Taming the Data Deluge: Computational Strategies for Large-Scale Chemogenomic NGS
The integration of next-generation sequencing (NGS) into chemogenomics—the study of how genes influence drug response—generates datasets of immense scale and complexity, creating significant computational bottlenecks.
Taming the Data Deluge: Computational Strategies for Large-Scale Chemogenomic NGS
Abstract
The integration of next-generation sequencing (NGS) into chemogenomics—the study of how genes influence drug response—generates datasets of immense scale and complexity, creating significant computational bottlenecks. This article provides a comprehensive guide for researchers and drug development professionals navigating the computational landscape of large-scale chemogenomic NGS data. We explore the foundational data challenges and the pivotal role of AI, detail modern methodological approaches including multi-omics integration and cloud computing, present proven strategies for pipeline optimization and troubleshooting, and finally, examine rigorous frameworks for analytical validation and performance comparison. By synthesizing these core areas, this article serves as a strategic roadmap for overcoming computational hurdles to accelerate drug discovery and the advancement of precision medicine.
The Scale of the Challenge: Foundational Concepts in Chemogenomic Data Complexity
The integration of Next-Generation Sequencing (NGS) into chemogenomics has propelled the field squarely into the "big data" era, characterized by the three V's: Volume, Velocity, and Variety [1] [2]. In chemogenomics, Volume refers to the immense amount of data generated from sequencing and screening; Velocity is the accelerating speed of this data generation and the rate at which it must be processed to be useful; and Variety encompasses the diverse types of data, from genomic sequences and gene expression to chemical structures and protein-target interactions [1] [2]. Managing these three properties presents significant computational challenges that require sophisticated data management and analysis strategies to advance drug discovery and precision medicine [3].
Table 1: The Three V's of Chemogenomic Data
| Characteristic | Definition in Chemogenomics | Example Data Sources |
|---|---|---|
| Volume | The vast quantity of data points generated from high-throughput technologies. | NGS platforms, HTS assays (e.g., Tox21), public databases (e.g., PubChem, ChEMBL) [1]. |
| Velocity | The speed at which new chemogenomic data is generated and must be processed. | Rapid sequencing runs, continuous data streams from live-cell imaging, real-time analysis needs for clinical applications [2] [3]. |
| Variety | The diversity of data types and formats that must be integrated. | DNA sequences, RNA expression, protein targets, chemical structures, clinical outcomes, spectral data [1] [3]. |
Quantifying the Data Deluge: Volume in Context
The volume of publicly available chemical and biological data has grown exponentially over the past decade. Key repositories have seen a massive increase in both the number of compounds and the number of biological assays, fundamentally changing the landscape of computational toxicology and drug discovery [1].
Table 2: Volume of Data in Public Repositories (2008-2018)
| Database | Record Type | ~2008 Count | ~2018 Count | Approx. Increase | Key Content |
|---|---|---|---|---|---|
| PubChem [1] | Unique Compounds | 25.6 million | 96.5 million | >3.7x | Chemical structures, bioactivity data |
| Bioassay Records | ~1,500 | >1 million | >666x | Results from high-throughput screens | |
| ChEMBL [1] | Bioassays | - | 1.1 million | - | Binding, functional, and ADMET data for drug-like compounds |
| Compounds | - | 1.8 million | - | ||
| ACToR [1] | Compounds | - | >800,000 | - | Aggregated in vitro and in vivo toxicity data |
| REACH [1] | Unique Substances | - | 21,405 | - | Data submitted under European Union chemical legislation |
Experimental Protocols & Methodologies
Protocol: Designing a Focused Anticancer Compound Library
This methodology outlines the construction of a targeted screening library, a common task in precision oncology that must contend with all three V's of chemogenomic data [4].
Objective: To design a compact, target-annotated small-molecule library for phenotypic screening in patient-derived cancer models, maximizing cancer target coverage while minimizing library size.
Step-by-Step Procedure:
Define the Target Space:
Identify Compound-Target Interactions (Theoretical Set):
Apply Multi-Stage Filtering (Large-scale & Screening Sets):
- Global Activity Filter: Remove compounds lacking robust evidence of biological activity [4].
- Potency Filter: For each target, select the most potent compounds to reduce redundancy [4].
- Availability Filter: Filter compounds based on commercial availability for screening, finalizing the physical library (e.g., 1,211 compounds) while retaining high target coverage (e.g., 84%) [4].
Validation via Pilot Screening:
Workflow: Data Generation to Analysis in NGS
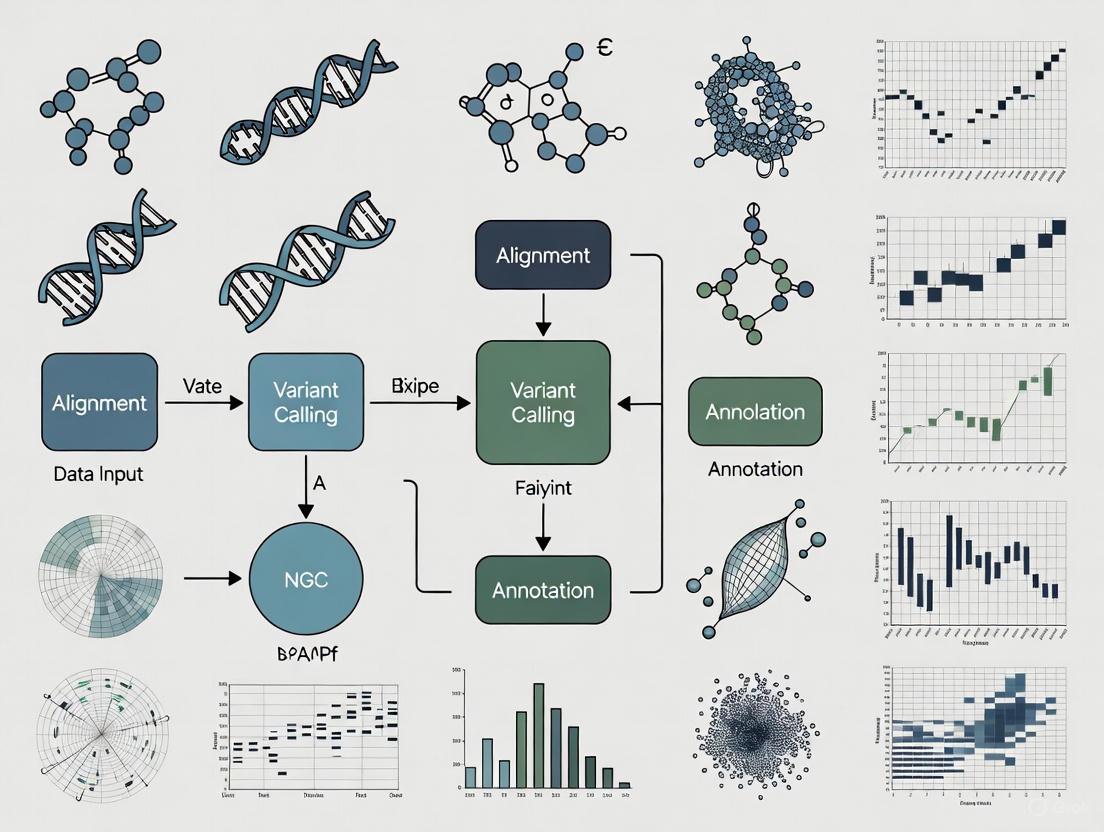
The following diagram illustrates the generalized workflow from sample preparation to data analysis in an NGS-based chemogenomic study, highlighting potential failure points.
Diagram 1: NGS workflow showing key failure points.
Troubleshooting Guides & FAQs
This section addresses common computational and experimental challenges faced by researchers working with large-scale chemogenomic data.
FAQ: Data Management & Analysis
Q: Our lab generates terabytes of NGS data. What are the most efficient strategies for storing and transferring these large datasets?
A: The volume and velocity of NGS data make traditional internet transfer inefficient. Recommended strategies include:
- Centralized Housing: Store data in a central location and bring high-performance computing (HPC) resources to the data, rather than moving the data itself [3].
- Physical Transfer: For initial transfers, copying data to large storage drives and shipping them is often more efficient than network transfer [3].
- Cloud & Heterogeneous Computing: Leverage cloud computing environments and specialized hardware accelerators to manage processing demands and costs [3].
Q: How can we integrate diverse data types (Variety) like genomic sequences, chemical structures, and HTS assay results?
A: The variety of data requires robust informatics pipelines.
- Standardization: Invest time in converting data into common, interoperable formats. The lack of industry-wide standards for NGS data beyond simple text files makes this a critical step [3].
- Advanced Modeling: Use computational environments designed for building complex models (e.g., Bayesian networks) that integrate diverse, large-scale data sets to predict complex phenotypes like disease susceptibility or drug response [3].
Q: What are the common computational bottlenecks in analyzing large chemogenomic datasets?
A: Understanding your problem's nature is key to selecting the right computational platform [3]. Bottlenecks can be:
- Network-Bound: Data is too large to efficiently copy over the network.
- Disk-Bound: Data cannot be processed on a single disk and requires distributed storage.
- Memory-Bound: The analysis algorithm requires more random access memory (RAM) than is available.
- Computationally Bound: The algorithm itself is intensely complex (e.g., NP-hard problems like reconstructing Bayesian networks) [3].
FAQ: NGS Experiment Troubleshooting
Q: My NGS library yield is low. What are the primary causes and solutions?
A: Low yield is a frequent issue often traced to early steps in library preparation [5].
Table 3: Troubleshooting Low NGS Library Yield
| Root Cause | Mechanism of Failure | Corrective Action |
|---|---|---|
| Poor Input Quality | Degraded DNA/RNA or contaminants (phenol, salts) inhibit enzymes. | Re-purify input sample; use fluorometric quantification (Qubit) over UV absorbance; check purity ratios (260/230 > 1.8) [5]. |
| Fragmentation Issues | Over- or under-shearing produces fragments outside the optimal size range for adapter ligation. | Optimize fragmentation time/energy; verify fragment size distribution on BioAnalyzer or similar platform [5]. |
| Inefficient Ligation | Suboptimal adapter-to-insert ratio or poor ligase performance. | Titrate adapter:insert molar ratios; ensure fresh ligase and buffer; maintain optimal reaction temperature [5]. |
| Overly Aggressive Cleanup | Desired library fragments are accidentally removed during purification or size selection. | Adjust bead-to-sample ratios; avoid over-drying magnetic beads during clean-up steps [5]. |
Q: My sequencing data shows a high percentage of adapter dimers. How do I resolve this?
A: A sharp peak around 70-90 bp in an electropherogram indicates adapter-dimer contamination [5].
- Root Cause: This is typically due to an imbalance in the adapter-to-insert molar ratio, with excess adapters promoting dimer formation, or inefficient ligation where adapters fail to ligate to the target insert [5].
- Solutions:
- Reanalyze Data: If possible, reanalyze the run with the correct barcode settings (e.g., select "RNABarcodeNone") to automatically trim the adapter sequence [6].
- Optimize Ligation: Precisely quantify your insert DNA and titrate the adapter amount to find the optimal ratio [5].
- Improve Cleanup: Use optimized bead-based cleanups to more effectively remove short adapter-dimer products prior to sequencing [5].
Q: Our automated variant calling pipeline is producing inconsistent results. What should I check?
A: Inconsistencies often stem from issues with data quality, formatting, or software configuration.
- Check Data Quality: Review sequence quality metrics (e.g., Phred scores), coverage depth, and alignment rates. Low-quality data will lead to unreliable variant calls.
- Verify File Formats: Ensure all input files are in the correct, standardized format (e.g., BAM, VCF) as required by your tools. Incompatibilities between tools are common [3].
- Review Parameters: Examine the software parameters and thresholds used in the analysis pipeline. Small changes can significantly impact results.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful navigation of the chemogenomic data deluge requires both wet-lab and computational tools.
Table 4: Key Research Reagent Solutions for Chemogenomic Studies
| Tool / Reagent | Function / Application | Example / Note |
|---|---|---|
| Focused Compound Libraries | Target-annotated sets of small molecules for phenotypic screening in relevant disease models. | C3L (Comprehensive anti-Cancer small-Compound Library): A physically available library of 789 compounds covering 1,320 anticancer targets for identifying patient-specific vulnerabilities [4]. |
| High-Throughput Screening Assays | Rapid in vitro tests to evaluate compound toxicity or bioactivity across hundreds of targets. | ToxCast/Tox21 assays: Used to profile thousands of environmental chemicals and drugs, generating millions of data points for predictive modeling [1]. |
| Public Data Repositories | Sources of large-scale chemical, genomic, and toxicological data for model building and validation. | PubChem: Bioactivity data [1]. ChEMBL: Drug-like molecule data [1]. CTD: Chemical-gene-disease relationships [1]. GDC Data Portal: Standardized cancer genomic data [7]. |
| Bioinformatics Pipelines | Integrated suites of software tools for processing and interpreting NGS data. | GDC Bioinformatics Pipelines: Used for harmonizing genomic data, ensuring consistency and reproducibility across cancer studies [7]. |
| Computational Environments | Platforms to handle the storage and processing demands of large, complex datasets. | Cloud Computing: Scalable resources for variable workloads [3]. Heterogeneous Computing: Uses specialized hardware (e.g., GPUs) to accelerate specific computational tasks [3]. |
The journey from raw FASTQ files to actionable biological insights is a complex computational process, particularly within large-scale chemogenomic research. This pipeline, which transforms sequencing data into findings that can inform drug discovery, is fraught with bottlenecks in data management, processing power, and analytical interpretation. This guide provides a structured troubleshooting resource to help researchers, scientists, and drug development professionals identify and overcome the most common challenges, ensuring robust, reproducible, and efficient analysis of next-generation sequencing (NGS) data.
Section 1: Data Quality & Preprocessing Bottlenecks
FAQ: Why is my initial data quality so poor, and how can I fix it?
Problem: The raw FASTQ data from the sequencer has low-quality scores, adapter contamination, or other artifacts that compromise downstream analysis.
Diagnosis & Solution: Poor data quality often stems from issues during sample preparation or the sequencing run itself. A thorough quality control (QC) check is the critical first step.
- Always verify file type, structure, and read quality before starting analysis [8]. Use QC tools like FastQC to assess base quality, adapter contamination, and overrepresented sequences [8].
- If problems are detected, use trimming tools like Trimmomatic or Cutadapt to remove low-quality bases and adapter sequences [8].
- Consult the following table to diagnose common quality issues:
| Failure Signal | Possible Root Cause | Corrective Action |
|---|---|---|
| Low-quality reads & high error rates | Over- or under-amplification during PCR; degraded input DNA/RNA | Trim low-quality bases. Re-check input DNA/RNA quality and quantity using fluorometric methods [5]. |
| Adapter dimer peaks (~70-90 bp) | Inefficient cleanup post-ligation; suboptimal adapter concentration | Optimize bead-based cleanup ratios; titrate adapter-to-insert molar ratio [5]. |
| Low library complexity & high duplication | Insufficient input DNA; over-amplification during library prep | Use adequate starting material; reduce the number of PCR cycles [5]. |
| "Mixed" sequences from the start | Colony contamination or multiple templates in reaction | Ensure single-clone sequencing and verify template purity [9]. |
Experimental Protocol: Standard Preprocessing Workflow
- Quality Control: Run FastQC on raw FASTQ files to generate a quality report.
- Adapter Trimming: Use Trimmomatic with parameters tailored to your sequencing kit and read length (e.g.,
ILLUMINACLIP:TruSeq3-PE.fa:2:30:10:2:True). - Post-trimming QC: Re-run FastQC on the trimmed FASTQ files to confirm issue resolution.
- Data Validation: Check for and resolve any incorrect metadata or incompatible file formats to ensure pipeline compatibility [8].
Section 2: Computational & Workflow Bottlenecks
FAQ: Why is my analysis pipeline so slow, and how can I scale it?
Problem: Data processing, especially alignment and variant calling, is prohibitively slow, making large-scale chemogenomic studies impractical.
Diagnosis & Solution: The computational burden of NGS analysis is a well-known challenge. The solution involves understanding your computational problem and leveraging modern, scalable infrastructure [3].
- Understand Your Computational Problem: Determine if your analysis is disk-bound (I/O limitations), memory-bound (insufficient RAM), or computationally bound (processor-intensive algorithms) [3].
- Use Structured Pipelines: Adopt workflow management systems like Snakemake or Nextflow to create reproducible, parallelized workflows that reduce human error [8].
- Leverage Efficient Formats and Cloud Computing: Use binary formats (BAM/CRAM) to save disk space. For large-scale data, consider a multi-cloud strategy to balance cost, performance, and customizability [10].
Workflow Diagram: From FASTQ to Variants
The following diagram illustrates the core steps and their logical relationships, highlighting stages that are often computationally intensive.
Section 3: Generating Biological Insights
FAQ: How do I transition from a list of variants to a chemogenomic insight?
Problem: You have a VCF file with thousands of variants but struggle to identify which are biologically relevant to drug response or mechanism of action.
Diagnosis & Solution: The bottleneck shifts from data processing to biological interpretation, requiring integration of multiple data sources and specialized tools.
- Use Specialized Variant Detection Tools: Beyond standard callers, employ tools like pGENMI (for analyzing variants in drug responses), CODEX (copy-number variant detection), and LUMPY (structural rearrangement detection) [11].
- Integrate with Public Databases: Annotate your variants using data from sources like the 1000 Genomes Project, Exome Aggregation Consortium (ExAC), and The Cancer Genome Atlas (TCGA) to assess population frequency and disease association [10] [11].
- Combine Genomic and Clinical Data: For true actionable insights in drug development, integrate genomic data with clinical information. Tools like OntoFusion demonstrate the ontology-based integration of genomic and clinical databases [11].
The following table details key software and data resources essential for a successful NGS experiment in chemogenomics.
| Item Name | Type | Function / Application |
|---|---|---|
| FastQC [8] | Software | Performs initial quality control checks on raw FASTQ data. |
| Trimmomatic [8] | Software | Removes adapter sequences and low-quality bases from reads. |
| BWA [12] [10] | Software | Aligns sequencing reads to a reference genome (hg38). |
| GATK [12] [11] | Software | Industry standard for variant discovery and genotyping. |
| IGV [11] | Software | Integrated Genome Viewer for visualizing aligned sequences. |
| Snakemake/Nextflow [8] | Workflow System | Orchestrates and automates analysis pipelines for reproducibility. |
| Reference Genome (GRC) | Data | A curated human reference assembly (e.g., hg38) from the Genome Reference Consortium for alignment [10]. |
| 1000 Genomes Project | Data | A public catalog of human genetic variation for variant annotation and population context [10] [11]. |
The Central Role of AI and Machine Learning in Decoding Genetic-Drug Interactions
Technical Troubleshooting Guide: Common AI and NGS Data Analysis Issues
This section addresses frequent computational challenges encountered when applying AI to genomic data for drug interaction research.
FAQ 1: My AI model for drug-target interaction (DTI) prediction is performing poorly, with high false negative rates. What could be the cause and how can I fix it?
- Problem: A common cause is severe class imbalance in the experimental datasets, where the number of known interacting drug-target pairs (positive class) is vastly outnumbered by non-interacting pairs [13] [14]. This leads to models that are biased toward the majority class and exhibit reduced sensitivity.
- Solution:
- Implement Data Balancing Techniques: Use Generative Adversarial Networks (GANs) to create high-quality synthetic data for the minority class [13]. One study demonstrated that this approach, combined with a Random Forest classifier, achieved a sensitivity of over 97% on benchmark datasets [13].
- Algorithmic Adjustment: Employ algorithms or loss functions designed for imbalanced data, such as weighted cross-entropy or focal loss, during model training to penalize misclassifications of the minority class more heavily.
FAQ 2: My genomic secondary analysis pipeline is too slow, creating a bottleneck in my research. How can I accelerate it?
- Problem: Traditional CPU-based alignment and variant calling tools cannot keep pace with the data deluge from next-generation sequencing (NGS). A single human genome can generate ~100 gigabytes of data, and global genomic data is projected to reach 40 exabytes by 2025 [15].
- Solution:
- Leverage Hardware Acceleration: Utilize ultra-rapid secondary analysis platforms that leverage GPU (Graphics Processing Unit) acceleration [16]. For instance, tools like the DRAGEN Bio-IT Platform or NVIDIA Parabricks have been shown to accelerate genomic analysis tasks, such as variant calling, by up to 80 times, reducing runtime from hours to minutes [15] [16].
- Optimize Data Storage: Ensure your data is in modern, compressed file formats (e.g., CRAM) and leverage efficient data management platforms like Illumina Connected Analytics to reduce data transfer and access times [16] [10].
FAQ 3: I want to identify novel drug targets from a protein-protein interaction network (PIN). What is a robust computational method for this?
- Problem: PIN data is high-dimensional and non-linear, making it difficult to extract meaningful features for predicting potential drug targets using traditional statistical methods [17].
- Solution:
- Apply Network Embedding with Deep Learning: Use a deep autoencoder to transform the high-dimensional adjacency matrix of the PIN into a low-dimensional representation [17].
- Protocol Overview:
- Data Preparation: Obtain a genome-wide PIN (e.g., with ~6,338 genes and ~35,000 interactions) [17].
- Feature Extraction: Build a symmetric deep autoencoder with multiple encoder and decoder layers. Train the network to reconstruct its input, using the bottleneck layer (e.g., 100 nodes) as the low-dimensional feature vector for each gene [17].
- Target Prediction: Use these latent features to train a classifier (e.g., XGBoost) to distinguish known drug targets from non-targets. This model can then prioritize novel candidate targets [17].
FAQ 4: The computational infrastructure for my large-scale chemogenomic project is becoming unmanageably expensive. What are my options?
- Problem: AI compute demand in biotech is surging and rapidly outpacing the supply of necessary infrastructure. Training large models, like AlphaFold, requires thousands of GPU-weeks of computation [18].
- Solution:
- Adopt a Multi-Cloud Strategy: Balance cost, performance, and customizability by not relying on a single cloud provider. This allows you to leverage best-in-class services for different tasks (e.g., specialized GPU instances for model training, optimized storage for genomic data) [10].
- Explore "Neocloud" Providers: Consider specialized GPU cloud providers like CoreWeave or Lambda, which are securing multi-billion dollar deals to supply compute specifically for AI workloads [18].
- Centralize Data and Workflows: House large datasets centrally in the cloud and bring your computation to the data to avoid costly and slow data transfers over the internet. Use workflow engines (e.g., Nextflow) to ensure reproducible and portable analyses across different cloud environments [10] [3].
Experimental Protocols for Key AI Applications in Drug Discovery
This section provides detailed methodologies for critical experiments in AI-driven genomics and drug interaction research.
Protocol: Predicting Drug-Target Interactions (DTI) with a Hybrid ML/DL and GAN Framework
This protocol is based on a 2025 Scientific Reports study that introduced a novel framework for DTI prediction [13].
1. Objective: To accurately predict binary drug-target interactions by addressing data imbalance and leveraging comprehensive feature engineering.
2. Materials & Data:
- Datasets: Use publicly available binding affinity datasets such as BindingDB (e.g., subsets for Kd, Ki, or IC50 values) [13].
- Software: Python with libraries including Scikit-learn (for Random Forest), TensorFlow or PyTorch (for implementing GANs).
3. Methodological Steps:
- Step 1: Feature Engineering
- Drug Features: Encode the molecular structure of each drug using MACCS keys, a type of structural fingerprint that represents the presence or absence of predefined substructures [13].
- Target Features: Encode the protein sequence of each target using its amino acid composition (frequency of each amino acid) and dipeptide composition (frequency of adjacent amino acid pairs) [13].
- Feature Vector Construction: Concatenate the drug and target feature vectors to create a unified representation for each drug-target pair.
- Step 2: Address Data Imbalance
- Identify Minority Class: The known interacting pairs (positive class) are typically the minority.
- Generate Synthetic Data: Train a Generative Adversarial Network (GAN) on the feature vectors of the minority class. The generator learns to produce realistic synthetic feature vectors for interacting pairs, which are then added to the training set to balance the class distribution [13].
- Step 3: Model Training and Prediction
- Classifier: Train a Random Forest Classifier on the balanced training dataset. The Random Forest is robust to overfitting and handles high-dimensional data well [13].
- Validation: Perform rigorous cross-validation and evaluate the model on held-out test sets from BindingDB.
4. Expected Outcomes: The proposed GAN+RFC model has demonstrated high performance on BindingDB datasets. You can expect metrics similar to the following [13]: Table: Performance Metrics of the GAN+RFC Model on BindingDB Datasets
| Dataset | Accuracy (%) | Precision (%) | Sensitivity (%) | Specificity (%) | F1-Score (%) | ROC-AUC (%) |
|---|---|---|---|---|---|---|
| BindingDB-Kd | 97.46 | 97.49 | 97.46 | 98.82 | 97.46 | 99.42 |
| BindingDB-Ki | 91.69 | 91.74 | 91.69 | 93.40 | 91.69 | 97.32 |
| BindingDB-IC50 | 95.40 | 95.41 | 95.40 | 96.42 | 95.39 | 98.97 |
Protocol: Prioritizing Novel Drug Targets using Deep Autoencoders on Protein Interaction Networks
This protocol is adapted from a 2021 study on target prioritization for Alzheimer's disease [17].
1. Objective: To infer novel, putative drug-target genes by learning low-dimensional representations from a high-dimensional protein-protein interaction network (PIN).
2. Materials & Data:
- PIN Data: A comprehensive human PIN (e.g., from curated databases like BioGRID or STRING).
- Known Drug Targets: A list of established drug targets for your disease of interest, available from databases like DrugBank [17].
- Software: A deep learning framework like Keras with a TensorFlow backend.
3. Methodological Steps:
- Step 1: Data Preparation
- Represent the PIN as a binary adjacency matrix where rows and columns are proteins, and a value of 1 indicates an interaction.
- Step 2: Dimensionality Reduction with Deep Autoencoder
- Network Architecture: Construct a symmetric deep autoencoder. The study used the following structure [17]:
- Encoder Layers: 6338 (input) -> 3000 -> 1500 -> 500 -> 250 -> 150 -> 100 (bottleneck).
- Decoder Layers: 100 -> 150 -> 250 -> 500 -> 1500 -> 3000 -> 6338 (output).
- Activation & Training: Use ReLU activation for all layers except the output layer, which uses a sigmoid function. Train the network to minimize the binary cross-entropy loss between the input and output matrices, forcing the bottleneck layer to learn a compressed, meaningful representation.
- Network Architecture: Construct a symmetric deep autoencoder. The study used the following structure [17]:
- Step 3: Target Gene Classification
- Feature Extraction: For each gene, use its 100-dimensional vector from the bottleneck layer as its feature set.
- Handle Class Imbalance: Since known drug targets are few, use techniques like SMOTE (Synthetic Minority Over-sampling Technique) to balance the training data [17].
- Train a Classifier: Use a powerful classifier like XGBoost on the low-dimensional features to predict the probability of a gene being a drug target.
4. Expected Outcomes: The model will output a prioritized list of genes ranked by their predicted likelihood of being viable drug targets. The original study successfully identified genes like DLG4, EGFR, and RAC1 as novel putative targets for Alzheimer's disease using this methodology [17].
Visualization of Workflows and Data Relationships
Below are diagrams illustrating the core experimental and computational workflows described in this guide.
AI for Genomic Data Analysis Workflow
Drug-Target Interaction Prediction with GAN
Table: Essential Computational Tools and Datasets for AI-Driven Genomic Research
| Resource Name | Type | Primary Function in Research | Key Features / Notes |
|---|---|---|---|
| BindingDB [13] | Database | A public database of measured binding affinities for drug-target interactions. | Provides curated data on protein-ligand interactions; essential for training and validating DTI prediction models. |
| DrugBank [17] | Database | A comprehensive database containing detailed drug and drug-target information. | Used to obtain known drug-target pairs for model training and validation in target prioritization tasks. |
| DRAGEN Bio-IT Platform [16] | Software | A secondary analysis platform for NGS data. | Provides ultra-rapid, accurate analysis of whole genomes, exomes, and transcriptomes via hardware-accelerated algorithms. |
| Deep Autoencoder [17] | Algorithm | A deep learning model for non-linear dimensionality reduction. | Transforms high-dimensional, sparse data (e.g., protein interaction networks) into low-dimensional, dense feature vectors. |
| Generative Adversarial Network (GAN) [13] | Algorithm | A framework for generating synthetic data. | Used to balance imbalanced datasets by creating realistic synthetic samples of the minority class (e.g., interacting drug-target pairs). |
| Random Forest Classifier [13] | Algorithm | A robust machine learning model for classification and regression. | Effective for high-dimensional data and less prone to overfitting; commonly used for final prediction tasks after feature engineering. |
| Illumina Connected Analytics [16] | Platform | A cloud-based data science platform for multi-omics data. | Enables secure storage, management, sharing, and analysis of large-scale genomic datasets in a collaborative environment. |
Troubleshooting Guides
Guide 1: Troubleshooting Data Storage and Transfer Issues
Problem: Inability to efficiently store, manage, or transfer large-scale NGS data.
| Problem | Possible Causes | Solutions & Best Practices |
|---|---|---|
| High Storage Costs [19] [20] | Storing all data, including raw and intermediate files, in expensive primary storage. | Implement a tiered storage policy. Use cost-effective cloud object storage (e.g., AWS HealthOmics) or archives (e.g., Amazon S3 Glacier) for infrequently accessed data, reducing costs by over 90% [19]. |
| Slow Data Transfer [3] | Network speeds are too slow for transferring terabytes of data over the internet. | For initial massive data migration, consider shipping physical storage drives. For ongoing analysis, use centralized cloud storage and bring computation to the data to avoid transfer bottlenecks [3]. |
| Performance Bottlenecks in Analysis [20] | Storage solution cannot support the parallel file access required by genomic workflows. | Choose a storage solution that supports parallel file access for rapid, reliable file retrieval during data processing [20]. |
| Data Security & Privacy Concerns [20] [21] | Lack of robust controls for protecting sensitive genetic information. | Select solutions with in-flight and at-rest encryption, role-based access controls, and compliance with regulations like HIPAA and GDPR [21]. |
Guide 2: Troubleshooting Workflow Reproducibility and Provenance
Problem: Inability to reproduce or validate previously run genomic analyses.
| Problem | Possible Causes | Solutions & Best Practices |
|---|---|---|
| Failed Workflow Execution in a New Environment [22] | Implicit assumptions in the original workflow (e.g., specific software versions, paths, or reference data) are not documented or captured. | Use explicit workflow specification languages like the Common Workflow Language (CWL) to define all steps, software, and parameters. Record prospective provenance (workflow specification) and retrospective provenance (runtime execution details) [22]. |
| Inconsistent Analysis Results [22] | Use of different software versions or parameters than the original analysis. | Capture comprehensive provenance for every run, including exact software versions, all parameters, and data produced at each step. Leverage Workflow Management Systems (WMS) designed for this purpose [22]. |
| Difficulty Reusing Published Work [22] | Published studies often omit crucial details like software versions and parameter settings. | Adopt a practice of explicit declaration in all publications. Provide access to the complete workflow code, data, and computational environment used whenever possible [22]. |
Frequently Asked Questions (FAQs)
Data Storage and Infrastructure
Q: What are the key features to look for in a genomic data storage solution? A: For large-scale projects, your storage solution should have:
- Scalability: The ability to scale to exabytes without performance loss, ideally in a hybrid cloud environment [20].
- Security & Compliance: Features like encryption and access controls that meet standards like HIPAA and GDPR [20] [21].
- Object Storage & Parallel File Access: Support for data lakes and parallel access to prevent bottlenecks during analysis [20].
- Cost-Effective Tiering: Integrated hot and cold storage options to manage lifecycle and reduce costs [19] [20].
Q: How can we manage the cost of storing petabytes of genomic data? A: The most effective strategy is a tiered approach. Move infrequently accessed data, such as raw sequencing data post-analysis, to low-cost archival storage like Amazon S3 Glacier Deep Archive, which can save over 90% in storage costs [19].
Reproducibility and Provenance
Q: What is the difference between reproducibility and repeatability in the context of genomic workflows? A:
- Repeatability: A researcher redoing their own analysis in the same environment to achieve the same outcome [22].
- Reproducibility: An independent researcher confirming or redoing the analysis, potentially in a different environment. Reproducibility is a higher standard and is crucial for validating scientific findings [22].
Q: What minimum information should be tracked to ensure a workflow is reproducible? A: At a minimum, you must capture:
- Prospective Provenance: The complete workflow specification, including all tools and their versions, parameters, and data inputs [22].
- Retrospective Provenance: The record of a specific workflow execution, including software versions, parameters, and data outputs at each step [22].
- Computational Environment: Details of the operating system, hardware, and library dependencies.
Workflow Management
Q: What are the main approaches to defining and executing genomic workflows? A: The three broad categories are:
- Pre-built Pipelines: Customized, command-line pipelines (e.g., Cpipe, bcbio-nextgen) supported by specific labs. They require significant computational expertise to reproduce [22].
- GUI-based Workbenches: Integrated platforms (e.g., Galaxy) with graphical interfaces that are more accessible but may be less flexible [22].
- Standardized Workflow Descriptions: Systems using standardized languages (e.g., Common Workflow Language - CWL) to define workflows in a portable and reproducible way, making them easier to share and execute across different environments [22].
Q: Why do workflows often fail when transferred to a different computing environment? A: Failure is often due to hidden assumptions in the original workflow, such as hard-coded file paths, specific versions of software installed via a package manager, or reliance on a particular operating system. Explicitly declaring all dependencies using containerization (e.g., Docker) and workflow specification languages mitigates this [22].
Workflow and Data Relationship Diagrams
NGS Data Management and Reproducibility Workflow
Genomic Workflow Reproducibility Lifecycle
Research Reagent Solutions
| Category | Item / Solution | Function in Large-Scale NGS Projects |
|---|---|---|
| Workflow Management Systems (WMS) | Galaxy [22] | A graphical workbench that simplifies the construction and execution of complex bioinformatics workflows without extensive command-line knowledge. |
| Common Workflow Language (CWL) [22] | A specification language for defining analysis workflows and tools in a portable and scalable way, enabling reproducibility across different software environments. | |
| Cpipe [22] | A pre-built, bioinformatics-specific pipeline for genomic data analysis, often customized by individual laboratories for targeted sequencing projects. | |
| Cloud & Data Platforms | AWS HealthOmics [19] | A managed service purpose-built for bioinformatics, providing specialized storage (Sequence Store) and workflow computing to reduce costs and complexity. |
| Illumina Connected Analytics [21] | A cloud-based data platform for secure, scalable management, analysis, and exploration of multi-omics data, integrated with NGS sequencing systems. | |
| DNAnexus [19] | A cloud-based platform that provides a secure, compliant environment for managing, analyzing, and collaborating on large-scale genomic datasets, such as the UK Biobank. | |
| Informatics Tools | DRAGEN Bio-IT Platform [21] | A highly accurate and ultra-rapid secondary analysis solution that can be run on-premises or in the cloud for processing NGS data. |
| BaseSpace Sequence Hub [21] | A cloud-based bioinformatics environment directly integrated with Illumina sequencers for storage, primary data analysis, and project management. |
Ethical and Security Considerations for Sensitive Pharmacogenomic Data
Fundamental Concepts and Importance
What are the primary security risks associated with storing pharmacogenomic data?
Pharmacogenomic data faces significant security challenges due to its sensitive, immutable nature. Unlike passwords or credit cards, genetic information cannot be reset once compromised, and a breach can reveal hereditary information affecting entire families [23]. Primary risks include:
- Data Privacy Compromises: Genomic data is personally identifiable and immutable. Exposure can lead to identity theft and genetic discrimination [23].
- Data Integrity Attacks: Cyberattacks can manipulate genetic information, leading to incorrect diagnoses or treatment recommendations [23].
- Third-Party and Collaboration Risks: Data sharing with external collaborators increases potential entry points for attacks [23].
- Regulatory Complexity: Strict compliance requirements (HIPAA, GDPR, GINA) are difficult to maintain, and breaches can result in significant fines [23].
Why is pharmacogenomic data considered particularly sensitive?
Pharmacogenomic data is uniquely sensitive because it reveals information not only about an individual but also about their biological relatives. This data is permanent and unchangeable, creating lifelong privacy concerns [24] [23]. The ethical implications are substantial, as genetic information could be misused for discrimination in employment, insurance, or healthcare access [24]. This has led to regulations like the Genetic Information Nondiscrimination Act (GINA) in the United States [24].
Security Framework Implementation
What technical security measures are recommended for protecting pharmacogenomic data?
A multi-layered security approach is essential for comprehensive protection of pharmacogenomic datasets [23]:
Table 1: Security Measures for Pharmacogenomic Data Protection
| Security Measure | Implementation Examples | Primary Benefit |
|---|---|---|
| Robust Encryption | Data encryption at rest and in transit; Quantum-resistant encryption [23] | Prevents unauthorized access |
| Strict Access Controls | Multi-factor authentication (MFA); Role-based access control (RBAC) [23] | Limits data exposure |
| AI-Driven Threat Detection | ML models to detect unusual access patterns; Real-time anomaly detection [23] | Identifies potential breaches |
| Blockchain Technology | Immutable records of data transactions; Secure data sharing [25] [23] | Ensures data integrity |
| Privacy-Preserving Technologies | Federated learning; Homomorphic encryption [23] | Enables analysis without exposing raw data |
How can blockchain technology enhance security for pharmacogenomic data?
Blockchain provides decentralized, distributed storage that eliminates single points of failure. Its immutability prevents alteration of past records, creating a secure audit trail [25]. Smart contracts on Ethereum platforms can store and query gene-drug interactions with time and memory efficiency, ensuring data integrity while maintaining accessibility for authorized research [25]. Specific implementations include index-based, multi-mapping approaches that allow efficient querying by gene, variant, or drug fields while maintaining cryptographic security [25].
Data Protection Workflow Using Blockchain
Ethical Framework and Compliance
What are the core ethical principles for handling pharmacogenomic data?
Ethical pharmacogenomic data management requires balancing innovation with fundamental rights [24]:
- Informed Consent: Patients must understand implications of genetic testing, including risks of unforeseen findings and complexities of disclosing information [24].
- Privacy Protection: Genetic data storage and sharing must prevent misuse of sensitive information [24].
- Equitable Access: Benefits of personalized medicine must be accessible across socioeconomic, racial, and ethnic groups [24].
- Non-Discrimination: Policies must prevent discrimination based on genetic predispositions in healthcare, employment, and insurance [24].
How should researchers address informed consent for pharmacogenomic studies?
Informed consent processes must clearly communicate how genetic data will be used, stored, and shared. Patients should understand the potential for incidental findings and the implications for biological relatives [24]. Consent forms should specify data retention periods, access controls, and how privacy will be maintained in collaborative research. In multi-omics studies, ensuring informed consent for comprehensive data sharing is complex but essential [26].
Troubleshooting Common Implementation Challenges
How can researchers troubleshoot data integrity and quality issues in pharmacogenomic analysis?
Data quality issues can arise from various sources in pharmacogenomic workflows:
- Genotype Calling Problems: Undetermined results may indicate sample quality issues, degradation, or impurities. Review amplification curves and real-time traces for "noisy" data [27].
- Contamination Issues: Examine QC images for leaks or contamination. Clean instrument blocks with 95% ethanol solution using lint-free cloths [27].
- Unexpected Negative Control Results: No-template controls clustering with samples may indicate probe cleavage. Analyze using lower cycle thresholds before spurious cleavage occurs [27].
What solutions address computational challenges with large-scale pharmacogenomic datasets?
Large-scale pharmacogenomic data requires sophisticated computational strategies:
- Cloud Computing Platforms: Amazon Web Services (AWS) and Google Cloud Genomics provide scalable infrastructure to handle terabyte-scale datasets [26].
- AI and Machine Learning: Tools like Google's DeepVariant utilize deep learning to identify genetic variants with greater accuracy than traditional methods [26].
- Multi-Omics Integration: Combine genomics with transcriptomics, proteomics, and metabolomics for comprehensive analysis [28] [26].
- Data Reduction Techniques: Implement efficient compression algorithms and data subsetting strategies for manageable analysis [26].
Regulatory Compliance and Data Sharing
What regulatory frameworks govern pharmacogenomic data management globally?
Table 2: Key Regulatory Frameworks for Pharmacogenomic Data
| Region | Primary Regulations | Key Requirements |
|---|---|---|
| United States | HIPAA, GINA, CLIA [29] | Privacy protection, non-discrimination, laboratory standards |
| European Union | GDPR, EMA Guidelines [23] [29] | Data protection, privacy by design, cross-border transfer rules |
| International | UNESCO Declaration, WHO Guidelines [29] | Ethical frameworks, genomic methodology implementation |
How can researchers enable secure data sharing for collaborative pharmacogenomics?
Secure data sharing requires both technical and policy solutions:
- Federated Learning: Analyze data across institutions without transferring raw genetic information [23].
- Blockchain-Based Sharing: Create immutable records of data transactions while maintaining transparency [25].
- Data Use Agreements: Establish clear terms for data access, purpose limitations, and security requirements.
- Standardized Formats: Use structured data formats like HL7's FHIR for consistent interpretation across systems [30].
Ethical Data Implementation Workflow
Table 3: Essential Pharmacogenomic Research Resources
| Resource Name | Primary Function | Key Features |
|---|---|---|
| PharmGKB | Pharmacogenomics Knowledge Repository | Clinical annotations, drug-centered pathways, VIP genes [31] |
| CPIC Guidelines | Clinical Implementation | Evidence-based gene/drug guidelines, clinical recommendations [29] [31] |
| dbSNP | Genetic Variation Database | Public archive of SNPs, frequency data, submitter handles [31] |
| DrugBank | Drug and Target Database | Drug mechanisms, interactions, target sequences [31] |
| SIEM Solutions | Security Monitoring | Real-time threat detection, compliance reporting, behavioral analytics [23] |
Frequently Asked Questions
How can we prevent genomic data breaches in multi-institutional research?
Preventing breaches requires a comprehensive approach: implement robust encryption both at rest and in transit, enforce strict access controls with multi-factor authentication, deploy AI-driven threat detection to identify unusual access patterns, utilize blockchain for data integrity, and ensure continuous monitoring with automated incident response [23]. Privacy-preserving technologies like federated learning allow analysis without exposing raw genetic information [23].
What are the solutions for managing computational demands of large-scale NGS data?
Computational challenges can be addressed through cloud computing platforms that provide scalable infrastructure [26], AI and machine learning tools for efficient variant calling [32] [26], multi-omics integration approaches [28] [26], and specialized bioinformatics pipelines for complex genomic data analysis [31]. Cloud platforms like AWS and Google Cloud Genomics can handle terabyte-scale datasets while complying with security regulations [26].
How do regulatory differences across countries impact global pharmacogenomic research?
Regulatory variations create significant challenges for international collaboration. While the United States has a comprehensive pharmacogenomics policy framework extending to clinical and industry settings [29], other regions have different requirements. Researchers must navigate varying standards for informed consent, data transfer, and privacy protection. Global harmonization efforts through organizations like WHO aim to foster international collaboration and enable secure data sharing [29].
Modern Computational Architectures and AI-Driven Analytical Methods
Leveraging Cloud Computing (AWS, Google Cloud) for Scalable Genomic Analysis
FAQs: Core Concepts and Configuration
Q1: Why should I use cloud platforms over on-premises servers for large-scale genomic studies?
Cloud platforms like AWS and Google Cloud provide virtually infinite scalability, which is essential for handling the petabyte-scale data common in chemogenomic NGS research. They offer on-demand access to High-Performance Computing (HPC) instances, eliminating the need for large capital expenditures on physical hardware and its maintenance. This allows research teams to process hundreds of genomes in parallel, reducing analysis time from weeks to hours. Furthermore, major cloud providers comply with stringent security and regulatory frameworks like HIPAA and GDPR, ensuring sensitive genomic data is handled securely [33] [34] [35].
Q2: What are the key AWS services for building a bioinformatics pipeline?
A robust bioinformatics pipeline on AWS typically leverages these core services [34]:
- Amazon S3: Provides durable and scalable object storage for raw sequencing data (FASTQ), intermediate files, and final results.
- AWS Batch: A fully managed service that dynamically provisions compute resources (Amazon EC2 instances) to run hundreds of thousands of batch jobs, such as alignment and variant calling, without managing the underlying infrastructure.
- Amazon EC2: Offers a broad selection of virtual server configurations, including compute-optimized and memory-optimized instances, tailored to different pipeline stages.
- AWS HealthOmics: A purpose-built service to store, query, and analyze genomic and other omics data, simplifying the execution of workflow languages like Nextflow and Cromwell [36].
- AWS Step Functions: Used to orchestrate and visualize the multiple steps of a genomic workflow, ensuring reliable execution and error handling [34].
Q3: What are the key Google Cloud services for rapid NGS analysis?
For rapid NGS analysis on GCP, researchers commonly use [37] [38] [39]:
- Compute Engine: Provides customizable Virtual Machines (VMs). High-CPU or GPU-accelerated machine types can be tailored for specific pipelines like Sentieon (CPU-optimized) or Parabricks (GPU-optimized).
- Cloud Storage: Serves a function similar to Amazon S3, offering a unified repository for large genomic datasets.
- Google Kubernetes Engine (GKE): Allows for the containerized deployment of bioinformatics tools, enabling scalable and portable pipeline execution.
- Batch: A fully managed service for scheduling, queueing, and executing batch jobs on Google's compute infrastructure, comparable to AWS Batch.
Q4: How can I control and predict costs when running genomic workloads in the cloud?
To manage costs effectively [34] [37]:
- Use Auto-Scaling: Leverage services like AWS Batch or GCP's instance groups to automatically scale compute resources down to zero when no jobs are queued, ensuring you only pay for what you use.
- Select the Right Storage Tier: For data that is infrequently accessed (e.g., archived raw data), use low-cost storage options like Amazon S3 Glacier or its GCP equivalents.
- Monitor and Optimize: Utilize cloud monitoring tools (e.g., Cloud Monitoring, Amazon CloudWatch) to track resource utilization. Benchmark different machine types for your specific tools to find the most cost-effective option.
- Set Budget Alerts: Define budgets and alerts within your cloud console to receive notifications before costs exceed a predefined threshold.
Troubleshooting Common Experimental Issues
Problem 1: Slow Data Transfer to the Cloud
- Symptoms: Uploading large FASTQ files from a local sequencer or data center takes days, delaying analysis.
- Solution:
- For datasets in the terabyte-to-petabyte range, use physical data transfer devices like the AWS Snow Family. You ship your data on a secure device directly to AWS, which then loads it into your S3 bucket [34].
- For large datasets transferred over the internet, use accelerated data transfer services. AWS DataSync can automate and accelerate moving data from on-premises network-attached storage (NAS) to Amazon S3, and it only transfers changed files for incremental updates [34].
- Ensure your local internet connection is not saturated by other traffic during transfers.
Problem 2: Genomic Workflow Jobs are Failing or Stuck
- Symptoms: Jobs submitted to AWS Batch or a similar orchestrator fail repeatedly or remain in a
RUNNABLEstate without starting. - Solution:
- Check Job Logs: First, examine the CloudWatch Logs for your failed job. The error message often points directly to the issue (e.g., a tool with a non-zero exit code, a missing input file in S3) [34].
- Verify Resource Allocation: Ensure the compute environment (e.g., the EC2 instance type) has sufficient vCPUs and memory for the job. A memory-intensive tool like a genome assembler will fail on an instance with insufficient RAM.
- Review IAM Permissions: Confirm that the IAM role associated with your compute environment has the necessary permissions to read from input S3 buckets and write to output S3 buckets [34].
- Inspect the Workflow Definition: For tools like Nextflow, check the
nextflow.logfile for errors in workflow definition or task execution.
Problem 3: High Costs Despite Low Compute Utilization
- Symptoms: The monthly cloud bill is unexpectedly high, but monitoring shows compute instances are idle for long periods.
- Solution:
- Implement Auto-Scaling: Configure your compute cluster (e.g., in AWS Batch) to automatically terminate instances when the job queue is empty. A common mistake is leaving a fixed-size cluster running 24/7 [40] [34].
- Use Spot Instances/Preemptible VMs: For fault-tolerant batch jobs, use AWS Spot Instances or GCP Preemptible VMs. These can reduce compute costs by 60-90% compared to on-demand prices [34].
- Optimize Storage: Apply Amazon S3 Lifecycle Policies to automatically transition old results and raw data that are no longer actively analyzed to cheaper storage classes like S3 Glacier [34].
Problem 4: Difficulty Querying Large Variant Call Datasets
- Symptoms: Researchers struggle to perform cohort-level analysis on hundreds of VCF files; queries are slow and require complex scripting.
- Solution:
- Transform your variant data into a structured, query-optimized format. Use a solution that converts VCF files into Apache Iceberg tables stored in Amazon S3 Tables. Once in this format, you can use standard SQL with Amazon Athena to run fast, complex queries across millions of variants without managing databases [36].
- Leverage AI-powered tools like an agent built on Amazon Bedrock to allow researchers to ask questions of the data in natural language, bypassing the need for SQL expertise entirely [36].
Experimental Protocols & Benchmarking
Protocol: Benchmarking Ultra-Rapid NGS Pipelines on Google Cloud Platform
This protocol outlines the steps to benchmark germline variant calling pipelines, such as Sentieon DNASeq and NVIDIA Clara Parabricks, on GCP. This is critical for chemogenomic research where rapid turnaround of genomic data can influence experimental directions [37].
1. Prerequisites:
- A GCP account with billing enabled.
- Basic familiarity with the bash shell and GCP Console.
- Valid software licenses if required (e.g., for Sentieon).
2. Virtual Machine Configuration: Benchmarking requires dedicated VMs tailored to each pipeline's hardware needs. The table below summarizes a tested configuration for cost-effective performance [37].
Table: GCP VM Configuration for NGS Pipeline Benchmarking
| Pipeline | Machine Series & Type | vCPUs | Memory | GPU | Approx. Cost/Hour |
|---|---|---|---|---|---|
| Sentieon DNASeq | N1 Series, n1-highcpu-64 |
64 | 57.6 GB | None | $1.79 |
| Clara Parabricks | N1 Series, custom (48 vCPU) |
48 | 58 GB | 1 x NVIDIA T4 | $1.65 |
3. Step-by-Step Execution on GCP:
- VM Creation: In the GCP Console, navigate to Compute Engine > VM Instances. Click "CREATE INSTANCE".
- Configuration: Name the VM and select a region/zone. For the Sentieon VM, select the
n1-highcpu-64machine type. For Parabricks, create a custom machine type with 48 vCPUs and 58 GB memory, and then add a NVIDIA T4 GPU. - Software Installation: Use the
gcloudcommand-line tool or SCP to transfer the pipeline software and license files to the VM. - Data Preparation: Download a publicly available WGS or WES FASTQ sample (e.g., from the SRA) to the VM's local SSD or attached persistent disk for fast I/O.
- Pipeline Execution: Run each pipeline with its default parameters on the same sample. Example commands for a WGS sample:
- Sentieon:
sentieon driver -t <num_threads> -i <input_fastq> -r <reference_genome> --algo ... output.vcf - Parabricks:
parabricks run --fq1 <read1.fastq> --fq2 <read2.fastq> --ref <reference.fa> --out-dir <output_dir> germline
- Sentieon:
- Data Collection: Record the total runtime, CPU utilization, and memory usage for each pipeline using GCP's monitoring tools or system commands like
time.
4. Expected Results and Analysis: The benchmark will yield quantitative data on performance and cost. The table below provides sample results from a study using five WGS samples [37].
Table: Benchmarking Results for Ultra-Rapid NGS Pipelines on GCP
| Pipeline | Average Runtime per WGS Sample | Average Cost per WGS Sample | Key Hardware Utilization |
|---|---|---|---|
| Sentieon DNASeq | ~2.5 hours | ~$4.48 | High CPU utilization, optimized for parallel processing. |
| Clara Parabricks | ~2.0 hours | ~$3.30 | High GPU utilization, leveraging parallel processing on the graphics card. |
Workflow Diagram: End-to-End Scalable Genomic Analysis
The following diagram illustrates the logical flow and key cloud services involved in a scalable genomic analysis pipeline, from data ingestion to final interpretation.
The Scientist's Toolkit: Research Reagent Solutions
This table details the essential software, services, and data resources required to conduct large-scale genomic analysis in the cloud.
Table: Essential Resources for Cloud-Based Genomic Analysis
| Category | Item | Function / Purpose |
|---|---|---|
| Core Analysis Software | Sentieon DNASeq | A highly optimized, CPU-based pipeline for secondary analysis (alignment, deduplication, variant calling) that provides results equivalent to GATK Best Practices with significantly faster speed [37]. |
| NVIDIA Clara Parabricks | A GPU-accelerated suite of tools for secondary genomic analysis, leveraging parallel processing to dramatically reduce runtime for tasks like variant calling [37]. | |
| GATK (Genome Analysis Toolkit) | A industry-standard toolkit for variant discovery in high-throughput sequencing data, often run within cloud environments [33]. | |
| Workflow Orchestration | Nextflow | A workflow manager that enables scalable and reproducible computational pipelines. It seamlessly integrates with cloud platforms like AWS and GCP, allowing pipelines to run across thousands of cores [34] [35]. |
| Cromwell | An open-source workflow execution engine that supports the WDL (Workflow Description Language) and is optimized for cloud environments [33] [34]. | |
| Cloud Services | AWS HealthOmics | A purpose-built service to store, query, and analyze genomic and other omics data, with native support for workflow languages like Nextflow and WDL [36]. |
| Amazon S3 / Google Cloud Storage | Durable, scalable, and secure object storage for housing input data, intermediate files, and final results from genomic workflows [34] [39]. | |
| AWS Batch / GCP Batch | Fully managed batch computing services that dynamically provision the optimal quantity and type of compute resources to run jobs [34] [39]. | |
| Reference Data | Reference Genomes (GRCh38) | The standard reference human genome sequence used as a baseline for aligning sequencing reads and calling variants. |
| ClinVar | A public archive of reports detailing the relationships between human genetic variations and phenotypes, with supporting evidence used for annotating and interpreting variants [36]. | |
| Variant Effect Predictor (VEP) | A tool that determines the functional consequences of genomic variants (e.g., missense, synonymous) on genes, transcripts, and protein sequences [36]. |
Technical Support & Troubleshooting Hub
This hub provides targeted support for researchers addressing the computational demands of large-scale chemogenomic NGS data. The guides below focus on specific, high-impact issues in variant calling and polygenic risk scoring.
DeepVariant Troubleshooting Guide
Q1: The pipeline fails with a TensorFlow error: "Check failed: -1 != path_length (-1 vs. -1)" and "Fatal Python error: Aborted". What should I do?
- Problem Overview: This is a known environment or dependency conflict issue, often occurring during the
call_variantsstep when the model loads [41]. It can be related to the TensorFlow library version or its interaction with the underlying operating system. - Diagnostic Steps:
- Check the full error log for any preceding warnings, such as end-of-life messages for libraries like TensorFlow Addons [41].
- Verify that the paths to all input files (BAM, FASTA) are correct and accessible within your container environment.
- Solution:
- Primary Action: Use a supported and updated version of DeepVariant. The error was reported on DeepVariant v1.6.1 [41]. Check the official repository for newer releases that contain bug fixes.
- Alternative Approach: If updating is not possible, ensure you are using a compatible and stable version of TensorFlow as required by your specific DeepVariant version. The Singularity container should ideally manage these dependencies.
- Prevention: Always use the standard Docker or Singularity images provided by the DeepVariant team to ensure a consistent and tested software environment.
Q2: I get a "ValueError: Reference contigs span ... bases but only 0 bases (0.00%) were found in common". Why does this happen?
- Problem Overview: This critical error occurs when the reference genome used to create the input BAM file does not match the reference genome provided to DeepVariant [42]. The tool detects no common genomic contigs between the two files.
- Diagnostic Steps:
- Use
samtools view -H your_file.bamto inspect the@SQlines (contig names) in your BAM header. - Use
grep ">" your_reference.fastato see the contig names in your reference FASTA file. - Compare the outputs; you will likely find mismatches in contig names (e.g., "chr1" vs. "1") [42].
- Use
- Solution:
- Immediate Fix: Ensure consistency. Re-align your sequencing reads using the correct
your_reference.fastafile, or obtain the correct reference genome that matches your BAM file's build. - Troubleshooting Tip: This is a common issue when switching between different human reference builds (like hg19 vs. GRCh38) or when working with non-human data. Always double-check reference genome versions at the start of your project [42].
- Immediate Fix: Ensure consistency. Re-align your sequencing reads using the correct
Q3: The "make_examples" step is extremely slow or runs out of memory. How can I optimize this?
- Problem Overview: The
make_examplesstage is the most computationally intensive and memory-hungry part of DeepVariant, requiring significant resources for large genomes and high-coverage data [43]. - Diagnostic Steps:
- Monitor your system resources (e.g., using
toporhtop) during the job to confirm it is memory-bound (slowed by swapping) or CPU-bound. - Check the logging output from DeepVariant to see the number of shards being processed and their progress.
- Monitor your system resources (e.g., using
- Solution:
- Increase Memory: The memory requirement for
make_examplesis approximately 10-15x the size of your input BAM file [43]. For a 30 GB BAM file, allocate 300-450 GB of RAM. - Parallelize the Task: Use the
--num_shardsoption to break the work into multiple parallel tasks. For example, on a cluster with 32 cores, you can set--num_shards=32to significantly speed up processing [41]. - Adjust Region: Use the
--regionsflag with a BED file to process only specific genomic intervals of interest, which is highly useful for targeted sequencing or exome data [43].
- Increase Memory: The memory requirement for
Table: Common DeepVariant Errors and Solutions
| Error Symptom | Root Cause | Solution |
|---|---|---|
| TensorFlow "path_length" error & crash [41] | Dependency or environment conflict | Use an updated, stable DeepVariant version and official container image. |
| "0 bases in common" between reference & BAM [42] | Reference genome mismatch | Re-align FASTQ or obtain the correct reference to ensure contig names match. |
| make_examples slow/OOM (Out-of-Memory) | High memory demand for large BAMs [43] | Allocate 10-15x BAM file size in RAM; use --num_shards for parallelization [41] [43]. |
| Pipeline fails on non-human data | Default settings for human genomes | Ensure reference and BAM are consistent; no specific model change is typically needed for non-human WGS [42]. |
Polygenic Risk Score (PRS) Implementation & FAQ
Q1: How do I choose the right Polygenic Risk Score for my study on a specific disease?
- Problem Overview: There is no single, universally standardized PRS for most diseases. Different scores, built with varying methods and GWAS summary statistics, can classify individuals into different risk categories, leading to discordant results [44].
- Guidelines:
- Consult the Polygenic Score Catalog (PGS Catalog): This is a primary, regularly updated repository of published PRS for a wide range of diseases and traits [44].
- Evaluate Performance Metrics: Prioritize scores that have been validated in independent cohorts. Look for metrics like Area Under the Curve (AUC), which indicates the score's ability to discriminate between cases and controls. For example, a breast cancer PRS combined with clinical factors achieved an AUC of 0.677, a significant improvement over clinical factors alone (AUC 0.536) [44].
- Check Ancestry Match: The vast majority of GWAS data (~91%) is from individuals of European ancestry [44]. A PRS developed in one ancestry group often has degraded performance and may overestimate risk in other ancestry groups [44]. Always check the ancestral background of the development cohort and seek out ancestry-matched or multi-ancestry PRS (MA-PRS) where possible.
Q2: What are the key computational and data management challenges when calculating PRS for a large cohort?
- Problem Overview: PRS calculation itself is less computationally intense than variant calling, but it depends on the management of large genomic datasets and the integration of multiple data sources [3].
- Key Challenges & Solutions:
- Data Transfer and Storage: Moving terabytes of genotyping or sequencing data (e.g., VCF files) is a major bottleneck. The most efficient solution is often to house data centrally in the cloud and bring computations to the data [3].
- Standardization of Data Formats: Working with data from different centers in different formats wastes time. Using standardized file formats (e.g., VCF, BCF) and interoperable toolkits (e.g., PLINK, bcftools) is crucial [3] [45].
- Integration with Clinical Data: The most accurate risk models combine PRS with clinical risk factors [44] [46]. This requires robust data pipelines to merge and manage genomic and clinical data securely.
Table: Key Considerations for Clinical PRS Implementation
| Consideration | Challenge | Current Insight & Strategy |
|---|---|---|
| Ancestral Diversity | Poor performance in non-European populations due to GWAS bias [44]. | Use ancestry-informed or MA-PRS; simple corrections can improve accuracy in specific groups [44]. |
| Risk Communication | Potential for misunderstanding complex genetic data [46]. | Communicate absolute risk (e.g., 17% lifetime risk) instead of relative risk (1.5x risk) [44]. |
| Clinical Integration | How to incorporate PRS into existing clinical workflows and decision-making [46]. | Combine PRS with monogenic variants and clinical factors in integrated risk models (e.g., CanRisk) [44]. |
| Regulatory Standardization | No universal standard for PRS development or validation [44]. | Rely on well-validated scores from peer-reviewed literature and the PGS Catalog; transparency in methods is key [44]. |
The Scientist's Toolkit
Table: Essential Research Reagents & Computational Tools
| Item | Function & Application | Notes |
|---|---|---|
| DeepVariant | A deep learning-based variant calling pipeline that converts aligned sequencing data (BAM) into variant calls (VCF/GVCF) [41] [43]. | Best run via Docker/Singularity for reproducibility. Model types: WGS, WES, PacBio [43]. |
| Bcftools | A versatile suite of utilities for processing, filtering, and manipulating VCF and BCF files [45]. | Used for post-processing variant calls, e.g., bcftools filter to remove low-quality variants [45]. |
| SAM/BAM Files | The standard format for storing aligned sequencing reads [10]. | Must be sorted and indexed (e.g., with samtools sort/samtools index) for use with most tools, including DeepVariant [45]. |
| VCF/BCF Files | The standard format for storing genetic variants [45]. | BCF is the compressed, binary version, which is faster to process [45]. |
| Polygenic Score (PGS) Catalog | A public repository of published polygenic risk scores [44]. | Essential for finding and comparing validated PRS for specific diseases and traits. |
| Reference Genome (FASTA) | The reference sequence to which reads are aligned and variants are called against [42]. | Critical that the version (e.g., GRCh38, hs37d5) matches the one used for read alignment [43] [42]. |
Experimental Protocol: A Typical Variant Calling Workflow with DeepVariant and Bcftools
This protocol details the steps from an aligned BAM file to a filtered set of high-confidence variants, integrating both DeepVariant and bcftools for a robust analysis [45].
1. Input Preparation
- Inputs: A coordinate-sorted BAM file and its index (
.bai), the reference genome in FASTA format and its index (.fai). - Software: DeepVariant (via Docker/Singularity), Bcftools.
2. Variant Calling with DeepVariant
- Run DeepVariant using the command appropriate for your data type (e.g.,
--model_type=WGSfor whole-genome data). This generates a VCF file containing all variant calls and reference confidence scores [41] [43]. - Example Command:
3. Post-processing and Filtering with Bcftools
- Step 1: Normalize Variants. Left-aligns and normalizes indels, which is critical for accurate counting and filtering. This step can merge and realign variants [45].
- Step 2: Apply Filters. Remove low-quality variants using hard filters. The specific thresholds should be tuned for your dataset. This command removes variants with a quality score below 30 or a read depth below 15 [45].
4. Output Analysis
- The final output,
filtered_variants.bcf, contains your high-confidence variant set. You can obtain a variant count withbcftools view -H filtered_variants.bcf | wc -l[45].
Workflow and Relationship Diagrams
DeepVariant Troubleshooting Logic
PRS Implementation Workflow
Multi-omics research represents a transformative approach in biological sciences that integrates data from various molecular layers—such as genomics, transcriptomics, and proteomics—to provide a comprehensive understanding of biological systems. The primary goal is to study complex biological processes holistically by combining these data types to highlight the interrelationships of biomolecules and their functions [47]. This integrated approach helps bridge the information flow from one omics level to another, effectively narrowing the gap from genotype to phenotype [47].
The analysis of multi-omics data, especially when combined with clinical information, has become crucial for deriving meaningful insights into cellular functions. Integrated approaches can combine individual omics data either sequentially or simultaneously to understand molecular interplay [47]. By studying biological phenomena holistically, these integrative approaches can significantly improve the prognostics and predictive accuracy of disease phenotypes, ultimately contributing to better treatment and prevention strategies [47].
Key Data Repositories for Multi-Omics Research
Several publicly available databases provide multi-omics datasets that researchers can leverage for integrated analyses. The table below summarizes the major repositories:
Table: Major Multi-Omics Data Repositories
| Repository Name | Primary Focus | Available Data Types |
|---|---|---|
| The Cancer Genome Atlas (TCGA) [47] | Cancer | RNA-Seq, DNA-Seq, miRNA-Seq, SNV, CNV, DNA methylation, RPPA |
| Clinical Proteomic Tumor Analysis Consortium (CPTAC) [47] | Cancer (proteomics corresponding to TCGA cohorts) | Proteomics data |
| International Cancer Genomics Consortium (ICGC) [47] | Cancer | Whole genome sequencing, somatic and germline mutation data |
| Cancer Cell Line Encyclopedia (CCLE) [47] | Cancer cell lines | Gene expression, copy number, sequencing data, pharmacological profiles |
| Molecular Taxonomy of Breast Cancer International Consortium (METABRIC) [47] | Breast cancer | Clinical traits, gene expression, SNP, CNV |
| TARGET [47] | Pediatric cancers | Gene expression, miRNA expression, copy number, sequencing data |
| Omics Discovery Index (OmicsDI) [47] | Consolidated datasets from multiple repositories | Genomics, transcriptomics, proteomics, metabolomics |
Multi-Omics Integration Strategies and Tools
Integration strategies are broadly categorized based on whether the data is matched (profiled from the same cell) or unmatched (profiled from different cells) [48]. The choice of integration method depends heavily on this distinction.
Types of Integration
- Matched Integration: Also known as vertical integration, this approach merges data from different omics within the same set of samples, using the cell as the anchor to bring these omics together [48]. This is possible with technologies that profile multiple distinct modalities from within a single cell.
- Unmatched Integration: Referred to as diagonal integration, this strategy integrates different omics from different cells or different studies [48]. Since the cell cannot serve as an anchor, these methods project cells into a co-embedded space or non-linear manifold to find commonality between cells in the omics space.
- Mosaic Integration: This alternative to diagonal integration is used when experimental designs have various combinations of omics that create sufficient overlap across samples [48]. Tools like COBOLT and MultiVI can integrate data in this mosaic fashion.
Computational Tools for Integration
A wide array of computational tools has been developed to address multi-omics integration challenges. The table below categorizes these tools based on their integration capacity:
Table: Multi-Omics Integration Tools and Methodologies
| Tool Name | Year | Methodology | Integration Capacity | Data Types Supported |
|---|---|---|---|---|
| Matched Integration Tools | ||||
| MOFA+ [48] | 2020 | Factor analysis | Matched | mRNA, DNA methylation, chromatin accessibility |
| totalVI [48] | 2020 | Deep generative | Matched | mRNA, protein |
| Seurat v4 [48] | 2020 | Weighted nearest-neighbour | Matched | mRNA, spatial coordinates, protein, accessible chromatin |
| SCENIC+ [48] | 2022 | Unsupervised identification model | Matched | mRNA, chromatin accessibility |
| Unmatched Integration Tools | ||||
| Seurat v3 [48] | 2019 | Canonical correlation analysis | Unmatched | mRNA, chromatin accessibility, protein, spatial |
| GLUE [48] | 2022 | Variational autoencoders | Unmatched | Chromatin accessibility, DNA methylation, mRNA |
| LIGER [48] | 2019 | Integrative non-negative matrix factorization | Unmatched | mRNA, DNA methylation |
| Pamona [48] | 2021 | Manifold alignment | Unmatched | mRNA, chromatin accessibility |
Experimental Workflows and Visualization
The integration of multiple omics data types follows specific computational workflows that vary based on the nature of the data and the research objectives. The diagram below illustrates a generalized workflow for multi-omics data integration:
Diagram: Multi-Omics Integration Workflow showing the process from raw data to biological insights.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful multi-omics research requires specific computational tools and resources. The table below details essential components of the multi-omics research toolkit:
Table: Essential Research Reagents and Computational Solutions for Multi-Omics Research
| Tool/Resource | Function/Purpose | Examples/Formats |
|---|---|---|
| Data Storage Formats | Standardized formats for efficient data storage and processing | FASTQ, BAM, VCF, HDF5 [10] |
| Workflow Management | Maintain reproducibility, portability, and scalability in analysis | Nextflow, Snakemake, Cromwell [10] |
| Container Technology | Ensure consistent computational environments across platforms | Docker, Singularity, Podman [10] |
| Cloud Computing Platforms | Provide scalable computational resources for large datasets | AWS, Google Cloud Platform, Microsoft Azure [3] [10] |
| Quality Control Tools | Assess data quality before integration | FastQC, MultiQC, Qualimap |
Troubleshooting Guides and FAQs
Data Management and Preprocessing Issues
Q: How can I handle the large-scale data transfer and storage challenges associated with multi-omics studies?
A: Large multi-omics datasets present significant data transfer challenges. Network speeds are often too slow to routinely transfer terabytes of data over the web [3]. Efficient solutions include:
- Centralized Data Housing: House datasets centrally and bring high-performance computing to the data [3]
- Cloud-Based Solutions: Utilize cloud platforms like Google Cloud Platform and Amazon Web Services, which host major datasets like the Sequencing Read Archive without end-user charges for data access within the same cloud region [10]
- Data Format Optimization: Use compressed and optimized file formats like CRAM instead of BAM to reduce storage footprint [10]
Q: How do I address the issue of heterogeneous data formats from different omics technologies?
A: Data format heterogeneity is a common challenge in multi-omics integration. Different centers generate data in different formats, and analysis tools often require specific formats [3]. Solutions include:
- Develop interoperable sets of analysis tools that can be run on different computational platforms
- Create analysis pipelines that can stitch together tools with different format requirements
- Utilize standardized preprocessing workflows for each data type before integration
- Employ data harmonization techniques to make different omics layers comparable
Integration Methodology Challenges
Q: What should I do when my multi-omics data has significant missing values across modalities?
A: Missing values are a common challenge in multi-omics datasets, particularly when integrating technologies with different sensitivities [48]. Consider these approaches:
- Imputation Methods: Use sophisticated imputation algorithms specifically designed for multi-omics data
- Deep Generative Models: Employ variational autoencoders (VAEs) that have demonstrated effectiveness for data imputation and augmentation in multi-omics contexts [49]
- Mosaic Integration Approaches: Utilize tools like COBOLT and MultiVI that are designed to handle datasets with varying combinations of omics [48]
- Prior Knowledge Integration: Implement methods like GLUE that use prior biological knowledge to anchor features and handle missing data [48]
Q: How can I choose between matched and unmatched integration methods for my specific dataset?
A: The choice depends on your experimental design and available data:
- Use Matched Integration when you have profiled multiple modalities from the same cells or samples [48]. This is ideal as the cell itself serves as a natural anchor.
- Use Unmatched Integration when different modalities come from different cells, even if they're from the same sample or tissue [48]. These methods project cells into a co-embedded space to find commonality.
- Consider Mosaic Integration when your experimental design includes various combinations of omics that create sufficient overlap across samples [48].
Computational and Analytical Challenges
Q: My multi-omics integration analysis is computationally intensive and taking too long. What optimization strategies can I implement?
A: Computational intensity is a significant challenge in multi-omics integration. Optimization strategies include:
- Understanding Algorithm Nature: Determine if your analysis is network-bound, disk-bound, memory-bound, or computationally bound to target resources effectively [3]
- Parallelization: Identify opportunities for parallelizing analysis algorithms across multiple computer processors [3]
- Heterogeneous Computing: Utilize specialized hardware accelerators like GPUs for specific computationally intense operations [3]
- Cloud and HPC Resources: Leverage high-performance computing systems or cloud-based solutions that can scale resources according to computational demands [10]
Q: How can I ensure my multi-omics integration results are biologically meaningful and not just computational artifacts?
A: Validation is crucial for multi-omics findings:
- Biological Replication: Ensure findings are consistent across multiple biological replicates
- Functional Validation: Plan follow-up experiments (e.g., CRISPR screens, pharmacological interventions) to test predictions
- Prior Knowledge Integration: Use tools that incorporate existing biological knowledge (e.g., GLUE) to ground results in established biology [48]
- Multiple Method Comparison: Test key findings using different integration methodologies to ensure robustness
- Clinical Correlation: When possible, correlate multi-omics findings with clinical outcomes or phenotypic measurements
Advanced Integration Techniques and Future Directions
The field of multi-omics integration continues to evolve with emerging computational approaches. Deep learning methods, particularly graph neural networks and generative adversarial networks, are showing promise for effectively synthesizing and interpreting multi-omics data [50]. Variational autoencoders have been widely used for data imputation, joint embedding creation, and batch effect correction [49].
Future directions include the development of foundation models for biology and the integration of emerging data modalities [49]. Large language models may also enhance multi-omics analysis through automated feature extraction, natural language generation, and knowledge integration [50]. However, these advanced approaches require substantial computational resources and careful model tuning, highlighting the need for ongoing innovation and collaboration in the field [50].
The Rise of Single-Cell and Spatial Transcriptomics in Understanding Tumor Heterogeneity and Drug Resistance
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
FAQ 1: What is the key difference between single-cell RNA sequencing (scRNA-seq) and spatial transcriptomics, and when should I use each?
scRNA-seq provides high-resolution gene expression data for individual cells but requires tissue dissociation, which destroys the native spatial context of cells within the tissue. Spatial transcriptomics technologies preserve the original location of transcripts, allowing researchers to map gene expression within the intact tissue architecture. Use scRNA-seq when you need to identify novel cell subpopulations, reconstruct developmental trajectories, or perform deep characterization of cellular heterogeneity. Implement spatial transcriptomics when investigating cellular interactions, tumor microenvironment organization, or region-specific biological processes where spatial context is critical [51] [52].
FAQ 2: What are the primary computational challenges when working with single-cell and spatial transcriptomic data?
The table below summarizes the key computational challenges and their implications:
| Challenge | Description | Impact |
|---|---|---|
| Data Volume | A single experiment can generate terabytes of raw sequencing data | Requires substantial storage infrastructure and data transfer solutions [3] |
| Data Transfer & Management | Network speeds often too slow for routine transfer of large datasets | Necessitates centralized data housing or physical storage drive shipment [3] |
| Format Standardization | Lack of industry-wide standards for raw sequencing data across platforms | Requires format conversion and tool adaptation, increasing analysis time [3] |
| Computational Intensity | Analysis algorithms (e.g., trajectory inference, network reconstruction) are computationally demanding | Requires high-performance computing (HPC) resources or specialized hardware [52] |
| Data Integration | Combining multiple data types (DNA, RNA, protein, spatial coordinates) poses modeling challenges | Demands advanced computational approaches for multi-omics integration [3] |
FAQ 3: How can I identify malignant cells from tumor scRNA-seq data?
A standard methodology involves:
- Isolate Epithelial Cells: First, subset epithelial cells from your complete cell atlas using canonical markers.
- Copy Number Variation (CNV) Analysis: Use tools like inferCNV to analyze chromosomal copy number variations, with normal epithelial cells from the same tissue as reference.
- CNV Score Clustering: Generate a CNV score matrix and perform unsupervised K-means clustering to partition cells into malignant (high CNV) or normal (low CNV) clusters based on CNV-driven cluster purity [52].
FAQ 4: What are common biomarkers of therapy resistance identified through transcriptomics?
The following table summarizes key resistance biomarkers revealed through transcriptomic profiling:
| Biomarker | Functional Role | Therapeutic Context | Reference |
|---|---|---|---|
| CCNE1 | Cyclin E1, promotes cell cycle progression | CDK4/6 inhibitor resistance in breast cancer | [53] |
| RB1 | Tumor suppressor, cell cycle regulator | CDK4/6 inhibitor resistance when downregulated | [53] |
| CDK6 | Cyclin-dependent kinase 6 | Upregulated in CDK4/6-resistant models | [53] |
| FAT1 | Atypical cadherin tumor suppressor | Downregulated in multiple resistant models | [53] |
| Interferon Signaling | Immune response pathway | Heterogeneous activation in palbociclib resistance | [53] |
| ESR1 | Estrogen receptor alpha | Frequently downregulated in resistant states | [53] |
Troubleshooting Experimental Protocols
Issue 1: Poor Cell Separation or Low Quality in scRNA-seq Data
Symptoms: Low number of genes detected per cell (<2,000), high mitochondrial gene percentage, poor separation in UMAP visualizations.
Solutions:
- Implement rigorous quality control filtering: remove cells with <250 genes detected, UMI counts >15,000, or mitochondrial gene percentage >20% [52].
- Use Scrublet (v0.2.3) or similar tools to identify and remove doublets.
- For cell annotation, employ a two-step approach: initial classification with SingleR and CellTypist using canonical markers, followed by refinement through secondary dimensionality reduction and iterative annotation [52].
Experimental Workflow:
Issue 2: Challenges in Spatial Transcriptomics Data Integration
Symptoms: Difficulty aligning spatial expression patterns with cell type identities, poor integration with complementary scRNA-seq datasets.
Solutions:
- For spatial data quality control: retain spots with ≥10 genes detected, UMI counts >20, and mitochondrial gene ratio <25% [52].
- Implement memory-efficient processing by subsampling 50,000 points using SketchData for large datasets.
- Use RCTD (v2.2.1) for cell type deconvolution with scRNA-seq data as reference.
- Apply AUCell (v1.24.0) to compute spatial enrichment scores for gene sets and visualize MCEP distribution patterns across tissue sections [52].
Spatial Data Analysis Pipeline:
Issue 3: Managing Large-Scale Data Storage and Computational Workflows
Symptoms: Inability to process large datasets efficiently, difficulty reproducing analyses, high computational costs.
Solutions:
- Adopt a multi-cloud strategy to balance cost, performance, and customizability [10].
- Implement workflow description languages and container technologies (e.g., Docker, Singularity) to ensure reproducibility and portability.
- For extremely large datasets, consider distributed storage solutions and high-performance computing resources capable of parallel processing [3].
- Utilize established data formats (FASTQ, BAM, VCF) and processing tools (bwa) that have become de facto standards in the field [10].
The Scientist's Toolkit: Essential Research Reagents & Computational Solutions
| Category | Item/Reagent | Function/Application |
|---|---|---|
| Wet Lab Reagents | Chromium Next GEM Chip | Single-cell partitioning in 10x Genomics platform |
| Visium Spatial Gene Expression Slide | Spatial transcriptomics capture surface | |
| Enzyme Digestion Mix | Tissue dissociation for single-cell suspension | |
| Barcoded Oligonucleotides | Cell and transcript labeling for multiplexing | |
| Computational Tools | CellRanger | Processing 10x Genomics single-cell data |
| Seurat (v5.1.0) | scRNA-seq data analysis and integration | |
| inferCNV (v1.18.1) | Identification of malignant cells via copy number variation | |
| Monocle3 (v1.3.5) | Pseudotime trajectory analysis | |
| NicheNet (v2.1.5) | Modeling intercellular communication networks | |
| Harmony (v0.1.0) | Batch effect correction across datasets | |
| Analysis Algorithms | cNMF (consensus NMF) | Identification of gene expression programs |
| UMAP | Dimensionality reduction and visualization | |
| RCTD (v2.2.1) | Cell type deconvolution in spatial data |
Advanced Computational Methodologies
Malignant Cell Expression Program (MCEP) Analysis
The consensus non-negative matrix factorization (cNMF) algorithm enables decomposition of malignant cell transcriptomes into distinct expression programs:
- Identify High-Variance Genes: Perform 200 iterations of 75% subsampling, retaining genes recurrently ranked among top 2,500 highly variable genes in ≥150 iterations [52].
- Matrix Factorization: Apply NMF to decompose the expression matrix into gene expression programs (GEPs) and their corresponding activity scores.
- Optimal Program Determination: Determine the optimal number of GEPs by minimizing reconstruction error and maximizing stability via elbow plot analysis.
- High-Weight Gene Selection: Rank genes by absolute weights in the cNMF gene coefficient matrix and select top 100 genes per program for downstream analysis [52].
Transcriptional Program Discovery:
Intercellular Crosstalk Network Construction
To investigate how malignant cell programs influence the tumor microenvironment:
- Identify Trajectory-Associated Genes: Use Monocle3's graph_test function (Moran's |I| > 0.25, q < 0.05) to find genes associated with immune/stromal cell development [52].
- Select Candidate Regulators: Choose top 100 weighted genes from each MCEP as potential regulators.
- Predict Ligand-Target Interactions: Apply NicheNet to generate regulatory potential matrices linking malignant cell regulators with target gene sets in immune/stromal cells.
- Network Visualization: Construct final interaction networks in Cytoscape using thresholded matrices for edge weighting, eliminating potential interactions in the lowest tertile of regulatory scores to remove spurious associations [52].
Troubleshooting Guides
Troubleshooting Common Data Analysis Issues
Problem: Low or No Significant Gene Enrichment
- Potential Cause: Insufficient selection pressure during the screening process, leading to a weak phenotypic signal and low signal-to-noise ratio [54].
- Solution: Increase the selection pressure (e.g., higher drug concentration, more stringent nutrient deprivation) and/or extend the duration of the screening. This allows for greater enrichment of positively selected cells [54].
Problem: High Variability Between sgRNAs Targeting the Same Gene
- Potential Cause: The editing efficiency of the CRISPR/Cas9 system is highly dependent on the intrinsic properties of each sgRNA sequence. Some sgRNAs naturally exhibit little to no activity [54].
- Solution: Design and use libraries with at least 3-4 sgRNAs per gene. This strategy mitigates the impact of individual sgRNA performance variability and provides more robust, consistent results for identifying gene function [54].
Problem: Large Loss of sgRNAs from the Library
- Potential Cause 1: If the loss occurs in the initial library cell pool, it indicates insufficient library representation and coverage [54].
- Solution: Re-establish the CRISPR library cell pool with a higher number of cells to ensure adequate coverage (>200x) and maintain >99% library representation [54].
- Potential Cause 2: If the loss occurs after screening in the experimental group, it may be due to excessive selection pressure [54].
- Solution: Titrate the selection pressure to a less stringent level to avoid the depletion of an overwhelming number of cells.
Problem: Unexpected Positive/Negative Log-Fold Change (LFC) Values
- Potential Cause: When using algorithms like Robust Rank Aggregation (RRA), the gene-level LFC is calculated as the median of its sgRNA-level LFCs. Extreme values from a few individual sgRNAs can skew the median, resulting in a positive LFC in a negative screen (where depletion is expected) or vice-versa [54].
- Solution: Inspect the LFC values for individual sgRNAs within a gene of interest. The gene-level metric can be misleading if a subset of sgRNAs behaves anomalously [54].
Problem: Low Mapping Rate in Sequencing Data
- Potential Cause: A portion of the sequencing reads cannot be aligned to the sgRNA reference library.
- Solution: A low mapping rate itself does not compromise reliability, as downstream analysis uses only successfully mapped reads. The critical factor is that the absolute number of mapped reads is sufficient to maintain the recommended sequencing depth (≥200x coverage) [54]. Focus on ensuring sufficient total data volume rather than the mapping rate percentage.
Troubleshooting Experimental Design Issues
Problem: Low Editing Efficiency
- Potential Cause 1: Suboptimal guide RNA (gRNA) design [55].
- Potential Cause 2: Inefficient delivery of CRISPR components [55].
- Solution: Optimize the delivery method (e.g., electroporation, lipofection, viral vectors) for your specific cell type. Confirm the delivery efficiency through control experiments [55].
- Potential Cause 3: Inadequate expression of Cas9 or gRNA [55].
- Solution: Use a promoter that is highly active in your chosen cell type to drive Cas9 and gRNA expression. Consider codon-optimizing the Cas9 gene for your host organism and verify the quality of your plasmid DNA or mRNA [55].
Problem: High Off-Target Effects
- Potential Cause: The Cas9 enzyme cuts at unintended sites in the genome with sequence similarity to the gRNA [55].
- Solution:
- Design highly specific gRNAs using online tools that predict potential off-target sites [55].
- Employ high-fidelity Cas9 variants (e.g., eSpCas9, SpCas9-HF1) engineered to reduce off-target cleavage [55] [57].
- Utilize modified gRNAs, such as hybrid guides with DNA substitutions, which have been shown to dramatically reduce off-target editing while maintaining therapeutic efficacy [58].
Frequently Asked Questions (FAQs)
Q1: How much sequencing data is required per sample for a CRISPR screen? It is generally recommended to achieve a sequencing depth of at least 200x coverage. The required data volume can be estimated with the formula: Required Data Volume = Sequencing Depth × Library Coverage × Number of sgRNAs / Mapping Rate. For a typical human whole-genome knockout library, this often translates to approximately 10 Gb of data per sample [54].
Q2: How can I determine if my CRISPR screen was successful? The most reliable method is to include well-validated positive-control genes in your library. If the sgRNAs targeting these controls show significant enrichment or depletion in the expected direction, it strongly indicates effective screening conditions. In the absence of known controls, you can assess screening performance by examining the degree of cellular response to selection pressure and analyzing the distribution and log-fold change of sgRNA abundance in bioinformatics outputs [54].
Q3: What are the most commonly used computational tools for CRISPR screen data analysis? The MAGeCK (Model-based Analysis of Genome-wide CRISPR-Cas9 Knockout) tool is currently the most widely used. It incorporates two primary statistical algorithms [54]:
- RRA (Robust Rank Aggregation): Best suited for experimental designs with a single treatment group and a single control group.
- MLE (Maximum Likelihood Estimation): Supports the joint analysis of multiple experimental conditions, providing improved statistical power for complex, multi-group comparisons.
Q4: Should I select candidate genes based on RRA score ranking or by combining LFC and p-value?
- RRA Score Ranking: The RRA algorithm integrates multiple metrics into a single composite score, providing a comprehensive gene ranking. Genes with higher ranks are more likely to be true hits, though it doesn't prescribe a clear cutoff [54].
- LFC and p-value Combination: This common biological approach allows for explicit threshold setting (e.g., LFC > 2, p-value < 0.05) but may yield a higher proportion of false positives as it relies on only two parameters [54].
- Recommendation: Prioritize RRA rank-based selection as your primary strategy for identifying target genes, as it is generally more robust [54].
Q5: What is the difference between negative and positive screening?
- Negative Screening: Applies a relatively mild selection pressure. The goal is to identify loss-of-function genes whose knockout causes cell death or reduced viability. This is done by detecting the depletion of corresponding sgRNAs in the surviving cell population [54].
- Positive Screening: Applies strong selection pressure, causing most cells to die. The goal is to identify genes whose disruption confers a selective advantage (e.g., drug resistance). This is done by detecting the enrichment of sgRNAs in the small number of surviving cells [54].
Essential Research Reagent Solutions
Table 1: Key research reagents and their functions in CRISPR screening.
| Reagent / Tool | Function | Key Considerations |
|---|---|---|
| sgRNA Library | A pooled collection of thousands of single-guide RNAs targeting genes across the genome for large-scale functional screens [59] [60]. | Libraries can be genome-wide or focused. Include 3-4 sgRNAs per gene to mitigate performance variability [54]. |
| Cas9 Nuclease | The enzyme that creates a double-strand break in DNA at the location specified by the gRNA [60] [57]. | Use high-fidelity variants (e.g., eSpCas9) to minimize off-target effects. Can be delivered as plasmid, mRNA, or protein [55] [57]. |
| dCas9-Effector Fusions (CRISPRi/a) | Catalytically "dead" Cas9 fused to repressor (KRAB) or activator (VP64, VPR) domains to silence (CRISPRi) or activate (CRISPRa) gene transcription without cutting DNA [60] [57]. | Allows for gain-of-function and loss-of-function studies without introducing DNA breaks, reducing toxicity [60]. |
| Base Editors | Fusion of a catalytically impaired Cas protein to a deaminase enzyme, enabling direct, irreversible conversion of one base pair into another (e.g., C•G to T•A) without double-strand breaks [56] [61]. | Useful for screening the functional impact of single-nucleotide variants. Limited by a specific "editing window" [60]. |
| Viral Delivery Vectors | Lentiviruses or other viruses used to efficiently deliver the sgRNA library into a large population of cells [60]. | Critical for achieving high transduction efficiency. The viral titer must be optimized to ensure each cell receives only one sgRNA. |
| MAGeCK Software | A comprehensive computational pipeline for analyzing CRISPR screen data, identifying positively and negatively selected genes [54]. | The industry standard. Supports both RRA and MLE algorithms for different experimental designs [54]. |
Quantitative Data Specifications
Table 2: Key quantitative metrics for ensuring a high-quality CRISPR screen.
| Parameter | Recommended Value | Purpose & Rationale |
|---|---|---|
| Sequencing Depth | ≥ 200x coverage per sample [54] | Ensures each sgRNA in the library is sequenced a sufficient number of times for accurate quantification. |
| Library Coverage | > 99% representation [54] | Ensures that almost all sgRNAs in the library are present in the initial cell pool, preventing loss of target genes before selection. |
| sgRNAs per Gene | 3-4 (minimum) [54] | Mitigates the impact of variable performance between individual sgRNAs, increasing the robustness of results. |
| Cell Coverage | 500-1000 cells per sgRNA [60] | Ensures sufficient representation of each sgRNA in the population to avoid stochastic loss. |
| Replicate Correlation (Pearson) | > 0.8 [54] | Indicates high reproducibility between biological replicates. If lower, pairwise analysis may be required. |
Experimental Protocol: A Standard CRISPR-KO Screen Workflow
1. Library Design and Selection
- Select a genome-wide or sub-library of genes relevant to your phenotype.
- Design a minimum of 3-4 sgRNAs per gene using established algorithms (e.g., from the Broad Institute's GPP Portal) to maximize on-target and minimize off-target activity [54] [56].
2. Library Cloning and Virus Production
- Synthesize the pooled sgRNA oligonucleotide library.
- Clone the library into a lentiviral sgRNA expression vector.
- Produce high-titer lentivirus from the pooled plasmid library in HEK293T cells.
3. Cell Transduction and Selection
- Transduce your Cas9-expressing cell line with the lentiviral library at a low Multiplicity of Infection (MOI ~0.3) to ensure most cells receive only one sgRNA.
- Culture the transduced cells for several days under antibiotic selection (e.g., puromycin) to eliminate non-transduced cells, creating the "initial pool" (T0) cell population.
4. Application of Selective Pressure
- Split the T0 population into control and experimental arms.
- Apply the selective pressure to the experimental arm (e.g., drug treatment, nutrient stress, FACS sorting based on a marker). The control arm remains untreated.
- Culture the cells for 2-3 weeks, allowing time for phenotypic enrichment or depletion.
5. Genomic DNA Extraction and Sequencing
- Harvest a representative number of cells from both the control (T0) and experimental populations.
- Extract high-quality genomic DNA.
- Amplify the integrated sgRNA sequences from the genomic DNA via PCR and prepare the amplicons for next-generation sequencing (NGS).
6. Computational Data Analysis
- Demultiplexing and Alignment: Demultiplex the NGS reads and align them to the reference sgRNA library to generate count tables for each sample.
- Normalization and Analysis: Use a tool like MAGeCK to normalize count data and perform statistical testing (e.g., using the RRA algorithm) to identify sgRNAs and genes that are significantly enriched or depleted in the experimental condition compared to the control [54].
- Hit Prioritization: Prioritize candidate genes based on statistical significance (RRA score and p-value) and magnitude of effect (log-fold change). Validate top hits in follow-up experiments.
Workflow and Pathway Visualizations
CRISPR screening data analysis workflow from raw sequencing data to biological validation.
Relationship between screen type, selection pressure, biological goal, and expected data readout.
Overcoming Bottlenecks: Proven Strategies for Pipeline Optimization
Establishing Robust Quality Control (QC) Metrics to Mitigate Sequencing Errors
Next-Generation Sequencing (NGS) has revolutionized genomics, enabling rapid, high-throughput analysis of DNA and RNA for applications ranging from cancer research to rare disease diagnosis [62]. However, the massive datasets generated by these technologies are susceptible to errors introduced at various stages, from sample preparation to final base calling. Quality control (QC) is therefore not merely a preliminary step but a critical, continuous process throughout the NGS workflow. Establishing robust QC metrics is essential to ensure data integrity, prevent misleading biological conclusions, and enable reliable downstream analysis, especially in the demanding context of large-scale chemogenomic research where accurate variant identification is paramount for linking chemical compounds to genetic targets [63] [64] [62].
Understanding Sequencing Quality Scores
The Q Score: A Fundamental Metric
The primary metric for assessing the accuracy of individual base calls is the Phred-like quality score (Q score) [65]. This score is defined by the equation: Q = -10log₁₀(e), where e is the estimated probability that the base was called incorrectly [65] [66]. This logarithmic relationship means that small changes in the Q score represent significant changes in accuracy.
The following table summarizes the relationship between Q scores, error probability, and base call accuracy:
| Quality Score | Probability of Incorrect Base Call | Inferred Base Call Accuracy |
|---|---|---|
| Q10 | 1 in 10 | 90% |
| Q20 | 1 in 100 | 99% |
| Q30 | 1 in 1000 | 99.9% |
A score of Q30 is considered a benchmark for high-quality data in most NGS applications, as it implies that virtually all reads will be perfect, with no errors or ambiguities [65]. Lower Q scores, particularly below Q20, can lead to a substantial portion of reads being unusable and significantly increase false-positive variant calls, resulting in inaccurate conclusions [65].
Platform-Specific Sequencing Errors
Different NGS platforms exhibit characteristic error profiles, which should inform the QC process:
- Illumina (Sequencing-by-Synthesis): This technology is highly accurate but can be affected by issues such as declining dye activity or partial overlap in the emission spectra of fluorophores, which complicates base calling [63]. Its quality tends to drop towards the ends of reads.
- Ion Torrent (Semiconductor Sequencing): This method detects pH changes from the release of hydrogen ions during DNA polymerization. It is generally more susceptible to errors in homopolymer regions (stretches of identical bases) [63].
The Quality Control Workflow: A Step-by-Step Guide
A comprehensive QC pipeline involves multiple stages, from raw data assessment to post-alignment refinement. The diagram below illustrates this integrated workflow:
Assess Raw Data Quality
The first QC checkpoint involves evaluating the raw sequencing reads in FASTQ format, which contain the nucleotide sequences and a quality score for every single base [66].
- Tool of Choice: FastQC [64] [66] [67]. This tool provides an initial overview through several key plots:
- Per Base Sequence Quality: Visualizes the distribution of quality scores across all positions in the read. Typically, quality is higher at the beginning and declines towards the 3' end. Any sharp, abnormal drops may indicate a technical issue [66].
- Per Sequence GC Content: Shows the distribution of GC content across all reads. The line should closely follow the theoretical distribution based on the reference genome.
- Adapter Content: Measures the proportion of adapter sequences present in your reads. High adapter content indicates the need for more aggressive trimming.
- Overrepresented Sequences: Identifies sequences that appear much more frequently than expected, which could point to contaminants or PCR artifacts.
Trim and Filter Reads
Based on the FastQC report, the next step is to "clean" the raw data by removing technical sequences and low-quality bases.
- Adapter Removal: Adapter sequences, essential for the sequencing reaction, can be incorporated into reads when the DNA fragment is shorter than the read length. Tools like Cutadapt and Trimmomatic are designed to locate and remove these adapter sequences [66] [67].
- Quality Filtering: The same tools are used to trim low-quality bases from the ends of reads and to entirely remove reads that fall below a specified quality threshold. A common practice is to trim bases with a Phred score below 20 (Q20) and discard reads that become too short after trimming (e.g., < 20-50 bases) [66] [67]. This step is crucial for maximizing the number of reads that can be accurately aligned later.
Evaluate Alignment Quality
After cleaning, reads are aligned to a reference genome. The resulting alignment files (BAM/SAM format) must then be subjected to their own QC.
- Alignment Metrics: Tools like SAMtools, Picard, and Qualimap provide vital statistics, including [64] [67]:
- Alignment Rate: The percentage of reads that successfully mapped to the reference. A low rate can indicate poor sample quality or contamination.
- Duplication Rate: The percentage of reads that are exact duplicates, often resulting from PCR over-amplification. High duplication levels can skew coverage metrics.
- Coverage Uniformity: How evenly reads are distributed across the target regions. Biases can indicate issues during library preparation.
- Mismatch Rate: The frequency of bases in the read that do not match the reference, which should be consistent with the expected error rate of the platform.
Perform Variant Calling QC
For chemogenomic applications where identifying true genetic variants is critical, this step is paramount.
- Variant Quality Filtering: After initial variant calling with tools like GATK's HaplotypeCaller, apply hard filters based on [67] [68]:
- Quality Scores: Each variant is assigned an internal quality score.
- Read Depth (DP): The number of reads supporting the variant call. Very low or very high depth can be problematic.
- Strand Bias: A strong bias where variants are only called from reads in one direction can indicate a false positive.
- Mendelian Inheritance Error (MIE) Checks: In family-based studies, MIEs—where a child's genotype is inconsistent with the inheritance patterns from its parents—are a powerful tool for identifying erroneous calls. These errors are often non-random and clustered in repetitive regions of the genome, and they can be significantly reduced by applying appropriate filters (e.g., SVM score filters) [68].
Generate Final QC Reports
- Tool of Choice: MultiQC [67]. This tool aggregates results from all the previous steps—FastQC, Trimmomatic, alignment statistics, and variant calling metrics—into a single, cohesive HTML report. This allows for easy comparison across multiple samples and provides a complete overview of data quality before proceeding to advanced analysis.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents, tools, and their functions that are essential for establishing a robust NGS QC pipeline.
| Tool/Reagent | Primary Function | Application in QC Workflow |
|---|---|---|
| Agilent TapeStation | Assess nucleic acid integrity (e.g., RIN for RNA) [66] | Sample QC: Evaluates quality of starting material pre-library prep. |
| SureSelect/SeqCap (Hybrid Capture) [63] | Enrich for target genomic regions | Library Prep: Creates targeted libraries for exome or panel sequencing. |
| AmpliSeq (Amplicon) [63] | Amplify target regions via PCR | Library Prep: Creates highly multiplexed targeted libraries. |
| Unique Molecular Identifiers (UMIs) [63] | Tag individual DNA molecules with random barcodes | Library Prep: Allows bioinformatic removal of PCR duplicates, improving quantification. |
| PhiX Control [65] | In-run control for sequencing quality monitoring | Sequencing: Provides a quality baseline and aids in base calling calibration. |
| FastQC [66] [67] | Initial quality assessment of raw FASTQ files | Bioinformatics: First-pass analysis of per-base quality, GC content, and adapters. |
| Trimmomatic/Cutadapt [66] [67] | Trim adapter sequences and low-quality bases | Bioinformatics: Data cleaning to remove technical sequences and poor-quality reads. |
| BWA/Bowtie2 [67] [62] | Align sequencing reads to a reference genome | Bioinformatics: Essential step for mapping sequenced fragments to their genomic origin. |
| SAMtools/Picard [67] | Analyze and manipulate alignment files (BAM) | Bioinformatics: Calculate mapping statistics, mark duplicates, and index files. |
| MultiQC [67] | Aggregate results from multiple tools into one report | Bioinformatics: Final quality overview and inter-sample comparison. |
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ 1: What is an acceptable Q score for my clinical research project?
For clinical research, where accuracy is critical, the benchmark is Q30 [65]. This means that 99.9% of base calls are correct, equating to only 1 error in every 1,000 bases. While data with a lower average quality (e.g., Q20-Q30) might be usable for some applications, it increases the risk of false-positive variant calls and may require more stringent filtering, which can also remove true variants.
FAQ 2: My FastQC report shows "Per base sequence quality" is poor at the ends. What should I do?
A gradual decline in quality towards the 3' end of reads is normal for some platforms like Illumina [66]. However, a sharp drop is a cause for concern. The standard solution is to use a trimming tool like Trimmomatic or Cutadapt to remove low-quality bases from the ends of reads. This "cleaning" process will increase your overall alignment accuracy, even though it may slightly reduce the average read length.
FAQ 3: After alignment, I have a high duplication rate. What does this mean and how can I fix it?
A high duplication rate indicates that a large proportion of your reads are exact copies, which is often a result of PCR over-amplification during library preparation [67]. While some duplication is expected, high levels can lead to inaccurate estimates of gene expression or allele frequency. If you used UMIs during library prep, you can bioinformatically remove these duplicates. If not, you can use tools like Picard MarkDuplicates to flag them. For future experiments, optimizing the number of PCR cycles during library prep can help mitigate this issue.
FAQ 4: My variant caller identified a potential mutation in a repetitive genomic region. Should I trust this call?
Be highly skeptical. Variant calling in repetitive regions (e.g., those enriched with SINEs, LINEs, or other repetitive elements) is notoriously error-prone due to misalignment of short reads [68]. These regions are known hotspots for Mendelian Inheritance Errors. You should apply stricter filters (e.g., higher depth and quality score requirements) and consider orthogonal validation methods, such as Sanger sequencing, for any putative variant in such a region before drawing biological conclusions.
FAQ 5: How can I check for sample contamination in my metagenomic dataset?
Contamination screening is a vital QC step. While FastQC can detect overrepresented sequences, specialized tools like QC-Chain are designed for de novo contamination identification without prior knowledge of the contaminant [69]. It screens reads against databases (e.g., of 18S rRNA) to identify contaminating species (e.g., host DNA in a microbiome sample) with high sensitivity and specificity, which is crucial for obtaining accurate taxonomical and functional profiles.
Standardizing Bioinformatics Pipelines to Ensure Consistency and Reproducibility
In large-scale chemogenomic NGS research, standardization is not a luxury but a necessity. The ability to reproduce computational results is a foundational principle of scientific discovery, yet studies reveal a grim reality: a systematic evaluation showed only about 11% of bioinformatics articles could be reproduced, and recent surveys of Jupyter notebooks in biomedical publications found only 5.9% produced similar results to the original studies [70]. The ramifications extend beyond academic circles—irreproducible bioinformatics in clinical research potentially places patient safety at risk, as evidenced by historical cases where flawed data analysis led to harmful patient outcomes in clinical trials [70]. This technical support center provides practical guidance to overcome these challenges through standardized, troubleshooted bioinformatics workflows.
The Five Pillars of Reproducible Computational Research
Reproducibility ensures that materials from a past study (data, code, and documentation) can regenerate the same outputs and confirm findings [70]. The following framework establishes five essential pillars for achieving reproducibility:
Literate Programming
Combine analytical code chunks with human-readable text using tools like R Markdown, Jupyter Notebooks, or MyST [70]. These approaches embed code, results, and narrative explanation in a single document, making the analytical process transparent.
Code Version Control and Sharing
Utilize Git systems to track changes, collaborate effectively, and maintain a complete history of your computational methods. Version control is essential for managing iterative improvements and identifying when errors may have been introduced [71].
Compute Environment Control
Containerize analyses using Docker or Singularity to capture exact software versions and dependencies. Workflow systems like Nextflow, Snakemake, CWL, or WDL ensure consistent execution across different computing environments [70].
Persistent Data Sharing
Store data in publicly accessible, versioned repositories with persistent identifiers. Ensure code can automatically fetch required data from these locations to enable end-to-end workflow automation [70].
Comprehensive Documentation
Maintain detailed records of pipeline configurations, tool versions, parameters, and analytical decisions. Proper documentation ensures others can understand, execute, and build upon your work [71].
Troubleshooting Guides
Guide 1: Addressing Low Sequencing Library Yield
Problem: Unexpectedly low final library yield after preparation.
Diagnostic Steps:
- Verify the yield is genuinely low: Compare quantification methods (Qubit vs qPCR vs BioAnalyzer) as one may overestimate usable material [5].
- Examine electropherogram traces: Look for broad peaks, missing target fragment sizes, or adapter dimer dominance.
- Check reagent logs and operator notes: Identify anomalies in lot numbers or procedural variations.
Common Causes and Solutions:
| Root Cause | Mechanism of Yield Loss | Corrective Action |
|---|---|---|
| Poor Input Quality | Enzyme inhibition from contaminants (phenol, salts, EDTA) | Re-purify input sample; ensure wash buffers are fresh; target high purity (260/230 > 1.8) [5] |
| Quantification Errors | Under-estimating input concentration leads to suboptimal enzyme stoichiometry | Use fluorometric methods (Qubit) rather than UV only; calibrate pipettes; use master mixes [5] |
| Fragmentation Issues | Over- or under-fragmentation reduces adapter ligation efficiency | Optimize fragmentation parameters; verify distribution before proceeding [5] |
| Adapter Ligation Problems | Poor ligase performance or incorrect molar ratios | Titrate adapter:insert ratios; ensure fresh ligase and buffer; maintain optimal temperature [5] |
Guide 2: Resolving Bioinformatics Pipeline Failures
Problem: Pipeline errors or inconsistent results between runs.
Diagnostic Steps:
- Analyze error logs to pinpoint specific failure points.
- Isolate the problematic stage in the workflow (alignment, variant calling, etc.).
- Check tool compatibility and version dependencies.
- Verify data integrity at each processing stage.
Common Issues and Solutions:
| Pipeline Stage | Common Failure Modes | Solutions |
|---|---|---|
| Data QC & Preprocessing | Poor quality reads, adapter contamination, incorrect formats | Use FastQC for quality checks; trim with Trimmomatic; validate file formats and metadata [71] [8] |
| Read Alignment | Low mapping rates, reference bias, multi-mapped reads | Use appropriate reference genome version; check for indexing; adjust parameters for repetitive regions; consider alternative aligners [72] |
| Variant Calling | High false positives/negatives, inconsistent results | Validate with known datasets; adjust quality thresholds; use multiple callers and compare; check for random seed settings [72] |
| Downstream Analysis | Batch effects, normalization errors, misinterpretation | Perform PCA to identify batch effects; use appropriate normalization methods; document all parameters [71] |
Guide 3: Handling Irreproducible Results Across Technical Replicates
Problem: Bioinformatics tools producing different results when run on technical replicates (same biological sample, different sequencing runs).
Diagnostic Steps:
- Confirm technical replicates were generated using identical experimental protocols.
- Check for algorithmic randomness (e.g., in machine learning or certain projection methods).
- Verify consistent tool versions and parameters across analyses.
- Examine whether read order affects results (relevant for some aligners like BWA-MEM) [72].
Solutions:
- Set random seeds: Initialize pseudo-random number generators with fixed values for stochastic algorithms [70].
- Control computational environments: Use containers to ensure consistent software versions and dependencies.
- Validate with gold standards: Use resources like Genome in a Bottle (GIAB) consortium benchmarks [72].
- Document all parameters: Maintain complete records of every adjustable setting.
Frequently Asked Questions (FAQs)
Q1: What is the primary purpose of bioinformatics pipeline troubleshooting? The primary purpose is to identify and resolve errors or inefficiencies in workflows, ensuring accurate and reliable data analysis while maintaining reproducibility across experiments and research teams [71].
Q2: How can I start building a standardized bioinformatics pipeline? Begin by defining clear research objectives, selecting appropriate tools, designing a modular workflow, testing on small datasets, implementing version control, and thoroughly documenting each step [71]. Consider established workflow managers like Nextflow or Snakemake from the start.
Q3: What are the most critical tools for maintaining pipeline reproducibility? Essential tools include workflow management systems (Nextflow, Snakemake), version control (Git), containerization (Docker, Singularity), quality control utilities (FastQC, MultiQC), and comprehensive documentation platforms [70] [71].
Q4: How do I ensure my pipeline remains accurate over time? Regularly validate results with known datasets, cross-check outputs using alternative methods, stay current with software updates, and implement continuous integration testing for your workflows [71].
Q5: What industries benefit most from reproducible pipeline troubleshooting? Healthcare, pharmaceutical development, environmental studies, agriculture, and biotechnology are among the industries that rely heavily on reproducible bioinformatics pipelines [71].
Essential Research Reagents and Computational Tools
| Item | Function | Application Notes |
|---|---|---|
| BWA-MEM | Read alignment to reference genomes | May show variability with read order; consider Bowtie2 for more consistent results [72] |
| GATK | Variant discovery and genotyping | Follow best practices guidelines; use consistent quality thresholds across analyses [71] |
| FastQC | Quality control of raw sequencing data | Essential first step; identifies adapter contamination, quality issues early [71] [8] |
| Nextflow/Snakemake | Workflow management | Enables portability, scalability, and reproducibility across computing environments [70] [71] |
| Docker/Singularity | Containerization | Captures complete computational environment for consistent execution [70] |
| Git | Version control | Tracks changes to code, parameters, and documentation [71] |
| FastQ Screen | Contamination check | Identifies cross-species or other contamination in samples [73] |
| MultiQC | Aggregate QC reports | Combines results from multiple tools into a single report for assessment [71] |
Troubleshooting Workflow Diagram
Standardizing bioinformatics pipelines requires both technical solutions and cultural shifts. Implement the five pillars of reproducibility—literate programming, version control, environment control, data sharing, and documentation—as foundational elements. Establish systematic troubleshooting protocols and promote collaboration between computational and experimental researchers. As computational demands grow in chemogenomic NGS research, these practices will ensure your work remains reproducible, reliable, and impactful, ultimately accelerating drug discovery and improving patient outcomes.
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary factors to consider when selecting computational infrastructure for large-scale chemogenomic NGS data research?
The key factors include data output volume, analysis workflow complexity, and collaboration needs. Modern NGS platforms can generate terabytes of data per run; for instance, high-throughput sequencers can output up to 16 terabases in a single run [74]. Your infrastructure must handle this scale. The integration of multi-omics approaches (combining genomics, transcriptomics, and proteomics) and AI-powered analysis further increases computational demands, requiring scalable solutions like cloud computing for efficient data processing and real-time collaboration [26] [28].
FAQ 2: Should our lab use on-premise servers or cloud computing for NGS data analysis?
The choice depends on your data volume, budget, and need for flexibility. Cloud computing (e.g., AWS, Google Cloud Genomics) is often advantageous for its scalability, ability to handle vast datasets, and cost-effectiveness for labs without significant initial infrastructure investments. It also facilitates global collaboration by allowing researchers from different institutions to work on the same datasets in real-time [26]. However, for labs with predictable, high-volume workloads and stringent data governance requirements, a hybrid or fully on-premise infrastructure might be preferable.
FAQ 3: How much storage capacity do we need for a typical large-scale chemogenomics project?
Storage needs are substantial and often underestimated. The table below summarizes estimated storage requirements for common data types, but note that raw data, intermediate files, and processed data can multiply these figures [74].
Table: Estimated NGS Data Output and Storage Needs
| Data Type / Application | Typical Data Output per Sample | Key Infrastructure Consideration |
|---|---|---|
| Whole-Genome Sequencing (WGS) | ~100 GB (raw data) [74] | Highest demand for storage and compute power |
| Targeted Sequencing / Gene Panels | Low to Medium (Mb – Gb) [74] | Cost-effective, requires less storage |
| RNA Sequencing (RNA-Seq) | Medium to High (Gb) [74] | Significant processing power for expression analysis |
FAQ 4: What are the best practices for ensuring data security and compliance in NGS research?
Genomic data is highly sensitive. When using cloud platforms, ensure they comply with strict regulatory frameworks like HIPAA and GDPR [26]. Employ advanced encryption algorithms for data both at rest and in transit. Establish clear protocols for informed consent and data anonymization, especially in multi-omics studies where data sharing is common [26].
Troubleshooting Guides
Problem 1: Analysis pipelines are running too slowly or timing out.
- Potential Cause: Insufficient computational resources (CPU, RAM) for the selected data analysis workflow.
- Solution:
- Profile your workflow: Identify which step (e.g., alignment, variant calling) is the bottleneck.
- Scale up resources: For on-premise clusters, allocate more cores and RAM to the task. In the cloud, switch to a higher-performance compute instance type.
- Optimize code: Use parallel processing and ensure your bioinformatics software is optimized for your hardware.
- Leverage optimized services: Consider using cloud-based genomic analysis platforms that offer pre-configured, optimized environments for common tools like DeepVariant [26] [74].
Problem 2: Costs for data storage and computation are escalating unexpectedly.
- Potential Cause: Unmanaged growth of data, especially intermediate files, and inefficient use of cloud resources.
- Solution:
- Implement a data lifecycle policy: Automate the archiving or deletion of temporary files and raw data after processing, keeping only essential results.
- Use cloud cost management tools: Set up budgets and alerts to monitor spending.
- Choose the right storage class: Use cheaper "cold storage" archives for data that is rarely accessed.
- Consolidate datasets: Use data compression and efficient file formats to reduce the physical storage footprint.
Problem 3: Inconsistent or irreproducible results from bioinformatics analyses.
- Potential Cause: Lack of version control for software, scripts, and reference genomes, leading to environment drift.
- Solution:
- Containerize workflows: Use Docker or Singularity to package your entire analysis environment (software, libraries, dependencies).
- Use workflow management systems: Adopt platforms like Nextflow or Snakemake, which ensure that workflows are executed consistently across different compute environments [74].
- Maintain a curated repository: Keep version-controlled records of all reference genomes, databases, and software used in each analysis.
The Scientist's Toolkit: Essential Computational Infrastructure Components
Table: Key Computational Resources for Large-Scale NGS Research
| Component | Function | Considerations for Selection |
|---|---|---|
| High-Performance Compute (HPC) Cluster / Cloud Compute Instances | Provides the massive parallel processing power needed for secondary analysis (alignment, variant calling). | Opt for machines with high core counts and large RAM for whole-genome analysis. Cloud instances specialized for genomics can offer better price-to-performance [28]. |
| Scalable Storage (NAS / Cloud Object Storage) | Stores vast amounts of raw sequencing data, intermediate files, and final results. | Requires a tiered strategy: fast SSDs for active analysis and cheaper, high-capacity disks or cloud archives for long-term storage [75]. |
| Bioinformatics Workflow Management Systems | Automates and orchestrates multi-step analysis pipelines, ensuring reproducibility and portability. | Nextflow and Snakemake are community standards that support both on-premise and cloud execution [74]. |
| Containerization Platform | Packages software and its environment into isolated units, eliminating "it works on my machine" problems. | Docker is widely used for development, while Singularity is common in HPC environments for security reasons. |
| Data Security & Encryption Tools | Protects sensitive genomic and patient data in compliance with regulations like HIPAA and GDPR. | Essential for both on-premise (encrypted filesystems) and cloud (managed key management services) deployments [26]. |
Workflow and Infrastructure Diagrams
NGS Infrastructure Planning
NGS Data Analysis Pipeline
Implementing Automation and Flexible, Vendor-Agnostic Workflows
Modern chemogenomic research generates vast datasets, where Next-Generation Sequencing (NGS) is used to understand the complex interactions between chemical compounds and biological systems. The scale of data produced presents significant computational challenges. As the table below illustrates, the global NGS data analysis market is substantial and growing rapidly, underscoring the critical need for efficient, scalable, and flexible computational workflows.
Table: Global NGS Data Analysis Market Snapshot (2025)
| Metric | Value |
|---|---|
| Market Value | ~USD 1.9 Billion [76] |
| Key Growth Driver | Precision Oncology (Used by ~65% of U.S. oncology labs) [76] |
| Cloud-Based Workflows | ~45% of all analysis pipelines [76] |
| U.S. Market Value | ~USD 750 Million [76] |
Automating these data analysis workflows is no longer a luxury but a necessity. It minimizes manual errors, accelerates reproducibility, and allows researchers to focus on scientific interpretation rather than computational logistics [77]. A vendor-agnostic approach, which avoids dependence on a single provider's ecosystem, is equally crucial. This flexibility prevents "vendor lock-in," a situation where switching providers becomes prohibitively difficult and costly, thereby protecting your research from technological obsolescence and enabling you to select the best tools for each specific task [78] [79].
Troubleshooting Guide: Common Automation Workflow Errors
This section addresses frequent issues encountered when automating NGS data analysis pipelines.
Q1: Our automated workflow fails because it cannot access a required data file or service. The error log mentions "AccessDenied" or similar permissions issues. What should we do?
This is typically an Identity and Access Management (IAM) error, where the automation service lacks the necessary permissions.
- Error Meaning: The automated process's identity (e.g., its service role or account) has not been granted the rights to perform a specific action, such as reading from a cloud storage bucket, writing to a directory, or invoking a computational API [80].
- Resolution Steps:
- Identify the Failing Step: Pinpoint which action in the workflow is triggering the error by checking the failure message and execution logs [80].
- Verify Service Role Permissions: Ensure the service role or account used by your automation tool has an IAM policy attached that grants it the required permissions (e.g.,
s3:GetObjectfor AWS S3 access, orssm:StartAutomationExecutionfor AWS Systems Manager). The principle of least privilege should be applied [80]. - Check for PassRole Permissions: If the automation needs to delegate permissions by passing a role to another service, the initial service role must have
iam:PassRolepermissions for the target role [80].
Q2: A step in our pipeline that uses a containerized tool fails to run. The error is "ImageId does not exist" or a similar "not found" message. How can we resolve this?
This indicates that the computing environment cannot locate the specified software container or machine image.
- Error Meaning: The container image (e.g., a Docker image) or machine image (AMI) referenced in your workflow configuration does not exist in the specified repository, has been deleted, or the workflow lacks permission to pull it [80].
- Resolution Steps:
- Verify Image Name and Tag: Check your workflow script for typos in the image name, tag, or version. Use a specific tag (e.g.,
v2.1.5) instead of a mutable tag likelatestto ensure consistency [80]. - Check Repository Location: Confirm that the image repository (e.g., Docker Hub, Amazon ECR, Google Container Registry) is correctly specified and that the compute environment has network access to it.
- Review Pull Permissions: Ensure the automation service's role has the necessary permissions to authenticate with and pull images from the private repository.
- Verify Image Name and Tag: Check your workflow script for typos in the image name, tag, or version. Use a specific tag (e.g.,
Q3: Our workflow executes but gets stuck and eventually times out. What are the common causes and solutions?
A workflow timeout suggests that a particular step is taking longer to complete than the maximum time allowed.
- Error Meaning: The execution time for a specific action or the entire workflow has exceeded the predefined
timeoutSecondsparameter. This can be caused by unexpectedly large input data, insufficient computational resources, or a hanging process [80]. - Resolution Steps:
- Profile the Workflow: Check the logs to identify which step is consuming the most time and resources.
- Adjust Timeout Settings: Increase the
timeoutSecondsparameter for the slow-running step to a more realistic value based on your profiling data [80]. - Scale Compute Resources: If the step is computationally intensive, configure the workflow to use a higher-performance compute instance (e.g., more CPU and memory) for that specific task.
- Optimize the Input Data or Code: Check if the input data size can be reduced or if the analysis script/algorithm can be optimized for better performance.
Q4: We encounter inconsistent results when running the same automated pipeline across different computing environments (e.g., on-premise HPC vs. different cloud providers). How can we ensure consistency?
This problem often stems from a lack of environment isolation and dependency management.
- Error Meaning: Differences in operating systems, software library versions, or system configurations between environments are leading to divergent outputs.
- Resolution Steps:
- Use Containerization: Package your analysis tools, all their dependencies, and the execution environment into a container (e.g., Docker or Singularity). This creates a consistent, isolated runtime environment that is portable across different platforms [78].
- Implement Dependency Management: Use a conda environment or a virtual environment with a locked version file to explicitly define and install every software package and its specific version.
- Adopt Standardized File Formats: Use community-standard, unambiguous file formats for data interchange between workflow steps to minimize parsing discrepancies.
FAQs on Implementing Vendor-Agnostic Workflows
Q1: What are the concrete benefits of a vendor-agnostic workflow for our research lab?
Adopting a vendor-agnostic strategy provides several key advantages that enhance the longevity, flexibility, and cost-effectiveness of your research:
- Avoid Vendor Lock-in: Prevents being tied to a single provider's proprietary ecosystem, which can lead to escalating costs and limited flexibility [78] [79].
- Application Portability: Enables you to move workflows between different computing environments (e.g., from one cloud to another, or to an on-premise cluster) with minimal changes, protecting your investments in workflow development [79].
- Optimize Cost and Performance: Allows you to "mix and match" best-of-breed services from different vendors to achieve the optimal balance of performance and cost for each project [78].
- Foster Interoperability: Facilitates collaboration with external partners who may use different technology stacks, as workflows are built on open standards and interchangeable components [79].
Q2: What are the best practices for designing workflows that are not locked into a single cloud provider?
Designing for portability requires a conscious architectural approach from the outset.
- Use Cloud-Agnostic Tools: Whenever possible, use open-source or multi-cloud supported tools for infrastructure provisioning (e.g., Terraform), container orchestration (e.g., Kubernetes), and workflow management (e.g., Nextflow, Snakemake) [78].
- Abstract Cloud-Specific Services: Create an abstraction layer for services like logging, messaging, or object storage. For instance, instead of directly calling a proprietary cloud storage API in your code, use a client library that can be configured to work with multiple backends [78].
- Consider Data Dependencies Early: Data transfer is often the most significant barrier to portability. Plan your data strategy—whether to co-locate data and computation, replicate data across clouds, or use a neutral storage format—from the beginning [78].
Q3: How can containerization and orchestration technologies like Docker and Kubernetes help?
These technologies are foundational for building vendor-agnostic, scalable automation.
- Containerization (e.g., Docker): Packages your application and its entire environment into a single, standardized unit. This ensures that your NGS analysis tool runs identically on a laptop, a high-performance computing cluster, or any cloud platform, eliminating the "it works on my machine" problem [78].
- Orchestration (e.g., Kubernetes): Provides a declarative API for deploying, managing, and scaling containerized applications across a cluster of machines. Since Kubernetes is an open standard supported by all major cloud providers, it allows you to deploy the same workflow definition anywhere Kubernetes runs, providing a consistent operational layer [78].
Q4: Our automated pipeline needs to integrate multiple best-in-class tools from different vendors. How can we ensure they work together seamlessly?
Successful integration in a multi-vendor environment hinges on standardizing interfaces.
- Adopt Standardized APIs and Data Formats: Prefer tools that offer and consume well-documented, standardized APIs (like REST) and use common, open data formats (e.g., SAM/BAM for aligned sequences, VCF for variants) for input and output.
- Leverage Integration Platforms: Utilize integration platforms or workflow management systems specifically designed to act as a central "orchestrator." These platforms can connect disparate systems through their APIs, standardize data flow, and manage the execution of complex, multi-step processes [77] [81].
Visualizing the Automated, Vendor-Agnostic NGS Workflow
The following diagram illustrates the logical flow and components of a robust, portable automation pipeline for large-scale chemogenomic data analysis.
Automated Vendor-Agnostic NGS Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key computational "reagents" and platforms essential for constructing and running automated, vendor-agnostic chemogenomic workflows.
Table: Key Solutions for Automated NGS Workflows
| Tool Category | Example | Function & Role in Vendor-Agnostic Automation |
|---|---|---|
| Workflow Management Systems | Nextflow, Snakemake | Defines, executes, and manages complex, multi-step data analysis pipelines. They are inherently portable, allowing the same workflow to run on different compute infrastructures without modification. |
| Containerization Platforms | Docker, Singularity | Packages software tools and all their dependencies into a single, portable unit (container), guaranteeing reproducibility and simplifying deployment across diverse environments. |
| Container Orchestration | Kubernetes | Automates the deployment, scaling, and management of containerized applications across clusters of machines, providing a uniform abstraction layer over underlying cloud or hardware resources. |
| Infrastructure as Code (IaC) | Terraform, Ansible | Enables the programmable, declarative definition and provisioning of the computing infrastructure (e.g., VMs, networks, storage) required for the workflow, making the environment itself reproducible and portable [77]. |
| Cloud-Agnostic Object Storage | (Standard S3 API) | Using the de facto standard S3 API for data storage ensures that data can be easily accessed and moved between different public clouds and private storage solutions that support the same protocol [78]. |
| NGS Data Analysis Platforms | DNAnexus, Seven Bridges | Provides managed, cloud-based platforms with pre-configured bioinformatics tools and pipelines. Many now support multi-cloud deployments, helping to avoid lock-in to a single cloud provider [76]. |
Addressing Tool Variability and Conflicting Results in Variant Interpretation
Troubleshooting Guides
Guide 1: Resolving Discrepancies from Computational Prediction Tools
Problem: Different in silico prediction tools provide conflicting pathogenicity scores for the same genetic variant, leading to inconsistent evidence application in ACMG/AMP classification.
Solution: Implement a standardized tool selection and reconciliation protocol.
Tool Selection Criteria:
- Prioritize predictors with proven performance in independent benchmark studies (e.g., CAGI challenges) over older, established tools [82].
- Select complementary tools based on different algorithmic approaches rather than multiple similar methods [82].
- Avoid using tools mentioned in guidelines as default recommendations without verifying their current performance status [82].
Discrepancy Resolution Workflow:
- When predictors conflict, defer to the tool with demonstrated superior performance metrics for your specific variant type [82].
- Do not use majority voting approaches that allow poorer-performing methods to overrule better ones [82].
- For critical variants, supplement computational evidence with additional functional data or clinical correlations [83].
Performance Validation:
Table 1: Performance Considerations for Computational Predictors
| Factor | Impact on Variant Interpretation | Best Practice Solution |
|---|---|---|
| Tool Age | Older methods may have 30%+ lower performance than state-of-the-art tools [82] | Regularly update tool selection based on recent benchmark studies |
| Algorithm Diversity | Using similar methods introduces bias [82] | Select predictors with different computational approaches |
| Training Data | Predictors cannot outperform their training data quality [82] | Verify training data composition and relevance to your variant type |
| Coverage | Percentage of predictable variants is not a quality indicator [82] | Focus on accuracy metrics rather than coverage |
Guide 2: Managing Evidence Conflicts in ACMG/AMP Classification
Problem: Applying ACMG/AMP guidelines leads to different variant classifications between laboratories or between automated systems and expert review.
Solution: Standardize evidence application and implement resolution pathways.
Evidence Strength Reconciliation:
- For functional data (PS3/BS3): Establish predefined criteria for acceptable experimental systems and validation approaches [84].
- For population data (BS1/PM2): Set laboratory-specific allele frequency thresholds based on disorder prevalence and inheritance patterns [85] [84].
- For case data (PS4): Define "multiple unrelated cases" thresholds consistently across classification teams [84].
Classification Review Protocol:
Automated System Validation:
Table 2: Common Sources of Classification Discrepancies and Resolution Strategies
| Evidence Category | Common Discrepancy Sources | Resolution Approaches |
|---|---|---|
| Population Frequency (PM2/BS1) | Different AF thresholds (0.1% vs 0.5% vs 1%) [85] | Establish gene- and disease-specific thresholds based on prevalence |
| Functional Data (PS3/BS3) | Disagreement on acceptable model systems or assays [84] | Predefine validated experimental approaches for each gene/disease |
| Case Data (PS4) | Variable thresholds for "multiple unrelated cases" [84] | Set quantitative standards (e.g., ≥3 cases) for moderate strength |
| Computational Evidence (PP3/BP4) | Different tool selections and concordance requirements [82] | Standardize tool suite and establish performance-based weighting |
Guide 3: Addressing Technical Variability in NGS Data Analysis
Problem: Technical differences in NGS workflows, including variant callers and quality thresholds, introduce variability in variant detection and interpretation.
Solution: Standardize technical protocols and implement cross-validation.
Wet Lab Protocol Harmonization:
Bioinformatic Pipeline Consistency:
Frequently Asked Questions (FAQs)
Q1: Why do different clinical laboratories classify the same variant differently, and how common is this problem?
Approximately 5.7% of variants in ClinVar have conflicting interpretations, with studies showing inter-laboratory disagreement rates of 10-40% [85] [86]. These conflicts primarily arise from:
- Differences in classification methods or modifications of ACMG/AMP guidelines [84]
- Variable application of evidence categories and strengths [84]
- Access to different evidence sources (literature, clinical data) [84]
- Interpreter opinions and expertise variations [84] Major classification differences that impact clinical care (Pathogenic/Likely Pathogenic vs. VUS/Benign) occur in approximately 4-22% of variants between laboratories [85].
Q2: What is the most effective strategy for selecting computational prediction tools to minimize variability?
The optimal strategy involves:
- Selecting a single proven high-performance predictor rather than multiple mediocre tools [82]
- Choosing tools based on independent benchmarking studies rather than guideline mentions [82]
- Ensuring selected tools use complementary approaches rather than similar algorithms [82]
- Regularly updating tool selection as better predictors become available [82] Avoid the common pitfall of requiring multiple tools to agree, as this approach gives decision power to the poorest-performing methods and reduces variant coverage [82].
Q3: How can our research team reduce variant classification discrepancies when working with large-scale chemogenomic datasets?
Implement a systematic approach:
- Standardize evidence collection: Use automated literature mining tools to ensure comprehensive evidence gathering [84]
- Establish laboratory-specific guidelines: Develop detailed specifications for ambiguous ACMG/AMP criteria [84]
- Implement regular reassessment: Use automated systems to re-evaluate variants as new evidence emerges [83]
- Participate in data sharing: Contribute to and utilize shared databases like ClinVar to resolve conflicts [84] [86] Evidence sharing between groups facilitates resolution of approximately 33% of classification discrepancies [84].
Q4: What are the specific challenges in variant interpretation for chemogenomics research compared to clinical diagnostics?
Chemogenomics research presents unique challenges:
- Scale: Analyzing thousands of variants across multiple chemical treatments requires automated, high-throughput interpretation pipelines [83]
- Functional focus: Greater emphasis on functional consequences (PS3/BS3) for understanding mechanism of action [84]
- Novel variants: Higher prevalence of rare or novel variants with limited population data [86]
- Polypharmacology: Need to assess variants across multiple gene targets for a single compound [87] Successful chemogenomic variant interpretation requires integration of computational predictions, functional assays, and chemical-target interaction data [87].
Experimental Protocols for Variant Interpretation Validation
Protocol 1: Benchmarking Computational Prediction Tools
Purpose: Systematically evaluate and select optimal computational predictors for your specific research context.
Materials:
- Curated dataset of known pathogenic and benign variants
- Access to multiple prediction tools (SIFT, PolyPhen-2, REVEL, etc.)
- Benchmarking framework (CAGI protocols or custom implementation)
Methodology:
- Dataset Preparation:
- Compile 500-1000 variants with validated clinical classifications
- Ensure balanced representation of pathogenic and benign variants
- Include variant types relevant to your research (missense, splicing, etc.)
Tool Execution:
- Run all candidate predictors on the benchmark dataset
- Record raw scores and recommended classifications
Performance Analysis:
- Calculate sensitivity, specificity, and accuracy metrics
- Generate ROC curves and calculate AUC values
- Identify top-performing tools for your variant type
Implementation:
- Select optimal tool(s) based on performance metrics
- Establish laboratory-specific score thresholds
- Document selection rationale for future reference
Protocol 2: Cross-Laboratory Variant Interpretation Concordance Study
Purpose: Identify and resolve systematic differences in variant interpretation between research teams or automated systems.
Materials:
- Set of 50-100 challenging variants with limited evidence
- Multiple interpretation teams or automated systems
- Standardized evidence database
Methodology:
- Blinded Interpretation:
- Distribute variant set to all participating teams/systems
- Provide identical evidence base (literature, population data)
- Apply respective interpretation protocols independently
Classification Comparison:
- Collect all variant classifications
- Identify discrepancies using standardized categories
- Calculate concordance rates and identify patterns
Discrepancy Resolution:
- Conduct structured discussions for conflicting variants
- Identify root causes of differences
- Develop consensus classifications for problematic variants
Process Improvement:
- Implement protocol adjustments to address systematic issues
- Establish ongoing quality assessment process
- Document lessons learned for future interpretations
Signaling Pathways and Workflow Diagrams
Variant Interpretation Workflow
Conflict Resolution Pathway
Research Reagent Solutions
Table 3: Essential Resources for Variant Interpretation
| Resource Category | Specific Tools/Databases | Primary Function | Application Notes |
|---|---|---|---|
| Variant Databases | ClinVar, gnomAD, dbNSFP | Provides clinical interpretations, population frequencies, and multiple computational predictions [83] [82] | Cross-reference multiple sources; note that 9% of ClinVar variants have conflicting classifications [84] |
| Computational Predictors | REVEL, CADD, SIFT, PolyPhen-2 | In silico assessment of variant pathogenicity [82] | Select based on benchmarking; avoid requiring multiple tools to agree [82] |
| Annotation Platforms | VarCards, omnomicsNGS | Integrates multiple evidence sources for variant prioritization [83] [82] | Automated re-evaluation crucial for maintaining current classifications [83] |
| Quality Assessment | EMQN, GenQA | External quality assurance for variant interpretation [83] | Participation reduces inter-laboratory discrepancies [83] |
| Literature Mining | PubMed, Custom automated searches | Comprehensive evidence gathering from scientific literature [84] | Critical for resolving 33% of classification discrepancies [84] |
Ensuring Rigor: Validation Frameworks and Comparative Technology Analysis
In the context of large-scale chemogenomic Next-Generation Sequencing (NGS) data research, establishing robust analytical validation is paramount for generating reliable, reproducible results. The astonishing rate of data generation by low-cost, high-throughput technologies in genomics is matched by significant computational challenges in data interpretation [3]. For researchers, scientists, and drug development professionals, this means that analytical validation must not only ensure method accuracy but also account for the substantial computational infrastructure required to manage and process these large-scale, high-dimensional data sets [3] [10].
The computational demands for large-scale data analysis present unique hurdles for validation protocols. Understanding how living systems operate requires integrating multiple layers of biological information that high-throughput technologies generate, which poses several pressing challenges including data transfer, access control, management, standardization of data formats, and accurate modeling of biological systems [3]. These factors directly impact how validation parameters are established and monitored throughout the research lifecycle.
Core Principles of Analytical Validation
Fundamental Concepts and Regulatory Framework
Analytical method validation ensures that pharmaceutical products consistently meet critical quality attributes (CQAs) for drug substance/drug product. The fundamental equations governing analytical method performance are:
- Product Mean = Sample Mean + Method Bias
- Reportable Result = Test sample true value + Method Bias + Method Repeatability [88]
Regulatory guidance documents provide direction for establishing validation criteria. The International Council for Harmonisation (ICH) Q2 discusses what to quantitate and report but implies rather than explicitly defines acceptance criteria [88]. The FDA's "Analytical Procedures and Methods Validation for Drugs and Biologics" states that analytical procedures are developed to test defined characteristics against established acceptance criteria [88]. The United States Pharmacopeia (USP) <1225> and <1033> emphasize that acceptance criteria should be consistent with the method's intended use and justified based on the risk that measurements may fall outside of product specifications [88].
Computational Considerations for Validation
In large-scale chemogenomic studies, validation approaches must account for the computational environment's impact on results. Key considerations include:
- Data Format Standardization: Different centers generate data in different formats, requiring time-consuming reformatting and re-integrating data multiple times during a single analysis [3]
- Algorithm Selection: Understanding whether analysis algorithms are computationally intense (NP-hard problems) helps determine appropriate computational resources [3]
- Workflow Management: Utilizing workflow engines and container technology maintains reproducibility, portability, and scalability in genome data analysis [10]
Establishing Acceptance Criteria for Key Validation Parameters
Quantitative Guidelines for Validation Parameters
Table 1: Recommended Acceptance Criteria for Analytical Method Validation
| Validation Parameter | Recommended Acceptance Criteria | Evaluation Method |
|---|---|---|
| Specificity | Excellent: ≤5% of toleranceAcceptable: ≤10% of tolerance | Specificity/Tolerance × 100 |
| Limit of Detection (LOD) | Excellent: ≤5% of toleranceAcceptable: ≤10% of tolerance | LOD/Tolerance × 100 |
| Limit of Quantification (LOQ) | Excellent: ≤15% of toleranceAcceptable: ≤20% of tolerance | LOQ/Tolerance × 100 |
| Bias/Accuracy | ≤10% of tolerance (for both analytical methods and bioassays) | Bias/Tolerance × 100 |
| Repeatability | ≤25% of tolerance (analytical methods)≤50% of tolerance (bioassays) | (Stdev Repeatability × 5.15)/(USL-LSL) |
Tolerance-Based Evaluation
Traditional measures of analytical goodness including % coefficient of variation (%CV) and % recovery should be report-only and not used as primary acceptance criteria [88]. Instead, method error should be evaluated relative to the specification tolerance:
- Tolerance = Upper Specification Limit (USL) - Lower Specification Limit (LSL) for two-sided limits
- Margin = USL - Mean or Mean - LSL for one-sided specifications [88]
This approach directly links method performance to its impact on product quality decisions and out-of-specification (OOS) rates.
Experimental Protocols and Methodologies
Protocol for Specificity Determination
Objective: To demonstrate the method measures the specific analyte without interference from other compounds or matrices.
Methodology:
- For identification: Demonstrate 100% detection of the specific analyte, reporting detection rate and 95% confidence limits
- For bias assessment: Measure the difference between results in the presence and absence of interfering matrices
- Calculate: Reportable Specificity = Measurement - Standard (in units, in the matrix of interest)
- Evaluate: Specificity/Tolerance × 100 [88]
Computational Considerations: In NGS data analysis, specificity must account for platform-specific variations in data formats and analysis tools, which may require adaptation across different computational environments [3].
Protocol for Limit of Detection (LOD) and Limit of Quantification (LOQ)
Objective: To establish the lowest levels of analyte that can be reliably detected and quantified.
Methodology:
- Prepare samples at progressively lower concentrations approaching the expected detection/quantification limits
- Analyze multiple replicates across different runs to establish signal-to-noise ratios
- For LOD: Typically determined as the concentration where signal-to-noise ratio is 3:1
- For LOQ: Typically determined as the concentration where signal-to-noise ratio is 10:1
- Evaluate both LOD and LOQ as a percentage of tolerance [88]
Additional Consideration: If specifications are two-sided and the LOD/LOQ are below 80% of the lower specification limit, they are considered to have no practical impact on product quality assessment [88].
Protocol for Linearity Assessment
Objective: To demonstrate the linear response of the method across the specified range.
Methodology:
- Evaluate linearity across minimally 80-120% of product specification limits or wider
- Fit a linear regression line correlating signal versus theoretical concentration
- Save studentized residuals from the curve
- Add reference lines at +1.96 and -1.96 (95% confidence interval)
- Fit a quadratic fit to the studentized residuals
- The range where the curve remains within ±1.96 of studentized residuals defines the linear range [88]
Analytical Validation Workflow
The following diagram illustrates the complete analytical validation workflow within the computational research environment:
Troubleshooting Common Validation Issues
FAQ 1: How do we handle excessive method variability in large-scale datasets?
Issue: Method shows acceptable %CV but still causes high out-of-specification (OOS) rates.
Solution:
- Evaluate repeatability as a percentage of tolerance rather than relying solely on %CV
- Use the formula: Repeatability % Tolerance = (Stdev Repeatability × 5.15)/(USL-LSL) for two-sided specifications
- If repeatability consumes more than 25% of tolerance (50% for bioassays), optimize method to reduce variability [88]
Computational Consideration: In NGS workflows, variability may stem from data processing inconsistencies. Implement workflow engines to maintain consistency across analyses [10].
FAQ 2: How do we validate methods when product specifications are not yet available?
Issue: Early development phase without established specification limits.
Solution:
- Use traditional measures (%CV, % recovery) temporarily but document as "report-only"
- Establish preliminary acceptance criteria based on clinical relevance or prior knowledge
- Reevaluate and update acceptance criteria once specifications are defined [88]
- For genomic data, leverage public datasets like the 1000 Genomes Project to establish baseline expectations [10]
FAQ 3: How do we manage data integration from multiple sequencing platforms?
Issue: Inconsistent data formats across platforms hinder validation.
Solution:
- Develop interoperable analysis tools that can run on different computational platforms
- Establish data format conversion pipelines as part of the validation protocol
- Utilize centralized data storage with standardized access methods [3]
- Consider cloud-based solutions that can handle petabyte-scale data [10]
Table 2: Key Research Reagent Solutions for Analytical Validation
| Item | Function | Considerations for Large-Scale Studies |
|---|---|---|
| Reference Standards | Establish accuracy and bias for quantitative methods | Requires proper storage and handling across multiple research sites |
| Quality Control Materials | Monitor method performance over time | Should cover entire analytical measurement range |
| Sample Preparation Kits | Standardize extraction and processing | Batch-to-batch variability must be monitored |
| Computational Resources | Data processing and analysis | Cloud computing balances cost, performance, and customizability [10] |
| Data Storage Solutions | Manage large-scale genomic data | Distributed storage systems needed for petabyte-scale data [3] |
| Workflow Management Systems | Maintain reproducibility and scalability | Container technology enables portable analyses [10] |
Advanced Topics: Computational Infrastructure for Validation
Data Management Strategies
Large-scale chemogenomic NGS data requires sophisticated data management approaches:
- Centralized Data Storage: Housing data sets centrally and bringing high-performance computing to the data reduces transfer challenges [3]
- Access Control: Implementing proper access control mechanisms for unpublished data while facilitating collaboration [3]
- Data Transfer Alternatives: For terabyte to petabyte-scale data, physical storage device transfer may be more efficient than network transfer [3]
Workflow Optimization
The following diagram illustrates the relationship between computational resources and analytical validation parameters:
Performance Considerations
Understanding the nature of your computational problem is essential for efficient validation:
- Network-Bound Applications: Dependent on data transfer speeds; benefit from centralized data storage [3]
- Disk-Bound Applications: Require distributed storage solutions for processing extremely large datasets [3]
- Memory-Bound Applications: Demand substantial random access memory (RAM) for operations like weighted co-expression networks [3]
- Computationally-Bound Applications: Require specialized hardware accelerators for NP-hard problems like Bayesian network reconstruction [3]
Establishing robust analytical validation guidelines for sensitivity, specificity, and limits of detection requires a holistic approach that integrates traditional method validation principles with contemporary computational strategies. By implementing tolerance-based acceptance criteria and leveraging appropriate computational infrastructure, researchers can ensure their analytical methods are fit-for-purpose in the context of large-scale chemogenomic NGS data research. The frameworks presented here provide a foundation for maintaining data quality and reproducibility while navigating the complex computational landscape of modern genomic research.
Benchmarking Bioinformatics Pipelines and Algorithm Performance
Troubleshooting Guides
Guide 1: Resolving Pipeline Execution Failures
Problem: My bioinformatics pipeline fails during execution with unclear error messages. How do I diagnose the issue?
Solution:
- Check Error Logs: First, analyze error logs and outputs to pinpoint the specific stage of failure [71]. Pipeline management systems like Nextflow or Snakemake provide detailed error logs for debugging [71].
- Identify Error Type: Determine if the error provides detailed information or is a general system error. Some systems specifically categorize these as "Error with detailed information" versus "Error with no detailed information" [89].
- Examine Tool Dependencies: Ensure all required tools and correct versions are installed. Conflicts between software versions or missing dependencies can disrupt workflows [71]. For example, a pipeline might fail if a specific tool version like
toolshed.g2.bx.psu.edu/repos/iuc/quast/quast/5.0.2is missing [89]. - Verify Computational Resources: Monitor for computational bottlenecks. Insufficient memory, storage, or processing power can cause failures, especially with large datasets [71]. Consider migrating to cloud platforms with scalable computing power if resources are limited [71].
- Consult Galaxy History (if applicable): If using Galaxy-based systems, examine the Galaxy History ID associated with the failed run for detailed tool-specific error messages [89].
Guide 2: Addressing Data Quality Issues
Problem: My pipeline runs to completion, but the variant calling results show unexpected accuracy issues.
Solution:
- Implement Quality Control Checks: Use quality control tools like FastQC and MultiQC on raw sequencing data to identify contaminants, adapter sequences, or low-quality reads [71].
- Validate with Benchmarking Workflows: Employ standardized benchmarking workflows to assess variant calling performance against known truth sets [90]. The Genome in a Bottle (GIAB) consortium provides reference materials with established ground-truth calls for SNVs and small InDels [90].
- Compare Caller Performance: Evaluate different variant calling algorithms on your dataset. For example, benchmarking reveals that GATK HaplotypeCaller may outperform FreeBayes-based workflows in detecting small InDels (1–20 base pairs) [90].
- Stratify by Genomic Region: Assess performance characteristics specifically within your reportable ranges, as variant calling performance is not uniform across different genomic regions [90].
Frequently Asked Questions
Q1: How do I ensure my benchmarking results are reproducible?
A: Reproducibility requires tracking all components of your analysis environment [90]:
- Use version control systems like Git for pipeline scripts [71]
- Implement container technologies (Docker, Singularity) to capture software dependencies
- Utilize workflow management systems (Nextflow, Snakemake) for structured execution [71]
- Document all parameters, software versions, and reference files used [71]
- Choose benchmarking workflows that can detect changes to input files, software libraries, and underlying operating systems [90]
Q2: What are the most common performance metrics for evaluating variant calling pipelines?
A: Standard performance metrics include [90]:
- Specificity: Proportion of true negatives correctly identified
- Precision: Positive predictive value of variant calls
- Sensitivity: Proportion of true variants correctly detected
These metrics should be evaluated separately for different variant types (SNPs, InDels) and across genomic regions of interest [90].
Q3: My pipeline is running too slowly with large-scale genomic data. How can I improve performance?
A: Consider these optimization strategies:
- Parallelization: Distribute computationally intense tasks across multiple processors [3]
- Cloud Migration: Utilize scalable cloud computing resources (AWS, Google Cloud, Azure) that can dynamically allocate resources based on workload demands [71]
- Data Format Optimization: Use efficient data formats and consider quality score binning to reduce file sizes without significant information loss [10]
- Hardware Acceleration: Explore specialized hardware or heterogeneous computing environments for specific computational tasks [3]
Benchmarking Metrics and Tools
Table 1: Standardized Benchmarking Tools for Bioinformatics Pipelines
| Tool Name | Primary Function | Variant Type Coverage | Key Features |
|---|---|---|---|
| hap.py | Variant comparison | SNPs, InDels | Variant allele normalization, genotype matching [90] |
| vcfeval | Variant comparison | SNPs, InDels | Robust comparison accounting for alternative variant representations [90] |
| SURVIVOR | SV analysis | Structural Variants | Breakpoint matching for structural variants [90] |
Table 2: Performance Metrics for Variant Calling Evaluation
| Metric | Calculation | Optimal Range | Clinical Significance |
|---|---|---|---|
| Sensitivity | TP/(TP+FN) | >99% for clinical assays [90] | Ensures disease-causing variants are not missed |
| Specificity | TN/(TN+FP) | >99% for clinical assays [90] | Reduces false positives and unnecessary follow-up |
| Precision | TP/(TP+FP) | Varies by variant type and region [90] | Indicates reliability of reported variants |
Experimental Protocols
Protocol 1: Benchmarking Germline Variant Callers Using GIAB Reference Materials
Purpose: To evaluate the performance of germline variant calling pipelines for clinical diagnostic assays [90].
Materials:
- Reference Samples: Genome in a Bottle (GIAB) consortium reference samples (e.g., NA12878/HG001) [90]
- Validation Variants: Clinically relevant variants from CDC or other validated sources [90]
- Computational Resources: High-performance computing cluster or cloud computing environment
Methodology:
- Sequence Data Acquisition: Obtain whole genome or exome sequencing data for GIAB reference samples [90]
- Variant Calling: Process data through candidate variant calling pipelines (e.g., GATK HaplotypeCaller, SpeedSeq/FreeBayes) [90]
- Performance Assessment: Compare variant calls to GIAB truth sets using standardized benchmarking tools (hap.py, vcfeval) [90]
- Metric Calculation: Generate performance metrics (sensitivity, specificity, precision) stratified by:
- Variant type (SNPs, InDels of different sizes)
- Genomic region (exonic, splice-site, intronic)
- Functional significance (clinically relevant variants) [90]
- Statistical Analysis: Compare performance across pipelines to identify optimal workflows for specific variant types and genomic contexts [90]
Protocol 2: Reproducible Benchmarking in Cloud Environments
Purpose: To implement a scalable and reproducible benchmarking workflow independent of local computational infrastructure [90].
Materials:
- Cloud Platform: AWS, Google Cloud, or Azure account with appropriate storage and computing resources
- Container Technology: Docker or Singularity for environment reproducibility
- Workflow Management: Nextflow, Snakemake, or similar workflow management system [71]
Methodology:
- Workflow Containerization: Package all software dependencies in containers to ensure consistent execution environments [90]
- Data Management: Establish standardized data storage and retrieval protocols, potentially using centralized data repositories [10]
- Pipeline Implementation: Deploy benchmarking workflow on cloud infrastructure with automated provisioning of computational resources [90]
- Result Tracking: Implement version control and metadata capture for all analysis steps to ensure complete reproducibility [90]
- Performance Monitoring: Track computational efficiency metrics (runtime, cost, scalability) alongside analytical performance [90]
Workflow Visualization
Benchmarking Workflow for Variant Calling Pipelines
Troubleshooting Decision Tree for Pipeline Failures
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Resources
| Resource Type | Specific Examples | Function/Purpose |
|---|---|---|
| Reference Materials | GIAB samples (NA12878/HG001) [90] | Provide ground-truth variant calls for benchmarking and validation |
| Clinical Variant Sets | CDC validated variants [90] | Assess performance on clinically relevant mutations |
| Benchmarking Tools | hap.py, vcfeval, SURVIVOR [90] | Standardized comparison of variant calls against truth sets |
| Workflow Management | Nextflow, Snakemake, Galaxy [71] | Orchestrate complex analytical pipelines and ensure reproducibility |
| Quality Control Tools | FastQC, MultiQC, Trimmomatic [71] | Assess data quality and identify potential issues early in pipeline |
| Container Platforms | Docker, Singularity | Create reproducible computational environments independent of host system |
Next-generation sequencing (NGS) has revolutionized genomics research, with Illumina, Oxford Nanopore Technologies (ONT), and Pacific Biosciences (PacBio) representing the leading platforms. Each technology offers distinct advantages and limitations that make them suitable for different research applications, particularly in large-scale chemogenomic studies where computational demands and data accuracy are paramount considerations.
Illumina technology dominates the short-read sequencing market, utilizing a sequencing-by-synthesis approach with reversible dye-terminators. This platform generates massive volumes of short reads (typically 50-300 bp) with very high accuracy, making it ideal for applications requiring precise base calling, such as variant detection and expression profiling [91] [92]. However, its short read length limits its ability to resolve complex genomic regions, structural variants, and highly repetitive sequences.
Oxford Nanopore Technologies employs a fundamentally different approach based on measuring changes in electrical current as DNA or RNA strands pass through protein nanopores. This technology produces exceptionally long reads (potentially exceeding 100 kb) and offers unique capabilities for real-time sequencing and direct detection of base modifications [93] [94]. While traditionally associated with higher error rates, recent improvements in flow cells (R10.4) and basecalling algorithms have significantly enhanced accuracy [94] [95].
Pacific Biosciences utilizes Single Molecule Real-Time (SMRT) sequencing, which monitors DNA synthesis in real-time within tiny wells called zero-mode waveguides (ZMWs). The platform's HiFi mode employs circular consensus sequencing (CCS) to generate long reads (15-20 kb) with exceptional accuracy (>99.9%) by sequencing the same molecule multiple times [93] [96] [95]. This combination of length and accuracy makes it particularly valuable for detecting structural variants, phasing haplotypes, and assembling complex genomes.
Technical Comparison Tables
Table 1: Core Technology Specifications
| Parameter | Illumina | Oxford Nanopore | PacBio |
|---|---|---|---|
| Technology | Sequencing-by-synthesis | Nanopore electrical signal detection | Single Molecule Real-Time (SMRT) |
| Read Length | 50-300 bp [92] | 20 bp -> 100+ kb [93] [94] | 500 bp - 20+ kb [93] |
| Accuracy | >99.9% (Q30) [92] | ~96-98% (Q20) with R10.4 [94] [95] | >99.9% (Q30+) with HiFi [93] [96] |
| Error Profile | Low, primarily substitution errors [91] | Higher, systematic indels in homopolymers [95] [97] | Random errors corrected via CCS [95] |
| DNA Input | Low, amplified | Low, native DNA | Moderate, native DNA |
| Run Time | 1-3.5 days | 1-72 hours [93] [97] | 0.5-30 hours |
| Real-time Analysis | No | Yes [94] | Limited |
Table 2: Application Suitability
| Application | Illumina | Oxford Nanopore | PacBio |
|---|---|---|---|
| Whole Genome Sequencing | Excellent for SNVs, small indels | Good for structural variants, repeats | Excellent for structural variants, phasing |
| Transcriptomics | Standard for RNA-seq | Direct RNA sequencing, isoform detection | Full-length isoform sequencing |
| Epigenetics | Bisulfite sequencing required | Direct detection of modifications [93] | Direct detection of 5mC, 6mA [93] |
| Metagenomics | High sensitivity for species ID | Long reads aid binning, real-time [94] [97] | High accuracy for species/strain ID |
| Antimicrobial Resistance | Limited by short reads | Excellent for context & plasmids [94] [98] | High confidence variant calling |
| Portability | Benchtop systems only | MinION is portable [93] [94] | Large instruments only |
Table 3: Computational Requirements and Costs
| Factor | Illumina | Oxford Nanopore | PacBio |
|---|---|---|---|
| Data per Flow Cell/Run | 20 GB - 1.6 TB | 50-200 Gb per PromethION cell [93] [99] | 30-120 Gb per SMRT Cell [93] |
| Raw Data Format | FASTQ (compressed) | FAST5/POD5 (~1.3 TB) [93] | BAM (60 GB Revio) [93] |
| Basecalling | On-instrument | Off-instrument, requires GPU [93] | On-instrument |
| Storage Cost/Month* | ~$0.46-36.80 | ~$30.00 [93] | ~$0.69-1.38 [93] |
| Primary Analysis | Standard pipelines | GPU-intensive basecalling [93] | CCS generation |
| Instrument Cost | Moderate-high | Low (MinION) to high (PromethION) | High |
Based on AWS S3 Standard cost of $0.023 per GB [93]
FAQs: Addressing Researcher Questions
Q1: Which platform is most suitable for identifying structural variants in cancer genomes?
A: PacBio HiFi sequencing is generally superior for comprehensive structural variant detection due to its combination of long reads and high accuracy. HiFi reads can span most repetitive regions and large structural variants while maintaining base-level precision sufficient to identify breakpoints precisely [93] [96]. Oxford Nanopore provides longer reads that can span even larger repeats but with higher error rates that may complicate precise breakpoint identification. Illumina's short reads are poor for detecting large structural variants but excel at identifying single nucleotide variants and small indels. For cancer genomics, a hybrid approach using Illumina for point mutations and PacBio for structural variants often provides the most comprehensive view.
Q2: How do computational requirements differ between platforms for large-scale studies?
A: Computational demands vary significantly:
- Illumina: Moderate requirements focused on alignment and variant calling. Storage needs are high but manageable with standard compression.
- Oxford Nanopore: Extremely demanding due to raw signal data (FAST5/POD5 files can reach ~1.3 TB per genome) and GPU-intensive basecalling. The PromethION A-Series requires 4× NVIDIA Ampere GPU cards, 512 GB RAM, and 60 TB SSD storage [93] [99]. Real-time analysis is possible but requires substantial computational infrastructure.
- PacBio: Moderate computational requirements once HiFi reads are generated. The Revio system performs basecalling on-instrument, significantly reducing downstream computational burden. Storage needs are moderate (~60 GB per Revio run) [93].
For large-scale chemogenomic studies involving hundreds of samples, Illumina and PacBio have more manageable computational requirements compared to Oxford Nanopore's substantial data processing and storage demands.
Q3: What are the key considerations for metagenomics studies involving complex microbial communities?
A: Platform selection depends on study goals:
- Species-level profiling: Illumina with 16S rRNA sequencing (V3-V4 regions) provides cost-effective community overview but limited resolution [97].
- Strain-level resolution: Oxford Nanopore's full-length 16S sequencing (~1,500 bp) enables precise taxonomic classification to species level [97].
- Functional potential: Both long-read technologies excel at recovering complete genes and operons from metagenomes. Oxford Nanopore is particularly valuable for identifying antibiotic resistance genes with their genomic context (plasmids, transposons) [94] [98].
- Real-time applications: Oxford Nanopore enables adaptive sampling during sequencing, allowing enrichment of low-abundance taxa without additional wet-lab work.
Recent studies show Illumina captures greater species richness in complex microbiomes, while Oxford Nanopore provides better resolution for dominant species and mobile genetic elements [97] [98].
Q4: How has accuracy improved for long-read technologies in recent years?
A: Significant improvements have been made:
- PacBio: HiFi sequencing achieves >99.9% accuracy through circular consensus sequencing, making it comparable to short-read technologies [93] [96] [95]. Error rates have decreased from ~15% in early continuous long reads to <0.1% with HiFi.
- Oxford Nanopore: Accuracy has dramatically improved from ~65% with R6 flow cells to ~96-98% with R10.4 chemistry and Q20+ kits [94] [95]. The R10 pore's dual reader head design particularly improves accuracy in homopolymer regions, a traditional weakness. Advanced basecallers like Dorado using deep learning further enhance accuracy.
These improvements have made both technologies suitable for clinical applications where high accuracy is critical, though PacBio maintains an accuracy advantage while Oxford Nanopore offers superior read lengths.
Troubleshooting Guides
Issue 1: Low-Quality Bases in Oxford Nanopore Data
Symptoms: High error rates, particularly in homopolymer regions; low Q-score; failed quality control metrics.
Solutions:
- Wet Lab:
- Use high-quality, high-molecular-weight DNA (check fragment size with FEMTO Pulse or Tapestation)
- Avoid excessive DNA shearing during extraction
- Follow library preparation protocols precisely, especially for DNA end-repair
- Dry Lab:
- Use latest basecalling model (e.g., Dorado super-accuracy mode)
- Apply adaptive sampling to focus sequencing on target regions
- Implement read filtering by Q-score (minimum Q10 for most applications)
- Use Medaka for additional polishing of consensus sequences
Prevention: Regular flow cell QC, use of R10.4.1 flow cells for improved homopolymer accuracy, and standardized DNA extraction protocols across samples [94] [95] [97].
Issue 2: Insufficient Coverage in PacBio HiFi Data
Symptoms: Incomplete genome assembly; gaps in coverage; low consensus accuracy.
Solutions:
- Wet Lab:
- Optimize DNA extraction to maximize molecular weight
- Use optimal DNA:polymerase ratio in SMRTbell preparation
- Size-select library to target appropriate insert size (15-20 kb for Revio)
- Dry Lab:
- Increase sequencing depth - target 20-30× for WGS, higher for complex regions
- Combine multiple SMRT cells if necessary
- Use alignment tools optimized for HiFi data (pbmm2, minimap2)
Prevention: Accurate DNA quantification, use of internal controls, and regular instrument calibration according to manufacturer specifications.
Issue 3: High Computational Demands for Oxford Nanopore Basecalling
Symptoms: Slow processing speeds; inadequate GPU memory errors; extended analysis times.
Solutions:
- Hardware:
- Ensure adequate GPU resources (NVIDIA Ampere architecture recommended)
- Allocate sufficient RAM (minimum 32 GB, 512 GB for PromethION scale) [99]
- Use high-speed SSDs for temporary storage during basecalling
- Software:
- Use Dorado basecaller for improved speed and accuracy
- Implement basecalling during sequencing (real-time)
- Consider basecalling after sequencing with optimized batch sizes
- Use Oxford Nanopore's high-performance computing recommendations [99]
Alternative Approach: Use cloud computing resources (AWS, Google Cloud, Azure) with GPU instances for large-scale projects to avoid capital expenditure on expensive hardware.
Experimental Protocols for Key Applications
Protocol 1: Full-Length 16S rRNA Sequencing for Microbiome Analysis (Oxford Nanopore)
Principle: Amplify and sequence the entire ~1,500 bp 16S rRNA gene to achieve species-level taxonomic resolution [97].
Materials:
- ONT 16S Barcoding Kit 24 V14 (SQK-16S114.24)
- MinION Flow Cell (R10.4.1 recommended)
- MinION Mk1C or GridION
- Qubit Fluorometer for DNA quantification
Procedure:
- DNA Extraction: Use mechanical lysis with bead beating for comprehensive cell disruption.
- PCR Amplification:
- Amplify full-length 16S gene with barcoded primers (25 cycles)
- Conditions: 95°C × 2 min; [95°C × 20 s, 55°C × 30 s, 65°C × 2 min] × 25; 65°C × 5 min
- Library Preparation:
- Pool barcoded samples in equimolar ratios
- Prepare sequencing library per kit instructions
- Sequencing:
- Load library onto flow cell
- Run for 24-72 hours using MinKNOW software
- Analysis:
- Basecall with Dorado (HAC model)
- Demultiplex with Guppy or Dorado
- Taxonomic classification with EPI2ME 16S Workflow or custom pipeline
Computational Notes: A 72-hour run generates ~5-10 GB data; analysis requires 16 GB RAM and 4 CPU cores for timely processing [97].
Protocol 2: Structural Variant Detection in Human Genomes (PacBio HiFi)
Principle: Use long, accurate HiFi reads to identify structural variants >50 bp with high precision [93] [96].
Materials:
- PacBio Revio or Sequel IIe system
- SMRTbell prep kit 3.0
- BluePippin or SageELF for size selection
- Qubit Fluorometer for DNA quantification
Procedure:
- DNA Extraction:
- Use fresh-frozen blood or tissue
- Extract HMW DNA with MagAttract HMW DNA Kit
- Assess quality: DNA integrity number (DIN) >8.0
- Library Preparation:
- Shear DNA to 15-20 kb target size (Megaruptor or g-Tubes)
- Repair DNA ends and ligate SMRTbell adapters
- Size-select with BluePippin (15-20 kb window)
- Sequencing:
- Bind polymerase to SMRTbell templates
- Load on Revio SMRT Cell (up to 8M ZMWs)
- Run for 24-30 hours with HiFi sequencing mode
- Analysis:
- Generate HiFi reads using SMRT Link CCS algorithm (minimum 3 full passes)
- Map to reference genome (pbmm2 or minimap2)
- Call SVs with pbsv, Sniffles, or PBSV2
- Annotate with AnnotSV or similar tool
Quality Metrics: Target >20× coverage, Q30 average read quality, mean read length >15 kb.
Technology Selection Workflow
Figure 1: A workflow to guide selection of sequencing technology based on primary research application and requirements.
Computational Analysis Pipeline
Figure 2: Computational analysis pipeline showing divergent paths for different sequencing technologies converging on common analysis goals.
Research Reagent Solutions
Table 4: Essential Research Reagents and Kits
| Reagent/Kits | Function | Platform | Key Applications |
|---|---|---|---|
| QIAseq 16S/ITS Region Panel | Amplifies V3-V4 regions | Illumina | 16S rRNA microbiome studies [97] |
| ONT 16S Barcoding Kit 24 V14 | Full-length 16S amplification | Oxford Nanopore | Species-level microbiome profiling [97] |
| SMRTbell Prep Kit 3.0 | Library preparation for SMRT sequencing | PacBio | HiFi sequencing for SV detection |
| Ligation Sequencing Kit V14 | Standard DNA library prep | Oxford Nanopore | Whole genome sequencing [99] |
| NBD114.24 Native Barcoding | Multiplexing for native DNA | Oxford Nanopore | Cost-effective sequencing of multiple samples |
| MagAttract HMW DNA Kit | High molecular weight DNA extraction | All platforms | Optimal long-read sequencing results |
The choice between Illumina, Oxford Nanopore, and PacBio technologies depends critically on research objectives, computational resources, and specific application requirements. Illumina remains the workhorse for high-accuracy short-read applications, while PacBio HiFi sequencing provides an optimal balance of read length and accuracy for structural variant detection and genome assembly. Oxford Nanopore offers unique capabilities in real-time sequencing, ultra-long reads, and direct detection of epigenetic modifications.
For large-scale chemogenomic studies, computational demands vary dramatically between platforms, with Oxford Nanopore requiring substantial GPU resources for basecalling, while PacBio performs this step on-instrument. Illumina's established analysis pipelines and moderate computational requirements make it accessible for most laboratories. As sequencing technologies continue to evolve, accuracy improvements and cost reductions are making all three platforms viable for increasingly diverse applications in genomics research and clinical diagnostics.
Researchers should carefully consider their specific needs for read length, accuracy, throughput, and computational resources when selecting a sequencing platform, and may benefit from hybrid approaches that leverage the complementary strengths of multiple technologies.
Clinical validation is a critical step in translating computational drug discoveries into real-world therapies. It provides the supporting evidence needed to advance a predicted drug candidate along the development pipeline, moving from a computational hypothesis to a clinically beneficial treatment [100]. For researchers working with large-scale chemogenomic NGS data, this process involves specific challenges, from selecting the right validation strategy to troubleshooting complex, data-intensive workflows. This guide addresses common questions and provides methodologies to robustly correlate your computational findings with patient outcomes.
Frequently Asked Questions (FAQs)
FAQ 1: What are the main types of validation for computational drug repurposing predictions?
There are two primary categories of validation methods [100]:
- Computational Validation: This method uses independent data sources to provide supporting evidence without new laboratory work. Common approaches include:
- Retrospective Clinical Analysis: Using Electronic Health Records (EHR) or insurance claims data to find evidence of off-label drug efficacy, or searching clinical trial registries (e.g., ClinicalTrials.gov) to see if a drug is already being tested for the new indication.
- Literature Support: Manually searching or systematically mining existing biomedical literature for published connections between a drug and a disease.
- Public Database Search: Leveraging independent protein interaction, gene expression, or other biological databases to find supporting evidence for the predicted drug-disease link.
- Non-Computational Validation: This involves generating new evidence through experiments or expert review. Methods include:
- In vitro, in vivo, or ex vivo experiments.
- Prospective clinical trials specifically designed for drug repurposing.
- Formal review of predictions by clinical and domain experts.
FAQ 2: Why is prospective validation considered the "gold standard" for AI/ML models in drug development?
Prospective evaluation in clinical trials is crucial because it assesses how an AI system performs when making forward-looking predictions in real-world conditions, as opposed to identifying patterns in historical data [101]. This process helps uncover issues like data leakage or overfitting and evaluates the model's integration into actual clinical workflows. For AI tools claiming a direct clinical benefit, regulatory acceptance often requires rigorous validation through Randomized Controlled Trials (RCTs) to demonstrate a statistically significant and clinically meaningful impact on patient outcomes [101].
FAQ 3: I am getting a "no space left on device" error despite having free storage. What could be wrong?
This common error in high-performance computing (HPC) environments can have causes beyond exceeding your storage quota [102]:
- Incorrect File Permissions: In shared project directories, files must have the correct group ownership. If the 'sticky bit' is not set on a subdirectory, you may encounter this error. You can fix it with the command:
chmod g+s directory_name. - Incorrect Group during Compilation: When compiling code, the process might use your primary Unix group. If this group doesn't have permission to write to the installation directory, it can cause a "no space" error. Switch to your research group using
newgrp group-namebefore installing. - Moving vs. Copying Files: Sometimes, moving (
mv) files from a location with different permissions can fail. Using the copy (cp) command instead can resolve this.
FAQ 4: How can I estimate the required sequencing coverage for my whole-genome study?
Coverage is calculated using a standard formula [103]:
Coverage = (Read length) × (Total number of reads) ÷ (Genome size)
The recommended coverage depends entirely on the research goal [103]:
| Research Goal | Recommended Coverage |
|---|---|
| Germline / frequent variant analysis | 20x - 50x |
| Somatic / rare variant analysis | 100x - 1000x |
| De novo assembly | 100x - 1000x |
FAQ 5: My computational job is stuck in "Eqw" (error) status. How can I diagnose it?
An "Eqw" status typically means your job could not start due to a jobscript error [104]. To investigate:
- Use the
qstat -j <job_ID>command to get a truncated error message. - For the full error, use
qexplain <job_ID>. If this command is not found, load the required module first:module load userscripts. - The most common reason is that a file or directory specified in your jobscript does not exist. Note that creating the missing directory after the job is in "Eqw" will not fix the job; you must delete and re-submit it [104].
Experimental Protocols for Validation
Protocol 1: Computational Validation via Retrospective Clinical Analysis
This protocol uses existing clinical data to validate a computational prediction that "Drug A" could be repurposed for "Disease B" [100].
- Objective: To find evidence in clinical records or trial registries that supports the hypothesized efficacy of Drug A for Disease B.
- Materials:
- Clinical Data: Access to de-identified Electronic Health Record (EHR) or insurance claims data.
- Trial Registry: Access to ClinicalTrials.gov or other regional clinical trial registries.
- Methodology:
- EHR/Claims Analysis:
- Identify a cohort of patients diagnosed with Disease B.
- Within this cohort, identify a subgroup that was treated with Drug A (likely for an unrelated, pre-existing condition).
- Compare the outcomes (e.g., disease progression, survival) of the group treated with Drug A against a matched control group that was not.
- A statistically significant improvement in outcomes in the treated group provides strong validation.
- Clinical Trial Registry Search:
- Search ClinicalTrials.gov for interventional studies that list both "Drug A" and "Disease B".
- The existence of a trial, especially in Phase II or III, is a powerful validation signal. The phase of the trial indicates the level of prior validation it has already passed [100].
- EHR/Claims Analysis:
- Troubleshooting:
- Data Accessibility: Clinical data often has privacy and access restrictions [100]. Plan for data use agreements and secure computing environments.
- Confounding Factors: In EHR analysis, ensure patient groups are well-matched to reduce the influence of confounding variables on the outcome.
Protocol 2: Experimental Validation using the IDACombo Framework for Drug Combinations
This protocol outlines how to validate predictions of drug combination efficacy based on the principle of Independent Drug Action (IDA), which posits that a combination's effect equals that of its single most effective drug [105].
- Objective: To experimentally test the in vitro efficacy of a predicted drug combination and compare the results to the IDA-based prediction.
- Materials:
- Cancer cell line panel (e.g., from NCI-60 or other screens).
- Monotherapy dose-response data for the drugs in the combination.
- In vitro drug combination screening platform.
- Methodology:
- Prediction: Use the IDACombo method on monotherapy screening data (e.g., from GDSC or CTRPv2) to predict the viability of cells treated with the drug combination.
- Experiment:
- Culture the cancer cell lines used in the prediction.
- Treat them with the drug combination at clinically relevant concentrations.
- Measure cell viability after treatment.
- Validation: Compare the experimentally measured combination viability to the IDACombo prediction. A strong correlation (e.g., Pearson’s r > 0.9, as demonstrated in the NCI-ALMANAC dataset) validates the predictive model [105].
- Troubleshooting:
- Discrepancy Between Prediction and Experiment: Large deviations may indicate drug synergy or antagonism, which the IDA model does not account for. Investigate the specific drug interaction.
- Cross-Dataset Validation: Be aware that predictions made with data from one screening dataset (e.g., GDSC) may show weaker correlation when validated experimentally in another system (e.g., NCI-ALMANAC) due to differences in methodology and cell line composition [105].
The workflow below illustrates the key steps for correlating computational findings with clinical outcomes, integrating both computational and experimental validation paths.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and resources used in the computational and experimental workflows described above.
| Item Name | Function / Explanation | Example Use Case |
|---|---|---|
| Public Genomic Databases | Provide large-scale reference data for analysis and validation. | Using 1000 Genomes Project data as a reference panel for genotype imputation [10]. |
| Cell Line Screening Datasets | Contain monotherapy drug response data for many compounds across many cell lines. | Using GDSC or CTRPv2 data with the IDACombo method to predict drug combination efficacy [105]. |
| Clinical Trial Registries | Databases of ongoing and completed clinical trials worldwide. | Searching ClinicalTrials.gov to validate if a predicted drug-disease link is already under investigation [100]. |
| High-Performance Computing (HPC) | Provides the computational power needed for large-scale NGS data analysis and complex modeling. | Running Bayesian network reconstruction or managing petabyte-scale genomic data [3]. |
| Structured Safety Reporting Framework | A digital system for submitting and analyzing safety reports in clinical trials. | The FDA's INFORMED pilot project streamlined IND safety reporting, saving hundreds of review hours [101]. |
| Bioinformatics Pipelines | A structured sequence of tools for processing NGS data (e.g., QC, alignment, variant calling). | Using FastQC for quality control, BWA for read alignment, and GATK for variant calling in WGS analysis [106] [107]. |
Clinical Trial Prediction & Validation Workflow
For AI/ML models in drug development, validating predictions against clinical trial outcomes is a robust method. The following diagram details the workflow for a study predicting the success of first-line therapy trials, which achieved high accuracy [105].
Technical Support Center: mNGS Troubleshooting & FAQs
This technical support center addresses common challenges researchers face when implementing mNGS for detecting pathogens in the context of drug-related infections and chemogenomic research.
Frequently Asked Questions
Q1: Our mNGS runs consistently yield low amounts of microbial DNA, resulting in poor pathogen detection. What could be the cause?
Low library yield in mNGS can stem from several issues in the sample preparation workflow [5]. The table below outlines primary causes and corrective actions.
| Primary Cause | Mechanism of Yield Loss | Corrective Action |
|---|---|---|
| Poor Input Quality / Contaminants | Enzyme inhibition from residual salts, phenol, or EDTA. [5] | Re-purify input sample; ensure wash buffers are fresh; target high purity (260/230 > 1.8). [5] |
| Inaccurate Quantification | Over- or under-estimating input concentration leads to suboptimal enzyme stoichiometry. [5] | Use fluorometric methods (Qubit) over UV absorbance; calibrate pipettes. [5] |
| Inefficient Host DNA Depletion | Microbial nucleic acids are dominated by host background (>99% of reads). [108] [109] | Optimize host depletion steps (e.g., differential lysis, saponin treatment, nuclease digestion). [110] [111] |
| Suboptimal Adapter Ligation | Poor ligase performance or incorrect molar ratios reduce adapter incorporation. [5] | Titrate adapter-to-insert molar ratios; ensure fresh ligase and buffer. [5] |
Q2: We are getting false-positive results, including environmental contaminants and index hopping artifacts. How can we improve specificity?
Improving specificity requires addressing both laboratory and bioinformatic procedures [110] [108].
- Wet-Lab Controls: Always include negative (no-template) controls and positive controls in every sequencing run to identify background contamination and confirm assay sensitivity. [111]
- Combat Index Hopping: On Illumina platforms, barcode index switching can cause cross-contamination between samples. [108] Use unique dual indexing (UDI) to mitigate this issue.
- Bioinformatic Filtering: Use a robust bioinformatic pipeline that filters out background contamination by comparing sequence reads to a database of common contaminants and establishing minimum read count thresholds based on control samples. [110]
Q3: The high computational cost and data volume of mNGS are prohibitive for our large-scale chemogenomic data research. What are the solutions?
Managing the computational demands of mNGS is a recognized challenge. [110] [3] Consider the following approaches:
- Cloud Computing: Leverage cloud platforms (e.g., Google Cloud Platform, Amazon Web Services) to access scalable, on-demand computational resources and avoid maintaining expensive local infrastructure. [3] [10]
- Targeted NGS (tNGS): For specific research questions, use tNGS panels that enrich for predefined pathogen and antimicrobial resistance gene targets. This method reduces sequencing data volume, lowers costs, and simplifies analysis while maintaining high sensitivity for targeted organisms. [110] [112]
- Standardized Pipelines: Implement standardized, portable bioinformatic pipelines using container technologies (e.g., Docker, Singularity) to ensure reproducibility and efficient use of computational resources. [10]
Quantitative Performance Data for mNGS
The performance of mNGS must be evaluated against other diagnostic methods. The following table summarizes key comparative data.
Table 1: Comparative Diagnostic Performance of mNGS and Other Methods
| Method | Typical Diagnostic Yield / Coincidence Rate | Key Advantages | Key Limitations |
|---|---|---|---|
| Metagenomic NGS (mNGS) | 63% in CNS infections vs <30% for conventional methods; [110] Coincidence rate of 73.9% in LRTIs [112] | Hypothesis-free, unbiased detection; can identify novel/rare pathogens and co-infections. [110] [108] | High host background; costly; complex data analysis; requires specialized expertise. [110] [109] |
| Targeted NGS (tNGS) | Coincidence rate of 82.9% in LRTIs; [112] Higher detection rate than culture (75.2% vs 19.0%) [112] | Faster and more cost-effective than mNGS; optimized for clinically relevant pathogens and AMR genes. [112] | Limited to pre-defined targets; cannot discover novel organisms. [110] [112] |
| Culture | Considered gold standard but low sensitivity (e.g., 19.0% in LRTIs); impaired by prior antibiotic use. [112] [109] | Enables antibiotic susceptibility testing; inexpensive. [108] [109] | Slow (days to weeks); cannot detect non-culturable or fastidious organisms. [110] [109] |
| Multiplex PCR | Rapid turnaround time. [108] | Rapid; able to detect multiple pre-defined organisms simultaneously. [108] | Limited target range; requires prior hypothesis; low specificity for some organisms. [108] |
CNS: Central Nervous System; LRTIs: Lower Respiratory Tract Infections; AMR: Antimicrobial Resistance.
Detailed Experimental Protocols for mNGS
Protocol 1: Standard mNGS Wet-Lab Workflow for Liquid Samples (e.g., BALF, CSF)
This protocol outlines a standard shotgun metagenomics approach for pathogen detection. [110] [108]
- Sample Processing: Centrifuge the sample to pellet cells. For respiratory samples like Bronchoalveolar Lavage Fluid (BALF), use a host depletion step, such as treatment with saponin solution, to lyse and remove human cells. [111]
- Nucleic Acid Extraction: Extract total nucleic acid (DNA and RNA) from the supernatant or pellet using a broad-spectrum kit (e.g., MagMAX Viral/Pathogen Nucleic Acid Isolation Kit). [112] [111]
- Library Preparation:
- DNA Sequencing: For DNA-based pathogen detection, the extracted DNA is fragmented (via enzymatic tagmentation or sonication), end-repaired, and ligated to sequencing adapters. [108] [111] A limited-cycle PCR amplification incorporates barcodes for sample multiplexing. [108]
- Dual DNA/RNA Sequencing: To comprehensively detect all pathogen types, split the extract. Process DNA as above. For the RNA fraction, perform random reverse transcription (using 9N primers) to generate cDNA, which is then PCR-amplified with barcoded primers. [112] [111]
- Library QC and Pooling: Quantify final libraries using a fluorometric method (e.g., Qubit dsDNA HS Assay). Pool barcoded libraries in equimolar ratios. [5] [111]
- Sequencing: Sequence the pooled library on a high-throughput platform (e.g., Illumina NovaSeq) for short-read sequencing or an Oxford Nanopore Technologies (ONT) device for real-time, long-read sequencing. [110] [108]
Protocol 2: A Rapid Metagenomic Sequencing Workflow for Critical Cases
For scenarios requiring faster results, a rapid nanopore-based protocol can be employed. [111]
- Rapid Host Depletion & Extraction: Use an optimized, rapid protocol for respiratory samples involving bead-beating in a Matrix Lysing E tube with Sputasol, followed by nucleic acid extraction. [111]
- Rapid Library Prep: Use a kit like the Rapid PCR Barcoding Kit (SQK-RPB114.24). The process involves a single-tube tagmentation and PCR amplification step, significantly reducing hands-on time. The entire library preparation can be completed in approximately 5 hours. [111]
- Real-Time Sequencing: Load the library onto an ONT MinION or GridION flow cell (e.g., R10.4.1). Sequencing and basecalling occur in real-time, allowing for preliminary analysis within hours of starting the run. [110] [111]
mNGS Experimental and Computational Workflows
The following diagram illustrates the core steps of a standard mNGS experiment, from sample to diagnosis, highlighting key decision points.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for mNGS Experiments
| Item | Function / Application | Example Product / Note |
|---|---|---|
| Host Depletion Reagents | Selectively lyse human cells or digest host nucleic acids to increase microbial sequencing depth. [110] [111] | Saponin solution; HL-SAN Triton Free DNase. [111] |
| Nucleic Acid Extraction Kit | Isolate total DNA and RNA from a wide variety of pathogens in complex clinical matrices. | MagMAX Viral/Pathogen Nucleic Acid Isolation Kit. [111] |
| Library Preparation Kit | Fragment DNA, attach sequencing adapters, and amplify libraries for sequencing. | Rapid PCR Barcoding Kit (SQK-RPB114.24) for ONT; various Illumina-compatible kits. [108] [111] |
| Reverse Transcriptase & Primers | For RNA virus detection: convert RNA to cDNA for sequencing. [111] | Maxima H Minus Reverse Transcriptase with RLB RT 9N random primers. [111] |
| Magnetic Beads | Purify and size-select nucleic acids after extraction, fragmentation, and PCR amplification. | Agencourt AMPure XP beads. [111] |
| Quantification Assay | Accurately measure concentration of amplifiable DNA libraries, critical for pooling. | Qubit dsDNA HS Assay Kit (fluorometric). [5] [111] |
| Bioinformatic Databases | Reference databases for classifying sequencing reads and identifying pathogens and AMR genes. | NCBI Pathogen Detection Project with AMRFinderPlus; GenBank. [110] [113] |
Conclusion
The computational demands of large-scale chemogenomic NGS are formidable but not insurmountable. Success hinges on a synergistic strategy that integrates scalable cloud infrastructure, sophisticated AI and multi-omics analytical methods, rigorously optimized and standardized pipelines, and robust validation frameworks. The future of computational chemogenomics points toward the routine use of integrated multi-omics from a single sample, the deepening application of foundation models and transfer learning for drug response prediction, and the continued decentralization of sequencing power to individual labs. By systematically addressing these computational challenges, researchers can fully unlock the potential of chemogenomic data, dramatically accelerating the discovery of novel therapeutic targets and the realization of truly personalized medicine, ultimately translating complex data into actionable clinical insights that improve patient outcomes.
References
- 1. Advancing Computational Toxicology in the Big Data Era by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6688471/]
- 2. What Are the 3 V's of Big Data? [https://www.techtarget.com/whatis/definition/3Vs]
- 3. Computational solutions to large-scale data management and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3124937/]
- 4. Chemogenomic library design strategies for precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10359939/]
- 5. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 6. NGS Software Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-software-support/ngs-software-support-troubleshooting.html]
- 7. Support | NCI Genomic Data Commons [http://gdc.cancer.gov/support]
- 8. Troubleshooting Your First NGS Dataset [https://genomebeans.com/blog/troubleshooting-your-first-ngs-dataset-how-genomebeans-simplifies-it]
- 9. Sanger DNA Sequencing: Troubleshooting [https://dnacore.mgh.harvard.edu/new-cgi-bin/site/pages/sequencing_pages/seq_troubleshooting.jsp]
- 10. Practical guide for managing large-scale human genome ... [https://www.nature.com/articles/s10038-020-00862-1]
- 11. Scream If You Wanna Go FASTA: Breaking the Bottleneck in... [https://www.technologynetworks.com/informatics/articles/scream-if-you-wanna-go-fasta-breaking-the-bottleneck-in-genomic-data-analysis-328366]
- 12. From FastQ data to high confidence variant calls: the Genome Analysis... [https://pubmed.ncbi.nlm.nih.gov/25431634/]
- 13. Predicting drug-target interactions using machine learning ... [https://www.nature.com/articles/s41598-025-03932-6]
- 14. Machine learning-based drug-drug interaction prediction [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344460/]
- 15. AI for Genomics: The 2025 Revolution [https://lifebit.ai/blog/ai-for-genomics/]
- 16. Sequencing Data Analysis | NGS software to help you ... [https://www.illumina.com/informatics/sequencing-data-analysis.html]
- 17. Artificial intelligence-based computational framework for drug ... [https://alzres.biomedcentral.com/articles/10.1186/s13195-021-00826-3]
- 18. AI Compute Demand in Biotech: 2025 Report & Statistics [https://intuitionlabs.ai/articles/ai-compute-demand-biotech]
- 19. Genomic Data Transfer & Storage Cloud Solutions [https://aws.amazon.com/health/genomics/solutions/data-transfer-and-storage/]
- 20. Complete Guide to Genomics Data Storage [https://www.weka.io/learn/cloud-storage/genomics-data-storage/]
- 21. Genomic & NGS Data Storage [https://www.illumina.com/informatics/infrastructure-pipeline-setup/genomic-data-storage-security.html]
- 22. Investigating reproducibility and tracking provenance [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-017-1747-0]
- 23. Cybersecurity in genomics and personalized medicine ... [https://www.manageengine.com/log-management/cyber-security/data-security-genomics-personalized-medicine.html]
- 24. Balancing Innovation with Privacy and Equity [https://americanpharmacogenomicsassociation.com/legal/ethical-dilemmas-in-pharmacogenomics/]
- 25. Using Ethereum blockchain to store and query pharmacogenomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7268467/]
- 26. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 27. Pharmacogenomics Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/pharmacogenomics-support/pharmacogenomics-support-troubleshooting.html]
- 28. 2025 Trends: NGS [https://www.genengnews.com/topics/genome-editing/2025-trends-ngs/]
- 29. Pharmacogenomics in drug therapy: global regulatory ... [https://www.nature.com/articles/s41431-025-01950-6]
- 30. Evaluating Pharmacogenomic Integration into Electronic Health... Data [https://www.linkedin.com/pulse/evaluating-pharmacogenomic-data-integration-health-records-miranda-zcp3c]
- 31. Bioinformatic challenges for pharmacogenomic study: tools ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1548991/full]
- 32. Transforming Pharmacovigilance With Pharmacogenomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598900/]
- 33. Cloud Solutions for Genomics [https://aws.amazon.com/health/genomics/]
- 34. How to Run Scalable Genomic Workloads on AWS Cloud [https://hypersense-software.com/blog/2025/05/28/running-genomic-workloads-on-aws-cloud/]
- 35. HPC & Cloud Pipelines for Genomic Data [https://hypersense-software.com/blog/2025/05/07/hpc-cloud-bioinformatics-genomic-data/]
- 36. Accelerating genomics variant interpretation with ... [https://aws.amazon.com/blogs/machine-learning/accelerating-genomics-variant-interpretation-with-aws-healthomics-and-amazon-bedrock-agentcore/]
- 37. Rapid NGS Analysis on Google Cloud Platform [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627752/]
- 38. Patterns for scalable and resilient apps [https://cloud.google.com/architecture/scalable-and-resilient-apps]
- 39. Google Cloud Platform Services Summary [https://cloud.google.com/terms/services]
- 40. Cloud Computing Best Practices 2025: 11 Steps to a ... [https://distantjob.com/blog/cloud-computing-best-practices/]
- 41. Error encountered while running on downsampled BAM #833 [https://github.com/google/deepvariant/issues/833]
- 42. Error running DeepVariant on non-human model organism [https://github.com/google/deepvariant/issues/292]
- 43. deepvariant: Usage [https://nf-co.re/deepvariant/dev/docs/usage]
- 44. Clinical implementation of polygenic risk scores [https://www.nature.com/articles/s41431-025-01931-9]
- 45. A Beginner's Guide to Genomic Data Analysis: Variant calling [https://medium.com/@manabeel.vet/a-beginners-guide-to-genomic-data-analysis-variant-calling-ad8515eebddf]
- 46. Considering Clinical Implementation of Polygenic Scores ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559137/]
- 47. Multi-omics Data Integration, Interpretation, and Its Application [https://pmc.ncbi.nlm.nih.gov/articles/PMC7003173/]
- 48. A Guide to Multi-omics Integration Strategies [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 49. A technical review of multi-omics data integration methods [https://arxiv.org/abs/2501.17729]
- 50. Multiomics Research: Principles and Challenges in ... [https://www.sciencedirect.com/science/article/pii/S2693125725000019]
- 51. Spatial Transcriptomics for Tumor Heterogeneity Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9309247/]
- 52. Single-cell and spatial transcriptomic analysis reveals ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1556386/full]
- 53. Single-cell transcriptomics reveals biomarker ... [https://www.nature.com/articles/s41523-025-00803-1]
- 54. CRISPR Screen Analysis: Expert Troubleshooting Q&A [https://www.ubigene.us/application/crispr-screening-data-analytics-faq.html]
- 55. Troubleshooting Guide for Common CRISPR-Cas9 Editing ... [https://synapse.patsnap.com/article/troubleshooting-guide-for-common-crispr-cas9-editing-problems]
- 56. Revolutionizing CRISPR technology with artificial intelligence [https://www.nature.com/articles/s12276-025-01462-9]
- 57. Unraveling the future of genomics: CRISPR, single-cell ... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1565387/full]
- 58. CMN Weekly (7 November 2025) [https://crisprmedicinenews.com/news/cmn-weekly-7-november-2025-your-weekly-crispr-medicine-news/]
- 59. CRISPR libraries: A powerful screening tool for function ... [https://www.sciencedirect.com/science/article/pii/S3050538025000389]
- 60. Perturbomics: CRISPR–Cas screening-based functional ... [https://www.nature.com/articles/s12276-025-01487-0]
- 61. CRISPR-based functional genomics tools in vertebrate models [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322193/]
- 62. Next generation DNA Sequencing data analysis and its ... [https://www.sciencedirect.com/science/article/abs/pii/S034403382500473X]
- 63. Bioinformatics and Computational Tools for Next- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7019349/]
- 64. Statistical guidelines for quality control of next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8408346/]
- 65. Sequencing Quality Scores [https://www.illumina.com/science/technology/next-generation-sequencing/plan-experiments/quality-scores.html]
- 66. How-to: NGS Quality Control [https://frontlinegenomics.com/how-to-ngs-quality-control/]
- 67. Comprehensive Quality Control (QC) in NGS Data Analysis [https://mgi-tech.eu/science/comprehensive-quality-control-(qc)-in-ngs-data-analysis-a-step-by-step-guide]
- 68. Using Mendelian inheritance errors as quality control criteria ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4144465/]
- 69. Assessment of quality control approaches for metagenomic ... [https://www.nature.com/articles/srep06957]
- 70. The five pillars of computational reproducibility: bioinformatics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10591307/]
- 71. Bioinformatics Pipeline Troubleshooting [https://www.meegle.com/en_us/topics/bioinformatics-pipeline/bioinformatics-pipeline-troubleshooting]
- 72. Genomic reproducibility in the bioinformatics era [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03343-2]
- 73. Garbage In, Garbage Out: Dealing with Data Errors ... [https://blog.omni-inc.com/blog/garbage-in-garbage-out-dealing-with-data-errors-bioinformatics]
- 74. Next Generation Sequencing Platform: Ultimate Guide 2025 [https://lifebit.ai/blog/next-generation-sequencing-platform/]
- 75. Key Strategies for Optimizing NGS Workflows [https://www.technologynetworks.com/genomics/articles/key-strategies-for-optimizing-ngs-workflows-395232]
- 76. 全球最佳下一代测序(NGS)数据分析公司[更新] |全球增长见解 [https://www.globalgrowthinsights.com/zh/blog/next-generation-sequencing-ngs-data-analysis-companies-905]
- 77. 什么是网络自动化? [https://www.ibm.com/cn-zh/think/topics/network-automation]
- 78. 避免供应商锁定的4个最佳做法 - TechTarget云计算 [https://searchcloudcomputing.techtarget.com.cn/5-27876/]
- 79. UniversalAutomation.org - 解锁您的自动化软件! [https://universalautomation.org/cn/homepage-2/]
- 80. Systems Manager 自动化故障排除 [https://docs.aws.amazon.com/zh_cn/systems-manager/latest/userguide/automation-troubleshooting.html]
- 81. IT 自动化与漏洞修复解决方案 [https://www.opentext.com/zh-cn/products/automation]
- 82. Problems in variation interpretation guidelines and in their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7507483/]
- 83. A Practical Guide to Clinical Variant Interpretation [https://www.euformatics.com/blog-post/a-practical-guide-to-clinical-variant-interpretation]
- 84. Discrepancies in Variant Classifications and How to ... [https://www.genomenon.com/blog/discrepancies-variant-classifications-resolve]
- 85. Reasons and Resolutions for Inconsistent Variant Interpretation [https://pmc.ncbi.nlm.nih.gov/articles/PMC11919222/]
- 86. Major Causes of Conflicting Interpretations of Variant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11355203/]
- 87. Computational target fishing: what should chemogenomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4508123/]
- 88. Establishing Acceptance Criteria for Analytical Methods [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 89. Troubleshooting Pipelines Guide - GitHub Pages [https://phac-nml.github.io/irida-documentation/user/administrator/troubleshooting/pipelines/]
- 90. Benchmarking workflows to assess performance and ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-020-03934-3]
- 91. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 92. DNA Sequencing: How to Choose the Right Technology [https://frontlinegenomics.com/dna-sequencing-how-to-choose-the-right-technology/]
- 93. Comparing long-read sequencing technologies [https://www.pacb.com/blog/sequencing-101-comparing-long-read-sequencing-technologies/]
- 94. The applications and advantages of nanopore sequencing ... [https://www.nature.com/articles/s44259-025-00157-5]
- 95. Error Rate of PacBio vs Nanopore: How Accurate Are Long ... [https://www.cd-genomics.com/blog/pacbio-nanopore-error-rate-correction-strategies/]
- 96. The truth about sequencing accuracy and how ... [https://www.pacb.com/blog/the-truth-about-sequencing-accuracy-and-how-pacbio-leads-the-way/]
- 97. Comparative analysis of illumina and oxford nanopore ... [https://www.nature.com/articles/s41598-025-18768-3]
- 98. Review Applications of Oxford Nanopore Technology in the ... [https://www.sciencedirect.com/science/article/abs/pii/S0304389425027438]
- 99. PromethION 24/48 A-Series Technical Specification [https://nanoporetech.com/document/requirements/promethion-spec]
- 100. Validation approaches for computational drug repurposing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10785886/]
- 101. AI in Drug Development: Clinical Validation and ... [https://globalforum.diaglobal.org/issue/june-2025/ai-in-drug-development-clinical-validation-and-regulatory-innovation-are-dual-imperatives/]
- 102. Frequently Asked Questions - Center for Computational Research [https://docs.ccr.buffalo.edu/en/latest/faq/]
- 103. FAQs Next Generation Sequencing [https://eurofinsgenomics.eu/en/eurofins-genomics/product-faqs/next-generation-sequencing/]
- 104. - UCL Troubleshooting Computing Documentation Research [https://www.rc.ucl.ac.uk/docs/Supplementary/Troubleshooting/]
- 105. Computationally predicting clinical drug combination ... [https://www.nature.com/articles/s41467-020-19563-6]
- 106. Four Primary Steps and Tools for NGS Data Analyses [https://www.goldbio.com/blogs/articles/four-steps-for-ngs-data-analyses?srsltid=AfmBOopNEL6cBnZj7l3SfgBG_lYAilHEnY5Xf4czi25P-CpPX_uUI2A3]
- 107. Computational Tools for Next-Generation Sequencing ... [https://dromicslabs.com/computational-tools-for-next-generation-sequencing-analysis-a-comprehensive-guide/]
- 108. Clinical Metagenomic Next-Generation Sequencing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6345613/]
- 109. Clinical metagenomics—challenges and future prospects [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1186424/full]
- 110. Metagenomic Next-Generation Sequencing in Infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384723/]
- 111. Rapid metagenomic sequencing for surveillance of ... [https://nanoporetech.com/document/rapid-sequencing-metagenomics-sqk-rpb114-24]
- 112. Utilizing Targeted Next-Generation Sequencing for Rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11748758/]
- 113. Pathogen Detection Help Document - NCBI [https://www.ncbi.nlm.nih.gov/pathogens/pathogens_help/]