcomes and Strategic Implications
The strategic differences between these workflows manifest in tangible performance metrics and developmental outcomes, which are critical for R&D decision-making.
Table 2: Quantitative and Strategic Implications of Drug Discovery Workflows
| Parameter | Traditional Drug Discovery | Chemical Biology Platform |
|---|---|---|
| Typical Discovery Timeline | 5+ years to clinical candidate [88]. | Potentially compressed; e.g., 18 months from target to Phase I candidate reported [47]. |
| Attrition Rate in Clinical Trials | ~90% failure rate from Phase I to approval [87]. | Aims to reduce attrition through better mechanistic validation and early go/no-go decisions [90] [1]. |
| Primary Cause of Failure | Lack of efficacy in humans (Phase II) and safety problems, often due to poor translational predictivity [90] [87]. | Mechanistic uncertainty is mitigated early; failure is intended to be earlier, faster, and cheaper [1]. |
| Cost Implications | ~$2.6 billion per approved drug; high cost of late-stage failures [87]. | Potential for significant cost reduction by failing candidates earlier and accelerating early phases [49] [87]. |
| Chemical & Target Exploration | Limited by the scale of physical HTS libraries and medicinal chemistry capacity [88]. | Explores vast virtual chemical spaces (e.g., 10³³ compounds via AI) and enables targeting of "undruggable" systems via novel modalities [87]. |
| Translational Confidence | Lower, due to reliance on animal models and descriptive bioassays [88]. | Higher, due to direct measurement of target engagement in physiologically relevant systems and use of human biomarkers [90] [1]. |
Experimental Protocols in Chemical Biology
The chemical biology platform is operationalized through a suite of sophisticated experimental protocols designed to provide mechanistic insight.
Protocol 1: CETSA for Cellular Target Engagement
Objective: To quantitatively confirm and measure the binding of a drug molecule to its intended protein target in a physiologically relevant environment (intact cells or tissues), bridging the gap between biochemical assays and cellular efficacy [90].
Detailed Methodology:
- Cell/Tissue Preparation: Treat live cells or tissue samples (e.g., from patient biopsies or animal models) with varying concentrations of the drug candidate or a vehicle control for a determined time.
- Heat Challenge: Aliquot the cell suspensions into multiple tubes and heat them at a range of precise temperatures (e.g., 50-65°C) for a fixed time (e.g., 3 minutes). This step denatures and precipitates unbound, unstable proteins.
- Cell Lysis and Clarification: Lyse the heated cells and centrifuge the lysates to separate the soluble (stable, drug-bound) protein from the precipitated (unstable, unbound) protein.
- Protein Quantification: Analyze the soluble fraction using a high-resolution method such as Western blot, immunoassay, or mass spectrometry to quantify the amount of intact target protein remaining.
- Data Analysis: Plot the fraction of soluble protein remaining versus temperature to generate a thermal stabilization curve (Thermal Shift Assay) or plot the fraction remaining at a single temperature versus drug concentration to generate an isothermal dose-response fingerprint (ITDRFCETSA). A rightward shift in the melting temperature (Tm) or increased protein stability at a given temperature in drug-treated samples indicates direct target engagement [90].
Protocol 2: High-Throughput Surface Plasmon Resonance (HT-SPR) for Kinetic Profiling
Objective: To characterize the binding kinetics (association rate, kon; dissociation rate, koff) and affinity (KD) of small molecule interactions with protein targets at a high-throughput scale, moving beyond simple "yes/no" binding data [91].
Detailed Methodology:
- Ligand Immobilization: A target protein (e.g., a kinase) is selectively immobilized onto the biosensor chip surface, often using biotin-streptavidin chemistry. HT-SPR allows for parallel immobilization of hundreds of different proteins or protein variants.
- Sample Injection: The small molecule analyte (e.g., from a fragment library or a set of optimized leads) is flowed over the chip surface in a continuous buffer stream at a range of concentrations.
- Real-Time Monitoring: The SPR instrument monitors the change in the refractive index at the chip surface in real-time (Response Units, RU) as molecules bind and dissociate.
- Regeneration: The chip surface is regenerated by flowing a solution that disrupts the binding interaction, preparing it for the next sample cycle.
- Data Processing and Kinetic Analysis: The resulting sensorgrams (RU vs. time) are processed and fitted to a binding model. This allows for the simultaneous determination of kon, koff, and the calculated KD (koff/kon) for thousands of interactions, providing a rich, quantitative profile of compound binding [91].
The Scientist's Toolkit: Key Research Reagents and Materials
The execution of advanced chemical biology protocols relies on a specialized set of reagents and tools.
Table 3: Essential Research Reagent Solutions for Chemical Biology
| Reagent / Material | Function in Experimental Protocol |
|---|---|
| Biotinylated Protein Panels (e.g., kinases) | Ready-to-use proteins for HT-SPR immobilization, enabling high-throughput kinetic screening against entire target families [91]. |
| DNA-Encoded Libraries (DEL) | Vast collections of small molecules (billions) each tagged with a unique DNA barcode, enabling ultra-high-throughput screening against purified protein targets via affinity selection [91]. |
| CETSA Kits / Reagents | Validated antibody panels or MS-ready kits for quantifying specific target proteins in the soluble fraction after cellular thermal denaturation [90]. |
| Fragment Libraries | Curated collections of low molecular weight, structurally simple compounds used for initial screening to identify efficient "hot spots" of binding, which are then optimized into leads [91]. |
| Synthetic Nucleosomes/Chromatin | Defined, chemically synthesized chromatin structures with specific histone modifications, enabling high-throughput biochemical screening of epigenetically relevant targets previously considered intractable [92]. |
| Cellular Assay Kits | Reporter gene assays, voltage-sensitive dyes for ion channels, and high-content multiparametric analysis kits for functional phenotypic screening in live cells [1]. |
Technology Enablers and Future Outlook
The modern ascendancy of the chemical biology platform is inextricably linked to concurrent technological revolutions. Artificial Intelligence (AI) and machine learning now serve as foundational capabilities, accelerating every step from AI-driven target identification to generative chemistry for de novo molecular design [90] [47] [49]. These tools are integrated into end-to-end platforms that compress design-make-test-analyze (DMTA) cycles from months to weeks [90] [87].
Furthermore, the resurgence of phenotypic screening, supercharged by high-content imaging and single-cell omics technologies, allows researchers to start with biology-first observations and use AI to deconvolute the mechanism of action, leading to the identification of novel therapeutic targets and pathways [89]. This integrative, data-rich approach is defining the future of drug discovery, moving the industry toward a more predictive, efficient, and successful model of therapeutic development centered on a deep understanding of human physiology and disease mechanisms [1] [89].
In modern drug discovery, the chemical biology platform has emerged as a critical organizational approach that optimizes drug target identification and validation while improving the safety and efficacy of biopharmaceuticals [1]. This platform achieves its goals through an emphasis on understanding underlying biological processes and leveraging knowledge gained from the action of similar molecules on these processes [1]. At the heart of this paradigm lies target engagement—the definitive demonstration that a therapeutic compound interacts with its intended biological target in a live, physiologically relevant context. Validating target engagement bridges the gap between in vitro potency and in vivo efficacy, providing crucial evidence for decision-making throughout the drug development pipeline.
The transition from traditional trial-and-error methods to mechanism-based approaches represents a fundamental shift in pharmaceutical research [1]. This evolution, deeply influenced by the advancement of the chemical biology platform, demands rigorous techniques to confirm that observed phenotypic outcomes result from specific target modulation rather than off-target effects. As a cornerstone of translational physiology—which examines biological functions across levels spanning from molecules to cells to organs to populations—target engagement validation provides the critical link between molecular interactions and physiological outcomes [1]. This article provides a comprehensive technical guide to the current methodologies and tools that enable researchers to confidently demonstrate target engagement in live cells and tissues, thereby de-risking the drug development process.
Essential Concepts and Definitions
Target Engagement: The specific binding and functional interaction of a small molecule or biologic therapeutic with its intended protein target in a physiologically relevant environment. Demonstration of target engagement provides direct evidence that a compound reaches its target and modulates its activity.
Chemical Biology Platform: An organizational approach to drug discovery that emphasizes understanding underlying biological processes and leverages knowledge from similar molecules to optimize drug target identification and validation [1]. This platform connects strategic steps to determine whether newly developed compounds could translate into clinical benefit using translational physiology [1].
Translational Physiology: The examination of biological functions across multiple levels, from molecular interactions to population-wide effects [1]. This approach has been deeply influenced by the advancement of chemical biology platforms [1].
Core Technologies for Validating Target Engagement
Genetic Modulation Approaches
Genetic approaches establish a target's role in disease mechanisms by altering gene function in relevant cellular models, including human induced pluripotent stem cells (iPSCs), primary cells, and immortalized cell lines [93].
Table 1: Genetic Approaches for Target Validation
| Method | Key Features | Experimental Readouts | Temporal Control |
|---|---|---|---|
| CRISPR-Cas9 KO | Permanent gene disruption; complete loss of function | Western blot, functional assays, phenotypic analysis | Irreversible |
| CRISPR-i/siRNA KD | Transient transcript reduction; partial loss of function | qPCR, functional assays, phenotypic analysis | Reversible (days) |
| CRISPR-a/Overexpression | Increased gene expression or function | qPCR, Western blot, functional assays | Tunable |
Direct Measurement Techniques
Cellular Thermal Shift Assay (CETSA)
CETSA measures target engagement by detecting ligand-induced thermal stabilization of proteins in cellular environments.
Protocol:
- Cell Preparation: Culture target cells in appropriate medium and harvest at 70-80% confluence.
- Compound Treatment: Incubate cells with test compound or DMSO control for predetermined time (typically 1-4 hours).
- Heat Challenge: Aliquot cell suspensions and heat at different temperatures (typically 40-65°C) for 3-5 minutes.
- Cell Lysis: Freeze-thaw cycles or detergent-based lysis to release soluble protein.
- Protein Quantification: Centrifuge to remove aggregates and quantify soluble target protein via Western blot or MSD immunoassay.
- Data Analysis: Calculate melting temperature (Tm) shifts; significant leftward shift indicates stabilization and target engagement.
Bioluminescence Resonance Energy Transfer (BRET)
BRET enables quantitative measurement of target engagement in live cells through energy transfer between luciferase and fluorescent protein tags.
Protocol:
- Construct Design: Create fusion proteins with target protein-NanoLuc and binding partner-HaloTag (or similar).
- Cell Transfection: Transfect constructs into relevant cell lines using appropriate method (e.g., lipofection, electroporation).
- Compound Treatment: Incubate with test compounds for specified duration.
- Substrate Addition: Add NanoLuc substrate (furimazine) at recommended concentration.
- Signal Detection: Measure emission at 460nm (donor) and 610nm (acceptor) using plate reader.
- Data Analysis: Calculate BRET ratio (acceptor/donor); decreased ratio indicates competitive displacement.
High-Content Imaging and Phenotypic Analysis
High-content screening (HCS) combines automated microscopy with multiparametric analysis of cellular events to provide rich phenotypic profiling [1] [93].
Table 2: High-Content Analysis Methods for Target Engagement
| Technique | Measured Parameters | Information Gained | Compatibility |
|---|---|---|---|
| Multiplexed Fluorescent Imaging | Cell viability, apoptosis, cell cycle, protein translocation [1] | Phenotypic fingerprint, infer target engagement [93] | Fixed and live cells |
| Multi-Electrode Array (MEA) | Electrical activity, calcium dynamics [93] | Functional phenotypic outcomes in excitable cells [93] | Neurons, cardiomyocytes |
| Calcium Oscillation Analysis | Calcium flux patterns, frequency, amplitude [93] | Pathway activation, functional response [93] | GPCR targets, ion channels |
Protocol: High-Content Analysis of Target Engagement:
- Cell Preparation: Plate cells in optical-grade microplates at optimized density.
- Staining: Apply fluorescent dyes or antibodies targeting:
- Nuclei (Hoechst/DAPI)
- Cytoskeletal markers (Phalloidin)
- Target protein (immunofluorescence)
- Pathway activation markers (phospho-antibodies)
- Image Acquisition: Automated microscopy at 20x-60x magnification, multiple sites per well.
- Image Analysis: Segment cells and quantify:
- Target protein intensity and localization
- Morphological changes (cell size, shape, texture)
- Colocalization with organelle markers
- Population distribution patterns
Advanced Functional Assays for Mechanistic Validation
Biochemical and Cell-Based Assays
Functional assays measure the biological activity of targets and effects of modulation, using tool molecules to demonstrate desired outcomes in vitro [93].
Table 3: Functional Assay Platforms
| Assay Type | Format | Key Readouts | Throughput |
|---|---|---|---|
| Biochemical Assays | Cell-free, molecular interactions | Enzymatic activity, binding affinity, potency [93] | High |
| Cell-Based Signaling | Live cells, pathway reporters | Pathway activation, gene expression, second messengers [93] | Medium-High |
| Ion Channel Activity | Voltage-sensitive dyes, patch-clamp [1] | Membrane potential, calcium flux, electrophysiology [1] | Low-Medium |
Transcriptomic and Proteomic Analysis
Expression Profiling: Assesses presence and distribution of targets in healthy versus diseased tissues, determining if target expression correlates with disease progression or severity [93].
Protocol: Expression Profiling for Target Validation:
- Sample Collection: Obtain matched diseased and healthy tissues or treated vs. control cells.
- RNA/Protein Extraction: Use standardized kits with quality control (RIN >8 for RNA).
- Global Profiling: RNA-seq or mass spectrometry-based proteomics.
- Data Analysis:
- Differential expression analysis (disease vs. normal)
- Pathway enrichment (GO, KEGG, GSEA)
- Correlation with clinical parameters
- Co-expression network analysis
The Scientist's Toolkit: Essential Research Reagents
Table 4: Research Reagent Solutions for Target Engagement Studies
| Reagent Category | Specific Examples | Function in Target Engagement |
|---|---|---|
| CRISPR Tools | CRISPR-Cas9 for KO, CRISPR-i/a for modulation [93] | Genetic validation of target-disease linkage [93] |
| Live-Cell Dyes | Voltage-sensitive dyes, calcium indicators (Fluo-4), viability markers [1] | Real-time monitoring of pathway activity and cellular health [1] |
| NanoLuc/Fluorescent Tags | NanoLuc luciferase, HaloTag, GFP variants [1] | Protein tagging for BRET, localization, and quantification studies [1] |
| Pathway Reporters | Luciferase constructs, FRET biosensors, transcriptional reporters [1] | Monitoring downstream signaling pathway activation [1] |
| Proteostasis Reagents | Proteasome inhibitors (MG132), protein synthesis inhibitors | Investigating protein turnover and stabilization (CETSA) |
| Validated Antibodies | Phospho-specific antibodies, conformation-sensitive antibodies [1] | Detecting post-translational modifications and activation states [1] |
Integrated Workflows and Data Analysis
Comprehensive Validation Strategy
A robust target engagement strategy integrates multiple orthogonal approaches to build compelling evidence for target-drug interaction.
Quantitative Analysis Methods
Effective analysis of target engagement data employs multiple quantitative approaches:
Statistical Analysis:
- Concentration-response curves (IC50, EC50 determination)
- Z'-factor and strictly standardized mean difference (SSMD) for assay quality
- One-way ANOVA with post-hoc testing for multiple comparisons
- Pearson/Spearman correlation for relationship analysis
Data Normalization:
- Min-max normalization for plate-based assays
- Z-score normalization for high-content screening data
- Housekeeping gene/protein normalization for expression data
The rigorous validation of target engagement in live cells and tissues represents a cornerstone of the modern chemical biology platform, providing critical evidence that bridges the gap between in vitro potency and physiological relevance [1]. By employing the integrated toolkit of genetic, biophysical, imaging, and functional approaches detailed in this technical guide, researchers can build compelling evidence for specific target engagement, thereby de-risking drug development and enhancing translational success [93]. As the field evolves, the continued refinement of these methods—particularly through increased spatial resolution, temporal monitoring, and integration with systems biology approaches—will further strengthen our ability to confidently advance therapeutic candidates from bench to bedside.
Precision medicine represents a fundamental shift in healthcare, moving away from a one-size-fits-all approach toward therapies tailored to individual patient characteristics. At the core of this paradigm lies target validation—the rigorous process of establishing that modulation of a specific biological molecule produces a therapeutic effect. The journey from biological insight to validated therapeutic target requires integration of chemical biology platforms and translational physiology, creating a multidisciplinary framework that connects molecular discoveries to clinical applications [1]. This approach has evolved significantly from traditional trial-and-error methods to a sophisticated, mechanism-based strategy that leverages systems biology techniques including proteomics, metabolomics, and transcriptomics [1].
The chemical biology platform serves as an organizational approach that optimizes drug target identification and validation while improving the safety and efficacy of biopharmaceuticals. This platform achieves these goals through deep understanding of underlying biological processes and leveraging knowledge gained from the action of similar molecules on these biological processes [1]. When combined with translational physiology—which examines biological functions across multiple levels from molecular interactions to population-wide effects—this integrated approach provides a powerful engine for driving precision medicine forward [1] [94]. The ultimate success of this approach depends on establishing a clear connection between target modulation and clinical benefit, creating a pathway that extends from bench to bedside and ultimately to community health impact [95].
The Target Validation Pipeline: From Concept to Clinic
Integrating Chemical Biology and Translational Physiology
The validation of therapeutic targets follows a structured pipeline that incorporates both chemical biology principles and translational physiology frameworks. This process begins with target identification and proceeds through increasingly rigorous validation stages, with decision gates that determine whether a target merits continued investment. The chemical biology platform connects a series of strategic steps to determine whether a newly developed compound could translate into clinical benefit using translational physiology [1]. This approach represents a significant departure from traditional methods, as it emphasizes targeted selection and integrates systems biology approaches to understand protein network interactions [1].
A key historical development in this field was the establishment of the Clinical Biology department at Ciba (now Novartis) in 1984, which implemented a systematic approach based on four key steps derived from Koch's postulates: (1) identify a disease parameter (biomarker); (2) show that the drug modifies that parameter in an animal model; (3) show that the drug modifies the parameter in a human disease model; and (4) demonstrate a dose-dependent clinical benefit that correlates with similar change in direction of the biomarker [1]. This framework, which represents an early organized effort in translational physiology, continues to influence modern target validation approaches, though with significantly advanced technological capabilities.
The contemporary target validation pipeline operates within a broader translational research continuum that encompasses multiple phases. T1 translation focuses on moving basic research findings to the clinical research setting (bench to bedside), while T2 translation extends insights from clinical research to medical practice. T3 translation further extends these findings to community health and public policy [94] [95]. This process is fundamentally bidirectional, with observations from clinical and community settings stimulating "reverse translation" back to basic research laboratories for mechanistic investigation [94] [95].
Technological Advances Driving Target Validation
Recent technological innovations have dramatically accelerated the target validation process. 3D multi-omics represents one particularly transformative approach that layers the physical folding of the genome with other molecular readouts to map how genes are switched on or off [96]. By capturing three-dimensional genomic context, researchers can move beyond statistical association and start uncovering the causal biology that drives disease. This approach addresses a fundamental challenge in therapeutic development: despite decades of genetic research, most common diseases still lack effective treatments, largely because identifying truly causal genes has proven difficult [96].
Traditional genomics approaches often assume that a disease-associated variant affects the nearest gene in the linear DNA sequence, but this assumption fails approximately half the time [96]. Without 3D context, conventional approaches often miss valuable targets or prioritize incorrect ones, adding cost and time to drug discovery. The 3D multi-omics approach makes the process of defining causality direct, scalable, and accessible at a genome-wide level in the most relevant cell types [96]. This method integrates genome folding data with other information layers—such as chromatin accessibility and gene expression—enabling researchers to identify the true regulatory networks underlying disease.
Additional technological platforms supporting modern target validation include high-throughput screening infrastructures such as EU-OPENSCREEN, the European research infrastructure for chemical biology and early drug discovery [37]. This consortium provides open access to high-throughput screening, chemoproteomics, and spatial MS-based omics platforms, along with medicinal chemistry expertise to support the discovery of new biologically active small molecules that serve as starting points for developing chemical tool compounds and drugs [37].
Figure 1: Integrated Target Validation Pipeline. This workflow illustrates the multidisciplinary approach combining chemical biology and translational physiology to advance targets from identification through clinical validation.
Cutting-Edge Technologies in Target Identification and Validation
Advanced Methodologies for Target Discovery
The initial stages of target identification and validation employ increasingly sophisticated methodologies that leverage recent technological advances. The following experimental protocols represent state-of-the-art approaches in the field:
3D Multi-omics for Causal Gene Mapping This protocol enables researchers to move beyond statistical associations to identify causally relevant genes and pathways [96]. The process begins with cell type selection based on disease relevance, followed by multi-omic profiling including genome folding (Hi-C), chromatin accessibility (ATAC-seq), and gene expression (RNA-seq) [96]. Researchers then generate a 3D reference atlas by integrating these data layers to map physical interactions between regulatory elements and genes. Disease-associated variants from genome-wide association studies (GWAS) are overlayed on this atlas to identify disruptions in normal gene-regulatory relationships. Functional validation occurs through CRISPR-based perturbation of identified candidate genes followed by assessment of phenotypic effects in relevant cellular models [96]. This integrated approach provides genetically validated targets with built-in evidence of causality rather than mere association.
PROTAC-Based Target Validation PROteolysis TArgeting Chimeras (PROTACs) represent a innovative chemical biology approach that enables validation through targeted protein degradation [97]. The process involves designing bifunctional molecules that consist of one ligand that binds to the target protein, another that recruits an E3 ubiquitin ligase, and a linker connecting these two moieties [97]. The optimized PROTAC molecule is then introduced to cells to assess target degradation efficiency and specificity. Researchers monitor protein levels through immunoblotting or targeted proteomics, followed by evaluation of phenotypic consequences of target loss. Counterproof experiments using mutant E3 ligase recruitment domains or proteasome inhibitors establish the mechanism of degradation [97]. This approach provides particularly compelling validation because it demonstrates that removing the target protein produces the desired therapeutic effect.
Chemical Biology Platform Implementation This organizational approach optimizes the entire target identification and validation process [1]. The methodology begins with target family selection based on therapeutic area and biological rationale, followed by knowledge accumulation regarding similar molecules and their effects on related biological processes [1]. The core process involves multidisciplinary team formation including chemists, biologists, physiologists, and clinical pharmacologists working in parallel processes. Teams employ systems biology techniques including transcriptomics, proteomics, metabolomics, and network analyses to understand protein network interactions [1]. The process incorporates iterative learning cycles where information from each stage informs subsequent experiments, creating an accumulating knowledge base that increases efficiency in decision-making about which targets to advance [1].
Research Reagent Solutions for Target Validation
Modern target validation relies on a sophisticated toolkit of research reagents and platforms that enable precise manipulation and measurement of biological systems. The table below details essential materials and their applications in the target validation process.
Table 1: Essential Research Reagent Solutions for Target Validation and Experimental Applications
| Research Tool Category | Specific Examples | Primary Function in Target Validation |
|---|---|---|
| High-Throughput Screening Platforms | EU-OPENSCREEN infrastructure [37] | Identification of biologically active small molecules through large-scale compound screening |
| 3D Multi-omics Technologies | Enhanced Genomics platform (Hi-C, ATAC-seq, RNA-seq) [96] | Mapping genome folding and regulatory networks to identify causal genes and pathways |
| Chemical Proteomics | EU-OPENSCREEN chemoproteomics [37] | Target deconvolution and identification of drug-protein interactions |
| Human Organoid Systems | Intestinal organoids for digestive physiology [21] | Physiologically relevant human models for testing target relevance and therapeutic safety/efficacy |
| Spatial MS-based Omics | EU-OPENSCREEN spatial MS platforms [37] | Spatial resolution of molecular distributions within tissues and cellular contexts |
| CRISPR Tools | Base-editing therapies [97] | Precision gene editing for functional validation of targets through genetic perturbation |
Therapeutic Modalities Enabled by Validated Targets
Emerging Therapeutic Classes in Precision Medicine
The rigorous validation of therapeutic targets has enabled the development of several innovative treatment modalities that form the foundation of modern precision medicine. These approaches leverage specific molecular insights to create highly targeted interventions:
PROTACs and Targeted Protein Degradation PROteolysis TArgeting Chimeras represent a breakthrough therapeutic modality that leverages validated targets for selective protein degradation [97]. These heterobifunctional molecules consist of one ligand that binds to a target protein of interest and another that recruits an E3 ubiquitin ligase, connected by a chemical linker [97]. This structure creates a ternary complex that promotes ubiquitination and subsequent proteasomal degradation of the target protein. The field has seen rapid growth, with more than 80 PROTAC drugs currently in development and over 100 commercial organizations involved in research [97]. While cancer remains the primary disease focus, PROTAC applications are expanding to neurodegenerative, infectious, and autoimmune diseases [97]. Current research focuses on expanding the E3 ligase toolbox beyond the four most commonly used ligases (cereblon, VHL, MDM2, and IAP) to include newer options such as DCAF16, DCAF15, DCAF11, KEAP1, and FEM1B, which could enable targeting of previously inaccessible proteins and reduce off-target effects [97].
Radiopharmaceutical Conjugates Radiopharmaceutical conjugates represent another precision modality that combines targeting moieties (antibodies, peptides, or small molecules) with radioactive isotopes for imaging or therapy [97]. These agents offer dual benefits—real-time imaging of drug distribution combined with highly localized radiation therapy [97]. For cancer treatment, radiopharmaceutical conjugates significantly reduce off-target effects and toxicity by directing therapeutic payloads specifically to diseased cells. These drugs improve efficacy through better tumor targeting with lethal radiation payloads [97]. The field anticipates increased use of these theranostic approaches as several radiopharmaceuticals have entered late-stage clinical trials or received regulatory designations [97].
Cell and Gene Therapies Advanced cell and gene therapies represent the cutting edge of personalized therapeutics, with chimeric antigen receptor (CAR) T-cell therapies demonstrating remarkable success in hematological malignancies [97]. The field is now advancing next-generation platforms to overcome current limitations, including allogeneic CAR-T (donor-derived or gene-edited cells that provide faster, more affordable "off-the-shelf" options) and dual-target/armored CAR-T cells that recognize two antigens or are engineered to secrete cytokines or resist immunosuppression [97]. Gene editing therapies have reached new milestones, with a recent case demonstrating the feasibility of rapid, individualized CRISPR editing—a seven-month-old infant with CPS1 deficiency received personalized CRISPR base-editing therapy developed in just six months [97]. This breakthrough highlights the potential for personalized gene editing even for life-threatening rare diseases with no existing treatments.
Quantitative Assessment of Therapeutic Modalities
The development and validation of these therapeutic modalities has generated substantial quantitative data that demonstrates their current impact and future potential. The table below summarizes key metrics for major therapeutic classes in precision medicine.
Table 2: Quantitative Landscape of Precision Medicine Therapeutic Modalities (2025)
| Therapeutic Modality | Pipeline Volume | Key Molecular Targets | Clinical Stage Distribution | Notable Efficacy Metrics |
|---|---|---|---|---|
| PROTACs | >80 drugs in development [97] | E3 ligases (cereblon, VHL, MDM2, IAP) [97] | Predominantly preclinical with advancing candidates | Expanding beyond cancer to neurodegenerative/infectious diseases [97] |
| Radiopharmaceutical Conjugates | Multiple in late-stage trials [97] | Tumor-associated antigens, receptors [97] | Late-stage clinical trials with regulatory designations | Reduced off-target effects and toxicity [97] |
| CAR-T Therapies | Numerous clinical trials [97] | CD19, CD22, BCMA, others [97] | Approved products + next-generation trials | Response rates >80% in certain hematologic malignancies [97] |
| CRISPR Therapies | Phase 3 for NTLA-2002 [97] | Varied monogenic disease targets [97] | Phase 1 to Phase 3, first personalized therapy | 86% LDL reduction with CTX310 in Phase 1 [97] |
| Microbiome-Targeted Therapies | >180 therapies in development [97] | Microbial species, metabolic pathways [97] | FDA approval for FMT in C. diff, others in development | FDA-approved FMT for recurrent C. difficile [97] |
Biomarkers and Diagnostic Tools in Precision Medicine
Enabling Early Diagnosis and Patient Stratification
Biomarkers—measurable biological indicators in blood, tissue, or bodily fluids—play a pivotal role in precision medicine by detecting diseases at their earliest, most treatable stages and enabling appropriate patient stratification for targeted therapies [97]. In cancer treatment, for example, BRCA1/2 genetic mutations have become an important component of preventive care for breast and ovarian cancers [97]. The field is now advancing blood-based and imaging biomarkers to detect early signs of neurodegenerative diseases like Alzheimer's and Parkinson's before clinical symptoms appear [97].
Recent studies have validated plasma biomarkers (e.g., phosphorylated tau) that correlate with early Alzheimer's pathology, enabling earlier diagnosis and trial enrollment [97]. This early detection capability could allow for timely intervention, improve clinical trial design, and shift the focus from symptom management to disease prevention [97]. The development of these biomarkers follows a rigorous validation process similar to therapeutic targets, requiring demonstration of analytical validity, clinical validity, and clinical utility across diverse patient populations.
The biomarker development process exemplifies the bidirectional nature of translational physiology, where observations made in clinical settings can stimulate reverse translation to basic research laboratories for mechanistic investigation [94] [95]. For example, epidemiological observations of relationships between dietary sodium intake and blood pressure led to both clinical trials testing sodium restriction and reverse translation studies investigating the physiological mechanisms underlying sodium's effects on cardiovascular function [94] [95].
AI-Enhanced Clinical Development
Artificial intelligence is transforming biomarker development and clinical trial design through powerful simulation capabilities. Quantitative systems pharmacology models and "virtual patient" platforms simulate thousands of individual disease trajectories, allowing research teams to test dosing regimens and refine inclusion criteria before a single patient is dosed [97]. AI-powered digital twins are also transforming clinical development and translational research, with companies like Unlearn.ai validating digital twin-based control arms in Alzheimer's trials [97]. This approach demonstrates that AI-augmented virtual cohorts can reduce placebo group sizes considerably, thereby ensuring faster timelines and more confident data without losing statistical power [97].
The integration of AI into clinical development represents a natural extension of the chemical biology platform approach, which emphasizes accumulating knowledge and using parallel processes to speed development timelines and reduce costs [1]. As these technologies mature, they promise to further accelerate the translation of validated targets into effective personalized therapeutics.
Future Directions and Challenges
Emerging Trends and Technologies
The field of precision medicine continues to evolve rapidly, with several emerging technologies poised to further transform target validation and therapeutic development. 3D multi-omics is expected to reshape drug discovery in the next decade as profoundly as next-generation sequencing has reshaped genetics [96]. This approach makes the process of defining causality direct, scalable, and accessible at a genome-wide level in the most relevant cell types, providing a credible path to developing the next wave of truly effective therapies for complex common diseases that have resisted traditional discovery approaches [96].
Epigenetic editing represents another emerging frontier, offering a "hit-and-run" approach to precise modification of gene expression without altering the underlying DNA sequence [61]. This modality has advanced from concept to clinical development, with tools and agents now entering early-stage human trials [61]. Similarly, in vivo CAR-T cell therapy approaches that use targeted delivery systems to generate CAR-T cells directly in patients are advancing, potentially bypassing the complex ex vivo manufacturing processes that currently limit accessibility [61].
The continued expansion of human organoid technologies provides increasingly sophisticated 3D in vitro platforms for studying disease mechanisms, drug efficacy, and toxicity [61]. These physiologically relevant models bridge the gap between traditional cell culture and human studies, though regulatory and practical challenges remain for their full integration into drug development pipelines [61].
Implementation Challenges and Solutions
Despite considerable progress, the implementation of precision medicine approaches faces significant challenges. The timeline from scientific discovery to clinical implementation remains protracted, averaging approximately 17 years according to some research [21]. This extended timeline reflects the complexity of establishing robust causal relationships between targets and clinical outcomes, developing specific therapeutic modalities, and demonstrating safety and efficacy in increasingly targeted patient populations.
The multidisciplinary nature of precision medicine creates both opportunities and challenges, as effective collaboration requires integration of diverse expertise spanning basic science, clinical research, and public health implementation [21]. Successful teams employ strategies including clear communication using straightforward language, patience in identifying appropriate collaborators, and perseverance in maintaining forward progress despite setbacks [21]. Research interest groups that bring together investigators from related but distinct fields have proven valuable in sparking productive multidisciplinary collaborations [21].
Figure 2: PROTAC Mechanism of Action. This diagram illustrates the targeted protein degradation pathway enabled by PROTAC molecules, which recruit E3 ubiquitin ligases to specific target proteins, leading to their ubiquitination and subsequent proteasomal degradation.
Funding constraints represent another persistent challenge, particularly for academic researchers pursuing translational investigations. Successful physiologists employ strategic approaches including adding extra experimental groups to existing studies to explore understudied populations, maintaining forward momentum on promising research directions even when dedicated funding is limited, and celebrating incremental successes that sustain motivation over extended timelines [21]. The compelling nature of the research questions and potential health impacts provide powerful motivation that helps researchers overcome inevitable frustrations and setbacks [21].
The path to precision medicine through validated targets represents a fundamental transformation in therapeutic development, enabled by the integration of chemical biology platforms and translational physiology approaches. This multidisciplinary framework provides a systematic process for identifying and validating therapeutic targets, developing specific modalities to modulate these targets, and translating these advances into clinical practice through appropriate biomarker strategies and patient selection approaches. The field has progressed from conceptual promise to tangible impact, with multiple targeted therapies now delivering personalized treatment options across diverse disease areas.
Future progress will depend on continued technological innovation, particularly in areas such as 3D multi-omics, epigenetic editing, and artificial intelligence-enhanced development. Equally important will be addressing implementation challenges including protracted development timelines, multidisciplinary collaboration barriers, and funding constraints. By building on the established foundations of target validation and pursuing emerging opportunities with rigor and persistence, the field promises to advance toward a future where therapies are increasingly matched to individual patient characteristics, maximizing benefit while minimizing harm—the ultimate realization of precision medicine's potential.
Conclusion
The chemical biology platform represents a paradigm shift in drug discovery, fundamentally intertwining with translational physiology to create a dynamic, evidence-driven engine for therapeutic innovation. By moving beyond traditional, siloed approaches to a multidisciplinary, mechanism-based framework, this platform successfully bridges the critical gap between potent compound development and demonstrable clinical benefit. The integration of advanced tools—from chemoproteomics and AI to combinatorial optimization—is systematically de-risking the pipeline and compressing development timelines. The future of biomedical research hinges on further embracing this integrative model, deepening our understanding of physiological context at the population level, and continuing to foster the collaborative ecosystems necessary to turn scientific discovery into widespread health impact. The ongoing evolution of this platform promises to further solidify its role as the cornerstone of precision medicine and effective therapeutic development.
References
- 1. The Evolution of Chemical Biology into Translational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12326334/]
- 2. Objective, Quantitative, Data-Driven Assessment of ... [https://www.sciencedirect.com/science/article/pii/S245194561730421X]
- 3. Quantitative Techniques and Organic Molecules [https://iastate.pressbooks.pub/isudp-2025-205/chapter/quantitative-techniques/]
- 4. Grand challenges in chemical biology from the perspective ... [https://www.frontiersin.org/journals/chemical-biology/articles/10.3389/fchbi.2025.1731631/full]
- 5. Drug discovery articles within Nature Chemical Biology [https://www.nature.com/subjects/drug-discovery/nchembio]
- 6. The QDπ dataset, training data for drug-like molecules and ... [https://www.nature.com/articles/s41597-025-04972-3]
- 7. Revolutionizing Pharma Drug Discovery in 2025 [https://newristics.com/revolutionizing-pharma-drug-discovery-in-2025.php]
- 8. How new approach methodologies are reshaping drug ... [https://www.mckinsey.com/industries/life-sciences/our-insights/the-synthesis/how-new-approach-methodologies-are-reshaping-drug-discovery]
- 9. 2025 AI in Drug Discovery: Predictions [https://lizard.bio/knowledge-hub/2025-ai-in-drug-discovery-predictions]
- 10. Algorithms and tools for data-driven omics integration to ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06446-x]
- 11. Bridging academia and industry: advancing systems ... [https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2025.1627214/full]
- 12. The Evolution of Chemical Biology into Translational ... [https://pubmed.ncbi.nlm.nih.gov/40668627/]
- 13. Integrating translational and clinical research to advance ... [https://www.ddw-online.com/how-integrating-translational-and-clinical-research-can-advance-drug-development-37444-202510/]
- 14. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 15. Drug discovery center integrates AI for big impact [https://www.unc.edu/posts/2025/11/24/drug-discovery-center-integrates-ai-for-big-impact/]
- 16. Milestones in Drug Development [https://dataverify.creative-biolabs.com/milestones-in-drug-development.htm]
- 17. A Chronology Of Biotechnology's Modern Era (1945-present) [https://briandcolwell.com/a-chronology-of-biotechnologys-modern-era-1945-present/]
- 18. Four milestones powering the genome sequencing revolution [https://www.ukri.org/blog/four-milestones-powering-the-genome-sequencing-revolution/]
- 19. Genomics Revolution: The Future of Biotechnology [https://www.sequencebiotech.com/blog/genomics-revolution-in-biotech]
- 20. The Chemical Biology–Medicinal Chemistry Continuum [https://www.sciencedirect.com/science/article/pii/S2451945617301824]
- 21. Translational Physiology How Scientists Are Turning ... [https://www.physiology.org/publications/news/the-physiologist-magazine/2025/march/translational-physiology--how-scientists-are-turning-research-into-treatments]
- 22. An artificial intelligence accelerated virtual screening ... [https://www.nature.com/articles/s41467-024-52061-7]
- 23. ICTR announces the recipients of the 2025 Advancing ... [https://ictr.wisc.edu/news/ictr-announces-the-recipients-of-the-2025-advancing-translational-research-science-pilot-award/]
- 24. Central dogma of molecular biology - Wikipedia [https://en.wikipedia.org/wiki/Central_dogma_of_molecular_biology]
- 25. Central dogma, redefined | Nature Chemical Biology [https://www.nature.com/articles/s41589-021-00850-2]
- 26. Exploration of the Central Dogma at the Interface of Chemistry and Biology: 2010 Yale Chemical Biology Symposium - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2946126/]
- 27. Proteolysis‐Targeting Chimera (PROTAC) - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495453/]
- 28. From Conception to Development: Investigating PROTACs ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2021.672267/full]
- 29. Recent Advances in the Development of Pro-PROTAC for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473374/]
- 30. Targeting the Undruggable: Recent Progress in PROTAC- ... [https://www.mdpi.com/2072-6694/17/11/1871]
- 31. Multitargeted protein degradation: Integrating small- ... [https://www.sciencedirect.com/science/article/pii/S259004982500089X]
- 32. Machine learning in targeted protein degradation drug ... [https://www.sciencedirect.com/science/article/pii/S1359644625002764]
- 33. CRISPR approaches to small molecule target identification [https://pmc.ncbi.nlm.nih.gov/articles/PMC5834945/]
- 34. A translational framework of genoproteomic studies for ... [https://www.nature.com/articles/s44325-024-00015-9]
- 35. Target identification of small molecules using large-scale ... [https://www.nature.com/articles/s41467-017-02349-8]
- 36. Will CRISPR Cut Out the Competition or Can RNAi Help ... [https://www.sciencedirect.com/science/article/pii/S2472555222072720]
- 37. Empowering research in chemical biology and early drug ... [https://www.sciencedirect.com/science/article/pii/S2472555225000218]
- 38. What is high-throughput screening (HTS) and how can ... [https://bioscience.lonza.com/lonza_bs/CH/en/what-is-high-throughput-screening-and-how-can-lonza-help]
- 39. How to choose colors for data visualizations [https://www.atlassian.com/data/charts/how-to-choose-colors-data-visualization]
- 40. What to consider when choosing colors for data visualization [https://academy.datawrapper.de/article/140-what-to-consider-when-choosing-colors-for-data-visualization]
- 41. Bridging the gap between target-based and phenotypic- ... [https://pubmed.ncbi.nlm.nih.gov/38747562/]
- 42. Phenotypic vs. Target-Based Drug Discovery: A Shift Back ... [https://www.linkedin.com/posts/souravroy-phd_drugdiscovery-phenotypicscreening-targetbaseddrugdiscovery-activity-7335447486536302592-Q1Yp]
- 43. Phenotypic Drug Discovery: Recent successes, lessons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9708951/]
- 44. Phenotypic Screening: A Powerful Tool for Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/phenotypic-screening-a-powerful-tool-for-drug-discovery-398572]
- 45. Trends in Target-Based Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/trends-in-target-based-drug-discovery-392990]
- 46. The computationally guided design of selective targeters ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537719/]
- 47. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 48. Advances of the Target-Based and Phenotypic Screenings ... [https://www.sciltp.com/journals/ijddp/articles/2504000136]
- 49. Transformative Role of Artificial Intelligence in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406033/]
- 50. How AI Virtual Human Replicas Could Transform Drug ... [https://news.northeastern.edu/2025/11/19/ai-drug-discovery-research/]
- 51. Optimizing drug design by merging generative AI with a ... [https://www.nature.com/articles/s42004-025-01635-7]
- 52. Mapping the Rise in Machine Learning in Environmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567794/]
- 53. AI in drug discovery: Key trends shaping therapeutics in 2025 [https://www.gubra.dk/blog/ai-in-drug-discovery-key-trends-shaping-therapeutics-in-2025/]
- 54. Cross-disciplinary perspectives on the potential for artificial ... [https://pubs.rsc.org/en/content/articlehtml/2025/cs/d5cs00146c]
- 55. Beyond Bench and Bedside: Disentangling the Concept of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4293498/]
- 56. Translational Chemical Biology: Gap assessment for ... [https://www.ddw-online.com/translational-chemical-biology-gap-assessment-for-advancing-drug-discovery-development-and-precision-medicine-1031-201612/]
- 57. Translational Medicine: Bridging the Gap Between Bench and ... [https://www.openaccessjournals.com/articles/translational-medicine-bridging-the-gap-between-bench-and-bedside-17072.html]
- 58. Bridging the Gap Between Bench and Bedside [https://falconediting.com/en/blog/translational-research-bridging-the-gap-between-bench-and-bedside/]
- 59. From bench to bedside and back again: Bridging the gap ... [https://www.jax.org/news-and-insights/2024/september/bridging-the-gap-for-translational-research-success]
- 60. Bench to Bedside: Translating Science from the Lab ... [https://www.docwirenews.com/post/bench-to-bedside-translating-science-from-the-lab-to-the-clinic]
- 61. Nature Reviews Drug Discovery [https://www.nature.com/nrd/]
- 62. Bench-to-Bedside Gap Shrinks with New Trial Designs [https://discoveries.vanderbilthealth.com/2025/02/bench-to-bedside-gap-closing-with-new-trial-design/]
- 63. Human disease models in drug development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10173243/]
- 64. Bridging the Gap: Translating Preclinical Biomarkers to ... [https://blog.crownbio.com/bridging-the-gap-translating-preclinical-biomarkers-to-clinical-success]
- 65. Pitfalls and limitations in translation from biomarker discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3599714/]
- 66. How AI & Biomarkers Are Reshaping the Next Frontier in ... [https://www.precisionformedicine.com/blog/how-ai-biomarkers-are-reshaping-the-next-frontier-in-drug-development]
- 67. Application of combinatorial optimization strategies in ... [https://www.nature.com/articles/s41467-020-16175-y]
- 68. Combinatorial optimization [https://en.wikipedia.org/wiki/Combinatorial_optimization]
- 69. Evaluation of combinatorial optimisation algorithms for c- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10386961/]
- 70. The optimization of combinatorial drug therapies [https://www.sciencedirect.com/science/article/abs/pii/S1359644621003263]
- 71. Reusable combinatorial libraries with high diversity for ... [https://pubmed.ncbi.nlm.nih.gov/40745130/]
- 72. How CETSA® Enhances Translational Studies – A Sitryx ... [https://www.pelagobio.com/cetsa-drug-discovery-resources/locked-content/on-demand-webinar-how-cetsa-enhances-translational-studies-a-sitryx-case-study/]
- 73. CETSA quantitatively verifies in vivo target engagement of ... [https://www.nature.com/articles/s41598-017-12513-1]
- 74. Applications of the Cellular Thermal Shift Assay to Drug ... [https://pubmed.ncbi.nlm.nih.gov/40362180/]
- 75. Current Advances in CETSA - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9218591/]
- 76. Thermal shift assays in drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S1056871925008007]
- 77. Perspective on CETSA Literature: Toward More ... [https://pubmed.ncbi.nlm.nih.gov/31665966/]
- 78. Collaborate With NCATS [http://ncats.nih.gov/research/collaborate-with-ncats]
- 79. Chemical biologist links basic discoveries to treatments for ... [https://news.uchicago.edu/story/chemical-biologist-links-basic-discoveries-treatments-disease]
- 80. The Quiet Evolution: How Basic Science Transforms Lives [https://news.med.miami.edu/the-quiet-evolution-how-basic-science-transforms-lives/]
- 81. Chemical Biology and Physiology 2025 [https://www.ohsu.edu/school-of-medicine/chemical-physiology-and-biochemistry/chemical-biology-and-physiology-2025]
- 82. Learning to Navigate the Four Phases of Clinical Trials [https://extendedstudies.ucsd.edu/news-events/extended-studies-blog/learning-to-navigate-the-four-phases-of-clinical-trials]
- 83. A framework for clinical and translational research in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8057461/]
- 84. A framework for evaluating the diversity of clinical trials [https://www.sciencedirect.com/science/article/abs/pii/S0895435624000544]
- 85. Comparative Analysis of Chemical Distribution Models for ... [https://www.mdpi.com/2305-6304/13/6/439]
- 86. One size does not fit all: revising traditional paradigms for ... [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-025-00948-y]
- 87. End to end drug discovery: Revolutionizing 2025 [https://lifebit.ai/blog/end-to-end-drug-discovery/]
- 88. How Modern Biotech Is Revolutionizing Drug Discovery in ... [https://federated-learning.sherpa.ai/en/blog/biotechnology-accelerating-drug-discovery]
- 89. The Future of Drug Discovery: Integrating Phenotypic Data ... [https://ardigen.com/the-future-of-drug-discovery-integrating-phenotypic-data-with-omics-and-ai/]
- 90. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 91. Drug Discovery Chemistry 2025 [https://carterra-bio.com/drug-discovery-chemistry-2025/]
- 92. The behind-the-scenes chemistry driving drug discovery [https://www.stjude.org/research/progress/2025/the-behind-the-scenes-chemistry-driving-drug-discovery.html]
- 93. AI-driven target identification and validation [https://axxam.com/innovative-biology/target-identification-and-validation/]
- 94. Translational physiology: from molecules to public health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3731607/]
- 95. Translational physiology in practice [https://www.physoc.org/magazine-articles/translational-physiology-in-practice/]
- 96. Mapping the genome in 3D to reveal new drug targets [https://www.drugtargetreview.com/article/190646/mapping-the-genome-in-3d-to-reveal-new-drug-targets/]
- 97. The latest trends in drug discovery [https://www.cas.org/resources/cas-insights/2025-drug-discovery-trends]