Phenotypic vs. Target-Based Screening: Analyzing Success Rates and Strategic Applications in Modern Drug Discovery
This article provides a comprehensive comparison of phenotypic and target-based drug screening strategies, tailored for researchers and drug development professionals.
Phenotypic vs. Target-Based Screening: Analyzing Success Rates and Strategic Applications in Modern Drug Discovery
Abstract
This article provides a comprehensive comparison of phenotypic and target-based drug screening strategies, tailored for researchers and drug development professionals. It explores the historical context and foundational principles of both approaches, examining key metrics such as their relative success in producing first-in-class medicines. The content delves into practical methodological applications, addresses common challenges and optimization tactics, and validates findings with recent case studies and success rates. By synthesizing evidence from industry and academia, it offers a strategic framework for selecting and integrating these methodologies to enhance drug discovery productivity and innovation.
Defining the Paradigms: The History and Core Principles of Phenotypic and Target-Based Screening
The landscape of drug discovery has been historically dominated by two fundamental strategies: phenotypic screening and target-based screening. While the late 20th century saw a significant shift toward target-based approaches, recent decades have witnessed a resurgence in phenotypic screening driven by its proven ability to deliver first-in-class therapies. This guide provides an objective comparison of these parallel methodologies, examining their success rates, experimental protocols, and practical applications in modern drug discovery pipelines. As of 2025, the field has evolved toward integrated workflows that combine the strengths of both approaches, leveraging advances in artificial intelligence, automation, and functional genomics to overcome their respective limitations.
Historical Context and Success Rates
Phenotypic screening, which identifies compounds based on measurable changes in biological function without prior knowledge of the molecular target, predates target-based approaches. Its resurgence follows compelling data on its productivity. Between 1999 and 2008, phenotypic screening was responsible for 28 first-in-class small molecule drugs, compared to 17 from target-based methods [1]. From 2012 to 2022, the application of phenotypic screening in major pharmaceutical companies grew from less than 10% to an estimated 25-40% of project portfolios [1].
Table 1: Comparative Success Rates of Discovery Approaches (1999-2017)
| Discovery Strategy | Number of Approved Drugs |
|---|---|
| Phenotypic Screening | 58 |
| Target-Based Screening | 44 |
| Monoclonal Antibody Therapies | 29 |
Data sources: Swinney and Anthony (2011); Haasen, et al. (2017) as cited in [1].
This renewed adoption stems from phenotypic screening's ability to address complex biological systems and identify novel mechanisms of action, particularly for diseases with multifactorial pathogenesis or poorly understood underlying biology.
Direct Comparison: Phenotypic vs. Target-Based Screening
Table 2: Fundamental Characteristics and Comparative Output
| Parameter | Phenotypic Screening | Target-Based Screening |
|---|---|---|
| Basic Approach | Measures biological effects without requiring known molecular mechanism [2] | Focuses on modulation of predefined molecular targets [2] |
| Key Strength | Identifies novel targets and mechanisms; captures biological complexity [2] [1] | Enables rational drug design; streamlined optimization [2] |
| Primary Limitation | Target deconvolution challenging; potentially longer discovery timelines [2] [3] | Limited to known biology; may miss complex network effects [2] |
| First-in-Class Success | Higher rate of first-in-class drug discovery [1] | Fewer first-in-class discoveries [1] |
| Therapeutic Area Strengths | Oncology, anti-fibrotics, rare diseases with unknown targets [1] [4] | Well-characterized pathways with validated targets [2] |
Experimental Protocols and Methodologies
Phenotypic Screening Workflows
Modern phenotypic screening employs sophisticated experimental designs that incorporate multiple readouts and model systems:
1. High-Content Cellular Screening Recent advances in high-content screening (HCS) combine automated imaging with machine learning-based image analysis to extract multiparametric data from cell-based assays. The workflow typically involves:
- Culturing disease-relevant cell types (primary cells or engineered lines) in multi-well plates
- Compound library addition using automated liquid handling systems
- Incubation for predetermined time periods (hours to days)
- Multiplexed staining with fluorescent dyes or antibodies
- Automated high-throughput microscopy image acquisition
- ML/AI-powered image analysis for phenotypic profiling [1]
2. Complex Model Systems To enhance physiological relevance, researchers are increasingly implementing:
- 3D Cell Cultures and Organoids: The MO:BOT platform automates seeding, media exchange, and quality control for organoids, providing more physiologically relevant data while improving reproducibility [5].
- CRISPR-Enhanced Screening: Genome-wide CRISPR screening combined with organoid models enables systematic investigation of gene-function relationships in biologically relevant contexts [6].
Target Deconvolution Methods
A critical step following phenotypic hit identification is target deconvolution—determining the precise molecular mechanism of action. Commonly employed methods include:
1. Affinity Chromatography
- Involves immobilizing small molecule tool compounds on solid supports
- Often requires compound labeling or modification that may affect binding properties
- Followed by mass spectrometry-based identification of binding partners [3]
2. Activity-Based Protein Profiling
- Uses specialized small molecule probes containing three parts: covalent modifier, linker, and tag for separation
- Targets specific protein classes (e.g., enzymes with active site nucleophiles)
- Enables profiling of enzyme activities in complex proteomes [3]
3. Label-Free Techniques
- Include methods like cellular thermal shift assays (CETSA) that detect drug-target engagement without compound modification
- Measure changes in protein thermal stability upon ligand binding
- Provide direct evidence of target engagement in physiologically relevant environments [7]
4. Genetic Approaches
- CRISPR-based screening identifies genes whose modulation mimics or rescues compound-induced phenotypes
- Expression cloning techniques that increase target expression to facilitate identification [3] [6]
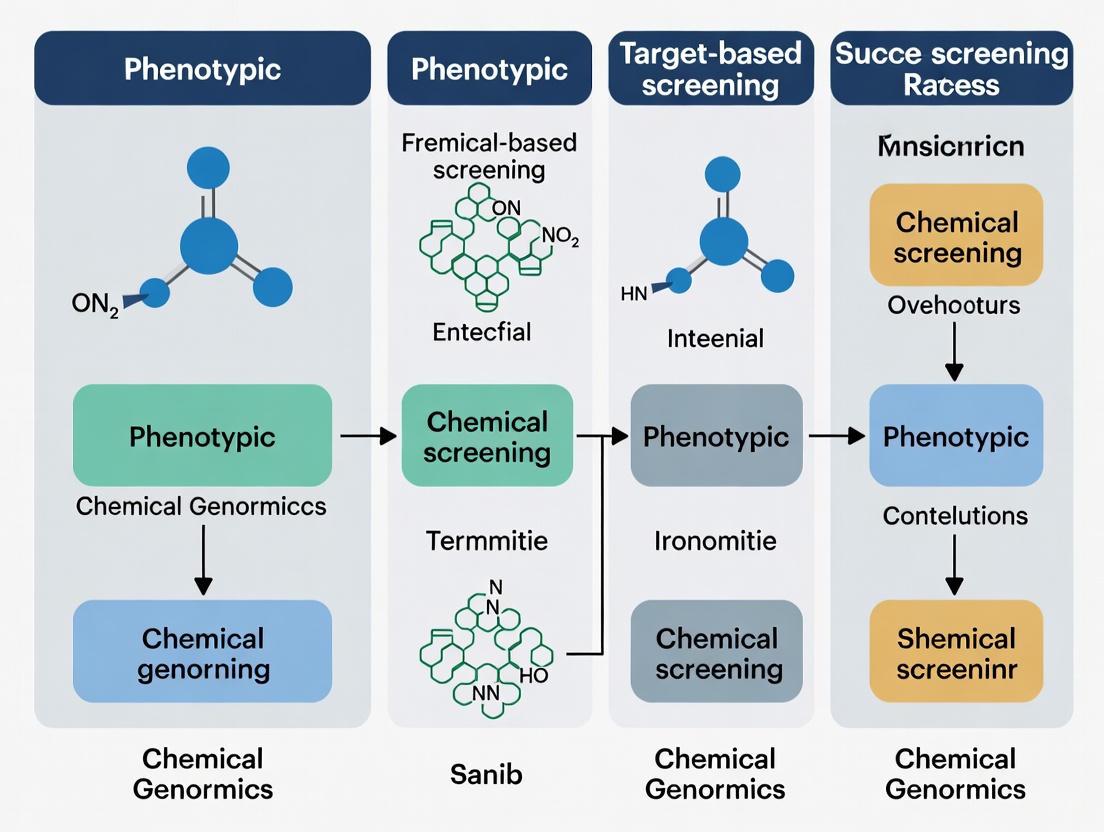
Figure 1: Phenotypic Screening and Target Deconvolution Workflow. Following hit identification from phenotypic assays, multiple parallel approaches are employed to determine the molecular target.
Recent Therapeutic Successes from Phenotypic Screening
Phenotypic screening has yielded multiple recently approved therapies addressing previously untreatable or poorly managed conditions:
Vamorolone (AGAMREE), approved in 2023 for Duchenne muscular dystrophy, was identified through phenotypic profiling that elucidated its unique "dissociative" steroid activity, separating efficacy from typical steroid safety concerns [1].
Risdiplam (Evrysdi), approved in 2020 for spinal muscular atrophy, modulates SMN2 pre-mRNA splicing. The SMN2 target lacked known activity and would have been unlikely identified through traditional target-based approaches [1].
Daclatasvir (Daklinza), a first-in-class NS5A inhibitor for hepatitis C, targets a viral protein with no enzymatic activity and a poorly understood mechanism—characteristics that made it elusive to target-based methods [1].
Lumacaftor (in ORKAMBI), for cystic fibrosis, was discovered using target-agnostic compound screens in cell lines expressing disease-associated CFTR variants [1].
Integrated Approaches and Technological Advancements
The distinction between phenotypic and target-based screening is increasingly blurred by integrated workflows that combine their strengths:
AI-Powered Predictive Models Tools like DrugReflector use active reinforcement learning to predict compounds that induce desired phenotypic changes based on transcriptomic signatures. This approach has demonstrated an order of magnitude improvement in hit rates compared to random library screening [8].
CRISPR-Enhanced Screening CRISPR-Cas9 technology enables high-throughput functional genomics that bridges phenotypic and target-based approaches. By systematically perturbing genes and observing phenotypic outcomes, researchers can:
- Identify novel therapeutic targets across various diseases
- Elucidate drug mechanisms of action
- Investigate gene-drug interactions at genome-wide scale [6]
Automated and Human-Relevant Model Systems Advanced automation platforms like the MO:BOT system standardize 3D cell culture, improving reproducibility and reducing the need for animal models. These systems produce consistent, human-derived tissue models that provide more predictive safety and efficacy data [5].
Figure 2: Convergence of Technologies in Modern Drug Discovery. Integrated approaches combine strengths of both phenotypic and target-based screening enhanced by computational and technological advances.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Technologies and Reagents for Modern Screening Approaches
| Technology/Reagent | Primary Function | Application Context |
|---|---|---|
| MO:BOT Platform | Automated 3D cell culture; standardizes organoid seeding, feeding, QC | Phenotypic screening with enhanced physiological relevance [5] |
| CETSA | Cellular thermal shift assay; measures target engagement in intact cells | Validation of direct drug-target interactions in physiological environments [7] |
| DrugReflector | AI model predicting compounds that induce desired phenotypic changes | Analysis of transcriptomic signatures; improves phenotypic screening hit rates [8] |
| CRISPR sgRNA Libraries | Genome-wide gene perturbation for functional genomics | Identification and validation of novel therapeutic targets [6] |
| High-Content Imaging Systems | Automated microscopy with multiparametric readouts | Phenotypic profiling and morphological analysis [1] |
| ChEMBL Database | Repository of bioactivity data; >20 million data points | Selectivity profiling; tool compound identification [3] |
| eProtein Discovery System | Automated protein expression and purification | Target-based screening; structural biology [5] |
The resurgence of phenotypic screening represents not a rejection of target-based approaches, but an evolution toward more integrated discovery paradigms. While phenotypic screening demonstrates superior performance in generating first-in-class therapies for complex diseases, target-based approaches remain valuable for optimizing compounds against validated targets. The most productive modern pipelines leverage both strategies—using phenotypic screening to identify novel mechanisms and target-based methods for rational optimization—supported by AI, functional genomics, and human-relevant model systems. This synergistic approach addresses the limitations of each method alone, creating a more robust framework for addressing unmet medical needs across diverse therapeutic areas.
The latter part of the 20th century witnessed a fundamental transformation in drug discovery, marked by the rise of target-based screening approaches. This shift was catalyzed by breakthroughs in molecular biology, genomics, and structural biology, which enabled researchers to move away from traditional phenotypic screening—which identifies compounds based on observable changes in cells or organisms without requiring knowledge of the specific molecular target—toward a more precise paradigm focused on well-defined molecular targets [2] [9]. Target-based screening involves identifying compounds that interact with a specific molecular target, often a protein with a established role in the disease process [10]. The strategic dichotomy between these approaches has shaped modern pharmaceutical development, with each offering distinct advantages and limitations for drug discovery professionals.
The molecular biology revolution provided the essential tools for this transition, offering unprecedented insights into disease mechanisms at the molecular level. Advances in recombinant DNA technology, protein purification, high-resolution structural determination methods like X-ray crystallography and cryo-electron microscopy, and ultimately the sequencing of the human genome created a foundation for target-based drug discovery [2] [11]. These technologies enabled the identification and validation of specific proteins, receptors, and enzymes as potential therapeutic targets, ushering in an era of rational drug design that promised greater precision, efficiency, and mechanistic understanding compared to traditional phenotypic approaches [10].
Historical Context: From Phenotypic Screening to Targeted Approaches
The Traditional Dominance of Phenotypic Screening
Before the molecular biology revolution, drug discovery relied heavily on phenotypic screening, which contributed to the development of numerous first-in-class therapeutics [1]. This approach identified compounds based on functional biological effects in complex systems without requiring prior knowledge of specific molecular targets [9]. Notable successes included antibiotics like penicillin, anticancer agents, and immunosuppressants discovered by observing their effects on cells, tissues, or whole organisms [1] [9]. Between 1999 and 2008, phenotypic screening was responsible for 28 first-in-class small molecule drugs compared to 17 from target-based methods [1].
The Molecular Biology Revolution
The period from the 1970s to the early 2000s brought transformative technological advances that enabled the shift to target-based screening. Key developments included recombinant DNA technology (1970s), polymerase chain reaction (1980s), high-throughput sequencing (1990s), and the completion of the Human Genome Project (2003) [2]. These breakthroughs provided researchers with an unprecedented view of disease mechanisms at the molecular level, creating the foundation for target-based approaches by identifying thousands of potential therapeutic targets [12]. The parallel development of high-throughput screening technologies allowed rapid testing of compound libraries against these newly identified targets, further accelerating the adoption of target-based paradigms in pharmaceutical research and development [2].
Fundamental Principles of Target-Based Screening
Conceptual Framework
Target-based screening operates on a fundamentally different principle from phenotypic screening. While phenotypic approaches ask "Does this compound produce a beneficial biological effect?", target-based screening asks "Does this compound modulate my specific molecular target?" [9]. This hypothesis-driven approach begins with the selection and validation of a molecular target—typically a protein, enzyme, receptor, or nucleic acid—with a well-established role in the disease process [2]. The target-based paradigm relies on a deep understanding of disease biology, wherein specific molecular entities are identified as critical drivers of pathology, and therapeutic intervention is designed to modulate their activity in a precise manner [10].
The strategic workflow typically begins with target identification and validation, followed by assay development to measure target engagement or functional modulation, high-throughput screening of compound libraries, hit validation and optimization, and finally preclinical and clinical development [13]. This structured approach allows for systematic optimization of drug candidates based on their interactions with the defined molecular target, leveraging structural biology and computational modeling to refine compound properties [2] [12].
Key Technological Enablers
Several technological advances have been instrumental to the success of target-based screening:
- Structural Biology Tools: X-ray crystallography, cryo-electron microscopy (cryo-EM), and NMR spectroscopy provide high-resolution views of target structures, enabling structure-based drug design [2] [11].
- Computational Methods: Molecular docking, virtual screening, and molecular dynamics simulations allow in silico prediction of compound-target interactions [13] [12].
- High-Throughput Screening (HTS) Robotics: Automation systems enable testing of thousands to millions of compounds against targets in miniaturized formats [9].
- Bioinformatics and Omics Technologies: Genomic, proteomic, and chemoproteomic methods facilitate target identification, validation, and selectivity profiling [2] [14].
Figure 1: Target-Based Drug Discovery Workflow. This diagram illustrates the sequential stages of target-based screening, from initial target identification through to preclinical development.
Comparative Analysis: Success Rates and Strategic Value
Quantitative Assessment of Drug Discovery Outcomes
The debate between phenotypic and target-based screening approaches often centers on their relative success rates in producing new therapeutics. Comprehensive analyses of FDA-approved drugs reveal distinct patterns of success for each approach.
Table 1: Drug Discovery Approaches and Their Success Rates (1999-2017)
| Discovery Strategy | Number of Approved Drugs | First-in-Class Drugs | Key Strengths |
|---|---|---|---|
| Phenotypic Screening | 58 | 28 (1999-2008) | Identifies novel mechanisms; effective for complex diseases |
| Target-Based Screening | 44 | 17 (1999-2008) | Enables rational optimization; higher specificity |
| Monoclonal Antibodies | 29 | N/A | High specificity; favorable pharmacokinetics |
Data adapted from Ardigen analysis of FDA approvals (1999-2017) [1].
More recent data from 2012 to 2022 shows that the application of phenotypic screening in large pharmaceutical companies has grown to approximately 25-40% of project portfolios, reflecting a balanced approach that leverages the strengths of both strategies [1]. This suggests that while target-based approaches remain important, the drug discovery field has recognized the value of maintaining a diversified strategy.
Strategic Advantages of Target-Based Screening
Target-based screening offers several distinct advantages that have secured its position in modern drug discovery:
- Mechanistic Clarity: From the outset, researchers understand precisely how a compound is intended to work, enabling more informed optimization [10].
- High Specificity: Compounds can be designed or selected for precise interaction with the intended target, reducing off-target effects [10].
- Efficient Optimization: Structure-activity relationships (SAR) can be systematically explored using structural biology and computational modeling [2] [12].
- Personalized Medicine Potential: Targets can be selected based on genetic evidence in specific patient populations, enabling precision medicine approaches [10].
- Higher Throughput Capability: Target-based assays are often more amenable to miniaturization and automation than complex phenotypic systems [9].
The success of target-based screening is exemplified by drugs like imatinib (chronic myelogenous leukemia), trastuzumab (HER2-positive breast cancer), and HIV antiretroviral therapies including reverse transcriptase and integrase inhibitors [10]. These therapies were developed with precise knowledge of their molecular targets, enabling highly specific therapeutic interventions tailored to particular disease mechanisms.
Limitations and Challenges of Target-Based Approaches
Despite its advantages, target-based screening faces several significant challenges:
- Dependence on Target Validation: The approach is only as good as the underlying target hypothesis; incorrect validation leads to clinical failure [15] [10].
- Limited Novelty: The hypothesis-driven nature may limit discovery of truly novel mechanisms outside established biological understanding [9].
- Oversimplification of Biology: Single-target approaches may fail to address complex, multifactorial diseases with redundant pathways [2] [10].
- High Validation Costs: Extensive resources are required to establish robust causal links between targets and diseases [15].
These limitations are particularly evident in complex diseases like Alzheimer's, schizophrenia, and bipolar disorder, where target-based approaches have struggled despite significant investment [10]. The reductionist nature of targeting single proteins often fails to capture the systems-level complexity of many disease processes.
Table 2: Strategic Comparison of Screening Approaches
| Characteristic | Target-Based Screening | Phenotypic Screening |
|---|---|---|
| Discovery Bias | Hypothesis-driven; limited to known pathways | Unbiased; allows novel target identification |
| Mechanism of Action | Defined from outset | Often unknown at discovery; requires deconvolution |
| Throughput | Typically high | Variable; often medium throughput |
| Technical Requirements | Structural biology, computational modeling, enzyme assays | High-content imaging, functional genomics, AI analysis |
| Optimal Application | Well-validated targets with clear disease linkage | Complex diseases with poorly understood mechanisms |
Comparison based on characteristics described in Technology Networks analysis [9].
Experimental Approaches and Methodologies
Standard Protocols for Target-Based Screening
Target-based screening employs well-established experimental protocols that have been refined through decades of pharmaceutical research. A representative protocol for high-throughput target-based screening typically includes the following stages:
Phase 1: Target Production and Validation
- Clone, express, and purify the recombinant target protein
- Validate target functionality through biochemical and biophysical assays
- Determine optimal buffer conditions for stability and activity
Phase 2: Assay Development and Optimization
- Develop a robust assay measuring target engagement or functional modulation
- Optimize assay parameters (pH, ionic strength, temperature, incubation time)
- Establish controls and determine Z-factor for assay quality assessment
- Miniaturize and adapt assay to high-throughput format
Phase 3: Primary Screening
- Screen compound library (typically 10,000-1,000,000 compounds)
- Include appropriate controls on each plate (positive, negative, vehicle)
- Collect raw data and normalize to plate controls
- Apply statistical thresholds for hit identification (typically >3σ from mean)
Phase 4: Hit Confirmation and Validation
- Confirm hits in dose-response format
- Exclude promiscuous binders/aggregators through counter-screens
- Assess selectivity against related targets
- Validate binding through orthogonal methods (SPR, ITC, NMR)
This systematic approach ensures identification of high-quality starting points for medicinal chemistry optimization [13].
Advanced Methodologies: Structure-Based Drug Design
Structure-based drug design represents the cutting edge of target-based approaches, leveraging high-resolution structural information to guide compound optimization [12]. Recent advances include:
- AI-Powered Molecular Generation: Models like DiffGui use equivariant diffusion models to generate novel molecules with optimized binding affinity and drug-like properties directly within target binding pockets [12].
- Cryo-EM Applications: Single-particle cryo-electron microscopy enables structure determination of challenging targets like membrane proteins and large complexes [2] [11].
- AlphaFold Integration: Computationally predicted protein structures expand the target space accessible to structure-based approaches [11] [12].
- Free Energy Perturbation: Physics-based calculations provide accurate prediction of binding affinities for compound prioritization.
These methodologies enable increasingly sophisticated target-based discovery, reducing reliance on serendipity and enabling more rational drug design [12].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Implementation of target-based screening requires specialized reagents and platforms that have become essential tools in modern drug discovery.
Table 3: Essential Research Reagents for Target-Based Screening
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| ChEMBL Database | Curated bioactivity data; drug-target interactions | Target identification; chemogenomic analysis [11] |
| AlphaFold DB | Protein structure prediction | Structure-based design for targets without experimental structures [11] [12] |
| Molecular Docking Software | Predicts ligand binding poses and affinities | Virtual screening; binding mode analysis [13] [12] |
| Cryo-EM Platforms | High-resolution structure determination | Membrane proteins; large complexes [2] [11] |
| SPR/BLI Instruments | Label-free binding kinetics | Hit validation; affinity measurement [14] |
| Thermal Shift Assay Kits | Protein stability measurement | Target engagement; binding confirmation [14] |
| Compound Libraries | Diverse chemical collections | High-throughput screening [2] [13] |
These tools collectively enable the implementation of sophisticated target-based screening campaigns, providing the necessary infrastructure for modern drug discovery.
Integrated Approaches and Future Directions
Hybrid Strategies in Modern Drug Discovery
The historical dichotomy between phenotypic and target-based screening is increasingly giving way to integrated approaches that leverage the strengths of both paradigms [2]. Modern drug discovery often employs:
- Phenotypic Screening for Novel Target Discovery: Using phenotypic approaches to identify new biological mechanisms, followed by target deconvolution to identify the molecular targets [1] [9].
- Target-Based Optimization: Applying target-based approaches to optimize compounds identified through phenotypic screening [2].
- Chemical Biology Integration: Using target-agnostic compound profiling to elucidate mechanisms of action for phenotypic hits [15] [14].
These hybrid workflows create a virtuous cycle where phenotypic screening identifies novel biology and target-based approaches enable precise optimization of therapeutic candidates [2].
Figure 2: Integrated Drug Discovery Strategy. This diagram illustrates how modern drug discovery combines phenotypic and target-based approaches, leveraging the strengths of both paradigms.
Emerging Technologies and Future Outlook
The future of target-based screening will be shaped by several emerging technologies:
- Artificial Intelligence and Machine Learning: AI methods are enhancing target identification, compound design, and prediction of binding affinities [2] [12].
- Cryo-EM Advances: Improving resolution and throughput enables more targets to be accessible for structure-based design [2] [11].
- Chemical Proteomics: Methods like thermal proteome profiling (TPP) enable target deconvolution and identification of mechanism of action [14].
- Gene Editing Technologies: CRISPR-based approaches facilitate more physiologically relevant target validation in native cellular contexts [15].
These technologies are expanding the scope and success rate of target-based approaches, particularly for challenging target classes that were previously considered "undruggable."
The rise of target-based screening represents a definitive paradigm shift in pharmaceutical research, enabled by the molecular biology revolution. This approach has demonstrated significant strengths in enabling rational drug design, providing mechanistic clarity, and facilitating the development of targeted therapies for specific patient populations. The quantitative success of target-based approaches is evidenced by numerous approved therapies across therapeutic areas, particularly where disease mechanisms are well-understood.
However, the comparative analysis with phenotypic screening reveals a more nuanced picture—each approach possesses distinct advantages and optimal applications. Rather than a binary choice, modern drug discovery increasingly leverages both strategies in complementary workflows: phenotypic screening to identify novel biology and target-based approaches to optimize therapeutic candidates. This integrated model, enhanced by emerging technologies in AI, structural biology, and chemical proteomics, represents the future of pharmaceutical innovation, promising more effective and targeted therapies for complex diseases.
The strategic selection between phenotypic and target-based approaches ultimately depends on the specific biological context, disease complexity, and stage of therapeutic development, with the most successful drug discovery programs maintaining flexibility to leverage both paradigms as appropriate to their specific challenges and opportunities.
In the pursuit of new medicines, two distinct philosophical approaches have emerged: target-agnostic (phenotypic) discovery and hypothesis-driven (target-based) discovery. The target-agnostic strategy identifies drugs based on their observable effects on disease phenotypes—such as cell death or morphological changes—without prior knowledge of the specific molecular target [16] [1]. In contrast, the hypothesis-driven approach begins with a predefined molecular target, typically a protein understood to play a critical role in the disease mechanism, and seeks compounds that modulate its activity [10] [17]. Historically, many pioneering medicines were discovered through phenotypic observation. However, with the advent of molecular biology and genomics, the target-based paradigm became dominant for its precision and rational design [16]. A pivotal 2012 analysis revealing that a majority of first-in-class drugs from 1999-2008 originated from phenotypic approaches catalyzed a major resurgence in this methodology, establishing it as a systematic and complementary discovery route [16] [18]. This guide provides an objective comparison of these two philosophies, examining their success rates, experimental protocols, and practical applications for modern drug discovery.
Success Rates and Comparative Performance
Quantitative analyses of new drug approvals provide critical insight into the relative strengths of each discovery paradigm. The following table summarizes key performance metrics, particularly the ability to deliver innovative, first-in-class therapies.
Table 1: Comparative Success Rates of Discovery Philosophies for New Medicines (1999-2017)
| Discovery Philosophy | Total Drugs Approved (1999-2017) | First-in-Class Drugs (1999-2008) | Representative Approved Drugs |
|---|---|---|---|
| Target-Agnostic (Phenotypic) | 58 [1] | 28 (Majority) [16] [18] | Risdiplam, Daclatasvir, Ivacaftor/Lumacaftor, Vamorolone [16] [1] |
| Hypothesis-Driven (Target-Based) | 44 [1] | 17 [16] [18] | Imatinib, Trastuzumab, HIV Antiretroviral Therapies [10] |
| Monoclonal Antibody-Based | 29 [1] | N/A |
The data reveals a clear trend: phenotypic screening has been disproportionately successful in generating first-in-class medicines [16] [18]. This is largely attributed to its unbiased nature, which allows for the identification of novel mechanisms of action (MoA) and the expansion of "druggable" target space to include unexpected cellular processes and multi-target therapies (polypharmacology) [16]. For example, the cystic fibrosis therapy Ivacaftor and the spinal muscular atrophy treatment Risdiplam were both discovered without a pre-specified target hypothesis, revealing entirely new MoAs after their efficacy was established [16] [1].
The hypothesis-driven approach, while slightly less prolific in producing first-in-class drugs, excels in developing highly selective, optimized therapies, especially for diseases with well-understood molecular pathways. It provides a straightforward path for rational drug design and optimization once a validated target is available [10]. The development of Imatinib for chronic myeloid leukemia and trastuzumab for HER2-positive breast cancer are prime examples of this precision [10].
Experimental Protocols and Methodologies
The core philosophies necessitate distinct experimental workflows, from initial screening to lead optimization. The following diagrams and descriptions detail the standard protocols for each approach.
Target-Agnostic (Phenotypic) Screening Workflow
The phenotypic screening workflow is a cyclic process of testing and analysis centered on a biologically relevant disease model. The following diagram maps this multi-stage protocol.
Diagram 1: Phenotypic screening is an iterative process centered on a functional assay.
Detailed Experimental Protocols for Phenotypic Screening:
- Step 1: Compound Library Screening. A diverse library of compounds is screened against a disease-relevant biological system. This system can range from 2D cell cultures to more complex 3D organoids or even whole organisms [16] [1]. High-content screening (HCS) is often employed, which uses automated microscopy and image analysis to capture complex phenotypic data [1].
- Step 2: Hit Identification. "Hits" are identified based on their ability to induce a therapeutically desirable phenotypic change (e.g., reversal of a disease-associated morphology, inhibition of pathogen replication, or induction of cancer cell death) [10]. The specific molecular target responsible for this change remains unknown at this stage.
- Step 3: Hit Validation and Lead Optimization. Confirmed hits undergo further testing in secondary, more complex phenotypic assays to validate the biological effect. Medicinal chemistry is then used to improve the drug's properties (potency, selectivity, pharmacokinetics), guided primarily by the phenotypic readouts, not target binding [16].
- Step 4: Target Deconvolution. A critical and often challenging phase where the MoA of the optimized lead compound is investigated. Techniques such as chemical proteomics, resistance generation, and functional genomics (e.g., CRISPR screens) are used to identify the specific molecular target(s) engaged by the compound [16]. For some drugs, like lithium for bipolar disorder, the precise target may remain unknown even after approval [10].
Hypothesis-Driven (Target-Based) Screening Workflow
The target-based workflow is a linear, hypothesis-testing process that begins with a deep understanding of disease biology. The following diagram outlines its sequential stages.
Diagram 2: The hypothesis-driven process is a linear path from target validation to candidate.
Detailed Experimental Protocols for Target-Based Screening:
- Step 1: Target Identification and Validation. A specific molecular target (e.g., a kinase, receptor, or ion channel) is identified and rigorously validated as critical to the disease process. Techniques include genetic association studies, gene knockout/knockdown, and proteomic analyses [10] [17].
- Step 2: Assay Development. A robust in vitro assay is developed to measure compound activity against the purified target or a simplified cellular system. Examples include enzymatic activity assays, ligand-binding displacement assays (e.g., AlphaScreen), or cell-based reporter assays [10] [19].
- Step 3: High-Throughput Screening (HTS). The target-specific assay is automated and used to screen large compound libraries (often >1 million compounds) to identify "hits" that modulate the target's activity [10].
- Step 4: Hit-to-Lead and Lead Optimization. Confirmed hits are refined into lead compounds. The known target structure enables rational drug design using techniques like molecular docking and structure-activity relationship (SAR) analysis to systematically improve affinity, selectivity, and drug-like properties [7] [17]. Tools like CETSA (Cellular Thermal Shift Assay) are used to confirm target engagement in a cellular environment [7].
The Scientist's Toolkit: Essential Research Reagents and Solutions
The execution of both discovery philosophies relies on a suite of specialized tools and reagents. The following table catalogs key solutions used in the featured experiments and general workflows.
Table 2: Key Research Reagent Solutions for Discovery Philosophies
| Item / Solution | Function in Research | Primary Application |
|---|---|---|
| 3D Organoids / Complex Cell Models | Provides a human-relevant, physiologically complex disease model for phenotypic screening [5]. | Target-Agnostic |
| CETSA (Cellular Thermal Shift Assay) | Measures drug-target engagement directly in intact cells or tissues, confirming mechanistic action [7]. | Both (Validation) |
| Phage/Yeast Display Libraries | Genotype-phenotype coupled libraries for target-agnostic antibody discovery against complex antigen mixtures (e.g., cell surfaces) [20]. | Target-Agnostic |
| High-Content Screening (HCS) Systems | Automated imaging systems that extract multiparametric morphological data from cells for rich phenotypic profiling [1]. | Target-Agnostic |
| Recombinant Proteins | Isolated, purified target proteins used to develop specific biochemical assays for high-throughput screening [17]. | Hypothesis-Driven |
| Molecular Docking Software (e.g., Glide, AutoDock) | In silico tools for predicting how a small molecule binds to a protein target of known structure, guiding optimization [7] [17]. | Hypothesis-Driven |
| AlphaFold Protein Structure DB | AI-predicted protein structures provide 3D target models for rational design when experimental structures are unavailable [17]. | Hypothesis-Driven |
Strategic Application and Future Outlook
The choice between target-agnostic and hypothesis-driven philosophies is not a matter of superiority but strategic alignment with project goals and biological context.
Phenotypic screening is most advantageous when: the goal is to discover a first-in-class medicine with a novel mechanism of action, when the disease pathophysiology is complex or poorly understood (e.g., Alzheimer's disease, psychiatric disorders), or when pursuing polypharmacology (multi-target drugs) for complex diseases [16] [10]. Its main challenges are the complexity and cost of assays, and the difficult process of target deconvolution [16] [10].
Target-based screening is most advantageous when: a well-validated molecular target with a clear causal link to the disease exists, as seen in many cancers and genetic disorders. It is highly efficient, cost-effective for HTS, and simplifies lead optimization due to the known target [10] [17]. Its primary risk is clinical failure if the initial hypothesis about the target's role in the human disease is incorrect [10].
The future of drug discovery lies in the strategic integration of both approaches, powered by new technologies. Artificial Intelligence (AI) and Machine Learning (ML) are accelerating both paradigms—from analyzing high-content phenotypic images to predicting protein structures and generating novel hit molecules in silico [21] [1] [7]. Furthermore, advanced in vitro models like 3D organoids and organs-on-chips are providing more physiologically relevant systems for phenotypic screening, bridging the gap between traditional cell assays and clinical efficacy [5]. By understanding the core distinctions and complementary strengths of these two philosophies, researchers can more effectively navigate the path to breakthrough therapies.
The strategic choice between phenotypic drug discovery (PDD) and target-based drug discovery (TDD) represents a fundamental crossroads in pharmaceutical research. For decades, the pendulum has swung between these two approaches, heavily influenced by technological capabilities and prevailing scientific dogma. Historically, many medicines were discovered through observation of their effects on disease physiology, a form of phenotypic screening. With the advent of the molecular biology revolution in the 1980s and the sequencing of the human genome in 2001, the industry focus dramatically shifted to the powerful but reductionist approach of modulating specific molecular targets [16].
A pivotal 2008 analysis covering 1999-2008 revealed a surprising finding: the majority of first-in-class drugs were discovered empirically without a predefined drug target hypothesis [16]. This revelation, published in 2011, triggered a major resurgence of interest in phenotypic approaches. Since 2011, modern phenotypic drug discovery has re-emerged as a systematic pursuit of therapeutic effects in realistic disease models, combining the original concept with contemporary tools and strategies [16]. This guide quantifies the industry's adoption rates of these competing paradigms from 2012 to the present, examining the quantitative evidence behind this strategic shift.
Quantitative Analysis of Adoption Rates (2012-Present)
Industry-Wide Adoption Trends
Comprehensive analysis of pharmaceutical portfolios reveals a substantial increase in the adoption of phenotypic screening approaches over the past decade. The data demonstrates a consistent upward trajectory in PDD implementation across major research organizations.
Table 1: Industry Adoption Rates of Phenotypic Screening (2012-2022)
| Year | Adoption Rate (%) | Data Source | Key Influencing Factors |
|---|---|---|---|
| 2012 | <10% | Novartis Portfolio Analysis [1] | Post-genomic focus on validated targets |
| 2015 | ~25% | Novartis Portfolio Analysis [1] | Growing recognition of PDD success in first-in-class drugs |
| 2022 | 25-40% | AstraZeneca and Novartis Portfolio Analysis [1] | Accumulation of PDD successes; improved disease models |
The expansion of phenotypic approaches is particularly evident in specific therapeutic areas. Oncology and infectious diseases have led this adoption, followed closely by neuroscience and rare genetic disorders [16] [1]. The driving forces behind this shift include the remarkable track record of PDD in delivering first-in-class medicines and technological advancements that have made complex phenotypic assays more reproducible and scalable.
Success Rate Comparison: PDD vs. TDD
The quantitative superiority of phenotypic screening in generating innovative therapies provides the fundamental rationale for its renewed adoption. Multiple analyses of FDA-approved drugs consistently demonstrate PDD's disproportionate contribution to pioneering therapeutics.
Table 2: Success Rate Analysis of Discovery Approaches (1999-2017)
| Discovery Strategy | Number of Approved Drugs | First-in-Class Medicines | Notable Examples |
|---|---|---|---|
| Phenotypic Drug Discovery | 58 | 28 (Primary Source) | Risdiplam, Daclatasvir, Lumacaftor [1] |
| Target-Based Drug Discovery | 44 | 17 | Imatinib, Selective kinase inhibitors [16] |
| Monoclonal Antibody Therapies | 29 | N/A | Various biologic therapies [1] |
This success rate advantage is particularly pronounced for unprecedented mechanisms of action and historically "undruggable" targets. Between 1999 and 2008, PDD accounted for 28 first-in-class small molecule drugs compared to just 17 from target-based methods [16] [1]. This trend has continued in the subsequent decade, with PDD contributing transformative treatments for conditions including spinal muscular atrophy (risdiplam), cystic fibrosis (lumacaftor/ivacaftor), and hepatitis C (daclatasvir) [16] [1].
Experimental Protocols for Comparative Analysis
Methodologies for Quantifying Screening Outcomes
Robust experimental protocols are essential for objectively comparing the performance of phenotypic and target-based screening approaches. The following methodologies represent standardized frameworks employed in key studies cited within this analysis.
High-Content Phenotypic Screening Protocol
Objective: To identify compounds that produce a desired phenotypic change in disease-relevant cellular models without preconceived target hypotheses.
Workflow:
- Model System Selection: Utilize physiologically relevant cell types (primary cells, iPSC-derived cells, or engineered cell lines) expressing disease-associated phenotypes. 3D cultures, co-cultures, or organoids are increasingly employed for enhanced biological relevance [5].
- Assay Development: Implement multiplexed readouts capturing multiple phenotypic features simultaneously (morphology, proliferation, apoptosis, protein localization/organization).
- Compound Screening: Screen diverse chemical libraries (10,000-100,000 compounds) using automated liquid handling systems.
- Image Acquisition: Employ high-content imaging systems to capture multiparametric data.
- Data Analysis: Extract ~1,000 quantitative morphological features per cell using machine learning algorithms. Cluster phenotypes and identify hit compounds inducing desired phenotypic profiles [1].
Validation: Confirm hits in secondary assays using orthogonal detection methods and dose-response curves (10-point dilution series).
Target-Based Screening Validation Protocol
Objective: To identify compounds modulating a specific molecular target with known disease relevance.
Workflow:
- Target Selection: Prioritize targets with strong genetic validation (human genetics, functional genomics) and understood biological function.
- Assay Development: Implement biochemical or simple cellular assays measuring direct target engagement (binding assays, enzymatic activity inhibition/activation).
- Compound Screening: Screen focused chemical libraries enriched for target class expertise.
- Counter-Screening: Test against related targets to establish selectivity profile.
- Cellular Efficacy: Confirm functional activity in cellular models expressing the target.
Validation: Demonstrate direct target engagement using biophysical methods (SPR, ITC) and cellular target engagement assays (CETSA, NanoBRET).
Performance Metrics for Screening Approaches
Standardized metrics enable direct comparison between screening strategies. The following quantitative measures are essential for objective evaluation:
Table 3: Essential Performance Metrics for Screening Approaches
| Metric | Calculation | Interpretation |
|---|---|---|
| Hit Rate | (Confirmed Hits / Compounds Screened) × 100 | Screening efficiency; typically 0.1-1% for PDD vs 0.5-5% for TDD |
| Attrition Rate | (Candidates failing / Total candidates) × 100 | Predictive validity; TDD often shows higher late-stage attrition |
| Chemical Diversity | Scaffold clusters per 100 hits | Structural novelty; PDD typically identifies more diverse chemotypes |
| Success to Clinic | (Clinical candidates / Discovery programs) × 100 | Ultimate productivity measure |
Visualization of Screening Pathways and Outcomes
Comparative Success of Discovery Approaches
Modern Phenotypic Screening Workflow
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of phenotypic screening requires specialized reagents and tools that enable biologically relevant assay development and sophisticated readouts.
Table 4: Essential Research Reagents for Modern Phenotypic Screening
| Reagent Category | Specific Examples | Function in Screening |
|---|---|---|
| Advanced Cell Models | iPSC-derived cells, Primary organoids, 3D co-culture systems [5] | Provide human-relevant disease biology beyond transformed cell lines |
| Biosensors | GFP-tagged proteins, FRET reporters, Calcium flux indicators | Enable dynamic monitoring of pathway activation and cellular responses |
| Phenotypic Dyes | Mitochondrial membrane potential dyes, Cell viability indicators, Apoptosis markers | Facilitate multiparametric assessment of cell health and function |
| High-Content Imaging Reagents | Multiplexable fluorescent antibodies, Live-cell compatible dyes, Nuclear stains | Support automated extraction of morphological features |
| Pathway Reporters | Luciferase-based pathway assays, CRE-reporter systems, Promoter-specific constructs | Enable monitoring of specific signaling pathway modulation |
| Cytokine Panels | Multiplex cytokine arrays, Chemokine panels, Growth factor maps | Characterize immune and secretory responses in complex models |
The quantitative evidence from 2012 to present demonstrates a substantial and sustained shift toward phenotypic screening strategies within pharmaceutical R&D. The adoption rates of PDD have increased from less than 10% to 25-40% of project portfolios in leading organizations, driven by its demonstrated superiority in generating first-in-class therapies with novel mechanisms of action [1]. This trend reflects an evolving understanding of biological complexity and the limitations of exclusively reductionist approaches.
The integration of advanced disease models (organoids, 3D cultures), sophisticated detection methods (high-content imaging), and computational tools (machine learning, AI) has addressed historical limitations of phenotypic screening while preserving its fundamental advantage: the ability to discover therapeutics without predetermined target biases [16] [5] [1]. This technological convergence suggests that the observed adoption trends will not only continue but likely accelerate, particularly for diseases with complex biology and unmet medical needs.
The optimal discovery strategy increasingly appears to be a hybrid approach that leverages the target-agnostic innovation potential of phenotypic screening alongside the precision and efficiency of target-based methods once mechanisms are established. This integrated framework represents the future of therapeutic discovery—one that respects biological complexity while employing increasingly sophisticated tools to decipher and modulate it.
Strategic Implementation: When and How to Apply Phenotypic and Target-Based Methods
Phenotypic drug discovery (PDD) has undergone a significant resurgence over the past decade, reclaiming its position as a powerful approach for identifying first-in-class therapies. This renewed interest follows a systematic analysis revealing that between 1999 and 2008, 28 first-in-class small molecule drugs were discovered through phenotypic methods compared to 17 from target-based approaches [1]. Modern PDD combines the original concept of observing therapeutic effects on disease physiology with advanced tools and strategies, enabling systematic drug discovery based on therapeutic effects in biologically relevant disease models [16]. Unlike target-based drug discovery (TDD), which relies on modulation of specific molecular targets with established causal relationships to disease, PDD operates in a target-agnostic fashion, focusing on measurable changes in disease phenotypes or biomarkers without requiring prior knowledge of the underlying molecular mechanism [2] [16]. This fundamental difference allows phenotypic screening to expand the "druggable target space" to include unexpected cellular processes and novel mechanisms of action that might otherwise remain undiscovered [16].
The strategic value of PDD lies in its ability to capture the complexity of biological systems and identify therapeutic interventions that address multifaceted disease mechanisms. As a result, pharmaceutical companies have dramatically increased their implementation of phenotypic screens, with estimates suggesting they now constitute 25-40% of the project portfolio of major pharmaceutical companies such as AstraZeneca and Novartis [1]. This strategic shift is powered by advancements in disease modeling, high-content imaging technologies, and computational analysis methods that have addressed historical challenges associated with phenotypic approaches.
Table 1: Comparative Analysis of Drug Discovery Approaches
| Parameter | Phenotypic Drug Discovery (PDD) | Target-Based Drug Discovery (TDD) |
|---|---|---|
| Fundamental Approach | Focus on observable traits/phenotypes in response to treatment [22] | Focus on modulation of specific, pre-validated molecular targets [2] |
| Target Requirement | No prior knowledge of molecular target required [1] | Well-characterized molecular target essential [2] |
| System Complexity | Uses complex biological systems (cells, tissues, organisms) [2] | Typically reductionist systems (purified proteins, simple cellular assays) [2] |
| Success Rate (First-in-Class) | 28 drugs (1999-2008) [1] | 17 drugs (1999-2008) [1] |
| Key Advantage | Identifies novel mechanisms; captures system complexity [16] | Enables rational drug design; typically faster timeline [2] |
| Primary Challenge | Target deconvolution; complex data interpretation [2] | Limited to known biology; may miss complex interactions [2] |
Technological Foundations of Modern Phenotypic Screening
High-Content Imaging and Analysis
High-content screening (HCS) represents the technological backbone of modern phenotypic discovery, using automated microscopy to generate rich, high-dimensional datasets that capture diverse cellular phenotypes. The Cell Painting protocol has emerged as a particularly powerful and widely adopted HCS method, using six fluorescent dyes imaged across five channels to examine multiple cellular components and organelles simultaneously: nuclei (Hoechst 33342), endoplasmic reticulum (concanavalin A–AlexaFluor 488), mitochondria (MitoTracker Deep Red), F-actin (phalloidin–AlexaFluor 568), Golgi apparatus and plasma membranes (wheat germ agglutinin–AlexaFluor 594), and nucleoli/cytoplasmic RNA (SYTO14) [23]. This comprehensive labeling strategy enables the extraction of hundreds of morphological features—including texture, shape, intensity, and spatial relationships—creating detailed phenotypic profiles that characterize cytological responses to chemical or genetic perturbations [24] [23].
Advanced statistical frameworks are essential for interpreting the complex data generated by HCS. Traditional analysis methods that aggregate cellular data into summary statistics (e.g., means, medians, Z-scores) often fail to capture important biological information, particularly when treatments create subpopulations of cells with different responses [24]. Modern analytical approaches instead utilize cell-level feature distributions and advanced metrics like the Wasserstein distance to detect subtle phenotypic changes that would be masked by well-averaged measures [24]. These methods can identify diverse response patterns, including global shifts in cellular feature distributions, stretching of distribution tails, or the emergence of bimodal distributions indicating heterogeneous cell responses [24]. The analytical workflow typically includes quality control measures, positional effect adjustment, data standardization, feature reduction, and phenotypic profiling to ensure robust and interpretable results [24].
Advanced Disease Models for Phenotypic Screening
The translational relevance of phenotypic screens depends heavily on the biological fidelity of the model systems employed. While traditional immortalized cell lines remain useful for certain applications, the field has increasingly shifted toward more human-relevant models that better recapitulate disease physiology [25]. Key advancements in this area include:
Patient-Derived Organoids: Self-organizing 3D structures that mimic key aspects of native tissues, derived directly from patient samples. These models preserve disease-specific characteristics and have been successfully used for phenotypic screening in cancer, inflammatory, and genetic diseases [25] [23].
Induced Pluripotent Stem Cell (iPSC) Systems: Reprogrammed adult cells that can be differentiated into various cell types, enabling disease modeling and compound screening in otherwise inaccessible human cell types, such as neurons or cardiomyocytes [25].
Complex Co-Culture Systems: Models incorporating multiple cell types to better mimic tissue microenvironment and cell-cell interactions, particularly valuable for immuno-oncology and inflammation research [23].
The industrialization of these complex biological models through automated cell culture systems (e.g., CellXpress.ai) has been crucial for enabling their use in early drug discovery, providing the reproducibility and scalability necessary for high-throughput phenotypic screening [25].
Innovative Methodologies: Compressed and Pooled Screening Approaches
Traditional phenotypic screens face significant scalability challenges when using high-content readouts and complex disease models due to resource constraints. Compressed screening has emerged as an innovative solution to this limitation, enabling researchers to pool multiple perturbations together while still deconvolving individual compound effects through computational methods [23]. This approach dramatically reduces the sample number, cost, and labor requirements—by a factor of P (pool size)—while maintaining the ability to identify bioactive compounds [23].
The fundamental principle behind compressed screening involves combining N perturbations into unique pools of size P, with each perturbation appearing in R distinct pools overall [23]. Following experimental execution, a computational framework based on regularized linear regression and permutation testing deconvolves the effects of individual perturbations from the pooled results [23]. Benchmarking studies using a 316-compound FDA drug repurposing library and Cell Painting readout have demonstrated that compressed screening can reliably identify compounds with the largest effects even at high compression levels (up to 80 drugs per pool) [23]. This approach has been successfully applied to map transcriptional responses to tumor microenvironment protein ligands in pancreatic cancer organoids and to identify immunomodulatory compounds in primary human peripheral blood mononuclear cells (PBMCs) [23].
Table 2: Experimental Protocol for High-Content Phenotypic Screening
| Experimental Stage | Key Procedures | Technical Considerations |
|---|---|---|
| Assay Development | - Cell model selection & validation- Marker panel design- Staining optimization- Image acquisition parameter optimization | - Ensure disease relevance- Minimize fluorescence bleed-through- Balance complexity with practicality- Include relevant positive/negative controls [24] |
| Screening Execution | - Compound/library application- Incubation period determination- Fixation/staining- Automated image acquisition | - Address positional effects through plate design- Include adequate controls across plates- Standardize incubation conditions- Implement quality control checkpoints [24] [23] |
| Image Analysis | - Illumination correction- Cell segmentation- Feature extraction- Data normalization | - Use appropriate segmentation algorithms- Extract comprehensive feature sets- Account for technical variability- Apply batch effect correction [24] |
| Data Processing | - Positional effect adjustment- Cell-level data standardization- Feature selection & reduction- Phenotypic profile generation | - Use methods like median polish for positional effects- Employ distribution-based statistics- Select most informative features- Create phenotypic fingerprints [24] |
| Hit Identification | - Multivariate distance calculation- Phenotypic clustering- Dose-response analysis- Hit confirmation | - Use Mahalanobis Distance for effect size- Identify phenotypic clusters- Validate through dose-response- Confirm in secondary assays [23] |
Success Stories: Therapeutic Breakthroughs from Phenotypic Screening
Phenotypic screening has generated numerous therapeutic breakthroughs across diverse disease areas, particularly for conditions with complex or poorly understood pathophysiology. These successes highlight the power of phenotypic approaches to identify novel mechanisms and first-in-class medicines:
Spinal Muscular Atrophy (SMA): Risdiplam (Evrysdi) was discovered through phenotypic screening that identified small molecules modulating SMN2 pre-mRNA splicing to increase levels of functional SMN protein [1] [16]. This unprecedented mechanism of action—stabilizing the U1 snRNP complex to promote inclusion of exon 7—would have been unlikely discovered through target-based approaches, as SMN2 lacked known functional activity and would not have been selected as a target in traditional campaigns [1] [16]. Approved in 2020, risdiplam represents the first oral disease-modifying therapy for SMA.
Cystic Fibrosis (CF): Ivacaftor, lumacaftor, tezacaftor, and elexacaftor were all identified through phenotypic screens using cell lines expressing wild-type or disease-associated CFTR variants [1] [16]. These compounds work through distinct mechanisms—ivacaftor acts as a "potentiator" that improves CFTR channel gating, while the "correctors" enhance CFTR folding and plasma membrane insertion [16]. The combination of elexacaftor, tezacaftor, and ivacaftor (Trikafta) addresses 90% of the CF patient population and represents a transformative therapy for this previously fatal genetic disease [16].
Hepatitis C Virus (HCV): Daclatasvir (Daklinza) was identified through a HCV replicon phenotypic screen and later found to target NS5A, a viral protein with no enzymatic activity that is essential for HCV replication [1] [16]. As a protein with no known enzymatic function and an incompletely understood mechanism, NS5A remained an elusive target for traditional drug discovery approaches [1]. Daclatasvir became the first in the class of NS5A inhibitors and a key component of curative DAA combinations for HCV [16].
Oncology: Thalidomide and its analogs (lenalidomide, pomalidomide) were discovered and optimized exclusively through phenotypic screening [2]. Their molecular target (cereblon) and mechanism of action (altering substrate specificity of the CRL4 E3 ubiquitin ligase complex) were only elucidated years after clinical approval [2] [16]. This novel mechanism is now being intensively explored in targeted protein degradation strategies, including PROTACs, representing one of the most exciting new modalities in drug discovery [2].
The Scientist's Toolkit: Essential Research Reagents and Technologies
Successful implementation of phenotypic screening workflows requires careful selection and optimization of research reagents and technologies. The following table outlines key solutions and their applications in modern phenotypic screening:
Table 3: Research Reagent Solutions for Phenotypic Screening
| Reagent/Technology | Primary Function | Application Notes | |
|---|---|---|---|
| Cell Painting Assay | Comprehensive morphological profiling using 6 fluorescent dyes [23] | - Standardized protocol enables cross-study comparisons- Captures ~1,000+ morphological features- Compatible with automated image analysis pipelines | |
| CETSA (Cellular Thermal Shift Assay) | Validation of target engagement in intact cells and tissues [7] | - Confirms direct binding in physiological environments- Useful for mechanism of action studies | - Compatible with high-resolution mass spectrometry |
| CRISPR Screening | Functional genomics for target identification and validation [6] | - Systematically investigates gene-drug interactions- Can be combined with phenotypic readouts (Perturb-seq)- Enables identification of resistance mechanisms | |
| Advanced Disease Models | Physiologically relevant screening systems [25] | - Patient-derived organoids maintain disease characteristics- iPSC systems enable human cell type screening- Co-culture models incorporate microenvironment interactions | |
| Automated Cell Culture Systems | Industrialized production of complex biological models [25] | - Enables scalable production of organoids and iPSCs- Improves reproducibility and standardization- Reduces manual labor and increases capacity | |
| AI/ML Analysis Platforms | High-dimensional data analysis and pattern recognition [22] [1] | - Identifies subtle phenotypic patterns | - Enables mechanism of action prediction- Accelerates hit identification and prioritization |
The evolution of phenotypic screening from a serendipity-dependent process to a systematic discovery engine represents a fundamental shift in drug discovery philosophy. Rather than positioning phenotypic and target-based approaches as competing strategies, the most productive path forward involves integrating both paradigms to leverage their complementary strengths [2]. Modern drug discovery pipelines increasingly employ hybrid workflows that use phenotypic screening for novel target and mechanism identification, followed by target-based approaches for lead optimization and mechanistic characterization [2].
This integration is being accelerated by advancements in artificial intelligence, multi-omics technologies, and functional genomics that bridge the historical gap between phenotypic observations and molecular mechanisms [2]. AI and machine learning play particularly important roles in parsing complex, high-dimensional phenotypic datasets and identifying predictive patterns that link morphological profiles to biological mechanisms [22] [1]. Furthermore, innovations in target deconvolution methods, including chemical proteomics, functional genomics, and bioinformatics, have dramatically improved our ability to identify the molecular mechanisms underlying phenotypic hits [2] [16].
As these trends continue, phenotypic screening will likely become increasingly central to drug discovery efforts, particularly for complex diseases where single-target approaches have shown limited success. The ongoing development of more physiologically relevant models, higher-content readouts, and more sophisticated analytical approaches will further enhance the predictive value and productivity of phenotypic screening, cementing its role as an indispensable tool for discovering the next generation of transformative medicines.
In modern drug discovery, two primary screening strategies are employed: target-based screening and phenotypic screening. Target-based screening begins with a specific, well-characterized molecular target—often a protein, enzyme, or receptor with a established role in disease pathology. This approach uses high-throughput technologies to identify compounds that interact with this predefined target, enabling rational drug design based on detailed knowledge of the target's structure and function [2] [10]. In contrast, phenotypic screening takes a more holistic approach by identifying compounds based on their measurable effects on cells, tissues, or whole organisms without requiring prior knowledge of the specific molecular mechanism of action [2]. This method captures the complexity of biological systems and has been instrumental in discovering first-in-class therapies, particularly for diseases with poorly understood underlying mechanisms [2] [10].
The strategic choice between these approaches has significant implications for drug discovery success rates, resource allocation, and eventual clinical outcomes. Target-based screening has gained substantial prominence within the pharmaceutical industry, supported by advances in automation, bioinformatics, and structural biology. The global market for high-throughput screening (HTS), which is predominantly target-based, is experiencing robust growth—projected to increase from USD 32.0 billion in 2025 to USD 82.9 billion by 2035, registering a compound annual growth rate (CAGR) of 10.0% [26]. Another analysis predicts the HTS market will reach USD 18.8 billion by 2029, expanding at a CAGR of 10.6% [27]. This growth is largely driven by rising research and development investments in pharmaceuticals and biotechnology, along with continuous technological innovations in automation and analytical capabilities [26] [27].
Table 1: Comparison of Screening Approaches in Drug Discovery
| Feature | Target-Based Screening | Phenotypic Screening |
|---|---|---|
| Starting Point | Defined molecular target [2] | Observable biological effect [2] |
| Throughput | Typically high [10] | Variable, often lower [10] |
| Mechanism Understanding | Known from outset [2] | Requires target deconvolution [2] |
| Key Advantage | Precision and rational design [10] | Captures biological complexity [2] [10] |
| Key Challenge | Relies on validated targets [2] | Resource-intensive and slower [10] |
| Notable Drug Examples | Imatinib, Trastuzumab [10] | Artemisinin, Lithium [10] |
Market Landscape and Adoption Trends
The adoption of target-based screening platforms continues to accelerate across the pharmaceutical and biotechnology sectors. Within the technology segment of the high-throughput screening market, cell-based assays currently dominate with a 39.40% share [26]. These assays provide physiologically relevant data and predictive accuracy in early drug discovery by allowing direct assessment of compound effects in biological systems [26]. However, ultra-high-throughput screening (uHTS) technology is anticipated to expand at a faster CAGR of 12% through 2035 [26]. This growth is fueled by uHTS's unprecedented ability to screen millions of compounds rapidly, enabling comprehensive exploration of chemical space and enhancing the probability of identifying novel therapeutic candidates [26].
The application of high-throughput screening for target identification represents another rapidly growing segment, projected to register a 12% CAGR from 2025 to 2035 [26]. This application is crucial for swiftly evaluating large chemical libraries against diverse biological targets, thereby accelerating the drug development process by identifying promising therapeutic candidates with high specificity and efficacy [26]. Technological advancements in automation and robotics have significantly improved the efficiency and throughput of these screening platforms, establishing them as indispensable tools for target identification in modern drug discovery [26].
Table 2: High-Throughput Screening Market Outlook by Application (2025-2035)
| Application Segment | Market Share (2025) | Projected CAGR | Primary Drivers |
|---|---|---|---|
| Primary Screening | 42.70% [26] | -- | Essential role in identifying active compounds from large libraries [26] |
| Target Identification | Significant segment [26] | 12% [26] | Ability to rapidly assess chemical libraries against multiple biological targets [26] |
| Toxicology | -- | -- | Increasing demand for early toxicity testing [26] |
From a geographical perspective, North America dominates the high-throughput screening market, accounting for approximately 50% of global market share [26] [27]. This leadership position is attributed to several factors including a strong biotechnology startup ecosystem, significant government investment in drug research, a robust biopharmaceutical industry, and heightened focus on addressing unmet medical needs [26]. The United States high throughput screening ecosystem specifically is anticipated to grow at a CAGR of 12.6% through 2035 [26]. Meanwhile, the Asia-Pacific region is emerging as the fastest-growing market, driven by increasing digital technology adoption by pharmaceutical companies and expanding collaborations with contract research organizations (CROs) [28] [29].
Technological Framework of Target-Based Screening
Core Components and Workflow
Target-based screening platforms integrate multiple advanced technologies to enable efficient drug discovery. The foundational infrastructure typically includes robotic automation systems for liquid handling and assay execution, microplate readers for absorbance and luminescence detection, and sophisticated data acquisition systems for processing large datasets [27]. These components work in concert to facilitate the screening of thousands to millions of compounds against specific biological targets in remarkably short timeframes. A key technological advancement has been assay miniaturization, implemented through multiplex assays and plate replication, which dramatically boosts productivity while reducing the time and cost associated with compound library screening [27].
The integration of artificial intelligence (AI) and machine learning (ML) has revolutionized target-based screening platforms. AI/ML-based drug discovery solutions currently represent the largest segment within the drug discovery SaaS platforms market, holding a 30% revenue share [28] [29]. These technologies enhance screening efficiency and precision by enabling more accurate analysis of large datasets, predicting compound behavior, and optimizing trial design [28]. The adoption of AI-driven platforms is particularly prominent in pharmaceutical companies, which account for 55% of the end-user market for drug discovery SaaS platforms [28] [29].
Experimental Protocols and Methodologies
A representative example of a target-based screening protocol comes from recent glioblastoma (GBM) research, which utilized a kinase inhibitor library to identify subtype-specific therapeutic vulnerabilities [30]. This study established a robust high-throughput screening assay using lineage-based GBM models to identify both common and subtype-specific small molecule inhibitors.
Experimental Workflow for Kinase Inhibitor Screening [30]:
- Cell Culture Preparation: Primary mouse GBM Type 1 and Type 2 cells were maintained in DMEM/F12 serum-free medium supplemented with B27 and N2, plus specific growth factors (EGF, Nrg1, and PDGF-AA).
- Assay Optimization: Parameters including cell density (500 cells/well), medium volume (40 μL/well), and incubation time (5 days post-treatment) were systematically optimized in 384-well plate formats to achieve high signal-to-noise ratios.
- Screening Execution: A kinase inhibitor library containing 900 compounds was screened in parallel against both GBM subtypes using CellTiter-Glo luminescent assay to measure intracellular ATP levels as a surrogate for cellular viability.
- Data Analysis: Hit selection was performed based on viability reduction compared to controls, with identification of common inhibitors (84 compounds), Type 1-specific inhibitors (11 compounds), and Type 2-specific inhibitors (18 compounds).
- Validation: Candidate compounds underwent confirmation screens and dose-response assays (IC50 determination) to verify subtype-specific activity.
This methodology successfully identified R406 and Ponatinib as selective inhibitors of Type 2 GBM cells, and further demonstrated synergistic effects between R406 and Tucatinib in Type 2 cells, providing a rationale for combination therapy approaches [30].
Comparative Performance Analysis
Success Rates and Efficiency Metrics
Target-based screening platforms demonstrate distinct advantages in throughput and efficiency compared to phenotypic approaches. Studies indicate that high-throughput screening can improve hit identification rates by up to 5-fold compared to traditional methods [27]. The implementation of ultra-high-throughput screening technologies has further enhanced capacity, with some platforms capable of screening 10,000 times faster than conventional techniques [27]. This dramatic improvement in efficiency translates to significant cost reductions, with reports indicating that HTS can lower operational costs by approximately 15% while improving forecast accuracy by about 20% [27].
The application of target-based screening in oncology drug discovery has been particularly productive. Currently, the oncology segment holds a 35% share of the drug discovery SaaS platforms market by therapeutic area [28] [29]. The dominance of this segment is largely attributable to the precision offered by target-based approaches, which enable researchers to identify novel oncogenic targets and design personalized treatment strategies through computational oncology tools [28]. This targeted approach has accelerated the discovery of immunotherapies and precision drugs, particularly for rare cancers with defined molecular drivers [28].
Table 3: Quantitative Performance Metrics of Target-Based Screening Platforms
| Performance Metric | Target-Based Screening | Industry Impact |
|---|---|---|
| Hit Identification Rate | Up to 5-fold improvement [27] | Faster lead candidate identification |
| Screening Throughput | 10,000x faster than traditional methods [27] | Rapid compound library screening |
| Operational Cost Reduction | ~15% [27] | More efficient resource allocation |
| Development Timeline Reduction | ~30% [27] | Accelerated time to market |
| Forecast Accuracy Improvement | ~20% [27] | Better pipeline planning |
Integration with Computational Approaches
The convergence of target-based screening with advanced computational methods has created powerful hybrid approaches for drug discovery. Bioinformatics and computational chemistry techniques now enable researchers to efficiently identify key molecular targets and screen potential compounds with high binding affinities [31]. Molecular docking simulations and molecular dynamics (MD) analyses provide critical insights into binding stability between compounds and protein targets, facilitating rational drug design [31].
A recent study demonstrating this integrated approach identified the adenosine A1 receptor as a key therapeutic target for breast cancer treatment [31]. Researchers employed pharmacophore modeling based on binding information to guide virtual screening of compounds, which led to the rational design and synthesis of a novel molecule (Molecule 10). This compound exhibited potent antitumor activity against MCF-7 breast cancer cells with an IC50 value of 0.032 µM, significantly outperforming the positive control 5-FU (IC50 = 0.45 µM) [31]. This case exemplifies how computational approaches enhance the precision and success rates of target-based screening platforms.
Essential Research Reagent Solutions
The implementation of successful target-based screening campaigns requires carefully selected reagents and specialized materials. The following table details key research reagent solutions essential for establishing robust screening platforms:
Table 4: Essential Research Reagents for Target-Based Screening Platforms
| Reagent/Material | Function | Application Example |
|---|---|---|
| Cell-Based Assay Kits | Deliver physiologically relevant data and predictive accuracy [26] | Assessment of compound effects in biological systems [26] |
| Kinase Inhibitor Libraries | Curated collections targeting key regulatory protein families [30] | Identification of subtype-specific therapeutic vulnerabilities [30] |
| Cell Viability Assay Reagents | Measure intracellular ATP as surrogate for viability [30] | Primary screening readout for compound efficacy [30] |
| Specialized Cell Culture Media | Support specific cell types with necessary growth factors [30] | Maintain relevant cellular models for screening [30] |
| Molecular Docking Software | Computational prediction of compound-target interactions [31] | Virtual screening and binding affinity assessment [31] |
| Microplates (384-well format) | Enable assay miniaturization and high-throughput processing [30] | Platform for screening large compound libraries [30] |
The reagents and kits segment currently holds a leading position in the high-throughput screening products and services category, accounting for 36.50% of market share [26]. This dominance reflects the critical role of high-quality consumables in ensuring reproducibility and accuracy in screening workflows. Manufacturers have focused on developing specialized reagent formulations optimized for specific assay platforms, supporting broader application compatibility and simplifying operations through ready-to-use assay kits that reduce setup time for laboratories [26].
Future Directions and Strategic Implications
The evolution of target-based screening platforms continues to be shaped by several converging technological trends. The integration of artificial intelligence and machine learning is expected to deepen, with AI/ML-based drug discovery platforms revolutionizing early-stage R&D by improving lead identification, molecular screening, and target validation [28]. These tools significantly reduce time-to-market by predicting compound behavior and optimizing trial design, making them increasingly indispensable for pharmaceutical firms focused on personalized medicine and drug repurposing [28].
Another significant trend is the shift toward cloud-based SaaS platforms, which currently represent 75% of the deployment mode for drug discovery solutions [28] [29]. These platforms provide scalable, cost-efficient access to advanced computational resources without requiring substantial infrastructure investment, thereby democratizing access to sophisticated screening tools for smaller research institutions and biotech startups [28]. The hybrid deployment segment, however, is anticipated to register the fastest growth over the forecast period (2025-2035), as it offers a balance between cloud flexibility and on-premise control for organizations handling sensitive clinical or genomic data [28] [29].
The strategic integration of target-based and phenotypic screening approaches represents the most promising future direction. As noted in recent research, "hybrid discovery workflows that integrate high-throughput screening, structural biology, and computational modeling" are becoming increasingly essential for addressing complex biological challenges [2]. This convergence enables researchers to leverage the precision of target-based methods while maintaining the biological relevance and serendipitous discovery potential of phenotypic approaches [2] [10]. As these platforms continue to evolve, they will undoubtedly reshape the drug discovery landscape, offering more efficient, cost-effective, and targeted pathways to novel therapeutics for diverse disease areas.
The strategic choice between phenotypic and target-based drug discovery is one of the most fundamental decisions in pharmaceutical research and development. These two approaches represent distinct philosophies: one starting with biological function and the other with molecular mechanism. Historical analysis reveals that phenotypic screening has been disproportionately successful for discovering first-in-class medicines, while target-based screening has excelled at developing best-in-class drugs that optimize known mechanisms [18] [32]. This guide provides an objective comparison of these approaches, supported by experimental data and methodological protocols, to help researchers match their strategy to their specific drug discovery goals.
Phenotypic Drug Discovery (PDD) involves testing compounds in biologically relevant model systems—such as cells, tissues, or whole organisms—and selecting hits based on their ability to modulate disease-relevant phenotypes without prior knowledge of the specific molecular target [16] [2]. This approach captures the complexity of biological systems and has expanded the "druggable target space" to include unexpected cellular processes and novel mechanisms of action [16].
Target-Based Drug Discovery (TDD) begins with a predefined molecular target that has been rigorously validated for its role in disease pathogenesis [2] [10]. This hypothesis-driven approach leverages advances in structural biology, genomics, and computational modeling to guide rational therapeutic design with precise target engagement [2].
Table 1: Fundamental Characteristics of Discovery Approaches
| Characteristic | Phenotypic Screening | Target-Based Screening |
|---|---|---|
| Starting Point | Disease-relevant biological system | Predefined molecular target |
| Knowledge Requirement | No target hypothesis needed | Requires validated target & mechanism |
| Throughput | Generally lower, more complex assays | Generally higher, simplified assay systems |
| Target Deconvolution | Required after hit identification | Known from outset |
| Chemical Optimization | Challenging without known mechanism | Straightforward with structural knowledge |
Success Rates and Comparative Performance Data
First-in-Class Medicine Discovery
Multiple analyses of FDA-approved drugs demonstrate a clear pattern in the origins of innovative therapeutics. Between 1999 and 2008, phenotypic screening was responsible for the discovery of 28 first-in-class small molecule drugs, compared to 17 from target-based methods [1]. This trend continued through 2017, with PDD contributing to 58 out of 171 total approved drugs, while traditional TDD accounted for 44 approvals [1].
The superiority of phenotypic approaches for first-in-class discovery is attributed to its unbiased nature, which allows identification of therapeutic interventions for novel and diverse targets [1]. Unlike target-based discovery, which typically focuses on enzymes and receptors, phenotypic approaches can reveal therapeutic routes acting via membranes, ion channels, ribosomes, microtubules, or large complex molecular structures like ATP synthase [1].
Approval Rates and Clinical Success
An analysis of discovery strategies and their outcomes reveals distinct success patterns:
Table 2: Success Rates by Discovery Approach
| Discovery Approach | First-in-Class Success Rate | Best-in-Class Success Rate | Notable Examples |
|---|---|---|---|
| Phenotypic Screening | Higher for novel mechanisms [18] | Lower | Risdiplam, Ivacaftor, Daclatasvir [16] [1] |
| Target-Based Screening | Lower | Higher for optimized therapies [32] | Imatinib, Trastuzumab, HIV antiretrovirals [10] |
| Hybrid Approaches | Emerging promise | Strong optimization potential | Immune checkpoint inhibitors [2] |
Target-based approaches face significant attrition due to lack of efficacy, often stemming from flawed target hypotheses or incomplete understanding of compensatory mechanisms [2]. Despite rational design against "well-validated" targets, many candidates fail in clinical trials due to the limitations of single-target approaches in addressing complex cellular signaling networks and adaptive resistance mechanisms [2].
Experimental Protocols and Methodologies
Phenotypic Screening Workflow
Modern phenotypic drug discovery employs sophisticated disease models and high-content readouts to identify compounds with therapeutic potential:
Protocol 1: High-Content Phenotypic Screening for Drug Discovery
Disease Model Establishment:
Compound Library Preparation:
- Curate diverse chemical libraries (10,000-100,000 compounds)
- Include known bioactive compounds for reference
- Format compounds in DMSO stocks at standardized concentrations
Automated Screening:
- Dispense cells and compounds using liquid handlers
- Incubate for predetermined time (24-72 hours typical)
- Include controls (vehicle, positive/negative controls) on each plate
High-Content Analysis:
- Fix and stain for relevant markers (cell viability, morphology, functional markers)
- Acquire images using automated microscopy
- Extract quantitative features using image analysis software
- Apply machine learning algorithms for phenotype classification [1]
Hit Validation:
- Confirm activity in dose-response (8-point curves recommended)
- Assess selectivity in counter-screens
- Evaluate chemical tractability and properties
Figure 1: Phenotypic Screening Workflow. This diagram illustrates the multi-stage process of phenotypic drug discovery, from model establishment to candidate selection.
Target-Based Screening Workflow
Target-based screening employs precise molecular assays to identify compounds that modulate specific targets:
Protocol 2: Target-Based High-Throughput Screening
Target Validation and Protein Production:
- Select molecular target with strong genetic/functional validation
- Express and purify recombinant protein (≥95% purity)
- Confirm structural integrity and functional activity
Assay Development and Optimization:
- Establish biochemical or biophysical assay (FRET, FP, TR-FRET, SPR)
- Optimize buffer conditions, substrate concentrations, and detection parameters
- Determine Z' factor (>0.5 required for HTS)
- Implement appropriate controls and reference compounds
High-Throughput Screening:
- Screen compound libraries (100,000-1,000,000 compounds)
- Use automation for compound transfer and assay readout
- Include quality control plates throughout screening run
Hit Identification and Confirmation:
- Apply statistical cutoff (typically mean ± 3SD of controls)
- Confirm hits in dose-response assays
- Eliminate promiscuous binders and assay artifacts
- Assess selectivity against related targets
Structural Biology and Optimization:
- Determine co-crystal structures of target-hit complexes
- Use structure-based drug design for optimization
- Evaluate cellular activity and target engagement
Figure 2: Target-Based Screening Workflow. This diagram shows the systematic process of target-based drug discovery, from target selection to candidate identification.
Target Deconvolution Methods
A critical challenge in phenotypic screening is identifying the molecular mechanism of action of hit compounds:
Protocol 3: Target Deconvolution for Phenotypic Hits
Affinity Chromatography:
- Immobilize compound of interest on solid support
- Incubate with cell lysates or tissue extracts
- Wash away non-specific binders
- Elute and identify bound proteins via mass spectrometry
Expression Cloning:
- Transfect cells with cDNA libraries
- Select for resistance to compound effect
- Identify rescuing cDNA through sequencing
Functional Genomics Approaches:
- Perform genome-wide CRISPR-Cas9 or RNAi screens
- Identify genetic modifiers of compound sensitivity
- Validate hits through secondary assays
Chemical Proteomics:
- Design chemical probes with photoaffinity labels
- Incorporate click chemistry handles for enrichment
- Identify interacting proteins through quantitative proteomics
Bioinformatics Integration:
- Utilize chemoproteomic databases (ChEMBL, DrugBank) [3]
- Apply similarity searching and machine learning
- Integrate multi-omics data for pathway identification
Key Reagents and Research Solutions
Successful implementation of both phenotypic and target-based screening requires specialized reagents and tools:
Table 3: Essential Research Reagents for Drug Discovery Screening
| Reagent/Tool Category | Specific Examples | Function in Screening | Approach |
|---|---|---|---|
| Cell Models | iPSCs, Primary cells, Organoids [32] | Physiologically relevant disease modeling | Phenotypic |
| Protein Production | Recombinant proteins, Membrane preps | Target-based assay development | Target-based |
| Detection Technologies | HCS, FLIPR, AlphaScreen, SPR | Signal readout and quantification | Both |
| Compound Libraries | Diversity sets, Targeted libraries, DNA-encoded libraries [33] | Chemical matter for screening | Both |
| Target Deconvolution Tools | Affinity matrices, CRISPR libraries, Proteomics kits | Mechanism of action determination | Phenotypic |
| Structural Biology | Crystallography platforms, Cryo-EM | Structure-based drug design | Target-based |
Recent Technological Advances and Future Directions
Artificial Intelligence and Machine Learning
AI and ML are transforming both phenotypic and target-based approaches. Convolutional neural networks like AtomNet can successfully identify novel hits across diverse therapeutic areas and protein classes, potentially replacing HTS as the primary screening method [33]. These systems can screen trillions of molecules in synthesis-on-demand libraries, far exceeding the capacity of physical HTS [33].
For phenotypic screening, ML algorithms enable automated analysis of cell image data, extraction of diverse morphological features, and clustering of cellular phenotypes to identify potential drug candidates [1]. Integrating chemical structure features with extracted image features significantly improves the prediction power for mechanism of action and bioactivity properties [1].
Advanced Disease Models
The field is moving toward more physiologically relevant assay systems, including:
- Induced pluripotent stem cells (iPSCs) for patient-specific disease modeling [32]
- Organoids and 3D culture systems that better recapitulate tissue architecture [32]
- Multi-organ chips that model systemic drug effects [32]
- CRISPR-engineered models that precisely mimic disease genetics [32]
These advanced models are particularly valuable for phenotypic screening, as they capture the complexity of human disease while maintaining scalability for screening applications.
Hybrid Screening Strategies
The most successful modern drug discovery programs increasingly integrate phenotypic and target-based approaches:
- Phenotypic primary screening with target-based secondary assays
- Target-based hit identification with phenotypic validation
- Parallel screening across multiple assay formats
- Computational integration of phenotypic and target-based data
This hybrid approach leverages the strengths of both strategies while mitigating their respective limitations, potentially increasing the probability of clinical success.
The choice between phenotypic and target-based screening should be guided by the specific goals of the drug discovery program. Phenotypic screening remains the preferred approach for first-in-class drug discovery when disease biology is incompletely understood or when seeking novel mechanisms of action. Target-based screening excels at optimizing known targets and developing best-in-class therapies with improved properties.
Emerging technologies—including artificial intelligence, advanced disease models, and hybrid screening strategies—are blurring the historical boundaries between these approaches. The most successful drug discovery organizations will be those that strategically match their screening approach to their specific goals while maintaining flexibility to integrate complementary methods throughout the discovery process.
In the competitive landscape of pharmaceutical research, phenotypic drug discovery (PDD) has re-established itself as a powerful engine for identifying first-in-class medicines with novel mechanisms of action. Unlike target-based drug discovery (TDD), which begins with a predefined and often well-validated molecular target, PDD employs a target-agnostic approach, screening compounds for their ability to induce therapeutic changes in physiologically relevant disease models without prior knowledge of the specific macromolecule involved [16] [34]. This fundamental difference in approach allows PDD to bypass the constraints of existing target hypotheses, directly interrogating the complexity of biological systems to uncover previously unknown therapeutic targets and pathways [2] [1]. This guide objectively compares the performance of PDD and TDD in generating novel targets and drugs, providing a detailed analysis of their success rates, key experimental methodologies, and the resulting expansion of the druggable genome.
Quantitative Comparison of Discovery Success
A critical measure of a discovery strategy's value is its tangible output in the form of new medicines. Numerous analyses of FDA-approved drugs reveal a striking trend: PDD disproportionately contributes to the discovery of first-in-class therapies. One seminal review found that between 1999 and 2008, PDD was responsible for 28 first-in-class small molecule drugs, compared to 17 from target-based methods [1]. A broader analysis covering 1999 to 2017 found that of 171 new drugs, PDD contributed to the development of 58, while traditional TDD accounted for 44 approvals [1]. This demonstrates the significant and sustained productivity of phenotypic approaches in pioneering new therapeutic areas.
The following table summarizes the discovery profiles and novel mechanisms of action for several notable therapies identified through phenotypic screening.
Table 1: Recently Approved Therapies Discovered via Phenotypic Screening
| Drug (Brand Name) | Therapeutic Area | Year Approved | Novel Target / Mechanism |
|---|---|---|---|
| Risdiplam (Evrysdi) [16] [1] | Spinal Muscular Atrophy | 2020 | SMN2 pre-mRNA splicing modifier [16] |
| Vamorolone (Agamree) [1] | Duchenne Muscular Dystrophy | 2023 | Dissociative steroidal modulator of the mineralocorticoid receptor [1] |
| Daclatasvir (Daklinza) [16] [1] | Hepatitis C Virus (HCV) | 2014/2015 | NS5A protein inhibitor (protein with no enzymatic activity) [16] [1] |
| Lumacaftor (component of Orkambi) [16] [1] | Cystic Fibrosis | 2015 | CFTR protein corrector (improves folding and trafficking) [16] |
| Perampanel (Fycompa) [1] | Epilepsy | 2012 | Whole-system, multi-parametric modeling [1] |
Experimental Protocols: Deconvoluting Phenotypic Hits
A central challenge in PDD is the process of "target deconvolution"—identifying the specific molecular target(s) responsible for the observed phenotypic effect. Several advanced experimental protocols have been developed to address this.
Drug Affinity Responsive Target Stability (DARTS)
DARTS is a label-free technique that leverages the principle that a small molecule binding to a protein can stabilize it against proteolytic degradation [35].
Detailed Protocol:
- Sample Preparation: Prepare protein libraries from cell lysates or purified proteins [35].
- Small Molecule Treatment: Incubate aliquots of the protein specimen with the drug candidate or vehicle control [35].
- Protease Digestion: Subject the treated and control samples to a nonspecific protease (e.g., thermolysin or proteinase K) [35].
- Stability Analysis: Analyze the proteolysis patterns using SDS-PAGE or mass spectrometry. Proteins stabilized by drug binding will show reduced degradation in the treated sample compared to the control [35].
- Target Identification: Identify the stabilized proteins via mass spectrometry, which represent potential molecular targets of the drug [35].
Advantages and Limitations: DARTS is advantageous as it requires no chemical modification of the drug and can be performed with complex protein mixtures [35]. Its main limitations include potential for misbinding and difficulty in detecting low-abundance proteins, making confirmation with secondary techniques like cellular thermal shift assays (CETSA) often necessary [35].
CRISPR-Based Functional Genomics Screening
CRISPR-Cas9 screening enables the systematic perturbation of genes across the genome to identify those that are essential for a disease phenotype or a drug's mechanism of action [6].
Detailed Protocol:
- Library Design: Select a comprehensive single-guide RNA (sgRNA) library targeting thousands of genes [6].
- Cell Transduction: Transduce a disease-relevant cell population (e.g., cancer cell lines, patient-derived cells) with the sgRNA library using lentiviral vectors at a low multiplicity of infection to ensure one guide per cell [6].
- Phenotypic Selection: Apply a selective pressure, such as treatment with the phenotypic hit compound, and culture the cells for multiple generations [6].
- Genomic DNA Extraction and Sequencing: Harvest cells, extract genomic DNA, and amplify the integrated sgRNA sequences by PCR for next-generation sequencing [6].
- Hit Analysis: Bioinformatically compare the abundance of each sgRNA before and after selection. sgRNAs that are depleted or enriched identify genes that confer sensitivity or resistance to the compound, pointing to its potential targets or pathways [6].
Advantages and Limitations: This approach is powerful for its scalability and precision in directly linking gene function to phenotype [6]. Challenges include off-target effects of CRISPR/Cas9, the complexity of data analysis, and the fundamental biological differences between genetic knockout and pharmacological inhibition [6] [15].
The workflow below illustrates the strategic application of these methods for target identification.
The Scientist's Toolkit: Key Research Reagent Solutions
Success in phenotypic screening and subsequent target deconvolution relies on a suite of specialized research reagents and tools.
Table 2: Essential Research Reagents for Phenotypic Drug Discovery
| Research Reagent / Tool | Critical Function in PDD |
|---|---|
| High-Content Imaging Systems | Enables automated, multi-parametric analysis of complex phenotypic changes (e.g., cell morphology, organelle structure) in cell-based assays [2] [1]. |
| Patient-Derived Cells / iPSCs | Provides disease-relevant biological systems for screening, offering a more translational path than engineered cell lines [34]. |
| sgRNA Libraries (CRISPR) | Allows for genome-wide functional screens to identify genes critical for disease phenotypes or drug response [6]. |
| Compound Libraries (Diverse & Annotated) | Collections of small molecules used for initial screening; diverse sets probe chemical space, while annotated (chemogenomic) libraries can aid early target hypotheses [15]. |
| Proteomics Kits (e.g., for DARTS/MS) | Facilitates the preparation and mass spectrometric analysis of samples for label-free target identification [35]. |
| Bioinformatics Platforms | Crucial for analyzing high-dimensional data from transcriptomics, proteomics, and CRISPR screens to infer mechanisms and targets [2] [6]. |
The data clearly demonstrates that phenotypic drug discovery is a uniquely powerful strategy for expanding the druggable space, responsible for a disproportionate share of first-in-class medicines with unprecedented mechanisms. While target-based discovery remains a highly effective strategy for optimizing drugs against known targets, PDD excels where the target landscape is poorly understood or when therapeutic efficacy requires polypharmacology [2] [16]. The future of innovative drug discovery lies not in choosing one paradigm over the other, but in integrating them. Modern workflows are increasingly hybrid, using phenotypic screening to identify novel biological starting points and advanced deconvolution methods to illuminate their mechanisms, thereby creating a virtuous cycle that fuels the next generation of transformative therapies [2] [35] [6].
Navigating Challenges: Overcoming Limitations in Both Screening Strategies
Phenotypic drug discovery (PDD), the strategy of identifying compounds based on their effects in realistic disease models rather than modulation of a predefined target, has experienced a major resurgence. Analysis has shown that between 1999 and 2008, a majority of first-in-class drugs were discovered empirically without a strict target hypothesis [16]. This approach successfully captures the complexity of biological systems, leading to novel therapies. However, a significant hurdle persists: once a phenotypic "hit" is identified, determining its precise Mechanism of Action (MoA)—specifically, its direct molecular target(s)—becomes the critical next step. This process, known as target deconvolution, is often considered a major bottleneck in phenotypic drug development [36]. Successful deconvolution bridges the gap between an observed therapeutic effect and the underlying molecular biology, enabling lead optimization, safety profiling, and the discovery of novel, druggable targets. This guide provides a comparative analysis of modern target deconvolution strategies, detailing their methodologies, applications, and performance to inform selection for research pipelines.
A Comparative Analysis of Target Deconvolution Strategies
The following table summarizes the core characteristics, strengths, and limitations of the primary experimental target deconvolution strategies in use today.
Table 1: Comparative Overview of Major Target Deconvolution Technologies
| Strategy | Core Principle | Typical Success Rate | Key Strengths | Major Limitations |
|---|---|---|---|---|
| Affinity-Based Pull-Down | Compound immobilized as "bait" to capture binding proteins from lysate [37]. | N/A | Considered a "workhorse"; provides dose-response (IC50) data [37]. | Requires high-affinity, immobilizable probe; may not work for transient/weak interactions [37]. |
| cDNA Expression Cell Microarrays | Expression of thousands of membrane proteins in live cells; binding of phenotypic molecule detected via fluorescence [36]. | ~70% for compatible phenotypic antibodies [36]. | High physiological relevance; identifies membrane protein targets; low false-positive rate [36]. | Limited to ~75% of membrane proteome; sensitivity depends on expression levels [36]. |
| Photoaffinity Labeling (PAL) | Trifunctional probe (compound, photoreactive group, handle) covalently crosslinks to target upon light exposure [37]. | N/A | Captures transient/weak interactions; ideal for integral membrane proteins [37]. | Probe synthesis can be complex; not suitable for shallow binding sites [37]. |
| Activity-Based Protein Profiling (ABPP) | Bifunctional probes covalently bind to enzyme active sites; targets identified via mass spectrometry [3] [37]. | N/A | Powerful for profiling specific enzyme classes (e.g., serine hydrolases, cysteine proteases) [37]. | Requires reactive residues in accessible regions of the target [37]. |
| Label-Free Techniques (e.g., TPP) | Measures proteome-wide protein stability changes (e.g., thermal stability) induced by ligand binding [37]. | N/A | No compound modification needed; works under native conditions [37]. | Challenging for low-abundance, very large, or membrane proteins [37]. |
Detailed Experimental Protocols for Key Strategies
Affinity-Based Pull-Down and Mass Spectrometry
This classic chemoproteomic workflow is a cornerstone of target deconvolution.
- Step 1: Probe Design and Synthesis. The hit compound is chemically modified to incorporate a linker (e.g., a polyethylene glycol chain) and a functional handle (e.g., biotin for streptavidin capture or an alkyne for subsequent "click chemistry" conjugation) [37]. A critical control probe, often an inactive analog of the compound, is also synthesized.
- Step 2: Sample Preparation and Pull-Down. Cell lysates are prepared from relevant biological systems (e.g., disease cell lines). The lysate is incubated with the immobilized compound (the "bait") to allow target proteins to bind. To reduce non-specific binding, the lysate is often pre-cleared with the solid support matrix alone [37].
- Step 3: Affinity Enrichment and Wash. The solid support (e.g., streptavidin beads if using a biotinylated probe) is added to capture the probe-protein complexes. After incubation, the beads are stringently washed with buffers to remove non-specifically bound proteins [37].
- Step 4: Protein Elution and Identification. Bound proteins are eluted, typically by boiling in SDS-PAGE buffer or via competitive elution with excess free compound. The eluted proteins are then digested with trypsin, and the resulting peptides are analyzed by liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) [37].
- Step 5: Data Analysis and Target Validation. Proteins enriched in the experimental sample compared to the inactive analog control are considered potential specific binders. Identified candidates must be validated through orthogonal methods such as cellular thermal shift assays (CETSA), siRNA knockdown, or surface plasmon resonance (SPR) [37].
cDNA Expression Cell Microarray for Membrane Targets
This technology is particularly powerful for identifying cell surface receptors for antibodies and other biologics.
- Step 1: Library Arraying. Expression vectors encoding full-length, untagged human plasma membrane proteins (a library of ~4,500 clones) are arrayed onto specialized slides in a lipid complex [36].
- Step 2: Cell Seeding and Reverse Transfection. Human cells (e.g., HEK293) are seeded onto the slides. Cells growing over the vector spots become reverse-transfected, leading to localized over-expression of a specific membrane protein in its native cellular context [36].
- Step 3: Binding Assay. The phenotypic molecule (e.g., an antibody) is applied to the slides and allowed to bind. Binding is detected using a fluorescent secondary antibody and high-resolution imaging. For small molecules, radiolabeled compounds can be used and detected by phosphorimaging [36].
- Step 4: Hit Confirmation. Primary hits from the full-library screen are sequenced and re-spotted onto custom slides for confirmation. Binding is re-assessed with appropriate controls and competition experiments to weed out non-specific interactions [36].
The workflow for this method is outlined below.
Thermal Proteome Profiling (TPP) - A Label-Free Method
This method leverages the principle that a protein's thermal stability often increases upon ligand binding.
- Step 1: Compound Treatment. Live cells or protein lysates are treated with the compound of interest or a vehicle control (e.g., DMSO). Treatment is typically performed in multiple replicates [37].
- Step 2: Heat Denaturation. Each sample is divided into aliquots and heated to a series of different temperatures (e.g., from 37°C to 67°C). This heat stress causes the denaturation and aggregation of proteins.
- Step 3: Soluble Protein Separation. The denatured, aggregated proteins are separated from the remaining soluble proteins by high-speed centrifugation. Only proteins that remain properly folded and soluble are kept for analysis.
- Step 4: Proteomic Digestion and Mass Spectrometry. The soluble fractions from each temperature point are digested with trypsin and analyzed by quantitative mass spectrometry to measure the abundance of each protein at each temperature.
- Step 5: Melting Curve Analysis. For each protein, a melting curve is generated by plotting its relative abundance in the soluble fraction against the temperature. A shift in this melting curve (i.e., increased thermal stability) in the compound-treated sample compared to the control identifies that protein as a potential target of the compound [37].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful target deconvolution relies on specialized reagents and tools. The following table details key solutions used in the featured methodologies.
Table 2: Key Research Reagent Solutions for Target Deconvolution
| Reagent / Solution | Function | Example Application / Note |
|---|---|---|
| Functionalized Chemical Probes | Serve as "bait" for affinity purification or crosslinking; contain the compound of interest linked to a handle (biotin, alkyne) or photoreactive group [37]. | Critical for affinity pull-down and PAL; design must ensure modified compound retains biological activity. |
| cDNA Expression Vector Library | Provides genetic material for over-expression of the human plasma membrane proteome [36]. | The largest available libraries contain ~4,500 clones, covering ~75% of the plasma membrane proteome [36]. |
| Stable Isotope Labeling (SILAC) | Enables accurate quantification of protein enrichment in MS-based methods by metabolic labeling of proteins with heavy/light isotopes [3]. | Allows direct comparison of experimental and control samples in a single MS run, improving quantification. |
| Streptavidin-Coupled Magnetic Beads | Solid support for efficient capture and purification of biotinylated probe-protein complexes [37]. | Essential for affinity pull-down assays; allow for stringent washing to reduce background noise. |
| Activity-Based Probes (ABPs) | Contain a reactive group that covalently binds to enzyme active sites, a linker, and a tag for separation/identification [3]. | Used in ABPP to target specific protein classes like kinases or hydrolases. |
| Selective Compound Libraries | Collections of highly selective tool compounds used in phenotypic screens to provide immediate target hypotheses [3]. | E.g., A library mined from ChEMBL used to screen cancer cell lines, instantly linking phenotype to potential target [3]. |
No single target deconvolution strategy is universally superior. The selection of an appropriate method depends on the nature of the phenotypic hit (e.g., small molecule vs. biologic), the suspected target class (e.g., membrane receptor, enzyme, protein-protein interaction), and available resources. Affinity-based pull-down remains a versatile workhorse, while cDNA microarrays offer a highly physiological solution for membrane protein targets. Emerging label-free techniques like thermal proteome profiling minimize compound modification but face their own challenges with certain protein classes.
The most effective modern approaches often integrate multiple technologies. A hit from a phenotypic screen might be first profiled using a selective compound library to generate early target hypotheses [3], followed by a definitive, direct method like affinity pull-down or cDNA microarray for confirmation [36] [37]. As phenotypic screening continues to be a vital source of first-in-class medicines, overcoming the deconvolution hurdle through the strategic application and integration of these powerful tools is paramount for accelerating the discovery of novel therapeutics.
Target-based drug discovery (TDD) has dominated pharmaceutical research for decades, offering a precise, mechanism-driven approach to therapeutic development. This strategy focuses on identifying compounds that interact with specific molecular targets—typically proteins with understood roles in disease processes [10]. The approach enables high-throughput screening and rational drug design, exemplified by breakthrough therapies like imatinib for chronic myeloid leukemia and trastuzumab for HER2-positive breast cancer [10]. However, this precision comes with a significant vulnerability: the entire investment depends on initial assumptions about a target's role in human disease, creating a fundamental risk that manifests as high attrition rates in later development stages.
The pharmaceutical industry faces a persistent productivity challenge, with late-stage failures representing enormous financial and scientific costs [16] [38]. A critical analysis reveals that inadequate target validation constitutes a primary contributor to this attrition problem [10]. When the fundamental hypothesis linking a target to disease pathology proves incomplete or incorrect, drug candidates inevitably fail despite optimizing their binding affinity and selectivity. This review examines the strategic integration of phenotypic approaches and advanced technologies to de-risk target-based programs, providing a framework for mitigating validation-related attrition while maintaining the efficiency advantages of targeted screening.
Comparative Analysis of Screening Approaches
Defining Characteristics and Historical Successes
Table 1: Fundamental Characteristics of Screening Approaches
| Feature | Target-Based Screening | Phenotypic Screening |
|---|---|---|
| Primary Focus | Modulation of predefined molecular target | Observation of therapeutic effect on disease phenotype |
| Knowledge Requirement | Deep understanding of target-disease relationship | Target-agnostic; requires relevant disease model |
| Typical Output | Compounds with known mechanism of action | Therapeutically active compounds with potentially novel mechanisms |
| Historical Success Examples | Imatinib (CML), HIV antiretroviral therapies, Trastuzumab (HER2+ breast cancer) | Artemisinin (malaria), Ivacaftor (cystic fibrosis), Risdiplam (spinal muscular atrophy) |
| Optimal Application | Well-validated targets with clear disease linkage | Complex diseases with poorly understood pathophysiology |
Target-based screening strategies have demonstrated remarkable successes when applied to diseases with well-characterized molecular drivers. The development of HIV antiretroviral therapies exemplifies this approach, where researchers identified key molecular targets essential for viral replication, such as reverse transcriptase and integrase enzymes, leading to effective combination therapies [10]. Similarly, the precision of trastuzumab for HER2-positive breast cancer emerged from clear validation of HER2 as a cancer driver [10].
In contrast, phenotypic drug discovery (PDD) approaches do not rely on knowledge of a specific drug target or a hypothesis about its role in disease [38]. Modern PDD has re-emerged as a systematic approach to drug discovery based on therapeutic effects in realistic disease models [16]. This strategy has produced notable first-in-class medicines, including the cystic fibrosis triple-combination therapy (elexacaftor/tezacaftor/ivacaftor) which originated from target-agnostic compound screens using cell lines expressing disease-associated CFTR variants [16]. Similarly, risdiplam for spinal muscular atrophy emerged from phenotypic screens identifying small molecules that modulate SMN2 pre-mRNA splicing [16].
Quantitative Success Rates and Attrition Patterns
Table 2: Comparative Success Rates and Output Characteristics
| Metric | Target-Based Screening | Phenotypic Screening |
|---|---|---|
| First-in-class drug output | Lower proportion | Disproportionately higher proportion [16] |
| Novel target identification | Limited to predefined targets | Expands "druggable" target space [16] |
| Therapeutic area limitations | Struggles with complex polygenic diseases | Particularly valuable for CNS, metabolic, rare diseases [10] |
| Polypharmacology capacity | Typically designed for specificity | Can intentionally or serendipitously engage multiple targets [16] |
| Translation to clinical success | Higher failure rate when target validation incomplete | Better captures disease complexity but has hit validation challenges [38] |
Analysis of drug discovery outcomes between 1999-2008 revealed that a majority of first-in-class drugs were discovered empirically without a predefined target hypothesis [16]. This surprising observation fueled the resurgence of phenotypic approaches in the pharmaceutical industry [16]. Phenotypic strategies have expanded the "druggable target space" to include unexpected cellular processes like pre-mRNA splicing, target protein folding, trafficking, and degradation [16]. They have revealed novel mechanisms of action for traditional target classes and unveiled entirely new classes of drug targets, such as bromodomains [16].
The comparative advantage of each approach varies significantly by therapeutic area. For neurodegenerative diseases like Alzheimer's, where the exact molecular mechanisms remain elusive, phenotypic screening offers a way to evaluate compound effects on neuronal cells or animal models without relying on an a priori hypothesis about the primary disease driver [10]. This is particularly valuable where previous attempts to target single molecules, such as amyloid-beta, have yielded limited therapeutic success [10].
Experimental Protocols for Enhanced Target Validation
Integrated Target Validation Framework
Figure 1: Integrated Multi-Tiered Target Validation Workflow
A robust target validation strategy requires orthogonal evidence streams converging on the same therapeutic hypothesis. The integrated framework above incorporates genetic, biological, and pharmacological validation tiers to de-risk targets before committing to full-scale drug discovery programs.
Genetic Validation Protocol:
- Human Genetic Evidence Collection: Utilize genome-wide association studies (GWAS), sequencing data from consortia, and rare variant analyses to establish natural human evidence for target-disease linkage [38].
- Functional Genomics Screening: Implement genome-wide CRISPR screens in disease-relevant cell models to identify genes whose manipulation modifies disease phenotypes [38].
- Protocol Details: For CRISPR validation, employ dual guide RNA systems to minimize off-target effects. Use multiple cell models including primary cells where possible. Measure both proliferation and disease-specific functional endpoints.
Biological Validation Protocol:
- Pathway Mapping: Apply multi-omics technologies (transcriptomics, proteomics, metabolomics) to map target function within broader disease networks [38].
- Target Engagement Assessment: Implement cellular thermal shift assays (CETSA) to confirm compound binding to intended targets in physiologically relevant environments [7].
- Protocol Details: For CETSA, prepare compound-treated cells in biological triplicate. Use temperature gradients and quantitative mass spectrometry detection. Include vehicle controls and reference compounds. Validate assay quality with known binders and non-binders.
Phenotypic Validation Methodologies
Table 3: Phenotypic Profiling Technologies for Target Validation
| Technology | Measured Parameters | Validation Application | Throughput |
|---|---|---|---|
| Cell Painting | Morphological features from fluorescent microscopy (organelle morphology, texture, size) | Identification of compound functional activity; mechanism prediction | High [39] |
| L1000 Gene Expression | mRNA expression of 978 landmark genes | Mechanism of action classification; pathway activity assessment | High [39] |
| High-Content Imaging | Multiparametric cellular features from automated microscopy | Phenotypic fingerprinting; toxicity assessment | Medium-High |
| Organoid/3D Models | Complex tissue organization, cell-cell interactions, differentiation | Disease modeling with enhanced physiological relevance | Medium |
Recent advances demonstrate that combining phenotypic profiles with chemical structures significantly improves bioactivity prediction accuracy. One large-scale study found that while chemical structures, morphological profiles (Cell Painting), and gene expression profiles (L1000) individually predicted compound activity for 6-10% of assays, in combination they predicted 21% of assays with high accuracy—a 2 to 3 times higher success rate than using a single modality alone [39]. This synergistic effect underscores the value of integrated data streams for validation.
Cell Painting Protocol for Target Validation:
- Cell Line Selection: Use disease-relevant cell lines with appropriate biological context.
- Staining Protocol: Employ six fluorescent dyes targeting nucleus, nucleoli, cytoplasmic RNA, endoplasmic reticulum, Golgi apparatus, plasma membrane, and mitochondria [39].
- Image Acquisition: Use high-content imaging systems with appropriate magnification (20x-60x) across multiple sites per well.
- Feature Extraction: Calculate morphological measurements for individual cells then aggregate per well.
- Data Analysis: Apply machine learning approaches to classify compound effects and compare to reference compounds with known mechanisms.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Research Reagents for Enhanced Target Validation
| Reagent Category | Specific Examples | Primary Application | Key Considerations |
|---|---|---|---|
| Target Engagement Assays | CETSA reagents, Cellular thermal shift assay kits | Confirming drug-target interaction in physiological environments | Requires target-specific detection antibodies or MS methods [7] |
| Functional Genomic Tools | CRISPR libraries, siRNA collections, ORF collections | Genetic validation of target-disease relationship | Essential to use multiple guides/constructs per gene to control for off-target effects |
| Phenotypic Profiling Platforms | Cell Painting dye sets, L1000 profiling reagents | Mechanism of action characterization | Standardized protocols enable cross-study comparisons [39] |
| Advanced Disease Models | iPSC-derived cells, Organoid cultures, Microphysiological systems | Disease modeling with enhanced translation | Requires thorough characterization of model relevance [38] |
| Multi-Omics Tools | RNA-seq kits, Proteomic panels, Phospho-specific antibodies | Pathway mapping and network analysis | Integration across data types maximizes biological insight |
| AI-Powered Prediction Tools | EviDTI framework, Molecular graph networks | Predicting drug-target interactions with uncertainty quantification | Well-calibrated uncertainty estimates crucial for reliable predictions [40] |
The EviDTI framework represents a significant advancement in drug-target interaction prediction by incorporating evidential deep learning to provide uncertainty estimates alongside interaction predictions [40]. This approach integrates multiple data dimensions including drug 2D topological graphs, 3D spatial structures, and target sequence features to generate more reliable predictions while quantifying confidence levels [40]. Such tools are particularly valuable for prioritizing targets with higher confidence predictions for experimental validation.
Strategic Integration Framework
Figure 2: Strategic Integration of Phenotypic and Target-Based Approaches
The most effective drug discovery pipelines strategically integrate phenotypic and target-based approaches at specific decision points. This framework enables programs to leverage the strengths of each methodology while mitigating their respective limitations.
Phenotypic-Driven Path Protocol:
- Application: Optimal for complex diseases with poorly understood pathophysiology or when seeking first-in-class medicines with novel mechanisms [16] [10].
- Hit Triage Process: Prioritize hits using biological knowledge including known mechanisms, disease biology, and safety considerations rather than structural parameters alone [41].
- Target Deconvolution: Implement systematic approaches including chemical proteomics, functional genomics, and biochemical methods to identify mechanisms of action for promising phenotypic hits [16].
Target-Driven Path Protocol:
- Application: Optimal for diseases with well-validated molecular targets or when developing best-in-class therapies against known mechanisms [10].
- Phenotypic Checkpoints: Incorporate phenotypic profiling at key milestones to confirm functional activity in disease-relevant models [39].
- Polypharmacology Assessment: Use broad profiling approaches to identify unintended target interactions that may contribute to efficacy or toxicity [16].
The dichotomy between phenotypic and target-based screening represents a false choice for modern drug discovery. The most productive approach strategically integrates both methodologies to leverage their complementary strengths—using phenotypic screening to identify novel therapeutic mechanisms and validate complex biology, while applying target-based approaches to optimize compounds against validated mechanisms. This integrated framework substantially de-risks the critical bottleneck of target validation, addressing the fundamental driver of attrition in late-stage development.
The convergence of advanced technologies—including functional genomics, evidential deep learning for target prediction, high-content phenotypic profiling, and physiologically relevant disease models—provides an unprecedented toolkit for target validation [40] [39] [7]. By adopting these integrated approaches, drug discovery organizations can advance more robust therapeutic candidates with higher probability of clinical success, ultimately delivering innovative medicines to patients more efficiently.
Leveraging AI and Machine Learning for Enhanced Data Analysis and Prediction
The pursuit of new therapeutic agents has long been structured around two fundamental approaches: phenotypic drug discovery (PDD) and target-based drug discovery (TDD). Phenotypic screening identifies compounds based on their effects in disease-relevant biological systems without requiring upfront knowledge of a specific molecular target, enabling the discovery of novel mechanisms and first-in-class medicines [1] [16]. In contrast, target-based screening employs hypothesis-driven approaches focused on modulating specific, pre-identified molecular targets [32]. Historically, PDD has demonstrated a slight advantage in producing first-in-class medicines, while TDD has yielded more best-in-class drugs [32]. However, both approaches face significant challenges including high costs, long timelines exceeding 10-15 years, and failure rates exceeding 90% for candidates entering clinical trials [42]. The integration of artificial intelligence (AI) and machine learning (ML) promises to transform both paradigms by enhancing predictive accuracy, accelerating timelines, and identifying novel biological mechanisms that would otherwise remain undiscovered [42] [33] [43].
Comparative Success Rates: Phenotypic vs. Target-Based Screening
Historical and Recent Performance Data
Table 1: Comparative Success Rates of Drug Discovery Approaches
| Metric | Phenotypic Drug Discovery (PDD) | Target-Based Drug Discovery (TDD) | Data Source/Time Period |
|---|---|---|---|
| First-in-class drugs | 28 drugs | 17 drugs | 1999-2008 [1] |
| Total drug approvals | 58 out of 171 drugs | 44 out of 171 drugs | 1999-2017 [1] |
| Industry portfolio share | Increased from <10% to 25-40% | Corresponding decrease | 2012-2022 (AstraZeneca, Novartis) [1] |
| Clinical trial success rate | ~10% (across all approaches) | ~10% (across all approaches) | Industry-wide average [42] |
| Major contributor to efficacy failures | Complex target deconvolution | False target-disease relationships (~92.6% false positive rate) [43] | Contemporary analysis |
The data reveals that phenotypic screening has been disproportionately successful in delivering first-in-class medicines, accounting for approximately 64% of such drugs approved between 1999-2008 [1]. This success has driven a substantial increase in the adoption of phenotypic screening within major pharmaceutical companies, with its representation in project portfolios growing from less than 10% to an estimated 25-40% between 2012 and 2022 [1]. This resurgence is notable given that the approach was largely supplanted by target-based methods during the molecular biology and genomics revolution of the 1980s-2000s [16].
Notable Recent Drug Approvals from Phenotypic Screening
Table 2: Recently Approved Therapies Identified Through Phenotypic Screening
| Drug (Brand Name) | Disease Area | Year Approved | Key Mechanism/Target |
|---|---|---|---|
| Risdiplam (Evrysdi) | Spinal Muscular Atrophy | 2020 | SMN2 pre-mRNA splicing modifier [1] [16] |
| Vamorolone (AGAMREE) | Duchenne Muscular Dystrophy | 2023 | Dissociative steroidal agent [1] |
| Lumacaftor/Ivacaftor (ORKAMBI) | Cystic Fibrosis | 2015 | CFTR corrector/potentiator [1] [16] |
| Daclatasvir (Daklinza) | Hepatitis C | 2014-2015 | NS5A replication complex inhibitor [1] [16] |
| Perampanel (Fycompa) | Epilepsy | 2012 | AMPA receptor antagonist [1] |
The drugs identified through phenotypic screening frequently reveal unprecedented mechanisms of action and target novel biological pathways. For example, risdiplam works through the novel mechanism of modulating SMN2 pre-mRNA splicing, while daclatasvir targets NS5A, a viral protein with no known enzymatic function [1] [16]. These targets would have been unlikely candidates in traditional target-based campaigns, demonstrating PDD's unique ability to expand the "druggable genome" and identify unexpected therapeutic strategies [1].
AI-Enhanced Screening: Methodologies and Experimental Protocols
AI in Phenotypic Screening
Modern phenotypic screening has been revolutionized by AI-driven image analysis and feature extraction. High-content screening (HCS) generates massive datasets of cellular images that can be processed using convolutional neural networks (CNNs) to quantify complex morphological changes and identify subtle phenotypic signatures [1] [43].
Experimental Protocol 1: AI-Enhanced High-Content Phenotypic Screening
- Model System Preparation: Establish disease-relevant cell models (primary cells, iPSCs, 3D organoids) in multi-well plates [32] [43].
- Compound Library Treatment: Apply chemical libraries (typically 10,000-100,000 compounds) across experimental wells, including appropriate controls.
- Multiparameter Imaging: Automated microscopy captures multiple channels (nuclei, cytoskeleton, organelles) and time points [43].
- AI-Based Image Analysis:
- Feature Extraction: CNNs (e.g., CellProfiler) identify and quantify hundreds of morphological features (cell shape, texture, organelle distribution) [43].
- Phenotypic Clustering: Unsupervised ML algorithms group compounds inducing similar morphological profiles.
- Hit Identification: Compounds producing disease-relevant phenotypic reversal are prioritized.
- Target Deconvolution: For confirmed hits, AI tools integrate chemical structure data with phenotypic profiles to predict mechanism of action [1] [43].
AI in Target-Based Screening
Structure-based virtual screening uses AI to predict compound binding to defined protein targets, accessing vastly larger chemical spaces than physical screening [33].
Experimental Protocol 2: AI-Driven Structure-Based Virtual Screening
- Target Preparation: Obtain high-resolution protein structures (X-ray, cryo-EM) or generate high-quality homology models [33].
- Chemical Library Curation: Prepare virtual compound libraries from synthesis-on-demand catalogs (billions of compounds) [33].
- AI Docking Screen:
- Structure-Based Prediction: CNN-based systems (e.g., AtomNet) analyze 3D protein-ligand interactions across the entire library [33].
- Binding Affinity Prediction: Models score and rank compounds by predicted binding probability.
- Diversity Selection: Algorithmic clustering selects top-ranked compounds representing diverse scaffolds.
- Experimental Validation:
- Compound Synthesis: Selected compounds are synthesized and quality-controlled (LC-MS, NMR to >90% purity) [33].
- Biochemical Assays: Test compounds in dose-response experiments against the target protein.
- Selectivity Profiling: Counter-screening against related targets to assess specificity.
Performance Comparison: AI vs. Traditional Methods
Table 3: AI Screening vs. Traditional HTS Performance (318-Target Study)
| Performance Metric | AI-Based Virtual Screening | Traditional High-Throughput Screening (HTS) |
|---|---|---|
| Average hit rate | 6.7% (internal projects), 7.6% (academic collaborations) [33] | 0.001-0.15% [33] |
| Success rate across diverse targets | 91% of projects yielded confirmed hits [33] | Variable, highly target-dependent |
| Chemical space coverage | 16 billion compounds (in silico) [33] | Typically 100,000-2 million (physical collection) |
| Resource requirements | High computational cost (40,000 CPUs, 3,500 GPUs per screen) [33] | High compound, reagent, and equipment costs |
| Scalability to novel target classes | Effective for PPI, allosteric sites, and targets without known binders [33] | Challenging for "undruggable" targets |
The empirical data from a massive 318-target study demonstrates that AI-based screening can achieve dramatically higher hit rates than traditional HTS while exploring substantially larger chemical spaces [33]. Notably, the AI approach succeeded across diverse protein families and target types, including those without known binders or high-quality crystal structures, demonstrating robust generalizability [33].
Visualization of Screening Workflows and AI Integration
Phenotypic Drug Discovery Workflow with AI Enhancement
AI-Enhanced Phenotypic Screening
Target-Based Drug Discovery Workflow with AI Enhancement
AI-Enhanced Target-Based Screening
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagent Solutions for AI-Enhanced Screening
| Reagent/Technology | Function in Screening | AI Integration |
|---|---|---|
| Synthesis-on-Demand Libraries | Provide access to billions of novel, easily synthesizable compounds [33] | Enlarge accessible chemical space for virtual screening |
| iPSCs & 3D Organoids | Create physiologically relevant disease models for phenotypic screening [32] [43] | Generate more predictive data for ML analysis |
| CRISPR-Cas9 Tools | Enable genetic validation of targets and create refined screening models [32] | Provide ground truth data for training AI models |
| High-Content Imaging Systems | Automate capture of cellular morphology data across multiple parameters [43] | Generate rich image datasets for deep learning analysis |
| Affinity Capture Platforms | Identify protein targets of phenotypic screening hits [44] | Validate AI-based target predictions experimentally |
| Public Datasets (e.g., JUMP-CP) | Provide large-scale annotated cellular imaging data [1] | Enable training and benchmarking of AI models |
The integration of AI and ML into both phenotypic and target-based screening represents a paradigm shift in early drug discovery. While both approaches benefit from AI enhancement, the technology is particularly transformative for phenotypic screening by addressing its historical bottleneck of target deconvolution [1] [43]. The empirical evidence demonstrates that AI-driven methods can substantially replace HTS as the primary screening tool, achieving higher hit rates while exploring vastly larger chemical spaces [33]. As AI models continue to advance in reasoning capability and biological accuracy, and as screening models become more physiologically relevant through technologies like organoids and complex co-culture systems, the synergy between AI and empirical screening promises to accelerate the discovery of novel therapeutics for diseases with high unmet need. The future of drug discovery lies not in choosing between phenotypic and target-based approaches, but in strategically integrating both, enhanced by AI, to leverage their complementary strengths in identifying transformative medicines.
In the field of drug discovery, the historical dichotomy between phenotypic screening and target-based approaches is increasingly giving way to a more powerful paradigm: integrated hybrid models. Historically, drug discovery has been guided by two principal strategies. Phenotypic drug discovery identifies compounds based on measurable biological responses in complex cellular or organismal systems, often without prior knowledge of the specific molecular target. Conversely, target-based drug discovery begins with a well-characterized molecular target and employs rational design to develop specific modulators [2]. While both strategies have yielded successful therapeutics, they possess complementary strengths and limitations. The integration of these approaches, supercharged by artificial intelligence (AI) and advanced computational modeling, is now reshaping drug discovery pipelines, enhancing precision, accelerating timelines, and overcoming historical challenges of efficacy and resistance [2] [21]. This guide explores the current landscape of these hybrid models, comparing their performance and providing a detailed toolkit for their implementation.
Table 1: Comparison of Traditional and Modern AI-Hybridized Discovery Approaches
| Approach | Key Characteristic | Typical Discovery Timeline (Preclinical) | Key Advantage | Primary Limitation | Representative Clinical-Stage Compound |
|---|---|---|---|---|---|
| Phenotypic Screening | Measures functional outcomes in complex biological systems [2] | ~5 years (traditional) | Unbiased discovery of novel biology and first-in-class mechanisms [45] | Challenging target deconvolution [2] | Lenaildomide (derived from thalidomide) [2] |
| Target-Based Screening | Rational design against a predefined molecular target [2] | ~5 years (traditional) | High mechanism specificity and straightforward optimization [2] | Reliant on validated, druggable targets; can miss complex biology [2] | Immune checkpoint inhibitors (e.g., anti-PD-1) [2] |
| AI-Driven Hybrid Platforms | Integrates phenotypic data, target insights, and generative chemistry [21] | 18-24 months (reported for leading platforms) [21] | Dramatically compressed design-make-test-learn cycles; explores vast chemical space [21] [45] | High computational resource demand; "black box" interpretability issues [21] [46] | ISM001-055 (Insilico Medicine, Phase II) [21] |
| Physics-Based + AI Integration | Combines molecular simulations (e.g., free energy perturbation) with machine learning [21] | ~2-3 years (estimated) | High-fidelity prediction of binding affinities and compound properties [21] | Computationally intensive; requires expert knowledge [21] | Zasocitinib (TAK-279, Phase III) [21] |
Experimental Protocols for Hybrid Workflows
AI-Driven Phenotypic-to-Targeted Screening Protocol
This protocol, employed by platforms like Recursion and Exscientia, integrates large-scale phenotypic data with AI to transition from observed biological effects to targeted compound design [21] [45].
- Complex Model Selection: Utilize physiologically relevant disease models such as patient-derived organoids, 3D co-cultures, or organ-on-chip systems [45].
- High-Content Phenotypic Screening: Treat models with diverse compound libraries (e.g., MCE 50K Diversity Library). Perform high-content imaging with multiparametric readouts (e.g., cell morphology, protein localization, metabolic activity) [45].
- AI-Enabled Data Integration and Target Deconvolution: Apply machine learning models to analyze high-dimensional imaging data and extract phenotypic "signatures." Integrate these signatures with complementary datasets (transcriptomics, proteomics) and chemical descriptors to infer the most likely molecular targets of active compounds [2] [45].
- Generative Chemistry and Validation: Use generative AI models (e.g., Exscientia's Centaur Chemist) to design novel chemical structures optimized for the predicted target and desired drug-like properties. Synthesize and validate these compounds in targeted biochemical and secondary phenotypic assays [21].
Knowledge-Graph-Driven Repurposing and Combination Protocol
This methodology, used by companies like BenevolentAI, leverages structured knowledge to identify new therapeutic opportunities for existing drugs or novel targets [21].
- Knowledge Graph Construction: Assemble a massive, dynamic knowledge graph integrating data from scientific literature, clinical trial records, genomics databases, patent documents, and chemical databases [21].
- Hypothesis Generation: Use AI algorithms to traverse the graph and identify novel, non-obvious relationships between diseases, biological pathways, genes, and existing compounds. For example, discover a previously unknown link between a specific protein and a disease pathology [21].
- Virtual Screening and Prioritization: Screen in-silico compound libraries (including approved drug libraries) against the newly identified target or pathway. Prioritize candidates using predictive models for binding affinity, selectivity, and ADME/Tox (Absorption, Distribution, Metabolism, Excretion, and Toxicity) properties [45].
- Experimental Confirmation: Test top-prioritized candidates in relevant in vitro and in vivo disease models to confirm the predicted efficacy [21].
Visualizing Hybrid Discovery Workflows
Phenotypic Screening and AI-Driven Target Deconvolution
This diagram illustrates the modern workflow that connects phenotypic screening with AI-powered analysis to accelerate target identification and compound optimization.
Integrated Target & Phenotypic Validation Loop
This diagram shows a hybrid workflow that tightly couples target-based design with phenotypic validation, creating a continuous feedback loop for optimization.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Tools for Integrated Discovery Workflows
| Item | Function in Hybrid Workflows | Key Considerations for Selection |
|---|---|---|
| Diverse Compound Libraries (e.g., MCE 50K Diversity Library) | Provides a broad foundation for unbiased phenotypic screening and initial hit identification [45]. | Prioritize libraries with high structural novelty, drug-likeness, and rigorous purity validation [45]. |
| Target-Focused Libraries (e.g., Kinase, GPCR, Epigenetic) | Enables efficient screening against well-validated target families, enriching for hits with a higher probability of success [45]. | Ensure detailed mechanistic annotation and coverage of key targets within the family of interest [45]. |
| FDA-Approved Drug Library | Critical for drug repurposing campaigns via phenotypic screening, leveraging existing safety profiles [45]. | --- |
| Specialized Libraries (Covalent, Fragment, DNA-Encoded) | Expands accessible chemical space and provides unique starting points for difficult targets [45]. | Choose based on specific campaign goals and compatibility with your screening technology (e.g., biophysical assays for fragments). |
| Physiologically Relevant Models (Organoids, 3D Co-cultures) | Provides a biologically complex and translationally relevant system for phenotypic screening and compound validation [45]. | Balance biological relevance with assay robustness and throughput capabilities. |
| AI-Driven Design Platforms (e.g., Exscientia, Insilico) | Accelerates lead optimization by generating novel compounds satisfying multiple parameters (potency, selectivity, ADME) [21]. | Consider integration capabilities with internal data and required computational infrastructure. |
| High-Content Imaging Systems | Generates rich, multiparametric phenotypic data from complex cellular assays, forming the basis for AI analysis [2] [45]. | Prioritize systems with high resolution, automation compatibility, and advanced image analysis software. |
Performance Analysis of Leading Hybrid Platforms
The efficacy of integrated models is best demonstrated by the progress of leading AI-driven drug discovery companies. Their pipelines and clinical outcomes provide tangible performance data.
Table 3: Clinical-Stage Performance of Leading AI-Hybrid Discovery Platforms
| Company / Platform | Core Hybridization Strategy | Key Clinical-Stage Asset & Indication | Reported Discovery Timeline & Efficiency | Partner(s) |
|---|---|---|---|---|
| Insilico Medicine | Generative AI from target discovery to compound design [21] | ISM001-055 (TNK2 inhibitor for Idiopathic Pulmonary Fibrosis) - Phase IIa [21] | ~18 months from target to Phase I (traditional average: 5 years) [21] | --- |
| Exscientia | "Centaur Chemist" AI design integrated with patient-derived phenotypic screening [21] | EXS-74539 (LSD1 inhibitor) - Phase I; EXS-73565 (MALT1 inhibitor) - IND-enabling [21] | AI design cycles ~70% faster, requiring 10x fewer synthesized compounds [21] | Bristol Myers Squibb, Sanofi, Merck KGaA [21] |
| Schrödinger | Physics-based simulation (FEP) combined with machine learning [21] | Zasocitinib (TAK-279, TYK2 inhibitor for psoriasis) - Phase III [21] | Physics-based approach enables high-fidelity prioritization, reducing experimental cycles [21] | Takeda, Nimbus Therapeutics [21] |
| Recursion | Massive-scale phenomics integrated with AI for target and drug discovery [21] | Pipeline in oncology and neurology (specific assets not detailed in search results) | Merged with Exscientia to create integrated "AI drug discovery superpower" [21] | --- |
| BenevolentAI | Knowledge-graph-driven target identification and repurposing [21] | Pipeline in immunology and oncology (specific assets not detailed in search results) | AI used to traverse scientific literature and databases for novel target-disease links [21] | --- |
The data from these platforms indicates a consistent trend: integrated hybrid models can significantly compress the early drug discovery timeline, in some cases reducing it from the traditional five-year average to under two years [21]. Furthermore, the ability to design and synthesize far fewer compounds to reach a clinical candidate represents a major efficiency gain in resource utilization [21].
The integration of phenotypic and target-based approaches into hybrid models represents a maturation of drug discovery. By leveraging the unbiased, biologically relevant insights from phenotypic screening alongside the precision and rational design of target-based methods, these workflows mitigate the inherent limitations of each standalone approach. The accelerating clinical progress of companies built on these integrated principles, powered by AI and advanced computational tools, provides compelling evidence of their superior efficiency and outcomes. For researchers and drug development professionals, adopting and adapting these hybrid frameworks is no longer a speculative future but a present-day imperative for improving the probability of success in delivering new therapeutics.
Data-Driven Decisions: Comparing Success Rates, Case Studies, and Future Trends
The development of new pharmaceuticals is a high-stakes endeavor, characterized by significant investment, lengthy timelines, and considerable uncertainty. Within this landscape, two fundamental drug discovery paradigms have emerged: phenotypic screening and target-based screening. Phenotypic drug discovery entails identifying active compounds based on measurable biological responses in cells, tissues, or whole organisms, often without prior knowledge of their specific molecular targets or mechanisms of action [2]. This approach captures the complexity of biological systems and has been instrumental in discovering first-in-class therapies [2]. In contrast, target-based drug discovery begins with a well-characterized molecular target—typically a protein with established involvement in the disease process—and employs rational design to develop compounds that modulate its activity [10]. This strategy benefits from advances in structural biology, genomics, and computational modeling to create highly specific therapeutic agents [2].
The debate between these approaches is not merely academic; it has profound implications for research and development (R&D) strategy, resource allocation, and ultimately, the success rate of drug development programs. This guide provides an objective comparison of these strategies, with a specific focus on their performance in generating first-in-class therapies versus approved drugs overall. We present quantitative success rates, detailed experimental methodologies, and key resources to inform the decision-making processes of researchers, scientists, and drug development professionals.
Quantitative Comparison of Success Rates
Drug development is notoriously challenging, with a high attrition rate throughout the clinical phases. Table 1 summarizes key success rate metrics for drug development programs, providing a baseline for understanding the broader context in which first-in-class drugs are developed.
Table 1: Overall Clinical Drug Development Success Rates
| Metric | Success Rate | Time Frame | Sample Size | Source/Reference |
|---|---|---|---|---|
| Likelihood of Approval (LoA) | 14.3% (average) | 2006-2022 | 2,092 compounds, 19,927 trials | [47] |
| Range Across Companies | 8% - 23% | 2006-2022 | 18 leading pharmaceutical companies | [47] |
| Probability of Success (POS) | 10% - 20% | 2000-2010 | 3,999 compounds | [48] |
| Rare Disease Drugs (Non-Oncology) | ~25% | 2016 analysis | Not specified | [49] |
| Biomarker-Included Projects | ~26% | 2016 analysis | Not specified | [49] |
Recent evidence suggests that after a period of decline, clinical trial success rates (ClinSR) have begun to plateau and even show signs of improvement in recent years [50]. Significant variation exists across therapeutic areas, with oncology historically demonstrating lower success rates (3.4% in one large study) compared to other disease categories [51]. However, this rate has shown recent improvement, reaching 8.3% in 2015 [51]. Drugs for infectious diseases, hematology, and ophthalmology typically show higher-than-average success probabilities [48].
First-in-Class Drug Success and Origins
First-in-class (FIC) drugs, defined as therapies with novel targets and mechanisms of action, are considered the main drivers of pharmaceutical innovation [52]. Table 2 compares the origins and success metrics of first-in-class drugs versus follow-on medications, with a specific focus on the discovery strategies employed.
Table 2: First-in-Class Drug Approvals and Discovery Strategies
| Parameter | First-in-Class Drugs | Follow-on Drugs | Notes and Context |
|---|---|---|---|
| Global Approvals (2023-2024) | 81 drugs | Not specified | 51.9% were small molecules; 48.1% were macromolecules [52] |
| Leading Therapeutic Area | Cancer (22.0%, 18 therapies) | Varies | High patient need drives FIC innovation in oncology [52] |
| Discovery Method (Historical) | 28 FIC drugs via phenotypic screening | 17 FIC drugs via target-based | 1999-2008 review [1] |
| Discovery Method (Recent) | 58 approvals via phenotypic screening | 44 via target-based | 1999-2017 data [1] |
| Common FIC Targets | Diverse enzymes (32.1%) | Varies | 26 novel targets identified in 2023-2024 [52] |
The data reveals that phenotypic screening has consistently contributed to a disproportionate share of first-in-class medicines over the past two decades. From 1999 to 2008, phenotypic screening was responsible for 28 first-in-class small molecule drugs compared to 17 from target-based methods [1]. This trend continued through 2017, with phenotypic approaches contributing to 58 approved drugs, compared to 44 from target-based discovery [1]. The percentage of phenotypic screens in the project portfolios of major pharmaceutical companies like AstraZeneca and Novartis has grown significantly, from less than 10% in 2012 to an estimated 25-40% by 2022 [1].
Experimental Protocols and Methodologies
Phenotypic Screening Workflows
Phenotypic drug discovery employs a target-agnostic approach that focuses on observing compound effects in biologically relevant systems. The following protocol outlines a standard workflow for phenotypic screening:
Model System Development: Establish physiologically relevant models that recapitulate key aspects of the human disease phenotype. This may include:
- Primary cell cultures from patients or diseased tissues
- Genetically engineered cell lines with disease-associated mutations
- 3D organoid or spheroid cultures that better mimic tissue architecture
- Whole organism models (e.g., zebrafish, C. elegans) for complex phenotypes
Assay Design and Implementation: Develop robust, quantitative assays capable of detecting meaningful phenotypic changes:
- High-content screening (HCS) using automated microscopy and image analysis
- Multi-parametric readouts capturing multiple aspects of cellular morphology and function
- Functional assays measuring relevant biological endpoints (e.g., cell viability, cytokine secretion, neurite outgrowth)
Compound Library Screening: Screen diverse chemical libraries against the phenotypic model:
- Library diversity is critical, encompassing various chemical scaffolds and origins
- Dose-response studies to establish potency and efficacy relationships
- Counter-screens to exclude compounds with non-specific or undesirable effects
Hit Validation and Characterization: Confirm and characterize initial hits through secondary assays:
- Dose-response confirmation in the primary assay system
- Specificity assessment across related but distinct phenotypic models
- Early safety and toxicity profiling
Target Deconvolution: Identify the molecular target(s) responsible for the observed phenotype:
- Chemical proteomics approaches (e.g., affinity chromatography, activity-based protein profiling)
- Genomic methods (e.g., RNAi screens, CRISPR-based genetic approaches)
- Resistance generation and whole-genome sequencing of resistant clones
- Biophysical methods (e.g., surface plasmon resonance, thermal shift assays)
This workflow has successfully identified numerous first-in-class therapies, including risdiplam for spinal muscular atrophy and vamorolone for Duchenne muscular dystrophy [1]. A key advantage is its ability to identify therapeutic interventions for novel and diverse targets, including those with unknown biological functions that would be missed by target-based approaches [1].
Figure 1: Phenotypic Screening Workflow. This diagram illustrates the key stages of phenotypic drug discovery, from model development to target identification.
Target-Based Screening Workflows
Target-based drug discovery follows a more reductionist approach, beginning with a specific molecular target believed to be critically involved in the disease process. The standard protocol includes:
Target Selection and Validation: Identify and confirm the relevance of a specific molecular target:
- Genetic evidence from genome-wide association studies (GWAS) or sequencing data
- Functional studies using genetic manipulation (knockdown, knockout, overexpression)
- Expression analysis in diseased versus normal tissues
- Biomarker development to establish target engagement and patient stratification strategies
Assay Development for Targeted Screening: Design biochemical or cell-based assays specific to the target:
- Biochemical assays measuring direct binding or enzymatic activity inhibition
- Cell-based reporter assays monitoring pathway modulation downstream of the target
- Binding assays (e.g., SPR, FRET, FP) to quantify compound-target interactions
- High-throughput screening optimization for rapid compound evaluation
Compound Screening and Hit Identification: Screen compound libraries against the specific target:
- Focused libraries enriched for target class expertise (e.g., kinase-focused libraries)
- Fragment-based screening using biophysical methods (e.g., NMR, X-ray crystallography)
- Virtual screening employing computational docking and structure-based design
Hit-to-Lead Optimization: Systematically optimize initial hits for improved properties:
- Structure-activity relationship (SAR) studies to refine potency and selectivity
- Structural biology guidance using X-ray co-crystallography or cryo-EM
- ADMET optimization addressing absorption, distribution, metabolism, excretion, and toxicity
- Physicochemical property optimization for drug-likeness
In Vivo Target Validation: Confirm target engagement and pharmacological effects in disease models:
- Pharmacodynamic biomarker development and implementation
- Target engagement assays in relevant tissues
- Efficacy studies in genetically engineered or patient-derived xenograft models
This approach has produced highly successful targeted therapies, including imatinib for chronic myeloid leukemia (targeting BCR-Abl) and trastuzumab for HER2-positive breast cancer [10]. The key advantage lies in the ability to precisely optimize compounds against a known mechanism, potentially reducing off-target effects and enabling patient stratification through biomarker development [10].
Figure 2: Target-Based Screening Workflow. This diagram illustrates the systematic process of target-based drug discovery, from target validation to candidate selection.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of either screening paradigm requires specialized reagents and tools. Table 3 catalogues key resources essential for contemporary drug discovery research.
Table 3: Essential Research Reagents and Solutions for Drug Discovery
| Reagent/Solution | Function and Application | Screening Context |
|---|---|---|
| High-Content Screening Systems | Automated microscopy and image analysis for multiparametric phenotypic assessment | Primarily Phenotypic |
| Disease-Relevant Cell Models | Primary cells, iPSC-derived cells, organoids that recapitulate disease pathology | Both (Emphasis in Phenotypic) |
| Compound Libraries | Diverse collections of small molecules for screening; target-class focused libraries | Both |
| Proteomics Platforms | Mass spectrometry, protein arrays for target identification and validation | Both (Emphasis in Phenotypic) |
| Genomic Tools | CRISPR-Cas9 systems, RNAi libraries for target validation and functional studies | Both |
| Structural Biology Tools | X-ray crystallography, Cryo-EM for structure-based drug design | Primarily Target-Based |
| Biophysical Assay Platforms | SPR, ITC, DSF for measuring binding affinity and kinetics | Primarily Target-Based |
| Multi-omics Databases | Integrated genomics, transcriptomics, proteomics data for target prioritization | Both |
| AI/ML Analysis Platforms | Machine learning algorithms for pattern recognition in complex datasets | Both (Growing importance) |
The selection of appropriate tools and reagents is critical for success in either screening paradigm. For phenotypic screening, the quality and biological relevance of the model system is paramount, while for target-based approaches, the robustness and specificity of the target assay are crucial. Recent advances in areas such as gene editing (CRISPR), stem cell biology (iPSC-derived models), and artificial intelligence are transforming both approaches, enabling more physiologically relevant models and more sophisticated data analysis [2] [1].
The evidence presented in this guide demonstrates that both phenotypic and target-based screening approaches have distinct strengths and contribute meaningfully to drug discovery. Phenotypic screening has historically shown a superior track record in generating first-in-class therapies, accounting for a disproportionate number of innovative medicines with novel mechanisms of action [1]. This approach is particularly valuable when disease biology is incompletely understood, as it does not require predetermined molecular hypotheses [10]. Conversely, target-based screening enables precise optimization of drug candidates against validated targets and has driven the development of highly effective targeted therapies, particularly in oncology [10].
Rather than viewing these approaches as competing strategies, the future of drug discovery lies in their strategic integration. The convergence of phenotypic and target-based paradigms is being accelerated by advancements in computational modeling, artificial intelligence, and multi-omics technologies [2]. Emerging hybrid workflows leverage the unbiased nature of phenotypic screening for novel target discovery combined with the precision of target-based approaches for candidate optimization [2]. Furthermore, the application of machine learning and AI tools for analyzing high-content screening data is enhancing the power and efficiency of phenotypic discovery [1].
For research and development organizations, the strategic decision between these approaches should be context-dependent, considering factors such as the state of disease knowledge, available tools and expertise, and the specific therapeutic objectives (first-in-class innovation versus best-in-class optimization). As technological capabilities continue to advance, the distinction between these paradigms will likely further blur, creating new opportunities for therapeutic innovation across the drug discovery landscape.
Phenotypic Drug Discovery (PDD) has experienced a major resurgence in modern pharmaceutical research, emerging as a powerful alternative to target-based drug discovery (TDD). This strategic shift follows the surprising observation that a majority of first-in-class drugs approved between 1999 and 2008 were discovered empirically without a predefined drug target hypothesis [16]. Modern PDD systematically pursues drug discovery based on therapeutic effects in realistic disease models, focusing on the modulation of a disease phenotype or biomarker rather than a pre-specified target [16]. This approach has proven particularly valuable for addressing the incompletely understood complexity of diseases and has delivered multiple breakthrough therapies across therapeutic areas where target-based approaches had struggled.
The fundamental distinction between PDD and TDD lies in their starting points. While TDD begins with a hypothesis about a specific molecular target's role in disease, PDD relies on chemical interrogation of a disease-relevant biological system in a molecular-target-agnostic fashion [16]. This biology-first strategy provides tool molecules that link therapeutic biology to previously unknown signaling pathways, molecular mechanisms, and drug targets, thereby expanding the "druggable target space" [16]. The following analysis examines notable phenotypic screening successes across neurology, oncology, and infectious diseases, comparing their outcomes against target-based approaches and detailing the experimental methodologies that enabled these discoveries.
Phenotypic Screening Successes by Therapeutic Area
Neurology and Central Nervous System Disorders
Central nervous system (CNS) drug development is notoriously plagued by high clinical failure rates, making it a prime area for phenotypic approaches [53]. Phenotypic assays promote clinical translation by reducing complex brain diseases to measurable, clinically valid phenotypes such as neuroinflammation, oxidative stress, pathological proteins, hyperexcitability, and neuroplasticity [53]. The field has increasingly adopted patient-derived brain cells and induced pluripotent stem cells (iPS) to recapitulate CNS disease phenotypes more accurately, balancing validity and scalability for screening purposes [53] [54].
Spinal Muscular Atrophy (SMA): Type 1 SMA is a rare neuromuscular disease with 95% mortality by 18 months of age, caused by loss-of-function mutations in the SMN1 gene [16]. Phenotypic screens by two research groups independently identified small molecules that modulate SMN2 pre-mRNA splicing and increase levels of full-length survival of motor neuron (SMN) protein [16]. These compounds work by engaging two sites at the SMN2 exon 7 and stabilizing the U1 snRNP complex—an unprecedented drug target and mechanism of action (MoA) [16]. One resulting compound, risdiplam, was approved by the FDA in 2020 as the first oral disease-modifying therapy for SMA [16].
Alzheimer's Disease and Neurodegeneration: Phenotypic screening has emerged as a crucial tool for neurodegenerative diseases like Alzheimer's, where the exact molecular mechanisms driving disease progression remain incompletely understood [10]. Given the multifaceted pathological landscape involving amyloid-beta plaques, tau tangles, neuroinflammation, and synaptic dysfunction, phenotypic screening offers a way to evaluate a compound's overall impact on neuronal cells or animal models without relying on an a priori hypothesis about the primary disease driver [10]. This unbiased approach is particularly valuable in Alzheimer's research, where previous attempts to target single molecules, such as amyloid-beta, have yielded limited therapeutic success [10].
Table 1: Phenotypic Screening Successes in Neurology
| Drug/Compound | Disease | Phenotypic Model | Key Findings/Mechanism | Development Status |
|---|---|---|---|---|
| Risdiplam | Spinal Muscular Atrophy (SMA) | SMN2 splicing modulation | Modulates SMN2 pre-mRNA splicing, stabilizes U1 snRNP complex | FDA Approved (2020) |
| Branaplam | Spinal Muscular Atrophy (SMA) | SMN2 splicing modulation | Modulates SMN2 pre-mRNA splicing | Clinical Development |
| SEP-363856 | Schizophrenia | Phenotypic screening | Novel mechanism unrelated to D2 receptor antagonism | Clinical Development |
| Various compounds under investigation | Alzheimer's Disease | Patient-derived neurons, animal models | Focus on synaptic activity, neuroinflammation, neuronal survival without predetermined targets | Preclinical/Clinical Development |
Oncology Applications
In oncology drug development, where failure rates exceed 90%, phenotypic approaches have provided valuable alternatives to target-based strategies [55]. The field has evolved from traditional 2D in vitro screening to more complex models that better recapitulate tumor biology, including 3D cultures, patient-derived organoids (PDOs), and patient-derived xenografts (PDXs) [55].
Lenalidomide and Novel Cancer Mechanisms: The optimized thalidomide analogue lenalidomide gained FDA approval for several blood cancer indications and has achieved substantial commercial success (sales > $12 billion in 2020) [16]. Significantly, the unprecedented molecular target and MoA of lenalidomide were only elucidated several years post-approval [16]. Researchers discovered that lenalidomide binds to the E3 ubiquitin ligase Cereblon and redirects its substrate selectivity to promote the ubiquitination and subsequent degradation of target proteins including the transcription factors IKZF1 and IKZF3 [16]. This novel MoA is now being intensively explored in developing further targeted protein degraders, dubbed 'bifunctional molecular glues' [16].
Imatinib and Polypharmacology: Initially regarded as an inhibitor of CML's BCR-ABL fusion protein, imatinib also exhibits activity towards c-KIT and PDGFR receptor tyrosine kinases, among other targets, which are believed to contribute to its activity in several types of cancer [16]. This exemplifies how even target-based approaches can yield drugs with unexpected polypharmacology that enhances their therapeutic utility.
Table 2: Phenotypic Screening in Oncology Drug Discovery
| Model System | Key Advantages | Limitations | Translational Relevance |
|---|---|---|---|
| 2D in vitro screening | Cost-effective, reproducible, high-throughput | Does not recapitulate tumor architecture and microenvironment | Fundamental for early anticancer drug development |
| 3D culture systems & patient-derived organoids (PDOs) | Better recapitulate tumor structure, more accurate predictions of clinical response | Challenges in standardization, validation, and regulatory acceptance | Provide more accurate predictions of clinical response |
| Patient-derived xenografts (PDX) | Gold standard for in vivo studies, robust and translationally relevant platforms | Expensive, time-consuming, requires immunodeficient animals | High translational relevance for efficacy testing |
| Hybrid models (PDXO/PDX, PDXDC/PDX) | Allow in vitro and in vivo insights from the same model, improve translational relevance | Complex to establish and maintain | Enhanced translational relevance |
Infectious Diseases
Phenotypic screening has played a crucial role in infectious disease drug discovery, particularly for pathogens with complex biology that defies simple target-based approaches.
Hepatitis C Virus (HCV): The treatment of HCV has been revolutionized by developing combinations of orally available direct-acting antivirals (DAAs) that inhibit HCV replication and clear the virus in >90% of infected patients [16]. Modulators of the HCV protein NS5A such as daclatasvir are a key component of these DAA combinations. The importance of NS5A, which is essential for HCV replication but has no known enzymatic activity, as well as its small-molecule modulators, were initially discovered using an HCV replicon phenotypic screen [16].
Malaria and Artemisinin: Phenotypic screening was instrumental in discovering artemisinin for malaria [10]. Instead of searching for a specific molecular target, researchers assessed the compound's effects on Plasmodium parasites in infected red blood cells. This screening method revealed artemisinin's ability to rapidly reduce parasite load, particularly during the early stages of infection, which was later found to be due to its action on heme and other parasite-specific factors [10]. This discovery occurred when malaria's molecular targets were poorly understood, highlighting phenotypic approaches' power where biological complexity defies simple target-based strategies [10].
Tuberculosis and Diarylquinolines: The discovery of novel anti-tuberculosis agents further demonstrates the power of phenotypic screening for infectious diseases [38]. Researchers identified diarylquinolines through phenotypic screening against Mycobacterium tuberculosis, leading to the development of bedaquiline, which targets the ATP synthase of the bacterium [38].
Experimental Protocols and Methodologies
Phenotypic Screening Workflows
Successful phenotypic screening requires carefully designed experimental protocols and workflows that balance physiological relevance with practical screening considerations. The fundamental process involves multiple stages from model selection to hit validation.
Key Methodological Details
CNS Drug Discovery Protocols: For neurological disorders, phenotypic screening with primary neurons involves quantifying phenotypic alterations such as neurite length, neuronal survival, or changes in fluorescently-tagged protein expression [54]. High-content analysis enables the systematic evaluation of compounds or genetic manipulations on complex neuronal phenotypes. For example, gain-of-function screening using cDNA overexpression has identified key regulators of CNS neurite outgrowth, including KLF transcription factors and STAT3, which promote axon regeneration in mammalian CNS neurons [54].
Oncology Screening Methods: Modern oncology phenotypic screening employs increasingly sophisticated models. The traditional 2D in vitro screening remains fundamental due to cost-effectiveness and reproducibility, but is now complemented by 3D in vitro culture systems, including patient-derived organoids that better recapitulate tumour structure [55]. Additionally, Organ-on-a-chip platforms further enhance physiological relevance and complement conventional animal toxicology models [55]. Patient-derived xenograft (PDX) models remain the gold standard for in vivo studies, offering robust and translationally relevant platforms for efficacy testing [55].
Target Deconvolution Techniques: A critical challenge in phenotypic screening is identifying the molecular target responsible for the observed phenotypic effect. Modern approaches include chemical proteomics, functional genomics, and artificial intelligence (AI)-driven methods [53] [7]. Cellular Thermal Shift Assay (CETSA) has emerged as a leading approach for validating direct target engagement in intact cells and tissues, providing quantitative, system-level validation that bridges the gap between biochemical potency and cellular efficacy [7].
Signaling Pathways and Mechanisms of Action
Phenotypic screening has uncovered novel therapeutic mechanisms that would have been difficult to predict through target-based approaches. The following diagram illustrates key pathways modulated by phenotypic screening-derived drugs across disease areas.
Comparative Analysis: Phenotypic vs. Target-Based Screening
Success Rate Comparison
The debate between phenotypic and target-based screening approaches continues across drug discovery, with each strategy offering distinct advantages and limitations. Analysis of first-in-class medicines reveals the disproportionate contribution of phenotypic approaches to innovative drug discovery.
Table 3: Comparative Analysis of Screening Approaches
| Parameter | Phenotypic Screening | Target-Based Screening |
|---|---|---|
| Starting Point | Disease phenotype in biologically relevant system | Hypothesis about specific molecular target |
| Target Requirement | No prior target knowledge needed | Requires validated molecular target |
| Success in First-in-Class Drugs | Majority of first-in-class drugs (1999-2008) [16] | Minority of first-in-class drugs |
| Novel Target Identification | Can reveal novel targets and mechanisms | Limited to known or hypothesized targets |
| Chemical Space | Unrestricted by target knowledge | Focused on target-binding chemotypes |
| Major Challenges | Target deconvolution, complex assay development | Target validation, physiological relevance |
| Resource Requirements | Higher per assay, but may reduce late-stage attrition | Lower per assay, but higher late-stage failure risk |
| Examples of Success | Risdiplam (SMA), Lenalidomide (cancer), Artemisinin (malaria) | Imatinib (CML), Trastuzumab (breast cancer), HIV antiretrovirals |
Advantages and Limitations
Phenotypic Screening Advantages:
- Expanded Druggable Target Space: Phenotypic strategies have expanded the "druggable target space" to include unexpected cellular processes (pre-mRNA splicing, target protein folding, trafficking, translation, and degradation), novel MoAs for traditional target classes, and revealed new classes of drug targets [16].
- Addressing Biological Complexity: Particularly valuable for complex, polygenic diseases with multiple underlying mechanisms often involving interactions with immune or nervous system components [16].
- Polypharmacology: Can identify molecules engaging multiple targets (polypharmacology), which may be advantageous for complex diseases where single-target approaches have shown limited success [16].
Phenotypic Screening Challenges:
- Target Deconvolution: Identifying the molecular target responsible for phenotypic effects remains a significant hurdle, though advances in chemical proteomics and AI are addressing this challenge [53] [7].
- Assay Complexity: Developing robust, reproducible phenotypic assays that accurately capture disease biology can be technically challenging and resource-intensive [38].
- Translation to Clinical Success: While phenotypic screening has contributed disproportionately to first-in-class drugs, not all phenotypic discoveries successfully translate to clinical benefit [16].
The Scientist's Toolkit: Essential Research Reagents and Materials
Implementing successful phenotypic screening campaigns requires specialized reagents and tools. The following table details key solutions for researchers designing phenotypic screening studies.
Table 4: Essential Research Reagents for Phenotypic Screening
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Patient-derived brain cells | Most accurately recapitulate CNS disease phenotypes | CNS drug discovery, neurological disorders [53] |
| Induced Pluripotent Stem Cells (iPSCs) | Disease-specific cell source for "disease-in-a-dish" modeling | Neurodegenerative diseases, patient-specific models [54] |
| 3D culture systems & organoids | Better recapitulate tumor structure and organization | Oncology drug discovery, personalized medicine [55] |
| Chemogenomic compound libraries | Diverse small molecule collections for screening | Initial hit identification across disease areas [53] |
| Fragment libraries | Smaller, simpler compounds for more tractable target deconvolution | Alternative to conventional compound libraries [53] |
| Cellular Thermal Shift Assay (CETSA) | Validates direct target engagement in intact cells and tissues | Target deconvolution, mechanism confirmation [7] |
| High-content imaging systems | Automated microscopy and image analysis for complex phenotypes | Neurite outgrowth, cell morphology, multiparameter analysis [54] |
| AI and machine learning platforms | Data analysis, pattern recognition, and target prediction | Hit prioritization, target identification, biomarker discovery [53] [7] |
Phenotypic drug discovery has firmly re-established itself as a powerful approach for identifying first-in-class therapies, particularly for diseases with complex or poorly understood biology. The case studies in neurology, oncology, and infectious diseases demonstrate how phenotypic screening can reveal novel therapeutic mechanisms and expand the druggable genome beyond what target-based approaches can achieve. While challenges remain in target deconvolution and assay design, advances in disease modeling, chemical biology, and computational approaches are steadily addressing these limitations.
The future of phenotypic screening lies in integrating these technological innovations—including improved disease models like organoids and organs-on-chips, advanced target identification methods like CETSA, and AI-driven data analysis—to create more predictive and efficient discovery platforms. Rather than viewing phenotypic and target-based approaches as competing strategies, the drug discovery community is increasingly recognizing their complementary value. Strategic deployment of both approaches, guided by the specific biological and therapeutic context, will maximize opportunities for delivering the innovative medicines that patients need.
Target-based drug discovery (TDD) is a foundational strategy in modern therapeutic development, operating on the principle of designing compounds to interact with specific, well-characterized molecular targets. This approach fundamentally differs from phenotypic drug discovery (PDD), which identifies compounds based on their effects on whole cells or organisms without prior knowledge of the specific biological target. The strategic value of TDD lies in its rational framework: by building upon established biological knowledge of disease mechanisms, researchers can precisely design drugs to modulate the activity of proteins, receptors, or nucleic acids critically involved in pathology. This mechanistic precision potentially streamlines optimization and enhances therapeutic specificity, though it requires extensive prior validation of the target's role in disease [2] [3].
The focus of this analysis is a comparative examination of target-based success stories across two distinct therapeutic areas: oncology and antiviral therapy. In oncology, the paradigm is exemplified by immune checkpoint inhibitors, while in antiviral therapy, the emergence of CRISPR-based technologies represents a new frontier. By dissecting these case studies, this guide provides a data-driven comparison of the performance, experimental protocols, and key reagents that underpin successful target-based discovery campaigns, offering a practical resource for research and development professionals.
Oncology Case Study: Immune Checkpoint Inhibitors
Scientific Rationale and Target Validation
The foundation for immune checkpoint inhibitor therapy rests on the seminal discovery that tumors exploit natural immune checkpoint pathways to evade destruction by the host immune system. The key molecular targets in this approach are the cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) and the programmed cell death protein 1 (PD-1) receptor and its ligand (PD-L1). These receptors, expressed on immune cells, normally function as "brakes" on the immune response to prevent autoimmunity and maintain self-tolerance. However, cancer cells frequently upregulate these checkpoint ligands, leading to T-cell exhaustion and allowing tumors to escape immune surveillance [2].
Robust genetic and clinical evidence validated these targets. Preclinical models demonstrated that genetic knockout or antibody-mediated blockade of CTLA-4 or the PD-1/PD-L1 axis resulted in potent anti-tumor immunity. This established a clear mechanistic hypothesis: therapeutic inhibition of these checkpoints would release these innate brakes, thereby restoring T-cell-mediated killing of cancer cells. This target-based rationale enabled the precise development of monoclonal antibodies designed to specifically block these interactions [2].
Key Performance Data and Clinical Impact
The clinical translation of this target-based hypothesis has revolutionized cancer treatment. The table below summarizes the profound impact of first-generation immune checkpoint inhibitors.
Table 1: Clinical Impact of Key Immune Checkpoint Inhibitors
| Target | Example Drug(s) | Key Approved Indications | Representative Clinical Outcome |
|---|---|---|---|
| CTLA-4 | Ipilimumab | Metastatic Melanoma | Long-term survival benefit; ~20% of patients show sustained response >10 years [2]. |
| PD-1 | Nivolumab, Pembrolizumab | Melanoma, Non-Small Cell Lung Cancer, Renal Cell Carcinoma, Hodgkin Lymphoma | Objective response rates of 20-45% across various cancers, often with durable responses [2]. |
| PD-L1 | Atezolizumab, Durvalumab | Urothelial Carcinoma, Non-Small Cell Lung Cancer | Improved progression-free and overall survival, particularly in patients with PD-L1 positive tumors [2]. |
Despite these successes, target-based approaches also reveal their own limitations. A significant challenge is the development of primary and acquired resistance, observed in a substantial proportion of patients. Furthermore, the narrow spectrum of validated immune checkpoint targets constrains broader therapeutic applicability, highlighting the ongoing need for novel target discovery [2].
Experimental Workflow and Key Methodologies
The development of immune checkpoint inhibitors followed a classic target-to-drug workflow, integrating iterative cycles of design, testing, and refinement.
Table 2: Key Experimental Models in Immune Checkpoint Inhibitor Development
| Stage | Model/Assay | Application & Rationale |
|---|---|---|
| Target Identification & Validation | Genetically engineered mouse models (e.g., CTLA-4 or PD-1 knockouts) | Validated the role of checkpoints in immune regulation and established proof-of-concept for blockade [2]. |
| Therapeutic Candidate Screening | In vitro T-cell activation assays with recombinant checkpoint proteins | Measured the ability of candidate antibodies to block protein-protein interactions and enhance T-cell function [2]. |
| Preclinical Efficacy | Syngeneic mouse tumor models | Tested anti-tumor activity of checkpoint blockers in immunocompetent hosts with a functional immune system [55]. |
| Biomarker Development | Immunohistochemistry (IHC) for PD-L1 expression on tumor cells | Identified patient populations more likely to respond to therapy, enabling precision oncology [2] [55]. |
Diagram 1: The PD-1/PD-L1 checkpoint is a key immunosuppressive pathway. Therapeutic antibodies block this interaction, restoring T-cell-mediated tumor cell killing.
Antiviral Case Study: CRISPR-Cas13 for RNA Viruses
Scientific Rationale and Target Selection
The rapid mutation rate of RNA viruses like SARS-CoV-2 and Dengue virus (DENV) presents a formidable challenge for traditional antiviral therapies, which often struggle to keep pace with viral evolution. A modern target-based approach addresses this by leveraging the CRISPR-Cas13 system, which can be programmed to directly target and cleave specific RNA viral genomes. Cas13 is an RNA-guided ribonuclease that, upon recognition of a complementary RNA sequence, cleaves the target RNA. This provides a highly specific and programmable mechanism for suppressing viral replication [56].
The critical step in this strategy is the identification of highly effective and conserved viral genomic sequences to target. This is a classic target-based problem: selecting the optimal molecular target (a specific viral RNA sequence) that is essential for the virus, conserved across variants to minimize escape mutations, and accessible for the Cas13-crRNA complex. To overcome the limitation of conventional empirical screening, an integrated bioinformatics and experimental platform was developed, combining the computational tool CaSilico with CRISPR-Cas13 in vitro detection to rapidly identify potent crRNA guides from thousands of candidates [56].
Key Performance Data and Antiviral Efficacy
This target-based screening platform demonstrated significant efficacy in identifying highly effective antiviral crRNAs. The table below summarizes key performance data from a study targeting Dengue virus (DENV) and SARS-CoV-2.
Table 3: Efficacy of CRISPR-Cas13 Antiviral crRNAs
| Virus Target | Identified crRNA | Experimental Model | Efficacy Outcome |
|---|---|---|---|
| Dengue Virus (DENV) | E−2330 (targeting E protein) | Vero and HepG2 cells | Achieved >90% suppression of viral replication across all four DENV serotypes, demonstrating broad-spectrum activity [56]. |
| SARS-CoV-2 | Multiple candidates via platform | Reporter gene system & cellular models | The platform successfully identified crRNAs with high predictive scores for antiviral activity, validating the screening methodology [56]. |
This platform's primary significance is methodological, offering a faster, more cost-effective, and scalable approach to identifying targets for CRISPR-based antiviral drugs. However, a key limitation is that validation, to date, has been performed primarily in cellular models. Questions regarding in vivo delivery efficiency, potential off-target effects, and immunogenicity remain to be fully addressed in animal models and human trials [56].
Experimental Workflow and Key Methodologies
The workflow for developing CRISPR-based antivirals is a tightly integrated cycle of computational prediction and experimental validation.
Table 4: Core Workflow for CRISPR-Cas13 Antiviral Development
| Stage | Method/Tool | Application & Rationale |
|---|---|---|
| Target Selection & crRNA Design | CaSilico Bioinformatics Tool | Rapidly analyzes viral genomes to predict highly efficient and specific crRNA target sites from thousands of candidates [56]. |
| In Vitro crRNA Potency Screening | CRISPR-Cas13 in vitro detection (e.g., fluorescence-based nucleic acid detection) | Provides a rapid, high-throughput proxy for antiviral efficacy by correlating fluorescence signal intensity with crRNA cleavage activity [56]. |
| In Vitro Antiviral Validation | Viral replication assays in mammalian cell lines (e.g., Vero, HepG2) | Directly measures the ability of selected crRNAs to suppress replication of live virus in relevant cellular models [56]. |
| Delivery System Development | Lipid Nanoparticles (LNPs), Adeno-Associated Viruses (AAVs) | Critical for in vivo application; these vectors are used to package and deliver the Cas13 and crRNA machinery into host cells [56]. |
Diagram 2: Integrated bioinformatics and experimental workflow for identifying highly effective antiviral crRNAs, accelerating the development of CRISPR-based therapies.
Comparative Analysis and Research Toolkit
Cross-Domain Comparison of Target-Based Approaches
While both case studies exemplify the power of a target-based strategy, they differ significantly in their application, maturity, and inherent challenges, as detailed below.
Table 5: Comparative Analysis of Target-Based Approaches in Oncology vs. Antiviral Therapy
| Aspect | Oncology: Immune Checkpoint Inhibitors | Antiviral Therapy: CRISPR-Cas13 |
|---|---|---|
| Target Class | Human cell surface proteins (Receptors: PD-1, CTLA-4) | Viral RNA genomes (Conserved sequences in SARS-CoV-2, DENV) |
| Therapeutic Modality | Monoclonal Antibodies (Biologics) | CRISPR-Cas13 ribonucleoprotein (RNA-targeting) |
| Discovery Timeline | Long (Decades from target discovery to approved therapy) | Greatly compressed (Weeks to identify lead crRNAs via screening platform) |
| Key Challenge | Resistance mechanisms, immune-related adverse events | In vivo delivery efficiency, potential off-target effects, immunogenicity |
| Clinical Stage | Mature (Multiple approved drugs, standard of care) | Preclinical/Emerging (Validation primarily in cellular models) [56] |
| Biomarker Utility | Established (PD-L1 IHC used for patient stratification) | Emerging (Viral sequence conservation as a predictive biomarker for crRNA design) |
| Development Hurdle | High cost of biologic development and manufacturing | Regulatory path for gene therapies is less defined |
The Scientist's Toolkit: Essential Research Reagents and Platforms
The successful implementation of the target-based strategies described relies on a suite of specialized research reagents and platforms.
Table 6: Key Research Reagent Solutions for Target-Based Discovery
| Research Reagent / Platform | Primary Function | Application Context |
|---|---|---|
| Recombinant Immune Checkpoint Proteins (e.g., hPD-1/Fc, hPD-L1/Fc) | In vitro binding and blockade assays; candidate antibody screening and characterization. | Oncology [2] |
| CRISPR-Cas13 Protein & crRNA Libraries | The core effector complex for programmed RNA cleavage; libraries enable high-throughput screening against viral genomes. | Antiviral Therapy [56] |
| Patient-Derived Xenograft (PDX) Models | In vivo models created by implanting human tumor tissue into immunodeficient mice, providing a more clinically relevant platform for efficacy testing. | Oncology [55] |
| CETSA (Cellular Thermal Shift Assay) | Measures target engagement and binding within intact cells, providing physiologically relevant confirmation of drug-target interaction. | Multi-domain, for validation [7] |
| AI/ML Drug Discovery Platforms (e.g., Exscientia, Insilico Medicine) | Utilize generative chemistry and predictive modeling to design novel compounds against specific targets, drastically shortening early-stage timelines. | Multi-domain, for candidate design [21] |
| Organoid & 3D Cell Culture Models | Advanced in vitro models that better recapitulate tumor structure or viral infection, providing more accurate predictions of clinical response. | Multi-domain, for efficacy & toxicity [5] [55] |
The case studies of immune checkpoint inhibitors in oncology and CRISPR-Cas13 platforms for antiviral therapy powerfully demonstrate the enduring strength and adaptability of the target-based drug discovery paradigm. The oncology story showcases a mature, clinically transformative application where targeting specific human immune receptors has unlocked durable responses in multiple cancers. In contrast, the antiviral case study illustrates a nimble, modern approach where targeting the viral genome itself with programmable technology offers a promising path to address rapidly evolving pathogens.
A critical insight from this comparison is that the success of the target-based approach is heavily dependent on the quality of the initial target validation and the availability of sophisticated tools—from bioinformatics platforms like CaSilico to predictive AI models—to guide the discovery process. While challenges remain, including resistance in oncology and delivery in antiviral therapy, the continued integration of advanced computational and experimental technologies is refining the TDD paradigm. This evolution promises to enhance its precision, expand the scope of "druggable" targets, and ultimately deliver more effective and targeted therapies to patients.
Drug discovery has historically been guided by two principal strategies: phenotypic drug discovery (PDD) and target-based drug discovery (TDD). Phenotypic screening identifies active compounds based on measurable biological responses in complex cellular or organismal systems, often without prior knowledge of the specific molecular target [2] [16]. This approach has been particularly productive for discovering first-in-class medicines, uncovering novel mechanisms of action, and targeting complex, polygenic diseases [16] [1]. In contrast, target-based discovery begins with a well-characterized molecular target and employs rational drug design to develop highly specific therapeutic agents [2]. While TDD offers precision and mechanistic clarity, its success is fundamentally constrained by the availability and validation of druggable targets [2] [16].
The contemporary drug discovery landscape is being reshaped by the convergence of these established approaches with transformative technologies. Artificial intelligence (AI) and machine learning (ML) are now enabling the integrative analysis of massive, high-dimensional datasets, while multi-omics technologies (genomics, transcriptomics, proteomics, metabolomics) provide comprehensive molecular portraits of disease states [57] [58]. Together, these advances are forging a new path toward precision medicine, where therapeutic strategies are increasingly tailored to individual patient molecular profiles [58] [59]. This guide examines how these technological forces are redefining screening strategies, moving the field beyond the traditional phenotypic versus target-based dichotomy toward integrated, data-driven workflows that enhance predictive accuracy, accelerate discovery timelines, and ultimately improve therapeutic success rates.
Traditional Screening Approaches: A Comparative Baseline
Defining Characteristics and Historical Success
The distinct philosophies underlying phenotypic and target-based screening have yielded different but complementary success patterns in drug discovery. An analysis of new FDA-approved treatments between 1999 and 2008 revealed that PDD was responsible for 28 first-in-class small molecule drugs, compared to 17 from target-based methods [1]. This trend has continued, with PDD contributing to the development of 58 out of 171 total drugs approved from 1999 to 2017, while traditional TDD accounted for 44 approvals [1].
Table 1: Comparative Analysis of Traditional Screening Approaches
| Parameter | Phenotypic Drug Discovery (PDD) | Target-Based Drug Discovery (TDD) |
|---|---|---|
| Core Strategy | Identification of compounds based on functional effects in biologically complex systems [2] [16] | Rational design against predefined molecular targets with known functions [2] |
| Target Requirement | No prior target knowledge needed; target-agnostic [16] [1] | Well-validated, druggable target required before screening [2] |
| Key Advantages | Discovers novel mechanisms; captures system complexity and polypharmacology; historically more productive for first-in-class drugs [2] [16] [1] | Clear mechanism of action; streamlined optimization; reduced risk of off-target effects [2] |
| Primary Limitations | Target deconvolution challenges; complex assay development; potentially longer discovery timelines [2] [16] | Limited to known biology; may miss complex system-level interactions; susceptible to compensatory pathways [2] [16] |
| Notable Examples | Thalidomide analogs (lenalidomide, pomalidomide), risdiplam, daclatasvir, ivacaftor/lumacaftor [2] [16] [1] | Imatinib, sunitinib, pazopanib [16] [31] |
| Therapeutic Areas | Particularly effective for CNS disorders, infectious diseases, cancer, and rare genetic disorders [16] [1] | Broad applicability across therapeutic areas with validated targets [2] |
Key Experimental Protocols in Traditional Screening
Phenotypic Screening Workflow typically begins with establishing a disease-relevant biological system (cell-based models, tissue explants, or whole organisms) that recapitulates key pathological features. Following compound exposure, multi-parametric readouts (cell viability, morphology, cytokine secretion, etc.) are quantified using high-content imaging, transcriptomic profiling, or functional assays [16] [1]. Hit compounds are then optimized through iterative medicinal chemistry cycles, with target deconvolution often pursued in parallel using methods like chemical proteomics, CRISPR screening, or transcriptomic profiling [16].
Target-Based Screening Workflow initiates with target identification and validation, followed by development of high-throughput screening assays (binding assays, enzymatic activity measurements). Structure-based drug design leveraging X-ray crystallography or cryo-EM structures often guides hit-to-lead optimization [2] [31]. Candidate compounds are subsequently evaluated in increasingly complex biological systems to assess cellular activity and therapeutic potential [2].
The Technological Transformation: AI and Multi-Omics Integration
AI-Driven Screening Platforms
Artificial intelligence has progressed from experimental curiosity to clinical utility in drug discovery, with multiple AI-designed therapeutics now in human trials [21]. Leading AI-driven platforms employ diverse technological strategies:
- Generative Chemistry (Exscientia, Insilico Medicine): Uses deep learning models trained on vast chemical libraries to design novel molecular structures satisfying specific target product profiles, significantly compressing design-make-test-learn cycles [21].
- Phenomics-First Systems (Recursion): Leverages high-content cellular imaging and AI-based pattern recognition to identify compounds that reverse disease-associated phenotypes [21].
- Physics-Plus-ML Design (Schrödinger): Combines molecular simulations with machine learning to predict binding affinities and optimize compound properties [21].
- Convolutional Neural Networks (AtomNet): Analyzes 3D structural information of protein-ligand interactions to predict binding probabilities across vast chemical spaces [33].
These platforms demonstrate tangible success. Exscientia has designed eight clinical compounds, while Insilico Medicine's generative-AI-designed idiopathic pulmonary fibrosis drug progressed from target discovery to Phase I trials in just 18 months [21]. AtomNet's convolutional neural network successfully identified novel hits across 318 projects, achieving an average hit rate of 7.6% in academic collaborations and 6.7% for internal targets, comparable to traditional HTS [33].
Multi-Omics Data Integration
Multi-omics technologies dissect the biological continuum from genetic blueprint to functional phenotype through interconnected analytical layers [57] [58]:
- Genomics identifies DNA-level alterations including single-nucleotide variants (SNVs), copy number variations (CNVs), and structural rearrangements.
- Transcriptomics reveals gene expression dynamics through RNA sequencing, quantifying mRNA isoforms and fusion transcripts.
- Proteomics catalogs the functional effectors of cellular processes, identifying post-translational modifications and signaling pathway activities.
- Metabolomics profiles small-molecule metabolites, providing real-time snapshots of physiological states [57] [58].
The integration of these diverse data layers encounters formidable computational challenges rooted in their intrinsic heterogeneity, including dimensional disparities, temporal dynamics, platform-specific artifacts, and missing data [57] [58]. AI and machine learning have emerged as essential tools to overcome these hurdles, with approaches including:
- Early Integration: Merging all omics features into one massive dataset before analysis [58].
- Intermediate Integration: Transforming each omics dataset into manageable representations before combination [58].
- Late Integration: Building separate predictive models for each omics type and combining their predictions [58] [39].
Experimental Data on Multi-Modal Predictions
A large-scale empirical study evaluated the predictive power of chemical structures (CS), cell morphology profiles (MO) from Cell Painting, and gene expression profiles (GE) from L1000 assays for predicting compound bioactivity across 270 assays [39]. The results demonstrated significant complementarity between these profiling modalities.
Table 2: Performance Comparison of Screening Modalities in Predicting Bioactivity
| Profiling Modality | Assays Predicted (AUROC >0.9) | Key Strengths | Limitations |
|---|---|---|---|
| Chemical Structure (CS) Alone | 16 assays (6%) | No wet lab experimentation required; enables virtual screening of non-existent compounds [39] | Limited to known structure-activity relationships; misses biological context |
| Morphology Profiles (MO) Alone | 28 assays (10%) | Captures system-level cellular responses; functional readout [39] | Requires physical compounds and experimentation |
| Gene Expression (GE) Alone | 19 assays (7%) | Direct measurement of transcriptional responses; mechanistic insights [39] | Limited scalability; may miss post-transcriptional regulation |
| CS + MO Combined | 31 assays (11.5%) | More than doubles prediction ability of CS alone; captures both structural and functional information [39] | Requires integration of computational and experimental workflows |
| All Three Modalities | 21% of assays | Maximum coverage of predictable assays; leverages full complementarity [39] | Most resource-intensive approach |
The study found that morphological profiles predicted the largest number of assays individually (28 vs 19 for GE and 16 for CS) at high accuracy thresholds (AUROC > 0.9) [39]. Critically, combining morphological profiles with chemical structures more than doubled the number of predictable assays compared to chemical structures alone (31 vs 16) [39]. In practice, the accuracy required depends on the application; at more permissive thresholds (AUROC > 0.7), chemical structures alone could predict approximately 37% of assays, while combination with phenotypic data increased this to 64% [39].
Integrated Workflows: The New Screening Paradigm
The convergence of AI, multi-omics, and traditional screening approaches has given rise to integrated workflows that leverage the strengths of each component. The following diagram illustrates how these elements combine in a modern drug discovery pipeline:
Integrated Drug Discovery Workflow
This integrated approach enables researchers to move beyond siloed screening strategies toward a unified framework where multi-omics data provides molecular context, phenotypic screening captures system-level biology, target-based approaches offer mechanistic precision, and AI serves as the unifying engine that detects patterns and generates predictive models across these diverse data layers [2] [57] [58].
The Scientist's Toolkit: Essential Research Reagents and Technologies
Table 3: Key Research Reagent Solutions for Modern Screening Approaches
| Technology/Reagent | Primary Function | Application Context |
|---|---|---|
| Cell Painting Assay | High-content morphological profiling using fluorescent dyes to label cellular components [39] | Phenotypic screening; mechanism of action studies; compound bioactivity prediction |
| L1000 Assay | High-throughput gene expression profiling measuring ~1,000 landmark transcripts [39] | Transcriptomic profiling; mechanism of action prediction; connectivity mapping |
| Synthesis-on-Demand Chemical Libraries | Access to vast chemical spaces (billions of compounds) not available in physical screening collections [33] | AI-powered virtual screening; expansion of accessible chemical diversity |
| CRISPR Screening Tools | High-throughput functional genomics for target identification and validation [16] | Target deconvolution from phenotypic screens; genetic vulnerability discovery |
| Proteomics Kits (Mass Spectrometry) | Protein identification, quantification, and post-translational modification analysis [57] [58] | Multi-omics integration; pathway activity analysis; biomarker discovery |
| Single-Cell Multi-Omics Platforms | Simultaneous measurement of multiple molecular layers (genome, transcriptome, epigenome) at single-cell resolution [57] | Tumor heterogeneity mapping; microenvironment analysis; rare cell population studies |
| Graph Neural Networks (GNNs) | Machine learning method for analyzing network-structured biological data [57] [58] | Integration of protein-protein interaction networks; multi-omics data analysis |
| Multi-Modal Transformers | AI architecture for integrating diverse data types (images, sequences, numerical data) [57] | Cross-modal data fusion; radiogenomic integration; clinical data analysis |
The future landscape of drug screening is unequivocally integrative, leveraging the complementary strengths of phenotypic and target-based approaches through the unifying power of AI and multi-omics technologies. The empirical evidence demonstrates that combining chemical structure information with phenotypic profiling more than doubles the number of predictable assays compared to either approach alone [39]. Furthermore, AI-driven screening platforms have demonstrated robust performance across hundreds of diverse targets, achieving hit rates comparable to traditional HTS while accessing vastly larger chemical spaces [33].
As these technologies mature, the distinction between phenotypic and target-based screening continues to blur, replaced by adaptive workflows that incorporate functional and mechanistic insights at multiple stages of the discovery process [2]. The emergence of clinical-stage AI-designed compounds signals a paradigm shift in the speed and efficiency of early drug discovery [21]. However, successful translation of these advances will require continued attention to challenges of data quality, model interpretability, and biological validation [57] [59].
For researchers and drug development professionals, this evolving landscape demands familiarity with both established screening principles and emerging computational tools. The most successful strategies will be those that strategically combine the unbiased discovery potential of phenotypic screening, the mechanistic clarity of target-based approaches, and the predictive power of AI-driven multi-omics integration—ultimately accelerating the delivery of precision medicines to patients.
Conclusion
The debate between phenotypic and target-based screening is not about declaring a single winner, but about strategically deploying each method based on project goals and biological context. Evidence confirms that phenotypic screening is a powerful engine for discovering first-in-class drugs with novel mechanisms, as demonstrated by recent therapies for spinal muscular atrophy and cystic fibrosis. Conversely, target-based screening excels at efficiently optimizing drugs for validated targets. The future of drug discovery lies in moving beyond a rigid dichotomy and adopting integrated, hybrid workflows. Leveraging AI for target prediction and data analysis, alongside advanced disease models, will enable researchers to harness the unbiased discovery potential of phenotypic screening while achieving the precision of target-based approaches. This synergistic strategy promises to accelerate the delivery of innovative therapies to patients.
References
- 1. Recent Successes in AI Phenotypic Drug Discovery and ... [https://ardigen.com/recent-successes-in-phenotypic-drug-discovery-and-the-future-of-ml-ai-methods/]
- 2. Phenotypic and targeted drug discovery in immune therapeutics [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03914b]
- 3. A data-driven journey using results from target-based drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062751/]
- 4. Discovery of novel anti-fibrotics through phenotypic ... [https://www.sciencedirect.com/science/article/pii/S1359644625001631]
- 5. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 6. CRISPR screening redefines therapeutic target ... [https://www.sciencedirect.com/science/article/pii/S2095177925001741]
- 7. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 8. Improving phenotypic screening | Nature Chemical Biology [https://www.nature.com/articles/s41589-025-02093-x]
- 9. Phenotypic Screening: A Powerful Tool for Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/phenotypic-screening-a-powerful-tool-for-drug-discovery-398572]
- 10. Target Identification vs. Phenotypic Screening in Drug ... [https://pharmafeatures.com/strategic-dichotomy-target-identification-vs-phenotypic-screening-in-drug-discovery/]
- 11. A precise comparison of molecular target prediction methods [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d5dd00199d]
- 12. Target-aware 3D molecular generation based on guided ... [https://www.nature.com/articles/s41467-025-63245-0]
- 13. Target screening and optimization of candidate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12098522/]
- 14. Label-free target identification in drug discovery via ... [https://www.sciencedirect.com/science/article/abs/pii/S1367593118301716]
- 15. The limitations of small molecule and genetic screening in ... [https://www.sciencedirect.com/science/article/pii/S2451945625003459?dgcid=rss_sd_all]
- 16. Phenotypic Drug Discovery: Recent successes, lessons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9708951/]
- 17. Delay skin aging with target -based drug discovery and computational... [https://www.cosmeticsdesign-europe.com/Headlines/Promotional-features/Delay-skin-aging-with-target-based-drug-discovery-and-computational-modeling/]
- 18. Phenotypic vs. target-based drug discovery for first-in-class ... [https://pubmed.ncbi.nlm.nih.gov/23511784/]
- 19. Advances of the Target-Based and Phenotypic Screenings ... [https://www.sciltp.com/journals/ijddp/articles/2504000136]
- 20. Sequence enrichment profiles enable target - agnostic antibody... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10261905/]
- 21. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 22. PhenoModel: A multimodal phenotypic drug design ... [https://www.sciencedirect.com/science/article/pii/S2211383525006446]
- 23. Scalable, compressed phenotypic screening using pooled ... [https://www.nature.com/articles/s41587-024-02403-z]
- 24. A statistical framework for high-content phenotypic profiling ... [https://www.nature.com/articles/s42003-022-04343-3]
- 25. Transforming Access to Human-Relevant Models [https://de.moleculardevices.com/lab-notes/3d-biology/transforming-access-to-human-relevant-models]
- 26. High Throughput Screening Market [https://www.futuremarketinsights.com/reports/high-throughput-screening-market]
- 27. High Throughput Screening (HTS) Market Size 2025-2029 [https://www.technavio.com/report/high-throughput-screening-market-industry-analysis]
- 28. Drug Discovery SaaS Platforms Market 2025 Trends and ... [https://www.towardshealthcare.com/insights/drug-discovery-saas-platforms-market-sizing]
- 29. Drug Discovery Saas Platforms Market Growth and ... [https://www.globenewswire.com/news-release/2025/10/13/3165688/0/en/Drug-Discovery-Saas-Platforms-Market-Growth-and-Competitive-Landscape-Insight-Towards-Healthcare.html]
- 30. Development of a comparative high-throughput screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12657333/]
- 31. Target screening and optimization of candidate ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1467504/full]
- 32. Phenotypic Versus Target-Based Screening for Drug ... [https://www.technologynetworks.com/drug-discovery/articles/phenotypic-versus-target-based-screening-for-drug-discovery-300037]
- 33. AI is a viable alternative to high throughput screening [https://www.nature.com/articles/s41598-024-54655-z]
- 34. Phenotypic Screening - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/phenotypic-screening]
- 35. The Art of Finding the Right Drug Target: Emerging Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11334170/]
- 36. Novel Drug Targets From Phenotypic Screening [https://www.ddw-online.com/novel-drug-targets-from-phenotypic-screening-1440-201710/]
- 37. The Deconvolution Revolution: Strategies for Target ... [https://momentum.bio/content/the-deconvolution-revolution-strategies-for-target-identification/]
- 38. Opportunities and challenges in phenotypic drug discovery [https://www.nature.com/articles/nrd.2017.111]
- 39. Predicting compound activity from phenotypic profiles and ... [https://www.nature.com/articles/s41467-023-37570-1]
- 40. Evidential deep learning-based drug-target interaction ... [https://www.nature.com/articles/s41467-025-62235-6]
- 41. Review Hit Triage and Validation in Phenotypic Screening [https://www.sciencedirect.com/science/article/pii/S2451945620303317]
- 42. Integrating artificial intelligence in drug discovery and early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11909971/]
- 43. Use of artificial intelligence to enhance phenotypic drug ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644621000404]
- 44. Target Identification of Compounds from a Cell Viability ... [https://www.sciencedirect.com/science/article/pii/S2472555222070721]
- 45. From Hits to Leads: Improving Early Drug Discovery With ... [https://www.technologynetworks.com/drug-discovery/blog/from-hits-to-leads-improving-early-drug-discovery-with-better-tools-404996]
- 46. AI-driven drug discovery using a context-aware hybrid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518806/]
- 47. Benchmarking R&D success rates of leading ... [https://www.sciencedirect.com/science/article/pii/S1359644625000042]
- 48. Approval success rates of drug candidates based on target, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8212735/]
- 49. Parsing clinical success rates [https://www.nature.com/articles/nrd.2016.136]
- 50. Dynamic clinical trial success rates for drugs in the 21st ... [https://www.nature.com/articles/s41467-025-64552-2]
- 51. Estimation of clinical trial success rates and related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6409418/]
- 52. Global first-in-class drugs approved in 2023–2024 [https://www.sciencedirect.com/science/article/pii/S2666675825000049]
- 53. Review Phenotypic approaches for CNS drugs [https://www.sciencedirect.com/science/article/pii/S0165614724001883]
- 54. Phenotypic screening with primary neurons to identify drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5243932/]
- 55. Advancing oncology drug development: Innovative ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X25002094]
- 56. Advancing precision antiviral therapy - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590221/]
- 57. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 58. Integrating Multi-Omics for Precision Medicine: 2025 Guide [https://lifebit.ai/blog/integrating-multi-modal-genomic-and-multi-omics-data-for-precision-medicine/]
- 59. Artificial Intelligence and Multi-Omics in Pharmacogenomics [https://www.sciencedirect.com/science/article/pii/S2949761225000537]