The Intrinsic Resistome: Unlocking Bacterial Defenses to Forge Next-Generation Antimicrobial Strategies
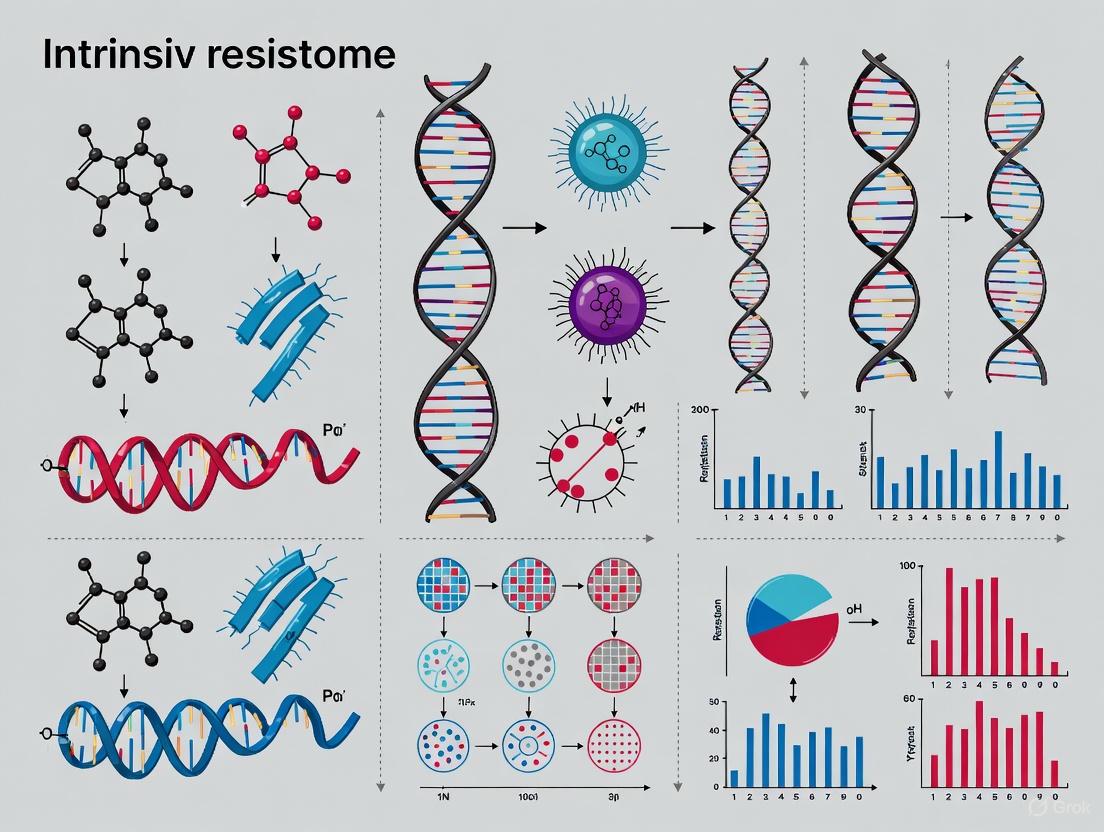
This article provides a comprehensive analysis of the intrinsic resistome—the complete set of chromosomal genes that contribute to the innate antibiotic resistance of bacterial pathogens.
The Intrinsic Resistome: Unlocking Bacterial Defenses to Forge Next-Generation Antimicrobial Strategies
Abstract
This article provides a comprehensive analysis of the intrinsic resistome—the complete set of chromosomal genes that contribute to the innate antibiotic resistance of bacterial pathogens. Tailored for researchers and drug development professionals, it explores the foundational concepts of intrinsic resistance, from core mechanisms like efflux pumps and membrane impermeability to the vast network of metabolic genes identified via genome-wide screens. The scope extends to methodological advances for resistome characterization, the challenges and evolutionary implications of targeting these pathways for antibiotic sensitization, and a comparative evaluation of resistance-breaking strategies. By synthesizing insights from genetic and pharmacological inhibition studies, this review aims to guide the development of novel adjuvants and 'resistance-proofing' therapeutic approaches to combat the escalating antimicrobial resistance crisis.
Deconstructing the Intrinsic Resistome: From Core Concepts to Ecological Origins
The intrinsic resistome encompasses the full complement of chromosomal genes that contribute to a bacterial pathogen's inherent susceptibility to antibiotics, independent of horizontal gene transfer or prior antibiotic exposure [1]. This concept represents a fundamental shift in how microbiologists understand and define bacterial resistance, moving beyond solely acquired mechanisms to include naturally occurring genetic determinants that form the baseline defensive capacity of a microorganism [2]. The clinical definition of antibiotic resistance has traditionally relied on breakpoints of minimal inhibitory concentrations (MICs) that predict therapeutic failure. In contrast, the ecological definition utilizes the ecological cut-off (ECOFF) value, which identifies the upper limit of the wild-type population's susceptibility [1]. The intrinsic resistome aligns with this ecological perspective, comprising elements that contribute directly or indirectly to antibiotic resistance regardless of clinical classification.
The intrinsic resistome includes not only classical resistance genes but also elements involved in basic bacterial metabolic processes [1]. These determinants collectively create the characteristic susceptibility phenotype of a bacterial species, representing what has been termed an "emergent property" resulting from the concerted action of numerous cellular components [1]. This conceptual framework has profound implications for understanding the evolution of resistance, the connection between bacterial metabolism and antibiotic susceptibility, and the development of novel therapeutic strategies to counteract resistance [2]. Research into the intrinsic resistome has revealed that its constituents can be categorized into two functional classes: genes whose inactivation increases antibiotic susceptibility (the bona fide intrinsic resistome) and those whose inactivation decreases susceptibility, thereby revealing potential evolutionary pathways to resistance [1].
Composition and Mechanisms of the Intrinsic Resistome
Core Components and Functional Classification
The intrinsic resistome comprises diverse genetic elements that collectively establish a bacterial strain's baseline antibiotic susceptibility profile. Table 1 summarizes the primary functional categories and their roles within the intrinsic resistome, demonstrating the mechanistic diversity underlying this fundamental bacterial characteristic.
Table 1: Functional Categorization of Intrinsic Resistome Elements
| Functional Category | Representative Elements | Mechanism of Action | Impact on Susceptibility |
|---|---|---|---|
| Antibiotic Efflux | AcrAB-TolC (E. coli), Mex efflux pumps (P. aeruginosa) | Active export of antibiotics from the cell | Broad-spectrum reduction in intracellular drug accumulation |
| Cell Envelope Permeability | Porins, Lipopolysaccharide structure | Restricts antibiotic entry into the cell | Reduced susceptibility to multiple drug classes |
| Drug Target Modification | Altered penicillin-binding proteins, Mutated RNA polymerase | Modification of antibiotic binding sites | Target-specific resistance |
| Metabolic Enzymes | Tricarboxylic acid cycle enzymes, Crc global regulator | Indirect modulation of cellular physiology | Altered susceptibility to multiple antibiotics |
| Chromosomal Resistance Genes | ampC β-lactamase, fosA fosfomycin resistance | Enzymatic inactivation of antibiotics | Drug class-specific resistance |
The functional diversity of intrinsic resistome elements underscores that antibiotic susceptibility is influenced by multiple interconnected cellular processes. While some components directly interact with antibiotics (e.g., efflux pumps, inactivating enzymes), others exert indirect effects through modulation of bacterial physiology [1] [2]. For instance, in Klebsiella pneumoniae, genes involved in routine cellular processes, including virulence, significantly contribute to the intrinsic resistance phenotype, demonstrating the pleiotropic nature of these determinants [2].
Quantitative Analysis of Resistome Components
Comparative analysis of intrinsic resistomes across bacterial species reveals significant variation in the number and type of contributing genes. Table 2 presents a quantitative overview of intrinsic resistome components identified through genome-wide studies in major bacterial pathogens, highlighting the scale and diversity of these defensive networks.
Table 2: Comparative Analysis of Intrinsic Resistome Components in Bacterial Pathogens
| Bacterial Pathogen | Total Genes Identified | Classical Resistance Genes | Metabolic/Miscellaneous Genes | Primary Screening Method |
|---|---|---|---|---|
| Klebsiella pneumoniae | 102 | ampG, acrB, tolC | Genes involved in virulence, basic physiology | Transposon mutant library screening [2] |
| Pseudomonas aeruginosa | 87 | Mex efflux components, ampC | Central metabolism, tRNA synthetases | High-throughput mutant screening [1] |
| Escherichia coli | Not specified | AcrAB efflux system | Multiple metabolic pathways | Transposon-directed insertion site sequencing [1] |
| Acinetobacter baylyi | 34 | Ade efflux components, β-lactamases | Cell envelope biogenesis, stress response | Plasmid-based gene overexpression [1] |
The quantitative data reveal that classical resistance mechanisms represent only a fraction of the intrinsic resistome, with numerous genes involved in fundamental cellular processes playing equally important roles in determining antibiotic susceptibility [2]. This expanded view of resistance determinants highlights the complexity of bacterial defense systems and explains why susceptibility phenotypes emerge from the integrated activity of diverse cellular components.
Methodologies for Intrinsic Resistome Analysis
High-Throughput Screening Approaches
Deciphering the intrinsic resistome requires systematic approaches to identify genes that influence antibiotic susceptibility. The following experimental workflow illustrates the primary methodology for genome-wide identification of intrinsic resistome components:
Genome-Wide Identification of Intrinsic Resistome Components
Two primary high-throughput methodologies dominate intrinsic resistome research: insertion or deletion library screening and plasmid library overexpression [1]. Insertion libraries, such as transposon-mutagenized collections, enable systematic assessment of how gene inactivation affects antibiotic susceptibility. This approach identified 102 genes influencing intrinsic resistance in K. pneumoniae, including both known resistance determinants and genes involved in basic physiological processes [2]. Alternatively, plasmid libraries containing genomic open reading frames allow researchers to evaluate how gene overexpression impacts resistance, particularly useful for identifying acquired resistance potential when transferred to heterologous hosts [1].
Advanced sequencing technologies have revolutionized intrinsic resistome analysis. Transposon-directed insertion site sequencing (Tn-Seq) combines traditional transposon mutagenesis with high-throughput sequencing to track mutant abundance after antibiotic exposure [2]. This method enables parallel assessment of thousands of mutations, identifying genes whose inactivation either increases or decreases antibiotic susceptibility. The main limitation of enrichment-based technologies is their bias toward mutations with minimal fitness costs, potentially missing important determinants that confer substantial fitness disadvantages [1].
Table 3: Essential Research Reagents for Intrinsic Resistome Studies
| Reagent/Resource | Function/Application | Specific Examples |
|---|---|---|
| Transposon Mutant Libraries | Genome-wide identification of susceptibility determinants | K. pneumoniae 52.145 library (5,320 mutants) [2] |
| Plasmid Expression Libraries | Assessment of gene overexpression effects | ORF libraries for E. coli, P. aeruginosa [1] |
| Specialized Culture Media | Selective growth conditions for mutant enrichment | LB medium for routine culture [2] |
| Antibiotic Stock Solutions | Selective pressure for mutant screening | Ciprofloxacin, polymyxin B, β-lactams [1] [2] |
| Bioinformatics Pipelines | Analysis of high-throughput sequencing data | MetaCompare for resistome risk assessment [3] |
| Reference Databases | Annotation of resistance genes and mechanisms | CARD, DeepARG-DB, mobileOG-DB [3] |
The research reagents outlined in Table 3 represent essential tools for comprehensive intrinsic resistome analysis. The development of standardized mutant libraries, such as the K. pneumoniae 52.145 transposon library containing 5,320 independent mutants, enables systematic screening across multiple antibiotic classes [2]. Complementing these experimental resources, bioinformatics pipelines like MetaCompare 2.0 provide computational frameworks for assessing resistome risk, differentiating between ecological and human health concerns by analyzing ARG mobility and host associations [3].
Case Studies: Paradigms of Intrinsic Resistance
The Intrinsic Resistome ofKlebsiella pneumoniae
Klebsiella pneumoniae represents a paradigm for intrinsic resistome research due to its clinical significance as an ESKAPE pathogen. A comprehensive analysis of a K. pneumoniae transposon mutant library identified 102 genes influencing antibiotic susceptibility to various drug classes [2]. This study revealed that only 27% of the identified genes represented classical resistance determinants, while the majority were involved in standard bacterial physiological processes. Particularly noteworthy was the discovery that 15 of the identified insertions were located in plasmid backbone genes rather than chromosomal elements, suggesting that plasmid scaffolds may harbor previously unrecognized resistance determinants beyond acquired resistance genes [2].
The K. pneumoniae intrinsic resistome includes expected elements such as the acrB and tolC efflux pump components and the ampG β-lactamase regulator, but also encompasses genes involved in central metabolism, tRNA synthesis, and virulence [2]. This functional diversity demonstrates that the intrinsic resistance phenotype emerges from interconnected cellular systems rather than discrete resistance mechanisms. The presence of intrinsic resistome elements on plasmids is particularly significant from an evolutionary perspective, as these genes may be co-transferred with acquired resistance determinants, potentially accelerating the development of multi-drug resistant strains.
Comparative Analysis of Gram-Negative Intrinsic Resistomes
Comparative analysis across Gram-negative pathogens reveals both conserved and species-specific elements within intrinsic resistomes. Pseudomonas aeruginosa exhibits formidable intrinsic resistance largely attributable to its low outer membrane permeability and constitutive expression of efflux systems like MexAB-OprM [1] [4]. The global regulator Crc in P. aeruginosa plays a significant role in coordinating metabolic functions with antibiotic susceptibility, demonstrating the connection between central metabolism and resistance phenotypes [1].
Escherichia coli possesses a well-characterized intrinsic resistome centered on the AcrAB-TolC efflux system, which contributes to natural resistance to macrolides, dyes, and detergents [1]. Research indicates that macrolides could potentially be effective against Gram-negative infections if combined with efflux pump inhibitors, highlighting the therapeutic implications of understanding intrinsic resistance mechanisms [1]. The variation in intrinsic resistome composition between bacterial species helps explain their characteristic susceptibility profiles and provides insights into the evolutionary adaptation of pathogens to antibiotic stress.
Research Implications and Future Directions
Therapeutic Applications and Resistance Inhibition
Understanding the intrinsic resistome opens innovative avenues for therapeutic intervention. Identifying genes that increase susceptibility when inactivated provides targets for potential resistance-breaking inhibitors that could restore antibiotic efficacy [1]. This approach mirrors the successful development of β-lactamase inhibitors, which are now routinely combined with β-lactams to overcome acquired resistance [1]. Efflux pump inhibitors represent another promising strategy, potentially expanding the spectrum of existing antibiotics to include intrinsically resistant pathogens [1].
The recognition that bacterial metabolism profoundly influences antibiotic susceptibility suggests additional therapeutic opportunities. Small molecules that disrupt metabolic pathways connected to intrinsic resistance could potentiate conventional antibiotics [1] [2]. For instance, inhibiting the Crc global regulator in P. aeruginosa might increase susceptibility to multiple antibiotic classes by altering the expression of intrinsic resistance elements [1]. These approaches require careful evaluation of selectivity to avoid detrimental effects on host cells or beneficial microbiota.
One Health Perspective and Ecological Considerations
The intrinsic resistome concept extends beyond clinical settings to encompass environmental and agricultural dimensions through the One Health framework [5]. Environmental bacteria represent the evolutionary source of many resistance genes that eventually emerge in clinical pathogens, with estimates suggesting that antibiotic resistance predates human antibiotic use by millions of years [5] [6]. Understanding the natural resistome in pristine environments provides a baseline for tracking human-mediated impacts on resistance dissemination.
Anthropogenic activities significantly influence resistome dynamics across ecosystems. Studies demonstrate that river systems receiving wastewater treatment plant effluent show increased abundance and diversity of resistance genes compared to pristine environments [5]. Similarly, agricultural practices, particularly livestock farming, contribute to the dissemination of resistance elements through environmental pathways [5] [7]. This ecological perspective highlights the importance of integrated surveillance strategies that monitor resistance emergence across human, animal, and environmental sectors to effectively combat the global antimicrobial resistance crisis.
The intrinsic resistome represents a fundamental component of bacterial defense systems, encompassing chromosomal genes that collectively determine baseline antibiotic susceptibility. Moving beyond the traditional focus on acquired resistance, this concept recognizes that antibiotic susceptibility emerges from the integrated activity of diverse cellular components, including classical resistance elements, metabolic enzymes, and global regulators. High-throughput methodologies have enabled comprehensive mapping of intrinsic resistomes in major pathogens, revealing unexpected connections between core cellular processes and antibiotic resistance.
The therapeutic implications of intrinsic resistome research are substantial, suggesting novel strategies to potentiate existing antibiotics through targeted inhibition of resistance mechanisms. From a broader perspective, understanding the flow of resistance elements between environmental and clinical settings through the One Health framework is essential for managing the global antimicrobial resistance crisis. As research continues to unravel the complexity of bacterial defense systems, the intrinsic resistome concept provides a foundational framework for developing next-generation approaches to combat antibiotic-resistant infections.
The intrinsic resistome encompasses the complete set of chromosomal elements that contribute to the innate antibiotic resistance of a bacterial pathogen, independent of acquired genetic mutations or horizontal gene transfer [8]. This inherent defensive capacity is a major contributor to the resilience of Gram-negative pathogens, complicating treatment and drug development efforts. The core mechanisms of this defense system are efflux pumps, membrane impermeability, and enzymatic inactivation, which often function synergistically to protect the bacterial cell [9]. Understanding these mechanisms is crucial for developing strategies to overcome multidrug resistance, particularly as the pipeline of new antibiotics continues to diminish. This review examines the molecular basis, regulation, and interplay of these defense systems within the framework of the intrinsic resistome, providing a technical foundation for researchers and drug development professionals working to combat antibiotic-resistant pathogens.
Membrane Impermeability: The Initial Barrier
The outer membrane (OM) of Gram-negative bacteria constitutes the first and most formidable barrier against antimicrobial agents. This sophisticated structure possesses unique architectural features that severely restrict compound entry, providing innate protection even in the absence of other resistance mechanisms.
Structural and Functional Organization
The Gram-negative OM is an asymmetric lipid bilayer with distinct composition in each leaflet. The inner leaflet consists primarily of phospholipids (approximately 80% phosphatidylethanolamine, 15% phosphatidylglycerol, and 5% cardiolipin), while the outer leaflet is composed of lipopolysaccharides (LPS) that create a densely packed, impermeable surface [10]. The LPS molecules are stabilized by divalent cations (Mg²⁺ and Ca²⁺) that bridge phosphate groups, further reducing membrane fluidity and creating an effective barrier against hydrophobic compounds [9]. This structural organization allows the OM to function as a highly selective filter, permitting nutrient uptake while excluding many harmful molecules, including numerous antibiotics.
Porin-Mediated Permeation
Hydrophilic antibiotics, such as β-lactams, rely primarily on porin channels for entry into the bacterial cell. These β-barrel proteins form water-filled channels that traverse the OM, acting as size-exclusion filters with defined physicochemical selectivity [10]. The composition and expression of porins significantly influence intrinsic susceptibility profiles across bacterial species and strains.
Table 1: Major Porins in Gram-Negative Bacterial Pathogens and Their Roles in Antibiotic Permeation
| Organism | Porin | Substrate Specificity | Role in Antibiotic Resistance |
|---|---|---|---|
| Escherichia coli | OmpF | Small hydrophilic molecules, β-lactams | Reduced expression decreases susceptibility to carbapenems, fluoroquinolones |
| Escherichia coli | OmpC | Small hydrophilic molecules | Mutations can restrict antibiotic influx |
| Klebsiella pneumoniae | OmpK36 | Carbapenems, cephalosporins | Loss associated with carbapenem resistance |
| Klebsiella pneumoniae | OmpK35 | β-lactams | Porin loss combined with ESBLs confers resistance |
| Pseudomonas aeruginosa | OprD | Basic amino acids, carbapenems | Specific for imipenem uptake; downregulation causes resistance |
| Enterobacter aerogenes | Omp36 | β-lactams | Modified expression in clinical resistant isolates |
The strategic importance of porins is exemplified by the correlation between porin modifications and clinical resistance. For instance, in K. pneumoniae, the loss of OmpK35 and OmpK36 porins, when combined with extended-spectrum β-lactamases (ESBLs), can lead to resistance to later-generation cephalosporins and carbapenems [10]. Similarly, in P. aeruginosa, the specific porin OprD facilitates imipenem uptake, and its downregulation represents a major carbapenem resistance mechanism in clinical isolates [10].
Efflux Pumps: Multidrug Extrusion Systems
Multidrug efflux pumps are ubiquitous transmembrane transporters that actively extrclude toxic compounds, including antibiotics, from the bacterial cell. These systems contribute significantly to both intrinsic and acquired resistance through their broad substrate recognition capabilities.
Major Efflux Pump Families
Bacteria encode several structurally distinct families of efflux pumps, each with unique energy coupling mechanisms and structural organizations:
Table 2: Major Families of Bacterial Multidrug Efflux Pumps
| Efflux Pump Family | Energy Source | Structural Organization | Representative Members | Key Antibiotic Substrates |
|---|---|---|---|---|
| RND (Resistance-Nodulation-Division) | Proton motive force | Tripartite complex (IMP-MFP-OMP) | AcrAB-TolC (E. coli), MexAB-OprM (P. aeruginosa) | β-lactams, macrolides, fluoroquinolones, tetracyclines, chloramphenicol |
| MFS (Major Facilitator Superfamily) | Proton motive force | Single-component transporters | NorA (S. aureus), PmrA (S. pneumoniae) | Fluoroquinolones, tetracyclines, chloramphenicol |
| ABC (ATP-Binding Cassette) | ATP hydrolysis | Single or multi-component | MsrA (S. aureus) | Macrolides, streptogramins |
| SMR (Small Multidrug Resistance) | Proton motive force | Four transmembrane segments | EmrE (E. coli) | Disinfectants, some antibiotics |
| MATE (Multidrug and Toxic Compound Extrusion) | Proton motive force or Na+ gradient | Twelve transmembrane segments | NorM (V. parahaemolyticus) | Fluoroquinolones, aminoglycosides |
The RND superfamily represents the most clinically significant efflux systems in Gram-negative pathogens due to their broad substrate profiles and essential contribution to intrinsic resistance [8] [11]. These tripartite complexes span the entire cell envelope, comprising an inner membrane pump (IMP) that drives extrusion, a membrane fusion protein (MFP) that spans the periplasmic space, and an outer membrane factor (OMF) that forms an exit channel through the outer membrane [11].
Regulation and Physiological Functions
Efflux pumps are tightly regulated chromosomal elements that serve essential physiological functions beyond antibiotic resistance. These transporters facilitate the extrusion of bacterial metabolites, quorum-sensing signals, organic pollutants, heavy metals, and plant-produced compounds [8]. This multifunctional role explains their conservation across bacterial species and their presence in all natural isolates.
In P. aeruginosa, the expression of RND pumps like MexAB-OprM is influenced by specific regulatory systems, and mutations in these regulators lead to pump overexpression and consequent multidrug resistance [11]. Similarly, in S. aureus, expression of the NorA efflux pump varies significantly across isolates, with elevated expression potentiating the evolution of ciprofloxacin resistance by increasing the fitness benefit provided by target site mutations [12].
Diagram 1: Regulatory pathways controlling RND efflux pump expression and their relationship to resistance outcomes. Regulatory mutations can lead to constitutive overexpression and treatment failure.
Quantitative Contribution in Clinical Isolates
The quantitative contribution of efflux to multidrug resistance in clinical isolates has been systematically evaluated through genetic studies. Research demonstrates that deleting tolC (encoding the outer membrane channel for multiple RND pumps) in clinical E. coli isolates abolishes detectable efflux activity in most strains and modulates antibiotic susceptibility [13]. However, these efflux-deficient mutants typically retain multidrug resistance due to the presence of other resistance mechanisms, highlighting that efflux inhibition alone may be insufficient to restore full antibiotic susceptibility in clinical settings when other resistance determinants are present [13].
Enzymatic Inactivation: Chemical Modification of Antibiotics
Bacteria produce numerous enzymes that directly modify or degrade antibiotics, rendering them ineffective before they reach their cellular targets. This mechanism represents one of the most versatile and widespread strategies for antibiotic resistance.
Major Enzyme Classes and Mechanisms
Enzymatic resistance can be categorized based on the biochemical strategy employed to neutralize antibiotics:
Table 3: Major Enzymatic Mechanisms of Antibiotic Inactivation
| Enzyme Class | Target Antibiotics | Catalytic Mechanism | Representative Enzymes |
|---|---|---|---|
| β-Lactamases | β-Lactams (penicillins, cephalosporins, carbapenems) | Hydrolysis of β-lactam ring | TEM-1, CTX-M, KPC, NDM, OXA-48 |
| Aminoglycoside-Modifying Enzymes | Aminoglycosides | Acetylation, adenylation, or phosphorylation of hydroxyl or amino groups | AAC(6')-Ib, ANT(2")-Ia, APH(3')-Ia |
| Chloramphenicol Acetyltransferases | Chloramphenicol | Acetylation of hydroxyl groups | CAT variants |
| Macrolide Esterases | Macrolides | Hydrolysis of lactone ring | EreA, EreB |
| Rifamycin ADP-ribosyltransferases | Rifamycins | ADP-ribosylation | Arr variants |
β-Lactamases constitute the most diverse and clinically significant family of antibiotic-inactivating enzymes. These enzymes have evolved to recognize and hydrolyze nearly all classes of β-lactam antibiotics, with the extended-spectrum β-lactamases (ESBLs) and carbapenemases posing particularly serious clinical threats [14] [9].
Target Modification Enzymes
Beyond direct antibiotic inactivation, bacteria employ enzymes that modify antibiotic targets, reducing drug binding affinity. Methyltransferases that modify ribosomal RNA represent a particularly important mechanism, as they can confer resistance to multiple classes of ribosome-targeting antibiotics simultaneously [9]. For example, erm genes encode methyltransferases that add methyl groups to specific adenine residues in the 23S rRNA, preventing binding of macrolides, lincosamides, and streptogramin B antibiotics (the MLSB phenotype) [14].
Similarly, modification of the peptidoglycan precursor lipid A by phosphoethanolamine transferases (e.g., MCR enzymes) reduces binding of the last-resort antibiotic colistin, representing a significant threat to treatment of multidrug-resistant Gram-negative infections [9].
Experimental Approaches and Methodologies
Assessing Efflux Pump Activity
Genetic Deletion of Efflux Components: The most definitive method for evaluating efflux contribution involves genetic deletion of essential pump components. For E. coli, this typically entails deleting tolC, which encodes the outer membrane channel required for multiple RND systems [13]. In P. aeruginosa, similar approaches target oprM or other outer membrane factors [13]. A versatile method for genetic engineering in multidrug-resistant clinical isolates utilizes a thiopurine-S-methyltransferase (tpm) selection marker that confers resistance to tellurite, enabling selection in strains resistant to conventional antibiotics [13]. Following the first recombination event, negative selection employs sucrose sensitivity conferred by levansucrase (sacB) in NaCl-free media to identify double-crossover mutants [13].
Flow Cytometry with Fluorescent Probes: Efflux activity can be quantified at single-cell resolution using fluorescent substrates and flow cytometric analysis [15]. Propidium iodide (PI) uptake serves as a reliable indicator of membrane integrity and efflux function, as this hydrophilic fluorescent dye is excluded by cells with functional membranes and active efflux [15]. Protocol: Harvest bacterial cells by centrifugation and resuspend in appropriate buffer. Incubate with fluorescent efflux substrates (e.g., ethidium bromide, Hoechst 33342) with or without efflux pump inhibitors. Analyze using flow cytometry with appropriate excitation/emission settings. Data interpretation should account for bacterial morphology, as larger cells may be more easily permeabilized than smaller cells [15].
Membrane Permeability Assays
Outer Membrane Permeability Measurement: The liposome swelling assay provides a quantitative measure of porin-mediated permeability [10]. Method: Prepare liposomes containing bacterial porins. Suspend liposomes in isosmotic solutions of test antibiotics and monitor swelling by light scattering or absorbance. Compare permeability rates to reference compounds with known diffusion characteristics.
Quantitative Mass Spectrometry for Antibiotic Influx: Recent advances employ mass spectrometry to directly quantify antibiotic accumulation in bacterial cells [10]. Protocol: Expose bacterial cultures to target antibiotics under controlled conditions. Rapidly separate cells from medium by filtration or centrifugation. Extract intracellular compounds and analyze by LC-MS/MS using appropriate internal standards. Normalize antibiotic concentrations to cell number or protein content.
Enzyme Activity Characterization
β-Lactamase Activity Assays: Hydrolytic activity against β-lactam antibiotics can be monitored spectrophotometrically by tracking absorbance changes associated with β-lactam ring cleavage [14]. Nitrocefin serves as a preferred chromogenic substrate due to its dramatic color change upon hydrolysis. For quantitative kinetic analysis: Prepare purified enzyme or cell lysates. Incubate with nitrocefin and monitor absorbance at 486 nm continuously. Calculate kinetic parameters (Km, kcat) from initial velocity measurements at varying substrate concentrations.
Molecular Characterization of Enzyme Variants: Cloning and expression of resistance genes followed by site-directed mutagenesis enables functional characterization of specific mutations [14]. Protocol: Amplify resistance genes from clinical isolates. Clone into expression vectors. Introduce point mutations using overlap extension PCR or commercial mutagenesis kits. Express and purify recombinant proteins. Determine MIC changes and kinetic parameters for wild-type and mutant enzymes.
Diagram 2: Integrated experimental workflow for comprehensive analysis of resistance mechanisms, combining genomic, phenotypic, genetic, and mechanistic approaches.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Studying Intrinsic Resistance Mechanisms
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Efflux Pump Inhibitors | PAβN (Phe-Arg-β-naphthylamide), CCCP (carbonyl cyanide m-chlorophenyl hydrazone), pyridopyrimidines, arylpiperazines | Competitive or allosteric inhibition of RND pumps; mechanistic studies | PAβN inhibits several but not all RND pumps; CCCP dissipates proton motive force but affects overall cell physiology |
| Fluorescent Efflux Substrates | Ethidium bromide, Hoechst 33342, propidium iodide | Flow cytometric quantification of efflux activity; membrane integrity assessment | Propidium iodide (PI) uptake indicates membrane permeabilization; excluded by intact cells |
| Genetic Engineering Tools | Tellurite resistance marker (tpm), sacB counter-selection, λ-Red recombinase system | Gene deletion in multidrug-resistant clinical isolates | Tellurite resistance enables selection in antibiotic-resistant strains; sacB provides negative selection |
| β-Lactamase Substrates | Nitrocefin, CENTA, fluorogenic cephalosporins | Spectrophotometric/fluorometric detection of β-lactamase activity | Nitrocefin provides visual color change; CENTA offers superior spectrophotometric properties |
| Antibiotic Accumulation Assays | Radiolabeled antibiotics (e.g., ³H-tetracycline), LC-MS/MS protocols | Quantitative measurement of intracellular antibiotic concentrations | LC-MS/MS provides specificity and sensitivity without radioactivity requirements |
| Porin Reconstitution Kits | Liposome swelling assay components | In vitro assessment of porin permeability | Requires purified porins; provides controlled system for permeability studies |
The intrinsic resistome of bacterial pathogens represents a formidable challenge in antimicrobial therapy, with efflux pumps, membrane impermeability, and enzymatic inactivation functioning as interconnected defense systems. The quantitative contribution of each mechanism varies across bacterial species and clinical isolates, but their combined effect creates a robust barrier to antibiotic efficacy [13]. Future research directions should focus on leveraging this understanding to develop novel therapeutic approaches, including efflux pump inhibitors that restore antibiotic susceptibility [8], compound engineering to bypass permeability barriers [10] [9], and β-lactamase inhibitors that overcome enzymatic inactivation [11]. The application of CRISPR/Cas9-based technologies for targeted editing of resistance genes in bacterial populations represents an emerging strategy to reverse resistance determinants [16]. As our understanding of the intrinsic resistome deepens, so too will our ability to develop innovative strategies to overcome these defense mechanisms and preserve the efficacy of existing and future antibiotics.
The antibiotic resistome encompasses the entire collection of antibiotic resistance genes (ARGs), their precursors, and associated expression and regulation machinery within microbial communities. Groundbreaking research over the past decade has fundamentally shifted our understanding, revealing that resistance is not a modern clinical artifact but an ancient and ubiquitous natural trait deeply embedded in the global microbiome. This whitepaper synthesizes evidence that the environmental resistome constitutes a vast genetic reservoir from which clinically relevant resistance can be mobilized. Understanding the resistome's ecological origins, evolutionary dynamics, and transmission pathways is critical for informing the development of novel therapeutic strategies and addressing the escalating antimicrobial resistance (AMR) crisis.
The term "antibiotic resistome" was first coined in 2006 to describe the collective resistance determinants present in soil bacteria, revealing a previously unappreciated breadth of multidrug resistance in environmental microbial communities [17] [5]. The concept has since been refined to include all types of ARGs—including acquired resistance genes (horizontally or vertically transferred), intrinsic resistance genes (taxa-specific, vertically transmitted), silent/cryptic resistance genes (functional but not expressed), and proto-resistance genes (requiring evolution to confer full resistance) [5] [18].
This framework positions the resistome as a fundamental and ancient component of microbial genomes, predating human antibiotic use by millennia. The resistome's foundations were laid long before the clinical introduction of antibiotics, with its constituent genes participating in complex ecological interactions beyond mere antibiotic defense [19] [18]. This perspective necessitates a paradigm shift from viewing resistance as a clinical problem to understanding it as a natural biological phenomenon with profound implications for pathogen evolution and drug discovery.
The Ancient and Ubiquitous Nature of the Resistome
Genetic and Biochemical Evidence of Ancient Origins
Compelling evidence for the resistome's antiquity comes from the analysis of ancient DNA. Metagenomic studies of Beringian permafrost dating back thousands of years have identified functional resistance genes for β-lactam, tetracycline, and glycopeptide antibiotics [17] [18]. Biochemical characterization of the ancient VanA protein, critical for vancomycin resistance, demonstrated a conserved three-dimensional structure and function compared to modern variants, confirming that resistance mechanisms were operative long before the antibiotic era [18].
Further evidence comes from isolated environments with limited anthropogenic influence. Bacteria collected from Lechuguilla Cave, isolated from surface input for over four million years, exhibited phenotypic resistance to 14 different antibiotic classes [18]. Genotypic and biochemical analyses confirmed that the resistance determinants in these pristine microbial communities were functionally conserved with those found in modern clinical pathogens, underscoring that ARGs are intrinsic components of the microbial pangenome, independent of human selection pressure [18].
The Environmental Resistome as a Primary Reservoir
The soil environment is recognized as the origin and a major reservoir of the antibiotic resistome [17] [5]. Soil-dwelling Actinobacteria and other environmental bacteria are prolific producers of antimicrobial compounds, and for viability, antibiotic production must evolve alongside self-protection resistance mechanisms [18]. This co-evolution has resulted in a vast and diverse environmental resistome.
Metagenomic surveys reveal that nearly all known classes of ARGs can be found in soil, water, and other environmental niches [17] [5]. The functional diversity of this reservoir is immense, with studies of soil metagenomes identifying nearly 200 distinct antibiotic resistance profiles among cultured isolates, demonstrating a robust and multifaceted defense capacity against both natural and synthetic antibiotics [17]. The table below summarizes key evidence for the ancient and ubiquitous nature of the resistome.
Table 1: Evidence Supporting the Ancient and Ubiquitous Nature of the Resistome
| Evidence Source | Key Findings | Implications |
|---|---|---|
| Ancient Permafrost [17] [18] | Identification of functional β-lactam, tetracycline, and glycopeptide resistance genes (e.g., vanHAX) in ancient DNA. | Resistance mechanisms were fully functional millennia before modern antibiotic use. |
| Lechuguilla Cave Bacteria [18] | Phenotypic resistance to 14 drug classes in bacteria isolated for ~4 million years. | ARGs are ancient, ubiquitous, and conserved components of the microbial pangenome. |
| Global Soil Metagenomes [17] | ~200 distinct antibiotic resistance profiles observed in soil bacteria across diverse environments. | The environmental resistome is highly diverse and robust, providing a deep resistance reservoir. |
| Comprehensive Antibiotic Resistance Database (CARD) [17] | Compilation of thousands of potential resistance genes from bacterial genomic data. | The genetic potential for resistance is vast and widely distributed across bacterial taxa. |
The Intrinsic Resistome of Bacterial Pathogens
The intrinsic resistome refers to the set of chromosomal genes in a bacterial pathogen that contribute to its innate, baseline level of resistance to antibiotics, excluding acquired mechanisms. These genes are not acquired via horizontal gene transfer but are part of the core genome and can be mutated or dysregulated to confer higher-level resistance [5]. The intrinsic resistome represents a significant challenge in treating infections, particularly those caused by Gram-negative bacteria.
Key Mechanisms of the Intrinsic Resistome
The primary mechanisms of intrinsic resistance involve limiting drug uptake and increasing drug efflux, effectively reducing the intracellular concentration of the antibiotic to a sub-lethal level [20] [21].
- Reduced Permeability of the Outer Membrane: The lipopolysaccharide (LPS) layer in Gram-negative bacteria acts as a formidable permeability barrier, intrinsically resistant to many antimicrobials, including glycopeptides and lipopeptides [20].
- Efflux Pump Systems: Chromosomally encoded multidrug efflux pumps, such as the AcrAB-TolC system in E. coli, can export a wide range of structurally diverse antibiotics, contributing to intrinsic and inducible resistance [20] [22] [23].
- Spontaneous Mutations in Core Genes: Mutations in housekeeping genes can lead to target modification or upregulation, bypassing antibiotic effects without the acquisition of foreign DNA [20].
Experimental Dissection of the Intrinsic Resistome
Genome-wide functional screens have been instrumental in identifying the genetic determinants of intrinsic resistance. A 2025 study performed a systematic screen of the E. coli Keio collection (~3,800 single-gene knockouts) to identify mutants hypersusceptible to trimethoprim and chloramphenicol [22] [23]. The workflow and key findings of this screen are detailed below.
Diagram 1: Workflow for a genome-wide intrinsic resistome screen.
The screen identified 35 and 57 knockouts that were hypersensitive to trimethoprim and chloramphenicol, respectively [22] [23]. Functional enrichment analysis revealed that genes involved in cell envelope biogenesis (e.g., rfaG, lpxM), membrane transport (e.g., acrB), and information transfer were overrepresented [22] [23]. The table below quantifies the susceptibility of key knockout strains validated in the study.
Table 2: Key Hypersensitive Knockout Strains from E. coli Genome-Wide Screen [22] [23]
| Knockout Gene | Gene Function | Phenotype | Validated Hypersensitivity to Trimethoprim |
|---|---|---|---|
| acrB | Component of AcrAB-TolC multidrug efflux pump | Reduced antibiotic efflux | Highest level of sensitization |
| rfaG | Lipopolysaccharide glucosyl transferase I | Perturbed outer membrane permeability | Strong hypersensitivity |
| lpxM | Lipid A myristoyl transferase | Altered lipopolysaccharide structure | Strong hypersensitivity |
| nudB | Dihydroneopterin triphosphate diphosphatase | Impaired folate biosynthesis | Drug-specific hypersensitivity |
One Health Perspective: Transmission Across Ecological Niches
The One-Health framework, which integrates human, animal, and environmental health, is essential for understanding the transmission and evolution of the resistome [5]. ARGs are not confined to single sectors but flow across interfaces, with the environment acting as a source and sink for resistance elements.
Reservoirs and Hotspots
- Natural Environments: Pristine soils, oceans, and rivers harbor diverse and ancient resistomes [17] [5]. However, anthropogenic activities significantly impact these reservoirs. Studies show that human-impacted river sites have a higher abundance and diversity of ARGs compared to pristine sites, with wastewater treatment plants (WWTPs) identified as major pollution sources and hotspots for horizontal gene transfer (HGT) [17] [5].
- Animals: Wildlife and livestock serve as important reservoirs. A large-scale genomic analysis of wild rodent gut microbiota identified 8,119 ARGs, with Enterobacteriaceae, particularly E. coli, being dominant carriers [24]. A strong correlation was observed between ARGs, virulence factor genes (VFGs), and mobile genetic elements (MGEs), highlighting the potential for co-selection and mobilization of resistance and virulence traits from wildlife to human populations [24].
- Humans: The human microbiome, including the gut and nasopharynx, harbors a complex resistome. The nasopharyngeal resistome, in particular, is a critical reservoir for the emergence of resistance in pathogens causing pneumonia, meningitis, and sepsis [18].
Mechanisms of Horizontal Gene Transfer
The mobilization of ARGs from environmental reservoirs to human pathogens occurs primarily through HGT [17]. Key mechanisms include:
- Conjugation: The plasmid-mediated transfer of genetic material, which is the most common route for ARG acquisition [20].
- Transformation: The uptake of free environmental DNA by naturally competent bacteria [20].
- Transduction: The bacteriophage-mediated transfer of genetic material [20].
The presence of ARGs on MGEs such as plasmids, transposons, and integrons is a critical factor determining their mobility and clinical relevance [17] [24]. The following diagram illustrates the flow of ARGs within the One-Health framework.
Diagram 2: The One-Health perspective on ARG transmission. MGEs facilitate ARG flow between all sectors.
Experimental Protocols for Resistome Research
Protocol: Genome-Wide Screen for Intrinsic Resistance Genes
This protocol is adapted from Balachandran et al. (2025) for identifying bacterial genes involved in intrinsic resistance [22] [23].
Objective: To identify single-gene knockouts that confer hypersensitivity to a specific antibiotic, thereby pinpointing genes that constitute the intrinsic resistome.
Materials:
- Keio Collection of E. coli knockouts or equivalent single-gene knockout library.
- Luria-Bertani (LB) broth and agar.
- Antibiotic stock solutions: Prepare trimethoprim, chloramphenicol, and other antibiotics of interest at appropriate concentrations.
- 96-well microtiter plates (sterile).
- Plate reader capable of measuring optical density at 600 nm (OD₆₀₀).
- Automated liquid handling system (recommended for high-throughput).
Procedure:
- Inoculation and Growth: From frozen glycerol stocks, inoculate knockout strains in duplicate into 200 µL of LB broth in 96-well plates. Include a wild-type control strain on every plate.
- Antibiotic Challenge: Grow cultures in the presence of the test antibiotic at a predetermined IC₅₀ concentration, and in a no-antibiotic control.
- Growth Measurement: Incubate plates with shaking and measure OD₆₀₀ at regular intervals until the wild-type control in the no-antibiotic condition reaches mid-log phase.
- Data Analysis:
- Calculate the average OD₆₀₀ for each knockout strain in the antibiotic condition.
- Normalize the data by expressing the OD as a fraction of the wild-type growth (fold over wild type).
- Plot the distribution of normalized growth values. It should approximate a Gaussian distribution with a mean of ~1.
- Classify knockouts with growth lower than two standard deviations from the median of the distribution as "hypersensitive."
- Validation: Confirm hypersensitivity by spotting knockout strains on LB agar plates containing the antibiotic at Minimum Inhibitory Concentration (MIC), MIC/3, and MIC/9. Assess compromised colony formation compared to the wild type.
Protocol: Experimental Evolution to Assess "Resistance-Proofing"
Objective: To evaluate the potential of targeting intrinsic resistance pathways to slow or prevent the evolution of de novo antibiotic resistance.
Materials:
- Hypersensitive knockout strains (e.g., ΔacrB, ΔrfaG, ΔlpxM).
- Wild-type parental strain.
- Antibiotic stock solutions.
- Flask or bioreactor for serial passaging.
Procedure:
- Evolution Setup: Initiate multiple (e.g., 8-12) independent replicate cultures of each knockout and the wild-type strain in a medium containing the antibiotic at a high selection pressure (e.g., near MIC) and a sub-inhibitory concentration.
- Serial Passaging: Daily, transfer a small aliquot of each culture into fresh medium containing the same concentration of antibiotic. Continue passaging for multiple generations (e.g., 20-30 days).
- Monitoring: Regularly monitor and record the growth (OD) of the cultures.
- Endpoint Analysis:
- Extinction Rate: Calculate the frequency at which knockout populations go extinct compared to wild-type populations under high drug pressure.
- Resistance Development: For populations that adapt, sequence the genomes of evolved clones to identify resistance-conferring mutations (e.g., in folA for trimethoprim resistance).
- Recovery Assessment: Measure the fitness and MIC of evolved clones to determine the extent of recovery from the initial hypersensitivity.
Table 3: Essential Research Materials for Intrinsic Resistome Studies
| Reagent / Resource | Function and Application in Resistome Research |
|---|---|
| Keio Collection (E. coli) [22] [23] | A curated library of ~3,800 single-gene knockouts, enabling genome-wide screens for identifying genes involved in intrinsic resistance and antibiotic hypersensitivity. |
| Comprehensive Antibiotic Resistance Database (CARD) [17] | A bioinformatic resource and database containing sequences, detection models, and curated information on ARGs, essential for annotating resistomes from genomic and metagenomic data. |
| Efflux Pump Inhibitors (EPIs)(e.g., Chlorpromazine, Piperine) [22] [23] | Small molecules used to chemically inhibit multidrug efflux pumps (e.g., AcrAB-TolC). Used to validate the role of efflux in intrinsic resistance and as potential antibiotic adjuvants. |
| Defined Gene Knockout Mutants(e.g., ΔacrB, ΔrfaG, ΔlpxM) [22] [23] | Clean genetic backgrounds for controlled experiments to characterize the specific contribution of intrinsic resistance mechanisms to antibiotic susceptibility and resistance evolution. |
| Metagenomic Sequencing Datasets(e.g., Tara Oceans, Earth Microbiome Project) [17] [5] [24] | Publicly available data from diverse environmental and host-associated microbiomes, allowing for large-scale comparative analysis of resistome structure, diversity, and distribution. |
The ecological perspective of the resistome fundamentally alters our approach to antimicrobial resistance. Recognizing resistance as an ancient, natural, and widely distributed trait forces a reconsideration of drug discovery and stewardship. The intrinsic resistome of bacterial pathogens represents a formidable barrier to therapy, yet its constituent pathways also present new targets for "resistance-breaking" adjuvants. Future research must leverage the One-Health approach to track critical ARGs at the human-animal-environment interface, elucidate the selective pressures driving their mobilization, and develop interventions that can "resistance-proof" existing antibiotics by targeting the very foundations of bacterial defense. A deep understanding of the resistome's ecological and evolutionary dynamics is our best strategy for mitigating the global AMR crisis.
The intrinsic antibiotic resistome encompasses the naturally occurring, chromosomally encoded mechanisms that enable bacterial survival upon exposure to antimicrobial agents, predating the clinical use of antibiotics [25]. In Gram-negative pathogens, this intrinsic resistance presents a formidable barrier to treatment, largely mediated by a restrictive outer membrane permeability barrier and chromosomally encoded efflux pumps that actively remove toxic compounds from the cell [23] [22]. The clinical significance of intrinsic resistance is profound, particularly in opportunistic pathogens like Pseudomonas aeruginosa and extraintestinal pathogenic Escherichia coli (ExPEC), where it complicates therapy and contributes to poor patient outcomes. For researchers and drug development professionals, understanding these core resistance networks is essential for designing novel therapeutic strategies that circumvent these innate bacterial defenses [26] [27].
The global health impact of antibiotic resistance underscores the urgency of this research. Antimicrobial resistance is projected to cause 10 million deaths annually by 2050 if left unaddressed, with resistant Gram-negative pathogens representing a substantial portion of this threat [28]. In India, for instance, 50-80% of hospital isolates of E. coli and Klebsiella pneumoniae in 2021 were resistant to beta-lactams, fluoroquinolones, or cephalosporins [23]. Similarly, P. aeruginosa is classified by the WHO as a "critical" priority pathogen due to rising carbapenem resistance rates exceeding 30% in some regions, severely limiting treatment options for life-threatening infections [27]. This review examines the intrinsic resistomes of E. coli and P. aeruginosa as case studies, providing a technical framework for researchers investigating resistance mechanisms and developing novel therapeutic interventions.
TheE. coliIntrinsic Resistome: Mechanisms and Experimental Approaches
Core Resistance Mechanisms inE. coli
Uropathogenic E. coli (UPEC), the primary causative agent of urinary tract infections, exemplifies how intrinsic resistance mechanisms contribute to the success of pathogenic E. coli lineages. The intrinsic resistome of E. coli is primarily governed by its outer membrane structure and the activity of efflux pump systems [26]. The outer membrane, with its lipopolysaccharide (LPS)-rich leaflet, creates a penetration barrier that limits the intracellular accumulation of diverse antimicrobials. Simultaneously, energy-dependent efflux pumps work synergistically with this barrier by actively extruding compounds that manage to penetrate the cell envelope [26] [25].
E. coli possesses several efflux systems belonging to distinct superfamilies, with the Resistance-Nodulation-Division (RND) family being particularly significant for multidrug resistance. The AcrAB-TolC system is the most characterized RND-type efflux pump in E. coli, with demonstrated activity against multiple antibiotic classes including fluoroquinolones, β-lactams, macrolides, tetracyclines, and chloramphenicol [26]. The operational model involves the inner membrane protein AcrB capturing substrates from the periplasm or cytoplasm, with the membrane fusion protein AcrA facilitating transport through the outer membrane channel TolC, effectively bypassing the periplasmic space [26]. Other important efflux families in E. coli include the Major Facilitator Superfamily (MFS), Multidrug and Toxic Compound Extrusion (MATE), Small Multidrug Resistance (SMR), and ATP-binding Cassette (ABC) transporters, each contributing to the intrinsic resistance profile [26].
Experimental Dissection of theE. coliResistome
A genome-wide screen of the Keio collection of E. coli knockouts (~3,800 single-gene deletions) identified specific genetic determinants of intrinsic resistance to chemically distinct antibiotics—trimethoprim and chloramphenicol [23] [22]. The experimental protocol involved growing knockout strains in LB media supplemented with antibiotics at their respective IC~50~ values or without antibiotic (control), with optical density at 600 nm measured and expressed as fold over wild type [23] [22]. Knockouts demonstrating growth lower than two standard deviations from the median of the distribution in antibiotic-containing media, but not in control media, were classified as hypersensitive [23].
This systematic approach identified 35 knockouts hypersensitive to trimethoprim and 57 knockouts hypersensitive to chloramphenicol, with enrichment in genes involved in cell envelope biogenesis, information transfer, and membrane transport pathways [23] [22]. Validation on solid media with trimethoprim concentrations (MIC, MIC/3, and MIC/9) confirmed hypersensitivity for 20 of 33 tested strains, with the most significant sensitization observed in knockouts of acrB (efflux pump), rfaG (LPS biosynthesis), lpxM (lipid A biosynthesis), and nudB (folate metabolism) [22].
Table 1: Key E. coli Intrinsic Resistance Genes Identified Through Genome-Wide Screening
| Gene | Function | Pathway | Hypersensitivity Phenotype |
|---|---|---|---|
| acrB | RND efflux pump component | Membrane transport | Trimethoprim, chloramphenicol, multiple antibiotics |
| rfaG | Lipopolysaccharide glucosyl transferase I | Cell envelope biogenesis | Trimethoprim, chloramphenicol |
| lpxM | Lipid A myristoyl transferase | Cell envelope biogenesis | Trimethoprim, chloramphenicol |
| nudB | Dihydroneopterin triphosphate diphosphatase | Folate metabolism | Trimethoprim-specific |
| rplA | 50S ribosomal protein L1 | Information transfer | Chloramphenicol-specific |
Experimental evolution under trimethoprim pressure revealed that strains with disruptions in intrinsic resistance pathways (ΔacrB, ΔrfaG, ΔlpxM) showed compromised ability to evolve resistance, with ΔacrB being most severely affected—establishing efflux inhibition as a promising "resistance proofing" strategy [22]. At sub-inhibitory concentrations, however, these knockouts demonstrated varying degrees of evolutionary recovery through mutations in drug-specific resistance pathways (e.g., folA upregulation) rather than compensatory evolution in the disrupted intrinsic resistance pathways [22].
Diagram 1: Experimental workflow for identification and validation of intrinsic resistance genes in E. coli using genome-wide screening.
3P. aeruginosa: A Paradigm of Extreme Intrinsic Resistance
Multilayered Resistance Architecture
Pseudomonas aeruginosa represents a model organism for studying extreme intrinsic resistance in Gram-negative pathogens, possessing one of the most formidable innate defense systems among clinically relevant bacteria [29]. Its resistance profile stems from the synergistic combination of low outer membrane permeability, constitutive and inducible efflux pump systems, and chromosomally encoded antibiotic-inactivating enzymes [30] [29] [27]. The outer membrane of P. aeruginosa is 12-100 times less permeable than that of E. coli, creating a substantial physical barrier to antibiotic penetration [27]. This inherent impermeability is complemented by multiple efflux systems that actively remove antimicrobial agents that successfully traverse the membrane barrier.
The Resistance-Nodulation-Division (RND) family of efflux pumps plays a particularly crucial role in P. aeruginosa's intrinsic resistome, with at least four major systems characterized: MexAB-OprM, MexXY-OprM, MexCD-OprJ, and MexEF-OprN [29] [27]. Each pump exhibits distinct substrate specificities and regulatory mechanisms:
- MexAB-OprM: Constitutively expressed, exports β-lactams, quinolones, chloramphenicol, tetracycline, novobiocin, and macrolides
- MexXY-OprM: Inducible by its substrates, exports aminoglycosides, β-lactams, quinolones, and erythromycin
- MexCD-OprJ: Not normally expressed in wild-type cells but inducible, exports β-lactams, quinolones, chloramphenicol, tetracyclines
- MexEF-OprN: Not normally expressed, exports quinolones, chloramphenicol, trimethoprim [29]
P. aeruginosa also possesses chromosomally encoded antibiotic-inactivating enzymes, most notably the inducible AmpC β-lactamase and the class D oxacillinase PoxB, which provide intrinsic resistance to a broad range of β-lactam antibiotics [29]. AmpC is particularly significant clinically, as mutational derepression leads to hyperproduction and resistance to penicillins and cephalosporins, representing the most common mechanism of β-lactam resistance in P. aeruginosa [29].
Table 2: Major Intrinsic Resistance Mechanisms in P. aeruginosa
| Mechanism | Key Components | Antibiotic Classes Affected |
|---|---|---|
| Reduced Permeability | Low-permeability outer membrane, specific porins (OprD) | Most antibiotics, particularly carbapenems (imipenem) |
| Efflux Systems | MexAB-OprM, MexXY-OprM, MexCD-OprJ, MexEF-OprN | β-lactams, fluoroquinolones, macrolides, tetracyclines, aminoglycosides |
| Enzymatic Inactivation | AmpC β-lactamase, PoxB oxacillinase | Penicillins, cephalosporins |
| Aminoglycoside Modification | Chromosomally encoded acetyltransferases, phosphotransferases | Aminoglycosides (gentamicin, tobramycin) |
Adaptive Resistance and Biofilm-Mediated Tolerance
Beyond its constitutive intrinsic resistance mechanisms, P. aeruginosa employs sophisticated adaptive resistance strategies that further complicate treatment. Biofilm formation represents a key adaptive mechanism, creating structured microbial communities encased in an exopolysaccharide matrix that significantly reduces antibiotic penetration and increases tolerance to antimicrobial agents [29] [31]. Within biofilms, bacteria exhibit altered metabolic states and heterogeneous gene expression patterns, including upregulated efflux pump activity and induction of the stringent response, collectively contributing to enhanced resistance [31].
The regulation of intrinsic resistance mechanisms in P. aeruginosa involves complex regulatory networks that respond to environmental stimuli and antibiotic exposure. Mutations in regulatory genes such as mexZ, nfxB, and mexT can lead to overexpression of efflux pumps, while two-component systems like PhoP-PhoQ and ParR-ParS modulate lipid A modifications and aminoglycoside resistance [30] [29]. This regulatory plasticity enables P. aeruginosa to fine-tune its resistance arsenal in response to specific environmental challenges, contributing to its success as a persistent pathogen.
Diagram 2: Multilayered intrinsic resistance architecture of P. aeruginosa showing synergistic mechanisms.
Experimental Methodologies for Resistome Characterization
Genome-Wide Screening Approaches
Systematic identification of intrinsic resistance genes employs comprehensive genome-wide knockout libraries such as the Keio collection for E. coli [23] [22]. The standard protocol involves:
- Library Preparation: Growing arrayed knockout strains in 96-well format with appropriate antibiotic maintenance
- Antibiotic Challenge: Replicating onto media containing sub-inhibitory concentrations of target antibiotics (typically IC~50~ values) alongside drug-free controls
- Phenotypic Assessment: Measuring growth inhibition via optical density (OD~600~) or colony formation after specified incubation periods
- Data Analysis: Normalizing growth values to wild-type controls, applying statistical cutoffs (e.g., <2 standard deviations from median) to identify hypersensitive strains
- Validation: Confirming hypersensitivity phenotypes through secondary assays including MIC determination, time-kill curves, and chemical-genetic interaction profiling [23] [22]
For P. aeruginosa, similar approaches using transposon mutant libraries (e.g., the PA14 Transposon Mutant Library) coupled with Transposon Sequencing (Tn-Seq) enable genome-wide fitness profiling under antibiotic selection, identifying genes essential for survival during drug challenge [30] [29].
Evolution Experiments and Resistance Development Assays
Tracking evolutionary trajectories of resistant mutants provides critical insights into the adaptability of bacteria with compromised intrinsic resistance mechanisms. The standard methodology includes:
- Strain Selection: Choosing hypersensitive mutants (e.g., ΔacrB, ΔrfaG, ΔlpxM) and wild-type controls
- Experimental Evolution: Serial passaging in liquid media with escalating sub-MIC antibiotic concentrations over multiple generations (typically 20-50 daily transfers)
- Monitoring Adaptation: Regularly plating populations on antibiotic-containing media to assess MIC changes and recovery from hypersensitivity
- Genetic Analysis: Whole-genome sequencing of evolved clones to identify compensatory mutations and resistance mechanisms [22]
This approach revealed that E. coli mutants with defects in intrinsic resistance pathways (efflux, LPS biosynthesis) can recover antibiotic resistance through mutations in drug-specific targets rather than restoring the original resistance mechanism, highlighting the remarkable adaptability of bacterial pathogens [22].
Therapeutic Implications and Research Applications
Targeting the Intrinsic Resistome for Antibiotic Adjuvants
The components of the intrinsic resistome represent promising targets for resistance-breaking adjuvants that could rejuvenate existing antibiotics. Efflux pump inhibitors (EPIs) targeting RND systems like AcrB in E. coli and Mex pumps in P. aeruginosa have demonstrated potential to resensitize resistant strains when combined with conventional antibiotics [22] [27]. However, studies comparing genetic versus pharmacological inhibition reveal important distinctions: while ΔacrB mutants showed compromised ability to evolve resistance, combination therapy with the EPI chlorpromazine led to rapid evolution of resistance to the inhibitor itself, underscoring the challenges in therapeutic targeting of resistance mechanisms [22].
Membrane permeabilizers that disrupt the integrity of the Gram-negative outer membrane offer another adjuvant strategy. Compounds that target LPS biosynthesis or integrity can potentiate a broad spectrum of antibiotics by increasing intracellular accumulation [22]. For P. aeruginosa, approaches targeting the unique structural features of its outer membrane, including the high lipid A modification status and specific porin networks, may provide pathogen-specific sensitizing strategies [29] [27].
Research Toolkit for Intrinsic Resistome Studies
Table 3: Essential Research Reagents and Resources for Intrinsic Resistome Investigation
| Resource/Reagent | Specifications | Research Application | Key Considerations |
|---|---|---|---|
| Keio Collection | ~3,800 single-gene knockouts in E. coli K-12 BW25113 | Genome-wide susceptibility screening | Essential gene knockouts maintained as heterozygous diploids |
| P. aeruginosa Mutant Libraries | PA14 Transposon Mutant Library (~5,400 mutants) | Identification of resistance determinants | Coverage limitations for essential genes |
| Efflux Pump Inhibitors | CCCP, PAβN, chlorpromazine, verapamil | Functional assessment of efflux activity | Cytotoxicity and off-target effects at high concentrations |
| Permeability Assay Reagents | N-phenyl-1-naphthylamine (NPN), 1-N-phenylnaphthylamine | Outer membrane permeability measurement | Solvent controls essential for interpretation |
| β-Lactamase Substrates | Nitrocefin, CENTA | AmpC activity monitoring and inhibition studies | Kinetic measurements required for induction studies |
| Animal Infection Models | Mouse UTI, pneumonia, neutropenic thigh infection models | In vivo relevance of resistance mechanisms | Species-specific differences in drug pharmacokinetics |
The intrinsic resistomes of E. coli and P. aeruginosa represent sophisticated, multi-component defense systems that significantly contribute to the antibiotic resistance crisis. Through complementary mechanisms including restricted membrane permeability, active drug efflux, and enzymatic inactivation, these pathogens limit intracellular antibiotic accumulation and survive antimicrobial challenge. Genome-wide studies have begun to systematically catalog the genetic determinants of intrinsic resistance, revealing both expected pathways (efflux pumps, outer membrane biogenesis) and unexpected contributors (information transfer, metabolic processes).
For researchers and drug development professionals, targeting the intrinsic resistome offers promising avenues for developing antibiotic adjuvants that could resensitize resistant pathogens. However, evolutionary studies demonstrate the remarkable adaptability of bacteria, which can bypass disruptions in intrinsic resistance through mutations in drug-specific pathways. This underscores the need for multi-target approaches and careful consideration of evolutionary consequences when designing resistance-breaking strategies. As the antibiotic resistance crisis intensifies, deepening our understanding of the intrinsic resistome will be essential for developing the next generation of antimicrobial therapies that can overcome these innate bacterial defenses.
The intrinsic resistome encompasses all chromosomal elements that contribute to a bacterium's innate ability to survive antibiotic treatment, distinct from acquired resistance mechanisms. For bacterial pathogens, understanding the intrinsic resistome is paramount for addressing the escalating antimicrobial resistance (AMR) crisis, projected to cause 10 million deaths annually by 2050 if unaddressed [6]. Genome-wide knockout libraries represent a powerful functional genomics approach for systematically identifying genes within the intrinsic resistome that, when inactivated, render bacteria hypersusceptible to antibiotics. This whitepaper provides an in-depth technical guide to identifying hypersusceptibility genes using these libraries, framing the methodology within broader resistome research aimed at developing novel therapeutic strategies against multidrug-resistant pathogens.
Core Concepts and Experimental Foundations
The Hypersusceptibility Phenomenon in Resistome Research
Hypersusceptibility occurs when a gene knockout enhances a bacterium's sensitivity to an antibiotic beyond that of the wild-type strain. This identifies genes whose products contribute to intrinsic resistance through various mechanisms, including reduced antibiotic influx, enhanced efflux, target protection, or bypass of metabolic pathways [22]. In the context of the intrinsic resistome, these genes represent potential targets for adjuvants that could resensitize resistant bacteria to conventional antibiotics. For instance, a 2025 study on E. coli demonstrated that knockouts of efflux pump components (acrB) and cell envelope biogenesis genes (rfaG, lpxM) resulted in hypersensitivity to multiple antibiotics, including trimethoprim and chloramphenicol [22].
Genome-Wide Knockout Libraries as Discovery Tools
Genome-wide knockout collections enable systematic interrogation of gene function across an entire organism. The Keio knockout collection, a cornerstone in E. coli research, comprises approximately 4,000 single-gene deletion mutants, each replaced with a kanamycin resistance cassette [32] [22]. This library provides comprehensive coverage of non-essential genes, allowing researchers to screen for phenotypes under diverse conditions, including antibiotic exposure. Similar resources have been developed for other pathogens, facilitating comparative resistome analyses. The power of these libraries lies in their ability to identify susceptibility determinants without prior assumptions about gene function, enabling discovery of novel resistance mechanisms.
Experimental Framework and Workflows
Core Screening Methodology
The fundamental workflow for identifying hypersusceptibility genes involves growing knockout library mutants under antibiotic pressure and identifying strains with compromised growth compared to wild-type controls. The standard protocol consists of several key phases, as visualized below:
Library Preparation and Inoculation: The process begins with careful preparation of the knockout library. For the Keio collection, glycerol stocks of ~4,000 mutants are typically stored in 96-well plates at -80°C. These are inoculated into liquid growth medium using a microplate replicator and grown overnight [32]. For solid medium screens, cultures are pinned onto agar plates containing sub-inhibitory concentrations of the target antibiotic.
Antibiotic Exposure and Incubation: A critical step involves determining appropriate antibiotic concentrations for screening. This is typically established through preliminary spot tests on wild-type and randomly selected mutants across a concentration gradient (e.g., 0-6 μg/mL for epetraborole) [32]. For the main screen, mutants are exposed to the antibiotic in duplicate or triplicate at concentrations approximating the IC50 (half-maximal inhibitory concentration) of the wild-type strain. Plates are incubated for extended periods (up to 5 days) with daily imaging to capture delayed phenotypes [32].
Growth Monitoring and Data Acquisition: Bacterial growth is quantified through optical density (OD600) measurements for liquid cultures or colony size assessment for solid media. Automated imaging systems capture temporal growth patterns, which is crucial for identifying mutants with delayed hypersensitivity responses. Modern screening approaches utilize high-throughput robotic systems to handle the scale of genome-wide libraries.
Advanced Screening Approaches
Recent technological advances have enhanced traditional knockout screening. CRISPR interference (CRISPRi) screening offers a powerful alternative, particularly for essential genes not represented in deletion libraries. A 2025 study employed a high-density sgRNA library targeting every 100 bp of the E. coli coding sequence to identify essential genes under antibiotic-induced stress [33]. This approach enables transcriptional modulation rather than complete gene knockout, revealing the importance of gene expression levels in antibiotic susceptibility.
Pooled screening approaches with barcode sequencing (Bar-seq) allow parallel assessment of mutant fitness under antibiotic pressure by tracking lineage-specific DNA barcodes through next-generation sequencing. This method provides highly quantitative fitness measurements but requires specialized computational analysis.
Data Analysis and Hit Validation
Identification and Classification of Hypersusceptible Mutants
Following screening, mutants are classified based on growth inhibition patterns. A common classification scheme includes:
- Hypersusceptible (HS): Complete growth inhibition at concentrations where wild-type grows normally
- Moderately Susceptible (MS): Significant but incomplete growth inhibition
- Low Susceptible (LS): Mild growth defect compared to wild-type
Statistical thresholds for classification typically involve comparing mutant growth to the population distribution, often defining hits as those falling below two standard deviations from the median growth [22]. The table below summarizes hypersusceptibility genes identified in recent studies:
Table 1: Hypersusceptibility Genes Identified in Recent Genome-Wide Screens
| Gene | Function | Antibiotic | Proposed Mechanism | Study |
|---|---|---|---|---|
| acrB | Multidrug efflux pump | Trimethoprim, Chloramphenicol | Reduced antibiotic efflux | [22] |
| rfaG | LPS biosynthesis | Trimethoprim, Chloramphenicol | Increased membrane permeability | [22] |
| lpxM | Lipid A biosynthesis | Trimethoprim, Chloramphenicol | Increased membrane permeability | [22] |
| leuD | Leucine biosynthesis | Epetraborole | Synergy with LeuRS inhibition | [32] |
| ubiG | Ubiquinone biosynthesis | Epetraborole | Metabolic vulnerability | [32] |
| trmU | tRNA modification | Epetraborole | tRNA dysregulation | [32] |
| rnb | RNA turnover | Epetraborole | RNA metabolism disruption | [32] |
Validation and Mechanistic Studies
Complementation Assays: Putative hypersusceptibility hits require validation through genetic complementation. This involves introducing a functional copy of the gene into the knockout mutant, typically via a plasmid vector, and demonstrating restoration of wild-type resistance levels. The ASKA plasmid library, which contains over 4,000 E. coli open reading frames cloned into expression vectors, is frequently used for this purpose [32].
Mechanistic Follow-up Studies: Validated hits undergo further characterization to elucidate their role in intrinsic resistance:
- Transcriptional analysis to examine expression changes in resistance pathways
- Metabolomic profiling to identify altered metabolic states
- Antibiotic accumulation assays to measure intracellular drug concentrations
- Molecular modeling to predict protein-antibiotic interactions
The relationship between different resistance mechanisms and antibiotic classes can be visualized as:
Research Reagent Solutions and Tools
Successful genome-wide screening requires specialized reagents and computational tools. The table below outlines key resources:
Table 2: Essential Research Reagents and Tools for Hypersusceptibility Screening
| Resource Type | Specific Examples | Application/Function | Key Features |
|---|---|---|---|
| Knockout Libraries | Keio Collection (E. coli) | Genome-wide deletion mutants | ~4,000 non-essential gene knockouts [32] |
| Plasmid Libraries | ASKA Library (E. coli) | Genetic complementation | >4,000 ORFs in expression vectors [32] |
| Bioinformatics Tools | ResistoXplorer | Resistome data analysis | Visualization, statistical analysis, functional profiling [34] |
| Screening Media | LB with antibiotics | Mutant growth under selection | Standardized conditions for phenotype expression |
| Statistical Methods | R packages (edgeR, DESeq2) | Differential abundance analysis | Normalization for compositional data [34] |
Case Studies and Research Applications
Epetraborole Mechanism Studies
A 2025 genome-wide screen of the Keio collection with epetraborole (EP), a boron-containing LeuRS inhibitor, identified 44 susceptible mutants beyond expected leucine biosynthesis targets [32]. Disrupted genes included leuD (leucine biosynthesis), rnb (RNA turnover), trmU (tRNA modification), ubiG (ubiquinone biosynthesis), and pncA (NAD salvage pathway). Bioinformatic analyses linked these genes to tRNA homeostasis and stress response networks, revealing that EP's primary inhibition of LeuRS synergizes with defects in these ancillary pathways [32]. This demonstrates how knockout screens can uncover complex vulnerability networks beyond primary drug targets.
Resistance-Breaking Strategies
A 2025 investigation of intrinsic resistance pathways identified knockouts that sensitized E. coli to trimethoprim and chloramphenicol [22]. Deletions in acrB (efflux), rfaG, and lpxM (both cell envelope biogenesis) showed strong hypersusceptibility. Evolutionary experiments revealed that while these genetic impairments initially enhanced antibiotic efficacy, bacteria frequently developed compensatory mutations under sub-inhibitory drug pressure [22]. This highlights both the promise and limitations of targeting intrinsic resistance mechanisms and underscores the importance of considering evolutionary trajectories in therapeutic development.
Innovative Screening Approaches
A proof-of-concept study demonstrated an alternative to conventional resistance breaking: "resistance hacking." Researchers engineered a florfenicol prodrug that was activated by Eis2, a resistance protein in Mycobacterium abscessus [35]. This created a perpetual cascade where antibiotic-induced resistance protein expression continuously generated more active drug, effectively turning the resistance mechanism against the bacterium [35]. Such innovative approaches showcase how mechanistic insights from genetic screens can inspire novel therapeutic strategies.
Genome-wide knockout libraries provide powerful platforms for systematically identifying hypersusceptibility genes within the intrinsic resistome of bacterial pathogens. The experimental framework outlined herein—encompassing library screening, hit validation, and mechanistic follow-up—enables researchers to pinpoint genetic vulnerabilities that can be exploited to overcome antibiotic resistance. As screening technologies advance with approaches like high-resolution CRISPRi and multiplexed phenotypic profiling, our understanding of bacterial resistomes will deepen. These insights are crucial for developing the next generation of antibiotic adjuvants and resistance-breaking strategies to address the escalating AMR crisis. Future research should focus on expanding these approaches to clinically relevant pathogens, exploring combination therapies that target multiple resistance mechanisms simultaneously, and integrating evolutionary perspectives to develop more durable resistance management strategies.
Mapping and Exploiting the Resistome: From High-Throughput Screens to Novel Therapies
The fight against antimicrobial resistance (AMR) requires a deep understanding of the intrinsic resistome—the set of genes native to a bacterial pathogen that contribute to its natural ability to withstand antibiotics [36]. Deciphering this complex background is crucial for identifying novel drug targets, understanding resistance emergence, and developing effective countermeasures. This whitepaper details three cornerstone methodological toolkits—transposon mutagenesis, knockout collections, and metagenomic sequencing—that are transforming intrinsic resistome research. These techniques enable systematic, genome-scale studies of bacterial fitness, gene essentiality, and the environmental reservoirs of resistance, providing researchers and drug development professionals with the tools to address AMR from a holistic, One-Health perspective [37] [38] [36].
Transposon Mutagenesis for Genome-Wide Fitness Profiling
Transposon mutagenesis, particularly Transposon Insertion Sequencing (Tn-seq), is a powerful method for conducting genome-scale forward genetic screens in bacteria [39]. It enables the identification of fitness determinants and essential genes by quantifying the survival of transposon mutants under selective conditions, such as antibiotic exposure or during infection.
Advanced Methodology: InducTn-seq
A significant recent advancement is InducTn-seq, which utilizes an arabinose-inducible Tn5 transposase to generate exceptionally diverse mutant libraries from a single colony [39].
- Core Principle: Temporal control of transposition allows for the continuous generation of mutants, overcoming population bottlenecks that plague traditional Tn-seq, especially in animal infection models [39].
- Key Workflow:
- Strain Engineering: A mobilizable plasmid introduces a mini-Tn5 transposon and its inducible transposase at a specific genomic attachment site (attTn7).
- Library Induction: Addition of arabinose induces random mini-Tn5 transposition throughout the genome.
- Selection & Sequencing: Mutants are subjected to a condition of interest (e.g., antibiotic treatment). The transposon-genome junctions are then amplified and sequenced to quantify insertion abundance in the resulting population [39].
- Application in Resistome Research: By comparing mutant abundances before (ON condition) and after (OFF condition) selection, researchers can directly quantify the fitness cost of gene disruptions. This sensitive framework identifies not only core essential genes but also those involved in intrinsic antibiotic resistance with subtle fitness effects [39].
The experimental workflow for InducTn-seq is outlined in the diagram below.
Research Reagent Solutions for Transposon Mutagenesis
Table 1: Key reagents for InducTn-seq and related transposon mutagenesis approaches.
| Reagent / Component | Function | Example / Description |
|---|---|---|
| Inducible Transposon System | Enables controlled, high-density mutagenesis. | Plasmid with arabinose-inducible Tn5 transposase (e.g., pTn donor) and mini-Tn5 with kanamycin resistance [39]. |
| Tn7 Helper Plasmid | Facilitates site-specific integration of the transposon system. | Provides Tns proteins for integration at the chromosomal attTn7 site [39]. |
| Selection Antibiotics | For selection of integrants and mutants. | Kanamycin (for transposon), Gentamicin (for Cre-based indicator system) [39]. |
| Inducer Molecule | Triggers random transposition. | L-Arabinose for PBAD promoter induction [39]. |
| Cre-loxP Indicator System | Reports population-level transposition frequency. | Flanking lox sequences; successful transposition activates a gentamicin resistance marker [39]. |
Knockout Collections for Defining Gene Essentiality
Ordered knockout collections represent another pinnacle of functional genomics, comprising defined mutants for every non-essential gene in a genome. These libraries are invaluable for systematically probing gene function and interactions.
Insights from Comparative Genomics
Large-scale comparative studies using transposon mutagenesis have revealed the dynamic nature of the essential genome. An analysis of 13 Enterobacteriaceae libraries identified a core essential genome of only 201 genes universally required for survival across species [40]. However, a substantial fraction of genes display conditional or context-dependent essentiality, influenced by genetic background and environmental conditions [40]. For instance, the σE stress response pathway has independently acquired essentiality multiple times, demonstrating that essentiality is not a fixed gene property but is shaped by evolutionary paths and genomic context [40].
Quantitative Data from High-Throughput Studies
Table 2: Quantitative findings on gene essentiality from high-throughput mutagenesis studies in Enterobacteriaceae.
| Metric | Finding | Implication for Resistome Research |
|---|---|---|
| Core Essential Genes | 201 genes universal across Enterobacteriaceae [40]. | Represents a high-value set of potential broad-spectrum antibiotic targets. |
| Variable Essentiality | ~1/3 of genes essential in one strain are non-essential in a related strain [40]. | Highlights context-dependency; resistome genes may be essential only in specific genetic backgrounds. |
| Transposon Library Density | InducTn-seq generates >1 million unique mutants [39]. | Enables highly sensitive detection of fitness defects, even for essential genes under non-inducing conditions. |
Metagenomic Sequencing for Resistome Surveillance and Discovery
Metagenomic sequencing bypasses culturing to analyze the collective genetic material of microbial communities directly from environmental, animal, or human samples [37]. It is a transformative tool for profiling the environmental resistome—the vast reservoir of ARM genes in nature.
Functional and Sequence-Based Approaches
Two primary metagenomic strategies are employed:
- Functional Metagenomics: Involves cloning environmental DNA into a host bacterium (e.g., E. coli) and screening for expressed resistance phenotypes [41]. This method is powerful for discovering novel resistance genes without prior sequence knowledge, as demonstrated by the identification of biocide resistance genes from textile effluent and sewage sludge [41].
- Sequence-Based Metagenomics: Directly sequences all DNA in a sample and uses computational tools to identify known ARGs, their microbial hosts, and associated mobile genetic elements (MGEs) [37] [42] [24].
Advanced Pipelines for Risk Assessment
The field is moving beyond mere ARG identification towards quantitative risk assessment. Tools like the Long-read based Antibiotic Resistome Risk Assessment Pipeline (L-ARRAP) integrate long-read sequencing data to calculate an Antibiotic Resistome Risk Index (L-ARRI) [42]. This index quantifies risk by considering:
- ARG Abundance
- Mobility Potential (linkage to MGEs like transposons, plasmids)
- Pathogenic Hosts (co-occurrence with human bacterial pathogens) [42]
This holistic workflow is depicted below.
Key Research Reagents for Metagenomics
Table 3: Essential reagents, databases, and tools for metagenomic resistome analysis.
| Category / Reagent | Function | Example / Application |
|---|---|---|
| Cloning Vector & Host | For functional metagenomic library construction. | Plasmid pCF430 in E. coli TransforMax EC100 cells [41]. |
| Selective Agents | To screen for resistance phenotypes. | Antibiotics (e.g., Tetracycline), Biocides (e.g., Benzalkonium Chloride) [41]. |
| Reference Databases | For annotating sequences in sequence-based metagenomics. | SARG (ARGs), MobileOG-db (MGEs), CARD (ARGs) [42] [24]. |
| Bioinformatic Pipelines | To process data and calculate risk. | L-ARRAP (for long-reads), ARGs-OAP [42] [43]. |
Integrated Application in Intrinsic Resistome Research
The synergy of these toolkits provides an unparalleled view of the intrinsic resistome. Transposon mutagenesis and knockout collections identify which genes are essential for survival under antibiotic stress within a pathogen. Metagenomic sequencing reveals where these genes and their variants originate, how they are mobilized, and their prevalence in diverse ecosystems.
For example, a functional metagenomic study of contaminated environments discovered that housekeeping genes like galE (UDP-galactose 4-epimerase) can confer cross-resistance to biocides and clinically important antibiotics when overexpressed [41]. This finding was only possible through a culture-independent functional screen. Furthermore, the discovery that these galE-like genes were co-located with transposons highlighted their potential for mobilization from the environment into pathogens [41], a pathway that can be monitored using the advanced risk assessment pipelines applied to human-influenced environments like wastewater [44].
In conclusion, the combined power of transposon mutagenesis, knockout collections, and metagenomic sequencing equips researchers with a comprehensive toolkit to deconvolute the complexities of the intrinsic resistome. From functional validation and essential gene mapping in the lab to ecological surveillance and risk assessment in the field, these methodologies are fundamental to guiding the development of next-generation antimicrobial strategies.
Antibiotic resistance has escalated from a localized clinical challenge to a global health crisis, threatening to undermine decades of medical progress. Modern understanding frames resistance not merely as a clinical phenomenon, but as the outcome of complex ecological and molecular interactions spanning environmental reservoirs, agriculture, animals, and humans [6]. Central to this understanding is the concept of the resistome—the comprehensive set of all antibiotic resistance genes (ARGs), including those intrinsic to bacterial genomes, those acquired via horizontal gene transfer, and cryptic determinants with potential to evolve into active resistance mechanisms [6]. The environmental resistome acts as a silent incubator for these genes, with horizontal gene transfer and stress-induced mutagenesis continuously fueling their evolution and dissemination into human pathogens [6].
Within this framework, genetic screens have emerged as powerful tools for dissecting the complex networks underlying bacterial survival under antibiotic pressure. These functional genomics approaches enable researchers to systematically identify both drug-agnostic susceptibility determinants—genetic factors that confer sensitivity across multiple antibiotic classes—and drug-specific susceptibility determinants—those that mediate resistance to particular drugs. By mapping these genetic interactions, scientists can pinpoint vulnerabilities that persist across therapeutic lineages and those that are context-dependent, providing a roadmap for novel antibacterial strategies and combination therapies aimed at overcoming multi-drug resistant infections.
Molecular Mechanisms of Resistance and Susceptibility
The Genetic Architecture of Antimicrobial Resistance
At the molecular level, antibiotic resistance manifests through a sophisticated repertoire of mechanisms that bacteria employ to survive lethal chemical attacks. Chromosomal mutations can alter drug-binding sites, as exemplified by mutations in gyrA and parC conferring fluoroquinolone resistance or ribosomal RNA mutations conferring resistance to macrolides and aminoglycosides [6]. Beyond direct target modification, antibiotic exposure induces bacterial stress responses, such as the SOS regulon—a DNA-damage repair system that promotes mutagenesis and facilitates mobilization of genetic elements [6]. Critically, even sub-inhibitory antibiotic concentrations, commonly detected in wastewater and agricultural soils, can amplify this effect by promoting DNA damage repair pathways and recombination, thereby accelerating adaptive evolution [6].
The mobilome—comprising plasmids, integrative conjugative elements (ICEs), transposons, and integrons—serves as the primary vehicle for disseminating ARGs across microbial communities. Multi-resistance plasmids can carry genes for β-lactamases, aminoglycoside-modifying enzymes, and efflux systems simultaneously, conferring survival advantages under diverse antibiotic exposures [6]. The discovery of mcr-9 and mcr-10 on self-transmissible plasmids underscores the role of horizontal transfer in the global spread of colistin resistance [6]. Integrons serve as natural gene capture and expression systems, facilitating the shuffling and dissemination of ARG cassettes, with sub-inhibitory β-lactam exposure shown to enhance integron recombination [6].
Efflux pumps represent another formidable resistance mechanism, with those of the Resistance-Nodulation-Division (RND) family capable of expelling structurally diverse antibiotics including fluoroquinolones, tetracyclines, and carbapenems [6]. Transcriptomic and proteomic analyses have revealed that efflux pumps are part of broader stress-response circuits, often co-regulated with oxidative stress defenses and biofilm formation, enhancing bacterial survival against both antibiotics and host immune defenses [6].
Master Regulators and the Concept of the Intrinsic Resistome
Some bacterial pathogens harbor master regulatory systems that coordinate broad-spectrum resistance programs. In Mycobacterium abscessus, a rapidly growing multidrug-resistant species dubbed the "antibiotic nightmare," the WhiB7 resistome acts as a master regulator of ribosomal stress [35]. When antibiotics such as chloramphenicol or clarithromycin target the ribosome, WhiB7 activates and controls over 100 proteins involved in antimicrobial resistance, creating a significant barrier for effective therapeutics [35]. This intrinsic resistome represents a complex set of antibiotic-limiting genes that act as a gauntlet for antibiotics to surpass, making treatments notoriously difficult and often requiring long-term, multi-drug regimens that can lead to host mitochondrial toxicity and microbiome disruption [35].
Table 1: Major Molecular Mechanisms of Antibiotic Resistance
| Mechanism Category | Molecular Components | Antibiotic Classes Affected | Key Examples |
|---|---|---|---|
| Enzymatic Inactivation | β-lactamases, aminoglycoside-modifying enzymes | β-lactams, aminoglycosides | CTX-M ESBLs, carbapenemases (KPC, NDM) |
| Target Modification | Mutated drug targets, protective proteins | Fluoroquinolones, macrolides, rifamycins | gyrA/parC mutations, Erm methylases |
| Efflux Systems | RND pumps, ABC transporters | Multiple classes (tetracyclines, macrolides, β-lactams) | MexAB-OprM (P. aeruginosa), AcrAB-TolC (E. coli) |
| Membrane Permeability | Porins, lipid modifications | β-lactams, colistin | OprD loss (P. aeruginosa), mcr genes |
| Regulatory Networks | Transcriptional regulators, two-component systems | Multiple classes | WhiB7 (Mycobacteria), marRAB operon (Enterobacteriaceae) |
Genetic Screening Technologies: A Technical Deep Dive
CRISPR-Based Functional Genomics
CRISPR-based screening technologies have revolutionized the systematic interrogation of gene function in bacteria, enabling sensitive detection of drug-gene interactions directly in relevant cellular contexts [45]. These approaches leverage the precision of CRISPR-Cas systems to create targeted genetic perturbations and identify genes that confer sensitivity or resistance to antimicrobial compounds.
The drugZ algorithm represents a specialized computational tool for identifying both synergistic and suppressor chemogenetic interactions from CRISPR screens [45]. This open-source Python software analyzes genome-scale drug modifier screens by calculating the log2 fold change of each guide RNA (gRNA) in a pool, normalizing read counts, and employing empirical Bayes variance estimation to compute Z-scores for each genetic perturbation [45]. The algorithm sums guide Z-scores across replicates to generate gene-level normZ scores, which are then used to identify genetic perturbations that significantly enhance or suppress drug activity [45].
Table 2: Key Genetic Screening Platforms for Antibiotic Resistance Research
| Screening Platform | Genetic Perturbation | Readout | Applications in Resistance Research |
|---|---|---|---|
| CRISPR Knockout | Gene knockout via Cas9-induced double-strand breaks | Growth survival under antibiotic pressure | Identification of essential genes for antibiotic efficacy |
| CRISPR Interference (CRISPRi) | Gene knockdown via catalytically dead Cas9 | Transcriptional repression phenotypes | Analysis of essential gene function without killing |
| Base Editing | Single nucleotide changes via deaminase-fused Cas9 | Specific mutation effects on drug sensitivity | Functional characterization of resistance mutations |
| Transposon Mutagenesis | Random insertion mutagenesis | Sequencing of insertion sites (Tn-seq) | Genome-wide identification of susceptibility determinants |
Base Editing Screens for Prospective Resistance Mapping
Base editing represents a particularly powerful approach for prospectively identifying genetic mechanisms of drug resistance. This technology uses a Cas9 nickase fused to a deaminase to enable programmed installation of C>T and A>G single nucleotide variants (SNVs) in the genome at high efficiency [46]. Unlike traditional resistance studies that depend on sequencing tumor biopsies from patients that relapse on treatment—a slow process limited to frequently observed variants—base editing allows for rapid, prospective, and systematic functional annotation of variants that could confer resistance [46].
In practice, researchers have used base editing screens to investigate resistance to multiple molecularly targeted agents by mutagenizing cancer genes that encode common drug targets or proteins within the same signaling pathway [46]. While these screens have been predominantly applied in oncology, the methodology is directly transferable to antimicrobial resistance research, particularly for understanding resistance to targeted antibacterials and for mapping structure-function relationships in bacterial resistance determinants.
Experimental Framework: From Screening to Validation
Workflow for Genome-Wide Resistance Screens
The following DOT visualization illustrates the comprehensive workflow for conducting genetic screens to identify susceptibility determinants:
Detailed Methodological Protocols
Lentiviral Library Production and Transduction
For CRISPR screening implementations requiring lentiviral delivery, the following protocol ensures high-quality library production:
Cell Preparation: Plate 9.0 × 10⁶ 293T cells in Dulbecco's high glucose modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 1× GlutaMAX, 100 mM sodium pyruvate, 1× non-essential amino acids (NEAA), and 1× penicillin-streptomycin [45].
Transfection: Co-transfect cells with psPAX2 (lentiviral packaging plasmid), pMD2.G (VSV-G envelope plasmid), and the CRISPR library plasmid (e.g., TKOV3) using a DNA transfection reagent such as X-tremeGENE 9 in medium with reduced antibiotic concentration (0.1× penicillin-streptomycin) [45].
Viral Harvest: Replace medium with viral harvest medium (DMEM + 1.1% BSA + 1× penicillin-streptomycin) 18 hours post-transfection. Collect virus-containing supernatant 24-48 hours post-transfection, centrifuge to remove cell debris, and store at -80°C [45].
Target Cell Transduction: Incubate target cells with lentiviral supernatant supplemented with 8μg/ml Polybrene. Begin selection with appropriate antibiotics (e.g., 20 μg/ml puromycin) 24 hours post-infection, maintaining selection for 72 hours or until control cells are completely eliminated [45].
Chemogenetic Screening Implementation
For actual screening experiments, the following steps ensure robust identification of genetic modifiers of antibiotic susceptibility:
Cell Expansion: Expand transduced cells to ensure adequate coverage (typically 15 × 10⁶ cells across multiple 15 cm dishes per replicate) [45].
Antibiotic Treatment: Split cells into technical replicates and treat with sub-lethal concentrations of target antibiotics. Include untreated control replicates. For concentration determination, perform preliminary dose-response curves to identify IC20-IC30 values that maintain cell viability over extended culture while inducing detectable drug-gene interactions [45].
Population Maintenance: Passage cells continuously, preventing confluence and maintaining representation of all library elements. Harvest cell pellets at beginning (T0) and after approximately 8 population doublings under selection [45].
Genomic DNA Extraction and Sequencing: Extract genomic DNA from harvested pellets. Amplify integrated gRNA sequences via PCR using barcoded primers, then sequence on an appropriate high-throughput platform (e.g., Illumina) [45].
Data Analysis and Hit Classification Framework
Computational Analysis of Screening Data
The analysis of chemogenetic screens requires specialized computational approaches to distinguish true genetic interactions from background noise. The drugZ algorithm implements a robust statistical framework for this purpose [45]:
Read Normalization: Normalize total read counts for each sample to a fixed number (e.g., 10 million reads) to enable cross-sample comparison.
Fold Change Calculation: Calculate log2 fold change for each gRNA using the formula:
where T represents treated samples, C represents control samples, t is time point, r is replicate, and pseudocount (default=5) prevents division by zero [45].
Variance Estimation: Estimate variance for each fold change by calculating the standard deviation of fold changes with similar abundance in the control sample using an empirical Bayes approach [45].
Z-score Calculation: Compute Z-score for each fold change using the variance estimate, then sum Z-scores across all gRNAs targeting the same gene and replicates, normalizing by the square root of the number of summed terms to generate a final normZ score [45].
Statistical Significance: Calculate P-values from normZ scores and correct for multiple hypothesis testing using the Benjamini-Hochberg method to control false discovery rate [45].
Classification of Genetic Modifiers of Antibiotic Susceptibility
Analysis of base editing screens across multiple drug treatments reveals that genetic variants modulating drug sensitivity fall into four distinct functional classes [46]:
Drug Addiction Variants: Confer proliferation advantage in drug presence but are deleterious without drug. These often represent activating mutations in pathway components (e.g., KRAS Q61R/E62G, MEK2 Y134H) that cause overactivation leading to oncogene-induced senescence in unperturbed conditions [46].
Canonical Drug Resistance Variants: Provide selective advantage only during drug treatment, typically through mutations that directly disrupt drug binding (e.g., MEK1 L115P, EGFR S464L within drug-binding pockets) [46].
Driver Variants: Confer growth advantage regardless of drug presence, representing general fitness-enhancing mutations that incidentally provide resistance.
Drug-Sensitizing Variants: Deleterious only during drug treatment, revealing genetic vulnerabilities that enhance antibiotic efficacy.
The following DOT visualization illustrates the decision framework for classifying these variant types:
Table 3: Functional Classification of Genetic Variants Modifying Antibiotic Susceptibility
| Variant Class | Phenotype in Drug | Phenotype Without Drug | Molecular Examples | Therapeutic Implications |
|---|---|---|---|---|
| Drug Addiction Variants | Resistant | Deleterious/fitness cost | KRAS Q61R, MEK2 Y134H | Drug holidays may eliminate resistant clones |
| Canonical Resistance Variants | Resistant | Neutral | MEK1 L115P, EGFR S464L | Require alternative inhibitors or combinations |
| Driver Variants | Resistant | Advantageous | Activating pathway mutations | Challenging to target; need for pathway switching |
| Drug-Sensitizing Variants | Sensitized | Neutral | Loss-of-function in resistance pathways | Opportunities for synthetic lethal combinations |
Research Reagent Solutions for Resistance Screening
Table 4: Essential Research Reagents for Genetic Screens of Antibiotic Resistance
| Reagent Category | Specific Examples | Function in Screening | Implementation Notes |
|---|---|---|---|
| CRISPR Libraries | TKOv3 (Toronto KnockOut), Brunello | Genome-wide gene knockout | Provide coverage of entire coding genome; include non-targeting controls |
| Base Editing Systems | cytidine base editor (CBE), adenine base editor (ABE) | Install specific nucleotide changes | Enable precise modeling of patient-derived resistance mutations |
| Delivery Systems | Lentiviral particles, electroporation | Introduce genetic perturbations | Lentiviral offers stable integration; electroporation for hard-to-transfect strains |
| Selection Markers | Puromycin, blasticidin, fluorescent reporters | Enumerate successfully modified cells | Antibiotic resistance allows selection; fluorescent markers enable FACS |
| Cell Culture Media | DMEM, RPMI-1640 with supplements | Support cellular proliferation | Must be optimized for specific bacterial pathogens or host cells |
| Antibiotic Compounds | Clinical antibiotics, experimental analogs | Selective pressure in screens | Use sub-lethal concentrations to detect both resistance and sensitization |
Emerging Applications and Therapeutic Translation
Resistance Hacking: Exploiting Resistance Mechanisms for Therapeutic Benefit
A groundbreaking approach emerging from resistance mechanism studies is "resistance hacking"—exploiting a bacterium's own resistance machinery for therapeutic benefit. Proof-of-concept research demonstrates that structurally modified versions of existing antibiotics can be engineered to exploit drug resistance mechanisms in pathogens [35]. For instance, a modified version of florfenicol was shown to act as a prodrug that is converted to its active form by Eis2, a protein that the WhiB7 resistome induces for drug resistance in Mycobacterium abscessus [35]. As WhiB7 activates, more Eis2 proteins are produced, generating more of the antibiotic's active form in a perpetual cascade that continuously amplifies the antibiotic's effect [35]. This approach effectively reverses resistance by turning the bacterial defense system against itself.
This strategy offers significant safety advantages, as the prodrug's lack of activity against host targets minimizes toxicity. Many antibiotics hit mitochondria, leading to mitochondrial toxicity—a significant problem with phenicol derivatives—but resistance hacking pathways can avoid this issue, providing a larger therapeutic window [35].
Artificial Intelligence and Predictive Resistance Modeling
The integration of artificial intelligence (AI) and machine learning (ML) with genetic screening data is accelerating drug discovery and resistance prediction, raising the possibility of precision-guided antimicrobial stewardship [6]. AI tools can analyze complex genetic interaction networks to predict resistance evolution pathways and identify optimal drug combinations that preempt resistance development. These computational approaches leverage the vast datasets generated by high-throughput genetic screens to build predictive models of resistance emergence, potentially enabling clinicians to stay one step ahead of adaptive bacterial populations.
Genetic screens provide an powerful functional framework for dissecting the complex molecular networks that underlie antibiotic resistance in bacterial pathogens. By systematically identifying both drug-agnostic and drug-specific susceptibility determinants, these approaches reveal vulnerabilities that can be exploited therapeutically. The classification of resistance modifiers into distinct functional categories—drug addiction variants, canonical resistance variants, driver variants, and drug-sensitizing variants—provides a conceptual framework for designing intervention strategies tailored to specific resistance mechanisms.
As resistance hacking approaches demonstrate, understanding resistance at a genetic level not only reveals how to overcome existing resistance but can also inspire novel therapeutic strategies that co-opt bacterial defense systems for therapeutic benefit. The continuing integration of improved screening technologies, computational analysis methods, and AI-driven prediction promises to accelerate the translation of genetic insights into clinical strategies for combating the growing threat of antimicrobial resistance.
The intrinsic resistome encompasses all chromosomally encoded elements that contribute to a bacterium's natural, baseline level of antibiotic resistance, independent of horizontal gene acquisition [1]. This concept reframes bacterial susceptibility as an emergent property of the cell, governed by a network of genes involved not only in classic defense but also in fundamental cellular processes [1]. Targeting the intrinsic resistome offers a promising strategic pivot in the fight against antimicrobial resistance (AMR), as it seeks to disarm core bacterial defenses, thereby sensitizing pathogens to existing antibiotics. This approach can potentially rejuvenate our therapeutic arsenal and slow the emergence of resistance. Among the myriad components of the intrinsic resistome, two functional categories stand out as particularly promising for intervention: multidrug efflux pumps (e.g., AcrB) and proteins critical to cell envelope biogenesis (e.g., RfaG and LpxM) [23]. These targets function as major gatekeepers of intracellular antibiotic accumulation and permeability barriers. The systematic genetic screens, such as those performed using the Keio collection of E. coli knockouts, have been instrumental in identifying these determinants, revealing that their inactivation often leads to hypersusceptibility to multiple, chemically diverse antibiotic classes [23]. This whitepaper provides an in-depth technical guide to these targets, summarizing the foundational evidence, elucidating the molecular mechanisms, detailing key experimental methodologies, and cataloging essential research tools for investigators in the field.
Target Characterization: Molecular Mechanisms and Biological Significance
The AcrB Efflux Pump: A Tripartite Multidrug Transporter
The AcrAB-TolC system is the predominant Resistance-Nodulation-Division (RND) family efflux pump in E. coli and other Enterobacteriaceae. This tripartite complex spans the entire cell envelope: AcrB is the inner membrane transporter that drives drug extrusion using the proton motive force; AcrA is a periplasmic adaptor protein that stabilizes the complex; and TolC is the outer membrane channel [47] [48]. The AcrB transporter itself is a homotrimer, and each monomer cycles through three conformational states (loose, tight, open) in a concerted, rotating mechanism that actively exports a stunningly broad spectrum of substrates, including fluoroquinolones, β-lactams, macrolides, tetracyclines, and bile salts [48]. The expression of the acrAB operon is tightly regulated by global transcriptional regulators like MarA, SoxS, and Rob, which are activated in response to environmental stressors, including antibiotic exposure [47]. A meta-analysis of 10 studies confirmed that overexpression of acrAB is a major contributor to multidrug resistance in clinical isolates of E. coli [47]. Beyond its role in antibiotic resistance, AcrAB is critically involved in virulence and pathogenesis. It influences adhesion to host cells, biofilm formation, and the export of virulence factors, as demonstrated in pathogens like Salmonella typhimurium and enteroaggregative E. coli (EAEC) [48]. This dual role makes it a high-value target for sensitization strategies.
Cell Envelope Biogenesis: RfaG and LpxM as Key Determinants
The Gram-negative cell envelope presents a formidable permeability barrier, and its integrity is paramount for intrinsic resistance. RfaG and LpxM are enzymes involved in the biogenesis of lipopolysaccharide (LPS), a major component of the outer membrane.
- RfaG (WaaG): This enzyme is a glycosyltransferase critical for the biosynthesis of the inner core region of LPS. It catalyzes the addition of the first heptose sugar to the inner core, a step essential for the proper assembly and stability of the LPS layer [23]. Mutations in rfaG result in a "deep rough" LPS phenotype, characterized by a severely truncated core oligosaccharide. This leads to a compromised outer membrane, increased permeability to hydrophobic molecules, and heightened sensitivity to host immune defenses like complement-mediated killing.
- LpxM (MsbB): This enzyme is an acyltransferase responsible for adding the final secondary laurate chain to the lipid A moiety of LPS. This step is crucial for achieving the optimal asymmetry and fluidity of the outer membrane [23]. Strains lacking lpxM produce a penta-acylated lipid A instead of the hexa-acylated form. This not only destabilizes the membrane, increasing permeability to antibiotics, but also reduces the endotoxic activity of lipid A, potentially modulating the host immune response.
The following diagram illustrates the functional roles and regulatory networks of these core targets within the bacterial cell.
Quantitative Evidence: Consolidating Hypersusceptibility and Resistance-Proofing Data
Empirical evidence from genome-wide screens and experimental evolution firmly establishes the potential of efflux pumps and cell envelope genes as sensitization targets. The data below summarize key phenotypic outcomes and resistance evolution profiles associated with these targets.
Table 1: Hypersusceptibility Profiles of Key Intrinsic Resistome Knockouts in E. coli
| Gene Target | Protein Function | Impact on Trimethoprim | Impact on Chloramphenicol | Key Antibiotic Classes Affected |
|---|---|---|---|---|
acrB |
RND family multidrug efflux pump | Hypersusceptible [23] | Hypersusceptible [23] | Fluoroquinolones, β-lactams, macrolides, tetracyclines [47] |
rfaG |
Glycosyltransferase for LPS core | Hypersusceptible [23] | Hypersusceptible [23] | Multiple, due to increased membrane permeability [23] |
lpxM |
Acyltransferase for Lipid A | Hypersusceptible [23] | Hypersusceptible [23] | Multiple, due to increased membrane permeability [23] |
Table 2: Evolutionary Adaptation and Resistance-Proofing Potential of Knockout Mutants
| Experimental Model | Findings for ΔacrB |
Findings for ΔrfaG / ΔlpxM |
Interpretation and Significance |
|---|---|---|---|
| Experimental Evolution under High Drug Pressure [23] | Most compromised in evolving resistance; driven to extinction more frequently than wild-type | More likely to be driven to extinction than wild-type | ΔacrB shows strong "resistance-proofing" characteristics under high selection |
| Adaptation at Sub-inhibitory Concentrations [23] | Recovered from hypersensitivity, but to a lesser extent than envelope mutants | Effectively recovered from hypersensitivity via drug-specific resistance mutations (e.g., folA upregulation) |
Resistance mutations can bypass defects in envelope biogenesis more easily than efflux deficiency |
Experimental Protocols: Methodologies for Validating Target Utility
Genome-Wide Susceptibility Screening with the Keio Collection
The Keio collection is a library of approximately 3,800 single-gene knockout mutants in E. coli K-12 BW25113, where each non-essential gene is replaced by a kanamycin resistance cassette [23]. This resource is fundamental for intrinsic resistome research.
Procedure:
- Growth Assay: Grow each knockout strain in 96-well plates containing Luria-Bertani (LB) broth supplemented with a target antibiotic at a predetermined concentration (e.g., the IC₅₀ for wild-type cells). Include a no-antibiotic control for each strain to account for general fitness defects.
- Phenotypic Measurement: After incubation, measure the optical density at 600 nm (OD₆₀₀) to quantify growth. Perform measurements in at least duplicate for statistical robustness.
- Data Analysis: Normalize the growth of each knockout strain to the wild-type control grown under the same condition. Calculate the fold-over-wild-type value. Hypersensitive mutants are typically defined as those showing growth lower than two standard deviations from the median of the resulting Gaussian distribution.
- Hit Validation: Candidates identified from the primary screen should be re-tested in dose-response assays (MIC determination) to confirm and quantify the degree of hypersusceptibility.
Laboratory Evolution of Hypersusceptible Mutants
This protocol tests the "resistance-proofing" potential of a sensitizing mutation by challenging a knockout strain to evolve resistance under antibiotic pressure.
Procedure:
- Inoculation: Start independent replicate cultures (e.g., 6-12) of the knockout mutant (e.g., Δ
acrB) and the wild-type control in liquid media containing a sub-inhibitory concentration of an antibiotic (e.g., trimethoprim). - Serial Passaging: Daily, transfer a small aliquot of each culture into fresh media containing the same or a progressively increasing concentration of the antibiotic. This constant selection pressure drives adaptive evolution.
- Monitoring: Regularly monitor the MIC of the evolved populations against the selecting antibiotic to track the emergence of resistance.
- Endpoint Analysis: After a predetermined number of generations (e.g., 200-300), sequence the genomes of the evolved populations that successfully grew at high antibiotic concentrations. Identify and compare the mutations that have fixed in the knockout versus the wild-type backgrounds to understand the constrained evolutionary pathways.
Assessing Biofilm Formation and Virulence
For efflux pumps like AcrB, which have roles beyond antibiotic resistance, functional assays are crucial.
Biofilm Formation Assay (Crystal Violet Staining):
- Growth: Grow bacterial strains (wild-type, Δ
acrB, and complemented mutant) in static cultures within polystyrene microtiter plates for 24-48 hours under conditions that promote biofilm formation. - Staining and Quantification: Carefully remove the planktonic cells, stain the adhered biomass with a crystal violet solution, and then dissolve the bound dye in acetic acid or ethanol.
- Measurement: Measure the absorbance of the dissolved dye at 570-595 nm. A significant reduction in absorbance in the Δ
acrBstrain compared to the wild-type indicates a defect in biofilm formation, as demonstrated in EAEC [48].
In Vivo Virulence Assay (C. elegans Killing Model):
- Infection: Feed Caenorhabditis elegans nematodes with the bacterial strain of interest (e.g., EAEC 17-2 and its Δ
acrBderivative) [48]. - Survival Monitoring: Transfer the infected nematodes to new plates and monitor their survival over several days.
- Analysis: Compare the survival curves of nematodes infected with the mutant strain versus the wild-type. A significant delay in killing by the mutant strain confirms the role of the target in virulence.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Intrinsic Resistome Investigation
| Reagent / Resource | Description | Key Application in Research |
|---|---|---|
| Keio Collection [23] | A nearly complete collection of single-gene knockouts in E. coli BW25113. | Genome-wide identification of genes that confer hypersusceptibility when knocked out. |
| Efflux Pump Inhibitors (EPIs) (e.g., PAβN, CCCP) [47] | Small molecules that block the activity of efflux pumps. | Pharmacological validation of efflux pump targets; used in combination assays to restore antibiotic susceptibility. |
| Chlorpromazine [23] | A known EPI that can be used in proof-of-concept studies. | Comparing genetic vs. pharmacological inhibition of efflux and studying evolutionary adaptation to EPI-antibiotic combinations. |
| pKD46 / pCP20 Plasmids [48] | Plasmids for Red recombinase-mediated gene knockout and subsequent antibiotic marker excision in E. coli. | Construction of clean, unmarked deletion mutants in clinical or other non-K-12 strains. |
| Complementation Vectors (e.g., pGIP7-derived) [48] | Cloning vectors with inducible promoters for expressing the gene of interest in trans. | Confirming that the observed phenotype is due to the specific gene deletion and not secondary mutations. |
The systematic exploration of the intrinsic resistome has firmly established efflux pumps like AcrB and cell envelope biogenesis factors like RfaG and LpxM as high-priority targets for antibacterial sensitization. Genetic and pharmacological inhibition of these systems significantly increases bacterial susceptibility to a broad spectrum of antibiotics. Critically, impairing these intrinsic resistance pathways, particularly efflux, can also constrain the evolutionary potential of bacteria, offering a dual strategy of sensitization and "resistance-proofing" [23]. Future research must focus on translating this genetic validation into clinically viable therapeutics. This endeavor requires overcoming the challenges associated with developing safe and effective small-molecule inhibitors, particularly against efflux pumps. Furthermore, a deeper understanding of the mutational repertoires that allow bacteria to bypass the inhibition of these intrinsic resistance pathways is essential for predicting and preempting resistance to the sensitizers themselves. The integration of advanced techniques, including structure-based drug design, machine learning, and high-throughput screening, will be paramount in leveraging these promising targets to rejuvenate our antibiotic arsenal.
The escalating crisis of antimicrobial resistance (AMR) represents one of the most significant threats to modern healthcare, with multidrug-resistant bacterial infections causing approximately 0.7 million deaths annually and projected to cause 10 million deaths by 2050 [49]. The drug discovery pipeline has failed to keep pace with evolving resistance mechanisms, creating an urgent need for innovative therapeutic strategies that extend the efficacy of existing antibiotics [49] [50]. Within this landscape, the concept of the "intrinsic resistome" – the collection of chromosomal genes that contribute to innate bacterial antibiotic resistance – has emerged as a promising therapeutic target [6] [23]. The adjuvant approach represents a paradigm shift from conventional antibiotic discovery by employing non-antibiotic compounds that specifically target bacterial resistance mechanisms, thereby revitalizing obsolete drugs and creating effective combination therapies against multidrug-resistant pathogens [49].
This strategy recognizes that intrinsic resistance mechanisms, including reduced membrane permeability, chromosomally encoded efflux pumps, and adaptive stress responses, form the foundational barriers that antibiotics must overcome before encountering their primary targets [20] [23]. By targeting these fundamental resistance pathways with specific inhibitors, the adjuvant approach seeks to sensitize resistant bacteria to conventional antibiotics, effectively expanding our therapeutic arsenal without requiring the development of entirely new drug classes [49]. This technical review examines the scientific foundations, mechanistic insights, and experimental methodologies underlying the development of intrinsic resistance inhibitors as antibiotic adjuvants, providing researchers with a comprehensive framework for advancing this promising field.
Core Mechanisms of Intrinsic Resistance as Therapeutic Targets
Bacterial Resistance Fundamentals
Bacteria employ sophisticated mechanisms to resist antibiotic action, which can be categorized as either acquired or intrinsic. Acquired resistance develops through horizontal gene transfer or mutations, while intrinsic resistance is an innate characteristic of a bacterial species, independent of prior antibiotic exposure [20] [50]. The intrinsic resistome encompasses genes involved in cell envelope biogenesis, membrane transport, and information transfer pathways that collectively limit antibiotic access and accumulation [23]. The major mechanisms of intrinsic resistance include:
Reduced Permeability Barriers: The outer membrane of Gram-negative bacteria, with its lipopolysaccharide (LPS) layer, serves as a formidable barrier to hydrophilic antibiotics, which must traverse porin channels for intracellular access [49]. Downregulation or mutation of porin proteins (e.g., OmpF and OmpC in Escherichia coli) significantly contributes to resistance against carbapenems and cephalosporins in Enterobacteriaceae [49].
Efflux Pump Systems: Resistance-nodulation-division (RND) family efflux pumps (e.g., AcrB in E. coli and MexB in Pseudomonas aeruginosa) actively export multiple classes of antibiotics from the cell [49] [6]. These homotrimeric complexes form tripartite systems with outer membrane channels and periplasmic adaptor proteins to facilitate drug extrusion across both membrane layers [49].
Enzymatic Inactivation and Modification: Bacteria produce enzymes that chemically modify or degrade antibiotics before they reach their targets, with β-lactamases being the most clinically significant example [20].
Target Modification and Protection: Mutations in antibiotic target sites (e.g., gyrase and topoisomerase for fluoroquinolones) or expression of proteins that protect these targets contribute to resistance [6] [50].
Table 1: Major Intrinsic Resistance Mechanisms and Examples
| Mechanism | Functional Components | Representative Antibiotics Affected |
|---|---|---|
| Reduced Permeability | Porins (OmpF, OmpC), LPS layer | β-lactams, Carbapenems, Vancomycin* |
| Efflux Systems | RND pumps (AcrB, MexB), MFS transporters | Fluoroquinolones, Tetracyclines, Macrolides |
| Enzymatic Inactivation | β-lactamases, Aminoglycoside-modifying enzymes | β-lactams, Aminoglycosides |
| Target Modification | RNA polymerase, Ribosomal subunits, DHFR | Rifampin, Macrolides, Trimethoprim |
Note: Vancomycin intrinsic resistance in Gram-negatives due to outer membrane impermeability [49]
The Intrinsic Resistome Concept
The term "intrinsic resistome" encompasses all chromosomal genes that contribute to intrinsic antibiotic resistance, regardless of their primary cellular functions [23]. Genome-wide screens in model organisms such as E. coli and Pseudomonas aeruginosa have identified diverse genes involved in cell envelope biogenesis, membrane transport, and central metabolism that significantly influence baseline antibiotic susceptibility [23]. For instance, a systematic screen of the E. coli Keio collection (comprising ~3,800 single-gene knockouts) identified 35 and 57 knockouts that were hypersensitive to trimethoprim and chloramphenicol, respectively, with enrichment in genes involved in cell envelope biogenesis, information transfer, and membrane transport pathways [23]. This demonstrates that intrinsic resistance is mediated by complex networks of genes beyond the canonical resistance mechanisms.
Strategic Approaches to Intrinsic Resistance Inhibition
Efflux Pump Inhibitors (EPIs)
Efflux pumps represent particularly attractive targets for adjuvant development due to their contribution to multidrug resistance phenotypes [49] [23]. RND-type efflux pumps recognize and export structurally diverse antibiotics, and their overexpression can confer clinically significant resistance levels [49]. Inhibiting these pumps through genetic knockout (e.g., ΔacrB) or pharmacological inhibition (e.g., with chlorpromazine) significantly increases bacterial susceptibility to multiple antibiotic classes [23]. However, evolutionary studies reveal that bacteria can develop resistance to EPIs themselves, highlighting the need for compounds with high barriers to resistance [23].
Membrane Permeabilizers
Compounds that disrupt the integrity of the bacterial outer membrane can potentiate antibiotics that have intracellular targets [49]. These include small molecules, antimicrobial peptides, and polymyxin derivatives that interact with lipopolysaccharide components to increase membrane permeability [23]. While effective sensitizers, many membrane permeabilizers face toxicity challenges that limit their clinical application [49].
Targeting Cell Wall Biosynthesis and Maintenance
Inhibitors of teichoic acid synthesis and other cell envelope components can disrupt critical resistance pathways in Gram-positive bacteria [49]. Similarly, perturbations in lipopolysaccharide biosynthesis (e.g., rfaG or lpxM knockouts in E. coli) increase susceptibility to hydrophobic antibiotics by altering outer membrane integrity [23]. These targets offer opportunities for developing selective adjuvants with activity against specific bacterial groups.
Enzymatic Inhibitors
The most clinically successful adjuvants to date are β-lactamase inhibitors (e.g., clavulanate, tazobactam, avibactam), which restore the activity of β-lactam antibiotics against resistant strains [49] [51]. Newer inhibitors like taniborbactam and zidebactam extend this approach to previously unmanageable carbapenemases [6]. This established clinical validation provides a roadmap for developing inhibitors against other resistance enzymes.
Table 2: Classes of Antibiotic Adjuvants Targeting Intrinsic Resistance
| Adjuvant Class | Molecular Targets | Representative Agents | Stage of Development |
|---|---|---|---|
| β-lactamase Inhibitors | Serine & metallo-β-lactamases | Clavulanate, Taniborbactam, Zidebactam | Clinically approved & late-stage development [6] [51] |
| Efflux Pump Inhibitors | RND transporters | Piperine, Chlorpromazine, Verapamil | Preclinical research [49] [23] |
| Membrane Permeabilizers | LPS, phospholipids | Polymyxin derivatives, Antimicrobial peptides | Some clinically approved with toxicity concerns [49] |
| Cell Wall Biosynthesis Inhibitors | Teichoic acid, LPS biosynthesis | Undeveloped chemical matter | Early research stage [49] [23] |
Experimental Methodologies and Workflows
Genome-wide Resistance Mechanism Identification
The systematic identification of intrinsic resistance genes requires comprehensive genetic screening approaches. The following workflow illustrates the process for identifying hypersensitive mutants:
Identification of Intrinsic Resistance Genes
Library Preparation: Begin with a comprehensive mutant collection such as the E. coli Keio collection (~3,800 single-gene knockouts) [23]. Grow mutants in 96-well format with appropriate controls.
Antibiotic Exposure: Culture knockout strains in duplicate in LB media supplemented with antibiotics at their IC50 values, alongside antibiotic-free controls [23]. Incubate with appropriate aeration and duration for the target pathogen.
Growth Assessment: Measure optical density at 600 nm (OD600) for each knockout strain and calculate as fold growth over wild type. Compile a Gaussian distribution of drug susceptibilities with a mean of approximately 1 [23].
Hypersusceptible Mutant Identification: Classify knockouts that show poor growth in the presence of antibiotic (lower than two standard deviations from the median distribution) but normal growth in control media as hypersensitive [23].
Secondary Validation: Confirm hypersensitivity phenotypes through dose-response curves and spot assays. Eliminate mutants with general growth defects.
Pathway Analysis: Categorize hypersensitive mutants by functional annotation using databases such as Ecocyc to identify enriched cellular pathways [23].
Adjuvant Screening and Synergy Testing
Once potential targets are identified, the following protocols facilitate the screening and characterization of adjuvant compounds:
Checkerboard Assay Protocol:
- Prepare serial two-fold dilutions of the antibiotic in Mueller-Hinton broth along the x-axis of a 96-well microtiter plate.
- Prepare serial two-fold dilutions of the potential adjuvant compound along the y-axis.
- Inoculate wells with approximately 5 × 10^5 CFU/mL of the target bacterial strain.
- Incubate plates at 35°C for 16-20 hours.
- Determine the fractional inhibitory concentration (FIC) index using the formula: FIC index = (MIC of antibiotic in combination/MIC of antibiotic alone) + (MIC of adjuvant in combination/MIC of adjuvant alone).
- Interpret results: FIC index ≤0.5 indicates synergy; >0.5-4 indicates additivity or indifference; >4 indicates antagonism [51].
Time-Kill Kinetics Assay:
- Prepare cultures with approximately 10^6 CFU/mL in the presence of: (a) antibiotic alone at relevant concentrations, (b) adjuvant alone, (c) antibiotic-adjuvant combination, and (d) growth control without agents.
- Incubate at 35°C with shaking and remove aliquots at 0, 4, 8, and 24 hours.
- Perform serial dilutions and plate on Mueller-Hinton agar for viable counts.
- Synergy is defined as a ≥2-log10 decrease in CFU/mL with the combination compared to the most active single agent after 24 hours [51].
Resistance Evolution Studies
Evaluating the evolutionary consequences of adjuvant use is critical for predicting clinical longevity:
Experimental Evolution Protocol:
- Initiate multiple (typically 6-12) parallel populations from isogenic clones of the target strain.
- Culture populations in the presence of: (a) antibiotic alone at sub-MIC concentrations, (b) adjuvant alone, and (c) antibiotic-adjuvant combination.
- Propagate cultures daily by transferring to fresh media with the same drug regimen.
- Monitor population densities and periodically archive frozen samples.
- After 20-50 daily passages, assess evolved populations for changes in susceptibility and cross-resistance.
- Sequence genomes of evolved clones to identify compensatory mutations and resistance mechanisms [23].
Research Reagent Solutions Toolkit
Table 3: Essential Research Tools for Adjuvant Development
| Reagent/Catalog | Specifications | Research Application | Key Considerations |
|---|---|---|---|
| Keio E. coli Knockout Collection | ~3,800 single-gene deletions [23] | Genome-wide identification of intrinsic resistance genes | Provides comprehensive coverage of non-essential genes |
| CARD Database | Comprehensive Antibiotic Resistance Database [24] | Annotation and identification of ARGs | Curated resource linking ARGs to molecular mechanisms |
| Chlorpromazine hydrochloride | Efflux pump inhibitor [23] | Proof-of-concept EPI studies | Off-target effects at higher concentrations; toxicity concerns |
| Mueller-Hinton Broth/Agar | Standardized per CLSI guidelines | Susceptibility testing and synergy assays | Essential for reproducible MIC determinations |
| 96-well Microtiter Plates | Sterile, tissue-culture treated | High-throughput screening assays | Enable automation for large compound libraries |
| CLSI Reference Strains | e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853 | Quality control for susceptibility testing | Ensure inter-laboratory reproducibility |
Visualization of Resistance and Adjuvant Mechanisms
The following diagram illustrates the major intrinsic resistance mechanisms and their corresponding adjuvant strategies:
Resistance Mechanisms and Adjuvant Targets
Quantitative Assessment of Adjuvant Efficacy
Table 4: Experimental Data from Genetic Inhibition of Intrinsic Resistance
| Genetic Modification | Antibiotic Tested | Fold Change in Susceptibility | Key Findings | Evolutionary Constraints |
|---|---|---|---|---|
| ΔacrB (efflux pump) | Trimethoprim | ≥8-fold increase [23] | Most compromised in evolving resistance; promising for "resistance proofing" | Limited evolutionary recovery; high extinction under drug pressure |
| ΔrfaG (LPS biosynthesis) | Trimethoprim | ≥8-fold increase [23] | Significant hypersensitivity; moderate evolutionary recovery | Partial recovery via target upregulation mutations |
| ΔlpxM (LPS biosynthesis) | Trimethoprim | ≥8-fold increase [23] | Significant hypersensitivity; substantial evolutionary recovery | Effective bypass via resistance mutations in drug-specific pathways |
| ΔacrB + Chlorpromazine | Trimethoprim | Similar to genetic knockout [23] | Qualitatively similar but distinct evolutionary outcomes | EPI resistance emergence; multidrug adaptation observed |
Future Directions and Implementation Challenges
The clinical translation of intrinsic resistance inhibitors faces several significant challenges. Toxicity concerns, particularly for membrane-targeting compounds, remain a major barrier [49]. Additionally, the evolutionary capacity of bacteria to develop resistance to adjuvants themselves, as demonstrated by adaptation to efflux pump inhibitors, necessitates careful consideration of combination regimens and dosing strategies [23]. Promising research directions include:
- Polypharmacological Approaches: Developing single compounds that simultaneously target multiple resistance mechanisms [49].
- Host-Directed Therapies: Modulating host immune responses to enhance bacterial clearance in combination with antibiotics [49].
- Artificial Intelligence and Machine Learning: Accelerating adjuvant discovery through predictive modeling of compound efficacy and resistance evolution [6].
- One Health Perspectives: Integrating surveillance of environmental resistomes to anticipate emerging resistance threats [6] [24].
The adjuvant strategy represents a versatile and orthogonal approach to conventional antibiotic discovery that leverages our growing understanding of bacterial intrinsic resistance mechanisms. By systematically targeting the foundational elements of the intrinsic resistome, this approach offers a promising pathway to extend the clinical utility of existing antibiotics and combat the escalating threat of antimicrobial resistance.
The intrinsic resistome encompasses all chromosomal genes and molecular pathways that contribute to a bacterium's innate ability to limit antibiotic efficacy [6]. Unlike acquired resistance mechanisms obtained through horizontal gene transfer, intrinsic resistance is a fundamental characteristic of bacterial species, encoded within their core genome and regulated by complex genetic networks [35]. This molecular framework presents a formidable barrier to conventional antibiotics, particularly in notorious pathogens such as Mycobacterium abscessus, which has been dubbed an "antibiotic nightmare" due to its multifaceted defense systems [35] [52]. The emerging paradigm of "resistance hacking" represents a fundamental shift in antimicrobial strategy, moving beyond circumventing resistance toward actively exploiting these intrinsic bacterial defense systems for therapeutic benefit [53]. This approach utilizes the molecular machinery of resistance—including regulatory networks, efflux systems, and enzymatic detoxification pathways—as precise triggers for antibiotic activation, thereby transforming the bacterium's protective mechanisms into vulnerability points [35].
Molecular Foundations of Bacterial Resistance Systems
The WhiB7 Resistome: A Master Regulatory Network
At the core of intrinsic resistance in mycobacterial species lies the WhiB7 regulon, a sophisticated stress response system that coordinates over 100 proteins involved in antimicrobial resistance [35]. WhiB7 functions as a master regulator of ribosomal stress, activating cascades of resistance mechanisms when bacteria encounter antibiotics that target protein synthesis [53]. This comprehensive response includes upregulation of efflux pumps, modification of antibiotic targets, and production of drug-inactivating enzymes [35]. The WhiB7 network exemplifies the complexity of the intrinsic resistome, demonstrating how bacterial pathogens integrate multiple defense strategies into a coordinated system that presents a formidable barrier to conventional antibiotic treatments [53] [35].
Table 1: Key Components of Bacterial Intrinsic Resistome Systems
| System Component | Function in Resistance | Pathogens Where Prominent |
|---|---|---|
| WhiB7 Regulon | Master regulator of ribosomal stress response; coordinates >100 resistance proteins [53] [35] | Mycobacterium abscessus, other mycobacteria [35] |
| Eis2 Enzyme | Acetyltransferase that modifies antibiotic structures [35] | Mycobacterium abscessus [35] |
| RND Family Efflux Pumps | Broad-spectrum antibiotic extrusion [6] | Pseudomonas aeruginosa, Escherichia coli [6] |
| Chromosomal β-lactamases | Enzymatic inactivation of β-lactam antibiotics [6] | Various Gram-negative bacteria [6] |
| SOS Regulon | DNA repair system induced by antibiotic stress; promotes mutagenesis [6] | Multiple bacterial pathogens [6] |
Enzymatic Resistance Mechanisms
Bacterial pathogens employ diverse enzymatic strategies to neutralize antibiotics, including modification, degradation, and target alteration. The Eis2 enzyme in M. abscessus exemplifies this strategy, functioning as an acetyltransferase that modifies antibiotic structures to render them ineffective [35]. Similarly, β-lactamases represent a broad family of resistance enzymes that hydrolyze β-lactam antibiotics, while aminoglycoside-modifying enzymes confer resistance through phosphorylation, adenylation, or acetylation of key antibiotic functional groups [6]. These enzymatic systems are particularly problematic in clinical settings because they can be horizontally transferred between bacterial species and are frequently subject to evolutionary optimization through point mutations that expand their substrate profiles [6].
Resistance Hacking: Theoretical Framework and Implementation
The Prodrug Concept in Antimicrobial Therapy
Prodrugs represent chemically modified versions of biologically active molecules that remain inert until undergoing specific activation within target cells or tissues [54]. This strategy addresses fundamental limitations in drug development, including poor solubility, limited bioavailability, metabolic instability, and off-target toxicity [54] [55]. In antimicrobial applications, prodrug design enables precise targeting of bacterial enzymatic systems while minimizing damage to host tissues [54]. It is estimated that over 10% of all marketed drugs utilize prodrug strategies, with increasing application in anti-infective development where targeted activation and reduced toxicity are paramount [54].
Case Study: Florfenicol Amine and the WhiB7-Eis2 Axis
A groundbreaking demonstration of resistance hacking involves the strategic redesign of florfenicol, a broad-spectrum antibiotic, to create a prodrug specifically activated by the WhiB7 resistance system in M. abscessus [53] [35]. The engineered florfenicol amine prodrug remains inactive until it enters bacterial cells, where it encounters Eis2, an acetyltransferase enzyme whose production is upregulated by WhiB7 as part of the intrinsic resistome [35]. Eis2 converts florfenicol amine into its active form, florfenicol acetyl, which subsequently inhibits bacterial ribosomes [35]. This ribosomal inhibition further activates WhiB7, creating a perpetual feed-forward loop that continuously amplifies antibiotic production within the bacterial cell [53] [35]. Remarkably, this system demonstrates exquisite specificity—the prodrug effectively kills wild-type M. abscessus but has no effect on strains lacking WhiB7, confirming that the resistance machinery is essential for drug activation [35].
Figure 1: The feed-forward activation mechanism of florfenicol amine prodrug. The bacterial resistance protein Eis2 converts the inert prodrug into its active form, which inhibits ribosomes and further activates WhiB7, creating a perpetual amplification cycle [53] [35].
Experimental Protocols for Resistance Hacking Research
Establishing Bacterial Culture and Mutant Validation
Materials:
- Wild-type Mycobacterium abscessus (ATCC 19977)
- WhiB7 knockout mutant strain
- Middlebrook 7H9 broth supplemented with 10% OADC enrichment
- Solid Middlebrook 7H10 agar plates
Methodology:
- Culture both wild-type and WhiB7 knockout strains in liquid 7H9 medium at 37°C with shaking at 120 rpm until mid-log phase (OD600 ≈ 0.6-0.8) [35].
- Prepare serial dilutions of bacterial cultures in sterile phosphate-buffered saline (PBS).
- Spot 10μL of each dilution onto 7H10 agar plates with and without antibiotic exposure.
- Confirm WhiB7 mutant phenotype through susceptibility testing with chloramphenicol and clarithromycin, which should show increased sensitivity in knockout strains compared to wild-type [35].
- Validate WhiB7 deletion through PCR amplification and sequencing of the WhiB7 locus.
Prodrug Susceptibility Testing and Mechanism Validation
Materials:
- Florfenicol amine prodrug stock solution (10mM in DMSO)
- Florfenicol standard (active control)
- Sterile 96-well tissue culture plates
- Microplate spectrophotometer
Methodology:
- Prepare two-fold serial dilutions of florfenicol amine and florfenicol in 7H9 broth across 96-well plates (concentration range: 0.5-128 μg/mL) [35].
- Inoculate wells with approximately 5×10^5 CFU/mL of either wild-type or WhiB7 knockout M. abscessus.
- Include growth control (no antibiotic) and sterility control (no bacteria) wells on each plate.
- Incubate plates at 37°C for 72 hours without shaking.
- Measure optical density at 600nm (OD600) using a microplate reader.
- Calculate minimum inhibitory concentration (MIC) as the lowest concentration that inhibits ≥90% of bacterial growth compared to growth control.
- Confirm paradoxical activity pattern: florfenicol amine should show potency against wild-type but not WhiB7 knockout strains, while conventional florfenicol shows reduced activity against both [35].
Enzyme Activation and Metabolic Conversion Assays
Materials:
- Purified Eis2 enzyme
- Radiolabeled or fluorescently tagged florfenicol amine substrate
- High-performance liquid chromatography (HPLC) system with mass spectrometry
- Acetyl coenzyme A (acetyl-CoA) cofactor
Methodology:
- Set up reaction mixtures containing 100μM florfenicol amine, 5μg purified Eis2 enzyme, and 200μM acetyl-CoA in appropriate reaction buffer [35].
- Incubate at 37°C and remove aliquots at predetermined time points (0, 15, 30, 60, 120 minutes).
- Terminate reactions with ice-cold methanol and remove precipitated protein by centrifugation.
- Analyze supernatants by HPLC-MS to detect conversion of florfenicol amine to florfenicol acetyl.
- Quantify reaction kinetics by measuring peak areas of substrate and product.
- Confirm identity of florfenicol acetyl through mass fragmentation patterns and comparison to synthetic standard.
Table 2: Quantitative Assessment of Florfenicol Amine Prodrug Activity
| Experimental Parameter | Wild-type M. abscessus | WhiB7 Knockout Mutant | Significance |
|---|---|---|---|
| Minimum Inhibitory Concentration (MIC) [35] | ≤4 μg/mL | >64 μg/mL | Confirms WhiB7-dependent activation |
| Rate of Intracellular Conversion to Active Drug [35] | High (within 2 hours) | Undetectable | Demonstrates Eis2-dependent activation |
| Induction of WhiB7 Regulon [35] | Strong upregulation | Not applicable | Validates feed-forward mechanism |
| Mitochondrial Toxicity in Mammalian Cells [35] | Significant reduction compared to conventional phenicols | Similar reduction | Enhanced therapeutic window |
| Efficacy in Macrophage Infection Model [35] | >3-log reduction in bacterial load | No significant reduction | Confirms intracellular activity |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Resistance Hacking Studies
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Bacterial Strains | Wild-type M. abscessus ATCC 19977, Isogenic WhiB7 knockout mutant [35] | Comparative validation of resistance-dependent activation |
| Prodrug Compounds | Florfenicol amine, Structural analogs with modified side chains [35] | Investigate structure-activity relationships and specificity |
| Enzymatic Assay Components | Purified Eis2 enzyme, Acetyl-CoA cofactor, HPLC-MS systems [35] | Quantify prodrug activation kinetics and metabolic conversion |
| Cell Culture Models | Murine macrophages (J774A.1), Human epithelial cell lines [35] | Assess intracellular antibacterial activity and host cell toxicity |
| Analytical Instruments | Microplate spectrophotometers, RT-qPCR systems, Mass spectrometers [35] | Quantify bacterial growth, gene expression, and metabolic products |
| Bioinformatics Tools | Whole-genome sequencing, Molecular docking software, Phylogenetic analysis [6] | Identify resistance homologs and predict prodrug-enzyme interactions |
Therapeutic Implications and Future Directions
The resistance hacking approach exemplified by the florfenicol amine prodrug offers substantial advantages over conventional antibiotic strategies. By leveraging the bacterial resistome for activation, this method achieves exceptional pathogen specificity, potentially minimizing disruption to commensal microbiota and reducing off-target toxicity [35]. The significantly reduced mitochondrial toxicity observed with florfenicol amine compared to conventional phenicol antibiotics demonstrates the potential for expanding therapeutic windows in clinical applications [35]. Future research directions include exploring the generalizability of this approach to other recalcitrant pathogens, optimizing prodrug pharmacokinetics through structural modification, and developing combination therapies that cycle between resistance-hacking antibiotics and conventional agents to prevent emergence of resistance [53] [35]. As computational methods advance, including machine learning and structural biology approaches, the systematic identification of resistance pathways amenable to hacking will accelerate, potentially transforming how we approach the growing crisis of antimicrobial resistance [6] [53].
Figure 2: Comprehensive experimental workflow for validating resistance-hacking prodrugs, from initial bacterial strain preparation through mechanistic studies and efficacy evaluation [35].
Navigating Evolutionary Roadblocks: Challenges in Targeting Intrinsic Resistance
The phenomenon of collateral sensitivity, wherein resistance to one antibiotic class confers heightened sensitivity to another, presents a promising avenue for combating antimicrobial resistance (AMR). This adaptive outcome creates a evolutionary constraint, potentially forcing pathogens into vulnerable states [56]. However, bacterial populations are dynamic systems capable of evolutionary recovery, where subsequent genetic changes can compensate for initial fitness trade-offs, allowing escape from these engineered vulnerabilities [57] [56]. Understanding the molecular mechanisms governing this recovery process within the framework of the intrinsic resistome—the native collection of chromosomal elements determining baseline susceptibility—is crucial for designing evolution-resistant therapeutic strategies [1].
This review synthesizes current knowledge on the molecular drivers of hypersensitivity and the evolutionary pathways enabling bacterial recovery. We analyze quantitative data from experimental evolution studies, detail methodologies for investigating these phenomena, and provide resources for researchers developing therapeutic strategies that exploit evolutionary constraints.
Molecular Foundations of Hypersensitivity and Recovery
Mechanisms Underlying Collateral Hypersensitivity
Collateral sensitivity arises when genetic adaptations conferring resistance to one antibiotic class simultaneously disrupt fundamental cellular processes that determine susceptibility to other antimicrobials. Key molecular mechanisms identified through laboratory evolution experiments include:
- Proton Motive Force (PMF) Reduction: Adaptation to aminoglycosides frequently selects for mutations that reduce the PMF across the inner membrane. While decreasing aminoglycoside uptake (a primary mechanism of resistance), this reduction concurrently diminishes the activity of PMF-dependent major efflux pumps like the AcrAB transporter, leading to hypersensitivity to multiple other antibiotic classes including β-lactams, fluoroquinolones, and tetracyclines [56].
- Efflux Pump Regulation: Mutations in global regulators (e.g., marA, soxS) or local repressors (e.g., mexR) can simultaneously alter expression of multiple efflux systems and porins, creating pleiotropic effects on drug susceptibility profiles [6] [1].
- Cell Envelope Remodeling: Modifications to membrane composition or cell wall biosynthesis pathways that provide resistance to specific drug classes can increase permeability to other antimicrobials, creating hypersensitive states [1].
Table 1: Primary Molecular Mechanisms Driving Collateral Hypersensitivity
| Mechanism | Resistance Conferred | Hypersensitivity Induced | Key Elements |
|---|---|---|---|
| PMF Reduction | Aminoglycosides | β-lactams, Fluoroquinolones, Tetracyclines | Membrane energetics, AcrAB efflux |
| Efflux Dysregulation | Multiple classes | Drug-specific patterns | MarA, SoxS, MexR regulators |
| Target Modification | Specific to target | Structurally unrelated drugs | Ribosomal mutations, Enzyme alterations |
| Envelope Remodeling | Detergents, Peptides | Hydrophobic compounds | LPS biosynthesis, Porin expression |
Pathways for Evolutionary Recovery
Evolutionary recovery from hypersensitivity occurs through genetic compensation that restores fitness without sacrificing primary resistance. Documented pathways include:
- Compensatory Mutations: Second-site mutations that restore PMF or efflux pump functionality without reinstating original drug uptake pathways. These mutations often occur in genes encoding metabolic enzymes or respiratory chain components that indirectly influence membrane energetics [57] [56].
- Regulatory Rewiring: Alterations in regulatory networks that fine-tune gene expression to balance resistance and sensitivity trade-offs. This includes mutations in two-component systems and small RNA regulators that modulate efflux pump expression with greater specificity [6].
- Horizontal Gene Transfer: Acquisition of plasmids or other mobile genetic elements carrying specialized resistance genes that bypass the original fitness cost, such as genes encoding drug-specific efflux pumps with reduced energy requirements [6] [24].
Diagram 1: Evolutionary recovery from antibiotic hypersensitivity
Quantitative Profiling of Hypersensitivity and Recovery
Patterns of Collateral Sensitivity
Large-scale laboratory evolution experiments with Escherichia coli have quantified the prevalence and strength of collateral sensitivity interactions. When populations were adapted to 12 different antibiotics, approximately 35% of all investigated antibiotic pairs showed collateral sensitivity in at least one direction [56]. The distribution of these interactions is non-random:
- Aminoglycoside Adaptation: 44% of all collateral sensitivity interactions involved aminoglycosides, with adapted strains showing 2- to 10-fold decreases in MIC to inhibitors of DNA synthesis, cell-wall synthesis, and other protein synthesis inhibitors [56].
- Target-Specific Depletion: Collateral sensitivity rarely occurs between antibiotic pairs targeting the same cellular subsystem (Fisher's exact test, P=0.013), suggesting common resistance mechanisms often confer cross-resistance rather than hypersensitivity [56].
- Trade-off Strength: The fitness cost of hypersensitivity mutations varies substantially, with some lineages showing minimal fitness defects in antibiotic-free medium while others exhibit significant growth impairment [56].
Table 2: Quantitative Profile of Collateral Sensitivity Interactions in E. coli
| Selecting Antibiotic | Hypersensitivity to | MIC Reduction (Fold) | Frequency in Evolved Populations |
|---|---|---|---|
| Aminoglycosides | β-lactams | 4-8x | 72% |
| Aminoglycosides | Fluoroquinolones | 3-6x | 68% |
| Aminoglycosides | Tetracyclines | 2-5x | 45% |
| β-lactams | Aminoglycosides | 2-4x | 31% |
| Tetracyclines | Aminoglycosides | 2-3x | 28% |
| Fluoroquinolones | β-lactams | 2-5x | 35% |
Dynamics of Evolutionary Recovery
The predictability of evolutionary recovery pathways depends on multiple factors, including the initial resistance mechanism, population size, and selective environment:
- Temporal Patterns: Recovery mutations typically emerge within 50-100 generations after the initial adaptation, with compensatory mutations generally preceding regulatory rewiring or horizontal gene transfer events [58].
- Genetic Constraints: The number of available compensatory mutations varies by gene, with essential genes and central metabolic pathways offering fewer evolutionary escape routes than regulatory elements [58].
- Population Dynamics: Larger populations recover more rapidly due to increased genetic diversity, while smaller populations may remain trapped in hypersensitive states for extended periods [58].
Experimental Framework for Investigating Recovery
Laboratory Evolution Protocols
Serial Passage under Dual Selection
This protocol tests evolutionary recovery under simultaneous pressure to maintain primary resistance while overcoming hypersensitivity:
- Initial Adaptation: Propagate 10-12 parallel populations of the target pathogen in increasing concentrations of Antibiotic A for 140-200 generations. Use daily 1:100 dilutions in fresh medium containing antibiotics [56].
- Hypersensitivity Validation: Measure MICs against Antibiotic B for all evolved populations. Confirm at least 4-fold decrease in MIC compared to ancestor.
- Recovery Phase: Propagate hypersensitive lineages in medium containing sub-MIC concentrations of both Antibiotic A (to maintain resistance) and Antibiotic B (to select against hypersensitivity). Continue for 100-150 generations with periodic fitness assessments.
- Whole-Genome Sequencing: Sequence endpoints of all recovery lineages and compare to hypersensitive intermediates to identify compensatory mutations.
Fitness Landscaping with Combinatorial Challenges
This approach maps the mutational pathways available for recovery from specific hypersensitivity profiles:
- Strain Construction: Generate isogenic strains carrying precise resistance mutations associated with hypersensitivity using CRISPR-based genome editing.
- Combinatorial Screening: Measure fitness of each engineered strain in 2D antibiotic matrices combining the primary drug with secondary agents to which hypersensitivity exists.
- Compensatory Mutation Identification: Use transposon mutagenesis or random mutagenesis to identify mutations that restore growth in the presence of both antibiotics.
- Trajectory Validation: Compete recovered mutants against ancestral hypersensitive strains to quantify fitness benefits.
Diagram 2: Experimental workflow for evolutionary recovery
Analytical Methods for Recovery Characterization
Genomic Analysis
- Whole-Genome Sequencing: Identify compensatory mutations through comparative analysis of hypersensitive and recovered lineages. Prioritize mutations occurring in parallel across independent lineages [56].
- Epistasis Mapping: Quantify interactions between primary resistance mutations and secondary compensatory mutations using fitness measurements in single and double mutants [58].
Functional Validation
- Proton Motive Force Quantification: Measure membrane potential using fluorescent dyes (e.g., DiOC₂(3)) to confirm restoration in recovered strains [56].
- Efflux Pump Activity Assays: Monitor efflux function using fluorescent substrates with and without efflux pump inhibitors to determine if recovery involves restored efflux capacity [6] [1].
- Transcriptomic Profiling: RNA sequencing of hypersensitive and recovered strains to identify regulatory changes contributing to recovery [6].
Research Toolkit for Hypersensitivity Studies
Table 3: Essential Research Reagents and Resources
| Category | Specific Reagents/Tools | Function/Application | Key Characteristics |
|---|---|---|---|
| Bacterial Strains | E. coli K-12 BW25113 | Laboratory evolution studies | Well-annotated genome, defined genetic background |
| Keio Collection knockout mutants | Functional validation of specific genes | Comprehensive single-gene knockout library [57] | |
| Selection Antibiotics | Aminoglycosides (gentamicin, tobramycin) | Inducing PMF-related hypersensitivity | |
| β-lactams (ampicillin, cefoxitin) | Counter-selection for hypersensitive strains | ||
| Analytical Tools | DiOC₂(3) fluorescent dye | PMF measurement and quantification | Membrane potential indicator |
| Carbonyl cyanide m-chlorophenyl hydrazone (CCCP) | PMF dissipation control | Protonophore positive control [56] | |
| Comprehensive Antibiotic Resistance Database (CARD) | ARG annotation and analysis | Curated resistance gene database [24] | |
| Genetic Tools | CRISPR-Cas9 genome editing | Precise introduction of resistance mutations | Allelic replacement in chromosomal genes |
| Transposon mutagenesis libraries | Recovery mutation identification | Genome-wide screening for compensatory mutations |
Understanding evolutionary recovery from antibiotic hypersensitivity provides critical insights for designing robust combination therapies that account for bacterial adaptive landscapes. The experimental frameworks outlined here enable systematic investigation of recovery pathways across diverse pathogen-drug combinations. By identifying and targeting the most constrained evolutionary trajectories—those with limited compensatory options—researchers can develop therapeutic sequences that effectively trap pathogens in hypersensitive states, extending the clinical lifespan of existing antibiotics and informing the design of next-generation antimicrobials with higher evolutionary barriers to resistance.
The intrinsic resistome encompasses all chromosomal genes and molecular systems that, through mutation, can confer a survival advantage to bacterial pathogens under antibiotic pressure [6] [24]. Unlike acquired resistance, which relies on horizontal gene transfer, this intrinsic capacity for adaptation is a fundamental property of a bacterial species' genome. Research into the intrinsic resistome reveals that bacterial pathogens are pre-equipped with a versatile genetic toolkit for survival. Mutations that bypass defects in primary resistance pathways represent a sophisticated evolutionary tactic within this toolkit. When a key resistance mechanism, such as an efflux pump or a drug-modifying enzyme, is compromised or becomes ineffective, selective pressure can favor mutations in seemingly unrelated genetic networks that circumvent the defect entirely, restoring fitness and resistance through alternative biochemical routes [59]. This review synthesizes current molecular insights and experimental evidence on how such bypass mutations fuel adaptation, framing them within the broader context of intrinsic resistome research and its implications for antimicrobial drug development.
Conceptual Frameworks: Genes-First and Phenotypes-First Adaptation
The emergence of resistance through mutation can be conceptualized through two complementary evolutionary models, which are crucial for understanding bypass mechanisms.
- The Genes-First Pathway: This classic model posits that a new, advantageous gene mutation is the primary event initiating a resistant phenotype. The genotype change directly and heritably drives the new adaptive trait. In chronic myeloid leukemia (CML), resistance to the targeted therapy imatinib arises predominantly through point mutations in the BCR-ABL1 kinase domain, which impair drug binding without bypassing the oncogene itself [60].
- The Phenotypes-First Pathway: This model suggests that genetically identical cells can fluctuate between different, non-heritable phenotypic states. A subpopulation of cells may exist in a transient, drug-tolerant state, which is later stabilized by genetic or epigenetic changes. This pathway is characterized by high-level cellular plasticity and can generate a continuum of resistance states. Evidence suggests that mutations in genes like TP53 can prime cells for such plasticity, enhancing their ability to explore phenotypic space and survive treatment long enough to acquire stabilizing mutations [60].
Table 1: Comparing Evolutionary Pathways to Resistance
| Feature | Genes-First Pathway | Phenotypes-First Pathway |
|---|---|---|
| Initial Event | New gene mutation | Phenotypic fluctuation in a genetically identical population |
| Heritability | Directly heritable | Initially non-heritable, later stabilized |
| Role of Plasticity | Low | High; a key driver of diversity |
| Temporal Dynamics | Step-wise | Continuum of states |
| Exemplary Mechanism | BCR-ABL1 kinase domain mutations in CML [60] | Transcriptional reprogramming in ovarian cancer treated with Olaparib [60] |
Diagram 1: Genes-first and phenotypes-first paths to resistance. The phenotypes-first path relies on initial non-heritable diversity, while the genes-first path originates from a new mutation.
Molecular Mechanisms of Bypass Mutations
Bypass mutations operate through diverse molecular mechanisms that rewire cellular networks. Key paradigms include:
Regulatory Network Rewiring
In Pseudomonas aeruginosa, the stringent response (SR) is a master regulator of virulence and stress survival. When the SR is defective, mutations in the transcriptional regulator MexT can bypass this defect and restore virulence activation. These mexT mutations act as a genetic switch, toggling virulence on and are concurrently associated with resistance to aminoglycosides and colistin. This demonstrates how a single regulatory mutation can circumvent a major defect and co-select for hypervirulence and multidrug resistance [59].
Exploiting Resistance Proteins
A proof-of-concept study in Mycobacterium abscessus demonstrates a unique form of "resistance hacking." A structurally modified version of the antibiotic florfenicol is engineered to be a prodrug. This prodrug is activated by Eis2, a protein that is part of the WhiB7-driven intrinsic resistome. The activated drug then inhibits the ribosome, which further activates WhiB7 and Eis2, creating a self-amplifying cycle that turns the bacterium's resistance machinery against itself [35].
Alternative Pathway Activation
In Escherichia coli evolving resistance to cefotaxime, mutator strains with limited ability to generate common TEM-1 β-lactamase mutations nonetheless achieved high-level resistance. This was accomplished by exploiting divergent paths, including alternative mutational pathways in PBP3, the antibiotic's primary cellular target. This highlights that when preferred mutational pathways are blocked, evolution can leverage mutations in alternative loci to achieve the same adaptive end [61].
Table 2: Exemplary Bypass Mutation Mechanisms in Bacterial Pathogens
| Bypass Target | Bypass Mechanism | Molecular Consequence | Pathogen | Reference |
|---|---|---|---|---|
| Stringent Response | Loss-of-function mutation in mexT | Derepression of virulence and resistance genes | Pseudomonas aeruginosa | [59] |
| WhiB7 Resistome | Prodrug activation by Eis2 resistance enzyme | Self-amplifying, perpetual antibiotic effect | Mycobacterium abscessus | [35] |
| TEM-1 β-lactamase | Mutations in PBP3 (antibiotic target) | Alternative target modification conferring high-level resistance | Escherichia coli | [61] |
Quantitative Foundations: Mutation Frequencies and Resistance
The likelihood of a bypass mutation emerging is governed by quantitative principles of mutability. The mutation rate (per generation) and the observed frequency of mutants in a population are distinct concepts influenced by a complex network of factors [62].
- Gene-Specific Mutability: Not all genes are equally mutable. The number of positions within a gene where a mutation is both non-lethal (permissive) and confers resistance directly influences its mutability. For example, in E. coli, quinolone resistance can arise from changes in at least seven positions in gyrA but only three in parC, making gyrA mutants more frequent [62].
- Multi-Locus Requirements: Resistance sometimes requires mutations in multiple genes. If mutations in either Gene A or Gene B confer resistance, the overall mutability is the sum of their individual mutabilities. However, if mutations in both Gene A and Gene B are required, the overall mutability is the product of their individual mutabilities, making such multi-step resistance far less probable [62].
- Physiological and Environmental Influences: Factors such as nutrient availability, antibiotic stress, and bacterial mutator phenotypes (caused by defects in DNA repair) can dramatically increase mutation rates, thereby enhancing the probability that rare bypass mutations will emerge [62].
Experimental Guide: Investigating Bypass Mutations
Studying bypass mutations requires methodologies that capture evolutionary dynamics and validate mechanistic hypotheses. The following provides a generalized protocol.
In Vitro Experimental Evolution
Objective: To select for and isolate mutants that bypass a defined genetic defect in a resistance pathway.
Detailed Protocol:
- Genetic Construction: Create an isogenic mutant strain with a deletion or disruption of a known primary resistance gene (e.g., a key efflux pump component or a regulatory gene like whiB7 or the stringent response machinery).
- Evolution Experiment: Serially passage the mutant strain and its wild-type control in parallel, in the presence of a sub-lethal to lethal concentration of the antibiotic of interest. Use a large number of independent populations (e.g., 96 as in [61]) to account for stochasticity.
- Population Monitoring: Periodically quantify the Minimum Inhibitory Concentration (MIC) for each population to track the trajectory of resistance evolution. Record population survival at critical concentrations as shown in survival curve analyses [61].
- Mutant Isolation: At the endpoint of the experiment or at points of significant MIC increase, plate cultures from evolved populations on solid media with and without antibiotic to isolate resistant clones.
Genomic and Transcriptomic Analysis
Objective: To identify the genetic basis and functional impact of the bypass mutation.
Detailed Protocol:
- Whole-Genome Sequencing: Sequence the genomes of evolved, resistant clones and compare them to the ancestral strain to identify single-nucleotide polymorphisms (SNPs), insertions, and deletions. Focus on mutations that are unique to the bypass clones evolved from the defective mutant background.
- Transcriptional Profiling: Perform RNA sequencing (RNA-seq) on the resistant bypass mutant, the ancestral strain, and the defective mutant. This identifies differentially expressed genes and pathways, revealing how the bypass mutation has rewired the regulatory network [59].
- Genetic Complementation: Clone the wild-type allele of the candidate bypass gene and reintroduce it into the resistant bypass mutant. A return to the susceptible phenotype confirms the causal role of the mutation.
Functional Validation
Objective: To confirm the mechanistic role of the identified mutation in the bypass phenotype.
Detailed Protocol:
- Site-Directed Mutagenesis: Engineer the specific identified point mutation into a clean genetic background (e.g., the original defective mutant) to reconstitute the bypass phenotype de novo.
- Biochemical Assays: Depending on the mechanism, perform assays such as:
- Electrophoretic Mobility Shift Assay (EMSA) to test if a regulatory protein's DNA-binding affinity is altered.
- Enzyme Activity Assays to measure the conversion of a prodrug to its active form [35].
- Drug Accumulation Assays to quantify intracellular antibiotic concentrations, assessing efflux activity.
- In Vivo Virulence Models: For pathogens, use animal models (e.g., a murine pulmonary model [59]) to compare the virulence of the bypass mutant with control strains, assessing if hypervirulence is part of the adapted phenotype.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Studying Bypass Mutations
| Reagent / Tool | Function in Research | Exemplary Use Case |
|---|---|---|
| Isogenic Mutant Strains | Provides a defined genetic background to study the specific effect of a deleted resistance gene. | Constructing a ΔmexT or ΔwhiB7 mutant to serve as the ancestor for evolution experiments [35] [59]. |
| CellDesigner with BioPAX Plug-in | Software for creating formal, machine-readable pathway diagrams, facilitating the modeling of network rewiring. | Mapping the altered regulatory network in a mexT mutant to visualize bypass connections [63]. |
| MdrDB Database | A large-scale database of mutation-induced drug resistance, used for comparing identified mutations against known resistant variants. | Annotating and assessing the potential impact of a novel PBP3 mutation identified in an evolved strain [64]. |
| Paxtools Library | A Java library for working with BioPAX pathway data, enabling computational analysis of molecular interactions. | Programmatically analyzing the output of the CellDesigner plug-in to identify central nodes in the bypass network [63]. |
| CARD (Comprehensive Antibiotic Resistance Database) | A curated database of ARGs and their mechanisms, used for annotating resistance genes in genomic or metagenomic data. | Identifying and classifying resistance genes in gut-derived bacterial genomes from wild rodents [24]. |
Diagram 2: A generalized workflow for the experimental identification and validation of bypass mutations.
Therapeutic Implications and Future Avenues
Understanding bypass mutations is critical for designing next-generation therapeutic strategies that anticipate and counter bacterial adaptation.
- Predicting Evolutionary Trajectories: Knowledge of common bypass routes allows for the forecasting of resistance evolution. For instance, if a drug inhibits a primary resistance enzyme, pre-emptive screens can be designed to identify mutations that activate alternative detoxification pathways.
- Combination Therapies: Therapeutics can be designed to simultaneously target the primary vulnerability and the most likely bypass pathway. This "one-two punch" approach, such as cycling between an antibiotic and a drug that blocks the predicted bypass route, could prevent resistance from emerging [35].
- Exploiting Resistance Mechanisms: The "resistance hacking" approach demonstrated with M. abscessus offers a paradigm-shifting strategy. By designing prodrugs activated specifically by the pathogen's resistance proteins, the therapeutic index can be dramatically improved, minimizing host toxicity and selectively targeting resistant bacteria [35].
- Addressing Phenotypic Plasticity: Combating phenotypes-first resistance requires drugs that target the mechanisms of cellular plasticity itself, such as specific epigenetic regulators or signaling nodes that facilitate state transitions, forcing the pathogen into a susceptible state [60].
Bypass mutations represent a fundamental and sophisticated component of the intrinsic resistome, allowing bacterial pathogens to navigate around genetic defects and therapeutic interventions through regulatory rewiring, alternative pathway activation, and even the co-option of their own defense systems. The interplay between genes-first and phenotypes-first pathways underscores the complexity of predicting resistance evolution. Moving forward, integrating evolutionary principles into drug discovery—through the predictive modeling of bypass routes, the development of combination therapies, and the innovative engineering of drugs that exploit resistance mechanisms—will be paramount in extending the lifespan of existing antibiotics and curbing the global antimicrobial resistance crisis.
{: .no_toc}
Table of Contents
- A markdown unordered list which will be replaced with the table of contents. {:toc}
The intrinsic resistome encompasses all chromosomally encoded elements that contribute to the innate antibiotic resistance of a bacterial species, with multidrug efflux pumps serving as one of its principal components [1]. The strategic inhibition of these pumps presents a promising avenue for rejuvenating the efficacy of existing antibiotics. However, a critical divergence exists between the validation of efflux pumps as targets through genetic knockout studies and the clinical application of pharmacological efflux pump inhibitors (EPIs). Genetic inactivation, such as deletion of the tolC gene in Escherichia coli or oprM in Pseudomonas aeruginosa, robustly demonstrates the potential of efflux blockade by significantly increasing bacterial susceptibility to a wide range of antibiotics [13] [65]. In contrast, the development of pharmacological EPIs has been fraught with challenges, including failure to restore full susceptibility in multi-drug resistant (MDR) clinical isolates, substrate-specific inhibition, cellular toxicity, and poor pharmacokinetics [66] [13] [11]. This whitepaper delineates the molecular basis, experimental methodologies, and emerging resistance mechanisms underlying this divergence, providing a technical guide for researchers and drug development professionals navigating this complex field. The integration of advanced genetic tools, structural biology, and machine learning is imperative for the rational design of next-generation EPIs that can bridge the gap between genetic promise and therapeutic reality.
The concept of the intrinsic resistome has reframed our understanding of antibiotic resistance. It is defined as the set of chromosomally encoded elements that contribute to antibiotic resistance, independent of previous antibiotic exposure or horizontal gene transfer [1]. This reservoir of resistance determinants is a fundamental property of a bacterial species, arising from genes often involved in basic metabolism and physiological functions [1] [6]. A major component of the intrinsic resistome is the arsenal of multidrug efflux pumps, transmembrane transporters that expel a diverse array of structurally unrelated antibiotics from the bacterial cell, thereby reducing intracellular accumulation to sub-toxic levels [66] [67] [68].
Efflux pumps are ubiquitous in bacteria and are broadly classified into six families based on their structure and energy source: the ATP-binding cassette (ABC) superfamily, the Major Facilitator Superfamily (MFS), the Resistance-Nodulation-Division (RND) family, the Multidrug and Toxic Compound Extrusion (MATE) family, the Small Multidrug Resistance (SMR) family, and the Proteobacterial Antimicrobial Compound Efflux (PACE) family [68] [65]. Of these, the RND-type pumps, such as AcrAB-TolC in E. coli and MexAB-OprM in P. aeruginosa, are particularly significant in Gram-negative pathogens due to their broad substrate profiles and contribution to intrinsic and acquired multidrug resistance [67] [11]. These pumps are tripartite complexes that span the entire cell envelope, actively extruding antibiotics from the inner membrane and periplasm directly to the external environment [67] [68].
The critical role of efflux pumps in the intrinsic resistome makes them attractive therapeutic targets. The central hypothesis is that inhibiting these pumps with Efflux Pump Inhibitors (EPIs) will potentiate the activity of existing antibiotics, effectively reversing resistance and restoring clinical utility [66]. However, the path to clinically viable EPIs has been marked by a significant divergence between the compelling results obtained through genetic inhibition and the more modest outcomes from pharmacological inhibition. This document explores the roots of this divergence, providing a technical and strategic framework for future research and development.
Molecular Mechanisms of Efflux and Inhibition
Efflux Pump Structure and Function
The RND efflux pumps, which are primary clinical targets, function as sophisticated tripartite complexes. The system comprises: (i) an inner membrane RND transporter (e.g., AcrB, MexB) that utilizes the proton motive force for energy; (ii) a periplasmic membrane fusion protein (MFP; e.g., AcrA, MexA) that structurally links the inner and outer membrane components; and (iii) an outer membrane factor (OMF; e.g., TolC, OprM) that forms a channel through the outer membrane [67] [68] [11]. The functional unit is a homotrimer, creating a contiguous conduit from the cytoplasm to the extracellular space [68].
These pumps operate via a sophisticated functional rotation mechanism. In the case of AcrB, the trimer cycles through three conformational states—loose (L), tight (T), and open (O)—in a concerted, cyclic manner. Substrates are initially recognized from the periplasm or the inner membrane leaflet in the L state. They are then transferred to the T state, where they are bound tightly, and finally expelled through the O state into the TolC channel [65]. This peristaltic mechanism allows for the efflux of an incredibly diverse set of substrates, including fluoroquinolones, β-lactams, macrolides, tetracyclines, dyes, and biocides [66] [65].
Genetic vs. Pharmacological Inhibition Mechanisms
The mechanisms for disabling efflux pumps differ fundamentally between genetic and pharmacological approaches.
- Genetic Inhibition: This typically involves the deletion or disruption of genes encoding essential components of the efflux pump machinery. For example, deleting tolC in E. coli or oprM in P. aeruginosa disables multiple RND pumps that rely on these shared outer membrane proteins, leading to a comprehensive loss of efflux function [13]. This approach provides a complete and unambiguous validation of the target's role in resistance.
- Pharmacological Inhibition: Small molecule EPIs employ diverse strategies to block efflux, including:
- Competitive Binding: Directly binding to the substrate binding pocket of the transporter (e.g., AcrB), thereby physically blocking antibiotic recognition and displacement [66] [65].
- Energy Dissipation: Collapsing the proton motive force (PMF) that energizes secondary active transporters. Compounds like Carbonyl cyanide m-chlorophenyl hydrazone (CCCP) are classic laboratory examples, though they are too toxic for clinical use [66].
- Inhibiting Assembly: Interfering with the assembly of the functional tripartite complex, thus preventing the formation of a functional conduit [66].
Figure 1: Mechanisms of Efflux Pump Inhibition. The diagram illustrates the structure of a tripartite RND efflux pump and the points of intervention for genetic knockout and different classes of pharmacological Efflux Pump Inhibitors (EPIs).
Quantitative Comparison of Inhibition Efficacy
A direct comparison of the outcomes from genetic and pharmacological inhibition reveals a stark efficacy gap, particularly in clinically relevant strains.
Table 1: Efficacy of Genetic vs. Pharmacological Efflux Inhibition in MDR Clinical Isolates
| Inhibition Method | Experimental Model | Impact on Antibiotic MIC | Key Findings and Limitations |
|---|---|---|---|
| Genetic Deletion | Deletion of tolC in 18 MDR clinical E. coli isolates [13] | Decreased MIC for multiple antibiotics; but all strains retained MDR status due to other resistance mechanisms. | Pro: Abolishes efflux activity. Con: Does not restore full susceptibility in complex MDR backgrounds. Highlights necessity of combination therapy. |
| Pharmacological Inhibition (Lab EPIs) | Use of CCCP or PAβN with laboratory strains [66] [13] | Dramatic increase in susceptibility; can render Gram-negative bacteria susceptible to Gram-positive-specific drugs (e.g., macrolides) [1]. | Pro: Validates the concept of efflux inhibition. Con: Results from lab strains poorly predict efficacy in clinical MDR isolates [13]. |
| Pharmacological Inhibition (Clinical Context) | Use of EPIs against MDR clinical isolates expressing multiple resistance mechanisms [13] [11] | Only moderate impact on resistance; insufficient to restore full clinical susceptibility for many drug classes. | Pro: Shows some potentiation. Con: EPI activity is often substrate-specific and incomplete; other co-existing resistance mechanisms (ESBLs, carbapenemases) dominate the phenotype. |
Table 2: Impact of Efflux on Novel β-lactam/β-lactamase Inhibitor (BL/BLI) Combinations
| Antibiotic Combination | Relevant Pathogen | Efflux-Mediated Resistance Mechanism | Experimental Evidence |
|---|---|---|---|
| Ceftazidime/Avibactam (CZA) | P. aeruginosa | Mutations leading to overexpression of MexAB-OprM [11]. | Genetically validated; overexpression alone can confer resistance. |
| Ceftolozane/Tazobactam (C/T) | P. aeruginosa | Overexpression of MexAB-OprM; mutations in MexVW and MexMN efflux systems [11]. | Identified via in vitro experimental evolution and genetic engineering. |
| Cefepime/Zidebactam (FEP/ZID) | P. aeruginosa | Involvement of under-characterized pumps like MexVW [11]. | Emerging genomic data from resistant clinical isolates and lab studies. |
The data clearly show that while genetic knockout provides a clean, system-wide abolition of efflux that is useful for target validation, its effect in clinical MDR isolates is tempered by the presence of other resistance genes [13]. Pharmacological inhibition, as demonstrated with both early-stage and modern EPIs, has so far failed to replicate the dramatic hypersusceptibility seen in genetically modified laboratory strains, underscoring the complexity of the clinical resistance landscape.
Experimental Protocols for Efflux Pump Research
Genetic Engineering of Efflux Mutants in MDR Isolates
The study of efflux in clinically relevant backgrounds requires robust genetic tools. A 2019 study developed a versatile method for generating gene deletions in multi-drug resistant clinical isolates, which often resist standard techniques due to their complex resistance profiles [13].
Protocol: Gene Deletion in MDR Clinical E. coli and P. aeruginosa
Selection Marker System:
- Positive Selection: Utilize a tellurite resistance cassette (tpm gene). Since most clinical isolates are susceptible to tellurite, this provides a powerful and broadly applicable selection marker that is independent of standard antibiotic resistance genes [13].
- Negative Selection: Use the sacB gene from Bacillus subtilis, which confers sucrose sensitivity. This allows for counterselection and the creation of markerless deletions [13].
Procedure:
- Clone the ~1 kb flanking regions (upstream and downstream) of the target gene (e.g., tolC, oprM) into a suicide vector containing the tpm-sacB cassette.
- Introduce the construct into the target MDR strain via conjugation.
- Select for first-crossover integrants on tellurite-containing plates.
- Plate the integrants on NaCl-free media containing sucrose to select for a second crossover and the excision of the vector, resulting in a clean, unmarked deletion mutant.
- Verify the deletion by PCR and whole-genome sequencing [13].
Phenotypic Assays for Efflux Activity and Inhibition
Ethidium Bromide (EtBr) Cartwheel Method [69] [11] This assay visually assesses efflux pump activity.
- Preparation: Create a gradient of EtBr concentrations (e.g., 0.25 µg/mL to 4.0 µg/mL) in agar plates, pouring them in a "cartwheel" pattern.
- Inoculation: Streep test bacteria along the radius of the plate.
- Incubation and Visualization: Incubate plates and then observe under UV light. Fluorescence indicates intracellular accumulation of EtBr. Strains with active efflux will only fluoresce at higher EtBr concentrations, while those with inhibited or absent efflux will fluoresce at lower concentrations.
Minimum Inhibitory Concentration (MIC) Reduction Assay [69] This is a standard method to evaluate the potency of an EPI.
- Broth Microdilution: Perform standard MIC testing for a substrate antibiotic (e.g., levofloxacin) in the presence and absence of a sub-inhibitory concentration of the EPI.
- Analysis: A significant reduction (e.g., 4-fold or greater) in the MIC of the antibiotic in the presence of the EPI indicates potentiation of activity and successful efflux inhibition. For example, fluphenazine decanoate has been shown to reverse efflux at 15.62 µg/mL in Salmonella typhi [69].
Flow Cytometry-Based Accumulation Assay [70] This powerful single-cell technique quantifies heterogeneity in efflux activity within a population.
- Staining: Treat a bacterial population (e.g., stationary phase E. coli) with a fluorescently-labeled antimicrobial substrate, such as tachyplesin-NBD [70].
- Analysis: Analyze the cells using flow cytometry. The distribution of fluorescence intensity across the population reveals sub-groups with high and low accumulation, directly correlating with efflux activity and phenotypic resistance [70].
- Inhibition: Repeat the assay in the presence of an EPI (e.g., sertraline). A shift in the population towards higher fluorescence indicates successful inhibition of efflux and increased intracellular drug accumulation [70].
Figure 2: Experimental Workflow for Efflux Pump Research. The diagram outlines a consolidated workflow integrating genetic, phenotypic, and single-cell approaches to validate efflux pump function and inhibition.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Efflux Pump and EPI Research
| Reagent / Tool | Category | Function in Research | Example Use Case |
|---|---|---|---|
| Tellurite (TeO₃²⁻) Resistance Cassette (tpm) | Genetic Tool | Positive selection marker for genetic engineering in MDR clinical isolates that are resistant to standard antibiotics [13]. | Generating clean tolC or oprM deletions in carbapenem-resistant P. aeruginosa [13]. |
| Ethidium Bromide (EtBr) | Phenotypic Probe | Fluorescent substrate for many MDR efflux pumps. Its accumulation is a direct indicator of efflux activity [69] [11]. | Cartwheel method to screen clinical isolates for baseline efflux pump activity [69]. |
| Carbonyl Cyanide m-Chlorophenylhydrazone (CCCP) | Pharmacological Probe (Energy Dissipator) | Collapses the proton motive force, de-energizing secondary active transporters. A positive control for efflux inhibition [66]. | Demonstrating that resistance to an antibiotic is efflux-mediated by showing MIC reduction in combination with CCCP. |
| Phenylalanyl-Arginyl-β-Naphthylamide (PAβN) | Pharmacological EPI | Early-generation, broad-spectrum EPI that competes with antibiotics for binding to RND pumps like AcrB [66]. | In vitro potentiation of levofloxacin and erythromycin in P. aeruginosa [66]. |
| Fluphenazine Decanoate | Pharmacological EPI | Phenothiazine derivative identified as an EPI; used in experimental models [69]. | Reversing ethidium bromide efflux in Salmonella Typhi at 15.62 µg/mL [69]. |
| Sertraline | Pharmacological EPI (Repurposed) | Clinically used antidepressant that also inhibits efflux pumps and reduces phenotypic resistance [70]. | Combination with tachyplesin to kill refractory stationary-phase E. coli by increasing peptide accumulation [70]. |
| Fluorescently-labeled AMPs (e.g., Tachyplesin-NBD) | Analytical Probe | Allows for quantification and visualization of intracellular antimicrobial accumulation via flow cytometry or microscopy [70]. | Identifying phenotypically resistant subpopulations with low drug accumulation in stationary phase cultures [70]. |
Resistance Mechanisms to EPIs and Future Directions
The failure of EPIs in the clinic is not solely due to poor efficacy; bacteria can also develop resistance to the inhibitors themselves. Understanding these mechanisms is crucial for designing robust next-generation EPIs.
- Mutational Bypass and Overexpression: Bacteria can develop resistance to an EPI-antibiotic combination through mutations that lead to the massive overexpression of the target efflux pump, effectively overwhelming the inhibitor [66]. Alternatively, mutations in the pump itself (e.g., in AcrB) can alter the inhibitor-binding site while preserving, or even expanding, the ability to export antibiotics [11].
- Redundancy in the Intrinsic Resistome: The presence of multiple, often redundant, efflux pumps in a single organism means that inhibiting one pump may be circumvented by the overexpression or increased activity of another [68] [11]. For instance, P. aeruginosa has at least 12 RND systems, creating a robust defensive network [11].
- Heterogeneous Expression and Phenotypic Resistance: Bacterial populations are not uniform. Subpopulations of cells can transiently exhibit high efflux activity, allowing them to survive antibiotic exposure without genetic mutation. This phenotypic resistance is a major contributor to treatment failure and the persistence of infections [70]. Flow cytometry studies have directly shown bacterial subpopulations with low intracellular drug accumulation due to heterogeneous efflux pump expression [70].
Future Directions and Strategic Approaches
- Targeting the Intrinsic Resistome Network: Instead of targeting single pumps, future strategies should aim to disrupt the regulatory networks that control the expression of multiple efflux systems or other components of the intrinsic resistome [1] [6].
- Structure-Guided and AI-Driven Design: Using high-resolution crystal structures of pump-inhibitor complexes (e.g., AcrB with an EPI) to design compounds that bind irreversibly or with higher affinity [65]. Machine learning can analyze vast chemical libraries to predict novel EPI scaffolds and optimize ADMET properties [68] [6].
- Exploiting Combination Therapies: As demonstrated by the synergy between sertraline and tachyplesin [70], repurposing existing drugs as EPIs offers a faster path to clinical application. Combining EPIs with antibiotics that are not typical pump substrates is another promising avenue.
- Validation in Clinically Relevant Models: It is imperative to prioritize the testing of novel EPIs not in laboratory-adapted strains, but in diverse MDR clinical isolates that represent the complex, multi-mechanistic resistance landscape encountered in the clinic [13] [11].
The critical divergence between genetic and pharmacological inhibition of efflux pumps is a central challenge in the battle against antimicrobial resistance. Genetic studies have irrefutably validated efflux pumps as high-value targets within the intrinsic resistome, yet translating this promise into effective therapeutics has proven exceptionally difficult. The limitations of current EPIs—their inability to fully reverse resistance in complex MDR backgrounds, the ease with which bacteria develop resistance to them, and issues with toxicity—stem from a fundamental underestimation of the robustness and redundancy of bacterial defense systems. Closing this gap requires a paradigm shift from a reductionist, single-target approach to a systems-level strategy that acknowledges the networked nature of the intrinsic resistome. The integration of advanced genetic tools, structural biology, single-cell analytics, and computational power provides an unprecedented opportunity to design the next generation of EPIs. By learning from the failures of the past and embracing these sophisticated tools, researchers can develop combination therapies that effectively neutralize this key pillar of bacterial resistance and reclaim the efficacy of our existing antibiotic arsenal.
The phenomenon of co-selection, wherein bacterial adaptation to one antimicrobial agent concurrently selects for resistance to multiple, structurally unrelated drugs, presents a critical challenge to public health and drug development. This process is deeply rooted in the intrinsic resistome of bacterial pathogens—the comprehensive set of chromosomal elements that contribute to innate antibiotic resistance, independent of horizontal gene transfer [1]. Understanding this intrinsic capacity is paramount, as it determines a pathogen's potential to evolve cross-resistance and dictates the evolutionary trajectories available under selective pressure. The intrinsic resistome encompasses not only classical resistance determinants like efflux pumps but also a wide array of housekeeping genes and global regulators that indirectly modulate susceptibility [1]. When bacteria are exposed to non-antibiotic agents, such as metals and biocides, the linkages within this resistome can lead to the unwanted selection of multidrug-resistant phenotypes, effectively undermining the efficacy of our antimicrobial arsenal [71] [72].
This technical guide synthesizes current research to elucidate the molecular mechanisms of co-selection, detail advanced methodologies for its investigation, and propose rational strategies for mitigation, all within the critical context of the intrinsic resistome. The focus is on providing researchers and drug development professionals with a foundational framework to navigate and counter this complex threat.
Molecular Mechanisms of Co-Selection
Co-selection operates through distinct but non-mutually exclusive molecular mechanisms that leverage the interconnectedness of bacterial stress response systems. These mechanisms allow selective pressures from one agent to directly or indirectly influence resistance to others.
Genetic Linkage and Co-Resistance
Co-resistance occurs when genes conferring resistance to different antimicrobials are physically linked on the same genetic element, such as a plasmid, transposon, or integron. Exposure to any one of these agents selects for the entire genetic unit, thereby promoting the persistence and spread of all linked resistance genes.
Large-scale genomic analyses have quantitatively demonstrated this phenomenon. A study of 2,522 bacterial genomes and 4,582 plasmids revealed that co-occurrence of biocide/metal resistance genes (BMRGs) and antibiotic resistance genes (ARGs) was significantly more common on plasmids of human and domestic animal origin (5-7%) compared to those from other environments (<0.7%) [73]. Notably, plasmids carrying both BMRG and ARG were more likely to be conjugative and carry toxin-antitoxin systems, enhancing their stability and dissemination potential [73]. Key examples of genetically linked resistance from this analysis are summarized in the table below.
Table 1: Common Genomic Co-occurrences Driving Co-Resistance
| Resistance Gene 1 | Resistance Gene 2 | Genetic Context | Implication |
|---|---|---|---|
| Mercury resistance (mer) | Multiple ARGs (e.g., β-lactamases) | Plasmids, Transposons | QAC and metal exposure can select for diverse antibiotic resistance [73]. |
| Quaternary Ammonium Compound resistance (qacEΔ1) | Aminoglycoside, β-lactam resistance genes | Class 1 Integrons | Common in clinical settings; disinfectant use promotes antibiotic resistance [73]. |
| Copper/Zinc resistance (pco, czc) | Bacitracin, β-lactam, macrolide resistance | Plasmids | Use of Cu/Zn in animal feed as growth promoters co-selects for antibiotic resistance [71] [73]. |
| Cadmium resistance (cad) | Vancomycin, tetracycline resistance | Chromosome/Plasmids | Metal pollution in environment selects for multi-antibiotic resistant pathogens [74]. |
Cross-Resistance via Shared Mechanisms
Cross-resistance arises when a single cellular mechanism—such as a mutated drug target or a broad-spectrum efflux pump—confers reduced susceptibility to multiple antimicrobials simultaneously. Unlike co-resistance, this does not necessarily require multiple genes.
- Efflux Pumps: Multidrug efflux pumps, particularly those of the Resistance-Nodulation-Division (RND) family, are major contributors to the intrinsic resistome and a primary source of cross-resistance. For example, the AcrAB-TolC system in E. coli can extrude a wide range of antibiotics, biocides, and detergents [1]. Mutations in regulatory genes (e.g., marA, soxS) that lead to pump overexpression result in a broad-spectrum resistant phenotype [6].
- Target Site Mutations: Mutations in a single gene can sometimes confer cross-resistance to multiple drug classes. A classic example is mutations in the gyrA gene (DNA gyrase) in E. coli, which can confer resistance to both fluoroquinolones and other drug classes like aminoglycosides and β-lactams by inducing broader stress responses [75].
- Membrane Permeability: Reduced membrane permeability, a hallmark of the intrinsic resistome in Gram-negative bacteria like Pseudomonas aeruginosa, acts as a non-specific barrier, providing innate, low-level resistance to multiple antibiotic classes, including β-lactams and macrolides [1].
Regulatory Networks and Co-Regulation
Co-regulation occurs when the expression of separate resistance mechanisms is controlled by a shared regulatory system. The presence of one antimicrobial can trigger a coordinated transcriptional response that upregulates defenses against other, unrelated compounds.
- Global Regulators: Systems like the multiple antibiotic resistance (mar) regulon in E. coli are activated by diverse stimuli, including antibiotics, biocides, and oxidative stress. Activation leads to the coordinated expression of efflux pumps and porin modifications, reducing intracellular concentrations of a wide array of drugs [6] [1].
- SOS Response: Antibiotic-induced DNA damage can activate the SOS response, which not only facilitates DNA repair but also promotes mutagenesis and the mobilization of integron-borne gene cassettes, accelerating the evolution and acquisition of resistance genes [6].
Diagram: The primary molecular mechanisms of co-selection.
Key Experimental Approaches and Methodologies
A multi-faceted approach is required to dissect the complex networks of co-selection, moving beyond traditional minimum inhibitory concentration (MIC) measurements to capture the full spectrum of bacterial adaptive responses.
Systematic Mapping of Cross-Resistance and Collateral Sensitivity
The concepts of cross-resistance (XR) and its converse, collateral sensitivity (CS)—where resistance to one drug increases susceptibility to another—are central to understanding co-selection networks. A groundbreaking chemical genetics approach used a systematic metric (Outlier Concordance-Discordance Metric, OCDM) on an E. coli single-gene deletion library screened against 40 antibiotics [76].
This method inferred 404 cases of cross-resistance and 267 of collateral sensitivity, a more than threefold expansion of known interactions. A key finding was that a single drug pair could exhibit XR or CS depending on the specific resistance mutation acquired, highlighting the importance of probing a wide genetic space [76]. This systematic mapping provides a roadmap for designing intelligent antibiotic cycling or combination therapies that leverage CS to suppress resistance.
Table 2: The Scientist's Toolkit: Key Reagents and Methodologies
| Tool / Reagent | Function/Description | Application in Co-Selection Research |
|---|---|---|
| Single-Gene Deletion Mutant Library (e.g., Keio collection for E. coli) | A comprehensive set of strains, each with a single non-essential gene knocked out. | Identifies genes which, when inactivated, alter susceptibility (the intrinsic resistome). Used in chemical genetics screens [76]. |
| Chemical Genetics (s-score) Profiling | Quantifies the fitness of each mutant in a drug condition compared to its fitness across all conditions. | Enables systematic inference of cross-resistance (concordant profiles) and collateral sensitivity (discordant profiles) across thousands of gene-drug interactions [76]. |
| Experimental Evolution | Serial passage of bacteria under sub-MIC antibiotic pressure for multiple generations. | Validates predicted XR/CS interactions and identifies real-world evolutionary paths to multi-drug resistance [76] [75]. |
| Metagenome-Assembled Genomes (MAGs) | Reconstruction of near-complete genomes from complex microbial community sequencing data. | Identifies bacterial hosts and genetic contexts (chromosomal vs. plasmid) of co-occurring BMRGs and ARGs in environmental samples like wastewater [77]. |
| Mutant Prevention Concentration (MPC) | The antibiotic concentration that prevents the growth of single-step resistant mutants. | Provides a more stringent, evolution-focused measure of resistance risk compared to MIC. Studies show the mutant selection window (MIC to MPC) can shift with collateral responses [75]. |
Genomic and Metagenomic Analysis of Co-Occurrence
Bioinformatic analysis of fully sequenced bacterial genomes and plasmids provides a powerful, large-scale method to identify the potential for co-selection based on the physical co-localization of resistance genes. This approach has shown that while BMRGs are found in 86% of bacterial genomes, their co-occurrence with ARGs on plasmids is relatively rare but significantly enriched in plasmids from human and animal sources [73]. Metagenomic studies of global wastewater treatment plants (WWTPs) have further revealed that activated sludge microbiomes harbor a core set of 20 ARGs present in all samples, accounting for over 80% of the total ARG abundance, with strong correlations between resistome composition and bacterial taxonomy [77]. These findings underscore specific environments and taxa as potential hotspots for co-selection risk.
Assessing Resistance Evolution via MIC and MPC
A dual-measurement approach that assesses both the Minimum Inhibitory Concentration (MIC) and the Mutant Prevention Concentration (MPC) provides a more complete picture of resistance risk. While MIC measures the concentration that inhibits growth, MPC defines the concentration required to block the growth of single-step resistant mutants, with the range between them known as the Mutant Selection Window (MSW) [75].
Research on Staphylococcus epidermidis has demonstrated that while patterns of cross-resistance and collateral sensitivity are often similar at the MIC and MPC levels, the correlation between these two metrics can weaken when cross-resistance does not evolve. Furthermore, the MSW often shifts and widens in resistant strains, indicating an expanded concentration range that can selectively enrich for resistant mutants [75]. This highlights the importance of considering MPC in dosing strategies to suppress resistance development.
Diagram: An integrated workflow for systematic analysis of co-selection.
Mitigation Strategies and Future Perspectives
Addressing the threat of co-selection requires a paradigm shift from reactive to proactive strategies that anticipate and circumvent bacterial evolutionary pathways.
- Leveraging Collateral Sensitivity in Therapy: The systematic identification of collateral sensitivity networks offers a promising strategy for designing intelligent treatment regimens. Using CS drug pairs in combination or in sequential cycles can theoretically suppress the emergence of resistance or even re-sensitize resistant populations [76]. For instance, applying newly identified CS pairs in combination has been shown to reduce resistance evolution in vitro compared to single-drug treatments [76].
- Inhibiting the Intrinsic Resistome: Targeting non-essential components of the intrinsic resistome, such as global regulators or efflux pumps, can re-sensitize bacteria to existing antibiotics. For example, inhibiting the AcrAB efflux pump in Gram-negative bacteria could potentially restore susceptibility to macrolides, a drug class to which they are normally intrinsically resistant [1]. This approach aims to "disarm" the bacterium's innate defensive capabilities.
- Environmental Monitoring and One Health Intervention: Given the evidence that metals and biocides in agricultural and wastewater settings drive co-selection, stricter regulation of these non-antibiotic selective agents is crucial [71] [74] [72]. Global resistome monitoring in key reservoirs like wastewater treatment plants can provide early warning signals of emerging threats and inform targeted interventions [77].
- Drug Development Informed by Co-Selection Risk: Early-stage screening of novel antibiotic candidates should include assessments of their potential for cross-resistance with existing drugs and their placement within collateral sensitivity networks. The goal is to prioritize compounds that, when resisted, trigger CS to other first-line therapies, thereby creating evolutionary "dead ends" for resistant pathogens [76].
In conclusion, mitigating the risk of multidrug adaptation and cross-resistance demands a sophisticated, multi-pronged approach grounded in a deep understanding of the intrinsic resistome. By integrating systematic genetic mapping, genomic surveillance, and evolutionary principles into drug discovery and clinical practice, the scientific community can develop more durable and sustainable solutions to the escalating crisis of antimicrobial resistance.
The antibiotic resistome—comprising all antibiotic resistance genes (ARGs) and their precursors in pathogenic and non-pathogenic bacteria—represents a profound challenge in managing infectious diseases [5]. This collective reservoir of resistance traits includes acquired resistance genes, intrinsic resistance, and silent or proto-resistance genes that can evolve into full resistance mechanisms [6] [5]. From a clinical perspective, the resistome is not static; it functions as a dynamic network where sub-inhibitory antibiotic concentrations can promote stress-induced mutagenesis and horizontal gene transfer, thereby accelerating the expansion of resistant bacterial populations [6]. This understanding fundamentally shifts the paradigm for antibiotic dosing from merely achieving clinical efficacy to deliberately suppressing the amplification of resistant subpopulations.
Pharmacokinetic/pharmacodynamic (PK/PD) modeling has emerged as a critical discipline for addressing this challenge by providing a quantitative framework to optimize antibiotic exposure against resistant pathogens. By integrating mathematical models of drug disposition (PK) with their pharmacological effects (PD), clinicians and researchers can design dosing strategies that maintain drug concentrations above the thresholds required to suppress resistant mutants throughout the dosing interval [78]. This approach represents a sophisticated evolution beyond conventional dosing, moving from containment to proactive prevention of antibiotic resistance, particularly for World Health Organization priority pathogens like Pseudomonas aeruginosa [78].
The Molecular Basis of Resistance Emergence
Mechanisms of Antibiotic Resistance
Bacteria employ diverse molecular strategies to circumvent antibiotic activity, with the primary mechanisms falling into several broad categories:
- Enzymatic inactivation: Production of enzymes such as β-lactamases (e.g., KPC, VIM, IMP, NDM, OXA-48) that hydrolyze antibiotics, or modifying enzymes like aminoglycoside acetyltransferases (AAC) and chloramphenicol acetyltransferases (CAT) that chemically alter drug molecules [20] [79].
- Target modification: Mutations in antibiotic target sites, such as alterations in DNA gyrase (gyrA, gyrB) and topoisomerase IV (parC, parE) for quinolones, or modifications in ribosomal RNA for macrolides and aminoglycosides [6] [79].
- Efflux pump overexpression: Upregulation of membrane transport proteins (e.g., RND family pumps) that actively export antibiotics from the bacterial cell, reducing intracellular accumulation [6] [20].
- Reduced permeability: Modifications to outer membrane porins (e.g., OprD in P. aeruginosa) that limit antibiotic penetration into bacterial cells [20] [79].
- Target protection: Production of proteins that physically shield antibiotic targets without altering the target itself, such as Tet(O) for tetracyclines [79].
Environmental Drivers and Horizontal Gene Transfer
The resistome extends far beyond clinical settings, with environmental reservoirs acting as incubators for resistance gene evolution. Mobile genetic elements (MGEs)—including plasmids, transposons, insertion sequences, and integrons—serve as vehicles for horizontal gene transfer (HGT), enabling the dissemination of ARGs across bacterial species and genera [6] [24]. This genetic mobility creates a complex network where resistance traits can transfer from environmental bacteria to human pathogens. Studies of wild rodent gut microbiomes have revealed extensive ARG diversity, with Enterobacteriaceae, particularly Escherichia coli, serving as prominent ARG carriers [24]. The strong correlation observed between MGEs and ARGs highlights the potential for co-selection and mobilization of resistance traits [24].
Diagram 1: The pathway from intrinsic resistome to clinical resistance, and the intervention point for PK/PD optimization.
PK/PD Principles for Resistance Suppression
Foundations of PK/PD Modeling
PK/PD modeling integrates two fundamental components: pharmacokinetics (what the body does to the drug), describing drug absorption, distribution, metabolism, and excretion; and pharmacodynamics (what the drug does to the body), characterizing the relationship between drug concentration and pharmacological effect [80]. For antibiotics, the primary PD indices include:
- ƒT
: Percentage of dosing interval that free drug concentration exceeds the minimum inhibitory concentration (MIC) - ƒAUC/MIC: Ratio of free drug area under the concentration-time curve to MIC
- ƒC
/MIC : Ratio of free peak concentration to MIC
Different antibiotic classes typically target different PK/PD indices. For β-lactams (e.g., ceftolozane/tazobactam), which exhibit time-dependent killing, ƒT
Aggressive PK/PD Targets for Resistance Suppression
Conventional dosing strategies typically aim to achieve drug concentrations that inhibit growth of susceptible populations, but often fail to prevent the emergence of resistance. Aggressive PK/PD targets are specifically designed to suppress resistant subpopulations by maintaining drug concentrations above a critical threshold throughout the dosing interval.
For β-lactam antibiotics, achieving trough concentrations that are ≥4 times the MIC has been associated with a nearly threefold reduction in resistance emergence (from 15.5% to 5.9%) according to clinical studies with ceftazidime/avibactam [78]. This target has been validated across multiple β-lactams, including meropenem, cefepime, and ceftazidime, demonstrating its broad applicability for resistance suppression [78].
Table 1: Aggressive PK/PD Targets for Resistance Suppression Across Antibiotic Classes
| Antibiotic Class | Traditional PK/PD Index | Resistance Suppression Target | Proposed Mechanism |
|---|---|---|---|
| β-Lactams | 40-70% ƒT |
ƒT<4×MIC> ≥100% | Prevents selective amplification of resistant mutants with elevated MICs |
| Fluoroquinolones | ƒAUC/MIC 100-125 | ƒAUC/MIC >200 | Suppresses resistant subpopulations through enhanced bactericidal activity |
| Aminoglycosides | ƒC |
ƒC |
Reduces adaptive resistance and prevents mutant selection |
| Glycopeptides | AUC/MIC >400 | AUC/MIC >600 | Limits heteroresistance emergence in Gram-positive pathogens |
Advanced PK/PD Modeling Approaches
Several sophisticated modeling methodologies support the development of optimized dosing regimens:
- Population PK (PopPK) Modeling: Analyzes drug disposition while accounting for interindividual variability, enabling identification of patient factors (e.g., renal function) that significantly impact drug exposure [78] [80].
- Physiologically-Based PK (PBPK) Modeling: Provides mechanistic, system-based predictions of drug distribution, particularly valuable for specialized tissue penetration (e.g., lung mucus) where clinical data are limited [81] [80].
- Spatial PK/PD Modeling: Accounts for drug distribution heterogeneity at infection sites, such as airway mucus, which can create microenvironments where subpopulations persist despite systemic adequate drug levels [81].
- Monte Carlo Simulations: Evaluates the probability of target attainment across virtual patient populations, allowing for regimen optimization against specific MIC distributions [78].
Implementing PK/PD-Optimized Regimens: A Case Study with Ceftolozane/Tazobactam
Experimental Protocol for PopPK/PD Analysis
A recent study demonstrates the comprehensive methodology for developing PK/PD-optimized regimens to suppress resistance in severe P. aeruginosa infections [78]:
Patient Population and Data Collection:
- Enrollment of 88 adult patients receiving continuous infusion ceftolozane/tazobactam with therapeutic drug monitoring (TDM)
- Collection of 171 steady-state plasma samples for ceftolozane concentration determination
- Documentation of demographic, clinical, and microbiological data, including:
- Renal function (eGFR using 2021 CKD-EPI equation)
- Disease severity (SOFA scores)
- Infection type and source
- Pathogen identification and MIC determination
Bioanalytical Methods:
- Drug concentration quantification using liquid chromatography-tandem mass spectrometry (LC-MS/MS)
- Calibration curves established over relevant concentration ranges (0.5–2,000 ng/mL)
- Quality control samples to ensure assay precision and accuracy
Population PK Modeling:
- Development of structural PK model using nonlinear mixed-effects modeling (NONMEM)
- Covariate analysis to identify patient factors influencing drug clearance
- Evaluation of renal function estimation equations for dose individualization
- Model validation using diagnostic plots and goodness-of-fit assessments
Monte Carlo Simulations:
- Generation of virtual patient populations (n=10,000) across renal function strata
- Simulation of continuous infusion regimens from 2/1 g to 6/3 g daily
- Calculation of probability of target attainment (PTA) for ƒT<4×MIC> against MIC distributions
- Determination of cumulative fraction of response (CFR) against local resistance epidemiology
Diagram 2: Workflow for developing PK/PD-optimized dosing regimens through population modeling and simulation.
Key Findings and Optimized Regimens
The analysis revealed that the 2021 non-race-based CKD-EPI equation with body surface area indexation provided the most reliable estimates of ceftolozane clearance, underscoring the importance of appropriate renal function assessment for dose individualization [78]. Monte Carlo simulations demonstrated that continuous infusion regimens of 4-6 g/2-3 g daily (ceftolozane/tazobactam) achieved optimal target attainment (≥90% PTA for ƒT<4×MIC>) across all kidney function strata for MICs up to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) breakpoint [78].
Table 2: Optimized Ceftolozane/Tazobactam Continuous Infusion Regimens for Resistance Suppression
| Renal Function (eGFR, mL/min/1.73m²) | Optimal Daily Dose (Ceftolozane/Tazobactam) | PTA for ƒT<4×MIC> at EUCAST Breakpoint | Cumulative Fraction of Response |
|---|---|---|---|
| Normal (>90) | 6/3 g | ≥95% | >90% against MDR P. aeruginosa |
| Mild Impairment (60-89) | 5/2.5 g | ≥92% | >85% against MDR P. aeruginosa |
| Moderate Impairment (30-59) | 4/2 g | ≥90% | >80% against MDR P. aeruginosa |
| Severe Impairment (15-29) | 3/1.5 g | ≥88% | >75% against MDR P. aeruginosa |
| ESRD (<15) | 2/1 g | ≥85% | >70% against MDR P. aeruginosa |
Notably, these optimized regimens maintained robust activity against key resistance phenotypes: multidrug-resistant (83.8%), pan-beta-lactam-nonsusceptible (78.2%), and difficult-to-treat resistant (71.7%) P. aeruginosa [78]. Even for isolates with elevated MICs (>4 mg/L), aggressive target attainment was achievable in 15-40% of cases, representing a significant improvement over conventional dosing approaches [78].
The Scientist's Toolkit: Essential Reagents and Methodologies
Table 3: Key Research Reagent Solutions for PK/PD Resistance Studies
| Reagent/Methodology | Function/Application | Technical Specifications |
|---|---|---|
| LC-MS/MS Systems | Quantitative drug concentration measurement in biological matrices | Sensitivity: 0.5-2000 ng/mL range; Precision: <15% CV; MRM transition monitoring |
| Population PK Modeling Software (NONMEM) | Nonlinear mixed-effects modeling for population PK analysis | Handles sparse sampling data; Covariate model implementation; Visual predictive check capabilities |
| Monte Carlo Simulation Software | Probability of target attainment analysis across virtual populations | Ability to simulate 10,000+ subjects; Incorporation of parameter variability and uncertainty |
| CKD-EPI 2021 Equation | Estimation of glomerular filtration rate for renal dose adjustment | Non-race-based algorithm; BSA indexation capability; Improved clearance prediction |
| Therapeutic Drug Monitoring Assays | Real-time drug concentration measurement for dose individualization | Rapid turnaround time (<24h); Validated precision and accuracy; Clinical decision support |
| Spatial PK Modeling Framework | Prediction of drug distribution in heterogeneous environments (e.g., airway mucus) | Partial differential equation implementation; Incorporation of diffusion coefficients and binding kinetics |
The strategic application of PK/PD modeling to suppress resistant subpopulations represents a paradigm shift in antimicrobial therapy, moving from reactive to proactive resistance management. By targeting aggressive exposure thresholds that specifically address the amplification of resistant mutants within the context of the intrinsic resistome, clinicians can potentially extend the therapeutic lifespan of valuable antimicrobial agents.
Future directions in this field include the development of real-time adaptive dosing systems that integrate therapeutic drug monitoring with Bayesian forecasting to individualize therapy against resistant pathogens. Additionally, multi-scale modeling approaches that incorporate bacterial population dynamics, resistance gene transfer mechanisms, and host-pathogen interactions will provide more comprehensive frameworks for regimen optimization [6] [81]. The emerging strategy of "resistance hacking"—exploiting bacterial resistance mechanisms against themselves, as demonstrated with modified florfenicol against Mycobacterium abscessus—represents an innovative approach that could be combined with exposure optimization for enhanced efficacy [35].
As antibiotic resistance continues to evolve, the integration of advanced PK/PD principles with molecular understanding of resistome dynamics will be essential for preserving the utility of existing agents and guiding the development of novel therapeutic strategies.
Evaluating Resistance-Breaking Strategies: Efficacy, Specificity, and Clinical Potential
Within the context of bacterial pathogen research, understanding the intrinsic resistome—the set of genes that contribute to innate antibiotic resistance—is paramount for developing novel therapeutic strategies. Functional genomics approaches are essential for identifying and characterizing these resistance determinants. Two predominant methods for probing gene function are genetic knockouts, which completely abolish gene function, and small-molecule inhibitors, which acutely inhibit protein activity. While these approaches are often used interchangeably to answer the same biological question—what happens when protein X is inactivated?—they can produce divergent phenotypic and evolutionary outcomes [82] [83]. This guide provides a comparative analysis of these methodologies, focusing on their mechanistic bases, experimental applications, and implications for the evolution of resistance in bacterial pathogens.
Fundamental Mechanisms and Key Differences
Basic Principles of Action
Genetic Knockouts: These involve the permanent disruption or deletion of a gene, leading to the complete and heritable absence of the encoded protein. In bacteria, this is commonly achieved via CRISPR-Cas systems or homologous recombination. The phenotype results from the loss of all protein functions, including potential scaffolding roles, and allows for compensatory evolutionary adaptations over time [83] [84].
Small-Molecule Inhibitors: These are pharmacologic agents that bind to and inhibit the activity of a target protein, typically in a reversible manner. The protein itself remains physically intact in the cell. Critically, inhibition can be substrate-selective, whereby a molecule inhibits the enzyme's activity on one substrate but not others, a phenomenon not possible with genetic knockout [85].
Comparative Analysis: Mechanism and Consequences
The table below summarizes the core differences between these two perturbation methods.
Table 1: Fundamental Differences Between Genetic Knockouts and Small-Molecule Inhibitors
| Feature | Genetic Knockout | Small-Molecule Inhibition |
|---|---|---|
| Molecular Effect | Complete, heritable removal of the gene/protein [83] | Acute, typically reversible inhibition of protein function [82] |
| Temporal Control | Chronic; protein loss is permanent [83] | Acute; inhibition can be titrated and timed [82] |
| Phenotypic Specificity | Abolishes all functions of the protein (catalytic, scaffolding) [82] | Can be substrate-selective; may inhibit only a subset of protein functions [85] |
| Cellular Adaptation | Allows for rewiring of pathways and compensatory adaptations [83] | Mimics acute stress; less time for systemic adaptation |
| Therapeutic Analogy | Models monogenic diseases or complete target blockade | Models pharmacological intervention [82] |
Experimental Design and Workflows
Standardized Protocols for Functional Genomics
To ensure reliable and interpretable results in resistome research, rigorous experimental designs must be employed.
Protocol 1: CRISPR-Cas9 Knockout Screen for Resistance Genes
- Library Design: Clone a single-guide RNA (sgRNA) library targeting epigenetic regulators or other genes of interest into a lentiviral transfer plasmid [86].
- Delivery: Infect activated primary bacterial cells or a suitable model with the sgRNA library and introduce Cas9 protein via electroporation [86].
- Selection Pressure: Apply the antibiotic of interest to select for cells where knockout of a specific gene confers a survival advantage (resistance) or disadvantage (sensitivity).
- Genomic DNA Extraction & Sequencing: Recover surviving cells, extract gDNA, and perform high-throughput sequencing of the integrated sgRNAs.
- Hit Identification: Statistically analyze sgRNA enrichment/depletion to identify genes essential for survival under antibiotic pressure [86] [87].
Protocol 2: Phenotypic Small-Molecule Screening
- Library Curation: Assay a library of biologically active compounds or a focused chemogenomics set. Note that even the best libraries only interrogate a fraction of the proteome [88].
- Dosing: Treat bacterial cultures with compounds at the lowest possible concentration that shows efficacy (preferably <10 μM) to minimize off-target effects [82].
- Phenotypic Assay: Measure a functional readout, such as minimum inhibitory concentration (MIC), time-kill kinetics, or toxin production.
- Confirmation: Use structurally related but inactive analogs as negative controls to confirm on-target effects. Employ rescue experiments by overexpressing the target protein to reverse the compound's effect [82].
Visualizing Experimental Workflows
The following diagram illustrates the key decision points and processes in a comparative study of these two methods.
Divergent Phenotypes and Evolutionary Implications
Case Studies of Phenotypic Discrepancy
The assumption that genetic knockout and pharmacological inhibition produce identical phenotypes is frequently violated, with critical implications for predicting resistance evolution.
PARP1: A striking example comes from DNA damage repair. The gene XRCC1, which interacts directly with PARP1, was identified as a top sensitizer for small-molecule PARP inhibition. However, in a PARP1 genetic knockout background, XRCC1 acted as a top buffering gene. This suggests that the presence of an inhibited protein (with small molecules) creates a different cellular state than its complete absence (with knockout), potentially leading to distinct resistance pathways [83].
MCL1: Studies comparing acute CRISPR knockout of the anti-apoptotic gene MCL1 with chronic knockout in single-cell clones revealed different synthetic lethal interactions. HSP90AB1 was synthetic lethal with acute MCL1 knockout but had no effect in chronic knockout cells. This indicates that cells can rewire their signaling networks over time to adapt to a permanent genetic loss, an evolutionary outcome masked by acute chemical inhibition [83].
Substrate-Selective Inhibition: Many enzymes, including kinases and proteases, have multiple substrates. Small-molecule inhibitors can be substrate-selective, blocking the enzyme's activity on one substrate but not others. Genetic knockout, by contrast, affects all downstream substrates simultaneously. In bacteria, this could mean that a drug inhibiting an enzyme involved in cell wall biosynthesis might only block one specific reaction, whereas a knockout would halt the entire pathway, potentially triggering a broader compensatory stress response [85].
Quantitative Comparison of Methodological Features
The following table provides a structured overview of key performance and application characteristics of both methods.
Table 2: Quantitative and Functional Comparison of Perturbation Methods
| Characteristic | Genetic Knockout | Small-Molecule Inhibition |
|---|---|---|
| Reversibility | Irreversible (permanent) [83] | Typically reversible [82] |
| Time to Effect | Slow (days, for protein turnover) [82] | Fast (minutes to hours) [82] |
| Target Coverage | High (can target any gene) [88] | Limited (~1,000-2,000 drugged targets) [88] |
| Specificity Control | Multiple independent sgRNAs; rescue with transgene [82] | Structure-activity relationships (SAR); inactive analogs [82] |
| Phenomenon Detected | Loss-of-function fitness effects; essential genes [84] | Chemical vulnerability; polypharmacology |
| Model for | Genetic diseases; complete target blockade | Pharmacological intervention [82] |
The Scientist's Toolkit: Essential Research Reagents
Success in functional genomics screens for antibiotic resistance relies on a suite of key reagents and tools.
Table 3: Essential Research Reagents for Knockout and Inhibition Studies
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| CRISPR sgRNA Library | Targets genes for knockout; enables genome-wide or focused screens [86] | Focused sublibraries (e.g., on epigenetic regulators) allow for more physiologically relevant in vivo screens [86]. |
| Cas9 Nuclease | Creates double-strand breaks at DNA sites specified by the sgRNA. | Delivery method (plasmid, mRNA, protein) can impact efficiency and timing. |
| Small-Molecule Chemogenomics Library | Collection of annotated compounds for phenotypic screening [88]. | Covers only a fraction of the genome; annotation quality is critical for target identification. |
| Negative Control siRNA/Compound | A mismatched/scrambled siRNA or an inactive structural analog of the inhibitor [82]. | Crucial for distinguishing on-target from off-target effects. |
| Drug-Resistant Transgene | A version of the target gene engineered to be resistant to the small-molecule inhibitor [82]. | Used in rescue experiments to confirm the on-target phenotype of a compound. |
Genetic knockouts and small-molecule inhibitors are powerful, complementary tools for deconvoluting the intrinsic resistome of bacterial pathogens. However, they are not functionally equivalent. Knockouts reveal the long-term fitness consequences and potential for cellular adaptation following complete gene loss, modeling scenarios where resistance arises from target inactivation. In contrast, small-molecule inhibitors probe acute chemical vulnerabilities and can unveil sophisticated, substrate-specific biology not accessible to genetic methods, more closely mimicking antibiotic treatment. The observed phenotypic discrepancies between these approaches are not merely technical artifacts but reflect fundamental biological differences between the permanent absence of a protein and its acute inhibition. A comprehensive resistance research strategy should therefore leverage both methodologies to build a more complete and clinically predictive model of how bacteria evolve to overcome antimicrobial pressure.
The intrinsic resistome encompasses all chromosomally encoded elements that contribute to a bacterial species' innate antibiotic resistance, independent of horizontal gene acquisition [1]. Among these elements, multidrug efflux pumps, particularly the Resistance-Nodulation-Division (RND) family in Gram-negative bacteria, serve as a first-line defense by actively extruding diverse antibiotics from the cell [89] [11]. This case study examines efflux pump inhibition (EPI) as a strategic approach to "resistance-proof" antimicrobial therapy. We explore the mechanistic basis of efflux-mediated resistance, evaluate promising EPI candidates, detail experimental methodologies for discovery and validation, and discuss the integration of EPIs into combination therapies to overcome intrinsic bacterial defenses and restore antibiotic efficacy.
The intrinsic resistome is defined as the set of chromosomal elements that contribute to antibiotic resistance, whose presence is independent of previous antibiotic exposure and not acquired via horizontal gene transfer [1]. This concept reframes bacterial susceptibility as an emergent property resulting from the concerted action of numerous cellular components, including classical resistance genes and basic metabolic functions [1]. A cornerstone of the intrinsic resistome in Gram-negative bacteria is their sophisticated efflux machinery.
Efflux pumps are active transport systems that recognize and expel toxic compounds, including multiple classes of antibiotics, reducing intracellular drug accumulation to sub-therapeutic levels [89] [66]. In clinically relevant Enterobacteriaceae and other ESKAPEE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, Enterobacter spp., and Escherichia coli), efflux pumps work synergistically with other resistance mechanisms, such as enzymatic inactivation and target modification, to create multidrug-resistant (MDR), extensively drug-resistant (XDR), and even pandrug-resistant (PDR) phenotypes [90]. The broad substrate specificity of many efflux pumps allows bacteria to develop resistance to new antibiotics rapidly, even before they are extensively used in the clinic [11]. Inhibiting these pumps therefore represents a strategic opportunity to counteract intrinsic resistance and extend the lifespan of existing antibiotics.
Efflux Pump Mechanisms and Structural Basis
Major Efflux Pump Families
Bacterial efflux systems are categorized into families based on structure and energy source. The most clinically significant in Gram-negative bacteria form tripartite complexes that span the inner and outer membranes [89].
Table 1: Major Efflux Pump Families in Bacteria
| Family | Energy Source | Representative Pump | Key Substrates | Clinical Significance |
|---|---|---|---|---|
| Resistance-Nodulation-Division (RND) | Proton Motive Force | AcrAB-TolC (E. coli), MexAB-OprM (P. aeruginosa) | Beta-lactams, Fluoroquinolones, Macrolides, Tetracyclines, Chloramphenicol [66] [11] | Primary contributor to intrinsic and acquired MDR in Gram-negative bacteria [89] [11] |
| Major Facilitator Superfamily (MFS) | Proton Motive Force | NorA (S. aureus), EmrAB-TolC (E. coli) | Fluoroquinolones, Tetracycline, Ethidium Bromide [66] | Predominant in Gram-positive bacteria; some tripartite systems in Gram-negatives [66] |
| ATP-Binding Cassette (ABC) | ATP Hydrolysis | MacAB-TolC (E. coli) | Macrolides, Peptides [89] | Less associated with antibiotic resistance in Gram-negatives; often specific substrates [89] |
| Multidrug and Toxic Compound Extrusion (MATE) | Proton/Sodium Ion Gradient | NorM (V. cholerae) | Fluoroquinolones, Aminoglycosides [66] | Contributes to resistance in some species; narrower substrate profile [66] |
The RND Tripartite Complex: A Structural Deep Dive
The RND pump AcrAB-TolC in E. coli is a paradigm for understanding efflux mechanisms. This tripartite system consists of:
- AcrB: An inner membrane transporter trimer that binds substrates and undergoes conformational changes to power export [89].
- AcrA: A periplasmic adaptor protein that structurally bridges AcrB and TolC [89].
- TolC: An outer membrane channel that forms the final exit duct for substrates [89].
AcrB operates via a functional rotating mechanism where each protomer cycles through three conformational states:
- Loose (L) state: Binds substrate from the periplasm or inner membrane.
- Tight (T) state: Traps the substrate in a deep binding pocket.
- Open (O) state: Extrudes the substrate into the TolC tunnel [89].
This asymmetric cycle ensures the unidirectional movement of substrates. Substrates access the binding pockets through distinct entry channels, which contribute to the pump's remarkable substrate promiscuity [89].
Diagram: The Tripartite RND Efflux Pump and Functional Rotation Mechanism. The AcrAB-TolC complex spans the Gram-negative cell envelope. The AcrB trimer undergoes a conformational cycle (L→T→O) to bind and expel antibiotics [89].
Current Landscape of Efflux Pump Inhibitors
Efflux pump inhibitors (EPIs) are adjuvants designed to block pump function, thereby increasing intracellular antibiotic concentration and restoring susceptibility [66]. They can act via several mechanisms:
- Competitive inhibition: Binding to the substrate pocket and blocking antibiotic binding.
- Energy dissipation: Collapsing the proton motive force that powers the pump.
- Inhibition of assembly: Preventing the formation of the functional tripartite complex [66].
Table 2: Promising Efflux Pump Inhibitors in Development
| EPI Candidate | Origin/Target | Proposed Mechanism | Development Status |
|---|---|---|---|
| PAβN (MC-207,110) | Synthetic Peptidomimetic; RND Pumps (e.g., AcrB) | Competitive inhibition; interferes with substrate binding [91] [66] | Early research; prototype EPI, but cytotoxic [66] |
| D13-9001 | Synthetic; MexB (P. aeruginosa) | Binds deep binding pocket (DBP), inhibiting efflux [91] | In vitro validation; low cytotoxicity [91] |
| Diphenylmethane (DPM) Scaffold | Natural (Seaweed) & Synthetic; AcrB | Binds distal/proximal pockets; inhibits efflux [91] | Lead optimization; DPE and BPA show efficacy in vitro [91] |
| Berberine | Natural Product; MdfA (E. coli) | Inhibits efflux, increases ciprofloxacin accumulation [91] | Experimental validation |
| CCCP | Synthetic; Protonophore | Energy dissipation; uncouples proton motive force [66] | Research tool only; toxic for therapeutic use [66] |
Recent studies have identified specific diphenylmethane-scaffold compounds, such as 2,2-diphenylethanol (DPE) and 4-(benzylphenyl)acetonitrile (BPA), which exhibit potent efflux inhibition. Molecular docking reveals these compounds bind the AcrB distal binding pocket with high affinity (free energy -8.2 to -8.5 kcal/mol), comparable to the known inhibitor PAβN (-8.8 kcal/mol) [91]. They enhance intracellular dye accumulation, inhibit ethidium bromide and erythromycin efflux, and demonstrate limited human-cell toxicity, making them promising candidates for further development [91].
Experimental Toolkit for EPI Discovery and Validation
A multi-faceted experimental approach is essential for identifying and validating novel EPIs. The following workflow integrates computational and laboratory techniques.
Key Research Reagents and Solutions
Table 3: Essential Research Reagents for EPI Studies
| Reagent / Assay | Function in EPI Research | Example Application |
|---|---|---|
| Fluorometric Accumulation Assays | Measures real-time intracellular concentration of fluorescent substrates (e.g., ethidium bromide) to directly quantify efflux activity [89] [91] | Confirmatory test for EPI activity; DPE and BPA enhanced intracellular dye accumulation [91] |
| Molecular Docking Software | In silico screening of compound libraries against efflux pump structures to predict binding affinity and pose [91] [92] | Screening of diphenylmethane-scaffold compounds against AcrB (PDB: 4DX5) [91] |
| MIC Modulation Assay | Determines if a candidate EPI lowers the Minimum Inhibitory Concentration (MIC) of an antibiotic for a resistant strain [91] | Primary screen for EPI activity; DPE reduced erythromycin IC50 in AcrB-overexpressing E. coli [91] |
| Real-time PCR | Quantifies expression levels of efflux pump genes in response to treatment or in resistant isolates [11] | Analyzing mexB or acrB overexpression in clinical isolates [11] |
| Ethidium Bromide Efflux Assay | Directly visualizes or quantifies the rate of substrate expulsion from pre-loaded cells upon energy addition [91] | DPE and BPA inhibited ethidium bromide efflux [91] |
| Traditional Chinese Medicine (TCM) Compound Libraries | Source of natural product-derived EPIs with novel chemical structures [92] | Screening for EPIs against polymyxin-resistant bacteria [92] |
Detailed Experimental Protocols
Protocol 1: Molecular Docking for EPI Screening
Objective: To identify potential EPIs by computationally screening compound libraries against the AcrB transporter structure.
- Protein Preparation: Obtain the crystal structure of the AcrB transporter (e.g., PDB ID 4DX5). Prepare the protein by removing water molecules and co-crystallized ligands, adding hydrogen atoms, and defining protonation states.
- Ligand Preparation: Generate 3D structures of compounds to be screened (e.g., a diphenylmethane-scaffold library). Assign correct bond orders and minimize their energy.
- Define Binding Site: Select the known drug-binding pockets within the AcrB monomer, typically the distal binding pocket (DBP) and proximal binding pocket (PBP) in the tight (T) state [91].
- Perform Docking: Use docking software (e.g., AutoDock Vina) to predict the binding pose and calculate the binding free energy (kcal/mol) for each compound.
- Analysis: Select hits based on high binding affinity (e.g., ≤ -8.0 kcal/mol) and analyze interaction residues (e.g., Phe610, Val612, Phe615, Phe617) for critical hydrogen bonds and hydrophobic interactions [91].
Protocol 2: In Vitro MIC Modulation Assay
Objective: To experimentally validate if a candidate compound reverses antibiotic resistance in a bacterial strain overexpressing an efflux pump.
- Strain Selection: Use a well-characterized efflux pump-overexpressing strain (e.g., E. coli Kam3-AcrB) and its susceptible parent for comparison.
- Broth Microdilution: In a 96-well plate, prepare two-fold serial dilutions of the antibiotic (e.g., erythromycin, ciprofloxacin) in Mueller-Hinton broth.
- Add Candidate EPI: To each well containing antibiotic, add a sub-inhibitory concentration of the candidate EPI (e.g., 8 mg/L for DPE) [91].
- Inoculate and Incubate: Inoculate wells with a standardized bacterial suspension (~5 × 10^5 CFU/mL) and incubate at 37°C for 16-20 hours.
- Determine MIC: The MIC is the lowest antibiotic concentration that prevents visible growth. A ≥4-fold reduction in the MIC of the antibiotic in the presence of the EPI compared to the antibiotic alone indicates significant modulation and efflux inhibition [91].
Protocol 3: Ethidium Bromide Accumulation and Efflux Assay
Objective: To directly measure the impact of an EPI on efflux pump activity using a fluorescent substrate.
- Cell Preparation and Loading: Grow the test strain to mid-log phase. Harvest cells, wash, and resuspend in buffer containing an energy source (e.g., glucose). Load cells with ethidium bromide (EtBr) in the presence of an energy poison (e.g., CCCP) to allow passive uptake while efflux is disabled.
- Baseline Measurement: Place the cell suspension in a fluorometer (excitation ~530 nm, emission ~600 nm) and record the fluorescence baseline.
- Initiate Efflux: Add glucose to the cuvette to energize the cells and activate efflux pumps. Observe the fluorescence decrease as EtBr is actively expelled.
- Test EPI Inhibition: Repeat the experiment, but add the candidate EPI to the cell suspension before adding glucose.
- Analysis: Compare the initial rates of fluorescence decrease and the final fluorescence levels between the EPI-treated and untreated samples. An effective EPI will result in a slower rate of fluorescence loss and a higher final fluorescence, indicating inhibition of EtBr efflux [91].
Diagram: A Workflow for Efflux Pump Inhibitor Discovery. The process begins with in silico screening, proceeds to in vitro validation of resistance reversal, confirms the mechanism of action, and culminates in lead optimization [91] [92].
Challenges and Future Perspectives
Despite the compelling rationale, no EPI has yet reached clinical use, hindered by several multifactorial barriers:
- Structural Complexity and Promiscuity: The large, flexible binding pockets of RND pumps make designing high-affinity, broad-spectrum inhibitors difficult [89].
- Pharmacokinetic Issues: Achieving optimal tissue distribution and concentration at the site of infection simultaneously with the companion antibiotic is challenging [89].
- Toxicity Concerns: A critical hurdle is the inhibition of human efflux proteins (e.g., P-glycoprotein), leading to potential off-target toxicity and altered drug metabolism [66] [93].
- Lack of Standardized Diagnostics: Clinical microbiology laboratories currently lack standardized methods to detect and report efflux-mediated resistance, complicating patient stratification for EPI therapy [89] [11].
Future success will depend on rational drug design informed by high-resolution structural data (e.g., from cryo-EM), the exploration of non-competitive allosteric inhibition strategies, and the development of diagnostic tools to identify patients with efflux-driven infections [89] [11]. Furthermore, the discovery of potential dual inhibitors that target efflux pumps in both bacteria and cancer cells represents a fascinating, though complex, frontier [93].
Efflux pumps are a cornerstone of the intrinsic resistome, providing Gram-negative pathogens with a robust, multi-drug defensive capability. Inhibiting these pumps offers a superior and strategic approach to "resistance-proof" our antimicrobial arsenal. By neutralizing this primary defense mechanism, EPIs can resensitize bacteria to existing antibiotics, impede the development of high-level resistance, and protect new agents from premature obsolescence. While significant challenges in compound development and diagnostics remain, the continued integration of structural biology, computational screening, and innovative chemistry holds the promise of bringing this powerful therapeutic strategy to the clinic, turning the tide against multidrug-resistant infections.
The intrinsic resistome encompasses the full complement of chromosomal resistance genes and inherent physiological traits that enable bacterial survival upon antibiotic exposure, forming the foundational layer of antimicrobial resistance (AMR). Understanding the pathogen-specific architecture of these resistomes is critical for developing novel therapeutic strategies and combating the global AMR crisis. This review provides a detailed technical comparison of the resistomes of three clinically significant pathogens with distinct ecological niches and resistance profiles: Escherichia coli, a versatile Gram-negative bacterium and major source of nosocomial infections; Pseudomonas aeruginosa, an opportunistic pathogen renowned for its extreme multidrug resistance; and Mycobacteroides abscessus, a rapidly-growing non-tuberculous mycobacterium with exceptional resistance to most antibiotics. By examining their molecular resistance mechanisms, genomic features, and experimental approaches for resistome characterization, this analysis aims to equip researchers and drug development professionals with the knowledge needed to advance targeted interventions against these formidable pathogens.
Comparative Resistome Profiles
The following tables summarize key resistance characteristics and mechanisms across the three target pathogens, highlighting their distinct resistance landscapes and clinical implications.
Table 1: Fundamental Resistance Characteristics of E. coli, P. aeruginosa, and M. abscessus
| Characteristic | E. coli | P. aeruginosa | M. abscessus |
|---|---|---|---|
| Gram Stain | Gram-negative | Gram-negative | Gram-positive (acid-fast) |
| WHO Priority Category | Critical [94] | Critical [95] | Not specified (NTM) |
| Intrinsic Resistance Breadth | Moderate | Extensive [30] | Extreme [96] |
| Key Intrinsic Resistance Mechanisms | Efflux pumps, porin modifications [94] | Efflux pumps, AmpC β-lactamases, low membrane permeability [30] | Cell envelope impermeability, drug-modifying enzymes, ribosomal methylation [97] [96] |
| Dominant Mobile Genetic Elements | Plasmids, transposons, integrons [98] | Integrons, plasmids, transposons [30] | Prophages, genomic islands [97] |
| Noteworthy Resistance Genes | blaCTX-M, blaTEM, tet(X4) [98] | blaNDM, mex efflux pump genes [95] | erm(41), rrs, rrl [96] |
Table 2: Quantitative Resistome Comparison Based on Genomic Studies
| Pathogen | Total ARGs Identified | Most Abundant ARG Classes | Dominant Bacterial Hosts/Subspecies |
|---|---|---|---|
| E. coli | High prevalence in gut microbiomes [24] | Sulfonamides (34.3%), Fluoroquinolones (32.9%), β-lactams [98] | Phylogroup B2 (ExPEC), ST131, ST1193, ST10 clones [98] |
| P. aeruginosa | 8119 ARG ORFs (in rodent gut microbiome study) [24] | Multidrug (39.2%), peptide (7.1%), tetracycline (7.1%) [24] | High-risk clones (e.g., ST1076) [95] |
| M. abscessus | Not quantified (intrinsic resistance predominates) | Macrolides, Aminoglycosides, Fluoroquinolones [96] | Subsp. abscessus, Subsp. massiliense, Subsp. bolletii [96] |
Table 3: Experimentally Determined Antibiotic Resistance Patterns
| Antibiotic Class | E. coli | P. aeruginosa | M. abscessus |
|---|---|---|---|
| β-Lactams | High ESBL and carbapenemase prevalence [98] | Intrinsic resistance to many; carbapenem resistance via porin loss, carbapenemases [30] [95] | Resistance to most β-lactams; susceptibility to cefoxitin and imipenem (inactivated by BlaMab) [97] |
| Aminoglycosides | Varying resistance rates [98] | Resistance via modifying enzymes, efflux, rRNA methylases [30] | Variable resistance; novel amikacin resistance genes identified [96] |
| Macrolides | Not primary concern | Intrinsic resistance [30] | Inducible resistance via Erm(41) in subsp. abscessus/bolletii; susceptibility in subsp. massiliense (truncated Erm(41)) [96] |
| Fluoroquinolones | High resistance (e.g., 32.9%) [98] | Resistance via target mutations, efflux pumps [30] | Resistance via gyrase mutations; novel moxifloxacin resistance genes suggested [96] |
| Polymyxins | Emerging mcr genes [6] | Resistance via LPS modifications, efflux, mcr genes [30] | Intrinsic resistance due to cell envelope [96] |
Molecular Mechanisms of Resistance
E. coli: Adaptability and Gene Transfer
E. coli's remarkable resistance plasticity stems from its ability to acquire and express a diverse array of resistance genes via horizontal gene transfer. Its resistome is characterized by a high prevalence of extended-spectrum β-lactamase (ESBL) genes (particularly blaCTX-M and blaTEM variants) and emerging resistance to last-resort antibiotics, including the discovery of the tet(X4) gene conferring tigecycline resistance in isolates from irritable bowel syndrome patients [98]. A significant molecular aspect involves the potential regulatory role of stress response systems, such as the CpxAR two-component system, which may coordinate resistance, efflux pump activity, and programmed cell death in response to envelope stress [94]. The dominance of high-risk clones like ST131, ST1193, and ST10, which often carry a combination of virulence factors and resistance determinants, underscores the successful integration of resistance and fitness in specific lineages [98].
P. aeruginosa: A Fortress of Intrinsic Defense
P. aeruginosa possesses one of the most formidable intrinsic resistomes among Gram-negative bacteria, limiting therapeutic options even for wild-type isolates [30]. Its resistance is multi-layered, comprising:
- Impermeable Outer Membrane and Efflux Pumps: The synergy between low outer membrane permeability and powerful Resistance-Nodulation-Division (RND) efflux pumps (e.g., MexAB-OprM, MexXY-OprM) creates a robust barrier against diverse antimicrobial classes, including fluoroquinolones, β-lactams, macrolides, and aminoglycosides [30].
- Chromosomal β-Lactamases: The inducible AmpC cephalosporinase provides innate resistance to penicillins and many cephalosporins. Hyperproduction of AmpC is a common acquired resistance mechanism [30].
- Acquired Carbapenem Resistance: Resistance to carbapenems, critical anti-pseudomonal drugs, arises through porin OprD loss, efflux pump overexpression, and acquisition of carbapenemase genes (e.g., blaVIM, blaIMP, blaNDM) [30] [95]. The emergence of ceftazidime/avibactam (CZA) resistance in carbapenem-resistant P. aeruginosa (CRPA) is often linked to metallo-β-lactamase production (particularly blaNDM), enhanced biofilm formation, and efflux pump overexpression [95].
M. abscessus: The Impervious Pathogen
M. abscessus exhibits exceptional intrinsic resistance to most antibiotics, making treatment exceptionally challenging [96]. Key mechanisms include:
- Barrier Function of the Cell Envelope: The complex, lipid-rich mycobacterial cell wall acts as a formidable physical and functional barrier, drastically reducing permeability to many antimicrobials [96].
- Drug-Modifying Enzymes and Ribosomal Protection: The intrinsic resistome encodes enzymes like the ribosomal methyltransferase Erm(41) and the β-lactamase BlaMab. The functional status of Erm(41) is a critical differentiator among subspecies: intact in M. abscessus subsp. abscessus and bolletii (conferring inducible macrolide resistance) and truncated in subsp. massiliense (resulting in macrolide susceptibility) [96]. BlaMab contributes to resistance against imipenem and cefoxitin [97].
- Chromosomal Mutations: Acquired resistance frequently occurs through mutations in target genes, such as rrs (conferring resistance to aminoglycosides like amikacin) and gyrA/gyrB (conferring resistance to fluoroquinolones) [96]. Comparative genomics continues to reveal potential novel resistance genes associated with amikacin and moxifloxacin resistance [96].
Experimental Methodologies for Resistome Characterization
A comprehensive understanding of resistomes relies on integrating phenotypic assays with advanced genomic techniques. The following workflow outlines a standard pipeline for resistome analysis.
Phenotypic Antimicrobial Susceptibility Testing (AST)
Broth Microdilution is the reference standard for determining Minimum Inhibitory Concentrations (MICs). The protocol involves:
- Preparing a logarithmic-phase bacterial suspension adjusted to a standard turbidity (e.g., 0.5 McFarland).
- Diluting the suspension in cation-adjusted Mueller-Hinton broth (or specific media like 7H9 for M. abscessus) to achieve a final inoculum of ~5 × 10^5 CFU/mL.
- Dispensing the inoculum into microtiter plates containing serial two-fold dilutions of antibiotics.
- Incubating under appropriate conditions (e.g., 35±2°C for 16-20 hours for E. coli and P. aeruginosa; 3-5 days or longer for M. abscessus).
- Reading the MIC as the lowest antibiotic concentration that completely inhibits visible growth. Results are interpreted per CLSI or EUCAST guidelines [95] [96] [98].
Disk Diffusion is a complementary method where antibiotic-impregnated disks are placed on a seeded agar plate. After incubation, the diameter of the zone of inhibition is measured and interpreted per guidelines [95].
Genomic Analysis of Resistance Determinants
Whole-Genome Sequencing (WGS) and subsequent bioinformatic analysis are indispensable for resistome characterization.
DNA Extraction and Sequencing: High-quality genomic DNA is extracted using commercial kits (e.g., Wizard Genomic DNA Purification Kit) [96] [98]. Sequencing is performed on platforms like Illumina Novaseq or DNBseq-T7 for short-read data, which is sufficient for most resistome analyses.
Genome Assembly and Annotation: Quality-controlled reads are assembled into contigs using assemblers like SPAdes [96] [98]. The assembled genomes are annotated to identify coding sequences.
Resistance Gene Identification: Assembled genomes or raw reads are screened against curated databases using tools like Abricate or Diamond. The Comprehensive Antibiotic Resistance Database (CARD) is the primary resource for annotating ARGs [24] [97]. Virulence factors can be identified using the Virulence Factor Database (VFDB) [97].
Molecular Typing and Phylogenetics: Multilocus Sequence Typing (MLST) is performed by sequencing and comparing seven housekeeping genes to assign sequence types (STs) and identify clonal lineages [95] [98]. For M. abscessus, subspecies identification is often done via rpoB gene sequence analysis [96].
Prophage Detection: Prophage sequences within bacterial genomes can be predicted using the PHASTER online tool, which assesses the intactness of prophage regions and annotates their gene content, including potential ARGs and virulence factors [97].
Table 4: Key Reagents and Resources for Resistome Research
| Item/Category | Specific Examples | Function/Application |
|---|---|---|
| Culture Media | Columbia blood agar, Mueller-Hinton agar/broth, 7H9/7H10 media for mycobacteria | Strain revival, cultivation, and antimicrobial susceptibility testing. |
| Identification Kits | VITEK 2 Compact system, MALDI-TOF MS | Accurate species-level identification of bacterial isolates. |
| DNA Extraction Kits | Wizard Genomic DNA Purification Kit | High-quality genomic DNA extraction for downstream sequencing. |
| Sequencing Platforms | Illumina NextSeq/NovaSeq, DNBseq-T7 | Whole-genome sequencing to generate genomic data for analysis. |
| Bioinformatics Tools | SPAdes (assembler), Abricate (gene detection), PHASTER (prophage prediction), MLST (typing) | Genome assembly, resistance gene screening, mobile genetic element analysis, and molecular typing. |
| Reference Databases | CARD, VFDB, PubMLST | Curated databases for annotating antibiotic resistance genes, virulence factors, and assigning sequence types. |
| Quality Control Strains | P. aeruginosa ATCC 27853, E. coli ATCC 25922 | Quality assurance for phenotypic antimicrobial susceptibility testing. |
The resistomes of E. coli, P. aeruginosa, and M. abscessus exemplify distinct evolutionary strategies for surviving antibiotic pressure. E. coli relies heavily on genomic plasticity and horizontal gene transfer to acquire a diverse arsenal of resistance determinants. In contrast, P. aeruginosa's defense is rooted in a powerful combination of intrinsic mechanisms that create a low-permeability barrier and actively expel drugs. M. abscessus represents an extreme case, where an impervious cell envelope and constitutive resistance genes render it naturally tolerant to most drug classes. These fundamental differences necessitate pathogen-specific diagnostic approaches and therapeutic interventions. Future research must leverage integrated 'One Health' surveillance, combining advanced genomics with functional assays to unravel the complex regulation of these resistomes and identify novel, species-specific vulnerabilities to overcome multidrug resistance.
The intrinsic resistome of bacterial pathogens—a collection of chromosomal genes that confer innate antibiotic resistance—poses a significant challenge in antimicrobial therapy [53] [52]. This resistome includes mechanisms such as enzymatic drug inactivation, efflux pumps, and target modification, which are regulated by master controllers like WhiB7 in Mycobacterium abscessus [52]. Targeted prodrug approaches exploit these very resistance pathways to achieve pathogen-specific activation, minimizing off-target toxicity and preserving the host microbiome [99] [53]. This technical guide synthesizes current advances in prodrug design, emphasizing experimental methodologies for evaluating specificity and toxicity within the framework of resistome research.
Theoretical Foundations: Prodrug Classes and Activation Mechanisms
Prodrugs are pharmacologically inactive compounds that undergo biotransformation into active drugs via enzymatic or chemical processes. They are classified into three main categories:
- Carrier-linked prodrugs: An active drug is linked to a promoiety (e.g., esters), which is cleaved to release the drug [99].
- Bioprecursor prodrugs: Molecular modifications (e.g., oxidation/reduction) activate the drug [99].
- Double prodrugs: Two linkers or active drugs are combined, requiring multiple steps for activation [99].
For antibacterial applications, prodrugs are engineered to be activated by pathogen-specific enzymes, such as β-lactamases or esterases, ensuring targeted drug release [99] [100]. This specificity reduces collateral damage to host cells and commensal bacteria, addressing key limitations of broad-spectrum antibiotics [101].
Case Studies: Targeting Bacterial Resistomes with Prodrugs
β-Lactamase-Activated Ciprofloxacin Prodrug
Objective: To deliver ciprofloxacin selectively to β-lactamase-expressing Escherichia coli while sparing non-resistant bacteria [99]. Prodrug Design: A cephalosporin core was linked to ciprofloxacin via a 3′-cephem ester. The cephalosporin moiety serves as a substrate for β-lactamase cleavage, releasing active ciprofloxacin intracellularly [99]. Key Findings:
- The prodrug showed no activity against non-β-lactamase-expressing strains.
- Enzyme-triggered activation minimized disruption of the host microbiome [99].
Florfenicol Amine: Hijacking the WhiB7 Resistome inM. abscessus
Objective: Exploit the WhiB7-regulated resistome to convert a prodrug into its active form [53] [52]. Mechanism:
- Florfenicol amine (prodrug) is acetylated by Eis2, an enzyme upregulated by WhiB7.
- The active form, florfenicol acetyl, inhibits ribosomal function, amplifying WhiB7 activation and creating a feed-forward loop for sustained drug release [52]. Advantages:
- Avoids mitochondrial toxicity due to selective bacterial activation.
- Demonstrates higher safety margins in animal models [52].
Experimental Protocols for Assessing Prodrug Specificity and Toxicity
1In VitroEnzyme Activation Assays
Protocol:
- Recombinant Enzyme Incubation: Incubate the prodrug (e.g., 100 µM) with purified bacterial enzymes (e.g., β-lactamase, Eis2) in buffer (pH 7.4, 37°C).
- Kinetic Monitoring: Use HPLC or LC-MS to quantify drug release over time. Calculate conversion rates using standard curves.
- Selectivity Validation: Test prodrug stability in human esterase-rich media (e.g., plasma, liver microsomes) to confirm pathogen-specific activation [99] [100].
Cell-Based Specificity and Toxicity Screening
Workflow:
- Bacterial Strains: Include target pathogens (e.g., β-lactamase-positive E. coli, M. abscessus) and non-target strains (e.g., WhiB7-knockout mutants).
- Minimum Inhibitory Concentration (MIC) Assays: Compare prodrug efficacy against active drugs. A significant MIC reduction in target strains indicates selective activation [52].
- Host Cytotoxicity: Expose mammalian cell lines (e.g., HEK-293) to prodrugs and measure viability via MTT assays. A high selectivity index (IC₅₀/MIC) confirms low host toxicity [52].
3In VivoEfficacy and Safety Models
Animal Studies:
- Infection Models: Administer prodrugs to mice infected with resistant bacteria (e.g., MRSA, M. abscessus). Monitor bacterial load reduction in organs (e.g., lungs, spleen).
- Toxicity Metrics: Assess mitochondrial toxicity (e.g., hearing loss) and microbiome disruption via 16S rRNA sequencing of fecal samples [52].
Visualization of Prodrug Activation Pathways
Signaling Pathway: Florfenicol Amine Activation via WhiB7
The feed-forward loop in M. abscessus illustrates how resistance mechanisms are co-opted for prodrug activation:
Title: Prodrug Activation via WhiB7-Eis2 Loop
Experimental Workflow for Prodrug Validation
A generalized protocol for evaluating prodrug specificity and toxicity:
Title: Prodrug Validation Workflow
Research Reagent Solutions for Prodrug Development
Table 1: Key Reagents and Their Applications in Prodrug Research
| Reagent/Assay | Function | Example Use Case |
|---|---|---|
| Recombinant β-lactamases | Hydrolyze β-lactam rings in prodrugs | Activating ciprofloxacin prodrugs [99] |
| Eis2 Acetyltransferase | Acetylate florfenicol amine | Targeting M. abscessus WhiB7 resistome [52] |
| HPLC-MS Systems | Quantify prodrug conversion kinetics | Measure drug release rates in vitro [99] |
| Bacterial Mutant Libraries (e.g., ΔWhiB7) | Validate mechanism-specific activation | Confirm target engagement [52] |
| Mammalian Cell Lines (HEK-293, HepG2) | Assess host cytotoxicity | Determine selectivity indices [52] |
| 16S rRNA Sequencing Kits | Analyze microbiome impact | Evaluate ecological safety [52] |
Discussion: Advantages and Future Directions
Targeted prodrugs address two critical challenges in antimicrobial therapy:
- Specificity: Bacterial enzyme-mediated activation confines drug release to pathogens, reducing off-target effects [99] [53].
- Toxicity Mitigation: By avoiding mitochondrial and human enzyme interactions, prodrugs like florfenicol amine exhibit improved safety profiles [52].
Future work should focus on expanding this approach to other resistance mechanisms (e.g., efflux pumps) and integrating machine learning to design prodrugs with optimized pharmacokinetics [53] [52].
The strategic design of prodrugs that exploit bacterial resistome elements represents a paradigm shift in overcoming antibiotic resistance. Through rigorous validation of specificity and toxicity, researchers can develop precision therapies that transform resistance mechanisms into therapeutic vulnerabilities.
The relentless expansion of antibiotic resistance represents one of the most pressing challenges to modern medicine, threatening to return healthcare to a pre-antibiotic era where routine infections become life-threatening. With multi-drug and pan-drug-resistant bacteria increasingly common in clinical settings, the infectious disease research community has been compelled to adopt novel approaches that fundamentally rethink our relationship with bacterial evolution [102]. Within this context, the concept of the intrinsic resistome—the collection of chromosomal genes that contribute to innate antibiotic tolerance—has emerged as a crucial framework for understanding and combating resistance [23]. These intrinsic resistance mechanisms, including efflux pumps, cell envelope permeability barriers, and stress response systems, represent the first line of bacterial defense and serve as potential gateways for evolutionary adaptation under antibiotic pressure.
Experimental evolution has established itself as an indispensable tool for dissecting adaptive paths to antibiotic resistance, allowing researchers to observe evolutionary dynamics in real-time under controlled laboratory conditions [103]. Unlike retrospective genomic analyses of clinical isolates, which can only provide snapshots of successful resistance mutations, experimental evolution enables the systematic reconstruction of evolutionary trajectories, revealing not only the mutations that confer resistance but also their order of appearance, fitness costs, epistatic interactions, and compensatory mechanisms [102] [104]. This review synthesizes recent advances in using experimental evolution to validate potential antibiotic targets, with particular emphasis on strategies that account for the evolutionary potential of bacterial pathogens and aim to develop evolution-resistant therapies.
Fundamental Principles of Experimental Evolution Design
The power of experimental evolution to illuminate resistance pathways hinges on carefully considered experimental parameters that balance ecological relevance with practical feasibility. Several key considerations must be addressed to design evolution experiments that yield actionable insights for target validation.
Population Parameters and Evolutionary Dynamics
The dynamics of adaptation are profoundly influenced by population genetics parameters, particularly effective population size (N~e~) and the number of replicate populations [104]. Population size determines the selection threshold—mutations with selective advantages greater than 1/N~e~ can be enriched by selection—while also influencing the diversity of beneficial lineages competing within a population (clonal interference). Practical implementations often utilize serial dilution regimens in 96-well plates, with daily 1:1,024 dilutions achieving approximately 10 generations per day at N~e~ ~ 10^5^ [104].
The number of experimental replicates represents perhaps the most critical parameter for distinguishing deterministic evolutionary outcomes from stochastic events. Research indicates that 48 replicate populations are generally sufficient to identify beneficially mutated genes through statistical overrepresentation [104]. High-throughput automated systems using liquid-handling robotics have dramatically increased the scale and reproducibility of these experiments, enabling the maintenance of hundreds of evolving populations in parallel [104].
The duration of evolution experiments must be calibrated to capture meaningful adaptation without introducing excessive contingency. Studies reveal that beneficial mutations emerge across vastly different timescales—some appearing within a few dozen generations, while others only surfacing after thousands of generations [104]. Long-term evolution experiments (LTEE), such as the landmark E. coli study now exceeding 75,000 generations, reveal a fascinating transition from strong parallelism in early adaptation to increasingly contingent, lineage-specific solutions as populations accumulate historical constraints [104].
Table 1: Key Parameters in Experimental Evolution Design
| Parameter | Considerations | Typical Implementation |
|---|---|---|
| Replicate Populations | More replicates increase power to detect parallel evolution; minimizes stochastic effects | 48+ replicates [104] |
| Population Size | Influences selection threshold and clonal interference | N~e~ ~ 10^5^-10^6^ [104] |
| Propagation Regime | Serial dilution vs. continuous culture; bottleneck size and frequency | 1:1,024 daily dilution (≈10 generations/day) [104] |
| Experimental Duration | Short-term vs. long-term adaptation; contingency effects | 100-1,000+ generations [104] |
| Selection Pressure | Constant vs. increasing concentration; combination therapies | Sub-MIC to supra-MIC gradients [102] |
Experimental Methodologies and Workflows
Core Protocol for Laboratory Evolution
A standardized approach to experimental evolution enables systematic comparison across studies and conditions. A representative protocol for evolving antibiotic resistance incorporates the following key steps [105] [104]:
Strain Selection and Preparation: Experiments typically commence with isogenic clones of target pathogens, sometimes including mutator strains (e.g., ΔmutS) to accelerate genetic diversity generation. Both non-mutator and hypermutable strains provide complementary insights—the former reflecting typical evolutionary dynamics, the latter expanding the mutational landscape [105].
Population Propagation: Daily transfer protocols involve inoculating fresh medium containing sub-inhibitory antibiotic concentrations with stationary-phase cultures from the previous cycle. A standard 1:1,000 dilution factor per transfer provides approximately 10 generations per day, maintaining populations in exponential growth phase [104].
Escalating Selection Pressure: Beginning from sub-MIC concentrations, antibiotic pressure is systematically increased—typically by doubling when populations demonstrate robust growth—creating a selective landscape that favors incremental resistance mechanisms [102] [105].
Fossil Record Preservation: Regular archiving of frozen population samples (e.g., weekly) enables retrospective analysis of evolutionary trajectories and allows "replay" experiments to test evolutionary repeatability [104].
Phenotypic Monitoring: Continuous assessment of growth kinetics (optical density), minimum inhibitory concentrations (MIC), and fitness relative to ancestor strains provides phenotypic context for genomic analyses [105].
Diagram 1: Experimental Evolution Workflow for Target Validation
Genomic Analysis of Evolved Populations
Next-generation sequencing of evolved populations enables comprehensive identification of genetic changes underlying adaptation. The following bioinformatic pipeline has proven effective for identifying targets of selection [104]:
Whole-Genome Sequencing: Sequence pooled populations or individual clones at multiple time points to capture dynamic evolutionary processes.
Variant Identification and Annotation: Tools like breseq efficiently identify mutations in laboratory-evolved microbes from sequencing data, detecting single-nucleotide variants, insertions/deletions, and structural variations [102].
Parallel Evolution Analysis: Statistical assessment of genes mutated across multiple replicate populations significantly beyond random expectation identifies the most critical resistance determinants.
Fitness Estimation: While direct competition assays provide the most accurate fitness measurements, tracking mutation frequencies through time offers a high-resolution view of evolutionary dynamics [104].
Pathway Enrichment Analysis: Mapping mutations to biochemical pathways reveals whether evolution targets specific cellular processes or distributes adaptive solutions across multiple systems.
Case Studies in Target Validation
Targeting Intrinsic Resistance Mechanisms
Experimental evolution has proven particularly valuable for validating targets within the intrinsic resistome—chromosomal genes that contribute to baseline antibiotic tolerance. A genome-wide screen of E. coli knockouts identified three key intrinsic resistance pathways whose disruption conferred hypersensitivity to trimethoprim and chloramphenicol: the AcrAB-TolC efflux system (acrB), and cell envelope biogenesis pathways (rfaG, lpxM) [23].
Subsequent experimental evolution under trimethoprim pressure revealed strikingly different evolutionary potential among these targets. While ΔacrB (efflux-deficient) populations were substantially compromised in their ability to evolve resistance—succumbing to extinction under high drug concentrations—ΔrfaG and ΔlpxM (cell envelope-deficient) populations frequently adapted to trimethoprim through mutations that upregulated the drug target (dihydrofolate reductase) [23]. This establishes efflux inhibition as a more promising "resistance-proofing" strategy compared to membrane disruption, though pharmacological inhibition of efflux faced challenges distinct from genetic ablation due to evolution of inhibitor resistance.
Exploiting Evolutionary Constraints inMycobacterium abscessus
An innovative approach to resistance-proofing emerged from studies of Mycobacterium abscessus, where researchers discovered that a structurally modified version of florfenicol could subvert the pathogen's resistance machinery [35]. Surprisingly, this compound demonstrated enhanced activity specifically against wild-type M. abscessus while showing no effect against strains lacking the transcriptional regulator WhiB7—precisely the opposite of conventional antibiotic behavior.
Mechanistic investigation revealed that the modified florfenicol functions as a prodrug that is activated by Eis2, a resistance protein induced by WhiB7. This creates a self-amplifying cycle: WhiB7 activation increases Eis2 production, which generates more active drug, further enhancing WhiB7 activation [35]. This "resistance hacking" strategy exploits the evolutionary constraint that pathogens cannot easily discard resistance mechanisms without incurring substantial fitness costs, thereby locking them into a suicidal resistance pathway.
Table 2: Validated Targets from Experimental Evolution Studies
| Target | Organism | Antibiotic | Evolutionary Validation | Reference |
|---|---|---|---|---|
| PmrAB regulatory system | Pseudomonas aeruginosa | Colistin | Parallel mutations in pmrB across replicates; chronology established | [102] |
| AcrAB-TolC efflux | Escherichia coli | Trimethoprim | Limited evolutionary recovery from hypersensitivity; extinction at high concentrations | [23] |
| WhiB7 regulon | Mycobacterium abscessus | Florfenicol analog | Resistance mechanism exploited for suicidal activation | [35] |
| LPS biosynthesis | Escherichia coli | Multiple classes | Compensatory evolution restored resistance despite initial hypersensitivity | [23] |
| PhoPQ regulatory system | Escherichia coli | Trimethoprim | Frequent mutations in mgrB regulator during adaptation | [23] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Experimental Evolution Studies
| Reagent / Tool | Function | Application Example |
|---|---|---|
| Keio Collection | Genome-wide single-gene knockout library of E. coli | Identification of hypersensitive mutants for intrinsic resistance genes [23] |
| breseq | Computational pipeline for identifying mutations from sequencing data | Analysis of evolutionary trajectories in laboratory-evolved populations [102] |
| Liquid Handling Robotics | Automated culture transfer and dilution | High-throughput evolution experiments in 96-well format [104] |
| CARD (Comprehensive Antibiotic Resistance Database) | Curated database of resistance genes, mechanisms, and targets | Annotation and classification of resistance mutations [24] |
| Mutator Strains | Strains with defective DNA repair (e.g., ΔmutS) | Accelerating mutational diversity to explore evolutionary potential [105] |
Emerging Frontiers and Conceptual Advances
Resistance Hacking and Evolutionary Traps
The conventional paradigm of antibiotic development seeks compounds that bypass existing resistance mechanisms. In contrast, "resistance hacking" strategies aim to co-opt resistance machinery for bactericidal purposes, as demonstrated by the engineered florfenicol prodrug activated by M. abscessus resistance proteins [35]. This approach essentially creates evolutionary traps—situations where expression of resistance genes becomes detrimental rather than beneficial. Such strategies potentially offer higher evolutionary barriers to resistance, as pathogens would need to simultaneously disable both the resistance mechanism and its hijacked function.
Incorporating Horizontal Gene Transfer
Most experimental evolution studies focus on chromosomal adaptation, despite the critical role of horizontal gene transfer (HGT) in clinical resistance dissemination. Incorporating HGT into evolution experiments presents methodological challenges but offers more clinically relevant insights [103]. Innovative approaches include co-culturing multiple bacterial strains to permit natural gene exchange, or introducing plasmid libraries containing resistance genes to study their stability and transfer dynamics under various selective regimes.
Bridging Laboratory and Clinical Evolution
A crucial validation of experimental evolution approaches comes from comparing laboratory-evolved mutations with those observed in clinical isolates. For instance, evolution of Pseudomonas aeruginosa to colistin resistance in bioreactors recapitulated mutations in the pmrAB regulatory system identical to those found in isolates from colistin-treated cystic fibrosis patients [102]. Such concordance reinforces the predictive power of well-designed evolution experiments and their utility in anticipating clinical resistance trajectories.
Diagram 2: Resistance Hacking Cycle in M. abscessus
Experimental evolution under antibiotic pressure has transformed from a basic science tool into an indispensable approach for validating antimicrobial targets and designing evolution-resistant therapies. The lessons from a decade of evolution experiments highlight several fundamental principles: (1) Resistance evolution often follows predictable, parallel trajectories when observed across sufficient replicates; (2) The fitness costs of resistance create vulnerabilities that can be exploited through appropriate drug combinations; (3) Targeting intrinsic resistance mechanisms, particularly efflux pumps, shows promise for limiting evolutionary escape routes; and (4) Innovative strategies that hijack resistance pathways themselves may provide higher evolutionary barriers than conventional antibiotics.
The integration of experimental evolution into the antibiotic development pipeline offers a path toward more durable therapies that explicitly account for bacterial adaptability. By subjecting potential targets to relentless evolutionary pressure in the laboratory, we can identify those least likely to succumb to resistance in the clinic—a crucial advantage in the ongoing arms race against bacterial pathogens. As these methods continue to mature and incorporate more complex ecological scenarios, including polymicrobial communities and host environments, their predictive power and clinical relevance will only increase, potentially heralding a new generation of evolution-proof antimicrobials.
Conclusion
The study of the intrinsic resistome reveals a complex landscape of bacterial defense that extends far beyond a few well-known mechanisms. Targeting these intrinsic pathways offers a powerful, broad-spectrum strategy to revitalize existing antibiotics and combat multidrug-resistant infections. However, the long-term success of such approaches hinges on overcoming the formidable capacity of bacteria for evolutionary adaptation, as evidenced by rapid recovery from hypersensitivity and the emergence of resistance to pharmacological inhibitors like Efflux Pump Inhibitors. Future research must prioritize the development of strategies that are not only effective in sensitizing pathogens but also evolutionarily robust. This will require a deeper integration of evolutionary principles into drug design, advanced PK/PD modeling to define dosing regimens that suppress resistance, and a continued exploration of innovative concepts like 'resistance hacking.' A concerted effort across basic science, translational research, and clinical practice, guided by a One-Health perspective, is essential to translate these promising findings into durable solutions for the global AMR crisis.
References
- 1. The intrinsic resistome of bacterial pathogens [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2013.00103/full]
- 2. The intrinsic resistome of Klebsiella pneumoniae [https://www.sciencedirect.com/science/article/abs/pii/S0924857918302711]
- 3. MetaCompare 2.0: differential ranking of ecological and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12116288/]
- 4. Understanding Antimicrobial Resistance [https://www.uspharmacist.com/article/understanding-antimicrobial-resistance]
- 5. Antibiotic resistome from the One-Health perspective [https://www.nature.com/articles/s12276-021-00569-z]
- 6. Beyond the Resistome: Molecular Insights, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561093/]
- 7. Deciphering Resistome and Virulome Diversity in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6144875/]
- 8. Bacterial Multidrug Efflux Pumps: Much More Than ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5029519/]
- 9. Tackling the outer membrane: facilitating compound entry ... [https://www.nature.com/articles/s44259-023-00016-1]
- 10. Understanding antibiotic resistance via outer membrane ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5903844/]
- 11. Efflux pump-mediated resistance to new beta lactam ... [https://www.nature.com/articles/s43856-024-00591-y]
- 12. Efflux pump activity potentiates the evolution of antibiotic ... [https://www.nature.com/articles/s41467-020-17735-y]
- 13. Quantitative contribution of efflux to multi-drug resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6443642/]
- 14. Bacterial Enzymes and Antibiotic Resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6351036/]
- 15. Membrane Permeabilization in Relation to Inactivation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC92986/]
- 16. Exploring molecular mechanisms of drug resistance in ... [https://www.sciencedirect.com/science/article/pii/S2699940425000438]
- 17. Resistome [https://en.wikipedia.org/wiki/Resistome]
- 18. Resistome - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/immunology-and-microbiology/resistome]
- 19. Origins and Evolution of Antibiotic Resistance - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2937522/]
- 20. An overview of the antimicrobial resistance mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604941/]
- 21. Resistance mechanisms – Antibiotic resistance – ReAct [https://www.reactgroup.org/toolbox/understand/antibiotic-resistance/resistance-mechanisms-in-bacteria/]
- 22. Impeding pathways of intrinsic resistance in Escherichia coli ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12543169/]
- 23. Impeding pathways of intrinsic resistance in Escherichia coli ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003443]
- 24. Comprehensive genome catalog analysis of the resistome ... [https://www.nature.com/articles/s41522-025-00746-2]
- 25. Intrinsic antibiotic resistance: mechanisms, origins ... [https://pubmed.ncbi.nlm.nih.gov/23499305/]
- 26. Molecular Factors and Mechanisms Driving Multidrug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9407594/]
- 27. Antibiotic-Resistant Pseudomonas aeruginosa: Current ... [https://www.mdpi.com/2076-2607/13/4/913]
- 28. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 29. Pseudomonas Aeruginosa: Resistance to the Max - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3128976/]
- 30. Resistance mechanisms and therapeutic strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576158/]
- 31. Pseudomonas aeruginosa: pathogenesis, virulence factors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9233671/]
- 32. Genome-wide Screening of the Escherichia coli Keio ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12457515/]
- 33. Rapid identification of key antibiotic resistance genes in E. ... [https://www.sciencedirect.com/science/article/pii/S2589004225006960]
- 34. ResistoXplorer: a web-based tool for visual, statistical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7991225/]
- 35. Approach to combat antibiotic resistance turns bacterium's ... [https://www.stjude.org/media-resources/news-releases/2025-medicine-science-news/approach-to-combat-antibiotic-resistance-turns-bacteriums-genes-against-it.html]
- 36. Antibiotic resistance: Time of synthesis in a post-genomic age [https://pmc.ncbi.nlm.nih.gov/articles/PMC8181582/]
- 37. Metagenomics as a Transformative Tool for Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11939754/]
- 38. Antibiotic resistance: Time of synthesis in a post-genomic age [https://www.sciencedirect.com/science/article/pii/S2001037021002154]
- 39. Inducible transposon mutagenesis identifies bacterial ... [https://www.nature.com/articles/s41564-025-01975-z]
- 40. High-throughput transposon mutagenesis in the family ... [https://pubmed.ncbi.nlm.nih.gov/39207104/]
- 41. Functional metagenomic libraries generated from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9995290/]
- 42. Quantifying antibiotic resistome risks across environmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12510455/]
- 43. Global livestock resistome: Antibiotic resistance is ... [https://amr.solutions/2025/08/15/global-livestock-resistome-antibiotic-resistance-is-widespread/]
- 44. Metagenome-Informed QMRA and Resistome Profiling ... [https://www.sciencedirect.com/science/article/pii/S2589914725001021]
- 45. Identifying chemogenetic interactions from CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6706933/]
- 46. Base editing screens define the genetic landscape of ... [https://www.nature.com/articles/s41588-024-01948-8]
- 47. Expression of multidrug efflux pump gene acrAB in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539121/]
- 48. The AcrAB efflux pump contributes to the virulence of ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1633585/full]
- 49. Antibiotic Adjuvants: A Versatile Approach to Combat Antibiotic Resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10061514/]
- 50. Mechanism of antibacterial resistance, strategies and next- ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1444781/full]
- 51. Alternatives Therapeutic Approaches to Conventional Antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC9774722/]
- 52. Prodrug Approach Overcomes Resistance in M. abscessus [https://www.technologynetworks.com/biopharma/news/antibiotic-resistance-reversed-using-bacterias-own-mechanisms-406444]
- 53. Antibiotic Prodrug Uses Bacteria's Resistance Genes to ... [https://www.insideprecisionmedicine.com/topics/translational-research/antibiotic-prodrug-uses-bacterias-resistance-genes-to-turn-against-itself/]
- 54. Editorial: Prodrug design and therapeutic applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10557042/]
- 55. Challenges and Strategies in Prodrug Design [https://sciensage.info/index.php/JASR/article/view/2430]
- 56. Bacterial evolution of antibiotic hypersensitivity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3817406/]
- 57. Bacterial evolution of antibiotic hypersensitivity [https://pubmed.ncbi.nlm.nih.gov/24169403/]
- 58. Quantitative systems-based prediction of antimicrobial ... [https://www.nature.com/articles/s41540-023-00304-6]
- 59. Mutations in mexT bypass the stringent response ... [https://www.sciencedirect.com/science/article/pii/S221112472401430X]
- 60. Genes-first and phenotypes-first paths to treatment ... [https://www.nature.com/articles/s41419-025-08127-5]
- 61. Bypass of genetic constraints during mutator evolution to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4375862/]
- 62. Mutation Frequencies and Antibiotic Resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC89960/]
- 63. support in CellDesigner - PMC BioPAX [https://pmc.ncbi.nlm.nih.gov/articles/PMC3232372/]
- 64. A mutation-induced drug resistance database (MdrDB) [https://www.nature.com/articles/s42004-023-00920-7]
- 65. Function and Inhibitory Mechanisms of Multidrug Efflux ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.737288/full]
- 66. for bacterial pathogens: From bench to... Efflux pump inhibitors [https://pmc.ncbi.nlm.nih.gov/articles/PMC6563736/]
- 67. Clinically Relevant Chromosomally Encoded Multidrug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1471989/]
- 68. Role of bacterial efflux pumps in antibiotic resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10268834/]
- 69. Molecular and phenotypic characterization of efflux and pumps ... efflux [https://jcoagri.uobaghdad.edu.iq/index.php/intro/article/view/2189]
- 70. Heterogeneous efflux expression underpins phenotypic... pump [https://elifesciences.org/articles/99752]
- 71. Co-Selection of Resistance to Antibiotics, Biocides and Heavy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4790313/]
- 72. Co-selection for antibiotic resistance by environmental ... [https://www.nature.com/articles/s44259-024-00026-7]
- 73. Co-occurrence of resistance genes to antibiotics, biocides and ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-015-2153-5]
- 74. Co-selection of multi-antibiotic resistance in bacterial ... [https://www.sciencedirect.com/science/article/abs/pii/S0045653518319751]
- 75. Evolution of antibiotic cross‐resistance and collateral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7086048/]
- 76. Systematic mapping of antibiotic cross-resistance and ... [https://www.nature.com/articles/s41564-024-01857-w]
- 77. Global diversity and distribution of antibiotic resistance ... [https://www.nature.com/articles/s41467-025-59019-3]
- 78. a population PK/PD blueprint for ceftolozane/tazobactam ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587603/]
- 79. Antibiotics, Resistome and Resistance Mechanisms [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.02066/full]
- 80. Utilizing NCA, PopPK/PD, and PBPK Tools for MIDD Success [https://premier-research.com/perspectives/choosing-the-right-pk-modeling-approach-utilizing-nca-poppk-pd-and-pbpk-tools-for-midd-success/]
- 81. Spatial Pharmacokinetic and Pharmacodynamic Modeling ... [https://link.springer.com/article/10.1007/s40262-025-01575-4]
- 82. Recognizing and exploiting differences between RNAi and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2924165/]
- 83. Not all loss-of-function approaches are created equal [https://communities.springernature.com/posts/not-all-loss-of-function-approaches-are-created-equal-differential-cellular-responses-to-small-molecule-inhibition-acute-crispr-perturbation-and-chronic-genetic-knockout]
- 84. Evaluating drug targets through human loss-of-function ... [https://www.nature.com/articles/s41586-020-2267-z]
- 85. Substrate-selective small-molecule modulators of enzymes [https://www.sciencedirect.com/science/article/abs/pii/S1367593122001168]
- 86. Genome editing or small molecule inhibition of KMT5A in CAR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12519333/]
- 87. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 88. The limitations of small molecule and genetic screening in ... [https://www.sciencedirect.com/science/article/pii/S2451945625003459?dgcid=rss_sd_all]
- 89. Efflux-Mediated Resistance in Enterobacteriaceae [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382670/]
- 90. An Overview of the Epidemiology of Multidrug Resistance and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472688/]
- 91. Screening and Evaluation of Potential Efflux with... Pump Inhibitors [https://pmc.ncbi.nlm.nih.gov/articles/PMC11274134/]
- 92. An undergraduate experimental research program, involving the... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-07340-2]
- 93. Identification of Compounds With Potential Dual Inhibitory ... [https://www.researchprotocols.org/2025/1/e66197]
- 94. Genomic and Functional Characterization of Multidrug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12291844/]
- 95. Study on resistance mechanisms and molecular ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1643755/full]
- 96. Mycobacteroides abscessus subspecies: a comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12090666/]
- 97. Characterization of Prophages and Their Genetic Cargo in ... [https://www.mdpi.com/2076-2607/13/9/2028]
- 98. Comprehensive antibiotic resistome comparison of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181972/]
- 99. Antibacterial Prodrugs to Overcome Bacterial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC7180472/]
- 100. Microbial esterases and ester prodrugs: An unlikely ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/30302779/]
- 101. 抗生素仍然是我們最有效的武器。 然而在抗藥性細菌越 ... [https://www.facebook.com/investigator.tw/posts/%E7%84%A1%E5%8F%AF%E6%95%91%E8%97%A5-%E6%8A%97%E7%94%9F%E7%B4%A0%E7%9A%84%E7%99%BC%E5%B1%95%E4%BD%95%E5%8E%BB%E4%BD%95%E5%BE%9E-1928%E5%B9%B4%E8%8B%B1%E5%9C%8B%E7%9A%84%E4%BD%9B%E8%90%8A%E6%98%8E%E7%88%B5%E5%A3%ABsir-alexander-fleming%E5%9C%A8%E7%9C%9F%E8%8F%8C%E7%A0%94%E7%A9%B6%E4%B8%AD%E6%84%8F%E5%A4%96%E7%99%BC%E7%8F%BE%E7%9A%84%E9%9D%92%E9%BB%B4%E7%B4%A0penicillin1-%E7%9B%B8%E4%BF%A1%E5%B7%B2%E7%B6%93/719207041600688/?locale=zh_CN]
- 102. Using experimental evolution to identify druggable targets ... [https://www.nature.com/articles/ja2017108]
- 103. Experimental evolution as an efficient tool to dissect ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764614000041]
- 104. Identifying targets of selection in laboratory evolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11197053/]
- 105. Experimental evolution of resistance to an antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1560030/]