Kinetic Profiling in Cytotoxicity Phenotypic Screening: Advancing Predictive Drug Discovery
This article explores the integration of kinetic profiling with phenotypic cytotoxicity screening, a transformative approach for modern drug discovery.
Kinetic Profiling in Cytotoxicity Phenotypic Screening: Advancing Predictive Drug Discovery
Abstract
This article explores the integration of kinetic profiling with phenotypic cytotoxicity screening, a transformative approach for modern drug discovery. Tailored for researchers and drug development professionals, it details how real-time, dynamic assessment of cellular responses moves beyond single-time-point assays to enhance the prediction of compound toxicity and efficacy. The scope covers foundational principles, advanced methodological applications including high-content imaging and live-cell analysis, strategies for troubleshooting and data optimization, and the critical validation of these approaches against traditional methods. By providing a comprehensive framework, this resource aims to equip scientists with the knowledge to implement kinetic strategies, thereby improving the identification of high-quality, safe therapeutic candidates and de-risking the development pipeline.
The Resurgence of Phenotypic Screening and the Case for Kinetic Cytotoxicity Assessment
Phenotypic Screening's Role in Discovering First-in-Class Medicines
Phenotypic screening is a drug discovery approach that identifies bioactive compounds based on their ability to produce a desired observable change in a biological system, without requiring prior knowledge of a specific molecular target [1]. Unlike target-based drug discovery, which focuses on modulating predefined proteins, phenotypic screening evaluates how compounds influence complex biological networks as a whole [2] [3].
This method has re-emerged as a powerful strategy following a 2011 review showing that between 2000 and 2008, phenotypic approaches yielded 28 first-in-class small molecule drugs compared to 17 from target-based strategies [3]. Modern phenotypic drug discovery combines this foundational concept with contemporary tools including high-content imaging, CRISPR functional genomics, and artificial intelligence, making it a critical testing ground for technical innovations in the life sciences [2] [3].
Troubleshooting Guides
Issue 1: Cytotoxic Compound Interference in Assay Readouts
Problem: Active compounds identified in primary screens demonstrate non-specific cytotoxicity rather than targeted modulation of the desired phenotype.
Troubleshooting Steps:
- Implement Early Cytotoxicity Counter-Screening: Profile your compound library against "normal" cell lines (e.g., HEK 293, NIH 3T3) in parallel to your disease model. Use a minimum of four normal cell lines to assess pan-activity and selectivity [4].
- Utilize Multiplexed Viability Assays: Incorporate a real-time, kinetic viability endpoint such as ATP-based luminescence (CellTiter-Glo) or caspase activation biosensors (e.g., NucView) to differentiate cytotoxic from cytostatic or phenotype-modifying effects [4] [5].
- Analyze Concentration-Response Relationships: Classify compounds based on full concentration-response curves. Triage compounds that show classic cytotoxic curves (Class -1.1, -1.2) with high efficacy (>80% inhibition) across multiple normal cell lines [4].
Prevention: Pre-screen chemical libraries for cytotoxicity before initiating large-scale phenotypic campaigns. One study profiling >100,000 compounds found a significant portion exhibited cytotoxic effects, which can be flagged and deprioritized upfront [4].
Issue 2: Challenges with Hit Validation and Target Deconvolution
Problem: Confirming that a phenotypic hit is acting "on-target" and identifying its mechanism of action (MoA) is complex and time-consuming.
Troubleshooting Steps:
- Employ Kinetic Profiling Early: Use live-cell, impedance-based systems (e.g., xCELLigence) to generate time-dependent cell response profiles (TCRPs). Compounds with similar mechanisms of action often cluster based on similar TCRPs, providing predictive mechanistic information before formal target identification [6].
- Implement Orthogonal Genetic Screens: Combine small-molecule screening with CRISPR/Cas9-based functional genomics. A genome-wide knockout screen (e.g., using a library with >76,000 sgRNAs) can identify genes whose mutation rescues or enhances the compound-induced phenotype, revealing potential targets or pathway members [7].
- Apply Multi-Omics Integration: After hit confirmation, use transcriptomic, proteomic, and phosphoproteomic profiling to build a comprehensive signature of compound activity. Tools like the Connectivity Map can help link this signature to known MoAs [8] [9].
Prevention: Design secondary assays that are mechanistically informative from the start. High-content imaging that captures multiple parameters (e.g., morphology, biomarker localization) provides a rich dataset for MoA hypothesis generation even before target deconvolution begins [5].
Issue 3: Poor Translation from In Vitro Models to Clinical Relevance
Problem: Hits identified in simplified 2D cell models fail to show efficacy in more physiologically relevant systems or in vivo.
Troubleshooting Steps:
- Advance Your Disease Model: Transition from 2D monocultures to more complex models such as 3D organoids, patient-derived primary cells, or co-culture systems that better recapitulate the tumor microenvironment or tissue architecture [3] [1].
- Incorporate Phenotypic Profiling in Complex Models: Use high-content imaging and analysis pipelines adapted for 3D and co-culture formats. While throughput is lower, the increased physiological relevance helps prioritize compounds with a higher probability of clinical success [5].
- Validate with Kinetic Live-Cell Assays: Kinetic analysis in live cells using reagents like NucView (for apoptosis) allows you to correlate the timing of phenotypic response with the in vivo pharmacokinetic properties of the hit, helping to predict optimal dosing schedules earlier [5].
Prevention: Invest in developing a high-value, disease-relevant biological system for the primary screen. "We really need to make sure that these cell models are of high value... We need to find a way to recreate the disease in a microplate. That way we can expect higher translation to patients," advises Fabien Vincent, Associate Research Fellow at Pfizer [3].
Frequently Asked Questions
Q1: When should I choose a phenotypic screening approach over a target-based one? A phenotypic approach is particularly advantageous when: 1) no attractive molecular target is known for your disease of interest; 2) the project goal is to obtain a first-in-class drug with a novel mechanism of action; or 3) the disease involves complex, polygenic pathways with potential redundancies and compensatory mechanisms [2] [9] [1]. It is especially well-suited for uncovering unexpected biology and expanding "druggable" target space [2].
Q2: What are the key considerations for setting up a high-throughput phenotypic screen?
- Biological Model: Select the most physiologically relevant model feasible for your throughput (e.g., iPSC-derived cells, 3D cultures) [1].
- Readout: Choose a high-content, information-rich readout (e.g., multiparameter imaging, transcriptomic profiling) that robustly captures the desired phenotype [8] [5].
- Library Design: Consider using annotated libraries (compounds with known MoA) alongside diverse chemical libraries to facilitate early MoA insights [4].
- Counter-Screens: Plan cytotoxicity and assay-interference counter-screens (e.g., luciferase inhibition assay) from the beginning to triage false positives [4].
Q3: How is AI transforming phenotypic screening? AI and machine learning are addressing key bottlenecks. For example, the DrugReflector model uses a closed-loop active reinforcement learning framework trained on transcriptomic signatures to predict compounds that induce desired phenotypic changes. This approach can improve hit rates by an order of magnitude compared to screening random libraries, enabling smaller, more focused, and more efficient screening campaigns [8] [9].
Q4: Can phenotypic screening be used for discovering combination therapies? Yes, phenotypic screening is a powerful tool for identifying rational drug combinations. Dose-ratio matrix screening in complex biological assays, followed by analysis using methods like the combination index theorem, can systematically identify synergistic, additive, or antagonistic effects. This approach is valuable for overcoming redundancy in disease pathways and addressing inherent or acquired resistance [5].
Quantitative Data and Protocols
Cytotoxicity Profiling of Screening Libraries
Large-scale cytotoxicity profiling provides essential reference data for triaging non-selectively cytotoxic compounds. The table below summarizes hit rates from profiling nearly 10,000 annotated and over 100,000 diverse library compounds [4].
Table 1: Cytotoxicity Hit Rates Across Cell Lines
| Cell Line | Type | Cytotoxicity Hit Rate (Annotated Library) | Cytotoxicity Hit Rate (Diversity Library) |
|---|---|---|---|
| HEK 293 | Normal (Embryonic Kidney) | Reported in study | ~1% |
| NIH 3T3 | Normal (Fibroblast) | Reported in study | ~1% |
| CRL-7250 | Normal (Fibroblast) | Reported in study | N/A |
| HaCat | Normal (Keratinocyte) | Reported in study | N/A |
| KB 3-1 | Cancer (HeLa subline) | Reported in study | N/A |
Note: The complete quantitative data for the annotated library is available in the source material [4]. The diversity library showed a lower hit rate, but the absolute number of cytotoxic compounds was significant due to the large library size.
Experimental Protocol: Kinetic Cell-Based Morphological Screening
This protocol uses impedance-based readouts to monitor the temporal effects of compounds, providing mechanistic information through kinetic profiling [6].
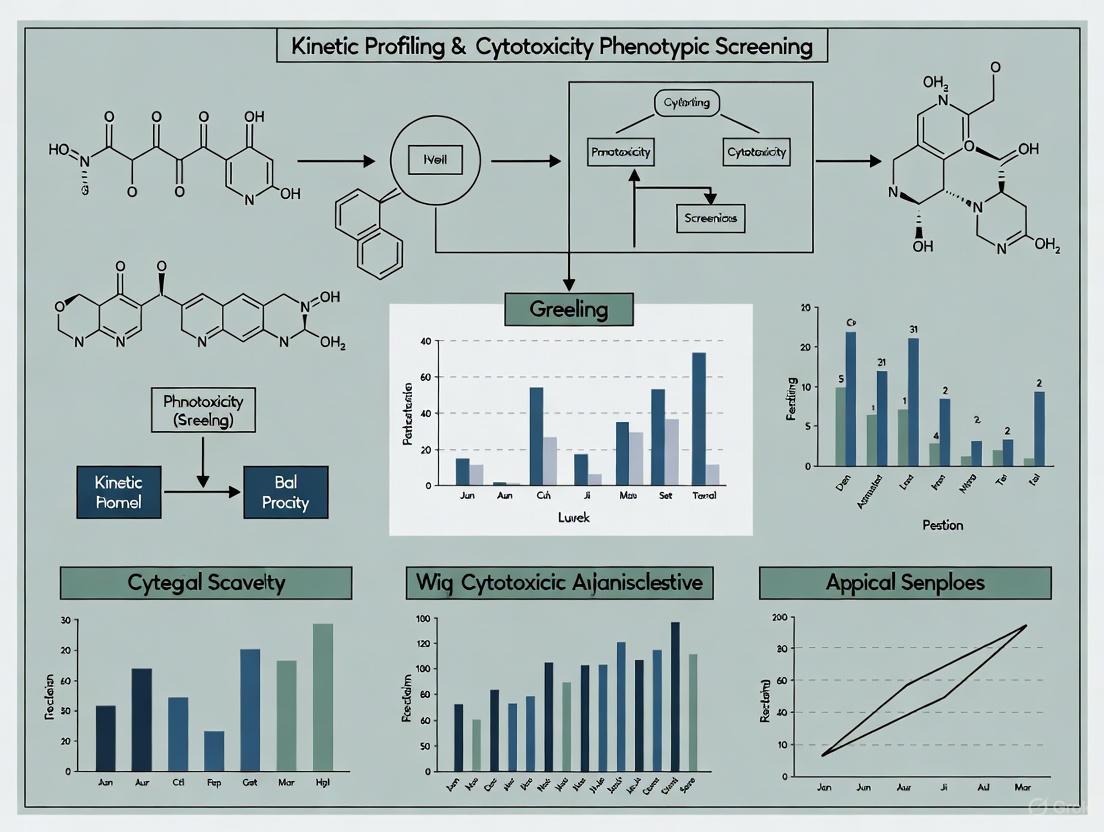
Workflow Overview: The following diagram illustrates the key steps in kinetic phenotypic screening leading to hit clustering and mechanistic prediction.
Key Materials:
- Equipment: Real-time cell analyzer (e.g., xCELLigence RTCA), automated liquid handler, CO2 incubator.
- Reagents: Appropriate cell line, compound library, cell culture medium and supplements.
- Software: Software for analyzing time-course data and performing hierarchical clustering.
Procedure:
- Cell Seeding: Seed cells in specialized 96- or 384-well E-plates that contain integrated microelectrodes. Allow cells to adhere and establish a stable baseline impedance signal (typically 24 hours).
- Compound Addition: Using an automated liquid handler, add compounds from your library across a range of concentrations (e.g., 3-4 logs). Include controls (DMSO vehicle and reference compounds with known mechanisms).
- Kinetic Data Acquisition: Place the E-plate in the analyzer inside the incubator. Monitor and record the impedance value (reported as Cell Index) continuously for 48-72 hours. The instrument typically takes readings every 15-30 minutes.
- Profile Generation: For each compound, normalize the Cell Index data over time to the point of compound addition to generate its unique TCRP.
- Data Analysis and Clustering: Use hierarchical clustering algorithms to group compounds with highly similar TCRPs. Co-clustering of a hit with compounds of known MoA provides a strong, predictive hypothesis for its own mechanism of action [6].
The Scientist's Toolkit
Table 2: Essential Research Reagents and Solutions
| Reagent / Solution | Function in Phenotypic Screening |
|---|---|
| CRISPR/Cas9 Genome-Wide Library (e.g., >76,000 sgRNAs) | Enables genome-wide knockout screens to identify genes essential for a phenotype, aiding in target identification and validation [7]. |
| CellTiter-Glo or Other Viability Assay Reagents | Provides a luminescent or fluorescent endpoint for quantifying ATP levels, a marker of cell viability, essential for cytotoxicity counter-screening [4]. |
| High-Content Imaging-Compatible Dyes (e.g., for nuclei, cytoskeleton, organelles) | Allow for multiplexed, multiparameter analysis of cell morphology and phenotype in fixed or live cells [5] [1]. |
| Real-Time Caspase Biosensors (e.g., NucView) | Enable kinetic profiling of apoptosis induction in live cells, helping to differentiate specific MoAs from general cytotoxicity [5]. |
| Impedance-Based Monitoring Systems (e.g., xCELLigence) | Facilitate label-free, kinetic monitoring of cell responses (proliferation, death, morphology) for mechanistic clustering of hits [6]. |
| Annotated Compound Libraries (e.g., FDA-approved drugs, known bioactives) | Serve as reference sets for MoA prediction via profiling and are valuable tools for drug repurposing efforts [4]. |
Kinetic profiling represents a transformative approach in cytotoxicity phenotypic screening, moving beyond traditional single time-point analyses to capture the dynamic response of cells to compound exposure over time. In modern drug discovery, cytotoxicity profiling of chemical libraries at an early stage is essential for increasing the likelihood of candidate success, helping researchers prioritize molecules with little or no cytotoxicity for downstream evaluation [4]. Unlike endpoint measurements that provide a static snapshot, kinetic profiling enables researchers to quantify the temporal progression of cell death, viability, and metabolic changes, offering richer data for distinguishing between specific pharmacological effects and general cytotoxic responses. This approach is particularly valuable in phenotypic screening, where understanding the dynamics of cellular response can provide critical insights into mechanism of action and improve the prediction of in vivo outcomes [2] [10].
Core Principles of Kinetic Profiling
Temporal Resolution and Dynamic Monitoring
Kinetic profiling requires continuous or frequent-interval monitoring of cellular parameters throughout the exposure period. This principle emphasizes that the timing and rate of cytotoxic response can be as informative as the final outcome. For example, different mechanisms of cell death (apoptosis, necrosis, pyroptosis) often exhibit distinct kinetic signatures that can be discriminated through proper temporal monitoring.
Multiparametric Assessment
True kinetic profiling integrates multiple complementary readouts to capture different aspects of cellular health and function. These typically include:
- Metabolic activity (e.g., ATP levels via CellTiter-Glo)
- Membrane integrity
- Morphological changes
- Specific pathway activation markers
Contextual Relevance
The kinetic parameters derived must be interpreted within the specific biological context of the assay system, including cell type, culture conditions, and compound exposure protocols. Research demonstrates that spatial organization significantly impacts cell signaling, requiring quantitative models that appreciate the importance of spatial organization in cellular membranes [11].
Quantitative Parameter Extraction
Kinetic profiling emphasizes derivation of quantitative parameters that describe the dynamics of cellular response, such as:
- EC50 values over time
- Maximum response rates (Vmax)
- Lag times before response initiation
- Area Under the Curve (AUC) for response trajectories
Essential Research Reagent Solutions
Table 1: Key Research Reagents for Kinetic Profiling in Cytotoxicity Screening
| Reagent/Assay | Function in Kinetic Profiling | Application Notes |
|---|---|---|
| CellTiter-Glo Luminescent Assay | Quantifies ATP levels as a marker of metabolically active cells | Used in high-throughput cytotoxicity profiling of compound libraries [4] |
| Pro-chromogenic substrates (e.g., indole-3-carboxaldehydes) | Enzyme activity detection through colorimetric change | Enables rapid, convenient screening adaptable for large sample numbers [12] |
| Firefly luciferase reporter systems | Monitoring specific pathway activities | Requires counter-screening for luciferase inhibitors to avoid artifacts [4] |
| Multiplexed assay components | Simultaneous measurement of multiple cell health parameters | Allows correlated kinetic analysis of different death pathways |
| Automated live-cell imaging dyes | Temporal tracking of morphological changes | Enables high-content kinetic profiling without fixed timepoints |
Kinetic Profiling Experimental Workflow
The following diagram illustrates the core workflow for implementing kinetic profiling in cytotoxicity screening:
Detailed Methodologies for Key Experiments
High-Throughput Kinetic Cytotoxicity Profiling
Protocol for 1536-well Plate Cytotoxicity Screening [4]
Cell Seeding: Seed HEK 293, NIH 3T3, CRL-7250, HaCat, or KB 3-1 cells into white 1536-well plates using a Multidrop Combi peristaltic dispenser at densities of 250-500 cells/well in 5 μL of medium, depending on cell line.
Compound Transfer: Use a pintool (Kalypsys) to transfer 23 nL of compound solution to the 1536-well assay plates.
Kinetic Incubation: Incubate plates at 37°C with 5% CO₂ and 85% humidity for the duration of the kinetic monitoring period (typically 48 hours).
Multi-timepoint Assessment: At designated timepoints (e.g., 6, 12, 24, 48 hours), dispense 2.5 μL of CellTiter-Glo reagent into each well using a dispenser with solenoid valves.
Signal Detection: Allow plates to equilibrate at room temperature for 10 minutes before imaging ATP-coupled luminescence using a ViewLux microplate imager.
Data Processing: Normalize raw plate reads for each titration point relative to positive control (9.2 μM Bortezomib, -100% activity) and DMSO-only wells (basal, 0% activity).
Parameter Estimation from Time-Course Data
Incremental Iterative Parameter Estimation Method [13]
Data Preprocessing: Perform data smoothing to reduce noise effects and obtain reliable slope estimates from time-course metabolite concentration data.
Two-Phase Estimation:
- Phase 1 (Slope Error Minimization): Estimate subset parameters associated with measured metabolites using minimization of slope errors, avoiding computationally expensive ODE integration.
- Phase 2 (Concentration Error Minimization): Solve the ODE model one equation at a time and obtain remaining model parameters by minimizing concentration errors.
Iterative Refinement: Iterate between the two estimation phases until parameter estimates converge (difference between iterations less than chosen convergence factor).
Global Optimization: Use scatter search global optimization (SSm) methods to solve optimization problems in both phases, as this approach has proven effective for multi-minima problems common in kinetic parameter estimation.
Kinetic Parameter Determination Methods
Table 2: Methods for Determining Kinetic Parameters from Experimental Data
| Method | Key Principle | Advantages | Limitations |
|---|---|---|---|
| Integration Method | Fits integrated rate equation to concentration-time data | Straightforward implementation; visual validation through linear plots | Requires assumption of reaction order; limited to simpler mechanisms [14] |
| Differential Method | Directly uses reaction rate equation with measured rate data | No need to assume specific integrated form; applicable to complex mechanisms | Amplifies noise through differentiation; requires high-quality data [14] |
| Incremental Iterative Estimation | Combines decoupling and ODE decomposition in iterative phases | Handles missing metabolite data; computationally efficient; avoids ODE stiffness issues [13] | Requires multiple iterations; complex implementation |
| Bayesian Computational Modeling | Uses probabilistic inference from target gene measurements | Quantitative measurement of functional pathway activity; handles biological variability [15] | Requires calibration samples with known pathway activity |
Signaling Pathways in Cytotoxicity Responses
The cellular response to cytotoxic compounds involves multiple interconnected signaling pathways. The following diagram illustrates key pathways relevant to cytotoxicity screening:
Frequently Asked Questions (FAQs)
Experimental Design and Optimization
Q1: How many timepoints are sufficient for reliable kinetic profiling in cytotoxicity screening?
For most cytotoxicity applications, a minimum of 5-8 timepoints across the exposure period is recommended. Critical early timepoints (2-8 hours) help capture rapid responses, while later timepoints (24-72 hours) assess longer-term effects. The optimal spacing depends on the specific cell type and mechanism being studied—proliferating cells may require more frequent early sampling to capture division-dependent effects.
Q2: What cell density should be used for kinetic cytotoxicity assays?
Cell density significantly impacts kinetic readouts and should be optimized for each cell line. As referenced in established protocols, densities typically range from 250-500 cells/well in 1536-well format [4]. Lower densities may enhance sensitivity to cytostatic effects, while higher densities can provide more robust signals for shorter-term kinetic profiling.
Technical Troubleshooting
Q3: How can we distinguish specific cytotoxic compounds from general nuisance compounds in kinetic profiling?
Kinetic profiling provides several discrimination strategies:
- Response Timing: Specific inhibitors typically show mechanistically consistent kinetic signatures, while nuisance compounds (e.g., firefly luciferase inhibitors) may show anomalous time-response relationships [4].
- Multi-parameter Correlation: Genuine cytotoxicity typically shows concordance across multiple measured parameters (metabolic activity, membrane integrity, morphology) with consistent kinetics.
- Pathway Analysis: Computational analysis of pathway activity can distinguish specific mechanisms from general toxicity [15].
Q4: Our kinetic data shows high variability between replicates. What are potential causes and solutions?
Common causes and solutions include:
- Cell Passage Effects: Use consistent passage number ranges and avoid extremes
- Edge Effects: Use proper plate sealing and consider specialized microplates to minimize evaporation
- Instrument Timing: Standardize time between reagent addition and reading across plates
- Data Normalization: Implement robust normalization protocols using reference controls
Data Analysis and Interpretation
Q5: What are the best practices for parameter estimation from noisy time-course data?
The incremental iterative parameter estimation method has proven effective for handling noisy biological data [13]. This approach:
- Combines slope error minimization with concentration error minimization in alternating phases
- Handles situations with missing metabolite measurements
- Uses global optimization strategies to avoid local minima
- Incorporates data smoothing while avoiding overfitting through careful validation
Q6: How can we quantitatively measure pathway activity relevant to cytotoxicity responses?
Bayesian computational models can infer pathway activity from mRNA levels of transcription factor target genes [15]. This approach:
- Uses calibrated computational network models to infer transcription factor activity
- Transforms probability scores into quantitative pathway activity scores (log2odds)
- Enables quantitative comparison of pathway activity across different samples and conditions
- Has been validated for multiple pathways including NF-κB, TGFβ, and others relevant to cytotoxicity
Advanced Applications and Future Directions
Kinetic profiling in cytotoxicity screening continues to evolve with technological advancements. Modern phenotypic drug discovery combines therapeutic effects in realistic disease models with modern tools and strategies [2]. Recent innovations include:
- High-Content Kinetic Imaging: Combining temporal resolution with spatial information at single-cell resolution
- Pathway-Specific Reporter Systems: Engineered systems that provide direct readouts of specific pathway activities in living cells
- Microphysiological Systems: Advanced culture models that provide more physiologically relevant kinetic responses
- Machine Learning Approaches: Pattern recognition algorithms that identify subtle kinetic signatures predictive of specific mechanisms
These advanced approaches enable researchers to move beyond simple viability assessments to understand the dynamic cellular response to chemical exposure, ultimately improving the prediction of compound behavior in more complex biological systems.
Why Cytotoxicity Profiling is a Critical Pillar in Hit Triage and Validation
Frequently Asked Questions
What is the primary role of cytotoxicity profiling in hit triage? Cytotoxicity profiling acts as a critical early filter in hit triage. It identifies compounds that are generally toxic to cells, helping researchers separate compounds with a desired therapeutic effect (on-target) from those that simply kill cells (off-target). This prevents the advancement of promiscuously toxic compounds that are likely to fail in later development stages [16].
A cytotoxicity assay indicates my hit compound is toxic. Does this mean it's a failed drug candidate? Not necessarily. A positive result in a cytotoxicity test indicates the compound has cytotoxic potential, but it is not a definitive indicator of clinical failure. The result must be evaluated within a comprehensive risk assessment. This includes the intended clinical use (e.g., an anticancer drug is expected to be cytotoxic), the therapeutic window, data from other biocompatibility endpoints, and a thorough toxicological risk assessment based on chemical characterization [17] [18].
Why might my hit compound show cytotoxicity in the assay but not in follow-up studies? Cytotoxicity assays are highly sensitive by design and can generate "false positives" for several reasons:
- Assay Interference: The compound may interfere with the assay readout, for example, by being intrinsically fluorescent, absorbing light at the detection wavelength, or directly reacting with the assay reagents [19] [20].
- Physical Effects: Insoluble particles or the physical presence of a material in direct contact with cells can cause reactivity that is not relevant to the in vivo situation [18].
- Chemical Contamination: The sample may be contaminated with endotoxins or solvents from the manufacturing process, which can cause a cytotoxic response [20].
Which cytotoxicity assay is most suitable for hit triage in phenotypic screening? No single assay is universally perfect. The choice depends on your needs. For a high-throughput primary screen, metabolic assays like MTT or resazurin (alamarBlue) are common. For a more detailed mechanism, combining an assay like LDH release (membrane integrity) with a metabolic assay can provide a multiparametric view of cell health. The key is to understand each assay's limitations and use a combination of methods for validation [21] [19].
How do I validate a cytotoxic hit for an anti-cancer application? For a candidate intended to be cytotoxic, such as in oncology, validation involves confirming the activity is specific and not due to general toxicity. This includes:
- Dose-Response: Establishing a concentration-response curve (e.g., IC₅₀).
- Selectivity Profiling: Testing against non-cancerous cell lines to determine a selectivity index.
- Counter-Screens: Ruling out common false-positive mechanisms like chemical aggregation, redox cycling, or interference with assay signals [16] [10].
- Mechanistic Studies: Using high-content imaging or flow cytometry to confirm the mode of cell death (e.g., apoptosis, necrosis) [19].
Troubleshooting Guides
Issue 1: High Background or Inconsistent Results in Cytotoxicity Assays
Problem: Assay results show high variability, high background signal, or inconsistent data between replicates, making it difficult to reliably identify true hits.
| Potential Cause | Explanation | Solution |
|---|---|---|
| Compound Interference | Test compounds may be intrinsically colored, fluorescent, or redox-active, interfering with colorimetric or fluorometric readouts. | Perform an interference check: Include control wells with the compound but no cells to measure background signal. Use an orthogonal assay with a different readout (e.g., switch from MTT to a LDH or ATP assay) to confirm results [19]. |
| Nanoparticle or Insoluble Material | Particles can adsorb assay dyes, scatter light, or settle on cells, causing physical stress and false positives. | Characterize the formulation: Use dynamic light scattering (DLS) to check for agglomeration. Centrifuge extracts to remove particulates before adding to cells. Consider using direct contact assays with caution [20] [18]. |
| Cell Seeding Density | Inconsistent cell numbers per well lead to variable metabolic activity and signal. | Optimize and standardize: Verify signal linearity with cell density. Use a standardized cell counting method and seeding protocol for every experiment [19]. |
| Contamination | Endotoxin or microbial contamination in samples or reagents can trigger a cytotoxic immune response in certain cell types. | Use sterilized, depyrogenated materials: Test samples for endotoxin. Use proper aseptic technique [20]. |
Issue 2: Different Cytotoxicity Assays Yield Conflicting Results for the Same Hit
Problem: A compound is identified as cytotoxic in one assay but shows low toxicity in another, creating uncertainty about its true profile.
| Potential Cause | Explanation | Solution |
|---|---|---|
| Different Biological Endpoints | Assays measure different aspects of cell health (e.g., MTT measures metabolic activity, LDH measures membrane integrity). A compound may inhibit metabolism without immediately lysing cells. | Adopt a multiparametric approach: Use at least two assays measuring different endpoints (e.g., metabolic activity + membrane integrity). This provides a more comprehensive view of cytotoxic mechanisms [19]. |
| Assay Kinetics and Timing | The timing of cytotoxic events may not align with the assay readout. For example, membrane rupture may occur after metabolic shutdown. | Perform kinetic profiling: Take readings at multiple time points (e.g., 24, 48, 72 hours) to capture the evolution of the toxic effect, which is a core principle of kinetic profiling in phenotypic screening [17] [19]. |
| Mechanism of Action | The compound may have a sub-lethal or cytostatic effect that is detected by more sensitive assays (e.g., high-content imaging) but not by basic viability assays. | Use high-content or mechanistic assays: Implement assays that can detect apoptosis (e.g., caspase activation), changes in mitochondrial membrane potential, or cell cycle arrest to understand the subtle effects [19] [10]. |
Experimental Protocols for Key Cytotoxicity Assays
The following protocols are adapted from standard guidelines (ISO 10993-5) and recent research for use in hit triage [21] [18].
MTT Assay for Metabolic Activity
Principle: Viable cells reduce yellow MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) to purple formazan crystals. The amount of formazan dissolved and measured is proportional to the number of viable cells [21] [19].
Detailed Methodology:
- Cell Seeding: Seed L-929 mouse fibroblast cells or another relevant cell line in a 96-well plate at a density of 5 × 10³ to 1 × 10⁴ cells/well in complete medium. Incubate at 37°C with 5% CO₂ for 24 hours to form a near-confluent monolayer.
- Sample Preparation (Extraction): Prepare extracts of your test compounds or materials. For solids, use the elution method: incubate the sample in cell culture medium (e.g., DMEM with serum) at 37°C for 24-72 hours with agitation. The addition of serum (5-10%) is critical for extracting both polar and non-polar constituents [17] [18].
- Application of Extract: Remove the growth medium from the cells and replace it with the compound extracts or control media (negative control: fresh medium; positive control: medium with 1-2% Triton X-100). Incubate for 24-48 hours at 37°C with 5% CO₂.
- MTT Incubation: After treatment, add MTT reagent (e.g., 0.5 mg/mL final concentration) to each well and incubate for 2-4 hours at 37°C.
- Solubilization: Carefully remove the MTT-containing medium. Add a solubilization solution (e.g., isopropanol or DMSO) to dissolve the formed formazan crystals.
- Absorbance Measurement: Measure the absorbance of each well at a wavelength of 570 nm, with a reference wavelength of 630-650 nm to correct for background.
- Data Analysis: Calculate cell viability as a percentage relative to the negative control group.
Cell Viability (%) = (Mean Absorbance of Test Group / Mean Absorbance of Negative Control) × 100
Lactate Dehydrogenase (LDH) Release Assay
Principle: LDH is a stable cytosolic enzyme released upon cell membrane damage. The released LDH in the culture supernatant is measured with a coupled enzymatic reaction that converts a tetrazolium salt into a red formazan product [19].
Detailed Methodology:
- Cell Treatment: Seed and treat cells in a 96-well plate as described in the MTT protocol. Include a "background control" (culture medium only), "low control" (untreated cells), and "high control" (cells treated with lysis buffer to release total LDH).
- Sample Collection: After the treatment period, centrifuge the plate at 250 × g for 10 minutes to pellet cells and debris.
- Reaction Setup: Transfer a portion of the supernatant from each well to a new clear 96-well plate.
- LDH Reaction: Add the LDH assay reaction mixture according to the manufacturer's instructions. This typically contains NAD⁺, lactate, iodonitrotetrazolium chloride (INT), and diaphorase.
- Incubation and Measurement: Incubate the plate for 30 minutes at room temperature, protected from light. Measure the absorbance at 490-500 nm.
- Data Analysis:
- Subtract the background control absorbance from all other values.
- Calculate cytotoxicity using the formula:
Cytotoxicity (%) = [(Test Sample - Low Control) / (High Control - Low Control)] × 100
Assay Comparison and Reagent Toolkit
Cytotoxicity Assay Comparison
| Assay | Measured Endpoint | Advantages | Limitations | HTS Compatibility |
|---|---|---|---|---|
| MTT | Metabolic activity (mitochondrial dehydrogenase) | Inexpensive, well-established, widely accepted [21] | End product is insoluble, requires solubilization step; subject to chemical interference [19] | Moderate |
| LDH Release | Membrane integrity | Easy to perform, measures a direct marker of cell death [19] | Can be affected by serum in media; measures only late-stage necrosis [19] | High |
| ATP Assay (Luminometric) | Cellular ATP levels (cell viability) | Highly sensitive, broad dynamic range, low background [21] [19] | Requires a luminometer; more expensive than colorimetric assays | High |
| Neutral Red Uptake (NRU) | Lysosomal function & cell viability | More sensitive to some toxicants than MTT; viable cells incorporate the dye [19] | pH-sensitive; longer incubation time required | Moderate |
| Resazurin Reduction (AlamarBlue) | Overall metabolic capacity | Non-toxic, allows for continuous monitoring of the same culture over time [19] | Signal can saturate quickly with high cell numbers | High |
The Scientist's Toolkit: Essential Research Reagents
| Reagent / Solution | Function in Cytotoxicity Profiling |
|---|---|
| L-929 Mouse Fibroblast Cells | A standard cell line recommended by ISO 10993-5 for biocompatibility testing of medical devices and materials [21] [18]. |
| Dulbecco's Modified Eagle Medium (DMEM) with Fetal Bovine Serum (FBS) | The standard culture medium for maintaining cells. Serum is crucial for extracting non-polar compounds from test materials during sample preparation [21] [18]. |
| MTT Reagent | A tetrazolium salt used to assess cell metabolic activity via mitochondrial dehydrogenases [21] [19]. |
| Triton X-100 | A detergent used as a positive control to induce 100% cell death (cytotoxicity) [19]. |
| Dimethyl Sulfoxide (DMSO) | A common solvent for dissolving water-insoluble compounds and for solubilizing formazan crystals in the MTT assay [21]. |
Experimental Workflow and Data Interpretation
Hit Triage Workflow Integrating Cytotoxicity Profiling
The following diagram illustrates a strategic workflow for integrating kinetic cytotoxicity profiling into the hit triage and validation process.
Cytotoxicity Data Interpretation and Risk Assessment
This diagram outlines the logical decision process for evaluating a cytotoxic hit based on its therapeutic context and comprehensive dataset.
Linking Dynamic Cellular Responses to Complex Disease Biology
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of kinetic profiling over endpoint cytotoxicity assays? Kinetic profiling provides continuous temporal data on cellular responses, revealing compound mechanism of action through time-dependent response patterns that single timepoint assays miss. This allows researchers to distinguish between different mechanisms of cell death, identify off-target effects, and determine optimal treatment durations for maximal efficacy [6] [5].
Q2: Why should cytotoxicity profiling be performed early in screening campaigns? Cytotoxicity profiling at an early stage helps triage compounds with promiscuous cell-killing activity that could lead to misleading results in phenotypic screens. In large-scale screening, approximately 1-5% of compounds may demonstrate cytotoxic effects, influencing future project directions and increasing the likelihood of candidate success [4].
Q3: How can researchers distinguish selective cytotoxicity against cancer cells versus general toxicity? This requires parallel profiling against both cancer and "normal" cell lines. Selective compounds show activity primarily in cancer cells, while pan-cytotoxic compounds affect all cell types. Using at least four normal cell lines (e.g., HEK 293, NIH 3T3, CRL-7250, HaCat) and one cancer cell line (e.g., KB 3-1) provides robust selectivity assessment [4].
Q4: What are common artifacts in cytotoxicity assays and how can they be addressed? Common artifacts include firefly luciferase inhibition (∼5% of compounds), air bubbles causing well-to-well variability, improper cell density, and cytotoxic effects of the detection dyes themselves. These can be mitigated through counter-screening assays, careful pipetting techniques, optimization of cell density, and validation of dye compatibility with specific cell types [4] [22] [23].
Q5: How can kinetic profiling guide combination therapy development? Kinetic profiling reveals optimal dosing schedules and sequences for drug combinations by showing when synergistic activity occurs temporally. This helps align in vitro findings with in vivo pharmacokinetic properties, ensuring co-exposure of drugs at target tissues during synergistic time windows [5].
Troubleshooting Guides
High Variability in Cytotoxicity Measurements
| Problem | Possible Causes | Solutions |
|---|---|---|
| High well-to-well variability | Air bubbles in wellsUneven cell seedingEdge effects in plates | Break bubbles with syringe needle [22]Optimize cell suspension mixingUse edge well controls |
| Low signal intensity | Insufficient cell densityIncorrect assay incubation timeImproper reagent storage | Determine optimal cell count empirically [22]Validate assay kinetics for specific cell typeFreshly prepare reagents |
| Inconsistent concentration-response | Compound solubility issuesPlate reader calibration driftCell passage number too high | Include solubility controls [4]Regular instrument maintenanceUse low-passage cells |
Optimization of Kinetic Profiling Assays
| Challenge | Optimization Strategy | Validation Approach |
|---|---|---|
| Determining optimal sampling frequency | Balance temporal resolution with phototoxicity | Test different intervals (15min-2hr) with control compounds [6] |
| Maintaining cell health during live-cell imaging | Optimize CO₂, temperature controlUse minimal light exposure | Compare endpoint viability with static controls [5] |
| Multiplexing kinetic cytotoxicity with other parameters | Spectral separation of probesStaggered addition protocols | Verify no interference between detection channels [23] |
Interpretation of Complex Kinetic Profiles
| Profile Pattern | Potential Interpretation | Follow-up Experiments |
|---|---|---|
| Rapid cytotoxicity followed by recovery | Transient membrane disruptionAdaptive stress response | Measure membrane repair mechanismsAssess oxidative stress markers [24] |
| Delayed cytotoxicity | Indirect mechanismCell cycle-dependent effects | Cell cycle synchronizationGene expression profiling |
| Cell line-specific temporal patterns | Tissue-selective toxicityMetabolic activation required | Metabolic profilingMechanistic studies in sensitive lines |
Experimental Protocols
Protocol 1: Kinetic Cytotoxicity Profiling Using Impedance-Based Monitoring
Principle: Continuous monitoring of cell viability through electrical impedance measurements reflecting cell adhesion, proliferation, and death [6].
Materials:
- Real-time cell analyzer (e.g., xCELLigence, Incucyte)
- Appropriate cell culture plates with integrated electrodes
- Test compounds and controls
- Cell culture media and supplements
Procedure:
- Prepare cell suspension at optimized density (determined empirically)
- Seed cells into specialized plates and pre-incubate for 24h to establish monolayer
- Establish baseline impedance reading (2-4 hours pre-treatment)
- Add test compounds using precision liquid handler
- Monitor impedance continuously (every 15 minutes) for 48-72 hours
- Normalize data to baseline and plot time-dependent cell response profiles (TCRPs)
- Cluster compounds based on TCRP similarity for mechanism prediction
Data Analysis:
- Calculate normalized cell index values
- Generate TCRPs for each compound
- Perform hierarchical clustering of TCRPs
- Compare profiles to reference compounds with known mechanisms
Protocol 2: High-Content Kinetic Cytotoxicity with Multiplexed Readouts
Principle: Simultaneous monitoring of multiple cell death parameters over time using fluorescent probes and automated microscopy [23] [5].
Materials:
- High-content imaging system with environmental control
- 96-well or 384-well imaging plates
- DNA binding dyes (SYTOX Green, propidium iodide)
- Apoptosis biosensors (NucView caspase substrates)
- Mitochondrial membrane potential dyes (TMRE, JC-1)
Procedure:
- Seed cells at optimized density and incubate 24h
- Add multiplexed dye cocktail 1h before compound treatment
- Treat with test compounds using concentration-response format
- Acquire images every 2-4 hours at 20x magnification
- Include vehicle and positive controls (e.g., staurosporine) on each plate
- Maintain environmental control (37°C, 5% CO₂) throughout experiment
Image Analysis Pipeline:
- Segment nuclei and cytoplasm
- Quantify dye intensity per cell
- Measure morphological parameters (cell area, nuclear condensation)
- Track individual cells over time when possible
- Calculate percentage of dead cells for each timepoint
| Cell Line | Type | Annotated Library (∼10,000 cpds) | Diversity Library (∼100,000 cpds) |
|---|---|---|---|
| HEK 293 | Normal | 3.2% | 1.8% |
| NIH 3T3 | Normal | 2.8% | 2.1% |
| CRL-7250 | Normal | 2.9% | N/D |
| HaCat | Normal | 3.5% | N/D |
| KB 3-1 | Cancer | 5.1% | 3.2% |
| Dye | Excitation/Emission (nm) | Permeability | Advantages | Limitations |
|---|---|---|---|---|
| Propidium Iodide | 535/617 | Dead cells only | Inexpensive, well-established | High background with RNA |
| SYTOX Green | 504/523 | Dead cells only | >500x fluorescence enhancement | Potential cytotoxicity with extended exposure |
| TO-PRO-3 | 642/661 | Dead cells only | Good for multiplexing with GFP | Requires far-red capable imager |
| Hoechst 33342 | 350/461 | All cells at high concentrations | Can distinguish cell cycle | Permeable to live cells at working concentrations |
Signaling Pathways in Cellular Stress Responses
Mitochondrial Stress Response Pathway
Kinetic Profiling Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Kinetic Cytotoxicity Profiling
| Category | Specific Reagents/Solutions | Function | Key Considerations |
|---|---|---|---|
| Cell Culture | HEK 293, NIH 3T3, CRL-7250, HaCat, KB 3-1 [4] | Normal vs. cancer cell cytotoxicity assessment | Use low passage numbers, regular authentication |
| Viability Detection | CellTiter-Glo ATP assay [4] | Quantification of metabolically active cells | Lyse cells before reading for maximum signal |
| Membrane Integrity | SYTOX Green, Propidium iodide [23] | Selective dead cell staining | Validate dye concentration for each cell type |
| Apoptosis Sensors | NucView caspase substrates [5] | Real-time apoptosis monitoring | Compatible with live cell imaging |
| Metabolic Probes | TMRE, JC-1 dyes [24] | Mitochondrial membrane potential | Calibrate for each cell type |
| Compound Libraries | Annotated libraries (∼10,000 compounds) [4] | Mechanism-based profiling | Include known cytotoxic agents as controls |
Instrumentation and Software Solutions
| Platform Type | Example Systems | Primary Application | Data Output |
|---|---|---|---|
| Impedance-Based | xCELLigence systems [6] | Real-time cell monitoring | Time-dependent cell response profiles |
| High-Content Imagers | ImageXpress, Incucyte [5] | Multiplexed kinetic imaging | Quantitative morphology and fluorescence |
| Plate Readers | ViewLux [4] | Endpoint cytotoxicity | Luminescence, fluorescence intensity |
| Analysis Software | TIBCO Spotfire, Genedata Screener [4] [5] | Profile clustering and synergy analysis | Heatmaps, combination indices |
Implementing Kinetic Cytotoxicity Assays: From Technologies to Workflow Integration
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: What are the key advantages of using real-time impedance biosensors over endpoint assays in cytotoxicity screening?
Real-time impedance biosensors, such as those used in Electrical Cell-substrate Impedance Sensing (ECIS), provide a label-free, continuous monitoring capability of cell physiology. Unlike endpoint assays, they allow researchers to track dynamic changes in cell status, including cell adherence, spreading, motility, and growth, which are sensitive indicators of cellular physiopathology and response to external stimuli [25]. This enables the capture of time-course dynamical data rather than just one-shot information, offering deeper insights into the kinetic profile of cytotoxic effects [25].
Q2: Our high-content imaging shows high background staining, compromising our data. What are the common causes and solutions?
High background staining, which results in a poor signal-to-noise ratio, can arise from several sources [26]:
- Cause: Endogenous enzymes (like peroxidases or phosphatases) in the tissue sample are reacting with the detection substrate.
- Solution: Quench endogenous peroxidases with 3% H₂O₂ in methanol or use a commercial peroxidase suppressor. Inhibit endogenous phosphatases with levamisole [26].
- Cause: Endogenous biotin or lectins in the sample.
- Solution: Use an avidin/biotin blocking solution. If using an avidin-biotin complex, consider using streptavidin or NeutrAvidin instead of avidin, as they are not glycosylated and won't bind to lectins [26].
- Cause: Nonspecific binding of the primary or secondary antibody.
- Solution: Optimize antibody concentrations. For the secondary antibody, increase the concentration of normal serum from the source species (up to 10%) in the blocking buffer. For the primary antibody, reduce its final concentration or add NaCl (0.15 M to 0.6 M) to the antibody diluent to reduce ionic interactions [26].
Q3: Why is careful parameter selection critical in Electrochemical Impedance Spectroscopy (EIS) for biosensing?
The accuracy and reliability of impedance-based biosensors can be highly dependent on the electrochemical parameters chosen for data analysis. Relying solely on a single parameter like charge transfer resistance (Rct) may ignore other valuable data. Research shows that:
- The signal gain and relative standard deviation (RSD) are dependent on the potential applied during measurement.
- Parameters such as real impedance at specific frequencies can offer a 2.7-fold higher signal gain with negligible RSD compared to conventional Rct analysis.
- Reasonable signals at frequencies above 100 Hz tend to be less dispersive.
- Increasing the concentration of the redox probe can also help reduce the relative standard deviation [27].
Troubleshooting Common Experimental Issues
Table 1: Troubleshooting Cell-Based Biosensor Performance
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Weak or No Target Staining (Imaging) | Primary antibody degradation or denaturation [26]. | Test antibody potency on a positive control; ensure proper storage pH (7.0-8.2) and avoid freeze/thaw cycles by aliquoting [26]. |
| High Background Staining (Imaging) | Nonspecific antibody binding; endogenous enzymes [26]. | Block with higher serum concentrations (up to 10%); quench endogenous enzymes; optimize antibody dilution [26]. |
| High Signal Variability (Impedance) | Inconsistent cell seeding; electrode passivation; suboptimal EIS parameters [25] [27]. | Standardize cell culture protocols; use fresh electrode surfaces; test multiple frequencies/concentrations to identify least dispersive parameters [27]. |
| Low Sensitivity / Dynamic Range | Limited cellular reactivity to the analyte; impractical biosensor regeneration [25]. | Utilize engineered cell reporters and synthetic gene circuits to enhance cellular reactivity to target analytes [25]. |
| Matrix Interference | Nonspecific binding from complex samples (e.g., serum) [28]. | Use blocking agents, antifouling coatings, or pre-filtration of samples [28]. |
Table 2: Troubleshooting Cytotoxicity Assay Results
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Poor Distinction Between Cytostatic & Cytotoxic Effects | End-point assay masking kinetic differences [25]. | Employ label-free, real-time biosensors (e.g., impedance, SPR) to dynamically monitor changes in cell adhesion and morphology [25]. |
| High False Positives in Phenotypic Screens | Undetected general cytotoxicity from screening compounds [4]. | Profile screening libraries for cytotoxicity early on; use orthogonal assays to confirm on-target activity and triage promiscuous cytotoxic compounds [4]. |
| Inconsistent Results in Metabolic Profiling | Use of in vitro enzyme parameters that do not reflect in vivo conditions [29]. | Utilize data-driven estimations of in vivo kinetic parameters (e.g., kcat) which are more stable and improve model predictions [29]. |
Experimental Protocols for Key Workflows
Protocol 1: Real-Time Impedance-Based Cytotoxicity and Kinetic Profiling
This protocol outlines the use of electrical impedance to monitor cell physiology and detect cytotoxic effects kinetically, based on established biosensing platforms [25] [30].
Key Materials & Reagents:
- Cell Lines: Adherent cell lines relevant to your research (e.g., HEK 293, NIH 3T3 for "normal" cells; HeLa sublines for cancer) [4].
- Instrumentation: Impedance analyzer or LCR meter, cell culture module with integrated microelectrode arrays [25] [30].
- Consumables: Multi-well plates with embedded gold film electrodes [25].
Detailed Methodology:
- Cell Seeding: Seed adherent cells onto the electrode-coated surface of the biosensor at a defined density (e.g., 250-500 cells/well in a 1536-well format) to form a monolayer [4] [30].
- Equilibration & Baseline Recording: Allow cells to adhere and spread for several hours (or overnight) in an incubator (37°C, 5% CO₂). Record the baseline impedance signal across a frequency range (e.g., 1 kHz to 300 kHz) for a stable period [25] [30].
- Compound Exposure: Using a pintool or liquid handler, transfer compounds from a library (e.g., annotated or diversity libraries) to the assay plates. Include controls (e.g., DMSO for vehicle, Bortezomib for full cytotoxicity) [4].
- Real-Time Kinetic Monitoring: Continuously monitor impedance, often at a specific frequency (e.g., 150 kHz), for a duration of 48-72 hours. The impedance value is directly related to cell number, adhesion, and morphology [25] [4] [30].
- Data Analysis:
- Normalize raw impedance data to the pre-treatment baseline.
- Generate concentration-response curves and fit them using a four-parameter logistic model to determine EC₅₀ and efficacy values [4].
- Classify compounds based on their cytotoxic kinetic profiles (e.g., rapid cytolysis vs. slow anti-proliferative effects).
Protocol 2: Multiparametric Label-Free Assay for Dynamic Cell Assessment
This protocol combines impedance with other techniques, such as Surface Plasmon Resonance (SPR), for a more comprehensive analysis of cell status under toxic insult [25].
Key Materials & Reagents:
- Combined System: A biosensing platform capable of simultaneous EIS and SPR measurements [25].
- Cells: Adherent cell lines capable of forming tight junctions (e.g., renal, endothelial) [25].
Detailed Methodology:
- Cell Culture on Sensor: Grow a confluent monolayer of cells directly on the sensor surface that supports both EIS and SPR.
- Establish Barrier Function: Confirm the development of tight junctions, which is indicated by a stable, high impedance baseline and a specific SPR signature [25].
- Toxic Insult Exposure: Introduce the cytotoxic compound or bioactive substance (e.g., calcium oxalate crystals, amyloid fibrils) to the cell medium [25].
- Simultaneous Multiparametric Recording:
- EIS: Monitor changes in cell-substrate adherence and the integrity of cell-cell connections.
- SPR/Optical Biosensor: Monitor dynamic mass redistribution and cytoskeletal remodeling within the cells [25].
- Data Fusion and Interpretation:
- Correlate the EIS and SPR kinetic data to deconvolve the complex cellular response.
- For example, a biphasic response upon exposure may correspond to an initial change in cell-substrate adherence followed by a later change in cell-cell tightening [25].
Research Reagent Solutions & Essential Materials
Table 3: Key Reagents for Cytotoxicity Phenotypic Screening
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| CellTiter-Glo Assay | Measures ATP content as a marker of metabolic activity and cell viability [4]. | End-point determination of cytotoxicity in high-throughput screening [4]. |
| Quinacrine (Mepacrine) | Fluorescent dye used to label platelets or cellular components for imaging [30]. | Real-time visualization of thrombus formation in impedance/imaging fusion biosensors [30]. |
| PPACK (D-Phenylalanyl-L-Prolyl-L-Arginine Chloromethyl Ketone) | Direct thrombin inhibitor; anticoagulant for blood sample preparation [30]. | Prevents blood coagulation in assays studying platelet adhesion and thrombus formation under flow [30]. |
| Type I Collagen | Protein substrate that induces platelet aggregation and adhesion [30]. | Used to coat microchannels in thrombosis-on-a-chip models to simulate a damaged vessel wall [30]. |
| Sodium Citrate Buffer (pH 6.0) | Common buffer used for heat-induced epitope retrieval (HIER) [26]. | Unmasking target antigens in formalin-fixed, paraffin-embedded (FFPE) tissue sections for IHC staining [26]. |
| Engineered Cell Reporters | Cells with synthetic gene circuits that enhance or tailor reactivity to specific stimuli [25]. | Creating highly sensitive and specific live-cell biosensors for targeted cytotoxic pathways [25]. |
Troubleshooting Guides
Organoid Culture Challenges
Q1: My patient-derived colorectal organoids show poor growth efficiency and low viability. What could be the cause and how can I improve this?
A: Poor organoid growth often stems from issues with initial tissue processing and handling. Based on standardized protocols for colorectal organoids, the following solutions are recommended [31]:
- Critical Tissue Handling: Ensure samples are transferred in cold Advanced DMEM/F12 medium supplemented with antibiotics immediately after collection. Processing delays significantly reduce cell viability [31].
- Appropriate Preservation: Select preservation method based on expected processing delay:
- Matrix Optimization: Ensure proper Matrigel concentration and distribution. Inhomogeneous matrix embedding creates suboptimal growth environments [32].
Table 1: Troubleshooting Organoid Viability Issues
| Problem | Potential Cause | Solution | Expected Outcome |
|---|---|---|---|
| Low cell viability | Delay in tissue processing | Process immediately or use appropriate preservation method | 20-30% improvement in viability [31] |
| Necrotic cores | Limited nutrient diffusion | Use organoids-on-chip with perfusion | Enhanced viability and extended culture [33] |
| High heterogeneity | Uncontrolled self-assembly | Implement automated liquid handling systems | Improved reproducibility and consistency [32] |
| Limited maturation | Lack of environmental cues | Incorporate mechanical stimulation in OoC platforms | Better functional maturation and physiology [33] |
Q2: My organoid models lack physiological complexity and fail to recapitulate native tissue functions. How can I enhance their functional maturity?
A: Limited organoid maturity is a common challenge that can be addressed through several engineering approaches [32]:
- Integrate Multiple Cell Types: Co-culture epithelial organoids with mesenchymal cells, immune cells, or endothelial cells to better mimic the tissue microenvironment [32].
- Provide Physiological Cues: Incorporate mechanical stimulation (fluid flow, stretching), electrical stimulation (for neural/cardiac models), or biochemical gradients to promote maturation [33].
- Extend Culture Duration: Allow extended differentiation time (e.g., 6-9 months for brain organoids to model later developmental stages) [33].
- Utilize Organ-on-Chip Technology: Microfluidic platforms provide continuous perfusion, mechanical stimuli, and tissue-tissue interfaces that enhance functional maturation [33] [34].
Organ-on-a-Chip Implementation Issues
Q3: When implementing organ-on-a-chip systems for cytotoxicity screening, I encounter high variability between devices. How can I improve reproducibility?
A: OoC variability often stems from inconsistent device fabrication and cell culture conditions. Implement these strategies [33] [32]:
- Standardized Fabrication: Use consistent PDMS curing protocols and quality control measures for chip production [33].
- Automated Fluid Handling: Implement automated perfusion systems to minimize operator-dependent variability in flow rates and medium changes [32].
- Quality Control Checkpoints:
- Integrated Sensors: Incorporate miniature biochemical sensors for real-time monitoring of metabolic parameters (O₂, pH, glucose) to ensure consistent culture conditions [32].
Q4: How can I model multi-organ interactions for systemic cytotoxicity assessment in organ-on-a-chip platforms?
A: Modeling organ-organ interactions requires integrated multi-OoC systems [33] [34]:
- Physiologically-Based Design: Scale organ compartments according to human physiological ratios (tissue size, fluid volumes) [35].
- Vascular Coupling: Create a shared circulatory network that allows communication via endothelial barriers while maintaining tissue-specific compartments [33].
- Sequential Dosing: Implement programmable flow patterns that mimic pharmacokinetic profiles after drug administration [35].
- Sensitive Endpoint Detection: Utilize integrated biosensors and high-content imaging to capture inter-organ signaling and distant toxic effects [32].
Experimental Protocols
Protocol: Establishing Patient-Derived Colorectal Cancer Organoids for Phenotypic Screening
Background: This protocol enables generation of patient-derived organoids (PDOs) from colorectal tissues for high-content cytotoxicity screening, maintaining tumor heterogeneity and patient-specific drug responses [31].
Materials: Table 2: Key Research Reagents for Organoid Culture
| Reagent/Category | Specific Examples | Function/Purpose |
|---|---|---|
| Basal Medium | Advanced DMEM/F12 | Foundation for culture medium |
| Essential Supplements | EGF, Noggin, R-spondin1 (L-WRN conditioned medium) | Maintain stem cell growth and differentiation [31] |
| Matrix | Matrigel (Basement Membrane Matrix) | Provides 3D structural support mimicking extracellular matrix [31] |
| Tissue Dissociation | Collagenase/Dispase enzyme mix | Liberates crypts and stem cell units from tissue samples [31] |
| Antibiotics | Penicillin-Streptomycin (100 U/mL) | Prevents microbial contamination [31] |
| Cryopreservation | DMSO (10%) in FBS (10%) with 50% L-WRN medium | Preserves tissue/cells for long-term storage [31] |
Step-by-Step Methodology [31]:
Tissue Procurement and Processing:
- Collect human colorectal tissue samples under sterile conditions immediately following surgical resection or biopsy.
- Transfer samples in 5-10 mL cold Advanced DMEM/F12 with antibiotics.
- Critical: Process within 1-2 hours or use validated preservation methods.
Crypt Isolation:
- Wash tissue 3x with cold PBS containing antibiotics.
- Mince tissue into <1 mm³ fragments using sterile scalpels.
- Digest with collagenase solution (2 mg/mL) for 30-60 minutes at 37°C with gentle agitation.
- Filter through 100 μm strainer to separate crypts from single cells and debris.
Organoid Culture Establishment:
- Mix isolated crypts with Matrigel (approximately 500-1000 crypts/50 μL dome).
- Plate as domes in pre-warmed culture plates and polymerize for 20 minutes at 37°C.
- Overlay with complete intestinal organoid medium containing EGF, Noggin, R-spondin, and other essential factors.
- Culture at 37°C with 5% CO₂, changing medium every 2-3 days.
Passaging and Expansion:
- Mechanically disrupt organoids every 7-14 days using gentle pipetting.
- Re-embed fragments in fresh Matrigel at appropriate dilution (typically 1:3-1:6 split ratio).
Quality Control:
- Verify organoid morphology: presence of crypt-like structures with bud formation.
- Confirm viability >80% via live/dead staining.
- Validate epithelial identity through immunofluorescence for cytokeratins.
Protocol: Integrating Organoids with Microfluidic Organ-on-a-Chip Platform
Background: This protocol describes the integration of pre-formed organoids into microfluidic chips to enhance physiological relevance for cytotoxicity screening applications [33].
Materials:
- Pre-formed organoids (7-14 days old)
- Microfluidic OoC device (commercial or custom-fabricated)
- ECM solution (Matrigel or collagen I)
- Perfusion medium (organ-specific)
- Programmable syringe pump or pneumatic perfusion system
- Tubing and connectors compatible with microfluidics
Step-by-Step Methodology [33]:
Organoid Preparation:
- Harvest organoids from conventional 3D culture.
- Gently break down into appropriate size fragments (50-200 μm diameter).
- Resuspend in diluted ECM solution (Matrigel reduced to 4-6 mg/mL concentration).
Chip Loading:
- Introduce organoid-ECM suspension into microfluidic culture chamber via inlet port.
- Allow ECM polymerization at 37°C for 30 minutes.
- Connect to perfusion system primed with culture medium.
Perfusion Culture Establishment:
- Initiate low flow rate (0.1-1 μL/min) for 24 hours to allow organoid acclimation.
- Gradually increase to physiological flow rates (2-5 μL/min) over 48 hours.
- Maintain continuous perfusion with medium replacement every 24-48 hours.
System Validation:
- Confirm organoid viability after 72 hours of perfusion using live/dead staining.
- Verify physiological morphology and polarization (apical-basal orientation when applicable).
- Assess barrier function if relevant (TEER measurements for epithelial models).
Compound Screening:
- Introduce test compounds through perfusion system at physiologically relevant concentrations.
- Implement real-time monitoring using integrated sensors or endpoint analyses.
- Include appropriate controls (vehicle, positive cytotoxicity controls).
Frequently Asked Questions (FAQs)
Q5: What are the key advantages of using phenotypic screening in cytotoxicity assessment compared to target-based approaches?
A: Phenotypic screening offers several distinct advantages for cytotoxicity assessment [2] [36]:
- Identification of Novel Mechanisms: Enables discovery of unexpected therapeutic targets and mechanisms of action without predetermined target hypotheses [2].
- Pathway Context: Evaluates compound effects within complete biological pathways and cellular networks, revealing complex polypharmacology [2].
- First-in-Class Potential: Historically, phenotypic screening has been more successful at generating first-in-class medicines with novel mechanisms [2] [36].
- Human Relevance: When using human-derived organoids, provides more clinically predictive data compared to animal models or simplified cell systems [36].
Q6: How do I determine whether my cytotoxicity findings in organoid models are physiologically relevant?
A: Establish these validation criteria for physiological relevance [32] [34]:
- Benchmarking: Compare compound responses to known clinical profiles (IC₅₀ values, therapeutic indices).
- Multiple Endpoints: Assess various cytotoxicity parameters (apoptosis, necrosis, metabolic inhibition, functional impairment) rather than single metrics.
- Histological Correlation: Verify that morphological changes in organoids mirror tissue responses observed in clinical specimens.
- Biomarker Concordance: Confirm that molecular markers of toxicity (e.g., stress response genes, damage-associated molecules) align with clinical toxicity signatures.
Q7: What are the current limitations in using advanced model systems for regulatory decision-making in drug development?
A: While rapidly evolving, current limitations include [32] [34]:
- Standardization Challenges: Lack of standardized protocols and quality control metrics across laboratories.
- Validation Gaps: Limited comprehensive validation against clinical outcomes for specific toxicity endpoints.
- Regulatory Acceptance: Evolving but not yet complete regulatory frameworks for accepting data from these novel platforms.
- Technical Complexity: Requirement for specialized expertise and infrastructure that may limit widespread adoption.
- Throughput Limitations: Despite improvements, most complex OoC systems have lower throughput than traditional 2D models.
However, regulatory attitudes are shifting, with recent FDA approvals incorporating OoC data supporting clinical trials, particularly for rare diseases where traditional models are inadequate [34].
Q8: What computational approaches can enhance the predictive power of cytotoxicity data from advanced model systems?
A: Several computational methods can augment phenotypic screening data [2] [36]:
- Multiparametric Analysis: Use machine learning algorithms to identify complex patterns in high-content screening data that predict clinical toxicity.
- Pathway Mapping: Integrate cytotoxicity data with known signaling pathways to identify vulnerable biological processes.
- Kinetic Modeling: Develop quantitative systems pharmacology models that simulate temporal compound effects and recovery dynamics.
- Cross-Species Translation: Build computational frameworks that translate findings between model systems and human physiology.
- Toxicity Prediction: Train classifiers on historical screening data to flag compounds with high probability of adverse effects.
Table 3: Comparison of Advanced Model Systems for Cytotoxicity Screening
| Parameter | 2D Monolayers | 3D Organoids | Organ-on-Chip |
|---|---|---|---|
| Physiological Relevance | Low | Moderate to High | High |
| Throughput Capacity | High (384+ well) | Moderate (96-384 well) | Low to Moderate (varies) |
| Complexity | Single cell type | Multiple cell types, self-organized | Multiple tissues, vascular perfusion |
| Cost per Data Point | Low | Moderate | High |
| Reproducibility | High | Moderate (batch variation) | Improving with standardization |
| Mechanistic Insight | Pathway-specific | Tissue context | Organ-level, systemic |
| Regulatory Acceptance | Established | Growing | Emerging |
| Best Use Case | Primary screening, mechanism | Disease modeling, efficacy | ADMET, systemic toxicity |
Frequently Asked Questions (FAQs)
Q1: What are the primary differences between phenotypic and target-based screening approaches, and when should I use each?
A1: The choice between phenotypic and target-based screening is foundational to your discovery strategy [9].
- Phenotypic Drug Discovery (PDD) identifies compounds based on a measurable biological response in a cell-based or whole-organism context, without prior knowledge of the specific molecular target [9]. This approach is powerful for uncovering novel biology and first-in-class therapies, as it captures the complexity of cellular systems and can reveal unanticipated mechanisms of action [9]. It is particularly useful when the underlying disease pathways are poorly characterized.
- Target-Based Drug Discovery (TDD) begins with a predefined, well-characterized molecular target (e.g., a specific enzyme or receptor) [9]. This approach allows for rational drug design, leveraging high-resolution structural biology to optimize compounds for specificity and potency [9].
The following table summarizes the core differences:
| Feature | Phenotypic Screening | Target-Based Screening |
|---|---|---|
| Starting Point | Measurable biological effect or phenotype [9] | Pre-validated molecular target [9] |
| Key Advantage | Unbiased discovery of novel targets and mechanisms; captures system complexity [9] [37] | Rational design; typically simpler optimization and validation [9] |
| Main Challenge | Requires subsequent target deconvolution, which can be complex and time-consuming [9] | Relies on a correct target hypothesis; may fail if the target is not disease-relevant in vivo [9] |
| Ideal Use Case | Identifying first-in-class drugs; complex diseases with multifactorial etiology [9] [37] | Optimizing compounds for a known pathway; developing best-in-class drugs [9] |
Q2: Our HTS campaign yielded an overwhelming number of hits. What are the critical first steps in triaging these for a cytotoxicity phenotypic screen?
A2: Effective hit triage is crucial for prioritizing the most promising candidates. A multi-parameter filtering approach is recommended.
- Confirm Activity: Begin with a dose-response confirmation assay to verify the initial hit and determine the half-maximal inhibitory concentration (IC50). This eliminates false positives from single-concentration screening.
- Assess Specificity and Safety: Test confirmed hits in counter-screens. For cytotoxicity screening, this includes assessing the effect on non-malignant or primary cell lines (e.g., astrocytes, CD34+ progenitor cells) to identify compounds with selective toxicity towards diseased cells [38].
- Evaluate Assay Interference: Rule out pan-assay interference compounds (PAINS) and other non-specific inhibitors that can generate false positives through mechanisms like colloidal aggregation or fluorescence [39].
- Analyse Structure-Activity Relationships (SAR): Cluster hits by chemical structure. If several structurally similar compounds show activity, it strengthens the validity of the hit series and provides a starting point for medicinal chemistry optimization.
Q3: What are the best practices for quality control (QC) in a high-throughput kinetic profiling assay?
A3: Robust QC measures are non-negotiable for generating reliable HTS data. These measures fall into two main categories [40]:
- Plate-Based Controls: These characterize the performance of the entire assay plate and help identify technical artifacts.
- Include maximum effect (e.g., 100% cell death control), minimum effect (vehicle/negative control), and if possible, a reference compound control on every plate.
- Monitor for spatial effects like the "edge effect," caused by evaporation from wells at the plate's periphery, which can lead to inconsistent results [40].
- Sample-Based Controls: These characterize the variability in biological responses.
- Use statistical tools like the Z'-factor to assess the quality and robustness of the assay itself. A Z'-factor > 0.5 is generally considered an excellent assay.
- The minimum significant ratio (MSR) is another QC tool that measures assay reproducibility and characterizes the potencies of controls or samples between different assay runs [40].
Q4: How can we integrate multi-omics data to deconvolute the mechanism of action for a phenotypically active hit?
A4: Integrating multi-omics technologies is a powerful strategy for linking a phenotypic outcome to its underlying molecular mechanism [9]. After identifying a robust hit, you can:
- Transcriptomics (RNA-Seq): Profile the global gene expression changes in cells treated with your hit compound versus a vehicle control. This can reveal which pathways are being up- or down-regulated, providing a hypothesis for the Mechanism of Action (MoA) [38].
- Proteomics (Thermal Proteome Profiling): This method identifies direct protein targets by measuring which proteins become stabilized or destabilized upon compound binding when subjected to a heat gradient. It is a direct way to identify the proteins engaged by your hit [38].
- Cellular Thermal Shift Assay (CETSA): Using antibodies, this assay can confirm the binding of the compound to specific targets that emerged from the thermal proteome profiling study [38].
Troubleshooting Guides
Issue: High Variability and Poor Reproducibility in HTS Readouts
| Symptom | Possible Cause | Solution |
|---|---|---|
| High well-to-well or plate-to-plate variability in signal. | Inconsistent liquid handling due to pipetting errors or clogged tips. | Calibrate automated liquid handlers regularly. Use visual or gravimetric checks to verify dispensed volumes. |
| Evaporation, leading to "edge effects." | Use microplates with seals or lids. Employ atmospheric control in incubators. Use assay buffers with low evaporation potential. | |
| Cell seeding density inconsistency. | Standardize cell counting methods and ensure a homogeneous cell suspension during seeding. Use automated cell counters. | |
| Low Z'-factor (<0.5). | High background signal or low signal-to-noise ratio. | Optimize assay reagent concentrations and incubation times. Switch to a more sensitive detection method (e.g., luminescence over absorbance). |
| High variance in positive or negative controls. | Ensure control compounds are fresh and prepared accurately. Check for contamination in cell cultures or reagents. |
Issue: Hit Confirmation and Validation Failures
| Symptom | Possible Cause | Solution |
|---|---|---|
| Hits from primary screen fail to show dose-response in confirmation. | The primary screen had a high false-positive rate. | Implement stricter hit-selection criteria in the primary screen (e.g., use of normalised percent inhibition and setting a robust Z-score threshold). |
| Compound instability or precipitation. | Check compound solubility in the assay buffer. Use fresh DMSO stocks and ensure proper storage conditions. | |
| Cytotoxic hits are also toxic to non-malignant cells. | The compound has a non-selective, generic mechanism of cytotoxicity. | Perform counter-screens on relevant primary or non-transformed cell lines early in the triage process [38]. This identifies and filters out non-selective compounds. |
| Potency decreases in more physiologically relevant (3D) models. | Poor compound penetration into spheroids/organoids. | Consider the compound's physicochemical properties. Extend treatment durations to allow for deeper tissue penetration. |
| The 3D model introduces microenvironmental factors (e.g., hypoxia, quiescence) that reduce efficacy. | Validate your 3D model to ensure it represents the key features of the tumor. Use longer exposure times or combination therapies. |
Experimental Protocols for Key Workflows
Protocol: High-Throughput Kinetic Profiling of Cytotoxicity in 3D Spheroids
Objective: To dynamically monitor the cytotoxic effects of compound libraries on patient-derived glioblastoma (GBM) spheroids over time, generating rich kinetic data (e.g., IC50 over time).
Materials:
- Cells: Low-passage patient-derived GBM cells [38].
- Assay Plate: Ultra-low attachment (ULA) 384-well microplates for spheroid formation.
- Compound Library: Prepared in DMSO as 10mM stocks, pre-plated in source plates.
- Automation: Liquid handling robot (e.g., Integra Viaflo), plate washer/dispenser.
- Viability Reagent: Real-time, homogenous cell viability indicator (e.g., CellTiter-Glo 3D).
- Detector: Plate reader capable of luminescence and fluorescence, with environmental control for long-term kinetic readings.
Methodology:
- Spheroid Formation: Seed GBM cells in ULA plates at a density optimized for forming uniform, single spheroids (e.g., 500-1,000 cells per well in 50 µL media). Centrifuge plates briefly (300 x g, 1 min) to aggregate cells. Incubate for 72-96 hours to form compact spheroids.
- Compound Addition: Using a liquid handler, transfer 50 nL of compound from source plates to assay plates, creating a final concentration range (e.g., 20 µM to 1 nM). Include DMSO-only wells as vehicle controls and a well-characterized cytotoxic agent as a positive control.
- Kinetic Reading: At defined time points post-compound addition (e.g., 0, 6, 24, 48, 72 hours), add an equal volume of CellTiter-Glo 3D reagent to each well. Orbital shake the plate for 5 minutes to induce cell lysis and equilibrate the signal. Measure luminescence.
- Data Analysis: Normalize luminescence values for each well to the vehicle control (100% viability) and positive control (0% viability). Plot normalized viability against compound concentration at each time point to generate time-resolved dose-response curves and calculate IC50(t).
Protocol: Thermal Proteome Profiling for Target Deconvolution
Objective: To identify the direct protein targets of a phenotypically active hit compound on a proteome-wide scale.
Materials:
- Cells: Relevant cell line (e.g., GBM cells) treated with hit compound or vehicle (DMSO).
- Equipment: PCR machine or thermal cycler for precise temperature control, centrifuge, mass spectrometer.
- Reagents: Protease inhibitors, detergent-compatible protein assay kit, trypsin.
Methodology:
- Compound Treatment & Heating: Treat cells with your hit compound or DMSO. Aliquot the cell suspensions into PCR tubes. Heat each aliquot to a different temperature (e.g., from 37°C to 67°C in 10 increments) for 3 minutes, then cool to room temperature.
- Soluble Protein Extraction: Lyse the heated cells. Centrifuge at high speed to separate the soluble (thermostable) protein fraction from the insoluble (aggregated) fraction.
- Proteomic Digestion and Analysis: Digest the soluble proteins from each temperature point with trypsin. Analyze the resulting peptides by liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS).
- Data Processing: Identify and quantify the proteins in each sample. For each protein, plot the amount in the soluble fraction across the temperature gradient. A shift in the melting curve (thermal stability) between the compound-treated and vehicle-treated samples indicates direct binding of the compound to that protein [38].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for setting up a high-throughput kinetic profiling cytotoxicity screen.
| Research Reagent / Material | Function in the Workflow |
|---|---|
| Ultra-Low Attachment (ULA) Microplates | Promotes the formation of uniform, single 3D cell spheroids by minimizing cell-surface adhesion [38]. |
| Real-Time Viability Assays (e.g., CellTiter-Glo 3D) | Homogeneous "add-mix-read" assays that quantify ATP levels, a marker of metabolic activity and cell viability, in a format optimized for 3D cultures. Allows for kinetic profiling. |
| Automated Liquid Handling Systems | Precisely and rapidly dispenses nanoliter to microliter volumes of compounds and reagents across 96- to 1536-well plates, enabling high-throughput screening [40]. |
| Patient-Derived Cell Lines | Cell cultures established directly from patient tumors. They better retain the genetic and phenotypic heterogeneity of the original tumor compared to immortalized cell lines, leading to more clinically relevant data [38]. |
| Druggable Genome-Tailored Compound Library | A focused library, potentially enriched by virtual screening against overexpressed or mutated proteins in the disease of interest (e.g., GBM), to increase the likelihood of finding hits with selective polypharmacology [38]. |
Workflow and Pathway Visualizations
Integrated HTS to Hit Characterization Workflow
Phenotypic Hit MoA Deconvolution Pathway
FAQs: Core Concepts and Troubleshooting
Q1: What is the primary advantage of kinetic phenotypic screening over endpoint assays? Kinetic profiling captures the temporal interaction of compounds with cells, allowing for the monitoring of both immediate, transient effects and long-term responses. This continuous sampling can reveal distinct, temporally isolated biological activities and off-target effects that are easily missed in single time-point endpoint assays [41].
Q2: During hit selection, my hit rate is unusually high. What could be the cause? A high hit rate can indicate assay interference or excessive background noise. Re-evaluate your hit selection criteria. A typical hit rate for a well-designed phenotypic screen should be around 1–3% [42]. Ensure your criteria for a significant change in the normalized cell index (or other readout) are stringent enough, for instance, requiring a change of 25-40% over the control, and confirm that controls are stable [41].
Q3: Many of my hit compounds show cellular toxicity. How can I address this early on? It is crucial to incorporate a toxicity assessment directly into your primary screening workflow. For microscopy-based assays, compare cell counts (e.g., nuclei count) between treated and control samples. For other formats, run a parallel viability assay like MTT. ruthlessly discard hits that show toxicity, even if mild, and focus on those with a high selectivity index (SI) [42].
Q4: Why is target deconvolution challenging after a phenotypic screen, and is it always necessary? Phenotypic screening is target-agnostic, so the molecular mechanism of action (MoA) for a hit compound is initially unknown. While identifying the target aids in lead optimization and safety profiling, it is not always strictly necessary for clinical development. There are examples of safe and effective drugs, such as cyclosporine and niclosamide, used without a full understanding of their MoA [42].
Technical Guides: Protocols and Best Practices
Experimental Protocol: Kinetic Profiling Using Impedance-Based Readouts
This protocol outlines the steps for performing kinetic phenotypic screening using a Real-Time Cell Electronic Sensing (RT-CES) system to monitor compound effects [41].
Step 1: Cell Seeding and Background Measurement
- Seed adherent mammalian cells (e.g., A549 lung cancer cells) into microelectronic plates (E-Plates) integrated with gold microelectrode arrays.
- Allow cells to adhere and establish growth. The system applies a low AC voltage (20 mV) to create an electric field between electrodes. The impedance readout, often expressed as a Cell Index, is proportional to the number of cells, their morphology, and adhesive characteristics [41].
Step 2: Compound Addition and Kinetic Data Acquisition
- Add the compound library to the cells. Screen libraries can include FDA-approved drugs, natural products, and bioactive compounds.
- Perform short-term kinetic monitoring: Sample the cellular response every 2 minutes immediately after compound addition for a duration of 1 hour to capture fast, transient events.
- Automatically proceed to long-term kinetic monitoring: Sample the cellular response every 30 minutes from 1 hour to 48 hours post-compound addition to capture slower, more complex phenotypic changes [41].
Step 3: Hit Identification and Selection Criteria
- Analyze the Time-Dependent Cell Response Profiles (TCRPs).
- For short-term responses: Classify a compound as a "hit" if it causes a normalized cell index change of ≥25% of the control mean at any time point within the first hour.
- For long-term responses: Classify a compound as a "hit" if it causes a normalized cell index change of ≥40% of the control at any time point between 1 and 48 hours. If the compound increases the signal above the control for the entire duration, use the 25% threshold [41].
Step 4: Profile Clustering and Mechanistic Prediction
- Cluster the TCRPs of the hit compounds using hierarchical clustering analysis.
- Compounds with similar biological mechanisms of action will typically cluster together, allowing for predictive mechanistic classification (e.g., calcium modulators, anti-mitotics, DNA damaging agents) [41].
Workflow Visualization: Kinetic Screening Campaign
The following diagram illustrates the key stages of a kinetic phenotypic screening campaign.
Troubleshooting Guide: Common Experimental Issues
The flowchart below provides a systematic approach to diagnosing and resolving common problems in kinetic screening.
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below lists key reagents and materials essential for setting up a kinetic phenotypic screening campaign, based on the protocols described in the search results.
Table 1: Key Research Reagent Solutions for Kinetic Phenotypic Screening
| Item | Function/Description | Example/Criteria |
|---|---|---|
| Cell Lines | Biologically relevant models used in the phenotypic assay. | A549 non-small lung cancer cells, PC3 prostate cancer cells, or other disease-relevant cell types [41]. |
| Compound Libraries | Collections of small molecules screened for biological activity. | Libraries containing FDA-approved drugs, natural products (29%), and bioactive compounds (18%) are commonly used [41]. |
| Microelectronic Plates (E-Plates) | Specialized plates with integrated gold microelectrode arrays for impedance-based monitoring. | Used in the RT-CES system to provide a non-invasive readout of cellular status [41]. |
| Viability Assay Kits | Used for parallel assessment of compound toxicity. | MTT assay kits are recommended to run alongside the primary screen to calculate a Selectivity Index [42]. |
| Follow-up Compound Subsets | Structurally related compounds for hit validation and optimization. | Panels of analogs for Structure-Activity Relationship (SAR) studies are critical post-hit identification [42]. |
Data Interpretation: Analyzing Kinetic Profiles
The kinetic profiles generated contain rich biological information. The table below summarizes how to interpret common Time-Dependent Cell Response Profile (TCRP) patterns.
Table 2: Interpreting Kinetic Profile Patterns in TCRP Analysis
| TCRP Pattern | Potential Biological Interpretation | Clustering Example |
|---|---|---|
| Rapid, transient change in Cell Index | Often indicates fast-acting pathways, such as GPCR or ion channel modulation [41]. | Calcium level and pathway modulators [41]. |
| Delayed, sustained decrease in Cell Index | Suggests mechanisms that require time to manifest, such as inhibition of cell proliferation or induction of apoptosis [41]. | Anti-mitotics, DNA damaging agents, and protein synthesis inhibitors [41]. |
| Multiple distinct kinetic phases | Can indicate a compound with multiple, temporally separated mechanisms of action or off-target effects [41]. | Complex clusters requiring sub-analysis; confirms the value of kinetic data over single time-points [41]. |
| Profile similarity across compounds | High similarity in TCRPs is predictive of a shared biological mechanism of action (MoA) [41]. | Compounds with known similar activity (e.g., steroidal nuclear receptor modulators) cluster together [41]. |
Overcoming Challenges: Best Practices and Pitfalls in Kinetic Data Generation
FAQs: Understanding and Identifying Artefacts
Q1: What are the most common types of compound-mediated interference in high-content phenotypic screening?
Compound-mediated interference can be broadly divided into two categories [43]:
- Technology-related interference: This includes compound autofluorescence and fluorescence quenching. These compounds interfere with the optical detection system itself, producing artifactual bioactivity readouts that can mask true biological effects [43].
- Non-technology-related biological interference: This primarily involves compound-induced cellular injury or cytotoxicity, and dramatic changes in cell morphology (e.g., cell rounding, detachment). These effects can lead to false positives or negatives, especially if cell loss is significant enough to invalidate the image analysis algorithm [43].
Q2: How can I determine if a hit from my cytotoxicity screen is a genuine positive or an artefact caused by compound autofluorescence?
Statistical analysis of fluorescence intensity data is a key first step, as autofluorescent compounds will typically appear as outliers. This should be followed by [43]:
- Manual image review: Visually inspect the images for unusually bright signals that are not cell-associated.
- Orthogonal assays: Implement a secondary assay that uses a fundamentally different detection technology (e.g., luminescence) to confirm the biological activity.
- Counter-screens: Run a dedicated assay to flag compounds with autofluorescent properties under your experimental conditions.
Q3: What experimental design strategies can mitigate the impact of compound-mediated cell loss in kinetic profiling assays?
Proactive experimental design is crucial for managing cell loss [43]:
- Optimal Cell Seeding Density: During assay development, determine a cell seeding density that is robust to minor compound-induced effects.
- Adaptive Image Acquisition: Configure the HCS instrument to acquire multiple fields of view until a pre-set threshold number of cells is imaged. This helps ensure statistical significance in wells with moderate cell loss, though it may be ineffective with substantial cell loss and can prolong acquisition times [43].
- Reference Compounds: Use known cytotoxic compounds and optically inert compounds as controls to establish expected ranges for nuclear counts and fluorescence intensity [43].
Q4: Beyond compounds, what other sources of artefacts should I consider in high-content screening?
Other common sources of interference include [43]:
- Endogenous substances: Culture media components like riboflavins can autofluoresce and elevate background signals. Cells and tissues themselves contain fluorescent molecules like NADH and FAD [43].
- Exogenous contaminants: Lint, dust, plastic fragments from labware, and microorganisms can cause image-based aberrations like focus blur and image saturation, complicating downstream analysis [43].
Table 1: Common Compound Interference Mechanisms and Mitigation Strategies
| Interference Mechanism | Impact on HCS Assay | Quantitative Flagging Method | Recommended Mitigation Strategy |
|---|---|---|---|
| Compound Autofluorescence | Artifactual increase in fluorescence signal; false positives/negatives [43] | Statistical outlier analysis of fluorescence intensity [43] | Orthogonal, non-fluorescence-based assay; counter-screens for autofluorescence [43] |
| Fluorescence Quenching | Artifactual decrease or loss of fluorescence signal; false negatives [43] | Statistical outlier analysis of fluorescence intensity [43] | Orthogonal, non-fluorescence-based assay; confirm activity with an alternative detection method [43] |
| Cytotoxicity / Cell Loss | Reduced cell count; dramatic morphological changes; compromised analysis [43] | Statistical outlier analysis of nuclear counts and intensity; Z-factor decline [43] | Adaptive image acquisition; use of viability markers; orthogonal viability assays [43] |
| Altered Cell Adhesion | Significant cell loss independent of death; invalidated segmentation [43] | Statistical outlier analysis of nuclear counts and cell area metrics [43] | Use of ECM-coated plates; optimize cell attachment during assay development [43] |
Table 2: Key Reagent Solutions for Mitigating Artefacts in Cytotoxicity Screening
| Research Reagent / Material | Function in Assay | Role in Artefact Mitigation |
|---|---|---|
| Well-Characterized Cell Lines | Provides a biologically relevant model system for phenotypic screening [44]. | Reduces biological variability and improves assay reproducibility, aiding in distinguishing true hits from artefacts [44]. |
| ECM/PDL Coated Microplates | Enhances cell attachment to the assay plate surface. | Mitigates artefactual signal loss caused by compound-induced disruption of cell adhesion [43]. |
| Reference Cytotoxic Compounds | Serves as a positive control for inducing cell death. | Establishes a baseline for expected morphological changes and viability metrics, helping to calibrate the assay [43]. |
| Reference Inert/Optically Neutral Compounds | Serves as a negative control for non-biological effects. | Helps identify and flag compounds that interfere with the assay detection technology (e.g., autofluorescence) [43]. |
| Cell Viability Dyes (e.g., Propidium Iodide) | Distinguishes live from dead cells. | Provides an orthogonal measurement of cytotoxicity to confirm phenotypes observed in the primary readout. |
| Riboflavin-Free / Phenol Red-Free Media | Supports cell health during live-cell imaging. | Reduces background autofluorescence from media components, improving signal-to-noise ratio [43]. |
Experimental Protocols
Protocol 1: Counter-Screen for Identification of Autofluorescent Compounds
Objective: To identify compounds in a library that exhibit autofluorescence within the spectral channels used in the primary HCS assay, allowing them to be flagged as potential artefacts [43].
Materials:
- Assay plates (e.g., 384-well microplates)
- Compound library
- Cell culture medium (without phenol red or fluorescent probes)
- Dimethyl sulfoxide (DMSO)
- High-content imaging system
Method:
- Plate Preparation: Dispense cell culture medium into all wells of the assay plate. Do not seed any cells.
- Compound Transfer: Transfer compounds from the library into the assay plate using the same concentration and volume of DMSO as used in the primary HCS assay.
- Control Wells: Include control wells containing medium with the same concentration of DMSO (vehicle control).
- Image Acquisition: Incubate the plate for the duration equivalent to your primary assay. Then, image the plate using the exact same microscope settings, light sources, and filter sets defined in your primary HCS assay protocol.
- Data Analysis: Measure the mean fluorescence intensity for each well in all relevant channels. Statistically identify compounds that show fluorescence intensity values that are outliers (e.g., more than 3 standard deviations above the mean of the vehicle controls) [43].
Protocol 2: Orthogonal Cell Viability Assay to Confirm Cytotoxicity
Objective: To confirm compound-induced cytotoxicity using a detection method independent of high-content imaging, such as luminescence.
Materials:
- CellTiter-Glo Luminescent Cell Viability Assay kit (or equivalent)
- White-walled, clear-bottom assay plates
- Compound-treated cells and appropriate controls
- Microplate reader capable of detecting luminescence
Method:
- Cell Seeding and Treatment: Seed cells and treat with test compounds in a white-walled assay plate, replicating the conditions of the HCS assay as closely as possible.
- Equilibration: After the treatment period, equilibrate the plate to room temperature for approximately 30 minutes.
- Reagent Addition: Add a volume of CellTiter-Glo Reagent equal to the volume of cell culture medium present in each well.
- Mixing and Incubation: Mix the contents on an orbital shaker for 2 minutes to induce cell lysis, and then incubate at room temperature for 10 minutes to stabilize the luminescent signal.
- Signal Measurement: Record the luminescence signal using a microplate reader. The signal is proportional to the amount of ATP present, which is directly proportional to the number of viable cells.
- Data Correlation: Compare the viability results from this orthogonal assay with the cell count data extracted from the HCS assay. Genuine cytotoxic compounds will show a strong correlation between decreased cell counts in imaging and decreased luminescent signal.
Visualization Diagrams
Experimental Workflow for Artefact Mitigation
Mechanisms of Compound Interference
Establishing Robust Controls and Determining Optimal Kinetic Sampling Intervals
FAQs and Troubleshooting Guides
FAQ 1: What defines a "robust" control in kinetic cytotoxicity profiling?
Answer: In kinetic cytotoxicity profiling, a "robust" control serves as a reliable benchmark that minimizes variability and ensures consistent assay performance across multiple experimental runs and plates. Robust controls are characterized by their ability to generate reproducible, high-quality data with a clear distinction between positive and negative effects, typically measured by a Z' factor ≥ 0.5, which indicates an excellent assay suitable for screening [45].
You should implement two primary types of controls:
- Positive Control: A compound known to induce a profound cytotoxic phenotype, such as staurosporine for apoptosis induction or cytochalasin D for cytoskeletal disruption [46] [47].
- Negative Control: A vehicle (e.g., DMSO) that does not alter cellular morphology or viability, establishing a baseline for untreated cells.
FAQ 2: How do I determine the optimal kinetic sampling intervals for my assay?
Answer: Determining optimal kinetic sampling intervals depends on the biological process being measured and the onset of the phenotypic changes. There is no universal interval; it must be empirically determined for each assay system.
Follow this strategic approach:
- Pilot Experiment: Conduct a wide-interval time-course experiment (e.g., 0, 2, 4, 8, 12, 24, 48 hours) after compound treatment to identify when key phenotypic events begin and stabilize [45].
- Refined Sampling: Based on pilot data, increase sampling frequency around the time points where dynamic changes occur. For example, if apoptosis initiation is observed between 4-8 hours, sample every hour within that window.
- Balance Practicality: Ensure the final sampling plan is logistically feasible. Long-duration experiments (over days or weeks) require less frequent sampling once a stable phenotype is established [45].
Table 1: Recommended Sampling Intervals for Common Cytotoxicity Phenomena
| Cellular Process | Early Phase Intervals (0-12h) | Late Phase Intervals (12-48h+) | Key Readouts |
|---|---|---|---|
| Apoptosis | Every 1-2 hours | Every 4-6 hours | Caspase-3/7 activation, nuclear fragmentation [47] |
| Mitochondrial Toxicity | Every 30-60 minutes | Every 4-8 hours | Loss of mitochondrial membrane potential [22] [47] |
| Cytoskeletal Disruption | Every 30 minutes | Every 2-4 hours | Actin fiber area, cell shape changes [47] |
| Necrosis / Loss of Membrane Integrity | Every 1-2 hours | Every 4-6 hours | LIVE/DEAD staining, membrane permeability dyes [22] |
| Proliferation Inhibition | N/A | Every 12 hours | EdU incorporation, cell count [47] |
FAQ 3: My assay has high well-to-well variability in cell count. How can I troubleshoot this?
Answer: High well-to-well variability compromises data quality. The issue often originates from cell preparation and handling steps.
Problem: Low or High Cell Density.
- Solution: Repeat the experiment to determine the optimal seeding cell count for your specific cell type and plate format. Ensure the cell suspension is homogeneous before seeding by gently mixing. Avoid excessive forceful pipetting, which can damage cells and create inconsistency [22].
Problem: Air Bubbles.
- Solution: Air bubbles in wells during imaging can cause focal plane shifts and analysis errors. Carefully check plates before reading and use a syringe needle to gently break any visible bubbles [22].
FAQ 4: My positive control is not producing the expected phenotype. What could be wrong?
Answer: Ineffective positive controls undermine your entire experiment.
Problem: Compound Degradation or Incorrect Preparation.
- Solution: Prepare fresh stock solutions of control compounds or aliquot and store them correctly to prevent freeze-thaw cycles. Verify the concentration and solvent used against published protocols [46].
Problem: Incorrect Cell Model or Assay Conditions.
- Solution: Confirm that your cell model expresses the target of your positive control. For example, some targeted electrophiles may not produce an effect if their protein target is absent or not highly expressed in the cell line used [46]. Optimize treatment duration and concentration in your specific system.
FAQ 5: How can I distinguish specific bioactivity from nonspecific cytotoxicity in high-content screens?
Answer: This is a central challenge in phenotypic screening. The key is to use multiparametric data to identify signatures of generalized cell injury.
- Strategy: Incorporate a panel of reference cytotoxic and nuisance compounds (e.g., microtubule poisons, nonspecific electrophiles) into your assay validation. By analyzing their multiparametric morphological profiles (e.g., using Cell Painting), you can define a "gross injury" cluster. Test compounds whose profiles cluster here at higher concentrations are likely acting through nonspecific cytotoxic mechanisms rather than a targeted bioactivity [46].
- Triage Workflow: Active compounds should be evaluated in a concentration-response format. Selective compounds typically show a window between their functional activity and the onset of the gross injury phenotype, whereas nonspecific compounds will induce cytotoxicity at or near their effective concentration [46].
Experimental Protocols
Protocol 1: Establishing a Robust Kinetic Apoptosis Profile
This protocol details how to kinetically profile compound-induced apoptosis using a fluorogenic caspase sensor.
Key Reagents:
- Invitrogen CellEvent Caspase-3/7 Green Detection Reagent [47]
- Nuclear stain (e.g., Hoechst 33342) [47]
- A pro-apoptotic positive control (e.g., 1 µM Staurosporine) [47]
Methodology:
- Cell Preparation: Seed cells in a 96-well microplate at an optimized density for confluence and allow to adhere overnight [22].
- Compound Treatment: Add the test compound, positive control (staurosporine), and vehicle control (DMSO) to respective wells.
- Kinetic Staining and Imaging: Add the CellEvent reagent and nuclear stain directly to the culture medium. This fluorogenic reagent does not require washing [47].
- Data Acquisition: Place the plate in a pre-warmed high-content imager. Program the instrument to image the same fields of view repeatedly at predetermined intervals (e.g., every hour for 24 hours).
- Analysis: Use HCS Studio software or equivalent to quantify the percentage of cells that are positive for the bright green-fluorescent caspase signal in each well at each time point [47].
Protocol 2: Kinetic Profiling of Cytoskeletal Disruption
This protocol measures changes in actin architecture over time in response to compounds.
Key Reagents:
- Alexa Fluor 488 phalloidin (to stain F-actin) [47]
- Anti-tubulin antibody (optional, for microtubule visualization) [47]
- Cytoskeletal disruptive agent (e.g., Cytochalasin D) as a positive control [47]
Methodology:
- Cell Preparation and Treatment: Seed cells in a 96-well plate. The following day, treat with a concentration range of the test compound and a positive control like cytochalasin D (e.g., from 0.375 µM to 50 µM) [47].
- Kinetic Sampling and Fixation: For kinetic sampling, at each selected time point (e.g., 1, 2, 4, 8 hours), remove a replicate plate from the incubator and immediately fix the cells with a fixation solution. Note: True kinetic imaging of live cells requires transfection with a fluorescent actin tag, as fixation is end-point.
- Staining: Permeabilize the fixed cells, stain with Alexa Fluor 488 phalloidin and other labels (e.g., HCS CellMask stain for cytoplasm), and counterstain nuclei with Hoechst 33342 [47].
- Image Acquisition and Analysis: Image the plate using a high-content analysis platform. Use the analysis software to segment cells and quantify the mean fiber area of actin per cell or other morphological parameters [47].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Kinetic Cytotoxicity Phenotypic Screening
| Reagent Name | Function | Key Application |
|---|---|---|
| HCS NuclearMask Stains (Blue, Red, Deep Red) | Segmentation; labels nucleus for cell identification and counting [47]. | Foundational for all high-content assays; enables cell cycle analysis via DNA content. |
| HCS CellMask Stains (Multiple colors) | Segmentation; labels the entire cytoplasm to define cell boundaries [47]. | Critical for analyzing cell shape, size, and morphological changes like neurite outgrowth. |
| CellEvent Caspase-3/7 Green Reagent | Apoptosis detection; fluorogenic probe activated by caspase-3/7 [47]. | Kinetic apoptosis profiling in live cells without wash steps. |
| HCS Mitochondrial Health Kit | Multiplexed viability and mitochondrial function [47]. | Simultaneously measures cell number, mitochondrial membrane potential, and cell viability. |
| CellROX Reagents | Detection of reactive oxygen species (ROS) [47]. | Profiling oxidative stress as a mechanism of cytotoxicity. |
| Click-iT EdU Assay | Cell proliferation measurement [47]. | Quantifies DNA synthesis and proliferation rates kinetically. |
| Alexa Fluor Phalloidin | Stains filamentous actin (F-actin) [47]. | Visualizing and quantifying cytoskeletal remodeling and disruption. |
| HCS LipidTOX Stains | Detection of phospholipidosis and steatosis [47]. | Assessing compound-induced lipid accumulation and organelle injury. |
Experimental Workflow and Signaling Pathways
Kinetic Profiling Workflow
The following diagram illustrates the end-to-end workflow for establishing a robust kinetic profiling experiment, from initial setup to data interpretation.
Cytotoxicity Mechanism Inference
This diagram outlines the logical decision process for interpreting multiparametric data to distinguish specific bioactivity from nonspecific cellular injury.
In kinetic profiling for cytotoxicity phenotypic screening, distinguishing between cytostatic (growth-arresting), cytotoxic (cell-killing), and adaptive (transiently resistant) cellular responses is fundamental to accurate drug evaluation and development. Traditional endpoint assays, which provide a single snapshot in time, often fail to capture the rich dynamic heterogeneity of these responses [48]. Multiparametric endpoints, derived from real-time, label-free technologies, provide a solution by quantifying temporal changes in key cellular parameters such as cell mass, metabolic activity, and membrane integrity [48] [49]. This technical support center provides guidelines and troubleshooting advice for implementing these kinetic approaches within your research, ensuring robust distinction of complex drug-induced phenotypes.
Frequently Asked Questions (FAQs) & Troubleshooting
1. FAQ: Our dose-response data shows high variability between replicates when testing novel compounds. What key factors should we control for?
- Answer: Irreproducibility in dose-response measurements often stems from uncontrolled variation in cell culture conditions. To ensure robust and reproducible data, please verify the following:
- Uniform Cell Growth: Conduct preliminary experiments to identify a plating density that ensures uniform, exponential growth throughout the entire assay duration, avoiding both lag phase and contact inhibition [50]. Growth conditions should be optimized for each cell line.
- Consistent Assay Conditions: Maintain strict consistency in media composition, serum batches, and the volume of medium in each assay well. The quality of multi-well plates can vary; we recommend pre-screening batches from vendors for their ability to support uniform cell growth [50].
- Appropriate Metrics: Use growth rate inhibition (GR) metrics that correct for confounding effects of variable cell division rates, rather than relying solely on viability percentages. This provides a more robust estimation of drug potency [50].
2. FAQ: How can we determine if a drug is cytostatic or cytotoxic using real-time data?
- Answer: The fundamental distinction lies in the trajectory of cell mass or number over an extended period.
- Cytostatic Response: The measured parameter (e.g., cell mass from QPI or normalized cell count) will plateau over time. The final cell number remains at or near the starting point, indicating a halt in proliferation without significant cell death [48] [51]. This is often observed with high doses of drugs like palbociclib [51].
- Cytotoxic Response: The measured parameter will show an initial increase followed by a pronounced decrease, falling below the starting cell number. This indicates active cell death and loss, as seen with drugs like paclitaxel and doxorubicin [48] [51].
- Protocol: Use a real-time cell imager (e.g., Incucyte) or a Quantitative Phase Imaging (QPI) system to track cell number/mass for at least 72 hours post-treatment. Compare the final cell number to the initial seeding number.
3. FAQ: We suspect our cell population has an adaptive response to a drug. What kinetic signature should we look for?
- Answer: An adaptive response is characterized by transient resistance. The kinetic profile typically shows a multi-phasic pattern [51] [49]:
- Initial Inhibition: An initial drop in growth rate or cell number immediately after drug addition.
- Recovery Phase: A subsequent recovery in growth rate or stabilization of cell number, indicating the population is adapting to the drug's pressure.
- Potential Secondary Decline: In some cases, a secondary decline may occur later, reflecting other mechanisms like nutrient depletion or the emergence of a different cell fate.
4. FAQ: Our high-content screening data reveals significant heterogeneity in single-cell responses. How should we analyze and interpret this?
- Answer: Single-cell heterogeneity is a biological reality, not noise. Embrace it with the right tools:
- Analysis: Use clustering algorithms to group single-cell trajectories based on their kinetic profiles (e.g., responders, non-responders, adaptive responders) [48] [49].
- Interpretation: The presence of distinct subpopulations can explain partial drug efficacy and the emergence of resistance. Quantify heterogeneity using metrics like the standard deviation of growth rates (SGR) across the population at different time points [48].
- Protocol: After segmenting single cells from time-lapse imaging data, extract metrics like specific growth rate (SGR) for each cell. Then, perform principal component analysis (PCA) and k-means clustering on the time-series data to identify distinct response clusters.
Quantitative Data and Experimental Protocols
Key Multiparametric Endpoints for Response Characterization
The following table summarizes critical quantitative parameters that can be derived from kinetic data to classify cellular responses.
Table 1: Key Multiparametric Endpoints for Cytotoxicity Profiling
| Parameter Name | Abbreviation | Description | Interpretation in Advanced Models |
|---|---|---|---|
| Specific Growth Rate [48] | SGR | Exponential growth constant, computed as the rate of change of cell mass over time, normalized by initial mass. | The core output of many models; can be made time-dependent (GR(t)) to capture adaptation [50]. |
| Half-Maximal Effective Concentration [48] | EC50 / GR50 | Therapy concentration at which cells exhibit 50% of their maximum response. | Can be calculated for different phenotypes (e.g., death rate vs. phase arrest) in a cell cycle model [51]. |
| Depth of Response [48] | DoR | Maximum difference in SGR between untreated cells and cells at the highest therapy concentration. | Reflects the combined cytostatic/cytotoxic efficacy inferred from the model. |
| Time of Response [48] | ToR | The average time required to elicit a measurable response to therapy. | Directly measurable from kinetic data; can be linked to the timescales of underlying molecular processes in a model. |
| Standard Deviation of SGR [48] | SD | Standard deviation of SGR across the cell population at a given time/concentration. | A direct measure of cell-to-cell heterogeneity in response. |
Detailed Experimental Protocol: Real-Time Kinetic Profiling using Quantitative Phase Imaging (QPI)
This protocol is adapted for a 96-well plate format to determine drug sensitivity, cytotoxicity, and heterogeneity [48].
Key Reagent Solutions:
- Cell Lines: Adherent cancer cell lines (e.g., MCF-7, BT-474, MDA-MB-231).
- Assay Plates: 96-well glass-bottom plates suitable for high-resolution microscopy.
- Drug Solutions: Prepare a 6-point dose-response curve for each therapy in triplicate, including solvent controls (e.g., DMSO).
- Validation Assay: CellTiter-Glo (CTG) ATP assay for endpoint viability comparison.
Procedure:
- Cell Seeding: Seed cells in the 96-well plate at a density that ensures exponential growth for the full 72-hour assay. This density must be determined empirically for each cell line [50].
- Equilibration: Incubate the plate for 3 hours to allow cells to adhere and stabilize.
- Drug Exposure & Imaging: Add drug solutions to the respective wells. Immediately transfer the plate to the QPI microscope housed inside a tissue culture incubator.
- Image Acquisition: For each well, automatically acquire images at nine predefined locations every 15-30 minutes for 72 hours. This typically yields data for 20,000 to 130,000 individual cells or cell clusters per experiment [48].
- Image Analysis:
- Segmentation: Automatically segment individual cells/clusters from the background in each frame.
- Mass Calculation: Calculate the dry mass of each cell/cluster from the quantified phase shift of light.
- Trajectory Extraction: For each segmented object, track its mass over time to generate mass-versus-time traces.
- Parameter Extraction:
- For each single-cell trajectory, perform a linear regression on the mass data from periods of steady growth to calculate the slope (dm/dt).
- Normalize this slope by the initial mass of the cell/cluster to compute the Specific Growth Rate (SGR).
- Endpoint Correlation (Optional): After 72 hours of imaging, lyse the plate and perform a CTG assay according to the manufacturer's instructions. Compare the QPI-derived EC50 values with CTG-derived EC50 values to validate the method [48].
Computational Modeling of Cell Cycle Effects
For a deeper understanding of how drugs induce cytostatic or cytotoxic effects, integrating kinetic data with computational models of the cell cycle is highly informative.
- Workflow Overview:
- Treat cells with drugs and collect time-lapse data for total cell numbers and cell cycle phase distribution (using a fluorescent reporter).
- Use a system of ordinary differential equations (ODEs) with a Linear Chain Trick (LCT) to model the cell cycle as a series of steps through G1 and S-G2-M phases. This model can capture oscillatory dynamics and phase-specific drug effects [51].
- Fit the model parameters to your experimental data to infer how the drug alters the rate of progression through specific cell cycle phases (e.g., G1 extension) and/or induces phase-specific cell death [51].
The diagram below illustrates the logic of using kinetic data to parameterize a computational model that distinguishes drug mechanisms.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Reagent Solutions for Kinetic Cytotoxicity Profiling
| Reagent / Technology | Function / Readout | Key Considerations |
|---|---|---|
| Quantitative Phase Imaging (QPI) [48] | Label-free measurement of cell mass and growth rate. | Ideal for long-term, multiparametric screening; directly measures mass accumulation. |
| Real-Time Glo/Flour Assays [49] | Multiplexed measurement of cell viability (metabolism) and cytotoxicity (membrane integrity) over time. | Allows kinetic profiling in standard plate readers; multiplexing validates mechanism. |
| CellTiter-Glo (CTG) [48] [4] | Endpoint ATP-based luminescent assay for cell viability. | Useful as a gold-standard endpoint for validation; does not provide kinetics. |
| Fluorescent Cell Cycle Reporters [51] | Live-cell tracking of cell cycle phase transitions (G1, S, G2, M). | Essential for linking cytotoxic effects to specific cell cycle perturbations. |
| Impedance-Based Systems (e.g., xCELLigence) [6] | Label-free, real-time monitoring of cell adhesion, proliferation, and death. | Excellent for tracking overall cytopathic effects; lower resolution than imaging. |
Data Handling and Analysis Strategies for Complex, Time-Resolved Datasets
Frequently Asked Questions (FAQs)
Q1: Our high-content screening (HCS) data shows high fluorescence background. What could be causing this and how can we mitigate it? High background fluorescence in HCS can stem from multiple sources. Key culprits include autofluorescence from culture media components like riboflavins, which fluoresce in the ultraviolet through green fluorescent protein (GFP) variant spectral ranges (ex. 375-500 nm and em. 500-650 nm) [43]. Test compounds themselves can be autofluorescent or act as fluorescence quenchers [43]. To mitigate this:
- Screen Compounds: Prior to HCS, screen test compounds for intrinsic fluorescence or color using "no-cell" blanks [19].
- Modify Media: For live-cell imaging, consider using media without fluorescent components like riboflavin to reduce background [43].
- Statistical Flagging: Use statistical analysis of fluorescence intensity data to identify outliers that may indicate compound interference [43].
Q2: How can we distinguish specific phenotypic changes from general cytotoxicity in our screening data? General cytotoxicity can obscure specific phenotypic changes and lead to false positives/negatives [43]. To address this:
- Multiparametric Analysis: Move beyond single-endpoint assays. HCS allows you to extract multiple features (e.g., organelle morphology, cell count, membrane integrity) that can differentiate specific phenotypes from general cell death [19] [52].
- Employ Counter-Screens: Implement dedicated cytotoxicity assays (e.g., LDH release for membrane integrity) in parallel with your phenotypic screen [43].
- Analyze Cell Number: Statistically analyze nuclear counts and stain intensity; substantial cell loss compared to controls is a clear indicator of cytotoxicity that may invalidate further phenotypic analysis [43].
Q3: What is the impact of cell seeding density on the robustness of phenotypic profiling assays like Cell Painting? Cell seeding density is a critical experimental factor. A 2025 study specifically demonstrated a significant inverse relationship between seeding density and the Mahalanobis distance (a measure of phenotypic change) in Cell Painting assays [52]. This means that the same compound at the same concentration can produce different quantitative results depending on how many cells were plated, directly impacting the calculated benchmark concentrations (BMCs) for toxicity.
- Best Practice: During assay development, verify signal linearity with cell density and optimize the seeding density for your specific cell line and plate format. A common range is 5 × 10³–2 × 10⁴ cells/well in 96-well plates [19]. Always report the seeding density used to ensure reproducibility [52].
Q4: Our data pipeline struggles with the volume and velocity of real-time kinetic data. What architectural principles should we adopt? Traditional batch processing ("store–analyze–act") is insufficient for real-time kinetic data. The paradigm must shift to "analyze–act–store" [53].
- In-Memory Computation: Use RAM as the active compute layer to keep latency in microseconds instead of seconds, enabling evaluation of millions of events per second [53].
- Stateful Processing: Choose systems that can track state to correlate related events over time, which is crucial for detecting patterns in kinetic data [53].
- Blend Live and Historical Data: Compare fresh streaming data against historical baselines to detect deviations and predict outcomes, enabling use cases like dynamic fraud scoring or demand forecasting [53].
Troubleshooting Guides
Problem 1: High Variability and Low Reproducibility in Multiparametric Readouts
Potential Causes and Solutions
| Cause Category | Specific Issue | Diagnostic Steps | Solution |
|---|---|---|---|
| Assay Execution | Inconsistent cell seeding density [52] | Review protocol; Count cells before seeding. | Optimize and standardize seeding density; Use automated cell counters and seed within validated linear range [19]. |
| Suboptimal assay reagent incubation [19] | Review protocol timing and conditions. | Adhere to optimized dye incubation times (e.g., 2–4 h for MTT; 3 h for Neutral Red Uptake) and report all conditions [19]. | |
| Compound Interference | Compound autofluorescence or quenching [43] | Include "no-cell" blanks with compounds; Manually review images. | Pre-screen compounds; Use orthogonal assays with different detection technologies [43]. |
| Compound-mediated cytotoxicity or altered adhesion [43] | Analyze nuclear counts and cell morphology; Check for significant cell loss. | Use adaptive image acquisition; Flag compounds causing substantial cell loss for further validation [43]. | |
| Data Processing | Inadequate normalization and background subtraction [19] | Review data processing scripts. | Subtract background from blank wells; Normalize viability to untreated (100%) and maximal lysis (0%) controls [19]. |
Problem 2: Managing and Analyzing Extremely Large, High-Dimensional Datasets from Kinetic Profiling
Symptoms: Inability to process data in a timely manner, system crashes, long query latencies that preclude real-time analysis.
System Architecture & Data Flow The following diagram illustrates the core components of a real-time data processing pipeline designed to handle high-velocity kinetic data.
Solutions and Best Practices
Implement a Real-Time Data Pipeline: Move from batch to event-driven architecture. As data is generated, it should be ingested, processed, and made available within seconds [53].
- Tools: Use event streaming platforms (e.g., Apache Kafka) for ingestion and stream processing engines (e.g., Apache Flink) or real-time databases (e.g., ClickHouse) for processing [53].
- Benefit: This enables "analyze–act–store" workflows, where insights and actions happen while the data is still in flight [53].
Leverage In-Memory Computation: For ultra-low latency, data should be processed in memory (RAM) rather than relying on disk writes and reads. This is essential for maintaining millisecond-level query latency, even with complex filters and aggregates [53].
Ensure Data Integrity from the Start: Build data quality checks directly into the pipeline.
- Data Validation: Implement checks during data entry for accuracy, consistency, and adherence to predefined rules [54].
- Audit Trails: Maintain detailed logs of data changes and access activities for monitoring and forensic analysis [54].
- Version Control: Use versioning for code and configurations to ensure reproducibility [55].
Problem 3: Integrating Multi-Omics Data with Phenotypic Screening Results
Symptoms: Difficulty correlating findings from different platforms (e.g., HCS images with transcriptomic or proteomic data), leading to fragmented insights.
Experimental Workflow for Integrated Profiling This workflow demonstrates how phenotypic screening can be seamlessly combined with high-plex molecular profiling, such as proteomics, within a single study.
Solutions and Best Practices
Adopt FAIR Data Principles: Ensure all datasets are Findable, Accessible, Interoperable, and Reusable [56]. This involves:
Use Unified Analysis Platforms: Leverage data portals or platforms that provide APIs for seamless integration with analysis workflows. This allows computation directly on the data without large-scale downloads, facilitating collaboration and reproducibility [56].
Apply Multivariate Statistical Analysis: For integrated analysis, use techniques that can handle high-dimensional data.
- Dimensionality Reduction: Apply Principal Component Analysis (PCA) to visualize and explore patterns across combined datasets [52].
- Quantitative Modeling: Calculate Mahalanobis distances to quantify overall phenotypic shift and model benchmark concentrations (BMCs) for chemical hazard assessment [52].
Research Reagent Solutions
The following table details key reagents and materials essential for robust kinetic profiling cytotoxicity assays.
| Item | Function / Application | Key Considerations |
|---|---|---|
| Cell Painting Dyes | Multiplexed fluorescence staining of cellular structures (Golgi, ER, cytoskeleton, etc.) for phenotypic profiling [52]. | Ensure dye compatibility with your imaging system's filters and check for spectral crosstalk. |
| nELISA Platform | High-throughput, high-plex (e.g., 191-plex) quantitative profiling of secreted proteins (e.g., cytokines) [57]. | Overcomes reagent cross-reactivity (rCR), enabling large-scale secretome analysis alongside phenotypic screens [57]. |
| Classical Cytotoxicity Assays (MTT, LDH, NRU) | Measure cell viability via metabolic activity (MTT), membrane integrity (LDH), or lysosomal function (NRU) [19]. | Pre-screen compounds for interference; use multiplexed endpoints for mechanistic insight [19]. |
| U-2 OS Human Osteosarcoma Cells | A common, well-characterized cell line used in phenotypic profiling and high-content screening studies [52]. | Maintain consistent culture conditions and passage number; seed at optimized density for assay format (96-well vs. 384-well) [52]. |
| Reference Compounds | Compounds with known phenotypic or cytotoxic effects (e.g., staurosporine) used as controls [52]. | Include positive (cytotoxic), negative (inert), and phenotypic reference controls in every experiment to validate assay performance [52]. |
Demonstrating Value: Validation Against Classical Assays and Translational Impact
Benchmarking Kinetic Profiling Against MTT, LDH, and Other Endpoint Assays
This technical support center provides troubleshooting guidance for researchers integrating kinetic profiling into cytotoxicity phenotypic screening. Kinetic profiling involves continuous, real-time monitoring of cellular responses, offering a dynamic view of compound effects that traditional endpoint assays can obscure [58] [59]. This resource addresses common experimental challenges, framed within the broader thesis that kinetic assays provide superior mechanistic insight and predictive power for modern drug development.
FAQ: Fundamental Concepts and Comparisons
1. What is the core technological difference between kinetic profiling and endpoint assays?
Endpoint assays, such as MTT and LDH, provide a single snapshot of cellular status at a fixed time after compound exposure [60] [61]. In contrast, kinetic profiling utilizes live-cell compatible reagents and instrumentation to take repeated measurements from the same well over the entire duration of an experiment, generating a continuous curve of cellular response [59]. This allows for the capture of critical transient events and the calculation of rates of change, rather than just a final outcome.
2. What are the key advantages of kinetic profiling for cytotoxicity assessment?
Kinetic live-cell assays reveal critical dynamic information that endpoint snapshots can miss, such as the delay in degradation onset, the rate of cell death, and rapid protein recovery [58]. This transforms cytotoxicity testing from a descriptive discipline into a multiparametric one capable of detecting adaptive and sub-lethal cellular responses [19]. Furthermore, kinetic parameters provide a quantitative framework for comparing compounds, even those with similar endpoint profiles, enabling more informed structure-activity relationship (SAR) decisions [58].
3. When should I prioritize traditional endpoint assays like MTT or LDH?
Endpoint assays remain valuable for high-throughput initial compound screening due to their lower cost, established protocols, and suitability for automation [4]. They are also practical when live-cell imaging equipment is unavailable or when the specific readout (e.g., membrane integrity via LDH) is explicitly required. However, data from these assays should be interpreted with caution and ideally confirmed with independent endpoints or kinetic follow-up [19].
4. Can kinetic and endpoint assays be used together in a workflow?
Yes, an integrated workflow is often most powerful. A common strategy is to use high-throughput endpoint assays (e.g., MTT, LDH) for initial compound library screening to identify active hits, followed by kinetic profiling on a select subset of compounds for deeper mechanistic investigation and lead optimization [58] [5]. This combines the breadth of endpoint screening with the depth of kinetic analysis.
Troubleshooting Guide: Common Experimental Challenges
Problem: Endpoint and kinetic assay results appear contradictory.
- Potential Cause 1: The chosen endpoint measurement timepoint may miss peak activity or recovery. A compound might induce rapid cytotoxicity followed by cellular recovery, which an endpoint assay would completely fail to capture [58].
- Solution: Use kinetic profiling to first establish the full time-course of response for your model system. This will identify the optimal time window for endpoint measurements and reveal transient effects.
- Potential Cause 2: The assays are measuring different biological endpoints. For example, MTT measures metabolic activity while an LDH-based kinetic assay measures membrane integrity; a compound may affect these at different times and potencies [60].
- Solution: Carefully review the biological principle of each assay. Consider running multiple kinetic assays in parallel (if compatible) to build a comprehensive picture of the cytotoxic mechanism [60] [5].
Problem: High variability in kinetic assay readouts.
- Potential Cause: Inconsistent environmental control (e.g., temperature, CO₂) during repeated plate readings can stress cells and affect signal.
- Solution: Use an environmental-controlled plate reader for long-term kinetic runs. Ensure the assay reagents and protocol are optimized for long-term cell health [59]. Normalize data to the initial (time-zero) reading for each well to account for minor seeding differences.
Problem: Kinetic data shows a weak or noisy signal.
- Potential Cause: The cell density may be too low, or the reagent concentration may be sub-optimal for the specific cell type and measurement interval.
- Solution: Prior to the main experiment, perform a cell titration and reagent optimization experiment to establish a linear signal-to-cell relationship and determine the ideal reagent concentration for robust, sustained detection [60] [59].
Problem: Significant background signal interferes with LDH release measurements.
- Potential Cause: The fetal bovine serum (FBS) in the culture medium contains endogenous LDH, which elevates the background signal [60] [62].
- Solution: Reduce the FBS concentration to 1% during the compound treatment and measurement period to lower background, or use heat-inactivated serum [60] [61]. Always include a "medium-only" background control and subtract this value from your experimental readings [62].
Quantitative Data Comparison
The table below summarizes a comparative study of four cytotoxicity assays, highlighting key performance metrics.
Table 1: Comparison of Cytotoxicity Assay Performance in ZFL Cells [60]
| Assay | Mechanism | Detection Mode | Key Advantage | Key Disadvantage | Max EC₁₀ Variability* |
|---|---|---|---|---|---|
| MTT | Metabolic activity (tetrazolium reduction) | Colorimetric (Endpoint) | Established, sensitive | Destructive; formazan crystal solubilization required | 7.0-fold |
| LDH Release | Membrane integrity (enzyme release) | Colorimetric (Endpoint) | Simple, measures direct toxicity | High intra- and inter-assay variability; serum background | - |
| alamarBlue (AB) | Metabolic activity (resazurin reduction) | Fluorometric (Kinetic-friendly) | Non-destructive, easy to handle, can be multiplexed | Signal can saturate with high metabolic activity | - |
| CFDA-AM | Esterase activity & membrane integrity | Fluorometric (Kinetic-friendly) | Non-destructive, indicates viable cell count | Requires esterase activity | - |
Maximum factor of variation in EC10 values across four model compounds.
Table 2: Key Reagent Solutions for Cytotoxicity Profiling
| Reagent / Tool | Function | Application Context |
|---|---|---|
| MTT Tetrazolium Salt | Reduced by metabolically active cells to colored formazan. | Endpoint measurement of metabolic activity [60]. |
| LDH Assay Kit | Measures lactate dehydrogenase released from damaged cells. | Endpoint measurement of membrane integrity/necrosis [62] [61]. |
| alamarBlue (Resazurin) | Reduced by cells to fluorescent resorufin. | Live-cell, kinetic-friendly measurement of metabolic activity [60] [59]. |
| CellTox Green Dye | Binds DNA in dead cells with compromised membranes. | Live-cell, kinetic measurement of cytotoxicity [59]. |
| RealTime-Glo MT Cell Viability Assay | Generates a luminescent signal proportional to viable cell number. | Real-time, kinetic monitoring of cell viability without cell lysis [59]. |
| HiBiT Tagging System | Enables precise tagging and monitoring of endogenous protein levels. | Live-cell kinetic analysis of protein degradation [58]. |
Detailed Experimental Protocols
Protocol 1: Establishing a Kinetic Cytotoxicity Profile Using Live-Cell Assays
This protocol is designed for benchmarking a compound's cytotoxic kinetics against endpoint assays in a 96-well format.
Materials:
- Cell line of interest (e.g., ZFL, HEK293, primary cells)
- Test compounds
- RealTime-Glo MT Cell Viability Assay Reagents (or similar live-cell viability reagent) [59]
- CellTox Green Cytotoxicity Assay Reagents (or similar membrane integrity dye) [59]
- White-walled, clear-bottom 96-well assay plates
- Plate reader capable of kinetic luminescence and fluorescence measurements
Procedure:
- Cell Plating: Plate cells at an optimized density (e.g., 25,000 cells/well for ZFL cells [60]) in a total volume of 100 µL complete medium per well. Include control wells for background (medium only), vehicle (e.g., DMSO), and a cytotoxic positive control (e.g., 1-2% Triton X-100). Incubate for 24 hours.
- Reagent Addition: Prepare a 2x master mix of the RealTime-Glo MT and CellTox Green reagents according to the manufacturer's instructions. Add 100 µL of this master mix directly to each well, resulting in a 1x reagent concentration and a final volume of 200 µL/well [59].
- Compound Treatment: Add test compounds at the desired concentrations. For dose-response kinetics, prepare a dilution series.
- Kinetic Measurement: Immediately place the plate into a controlled-environment plate reader. Program the reader to take repeated measurements of luminescence (cell viability) and fluorescence (cytotoxicity) every 2-4 hours for 48-72 hours.
- Data Analysis: Normalize the raw luminescence and fluorescence values at each time point to the initial (T=0) reading or to vehicle controls. Plot the data as normalized signal over time to generate kinetic curves for viability loss and cytotoxicity induction.
Protocol 2: Standard Endpoint LDH Release Assay for Cross-Validation
This protocol provides a standardized method for the colorimetric LDH release assay [62] [61].
- Materials:
- Cell culture supernatant from treated cells
- Custom LDH assay reagents [62]:
- Buffer A (4mM INT in 0.2 M Tris-HCl, pH 8.2)
- Buffer B (6.4 mM NAD⁺, 320 mM lithium lactate, in 0.2 M Tris-HCl buffer)
- 1-Methoxyphenazine methosulfate (MPMS) supplement
- Stop Solution (1 M Acetic Acid)
- Clear 96-well plate
- Sample Collection: After compound treatment, centrifuge the cell culture plate at 1,500-2,000 rpm for 5 minutes. Carefully transfer 50 µL of supernatant from each well to a new clear 96-well assay plate without disturbing the cell pellet [62] [61].
- Assay Reagent Preparation: For one 96-well plate, combine 2.5 mL of Buffer A and 2.5 mL of Buffer B. Add 0.5 µL of MPMS supplement and mix thoroughly. Note: The reagent is light-sensitive.
- Reaction: Add 50 µL of the prepared Assay Reagent to each well containing the 50 µL supernatant. Mix gently on an orbital shaker (300-500 rpm for 15 seconds).
- Incubation: Incubate the plate in the dark at room temperature for 30-60 minutes.
- Stop Reaction: Add 50 µL of Stop Solution (1 M Acetic Acid) to each well to stabilize the colorimetric product.
- Measurement: Record the absorbance at 490 nm in a plate reader. Calculate % cytotoxicity by normalizing to vehicle control (0%) and lysed cell control (100%) values [62].
Signaling Pathways and Workflow Diagrams
The following diagrams illustrate the core biochemical principles and an integrated experimental workflow for benchmarking kinetic and endpoint assays.
Diagram 1: Principles of Kinetic vs. Endpoint Assays. Kinetic assays (yellow) enable continuous monitoring of various live-cell processes, while endpoint assays (red) provide a single snapshot of specific biochemical activities at the cost of cell viability. The LDH and MTT pathways exemplify common endpoint mechanisms.
Diagram 2: Integrated Workflow for Benchmarking. This workflow illustrates a parallel experimental design where the same cell treatment is analyzed using both kinetic profiling and endpoint assays, allowing for direct comparison and validation of results in the final integrated analysis.
Troubleshooting Guides
Low Signal Intensity in Kinetic Apoptosis Assays
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Low fluorescence or absorbance signal | Low cell seeding density [22] [63] | Perform a cell serial dilution to determine and use the optimal cell density for the assay. |
| Excessive or forceful pipetting during cell handling [22] | Handle cell suspension gently during plate setup and all assay procedures. | |
| Insufficient compound incubation time [64] | Extend the kinetic measurement period to capture the peak apoptotic response. | |
| High background signal | High concentration of serum in the culture medium [63] | Reduce the amount of serum in the media to the minimal amount required to keep cells healthy. |
| Air bubbles in assay wells [22] | Check wells for bubbles and remove them with a syringe needle before reading the plate. | |
| Lack of reagent wash steps [64] | For no-wash protocols (e.g., Incucyte), ensure integrated software is used for automatic background segmentation. |
Challenges in Translating In Vitro Kinetics to In Vivo Scheduling
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Poor correlation between in vitro apoptosis and in vivo efficacy | Use of an animal model that poorly replicates the human disease context [65] | Conduct a literature review to select a genetically precise in vivo model with a validated apoptotic response. |
| High variability in in vivo outcomes due to uncontrolled bias [65] | Implement strict randomization and blinding procedures for animal assignment and data analysis. | |
| Inability to determine optimal treatment schedule | Single endpoint measurements missing kinetic profiles [66] [64] | Use real-time, high-content imaging to establish a detailed kinetic curve of the apoptotic response in vitro. |
| Lack of multiplexed data on both apoptosis and proliferation [64] | Use multiplexed assays (e.g., Caspase-3/7 dye with nuclear label) to measure cell death and anti-proliferative effects simultaneously. |
Frequently Asked Questions (FAQs)
Q1: Why should I use kinetic apoptosis assays instead of traditional endpoint assays?
Kinetic assays provide continuous, real-time data that captures the full dynamics of the apoptotic response, rather than a single snapshot in time [64]. This allows for a more sensitive and accurate determination of when the peak apoptotic response occurs following treatment, which is critical for scheduling subsequent in vivo doses [66]. Endpoint assays can miss this optimal window.
Q2: How can I ensure my in vitro kinetic apoptosis data will reliably inform my in vivo study design?
The key is to use a highly sensitive and quantitative in vitro method. Research indicates that real-time high-content kinetic analysis with Annexin V labeling is 10-fold more sensitive than flow cytometry and outperforms viability dye methods [66]. Using this robust in vitro data, you can model the time-to-peak response, which provides a strong scientific rationale for scheduling the first few doses in your in vivo study. This should then be refined with real-time in vivo apoptosis monitoring techniques where possible [67].
Q3: My kinetic data is highly variable between experimental replicates. What steps can I take?
First, review your cell culture practices. Ensure consistent cell seeding density and gentle handling to prevent accidental cell death [22]. Second, in the context of in vivo work, apply strict experimental design principles. This includes using animals from multiple litters, including both sexes in your study cohort where scientifically justified, and proper randomization to control for biological variation [65]. Finally, when aggregating data, capture the raw data from the smallest experimental unit (e.g., per animal) to improve statistical power and reproducibility [68].
Q4: What are the advantages of a no-wash, live-cell apoptosis assay protocol?
No-wash protocols, such as those used with live-cell analysis systems, minimize the loss of dying cells that can occur during centrifugation and washing steps [66] [64]. This eliminates a key source of bias, as these dying cells are often the population of greatest interest. Furthermore, it reduces hands-on time, simplifies the workflow for higher throughput, and allows for true real-time kinetic measurement without disturbing the cells.
Experimental Protocols for Key Kinetic Apoptosis Assays
Protocol 1: Real-Time, High-Content Kinetic Apoptosis Assay using Annexin V
This protocol is adapted from a highly sensitive method for quantifying extrinsic and intrinsic inducers of apoptosis [66].
Key Materials:
- Real-time live-cell imaging system (e.g., Incucyte)
- Annexin V conjugated to a fluoroprobe (e.g., Incucyte Annexin V Dye)
- 96-well or 384-well microplate
- Appropriate cell culture medium
Procedure:
- Cell Preparation: Collect, count, and wash your cells. Prepare a cell suspension and seed it into the wells of a microplate at the optimal density. Incubate the plate until cells have properly adhered [22].
- Compound Treatment: Prepare serial dilutions of your test compound. Add the compounds to the wells, ensuring you include positive (e.g., a known apoptosis inducer like Camptothecin) and negative (vehicle) controls.
- Dye Addition and Kinetic Imaging: Add the Annexin V dye directly to the wells according to the manufacturer's instructions—no wash steps are required. Place the plate in the live-cell imager and initiate a kinetic program that acquires images (both phase-contrast and fluorescent) at regular intervals (e.g., every 2-4 hours) for the desired duration (e.g., 48-72 hours) [64].
- Data Analysis: Use integrated software to automatically quantify the fluorescent objects (apoptotic cells) in each well over time. Generate kinetic curves of apoptosis for each treatment condition.
Protocol 2: Multiplexed Kinetic Measurement of Apoptosis and Proliferation
This protocol allows for the simultaneous monitoring of cell death and anti-proliferative effects, providing a more comprehensive picture of compound activity [64].
Key Materials:
- Live-cell analysis system (e.g., Incucyte)
- Caspase-3/7 Green Dye
- Nuclight NIR Lentivirus Reagent (or similar for nuclear labeling)
- 96-well microplate
Procedure:
- Generate Stable Cell Line: Stably transduce your cells of interest with the Nuclight NIR Lentivirus to label the nuclei. This creates a constant fluorescent signal in all nuclei.
- Cell Seeding and Treatment: Seed the labeled cells into a microplate. The next day, prepare and add your test compound in a serial dilution.
- Dye Addition and Imaging: Simultaneously add the Caspase-3/7 Green Dye to the wells. Place the plate in the imager and set up a kinetic program to acquire both red (or NIR, for nuclei) and green (for apoptosis) fluorescence channels.
- Analysis: The integrated software will automatically quantify the total number of nuclei (proliferation/confluence) and the number of caspase-3/7 positive objects (apoptosis) over time. This allows you to plot kinetic curves for both parameters on the same graph.
Signaling Pathways and Experimental Workflows
Apoptosis Signaling Pathways in Cytotoxicity Screening
Workflow: Informing In Vivo Scheduling with In Vitro Kinetics
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Assay | Function in Kinetic Profiling | Key Advantage for Scheduling |
|---|---|---|
| Annexin V Conjugates (e.g., CF Dyes) [64] | Binds to phosphatidylserine (PS) exposed on the outer leaflet of the plasma membrane during early apoptosis. | Provides a sensitive, early marker of cell death. Kinetic data reveals the onset and progression of apoptosis. |
| Caspase-3/7 Substrates (DEVD-based) [64] | Non-fluorescent substrates cleaved by executioner caspases, releasing a fluorescent DNA-binding dye. | Indicates irreversible commitment to apoptosis. Multiplexing allows correlation with proliferation. |
| Nuclear Labeling Reagents (e.g., Nuclight) [64] | Labels the nucleus of living cells with a fluorescent protein (e.g., NIR). | Enables multiplexed counting of total cell number (proliferation/viability) alongside apoptosis markers. |
| Cytotoxicity Dyes (e.g., LDH Assay, membrane integrity dyes) [22] [63] | Measures loss of cell membrane integrity, a late-stage event in cell death. | Helps distinguish apoptotic from necrotic death mechanisms. Useful as a secondary readout. |
| No-Wash, Live-Cell Assay Reagents [66] [64] | Optimized reagents for real-time analysis without washing steps, minimizing disturbance to cells. | Crucial for generating high-quality, continuous kinetic data without artifact introduction. |
Correlating In Vitro Kinetic Signatures with Clinical Toxicity Outcomes
FAQs and Troubleshooting Guides
FAQ: Fundamental Concepts and Applications
Q1: What is the core value of correlating in vitro kinetic signatures with clinical outcomes? Integrating in vitro kinetic data with computational models allows for the prediction of in vivo human toxicity, bridging a critical data gap in next-generation risk assessment. This approach helps infer human health risk from chemical exposure based on human cell-based testing, addressing limitations of traditional animal studies and supporting population-stratified risk assessment [69].
Q2: What are the main technical challenges in this correlation process? Key challenges include: mimicking physiological in vivo environments in cell cultures, emulating chemical bioactivation processes (e.g., liver metabolism), defining proper in vitro points of departure (PoD), and extrapolating cellular-level dose metrics to in vivo exposure scenarios and human population variability [69].
Q3: How can in vitro to in vivo extrapolation (IVIVE) be successfully implemented? Two primary modeling approaches are required:
- Organism-level models (e.g., Adverse Outcome Pathway models) for toxic effects involving systemic regulations, such as endocrine disruption.
- Physiologically-based toxicokinetic (PBTK) modeling to extrapolate in vitro PoD dose metrics into external doses for expected human exposure scenarios [69].
Troubleshooting Guide: Experimental Pitfalls and Solutions
Q4: Our cytotoxicity assays show low absorbance values, leading to poor signal. What could be the cause? This is most frequently due to low cell density in your assay wells [22].
- Solution: Repeat the experiment to determine and use the optimal cell count for your specific cell line and assay platform [22].
Q5: We are observing high well-to-well variability in absorbance readings during cytotoxicity measurements. How can this be resolved? High variability can often be traced to the formation of air bubbles within the wells during plate setup [22].
- Solution: Visually inspect wells for bubbles after pipetting. If present, carefully break them using a syringe needle before reading the plate [22].
Q6: How can we ensure our in vitro kinetic data is suitable for extrapolation to in vivo effects? Focus on generating data that can calibrate computational models.
- Solution: Report both the degree of pathway perturbation and chemical biokinetics in the culture medium. This data is essential for calibrating toxicity pathway and virtual tissue models, which can then predict Points of Departure (PoD) based on in vivo chemical dosimetry [69].
Experimental Protocols for Kinetic Profiling
Detailed Cytotoxicity Assay Protocol
This protocol provides a foundation for generating kinetic signatures of cytotoxicity, a key phenotypic endpoint [22].
1. Cell Sample Preparation
- Collect and count your cells.
- Wash and prepare a single-cell suspension using an assay buffer.
- Dilute the cell suspension in assay medium to the appropriate concentration.
- Add a quantitative amount of the cell suspension to the wells of a 96-well plate.
- Incubate the plate for the appropriate time under standard culture conditions (e.g., 37°C, 5% CO₂) [22].
2. Compound Treatment
- Prepare your test compound(s).
- Perform serial dilutions as required for your experimental design.
- Add equal amounts of the compound to each assigned well.
- Include controls: Set up positive (e.g., a known cytotoxic agent) and negative (e.g., vehicle control) controls on the same plate.
- Incubate the plate for the desired treatment duration [22].
3. Dyeing (Endpoint Detection)
- Select an appropriate dye based on your readout. Common choices include:
- DNA dyes to stain cells with damaged membranes.
- Amine-reactive dyes to weakly stain live cells and strongly stain cells with compromised membrane integrity.
- Add equal amounts of the dye solution to each well.
- Incubate in the dark at room temperature for the recommended time.
- Wash to remove unbound staining solution, if required by the protocol [22].
4. Measurement and Data Analysis
- Measure the absorbance at the reference wavelength using a microplate reader.
- Correct for background by subtracting the control values from all sample readings.
- Calculate the percentage of cytotoxicity using the formula specified by your assay kit or standard operating procedure [22].
In Vitro Pharmacologic Profiling Protocol
This methodology is used for systemic toxicity assessment by profiling chemical activities against a panel of pharmacological targets [70].
- Panel Design: Develop a panel of target assays, which may include targets used in pharmaceutical development alongside additional targets linked to systemic toxicities. An example is the Adapted in vitro Pharmacology Profiling Panel (APPP) comprising 83 target assays [70].
- Profiling: Screen chemicals of interest (e.g., 129 cosmetic-relevant chemicals with diverse structures) against the panel.
- Data Generation: Generate both single-concentration and concentration-response data to ensure robustness and internal consistency [70].
- Data Integration: Analyze the profiling data in the context of other New Approach Methodologies (NAMs) to support risk assessments without new animal studies [70].
The tables below summarize key quantitative data for experimental planning and benchmarking.
Table 1: Troubleshooting Cytotoxicity Assay Readouts
| Symptom | Likely Cause | Recommended Solution |
|---|---|---|
| Low absorbance value | Low cell density [22] | Repeat experiment to determine optimal cell count [22]. |
| High spontaneous control absorbance | High cell density or forceful pipetting [22] | Re-optimize cell density; handle cell suspension gently during plating [22]. |
| High medium control absorbance | High concentration of interfering substances in culture medium [22] | Test medium components and reduce their concentration if possible [22]. |
| High well-to-well variability | Air bubbles in wells [22] | Break bubbles with a syringe needle before measurement [22]. |
Table 2: Key Parameters for In Vitro Pharmacology Profiling
| Parameter | Description | Example from Literature |
|---|---|---|
| Panel Size | Number of target assays in the profiling panel | 83 target assays in an APPP [70]. |
| Chemical Throughput | Number of chemicals profiled | 129 cosmetic-relevant chemicals [70]. |
| Data Robustness Check | Method to ensure internal data consistency | Reproducibility between single concentration and concentration-response data [70]. |
| External Concordance | Comparison with external datasets to validate findings | Good concordance with ToxCast and drug excipient datasets [70]. |
Research Reagent Solutions
Table 3: Essential Reagents for Cytotoxicity and Kinetic Assays
| Reagent / Solution | Function in the Experiment |
|---|---|
| Assay Buffer | Provides a physiologically compatible environment for washing and maintaining cells during the assay procedure [22]. |
| Assay Medium | The nutrient-containing solution in which cells are diluted and the assay is performed [22]. |
| Fixation Solution | Preserves cellular morphology and architecture at a specific time point by cross-linking proteins and hardening biological structures. |
| Dilution Buffer | Used to prepare accurate serial dilutions of the test compound for dose-response studies [22]. |
| Dye Solution | Contains a chromogenic or fluorogenic marker to report on cell viability or a specific cellular event, such as membrane integrity [22]. |
| Washing Buffer | Used to remove unbound dye, excess compound, or other reagents to reduce background signal [22]. |
Experimental and Data Workflow Diagrams
The Role of Kinetic Profiling in Emerging Frameworks like IATA and NAMs
Frequently Asked Questions (FAQs)
1. How is kinetic profiling integrated into a tiered IATA? Kinetic profiling is fundamental to a tiered IATA, moving from simple screening to complex, human-relevant risk assessments [71]. In early tiers, it helps set bioactivity indicators from high-throughput in vitro data (e.g., ToxCast AC50 values) [71]. In higher tiers, physiologically based kinetic (PBK) modeling is used to translate external doses and in vitro effect concentrations into predicted human internal doses at the target site. This allows for a direct comparison between bioactivity and exposure to calculate a Bioactivity Exposure Ratio (BER) or Margin of Exposure (MoE) for risk-based decision-making [71] [72].
2. What are common pitfalls when deriving kinetic parameters for NAMs, and how can they be avoided? Common pitfalls include:
- Ignoring assay interference: Test compounds can intrinsically fluoresce or adsorb assay dyes, leading to false results [19]. Always include appropriate "no-cell" blanks and use orthogonal assays to confirm key findings [19].
- Using only nominal concentrations: Relying on the nominal concentration of a test chemical in the well, rather than modeling or measuring the intracellular concentration available to interact with the molecular target, can lead to inaccurate potency estimates [71] [72]. Use PBK modeling to estimate free intracellular concentrations [71].
- Insufficient model parameterization: PBK models parameterized solely with in silico predictions can have high uncertainty [72]. Use in vitro-derived parameters (e.g., metabolic clearance from hepatocytes) where possible and employ Bayesian methods to quantify and refine this uncertainty [72].
3. Our in vitro NAM data and in vivo results are conflicting. How can kinetic modeling help resolve this? Discrepancies often arise from differences in toxicokinetics (what the body does to the chemical) rather than toxicodynamics (what the chemical does to the body) [71]. Kinetic modeling can reconcile these by:
- Refining the Point of Departure (POD): Using PBK models to estimate the internal (blood or tissue) concentration in the in vivo study at the dose level corresponding to the No-Observed-Adverse-Effect-Level (NOAEL) [71].
- Enabling in vitro-in vivo comparison: Comparing this estimated in vivo internal concentration with the active in vitro concentration from your NAMs. Coherent results between the two, based on internal dose, increase confidence in the NAM data and suggest the in vivo response may be influenced by factors like higher peak concentrations or metabolism not captured in the vitro system [71].
4. Which in vitro models are best suited for kinetic profiling in respiratory irritation assessments? For respiratory irritation, models that mimic the human airway architecture are preferred. While no single system contains all 40+ respiratory cell types, the key is to use models with cells critical to the pathogenesis [73].
- Air-Liquid Interface (ALI) cultures are particularly valuable as they allow for direct and realistic exposure of the epithelial surface to inhaled aerosols, mimicking human inhalation dosimetry more accurately than submerged cultures [73].
- These systems can be based on primary human cells or cell lines and are used to measure endpoints like epithelial barrier integrity, cytokine release (inflammation), and cytotoxicity [73].
Troubleshooting Guides
Issue 1: High Uncertainty in PBK Model Estimates
Problem: Your physiologically based kinetic (PBK) model predictions have wide confidence intervals, making it difficult to draw definitive conclusions for risk assessment.
| Solution Step | Action | Rationale & Reference |
|---|---|---|
| 1. Identify Key Parameters | Perform a sensitivity analysis to determine which input parameters (e.g., metabolic clearance, tissue partitioning) have the largest impact on the model output (e.g., Cmax). | Focuses refinement efforts on the most influential parameters, increasing model efficiency [72]. |
| 2. Incorporate In Vitro Data | Replace in silico predictions for critical parameters with experimental data. For metabolism, use clearance data from human hepatocytes or microsomes. | Using experimentally derived parameters significantly reduces uncertainty compared to models parameterized solely with in silico predictions [72]. |
| 3. Apply Bayesian Analysis | Use Bayesian methods to quantify the uncertainty in the PBK model predictions based on the quality and source of the input parameters. | Provides a probabilistic distribution of the internal exposure estimate (e.g., Cmax), allowing for a more robust and transparent accounting of uncertainty in the final risk assessment [72]. |
Issue 2: Integrating Disparate Data Streams in an IATA
Problem: You have data from multiple NAMs (in silico, in chemico, in vitro) but are unsure how to weight and integrate them into a single assessment.
Solution: Employ a structured framework like the Adverse Outcome Pathway (AOP) to organize and interpret your data [74] [75].
- Map Data to Key Events: Align each data stream to a specific Molecular Initiating Event (MIE) or Key Event (KE) within a relevant AOP. For example, map in vitro receptor activation data to an MIE, and transcriptomic changes to a subsequent KE [75] [76].
- Establish a Data Hierarchy: Adopt a confidence-based hierarchy for your data. A common approach is to prioritize data in this order: in vivo > in vitro > in silico. Within NAMs, you can assign higher confidence to assays that are thoroughly characterized and standardized [76].
- Use Defined Approaches (DAs): For specific endpoints, use pre-validated DAs, which are fixed data interpretation procedures that combine results from multiple information sources. The OECD provides reporting templates for DAs to ensure consistency [74].
Issue 3: Translating In Vitro Bioactivity to a Protective Point of Departure (POD)
Problem: Determining a protective POD from in vitro bioactivity data that is relevant for human safety decisions.
Solution: A multi-platform approach is recommended to ensure broad biological coverage [72].
- Generate Platform-Specific PODs: Test your chemical across multiple bioactivity platforms, such as:
- High-Throughput Transcriptomics: To identify the lowest concentration causing genome-wide changes (transcriptomic POD or tPOD) [76] [72].
- Cell Stress Panel: To measure general cytotoxicity and cellular stress responses [72].
- In Vitro Pharmacological Profiling: To screen for activity against a wide range of receptors, enzymes, and ion channels [72].
- Select the Most Sensitive POD: The final POD for risk assessment is the lowest relevant bioactivity concentration obtained from any of the platforms. This ensures the assessment is protective of any potential bioactivity [72].
- Extrapolate to Human Dose: Use a PBK model to convert this most sensitive in vitro POD into an equivalent human external dose, which can then be compared to exposure estimates [72].
The Scientist's Toolkit: Essential Reagents & Materials
The following table details key materials used in kinetic profiling within NAM-based frameworks.
| Item | Function / Application in Kinetic Profiling |
|---|---|
| Physiologically Based Kinetic (PBK) Modeling Software (e.g., PKSim) | Software platform used to simulate and model the absorption, distribution, metabolism, and excretion (ADME) of chemicals in a virtual human body. It estimates internal target-site concentrations from external doses [71]. |
| High-Throughput Transcriptomics Platforms | Used to generate transcriptomic Points of Departure (tPODs) by measuring genome-wide gene expression changes in response to chemical exposure in human cell lines (e.g., HepG2, HepaRG) [76] [72]. |
| Air-Liquid Interface (ALI) Culture Systems | In vitro models where respiratory cells are grown at the interface of air and culture medium. These are essential for realistic kinetic profiling of inhaled chemicals, allowing for direct exposure and measurement of endpoints like epithelial barrier integrity and cytokine release [73]. |
| Cell Stress & Viability Assay Kits (e.g., MTT, LDH, NRU) | Classical and standardized assay kits used to measure cytotoxicity and cellular stress. They provide critical data for setting bioactivity thresholds and checking for assay interference [19]. |
| ToxCast/Tox21 Bioactivity Database | A large publicly available database containing bioactivity profiles for thousands of chemicals across hundreds of assay endpoints. Used for initial hazard identification and hypothesis generation in tiered assessments [71]. |
Experimental Workflow & Data Integration
The following diagram illustrates the iterative, tiered workflow for integrating kinetic profiling into an IATA.
Kinetic Data in Risk Assessment
The table below summarizes the types of quantitative data used in kinetic-informed safety assessments and how they are applied.
| Data Type | Source | Application in Risk Assessment |
|---|---|---|
| AC50 | High-throughput in vitro assays (e.g., ToxCast) [71]. | The concentration of a substance that causes 50% of its maximal activity in a given assay; used for initial bioactivity screening and potency ranking. |
| Point of Departure (POD) | In vitro assays (transcriptomics, cell stress), in vivo studies [76] [72]. | The lowest dose or concentration at which a measurable adverse or bioactive effect is observed. Used as the basis for deriving safe exposure levels. |
| Transcriptomic POD (tPOD) | High-throughput transcriptomics data from human cell models [76]. | A specific POD based on the lowest dose causing a significant gene expression change. Used to derive a protective reference dose (RfD) when in vivo data is lacking [76]. |
| Bioactivity Exposure Ratio (BER) | Calculated from PBK model and in vitro POD [72]. | The ratio between the in vitro bioactivity concentration (POD) and the predicted human internal exposure. A high BER indicates a low risk. |
| Margin of Exposure (MoE) | Calculated from in vivo NOAEL or in vitro POD and human exposure [71]. | The ratio between a toxicological benchmark (e.g., NOAEL from animal study) and the estimated human exposure level. Used for priority setting and risk characterization. |
Conclusion
Kinetic profiling represents a paradigm shift in cytotoxicity phenotypic screening, moving the field from static snapshots to a dynamic, mechanism-rich understanding of compound effects. This synthesis of foundational concepts, advanced methodologies, robust troubleshooting, and rigorous validation underscores that time-resolved data is no longer a luxury but a necessity for de-risking drug discovery. It enables the critical distinction between transient and irreversible cellular damage, reveals complex mechanisms of action, and provides superior predictive power for in vivo outcomes. Future directions will be shaped by deeper integration with artificial intelligence for predictive modeling, the widespread adoption of human-centric models like organoids and organs-on-chips, and the formal inclusion of kinetic parameters into regulatory decision-making frameworks. By embracing these advanced kinetic approaches, researchers can systematically prioritize safer and more effective therapeutic candidates, ultimately accelerating the development of novel medicines for complex diseases.
References
- 1. Phenotypic Screening: A Powerful Tool for Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/phenotypic-screening-a-powerful-tool-for-drug-discovery-398572]
- 2. Phenotypic Drug Discovery: Recent successes, lessons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9708951/]
- 3. Phenotypic Drug Discovery Modern Successes [https://www.pfizer.com/news/articles/that_which_is_old_is_new_again_phenotypic_drug_discovery_makes_a_comeback]
- 4. Cytotoxic Profiling of Annotated and Diverse Chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10791069/]
- 5. Quantitative phenotypic and pathway profiling guides ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2014.00118/full]
- 6. Kinetic Cell-Based Morphological Screening: Prediction of ... [https://www.sciencedirect.com/science/article/pii/S1074552109001811]
- 7. Genome-wide phenotypic screening using CRISPR/Cas9 [https://www.takarabio.com/learning-centers/gene-function/gene-editing/genome-wide-screening?srsltid=AfmBOoqic39OsTSWMCNtckXc2vGtJytbrrIQG_tUxDodXxgVIMkSnAce]
- 8. Improving phenotypic screening | Nature Chemical Biology [https://www.nature.com/articles/s41589-025-02093-x]
- 9. Phenotypic and targeted drug discovery in immune therapeutics [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03914b]
- 10. Innovating cancer drug discovery with refined phenotypic ... [https://www.sciencedirect.com/science/article/pii/S0165614724001202]
- 11. Quantitative understanding of cell signaling: The importance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2967365/]
- 12. Engineering of a chromogenic enzyme screening system ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6692525/]
- 13. Parameter estimation of kinetic models from metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6281308/]
- 14. Kinetic Parameter - an overview [https://www.sciencedirect.com/topics/engineering/kinetic-parameter]
- 15. quantifying signal transduction pathway activity across cell ... [https://www.nature.com/articles/s41598-018-38179-x]
- 16. Hit Identification in Drug Discovery [https://www.vipergen.com/hit-identification-in-drug-discovery/]
- 17. Navigating Cytotoxicity Failures in Medical Devices [https://namsa.com/resources/blog/navigating-cytotoxicity-failures-in-medical-devices-comprehensive-risk-management-strategies/]
- 18. Cytotoxicity Testing for Medical Devices: A Guide to ... [https://www.mddionline.com/testing/cytotoxicity-testing-for-medical-devices-a-guide-to-compliance-best-practices]
- 19. Advances in Cytotoxicity Testing: From In Vitro Assays to In ... [https://www.mdpi.com/1422-0067/26/22/11202]
- 20. Problems and challenges in the development and validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3045340/]
- 21. A review of cytotoxicity testing methods and in vitro study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534221/]
- 22. Cytotoxicity Assay Protocol & Troubleshooting - Creative Biolabs [https://www.creativebiolabs.net/cytotoxicity-assay.htm]
- 23. Cytotoxicity Assays: In Vitro Methods to Measure Dead Cells [https://www.ncbi.nlm.nih.gov/books/NBK540958/]
- 24. Mitochondrial dynamics in adaptive and... | Nature Cell Biology [https://www.nature.com/articles/s41556-018-0133-0?error=cookies_not_supported&code=fa7411a0-0bb2-4194-a431-7162eb2142f6]
- 25. A short review on cell-based biosensing: challenges and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8383170/]
- 26. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 27. Improving accuracy and reliability of an electrochemical ... [https://www.sciencedirect.com/science/article/pii/S221171562400184X]
- 28. A Closer Look at Biosensors: A Practical Tutorial for ... [https://www.spectroscopyonline.com/view/a-closer-look-at-biosensors-a-practical-tutorial-for-spectroscopists]
- 29. Kinetic profiling of metabolic specialists demonstrates stability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7502767/]
- 30. Impedance biosensor for real-time monitoring and prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5602635/]
- 31. A Practical Guide to Developing and Troubleshooting Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566426/]
- 32. Strategies to overcome the limitations of current organoid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12033597/]
- 33. Organoids-on-a-chip: microfluidic technology enables culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11933005/]
- 34. 3D organ-on-a-chip: The convergence of ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.1043117/full]
- 35. A guide to the organ-on-a-chip [https://www.nature.com/articles/s43586-022-00118-6]
- 36. Opportunities and challenges in phenotypic drug discovery [https://www.nature.com/articles/nrd.2017.111]
- 37. Discovery of novel anti-fibrotics through phenotypic ... [https://www.sciencedirect.com/science/article/pii/S1359644625001631]
- 38. Phenotypic Screening of Chemical Libraries Enriched by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7919753/]
- 39. - High of Natural Product and Synthetic... Throughput Screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC10220967/]
- 40. An Overview of High | The Scientist Throughput Screening [https://www.the-scientist.com/an-overview-of-high-throughput-screening-71561]
- 41. Kinetic Cell-based Morphological Screening: Prediction of Mechanism of Compound Action and Off-Target Effects - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2836189/]
- 42. How to survive a phenotypic antiviral screening [https://virologyresearchservices.com/2017/06/18/screening/]
- 43. Interference and Artifacts in High-content Screening - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK615088/]
- 44. Navigating the Bottlenecks in Pre-Clinical Drug Discovery [https://absbio.com/abs-blog/navigating-the-bottlenecks-in-pre-clinical-drug-discovery/]
- 45. Phenotypic Screening of Prospective Analgesics Among FDA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10953557/]
- 46. Reference compounds for characterizing cellular injury in ... [https://www.nature.com/articles/s41467-023-36829-x]
- 47. Tools and Protocols for High-Content Imaging and Analysis [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-77/high-content-imaging-analysis-hardware-software-fluorescent-labels.html]
- 48. Multiparametric quantitative phase imaging for real-time, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9360018/]
- 49. Real-time cell toxicity profiling of Tox21 10K compounds ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0177902]
- 50. Measuring Cancer Drug Sensitivity and Resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5538315/]
- 51. Analysis and modeling of cancer drug responses using cell ... [https://www.nature.com/articles/s41467-023-39122-z]
- 52. replicating high-throughput phenotypic profiling in a ... [https://link.springer.com/article/10.1007/s00204-025-04165-2]
- 53. How to do Real-time Data Processing for modern analytics ... [https://www.tinybird.co/blog/real-time-data-processing]
- 54. Essential Data Integrity Best Practices for 2025 [https://atlan.com/data-integrity-best-practices/]
- 55. Data Analytics Pipeline 2025: Tools, Techniques & Strategies [https://kanerika.com/blogs/data-analytics-pipeline/]
- 56. From Data Chaos to Clarity: Best Practices for Managing ... [https://www.kitware.com/from-data-chaos-to-clarity-best-practices-for-managing-complex-datasets/]
- 57. nELISA: a high-throughput, high-plex platform enables ... [https://www.nature.com/articles/s41592-025-02861-6]
- 58. Unlocking the Power of Live-Cell Kinetics in Degrader ... [https://www.promegaconnections.com/unlocking-the-power-of-live-cell-kinetics-in-degrader-development/]
- 59. Live-Cell Kinetic Assays for Time Course Analysis [https://www.promega.com/resources/guides/cell-biology/time-course-analysis/]
- 60. Comparison of four different colorimetric and fluorometric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2438350/]
- 61. LDH assay kit guide: Principles and applications [https://www.abcam.com/en-us/knowledge-center/cell-biology/ldh-assay-kit-guide-principles-and-application]
- 62. Quantification of lactate dehydrogenase for cell viability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5501254/]
- 63. Pierce™ LDH Cytotoxicity Assay Kit - FAQs [https://www.thermofisher.com/order/catalog/product/88954/faqs]
- 64. Kinetic quantification of apoptosis using Incucyte® live-cell ... [https://www.news-medical.net/whitepaper/20251027/Kinetic-quantification-of-apoptosis-using-Incucytec2ae-live-cell-imaging-assays.aspx]
- 65. Tackling In Vivo Experimental Design [https://www.modernvivo.com/post/5-effective-strategies-to-tackle-in-vivo-experimental-design-challenges]
- 66. Robust high-throughput kinetic analysis of apoptosis with real ... [https://pubmed.ncbi.nlm.nih.gov/27906190/]
- 67. In vivo magnetic resonance imaging of treatment-induced ... [https://www.nature.com/articles/s41598-019-45864-y]
- 68. Eleven quick tips to unlock the power of in vivo data science [https://pmc.ncbi.nlm.nih.gov/articles/PMC12005514/]
- 69. Bridging the Data Gap From in vitro Toxicity Testing to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6141783/]
- 70. In vitro pharmacologic profiling aids systemic toxicity ... [https://www.sciencedirect.com/science/article/pii/S0041008X24003302]
- 71. A tiered next-generation risk assessment framework ... [https://link.springer.com/article/10.1007/s00204-025-04045-9]
- 72. Are Non-animal Systemic Safety Assessments Protective? ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9412174/]
- 73. New approach methodologies (NAMs) for the in vitro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11493779/]
- 74. Integrated Approaches to Testing and Assessment (IATA) [https://www.oecd.org/en/topics/sub-issues/assessment-of-chemicals/integrated-approaches-to-testing-and-assessment.html]
- 75. New Approach Methodologies (NAMs) for Neurotoxicity ... [https://pubmed.ncbi.nlm.nih.gov/40370040/]
- 76. Advancing NAMs for Risk Assessment: Perspectives from SOT ... [https://www.jhutoxicologypolicyresearch.org/tox-blog/blog43]