Strategic Cell Health Assessment: A Guide to Effective Compound Toxicity Filtering in Drug Discovery
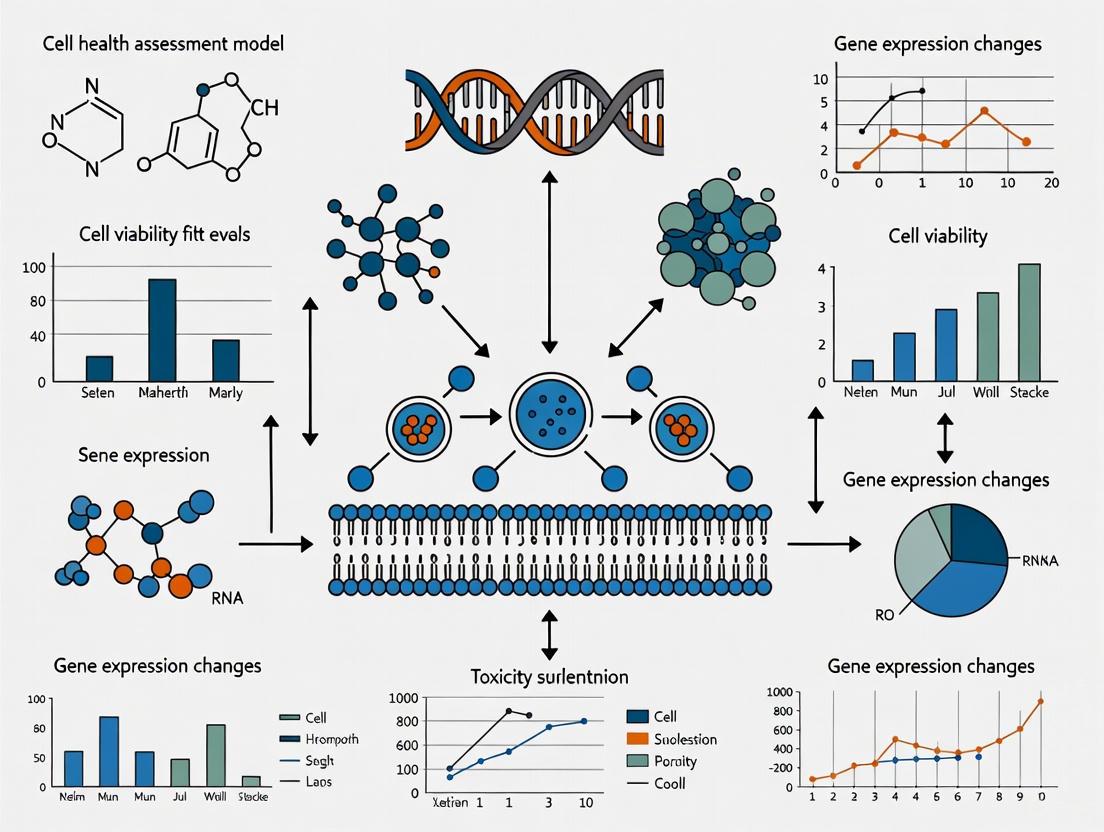
This article provides a comprehensive guide for researchers and drug development professionals on leveraging cell health assessment for early and predictive compound toxicity filtering.
Strategic Cell Health Assessment: A Guide to Effective Compound Toxicity Filtering in Drug Discovery
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on leveraging cell health assessment for early and predictive compound toxicity filtering. It covers the foundational mechanisms of cell toxicity, including oxidative stress, mitochondrial dysfunction, and DNA damage. The scope extends to a detailed comparison of traditional and advanced methodological approaches, such as high-throughput screening and multiplexed assays, while addressing common troubleshooting challenges like assay misinterpretation and timing. Furthermore, it explores validation strategies and the comparative analysis of emerging technologies, including 3D models, high-content imaging, and AI-driven analytics, to enhance predictive accuracy and streamline the drug development pipeline.
Understanding the Core Mechanisms of Cell Toxicity
Defining Cell Viability and Cytotoxicity in a Toxicological Context
Core Definitions and Their Importance in Toxicology
What is the fundamental difference between cell viability and cytotoxicity?
In the context of assessing compound toxicity, cell viability and cytotoxicity are two complementary yet distinct concepts that form the foundation of cell health assessment.
- Cell Viability refers to the number of healthy, functioning cells in a population and their capacity to maintain normal physiological processes under specific conditions, such as exposure to a test compound. It is a direct indicator of overall cell health and function. [1]
- Cytotoxicity is the property of a substance or compound to cause damage or death to cells. It specifically refers to the ability to disrupt essential cellular processes, leading to cell injury or death. Cytotoxicity assessment is a crucial parameter for evaluating the potential harm of compounds in drug development and environmental safety testing. [1]
In practice, viability assays measure the proportion of living cells, while cytotoxicity assays measure the degree of damage caused by a toxic agent. For a comprehensive safety profile in compound filtering research, it is essential to employ both types of assays, as they provide different pieces of the puzzle regarding a compound's biological impact. [1] [2]
Assay Selection Guide: Mechanisms and Applications
How do I choose the right assay to measure viability or cytotoxicity?
Selecting the appropriate assay is critical for generating reliable and meaningful data in toxicity screening. The choice depends on the mechanism of action you wish to probe and the specific readout required. The table below summarizes the most common assays used in toxicological contexts.
Table 1: Common Cell Viability and Cytotoxicity Assays in Toxicology
| Assay Name | Primary Measurement | Mechanism of Action / Target | Common Application in Toxicity Screening |
|---|---|---|---|
| MTT[ [3] [4] | Metabolic Activity (Viability) | Reduction of tetrazolium salt to formazan by mitochondrial dehydrogenases. | Measuring metabolic competence of cells after compound exposure. |
| WST-1[ [5] | Metabolic Activity (Viability) | Reduction of tetrazolium salt to water-soluble formazan by cellular enzymes. | Ideal for high-throughput screening; does not require a solubilization step. |
| ATP Assay (e.g., CellTiter-Glo)[ [3] [6] | Metabolic Activity (Viability) | Quantification of cellular ATP levels using luciferase-luciferin reaction. | Highly sensitive marker for viable cell number; rapid and homogeneous. |
| LDH Release[ [7] | Membrane Integrity (Cytotoxicity) | Measurement of Lactate Dehydrogenase (LDH) enzyme released from damaged cells. | Quantifying cell membrane damage and necrotic cell death. |
| Neutral Red Uptake (NRU)[ [2] | Lysosomal Function & Membrane Integrity (Viability) | Uptake and retention of the supravital dye Neutral Red by viable cells. | Assessing the capacity of viable cells to incorporate and bind the dye. |
| Caspase-Glo 3/7[ [6] | Apoptosis (Cytotoxicity Mechanism) | Measurement of caspase-3 and -7 activity, key executioners of apoptosis. | Differentiating apoptotic cell death from other mechanisms like necrosis. |
| Live/Dead Staining[ [6] | Membrane Integrity (Viability/Cytotoxicity) | Simultaneous staining with fluorescent markers for live (calcein-AM) and dead (propidium iodide) cells. | Visualizing and quantifying the ratio of live to dead cells in a population. |
| Colony Forming Unit (CFU)[ [2] | Proliferative Capacity (Viability) | Ability of a single cell to grow into a colony, indicating long-term reproductive health. | Measuring the clonogenic potential of cells after treatment with a compound. |
Visual Guide to Assay Selection
The following diagram illustrates the decision-making process for selecting an assay based on the biological question and the nature of the compound being tested.
Detailed Experimental Protocols
What are the standard protocols for key viability and cytotoxicity assays?
Below are detailed methodologies for two commonly used and complementary assays: the MTT assay for viability and the LDH assay for cytotoxicity.
Principle: Metabolically active cells reduce the yellow tetrazolium salt MTT to purple, insoluble formazan crystals. The amount of formazan produced is proportional to the number of viable cells.
Reagents & Materials:
- MTT reagent: Prepare at 5 mg/mL in Dulbecco’s Phosphate Buffered Saline (DPBS) and filter-sterilize.
- Solubilization Solution: 40% Dimethylformamide (DMF), 2% Glacial Acetic Acid, 16% Sodium Dodecyl Sulfate (SDS), pH adjusted to 4.7.
- 96-well tissue culture-treated plate
- Microplate reader capable of measuring absorbance at 570 nm.
Step-by-Step Procedure:
- Cell Seeding and Treatment: Seed cells at an optimal density in a 96-well plate and culture overnight. Expose cells to your test compounds for the desired duration.
- MTT Incubation: Add the prepared MTT solution directly to each well to achieve a final concentration of 0.2 - 0.5 mg/mL. Typically, 10-20 µL of MTT stock is added to 100 µL of culture medium.
- Incubation: Incubate the plate for 1 to 4 hours at 37°C in a humidified CO2 incubator. Monitor for the formation of purple formazan crystals under a microscope.
- Solubilization: Carefully remove the culture medium containing MTT. Add the solubilization solution (e.g., 100 µL per well for a 96-well plate). Agitate the plate gently on an orbital shaker to fully dissolve the formazan crystals. This may take 10-30 minutes.
- Absorbance Measurement: Read the absorbance of each well at 570 nm using a microplate reader. A reference wavelength of 630-650 nm can be used to subtract background.
Data Analysis: Calculate the percentage of cell viability relative to the untreated control cells after subtracting the background absorbance from wells with medium and MTT only (blank).
Principle: This assay measures the activity of the cytosolic enzyme Lactate Dehydrogenase (LDH) released into the culture medium upon cell membrane damage. The released LDH is quantified by a coupled enzymatic reaction that results in a colored product.
Reagents & Materials:
- LDH assay kit (typically containing reaction buffer, substrate, and dye).
- Lysis solution (for generating maximum LDH release control).
- 96-well plate (clear flat-bottom).
- Microplate reader capable of measuring absorbance at 490-500 nm.
Step-by-Step Procedure:
- Sample Preparation: At the end of compound treatment, centrifuge the cell culture plate (e.g., 250 × g for 5 minutes) to pellet any detached cells and debris.
- Transfer Supernatant: Carefully transfer a portion of the cell-free supernatant (typically 50 µL) to a new clear 96-well assay plate.
- Reaction Setup: Add the LDH reaction mixture to each well containing the supernatant, following the kit manufacturer's instructions. Incubate for 15-30 minutes at room temperature, protected from light.
- Signal Measurement: Add the stop solution (if provided) and measure the absorbance at 490-500 nm.
Data Analysis:
- Spontaneous LDH Activity: LDH released from untreated control cells (background cell death).
- Maximum LDH Activity: LDH released from control cells treated with lysis solution (represents 100% cytotoxicity).
- Compound-induced LDH Activity: LDH released from compound-treated cells.
Calculate the percentage of cytotoxicity using the formula: % Cytotoxicity = (Compound LDH - Spontaneous LDH) / (Maximum LDH - Spontaneous LDH) × 100
Workflow for a Combined Viability and Cytotoxicity Assessment
For a comprehensive analysis, researchers often run viability and cytotoxicity assays in parallel. The following diagram outlines a typical integrated workflow.
Frequently Asked Questions (FAQs) & Troubleshooting
Why is my viability assay showing increased signal with a known cytotoxic compound?
This phenomenon, often called "hyper-metabolism," can occur with certain compounds at specific concentrations. Some toxicants, like oxidative phosphorylation uncouplers (e.g., tolcapone, benzarone), can cause a compensatory increase in metabolic rate and a transient rise in the signal of assays like MTT or Realtime-Glo before cell death occurs. [7] Solution: Always use multiple assays that probe different biological endpoints (e.g., combine a metabolic assay like MTT with a membrane integrity assay like LDH). This provides a more complete picture and helps identify such artifacts. [7] [6]
My assay results have high variability between replicates. What could be the cause?
High variability often stems from technical inconsistencies. Solution: Ensure a homogeneous single-cell suspension before seeding by pipetting thoroughly. Optimize and maintain consistent cell seeding density across all wells. Use multichannel pipettes for reagent addition to minimize timing differences. Finally, avoid placing control or treated wells on the edges of the plate if "edge effect" is suspected due to evaporation; instead, fill perimeter wells with PBS or medium only. [4] [5]
The formazan crystals in my MTT assay are not dissolving properly. How can I fix this?
Incomplete solubilization is a common issue. Solution: First, ensure you are using the correct solubilization solution (e.g., DMSO, acidified isopropanol, or SDS-based solutions). [4] After adding the solubilization solution, seal the plate with parafilm and incubate on an orbital shaker for an extended period (up to 1 hour). If crystals persist, gently pipette up and down or briefly sonicate the plate in a water bath sonicator. [4]
My test compound is colored and interferes with the absorbance reading. How can I account for this?
Colorimetric interference is a well-known limitation of assays like MTT and WST-1. Solution: Include control wells containing the compound at the tested concentrations in culture medium without cells. Subtract the absorbance values of these "compound-only" backgrounds from the corresponding test wells during data analysis. [4] [5] Alternatively, consider switching to a non-colorimetric assay, such as a luminescent ATP assay or a fluorometric assay like CFDA-AM or alamar blue. [3]
Research Reagent Solutions
A successful experiment relies on high-quality reagents. The table below lists essential materials and their functions for cell health assessment assays.
Table 2: Essential Research Reagents for Viability and Cytotoxicity Testing
| Reagent / Material | Function | Example Assays |
|---|---|---|
| Tetrazolium Salts (MTT, WST-1, MTS) | Substrates reduced by metabolically active cells to generate a colorimetric signal. | MTT, WST-1, MTS Assays [3] [4] [5] |
| LDH Assay Kit | Provides optimized reagents for the coupled enzymatic reaction to quantify lactate dehydrogenase released from damaged cells. | LDH Release Assay [7] |
| ATP Detection Reagent | Luciferase enzyme that produces luminescence in the presence of ATP, a marker of metabolically active cells. | CellTiter-Glo [3] [6] |
| Caspase Substrate | Proteolytic substrate that generates a luminescent or fluorescent signal when cleaved by active caspase-3/7. | Caspase-Glo 3/7 Assay [6] |
| Fluorescent Viability Dyes (Calcein-AM, Propidium Iodide) | Live cells esterify non-fluorescent Calcein-AM to green-fluorescent calcein. Dead cells with compromised membranes are stained by red-fluorescent PI. | Live/Dead Staining [6] |
| Cell Culture Microplates | Specially treated plasticware with clear, flat bottoms for optimal cell attachment and accurate optical readings. | All microplate-based assays |
| Microplate Reader | Instrument capable of detecting absorbance, luminescence, and/or fluorescence signals from multi-well plates. | All assays |
Core Mechanisms and Scientific Background
What are the key mechanisms linking oxidative stress, ROS, and mitochondrial dysfunction in compound toxicity screening?
Mitochondrial dysfunction is a central mechanism in compound toxicity, primarily through excessive reactive oxygen species (ROS) production and impaired cellular energy metabolism. During oxidative phosphorylation, electrons leak from mitochondrial complexes I and III, reducing oxygen to superoxide anion (O₂⁻), which is converted to other ROS like hydrogen peroxide (H₂O₂) [8] [9]. This creates oxidative stress when ROS production overwhelms antioxidant defenses, leading to cellular damage that is critical to assess in toxicity screening [9] [10].
The resulting oxidative damage impairs ATP production, damages mitochondrial DNA (mtDNA), and disrupts calcium homeostasis [10] [11]. mtDNA is particularly vulnerable due to its proximity to ROS generation sites and lack of histone protection [9]. This mitochondrial impairment activates programmed cell death pathways, making it a key endpoint for assessing compound toxicity [10] [12].
Table 1: Primary Sources and Characteristics of Mitochondrial ROS
| ROS Source | Location | Primary ROS Produced | Significance in Toxicity |
|---|---|---|---|
| Complex I (NADH:ubiquinone oxidoreductase) | Mitochondrial matrix | O₂⁻ | Major electron leak site during impaired electron transport [8] [9] |
| Complex III (cytochrome c reductase) | Mitochondrial inner membrane | O₂⁻ | Produces ROS in both matrix and intermembrane space [9] |
| Reverse Electron Transport (RET) | Mitochondrial electron transport chain | O₂⁻ | Significant superoxide generation during electron backflow [9] |
| Glycerol 3-phosphate dehydrogenase | Mitochondrial inner membrane | O₂⁻ or H₂O₂ | Additional mitochondrial ROS generation site [8] |
How does mitochondrial dysfunction propagate cellular damage in response to toxic compounds?
Mitochondrial dysfunction propagates cellular damage through several interconnected mechanisms that amplify initial toxic insults. The process typically begins with impaired electron transport chain function, leading to reduced ATP synthesis and increased electron leakage [9] [10]. These electrons directly reduce molecular oxygen, generating superoxide anions that initiate a cascade of oxidative damage [8].
The oxidative stress damages mtDNA, proteins, and lipids, creating a vicious cycle that further compromises mitochondrial function [10] [11]. Key proteins regulating mitochondrial dynamics become impaired, disrupting the balance between fission and fusion processes [8]. This leads to abnormal mitochondrial morphology and compromised quality control mechanisms, including impaired mitophagy [11].
As dysfunction progresses, the mitochondrial permeability transition pore (mPTP) opens, releasing cytochrome c and other pro-apoptotic factors that activate caspase-dependent apoptosis [10] [12]. Simultaneously, oxidative stress triggers inflammatory responses through damage-associated molecular patterns (DAMPs), including mtDNA released into the cytoplasm, which activates inflammasomes and amplifies cellular injury [8].
Figure 1: Oxidative Stress Amplification Cycle in Compound Toxicity. This diagram illustrates how initial mitochondrial insult creates a self-amplifying cycle of damage through ROS production and oxidative stress.
Troubleshooting Guides: Experimental Issues and Solutions
Why is there no assay window in my mitochondrial toxicity assay, and how can I resolve this?
A completely absent assay window typically indicates fundamental issues with instrument setup or reagent problems. First, verify your microplate reader is properly configured for your specific assay type. For TR-FRET assays, ensure you're using exactly the recommended emission filters, as incorrect filter selection is the most common failure point [13].
Test your instrument setup using control reagents before running your actual experiment. Check that all stock solutions are prepared correctly at specified concentrations (typically 1 mM), as differences in stock solutions between labs frequently cause EC50/IC50 variability [13]. For cell-based assays, confirm your compounds can cross cell membranes and aren't being pumped out, which would prevent intracellular target engagement [13].
Table 2: Antioxidant Defense Systems in Mitochondrial Toxicity Assessment
| Antioxidant System | Components | Function in Toxicity Mitigation | Measurement in Assays |
|---|---|---|---|
| Glutathione System | GSH, GSSG, GPx, GR | Reduces H₂O₂ to H₂O while oxidizing GSH to GSSG; regenerated by GR [8] | GSH/GSSG ratio, GPx activity |
| Enzymatic Defenses | SOD, Catalase, Peroxiredoxin | SOD converts O₂⁻ to H₂O₂; catalase/peroxiredoxin decompose H₂O₂ to H₂O and O₂ [8] [10] | SOD activity, catalase activity |
| Small Molecule Antioxidants | Melatonin, CoQ10 | Directly scavenge ROS and indirectly boost antioxidant enzymes [8] [11] | Concentration measurements |
| Mitochondrial Dynamics | Drp1, OPA1, Mfn1/2 | Regulate fission/fusion balance; dysregulated in toxicity [8] [11] | Protein expression, localization |
Why am I getting inconsistent EC50/IC50 values between experiments when screening compounds for mitochondrial toxicity?
Inconsistent potency values typically stem from three main sources: stock solution preparation, cellular context variability, and assay execution differences. The primary reason for EC50/IC50 differences between labs is variation in stock solution preparation, particularly at the critical 1 mM concentration [13]. Use freshly prepared stocks with verified purity and concentration.
Passage number significantly influences experimental outcomes in cell-based assays [14]. Use consistent passage ranges and ensure thorough cell authentication. Mycoplasma contamination can profoundly alter mitochondrial function and cellular responses - implement regular testing using appropriate detection methods [14].
For kinase-targeted compounds, remember that cell-based assays may target inactive kinase forms or upstream/downstream kinases, while biochemical assays require active kinases [13]. This fundamental difference can explain potency discrepancies between assay formats. Always include appropriate reference compounds and controls to normalize results between experimental runs.
Figure 2: Troubleshooting Inconsistent Potency Measurements. This flowchart outlines common sources of variability in mitochondrial toxicity screening and corresponding corrective actions.
Experimental Protocols: Key Methodologies
What is a robust protocol for assessing compound-induced mitochondrial dysfunction through oxidative stress parameters?
Principle: This protocol measures key oxidative stress parameters to evaluate compound-induced mitochondrial dysfunction, focusing on ROS production, antioxidant depletion, and oxidative damage markers [8] [10].
Materials:
- Cell culture system relevant to your toxicity model (primary cells or appropriate cell lines)
- Compounds for screening with appropriate vehicle controls
- ROS detection probes (DCFDA for general ROS, MitoSOX for mitochondrial superoxide)
- GSH/GSSG detection kit
- Lipid peroxidation assay (MDA detection)
- mtDNA damage detection reagents (Long-range PCR or appropriate kits)
- Microplate reader with appropriate filters
Procedure:
- Cell Preparation: Plate cells at optimized density in appropriate multi-well plates. Use consistent passage numbers and authenticate cell lines regularly [14].
- Compound Treatment: Treat cells with test compounds across a concentration range (typically 0.1-100 μM) for 4-24 hours depending on mechanism. Include vehicle and positive controls.
- ROS Measurement:
- Load cells with 10 μM DCFDA or 5 μM MitoSOX in serum-free media
- Incubate 30-45 minutes at 37°C
- Wash with PBS and measure fluorescence (DCFDA: Ex/Em 485/535nm; MitoSOX: Ex/Em 510/580nm)
- Glutathione Measurement:
- Collect cells and process for GSH/GSSG detection per kit instructions
- Measure absorbance or fluorescence to determine GSH/GSSG ratio
- Lipid Peroxidation Assessment:
- Measure malondialdehyde (MDA) levels using thiobarbituric acid reactive substances (TBARS) assay
- Incubate samples with TBA reagent at 95°C for 60 minutes
- Measure absorbance at 532nm
- mtDNA Damage Assessment:
- Extract total DNA including mtDNA
- Perform long-range PCR of mitochondrial genes versus nuclear genes
- Quantify amplification efficiency reduction as indicator of DNA damage
Data Analysis: Calculate fold-change relative to vehicle controls for each parameter. Establish significance thresholds based on positive controls. Compounds showing concentration-dependent increases in ROS and MDA with decreased GSH/GSSG ratio indicate mitochondrial oxidative stress.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Mitochondrial Toxicity Assessment
| Reagent/Category | Specific Examples | Function in Mitochondrial Assessment |
|---|---|---|
| ROS Detection Probes | DCFDA, MitoSOX Red, H₂DCFDA | General and mitochondrial-specific ROS detection [10] [12] |
| Antioxidant Assays | GSH/GSSG-Glo, Total Glutathione kits | Quantify redox balance and antioxidant capacity [8] [15] |
| Oxidative Damage Markers | TBARS assay kits, Protein carbonylation kits | Lipid peroxidation (MDA) and protein oxidation measurement [10] [15] |
| Mitochondrial Function Assays | Seahorse XF kits, JC-1 dye, TMRM | Respiration, membrane potential, and function analysis [16] [11] |
| Cell Viability/Cytotoxicity | CellTiter-Glo, MTT, LDH assays | Viability correlation with mitochondrial parameters [17] |
| mtDNA Damage Detection | Long-range PCR kits, mtDNA-specific primers | Mitochondrial genome integrity assessment [9] [10] |
Frequently Asked Questions
How do I determine whether observed mitochondrial toxicity is primary or secondary to other cellular damage?
Primary mitochondrial toxicity manifests as direct, concentration-dependent impairment of mitochondrial parameters that precedes other signs of cellular distress. Key indicators include early disruption of oxygen consumption rate (OCR), decreased ATP production, and increased mitochondrial ROS specifically occurring before significant plasma membrane permeability or nuclear condensation [10] [11]. The toxic compound typically directly targets electron transport chain components, mitochondrial membranes, or mtDNA [9].
Secondary mitochondrial dysfunction occurs as a consequence of other primary insults, such as calcium overload, glutathione depletion, or activation of death receptors. This typically manifests later in the toxicity timeline and may be prevented by inhibitors of the primary insult [10] [12]. To distinguish between these mechanisms, perform time-course experiments measuring mitochondrial parameters alongside other cell health indicators, and use specific mitochondrial protectants like cyclosporine A (mPTP inhibitor) or antioxidants to determine if they prevent toxicity.
What are the most relevant positive controls for establishing mitochondrial toxicity assay performance?
For general oxidative stress induction, tert-butyl hydroperoxide (tBHP) and antimycin A are excellent positive controls. tBHP directly induces peroxidative stress, while antimycin A specifically inhibits complex III, increasing superoxide production [9]. For complex I-specific dysfunction, use rotenone or piericidin A [9] [11]. For mitochondrial permeability transition, use calcium ionophores in combination with inorganic phosphate.
Include both acute (1-4 hour) and longer-term (24-hour) exposures to capture different mechanisms. Validate your positive controls against literature values for potency and maximal effects. For antioxidant response measurements, compounds like sulforaphane that induce Nrf2-mediated antioxidant responses can serve as positive controls for protective pathways [8] [15].
The Role of Apoptosis, Necrosis, and Other Cell Death Pathways
Troubleshooting Guides and FAQs
FAQ: General Cell Death Concepts
Q1: What is the core difference between accidental and regulated cell death?
A1: The fundamental difference lies in the control and physiological implications of the process.
- Accidental Cell Death (ACD): This is an uncontrolled, passive process triggered by severe physical, chemical, or mechanical insults that exceed the cell's tolerance. It is not genetically encoded and typically leads to inflammation. Necrosis is the classic example of ACD. [18]
- Regulated Cell Death (RCD): This is an active, genetically programmed process that requires specific molecular machinery. RCD plays crucial roles in development, tissue homeostasis, and the removal of damaged cells. Apoptosis, pyroptosis, and ferroptosis are all forms of RCD. The term Programmed Cell Death (PCD) is often used interchangeably with RCD. [18] [19]
Q2: My viability assay shows reduced cell numbers, but I'm unsure if it's due to death or proliferation arrest. How can I tell?
A2: This is a common challenge, as metabolic activity assays like MTT/MTS can be influenced by both cell death and slowed metabolism. [20] To distinguish between these, a multi-parametric approach is essential.
- Confirm Cell Death Directly: Use a LIVE/DEAD assay (e.g., calcein-AM for live cells, EthD-1 or propidium iodide (PI) for dead cells) or an Annexin V/PI assay to directly quantify the proportion of dead and dying cells. [20] [21]
- Assess Proliferation: Incorporate a proliferation-specific dye like CellTrace Violet or BrdU to track cell division. A decrease in viable cell number without an increase in dead cell markers strongly suggests cytostatic effects. [20] [21]
Q3: I've heard about "crosstalk" between cell death pathways. What does this mean for my experiments?
A3: Crosstalk refers to the extensive molecular interactions where one cell death pathway can influence the initiation or execution of another. [19] [22] This has critical experimental implications:
- Inhibition is Not Always Clean: Using a caspase inhibitor (e.g., Q-VD-OPh) to block apoptosis may not prevent cell death if the stimulus is strong enough to activate a backup pathway like necroptosis. [20]
- Combined Targeting May Be Needed: For effective therapeutic outcomes, especially in cancer, it may be necessary to target multiple RCD pathways simultaneously to overcome resistance. [23] [24]
- Always Use Multiple Assays: Relying on a single method to define a cell death type is risky. Confirm your findings with complementary techniques that assess different hallmarks (e.g., morphology, caspase activation, lipid peroxidation). [20]
Troubleshooting Guide: Identifying Specific Cell Death Pathways
Q4: How can I confirm that cell death in my model is truly apoptosis?
A4: Apoptosis should be confirmed by assessing multiple hallmarks. The table below summarizes key characteristics and detection methods.
| Feature to Assess | Key Markers & Reagents | Detection Method |
|---|---|---|
| Morphology | Cell shrinkage, chromatin condensation, apoptotic bodies | Phase-contrast microscopy, fluorescent DNA dyes (Hoechst) |
| Phosphatidylserine Exposure | Annexin V (requires calcium buffer) | Flow cytometry, fluorescence microscopy |
| Membrane Integrity | Propidium Iodide (PI) or EthD-1 | Flow cytometry (used with Annexin V) |
| Caspase Activation | Fluorogenic caspase substrates (e.g., DEVD-FMK for caspase-3), cleaved caspase-3 antibodies | Flow cytometry, Western blot, fluorescence microscopy |
| Mitochondrial Pathway | Cytochrome c release, Bax/Bak activation | Western blot (cytochrome c in cytosol), immunofluorescence |
| Key Protein Cleavage | Cleaved PARP, cleaved caspase substrates | Western blot |
| Pharmacological Inhibition | Pan-caspase inhibitor (e.g., Q-VD-OPh, Z-VAD-FMK) | Pre-treatment to rescue viability |
Experimental Protocol: Annexin V/PI Staining for Flow Cytometry
- Harvest Cells: Collect both adherent and floating cells.
- Wash: Resuspend cell pellet in cold PBS.
- Staining: Resuspend ~100,000 cells in 100 µL of Annexin V Binding Buffer.
- Add Dyes: Add Annexin V-fluorochrome conjugate (e.g., FITC) and PI. Incubate for 15 minutes in the dark at room temperature.
- Analyze: Add more binding buffer and analyze immediately by flow cytometry.
Q5: My cells are dying, but it doesn't look like classic apoptosis. What other pathways should I investigate?
A5: Many non-apoptotic RCD pathways can be triggered, especially by chemotherapeutic agents or in resistant cancer cells. The table below outlines alternative pathways and their key markers.
| Pathway | Key Inducers/Inhibitors | Critical Markers & Detection Methods |
|---|---|---|
| Ferroptosis | Inducers: Erastin, RSL3, sulfasalazine.Inhibitors: Ferrostatin-1, liproxstatin-1. | Lipid Peroxidation: C11-BODIPY 581/591 probe, MDA assay.GPX4 Inactivation: Western blot.Iron Chelation: Deferoxamine (inhibits).Morphology: Shrunken mitochondria with intact nuclei. [25] |
| Necroptosis | Inducer: TNF-α + caspase inhibitor (e.g., Z-VAD) + IAP inhibitor (e.g., SMAC mimetic).Inhibitor: Necrostatin-1 (RIPK1 inhibitor). | Phospho-RIPK1/RIPK3, MLKL oligomerization: Western blot.Morphology: Necrotic-like swelling and rupture. [20] [24] |
| Pyroptosis | Inducers: Intracellular pathogens, DAMPs/PAMPs. | Cleaved Gasdermin D (GSDMD): Western blot.Active Caspase-1: Western blot/assay.Inflammasome Formation.Lactate Dehydrogenase (LDH) Release: Cytotoxicity assay. [26] |
| Autophagic Cell Death | Inducer: Rapamycin, nutrient starvation.Inhibitor: Chloroquine, bafilomycin A1. | LC3-I to LC3-II conversion: Western blot.Autophagosome formation: GFP-LC3 puncta by microscopy.SQSTM1/p62 degradation: Western blot. [19] [24] |
Q6: I need a comprehensive view of cell health in one sample. Is there an integrated workflow?
A6: Yes, a multiparametric flow cytometry protocol can assess proliferation, cell cycle, apoptosis, and mitochondrial health simultaneously from a single sample. [21]
Experimental Protocol: Integrated Flow Cytometry Workflow
- Proliferation Staining: Prior to treatment, stain cells with CellTrace Violet dye, which dilutes with each cell division.
- Treatment & Incubation: Expose cells to your compound for the desired time.
- BrdU Incorporation: Add BrdU for a pulse (e.g., 1-2 hours) to label S-phase cells.
- Harvest and Stain:
- Mitochondrial Membrane Potential (ΔΨm): Stain with JC-1 dye. Healthy mitochondria show red (J-aggregates) and green (monomer) fluorescence; depolarized mitochondria show only green.
- Apoptosis & Death: Stain with Annexin V and PI.
- Cell Cycle/Fixation: Fix and permeabilize cells, then digest RNA and stain DNA with PI. Detect incorporated BrdU with a fluorescent antibody.
- Flow Cytometry Analysis: Acquire data on all fluorescent channels. This provides eight key parameters from one sample: CellTrace Violet (proliferation), BrdU (S-phase), PI for DNA content (cell cycle), JC-1 (ΔΨm), Annexin V (apoptosis), and PI permeability (cell death). [21]
Research Reagent Solutions
This table lists essential reagents for studying different cell death pathways, along with their primary functions.
| Reagent / Tool | Function / Application |
|---|---|
| Q-VD-OPh | Broad-spectrum, pan-caspase inhibitor used to confirm apoptosis and prevent caspase-dependent death. [20] |
| Annexin V (FITC/APC) | Binds to phosphatidylserine (PS) exposed on the outer leaflet of the plasma membrane during early apoptosis. [20] [21] |
| Propidium Iodide (PI) | DNA intercalating dye that is impermeant to live and early apoptotic cells. Used to mark dead cells with compromised membranes. [21] |
| Ferrostatin-1 (Fer-1) | Specific inhibitor of ferroptosis; acts as a radical trapping antioxidant to prevent lipid peroxidation. [20] [25] |
| Necrostatin-1 (Nec-1) | Specific inhibitor of RIPK1 kinase activity, used to inhibit necroptosis. [20] |
| Chloroquine (CQ) | Lysosomotropic agent that inhibits autophagy by raising lysosomal pH and preventing autophagosome degradation. [20] |
| JC-1 Dye | Mitochondrial membrane potential (ΔΨm) sensor. A decrease in red/green fluorescence ratio indicates mitochondrial depolarization, an early event in intrinsic apoptosis. [21] |
| C11-BODIPY 581/591 | Lipid peroxidation sensor. Oxidation causes a shift in fluorescence from red to green, detectable by flow cytometry or microscopy. [25] |
| CellTrace Violet | Fluorescent cell proliferation dye that dilutes equally with each cell division, allowing tracking of proliferation kinetics. [21] |
| Z-VAD-FMK | Another common pan-caspase inhibitor, used similarly to Q-VD-OPh to block apoptotic signaling. [24] |
Signaling Pathway Diagrams
The following diagrams illustrate the core molecular mechanisms of key cell death pathways, providing a visual reference for understanding their components and crosstalk.
Apoptosis Signaling Pathways
Ferroptosis Core Mechanism
Integrated Cell Death Crosstalk
Reactive Oxygen Species (ROS) as a Central Modulator in Toxicity
Reactive Oxygen Species (ROS) are a group of chemically reactive molecules containing oxygen, produced as natural byproducts of aerobic metabolism. In the context of compound toxicity screening, understanding ROS is paramount because they function as a double-edged sword: at low/moderate concentrations, they act as crucial signaling molecules for normal physiological processes, but at excessive levels, they induce oxidative stress, leading to macromolecular damage and cell death [27] [28].
The dual role of ROS makes them a central modulator in toxicity. Oxidative stress occurs when the production of ROS overwhelms the cell's antioxidant defenses [29]. This imbalance can be induced by toxic compounds and can severely compromise cell health, damaging lipids, proteins, and DNA, which can ultimately lead to carcinogenesis, neurodegeneration, and other disease states [29] [28]. Therefore, accurate assessment of ROS and the resulting oxidative damage is a critical component of cell health assessment in compound toxicity filtering research.
Core Concepts and Terminology
What are the key ROS molecules? ROS is a collective term that includes both oxygen radicals and certain non-radical oxidizing agents [28]. The key species, their sources, and primary reactivities are summarized in the table below.
Table 1: Key Reactive Oxygen Species (ROS) in Biological Systems
| ROS Species | Chemical Symbol | Primary Sources | Reactivity & Role in Toxicity |
|---|---|---|---|
| Superoxide | O₂•⁻ | Mitochondrial ETC (Complex I & III), NOX enzymes [27] [30] | Not highly reactive itself, but a progenitor to other ROS; inactivates Fe-S cluster proteins [27] [31] |
| Hydrogen Peroxide | H₂O₂ | Dismutation of O₂•⁻ by SOD, various oxidase enzymes [27] [31] | Poorly reactive but long-lived; diffuses easily; key signaling molecule and substrate for more reactive species [31] |
| Hydroxyl Radical | HO• | Fenton reaction (H₂O₂ + Fe²⁺) [30] [28] | Extremely reactive; causes immediate, indiscriminate oxidative damage to all nearby biomolecules [31] |
| Peroxynitrite | ONOO⁻ | Reaction of O₂•⁻ with nitric oxide (NO) [27] [30] | Potent oxidant; causes nitrosative stress, leading to protein nitration and lipid peroxidation [27] |
What is the relationship between ROS, oxidative stress, and antioxidants?
- Oxidative Stress: A condition characterized by an imbalance between the production of ROS and the ability of the biological system to readily detoxify the reactive intermediates or repair the resulting damage [29].
- Antioxidants: Molecules that mitigate oxidative damage. They include enzymatic systems like superoxide dismutase (SOD), catalase, and peroxidases, as well as small molecules like glutathione (GSH) [27] [31]. It is critical to note that "antioxidant" is a broad term, and the specific chemistry, location, and concentration of each antioxidant must be considered when interpreting experiments [31].
The following diagram illustrates the core dynamic between ROS production, cellular defenses, and the resulting toxicological outcomes.
Diagram 1: ROS as a Central Modulator in Compound-Induced Toxicity.
Methodologies for ROS and Oxidative Damage Assessment
Accurately measuring ROS and oxidative damage is technically challenging due to the high reactivity and short half-lives of many species. The following section provides guidelines, protocols, and a critical comparison of common methods.
Direct ROS Measurement
Direct measurement aims to quantify the levels of specific ROS molecules in cells or tissues.
Table 2: Comparison of Common Direct ROS Detection Methods
| Method / Probe | Target ROS | Principle | Key Advantages | Key Limitations & Artefacts |
|---|---|---|---|---|
| Dihydroethidium (DHE) / MitoSOX Red | Superoxide (O₂•⁻) | Oxidation by O₂•⁻ forms fluorescent 2-hydroxyethidium (2-OH-E+) [32]. | MitoSOX is targeted to mitochondria. HPLC separation allows specific quantification of 2-OH-E+ [32]. | Simple fluorescence (e.g., microscopy) cannot distinguish 2-OH-E+ from other oxidation products; can overestimate O₂•⁻ [32]. |
| H2DCFDA (DCFH-DA) | Various (H₂O₂, ROO•, HO•) [33] [29] | Cell-permeable probe is hydrolyzed and oxidized to fluorescent DCF [33]. | Widely used; amenable to plate readers for throughput [33]. | Not specific for H₂O₂; subject to redox cycling and artificial signal amplification; metal- and peroxidase-sensitive [32]. |
| Amplex Red | Extracellular H₂O₂ | Horseradish peroxidase uses H₂O₂ to oxidize Amplex Red to fluorescent resorufin [32]. | Highly specific and sensitive for H₂O₂; good for measuring H₂O₂ release from cells or isolated organelles [32]. | Measures extracellular H₂O₂ only. Can be interfered with by O₂•⁻ or reducing agents like NADH [32]. |
| Electron Spin Resonance (ESR/EPR) | Radical species (O₂•⁻, HO•) | Directly detects molecules with unpaired electrons. Often used with spin traps (e.g., DMPO) [32] [34]. | Considered the "gold standard" for direct radical detection; provides structural information [34]. | Technically complex; requires specialized equipment. Spin traps (e.g., DMPO) can be toxic and react slowly [32]. |
| Genetically Encoded Sensors (e.g., roGFP, HyPer) | H₂O₂ (roGFP, HyPer) | roGFP has redox-sensitive disulfides; excitation ratio changes with oxidation [33]. | Subcellular targeting; minimal perturbation; ratiometric measurement reduces artefacts [33]. | Requires genetic manipulation; signal may be influenced by the local glutathione pool [33]. |
Expert Recommendation: No single method is perfect. The research community strongly recommends against relying solely on DCFH-DA as a measure for H₂O₂ due to its lack of specificity [31] [32]. For superoxide, the HPLC-based method for DHE is preferred over simple fluorescence imaging. The use of specific ROS generators and inhibitors is encouraged to corroborate findings [31].
Protocol: HPLC-Based Detection of Superoxide Using Dihydroethidium
This protocol provides a specific and quantitative method for measuring superoxide levels in cell cultures, critical for assessing compound-induced toxicity [32].
Principle: DHE is oxidized specifically by superoxide to form 2-hydroxyethidium (2-OH-E+). HPLC separation allows for the precise quantification of 2-OH-E+, distinguishing it from other fluorescent products like ethidium, which are formed by non-specific oxidation.
Materials:
- Dihydroethidium (DHE)
- Acetonitrile (HPLC grade)
- Phosphoric acid
- C18 reverse-phase HPLC column
- Cell culture samples (treated with test compounds)
- Microplate reader or fluorometer
Procedure:
- Cell Treatment & Staining: Culture cells in appropriate plates. After treatment with the compounds of interest, load cells with DHE (e.g., 5-50 µM) in buffer for 30-60 minutes at 37°C.
- Cell Extraction: Wash cells to remove excess probe. Lyse cells and precipitate proteins. Centrifuge and collect the supernatant containing the fluorescent products.
- HPLC Analysis: Inject the supernatant onto a C18 reverse-phase HPLC column.
- Mobile Phase: Use a gradient or isocratic elution with a solvent mixture such as acetonitrile and water (containing 0.1% trifluoroacetic acid or phosphoric acid).
- Detection: Use a fluorescence detector with excitation at 510 nm and emission at 595 nm.
- Quantification: Identify the peak for 2-OH-E+ by comparison with a pure standard if available. Quantify the peak area, which is proportional to the superoxide production in the sample.
Assessment of Oxidative Damage
Indirect measurement of ROS through the stable biomarkers of oxidative damage they leave behind is a reliable and widely used approach.
Lipid Peroxidation:
- Marker: Malondialdehyde (MDA) is a well-studied end product.
- Method: Thiobarbituric Acid Reactive Substances (TBARS) assay. MDA reacts with TBA to form a pink chromophore measurable at 532 nm [29].
- Caveat: The TBARS assay can be non-specific. For greater accuracy, HPLC or GC-MS methods are recommended [29].
Protein Oxidation:
- Marker: Protein Carbonyls (PC).
- Method: Reaction of protein carbonyls with 2,4-dinitrophenylhydrazine (DNPH) to form hydrazones, which can be measured spectrophotometrically at 375 nm or via Western blot (OxyBlot) [29].
DNA Damage:
- Marker: 8-hydroxy-2'-deoxyguanosine (8-OHdG).
- Method: Typically measured using ELISA kits or HPLC with electrochemical detection.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for ROS and Oxidative Stress Research
| Reagent / Kit Name | Primary Function | Brief Description & Utility in Toxicity Screening |
|---|---|---|
| H2DCFDA / carboxy-H2DCFDA | General ROS sensing | A ubiquitous, cell-permeable fluorescent probe for a broad range of ROS. Useful for initial, high-throughput compound screening despite specificity limitations [33] [29]. |
| MitoSOX Red | Mitochondrial superoxide sensing | A live-cell permeant probe targeted to mitochondria. Critical for assessing compounds suspected of inducing mitochondrial toxicity [33] [32]. |
| Amplex Red Assay Kit | Extracellular H₂O₂ quantification | A highly specific and sensitive assay for measuring H₂O₂ released from cells. Ideal for profiling compound effects on extracellular H₂O₂ production [32]. |
| GSH/GSSG-Glo Assay | Glutathione redox ratio | A luminescent assay to detect both reduced (GSH) and oxidized (GSSG) glutathione. The GSH/GSSG ratio is a central indicator of cellular redox status and oxidative stress [35]. |
| ROS-Glo Assay | H₂O₂ measurement | A luminescent, H₂O2-sensitive assay designed for high-throughput screening. Uses a substrate that generates a luminescent signal proportional to H₂O₂ levels [35]. |
| MitoPQ | Mitochondrial superoxide generation | A research tool that generates O₂•⁻ within mitochondria. Used as a positive control or to study the consequences of site-specific superoxide production [31]. |
| d-Amino Acid Oxidase (DAAO) | Controlled intracellular H₂O₂ generation | A genetically encoded system that allows controlled, dose-dependent generation of H₂O₂ inside cells by adding d-alanine. Excellent for mechanistic studies of H₂O2-mediated toxicity [31]. |
Troubleshooting Guides & FAQs
FAQ 1: My DCF fluorescence signal is very high, but other markers of oxidative stress (like protein carbonyls) are low. What could be the cause? This is a classic sign of artefactual signal generation from the DCFH-DA probe. The most likely cause is redox cycling, where the partially oxidized DCF radical reacts with oxygen to generate more superoxide and H₂O₂, artificially amplifying the signal [32]. Other causes include interference from cellular peroxidases or transition metals in your buffer.
- Solution: Do not rely on DCFH-DA alone. Confirm oxidative stress using a more specific method, such as measuring the GSH/GSSG ratio, protein carbonyls, or using a genetically encoded sensor like roGFP.
FAQ 2: I am using "antioxidants" like N-acetylcysteine (NAC) to test the role of ROS in a toxic response, but the results are unclear. Why? The term "antioxidant" is often used imprecisely. NAC is a poor direct scavenger of H₂O₂ [31]. Its primary effects may be through increasing cellular cysteine pools for glutathione synthesis, cleaving protein disulfides, or generating H₂S, rather than directly neutralizing ROS.
- Solution: Be specific about the antioxidant's proposed mechanism. Use a panel of tools: enzymatic antioxidants (e.g., catalase), specific scavengers, and genetic knockdown of ROS-producing enzymes like NOX to build a compelling case.
FAQ 3: How can I be sure that the superoxide signal I'm measuring with MitoSOX is real and not an artefact? Simple fluorescence microscopy or plate reader measurements with MitoSOX can be misleading, as the fluorescence can come from both the specific product (2-OH-E+) and non-specific oxidation products.
- Solution: The gold standard is to validate your findings using HPLC to separate and quantify the specific 2-OH-E+ adduct [32]. Alternatively, use specific pharmacological inhibitors of mitochondrial superoxide production or correlate with other mitochondrial dysfunction parameters.
FAQ 4: The inhibitors apocynin and diphenyleneiodonium (DPI) are often used to implicate NOX enzymes. Is this sufficient? No. Both apocynin and DPI are not specific to NADPH oxidases (NOX). DPI inhibits all flavoproteins, including mitochondrial complex I and nitric oxide synthases [31].
- Solution: Use more specific NOX inhibitors (if available) or, preferably, use genetic approaches such as siRNA knockdown or CRISPR/Cas9 knockout of specific NOX isoforms (e.g., NOX2, NOX4) to confirm their involvement.
The following workflow diagram integrates these troubleshooting concepts into a logical framework for diagnosing and resolving common ROS measurement issues.
Diagram 2: Troubleshooting Workflow for Common ROS Measurement Issues.
Frequently Asked Questions (FAQs)
Q1: What are the primary types of DNA damage my assays might detect, and what are their common causes? DNA damage can be broadly categorized based on its origin. Endogenous damage arises from within the cell, including reactive oxygen species (ROS) from metabolism, hydrolysis, and replication errors such as base mismatches or slippage at repetitive sequences [36]. Exogenous damage is caused by external agents like UV radiation (creating cyclobutane pyrimidine dimers), ionizing radiation (causing single- and double-strand breaks), and chemical agents (e.g., alkylating agents, crosslinking agents) [36].
Q2: Which DNA repair pathways are most critical to consider in the context of compound toxicity screening? Cells employ several major, substrate-specific repair pathways. The choice of assay can help infer which pathway is active. Key pathways include:
- Base Excision Repair (BER): Corrects small, non-helix-distorting base lesions, such as those caused by oxidation or alkylation [36].
- Nucleotide Excision Repair (NER): Addresses bulky, helix-distorting lesions, such as those induced by UV light [36].
- Mismatch Repair (MMR): Corrects errors of DNA replication, such as base-base mismatches and small insertion/deletion loops [36].
- Homologous Recombination (HR) & Non-Homologous End Joining (NHEJ): These are the two main pathways for repairing DNA double-strand breaks, with HR being error-free and requiring a sister chromatid template, and NHEJ being error-prone [36].
Q3: My high-throughput genotoxicity screening results show inconsistencies. What could be the source? Inconsistencies in high-throughput screening (HTS) can stem from several factors:
- Experimental Condition Variability: Results are highly sensitive to species, administration route, and measurement indicators (e.g., LD50, TDLo) [37].
- Data Imbalance: Sparse data for specific target endpoints (e.g., human oral TDLo) can lead to poor model performance and unpredictable results [37].
- Compound-Specific Effects: The same compound can yield vastly different toxicity results under different testing conditions, making extrapolation challenging [37]. Using New Approach Methodologies (NAMs) that integrate in vitro and in silico data can help mitigate these issues and improve reliability [38] [39].
Q4: How can I leverage computational tools to reduce reliance on animal testing for genotoxicity assessment? Computational toxicology offers powerful alternatives:
- Machine Learning (ML) and AI: Models like graph convolution networks (GCNs) can predict acute toxicity by learning from chemical structure data and existing toxicological databases (e.g., TOXRIC, ToxValDB) [37] [38] [39].
- Integrated Testing Strategies: Frameworks like ToxACoL use an "Adjoint Correlation Learning" paradigm to model relationships between multiple toxicity endpoints, improving prediction accuracy for data-scarce endpoints and reducing the required training data by 70-80% [37].
- QSAR and Read-Across: Quantitative Structure-Activity Relationship (QSAR) models and read-across methods use existing data on similar chemicals to predict the toxicity of data-poor compounds [38] [39].
Troubleshooting Guides
The Comet Assay (Single Cell Gel Electrophoresis)
Purpose: To detect primary DNA damage at the level of single cells, including single- and double-strand breaks and alkali-labile sites [40] [41].
Table 1: Troubleshooting the Comet Assay
| Problem | Potential Cause | Solution |
|---|---|---|
| High Background DNA Damage in control cells | 1. Apoptotic or necrotic cells.2. Excessive UV exposure during processing.3. Overly harsh cell processing (e.g., vigorous pipetting). | 1. Use viability assays to ensure >85% cell viability. Exclude apoptotic cells by morphology.2. Use yellow or red light for sample processing.3. Use wide-bore tips and handle cell suspensions gently. |
| No "Comet" Tails | 1. Insufficient DNA unwinding or electrophoresis.2. Inappropriate lysis conditions.3. Electrophoresis buffer pH is incorrect. | 1. Optimize unwinding time (typically 20-40 min). Ensure electrophoresis voltage and time are adequate (e.g., 0.7 V/cm for 30 min).2. Ensure fresh lysis solution is used and contains all necessary components (e.g., DMSO, Triton X-100).3. Calibrate pH meter; ensure buffer pH is >13 for alkaline comet assay. |
| Irregular or Streaky Comets | 1. Uneven agarose layer.2. Air bubbles trapped in agarose.3. Cells are not in a single plane. | 1. Ensure slides are perfectly horizontal while agarose sets.2. Carefully pipette agarose to avoid bubbles.3. Use a low concentration of cells and ensure they are well-suspended before embedding. |
| High Intra-Sample Variability | 1. Inhomogeneous cell suspension.2. Inconsistent electrophoresis conditions.3. Slide staining is uneven. | 1. Mix cell suspension thoroughly before embedding. Prepare multiple replicate slides.2. Ensure the electrophoresis tank is level and buffer volume is consistent and sufficient.3. Use a fluorescent DNA stain at the appropriate concentration and ensure slides are mounted evenly. |
In Vivo Micronucleus Assay
Purpose: To detect chromosomal damage and/or damage to the mitotic apparatus, resulting in the formation of micronuclei in erythrocytes or other cell types [40].
Table 2: Troubleshooting the Micronucleus Assay
| Problem | Potential Cause | Solution |
|---|---|---|
| Low Frequency of Micronucleated Cells | 1. Insufficient dosing or sampling time.2. Bone marrow toxicity not considered.3. Inadequate number of cells scored. | 1. Confirm dose levels based on prior toxicity studies. Sample at appropriate times post-treatment (e.g., 24-48 hours for rodents).2. Monitor the proportion of immature (polychromatic) erythrocytes (PCE) to normochromatic erythrocytes (NCE). A decrease indicates bone marrow exposure.3. Score a minimum of 2000 PCEs per animal as per OECD guidelines. |
| High Variability Between Replicates | 1. Inconsistent animal handling or dosing.2. Subjective scoring criteria.3. Slide preparation artifacts. | 1. Standardize dosing procedures and randomize animal treatment.2. Use double-blinded scoring and train all scorers with reference images. Consider automated flow cytometry-based analysis [40].3. Follow standardized protocols for smear preparation and staining to ensure uniform cell distribution. |
| Difficulty Differentiating PCEs and NCEs | 1. Suboptimal staining.2. Use of an inappropriate stain. | 1. Use fresh Giemsa or acridine orange stain. Optimize staining time and concentration.2. Confirm the stain is suitable for distinguishing RNA (in PCEs) from DNA. |
High-Throughput Screening (HTS) and Computational Models
Purpose: To rapidly assess the genotoxic potential of thousands of compounds using in vitro and in silico methods [38].
Table 3: Troubleshooting HTS and Computational Models
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor Predictive Accuracy for Human Endpoints | 1. Model trained on imbalanced data (scarce human data).2. Failure to account for metabolic differences.3. Over-reliance on a single data type or assay. | 1. Use advanced ML paradigms like ToxACoL that use graph topology to model endpoint associations and transfer knowledge from data-rich to data-scarce endpoints [37].2. Incorporate in vitro metabolic activation systems (e.g., S9 mix) or use metabolic simulators in silico.3. Adopt an integrated weight-of-evidence approach using multiple assays and data sources (e.g., ToxValDB) to build consensus [38] [39]. |
| Model Fails to Generalize to New Chemical Classes | 1. The model is overfit to the training set.2. New chemicals are outside the model's "applicability domain". | 1. Use rigorous cross-validation and apply regularization techniques during model training. Ensure the training set is chemically diverse.2. Define the model's applicability domain (AD) using chemical descriptors. Flag predictions for compounds outside the AD for further scrutiny [37]. |
| Inconsistencies Between In Vitro and In Silico Results | 1. False positives/negatives in the HTS assay.2. The computational model does not capture the relevant biology. | 1. Confirm HTS results with a secondary, orthogonal assay (e.g., follow a positive Ames test with a micronucleus assay).2. Use mechanistic models that incorporate biological pathways, or multi-task models that learn from multiple toxicity endpoints simultaneously [37] [38]. |
Key Signaling Pathways in DNA Damage Response
The cellular response to DNA damage is a coordinated network of pathways that sense, signal, and repair lesions. Failure in these pathways is a hallmark of cancer and can be exploited in targeted therapies [42]. The diagram below illustrates the core DNA Damage Response (DDR) network.
Experimental Workflow for Genotoxicity Assessment
Integrating multiple assays provides a comprehensive view of a compound's genotoxic potential. The following workflow outlines a standard strategy for tiered genotoxicity testing.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Resources for Genotoxicity Research
| Item | Function/Description | Example Application |
|---|---|---|
| Bacterial Tester Strains (S. typhimurium TA98, TA100, etc.) | Engineered strains sensitive to specific types of base-pair or frameshift mutations. | The core reagent for the Ames test to assess mutagenicity [40]. |
| Mouse Lymphoma Cells (L5178Y Tk+/−) | Mammalian cell line for detecting gene mutations (at the Tk locus) and chromosomal damage. | In vitro mouse lymphoma assay (MLA) [40]. |
| Acridine Orange / Giemsa Stain | Fluorescent (Acridine Orange) or histological (Giemsa) dyes that bind nucleic acids. | Differentiating immature and mature erythrocytes for scoring micronucleated PCEs in the micronucleus assay [40]. |
| Low-Melting Point Agarose | A low-gelling temperature agarose used to embed cells without causing significant additional DNA damage. | Matrix for immobilizing single cells in the comet assay [40] [41]. |
| Specific DNA Repair Enzyme Inhibitors | Small molecules that selectively inhibit key DNA repair proteins (e.g., PARP, DNA-PK, ATM/ATR inhibitors). | Used as positive controls or to probe synthetic lethal interactions in targeted cancer therapy research [42] [43]. |
| ToxValDB / TOXRIC Database | Curated databases of experimental and derived human health-relevant toxicity data for thousands of chemicals. | Used for benchmarking, chemical prioritization, and as a training resource for QSAR and machine learning models [37] [39]. |
| CRISPRi/a Libraries (e.g., SPIDR) | Libraries of guide RNAs for targeted gene knockdown or activation across the genome or specific gene sets like DNA repair. | Systematically mapping genetic interactions and synthetic lethality in the DNA Damage Response (DDR) [43]. |
A Practical Guide to Cell Viability Assays and High-Throughput Implementation
Navigating the OECD Classification of Cell Viability Methods
Frequently Asked Questions
1. What is the OECD classification for cell viability methods and why is it important? The Organisation for Economic Co-operation and Development (OECD) provides a standardized classification system that categorizes cell viability assessment methods into distinct groups based on their operating principles. This classification is crucial for ensuring consistency, reliability, and regulatory compliance in scientific research, particularly in toxicology and drug development. The OECD guidelines are globally accepted and help validate results across different studies, making them essential for regulatory submissions of new drugs and chemicals [44].
2. What are the main categories of cell viability methods according to the OECD framework? The OECD classifies cell viability methods into four primary categories:
- Non-invasive cell structure damage assessment
- Invasive cell structure damage assessment
- Cell growth-based methods
- Cellular metabolism-based methods
Additionally, novel methods based on cell membrane potential have been identified as an emerging category beyond the current OECD classification [44].
3. How do I choose the most appropriate cell viability assay for my compound toxicity research? Selecting the optimal assay requires considering your specific experimental endpoints, available resources (instrumentation, budget, technical expertise), and the characteristics of your test compounds. Membrane integrity assays (like LDH or trypan blue) are ideal for detecting necrotic cell death, while metabolic assays (like MTT) better reflect cellular health. Apoptosis-specific assays (caspase activation, annexin V) are preferable when studying programmed cell death pathways. Always validate your method with positive and negative controls relevant to your toxicity model [44].
4. What are common pitfalls in cell viability assessment and how can I avoid them? Common issues include false positives/negatives due to assay interference, background signals in LDH assays, dye leakage in membrane permeability assays, and metabolic activity changes unrelated to viability. To minimize these problems: use multiple assay types to confirm results, include appropriate controls, optimize incubation times to prevent dye toxicity, consider compound characteristics that might interfere with assay chemistry, and validate methods against morphological assessment [44].
Troubleshooting Guides
Issue 1: Inconsistent Results in Membrane Integrity Assays
Problem: Variable results when using trypan blue or propidium iodide staining.
Solutions:
- Shorten incubation time: Prolonged incubation with trypan blue can lead to false positives as dye aggregates dissociate and penetrate viable cells. Keep incubation periods brief [44].
- Check osmolarity: Changes in solution osmolarity can cause spontaneous dye penetration into otherwise viable cells, generating false positives [44].
- Use fresh dyes: Prepare new dye solutions regularly as aging dyes can form aggregates that affect staining specificity.
- Combine with other methods: Confirm results with a metabolic activity assay to distinguish between true membrane damage and artifactual staining.
Issue 2: High Background in LDH Assay
Problem: Elevated background signals in lactate dehydrogenase (LDH) release assays.
Solutions:
- Centrifuge samples properly: Ensure complete removal of cells and debris before measuring supernatant LDH activity.
- Account for serum LDH: Fetal bovine serum contains LDH; use serum-free media during the assay period or subtract appropriate background controls.
- Check compound interference: Some test compounds might inhibit or enhance LDH activity; include appropriate controls without cells to detect interference.
- Validate in your system: LDH may underestimate cytotoxicity in certain co-culture systems; confirm with an alternative viability method [44].
Issue 3: Discrepancies Between Metabolic and Membrane Integrity Assays
Problem: Different viability conclusions when comparing MTT/ATP assays with membrane dye exclusion.
Solutions:
- Consider biological context: Metabolic assays measure different aspects of cell health than membrane integrity assays. Senescent or quiescent cells may show reduced metabolic activity with intact membranes.
- Check assay timing: Early apoptosis may preserve metabolic activity despite membrane changes.
- Use multiple endpoints: Combine different assay types to gain comprehensive understanding of cell status.
- Include morphological assessment: Use microscopy to visually confirm cell health and identify potential confounding factors.
OECD Cell Viability Method Comparison
Table 1: Classification and Characteristics of Major Cell Viability Assessment Methods
| OECD Category | Specific Method | Measurement Principle | Common Applications | Key Limitations |
|---|---|---|---|---|
| Structural Cell Damage (Non-invasive) | LDH Release | Measures lactate dehydrogenase enzyme released from damaged cells | General cytotoxicity screening, high-throughput compound testing | High background in some systems, may underestimate cytotoxicity in co-cultures [44] |
| Adenylate Kinase (AK) Release | Detects AK enzyme released through compromised membranes | High-throughput toxicology | Potential leakage from stressed but viable cells | |
| Structural Cell Damage (Invasive) | Trypan Blue Exclusion | Dye penetration into membrane-compromised cells | Basic research, cell culture maintenance | False positives with prolonged incubation, underestimation of dead cells with short incubation [44] |
| Propidium Iodide Staining | DNA binding in cells with permeable membranes | Flow cytometry, apoptosis studies | Potential false positives from membrane invagination [44] | |
| Esterase Cleavage Assays (Calcein-AM) | Enzymatic conversion of non-fluorescent to fluorescent compounds | Live cell imaging, viability tracking | Dye leakage from viable cells, measures enzyme activity rather than direct viability [44] | |
| Cell Growth | Population Doubling | Increase in cell number over time | Long-term toxicity studies, cancer research | Does not detect non-dividing viable cells |
| Cellular Metabolism | MTT/MTS/XTT Assays | Mitochondrial reductase activity | Drug screening, toxicology | Affected by metabolic changes unrelated to viability [44] |
| ATP Assay | Cellular ATP levels | High-throughput screening, rapid toxicity assessment | Sensitive to handling conditions, requires cell lysis | |
| Beyond OECD Classification | Membrane Potential Assays | Changes in transmembrane electrical potential | Early apoptosis detection, mechanistic studies | Emerging methods, less standardized [44] |
Table 2: Research Reagent Solutions for Cell Viability Assessment
| Reagent/Kit | Manufacturer | Function | Compatible Detection Methods |
|---|---|---|---|
| ToxiLight BioAssay Kit | LONZA | Detects adenylate kinase (AK) release from damaged cells | Luminescence reader [44] |
| CytoTox Assay | Promega | Measures dead-cell protease activity released from compromised cells | Fluorescence microplate reader [44] |
| aCella-TOX | Promega | Detects Glyceraldehyde-3 Phosphate Dehydrogenase (G3PDH) release | Colorimetric microplate reader [44] |
| Vybrant/CyQUANT Cytotoxicity Assay | Thermo Fisher Scientific | Measures Glucose-6-phosphate dehydrogenase (G6PD) release | Fluorescence microplate reader [44] |
| SYTOX Dead Cell Stains | Thermo Fisher Scientific | Nucleic acid staining of membrane-compromised cells | Flow cytometry, fluorescence microscopy [44] |
| CellTox Green Cytotoxicity Assay | Promega | DNA-binding dye for dead cells | Fluorescence microplate reader, imaging [44] |
| Life/dead Kit | Thermo-Fisher Scientific | Dual staining combining membrane integrity and esterase activity | Flow cytometry, fluorescence microscopy [44] |
Experimental Protocols
Protocol 1: LDH Release Assay for Compound Toxicity Screening
Principle: Measures lactate dehydrogenase release from cells with compromised membranes [44].
Materials:
- LDH assay kit
- Clear 96-well plate
- Microplate reader capable of measuring 490-500 nm absorbance
- Compound treatment plates
- Centrifuge
Procedure:
- Seed cells in 96-well plates at optimal density and incubate for 24 hours.
- Treat cells with test compounds at appropriate concentrations, including vehicle controls and lysis controls (for maximum LDH release).
- Following treatment period (typically 24-48 hours), centrifuge plates at 250 × g for 10 minutes.
- Transfer 50 µL of supernatant from each well to a new clear 96-well plate.
- Add 50 µL of reaction mixture from LDH assay kit to each well.
- Incubate for 30 minutes at room temperature, protected from light.
- Measure absorbance at 490-500 nm, subtracting reference wavelength at 680 nm.
- Calculate percentage cytotoxicity: (Test compound LDH - Spontaneous LDH) / (Maximum LDH - Spontaneous LDH) × 100
Troubleshooting Notes: High background may occur with serum-containing media; consider serum-free conditions during assay. Some nanomaterials interfere with LDH measurement; validate with alternative methods [44].
Protocol 2: Trypan Blue Exclusion for Rapid Viability Assessment
Principle: Membrane-impermeant dye enters and stains dead cells with compromised membranes [44].
Materials:
- 0.4% Trypan blue solution
- Hemocytometer or automated cell counter
- PBS for dilution
- Microcentrifuge tubes
Procedure:
- Harvest cells by gentle trypsinization or scraping.
- Centrifuge cell suspension at 150 × g for 5 minutes and resuspend in PBS.
- Mix 10 µL of cell suspension with 10 µL of 0.4% trypan blue solution.
- Incubate for exactly 1-3 minutes (do not exceed 5 minutes).
- Load mixture onto hemocytometer or automated cell counter slide.
- Count unstained (viable) and blue-stained (non-viable) cells.
- Calculate viability percentage: Viable cells / Total cells × 100
Troubleshooting Notes: Strictly control incubation time as prolonged exposure can lead to false positives. For automated counters, validate settings with manual counting. For adherent cells, ensure complete detachment without causing additional damage [44].
Method Selection Workflow
Method Selection Workflow: This diagram outlines a systematic approach for selecting the most appropriate cell viability assay based on experimental requirements and constraints.
OECD Classification Framework
OECD Classification Framework: This diagram illustrates the hierarchical structure of the OECD classification system for cell viability assessment methods, including the five main categories and their specific methodologies.
Assay Selection Guide & Comparison
Frequently Asked Questions
Q1: How do I choose the right assay for my cell health assessment study? The choice depends on your experimental goals, cell type, and required throughput. For high-throughput screening where sensitivity and speed are critical, ATP-based luminescence assays are superior. For standard colorimetric measurement in academic settings with ample time, MTT is a common choice. If you want a simpler "add-mix-measure" colorimetric protocol, consider MTS, XTT, or WST-1 assays. [4] [45]
Q2: My MTT assay shows high background; what could be the cause? High background in MTT assays can result from several factors:
- Chemical interference from reducing compounds in your test compounds (ascorbic acid, sulfhydryl compounds)
- Exposure of MTT reagent to light or elevated pH during storage
- Microbial contamination in cell cultures
- Incomplete solubilization of formazan crystals Run appropriate controls without cells to test for chemical interference. [4] [45]
Q3: Why does my ATP assay show higher sensitivity compared to tetrazolium-based assays? ATP assays utilize luminescent detection, which generally offers greater sensitivity than colorimetric absorbance methods used in tetrazolium assays. While tetrazolium reduction assays typically detect 200-1,000 cells per well, luminescent ATP assays can detect fewer cells, making them more suitable for miniaturization and high-throughput applications. [45]
Q4: Can I multiplex these viability assays with other endpoints? Yes, but with considerations. The MTT assay requires solubilization solutions that destroy cell architecture, limiting multiplexing options unless the other assay is performed first. ATP assays involve cell lysis, making them endpoint measurements. For multiplexing, consider less destructive assays like the CellTiter-Fluor Assay, which measures protease activity, or the RealTime-Glo Assay, which allows continuous monitoring. [45]
Comparative Assay Characteristics
Table 1: Key characteristics of metabolic activity assays
| Assay Parameter | MTT | MTS/XTT/WST-1 | ATP-based Luminescence |
|---|---|---|---|
| Detection Method | Colorimetric (Absorbance) | Colorimetric (Absorbance) | Luminescence |
| Detection Sensitivity | 200-1,000 cells/well | 200-1,000 cells/well | Higher than tetrazolium assays |
| Assay Steps | Two-step procedure | Homogeneous "add-mix-measure" | Add-mix-measure |
| Incubation Time | 1-4 hours | 1-4 hours | 10 minutes to several hours |
| Signal Stability | Requires prompt reading | More stable than MTT | Stable for extended periods |
| Multiplexing Potential | Limited | Moderate | Limited (lytic method) |
| Key Limitations | Formazan solubilization required; chemical interference; reagent toxicity | Still susceptible to chemical interference | Luciferase enzyme inhibitors may interfere |
| Best Applications | Academic research; endpoint measurements | Higher-throughput colorimetric screening | High-throughput screening; maximal sensitivity |
Table 2: Troubleshooting common assay problems
| Problem | Possible Causes | Solutions |
|---|---|---|
| High Background Signal | Chemical reducing compounds; contaminated reagents; microbial contamination | Include no-cell controls; filter-sterilize reagents; use fresh solutions |
| Low Signal Intensity | Insufficient cells; suboptimal incubation time; loss of metabolic activity | Optimize cell seeding density; extend incubation time (avoiding toxicity); ensure cells in log growth phase |
| Poor Reproducibility | Inconsistent cell seeding; uneven solubilization; edge effects in plates | Standardize cell preparation; ensure complete formazan dissolution; use plate seals to prevent evaporation |
| Abnormal Cell Morphology | Cytotoxicity of assay reagents | Reduce MTT concentration or incubation time; consider less toxic alternatives |
Experimental Protocols
MTT Assay Protocol
The MTT assay measures the reduction of yellow tetrazolium salt to purple formazan crystals by metabolically active cells. [4] [46]
Reagent Preparation:
- MTT Solution: Dissolve MTT in DPBS to 5 mg/mL. Filter-sterilize (0.2 µm), protect from light, and store at 4°C. [4]
- Solubilization Solution: Prepare 40% dimethylformamide with 16% SDS in 2% glacial acetic acid, pH 4.7. [4]
Procedure for Adherent Cells:
- Plate cells in 96-well plates at optimized density (typically 1,000-100,000 cells/well). [46]
- Apply experimental treatments for desired duration.
- Add MTT solution to each well (final concentration 0.2-0.5 mg/mL).
- Incubate 2-4 hours at 37°C with 5% CO₂ until purple formazan crystals are visible.
- Carefully aspirate MTT solution without disturbing crystals.
- Add solubilization solution (DMSO, acidified isopropanol, or SDS solution).
- Agitate plate gently to completely dissolve crystals.
- Measure absorbance at 570 nm with reference wavelength of 630 nm. [4] [46]
Procedure for Suspension Cells:
- After treatment, centrifuge plate at 1,000 × g for 5 minutes.
- Aspirate supernatant carefully.
- Add MTT solution and resuspend cell pellet gently.
- Incubate 2-4 hours at 37°C.
- Centrifuge again to pellet cells with formazan crystals.
- Aspirate supernatant and add solubilization solution.
- Measure absorbance at 570 nm. [46]
ATP Assay Protocol
ATP assays measure cellular ATP content using luciferase enzyme, which produces light proportional to ATP concentration.
Procedure:
- Culture cells in white-walled multiwell plates to minimize light scattering.
- Apply experimental treatments.
- Equilibrate CellTiter-Glo Reagent to room temperature.
- Add equal volume of reagent to each well.
- Mix contents for 2 minutes on orbital shaker to induce cell lysis.
- Allow plate to incubate at room temperature for 10 minutes to stabilize signal.
- Measure luminescence using plate-reading luminometer. [45]
Assay Workflow Visualization
MTT Assay Workflow
ATP Assay Workflow
The Scientist's Toolkit
Table 3: Essential research reagents and materials
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| MTT Tetrazolium Salt | Substrate reduced by metabolically active cells to formazan | Light-sensitive; prepare fresh or store protected from light; cytotoxic at high concentrations |
| DMSO or Alternative Solvents | Dissolves formazan crystals for absorbance measurement | Use pure, sterile solvents; potential cytotoxicity at high concentrations |
| CellTiter-Glo Reagent | Luciferase-based system for ATP detection | Equilibrate to room temperature before use; compatible with multiwell formats |
| 96-Well Microplates | Cell culture and assay measurement | Use flat-bottom plates for adherence; white-walled for luminescence |
| Plate Reader | Detect absorbance or luminescence signals | Ensure proper calibration and wavelength selection (570 nm for MTT) |
| Sterile PBS | Physiological buffer for reagent preparation | Maintain pH at ~7.4 for optimal MTT stability and activity |
Advanced Technical Notes
Mechanistic Insights: While historically believed to measure specifically mitochondrial activity, MTT reduction occurs in multiple cellular compartments including mitochondria, endoplasmic reticulum, and plasma membrane. The assay reflects overall cellular metabolic activity and reducing power, primarily through NADH or similar reducing molecules. [4] [46] [45]
Metabolic Considerations: Tetrazolium reduction assays measure metabolic activity, not directly cell number. Culture conditions that alter metabolism (pH, glucose depletion, confluence) will affect reduction rates independent of cell number. Activated or rapidly dividing cells show higher reduction rates per cell than quiescent cells. [4] [45]
Toxicity Testing Application: In compound toxicity filtering research, these assays provide crucial data on cell health after compound exposure. Understanding each assay's mechanism ensures appropriate interpretation—what affects metabolic activity might not immediately affect ATP levels, and vice versa. For comprehensive assessment, consider orthogonal methods measuring different viability markers. [4] [45]
For researchers in drug development, accurately assessing cell health is a critical step in filtering compound toxicity. Membrane integrity assays provide a direct and reliable window into cell viability, as the loss of plasma membrane integrity is a definitive indicator of cell death. This technical support center details three cornerstone techniques for this purpose: the Lactate Dehydrogenase (LDH) Release assay, the Trypan Blue Exclusion assay, and modern fluorescent dye-based assays. The following guides, protocols, and troubleshooting FAQs are designed to help you execute these assays with precision and interpret your results with confidence, ensuring robust data for your pre-clinical toxicity research.
Assay Comparison at a Glance
The following table summarizes the key characteristics of the three primary membrane integrity assays to help you select the most appropriate method for your experimental needs.
| Assay Feature | LDH Release Assay [47] [48] | Trypan Blue Exclusion [49] [50] | Fluorescent Dyes (e.g., SYTO 9/PI) [51] |
|---|---|---|---|
| What It Measures | Release of cytoplasmic enzyme Lactate Dehydrogenase (LDH) into culture medium. | Physical exclusion of a dye by an intact cell membrane. | Membrane permeability to fluorescent nucleic acid stains. |
| Principle | Coupled enzymatic reaction detecting LDH activity; signal is proportional to dead cells. | Viable cells exclude the dye and appear clear; non-viable cells uptake dye and appear blue. | Live cells stain green with SYTO 9; dead cells with compromised membranes stain red with PI. |
| Detection Method | Colorimetric, Fluorometric, or Luminescent (plate reader). | Bright-field microscopy with a hemacytometer. | Flow cytometry or fluorescence microscopy. |
| Throughput | High (96- or 384-well plate format). | Low (manual counting). | High (flow cytometry allows for thousands of cells in seconds). |
| Key Advantage | Homogeneous format; multiplexing capability; objective, quantitative readout. | Simple, inexpensive, and rapid. | Distinguishes live, dead, and an intermediate "damaged" population. |
| Key Limitation | LDH background in serum-containing media requires careful control setup. | Subjective; cannot detect early-stage membrane damage. | Requires specialized and costly equipment (flow cytometer/confocal microscope). |
Detailed Experimental Protocols
LDH Release Assay (Colorimetric)
This protocol measures the release of the stable cytoplasmic enzyme lactate dehydrogenase (LDH) from cells with damaged membranes. The activity of LDH in the culture supernatant is directly proportional to the number of dead or damaged cells [48].
Materials from Standardized Kits Typically Include:
- LDH Assay Buffer and Substrate Mix (containing INT, lactate, NAD⁺)
- Lysis Solution (e.g., 9% Triton X-100)
- Stop Solution (e.g., 1M Acetic Acid)
- NADH Standard Control [48]
Step-by-Step Procedure:
- Cell Culture Preparation: Seed cells in a 96-well flat-bottom microtiter plate at a density of 1 × 10⁴ – 5 × 10⁴ cells/well in 100 µL of culture medium. Incubate overnight in a humidified 37°C, 5% CO₂ incubator [48].
- Application of Treatment: Apply your compound treatment to the cells. Ensure you include the following essential controls in triplicate [48]:
- Spontaneous LDH Release Control: Untreated cells (background cell death).
- Maximum LDH Release Control: Cells treated with lysis solution (100% death control).
- Culture Medium Background: Medium without cells (serum background control).
- Supernatant Collection: After treatment, centrifuge the microtiter plate at 1,500–2,000 rpm for 5 minutes. Carefully transfer 50 µL of the culture supernatant from each well to a new, clear assay plate without disturbing the cell pellet [48].
- Reaction Setup and Measurement: Prepare the reaction mixture as per your kit's instructions. Typically, you will add a prepared substrate mix to each well containing the supernatant. Incubate the plate for 30 minutes at room temperature, protected from light. Add the stop solution and measure the absorbance at 490 nm using a microplate reader [48].
Trypan Blue Exclusion Assay
This classic, straightforward method distinguishes viable from non-viable cells based on the integrity of the cell membrane. Viable cells with intact membranes exclude the trypan blue dye, while non-viable cells permit its entry [50].
Key Reagent:
- 0.4% Trypan Blue solution (store in a dark bottle and filter after prolonged storage) [50].
Step-by-Step Procedure:
- Prepare Cell Suspension: Centrifuge an aliquot of your cell suspension and discard the supernatant. Resuspend the cell pellet in 1 mL of PBS or serum-free medium. Using a serum-free solution is critical, as serum proteins can stain with trypan blue and produce misleading results [50].
- Stain Cells: Mix 1 part of the 0.4% trypan blue solution with 1 part of the cell suspension (a 1:1 dilution). Gently pipette to mix and allow the mixture to incubate for approximately 3 minutes at room temperature [50].
- Count Cells: Within 3 to 5 minutes of mixing, apply a drop of the mixture to a hemacytometer. Place it on the stage of a microscope and focus on the cells [50].
- Calculate Viability:
- Count the unstained (viable) and stained (nonviable) cells separately.
- Percentage of Viable Cells (%) = (Total Number of Viable Cells per mL / Total Number of Cells per mL) × 100 [50].
Fluorescent LIVE/DEAD Assay with Flow Cytometry
This protocol uses the differential staining of SYTO 9 and propidium iodide (PI) to provide a rapid, high-throughput, and quantitative assessment of yeast survival after stress or compound treatment. It can distinguish live, dead, and damaged cell populations [51].
Key Reagents:
- FungaLight Yeast LIVE/DEAD Kit (or SYTO 9 and PI purchased separately)
- Sterile 0.85% saline buffer (minimizes staining artifacts) [51]
Step-by-Step Procedure:
- Apply Stress/Treatment: Treat your yeast cells (e.g., Candida glabrata) with the compound of interest. Include a mock treatment and a lethal dose control (e.g., 1M H₂O₂). Incubate for the desired time (e.g., 120 min at 30°C with shaking) [51].
- Prepare Cells for Staining: Pellet cells by centrifugation. Carefully aspirate the supernatant and resuspend the cells in sterile 0.85% saline buffer, standardizing to an optical density (e.g., OD₆₀₀ = 1) [51].
- Stain Cells: Prepare working stocks of SYTO 9 (33.4 µM, prepare fresh) and PI (0.2 mM). Add the dyes to the cell suspension and incubate. The optimal staining time and dye concentrations should be determined empirically [51].
- Analyze by Flow Cytometry: Analyze the samples using a flow cytometer. Live cells with intact membranes will fluoresce green (SYTO 9), while dead cells with compromised membranes will fluoresce red (PI). Cells with damaged membranes may show an intermediate staining pattern [51].
Troubleshooting FAQs
Q1: My LDH assay shows a high background signal in all wells, including the medium-only control. What could be the cause?
- Serum Interference: Fetal Bovine Serum (FBS) used in culture media contains endogenous LDH. Always subtract the background signal from your medium-only control from all experimental values [48].
- Cell Handling: Overly vigorous pipetting or scraping can mechanically lyse cells, causing unintended LDH release. Handle cells gently during all steps [48].
- Insufficient Centrifugation: If cells are not properly pelleted during supernatant collection, you may carry over intact cells, which will lyse in the assay and contribute to background. Ensure centrifugation speed and time are adequate [48].
Q2: During Trypan Blue counting, almost all my cells appear blue, even in my healthy control culture. What might have gone wrong?
- Incubation Time: Leaving cells in contact with trypan blue for too long (>5-10 minutes) can be toxic and lead to increased dye uptake. Count cells within 3-5 minutes of mixing [50].
- Serum Presence: As noted in the protocol, performing the assay in a serum-free solution is mandatory. Serum proteins bind the dye and create a blue background, making it impossible to distinguish viable cells [50].
- Cell Condition: The culture may genuinely be non-viable. Confirm the health of your control culture using an alternative method if possible.
Q3: In my fluorescent SYTO 9/PI staining, I see high background fluorescence or a poor distinction between live and dead populations. How can I improve this?
- Staining Buffer: The composition of the staining buffer is critical. Using deionized water or growth media can cause artifacts. For yeast, 0.85% saline buffer has been shown to produce minimal background [51].
- Dye Concentration and Incubation: The concentration of SYTO 9 and PI, as well as the incubation time, must be optimized for your specific cell type and conditions. Perform a dye titration experiment [51] [52].
- Autofluorescence/Cross-talk: Include an unstained control to assess cellular autofluorescence. For multicolor experiments, use single-stain controls to check for fluorescence cross-talk between the green (SYTO 9) and red (PI) channels and adjust your flow cytometry compensation or microscope settings accordingly [52] [53].
Q4: I get inconsistent results between my membrane integrity assay (e.g., LDH or Trypan Blue) and my colony-forming unit (CFU) assay. Why?
- Fundamental Difference: This is a common and expected finding that reflects the different biological endpoints these assays measure. Membrane integrity assays provide a snapshot of viability immediately after treatment, identifying cells that have reached a "point of no return" [51]. A CFU assay, however, measures clonogenicity—the ability of a cell to recover, replicate, and form a colony days later [51]. A cell with a slightly damaged membrane might be scored as "nonviable" by Trypan Blue but could repair itself and form a colony, while a cell that is metabolically doomed might initially exclude dye but never divide again.
The Scientist's Toolkit: Essential Research Reagents
| Reagent / Kit | Primary Function | Key Considerations |
|---|---|---|
| CytoTox-ONE Assay [47] | Fluorometric measurement of LDH release from damaged cells. | Homogeneous format (no transfer step); 10-minute incubation; can be multiplexed with other assays. |
| FungaLight LIVE/DEAD Kit [51] | Two-component fluorescent stain (SYTO 9 & PI) for viability via flow cytometry. | Distinguishes live, dead, and damaged cells; requires flow cytometer or fluorescence microscope. |
| Trypan Blue Solution [50] | Dye for microscopic viability count based on membrane exclusion. | Must be used serum-free; incubation time must be short (<5 min); subjective to user counting. |
| LDH Assay Buffer & Substrate Mix [48] | Contains reagents (INT, NAD⁺, lactate) for the coupled enzymatic reaction to detect LDH. | Avoid repeated freeze-thaw cycles; store in aliquots at -20°C. |
| Lysis Solution (Triton X-100) [48] | Provides the maximum LDH release control by lysing all cells in a well. | Critical for calculating the percentage of cytotoxicity in LDH assays. |
| Propidium Iodide (PI) [51] | Red-fluorescent nucleic acid stain that is excluded by viable cells. | A common component of many LIVE/DEAD assays; can often be used alone. |
Multiplexing Assay Troubleshooting Guide
This guide addresses common issues encountered when performing multiplexed assays for viability, cytotoxicity, and apoptosis.
Signal Detection Issues
| Problem Description | Possible Causes | Recommendations |
|---|---|---|
| Weak or No Signal [54] | Critical reagent omitted [54] | Confirm all reagents were added according to protocol [54]. |
| Low target expression [54] | Use a control slide/tissue to confirm target expression and rule out reagent issues [54]. | |
| Insufficient amplification [54] | Ensure the correct number of complete amplification rounds (e.g., at least 8) are performed [54]. | |
| Missing Signal in One Channel [54] | Incorrect imager settings or filter sets [54] | Confirm the correct laser, filter set (e.g., Texas Red for 594 nm, not TRITC), excitation, and emission settings per protocol [54]. |
| Specific oligos or antibodies not added [54] | Confirm all amplification oligos and complementary oligos for each fluorescent channel were added [54]. | |
| Low Bead Counts (Luminex) [55] | Sample debris or aggregation [55] | Thaw, vortex, and centrifuge samples at ≥10,000 x g to remove particulates. For sticky samples, resuspend beads in Wash Buffer and read within 4 hours [55]. |
| Inadequate instrument maintenance [55] | Clean instrument regularly (e.g., using enhanced NaOH and bleach methods for MAGPIX). Ensure proper calibration [55]. |
Background and Specificity Problems
| Problem Description | Possible Causes | Recommendations |
|---|---|---|
| High Background Fluorescence [54] | Non-specific antibody binding [54] | Titrate antibody concentration (e.g., 0.5-fold decrease may reduce background) [54]. |
| Necrotic tissue or autofluorescence [54] | For autofluorescent tissues (e.g., brain), use reagents like TrueBlack Lipofuscin or place a strong phenotypic marker in the problematic channel during panel design [54]. | |
| Deviation from antigen retrieval protocol [54] | Use the antigen retrieval method specified in the protocol [54]. | |
| Spectral Bleed-Through (Overlapping Signals) [54] | Strong signal from one channel bleeding into another [54] | During panel design, spectrally separate strong markers from weakly expressed ones. Decrease antibody concentration for the strong marker [54]. |
| Incorrect oligo combination [54] | Ensure different imaging rounds do not contain complementary oligos of the same fluorescent channel [54]. | |
| High Assay Variability [55] | Inconsistent sample/reagent handling [55] | Warm all reagents to room temperature before use. Vortex thoroughly. Use proper pipetting technique and calibrated pipettes [55]. |
| Incomplete or inconsistent washing [55] | Use a calibrated orbital shaker (500-800 rpm). For manual washing, ensure plate is firmly attached to magnetic separator and blot gently after decanting [55]. |
Assay Performance and Optimization
| Problem Description | Possible Causes | Recommendations |
|---|---|---|
| Poor Signal Separability in Digital PCR [56] | Suboptimal elongation temperature or primer/probe interactions [56] | Perform single-plex reactions first to optimize temperature for each assay. Use in silico tools to check for primer/probe dimers before testing [56]. |
| Loss of Signal Over Time [54] [55] | Delayed imaging or reading [54] [55] | Image fluorescent slides within 8 hours of staining [54]. Read Luminex plates immediately; if stored, keep at 2-8°C for up to 72 hours and re-agitate before reading [55]. |
| Inaccurate Cytotoxicity Interpretation | Using a single endpoint assay [57] [58] | Use live-cell kinetic assays (e.g., Incucyte Cytotox Dyes) to monitor dynamics over time, or multiplex with viability and apoptosis assays in the same well [57] [58]. |
Frequently Asked Questions (FAQs)
Q1: Why should I multiplex viability, cytotoxicity, and apoptosis assays instead of running them separately? Multiplexing provides several key advantages:
- Data Quality: It enables normalization for differences in cell number and provides a more complete, internally controlled picture of cell health from the same population of cells, reducing variability that can occur when running parallel assays [59] [57].
- Mechanistic Insight: Combining these readouts supports conclusions about the mechanism of cell death (e.g., apoptotic vs. necrotic) [59].
- Efficiency: It saves precious time, sample volume (e.g., only 25-50 µL required), and reagents, while also reducing hands-on labor and overall costs [60] [57].
Q2: Can I perform these multiplexed assays with live-cell, kinetic monitoring? Yes. Live-cell kinetic assays are highly suitable for multiplexing. For example, you can use instruments like the Incucyte system with compatible dyes (e.g., Cytotox Dyes for membrane integrity) to monitor cytotoxicity continuously in your incubator over time, without fixing or lifting cells. These kinetic assays can also be multiplexed with endpoint apoptosis or viability assays [57] [58].
Q3: My multiplex assay shows unexpected background in one fluorescent channel. What steps can I take to resolve this? First, confirm the correct filter sets are being used on your imager, as misalignment is a common cause [54]. If the problem persists, it could be due to:
- Autofluorescence: Common in certain tissues like brain; consider using an autofluorescence quenching reagent [54].
- Antibody Concentration: The antibody for that channel may be too concentrated; try a 0.5-fold dilution [54].
- Spectral Bleed-Through: If a very bright marker in one channel is causing spillover into an adjacent channel, try reducing the concentration of the bright marker's antibody or reassign it to a more spectrally distant channel in your panel design [54].
Q4: How do I ensure my multiplex digital PCR assay is optimized? Stilla Technologies recommends a systematic approach [56]:
- Single-Plex First: Always run and optimize each primer/probe set individually in a single-plex reaction before combining them.
- Temperature Optimization: Evaluate a range of elongation temperatures to find a common optimal temperature that provides good separability between positive and negative populations for all targets without non-specific amplification.
- In Silico Design: Use software tools to check for potential primer-primer or primer-probe interactions before ordering reagents.
Q5: I have low bead counts in my Luminex assay. What can I do? Low bead counts are often related to sample preparation or bead handling [55]:
- Clarify Samples: Always thaw, vortex, and centrifuge samples (≥10,000 x g) before use to remove debris and lipids.
- Prevent Aggregation: Resuspend beads in Wash Buffer (instead of Sheath Fluid) for the final reading to prevent clumping, but read the plate within 4 hours.
- Check Washer Settings: If using a plate washer, ensure the aspiration probe does not touch the bottom of the well where beads are collected.
Experimental Workflow for Multiplexed Cell Health Assessment
The following diagram illustrates a generalized workflow for setting up and running a multiplexed experiment to measure viability, cytotoxicity, and apoptosis. This workflow incorporates steps from various platforms to highlight key considerations.
Research Reagent Solutions
The table below lists key reagents and their functions for multiplexed cell health assays.
| Reagent / Kit Name | Primary Function | Key Feature / Application Note |
|---|---|---|
| MILLIPLEX Multiplex Kits [61] | Simultaneously measure multiple soluble biomarkers (e.g., cytokines) via bead-based immunoassays. | One-day assay protocol available; high lot-to-lot reproducibility; validated for multiple species [61]. |
| Incucyte Cytotox Dyes [58] | Label nuclei of dying cells upon loss of membrane integrity (cytotoxicity). | Live-cell, kinetic, mix-and-read format; can be multiplexed with proliferation and apoptosis dyes (e.g., Nuclight, Caspase-3/7) [58]. |
| Incucyte Caspase-3/7 Dye [58] | Detect activation of caspase-3/7 enzymes, a key indicator of apoptosis. | Enables apoptosis monitoring in real time when multiplexed with cytotoxicity and viability assays [58]. |
| Incucyte Nuclight Reagents [58] | Stably label nuclei in live cells for automated cell counting (proliferation/viability). | Provides a viable cell count, allowing direct calculation of a cytotoxic index when used with Cytotox Dyes [58]. |
| ApoTox-Glo, MultiTox-Glo Assays [57] | Multiplexed triplex assays measuring viability, cytotoxicity, and caspase activity (apoptosis) in a single well. | End-point assay format; designed for compatibility to measure three key parameters from one sample aliquot [57]. |
| CellTox Green Assay [57] | Fluorescent cytotoxicity assay that measures changes in membrane integrity. | Live-cell kinetic assay; can be multiplexed with viability assays like CellTiter-Glo [57]. |
| LDH-Glo Assay [57] | Bioluminescent assay to measure lactate dehydrogenase (LDH) release upon cell membrane damage. | Homogeneous, bioluminescent format suitable for multiplexing and higher-throughput screening [57]. |
Implementing Quantitative High-throughput Screening (qHTS) for Toxicity Profiling
Troubleshooting Guide: Common qHTS Experimental Issues
Why are my concentration-response curves poorly defined or parameter estimates highly variable?
Poorly defined curves often result from suboptimal experimental design rather than assay execution.
- Root Cause: Inadequate concentration range that fails to define both the upper and lower asymptotes of the response curve, improper spacing of concentration points, or high measurement variability [62].
- Solution: Ensure your tested concentration range adequately captures the full response curve. Simulated data shows that when the concentration range defines both asymptotes (e.g., AC50 = 0.1 μM with Emax ≥50%), parameter estimates like AC50 are precise. When only one asymptote is defined, confidence intervals for AC50 can span several orders of magnitude [62].
- Preventive Measure: Conduct pilot studies to approximate the AC50, then design your dilution series to capture data points both above and below this value. Increase experimental replicates to improve measurement precision [62].
How do I distinguish true bioactivity from cytotoxic interference in my qHTS assay?
Cytotoxicity can mask specific bioactivity or generate false positives.
- Root Cause: Compounds causing general cell death can appear as "hits" in a target-specific assay, especially at higher concentrations [7].
- Solution: Implement orthogonal counter-screens to detect cytotoxicity.
- Viability Metrics: Incorporate multiplexed cytotoxicity assays such as metabolic activity (e.g., Realtime-Glo MT) and membrane integrity (e.g., Lactate Dehydrogenase (LDH) release) measured from the same well or parallel plates [7].
- Morphological Profiling: Use the Cell Painting assay to detect subtle, specific morphological changes indicative of a targeted mechanism of action, which often occurs at lower concentrations than general cytotoxicity [7].
- Interpretation: A compound showing activity in a target assay only at concentrations that also cause cytotoxicity in counter-screens is likely a false positive. Specific bioactivity is more likely if a compound shows a targeted response (e.g., in Cell Painting or a functional assay) at concentrations below the cytotoxic threshold [7].
What steps can I take to minimize false positives and false negatives?
Minimizing incorrect activity calls is crucial for efficient use of resources in follow-up studies.
For False Positives:
- Counter-Screening: Use assays designed to identify compounds that interfere with the detection technology (e.g., auto-fluorescent compounds in a fluorescence-based assay, luciferase inhibitors in a reporter assay) [63].
- Orthogonal Assays: Confirm primary HTS hits using a different detection technology or assay format (e.g., confirm a binding hit with a functional cellular assay) [63].
- Hit Confirmation: Always re-test primary hits from the original stock to confirm activity before initiating dose-response studies [63].
For False Negatives:
- Use qHTS over HTS: Traditional single-concentration HTS has a higher prevalence of false negatives compared to qHTS, which tests multiple concentrations [64].
- Expand Concentration Range: "Flat" profiles from highly potent compounds can be misclassified as inactive if the tested concentration range is too low to elicit a response. Ensure your maximum concentration is sufficiently high [62].
- Data Analysis: Employ advanced data analytics and machine learning that can help identify potential false negatives from primary screening data [63].
Frequently Asked Questions (FAQs)
What is the fundamental difference between traditional HTS and qHTS?
- Traditional HTS tests each compound in a library at a single concentration (often 10 μM), generating a simple "active/inactive" call. This approach is burdened by higher rates of false positives and false negatives and requires extensive follow-up testing to generate concentration-response data [64] [65].
- qHTS tests compounds across a range of multiple concentrations (e.g., 8-15 points) in the primary screen. This immediately generates concentration-response curves for every compound, providing quantitative data on potency (e.g., AC50, IC50) and efficacy (Emax). qHTS more efficiently identifies a wide range of activities and provides richer data sets for structure-activity relationship analysis directly from the primary screen [64] [62].
When should I use a cell-based assay versus a biochemical assay for toxicity profiling?
The choice depends on the biological question and the nature of the target. Table: Comparison of Cell-based and Biochemical Assays for qHTS
| Feature | Cell-Based Assays | Biochemical Assays |
|---|---|---|
| Physiological Context | High; includes cellular metabolism, membrane permeability, and complex pathway interactions [63]. | Low; conducted in a cell-free environment [63]. |
| Primary Use Case | Phenotypic screening, functional responses, cytotoxicity, understanding MoA in a systems context [7] [63]. | Target-based screening for direct binding or modulation of a purified protein/enzyme [63]. |
| Throughput | Generally lower due to longer preparation and incubation times. | Generally higher and more straightforward. |
| Interference | Susceptible to non-specific cytotoxicity. | Susceptible to assay-specific interference (e.g., compound aggregation, fluorescence). |
| Hit Identification | Identifies compounds that act in a physiologically relevant environment. | Identifies compounds that directly interact with the target. |
How can I leverage machine learning and public data for my qHTS studies?
- Utilize Public Toxicity Databases: Resources like ToxValDB (containing over 240,000 records of experimental and derived toxicity values) and the TOXRIC database (with 59 multi-species acute toxicity endpoints) provide vast amounts of curated data for model training and benchmarking [39] [37].
- Adopt Advanced Modeling Paradigms: Frameworks like ToxACoL use adjoint correlation learning to model relationships between multiple toxicity endpoints (e.g., different species, routes). This allows for knowledge transfer from data-rich endpoints (e.g., rodent) to predict data-scarce human endpoints, significantly improving prediction accuracy for human toxicity with less training data [37].
- Application: These models can be used to prioritize compounds for screening, fill data gaps for untested chemicals, and gain insights into structural alerts and potential mechanisms of acute toxicity [39] [37].
Experimental Workflow & Data Analysis
qHTS Experimental Workflow
The following diagram illustrates the key stages of a qHTS campaign, from assay development to hit confirmation.
qHTS Data Analysis Pathway
After data acquisition, a robust analytical pathway is required to transform raw data into reliable hits.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Reagents and Materials for qHTS in Toxicity Profiling
| Item | Function / Application | Example / Notes |
|---|---|---|
| Cell Lines | Provide the biological system for cell-based assays. | Primary human hepatocytes are relevant for liver toxicity studies [7]. Immortalized lines (e.g., HepG2) are also common. |
| Biochemical Assay Kits | Measure specific enzymatic activities or binding events in cell-free systems. | Kits for kinase activity, protease activity, receptor binding, etc. |
| Viability/Cytotoxicity Assays | Assess general cellular health and detect cytotoxic compounds. | Metabolic Activity (MT/MTT): Measures mitochondrial function [7]. LDH Release: Measures membrane integrity [7]. |
| Cell Painting Dyes | Enable high-content morphological profiling by staining cellular components. | Six fluorescent dyes to label DNA, RNA, mitochondria, actin, Golgi, and ER [7]. |
| qHTS Compound Library | The collection of chemicals screened for biological activity. | Libraries should be diverse, high-quality, and curated for drug-likeness. Evotec's library of >850,000 compounds is an example [63]. |
| Microtiter Plates | The vessel for miniaturized, parallel assay execution. | 384-well or 1536-well plates are standard for HTS to reduce reagent use and increase throughput [62] [65]. |
| Automation & Detection Platforms | Enable rapid liquid handling, incubation, and signal reading. | Robotic plate handlers, dispensers, and high-sensitivity plate readers (e.g., for fluorescence, luminescence, absorbance) [63]. |
Overcoming Common Pitfalls and Optimizing Assay Design
Troubleshooting Guides
This guide addresses common experimental issues in compound toxicity studies, helping you identify and correct critical parameters to ensure data reliability.
| Problem Symptom | Possible Root Cause | Recommended Solution | Key Parameters to Re-Evaluate |
|---|---|---|---|
| High well-to-well variability | Inconsistent cell seeding density; improper compound serial dilution. | Standardize cell suspension protocol; use electronic multichannel pipettes for dilution. | Timing (cell recovery post-thaw); Dosage (dilution factor accuracy). |
| Inconsistent IC50 values | Compound precipitation at high concentrations; extended pre-dilution storage. | Include a visual check for precipitation; prepare fresh compound stocks for each assay. | Dosage (solubility limit); Timing (compound stability). |
| Poor Z'-factor (<0.5) | Low signal-to-noise ratio; excessive background fluorescence from DMSO. | Optimize assay reagent incubation time; reduce final DMSO concentration (e.g., to <0.5%). | Timing (signal development period); Dosage (DMSO vehicle concentration). |
| No dose-response observed | Incorrect stock concentration; cells reaching over-confluence before endpoint measurement. | Verify stock concentration via QC (e.g., LC-MS); optimize seeding density and exposure period. | Dosage (actual concentration); Exposure Period (cell doubling time). |
Frequently Asked Questions (FAQs)
Q1: How do we determine the appropriate range of dosages for a novel compound? Start with a broad range (e.g., 10 µM to 1 pM) based on the known toxicity of structural analogs or a preliminary single-high-dose screen. Subsequent experiments should use a narrower range with 3-4-fold serial dilutions centered on the estimated IC₅₀ to accurately define the dose-response curve.
Q2: What is the critical timing for adding the detection reagent in a cell viability assay? The reagent should be added immediately after the compound exposure period concludes. A significant delay (e.g., >30 minutes) can allow cells to initiate recovery processes, skewing results. Adhere strictly to the manufacturer's protocol for incubation time before reading the plate.
Q3: Our negative control shows reduced viability. What is the most likely cause? This often indicates cytotoxicity from the vehicle, typically DMSO. Ensure the final concentration of DMSO in all wells, including controls, does not exceed the tolerance level for your cell line (usually 0.1% - 1.0%). Prepare compound stocks at a high concentration to minimize the vehicle volume added.
Q4: How long should a compound exposure period typically last? The standard exposure period is 24, 48, or 72 hours. A 48-hour exposure is common for many immortalized cell lines. The choice depends on the compound's mechanism of action and the cell line's doubling time. Longer exposures may be needed for cytostatic compounds.
Q5: What steps can we take if a positive control fails to produce the expected signal? Verify the preparation and storage conditions of the control compound (e.g., Staurosporine for apoptosis). Confirm that the assay reagents are within their expiration date and were stored correctly. Finally, re-optimize the concentration and exposure time of the positive control for your specific experimental setup.
The following tables consolidate key quantitative benchmarks for designing and interpreting compound toxicity experiments.
Table 1: Standard Dosage and Exposure Parameters for Common Assays
| Assay Type | Typical Dosage Range | Standard Exposure Period | Key Readout |
|---|---|---|---|
| MTT/Cell Viability | 1 nM - 100 µM | 48 - 72 hours | IC₅₀ / EC₅₀ |
| Caspase-3/7 Apoptosis | 10 nM - 30 µM | 4 - 24 hours | Fold Induction |
| High Content Imaging (Cell Count) | 1 nM - 10 µM | 72 hours | IC₅₀ |
| Membrane Integrity (LDH) | 100 nM - 50 µM | 24 hours | % Cytotoxicity |
Table 2: Acceptance Criteria for Assay Quality Control
| Parameter | Formula | Target Value | Interpretation |
|---|---|---|---|
| Z'-Factor | 1 - (3σc⁺ + 3σc⁻) / |μc⁺ - μc⁻| | >0.5 | Excellent assay suitable for HTS. |
| Signal-to-Noise (S/N) | (μsignal - μbackground) / σ_background | >10 | Robust and reproducible signal. |
| Coefficient of Variation (CV) | (σ / μ) × 100 | <20% | Acceptable level of technical variation. |
Experimental Protocol: Determining IC₅₀
This protocol details the steps to determine the half-maximal inhibitory concentration (IC₅₀) of a compound on cell viability, using a 96-well format and a standard MTT assay.
Key Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| Cell Culture Medium | Provides essential nutrients to maintain cells during compound exposure. |
| DMSO (Cell Culture Grade) | Serves as a vehicle to solubilize and deliver water-insoluble test compounds. |
| MTT Reagent | A yellow tetrazolium salt reduced to purple formazan by metabolically active cells. |
| Lysis Buffer (SDS Solution) | Solubilizes cells and the formed formazan crystals to create a homogeneous colored solution. |
| Positive Control (e.g., Staurosporine) | A known cytotoxic compound used to validate assay performance and maximum effect. |
Methodology
- Cell Seeding: Harvest exponentially growing cells and seed them in a 96-well plate at a density of 5,000 - 10,000 cells per well in 100 µL of medium. Incubate for 24 hours to allow cell adhesion.
- Compound Treatment:
- Prepare a 10 mM stock of the test compound in DMSO.
- Perform a 1:3 or 1:4 serial dilution in DMSO to create an 11-point dose-response curve.
- Further dilute the compound intermediates in medium so that the final DMSO concentration is ≤0.5% when added to cells. Add 100 µL of these working solutions to the cell plate. Include a vehicle control (0.5% DMSO) and a positive control.
- Exposure Period: Incubate the plate for the predetermined exposure period (e.g., 48 hours) in a 37°C, 5% CO₂ incubator.
- Viability Measurement (MTT Assay):
- After 48 hours, carefully aspirate the medium.
- Add 110 µL of fresh medium containing 10% (v/v) MTT stock solution (5 mg/mL).
- Incubate for 2-4 hours at 37°C.
- Carefully remove the MTT-containing medium without disturbing the formed formazan crystals.
- Add 150 µL of lysis buffer (10% SDS in 0.01M HCl) to solubilize the crystals.
- Place the plate on an orbital shaker for 15 minutes and then read the absorbance at 570 nm on a microplate reader.
- Data Analysis:
- Normalize the absorbance values: % Viability = (Abssample - Absblank) / (Absvehiclecontrol - Abs_blank) × 100.
- Fit the normalized data to a four-parameter logistic (4PL) model using software like GraphPad Prism to calculate the IC₅₀ value.
Experimental Workflow and Pathway Visualization
FAQ: What is the fundamental difference between a cytostatic and a cytotoxic effect?
A cytostatic effect refers to the halt or slowing of cell growth and proliferation without directly killing the cell [66]. The cell remains alive but ceases to divide. In contrast, a cytotoxic effect leads directly to cell death [66] [20]. This distinction is critical in drug discovery because a decrease in cell population observed in an assay can result from either process, and they involve different underlying molecular mechanisms.
FAQ: Why can't I rely on a single assay like MTT/MTS to distinguish these effects?
Single metabolic assays like MTT or MTS measure the activity of cellular enzymes (e.g., NAD(P)H-dependent oxidoreductases) which reflect cell metabolism and the number of metabolically active cells [20]. A reduction in signal can be caused by either a decrease in cell metabolism (which can occur in proliferation arrest or cytostasis) or by actual cell death (cytotoxicity) [20]. Without additional context, the assay cannot differentiate between these two fundamentally different outcomes. Relying solely on it can lead to misinterpretation of a drug's mechanism of action.
FAQ: What is a foundational assay combination to start with?
A robust foundational combination includes a metabolic/proliferation assay and a direct viability/death assay.
- Metabolic/Proliferation Assay: MTS, MTT, or similar tetrazolium-based assays. These measure metabolic activity as a proxy for cell health and number.
- Viability/Death Assay: A LIVE/DEAD assay, such as one utilizing calcein-AM (for esterase activity in live cells) and ethidium homodimer-1 (for DNA in dead cells), or an Annexin V/PI assay to detect apoptosis [20].
Interpreting the results from both assays in tandem provides a clearer picture. For instance, a strong decrease in the MTS signal with a corresponding strong increase in the dead cell population indicates a cytotoxic effect. A moderate decrease in MTS signal with no increase in cell death suggests a cytostatic effect.
FAQ: My assays are giving conflicting results. What could be wrong?
Conflicting results are a key reason why multiple assays are essential. A study treating SW620 cells with cisplatin demonstrated this: the MTS assay showed a significant viability drop, and the LIVE/DEAD assay confirmed cell death. However, when apoptosis was inhibited, the LIVE/DEAD assay showed no cell death, but the MTS signal did not recover fully, revealing an underlying cytostatic component that was masked by the dominant cytotoxic effect [20]. This shows that a cytostatic effect can be obscured by concurrent cell death. If your results conflict, consider:
- The specific mechanism of your compound: Does it primarily arrest the cell cycle or induce a death pathway?
- The time point of your assay: A cytostatic effect may precede a cytotoxic one.
- Assay limitations: Ensure you understand what each assay is actually measuring.
FAQ: How can I confirm the specific type of cell death occurring?
To confirm specific cell death modalities like apoptosis, necroptosis, or ferroptosis, you must move beyond general viability assays to mechanistic biochemical assays.
- Western Blotting: Detect key biomarkers such as cleaved caspase-3 and cleaved PARP for apoptosis, phosphorylated RIPK1 for necroptosis, or lipid peroxidation for ferroptosis [20].
- Selective Pharmacological Inhibitors: Use inhibitors targeting specific death pathways (e.g., Q-VD-Oph for apoptosis, Necrostatin-1 for necroptosis, Ferrostatin-1 for ferroptosis) and observe if they rescue cell death in your assay [20].
Table 1: Key Biomarkers for Cell Death Modalities
| Cell Death Modality | Key Biomarkers | Selective Inhibitors |
|---|---|---|
| Apoptosis | Cleaved Caspase-3, Cleaved PARP [20] | Q-VD-Oph [20] |
| Necroptosis | Phosphorylated RIPK1 [20] | Necrostatin-1 [20] |
| Autophagy | SQSTM1/p62 degradation, MAP1LC3B-I to MAP1LC3B-II lipidation [20] | Chloroquine [20] |
| Ferroptosis | Lipid peroxidation [67] | Ferrostatin-1 [20] |
FAQ: What are the best practices for assay workflow and data interpretation?
A logical, multi-step workflow is crucial for accurate distinction.
- Begin with a metabolic assay (e.g., MTS) to identify a reduction in cell number/metabolism.
- Follow with a viability stain (e.g., LIVE/DEAD) to quantify the proportion of dead cells.
- If cytotoxicity is confirmed, use Western blotting and selective inhibitors to pinpoint the exact death pathway.
- For cytostatic effects, use complementary methods like cell cycle analysis (e.g., PI staining and flow cytometry) or direct cell counting to confirm proliferation arrest.
The following workflow diagram outlines this multi-assay strategy:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Cytostatic/Cytotoxic Effect Analysis
| Reagent / Assay Kit | Primary Function | Key Insight for Use |
|---|---|---|
| MTT/MTS/XTT Assays | Measures metabolic activity of cells via NAD(P)H-dependent oxidoreductases [20]. | A signal reduction indicates loss of cell number or metabolism but cannot distinguish between cytostasis and cytotoxicity [20]. |
| LIVE/DEAD Viability/Cytotoxicity Kits | Simultaneously labels live cells (e.g., calcein-AM) and dead cells (e.g., EthD-1) [20]. | Directly quantifies the proportion of dead cells in a population, providing a clear measure of cytotoxicity [20]. |
| Annexin V / Propidium Iodide (PI) | Distinguishes early apoptotic (Annexin V+/PI-), late apoptotic/necrotic (Annexin V+/PI+), and live cells (Annexin V-/PI-) [20]. | Essential for identifying apoptotic mechanisms. Flow cytometry analysis is required. |
| Selective Pathway Inhibitors | Pharmacologically inhibits specific cell death pathways (e.g., Q-VD-Oph for apoptosis) [20]. | Used to confirm the contribution of a specific death pathway to the overall cytotoxic effect observed. |
| Antibodies for Cell Death Biomarkers | Detects key proteins (e.g., Cleaved Caspase-3, p-RIPK1) via Western Blot [20]. | Provides biochemical confirmation of the activation of specific cell death machinery. |
FAQ: How do cytostatic and cytotoxic drugs differ in their impact on cancer progression?
The differential impact is rooted in their effect on tumor cell population dynamics. A mathematical model comparing treatments with equal net growth reduction showed that cytotoxic therapy (increasing cell death rate) and cytostatic therapy (decreasing cell birth rate) can have substantially different outcomes on the evolution of a tumor [68]. These treatments can differentially influence the rate at which driver mutations are acquired or metastases are seeded, which are stochastic processes tied to cell division and population size [68]. Therefore, the choice between a cytostatic or cytotoxic agent is not just about shrinking a tumor; it can also affect the long-term evolutionary trajectory of the disease and the emergence of resistance.
The diagram below illustrates how cytostatic and cytotoxic compounds influence key cellular processes and fate:
Addressing False Positives and False Negatives in Common Assay Formats
FAQs: Understanding and Troubleshooting Assay Errors
Q1: What are false positives and false negatives in the context of compound toxicity assays?
A false positive occurs when an assay incorrectly indicates a toxic effect for a safe compound (a "false alarm") [69] [70]. A false negative is when an assay fails to detect the genuine toxic effect of a compound, meaning a harmful substance is wrongly cleared [69] [70]. In cell health assessment, this could mean a toxic compound mistakenly passes through the screening process.
Q2: What are the most common causes of false positives in cell-based viability assays?
Common causes include [69] [71]:
- Compound Interference: The test compound itself is fluorescent or absorbs light at wavelengths used in the assay, interfering with the detection signal.
- Impurities in Samples: Contaminants or closely related compounds in complex biological samples can trigger a positive signal.
- Inappropriate Method Parameters: Using an assay method whose detection limits are not optimized for the expected concentration range of your compounds.
- Environmental Variations: Fluctuations in factors like temperature or CO2 levels in incubators can affect cell health and assay readouts.
Q3: Our high-content screening for cytotoxicity generates many false negatives. What should we investigate?
You should focus on [69] [71]:
- Assay Sensitivity: Verify that your assay's Limit of Detection (LOD) is sufficiently low to detect subtle toxic effects.
- Sample Preparation: Inefficient cell lysis or compound solubilization can prevent the assay from detecting the toxicant.
- Validation Logic: Review the data analysis scripts or algorithms to ensure they are correctly calibrated to identify all relevant toxic phenotypes.
- Cell Model Relevance: Confirm that the cell line or model used is biologically relevant and expresses the target pathways you are investigating.
Q4: How can we balance the trade-off between reducing false positives and minimizing false negatives?
There is an inherent trade-off; reducing one often increases the other [69] [70]. The optimal balance depends on the consequences of each error type for your research goals. For toxicity filtering in drug development, a false negative (missing a toxic compound) is typically considered more dangerous than a false positive (unnecessarily flagging a safe compound) [69]. You can adjust this balance by concentrating your sample to reduce false negatives or diluting it to reduce false positives [69].
Q5: What is the most effective strategy to significantly reduce both types of errors?
The most effective single strategy is to improve and optimize your assay method [69]. Furthermore, using a second, orthogonal analytical method to confirm results can dramatically increase overall accuracy [69]. For instance, if your primary screen is a fluorescence-based viability assay, a luminescence-based or impedance-based assay could serve as a powerful confirmatory tool.
Table 1: Characterizing Assay Error Outcomes
| Outcome | Definition | Consequence in Toxicity Filtering |
|---|---|---|
| True Positive | Correctly identifying a toxic compound. | Correctly failing a harmful compound. |
| False Positive (Type I Error) | Incorrectly flagging a safe compound as toxic [69] [70]. | Wasting resources on further investigation of a safe compound. |
| True Negative | Correctly identifying a safe compound. | Correctly advancing a safe compound. |
| False Negative (Type II Error) | Failing to detect a truly toxic compound [69] [70]. | Allowing a harmful compound to advance, posing a safety risk. |
Table 2: Key Reagent Solutions for Cell Health Assays
| Research Reagent | Function in Assay |
|---|---|
| MTT/XTT Reagents | Measures cellular metabolic activity as a marker of viability via mitochondrial reductase enzymes. |
| Caspase-Glo Assay | Detects caspase enzyme activity, a key marker of apoptosis. |
| ATP-Lite Assay | Quantifies cellular ATP levels, a direct indicator of metabolically active cells. |
| Hoechst 33342 | A cell-permeable DNA stain used to count total nuclei and assess cell number/viability. |
| Propidium Iodide (PI) | A DNA stain that is impermeant to live cells, identifying dead cells with compromised membranes. |
| HCS CellMask Stains | General stains for cytoplasm and plasma membrane used to segment cells and assess morphology in high-content imaging. |
Experimental Protocol 1: Method for Determining Limit of Detection (LOD) and Limit of Quantification (LOQ)
Purpose: To empirically establish the lowest concentration of an analyte that can be reliably detected and quantified by your assay, which is critical for avoiding false negatives at low concentrations [69].
Procedure:
- Prepare Standards: Serially dilute a known toxic compound with a defined EC50 to create a standard curve covering a broad concentration range, including levels expected to be near the detection limit.
- Run Assay: Perform your cell health assay (e.g., ATP measurement) in replicate for each concentration point on the standard curve, including multiple replicates of your blank (vehicle control).
- Calculate LOD: LOD is typically determined as the mean signal of the blank plus three times the standard deviation of the blank.
- Calculate LOQ: LOQ is typically determined as the mean signal of the blank plus ten times the standard deviation of the blank. Concentrations below the LOQ are highly susceptible to inaccuracies [69].
Experimental Protocol 2: Orthogonal Confirmation Assay Workflow
Purpose: To validate hits from a primary screen and drastically reduce both false positives and false negatives [69].
Procedure:
- Primary Screening: Conduct your initial toxicity screen (e.g., a fluorescence-based viability assay) on your compound library.
- Hit Identification: Identify all compounds that register as positive (toxic) in the primary screen.
- Orthogonal Assay: Subject these hit compounds to a second, independent assay that measures a different physiological aspect of toxicity (e.g., if the primary was metabolic activity, use a high-content imaging assay for nuclear fragmentation).
- Result Analysis:
- True Positive: Compound is toxic in both primary and orthogonal assays.
- False Positive: Compound shows toxicity only in the primary assay.
- Further Investigation: Discrepancies require additional analysis to determine the true biological effect.
Experimental Workflow and Pathway Diagrams
Decision Workflow for Orthogonal Assay Confirmation
Assay Outcome Decision Matrix
In compound toxicity filtering, relying on a single endpoint measurement is like judging a movie by one frame. Traditional endpoint assays, which provide a snapshot of cell health at a single time point, can obscure the dynamic reality of how a population of cells dies. Kinetic cell death analysis—the time-course monitoring of cell populations after exposure to a compound—reveals critical information that is invisible to endpoint methods. This includes the time of death onset, the maximum rate of cell death, and the heterogeneity of cellular responses within a population [72] [73].
Integrating kinetic analysis into your research provides a more powerful and predictive dataset for safety assessments. It can help you:
- Distinguish between compounds with similar final toxicity but different mechanisms of action.
- Identify rapid-onset lethal phenotypes that might be missed in fixed-time assays.
- Optimize dosing schedules in later-stage studies by understanding the temporal dynamics of compound toxicity.
- Reduce costly late-stage failures in drug development by building a more robust early toxicity profile [72] [74].
Kinetic Assays vs. Endpoint Assays: A Quantitative Comparison
The table below summarizes the core differences between these two approaches, highlighting why kinetic monitoring provides a superior data structure for decision-making.
Table 1: Key Differences Between Kinetic and Endpoint Assays
| Feature | Kinetic (Time-Course) Assays | Traditional Endpoint Assays |
|---|---|---|
| Data Output | Continuous, movie-like data from a single experiment [73] | Single, snapshot data point from one experiment [73] |
| Key Parameters | Death Onset (DO), Max Death Rate (DR), and cell death trajectory over time [72] | Overall lethality at one time (e.g., % viability at 48 h) [72] |
| Information on Heterogeneity | Reveals cell-to-cell variation in death timing [72] | Obscures population heterogeneity |
| Resource Efficiency | Saves time and resources by eliminating the need for multiple parallel time-point experiments [73] | Requires multiple experiments and plates to approximate a time course |
| Mechanistic Insight | High; can infer mechanism from death kinetics (e.g., rapid vs. slow onset) [72] | Low; provides little insight into the dynamics of the death process |
The Scientist's Toolkit: Essential Reagents & Instruments for Kinetic Analysis
Building a robust kinetic assay requires the right combination of reagents, instruments, and detection strategies.
Table 2: Key Research Reagent Solutions for Kinetic Cell Death Analysis
| Item | Function/Principle | Example Assays/Notes |
|---|---|---|
| Nuclear-Localized Fluorescent Protein (e.g., Nuc::mKate2) | Labels live cells; allows tracking of nuclei and quantification of live cell count over time [72] | Used in the STACK method; provides a stable marker for proliferating cells [72] |
| Membrane-Impermeant DNA Dye (e.g., Sytox Green, Propidium Iodide) | Distinguishes dead cells; enters only upon loss of membrane integrity, a hallmark of cell death [72] | Sytox Green is used in live-cell imaging; Propidium Iodide is common in flow cytometry and can be used in endpoint assays [72] [75] |
| Annexin V Conjugates | Binds to phosphatidylserine (PS), which is externalized in early apoptosis [75] | Often used with a viability dye like PI to distinguish early apoptotic (Annexin V+/PI-) from late apoptotic/necrotic (Annexin V+/PI+) cells [75] |
| Caspase Activity Probes (e.g., FLICA) | Fluorochrome-labeled inhibitors that bind to active caspases, marking cells undergoing apoptosis [76] | Allows for multiplexing with other dyes like PI to stage apoptosis [76] |
| Tetramethylrhodamine Methyl Ester (TMRM) | A fluorescent dye that accumulates in active mitochondria; loss of signal indicates loss of mitochondrial membrane potential (Δψm), an early apoptotic event [76] | A sensitive marker for early apoptosis; useful for multiparameter assays [76] |
| RealTime-Glo MT Cell Viability Assay | A bioluminescent method for monitoring viable cell number in real time without cell lysis [73] | Ideal for high-throughput screening; can be multiplexed with cytotoxicity assays [73] |
- Live-Cell Imaging Systems (e.g., Incucyte): Automated, high-throughput microscopes housed inside tissue culture incubators. They are the workhorse for kinetic imaging, allowing you to track the same population of cells over hours or days using phase contrast and fluorescent channels [72] [77].
- Confocal Microscopy: Provides higher-resolution images by eliminating out-of-focus light. Essential for 3D models like spheroids or for precise intracellular localization studies [77].
- Flow Cytometers: While typically used for endpoint analysis, they can be powerful for "snapshot" kinetic studies by analyzing multiple time-point samples. They excel in multiparameter analysis at the single-cell level [76].
Core Methodologies & Experimental Protocols
The STACK Method: Scalable Time-lapse Analysis of Cell Death Kinetics
The STACK method is a powerful framework specifically designed for quantifying population cell death kinetics in large-scale compound screening [72].
Workflow Diagram:
Key Experimental Parameters from the Original Study:
- Cell Seeding: Seed cells to ensure they are less than 50% confluent at the time of compound addition to avoid density-induced artifacts [72].
- Imaging: Image plates every 2 hours for up to 72 hours, starting immediately after compound addition [72].
- Data Modeling: Fit the resulting Lethal Fraction (LF) over time to a "lag exponential death" (LED) model to extract two critical parameters:
- Death Onset (DO): The time lag between compound addition and the onset of cell death in the population.
- Death Rate (DR): The maximal rate of cell death within the population [72].
Multiplexed Kinetic Viability/Cytotoxicity Assay
This protocol uses a combination of a live-cell viability assay and a cytotoxicity assay, added at the beginning of the experiment, to simultaneously monitor both live and dead cell counts in real time [73].
Protocol Steps:
- Plate cells in a multi-well plate and allow them to adhere.
- Add compounds at the desired concentrations.
- Add assay reagents directly to the culture medium. This includes:
- RealTime-Glo MT Cell Viability Assay Reagent: A bioluminescent measure of metabolically active, live cells.
- CellTox Green Cytotoxicity Assay Reagent: A fluorescent dye that binds to DNA in dead cells with compromised membranes.
- Place the plate in a compatible reader (e.g., a luminometer-equipped incubator or live-cell imager).
- Take repeated measurements from the same plate over the desired time course (e.g., every 2-4 hours for 72 hours).
- Analyze the data by plotting the normalized viability and cytotoxicity signals over time to visualize the dynamic relationship between cell death and loss of viability [73].
Signaling Pathways in Programmed Cell Death
Understanding the major cell death pathways is crucial for interpreting kinetic data, as different mechanisms can manifest with distinct kinetic profiles.
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Our kinetic data is noisy and inconsistent between replicates. What could be the cause?
- A: This is often a cell culture issue. Ensure consistent cell seeding density and passage number. High cell density can dramatically alter sensitivity to lethal compounds. Also, verify that your incubator's temperature, humidity, and CO₂ levels are stable, as fluctuations can affect cell health and compound activity [72].
Q2: Why should I use kinetic assays instead of trusted endpoint methods like MTT or LDH?
- A: Endpoint assays like MTT measure metabolic activity, which can be conflated with cytostatic (growth-arresting) effects, not just cell death. Kinetic assays using direct live/dead markers (like Nuc::mKate2/Sytox Green) specifically count live and dead cells, providing a clearer picture of the death process itself. Furthermore, kinetic assays capture the dynamic progression of death, revealing critical parameters like Death Onset that a single time point cannot [72] [73].
Q3: How can I distinguish between apoptosis and necrosis in a live-cell kinetic assay?
- A: Use multiplexing. Combine a general dead cell dye (like Sytox Green) with early-stage apoptotic markers:
- For Apoptosis: Use a FLICA (Caspase activity) probe or an Annexin V conjugate. Apoptotic cells will often be Caspase+ or Annexin V+ before they become Sytox Green+.
- For Necrosis: Primary necrotic cells will become Sytox Green+ rapidly after insult without prior Caspase or Annexin V activation. However, note that late-stage apoptotic cells also lose membrane integrity (secondary necrosis), so timing and context are key [78] [75] [76].
Q4: We see a drop in the Sytox Green signal after it peaks in our time-lapse data. Is this technical failure?
- A: Not necessarily. This is a known phenomenon, most likely due to the loss of Sytox Green fluorescence from long-dead cells as they disintegrate. The STACK methodology accounts for this by using an integrated metric (Lethal Fraction) and modeling the kinetics, rather than relying solely on the raw dead cell count at a single time point [72].
Q5: What are the advantages of bioluminescence over fluorescence for kinetic assays?
- A: Bioluminescence generally has a much lower background signal because it doesn't require excitation light, which can cause autofluorescence. This results in a higher signal-to-background ratio, improving assay sensitivity and often enabling miniaturization to 384- or 1,536-well formats for high-throughput screening [73].
Selecting the Right Assay for Your Specific Cell Type and Compound Class
Within the framework of cell health assessment for compound toxicity filtering, selecting the appropriate assay is a critical step that can determine the success or failure of your research. This guide addresses common challenges and provides actionable solutions to ensure your cytotoxicity screening is robust, reliable, and relevant.
FAQs and Troubleshooting Guides
How do I choose the right cell line for my cytotoxicity assay?
Challenge: A researcher is obtaining inconsistent cytotoxicity results for a new kinase inhibitor library across different labs.
Solution: The choice of cell line must balance experimental amenability with biological relevance [79].
- Fibroblast lines (e.g., HEK293, Cos cells): Easy to culture and transfer, making them an amenable experimental system, but they may lack relevance for your specific research question [79].
- Cancer lines (e.g., HepG2, PC-3, MCF-7): Often more relevant for drug discovery studies and generally easy to use. However, they can contain mutations that affect experimental outcomes. For example, the MCF-7 cancer cell line lacks functional caspase-3, which would lead to an underestimation of apoptosis in assays using DEVD substrates [79].
- Primary cells (e.g., HUVECs, hepatocytes): Provide the most accurate picture of a typical in vivo situation but can be difficult to grow and transfect. Primary cells also have a higher spontaneous rate of death, leading to a higher background in cytotoxicity assays like LDH release [79].
Key Consideration: Always consult the literature for recommended protocols and conduct preliminary dose-response and time-course experiments to determine optimal conditions for your specific cell type and compound [79].
Why is the timing of my assay readout critical for accurate mechanism interpretation?
Challenge: A compound appears to cause primary necrosis in a 48-hour endpoint assay, contradicting literature suggesting it is a pro-apoptotic agent.
Solution: The mechanism of cell death can be misinterpreted if assays are performed at a single, ill-timed endpoint. The kinetics of biomarker appearance and decay vary significantly between compounds [80].
- Staurosporine (apoptosis inducer): At 6 hours of exposure, a large increase in caspase-3/7 activity is evident. By 23 hours, this apoptotic signal is much lower due to progression to secondary necrosis. An assay only at 23 hours would miss the apoptotic mechanism [80].
- Colchicine (microtubule poison): Its peak apoptotic signal (caspase-3/7 activation) may occur much later, around 24 hours, and decrease at later time points as cells progress to secondary necrosis [80].
Recommendation: Perform multi-parameter, time-course experiments rather than single-endpoint assays. Monitor viability, cytotoxicity, and apoptosis from early (e.g., 3-6 hours) to late (e.g., 48-72 hours) time points to capture the dynamic nature of cell death and avoid misclassification [80].
How does compound dosage influence the observed cytotoxic effect and its mechanism?
Challenge: A development candidate shows a clean cytotoxicity profile up to 10 µM, but a repeat at 100 µM suggests severe toxicity, jeopardizing the project.
Solution: Compounds can affect cells in different ways at different concentrations. Testing a wide concentration range is essential to avoid misinterpreting a compound's biological impact [80].
- Narrow Window (e.g., Terfenadine): At 10 µM, it may show a clear apoptotic response (increased caspase activity). At 100 µM, it may cause rapid primary necrosis (high cytotoxicity, low apoptosis). Testing only the 100 µM concentration would lead to an incorrect conclusion about its mechanism [80].
- Broad Window (e.g., Colchicine): Effects may be observable over a large concentration range (e.g., 0.1–100 µM) [80].
- High Concentration Only (e.g., Aflatoxin): Effects may only be seen at high concentrations (e.g., 100 µM), especially if it is a pro-toxin that requires metabolic activation [80].
Best Practice: Serially dilute compounds (e.g., tenfold from 100 µM to 0.01 µM) to establish a full concentration-response profile. This helps identify the relevant cytotoxic concentration and the appropriate therapeutic window [80].
What are the key advantages of multiplexed assays over single-endpoint assays?
Challenge: A team is using separate plates for viability and apoptosis assays, leading to high variability and inconclusive results on the mode of action.
Solution: Multiplexing assays to gather more than one set of data from a single sample well provides several key advantages [80].
- More Data per Well: Provides complementary information on cellular response and mechanism of cell death (e.g., simultaneously measuring viability, cytotoxicity, and apoptosis) [80].
- Improved Consistency: Data is generated from the same population of cells, reducing well-to-well variability compared to running parallel assays on different plates [80].
- Informed Decision-Making: Technologies like the ApoTox-Glo Triplex Assay allow for the simultaneous measurement of viability (via a live-cell protease), cytotoxicity (via a dead-cell protease), and apoptosis (via caspase-3/7 activation) in the same well, providing a comprehensive picture of cell health [80].
My compound interferes with a colorimetric assay. What alternative methods can I use?
Challenge: A lead compound contains a chemical group that reduces a tetrazolium dye (MTT) in a cell-free system, generating a false positive signal.
Solution: Assay interference is a common issue. Employing orthogonal assays (different detection principles) can confirm true biological effects [4].
Alternative Viability/Cytotoxicity Assays:
- ATP-based Luminescence Assays: Measure ATP levels using luciferase, a highly sensitive and rapid "glow-type" method that is less prone to chemical interference [80] [4].
- Protease Activity Viability Markers: Use cell-permeant, fluorogenic substrates that are cleaved by live-cell proteases [80].
- Resazurin Reduction Assays: Measure the metabolic reduction of resazurin (blue, non-fluorescent) to resorufin (pink, fluorescent) [4].
- Cytotoxicity Marker Assays: Measure the activity of released enzymes like Lactate Dehydrogenase (LDH) or dead-cell proteases using cell-impermeant substrates [80] [7].
Advanced Profiling Approach:
- Image-based Profiling (e.g., Cell Painting): This high-content assay uses fluorescent dyes to label multiple cellular components and can detect subtle, morphology-based bioactivity at lower concentrations than standard cytotoxicity assays, providing rich mechanistic information [7].
Essential Experimental Protocols
Protocol 1: Multiplexed Viability, Cytotoxicity, and Apoptosis Assay (Time-Course)
This protocol is adapted from the methodology used to profile compound effects over time, allowing for the dynamic tracking of cell health biomarkers [80].
Workflow Overview:
Detailed Methodology:
- Cell Seeding and Treatment: Plate cells in a 96-well or 384-well plate at an optimized density. After cell attachment, treat wells with serially diluted compounds. Include negative control (vehicle, e.g., DMSO) and positive control (e.g., 10 µM Staurosporine for apoptosis) wells [80] [79].
- Time-Course Incubation: Incubate the plate for a predetermined time course (e.g., 3, 6, 23, 31, 47, 55, and 72 hours). Using multiple plates for destructive readouts at each time point is recommended [80].
- Viability and Cytotoxicity Measurement: Simultaneously add the fluorescent reagents for the live-cell protease (viability) and dead-cell protease (cytotoxicity) markers. Incubate for the time recommended by the manufacturer (e.g., 30-60 minutes). Simultaneously measure the two fluorescence signals using a plate reader with appropriate filter sets [80].
- Apoptosis Measurement: Directly add a single reagent for caspase-3/7 activity (e.g., Caspase-Glo 3/7 Reagent) to the same wells. Mix and incubate to allow for cell lysis and the generation of a "glow-type" luminescent signal. Measure luminescence, which is proportional to caspase-3/7 activity [80].
Protocol 2: MTT Cell Viability Assay
The MTT assay is a widely used colorimetric method for measuring metabolic activity as a marker of cell viability [4].
Workflow Overview:
Detailed Methodology:
- Reagent Preparation: Dissolve MTT in PBS to a concentration of 5 mg/mL and filter-sterilize. Prepare a solubilization solution (e.g., 40% DMF, 16% SDS in 2% acetic acid, pH 4.7) [4].
- Cell Treatment: After treating cells in a microplate, add the MTT solution to each well to a final concentration of 0.2-0.5 mg/mL.
- Incubation: Incubate the plate for 1-4 hours at 37°C. Metabolically active cells will convert the yellow MTT to purple formazan crystals.
- Solubilization: Carefully remove the medium and add the solubilization solution to dissolve the formazan crystals.
- Absorbance Measurement: Read the absorbance at 570 nm using a microplate reader. The amount of formazan produced is proportional to the number of viable, metabolically active cells.
Troubleshooting Note: MTT is toxic to cells, making this an endpoint assay. Be aware that reducing agents in compounds or culture medium can cause non-enzymatic reduction of MTT, leading to false positives. Always include control wells without cells to test for compound interference [4].
Data Presentation: Assay Comparison
Table 1: Comparison of Common Cell Viability and Cytotoxicity Assays
| Assay Type | Detection Method | Target / Principle | Key Advantages | Key Limitations |
|---|---|---|---|---|
| MTT [4] | Colorimetric (Absorbance) | Metabolic reduction of tetrazolium salt | Inexpensive; widely used & cited. | Endpoint only; formazan insolubility; compound interference possible. |
| ATP Content [80] [4] | Bioluminescence | Cellular ATP levels via luciferase reaction | Highly sensitive; rapid "glow" signal; simple protocol. | Luciferase inhibitors can cause interference. |
| Resazurin Reduction [4] | Fluorescence | Metabolic reduction of resazurin to resorufin | Homogeneous; non-destructive (can monitor over time). | Slower signal development; can be less sensitive. |
| Protease Activity [80] | Fluorescence | Cleavage of cell-permeant substrate by live-cell proteases | Can be multiplexed with cytotoxicity markers. | Signal depends on protease activity, which can vary. |
| LDH Release [7] | Colorimetric or Fluorescence | Release of lactate dehydrogenase from damaged membranes | Direct marker of membrane integrity (necrosis). | Can have high background with primary cells; requires collection of supernatant. |
| Caspase-3/7 Activity [80] | Bioluminescence | Cleavage of DEVD-luciferin substrate by executioner caspases | Specific marker for apoptosis; highly sensitive. | Signal is transient (peaks and decays). |
| Cell Painting [7] | High-Content Imaging (Fluorescence) | Morphological profiling with 6-8 fluorescent dyes | Rich, multi-parametric data on mode-of-action; detects bioactivity at low concentrations. | High data load; requires sophisticated image analysis. |
Table 2: Point-of-Departure (POD) Comparison for Bioactivity Detection
| Assay Method | Percentage of Compounds Showing Activity | Key Finding |
|---|---|---|
| Metabolic Activity (MT) [7] | 40% (430 of 1085 compounds) | Most active assay; detected decrease in activity for most cytotoxic compounds. |
| Cell Count (from imaging) [7] | 20% (221 of 1085 compounds) | Direct measure of cell number loss. |
| Membrane Damage (LDH) [7] | 13% (144 of 1085 compounds) | Specific measure of necrotic cell death. |
| Image-Based Morphology (Cell Painting) [7] | Detects bioactivity at lower concentrations than cytotoxicity assays. | Can reveal bioactivity before overt cytotoxicity is observed. |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for Cell Health Assessment
| Reagent / Kit Name | Function / Application | Key Features |
|---|---|---|
| ApoTox-Glo Triplex Assay [80] | Multiplexed measurement of viability, cytotoxicity, and apoptosis in the same well. | "Add-mix-measure" format; combines fluorescence and luminescence readouts. |
| Caspase-Glo 3/7 Assay [80] | Bioluminescent measurement of caspase-3/7 activity. | Homogeneous, "glow-type" signal; high sensitivity. |
| CellTiter 96 MTT Assay [4] | Colorimetric measurement of cell viability via metabolic activity. | Well-established protocol; non-radioactive. |
| Realtime-Glo MT Assay [7] | Luminescent measurement of metabolic activity in real-time. | Allows for continuous monitoring of cell health over time. |
| Cell Painting Dye Set [7] | Stains multiple organelles for high-content, image-based profiling. | Provides rich morphological data for mode-of-action analysis. |
| LDH Cytotoxicity Assay Kits [7] [81] | Colorimetric or fluorescent measurement of lactate dehydrogenase release. | Direct indicator of plasma membrane damage. |
Validating Results and Leveraging Next-Generation Technologies
Benchmarking with Reference Cytotoxic and Nuisance Compounds
In cell health assessment and compound toxicity filtering research, nuisance compounds present a significant challenge. These are compounds that exhibit assay interference or undesirable mechanisms of bioactivity, which can lead to false positives or misinterpreted results in cellular assays [82]. A key distinction exists between artifacts (compounds that interfere with the assay readout technology) and compounds that genuinely modulate bioactivity but through undesirable mechanisms of action (MOAs) [82]. If not properly identified, these compounds can waste significant scientific resources and erode trust in research findings. For example, the prototypical nuisance compound curcumin has consumed over $150 million in NIH funding despite not being recommended as a probe or drug [82]. Understanding and benchmarking against these compounds is therefore crucial for robust toxicity filtering in drug development.
Understanding Nuisance Mechanisms & Cytotoxicity
Frequently Encountered Nuisance Compound Mechanisms
Nuisance compounds in cellular assays typically operate through a range of undesirable mechanisms that can broadly be categorized as causing cellular injury [82]. The table below summarizes the most common types and their impacts on cell health assessment.
Table 1: Common Nuisance Compound Mechanisms in Cellular Assays
| Mechanism Type | Specific Examples | Impact on Cellular Assays & Cell Health |
|---|---|---|
| Direct Cellular Injury | Genotoxins, Lysosomotropic agents, Membrane disruptors, Tubulin poisons [82] | Causes general cellular stress or death; phenotypes can be mistaken for specific bioactivity. |
| Technology Interference | Fluorescence interference/quenching, Luciferase inhibitors, AlphaScreen singlet oxygen (¹O₂) quenchers [82] | Directly interferes with detection technology, creating false signals. |
| Undesirable Chemistries | Nonspecific electrophiles, Promiscuous aggregates, Redox cyclers, Chelators [82] [83] | Modulates biological targets via non-druglike, covalent, or ionic interactions. |
| Cationic Amphiphilic Drugs (CADs) | Chlorpromazine, Amiodarone [82] | Accumulate in lysosomes, causing phospholipidosis and perturbing membrane dynamics. |
The Cytotoxicity Burst and Black Box Challenges
A critical concept in cytotoxicity assessment is the "cytotoxicity burst," identified by the NIH/EPA Tox21 program. This phenomenon occurs at relatively high compound concentrations when cellular activities result from the activation of multiple stress responses rather than a specific molecular target [82]. This complicates data interpretation, as the observed activity is non-specific.
Cellular assays often function as a "black box" where the precise mechanism behind a compound's readout is not immediately clear [82]. A common trap is performing a biochemical validation assay, observing a desired response, and incorrectly equating the original cellular readout to this specific activity. The converse is also problematic: low-quality compounds from biochemical screens can show apparent confirmatory cellular activity driven by cytotoxicity or loss-of-signal effects [82].
Diagram 1: Cellular Assay Black Box. This diagram visualizes how a single test compound can lead to different interpretation pathways in a cellular assay, resulting in genuine, nuisance, or artifactual readouts.
Technical Support & Troubleshooting Guide
This section addresses common experimental issues in the form of a Frequently Asked Questions (FAQ) guide for researchers.
FAQ 1: My high-throughput screen yielded many "hits," but I suspect non-specific cytotoxicity is a major confounder. How can I triage these results?
Answer: A cascade of follow-up assays is essential for effective triage [82]. Prioritize compounds based on potency and structure-activity relationships (SAR).
- Confirm Cytotoxicity: Use a orthogonal viability assay (e.g., MTT, CCK-8) to confirm cytotoxic effects and determine IC₅₀ values [84].
- Check for Undesirable Chemistries: Test for common nuisance behaviors:
- Aggregation: Use detergent (e.g., Triton X-100) addition; if activity is suppressed, colloidal aggregation may be the cause [82].
- Redox Activity: Measure cellular redox state changes or use enzymatic systems like glutathione to assess redox cycling potential.
- Electrophilicity: Probe for covalent binding using nucleophilic reagents like glutathione or run mass spectrometry-based assays.
- Assess Specificity: Evaluate the "cytotoxicity burst" by testing compounds across multiple cell lines with different metabolic states (e.g., glycolytic vs. oxidative phosphorylation) [82]. Compounds with selective, rather than universal, cytotoxicity are more promising.
- Inspect SAR: Look for meaningful SAR. A sharp "cliff" in potency with small structural changes or activity spread across structurally diverse compounds can indicate nuisance mechanisms.
FAQ 2: A known drug from a repurposing library shows activity in my cell health assay, but it's a Cationic Amphiphilic Drug (CAD). How do I determine if the activity is specific?
Answer: CADs frequently appear as bioactive in repurposing screens due to nonspecific cellular perturbations [82]. To investigate specificity:
- Determine Lysosomotropism: Use LysoTracker dyes to visualize and quantify compound accumulation in lysosomes.
- Check for Phospholipidosis: Assess for phospholipidosis, a hallmark of CADs, using fluorescent phospholipid probes or electron microscopy.
- Conduct Time-Course and Dose-Response Experiments: Compare the timing and concentration-dependence of the observed phenotype with known markers of lysosomal disruption or general membrane perturbation. Specific target engagement often occurs at lower concentrations and earlier time points than these nuisance effects.
- Use Comparative Analysis: Test a small panel of structurally distinct CADs. If all produce a similar phenotype, it strongly suggests a class-based nuisance effect rather than specific target modulation.
FAQ 3: My compound is cytotoxic in my primary cell-based assay, but I cannot detect any activity in the follow-up biochemical target assay. What are possible explanations?
Answer: This discrepancy is a classic sign of a nuisance compound [82].
- Cellular Injury Mechanism: The compound is likely causing cytotoxicity through a non-specific injury mechanism (see Table 1), such as membrane disruption or induction of a general stress response, which would not be detectable in a purified biochemical system [82].
- Assay Impermeability: The compound might not penetrate the cell membrane in the biochemical assay setup, whereas it could in the cellular assay.
- Off-Target Effects: The compound is bioactive in cells, but through an off-target, nuisance mechanism like tubulin poisoning or topoisomerase inhibition, which was not the focus of your biochemical assay.
- Metabolic Activation: The compound may be a pro-drug that requires metabolic activation within the cellular environment to become cytotoxic.
Reference Compound Database & Benchmarking
Benchmarking new compounds against known reference compounds with well-characterized mechanisms is a foundational practice for validating cell health assays and interpreting screening results.
Reference Cytotoxic Compounds
Table 2: Benchmark Cytotoxic Compounds for Assay Validation
| Compound Name | Primary Mechanism of Action (MOA) | Reported Potency (e.g., IC₅₀/ BMC) | Key Assay Readouts | Use in Benchmarking |
|---|---|---|---|---|
| Etoposide (ETP) | Topoisomerase II inhibitor; causes DNA double-strand breaks [85] | BMC values can be derived from micronucleus assay dose-response [85] | ↑ Micronucleus formation, ↓ Cell proliferation, G2/M cell cycle arrest [85] | Positive control for genotoxicity/DNA damage. |
| Methyl Methanesulfonate (MMS) | DNA-alkylating agent [85] | BMC values can be derived from micronucleus assay dose-response [85] | ↑ Micronucleus formation, cytotoxicity [85] | Positive control for clastogenic activity (chromosome breakage). |
| Ethyl Methanesulfonate (EMS) | DNA-alkylating agent (similar MoA to MMS) [85] | BMC values can be derived from micronucleus assay dose-response [85] | ↑ Micronucleus formation, cytotoxicity [85] | Used in mixture studies with MMS to model compounds with similar MoA [85]. |
Reference Nuisance Compounds
Table 3: Benchmark Nuisance Compounds for Assay Quality Control
| Compound Name | Nuisance Category | Specific Mechanism / Property | Observed Interference in Cellular Assays |
|---|---|---|---|
| Chlorpromazine | Cationic Amphiphilic Drug (CAD) [82] | Lysosomotropism, membrane permeability alteration [82] | Induces phospholipidosis; can produce positive signals in phenotypic screens unrelated to its primary target. |
| Curcumin | Pan-Assay Interference Compound (PAINS) / Reactive Compound [82] | Electrophilicity, redox activity, metal chelation [82] | Promiscuous activity across diverse assay types; consumes significant research resources as a false lead. |
| Remodelin | Nonspecific Electrophile [82] | Hydrazone-based promiscuous reactivity [82] | Originally published as a NAT10 inhibitor but later shown to not modulate intended target; phenocopies knockdown phenotypes via nonspecific stress. |
| Colloidal Aggregators | Assay Artifact [82] | Forms colloidal aggregates that denature proteins [82] | Inhibits enzyme activity non-specifically in cell-free assays; can perturb membrane targets like GPCRs in cellular assays. |
Essential Experimental Protocols
Protocol: In Vitro Micronucleus (MNvit) Test for Genotoxicity Assessment
The MNvit test is a well-established method for quantifying genotoxic stress, a key endpoint in cell health assessment [85].
Principle: The assay detects micronuclei (MN), which are small, extranuclear bodies formed from acentric chromosome fragments or whole chromosomes that lag behind during cell division. An increase in MN frequency is indicative of genotoxic damage.
Key Steps [85]:
- Cell Culture: Seed an appropriate cell line (e.g., TK6 human lymphoblastoid cells) at a density of ~75,000 cells/mL in multi-well plates.
- Compound Exposure: 24 hours after seeding, expose cells to a range of concentrations of the test compound, reference genotoxicant (e.g., MMS), and solvent (negative control) for a defined period (e.g., 24 hours).
- Cytokinesis Block: Add cytochalasin B (e.g., 3 µg/mL) to arrest cells during cytokinesis, resulting in binucleated cells. This allows for scoring of MN specifically in cells that have completed one division cycle.
- Cell Harvesting and Preparation: Treat cells with a hypotonic solution (e.g., 0.075 M KCl) to swell the cells, then fix them and spread onto microscope slides.
- Staining and Scoring: Stain slides with DNA-specific dyes (e.g., DAPI, Propidium Iodide). Score the frequency of micronuclei in binucleated cells manually via fluorescence microscopy or using an automated system (e.g., Metafer). A minimum of 10,000 cells per concentration is recommended for statistical power [85].
- Cytotoxicity Assessment: In parallel, calculate the Cytokinesis-Block Proliferation Index (CBPI) to monitor compound-induced cytotoxicity, ensuring that genotoxic effects are not simply a consequence of general cell death.
Data Analysis: Use BMC (Benchmark Concentration) modeling with tools like PROAST to calculate the concentration that induces a predefined increase in MN frequency (e.g., a 50% or 100% change over the background) [85]. This provides a quantitative measure of genotoxic potency.
Diagram 2: MNvit Test Workflow. This flowchart outlines the key steps in the In Vitro Micronucleus test, a standardized protocol for assessing the genotoxic potential of compounds.
Protocol: Benchmark Concentration (BMC) Approach for Mixture Assessment
This quantitative strategy is used to evaluate the combined effects of genotoxic compounds, which is highly relevant for understanding complex toxicity profiles [85].
Workflow [85]:
- Collect Individual Compound Data: Perform concentration-response experiments (e.g., MNvit test) for each compound in the potential mixture. Test a minimum of five concentrations to capture low, moderate, and high response levels. Conduct at least three independent replicates.
- Calculate BMCs: Use a computational tool (e.g., the PROAST web tool) to fit dose-response models and calculate BMC values for each compound at various Benchmark Response (BMR) levels (e.g., 0.5, 1, 1.5 corresponding to 50%, 100%, 150% increases over background).
- Compose Mixtures: Design binary (or more complex) mixtures based on the BMC ratios. For example, create a mixture containing compound A and B, each at a concentration equivalent to their BMC₁ (the concentration causing a 100% effect increase).
- Test Mixtures Experimentally: Test the designed mixtures in the biological assay (e.g., MNvit) using the same protocol as for the individual compounds.
- Compare Predictions to Data: Model the expected additive effect of the mixture using principles like Concentration Addition (CA). Compare the experimental results from step 4 to these model predictions to determine if the mixture effect is additive, synergistic, or antagonistic.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Resources for Cytotoxicity and Nuisance Compound Research
| Tool / Resource | Type | Primary Function / Utility | Example Sources / Names |
|---|---|---|---|
| Toxicity Databases | Data Repository | Provide curated data on compound toxicity for model training and validation. | TOXRIC, ICE, DSSTox, ChEMBL, PubChem [84]. |
| Cell Viability Assays | Biochemical Assay | Measure overall cellular health and compound cytotoxicity. | MTT assay, CCK-8 assay [84]. |
| Mechanistic Toxicity Assays | Cell-Based Assay | Probe specific toxicity pathways and mechanisms. | In Vitro Micronucleus (MNvit) test (for genotoxicity) [85]. |
| Phenotypic Profiling | High-Content Imaging | Capture complex morphological changes for mechanism hypothesis generation. | Cell Painting [74]. |
| In Silico Prediction Tools | Software / AI Model | Predict toxicity risks from chemical structure prior to synthesis or testing. | Trialblazer (toxicity risk predictor), Deep Neural Network models for cytotoxic substructures [86] [83]. |
| Advanced Cell Models | Biological Model System | Provide more physiologically relevant contexts for toxicity testing. | 3D spheroids, Organ-on-a-chip systems [74]. |
The Role of High-Content Screening and Cell Painting in Phenotypic Triage
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary advantage of using Cell Painting for hit triage in phenotypic screening?
Cell Painting provides an unbiased, multiparametric profiling tool that captures hundreds to thousands of morphological features at single-cell resolution. This allows for the characterization of compound mechanisms of action (MoA) and the early identification of undesirable, cytotoxic compounds based on their phenotypic profiles. Unlike target-based assays that measure a few predefined parameters, Cell Painting captures a comprehensive view of cell state, enabling the distinction between specific bioactive compounds and those causing nonspecific cellular injury [87] [88].
FAQ 2: How can Cell Painting help distinguish high-quality from low-quality compounds?
By comparing the morphological profiles of new hits to a reference set of prototypical cytotoxic and nuisance compounds, researchers can identify compounds with undesirable mechanisms. For instance, nonspecific electrophiles (NSEs) often produce a "gross injury" phenotypic cluster, while their less reactive analogs (NSE-IAs) and more selective targeted electrophiles (TEs) are often inactive or show distinct profiles. This allows for the triage of compounds with promiscuous, hard-to-optimize mechanisms early in the screening funnel [87].
FAQ 3: My Cell Painting stain intensity is too low for accurate segmentation. What should I do?
Low stain intensity can often be optimized by titrating the probes and adjusting incubation times. It is recommended to perform a time-course experiment to determine the optimal conditions. The table below outlines an example optimization strategy for a 12-well slide kit [89].
Table: Example Optimization Strategy for Cell Paint Staining Intensity
| Well Position | Incubation Time (Variant A) | Incubation Time (Variant B) |
|---|---|---|
| A | 2 minutes | 30 minutes |
| B | 5 minutes | 20 minutes |
| C | 10 minutes | 15 minutes |
| D | 15 minutes | 10 minutes |
| E | 20 minutes | 5 minutes |
| F | 30 minutes | 2 minutes |
After optimization, visually inspect the results to ensure clear cell boundaries and sufficient signal for both membrane and nuclear stains [89].
FAQ 4: What are some common phenotypic clusters associated with cellular injury?
Unsupervised analysis of cytotoxic compounds reveals distinct morphological clusters. For example, tubulin poisons and genotoxins often form their own distinct clusters, while a larger, more variable cluster is associated with "gross cellular injury." This cluster can include nonspecific electrophiles, proteasome inhibitors, and miscellaneous cytotoxins that do not fit a specific MoA [87].
Troubleshooting Guides
Issue 1: Differentiating Specific Bioactivity from Nuisance Compounds
Problem: A screening hit shows a strong phenotypic profile, but it is unclear if this is due to a specific, interesting mechanism or nonspecific cytotoxicity.
Solution:
- Utilize a Reference Set: Profile your hits alongside a defined set of reference cytotoxic and nuisance compounds (e.g., 218 prototypical compounds as described in the literature) [87].
- Concentration-Response Profiling: Test compounds in a quantitative High-Throughput Screening (qHTS) format across a range of concentrations (e.g., 0.6 to 20 μM). Nuisance compounds often show a strong correlation between increased CP activity score, decreased cell count, and a migration of their phenotypic profile towards the "gross injury" cluster at higher concentrations [87].
- Compare Feature Signatures: Analyze the morphological feature signatures of your hits. Compare them to the signatures of known nuisance compounds, such as nonspecific electrophiles. A high similarity, especially at lower concentrations, suggests an undesirable mechanism [87].
Issue 2: Low Cell Counts and Viability Confounding Morphological Analysis
Problem: Treatments causing significant cell death make it difficult to obtain robust morphological data from surviving cells.
Solution:
- Adjust Treatment Conditions: Reduce the compound concentration or shorten the treatment duration to find a window where morphological changes can be observed without complete cell loss [87].
- Incorporate Viability Metrics: Use the assay to simultaneously extract data on relative cell count. This serves as a critical quality control metric and is often inversely correlated with CP activity scores for cytotoxic compounds [87].
- Validate with Orthogonal Assays: Follow up with dedicated cell health assays (e.g., measuring apoptosis, mitochondrial integrity) to confirm and further characterize the cytotoxic effects suspected from the Cell Painting data [90].
Issue 3: Reproducibility and Generalizability of Phenotypic Profiles
Problem: Concerns about whether the cellular injury phenotypes detected are reproducible across experiments and applicable to other compound libraries.
Solution:
- Ensure Assay Robustness: Independent experiments have shown that CP phenotypes for cellular injury compounds are highly reproducible, with mean correlations of 0.87 ± 0.06 between replicates [87].
- Leverage Public Data: Analyze your data in the context of large public datasets, such as the NIH Molecular Libraries Initiative (MLI) data. This allows you to correlate your hits with established phenotypic clusters. One study found that 82% of compounds from a historical dataset that were highly correlated with the "gross injury" phenotype were confirmed as bioactive upon retesting [87].
- Standardize Workflows: Use established, detailed Cell Painting protocols to ensure consistency. The workflow below outlines a standard process from cell seeding to data analysis [88].
Diagram: Standard Cell Painting Workflow for Phenotypic Triage
Key Experimental Protocols
Detailed Protocol: Cell Painting Assay for Detecting Cellular Injury
This protocol is adapted from established methods for characterizing cytotoxic compounds [87] [88].
1. Cell Culture and Plating:
- Use U-2 OS cells (or another relevant cell line).
- Seed cells into 384-well μClear plates at a density of 2,000 cells per well in 40 μL of complete growth medium.
- Incubate plates at 37°C with 5% CO₂ for 24 hours.
2. Compound Treatment:
- Prepare a dilution series of test and reference compounds. A typical range is 0.6 μM to 20 μM, in a 1:3 dilution series.
- Replace the medium with a low-serum medium (e.g., containing 2% FBS) before adding compounds.
- Include DMSO vehicle controls and appropriate positive controls (e.g., known cytotoxins like staurosporine).
- Treat cells for 24 hours.
3. Staining with Cell Painting Dyes:
- Live-cell staining: Incubate with MitoTracker Deep Red (500 nM) for 30 minutes at 37°C to label mitochondria.
- Fixation: Fix cells with 3.2% paraformaldehyde (PFA) for 20 minutes.
- Permeabilization: Permeabilize cells with 0.1% Triton X-100 for 20 minutes at room temperature.
- Staining Solution: Prepare a cocktail in blocking solution (1X HBSS, 1% BSA) containing:
- Hoechst 33342 (5 μg/mL) for DNA/nuclei.
- Phalloidin (e.g., 5 μL/mL) for F-actin.
- Concanavalin A, Alexa Fluor conjugate (100 μg/mL) for endoplasmic reticulum.
- Wheat Germ Agglutinin (WGA), Alexa Fluor conjugate (1.5 μg/mL) for Golgi apparatus and plasma membrane.
- SYTO 14 (3 μM) for cytoplasmic RNA and nucleoli.
- Incubate with the staining solution for 30 minutes at room temperature protected from light.
- Wash cells three times with 1X HBSS.
4. Image Acquisition:
- Use a confocal high-content imaging system (e.g., ImageXpress Micro Confocal, Opera Phenix, or CellInsight CX7).
- Acquire images with a 20x objective.
- Collect Z-stacks (e.g., 3 images per site) and use best-focus projection.
- Acquire multiple fields of view per well to ensure adequate cell numbers for statistics.
5. Image and Data Analysis:
- Use image analysis software (e.g., IN Carta, HCS Studio, or Harmony) to segment cells and organelles.
- Extract hundreds of morphological features (e.g., intensity, texture, shape, spatial relationships) for each cell.
- Export single-cell data and perform data cleaning (e.g., remove wells with fewer than 50 cells).
- Use data analysis platforms (e.g., HC StratoMineR) for data transformation, scaling, and dimensionality reduction (Principal Component Analysis - PCA).
- Calculate a distance score (e.g., Mahalanobis distance) to quantify the phenotypic effect of each treatment.
- Perform hierarchical clustering to group compounds with similar phenotypic profiles.
Protocol: Triage Strategy for Electrophilic Compounds
This specific protocol helps distinguish nonspecific electrophiles (NSEs) from targeted electrophiles (TEs) and inactive analogs (NSE-IAs) [87].
- Profile Compound Sets: In the same Cell Painting experiment, profile your compounds of interest alongside a panel of known NSEs, NSE-IAs, and high-quality TEs.
- Concentration Analysis: Pay close attention to the concentration at which compounds induce a phenotype. High-quality TEs may only show a gross injury phenotype at concentrations far exceeding their target-specific EC₅₀, while NSEs will show this phenotype at lower, therapeutically relevant concentrations.
- Cluster Analysis: Analyze which phenotypic cluster the compounds occupy, particularly at higher tested concentrations (e.g., 20 μM). A high proportion of NSEs (e.g., 72%) will fall into the "gross injury" cluster, while most NSE-IAs (e.g., 93%) will remain inactive [87].
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table: Key Research Reagent Solutions for Cell Painting and Toxicity Triage
| Reagent / Solution Name | Function in the Assay | Example Targets / Use-Case |
|---|---|---|
| MitoTracker Deep Red | Live-cell stain for mitochondria. | Assesses mitochondrial mass, membrane potential, and network morphology. Changes indicate metabolic stress or toxicity [88]. |
| Phalloidin (Fluorescent conjugate) | Binds and stains filamentous actin (F-actin). | Visualizes cytoskeletal structure. Disruption is a common feature of many cytotoxins [88]. |
| Concanavalin A, Alexa Fluor conjugate | Binds to glycoproteins in the endoplasmic reticulum (ER). | Labels the ER; morphological changes can indicate cellular stress or altered protein synthesis [88]. |
| Wheat Germ Agglutinin (WGA), conjugate | Binds to sialic acid and N-acetylglucosamine on the plasma membrane and Golgi. | Outlines cell shape and Golgi apparatus integrity [88]. |
| Hoechst 33342 | Cell-permeable DNA stain. | Identifies and segments nuclei. Used to assess nuclear morphology and count cells [88]. |
| SYTO 14 Green Fluorescent Nucleic Acid Stain | Permeant stain for RNA. | Highlights nucleoli and cytoplasmic RNA, providing information on nucleolar shape and number [88]. |
| Reference Cytotoxin Panel | A set of well-characterized cytotoxic/nuisance compounds. | Serves as a positive control and a baseline for identifying undesirable MoAs (e.g., staurosporine, gliotoxin, paclitaxel) [87]. |
| Targeted & Nonspecific Electrophile Set | A curated set of electrophilic compounds. | Enables benchmarking of new hits against known reactive compounds to assess potential for off-target toxicity [87]. |
Data Interpretation Guide
The following diagram illustrates the logical process for triaging hits based on their phenotypic profiles in relation to cellular health.
Diagram: Hit Triage Logic for Cytotoxicity Assessment
Advancing Predictive Power with 3D Cell Models and Organoids
Frequently Asked Questions (FAQs)
FAQ 1: What are the key advantages of using organoids over traditional 2D cell lines for toxicity screening? Organoids are three-dimensional (3D) in vitro models that closely mimic the architecture and function of native organs, providing a more physiologically relevant system for toxicity testing. Unlike two-dimensional (2D) cell lines, which consist of a single cell type and lack complex tissue structure, organoids retain the 3D structure, cellular heterogeneity, and key functions of their source tissue. This allows them to more accurately predict human physiological and toxicological responses, reducing the high failure rates of drug candidates in later development stages due to unacceptable toxicity [91] [92] [93].
FAQ 2: How can I improve the success rate of establishing patient-derived organoid cultures? Successful establishment of patient-derived organoids (PDOs) depends on careful tissue processing and selection of culture conditions. For colorectal tissues, use a defined medium containing essential factors like EGF, Noggin, and R-spondin. To manage variability in sample processing, if a delay of 6-10 hours is expected, store tissue at 4°C in DMEM/F12 with antibiotics. For longer delays, cryopreservation is recommended, though note that a 20-30% variability in cell viability can occur between these two preservation methods. Efficiently generating organoids from diverse colorectal tissues requires this standardized approach [94].
FAQ 3: What are the common challenges in maintaining long-term organoid cultures, and how can they be addressed? Common challenges include inter-batch variability, loss of cellular heterogeneity during extended culture, and difficulties in mimicking the complete tumor microenvironment (TME), particularly the immune and vascular components. To address these, researchers are adopting a framework known as "Organoid Plus and Minus," which combines technological augmentation (Plus) with culture system refinement (Minus). This includes using defined, tunable biomaterials to replace conventional Matrigel, integrating microfluidic systems for better microenvironment control, and developing low-growth-factor media to preserve phenotypic stability [95] [96].
FAQ 4: Which technologies are best suited for quantifying toxicity in 3D organoid models? Automated high-content imaging systems are highly effective for quantifying compound toxicity in 3D organoids. These systems can acquire confocal Z-stack images and perform automated image analysis to measure key parameters such as the number of cells with intact cytoskeletons or mitochondria, total live cell area, and average organoid volume. This approach allows for robust, quantitative assessment of phenotypic changes in response to compound treatment in a high-throughput compatible format [93].
FAQ 5: Can organoid models fully replace animal testing in preclinical drug development? While organoids cannot yet fully replicate the systemic interactions of a whole organism, they are recognized as powerful tools that can reduce and refine animal testing. In a significant policy shift, the U.S. FDA has announced plans to phase out traditional animal testing in favor of advanced non-animal systems, like organoids and organ-on-a-chip, for drug safety evaluation. This positions organoids as a cornerstone for more human-relevant preclinical models, though they are currently complementary to, rather than a complete replacement for, animal models for studying complex whole-body responses [96] [97].
Troubleshooting Guides
Table 1: Common Organoid Culture Issues and Solutions
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low viability after thawing | Improper cryopreservation or thawing process | Use a ROCK inhibitor (Y-27632) in the recovery medium for the first 48-72 hours to inhibit apoptosis [98]. |
| Contamination | Non-sterile technique or contaminated reagents | Avoid routine use of antibiotics to mask low-level contamination; implement rigorous sterility testing of all reagents and medium components [98]. |
| Failed organoid formation | Incorrect extracellular matrix (ECM) or poor-quality tissue sample | Ensure ECM is properly thawed on ice and kept cold during handling. For tissue, optimize digestion time and use high-quality samples processed promptly or cryopreserved with validated methods [94] [98]. |
| High batch-to-batch variability | Undefined components in ECM (e.g., Matrigel) and growth factors | Where possible, transition to defined, synthetic hydrogels. Pre-test and qualify new lots of critical reagents like Matrigel and growth factor-conditioned media [96] [99]. |
| Loss of cellular heterogeneity over time | Selective overgrowth of a dominant cell subpopulation during extended culture | Limit the number of passages. Use chemically defined media with minimized growth factors to reduce selective pressure and maintain a more representative cell population [95] [96]. |
Table 2: Troubleshooting Toxicity Assay Readouts
| Assay Readout Issue | Potential Cause | Troubleshooting Action |
|---|---|---|
| High background signal in imaging | Inadequate washing or non-specific staining | Increase wash steps and optimize dye and antibody concentrations. Include controls without primary antibody or with vehicle-only treatment [93]. |
| Poor segmentation of organoids in image analysis | Organoids too dense or overlapping | Optimize seeding density to prevent overlap. Use confocal imaging and Z-stack projections to improve 3D object definition [93]. |
| Lack of dose-response in toxicity assay | Compound solubility issues or insufficient exposure time | Verify compound solubility in DMSO and culture medium. Extend treatment duration to capture delayed toxic effects [100] [93]. |
| High variability between technical replicates | Inconsistent organoid size or Matrigel dome formation | Standardize the process of organoid dissociation and seeding. Use automated dispensers for consistent dome formation in wells [98] [93]. |
Experimental Protocols
Protocol 1: Establishing a Mouse Intestinal Organoid Model for Compound Toxicity
This protocol outlines the steps for culturing mouse intestinal organoids and assessing compound toxicity using high-content imaging, adapted from a published methodology [93].
Materials & Reagents:
- Primary Mouse Intestinal Organoids (e.g., from StemCell Technologies)
- Matrigel (e.g., Corning)
- IntestiCult Organoid Growth Medium (Mouse)
- CellXpress.ai Automated Cell Culture System or manual pipettes
- ImageXpress HCS.ai High-Content Screening System
- IN Carta Image Analysis Software
- 96-well plates (e.g., Ibidi plates)
- Staining dyes: Hoechst (nuclei), MitoTracker Orange (mitochondria), Alexa Fluor 488 Phalloidin (F-actin)
Methodology:
- Culture Setup: Seed primary mouse intestinal organoids in Matrigel domes (15 µL per dome) in a 96-well plate. Use IntestiCult media as per the manufacturer's protocol. Aim for approximately 60 organoids per dome to avoid overlap for imaging.
- Maintenance: Culture organoids for 48 hours before compound addition. Perform automated or manual media exchanges every 24 hours.
- Compound Treatment: Prepare test compounds in a 7-point, 4-fold serial dilution. Add compounds to the culture medium and treat organoids for 72 hours. Include a negative control (e.g., 0.1% DMSO) and a positive control (e.g., 1 µM Staurosporine).
- Staining and Fixation: After treatment, stain live organoids with Hoechst and MitoTracker Orange. Fix with 4% paraformaldehyde and then permeabilize and stain with Alexa Fluor 488 Phalloidin.
- Image Acquisition: Image organoids using a high-content confocal imaging system (e.g., ImageXpress HCS.ai). Acquire Z-stacks (e.g., 16 images at 8 µm intervals) at 10X magnification using DAPI, FITC, and TRITC channels. Generate maximum projection images for 2D analysis.
- Image and Data Analysis: Use image analysis software (e.g., IN Carta) to segment organoids and individual cells. Quantify key parameters:
- Number of cells with intact actin (Phalloidin-positive) per organoid.
- Number of cells with damaged actin (Phalloidin-negative) per organoid.
- Number of cells with intact mitochondria (MitoTracker-positive) per organoid.
- Total area of actin-positive cells and average organoid volume.
- Calculate EC50 values for each compound using curve-fitting software.
The workflow for this protocol is summarized in the diagram below:
Protocol 2: Generating Patient-Derived Colorectal Organoids
This protocol provides a guide for establishing PDOs from colorectal tissues, crucial for personalized drug screening [94].
Materials & Reagents:
- Human colorectal tissue samples (normal, polyp, or tumor)
- Cold Advanced DMEM/F12 medium with antibiotics
- Digestion enzymes (e.g., Collagenase)
- Basal culture medium: Advanced DMEM/F12 supplemented with HEPES, L-Glutamine, N-Acetylcysteine, B-27, and A83-01
- Growth factors: EGF, Noggin, R-spondin (often as conditioned media)
- Engelbreth-Holm-Swarm (EHS) murine sarcoma extracellular matrix (ECM)
Methodology:
- Tissue Procurement and Processing: Collect human colorectal tissue samples under sterile conditions immediately after colonoscopy or surgical resection. Place the sample in cold Advanced DMEM/F12 medium with antibiotics.
- Critical Step - Tissue Preservation:
- If processing within 6-10 hours: Wash tissue with an antibiotic solution and store at 4°C in DMEM/F12 with antibiotics.
- If delay exceeds 14 hours: Cryopreserve the tissue after an antibiotic wash using a freezing medium (e.g., 10% FBS, 10% DMSO in 50% L-WRN conditioned medium).
- Crypt Isolation and Seeding: Mince the tissue finely and digest with collagenase to isolate crypts. Pellet the crypts and resuspend in a predefined ECM. Spot the ECM-cell suspension as domes in a culture plate and solidify at 37°C.
- Organoid Culture: Overlay the solidified domes with complete intestinal organoid medium, which typically contains EGF, Noggin, R-spondin-1, and other tissue-specific factors. Refresh the medium every 2-3 days.
- Passaging and Expansion: For expansion, mechanically or enzymatically dissociate the organoids after 7-14 days. Re-embed the fragments in fresh ECM and continue culture with the appropriate medium.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Organoid Culture and Toxicity Assessment
| Item | Function | Example Application |
|---|---|---|
| Matrigel / ECM Matrix | Provides a 3D scaffold that mimics the native basement membrane, supporting complex organoid structure and signaling. | Standard scaffold for embedding intestinal, hepatic, and mammary organoids [98] [93]. |
| Noggin | A BMP signaling pathway inhibitor. Promotes epithelial growth and prevents differentiation in many organoid types. | Essential component in colon, esophageal, and pancreatic organoid media [98] [99]. |
| R-spondin 1 | Potent activator of the Wnt signaling pathway by binding to LGR receptors. Critical for maintaining stemness. | Used in colon and esophageal organoid cultures to support stem cell expansion [94] [98]. |
| EGF (Epidermal Growth Factor) | Stimulates epithelial cell proliferation and survival via the EGFR signaling pathway. | A common mitogen in nearly all epithelial organoid culture media formulations [98] [99]. |
| A83-01 | A TGF-β type I receptor inhibitor. Suppresses epithelial differentiation into fibroblasts (EMT). | Included in colon and pancreatic organoid media to maintain epithelial proliferation [98]. |
| ROCK Inhibitor (Y-27632) | Inhibits Rho-associated coiled-coil kinase. Reduces anoikis (cell death after detachment) and improves viability after passaging or thawing. | Added to the medium for the first few days after thawing or passaging cryopreserved organoids [98]. |
| Hoechst 33342 | Cell-permeant blue-fluorescent nuclear stain. Used to identify all cells and segment structures in image analysis. | Standard nuclear counterstain for immunofluorescence and viability assays in organoids [93]. |
| Phalloidin (e.g., Alexa Fluor 488) | High-affinity green-fluorescent stain for F-actin, outlining the cytoskeleton and cell morphology. | Used to visualize organoid structure and quantify cells with an intact cytoskeleton in toxicity assays [93]. |
| MitoTracker (e.g., Orange CMTMRos) | Orange-fluorescent dye that accumulates in active mitochondria, serving as a marker of cell viability and metabolic activity. | Used in tandem with Phalloidin to quantify the number of healthy cells per organoid after compound treatment [93]. |
The core signaling pathways involved in maintaining intestinal stem cells within organoids are illustrated below:
Integrating AI and Machine Learning for Automated Morphological Analysis
Troubleshooting Guides
Data Quality and Preparation Issues
Problem: High Dimensionality and Complex Data Sets Become Unwieldy Managing the high dimensionality of morphological feature data from high-content screens is a common challenge that can slow down analysis and reduce model performance [101].
- Solution: Implement feature selection and dimensionality reduction techniques as a standard pre-processing step. Before model training, use methods like Principal Component Analysis (PCA) to identify the most informative features. This simplifies the computational load and can improve model accuracy by removing redundant data [102].
Problem: Model Performance is Skewed by Background Noise or Artifacts A frequent issue is that the AI model learns to recognize irrelevant background features or technical artifacts instead of the true biological signal. For example, a model might associate a snowy background with a specific dog breed, or a particular plate layout with a toxic effect [103].
- Solution:
- Data Augmentation: During training, use augmented data that includes random cropping, rotation, and color variations. This forces the model to focus on invariant morphological features of the target itself [103].
- Quality Control Checks: Integrate automated quality control (QC) metrics into your pipeline. Flag samples with abnormal quality metrics (e.g., out-of-focus images, low cell count) for re-run or exclusion, as demonstrated by Ardigen's phenAID platform [102].
- Explainable AI (XAI): Use techniques like Class Activation Maps (CAMs) to visualize which pixels in an image most influenced the model's decision. This allows researchers to verify the model is focusing on biologically relevant structures [104].
Problem: Inconsistent Manual Annotations Introduce Subjectivity Manual assessment of morphological changes is time-consuming and prone to subjectivity, leading to inconsistent labels for training data [105].
- Solution: Employ a multi-view convolutional neural network (MVCNN) approach. As used in zebrafish toxicity screening, this technique aggregates predictions from multiple views of the same subject, reducing reliance on a single, potentially subjective annotation and achieving a high F1 score (0.88) in distinguishing normal from abnormal morphologies [105].
Model Training and Performance Issues
Problem: Model Fails to Generalize to New Chemical or Genetic Perturbations A model performs well on its training data but fails when presented with new types of compounds or genetic backgrounds. This is often due to underlying bias in the training data [106].
- Solution: Use the Biological Bias Assessment Guide during model development [106].
- Data Considerations: Proactively ask if your dataset over-represents certain chemical classes or cell types. Intentionally seek to include a diverse set of perturbations.
- Model Evaluation: Evaluate model performance not just on a held-out test set, but on completely external datasets that represent new biological contexts. High-level metrics can obfuscate critical variability in performance across different classes [106].
Problem: Difficulty Distinguishing Subtle Morphological Differences Between Phenotypes The model struggles to tell the difference between visually similar phenotypes, such as different types of edema or specific craniofacial malformations [103].
- Solution: Implement a structured, multi-scale feature extraction architecture inspired by human visual perception.
- Morphological Feature Extractor: Design parallel analyzers in your neural network, each focusing on a specific aspect (e.g., overall body proportion, head shape, texture). This "coarse-to-fine" processing mimics how experts analyze morphology and improves recognition of subtle differences [103].
- Group Related Abnormalities: If classifying specific, fine-grained features is challenging, group related abnormalities into a broader category for initial screening. In zebrafish models, grouping related abnormalities improved classifier performance, with five out of seven grouped classifiers achieving F1 scores near 0.80 [105].
Problem: Model is a "Black Box" and Lacks Biological Interpretability The model's predictions are accurate but not trusted by biologists because the reasoning is not transparent [107] [108].
- Solution:
- Prioritize the development of explainable AI (XAI) models. The field is moving beyond "black box" models towards those that provide insights into the morphological features driving the prediction [107].
- Use model interpretation tools like feature visualization. For example, in a dog breed identification project, the "Morphological Feature Extractor" was designed to provide explicit, human-understandable features (e.g., ear shape, fur texture), making the model's decision-making process more interpretable [103].
Implementation and Workflow Issues
Problem: AI Tool is Not Adopted by End-Users Due to Workflow Disruption The AI solution is technically sound but is not used because it doesn't fit into the existing research workflow or is perceived as a burden [109].
- Solution: Conduct implementation science research before deployment [109].
- Engage end-users (scientists) early in the design process to understand their workflow and customize the user interface to minimize disruption.
- Use qualitative methods like surveys and focus groups to ascertain barriers to adoption and perceptions of the tool's integration [109].
Problem: Separating Toxicity-Driven Signals from Biologically Relevant Hits In phenotypic screening, a strong toxic signal can mask a more subtle, therapeutically relevant phenotypic change [102].
- Solution: Use advanced phenotypic profiling that can disentangle multiple morphological effects. Ardigen's approach involves using a combination of CellProfiler and deep learning features to cross-reference results with controls and actively separate toxicity-related effects from relevant phenotypes [102].
Frequently Asked Questions (FAQs)
Q1: What are the first steps I should take if my AI model's performance drops significantly after deployment? First, check for data drift. The new data being processed may differ statistically from the data the model was trained on. Continuously monitor input data and model predictions, and establish a retraining pipeline with new, curated data to maintain model performance over time [106].
Q2: How can I assess and mitigate bias in my morphological analysis model? Follow a structured framework like the Biological Bias Assessment Guide [106]. This involves:
- Identifying Bias: Question whether your training data over-represents certain chemical structures, cell lines, or experimental conditions.
- Mitigating Bias: Actively curate your datasets to be more representative of the biological diversity you expect to encounter. Use techniques like stratified sampling to ensure all relevant groups are included.
- Documenting Bias: Use tools like Datasheets for Datasets to document the composition, collection process, and known limitations of your data, promoting transparency [106].
Q3: My segmentation model for cellular structures is inaccurate. What can I do? Ensure you are using the right architecture and sufficient high-quality labels.
- Architecture: Use state-of-the-art segmentation architectures like UNet++, which have been successfully applied for delineating regions of interest (e.g., head, tail, bladder) in zebrafish larvae, achieving high Intersection over Union (IoU) scores above 0.80 [105].
- Data: Review the quality and consistency of your ground truth segmentation masks. Inconsistent annotations will directly lead to poor model performance.
Q4: What is the difference between using deep learning features and traditional hand-crafted features for morphological analysis?
- Hand-crafted features (e.g., from CellProfiler) are based on pre-defined measurements (size, shape, intensity) and are highly interpretable.
- Deep learning features are learned automatically from the data and can capture complex, subtle patterns that may be missed by pre-defined measurements. The most powerful approach is often a combination of both, leveraging the interpretability of hand-crafted features and the power of deep learning for complex pattern recognition [102].
Q5: How do I validate that my AI model is truly improving patient care or drug discovery outcomes? Internal validation (e.g., high accuracy on a test set) is not enough [109].
- Clinical/Biological Validation: Compare your model's predictions to those of expert scientists or biologists, or to validated experimental outcomes.
- Outcome Evaluation: The gold standard is a randomized controlled trial (RCT), but these can be challenging. Alternatives include matched cohort studies or prospective before-and-after studies to establish the model's impact on research efficiency or decision-making [109].
Quantitative Performance Data
The table below summarizes key performance metrics from recent AI models applied to morphological analysis in toxicology and biology, providing benchmarks for your own experiments.
Table 1: Performance Benchmarks for AI in Morphological Analysis
| Application Domain | Model Architecture | Key Performance Metrics | Reference |
|---|---|---|---|
| Zebrafish Developmental Toxicity Screening | Multi-View CNN (MVCNN) | F1 Score: 0.88 (binary classification: normal vs. any morphological change) | [105] |
| Zebrafish Developmental Toxicity Screening | Grouped Classifiers | F1 Score: ~0.80 (for 5 out of 7 groups of related abnormalities) | [105] |
| Zebrafish Developmental Toxicity Screening | Segmentation Models (e.g., UNet++) | IoU Score: >0.80 (for 9 out of 11 regions of interest) | [105] |
| Phenotypic Hit Identification (General) | Combination of CellProfiler & Deep Learning Features | Enabled separation of toxicity effects from relevant phenotypes; improved biological relevance of hits. | [102] |
Experimental Protocol: AI-Driven Zebrafish Toxicity Screening
This protocol is adapted from the SEAZIT project, which used AI for developmental toxicity chemical screening [105].
Objective: To automate the classification and segmentation of morphological changes in zebrafish larvae exposed to compounds for developmental toxicity screening.
Workflow Overview:
Step-by-Step Methodology:
Image Acquisition:
- Expose zebrafish embryos to various test chemicals for 5 days.
- Acquire high-resolution images of the larvae using a high-content screening microscope. Capture multiple views per larva if using a Multi-View CNN (MVCNN) architecture.
Data Preprocessing and Labeling:
- Labeling for Classification: Manually label images for 20 distinct types of larval morphological changes (e.g., yolk sac edema, craniofacial malformations, pericardial edema). This creates the ground truth data for the classification model.
- Annotation for Segmentation: Manually annotate the regions of interest (ROIs) such as head, tail, bladder, and yolk sac on the images to create the ground truth for the segmentation model.
Model Training:
- For Classification:
- Use architectures like EfficientNet or ResNet.
- Train a binary classifier to distinguish normal from abnormal embryos.
- Train additional classifiers for specific morphological changes. Consider grouping related abnormalities to improve performance (e.g., a single "edema" group).
- For Segmentation:
- Use an architecture like UNet++.
- Train the model to pixel-wise delineate the annotated ROIs. The loss function (e.g., Dice loss) will optimize the overlap between the prediction and the ground truth mask.
- For Classification:
Model Inference and Analysis:
- Classification: Input new larval images into the trained classification model to obtain predictions (normal/abnormal or specific phenotype).
- Segmentation: Input new images into the segmentation model to generate precise masks of the ROIs. Use the resulting masks to extract quantitative measurements (e.g., yolk sac area, head size).
- Validation: Compare AI-generated results with manual assessments from experienced screeners to validate accuracy and reduce subjectivity.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for AI-Based Morphological Analysis in Toxicology
| Tool / Resource | Function | Example Use Case |
|---|---|---|
| phenAID Platform (Ardigen) | An AI-powered platform for hit identification in phenotypic screens. Combines CellProfiler and deep learning features. | Filters out toxicity-driven signals to identify biologically relevant hits in high-throughput compound screening [102]. |
| Biological Bias Assessment Guide (CZI) | A structured framework to identify and address bias in AI models for biology. | Used during model development to ensure models are robust and reliable across different biological contexts and populations [106]. |
| CellProfiler | Open-source software for measuring and analyzing cell images. Extracts hand-crafted morphological features. | Generates interpretable, quantitative features from cellular images for use in machine learning models or to complement deep learning features [102]. |
| Zebrafish (Danio rerio) Model | A vertebrate model organism for developmental toxicity and disease modeling. | Used in the SEAZIT project to generate image data for training AI models to classify and segment developmental abnormalities [105]. |
| Class Activation Maps (CAMs) | An explainable AI (XAI) technique that produces visual explanations for decisions from CNNs. | Helps researchers verify that an AI model is basing its toxicity prediction on biologically relevant morphological structures and not artifacts [104]. |
Core Concepts and Frequently Asked Questions
FAQ 1: What is the fundamental difference between traditional and label-free flow cytometry?
Traditional flow cytometry relies on fluorescent labels or dyes that bind to specific cellular components (e.g., proteins, nucleic acids) to generate a detectable signal. This requires extensive sample preparation and staining, which can be time-consuming, costly, and may potentially alter cell function or viability due to chemical toxicity or steric hindrance [110] [111]. In contrast, label-free flow cytometry analyzes cells in their native, unperturbed state by leveraging intrinsic cellular properties. It uses techniques that measure light scatter profiles, morphological features, or chemical "fingerprints" without the need for exogenous labels, thereby simplifying sample preparation and providing a more direct assessment of cellular physiology [112] [113] [111].
FAQ 2: Why is label-free analysis particularly important for cell health assessment in compound toxicity filtering?
Label-free methods are crucial for toxicity screening because they provide a more unbiased view of cell health. Fluorescent labels themselves can sometimes be cytotoxic or interfere with the very cellular processes being studied, leading to artifacts [110]. Label-free approaches, such as monitoring scatter light profiles or metabolic activity, can rapidly detect early signs of stress or injury at a single-cell level, often before irreversible cell death occurs [112] [110]. This allows for a more sensitive and accurate determination of a compound's cytotoxic potential, supporting the principles of New Approach Methodologies (NAMs) which aim to provide more human-relevant toxicity data while reducing reliance on animal models [114].
FAQ 3: My label-free viability data doesn't match our traditional culture-based results. Why?
This is a common issue, often indicating a key strength of label-free flow cytometry. Culture-based methods (e.g., colony-forming unit counts) can only detect bacteria that are able to proliferate on a specific growth medium. Chemical disinfectants or toxic compounds can induce a "Viable But Non-Culturable" (VBNC) state in cells, where they remain metabolically active and intact but cannot grow on standard media, leading to false negatives in culture tests [112]. Label-free flow cytometry, which assesses properties like membrane integrity via light scatter, can detect these VBNC cells, providing a more accurate picture of true viability and the bacteriostatic versus bactericidal nature of a treatment [112].
FAQ 4: What are the main technical challenges associated with label-free flow cytometry, and how can they be mitigated?
A primary challenge is the weaker signal in some modalities, such as Raman flow cytometry, which can lead to lower throughput as signals need to be collected over longer periods [111]. Data complexity is another hurdle; high-dimensional data from spectral or imaging flow cytometry requires advanced computational tools, including machine learning, for robust analysis and interpretation [114] [115]. Mitigation strategies include technological innovations like time-delay integration (TDI) to enhance signal-to-noise ratio and throughput in Raman cytometry, and the adoption of standardized data analysis frameworks and AI-driven software to manage and extract meaningful insights from complex datasets [114] [115] [111].
Troubleshooting Common Experimental Issues
| Problem | Potential Causes | Solutions & Troubleshooting Steps |
|---|---|---|
| Low Signal-to-Noise in Label-Free Readouts | • Suboptimal laser power or detector gain• Poorly focused flow stream• High background from cell debris or media components• Inherently weak signal (e.g., in Raman cytometry) | • Calibrate instrument optics and photomultiplier tubes (PMTs)• Use acoustic focusing to align cells in the center of the stream [111]• Centrifuge and resuspend sample in a clean, low-fluorescence buffer• For Raman, employ Time-Delay Integration (TDI) to accumulate signal [111] |
| High Background in Scatter Plots | • Cell aggregation or clumping• Excessive debris from dead cells or sample preparation• Contaminated sheath fluid or dirty flow cell | • Filter cells through a sterile mesh (e.g., 40µm) before analysis• Optimize washing and centrifugation steps to preserve membrane integrity [110]• Perform rigorous instrument cleaning and use filtered, sterile sheath fluid |
| Poor Correlation with Viability Standards | • Detection of Viable But Non-Culturable (VBNC) populations [112]• Assays measuring different physiological states (e.g., metabolic activity vs. membrane integrity) [110]• Incorrect gating strategy on flow cytometry data | • Use an orthogonal method (e.g., a metabolic dye) to confirm the VBNC state [112]• Understand the mechanism of your assay; use a combination of membrane integrity and metabolic assays for a complete picture [110]• Include appropriate controls (live, dead, compound-treated) to set gates accurately |
| Low Throughput in Label-Free Modalities | • Slow data acquisition rates to capture sufficient signal• Complex data processing pipelines• Cell settling or aggregation in the sample tube | • Optimize flow rate; balance with signal quality. For Raman, implement TDI methods [111]• Utilize high-performance computing and pre-trained AI models for faster analysis [115]• Use sample mixers or vortex samples gently between runs |
Detailed Experimental Protocols
Protocol 1: Label-Free Flow Cytometry for Disinfectant Efficacy Testing (Bactericidal Assessment)
This protocol, adapted from a 2025 study, provides a rapid (≈4 hours) alternative to standard culture-based tests (which take up to 48 hours) for evaluating compound toxicity on bacterial strains [112].
1. Key Research Reagent Solutions
| Reagent/Solution | Function in the Protocol |
|---|---|
| Chemical Disinfectant (e.g., Alcohols, Oxidizing Agents) | The test compound whose toxicity is being evaluated. |
| Sterile Distilled Water | Used for preparing disinfectant dilutions as per manufacturer recommendations. |
| Tryptic Soy Broth (TSB) | Growth medium for bacterial culture and post-treatment recovery. |
| Neutralizing Solution | Critical for stopping the disinfectant's action at the end of the contact time to prevent continued toxicity. |
2. Step-by-Step Methodology
- Step 1: Bacterial Culture Preparation. Grow reference or clinical bacterial strains (e.g., Staphylococcus aureus, Pseudomonas aeruginosa) to mid-logarithmic phase in an appropriate broth like TSB [112].
- Step 2: Disinfectant Exposure. Dilute the chemical disinfectant to the desired concentration in sterile distilled water. Mix the bacterial suspension with the disinfectant solution and incubate for the manufacturer-recommended contact time (e.g., 1-15 minutes) at room temperature [112].
- Step 3: Reaction Neutralization. After the contact time, immediately add a neutralizing solution to the mixture to quench the disinfectant's activity. This is a crucial step for accurate assessment of the effect at the precise contact time.
- Step 4: Sample Preparation for FCM. Centrifuge the neutralized mixture, wash the bacterial pellet, and resuspend in a saline or buffer solution to a standardized concentration for flow cytometry analysis.
- Step 5: Label-Free Flow Cytometry Analysis. Analyze the sample using a flow cytometer. The label-free assessment is based on scatter light profiles: forward scatter (FSC-H, indicating cell size) and side scatter (SSC-H, indicating cell granularity/complexity). Viable, injured, and dead cells will occupy distinct regions in the FSC-H/SSC-H dot plot [112].
- Step 6: Data Interpretation. The bactericidal efficacy is determined by the reduction in the count of cells within the "viable" gate on the scatter plot compared to an untreated control. This method has shown strong correlation with standard culture tests, with 91.4% agreement, 94% sensitivity, and 98% specificity [112].
Protocol 2: Orthogonal Viability Assessment Using Fluorescent Staining
This protocol can be used in tandem with label-free scattering to confirm results, especially to investigate sub-populations like VBNC cells [112] [110].
1. Key Research Reagent Solutions
| Reagent/Solution | Function in the Protocol |
|---|---|
| Membrane Integrity Dye (e.g., Propidium Iodide - PI) | Stains nucleic acids of cells with compromised membranes, indicating dead/necrotic cells. |
| Metabolic Activity Dye (e.g., SYTO 9, CFSE) | Stains all cells (live and dead) or tracks division in live, metabolically active cells. |
| Staining Buffer (e.g., PBS) | A non-toxic buffer for diluting and applying fluorescent dyes. |
2. Step-by-Step Methodology
- Step 1: Sample Preparation. Follow steps 1-4 from Protocol 1 to obtain a washed, neutralized cell pellet.
- Step 2: Fluorescent Staining. Resuspend the cell pellet in a staining buffer containing a combination of fluorescent dyes. A common combination is PI (which only enters dead cells) and a membrane-permeant dye like SYTO 9 (which enters all cells). Alternatively, a metabolic activity assay like CFSE can be used to track proliferation [110].
- Step 3: Incubation and Analysis. Incubate the stained cells in the dark for a manufacturer-specified time, then analyze using flow cytometry with the appropriate laser and filter sets.
- Step 4: Data Interpretation. Create a two-color dot plot (e.g., SYTO 9 vs. PI) to distinguish the populations: SYTO 9+/PI- (live cells), SYTO 9+/PI+ (injured or late apoptotic cells), and SYTO 9-/PI+ (dead cells). This provides an orthogonal validation of the viability status inferred from the label-free scatter profiles in Protocol 1 [112] [110].
Quantitative Data Comparison: Traditional vs. Label-Free Methods
Table: Performance Comparison of Cell Viability and Toxicity Assessment Methods
| Methodology | Key Measured Parameter(s) | Approximate Time to Result | Ability to Detect VBNC State | Throughput | Key Limitations |
|---|---|---|---|---|---|
| Traditional Culture-Based (e.g., EN 13727+A2) [112] | Microbial growth on solid media | 24 - 48 hours | No | Low | Time-consuming; misses VBNC cells; provides population-average data only. |
| Traditional Flow Cytometry (Fluorescence-Based) [110] | Fluorescence from DNA/RNA dyes, viability stains, antibody tags | 2 - 4 hours (plus staining time) | Yes (with appropriate dyes) | High (up to thousands of cells/sec) | Requires staining, which can be toxic, expensive, and alter cell biology. |
| Label-Free Flow Cytometry (Light Scatter) [112] | Forward Scatter (FSC) & Side Scatter (SSC) | ~4 hours | Yes | High | Less specific; can be confounded by debris or cells of similar size/granularity. |
| Label-Free Imaging Flow Cytometry [115] | Morphology, size, texture, and optical density | Minutes to hours (depends on sample size) | Yes | Medium | Generates very large, complex datasets requiring advanced analysis tools. |
| Label-Free Raman Flow Cytometry [111] | Molecular vibrational "fingerprint" | Seconds per cell (Throughput: ~32 cells/sec) | Potentially Yes | Low (currently a bottleneck) | Very weak signal; requires sophisticated optics and data analysis. |
Visualized Workflows and Signaling Pathways
The following diagrams illustrate the core workflows and logical decision processes in traditional and label-free flow cytometry for toxicity assessment.
Diagram 1: Traditional vs. Label-Free Flow Cytometry Workflow
Diagram 2: Cell Death Pathway Analysis in Toxicity Screening
Conclusion
Effective compound toxicity filtering hinges on a strategic, multi-parametric approach to cell health assessment. Relying on a single assay endpoint is insufficient; instead, a combination of methods that probe different aspects of cell physiology is critical for distinguishing true mechanistic toxicity from assay artifacts. The integration of high-throughput methodologies with advanced, physiologically relevant 3D models and AI-driven analytics represents the future of predictive toxicology. By adopting these comprehensive and kinetic profiling strategies, researchers can derisk drug candidates earlier, reduce late-stage attrition due to toxicity, and ultimately accelerate the development of safer therapeutics. The ongoing shift towards human cell-based systems and the standardization of phenotypic profiling promise to further enhance the predictive accuracy of in vitro toxicity screening, paving the way for more efficient and successful drug discovery pipelines.
References
- 1. What is the difference between cytotoxicity and cell viability? [https://www.susupport.com/blogs/knowledge/what-is-the-difference-between-cytotoxicity-and-cell-viability]
- 2. Cytotoxicity - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/cytotoxicity]
- 3. A review of cytotoxicity testing methods and in vitro study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534221/]
- 4. Cell Viability Assays - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK144065/]
- 5. WST-1 Assay: principles, protocol & best practices for cell ... [https://www.abcam.com/en-us/knowledge-center/cell-biology/wst-1-assay-principles-protocols-and-best-practices-for-cell-viability]
- 6. Multi-assay assessment of cytotoxicity reveals multiple ... [https://www.nature.com/articles/s41598-025-86792-4]
- 7. Cell Painting for cytotoxicity and mode-of-action analysis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11785178/]
- 8. Mitochondria in oxidative stress, inflammation and aging [https://www.nature.com/articles/s41392-025-02253-4]
- 9. Mitochondrial Oxidative Stress—A Causative Factor and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8707347/]
- 10. Oxidative stress and mitochondrial impairment: Key drivers ... [https://www.sciencedirect.com/science/article/abs/pii/S1568163725000133]
- 11. Mitochondrial dysfunction: mechanisms and advances in ... [https://www.nature.com/articles/s41392-024-01839-8]
- 12. Oxidative cell death in the central nervous system [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1562344/full]
- 13. Drug Discovery Assays Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/drug-discovery-development-support-center/drug-discovery-assays-support/drug-discovery-assays-support-troubleshooting.html]
- 14. Troubleshooting Cell-based Assays Ask the Experts to ... [https://www.promega.com/resources/webinars/promega-germany/210730-troubleshooting-cell-based-assays/]
- 15. Mitochondrial Dysfunction, Its Oxidative Stress-Induced ... [https://www.mdpi.com/1420-3049/29/12/2738]
- 16. Mitochondrial Dysfunction and Oxidative Stress: Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383163/]
- 17. Assay Guidance Manual - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK53196/]
- 18. Comprehensive landscape of cell death mechanisms [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1611055/full]
- 19. Insights on the crosstalk among different cell death ... [https://www.nature.com/articles/s41420-025-02328-9]
- 20. Drug toxicity assessment: cell proliferation versus cell death [https://www.nature.com/articles/s41420-022-01207-x]
- 21. Comprehensive analysis of cellular metrics [https://www.nature.com/articles/s41420-025-02391-2]
- 22. Comprehensive analysis of regulated cell death pathways [https://pubmed.ncbi.nlm.nih.gov/40830711/]
- 23. Editorial: Regulated cell death (RCD) in cancer: signaling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436450/]
- 24. Therapeutic Targeting of Apoptosis, Autophagic Cell Death ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293011/]
- 25. Ferroptosis, a Distinct Form of Cell Death, and Research ... [https://www.mdpi.com/1424-8247/18/12/1785]
- 26. Cell death signaling and immune regulation - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355773/]
- 27. Reactive oxygen species: toxic molecules or spark of life? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1550838/]
- 28. chemistry and biology of reactive oxygen species [https://www.sciencedirect.com/science/article/abs/pii/S1744165X10000363]
- 29. Approaches and Methods to Measure Oxidative Stress in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6434272/]
- 30. Reactive oxygen species [https://en.wikipedia.org/wiki/Reactive_oxygen_species]
- 31. Guidelines for measuring reactive oxygen species and ... [https://www.nature.com/articles/s42255-022-00591-z]
- 32. Methods for Detection of Mitochondrial and Cellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3887411/]
- 33. Reactive Oxygen Species (ROS) Detection [https://www.bmglabtech.com/en/blog/reactive-oxygen-species-detection/]
- 34. Methods for the detection of reactive oxygen species [https://pubs.rsc.org/en/content/articlelanding/2018/ay/c8ay01339j]
- 35. Oxidative Stress Assays | Reactive Oxygen Species ... [https://www.promega.com/products/cell-health-assays/oxidative-stress-assays/]
- 36. Mechanisms of DNA damage, repair and mutagenesis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5474181/]
- 37. ToxACoL: an endpoint-aware and task-focused compound ... [https://www.nature.com/articles/s41467-025-60989-7]
- 38. Revisiting the approaches to DNA damage detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12054138/]
- 39. Development of the toxicity values database, ToxValDB [https://www.sciencedirect.com/science/article/abs/pii/S2468111325000258]
- 40. Genotoxicity Assessment: Methods and Protocols [https://link.springer.com/book/10.1007/978-1-4939-9646-9]
- 41. Advances in DNA damage detection: Current progress, ... [https://www.sciencedirect.com/science/article/pii/S0165993625001141]
- 42. DNA damage repair: historical perspectives, mechanistic ... [https://www.nature.com/articles/s41392-021-00648-7]
- 43. Comprehensive interrogation of synthetic lethality in the ... [https://www.nature.com/articles/s41586-025-08815-4]
- 44. An Overview of the Current State of Cell Viability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11719996/]
- 45. Is Your MTT Assay the Right Choice? [https://www.promega.com/resources/pubhub/is-your-mtt-assay-really-the-best-choice/]
- 46. MTT assay and its use in cell viability and proliferation ... [https://www.abcam.com/en-us/knowledge-center/cell-biology/mtt-assay]
- 47. CytoTox-ONE™ Homogeneous Membrane Integrity Assay [https://www.promega.com/products/cell-health-assays/cell-viability-and-cytotoxicity-assays/cytotox_one-homogeneous-membrane-integrity-assay/]
- 48. LDH assay kit guide: Principles and applications [https://www.abcam.com/en-us/knowledge-center/cell-biology/ldh-assay-kit-guide-principles-and-application]
- 49. Trypan blue dye exclusion assay: Principles, protocols, and ... [https://deepscienceresearch.com/dsr/catalog/book/107/chapter/387]
- 50. Trypan Blue Exclusion Test of Cell Viability - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6716531/]
- 51. An Optimized LIVE/DEAD Assay Coupled with Flow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453624/]
- 52. Troubleshooting Tips for Fluorescence Staining [https://biotium.com/tech-tips-protocols/troubleshooting-tips-for-fluorescence-staining/]
- 53. Troubleshooting in Fluorescent Staining [https://www.creative-bioarray.com/support/troubleshooting-in-fluorescent-staining.htm]
- 54. SignalStar® Multiplex IHC Troubleshooting Guide [https://www.cellsignal.com/applications/signalstar-troubleshooting-guide?srsltid=AfmBOoo0bKcqDwHUFOrLwi8uX0InB_Emje5xhDT5qS5DZi_p7ep4cTWx]
- 55. Tips & Tricks | Immunoassay Protocols & Troubleshooting [https://www.merckmillipore.com/AL/en/technical-documents/product-supporting/milliplex/tips-tricks-immunoassay-protocol-troubleshooting-advice]
- 56. Guidelines for 3-color multiplex assay design for optimized ... [https://www.stillatechnologies.com/digital-pcr/naica-system-analysis/guidelines-for-3-color-multiplex-assay-design-for-optimized-performance-with-crystal-digital-pcr/]
- 57. Save Precious Time with Same-Well Multiplexing [https://www.promegaconnections.com/save-precious-time-with-same-well-multiplexing/]
- 58. Incucyte® Cytotoxicity Assays for Live-Cell Analysis [https://www.sartorius.com/en/applications/life-science-research/live-cell-assays/cytotoxicity]
- 59. "Multiplexed viability, cytotoxicity, and caspase activity ... [https://pubmed.ncbi.nlm.nih.gov/25308259/]
- 60. Guide to Multiplex Immunoassays: Multiplex ELISA and More [https://www.thermofisher.com/blog/life-in-the-lab/guide-to-multiplex-immunoassays-multiplex-elisa-and-more/]
- 61. Tips & Tricks | Guide to Multiplexing | MILLIPLEX® Assays [https://www.sigmaaldrich.com/US/en/technical-documents/product-supporting/milliplex/tips-tricks-guide-multiplexing-milliplex-assays?srsltid=AfmBOop1KlhPcQWOCShLBOzpq6BF-9u95mLADswAG9OXH0Ib1XFwULoo]
- 62. Quantitative high-throughput screening data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4375054/]
- 63. High Throughput Screening (HTS) Services [https://www.evotec.com/solutions/drug-discovery-preclinical-development/discovery/hit-identification-services/high-throughput-screening-hts-services]
- 64. Quantitative high-throughput screening - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/16864780/]
- 65. High Throughput Screening - an overview [https://www.sciencedirect.com/topics/chemistry/high-throughput-screening]
- 66. Cytotoxic and Cytostatic [https://www.ecct-asia.com/info-for-cancer-patient-or-caretaker/cytoeffect]
- 67. Molecular mechanisms of cell death: recommendations ... [https://www.nature.com/articles/s41418-017-0012-4]
- 68. Contrasting the impact of cytotoxic and cytostatic drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6886869/]
- 69. How to Avoid False Positives and False Negatives in ... [https://www.acdlabs.com/blog/how-to-avoid-false-positives-and-false-negatives-in-analytical-chemistry/]
- 70. Practices of Science: False Positives and False Negatives [https://manoa.hawaii.edu/exploringourfluidearth/chemical/matter/properties-matter/practices-science-false-positives-and-false-negatives]
- 71. How to avoid False Positives and False Negatives in ... [https://www.browserstack.com/guide/false-positives-and-false-negatives-in-testing]
- 72. Systematic Quantification of Population Cell Death Kinetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5509363/]
- 73. How to monitor cell health in real-time [https://www.nature.com/articles/d42473-024-00005-6]
- 74. Advancing predictive toxicology: overcoming hurdles and ... [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d4dd00257a]
- 75. Cell Death Assays: Methods, Applications, and Key ... [https://gmpplastic.com/blogs/useful-articles-on-lab-supplies-faq-section/cell-death-assays-methods-applications-and-key-techniques?srsltid=AfmBOopH6CBa8jxrQ41bx7bhObiKFg209w74fcbM3yqN_qvWBVT4mkI4]
- 76. Flow cytometry-based apoptosis detection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3863590/]
- 77. Blog: Frequently Asked Questions (FAQs) for Microscopy [https://abzena.com/articles/blog/abzena-faqs-for-microscopy/]
- 78. Apoptosis Assays | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-viability-and-regulation/apoptosis.html]
- 79. Considerations for Successful Cell-Based Assays I [https://www.promegaconnections.com/considerations-for-successful-cell-based-assays-i-choosing-your-cells/]
- 80. Profiling Compound Effects on Cell Health in a Time ... [https://www.promega.com/resources/pubhub/profiling-compound-effects-on-cell-health-in-a-time-course-using-a-multiplexed-same-well-assay/]
- 81. A beginners guide to ADME Tox [https://www.cellgs.com/blog/a-beginners-guide-to-adme-tox.html]
- 82. Nuisance compounds in cellular assays - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC7979533/]
- 83. Revealing cytotoxic substructures in molecules using deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7292813/]
- 84. Artificial Intelligence-Driven Drug Toxicity Prediction [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299075/]
- 85. A benchmark concentration-based strategy for evaluating ... [https://link.springer.com/article/10.1007/s00204-025-03971-y]
- 86. Trialblazer: A Chemistry-Focused Predictor of Toxicity ... [https://www.sciencedirect.com/science/article/pii/S0223523425010712]
- 87. Reference compounds for characterizing cellular injury in... [https://www.nature.com/articles/s41467-023-36829-x?error=cookies_not_supported&code=06c59289-e58f-4343-8165-48f98367f593]
- 88. - High Profiling with Content Assay Phenotypic Cell Painting [https://www.moleculardevices.com/en/assets/app-note/dd/img/high-content-phenotypic-profiling-using-the-cell-painting-assay]
- 89. Troubleshooting Low Cell Paint Intensity [https://www.elementbiosciences.com/knowledge-base/troubleshooting-low-cell-paint-intensity]
- 90. Review of High-content Screening Applications in Toxicology [https://pmc.ncbi.nlm.nih.gov/articles/PMC7011178/]
- 91. Review Organoids pharmacology and toxicology [https://www.sciencedirect.com/science/article/pii/S2950489925000351]
- 92. Research Progress, Challenges, and Breakthroughs of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.740574/full]
- 93. Evaluating Compound Toxicity on Intestinal Organoids ... [https://www.moleculardevices.com/en/assets/app-note/dd/img/evaluation-compound-toxicity-effects-on-healthy-intestinal-organoids-using-imaging]
- 94. A Practical Guide to Developing and Troubleshooting Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566426/]
- 95. Trends and challenges in organoid modeling and expansion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11608026/]
- 96. Iteration of Tumor Organoids in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566727/]
- 97. Organoids in Biomedical Research: Opportunities and ... [https://www.wpiinc.com/blog/post/organoids-in-biomedical-research-opportunities-and-challenges?srsltid=AfmBOootb1npFp7Tb8msHPw3m-K3yWU7BxMbxlfAo_07UhBp7FsTd5_d]
- 98. Organoid Culture Guide [https://www.atcc.org/resources/culture-guides/organoid-culture-guide]
- 99. Breakthroughs and challenges of organoid models for ... [https://www.nature.com/articles/s41420-025-02505-w]
- 100. Assessing compound toxicity in healthy intestinal organoids [https://www.news-medical.net/whitepaper/20250612/Assessing-compound-toxicity-in-healthy-intestinal-organoids.aspx]
- 101. What Is A Morphological Analysis? | AI Glossary [https://flowgent.ai/ai-glossary/morphological-analysis]
- 102. Phenotypic Hit Identification: AI-Based Morphological ... [https://ardigen.com/identifying-hits-in-phenotypic-studies-using-artificial-intelligence-based-morphological-analysis/]
- 103. From Fuzzy to Precise: How a Morphological Feature ... [https://towardsdatascience.com/from-fuzzy-to-precise-how-a-morphological-feature-extractor-enhances-ais-recognition-capabilities-2/]
- 104. Comprehensive guide and checklist for clinicians to evaluate ... [https://jmai.amegroups.org/article/view/9123/html]
- 105. driven morphological assessment of zebrafish larvae for ... [https://www.sciencedirect.com/science/article/pii/S0166445X25001808]
- 106. A Framework for Identifying, Assessing and Mitigating ... [https://virtualcellmodels.cziscience.com/micro-pub/bias-assessment-guide]
- 107. AI-based toxicity prediction models using ToxCast data [https://www.sciencedirect.com/science/article/pii/S0300483X25001891]
- 108. 12 Plagues of AI in Healthcare: A Practical Guide to ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2022.765406/full]
- 109. Evaluation of machine learning solutions in medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8443287/]
- 110. From dye exclusion to high-throughput screening: A review ... [https://www.sciencedirect.com/science/article/pii/S0734975025002502]
- 111. Raman flow cytometry using time-delay integration [https://opg.optica.org/optica/abstract.cfm?uri=optica-12-4-479]
- 112. Label-Free Flow Cytometry: A Powerful Tool to Rapidly and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114458/]
- 113. Label-free live cell recognition and tracking for biological ... [https://www.nature.com/articles/s44303-024-00046-y]
- 114. Flow Cytometry: A Tool for New Approach Methodologies [https://www.criver.com/eureka/flow-cytometry-tool-new-approach-methodologies]
- 115. Imaging flow cytometry: from high - resolution ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1580749/full]