Intrinsic Resistance Unplugged: The Definitive Guide to Bacterial Efflux Pumps in Antimicrobial Defense
This article provides a comprehensive analysis of the critical role efflux pumps play as a primary mechanism of intrinsic antimicrobial resistance in bacteria.
Intrinsic Resistance Unplugged: The Definitive Guide to Bacterial Efflux Pumps in Antimicrobial Defense
Abstract
This article provides a comprehensive analysis of the critical role efflux pumps play as a primary mechanism of intrinsic antimicrobial resistance in bacteria. Aimed at researchers and drug development professionals, it synthesizes foundational knowledge on pump structure, classification, and physiological functions with advanced methodological approaches for their study. The content further explores the challenges efflux poses in clinical settings and drug development, detailing current strategies to circumvent this resistance, including the development of efflux pump inhibitors and the design of evader compounds. By integrating validation frameworks and comparative analyses of key pathogen-specific pumps, this resource offers a roadmap for overcoming one of the most significant barriers in modern antimicrobial therapy.
The Essential Gatekeepers: Deconstructing Efflux Pump Biology and Intrinsic Resistance Mechanisms
Bacterial resistance to antimicrobial agents represents a critical challenge to global public health, undermining the efficacy of conventional treatments and complicating therapeutic interventions. This resistance manifests through two primary pathways: intrinsic resistance, an innate, inherited characteristic of a bacterial species, and acquired resistance, which occurs through genetic mutations or horizontal gene transfer from other organisms [1] [2]. Within the framework of bacterial defense strategies, intrinsic resistance mechanisms constitute the "first line of defense," providing immediate protection against antimicrobial agents without prior exposure [3]. Among these mechanisms, efflux pumps stand as fundamental components of intrinsic resistance, actively extruding toxic compounds from bacterial cells and substantially reducing intracellular antibiotic concentrations [4] [5]. This whitepaper delineates the distinctions between intrinsic and acquired resistance, with particular emphasis on the structural and functional roles of efflux pumps as primary defensive apparatuses, while providing technical methodologies for investigating these systems in research settings.
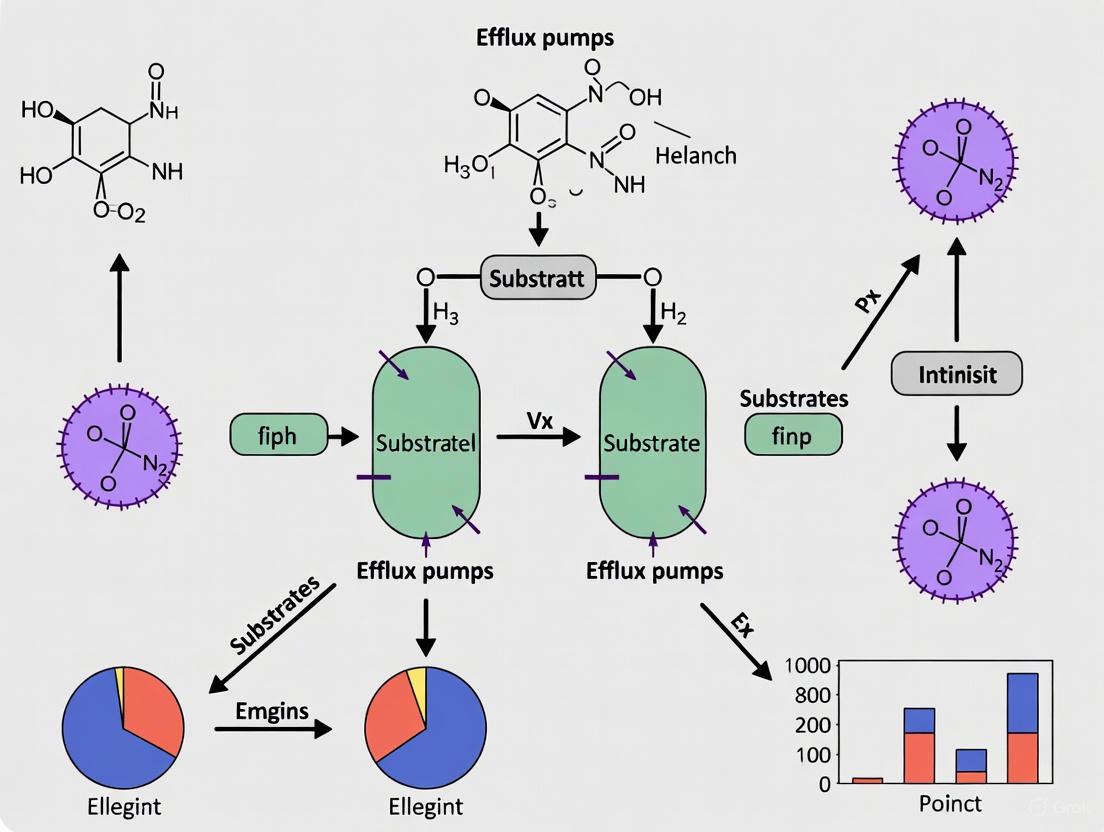
The following conceptual framework illustrates the sequential nature of bacterial defense lines, positioning intrinsic efflux systems as the foundational protective barrier:
Fundamental Concepts: Intrinsic Versus Acquired Resistance
Definitional Distinctions and Key Characteristics
Bacterial resistance mechanisms demonstrate remarkable diversity in origin and function, with intrinsic and acquired resistance representing fundamentally distinct evolutionary adaptations:
Intrinsic Resistance refers to the innate, chromosomally encoded capacity of a bacterial species to withstand antimicrobial agents without prior exposure [1] [2]. This form of resistance is a universal trait within a species, independent of horizontal gene transfer, and results from the inherent structural or functional characteristics of the microorganism [1]. For instance, Gram-negative bacteria exhibit intrinsic resistance to vancomycin due to their outer membrane impermeability to large glycopeptide molecules, while anaerobic bacteria display natural resistance to aminoglycosides because they lack the oxygen-dependent transport system required for drug uptake [1] [2].
Acquired Resistance emerges in previously susceptible bacterial populations through genetic alterations that may occur via mutation in existing genes or acquisition of new genetic material through horizontal gene transfer mechanisms (conjugation, transduction, or transformation) [1] [2]. This form of resistance is strain-specific rather than species-wide and develops in response to selective pressure from antimicrobial exposure. Notable examples include the acquisition of the mecA gene in methicillin-resistant Staphylococcus aureus (MRSA), which confers resistance to β-lactam antibiotics, and the plasmid-mediated acquisition of extended-spectrum β-lactamase (ESBL) genes in Enterobacteriaceae [6] [2].
Table 1: Comparative Analysis of Intrinsic Versus Acquired Resistance
| Characteristic | Intrinsic Resistance | Acquired Resistance |
|---|---|---|
| Genetic Basis | Chromosomal genes present in all members of a species | Mutations or acquired genetic elements (plasmids, transposons) |
| Scope | Species-wide | Strain-specific |
| Dependence on Prior Antibiotic Exposure | Independent | Dependent |
| Transferability | Vertical inheritance only | Horizontal gene transfer possible |
| Examples | Vancomycin resistance in Gram-negative bacteria; β-lactam resistance in Klebsiella spp. | MRSA (mecA gene); ESBL-producing Enterobacteriaceae |
| Overcoming Strategies | Drug design bypassing inherent barriers | Combination therapy; antimicrobial stewardship |
The Resistance Continuum: From Intrinsic to Multidrug Resistance
Bacterial resistance exists along a spectrum, with intrinsic resistance representing the foundational layer upon which additional resistance mechanisms can accumulate. When bacteria acquire multiple resistance determinants, they may progress to become multidrug-resistant (MDR), defined as resistance to three or more antimicrobial categories [2]. Further accumulation of resistance mechanisms can lead to extensively drug-resistant (XDR) and pan-drug-resistant (PDR) phenotypes, creating significant therapeutic challenges [2]. Efflux pumps play a particularly insidious role in this progression, as their broad substrate specificity can confer resistance to multiple antibiotic classes simultaneously, thereby facilitating the selection of additional, more specific resistance mechanisms [5] [7].
Efflux Pumps: Architects of Intrinsic Resistance
Structural Classification and Functional Mechanisms
Efflux pumps are active transporter proteins embedded in bacterial membranes that extrude toxic substances, including antibiotics, from the cellular interior. These systems are phylogenetically categorized into six major superfamilies based on their structure and energy coupling mechanisms [5] [8] [9]:
Table 2: Major Efflux Pump Superfamilies in Bacteria
| Superfamily | Energy Source | Primary Organisms | Representative Pumps | Key Substrates |
|---|---|---|---|---|
| RND (Resistance-Nodulation-Division) | Proton motive force | Gram-negative | AcrAB-TolC (E. coli), AdeABC (A. baumannii) | Broad spectrum: β-lactams, fluoroquinolones, aminoglycosides, tetracyclines |
| MFS (Major Facilitator Superfamily) | Proton motive force | Gram-positive and Gram-negative | EmrB (E. coli), NorA (S. aureus) | Fluoroquinolones, tetracyclines, chloramphenicol |
| ABC (ATP-Binding Cassette) | ATP hydrolysis | Both Gram-positive and Gram-negative | MacAB-TolC (E. coli) | Macrolides, polypeptides |
| SMR (Small Multidrug Resistance) | Proton motive force | Both Gram-positive and Gram-negative | EmrE (E. coli) | Disinfectants, dyes, some antibiotics |
| MATE (Multidrug and Toxic Compound Extrusion) | Sodium or proton gradient | Both Gram-positive and Gram-negative | NorM (V. cholerae) | Fluoroquinolones, aminoglycosides |
| PACE (Proteobacterial Antimicrobial Compound Efflux) | Proton motive force | Gram-negative | AceI (A. baumannii) | Chlorhexidine, other biocides |
The tripartite architecture of Gram-negative efflux systems, particularly well-characterized in RND family pumps, exemplifies the structural sophistication of these intrinsic resistance mechanisms. Systems such as AcrAB-TolC (E. coli) and AdeABC (A. baumannii) span both the inner and outer membranes, comprising three essential components: an inner membrane transporter (e.g., AcrB) that recognizes substrates and couples extrusion to proton influx; a periplasmic adapter protein (e.g., AcrA) that bridges the inner and outer membrane components; and an outer membrane channel (e.g., TolC) that forms an exit conduit for extruded compounds [5] [8]. This tripartite organization enables direct extrusion of substrates from the cytosol or periplasm to the extracellular environment, bypassing both membrane barriers efficiently.
Molecular Mechanisms of Substrate Extrusion
RND efflux pumps operate through a sophisticated rotational mechanism in which each proton that enters the cell drives the conformational changes necessary to export one substrate molecule [5]. The AcrB trimer, the prototypical RND transporter, exhibits functional asymmetry with its three protomers cycling consecutively through loose (L), tight (T), and open (O) conformations [8]. This cyclic conformational change creates a peristaltic motion that propels substrates from the binding pockets through the channel to the extracellular space. Substrate recognition involves multiple substrate-binding pockets with broad specificity, recognizing compounds based on physicochemical properties like hydrophobicity and aromaticity rather than specific molecular structures [7] [9].
The following diagram illustrates the operational mechanism of the tripartite AcrAB-TolC efflux system:
Methodological Approaches for Investigating Efflux-Mediated Resistance
Quantitative Assessment of Antibiotic Accumulation
Determining intracellular antibiotic concentrations provides direct evidence of efflux pump activity. Liquid chromatography-mass spectrometry (LC-MS) offers a highly sensitive approach for quantifying antibiotic accumulation in bacterial cells [4].
Protocol: LC-MS-Based Antibiotic Accumulation Assay
Bacterial Culture and Preparation: Grow the bacterial strain of interest (e.g., Mycobacterium abscessus ATCC19977) to mid-logarithmic phase in appropriate medium. Harvest cells by centrifugation (3,500 × g, 10 minutes) and wash twice with phosphate-buffered saline (PBS) or assay buffer.
Antibiotic Exposure: Resuspend bacterial pellets to a standardized optical density (OD₆₀₀ ≈ 0.5) in pre-warmed medium containing the target antibiotic at clinically relevant concentrations (typically 1-10× MIC). Include control samples without antibiotics for background subtraction.
Incubation and Sampling: Incimate the bacterial suspension with shaking at optimal growth temperature. Remove aliquots at predetermined time points (e.g., 0, 30, 60, 120, 240 minutes) and immediately separate cells from medium by rapid filtration (0.45 μm pore size filters) or silicone oil centrifugation.
Sample Processing: Lyse cell pellets using a combination of mechanical disruption (bead beating) and chemical lysis in acetonitrile:water (70:30) containing internal standards. Remove cellular debris by centrifugation (15,000 × g, 15 minutes, 4°C).
LC-MS Analysis:
- Chromatography: Separate analytes using reverse-phase C18 columns with gradient elution (mobile phase A: 0.1% formic acid in water; B: 0.1% formic acid in acetonitrile).
- Mass Spectrometry: Operate mass spectrometer in multiple reaction monitoring (MRM) mode with electrospray ionization. Use antibiotic-specific transitions for quantification.
Data Analysis: Calculate intracellular antibiotic concentrations using standard curves of pure antibiotics normalized to protein content or cell count. Express accumulation as the ratio of intracellular to extracellular drug concentration over time [4].
Genetic Screening for Efflux Components
Transposon mutagenesis coupled with next-generation sequencing (Tn-Seq) enables genome-wide identification of genetic determinants contributing to efflux-mediated resistance.
Protocol: Transposon Mutagenesis Screening for Efflux Determinants
Transposon Library Construction: Generate a comprehensive transposon mutant library using a mariner-based transposon system (e.g., Himar1) delivered via phage or conjugation. Achieve coverage of >100,000 independent insertion mutants to ensure comprehensive genome coverage.
Selection Pressure: Divide the mutant library and expose to sub-inhibitory and inhibitory concentrations of target antibiotics (e.g., linezolid for M. abscessus [4]). Include an untreated control pool cultured in parallel.
Library Harvest and DNA Preparation: After 24-48 hours of antibiotic exposure, harvest bacterial cells from both treated and control conditions. Extract genomic DNA using a method that preserves short fragments (e.g., phenol-chloroform extraction).
Library Preparation and Sequencing:
- Fragment genomic DNA by sonication or enzymatic digestion.
- Add sequencing adapters using ligation or transposase-based methods.
- Amplify transposon-chromosome junctions using primers specific to the transposon ends.
- Sequence amplified libraries using Illumina platforms to obtain >10 million reads per condition.
Bioinformatic Analysis:
- Map sequencing reads to the reference genome to identify transposon insertion sites.
- Compare insertion abundance between antibiotic-treated and control conditions using specialized software (e.g., TRANSIT, ESSENTIALS).
- Identify genes with significantly depleted insertions under antibiotic selection, indicating essentiality for survival under antibiotic pressure.
Validation: Confirm hits by constructing defined deletion mutants and complementation strains, then reassessing antibiotic susceptibility profiles [4].
Research Reagent Solutions for Efflux Pump Studies
Table 3: Essential Research Reagents for Efflux Pump Investigation
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Model Organisms | Escherichia coli K-12; Acinetobacter baumannii ATCC 19606; Mycobacterium abscessus ATCC 19977 | Comparative studies of efflux pump conservation and function | Select strains with well-annotated genomes and genetic tractability |
| Efflux Pump Inhibitors | Phe-Arg-β-naphthylamide (PAβN); Carbonyl Cyanide m-Chlorophenylhydrazone (CCCP); Verapamil | Functional assessment of efflux activity through potentiation assays | Use appropriate solvent controls; CCCP depletes proton motive force non-specifically |
| Fluorescent Substrates | Ethidium bromide; Hoechst 33342; Rhodamine 6G | Real-time monitoring of efflux activity via fluorometry | Optimize loading concentrations; confirm specificity with inhibitor controls |
| Genetic Tools | Himar1 transposon system; CRISPRI knockdown; Plasmid-based overexpression vectors | Genetic dissection of efflux pump components and regulators | Include appropriate antibiotic resistance markers for selection |
| Antibiotic Panels | Fluoroquinolones, β-lactams, aminoglycosides, tetracyclines, macrolides | Substrate specificity profiling | Use clinical isolates with defined resistance profiles for comparison |
| Analytical Standards | Isotope-labeled antibiotic internal standards (e.g., ¹³C-levofloxacin) | LC-MS quantification of intracellular drug accumulation | Ensure chromatographic separation of analogs and metabolites |
Efflux pumps represent a fundamental component of the bacterial intrinsic resistance arsenal, serving as an essential first line of defense against antimicrobial agents. Their structural complexity, broad substrate specificity, and genetic conservation across bacterial species make them formidable barriers to antibiotic therapy. The distinction between intrinsic and acquired resistance mechanisms is crucial for developing effective strategies to combat antimicrobial resistance, as each demands different therapeutic approaches. For intrinsic resistance mediated by efflux, potential solutions include the development of efflux pump inhibitors (EPIs) to be used as antibiotic adjuvants, design of novel antibiotics that bypass efflux systems, or manipulation of efflux pump expression. The methodological frameworks presented herein provide robust approaches for investigating these resistance mechanisms, enabling researchers to quantify antibiotic accumulation, identify genetic determinants of efflux, and screen for potential inhibitors. As the antimicrobial resistance crisis intensifies, understanding and targeting the first line of bacterial defense—intrinsic resistance mechanisms like efflux pumps—will be paramount in developing the next generation of effective antibacterial therapies.
Resistance-Nodulation-Division (RND) efflux pumps represent sophisticated tripartite molecular assemblies that traverse the entire cell envelope of Gram-negative bacteria, constituting a primary mechanism of intrinsic multidrug resistance. These protein complexes function as specialized architectural constructs with precisely engineered components spanning from the inner to the outer membrane. This technical review delineates the structural blueprint and functional dynamics of RND efflux pumps, with particular emphasis on the paradigm systems MexAB-OprM of Pseudomonas aeruginosa and AcrAB-TolC of Escherichia coli. We provide detailed experimental methodologies for studying these complexes, alongside quantitative analyses of their components and functions. Understanding these intricate membrane-spanning structures provides critical insights for developing novel therapeutic strategies to counteract multidrug resistance in pathogenic bacteria.
Structural Architecture of RND Efflux Pumps
RND efflux pumps exemplify remarkable structural engineering, forming continuous conduits that export antimicrobial compounds directly from the bacterial cell. These tripartite complexes comprise three essential components that collaboratively span the entire Gram-negative cell envelope [10].
Table 1: Core Components of RND Efflux Pumps
| Component | Location | Structural Features | Primary Function |
|---|---|---|---|
| Inner Membrane Transporter (e.g., AcrB, MexB) | Inner membrane | Homo-trimer with 12 transmembrane α-helices per monomer; large periplasmic domain (~7 nm) | Substrate recognition and proton antiport; primary engine of the efflux system |
| Periplasmic Adaptor Protein (e.g., AcrA, MexA) | Periplasmic space, anchored to inner membrane | Tetratricopeptide repeat domains; α-helical hairpin; lipoyl domain | Structural and functional coupling between inner and outer membrane components |
| Outer Membrane Channel (e.g., TolC, OprM) | Outer membrane | Homo-trimeric β-barrel transmembrane domain; periplasmic α-helical tunnel (~10 nm) | Final efflux duct for substrate extrusion into extracellular space |
The inner membrane transporter (IMP) component serves as the engine of the efflux system. MexB and AcrB form trimers where each protomer contains a transmembrane domain of 12 α-helices that facilitates proton translocation, and a large periplasmic portion comprising porter and funnel domains that extend approximately 7 nm into the periplasm [11]. This periplasmic domain is responsible for substrate recognition and initial capture.
The outer membrane factor (OMF) component, exemplified by OprM and TolC, exhibits a distinctive trimeric organization featuring a 4-nm-long transmembrane domain forming a β-barrel structure, complemented by a 10-nm-long periplasmic domain consisting of 12 α-helices and a mixed α/β equatorial domain [11]. This architecture creates a sealed conduit spanning the outer membrane and periplasmic space.
Linking these membrane-embedded components, the periplasmic adaptor protein (PAP) or membrane fusion protein forms critical connections between the IMP and OMF. MexA/AcrA proteins are arranged in four consecutive domains: membrane proximal, β-barrel, lipoyl, and α-helical hairpin domains, with anchoring to the inner membrane via palmitoylation of an N-terminal cysteinyl residue [11]. Recent evidence suggests these adaptor proteins may form hexameric assemblies when binding to their respective outer membrane channels, creating an extended funnel structure [12].
Assembly and Functional Dynamics
Tripartite Complex Assembly
The assembly of RND efflux pumps represents a sophisticated process wherein individually stable components form a functional complex without direct physical interaction between the inner and outer membrane components [11]. The periplasmic adaptor protein serves as the crucial architectural element bridging this intermembrane space.
Single-particle electron microscopy studies of reconstituted native P. aeruginosa MexAB-OprM and E. coli AcrAB-TolC complexes reveal elongated structures measuring approximately 33 nm along their main axis, with the inner and outer membrane protein components linked exclusively via the periplasmic adaptor protein [11]. This structural arrangement emphasizes the role of the adaptor protein as an integral part of the exit duct, with no physical contact occurring directly between the inner and outer membrane components.
Notably, these complexes demonstrate an intrinsic ability to self-assemble, evidenced by the formation of stable interspecies AcrA–MexB–TolC complexes, suggesting a conserved mechanism of tripartite assembly across bacterial species [11]. This evolutionary conservation underscores the fundamental importance of this architectural design in bacterial physiology and resistance mechanisms.
Functional Transport Mechanism
RND efflux pumps operate through a sophisticated peristaltic mechanism driven by proton motive force. The inner membrane transporter undergoes a functional rotation cycle through three distinct conformational states in each protomer:
- Loose (L) or Access state: Facilitates substrate entry from the periplasm or outer leaflet of the inner membrane
- Tight (T) or Binding state: Encloses the substrate within binding pockets
- Open (O) or Extrusion state: Directs the substrate toward the adaptor protein and outer membrane channel [12] [10]
This asymmetric conformational cycling creates a directional peristaltic motion that propels substrates through the complex. The proton motive force drives this process through protonation and deprotonation of key residues in the transmembrane domain of the IMP, with energy transduction achieved via allosteric coupling between the transmembrane and periplasmic domains [10].
Multiple substrate entry pathways have been identified, including:
- CH1 and CH4: Transmembrane grooves (between TM1/TM2 and TM7/TM8) for substrates from the membrane bilayer
- CH2: A periplasmic cleft formed by PC1/PC2 subdomains
- CH3: An interfacial channel between protomers that bypasses the access pocket [10]
These multiple entry pathways contribute to the remarkable polyspecificity of RND transporters, enabling recognition of structurally diverse compounds.
Diagram: Functional rotation mechanism of RND efflux pumps
Experimental Methodologies for Structural Analysis
Nanodisc Reconstitution Protocol
The reconstitution of native tripartite efflux complexes using lipid nanodisc technology represents a significant advancement for structural studies [11]. This methodology enables the visualization of membrane protein complexes in a near-native lipid environment.
Experimental Workflow:
Separate Membrane Protein Insertion into Nanodiscs
- Utilize two different membrane scaffold proteins (MSPs) to control complex assembly:
- MSP1D1: For outer membrane proteins (OprM/TolC) with smaller transmembrane domains (~40-55 Å diameter)
- MSP1E3D1: For inner membrane transporters (MexB/AcrB) with larger transmembrane domains (~80 Å diameter)
- Employ 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine (POPC) lipids
- Optimize molar ratios for single molecule insertion per nanodisc:
- For OprM–ND: MSP:lipid:OprM molar ratio of 1:36:0.4
- For MexB–ND: MSP:lipid:MexB molar ratio of 1:27:1
- Utilize two different membrane scaffold proteins (MSPs) to control complex assembly:
Tripartite Complex Assembly
- Combine separately reconstituted components:
- Mix OprM–ND, MexB–ND, and lipidated MexA in 1:1:10 molar ratio
- Incubate under appropriate buffer conditions to facilitate self-assembly
- Combine separately reconstituted components:
Complex Validation
- Analyze complex formation using native PAGE electrophoresis
- Identify electrophoretic mobility shifts indicating successful complex formation
- Employ electron microscopy with negative uranyl acetate staining for structural validation
This protocol successfully demonstrates the intrinsic ability of native efflux pump components to self-assemble into functional tripartite complexes, confirmed through single-particle electron microscopy analysis [11].
Molecular Dynamics Simulation Approaches
Molecular dynamics (MD) simulations provide critical insights into the dynamic behavior of RND efflux pumps, complementing structural data with functional dynamics at atomic resolution [12].
Key Methodological Considerations:
- System Setup: Embed membrane protein complexes in asymmetric phospholipid bilayers with explicit solvent representation
- Simulation Parameters:
- Perform independent unbiased atomistic MD simulations (e.g., 6 × 50 ns trajectories)
- Apply periodic boundary conditions with particle-mesh Ewald electrostatics
- Maintain physiological temperature (310 K) and pressure (1 atm)
- Enhanced Sampling Techniques:
- Steered or targeted MD for probing specific conformational transitions
- Multiple copy simulations with different initial velocity distributions
- Umbrella sampling for free energy calculations along reaction coordinates
MD simulations have elucidated fundamental aspects of RND pump function, including:
- Identification of protein-internal water distributions and proton conduction pathways
- Characterization of substrate transport routes and binding pocket dynamics
- Analysis of allosteric coupling between transmembrane and periplasmic domains
- Investigation of protein-lipid interactions critical for complex stability and function [12]
Table 2: Key Insights from MD Simulations of RND Efflux Pumps
| Simulation Focus | Key Findings | Methodological Approach |
|---|---|---|
| Proton Transport | Identification of cytoplasmic and periplasmic water channels; intermediate-specific hydration patterns | Unbiased atomistic MD of asymmetric trimers with intermediate-specific protonation states |
| Substrate Pathways | Characterization of multiple substrate access channels (CH1-CH4); gating residue dynamics | Analysis of solvent pathways; steered MD for substrate translocation |
| Polyspecificity | Dynamic binding pocket architectures; multiple substrate recognition mechanisms | Docking and MD with diverse antibiotic classes; binding free energy calculations |
| Complex Assembly | Protein-lipid interactions; interfacial stability; adaptor protein conformational coupling | Coarse-grained and all-atom MD of membrane-embedded complexes |
Research Reagent Solutions
Table 3: Essential Research Reagents for RND Efflux Pump Studies
| Reagent/Category | Specific Examples | Research Application | Function/Utility |
|---|---|---|---|
| Membrane Scaffold Proteins | MSP1D1, MSP1E3D1 | Nanodisc reconstitution | Control nanodisc size for specific membrane protein insertion |
| Lipid Systems | POPC (1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine) | Membrane mimetics | Provide native-like lipid environment for membrane proteins |
| Electron Microscopy Reagents | Uranyl acetate | Negative staining | Enhance contrast for single-particle EM analysis |
| Computational Force Fields | CHARMM, AMBER, Martini | Molecular dynamics simulations | Parameterize atomic interactions for accurate dynamics prediction |
| Efflux Pump Inhibitors | D13-9001, phenylalanyl-arginyl-β-naphthylamide (PAβN) | Functional characterization | Competitive and allosteric inhibition studies; therapeutic development |
| Fluorescent Substrates | Ethidium bromide, Hoechst 33342 | Transport assays | Real-time monitoring of efflux activity; inhibitor screening |
Role in Intrinsic Resistance and Clinical Implications
Within the context of intrinsic resistance, RND efflux pumps serve as first-line defense mechanisms that significantly reduce bacterial susceptibility to antimicrobial agents. In P. aeruginosa, even relatively susceptible strains actively extrude tetracycline, chloramphenicol, and fluoroquinolones, with enhanced efflux activity in strains showing elevated intrinsic resistance [13]. This fundamental role in intrinsic resistance is further demonstrated by the hypersusceptibility of mutant strains lacking functional efflux systems [13].
The clinical relevance of RND efflux pumps continues to escalate with the emergence of resistance to novel beta-lactam antibiotics and beta-lactam/beta-lactamase inhibitor combinations [14]. Mutations in RND efflux pumps and their regulatory systems represent common adaptive mechanisms in clinical isolates, leading to increased expression or altered substrate specificity that compromises therapeutic efficacy [14]. Particularly concerning is the observation that P. aeruginosa strains with elevated intrinsic resistance overproduce specific cytoplasmic and outer membrane proteins, including components of efflux systems [13].
Beyond their role in antibiotic resistance, RND efflux pumps contribute significantly to bacterial physiology and pathogenesis through:
- Export of quorum-sensing molecules and virulence factors
- Biofilm formation and maturation
- Stress response and adaptation to hostile environments
- Heavy metal detoxification [15] [16] [10]
Diagram: Multifunctional role of RND pumps in bacterial resistance
The architectural blueprint of RND efflux pumps reveals sophisticated membrane-spanning complexes that efficiently coordinate substrate translocation from the inner membrane to the extracellular space. Their tripartite structural organization, dynamic functional mechanism, and critical role in intrinsic antibiotic resistance establish these systems as pivotal determinants of multidrug resistance in Gram-negative pathogens. Advanced experimental methodologies, including nanodisc reconstitution and molecular dynamics simulations, continue to unravel the intricate details of their assembly and operation. As clinical resistance to novel antimicrobial compounds increasingly involves efflux-mediated mechanisms, comprehensive understanding of these molecular machines provides an essential foundation for developing innovative therapeutic strategies to counteract multidrug resistance. Future research directions should focus on exploiting structural vulnerabilities in these complexes for the rational design of efflux pump inhibitors that can restore antibiotic efficacy in resistant bacterial infections.
Bacterial efflux pumps are membrane-embedded protein complexes that actively transport a wide variety of substrates—including antibiotics, toxic compounds, and metabolic byproducts—out of bacterial cells, serving as a fundamental component of intrinsic antimicrobial resistance [17]. By reducing the intracellular concentration of antibiotics below effective levels, these systems allow bacteria to survive in the presence of antimicrobial agents and create opportunities for the acquisition of more sophisticated resistance mechanisms [5] [15]. This portfolio systematically classifies the six major efflux pump families—ABC, RND, MFS, MATE, SMR, and PACE—detailing their molecular architectures, energy coupling mechanisms, substrate specificities, and roles in bacterial physiology. Understanding these systems is critical for developing novel therapeutic strategies, including efflux pump inhibitors (EPIs), to combat multidrug-resistant bacterial infections [15] [18].
Efflux Pump Family Classification and Characteristics
Bacterial efflux systems are categorized into six major families based on structural features, energy coupling mechanisms, and genetic organization [15] [17]. The table below provides a comprehensive comparison of their key characteristics.
Table 1: Classification and Characteristics of Major Bacterial Efflux Pump Families
| Family | Full Name | Energy Source | Typical Structure | Primary Substrates | Physiological Roles |
|---|---|---|---|---|---|
| ABC | ATP-Binding Cassette | ATP hydrolysis [15] | Tripartite complexes; Two TMDs and two NBDs [15] | Drugs, lipids, sterols [15] | Virulence, nutrient uptake, LPS/CPS export [15] |
| RND | Resistance-Nodulation-Division | Proton motive force [5] | Tripartite (IMP-MFP-OMP) [5] [14] | Broad spectrum: β-lactams, FQs, aminoglycosides, dyes [5] [14] | Virulence, biofilm formation, stress response [5] [14] |
| MFS | Major Facilitator Superfamily | Proton motive force [15] | Single component (12-14 TMS) or tripartite [18] | Structurally diverse compounds [15] | Metabolic waste removal, toxin extrusion [17] |
| MATE | Multidrug and Toxic Compound Extrusion | Proton or sodium ion gradient [15] | Single component (12 TMS) [15] | Fluoroquinolones, aminoglycosides [15] | Detoxification, cation export [15] |
| SMR | Small Multidrug Resistance | Proton motive force [15] | Small tetrameric (4 TMS) [15] | Lipophilic cations, dyes [15] | Quaternary amine compound resistance [15] |
| PACE | Proteobacterial Antimicrobial Compound Efflux | Proton motive force [15] | Single component (4 TMS) [15] | Chlorhexidine, acriflavine [15] | Disinfectant resistance, adaptation [15] |
Molecular Architectures and Transport Mechanisms
ATP-Binding Cassette (ABC) Superfamily
ABC transporters are primary active transporters that utilize energy from ATP hydrolysis to translocate substrates across cellular membranes [15]. They typically consist of two transmembrane domains (TMDs) that form the substrate conduction pathway and two nucleotide-binding domains (NBDs) that bind and hydrolyze ATP [15]. These transporters can function as "full transporters" with all domains contained within a single polypeptide or "half transporters" that homodimerize or heterodimerize to form functional units [15]. In Gram-negative bacteria, some ABC transporters form tripartite efflux systems spanning both membranes, such as the MacAB-TolC system which includes a MacB dimer (inner membrane), hexameric MacA (periplasmic adapter protein), and a TolC trimer (outer membrane channel) [18]. ABC transporters operate via an 'alternate access' mechanism, cycling between inward-facing and outward-facing conformations to extrude substrates [15].
Resistance-Nodulation-Division (RND) Superfamily
RND transporters are among the most clinically significant efflux systems in Gram-negative bacteria due to their broad substrate specificity and contribution to multidrug resistance [5] [14]. These complexes form sophisticated tripartite architectures that span the entire cell envelope, consisting of an inner membrane RND transporter (e.g., AcrB, AdeB), a periplasmic adapter protein (membrane fusion protein, MFP), and an outer membrane factor (OMF) that forms an exit channel [5] [14]. The RND transporter itself typically contains 12 transmembrane segments with two large periplasmic loops that form substrate-binding domains [5]. These pumps function as proton antiporters, coupling substrate efflux to proton import via the proton motive force [5]. The transport mechanism involves sophisticated conformational cycling; in the prototypical AcrB transporter, the trimeric complex operates asymmetrically with each protomer adopting consecutive loose (L), tight (T), and open (O) conformations to create a peristaltic pumping action [18]. Substrates access binding pockets through multiple entry channels and are extruded through the central funnel domain and outer membrane channel [18].
Table 2: Characterized RND Efflux Pumps in Acinetobacter baumannii
| Efflux Pump | Regulator(s) | Genetic Location | Key Substrate Classes |
|---|---|---|---|
| AdeABC | AdeRS, BaeSR [5] | Chromosomal [5] | Aminoglycosides, fluoroquinolones, β-lactams, tetracyclines, tigecycline* [5] |
| AdeFGH | AdeL, ddrR, abaI [5] | Chromosomal [5] | Trimethoprim, chloramphenicol, fluoroquinolones, tetracyclines [5] |
| AdeIJK | AdeN, BaeSR [5] | Chromosomal [5] | β-lactams, cephalosporins, fluoroquinolones, rifampin [5] |
| AdeDE | Unknown [5] | Chromosomal [5] | Meropenem, erythromycin, chloramphenicol, ceftazidime [5] |
Major Facilitator Superfamily (MFS)
The MFS represents the largest known superfamily of secondary active transporters, found ubiquitously across bacteria, archaea, and eukaryotes [15]. These transporters typically possess 12-14 transmembrane segments and utilize proton motive force to drive substrate translocation [15]. While many MFS transporters function as single-component systems, some form tripartite efflux complexes in Gram-negative bacteria, such as EmrAB-TolC, which exports protonophores like CCCP and nalidixic acid [18]. Unlike RND pumps that primarily capture substrates from the periplasm, MFS transporters like EmrB typically interact with cytoplasmic or inner membrane-localized substrates [18].
Minor Efflux Pump Families (MATE, SMR, PACE)
The MATE family represents the most recently classified multidrug efflux transporters, utilizing either proton or sodium ion gradients to drive substrate extrusion [15]. These transporters typically contain 12 transmembrane segments and exhibit specificity for fluorochinolones and aminoglycosides [15]. The SMR family comprises the smallest multidrug resistance transporters, with typical members containing four transmembrane segments and forming homo-tetrameric complexes that use proton motive force to export lipophilic cations and various dyes [15]. The PACE family represents a more recently discovered group of transporters particularly implicated in resistance to disinfectants like chlorhexidine and to compounds like acriflavine [15].
Experimental Methodologies for Efflux Pump Characterization
Protocol 1: Minimum Inhibitory Concentration (MIC) Determination with Efflux Pump Inhibitors
Purpose: To evaluate efflux pump contribution to antibiotic resistance by measuring MIC reduction in presence of EPIs. Reagents:
- Cation-adjusted Mueller-Hinton broth
- Antibiotic stock solutions
- Efflux pump inhibitors (e.g., CCCP, PAβN, verapamil)
- DMSO (solvent control)
- Late-log phase bacterial culture
Procedure:
- Prepare serial two-fold dilutions of the test antibiotic in broth
- Add subinhibitory concentrations of EPI (e.g., 10-50 μg/mL for PAβN) or equivalent DMSO control
- Inoculate wells with ~5×10^5 CFU/mL bacterial suspension
- Incubate at 35±2°C for 16-20 hours
- Record MIC as lowest antibiotic concentration inhibiting visible growth
- Interpret significant efflux activity as ≥4-fold MIC reduction in EPI-containing wells versus control
Validation: Include control strains with known efflux pump overexpression and deletion mutants [18].
Protocol 2: Ethidium Bromide Accumulation Assay
Purpose: To directly measure efflux pump activity using fluorescent substrates. Reagents:
- Ethidium bromide stock solution (1 mg/mL)
- Phosphate-buffered saline (PBS) or appropriate buffer
- Efflux pump inhibitors (CCCP, PAβN)
- Glucose solution (20% w/v)
- Late-log phase bacterial culture
Procedure:
- Harvest bacteria by centrifugation and wash twice with PBS
- Resuspend to OD600 of 0.2 in PBS containing 0.4% glucose
- Add ethidium bromide to final concentration of 1-5 μg/mL
- Distribute aliquots to microtiter plate with and without EPIs
- Monitor fluorescence continuously (excitation: 530 nm, emission: 600 nm)
- Calculate accumulation rates and compare between conditions
Interpretation: Increased fluorescence in EPI-treated samples indicates impaired efflux activity [18].
Protocol 3: Real-time PCR for Efflux Pump Gene Expression
Purpose: To quantify efflux pump gene expression in clinical isolates versus reference strains. Reagents:
- RNA extraction kit with DNase treatment
- cDNA synthesis kit
- SYBR Green PCR master mix
- Gene-specific primers for target efflux pumps and housekeeping genes
- Late-log phase bacterial culture
Procedure:
- Extract total RNA from bacterial cultures
- Treat with DNase to remove genomic DNA contamination
- Synthesize cDNA using reverse transcriptase
- Perform qPCR with gene-specific primers
- Calculate relative expression using 2^(-ΔΔCt) method
- Normalize to housekeeping genes (rpoB, gyrB, or recA)
Controls: Include reference strain and no-template controls [5].
Research Reagent Solutions for Efflux Pump Studies
Table 3: Essential Research Reagents for Efflux Pump Characterization
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Efflux Pump Inhibitors | CCCP, PAβN, verapamil, D13-9001 [14] [18] | Functional characterization of efflux activity | Cytotoxicity, specificity, solvent controls required |
| Fluorescent Substrates | Ethidium bromide, Hoechst 33342, rhodamine 6G [18] | Real-time efflux activity measurements | Substrate specificity varies between pumps |
| Genetic Tools | Knockout mutants, overexpression plasmids, reporter fusions [19] | Mechanistic studies of pump regulation | Complementation controls essential |
| Antibiotic Panels | β-lactams, fluoroquinolones, tetracyclines, aminoglycosides [5] | Substrate profiling | Include novel BL/BLI combinations [14] |
| Structural Biology Reagents | Detergents, crystallization screens, cryo-EM grids [18] | Molecular mechanism studies | Membrane protein stability challenges |
Visualizing Efflux Pump Regulation and Experimental Workflows
Efflux-Mediated Resistance Development Pathway
Diagram 1: Efflux-mediated evolution of antibiotic resistance. Research demonstrates that efflux activation under antibiotic pressure downregulates DNA repair pathways, increasing mutation frequency and accelerating fixation of resistance mutations in bacterial populations [19].
Tripartite RND Efflux Pump Architecture
Diagram 2: Tripartite RND efflux pump structure. The complex spans both membranes, with the inner membrane RND transporter (e.g., AdeB, AcrB) capturing substrates, the membrane fusion protein (MFP) bridging the periplasmic space, and the outer membrane factor (OMF) forming the exit channel [5] [14] [18].
The comprehensive classification of efflux pump families reveals sophisticated bacterial defense systems that contribute significantly to intrinsic antibiotic resistance. The ABC, RND, MFS, MATE, SMR, and PACE families represent distinct evolutionary solutions to the challenge of xenobiotic extrusion, each with unique structural features and energy-coupling mechanisms [5] [15] [17]. Beyond their role in antibiotic resistance, these systems participate fundamentally in bacterial physiology, influencing virulence, biofilm formation, stress response, and intercellular communication [15] [14]. The emerging understanding that efflux activity is genetically linked to DNA repair downregulation and accelerated evolution of resistance mutations highlights the complex role these systems play in bacterial adaptation [19]. Future research directions should prioritize the development of broad-spectrum efflux pump inhibitors that can rejuvenate existing antibiotics, standardized methodologies for clinical detection of efflux-mediated resistance, and structural-guided approaches to overcome the substrate promiscuity of these systems [15] [18]. Addressing these challenges will require interdisciplinary approaches combining structural biology, chemical genomics, and clinical microbiology to develop effective strategies against multidrug-resistant pathogens.
Efflux pumps are integral membrane transporters known for their role in extruding antibiotics, thereby conferring multidrug resistance (MDR) in pathogenic bacteria [15] [9]. However, their functions extend far beyond this classical role. This whitepaper delineates the critical physiological roles of efflux pumps in bacterial virulence, biofilm formation, and stress response, framing these functions within the context of intrinsic resistance research. A comprehensive understanding of these roles is paramount for developing novel therapeutic strategies that target bacterial pathogenicity and resilience, potentially circumventing conventional resistance mechanisms [5] [16].
Physiological Roles of Efflux Pumps
Bacterial efflux pumps are not merely drug ejectors; they are fundamental components of bacterial physiology, adaptation, and pathogenesis. Their activity is intricately linked to the regulation of internal homeostasis, response to environmental stresses, and the expression of virulence factors.
Regulation of Virulence and Pathogenesis
Efflux pumps contribute significantly to bacterial virulence, enabling pathogens to colonize host tissues, evade immune responses, and cause disease.
- Colonization and Host Interaction: In Erwinia amylovora, the AcrAB efflux system is crucial for virulence, plant colonization, and resistance to host-produced plant toxins [9]. Similarly, in Escherichia coli, the AcrAB system pumps out bile acids and fatty acids encountered in the gastrointestinal tract, reducing their toxicity and facilitating colonization [9].
- Adhesion and Invasion: Research indicates a significant reduction in the ability of efflux pump mutants of E. coli and Salmonella enterica to adhere to and invade host cells, underscoring the role of pumps like AcrB in successful infection establishment [15].
- Virulence Factor Transport: Efflux pumps are implicated in exporting molecules essential for pathogenesis. For instance, ABC family transporters contribute to virulence by exporting components for lipopolysaccharides and capsular polysaccharides in major human pathogens [15].
Modulation of Biofilm Formation
Biofilms are structured, surface-attached bacterial communities that are highly resistant to antimicrobials. Efflux pumps are pivotal in multiple stages of biofilm development and maintenance.
- Extrusion of Biofilm-Related Molecules: Pumps actively expel toxins, metabolic waste, and, crucially, quorum sensing (QS) signals and molecules that form the extracellular polymeric substance (EPS) matrix, which is critical for biofilm structure and stability [16] [20].
- Direct Regulation of Biofilm Phenotype: Studies involving efflux pump gene mutagenesis and inhibitors have demonstrated their direct impact on biofilm formation. Key systems include AcrAB-TolC in E. coli, MexAB-OprM in P. aeruginosa, and AdeFGH in A. baumannii [21]. Overexpression of efflux pumps in biofilm-forming bacteria is directly linked to enhanced survival and the establishment of chronic, hard-to-treat infections [16].
- Stage-Dependent Function: The role of a specific efflux pump can vary depending on the stage of biofilm formation, its expression level, and the type and concentration of substrates present in the environment [20]. This dynamic function suggests a complex regulatory network governing biofilm architecture and resilience.
Management of Oxidative and Nitrosative Stress
Inside host cells, bacteria are exposed to lethal reactive oxygen and nitrogen species generated by the immune system. Efflux pumps provide a key defense mechanism against this assault.
- Stress Relief: In Acinetobacter baumannii, it is believed that Resistance-Nodulation-Division (RND) efflux pumps play a role in oxidative and nitrosative stress relief, enhancing bacterial survival within the host [5].
- Intramacrophage Survival: The MacAB efflux pump in Salmonella enterica serovar Typhimurium aids bacterial survival against oxidative stress encountered inside macrophages, a critical step in systemic infection [15].
Heavy Metal Detoxification and Intercellular Signaling
- Heavy Metal Resistance: Efflux pumps confer resistance to heavy metal ions such as Ag²⁺, Cu²⁺, Co²⁺, Zn²⁺, Cd²⁺, and Ni²⁺ by exporting them from the cell. In Gram-negative bacteria, this involves reducing concentrations in both the cytoplasm and the periplasm [15].
- Quorum Sensing and Metabolite Transport: Efflux pumps are involved in the transport of quorum sensing molecules (autoinducers), bacterial metabolites, and other intercellular communication signals, thereby influencing population-level behaviors [15] [14] [9].
Table 1: Key Physiological Functions of Bacterial Efflux Pumps Beyond Antibiotic Resistance
| Physiological Function | Mechanism of Action | Example Efflux Pump(s) | Pathogen Example |
|---|---|---|---|
| Virulence & Colonization | Resistance to host bile acids/fatty acids, adhesion, invasion, toxin export | AcrAB-TolC, AcrAB | E. coli, Erwinia amylovora, Salmonella enterica [15] [9] |
| Biofilm Formation | Extrusion of QS signals, EPS components, and toxic metabolites; direct genetic regulation | AdeFGH, AcrAB-TolC, MexAB-OprM | A. baumannii, E. coli, P. aeruginosa [21] [16] |
| Stress Response | Relief from oxidative and nitrosative stress | RND Pumps, MacAB | A. baumannii, S. enterica [5] [15] |
| Heavy Metal Resistance | Export of toxic metal ions from cytoplasm and periplasm | RND, PACE, ABC families | Various Gram-negative bacteria [15] |
| Intercellular Signaling | Transport of quorum sensing molecules and bacterial metabolites | MexAB-OprM, AcrAB-TolC | P. aeruginosa, E. coli [15] [14] |
Experimental Methodologies for Functional Analysis
Studying the non-antibiotic roles of efflux pumps requires a combination of phenotypic, genotypic, and functional assays. Below are detailed protocols for key experiments.
Assessing Efflux Pump Activity and Biofilm Formation
Protocol 1: Evaluating Efflux Pump Contribution to Biofilm Formation via Gene Inactivation
- Objective: To determine the functional role of a specific efflux pump gene in biofilm development.
- Methodology:
- Strain Construction: Create an isogenic mutant strain with a deletion or disruption of the target efflux pump gene (e.g.,
ΔadeBin A. baumannii). A complementary strain with the gene restored on a plasmid should also be generated. - Biofilm Cultivation: Grow wild-type, mutant, and complementary strains in appropriate media (e.g., Tryptic Soy Broth with 1% glucose for enhanced biofilm) in static conditions using 96-well polystyrene plates for 24-48 hours at the optimal growth temperature [21].
- Biofilm Quantification:
- Remove planktonic cells and gently wash the adhered biofilm.
- Fix the biofilm with methanol or ethanol for 15 minutes.
- Stain with a 0.1% (w/v) crystal violet solution for 20 minutes.
- Wash to remove excess stain.
- Dissolve the bound crystal violet in 33% acetic acid.
- Measure the optical density at 570 nm (OD₅₇₀) using a microplate reader. A significant reduction in the mutant's OD compared to the wild-type indicates the pump's role in biofilm formation [21].
- Strain Construction: Create an isogenic mutant strain with a deletion or disruption of the target efflux pump gene (e.g.,
- Interpretation: Confirmation is achieved if the complementary strain shows restored biofilm formation, directly linking the gene to the phenotype.
Protocol 2: Phenotypic Detection of Efflux Activity Using Fluorometric Assays
- Objective: To measure the real-time efflux capability of bacterial strains.
- Methodology:
- Cell Preparation: Grow bacterial cells to mid-log phase. Harvest and wash them in a buffer (e.g., Phosphate Buffered Saline, PBS) at pH 7.0.
- Substrate Loading: Incubate the cell suspension with a fluorescent efflux pump substrate (e.g., Ethidium Bromide (EtBr) at 1-2 µg/mL) for 30-60 minutes to allow intracellular accumulation.
- Energy Depletion: To arrest active efflux, add an energy inhibitor like Carbonyl Cyanide m-Chlorophenylhydrazone (CCCP), a proton motive force uncoupler, to a final concentration of 10-50 µM. Incubate for an additional 10-15 minutes.
- Efflux Measurement:
- Centrifuge the cells and resuspend them in fresh, pre-warmed buffer without EtBr or CCCP.
- Immediately transfer the suspension to a quartz cuvette or a microplate.
- Monitor the fluorescence intensity over time (e.g., every 30 seconds for 10-15 minutes) using a spectrofluorometer (for EtBr: excitation 530 nm, emission 585 nm) [16] [16].
- Data Analysis: Strains with high efflux activity will show a rapid decrease in fluorescence as the substrate is extruded. The inclusion of a known efflux pump inhibitor (EPI) serves as a control to confirm the efflux mechanism.
Gene Expression Analysis in Biofilms
Protocol 3: Quantifying Efflux Pump Gene Expression using RT-PCR
- Objective: To compare efflux pump gene expression levels between planktonic and biofilm states.
- Methodology:
- RNA Isolation:
- Grow biofilms on a large surface area (e.g., in a biofilm reactor or on multiple plates). Harvest biofilm cells by scraping or sonication.
- In parallel, harvest planktonic cells from the same culture.
- Stabilize RNA immediately using a reagent like RNAprotect Bacteria Reagent.
- Extract total RNA using a commercial kit with an on-column DNase I digestion step to remove genomic DNA contamination.
- cDNA Synthesis: Use a high-capacity cDNA reverse transcription kit with random hexamers to synthesize first-strand cDNA from 500 ng to 1 µg of purified RNA.
- Quantitative PCR (qPCR):
- Design gene-specific primers for the target efflux pump (e.g.,
adeB,acrB,mexB) and for reference housekeeping genes (e.g.,rpoB,gyrB,16S rRNA). - Prepare a SYBR Green qPCR master mix according to manufacturer instructions and run the reactions in triplicate on a real-time PCR instrument.
- Use a standard thermal cycling protocol (e.g., 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min).
- Design gene-specific primers for the target efflux pump (e.g.,
- Data Analysis: Calculate the relative gene expression using the comparative 2^–ΔΔCq method. Normalize the Cq values of the target gene to the reference gene(s) and compare the biofilm samples to the planktonic control [16] [22]. An upregulation in biofilms suggests a functional role for the pump in this mode of growth.
- RNA Isolation:
Research Reagent Solutions Toolkit
Table 2: Essential Reagents for Investigating Efflux Pump Physiology
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Isogenic Mutant Strains | To study the specific function of a single efflux pump gene by comparison to wild-type. | Comparing biofilm formation in ΔacrB vs. wild-type E. coli [21]. |
| Efflux Pump Inhibitors (EPIs) | To chemically block pump activity and observe resultant phenotypic changes. | Using CCCP or PAβN to assess restoration of antibiotic susceptibility in biofilms [16]. |
| Fluorescent Substrates | To act as a tracer for direct measurement of efflux pump activity. | Using Ethidium Bromide in fluorometric assays to quantify real-time efflux [16]. |
| Gene Expression Assays | To quantify mRNA levels of efflux pump genes under different conditions. | SYBR Green-based RT-PCR to measure adeIJK expression in A. baumannii biofilms [16]. |
| Crystal Violet Stain | To quantify total biomass in static biofilm models. | Standard staining protocol for 96-well plate biofilm assays [21]. |
Visualizing Efflux Pump Regulation and Function
The following diagrams illustrate the regulatory pathways of efflux pumps and a standardized experimental workflow.
Efflux Pump Regulation and Physiological Impact
Diagram 1: Regulatory network of efflux pump expression and its physiological consequences. Environmental stressors activate regulatory systems, leading to efflux pump overexpression which directly influences key physiological traits like biofilm formation, virulence, and stress response [5] [14] [16].
Experimental Workflow for Functional Analysis
Diagram 2: A multi-faceted experimental workflow for analyzing efflux pump functions. The process begins with genetic manipulation, followed by parallel phenotypic, functional, and molecular analyses to comprehensively characterize pump roles [21] [16] [22].
The physiological functions of efflux pumps in virulence, biofilm formation, and stress response are fundamental to bacterial survival and pathogenesis. Viewing these transporters solely as antibiotic resistance elements provides an incomplete picture. Future research and therapeutic development should focus on these intrinsic roles, potentially leading to novel anti-virulence strategies and efflux pump inhibitors that disarm pathogens rather than directly killing them, thereby reducing selective pressure for resistance.
In the landscape of antimicrobial resistance (AMR), multidrug efflux pumps represent a primary defense mechanism for bacterial pathogens, contributing significantly to intrinsic and acquired resistance. Among Gram-negative bacteria, Acinetobacter baumannii and Pseudomonas aeruginosa stand out due to their formidable ability to expel a wide range of antimicrobial agents. A. baumannii, particularly its carbapenem-resistant form (CRAB), is classified by the World Health Organization as a critical priority pathogen, while P. aeruginosa is a leading cause of life-threatening nosocomial infections [23] [24]. The core of this defensive capability lies in their Resistance-Nodulation-Division (RND) family efflux pumps: the Ade pumps in A. baumannii and the Mex pumps in P. aeruginosa. These sophisticated transporter systems not only extrude antibiotics but are also intricately linked to fundamental bacterial physiology, including virulence, biofilm formation, and stress response [25] [26]. This whitepaper provides an in-depth technical analysis of these efflux systems, detailing their operational mechanisms, regulatory networks, and methods for their experimental investigation, framed within the broader context of intrinsic resistance research.
Ade Pumps in Acinetobacter baumannii
Major Ade Pumps and Their Characteristics
Acinetobacter baumannii possesses several RND efflux pumps, among which three are clinically most significant: AdeABC, AdeIJK, and AdeFGH. Their characteristics are summarized in Table 1.
Table 1: Major RND Efflux Pumps in Acinetobacter baumannii
| Efflux Pump | Genomic Context | Key Regulator | Primary Regulatory Mechanism | Common Antibiotic Substrates |
|---|---|---|---|---|
| AdeABC [26] | Core genome (some strains have AdeC) | AdeSR [26] | Two-component system (TCS) | Tetracyclines (e.g., Tigecycline), Aminoglycosides, Fluoroquinolones, Chloramphenicol [23] [26] |
| AdeIJK [26] | Core genome | Unknown (non-local) | Putative GntR-type regulator; AdeN suspected [26] | Broad spectrum of antibiotics, β-lactams [26] |
| AdeFGH [26] | Core genome | AdeL [26] | LysR-type transcriptional regulator (LTTR) | Fluoroquinolones, Chloramphenicol, Trimethoprim, Clindamycin [23] |
AdeABC is the most frequently overexpressed pump in multidrug-resistant (MDR) clinical isolates. Its expression is controlled by the AdeSR two-component system, where AdeS is a histidine kinase and AdeR is a response regulator [26]. Upon sensing environmental signals (e.g., antibiotic presence), AdeS autophosphorylates and transfers the phosphate to AdeR. Phosphorylated AdeR then binds to the intercistronic region between adeR and adeA, activating transcription of the adeABC operon [26]. Mutations in adeS or adeR are a common mechanism for constitutive overexpression of this pump in clinical strains [26].
AdeIJK is considered the ancestral efflux pump of the Acinetobacter genus and is present in the core genome of all species. Its basal activity contributes to intrinsic resistance, and its overexpression leads to a broad MDR phenotype. In contrast, AdeFGH is the least studied, and its full clinical impact is still being elucidated [26].
Regulatory Pathways of Ade Pumps
The following diagram illustrates the complex transcriptional regulation of the key Ade efflux pumps in A. baumannii.
Diagram Title: Transcriptional Regulation of A. baumannii Ade Pumps
Mex Pumps in Pseudomonas aeruginosa
Major Mex Pumps and Their Roles
Pseudomonas aeruginosa's resistance is heavily mediated by four clinically relevant Mex efflux pumps of the RND family. These tripartite systems span the cell envelope and are composed of an inner membrane RND transporter (e.g., MexB), a periplasmic membrane fusion protein (MFP, e.g., MexA), and an outer membrane factor (OMF, e.g., OprM) [27] [24]. Their individual profiles are detailed in Table 2.
Table 2: Major RND Efflux Pumps in Pseudomonas aeruginosa
| Efflux Pump | Expression | Key Regulatory Gene(s) | Primary Antibiotic Substrates | Other Functions |
|---|---|---|---|---|
| MexAB-OprM [28] [27] [24] | Constitutive | nalC, nalB, naID [24] | β-lactams, Fluoroquinolones, Tetracycline, Chloramphenicol [28] [24] | Bile acid & fatty acid extrusion [24] |
| MexXY-OprM [28] [27] | Inducible | mexZ [27] | Aminoglycosides, Fluoroquinolones, Tetracycline, Erythromycin [28] [27] | Induced by ribosome-targeting antibiotics [27] |
| MexCD-OprJ [28] | Repressed in wild-type | nfxB [27] | Fluoroquinolones, Tetracycline, Chloramphenicol, Cephems [28] | - |
| MexEF-OprN [28] | Repressed in wild-type | nfxC [27] | Fluoroquinolones, Chloramphenicol, Trimethoprim [28] | - |
MexAB-OprM is constitutively expressed and provides a baseline level of intrinsic resistance to a wide range of antibiotic classes. In contrast, MexXY is noteworthy for its inducibility by ribosome-inhibiting antibiotics and its central role in aminoglycoside resistance, particularly in cystic fibrosis isolates [27]. MexCD-OprJ and MexEF-OprN are typically silent in wild-type strains but can be derepressed through mutations, leading to increased resistance to their specific substrate profiles [28] [27].
Regulatory Network of Mex Pumps
The regulation of Mex pumps is multi-layered, involving local repressors and global regulators that respond to environmental stresses. The following diagram maps this complex regulatory network.
Diagram Title: Regulatory Network of P. aeruginosa Mex Pumps
Experimental Approaches for Efflux Pump Research
Workflow for Identifying Natural Substrates via Metabolomics
Understanding the full physiological role of efflux pumps requires identifying their natural substrates. A powerful approach for this is untargeted metabolomics, as exemplified by a recent study on P. aeruginosa [28]. The experimental workflow is outlined below.
Diagram Title: Metabolomic Workflow for Identifying Natural Substrates
Detailed Methodology:
- Strain Construction: Create a mutant strain (e.g., PA14Δ4mex) genetically deleted for the four major Mex efflux pumps (mexAB-oprM, mexCD-oprJ, mexXY-oprM, and mexEF-oprN) to serve as a background with minimal efflux activity [28].
- Genetic Complementation: Clone the operon of each efflux pump into an expression vector (e.g., pSRKGm) under the control of an inducible promoter (e.g., lac promoter). Introduce these constructs individually into the mutant strain to create a panel of isogenic strains, each overexpressing a single, specific efflux pump [28].
- Functional Validation: Verify the functionality of the overexpressed pumps by determining the Minimum Inhibitory Concentration (MIC) of known antibiotic substrates against each strain in the panel. A successful complementation should restore resistance levels to the substrates of the specific pump being expressed [28].
- Sample Preparation: Grow the wild-type, pump-deficient mutant, and individual pump-overexpressing strains under defined conditions. Collect culture supernatants at the desired growth phase and remove bacterial cells via filtration or centrifugation to obtain the "exo-metabolome" for analysis [28].
- LC-HRMS Analysis: Analyze the supernatant samples using Liquid Chromatography-High Resolution Mass Spectrometry (LC-HRMS) in an untargeted mode. This allows for the detection of a wide array of metabolic features [28].
- Data Analysis: Process the raw metabolomic data using specialized software for feature detection, alignment, and normalization. Statistically compare the abundance of each metabolic feature in the supernatant of each pump-overexpressing strain against the pump-deficient mutant. Features that are significantly more abundant when a specific pump is overexpressed are considered potential natural substrates for that pump [28].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Efflux Pump Studies
| Reagent / Material | Function / Application in Research | Example / Note |
|---|---|---|
| pSRKGm Expression Vector [28] | Inducible expression of efflux pump operons for genetic complementation and overexpression studies. | Used in P. aeruginosa for controlled EP expression from a lac promoter [28]. |
| LC-HRMS System [28] | Untargeted metabolomic analysis for identifying and characterizing natural substrates of efflux pumps. | Critical for detecting a wide range of metabolic features in culture supernatants [28]. |
| Efflux Pump Inhibitors (EPIs) [15] [24] | Tool compounds to probe efflux pump function; potential leads for adjuvant therapy. | PAβN (Phenylarginyl-β-naphtylamide) is a widely used research EPI, though toxic for clinical use [24]. |
| Defined Mutant Libraries [28] [15] | Isogenic strains with single or multiple efflux pump gene deletions for functional genomics. | Essential for controlled experiments to assign specific functions to individual pumps. |
| RNA Sequencing (RNAseq) [28] | Transcriptomic profiling to analyze EP gene expression and regulatory networks. | Used to verify no compensatory overexpression of other EPs in multi-pump deletion mutants [28]. |
The Ade and Mex RND efflux pumps are fundamental components of the intrinsic resistome of A. baumannii and P. aeruginosa, respectively. Their ability to extrude diverse antimicrobials, coupled with complex regulatory networks that fine-tune their expression, makes them formidable adversaries. Research efforts are increasingly shifting towards understanding their natural physiological roles and regulatory mechanisms, as this knowledge is crucial for developing next-generation antimicrobial strategies. Promising approaches include the discovery of competitive efflux pump inhibitors (EPIs) based on natural substrate structures [28], and the targeting of transcriptional regulators like AdeR to sensitize bacteria to existing antibiotics [26]. Overcoming the technical challenges associated with EPI development, such as achieving potency and avoiding eukaryotic toxicity, remains a key frontier. A deep and integrated understanding of efflux pump biology, from molecular structure to physiological function, is therefore indispensable for combating multidrug-resistant infections caused by these priority pathogens.
From Bench to Diagnostics: Advanced Techniques for Detecting and Quantifying Efflux Activity
Efflux pumps are a critical component of intrinsic antibiotic resistance in bacteria, significantly reducing the intracellular concentration of antimicrobial agents and contributing to the multidrug-resistant (MDR) phenotype [29] [30]. Phenotypic assays that measure the reduction of minimum inhibitory concentrations (MICs) in the presence of efflux pump inhibitors (EPIs), combined with fluorometric assays that directly quantify efflux activity, provide powerful tools for quantifying this resistance mechanism and screening for novel therapeutic adjuvants. This technical guide details the core methodologies and applications of these assays within intrinsic resistance research, providing a standardized framework for researchers and drug development professionals.
Quantitative Profiling of Efflux Pump Inhibitors via MIC Reduction Assays
The MIC reduction assay is a foundational phenotypic method for evaluating the efficacy of EPIs. It determines the fold increase in antibiotic susceptibility conferred by a candidate EPI, providing a direct measure of its potential to reverse efflux-mediated resistance.
Table 1: Representative EPI Efficacy from MIC Reduction Assays
| EPI Candidate | Bacterial Strain | Antibiotic Potentiated | MIC Reduction (Fold) | Key Findings |
|---|---|---|---|---|
| Sertaconazole & Oxiconazole [29] | S. aureus (MSSA & MRSA) | Norfloxacin, Cefotaxime, Moxifloxacin | Significant reduction (specific values not provided) | Restored antibiotic efficacy; minimal cytotoxicity; effective in murine infection model. |
| KSA5_1 [31] | MDR A. baumannii | Ciprofloxacin | Up to 512-fold | Superior to PAβN; inhibits AdeG efflux pump gene expression. |
| Vitamin D & Vitamin K [30] | K. pneumoniae & P. aeruginosa | Ciprofloxacin | 64-fold | Powerful anti-efflux activity observed via EtBr accumulation. |
| Omeprazole (OME) [30] | K. pneumoniae & P. aeruginosa | - | - | Decreased expression of acrB and mexA efflux genes by 91.5% and 99.7%, respectively. |
| D13-9001 [32] | E. coli producing MexAB-OprM | Aztreonam, Ciprofloxacin, Erythromycin | Synergy observed (specific fold reduction not provided) | Specific inhibitor of MexAB-OprM; no activity against MexXY-OprM. |
| Chlorpromazine [33] | E. coli | Trimethoprim | Synergy observed | Efflux pump inhibitor used in resistance-proofing studies. |
Experimental Protocol: Broth Microdilution for MIC Reduction
Principle: This method assesses the ability of an EPI to lower the MIC of a co-administered antibiotic by inhibiting active efflux, thereby increasing intracellular antibiotic accumulation [29] [30] [31].
Materials:
- Cation-adjusted Mueller-Hinton broth (CAMHB)
- Sterile 96-well microtiter plates
- Logarithmic-phase bacterial suspension (e.g., adjusted to 1 × 10⁶ CFU/mL)
- Antibiotic stock solutions (e.g., norfloxacin, ciprofloxacin)
- EPI stock solution (e.g., sertaconazole, KSA5_1)
Method:
- Preparation: Dispense CAMHB into the wells of the microtiter plate.
- Antibiotic Dilution: Perform two-fold serial dilutions of the antibiotic in the growth medium along the rows of the plate.
- EPI Addition: Add the candidate EPI at a sub-inhibitory concentration (e.g., 0.25× or 0.5× its predetermined MIC) to all test wells [30]. A control without the EPI must be included.
- Inoculation: Inoculate all wells with the standardized bacterial suspension. Include growth control and sterility control wells.
- Incubation: Incubate the plate at 37°C for 16–20 hours.
- Analysis: Determine the MIC of the antibiotic in the presence and absence of the EPI. The MIC is the lowest concentration that completely inhibits visible growth. The fold reduction is calculated as: MIC(antibiotic alone) / MIC(antibiotic + EPI).
Validation: A significant reduction (typically ≥4-fold) in the MIC of the antibiotic in the presence of the EPI is indicative of efflux pump inhibition [29] [31].
Direct Measurement of Efflux Activity via Fluorometric Assays
Fluorometric assays provide direct, real-time functional data on efflux pump activity by tracking the accumulation or extrusion of fluorescent substrate dyes in the presence of EPIs.
Table 2: Key Fluorometric Assays for Efflux Activity
| Assay Type | Fluorogenic Substrate | Key Readout | Application & Advantage |
|---|---|---|---|
| Ethidium Bromide (EtBr) Accumulation Assay [29] [30] | Ethidium Bromide (EtBr) | Increase in fluorescence intensity indicates EPI-mediated efflux inhibition. | Standard method; real-time kinetic measurement; adaptable to high-throughput. |
| FDG-Based Microfluidic Assay [32] | Fluorescein-di-β-d-galactopyranoside (FDG) | Intracellular fluorescence after hydrolysis indicates reduced efflux. | Highly sensitive; allows single-cell analysis; visualizes real-time efflux inhibition. |
| MALDI-TOF MS Efflux Monitoring [34] | EtBr, Hoechst 33342, Nile Red, drugs | Direct measurement of substrate abundance in extracellular medium over time. | Label-free; avoids fluorescence quenching issues; monitors multiple substrates. |
Experimental Protocol: Ethidium Bromide (EtBr) Accumulation Assay
Principle: EtBr is a substrate for many efflux pumps. Its fluorescence is quenched in aqueous environments and strongly enhances upon binding to intracellular DNA. Inhibition of efflux pumps leads to increased intracellular accumulation of EtBr and a corresponding increase in fluorescence [29] [30].
Materials:
- Phosphate-buffered saline (PBS), pH 7.4
- Bacterial cells in mid-logarithmic phase (OD600 ~ 0.6)
- Ethidium Bromide stock solution (1 mg/mL)
- Candidate EPI (e.g., sertaconazole, oxiconazole)
- Glucose solution (for energy-dependent efflux)
- 96-well black-walled microplate
- Multi-mode plate reader with fluorescence capabilities (excitation ~530 nm, emission ~590 nm)
Method:
- Cell Preparation: Harvest bacterial cells by centrifugation and resuspend in PBS to an OD600 of ~0.3.
- Plate Setup: Dispense the cell suspension into the wells of a black microplate.
- Treatment: Add EtBr (e.g., 1 µg/mL) to all experimental wells. Add the candidate EPI (e.g., 10 µM) to the test wells. Include controls:
- Negative Control: Cells + EtBr + Glucose (0.4% to energize efflux)
- Positive Control: Cells + EtBr + known EPI (e.g., Thioridazine at 16 µg/mL)
- Test: Cells + EtBr + candidate EPI
- Measurement: Immediately transfer the plate to a pre-warmed (37°C) plate reader. Shake the plate continuously and measure the fluorescence intensity every 5 minutes for 60 minutes.
- Data Analysis: Plot fluorescence intensity versus time. A steeper slope and higher final fluorescence in the test well compared to the negative control indicate successful inhibition of efflux activity [29].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Efflux Assays
| Reagent | Function in Assay | Example Usage & Note |
|---|---|---|
| Ethidium Bromide (EtBr) [29] [34] [30] | Fluorescent efflux pump substrate. | Used in accumulation/efflux assays; fluorescence increases upon DNA binding. |
| Carbonyl Cyanide m-Chlorophenyl Hydrazone (CCCP) [34] [30] | Protonophore that dissipates proton motive force (PMF). | Positive control for EPI; inhibits PMF-driven secondary transporters. |
| Phenylarginine-β-Naphthylamide (PAβN) [34] [32] [31] | Broad-spectrum EPI for RND pumps. | Commonly used positive control for Gram-negative bacteria; can have membrane permeabilizing effects. |
| Fluorescein-di-β-d-galactopyranoside (FDG) [32] | Fluorogenic substrate hydrolyzed intracellularly to fluorescent fluorescein. | Used in specialized microfluidic assays; both FDG and fluorescein are efflux substrates. |
| Sertraline [35] | Clinically used antidepressant identified as an EPI. | Prevents formation of phenotypically resistant subpopulations to AMPs in stationary phase cells. |
Signaling Pathways and Mechanisms of Efflux Inhibition
A key mechanism of efflux pump inhibition involves disruption of the energy source required for pump activity. Secondary active transporters, such as those in the Major Facilitator Superfamily (MFS) and Resistance-Nodulation-Division (RND) family, utilize the proton motive force (PMF) [29].
Diagram Title: EPI Inhibition of PMF-Dependent Efflux
Studies on EPIs like sertaconazole and oxiconazole demonstrate that they alter the PMF, diminishing the membrane potential (ΔΨ) while increasing the ΔpH component, thereby robbing the efflux pumps of their energy source and ultimately inhibiting ATP production [29].
Advanced Methodologies and Future Directions
Novel Analytical and Single-Cell Approaches
MALDI-TOF MS for Efflux Monitoring: This label-free method directly measures the efflux of substrates by tracking their abundance in the extracellular medium over time using mass spectrometry. It avoids potential issues associated with fluorescent dyes, such as signal quenching, and can monitor multiple substrates simultaneously [34].
Microfluidic Single-Cell Analysis: Microfluidic devices, combined with fluorogenic substrates like FDG, enable the observation of efflux inhibition in real-time at the single-cell level. This high-sensitivity approach can reveal heterogeneous efflux pump expression and activity within a clonal population, which is crucial for understanding phenotypic resistance [32] [35].
Experimental Workflow for Comprehensive Profiling
Diagram Title: Workflow for EPI Profiling
The path to a successful EPI involves multiple, complementary assays. The workflow typically begins with basic phenotypic screening (MIC reduction) and functional analysis (fluorometric assays), progressing to molecular confirmation of EP gene expression, and finally, advanced profiling using techniques like microfluidics and metabolomics [29] [30] [28]. This multi-faceted approach is essential for deciphering the role of efflux pumps in intrinsic resistance and for developing effective therapeutic strategies to combat multidrug-resistant pathogens.
Antimicrobial resistance (AMR) represents a critical threat to global public health, with projections of 10 million annual deaths by 2050 if left unaddressed [36]. Among the various mechanisms bacteria employ to resist antibiotics, multidrug efflux pumps constitute a formidable first line of defense through intrinsic resistance [37]. These membrane-associated transporters actively extrude diverse toxic compounds, including multiple classes of antibiotics, from the bacterial cell before they reach their intracellular targets [38]. The resistance-nodulation-division (RND) family of efflux pumps, exemplified by AcrAB-TolC in Escherichia coli and Enterobacteriaceae and MexAB-OprM in Pseudomonas aeruginosa, are particularly noteworthy for their exceptionally broad substrate specificity and clinical significance [39] [40].
Genotypic profiling of efflux pump gene expression has therefore become indispensable in AMR research. Quantitative PCR (qPCR) and RNA sequencing (RNA-seq) are the cornerstone technologies for quantifying expression changes in genes like acrAB and mexB, providing insights into their regulation and contribution to resistance phenotypes [41] [42]. This technical guide details the application of these methodologies within the context of intrinsic resistance research, providing standardized protocols, data interpretation frameworks, and analytical tools for researchers and drug development professionals.
Technological Platforms for Expression Analysis
qPCR vs. RNA-seq: A Comparative Analysis
The choice between qPCR and RNA-seq is guided by the research objectives, throughput requirements, and available resources.
Table 1: Comparison of qPCR and RNA-seq for Efflux Pump Gene Expression Analysis
| Feature | Quantitative PCR (qPCR) | RNA Sequencing (RNA-seq) |
|---|---|---|
| Throughput | Low to medium; targets a predefined set of genes [43] | High; profiles the entire transcriptome [41] |
| Hypothesis | Targeted; confirms specific gene expression changes | Discovery-oriented; identifies novel regulators and pathways |
| Sensitivity | High; capable of detecting low-abundance transcripts [44] | Moderate; may miss extremely low-expression genes |
| Data Output | Cycle threshold (Ct) values for relative quantification [43] | Counts of sequencing reads mapped to genomic features |
| Primary Application | Validating expression changes in known efflux pump and regulator genes [42] | Uncovering global transcriptional responses and novel resistance mechanisms [41] |
| Cost and Expertise | Lower cost; requires standard molecular biology lab skills | Higher cost; requires bioinformatics expertise for data analysis |
Experimental Workflow for Genotypic Profiling
The following diagram outlines the generalized workflow for a gene expression study in efflux pump research, from experimental design to data interpretation:
Figure 1: Generalized workflow for efflux pump gene expression studies using qPCR and RNA-seq.
Detailed Experimental Methodologies
Quantitative PCR (qPCR) Protocol
The qPCR protocol provides a sensitive and reproducible method for targeted quantification of efflux pump gene expression.
3.1.1 Sample Preparation and RNA Extraction
- Culture Conditions: Grow bacterial strains to the late log phase (OD₆₀₀ ≈ 0.6) under defined conditions (e.g., 37°C with aeration). Include experimental groups exposed to sub-inhibitory concentrations of the antibiotic of interest and an unexposed control group [43].
- RNA Extraction: Use commercial kits (e.g., RNeasy Kit, Qiagen) for RNA extraction, following the manufacturer's instructions. It is critical to include an on-column DNase digestion step to remove genomic DNA contamination [43].
- Quality Control: Assess RNA integrity and concentration using spectrophotometry (NanoDrop) or microfluidics-based systems (e.g., Bioanalyzer). High-quality RNA (A₂₆₀/A₂₈₀ ratio of ~2.0) is essential for reliable results.
3.1.2 cDNA Synthesis and qPCR Setup
- Reverse Transcription: Synthesize cDNA from 0.5-1 µg of total RNA using a reverse transcription kit (e.g., PrimeScript cDNA synthesis kit, TaKaRa) with random hexamers and/or gene-specific primers [43].
- qPCR Reaction: Prepare reactions using a SYBR Green or TaqMan master mix. A typical 20 µL reaction contains 1X master mix, gene-specific primers (0.2-0.5 µM each), and cDNA template (typically 1-10 ng equivalent of input RNA) [43].
- Primer Design: Ensure primers are specific and designed to amplify a 75-200 bp product. Validate primer efficiency through a standard curve before use. Table 3 in the appendix provides an example primer set.
3.1.3 Data Analysis
- Normalization: Normalize the expression of the target genes (e.g., acrB, mexB) to that of a stable endogenous reference gene, most commonly the 16S ribosomal RNA gene (rrsE) [43] [44].
- Relative Quantification: Calculate the fold change in gene expression using the comparative 2^(-ΔΔCt) method [43]. Report the results as the mean fold change ± standard deviation from at least three independent biological replicates, each run in technical triplicate.
RNA Sequencing (RNA-seq) Protocol
RNA-seq offers a hypothesis-free, comprehensive view of the transcriptional landscape.
3.2.1 Library Preparation and Sequencing
- RNA Preparation: Follow the steps in section 3.1.1 to obtain high-quality total RNA. For bacterial RNA-seq, ribosomal RNA (rRNA) depletion is typically performed instead of poly-A selection, as bacterial mRNAs lack poly-A tails.
- Library Construction: Use a stranded RNA-seq library preparation kit according to the manufacturer's protocol. This involves RNA fragmentation, cDNA synthesis, adapter ligation, and PCR amplification.
- Sequencing: Sequence the libraries on an appropriate platform (e.g., Illumina NovaSeq) to generate a minimum of 10-20 million paired-end reads per sample to ensure sufficient depth for transcriptional profiling.
3.2.2 Bioinformatic Analysis
- Quality Control and Trimming: Use tools like FastQC to assess raw read quality. Trim adapter sequences and low-quality bases with tools such as Trimmomatic or Cutadapt.
- Alignment and Quantification: Map the quality-filtered reads to a reference genome using a splice-aware aligner like HISAT2 or STAR. Then, use featureCounts or HTSeq to count the number of reads aligned to each gene.
- Differential Expression Analysis: Input the read counts into statistical software packages in R (e.g., DESeq2, edgeR) to identify genes that are significantly differentially expressed between experimental conditions (e.g., antibiotic-exposed vs. control). A common significance threshold is an adjusted p-value (FDR) of < 0.05 and a |log2 fold change| > 1.
Key Research Reagent Solutions
Successful execution of these protocols relies on a suite of specific reagents and tools.
Table 2: Essential Research Reagents and Materials for Efflux Pump Expression Studies
| Reagent / Material | Function / Application | Examples & Notes |
|---|---|---|
| RNA Extraction Kit | Isolation of high-quality, DNA-free total RNA | RNeasy Kit (Qiagen) [43] |
| Reverse Transcription Kit | Synthesis of first-strand cDNA from RNA templates | PrimeScript cDNA Synthesis Kit (TaKaRa) [43] |
| qPCR Master Mix | Amplification and fluorescence-based detection of cDNA | SYBR Green or TaqMan master mixes [43] |
| rRNA Depletion Kit | Removal of ribosomal RNA prior to RNA-seq library prep | Crucial for bacterial transcriptome studies |
| RNA-seq Library Prep Kit | Preparation of sequencing-ready libraries from cDNA | Illumina TruSeq Stranded Total RNA Kit |
| Efflux Pump Inhibitors (EPIs) | Functional validation of efflux pump activity | Carbonyl Cyanide m-chlorophenylhydrazone (CCCP) [40] [38], Verapamil [44] |
| Reference Gene Primers | Endogenous control for qPCR normalization | 16S rRNA (rrsE) gene primers [43] [44] |
Data Interpretation and Integration with Phenotypic Assays
Correlating Genotype with Phenotype
A crucial step in intrinsic resistance research is linking gene expression data to observable physiological outcomes.
- Minimum Inhibitory Concentration (MIC) Assays: Determine the MIC of antibiotics against the strain of interest using broth microdilution according to CLSI/EUCAST guidelines. A significant reduction in MIC (e.g., ≥ 4-fold) upon the addition of an EPI like CCCP provides direct functional evidence of efflux pump-mediated resistance [40] [38]. For example, a study on P. aeruginosa showed that CCCP reduced the MIC of ciprofloxacin for 83.3% of resistant isolates [38].
- Meta-Analysis Evidence: A systematic review confirmed that acrAB overexpression is significantly associated with multidrug resistance in E. coli, and EPIs significantly restore antibiotic susceptibility (Risk Ratio: 4.2, 95% CI: 3.0–5.8) [42].
Regulatory Pathways Governing Efflux Pump Expression
Interpreting expression data requires an understanding of the complex regulatory networks controlling efflux pumps. The following diagram illustrates the key regulators of the acrAB operon in E. coli:
Figure 2: Key transcriptional regulators of the acrAB-tolC efflux pump in E. coli. Regulators like MarA, SoxS, and Rob are activated by environmental stressors and bind to the acrAB promoter to upregulate its expression, leading to the MDR phenotype [42].
Application in Research: Key Findings and Case Studies
The application of qPCR and RNA-seq has yielded critical insights into the role of efflux pumps in virulence and resistance across pathogens.
Table 3: Key Research Findings on Efflux Pump Gene Expression from Recent Studies
| Pathogen / Context | Key Finding | Method Used | Experimental Detail |
|---|---|---|---|
| EnteroaggregativeE. coli (EAEC) | Deletion of acrB prevented biofilm formation, reduced eDNA export, and attenuated lethality in a C. elegans infection model [39]. | qPCR / Genetic deletion | Study compared wild-type, ΔacrB, and complemented strains. |
| P. aeruginosa(Medical Implants) | 57% of isolates were MDR; 12% were XDR. Active efflux confirmed by significant MIC reduction with CCCP (p<0.05). mexB genes prevalent in resistant isolates [40]. | PCR, MALDI-TOF, MIC assays | 42 clinical isolates from implant-related infections were analyzed. |
| M. tuberculosis(Clinical Isolates) | 88.9% of MDR isolates overexpressed one or more of 10 putative efflux pump genes. Rv0933 and Rv1250 were most frequently overexpressed [44]. | qPCR with two reference genes | 46 clinical isolates (sensitive, mono-resistant, MDR) were analyzed. |
| M. tuberculosis(Kanamycin Resistance) | 12 genes (e.g., Rv1258c, Rv3065) were overexpressed after kanamycin exposure, suggesting a role in resistance beyond rrs mutations [41]. | RNA-seq | Compared expression at MIC₂₅ and MIC₅₀ in wild-type and rrs mutant strains. |
Genotypic profiling via qPCR and RNA-seq is non-negotiable for modern research into intrinsic resistance mediated by efflux pumps. While qPCR remains the gold standard for targeted, sensitive, and cost-effective validation of specific gene expression changes, RNA-seq is a powerful discovery tool for revealing the global transcriptional adaptations underlying the MDR phenotype. The consistent finding that efflux pump gene overexpression is a widespread mechanism across diverse bacterial pathogens—from E. coli and P. aeruginosa to M. tuberculosis—highlights its fundamental role in AMR [39] [40] [44]. Integrating these genotypic data with functional phenotypic assays like MIC determination provides a comprehensive framework for validating efflux pump activity and identifying novel targets for EPIs. As research progresses, standardizing these methodologies and leveraging their synergies will be vital for developing effective adjuvant therapies to combat multidrug-resistant infections.
Appendix
Table 4: Example Primer Sequences for qPCR Analysis of E. coli acrAB
| Gene | Primer Sequence (5' to 3') | Amplicon Size | Note |
|---|---|---|---|
| acrA | F: CGGTCTGCTGGAGTTCGTCR: TGCCAGCGAAACCATTGAG | ~150 bp | Example only; validate efficiency before use. |
| acrB | F: AACTGGTTGCCGCTCTACACR: CACCAGACGATGCCGAAATC | ~120 bp | Example only; validate efficiency before use. |
| rrsE (16S) | F: GGAGTAAAGTTAATACCTTTGCTCR: TGCAGGCTCAACCTTATACT | ~100 bp | Common reference gene for normalization [43]. |
Efflux pumps are membrane transporter proteins that actively extrude toxic compounds, including antibiotics, from bacterial cells and are a major component of intrinsic and acquired multidrug resistance [16]. In clinical pathogens such as Mycobacterium abscessus, Pseudomonas aeruginosa, and Escherichia coli, these pumps contribute significantly to broad-spectrum antibiotic resistance, reducing treatment efficacy for infections [4] [45] [46]. The intrinsic resistance mediated by efflux is particularly challenging as it often precedes and facilitates the development of higher-level, acquired resistance. Inhibiting these pumps is a promising strategy to reverse resistance and restore the efficacy of existing antibiotics [47] [45]. High-throughput screening (HTS) technologies have become indispensable in the effort to systematically identify efflux pump substrates and inhibitors, accelerating the discovery of novel therapeutic agents and resistance-reversal adjuvants.
Core High-Throughput Screening Platforms
High-throughput screening for efflux pump activity employs various platforms, each with unique strengths for different applications. The table below summarizes the core HTS platforms used in the field.
Table 1: Core High-Throughput Screening Platforms for Efflux Studies
| Platform | Key Principle | Measured Output | Key Advantages | Example Applications |
|---|---|---|---|---|
| Functional Flow Cytometry [47] | Measures accumulation/retention of fluorescent dye substrates in cells. | Fluorescence intensity of cells, indicating efflux pump activity. | Multiparametric, single-cell resolution, amenable to substrate multiplexing. | Identification of inhibitors in mammalian and microbial efflux systems; Side Population (stem cell) assays [47]. |
| Quantitative HTS (qHTS) [48] | Tests compounds across a range of concentrations in a single, miniaturized experiment. | Concentration-response curves; parameters like AC50 (potency) and Emax (efficacy). | Generates rich data for potency ranking, lowers false-positive/negative rates. | Large-scale chemical library screening for lead candidates in drug discovery and toxicity testing [48]. |
| Multiplexed Phenotype Microarrays [49] | Heterologous expression of efflux pumps followed by high-throughput growth profiling under antimicrobial stress. | Bacterial growth under hundreds of antimicrobial conditions. | Rapid, economical, simultaneous phenotypic testing against many conditions. | Identifying drug resistance phenotypes for putative efflux pumps in A. baumannii [49]. |
| In Silico Virtual Screening [45] | Computational docking of compound libraries into 3D structures of efflux pump proteins. | Docking scores, binding affinities, and predicted binding modes. | Fast, cost-effective; can pre-filter compounds for experimental testing; uses pharmacophore models. | Identification of natural compound inhibitors (e.g., lanatoside C, diadzein) for MexB and AcrB pumps [45]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) [4] | Direct measurement of antibiotic accumulation inside bacterial cells. | Absolute or relative intracellular concentration of antibiotics. | Direct, label-free quantitation; not reliant on fluorescent properties of substrates. | Comparative analysis of antibiotic uptake in M. abscessus; identified linezolid as the least accumulated antibiotic [4]. |
Experimental Protocols for Key Assays
Functional Efflux Assay Using Flow Cytometry
This protocol measures the ability of a transporter to move fluorescent substrates against a concentration gradient, allowing for the identification of inhibitors.
- Principle: Cells are loaded with a lipophilic, non-fluorescent dye (e.g., calcein-AM, rhodamine). Upon entering the cell, intracellular esterases cleave the AM ester group, converting it to a fluorescent, charged molecule (e.g., calcein) that is trapped inside. Active efflux pumps reduce intracellular fluorescence by exporting the substrate. An active Efflux Pump Inhibitor (EPI) blocks this export, leading to dye accumulation and increased fluorescence [47] [50].
- Protocol Steps:
- Cell Preparation: Use either efflux pump-overexpressing cell lines (e.g., KB-V1 for human ABCB1) or bacterial strains. Include a pump-deficient strain as a control [50].
- Dye Loading (Accumulation Assay): Incubate cells with the fluorescent substrate (e.g., 0.1-1 µM Calcein-AM) in the presence or absence of the test compound (potential inhibitor).
- Incubation: Allow the reaction to proceed for a defined period (e.g., 30-60 minutes) at 37°C. The assay requires no washing steps, as the readout is the fluorescence from hydrolyzed calcein retained within the cells [50].
- Detection: Analyze samples using a high-throughput flow cytometer or a fluorescent imaging system. The fluorescence intensity of the cell population is directly proportional to efflux pump inhibition [47] [50].
- Data Analysis: Calculate the fold-increase in fluorescence relative to the untreated control (pump-active cells). A dose-dependent increase in fluorescence confirms EPI activity.
Checkerboard Synergy Assay for EPI Validation
This assay validates the ability of an identified EPI to potentiate the activity of a conventional antibiotic.
- Principle: The assay tests the combined effect of an EPI and an antibiotic in a two-dimensional, serial dilution scheme. A synergistic effect is confirmed if the combination lowers the Minimum Inhibitory Concentration (MIC) of the antibiotic beyond an additive effect [45].
- Protocol Steps:
- Plate Setup: In a 96-well microtiter plate, serially dilute the antibiotic along the rows and the EPI along the columns.
- Inoculation: Add a standardized bacterial inoculum (e.g., 5 x 10^5 CFU/mL) to each well.
- Incubation: Incubate the plate at the appropriate temperature for 16-24 hours.
- Analysis: Determine the MIC of the antibiotic alone and in combination with various concentrations of the EPI. The Fractional Inhibitory Concentration (FIC) index is calculated as (MIC of antibiotic in combination/MIC of antibiotic alone) + (MIC of EPI in combination/MIC of EPI alone). An FIC index of ≤0.5 is generally considered synergistic [45].
Ethidium Bromide Accumulation Assay
This fluorescence-based assay directly visualizes efflux inhibition by measuring the intracellular accumulation of ethidium bromide (EtBr).
- Principle: EtBr is a substrate for many bacterial efflux pumps. In the absence of an EPI, it is efficiently extruded. When an EPI is present, EtBr accumulates in the cell, intercalates into DNA, and exhibits enhanced fluorescence.
- Protocol Steps:
- Cell Handling: Bacterial cells are harvested, washed, and resuspended in an appropriate buffer.
- Loading: EtBr and the test EPI are added to the cell suspension.
- Monitoring: Fluorescence is measured over time (e.g., every 5-10 minutes for 60 minutes) using a plate reader (excitation ~530 nm, emission ~585 nm). An increase in fluorescence over time indicates inhibition of efflux activity [45].
Diagram 1: Functional efflux assay workflow for inhibitor identification.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful HTS campaigns for efflux substrates and inhibitors rely on a suite of specialized reagents and tools.
Table 2: Essential Research Reagents for Efflux Studies
| Reagent / Tool | Function in Efflux Research | Specific Examples & Notes |
|---|---|---|
| Fluorescent Substrate Dyes | Serve as reporter molecules for efflux pump activity; their intracellular accumulation is inversely proportional to pump activity. | Rhodamine 123, Calcein-AM [47], Hoechst 33342 (for Side Population assays) [47], Ethidium Bromide [45] [16], Red Orange [47], eFluxx-ID Dyes (specific for mammalian ABC transporters) [47]. |
| Validated Efflux Pump Inhibitors (EPIs) | Used as positive controls in experimental assays to validate the efflux system and the assay's functionality. | Verapamil (1st gen, mammalian) [47] [50], Cyclosporin A [50], Tariquidar (XR9576, 3rd gen, mammalian) [47] [50], PAβN (MC-207,110, for Gram-negative bacteria) [45], CCCP (uncoupler, de-energizes pumps) [45]. |
| Engineered Cell Lines | Provide a controlled system with high efflux pump expression and minimized background signals. | KB-V1 (human cervical carcinoma, overexpresses ABCB1) [50], MDCKII-LE (low efflux Madin-Darby canine kidney cells) [47], Strains lacking or overexpressing specific efflux pumps (e.g., ΔmexEF-oprN P. aeruginosa) [46]. |
| Computational Chemistry Tools | Enable in silico prediction of efflux pump interactions through docking and pharmacophore modeling, filtering large compound libraries before wet-lab testing. | Molecular docking software (e.g., Glide for XP docking); Pharmacophore models based on known efflux substrates (e.g., AADHR, AAHNR) to exclude substrate-like compounds [45]. |
Advanced Screening Strategies and Data Analysis
Quantitative HTS (qHTS) and the Hill Equation
qHTS represents a significant advancement over single-concentration screening by profiling thousands of chemicals across multiple concentrations. The data are typically fitted to the Hill equation (HEQN) to derive pharmacological parameters [48]:
( Ri = E0 + \frac{(E{\infty} - E0)}{1 + \exp{-h[\log Ci - \log AC{50}]}} )
Where ( Ri ) is the response at concentration ( Ci ), ( E0 ) is the baseline response, ( E{\infty} ) is the maximal response, ( h ) is the Hill slope, and ( AC_{50} ) is the concentration producing a half-maximal response. While powerful, parameter estimation from the HEQN can be highly variable if the concentration range does not adequately define the upper and lower asymptotes of the response curve, leading to unreliable potency rankings [48]. Therefore, careful experimental design and data interpretation are critical.
Transposon Mutagenesis Screening for Resistance Mechanisms
This genetic approach identifies genes involved in intrinsic resistance, including those affecting membrane permeability and efflux. In M. abscessus, a transposon mutagenesis screen under linezolid pressure identified multiple transporters that confer resistance, highlighting the combined role of the cell wall barrier and active efflux in intrinsic drug resistance [4]. This method provides a direct, functional link between specific genes and the efflux-mediated resistance phenotype.
Diagram 2: Genetic screening workflow for identifying efflux and permeability genes.
High-throughput screening technologies have profoundly advanced our ability to dissect the mechanisms of efflux-mediated intrinsic resistance. The integration of functional assays like HTS flow cytometry, genetic screens, and direct chemical measurement via LC-MS provides a multi-faceted toolkit for researchers [47] [4]. The future of this field lies in further refining these technologies—for instance, by improving the reliability of qHTS data analysis and developing more predictive in silico models. Furthermore, the successful identification of natural compound inhibitors like lanatoside C and diadzein underscores the potential of combining computational and experimental HTS approaches to discover novel, clinically applicable Efflux Pump Inhibitors [45] [16]. As these screening strategies continue to evolve, they will play an increasingly vital role in overcoming multidrug resistance and extending the therapeutic life of existing antibiotics.
The global health crisis of antimicrobial resistance (AMR) is driven in part by the ability of pathogenic bacteria to expel a broad spectrum of antibiotics via multidrug efflux pumps [15]. Among these, Resistance-Nodulation-Division (RND) superfamily transporters are particularly effective in mediating multidrug resistance in Gram-negative bacteria [51] [52]. Structural biology has been instrumental in deciphering the molecular mechanisms of these efflux pumps, providing the foundational knowledge required to develop novel therapeutic strategies. This whitepaper details how two pivotal structural biology techniques—X-ray crystallography and cryo-electron microscopy (cryo-EM)—are employed to elucidate the architectures and functional dynamics of RND efflux pumps, thereby informing drug discovery efforts aimed at overcoming intrinsic and acquired antibiotic resistance.
Tools for Structural Elucidation of Efflux Pumps
X-ray Crystallography
X-ray crystallography has historically been the primary method for determining the high-resolution structures of membrane proteins, including RND efflux pumps. This technique involves purifying and crystallizing the protein of interest, then analyzing the diffraction patterns generated when an X-ray beam passes through the crystal [51] [53].
- Key Insights: The first crystal structure of an RND transporter, E. coli AcrB, was solved in 2002, revealing a homotrimeric assembly and providing the initial structural blueprint for this protein family [51] [53]. Subsequent crystallographic studies have captured these pumps in different conformational states (loose, tight, open), leading to the proposal of the "functional rotation" mechanism where each monomer of the trimer cycles through different states to propel substrates out of the cell [53].
- Limitations and Advances: A significant challenge has been producing high-quality crystals of membrane proteins in their functional state. The process often requires detergent-based extraction from the native lipid membrane, which can destabilize the protein or impede crystallization [51]. To overcome this, researchers have developed lipid bilayer mimetics such as lipid cubic phase and nanodiscs, which help maintain proteins in a more native-like environment [51].
Cryo-Electron Microscopy (cryo-EM)
The emergence of single-particle cryo-EM has revolutionized membrane protein structural biology. This technique involves flash-freezing a purified protein sample in vitreous ice and using an electron microscope to collect images of individual particles, which are then computationally reconstructed into a 3D model [51].
- Advantages for Efflux Pump Studies: Cryo-EM is particularly powerful for studying large, multi-protein complexes that are difficult to crystallize. It does not require crystals and is better suited for capturing multiple conformational and assembly states from a single, heterogeneous sample [51]. This has enabled the determination of structures of full tripartite efflux complexes (comprising inner membrane RND transporters, periplasmic adaptor proteins, and outer membrane channels) in near-native conditions [51] [54].
- Recent Breakthroughs: For example, the 2025 cryo-EM structure of P. aeruginosa MexY, an RND pump conferring aminoglycoside resistance, was resolved to 3.63 Å. This structure revealed an asymmetric trimer with protomers in "binding," "resting," and "extrusion" states, providing a dynamic snapshot of the transport cycle and identifying key residues for substrate specificity [54].
Comparative Analysis of Structural Techniques
The table below summarizes the core attributes, strengths, and limitations of X-ray crystallography and cryo-EM in the context of efflux pump research.
Table 1: Comparative Analysis of X-ray Crystallography and Cryo-EM for Efflux Pump Studies
| Feature | X-ray Crystallography | Cryo-Electron Microscopy |
|---|---|---|
| Specimen State | Static crystal lattice | Proteins in vitreous ice (near-native state) |
| Sample Requirement | High purity and concentration for crystal formation | Lower concentration, high purity still critical |
| Resolution Range | Atomic to near-atomic (traditionally higher) | Near-atomic to atomic (now routinely achievable) |
| Ideal Application | Determining high-resolution static structures; studying small molecule binding | Analyzing large, flexible complexes; capturing multiple conformational states |
| Key Limitation | Difficulties with membrane protein crystallization; potential for structural artifacts | Requires significant computational resources; particle heterogeneity challenges |
| Notable Efflux Pump Structures | AcrB (2002), MexB (2009), CusA (2010) [51] [53] | AdeB (2019), MtrD (2020), MexY (2025) [51] [54] |
Experimental Workflows in Efflux Pump Research
The following diagrams outline generalized protocols for determining efflux pump structures using crystallography and cryo-EM, highlighting key decision points and methodologies.
Workflow for X-ray Crystallography of Membrane Proteins
Workflow for Single-Particle Cryo-EM Analysis
Case Studies: Mechanism Elucidation
Substrate Binding and Transport in RND Pumps
Structural studies have revealed that RND transporters like AcrB and MexB possess large, multifunctional binding pockets. A 2019 crystallography study of P. aeruginosa MexB demonstrated that the detergent lauryl maltose neopentyl glycol (LMNG), despite its high molecular mass, binds to the distal binding pocket [53]. One of its alkyl chains inserts into a hydrophobic pit, a site known to bind pyridopyrimidine-based efflux pump inhibitors (EPIs). Functional assays confirmed LMNG is both a substrate and a competitive inhibitor of the MexAB-OprM system, illustrating how structural data can identify specific, targetable binding regions [53].
Aminoglycoside Recognition by MexY
The recent cryo-EM structure of P. aeruginosa MexY revealed the molecular basis for its role in aminoglycoside resistance [54]. The structure shows that the periplasmic binding cavity is lined with anionic residues (e.g., E129, D133, E175) and aromatic residues (e.g., Y127, Y613), suggesting a preference for binding positively charged drugs like aminoglycosides. Mutations at D133 and Y613 were previously shown to compromise resistance, and the structure confirms their critical location within the binding site. This provides a direct link between atomic-level architecture and physiological function, guiding the design of novel EPIs or antibiotic modifications to evade efflux [54].
Essential Research Reagent Solutions
Successful structural studies of efflux pumps rely on specialized reagents and tools. The following table catalogues key materials used in this field.
Table 2: Key Research Reagent Solutions for Efflux Pump Structural Biology
| Reagent / Material | Function and Application | Specific Examples / Notes |
|---|---|---|
| Detergents | Solubilize membrane proteins from lipid bilayers for purification and crystallization. | DDM, LMNG; LMNG was used to solve the MexB structure and was identified as a substrate [53]. |
| Lipid Bilayer Mimetics | Provide a native-like lipid environment for membrane proteins, stabilizing native conformations. | Bicelles, Lipid Cubic Phase (LCP), Nanodiscs (e.g., MSP-based), Styrene Maleic Acid Lipid Particles (SMALPs) [51]. |
| Efflux Pump Inhibitors (EPIs) | Used in co-structural studies to identify binding sites and mechanisms of inhibition for drug development. | Pyridopyrimidine derivatives (e.g., ABI-PP) bind a hydrophobic pit in AcrB/MexB [53]. |
| Expression Systems | Produce high yields of recombinant efflux pump proteins for structural studies. | E. coli, insect cell (e.g., Baculovirus), mammalian cell systems. |
| Cryo-EM Grids | Support the thin layer of vitrified ice containing the protein sample for EM imaging. | UltrAuFoil, Quantifoil grids; surface properties are critical for optimal ice thickness and particle distribution. |
X-ray crystallography and cryo-EM are complementary and powerful techniques that have profoundly advanced our understanding of multidrug efflux pumps. Crystallography provides ultra-high-resolution snapshots, while cryo-EM offers the ability to visualize dynamic complexes and multiple conformational states in a near-native environment. The structural insights gained from these methods—into substrate specificity, transport mechanisms, and inhibition—are invaluable for combating antibiotic resistance. They provide a rational path forward for the development of efflux pump inhibitors, which can rejuvenate the efficacy of existing antibiotics and safeguard our future against multidrug-resistant bacterial infections.
Intrinsic antibiotic resistance, the innate ability of a bacterium to resist classes of antibiotics, presents a significant challenge in treating bacterial infections. A primary driver of this phenotype is the activity of efflux pumps—membrane transporters that actively expel a wide range of toxic compounds, including antibiotics, from the bacterial cell [8]. In pathogens like Mycobacterium abscessus, this mechanism, coupled with a highly impermeable cell wall, contributes to broad-spectrum resistance, reducing treatment success rates to as low as 30-50% despite aggressive therapy [4]. Similarly, in Gram-negative bacteria such as Pseudomonas aeruginosa and members of the ESKAPEE group, efflux pumps are a first-line defense, reducing intracellular antibiotic concentration and facilitating the acquisition of additional, higher-level resistance mechanisms [8] [55].
Understanding and predicting which compounds are susceptible to efflux is therefore critical for antibiotic discovery and development. Machine learning (ML) has emerged as a powerful, cost-effective technology to address this challenge. By learning from known chemical-efflux interactions, ML models can predict the efflux potential of novel compounds based solely on their chemical structures, providing invaluable insights early in the drug development pipeline [56].
Machine Learning Workflows for Efflux Prediction
The development of a robust ML model for predicting efflux susceptibility follows a structured pipeline, from data curation to model deployment. The overall workflow integrates multiple steps to ensure predictive accuracy and biological relevance.
Data Acquisition and Curation
The foundation of any effective ML model is a large, high-quality dataset. Recent studies have undertaken the manual curation of over 24,000 bioactivity records from public databases such as ChEMBL, PubChem, and Metrabase [56]. This process involves:
- Data Retrieval: Using programming libraries (e.g.,
chembl-webresource-clientin Python) to systematically extract bioactivity data for key efflux transporters like P-glycoprotein (P-gp), BCRP, MRP1, and MRP2 [56]. - Labeling and Harmonization: Each experimental record is manually reviewed and classified based on conservative thresholds. For example, a compound with a reported half-maximal inhibitory concentration (IC₅₀) of ≤ 10 µM might be labeled as an "inhibitor" (class 1), while one with an IC₅₀ > 10 µM would be a "non-inhibitor" (class 0) [56]. In case of conflicting data for a single chemical, a majority vote is used to assign the final label.
- Chemical Standardization: The structures of curated compounds are standardized using tools like CASE Ultra or Open Babel to ensure consistency in subsequent descriptor calculation [56].
Table 1: Public Data Sources for Efflux Transporter Bioactivities
| Database | Description | Key Feature |
|---|---|---|
| ChEMBL | Manually curated repository of bioactive molecules | Contains literature-sourced bioactivity data and assay details [56] |
| PubChem | Largest publicly available chemical database | Provides bioassay data for over 100 million chemicals [56] |
| Metrabase | Transporter-specific database | Focuses on substrate and inhibitor data for transporters [56] |
| DrugBank | Comprehensive drug and target database | Offers ADME profiles and known transporter interactions for drugs [56] |
Molecular Descriptor Calculation and Feature Generation
A molecule's structure is converted into a numerical representation that an ML algorithm can process. The PaDEL-Descriptor software is widely used for this purpose, capable of calculating 797 molecular descriptors and 10 types of fingerprints from a compound's Simplified Molecular-Input Line-Entry System (SMILES) notation [57]. These descriptors capture essential chemical properties that influence efflux, such as:
- Physicochemical Properties: Molecular weight, logP (lipophilicity), topological polar surface area.
- Electronic Properties: Partial charges, electronegativity.
- Structural Fingerprints: Binary vectors indicating the presence or absence of specific substructures or functional groups.
Model Training and Validation
With features and labels prepared, the next step is model training. A combination of multiple ML algorithms and descriptor sets is often employed to identify the best-performing model [56].
- Algorithms: Commonly used algorithms include Random Forest (RF), eXtreme Gradient Boosting (XGBoost), Support Vector Machines (SVM), and Deep Neural Networks (DNN) [58] [57].
- Validation: Model performance is rigorously evaluated using 5-fold cross-validation, which assesses the model's ability to generalize to unseen data [56] [57]. Performance is measured using metrics such as:
- Accuracy: The proportion of correct predictions.
- Concordance Index (C-index): The probability that two randomly chosen predictions are ranked correctly.
- Matthews Correlation Coefficient (MCC): A balanced measure of prediction quality, especially useful for imbalanced datasets.
The resulting models have demonstrated excellent predictive capability, with one study reporting an average correct classification rate (CCR) of 0.839 for inhibition models [56].
Experimental Protocols for Model Training and Validation
Protocol 1: Building a Quantitative Structure-Activity Relationship (QSAR) Model
This protocol outlines the steps for developing a classifier to predict if a compound is an efflux pump substrate [56].
- Define the Biological Endpoint: Clearly specify the efflux-related activity to be predicted (e.g., "P-gp substrate," "BCRP inhibitor").
- Compile and Curate Training Data: Assemble a dataset of compounds with known efflux activity from ChEMBL and PubChem. Apply consistent thresholds to label compounds as substrates/inhibitors (1) or non-substrates/non-inhibitors (0).
- Generate Molecular Descriptors: For each compound in the curated set, compute chemical descriptors and fingerprints using software like PaDEL-Descriptor [57].
- Train Multiple ML Models: Using the labeled data and computed descriptors, train multiple classifier algorithms (e.g., RF, SVM, XGBoost). Utilize a 5-fold cross-validation approach to tune model hyperparameters and prevent overfitting.
- Evaluate Model Performance: Assess the final model on a held-out test set. Compare key metrics (Accuracy, MCC, AUC) against a baseline "random" model to ensure the model has learned meaningful signal from the data [59].
Protocol 2: Validating Model Predictions with Experimental Data
Predictions from in silico models must be validated with experimental evidence. The following protocol describes a standard mass spectrometry-based accumulation assay [4].
- Bacterial Culture: Grow the bacterial strain of interest (e.g., M. abscessus ATCC19977) to mid-log phase in appropriate culture medium.
- Antibiotic Exposure: Incubate the bacterial cells with the antibiotic of interest for a defined period (e.g., 4 hours).
- Cell Washing and Lysis: Pellet the bacterial cells and wash thoroughly with buffer to remove any antibiotic adsorbed to the cell surface. Lyse the cells to release intracellular contents.
- Sample Analysis: Quantify the intracellular antibiotic concentration using Liquid Chromatography-Mass Spectrometry (LC-MS).
- Data Interpretation: Calculate relative antibiotic accumulation. A low accumulation ratio suggests the compound is either poorly imported or actively effluxed. Genetic knockout strains (e.g., efflux pump mutants) can be used to confirm the role of specific transporters [4].
Table 2: Key Reagents and Resources for Efflux Research
| Category / Reagent | Function / Description | Example Sources/Tools |
|---|---|---|
| Chemical Databases | Provide bioactivity data for model training | ChEMBL, PubChem, Metrabase, DrugBank [56] |
| Descriptor Software | Calculates numerical features from chemical structures | PaDEL-Descriptor, Chemistry Development Kit (CDK) [57] |
| ML Algorithms | Trains predictive models from features and labels | Random Forest, XGBoost, Support Vector Machines [58] [57] |
| Model Validation | Assesses model performance and generalizability | 5-fold cross-validation, external test sets [56] [59] |
| Experimental Validation | ||
| ┣ Liquid Chromatography-Mass Spectrometry (LC-MS) | Quantifies intracellular antibiotic accumulation [4] | |
| ┣ Transposon Mutagenesis | Identifies efflux-related genes through genetic screening [4] | |
| ┗ Efflux Pump Inhibitors (EPIs) | Confirms efflux activity by blocking pump function [8] [55] |
Applications and Integration into the Drug Development Pipeline
The primary application of these ML models is to forecast the efflux potential of new chemical entities early in the drug discovery process. This allows medicinal chemists to prioritize compounds less likely to be extruded by major efflux pumps, thereby increasing the chance of achieving effective intracellular concentrations.
Furthermore, these predictions can be integrated into more complex pharmacokinetic (PK) models. For instance, compounds predicted to be substrates of P-gp and BCRP were twice as likely to have low brain exposure, a critical factor in treating central nervous system infections [56]. This demonstrates how transporter models can estimate a drug's ability to penetrate protected tissues, a key aspect of its overall PK profile.
Future Directions and Challenges
While ML models for efflux prediction show great promise, several challenges remain. The structural heterogeneity and broad substrate specificity of efflux pumps like AcrB make complete mechanistic modeling difficult [8]. Future efforts will focus on:
- Developing Interpretable ML Models: Moving beyond "black box" predictions to models that provide insights into which structural features confer susceptibility to efflux, thereby directly guiding chemical optimization [58].
- Expanding to Additional Transporters: Building comprehensive models for other clinically relevant efflux pumps from the RND, MFS, and ABC families [4] [8].
- Incorporating Advanced Modeling Techniques: Integrating molecular dynamics simulations to understand the atomic-level interactions between compounds and efflux pumps, which could further refine predictive models [57].
Overcoming these barriers is essential for the rational development of less efflux-prone antibiotics or effective efflux pump inhibitors, ultimately helping to combat the global crisis of antimicrobial resistance.
Overcoming the Efflux Barrier: Strategies for Inhibitor Development and Compound Optimization
Bacterial multidrug efflux pumps are transmembrane transporter proteins that actively export a wide range of structurally diverse toxic compounds, including antibiotics, from the bacterial cell [60]. This extrusion mechanism significantly reduces intracellular antibiotic concentration, thereby lowering drug efficacy and contributing substantially to the intrinsic antibiotic resistance observed in many pathogenic bacteria [61] [62]. The expression of efflux pumps is a fundamental component of the bacterial arsenal, allowing pathogens to survive in hostile environments, including those containing antimicrobial agents [5].
Efflux pumps predate clinical antibiotic use and serve crucial physiological functions in bacterial cells. These functions include regulating nutrient and heavy metal levels, relieving cellular stress, extruding toxins and metabolites, participating in bacterial virulence, facilitating biofilm formation, and enabling interbacterial communication [5] [16] [8]. For instance, in Salmonella, efflux pumps contribute significantly to pathogenicity in mouse infection models, with the MacAB system playing a key role in this process [61]. The constitutive expression of these pumps, combined with low membrane permeability, provides a baseline level of intrinsic resistance that allows bacteria to survive initial antibiotic exposure [5] [62]. This survival advantage creates a window for the development of higher-level resistance through additional mechanisms such as target mutations or enzymatic inactivation.
The World Health Organization (WHO) has identified multidrug resistance (MDR) as a major threat to public health, with efflux-mediated resistance playing an increasingly recognized role in treatment failures [63] [62]. As the pipeline for novel antibiotics dwindles, targeting efflux pumps presents a promising strategy to rejuvenate existing antibiotics and combat the rising tide of antimicrobial resistance.
Efflux Pump Families and Their Mechanisms of Action
Classification of Efflux Pump Families
Bacterial efflux pumps are classified into several major families based on their structure, energy source, and mechanism of action. The table below summarizes the key characteristics of these families.
Table 1: Major Families of Bacterial Efflux Pumps
| Family | Energy Source | Structural Features | Examples | Clinical Significance |
|---|---|---|---|---|
| RND (Resistance-Nodulation-Division) | Proton Motive Force | Tripartite complex: Inner membrane RND protein, Periplasmic Adapter Protein (PAP), Outer Membrane Protein (OMP) | AcrAB-TolC (E. coli), MexAB-OprM (P. aeruginosa), AdeABC (A. baumannii) | Most clinically significant in Gram-negative bacteria; broad substrate range [5] [60] [8] |
| MFS (Major Facilitator Superfamily) | Proton Motive Force | Typically 12 or 14 transmembrane segments; single-component transporters | NorA (S. aureus), EmrB (E. coli) | Predominant in Gram-positive bacteria [63] [61] |
| ABC (ATP-Binding Cassette) | ATP Hydrolysis | Two nucleotide-binding domains and two transmembrane domains | MacAB-TolC (E. coli, Salmonella) | Less common in antibiotic resistance; specific substrates like macrolides [5] [8] |
| MATE (Multidrug and Toxic Compound Extrusion) | Proton or Sodium Ion Gradient | Typically 12 transmembrane segments | NorM (V. parahaemolyticus) | Extrudes cationic drugs [61] [8] |
| SMR (Small Multidrug Resistance) | Proton Motive Force | Small size; 4 transmembrane segments | EmrE (E. coli) | Extrudes small, cationic compounds [61] [8] |
| PACE (Proteobacterial Antimicrobial Compound Efflux) | Proton Motive Force | 4 transmembrane segments; recently characterized | AceI (A. baumannii) | Involved in biocide resistance [60] [8] |
Molecular Mechanisms of Substrate Extrusion
The RND family efflux pumps, particularly in Gram-negative bacteria, represent the most sophisticated and clinically significant extrusion systems. These tripartite complexes form continuous conduits that span both the inner and outer membranes, enabling direct export of substrates from the cell interior or periplasm to the external environment [5] [8].
The prototypical RND pump AcrB in E. coli operates through a sophisticated functional rotating mechanism. Each AcrB trimer protomer cycles through three distinct conformational states:
- Loose (L) state: The protomer binds substrate from the periplasm or inner membrane.
- Tight (T) state: The substrate is trapped within the binding pocket.
- Open (O) state: The substrate is expelled into the external channel toward TolC [8] [62].
This asymmetric trimer structure creates a peristaltic pump action that efficiently moves substrates outward. Substrate recognition flexibility in AcrB stems from multiple substrate entry pathways and two large binding pockets in the porter domain: the proximal binding pocket (PBP) and the distal binding pocket (DBP), separated by the Phe-617 "switch loop" that controls substrate passage between pockets [8].
The pump utilizes the proton motive force for energy, functioning as a proton antiporter that exchanges one hydrogen ion for one molecule of substrate [5]. Some evidence suggests that certain RND pumps can directly efflux substrates from the cytoplasm, challenging the traditional view that they only transport compounds from the periplasm [5].
Figure 1: Tripartite RND Efflux Pump Mechanism. The diagram illustrates the assembly of RND efflux pumps across Gram-negative bacterial membranes and the functional rotating mechanism for antibiotic extrusion.
Current Landscape of Efflux Pump Inhibitors
Mechanisms of Efflux Inhibition
Efflux Pump Inhibitors (EPIs) are molecules that block the activity of efflux pumps through various mechanisms, potentially restoring susceptibility to antibiotics. The primary mechanisms of efflux inhibition include:
Competitive and Allosteric Inhibition: Direct binding to the substrate binding sites of the efflux pump, preventing antibiotics from being recognized and transported [63] [8]. This approach includes molecules that bind to the proximal or distal binding pockets of RND transporters like AcrB.
Energy Dissipation: Disruption of the energy source required for efflux activity. For instance, carbonyl cyanide-m-chlorophenylhydrazone (CCCP) collapses the proton motive force that powers secondary transporters [63] [8].
Inhibition of Pump Assembly: Interference with the proper assembly of the tripartite complex components, preventing formation of functional efflux conduits [63].
Genetic Regulation Interference: Downregulation of efflux pump gene expression by targeting regulatory pathways [63] [16].
Classes of EPIs and Developmental Status
Despite decades of research, no EPI has reached clinical approval, highlighting the significant challenges in their development. The following table summarizes prominent EPI classes and their current status.
Table 2: Classes of Efflux Pump Inhibitors and Their Status
| EPI Class/Compound | Source | Target Pumps | Mechanism of Action | Current Status |
|---|---|---|---|---|
| PAβN (MC-207,110) | Synthetic | RND pumps (P. aeruginosa) | Competitive inhibition; de-energizes pump | First discovered (2001); preclinical; toxicity issues [63] [8] |
| ABI-PP | Synthetic pyridopyrimidine | AcrAB/MexAB (RND) | Specific inhibitor of AcrB/MexB | Preclinical; limited by pump redundancy [60] [62] |
| CCCP | Synthetic | Proton-dependent pumps | Protonophore collapses proton motive force | Laboratory use only; toxic for therapeutic use [63] [8] |
| Verapamil | FDA-approved (cardiac) | MATE pumps | Inhibition of efflux activity | Repurposing candidate; drug interaction problems [60] |
| Plant-derived Compounds (e.g., lanatoside C, daidzein) | Natural | Various efflux pumps | Multiple mechanisms including competitive inhibition | Early research; shows dual EPI and anti-biofilm activity [16] |
| Microbe-derived EPIs | Natural | RND pumps | Restores antibiotic susceptibility | Early discovery phase; limited characterization [60] |
Pharmacological and Development Challenges
The transition from promising EPI candidates to clinically viable therapeutics faces substantial pharmacological and development hurdles that have prevented any EPI from reaching clinical use despite decades of research [63] [60].
Biological and Toxicity Challenges
Pump Redundancy and Broad Substrate Recognition: Bacteria typically express multiple types of efflux pumps capable of extruding antibiotics. Inhibiting a single pump type is often insufficient to reverse resistance, as complementary pumps maintain extrusion capacity. For example, the EPI ABI-PP inhibits MexB but not MexY efflux pumps in P. aeruginosa, both of which contribute significantly to drug resistance in this pathogen [60].
Off-Target Toxicity: Due to the structural and functional conservation of efflux pumps across biological systems, less specific EPIs may inhibit eukaryotic efflux pumps such as P-glycoprotein (MDR1), leading to unacceptable toxicity profiles. This cross-reactivity presents a significant barrier to developing safe, broad-spectrum EPIs [63] [60].
Physiological Roles of Efflux Pumps: Efflux pumps have natural functions in bacterial physiology, including intercellular signaling, virulence, and stress response. Inhibition may disrupt these processes unpredictably or select for compensatory mutations [61] [46]. Recent research on P. aeruginosa reveals that inactivation of the mexEFoprN efflux pump unexpectedly increases virulence through enhanced quorum sensing, demonstrating the complex relationship between efflux function and pathogenicity [46].
Pharmacokinetic and Development Barriers
Pharmacokinetic Mismatch: For effective combination therapy, EPIs and antibiotics must have similar pharmacokinetic profiles, including absorption, distribution, and elimination characteristics. Achieving this concordance is challenging and rarely addressed in early EPI discovery phases [60].
Drug-Drug Interactions: Some EPI candidates, particularly those repurposed from existing drugs like verapamil, demonstrate problematic interactions with antibiotics. For instance, clarithromycin interferes with verapamil metabolism, making concurrent administration potentially dangerous [60].
Regulatory and Economic Hurdles: As no EPI has previously gained regulatory approval, any new EPI would be considered a New Chemical Entity (NCE), requiring extensive safety and efficacy testing under stringent regulatory frameworks. The high development costs combined with uncertain returns have limited pharmaceutical company investment in this field [60].
Experimental Methods for EPI Research
Assessing Efflux Activity and Inhibition
Research on efflux pumps and their inhibitors relies on a combination of phenotypic, genotypic, and direct measurement approaches.
Table 3: Key Experimental Methods in Efflux Pump Research
| Method Category | Specific Techniques | Application | Key Reagents |
|---|---|---|---|
| Phenotypic Assays | MIC reduction assays with/without EPIs; Ethidium bromide accumulation assays; Fluorometric transport assays | Detection of efflux activity; Screening for EPI activity | CCCP; PAβN; Ethidium bromide; Fluorescent substrates [16] [8] |
| Genotypic Methods | RT-PCR; Microarray analysis; Transposon mutagenesis screening | Quantification of efflux pump gene expression; Identification of efflux-related genes | Primers for efflux pump genes; Transposon libraries [4] [16] |
| Direct Quantification | Liquid Chromatography-Mass Spectrometry (LC-MS); Accumulation assays | Direct measurement of intracellular antibiotic concentration | Antibiotic standards; Internal standards for LC-MS [4] [8] |
| Structural Approaches | X-ray crystallography; Cryo-electron microscopy; Molecular modeling | Elucidation of pump structures and inhibitor binding modes | Purified efflux pump components; Crystallization reagents [61] [8] |
The Researcher's Toolkit: Essential Reagents and Methods
Figure 2: Integrated Workflow for EPI Discovery and Characterization. The diagram outlines the multidisciplinary approach required for comprehensive efflux pump inhibitor research.
Standardized Experimental Protocols
Ethidium Bromide Accumulation Assay:
- Grow bacterial cultures to mid-logarithmic phase (OD600 ≈ 0.4-0.6)
- Harvest cells by centrifugation and wash with appropriate buffer
- Resuspend cells in buffer containing glucose as energy source
- Divide suspension into aliquots with and without EPI candidate
- Add ethidium bromide to all samples and monitor fluorescence over time
- Include CCCP as positive control for complete inhibition
- Calculate accumulation ratios comparing EPI-treated vs. untreated cells [16]
MIC Reduction Assay:
- Prepare serial dilutions of antibiotics in microtiter plates
- Add bacterial inoculum standardized to ~5×10^5 CFU/mL
- Include test wells with fixed concentration of EPI candidate
- Incubate at appropriate temperature for 16-20 hours
- Determine MIC with and without EPI
- A ≥4-fold reduction in MIC with EPI indicates significant inhibition [16] [8]
LC-MS Antibiotic Accumulation Measurement:
- Expose bacterial cultures to target antibiotic for defined period
- Rapidly separate cells from medium by filtration or centrifugation
- Wash cells to remove extracellular antibiotic
- Lyse cells and extract intracellular compounds
- Analyze extracts using LC-MS with appropriate calibration standards
- Normalize antibiotic concentration to cell number or protein content [4] [8]
Efflux pump inhibitors represent a promising therapeutic strategy to address the growing crisis of antimicrobial resistance, particularly by potentiating existing antibiotics against multidrug-resistant pathogens. However, the journey from concept to clinic has proven exceptionally challenging, with no EPI candidates having successfully navigated the path to clinical approval.
The future of EPI development will likely require:
- Multitarget Approaches: Developing EPIs that simultaneously inhibit multiple efflux pump systems to overcome redundancy [60] [8].
- Rational Design Leveraging Structural Insights: Utilizing the wealth of structural information from cryo-EM and crystallography to design more specific inhibitors with reduced off-target effects [61] [8].
- Pharmacokinetic Optimization: Early attention to concordant pharmacokinetic properties between EPIs and their companion antibiotics [60].
- Exploration of Alternative Strategies: Investigating approaches beyond direct inhibition, such as interference with efflux pump regulation or combination with other anti-resistance strategies [16] [46].
While significant challenges remain, the continued research into efflux pump inhibition reflects its crucial potential in overcoming antimicrobial resistance. As our understanding of efflux pump physiology and structure deepens, the prospect of clinically viable EPIs remains an important goal in the global effort to preserve antibiotic efficacy.
The escalating crisis of antimicrobial resistance represents one of the most significant threats to modern healthcare. Among the various resistance mechanisms employed by bacteria, active drug efflux stands as a major contributor to intrinsic and acquired multidrug resistance, particularly in Gram-negative pathogens. This technical guide explores the emerging paradigm of rational drug design focused on creating "efflux evader" molecules – antimicrobial agents structurally engineered to bypass recognition and extrusion by bacterial efflux pumps. By synthesizing recent advances in structural biology, computational analysis, and medicinal chemistry, this review provides a comprehensive framework for understanding the molecular principles of efflux avoidance, alongside practical experimental methodologies for identifying and validating such compounds. The strategies outlined herein offer a promising pathway to revitalize existing antibiotic classes and guide the development of novel agents capable of overcoming one of the most formidable barriers in antimicrobial therapy.
Efflux pumps are bacterial transport proteins that actively extrude toxic compounds, including antibiotics, from the cellular interior to the external environment [63]. These systems contribute significantly to intrinsic antibiotic resistance in bacteria, particularly in Gram-negative pathogens where they function as tripartite complexes spanning both inner and outer membranes [5] [14]. The physiological role of efflux pumps extends beyond antibiotic resistance to include vital functions such as regulating nutrient and heavy metal levels, relieving cellular stress, extruding toxins, facilitating bile tolerance for host colonization, and participating in quorum sensing and biofilm formation [5] [14].
In clinical settings, efflux pump-mediated resistance presents a critical challenge. Acinetobacter baumannii, one of the classic examples of multidrug-resistant pathogens, carries multiple efflux pump systems that allow it to exhibit multidrug-to-pan-drug resistance, placing it on the World Health Organization's priority list of pathogens requiring urgent antibiotic development [5]. Similarly, in Pseudomonas aeruginosa, mutations in efflux pump regulatory systems leading to pump overexpression are among the most common efflux-related mechanisms for drug resistance [14]. The Resistance-Nodulation-Division (RND) family of efflux pumps is particularly significant in Gram-negative bacteria, with demonstrated activity against newer beta-lactam antibiotics and beta-lactam/beta-lactamase inhibitor combinations [14].
The development of efflux evader molecules represents a paradigm shift from the traditional approach of discovering efflux pump inhibitors (EPIs). While EPIs aim to block pump function, often requiring co-administration with antibiotics, efflux evaders are designed to avoid recognition by these pumps altogether, potentially offering a more sustainable resistance-breaking strategy [64] [65].
Molecular Principles of Efflux Evasion
Quantitative Analysis of Structural Features
Large-scale computational analyses of compound libraries have revealed distinct structural and physicochemical properties that influence efflux susceptibility. A comprehensive study of 73,737 compounds from the publicly accessible CO-ADD database classified molecules based on their activity across three strains of Escherichia coli – wild-type, efflux-deficient tolC variant, and hyper-permeable lpxC variant [64]. This systematic approach identified key molecular features that promote efflux evasion.
Table 1: Physicochemical Properties Differentiating Efflux Substrates from Evaders
| Property | Efflux Substrates | Efflux Evaders | Analytical Method |
|---|---|---|---|
| Hydrophilicity (LogD) | Generally more hydrophobic | More hydrophilic (lower LogD) | Chromatographic measurement & computational calculation |
| Molecular Size/Weight | Tend to be larger | Generally smaller compounds preferred | Matched Molecular Pair Analysis (MMPA) |
| Resonant Structure Count | Higher | Lower | Computational descriptor analysis |
| Specific Chemical Groups | Varies by pump | Presence/absence of specific moieties | Structural-activity relationship studies |
| Charge Characteristics | Often neutral or anionic | Positively charged primary amines in some cases | Electrostatic potential mapping |
The classification scheme from this large-scale analysis identified 200 efflux evaders (compounds active against both wild-type and efflux-deficient E. coli) and 760 efflux substrates (compounds active only in the efflux-deficient strain) from the initial set of 73,737 compounds [64]. This dataset provides a robust foundation for understanding the structural modifications that convert substrates into evaders.
Chemical Modifications for Efflux Avoidance
Matched Molecular Pair Analysis (MMPA) has identified specific structural changes that repeatedly convert efflux substrates into evaders [64]:
Introduction of primary amine moieties: Positively charged primary amines have been shown to enhance entry into Gram-negative bacteria while potentially reducing efflux recognition [64].
Strategic reduction of hydrophobicity: Controlled decrease in LogD through introduction of polar groups can diminish interactions with hydrophobic binding pockets in efflux pumps [64].
Steric shielding of recognition elements: Adding strategically positioned bulky groups can mask structural features recognized by efflux pumps without compromising target engagement.
Structural rigidification: Reducing molecular flexibility through ring formation or conformational constraints can limit the ability of efflux pumps to accommodate the compound in their binding pockets.
The "efflux resistance breaker" (ERB) technology represents an applied example of these principles, where specific pharmacophores are incorporated into antibiotic scaffolds to reduce efflux liability [65]. Application of this technology to fluoroquinolones has resulted in compounds with notably better activity against multidrug-resistant bacteria, with up to a 512-fold reduction in MIC (MIC90 0.03 to 2 µg/mL) compared to parent compounds [65].
Experimental Methodologies for Evaluating Efflux Evasion
Strain-Based Screening Approaches
A robust method for identifying efflux evaders involves comparative screening across genetically modified bacterial strains with differential efflux capabilities [64]:
Diagram 1: Compound Classification Workflow
This comparative screening approach enables categorization of compounds based on their efflux susceptibility profiles. The workflow begins with parallel screening against wild-type and efflux-compromised bacterial strains, followed by systematic classification based on differential activity patterns.
Detailed Protocol:
- Bacterial Strains: Utilize isogenic pairs of wild-type and efflux-deficient strains (e.g., E. coli ATCC 25922 as wild-type and MB5747 as tolC variant) [64]
- Growth Inhibition Assay: Measure optical density (OD600) after treatment with compounds
- Activity Threshold: Classify as active if growth inhibition ≥ [μ + 4σ] above mean compound activity
- Classification Criteria:
- Efflux Evaders: Active against both wild-type and tolC strains
- Efflux Substrates: Active only in tolC strain but inactive in wild-type
- Generally Inactive: Inactive in both strains
- Permeability Assessment: Include lpxC hyperpermeable strain to differentiate efflux from permeability issues
Fluorescent-Based Efflux Assays
Flow cytometric assays using fluorescent probes provide a high-throughput method for evaluating efflux activity and inhibition [66] [67]:
Table 2: Research Reagent Solutions for Efflux Studies
| Reagent/Assay | Function/Application | Key Features | Experimental Considerations |
|---|---|---|---|
| JC-1 (T3168) | J-aggregate-forming lipophilic cation substrate for ABC transporters | Differential fluorescence emission based on membrane potential | Effective for ABCB1, ABCC1, and ABCG2 transporters; requires 488nm excitation |
| Calcein AM (C1430) | Non-fluorescent ester that becomes fluorescent after intracellular hydrolysis | Accumulation indicates efflux inhibition | Useful for high-throughput screening; compatible with flow cytometry |
| CO-ADD Database | Publicly accessible compound screening database | Contains growth inhibition data for 73,737 compounds across modified E. coli strains | Enables classification based on efflux susceptibility [64] |
| HyperCyt Platform | High-throughput flow cytometry system | Sequential sampling from 384-well plates at 40 samples/minute | Enables rapid screening of compound libraries [66] |
| Efflux Pump Inhibitors | Positive controls for efflux inhibition (e.g., CCCP, PAβN) | Collapse proton motive force or competitively inhibit transport | Verify assay functionality; CCCP is a protonophore that dissipates energy source [63] |
Detailed Protocol:
- Cell Preparation: Use transporter-overexpressing cell lines and their parental counterparts (e.g., CCRF-ADR5000 for ABCB1/P-gp) [66]
- Substrate Incubation: Serially dilute fluorescent substrates (1:3, 8 times) creating concentration ranges from 15 pM to 100 nM
- Inhibitor Testing: Include known efflux pump inhibitors as controls (e.g., verapamil, nicardipine)
- Flow Cytometric Analysis:
- Excitation: 488 nm and 635 nm lasers
- Detection: Multiple fluorescence channels (530/40, 575/25, 613/20, 680/30, 665/20, 750 LP filters)
- Sampling rate: 40 samples per minute using HyperCyt platform
- Data Analysis: Calculate efflux ratio based on fluorescence accumulation in presence vs. absence of inhibitors
Minimum Inhibitory Concentration (MIC) Profiling
The most direct assessment of efflux evasion capability involves comparing MIC values in wild-type versus efflux-deficient strains:
Standard Protocol:
- Broth Microdilution: Perform according to CLSI guidelines using cation-adjusted Mueller-Hinton broth
- Strain Panel: Include wild-type, efflux-deficient, and hyperpermeable strains
- Compound Dilution: Two-fold serial dilutions of test compounds across 96-well plates
- Inoculum Standardization: 5×10^5 CFU/mL final concentration
- Incubation: 35±2°C for 16-20 hours
- Efflux Ratio Calculation: MIC in wild-type / MIC in efflux-deficient strain
- Ratio <4: Limited efflux impact
- Ratio 4-8: Moderate efflux substrate
- Ratio >8: Strong efflux substrate
- Ratio ~1: Potential efflux evader
Structural Insights for Rational Design
RND Efflux Pump Architecture and Substrate Recognition
Structural studies of RND efflux pumps, particularly AcrB from E. coli, have revealed critical insights into substrate recognition principles that inform evader design [18]:
Asymmetric trimer organization: AcrB functions as a functional asymmetric trimer with each protomer adopting distinct conformational states – loose (L), tight (T), and open (O) – creating a peristaltic pump mechanism [18]
Multiple substrate binding pockets: Two primary binding pockets exist – the proximal binding pocket (PBP) in the L protomer and the distal binding pocket (DBP) in the T protomer – separated by the Phe-617 "switch loop" that controls substrate passage [18]
Diverse access pathways: Substrates reach binding pockets through four identified access channels (Ch1-Ch4) with distinct locations, conformational accessibility, and substrate preferences [18]
Broad substrate specificity: The drug binding cavity can be partitioned into an upper portion with mostly hydrophobic and aromatic interactions, and a lower space containing polar interactions, accounting for polyspecificity [66]
Computational Approaches for Evader Design
Structure-based drug design leveraging computational methods has emerged as a powerful tool for creating efflux evaders:
Molecular Dynamics Simulations: Model compound interactions with efflux pump binding pockets to identify unfavorable interactions that promote recognition
Machine Learning Classification: Utilize large-scale screening data to build predictive models of efflux susceptibility based on molecular descriptors [64]
Matched Molecular Pair Analysis: Identify specific structural transformations that consistently reduce efflux recognition while maintaining antibacterial activity [64]
Free Energy Perturbation Calculations: Precisely calculate binding free energies of compounds to efflux pumps to guide structural modifications
Case Studies and Clinical Applications
Efflux Resistance Breaker Technology
The application of efflux resistance breaker (ERB) technology to fluoroquinolones demonstrates the practical implementation of efflux evasion principles [65]:
Lead Compounds: KSN-L22 and BL-7 showed MICs of 0.03 to 0.5 µg/mL against MRSA, 0.03 to 2 µg/mL against Acinetobacter baumannii, and 0.03 to 2 µg/mL against Escherichia coli strains
Mechanism Preservation: ERB-fluoroquinolones maintain target inhibition against both wild-type and mutant (GyrA S84L) DNA gyrases (IC50 ~3.8 µg/mL)
In Vivo Efficacy: 5-log reduction of bacterial load in thigh infection models at 20 and 50 mg/kg oral dose levels with favorable PK/PD profiles
Safety Profile: No toxicity observed at 1200 mg/kg/day in mice, with clean off-target screening including hERG channel and cytochrome p450 enzymes
Clinical Pathogens and Efflux Evasion Strategies
Table 3: Efflux-Mediated Resistance in Priority Pathogens and Evasion Approaches
| Pathogen | Primary Efflux Pumps | Key Substrates | Evasion Strategies |
|---|---|---|---|
| Acinetobacter baumannii | AdeABC, AdeIJK, AdeFGH | Aminoglycosides, fluoroquinolones, β-lactams, tigecycline* [5] | Reduce molecular flexibility; introduce primary amines; moderate LogD |
| Pseudomonas aeruginosa | MexAB-OprM, MexXY-OprM | Beta-lactams, fluoroquinolones, aminoglycosides [14] | Strategic hydrophobicity reduction; steric shielding of recognition elements |
| Escherichia coli | AcrAB-TolC | Broad substrate spectrum including multiple antibiotic classes [64] [18] | Optimize size/resonant structure count; incorporate evasion pharmacophores |
| Klebsiella pneumoniae | AcrAB-TolC, OqxAB | Fluoroquinolones, chloramphenicol, tigecycline [18] | Balanced charge distribution; targeted polarity adjustments |
The rational design of efflux evader molecules represents a promising strategy to overcome one of the most significant barriers in antimicrobial therapy. By leveraging insights from structural biology, computational analysis, and medicinal chemistry, researchers can now systematically design antibiotics that bypass efflux recognition while maintaining potent target engagement. The experimental methodologies outlined in this review provide a framework for identifying and validating such compounds, with the potential to revitalize existing antibiotic classes and guide the development of novel agents.
As the field advances, the integration of machine learning approaches with high-throughput screening data will further refine our understanding of the molecular determinants of efflux recognition. Additionally, the combination of efflux evasion strategies with other resistance-breaking approaches may yield compounds capable of overcoming multiple concurrent resistance mechanisms. Ultimately, the systematic application of these principles offers a pathway to address the growing threat of multidrug-resistant infections and secure the efficacy of antimicrobial therapy for future generations.
Within the broader context of intrinsic resistance research, efflux pumps represent a primary barrier to antibiotic efficacy in Gram-negative bacteria. The tripartite efflux machinery, particularly the TolC-dependent systems in Escherichia coli, recognizes and extrudes a remarkably broad spectrum of chemically diverse compounds, significantly contributing to the intrinsic multidrug resistance observed in these pathogens [68] [69] [18]. A critical challenge in antibiotic discovery is understanding why some compounds are efficiently expelled while others evade recognition and retain their antibacterial activity. This guide provides an in-depth analysis of the molecular principles that distinguish efflux evaders from substrates, drawing on recent large-scale empirical studies. By elucidating these features and detailing the experimental methodologies for their identification, this work aims to equip researchers with the knowledge to rationally design antibiotics that circumvent this major resistance mechanism.
Molecular Determinants of Efflux Evasion
Key Physicochemical Properties
Recent high-throughput analyses have quantitatively defined the physicochemical space associated with efflux evasion. A study examining 73,737 compounds from the CO-ADD database classified molecules based on their activity in wild-type (WT) versus efflux-compromised (tolC) E. coli strains [68]. The findings indicate that efflux evaders—compounds active in both WT and tolC strains—occupy a specific chemical territory.
Table 1: Physicochemical Properties of Efflux Evaders vs. Substrates
| Physicochemical Property | Efflux Evaders | Efflux Substrates | Notes |
|---|---|---|---|
| Hydrophilicity (LogD) | Generally lower logD [68] | Generally higher logD [68] | Lower logD reduces susceptibility to efflux [68] |
| Molecular Size/Weight | Slightly larger [68] | Variable | Contrary to some historical assumptions [68] |
| Resonant Structure Count | Not explicitly stated | Higher count [68] | A key descriptor for efflux susceptibility [68] |
| Primary Amine Moieties | Presence can be important [68] | Not specified | Positively charged amines aid entry into GN bacteria [68] |
Alongside these collective properties, the presence or absence of specific chemical groups substantially alters a compound's probability of avoiding efflux [68]. For instance, the presence of positively charged primary amine moieties has been identified as favorable for bacterial entry and potentially for evading efflux [68] [70].
Strategic Implications for Drug Design
The properties of evader compounds suggest strategic directions for antibiotic design. A promising avenue is developing compounds with dual modes of action that include membrane permeabilization [70]. Such antibiotics, including POL7306, Tridecaptin M152-P3, and SCH79797, demonstrate significantly limited resistance development in ESKAPE pathogens [70]. This is likely because their membrane-targeting activity disrupts the integrity of the envelope, which houses the efflux machinery itself, making it more difficult for bacteria to evolve resistance through single mutations [70].
Experimental Protocols for Identifying Evaders
A robust experimental workflow is essential for correctly classifying compounds as efflux evaders, substrates, or permeation-limited. The following protocol, adapted from a large-scale public-domain study, provides a reliable methodology [68].
Bacterial Strains and Growth Conditions
A. Required Strains: The assay necessitates the use of three isogenic E. coli strains to disentangle the effects of efflux from outer membrane permeability [68]:
- Wild-Type (WT) Strain: (e.g., ATCC 25922) possessing an intact efflux system and outer membrane.
- Efflux-Deficient Strain: (e.g., MB5747) with a deletion in the tolC gene, which is essential for the function of multiple major RND efflux pumps [68] [69].
- Hyper-Permeable Strain: (e.g., MB4902) featuring an lpxC mutation that reduces lipopolysaccharide (LPS) content, creating porin-independent permeation pathways [68].
B. Culture Conditions: Bacteria are cultured in standard broth media (e.g., Mueller-Hinton Broth) according to CLSI guidelines. The optical density (OD₆₀₀) is monitored to ensure cultures are in the appropriate growth phase for inhibition assays [68].
Growth Inhibition (GI) Assay and Data Analysis
A. Compound Exposure:
- Prepare compounds of interest in a suitable solvent (e.g., DMSO), ensuring the final concentration does not exceed 1-2% to avoid solvent toxicity.
- Exponentially growing bacterial cultures are treated with the compounds in a 96-well or 384-well microtiter plate format.
- Incubate plates under optimal growth conditions for a defined period (e.g., 16-20 hours at 37°C) [68].
B. Quantification of Growth Inhibition:
- Measure the final bacterial density using a plate reader (OD₆₀₀).
- Calculate the percentage of Growth Inhibition (GI) for each well using the formula:
GI (%) = [(OD_control - OD_compound) / (OD_control - OD_media)] * 100whereOD_controlis the average OD from untreated bacteria, andOD_mediais the average OD from sterile media [68].
C. Compound Classification:
- Set a strict activity threshold to minimize noise. For example:
GI ≥ μ + 4σ, whereμis the mean compound activity andσis the standard deviation of the entire dataset [68]. - Classify compounds based on their activity profile across the three strains using the logic in the diagram below.
Diagram 1: Logic flowchart for classifying compounds based on their activity in WT, tolC, and lpxC E. coli strains. Adapted from [68].
Structural and Mechanistic Basis of Efflux Recognition
Conformational Dynamics of RND Pumps
The ability of efflux pumps to recognize diverse substrates is rooted in their structure and dynamics. Resistance Nodulation Division (RND) transporters like AcrB are trimeric proteins that function through a peristaltic mechanism. Each monomer cycles through three conformational states: Loose (L, access), Tight (T, binding), and Open (O, extrusion) [71] [18]. Substrates enter the transporter via access channels in the L state, bind in large, flexible pockets in the T state, and are expelled into the outer membrane channel TolC in the O state [71] [18].
Table 2: Key Structural Features of RND Pumps Influencing Substrate Recognition
| Structural Element | Function in Substrate Recognition/Transport |
|---|---|
| Proximal Binding Pocket (PBP) | Initial binding site in the L protomer; more voluminous in the access state [18]. |
| Distal Binding Pocket (DBP) | Deep binding site in the T protomer; engages substrates more tightly [18]. |
| Switch Loop (e.g., Phe-617 in AcrB) | Flexible loop separating PBP and DBP; controls substrate passage between pockets [18]. |
| Access Channels (Ch1-Ch4) | Distinct pathways from the periplasm or membrane interior to the binding pockets [18]. |
| Hydrophobic Trap | A patch of aromatic residues in the DBP that engages in hydrophobic interactions with substrates [72]. |
| F-loop | A flexible loop near the entrance cleft; involved in guiding substrates and conformational changes [72]. |
Phylogenetic analyses reveal that RND pumps cluster into groups with conserved binding pocket residues, and their conformational equilibria differ. For instance, AcrB and OqxB, representing different clusters, adopt fundamentally different resting states, implying distinct initial substrate binding mechanisms [71]. This plasticity is a key factor in the diversification of resistance phenotypes.
Mechanisms of Evasion and Inhibition
Evader compounds may exploit these structural principles by either failing to bind effectively to the transporter's pockets or by binding in a way that disrupts the conformational cycle. The diagram below illustrates the transport cycle and potential inhibition/evasion sites.
Diagram 2: The functional rotation mechanism of RND transporters and potential points of intervention for evader compounds and Efflux Pump Inhibitors (EPIs). Based on [71] [72] [18].
Efflux Pump Inhibitors (EPIs) often function by binding tightly to the DBP (the "hydrophobic trap"), thereby sterically blocking substrate binding and/or stalling the conformational cycle [72]. Mutations in critical residues, such as those in the access cleft (e.g., R701) or flexible loop (e.g., E675) of the AdeJ transporter in A. baumannii, can confer resistance to specific classes of EPIs, demonstrating the direct link between these structural features and compound recognition [72].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Efflux and Evasion
| Reagent / Tool | Function/Description | Example Use Case |
|---|---|---|
| Isogenic E. coli Panel | WT, tolC-, and lpxC- strains. | Dissecting contributions of efflux vs. permeability to compound activity [68]. |
| Fluorescent Efflux Probes | Substrates like Ethidium Bromide (EtBr), Hoechst 33342. | Real-time assessment of efflux pump activity via fluorometric assays [72]. |
| Known EPIs | e.g., Phenylalanine-arginine β-naphthylamide (PAβN). | Positive controls for efflux inhibition studies [18]. |
| Surface Plasmon Resonance (SPR) | A biophysical technique to measure biomolecular interactions. | Studying binding kinetics between MFPs (e.g., AcrA) and TolC [73]. |
| Molecular Docking & MD Software | Computational tools for simulating protein-ligand interactions. | Predicting binding poses of compounds in pumps like AcrB and AdeJ [71] [72]. |
The systematic analysis of efflux evaders reveals that overcoming intrinsic resistance in Gram-negative bacteria requires a multi-faceted strategy. Successful compounds often exhibit a combination of specific physicochemical properties—such as lower logD—and distinct chemical groups that allow them to bypass recognition by promiscuous RND transporters. The integration of robust phenotypic screening using defined bacterial panels with advanced structural and computational biology provides a powerful framework for identifying these features. Moving forward, the rational design of antibiotics that either inherently evade efflux or are combined with targeted EPIs represents a promising path to breaking through the efflux barrier and revitalizing the antibiotic pipeline.
The escalating crisis of antimicrobial resistance (AMR) poses a significant threat to global public health. Efflux pumps, which actively expel antibiotics from bacterial cells, are a major contributor to intrinsic and acquired multidrug resistance. This in-depth technical guide explores the therapeutic strategy of combining antibiotics with Efflux Pump Inhibitors (EPIs) to restore the efficacy of existing antimicrobials. Framed within broader research on intrinsic resistance, this whitepaper synthesizes current knowledge on EPI mechanisms, presents structured quantitative data on key efflux systems, details essential experimental protocols for evaluating combination therapy, and visualizes critical pathways and workflows. Aimed at researchers and drug development professionals, this review underscores the potential of EPI-antibiotic synergism to counteract efflux-mediated resistance and rejuvenate our antibiotic arsenal.
Efflux pumps are membrane transporter proteins that facilitate the active extrusion of toxic substrates, including a wide range of antibiotics, from the bacterial cell. This activity reduces the intracellular concentration of antimicrobial agents, thereby conferring resistance [74] [15]. In the context of intrinsic resistance, many efflux pumps are constitutively expressed at low levels as part of the bacterium's normal physiology, contributing to baseline resistance to certain drug classes [1]. However, upon exposure to antibiotics, bacteria can upregulate the expression of these pumps, leading to heightened resistance phenotypes [75].
The overexpression of efflux pumps is a key driver of multidrug resistance (MDR) in many clinically significant pathogens, including Acinetobacter baumannii, Pseudomonas aeruginosa, Escherichia coli, and Klebsiella pneumoniae [74] [5] [14]. Given the slow pace of novel antibiotic discovery, alternative strategies are urgently needed. One promising approach is combination therapy, wherein a conventional antibiotic is co-administered with an EPI. EPIs block the function of efflux pumps, preventing antibiotic extrusion and restoring bacterial susceptibility [74] [18]. This strategy aims to prolong the lifespan of existing antibiotics and enhance treatment outcomes for infections caused by MDR pathogens. This review delves into the scientific foundation, current evidence, and methodological approaches for developing this innovative therapeutic strategy.
Efflux Pump Families and Their Role in Resistance
Bacterial efflux pumps are classified into several families based on their structure and energy source. The most clinically significant families in Gram-negative bacteria are the Resistance-Nodulation-Division (RND) family, the Major Facilitator Superfamily (MFS), and the ATP-Binding Cassette (ABC) superfamily [15] [18].
- RND Pumps: These are tripartite complexes that span the entire cell envelope of Gram-negative bacteria. They consist of an inner membrane transporter, a periplasmic adapter protein (PAP), and an outer membrane channel. RND pumps, such as AcrAB-TolC in E. coli and MexAB-OprM in P. aeruginosa, are particularly effective at conferring broad-spectrum resistance due to their ability to transport a wide variety of compounds directly from the cell interior to the external environment [14] [18]. They are secondary active transporters that utilize the proton motive force.
- ABC Pumps: These are primary active transporters that hydrolyze ATP to energize substrate extrusion. An example is the MacAB-TolC system in E. coli, which is involved in expelling macrolides and polypeptide virulence factors [74] [15].
- MFS Pumps: These are secondary active transporters that utilize ion gradients. While common in Gram-positive bacteria, they can also form tripartite systems in Gram-negatives, such as EmrAB-TolC in E. coli, which exports protonophores like carbonyl cyanide m-chlorophenylhydrazone (CCCP) [15] [18].
Table 1: Major Efflux Pump Families in Gram-Negative Bacteria
| Family | Energy Source | Representative Pump(s) | Key Antibiotic Substrates |
|---|---|---|---|
| RND | Proton Motive Force | AcrAB-TolC (E. coli), MexAB-OprM (P. aeruginosa), AdeABC (A. baumannii) | β-lactams, fluoroquinolones, tetracyclines, chloramphenicol, macrolides, aminoglycosides [74] [5] [14] |
| ABC | ATP Hydrolysis | MacAB-TolC (E. coli) | Macrolides, polypeptides [74] [15] |
| MFS | Proton Motive Force | NorA (S. aureus), Tet38 (S. aureus), EmrAB-TolC (E. coli) | Fluoroquinolones, tetracyclines, protonophores [74] [15] [18] |
| MATE | Proton/Sodium Ion Gradient | MepA (S. aureus), PmpM (P. aeruginosa) | Fluoroquinolones, aminoglycosides [74] [5] |
The following diagram illustrates the structure and operational mechanism of a typical RND efflux pump, the most clinically significant system in Gram-negative bacteria.
Diagram 1: Structure and Function of a Tripartite RND Efflux Pump. The diagram shows how the inner membrane pump (IMP), periplasmic adapter protein (PAP), and outer membrane protein (OMP) work together to extrude antibiotics from the cytoplasm using the proton motive force (H+).
Mechanisms of Efflux Pump Inhibitors (EPIs)
EPIs counteract efflux through several distinct mechanisms, which can be exploited for therapeutic development. The primary modes of action include:
- Competitive Inhibition: Some EPIs, such as phenylalanyl arginyl β-naphthylamide (PAβN), act as competitive substrates for the efflux pump. They bind to the substrate recognition site with high affinity, blocking the binding of antibiotics without being effectively transported themselves, thereby preventing antibiotic extrusion [74] [75].
- Energy Depletion: EPIs like carbonyl cyanide m-chlorophenylhydrazone (CCCP) disrupt the proton motive force (PMF) across the inner membrane. Since RND, MFS, and other secondary transporters rely on the PMF for energy, this action effectively "unplugs" the power source of the efflux pump [74] [15].
- Inhibition of Assembly or Function: Some inhibitors interfere with the proper assembly of the tripartite efflux complex or disrupt the conformational changes necessary for the peristaltic pump mechanism. For instance, certain compounds target the interactions between the PAP and the IMP [15] [18].
- Downregulation of Gene Expression: While less common, some compounds can indirectly inhibit efflux by targeting regulatory proteins that control the expression of efflux pump genes, preventing their overexpression in response to antibiotic stress [74].
Recent research has focused on identifying natural product-derived EPIs and optimizing synthetic compounds with lower cytotoxicity and better pharmacological properties than early inhibitors like PAβN and CCCP [74] [15].
Current Evidence for EPI-Antibiotic Synergy
Quantitative Data from Key Studies
Substantial evidence from in vitro studies demonstrates the synergistic effect of EPIs when combined with antibiotics against MDR pathogens. The following table summarizes key findings from recent research.
Table 2: Synergistic Effects of EPIs and Antibiotics Against MDR Pathogens
| Pathogen | Efflux Pump(s) | Antibiotic | EPI | Observed Effect (MIC Reduction, Gene Expression, etc.) | Citation |
|---|---|---|---|---|---|
| Escherichia coli & Klebsiella pneumoniae | AcrAB-TolC, OqxAB, others | Various (not specified) | PAβN | Upregulation of efflux genes under antibiotic stress; downregulation and restored susceptibility with EPI co-administration [75]. | |
| Escherichia coli | AcrAB-TolC | Ampicillin (AMP) | - (Molecular dynamics simulation under stress) | Increased rigidity and opening of TolC pore, correlating with experimental observation of increased AMP resistance post-aerosolization [37]. | |
| Pseudomonas aeruginosa | MexAB-OprM, MexVW, MexMN | Ceftazidime/Avibactam (CZA), Ceftolozane/Tazobactam (C/T) | - (Study of pump mutations) | Mutations leading to pump overexpression or altered specificity confer resistance to novel β-lactam/β-lactamase inhibitor combinations [14]. | |
| Acinetobacter baumannii | AdeABC, AdeFGH, AdeIJK | Aminoglycosides, β-lactams, tetracyclines, tigecycline | - (Intrinsic overexpression) | Overexpression of Ade pumps is a major contributor to MDR in CRAB; identified as a key target for EPI development [5]. | |
| Mycobacterium abscessus | MmpL, other transporters | Linezolid, other antibiotics | - (Genetic screen) | Transposon mutagenesis identified membrane transporters and efflux pumps as key factors in low drug accumulation and intrinsic resistance [4]. |
EPIs in Restoring Susceptibility to Novel β-Lactam/β-Lactamase Inhibitors
The emergence of resistance to even the newest β-lactam/β-lactamase inhibitor combinations (BL/BLIs) like ceftazidime/avibactam (CZA) and ceftolozane/tazobactam (C/T) is a major concern. A significant body of evidence implicates RND efflux pumps in this process. In P. aeruginosa, mutations that lead to the overexpression of MexAB-OprM are a common mechanism of resistance to CZA and C/T [14]. Furthermore, studies have shown that mutations in other less-characterized pumps, such as MexVW and MexMN, can also contribute to reduced susceptibility to these novel agents [14]. This underscores that efflux is a versatile and underappreciated mechanism of resistance to the latest antibiotics and highlights the potential utility of broad-spectrum EPIs to preserve their efficacy.
Experimental Protocols for Evaluating Combination Therapy
Robust experimental methodologies are essential for validating the efficacy of EPI-antibiotic combinations. The following section details key protocols, from initial screening to mechanistic studies.
Core Workflow for EPI Synergy Testing
The standard workflow for evaluating the potential of an EPI begins with phenotypic assays and progresses to molecular analyses.
Diagram 2: Experimental Workflow for EPI Synergy Evaluation. This flowchart outlines the key steps, from initial screening to molecular confirmation, used to assess the efficacy of Efflux Pump Inhibitors.
Detailed Methodologies
5.2.1 Checkerboard Assay and MIC Determination This is a fundamental first step for screening synergistic interactions.
- Procedure: A two-dimensional microdilution assay is performed. Serial dilutions of the antibiotic are prepared in one direction, and serial dilutions of the EPI are prepared in the perpendicular direction in a 96-well plate. Each well is inoculated with a standardized bacterial suspension (~5 × 10^5 CFU/mL) [75].
- Analysis: The Fractional Inhibitory Concentration (FIC) index is calculated after incubation.
- FIC Index = (MIC of antibiotic in combination / MIC of antibiotic alone) + (MIC of EPI in combination / MIC of EPI alone)
- Synergy is typically defined as an FIC index ≤ 0.5. The results identify the combination ratios that warrant further investigation [75].
5.2.2 Time-Kill Assay This dynamic assay provides information on the bactericidal activity of the combination over time.
- Procedure: Bacterial cultures are exposed to: a) the antibiotic at a sub-inhibitory concentration (e.g., 0.5x MIC), b) the EPI alone, and c) the combination of both. Samples are withdrawn at predetermined time intervals (e.g., 0, 2, 4, 6, 24 hours), serially diluted, and plated on agar to enumerate viable colonies (CFU/mL) [18].
- Analysis: Synergy is defined as a ≥ 2-log10 reduction in CFU/mL by the combination compared to the most active single agent at 24 hours. This confirms that the combination is not just inhibitory but actively killing the bacteria.
5.2.3 Ethidium Bromide (EtBr) Accumulation Assay This fluorometric assay directly measures efflux pump activity.
- Procedure: Bacterial cells are harvested and suspended in a buffer with a non-lethal concentration of the efflux pump substrate EtBr. The fluorescence of intracellularly accumulated EtBr is measured over time using a fluorometer (excitation ~530 nm, emission ~590 nm). The assay is run with and without the EPI (e.g., PAβN or CCCP) [5] [4].
- Analysis: A significant increase in fluorescence intensity in the presence of the EPI indicates successful inhibition of the efflux pumps, leading to greater intracellular accumulation of the fluorescent substrate.
5.2.4 Quantitative PCR (qPCR) for Gene Expression This molecular technique assesses the impact of EPIs on the genetic regulation of efflux pumps.
- Procedure: Bacterial RNA is extracted from cultures treated with sub-inhibitory concentrations of antibiotic, EPI, or their combination. The RNA is reverse-transcribed into cDNA, which is used as a template for qPCR with primers specific for target efflux pump genes (e.g., acrB, adeB) and housekeeping genes (e.g., rpoB, gyrB) [75].
- Analysis: The relative fold change in efflux pump gene expression is calculated using the 2^(-ΔΔCt) method. Co-administration of an effective EPI often leads to downregulation of efflux genes that were upregulated by antibiotic exposure alone [75].
Advanced Techniques: Molecular Dynamics Simulations
Molecular dynamics (MD) simulations provide atomistic insights into the interactions between efflux pumps, antibiotics, and EPIs. As demonstrated in a study on E. coli's AcrAB-TolC pump, MD can model how environmental stresses (like increased pressure from aerosolization) affect pump dynamics and antibiotic binding [37].
- Procedure: High-resolution structures of the efflux pump (e.g., from cryo-EM) are placed in a simulated lipid bilayer and solvated. Ligands (antibiotics/EPIs) are docked into the binding pocket. Simulations are run under different conditions (e.g., standard vs. increased pressure) for hundreds of nanoseconds.
- Analysis: Metrics such as root-mean-square deviation (RMSD), root-mean-square fluctuation (RMSF), and binding free energies (e.g., MM-GBSA) are calculated. These analyses can reveal how ligands stabilize or destabilize the pump and trigger conformational changes required for efflux [37].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Efflux Pump and EPI Research
| Reagent / Solution | Function / Application in EPI Research |
|---|---|
| PAβN (Phe-Arg-β-naphthylamide) | A broad-spectrum, competitive EPI commonly used as a positive control in in vitro assays (e.g., checkerboard, EtBr accumulation) to validate efflux-mediated resistance [74] [75]. |
| CCCP (Carbonyl cyanide m-chlorophenyl hydrazone) | A protonophore that dissipates the proton motive force; used to confirm the energy-dependent nature of an efflux pump in functional assays [74] [15]. |
| Ethidium Bromide (EtBr) | A fluorescent substrate for many multidrug efflux pumps; used in fluorometric accumulation/efflux assays to directly visualize and quantify pump activity and its inhibition [5] [4]. |
| qPCR Reagents | Kits and primers for quantifying the expression levels of efflux pump genes and their regulators under different treatment conditions [75]. |
| Molecular Dynamics Software | Software suites (e.g., GROMACS, NAMD) and high-performance computing resources for simulating pump-ligand interactions and understanding inhibition mechanics at an atomic level [37]. |
Combination therapy employing antibiotics and efflux pump inhibitors represents a promising and scientifically robust strategy to combat multidrug-resistant bacterial infections. By targeting the fundamental mechanism of reduced intracellular drug concentration, EPIs can restore the efficacy of a wide range of antibiotics, including the newest BL/BLI combinations. The path to clinical translation requires a concerted effort to discover and optimize non-toxic, potent EPIs, validated through the comprehensive experimental frameworks outlined in this review. Integrating EPIs into the antimicrobial arsenal holds the potential to dramatically improve outcomes in the relentless fight against antibiotic resistance.
Multidrug efflux pumps are a fundamental component of intrinsic resistance in Gram-negative bacteria, significantly reducing intracellular antibiotic concentrations and compromising treatment efficacy [76] [8]. Efflux pump inhibitors (EPIs) represent a promising therapeutic strategy to resensitize resistant pathogens to conventional antibiotics; however, their transition from laboratory research to clinical application has been fraught with challenges [77]. The very attributes that make efflux pumps formidable resistance determinants—their structural complexity, genetic regulation, and physiological roles—also make them difficult targets for selective inhibition [14]. This technical guide examines the core obstacles hindering the clinical translation of EPIs, with particular focus on the intersecting challenges of compound toxicity and target specificity. By synthesizing current research and methodological approaches, we provide a framework for navigating these barriers in EPI development programs.
Efflux Pump Fundamentals and Clinical Relevance
Structural and Functional Diversity of Efflux Systems
Bacterial efflux transporters are classified into several phylogenetically distinct families based on protein sequence and energy coupling mechanisms [76]. The most clinically significant pumps in Gram-negative bacteria belong to the Resistance-Nodulation-Division (RND) superfamily, which form tripartite complexes spanning both the inner and outer membranes [14] [8]. These complexes typically consist of an inner membrane transporter (e.g., AcrB in E. coli or MexB in P. aeruginosa), a periplasmic adaptor protein (e.g., AcrA, MexA), and an outer membrane channel (e.g., TolC, OprM) [76] [8]. This organization enables direct extrusion of substrates into the external medium, bypassing the periplasmic space and leveraging the outer membrane as a synergistic permeability barrier [76].
Table 1: Major Efflux Pump Families in Gram-Negative Bacteria
| Family | Energy Source | Representative Systems | Key Substrates |
|---|---|---|---|
| RND | Proton motive force | AcrAB-TolC (E. coli), MexAB-OprM (P. aeruginosa) | Beta-lactams, fluoroquinolones, macrolides, novobiocin |
| MFS | Proton motive force | EmrB-TolC (E. coli) | Nalidixic acid, carbonyl cyanide m-chlorophenylhydrazone |
| ABC | ATP hydrolysis | MacAB-TolC (E. coli) | Macrolides |
| MATE | Proton/sodium motive force | Not well characterized in tripartite systems | Fluoroquinolones, ethidium |
| SMR | Proton motive force | Not typically tripartite | Quaternary ammonium compounds, dyes |
Physiological Roles Beyond Antibiotic Resistance
Efflux pumps serve essential physiological functions that complicate therapeutic inhibition [78] [79]. They facilitate the expulsion of endogenous toxic metabolites, bacterial communication through quorum sensing molecules, biofilm formation, and virulence factor expression [14] [8]. For instance, in P. aeruginosa, RND pumps participate in the export of autoinducers involved in quorum sensing, while in E. coli, AcrAB-TolC contributes to bile salt resistance in the gut environment [76] [14]. This multifunctionality means that complete inhibition of essential efflux systems may disrupt bacterial homeostasis and viability, potentially leading to cytotoxicity that limits therapeutic windows [77].
Core Challenges in EPI Development
Target Specificity and Off-Target Effects
The development of specific EPIs faces substantial hurdles due to structural conservation between bacterial and mammalian transporters [80]. Many inhibitor compounds identified through high-throughput screening demonstrate activity against both bacterial RND pumps and human efflux systems such as P-glycoprotein (P-gp), leading to potential drug-drug interactions and altered pharmacokinetics of co-administered therapeutics [80] [77]. For example, early-stage EPIs targeting the Staphylococcus aureus NorA pump frequently showed cross-reactivity with P-gp, complicating their therapeutic application [80]. This lack of specificity stems from similarities in substrate-binding domains and conserved mechanistic elements across evolutionarily distant efflux systems [77].
Compound Toxicity and Pharmacological Limitations
Toxicity profiles present a critical barrier to clinical translation of EPIs [77]. Many promising inhibitor candidates demonstrate unacceptable cytotoxicity at concentrations required for effective efflux blockade, often due to interference with mammalian cellular processes or disruption of essential mitochondrial functions [77]. Additionally, the pharmacological properties necessary for effective EPI activity—including appropriate molecular weight, lipophilicity, and membrane permeability—often conflict with optimal drug-like characteristics [8] [77]. The requirement for EPIs to reach their target sites in the bacterial cell envelope further complicates formulation strategies and tissue distribution profiles [8].
Structural and Mechanistic Challenges
The structural complexity of RND efflux pumps creates significant obstacles for inhibitor design [8]. These systems operate through sophisticated peristaltic mechanisms with multiple conformational states and substrate-binding pockets [8]. For instance, AcrB functions as an asymmetric trimer with each protomer adopting distinct conformational states (loose, tight, and open) during the transport cycle [8]. This dynamic mechanism means that effective inhibition may require compounds that either compete with substrates for binding pockets or allosterically disrupt the transport cycle—both challenging design objectives [8] [77]. Additionally, the presence of multiple substrate entry channels and binding sites within a single transporter complicates comprehensive inhibition [8].
Figure 1: Roadmap of key challenges in EPI development and their interrelationships
Methodological Approaches for EPI Characterization
Efflux Inhibition Assays
Standardized methods for evaluating EPI activity are essential for comparing compound efficacy and mechanism of action [8]. The following protocols represent cornerstone approaches in the field:
Minimum Inhibitory Concentration (MIC) Reduction Assay
- Prepare serial dilutions of the test antibiotic in appropriate growth medium
- Add subinhibitory concentrations of the EPI candidate (typically 0.5-50 µg/mL depending on compound toxicity)
- Inoculate with standardized bacterial suspension (∼5 × 10^5 CFU/mL)
- Incubate for 16-20 hours at 37°C
- Determine MIC as the lowest antibiotic concentration completely inhibiting visible growth
- Significant MIC reduction (≥4-fold) in presence of EPI indicates efflux inhibition [8]
Ethidium Bromide Accumulation Assay
- Harvest mid-log phase bacteria and wash with appropriate buffer
- Resuspend to OD600 = 0.2 in buffer containing glucose (0.2%) for energy-dependent efflux
- Add EPI candidate at desired concentration and pre-incubate for 5 minutes
- Add ethidium bromide (1-2 µg/mL) and monitor fluorescence over time (excitation: 530 nm, emission: 600 nm)
- Include positive (CCCP, 50 µM) and negative (no inhibitor) controls
- Increased fluorescence accumulation rate indicates efflux inhibition [8]
Real-time Fluorometric Accumulation Assays
- Grow bacterial cultures to mid-log phase and wash twice with PBS
- Resuspend in PBS with glucose (0.2%) to OD600 = 0.2
- Distribute into black 96-well plates with transparent bottoms
- Add fluorescent substrate (e.g., Hoechst 33342, Nile red) with or without EPI candidate
- Monitor fluorescence intensity kinetically using plate reader
- Calculate initial accumulation rates and steady-state levels [8]
Table 2: Key Methodologies for Evaluating EPI Activity
| Method | Key Readout | Advantages | Limitations |
|---|---|---|---|
| MIC reduction | Fold-change in antibiotic susceptibility | Clinically relevant, simple setup | Indirect measure of efflux inhibition |
| Ethidium bromide accumulation | Fluorescence intensity over time | Direct efflux measurement, real-time kinetics | Non-specific dye interactions possible |
| Radio-labeled antibiotic accumulation | Radiolabel counts in bacterial pellets | Direct substrate-specific measurement | Requires specialized facilities and reagents |
| Real-time fluorometry | Kinetic fluorescence parameters | High-throughput capability, multiple timepoints | Limited to fluorescent substrates |
| Efflux pump gene expression | qRT-PCR of pump components | Molecular mechanism insight | Does not directly measure functional activity |
Specificity and Toxicity Assessment
Comprehensive evaluation of EPI candidates requires rigorous assessment of selectivity and cellular toxicity:
Mammalian Cell Cytotoxicity Assays
- Culture appropriate mammalian cell lines (e.g., HepG2, HEK293) in 96-well plates
- Expose to serial dilutions of EPI candidates for 24-72 hours
- Assess viability using MTT, resazurin, or ATP-based assays
- Calculate CC50 (concentration causing 50% cytotoxicity) and selectivity index (CC50/effective EPI concentration) [77]
P-glycoprotein Inhibition Screening
- Prepare membrane vesicles overexpressing human P-gp
- Measure ATPase activity in presence of EPI candidates
- Alternatively, use fluorescent P-gp substrates (e.g., calcein-AM) in sensitive cell lines
- Quantify inhibition potency (IC50) relative to known P-gp inhibitors [80]
Mechanistic Toxicity Profiling
- Assess mitochondrial membrane potential using JC-1 or TMRM dyes
- Evaluate reactive oxygen species production with H2DCFDA
- Monitor apoptosis markers (caspase activation, phosphatidylserine externalization)
- Determine effects on bacterial membrane integrity without bactericidal activity [77]
Figure 2: Experimental workflow for comprehensive EPI evaluation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for EPI Investigations
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Fluorescent efflux substrates | Ethidium bromide, Hoechst 33342, Nile red | Accumulation and inhibition assays | Varying specificity for different pump classes; concentration optimization required |
| Protonophores | CCCP, valinomycin | Positive controls for energy-dependent efflux assays | Cytotoxic at higher concentrations; solvent compatibility |
| Reference EPIs | PAβN, verapamil, reserpine | Benchmark compounds for validation | Varying potency across bacterial species; solubility limitations |
| Genetically modified strains | Knockout mutants (ΔacrB, ΔtolC); Overexpression strains | Mechanism of action confirmation | Genetic background effects; complementation required for verification |
| Antibiotic substrates | Ciprofloxacin, levofloxacin, erythromycin, azithromycin | MIC reduction assays | Consider intrinsic activity against test strain |
| Mammalian cytotoxicity assays | MTT, resazurin, LDH release | Selectivity index determination | Cell line-specific responses; incubation time optimization |
| P-gp inhibition screening | Calcein-AM accumulation, ATPase activity | Specificity profiling | Required for dual NorA/P-gp inhibitor identification [80] |
| Structural biology tools | Cryo-EM, X-ray crystallography, molecular docking | Mechanistic studies | Technical expertise requirements; equipment accessibility |
Emerging Strategies and Future Directions
Innovative Approaches to Overcome Translational Barriers
Recent advances in EPI discovery have focused on addressing the core challenges of specificity and toxicity through multiple innovative strategies:
Structural Biology-Informed Design High-resolution structural data from cryo-electron microscopy and X-ray crystallography have revealed detailed interaction networks between RND pumps and their substrates [8]. This information enables structure-based drug design targeting specific subpockets within transporter binding sites [8] [77]. For example, the asymmetric conformation of AcrB with distinct loose, tight, and open states presents opportunities for state-specific inhibitors that may offer greater selectivity [8].
Hybrid Antibiotic-EPI Conjugates Chemical conjugation of EPIs to antibiotics creates dual-action compounds that co-localize both activities at the infection site [77]. The tobramycin-EPI vector approach demonstrates enhanced synergy against multidrug-resistant P. aeruginosa while potentially reducing off-target effects [77]. These constructs leverage bacterial uptake mechanisms to deliver inhibitory activity specifically to pathogens [77].
Natural Product-Derived Inhibitors Plant-derived flavonoids and other natural products offer scaffolds with inherently lower cytotoxicity profiles [77]. Their complex chemical structures often interact with multiple targets simultaneously, potentially overcoming redundancy in efflux systems [77]. Semisynthetic modification of these cores can further enhance potency and pharmacological properties [77].
Regulatory Network Targeting Rather than directly inhibiting pump activity, alternative approaches target the regulatory networks controlling efflux pump expression [14]. Small molecules that modulate transcriptional regulators like RamA or MarA could reduce pump overexpression without completely abolishing essential physiological functions [14] [77].
Technical Advances in Assessment Methodologies
Improved assay systems and analytical techniques are addressing historical limitations in EPI characterization:
Advanced Accumulation Quantification Mass spectrometry-based methods now enable direct quantification of antibiotic accumulation in bacteria, providing substrate-specific efflux measurements beyond fluorescent proxies [8]. These approaches yield absolute quantification of intracellular concentrations under various inhibitory conditions [8].
High-Content Screening Platforms Automated imaging systems combined with multiplexed assays allow simultaneous assessment of antibacterial activity, mammalian cell toxicity, and compound localization in miniaturized formats [80]. These platforms generate rich datasets for structure-activity relationship (SAR) analysis early in the discovery pipeline [80].
Biomarker Development for In Vivo Monitoring Transcriptional biomarkers of efflux activity, similar to those developed for other transporter systems, could enable pharmacokinetic/pharmacodynamic (PK/PD) modeling and target engagement verification in clinical settings [81]. For instance, monitoring expression of LXR target genes in peripheral blood cells has proven useful for clinical development of LXR modulators [81].
The clinical translation of efflux pump inhibitors remains hampered by the intertwined challenges of target specificity and compound toxicity. Successfully navigating these hurdles requires integrated methodological approaches that address both antibacterial efficacy and mammalian cell compatibility from early discovery stages. Advances in structural biology, chemical design, and assessment technologies are providing new paths forward, yet the fundamental tension between effective efflux inhibition and acceptable safety profiles persists. Future EPI development must continue to balance these competing demands through innovative chemical strategies and comprehensive biological characterization, with the goal of restoring the efficacy of existing antibiotics against increasingly resistant bacterial pathogens.
Cross-Species Validation and Comparative Analysis of Clinically Significant Efflux Systems
Efflux pumps are active transport systems that recognize and expel a wide range of toxic molecules, including antibiotics, from bacterial cells. This expulsion mechanism represents one of the fundamental components of intrinsic and acquired antimicrobial resistance in bacterial pathogens [8]. Unlike other resistance mechanisms such as enzymatic modification or target mutations, efflux is particularly challenging to detect and counteract in clinical settings, and no standardized methods are currently available to diagnose or inhibit this mechanism effectively [8]. Within the broader context of intrinsic resistance research, validating the functional impact of efflux pump gene expression on resistance phenotypes remains a critical methodological challenge. This technical guide provides comprehensive methodologies and analytical frameworks for researchers seeking to establish robust correlations between efflux gene expression and demonstrable resistance phenotypes, with particular emphasis on quantitative approaches suitable for drug development applications.
The significance of efflux-mediated resistance continues to grow with the recognition that efflux activity not only directly reduces intracellular antibiotic concentrations but also accelerates the evolution of resistance by generating mutational hotspots in bacterial populations [82]. Recent findings indicate that high efflux is linked to downregulation of DNA repair pathways, creating a hypermutatable state that facilitates the accumulation of antibiotic-resistance mutations [82]. This dual role of efflux in both immediate resistance and long-term resistance evolution underscores the critical importance of validated assessment methods for efflux activity and its phenotypic consequences.
Efflux Pump Systems: Structural and Genetic Foundations
Major Efflux Pump Families in Bacteria
Bacterial efflux systems are categorized into several major families based on structural features and energy sources. A comprehensive understanding of these families is essential for designing appropriate validation strategies.
Table 1: Major Bacterial Efflux Pump Families and Their Characteristics
| Efflux Family | Energy Source | Genetic Components | Representative Systems | Substrate Profile |
|---|---|---|---|---|
| RND (Resistance-Nodulation-Division) | Proton motive force | Inner membrane transporter, periplasmic adaptor, outer membrane channel | AcrAB-TolC (E. coli), MexAB-OprM (P. aeruginosa) | Extremely broad; multiple antibiotic classes |
| ABC (ATP-Binding Cassette) | ATP hydrolysis | Two nucleotide-binding domains, two transmembrane domains | MacAB-TolC (E. coli) | Macrolides, specific compounds |
| MFS (Major Facilitator Superfamily) | Proton motive force | 12-14 transmembrane α-helices | NorA (S. aureus), EmrAB-TolC (E. coli) | Fluoroquinolones, dyes, disinfectants |
| SMR (Small Multidrug Resistance) | Proton motive force | 4 transmembrane helices | EmrE (E. coli) | Quaternary ammonium compounds, dyes |
| MATE (Multidrug and Toxic Compound Extrusion) | Sodium or proton motive force | 12 transmembrane domains | NorM (V. cholerae) | Fluoroquinolones, aminoglycosides |
Genetic Organization and Regulation
The genetic architecture of efflux systems varies significantly between families. In Gram-negative bacteria, RND systems typically form tripartite complexes that span both inner and outer membranes [8]. For example, the AcrAB-TolC system in Escherichia coli consists of the inner membrane transporter AcrB, the periplasmic adaptor protein AcrA, and the outer membrane channel TolC [8]. Similarly, ABC transporters like MacAB-TolC assemble with a MacB dimer (inner membrane), hexameric MacA (periplasmic adaptor), and a TolC trimer (outer membrane) [83].
In Helicobacter pylori, three homologous gene clusters encode proteins belonging to the RND family transporter, named hefA/B/C, hefD/E/F, and hefG/H/I, respectively [84]. Among these, hefA, hefD, and hefG encode outer membrane channel proteins and play pivotal roles in the efflux pump system [84]. Understanding these genetic arrangements is essential for designing expression analysis methods that account for co-regulation of system components.
Methodological Framework for Efflux Validation
Quantitative Gene Expression Analysis
Accurate measurement of efflux pump gene expression represents the foundational step in correlating expression with resistance phenotypes. Reverse transcription quantitative PCR (RT-qPCR) provides the most sensitive and reproducible approach for targeted expression analysis.
Experimental Protocol: RT-qPCR for Efflux Pump Genes
- RNA Extraction: Isolate total RNA from bacterial cultures grown under standardized conditions (OD600 = 0.2) using commercial kits with DNase treatment to remove genomic DNA contamination [84].
- cDNA Synthesis: Reverse transcribe 1μg of total RNA using reverse transcriptase with random hexamers or gene-specific primers [84].
- qPCR Amplification: Perform quantitative PCR using gene-specific primers (e.g., for H. pylori hefA: F-5'-TATGCCCGCTGTTGA-3', R-5'-GAGGAAATACGACGCTAA-3'; product 143bp) [84].
- Normalization: Normalize expression levels using stable reference genes (e.g., 16S rRNA) and calculate relative expression using the 2^(-ΔΔCt) method [84].
- Quality Control: Include no-template controls and no-reverse transcription controls to detect contamination or genomic DNA amplification.
Phenotypic Resistance Assessment
Minimum Inhibitory Concentration (MIC) determination provides the standard phenotypic measure of antibiotic resistance. However, specific modifications enhance detection of efflux-mediated resistance.
Experimental Protocol: MIC Determination with Efflux Inhibition
- Standard MIC Testing: Determine baseline MICs using broth microdilution or E-test methods according to CLSI/EUCAST guidelines [84].
- Efflux Pump Inhibition: Repeat MIC testing in the presence of subinhibitory concentrations of efflux pump inhibitors (e.g., CCCP, PAβN, verapamil) [8].
- Fold Reduction Calculation: Calculate the fold reduction in MIC in the presence of inhibitors as an indicator of efflux contribution.
- Threshold Definition: Define significant efflux contribution as ≥4-fold reduction in MIC with inhibitors [85].
Table 2: Interpretation of MIC Changes with Efflux Pump Inhibition
| Fold Reduction in MIC with EPI | Interpretation | Suggested Follow-up |
|---|---|---|
| <2-fold | No significant efflux contribution | Investigate other resistance mechanisms |
| 2-4 fold | Moderate efflux contribution | Confirm with genetic methods |
| ≥4-fold | Significant efflux contribution | Proceed with genetic validation |
| ≥8-fold | Major efflux contribution | Consider as priority for inhibitor development |
Functional Efflux Activity Assays
Direct measurement of efflux activity provides functional validation beyond gene expression correlations.
Experimental Protocol: Fluorometric Accumulation Assays
- Dye Selection: Select fluorescent substrates appropriate for the efflux system under investigation (e.g., ethidium bromide, Hoechst 33342, rhodamine) [8].
- Dye Loading: Incubate bacteria with fluorescent substrate in energy-depleted conditions (low temperature, energy inhibitors) to allow passive accumulation.
- Efflux Initiation: Restore energy sources (glucose, ATP precursors) to initiate active efflux.
- Kinetic Monitoring: Measure fluorescence decrease over time using a plate reader or fluorometer [8].
- Data Analysis: Calculate efflux rates and compare between strains with different expression levels.
Experimental Protocol: Direct Antibiotic Accumulation Measurement Recent advances enable direct quantification of intracellular antibiotic concentrations using mass spectrometry [4].
- Antibiotic Exposure: Incubate bacteria with therapeutic concentrations of antibiotics for standardized durations (typically 4 hours) [4].
- Rapid Separation: Pellet bacteria through silicone oil or rapid filtration to separate from extracellular antibiotic.
- Antibiotic Extraction: Lyse cells and extract antibiotics using appropriate solvents.
- LC-MS Quantification: Measure antibiotic concentrations using liquid chromatography-mass spectrometry with stable isotope internal standards [4].
- Normalization: Normalize intracellular concentrations to cell number or protein content.
Advanced Genetic Validation Approaches
Genetic Knockout and Complementation
Definitive validation of efflux impact requires genetic manipulation to establish causality between gene expression and resistance phenotypes.
Experimental Protocol: Gene Knockout in Clinical Isolates
- Selection Marker Strategy: For multidrug-resistant clinical isolates, use alternative selection markers (e.g., tellurite resistance conferred by tpm gene) since standard antibiotic resistance cassettes may not provide selectable phenotypes [85].
- Two-Step Recombination: Employ λ-Red recombinase systems with positive-negative selection using sacB for counterselection [85].
- Mutant Verification: Verify gene deletion by PCR and sequencing across the deletion junction.
- Phenotypic Characterization: Compare MIC values and accumulation assays between wild-type and knockout strains.
Experimental Protocol: Genetic Complementation
- Vector Selection: Clone intact efflux pump genes into appropriate expression vectors with selectable markers.
- Controlled Expression: Use inducible promoters where possible to avoid toxicity from overexpression.
- Functional Testing: Measure restoration of resistance phenotype in complemented strains compared to knockout and wild-type strains.
Transposon Mutagenesis Screening
For discovery-based approaches, transposon mutagenesis identifies efflux-related genes involved in resistance to specific antibiotics [4].
Experimental Protocol: Transposon Screening for Efflux Components
- Library Generation: Create comprehensive transposon mutant libraries using mariner-based or other transposon systems.
- Selection Pressure: Grow libraries under subinhibitory concentrations of antibiotics of interest.
- Deep Sequencing: Extract genomic DNA and sequence transposon insertion sites using Tn-seq approaches.
- Bioinformatic Analysis: Identify genes with significant enrichment or depletion under antibiotic selection [4].
- Validation: Confirm hits with targeted knockouts and phenotypic testing.
Integrative Data Analysis and Interpretation
Correlation Analysis Framework
Establishing meaningful correlations between expression data and resistance phenotypes requires appropriate statistical approaches and interpretation frameworks.
Analytical Protocol: Expression-Phenotype Correlation
- Data Transformation: Normalize expression data using appropriate reference genes and resistance data using log2(MIC) transformation.
- Correlation Analysis: Calculate Pearson or Spearman correlation coefficients between expression levels and MIC values across multiple strains/conditions.
- Significance Testing: Apply appropriate multiple testing corrections when analyzing multiple gene-phenotype pairs.
- Threshold Establishment: Define biologically relevant correlation thresholds based on negative controls and known relationships.
Recent studies in H. pylori demonstrate the complexity of these relationships, where hefA and hefD expression was significantly higher in multidrug-resistant strains compared to susceptible ones, yet the relationship was not consistently linear across all resistance profiles [84]. Similarly, research in Mycobacterium abscessus revealed a statistically significant negative correlation (Pearson r = -0.791) between intracellular antibiotic accumulation and MIC values for antibiotics with intracellular targets [4].
Multivariate Analysis Approaches
Single-gene approaches often fail to capture the complexity of efflux-mediated resistance, necessitating multivariate frameworks.
Analytical Protocol: Multivariate Modeling
- Feature Selection: Include expression data for multiple efflux pump components, regulatory genes, and permeability-related genes.
- Model Construction: Build multiple linear regression or machine learning models to predict resistance phenotypes from expression features.
- Model Validation: Use cross-validation or independent test sets to validate prediction accuracy.
- Feature Importance: Calculate relative contribution of different efflux components to overall resistance.
Research Reagent Solutions
Table 3: Essential Research Reagents for Efflux Validation Studies
| Reagent Category | Specific Examples | Application Notes | Key Considerations |
|---|---|---|---|
| Efflux Pump Inhibitors | CCCP, PAβN, verapamil, reserpine | Functional confirmation of efflux activity | Concentration optimization required; potential off-target effects |
| Fluorescent Substrates | Ethidium bromide, Hoechst 33342, rhodamine 6G | Efflux activity assays | Substrate specificity varies between pump systems |
| qPCR Reagents | SYBR Green, TaqMan probes, reverse transcriptase | Gene expression quantification | Validation of reference genes essential for normalization |
| Genetic Manipulation Tools | λ-Red recombinase, sacB counter-selection, tellurite resistance (tpm) | Knockout construction in clinical strains | Alternative selection markers needed for MDR strains |
| LC-MS Standards | Stable isotope-labeled antibiotics | Antibiotic accumulation measurements | Internal standards for precise quantification |
| Cell Viability Assays | Resazurin, CFU plating, OD measurements | Cytotoxicity assessment for inhibitor studies | Distinguish between bactericidal and bacteriostatic effects |
Case Studies and Applications
Validation in Clinical Isolates
Studies in clinical E. coli isolates demonstrate the importance of validation in genetically diverse backgrounds. Research shows that while tolC deletion (disrupting multiple RND efflux systems) abolishes detectable efflux activity in most clinical E. coli strains, the mutant strains often retain multidrug resistance due to the presence of other resistance mechanisms [85]. This highlights the necessity of comprehensive resistance genotyping alongside efflux validation studies.
In one systematic approach, deletion of the central outer membrane efflux channel TolC in 18 clinical MDR E. coli isolates modulated antibiotic susceptibility but did not restore full susceptibility to most antibiotics, emphasizing that efflux inhibition alone may be insufficient to reverse resistance in clinical strains possessing multiple resistance mechanisms [85].
Interplay with Other Resistance Mechanisms
Efflux pumps do not function in isolation, and their validation must consider complex interactions with other cellular processes. Research in Helicobacter pylori reveals intricate cross-talk between efflux pump expression and resistance gene mutations [84]. Strains with specific mutations (A2143G or A2142G in 23S rRNA) exhibited lower hefA expression, while strains with gyrA mutations (87K/91N, 87N/91G, 87K/91D, or 87N/91Y) showed higher hefA expression compared to wild-type strains [84].
Additionally, recent findings demonstrate that efflux activity can promote increased mutation rates by downregulating DNA repair pathways, creating a hypermutatable state that accelerates the evolution of resistance [82]. This relationship creates a concerning feedback loop where efflux not only provides immediate protection but also enhances the potential for developing additional resistance mechanisms.
Validating the impact of efflux pump gene expression on resistance phenotypes requires an integrated, multi-method approach. No single assay provides definitive evidence, and the most robust conclusions draw concordance from expression analysis, functional assays, and genetic manipulation. The field continues to evolve with new technologies such as real-time efflux monitoring [83] and direct antibiotic accumulation measurement [4] providing increasingly sophisticated validation tools.
For researchers in antibiotic discovery and development, rigorous efflux validation in clinically relevant strains remains essential, as overreliance on laboratory strains may overestimate the potential of efflux inhibition strategies [85]. Future directions include standardized validation pipelines, high-throughput screening approaches, and integrated models that account for the complex interplay between efflux, permeability, and other resistance mechanisms.
Antimicrobial resistance (AMR) represents a critical global health threat, with multidrug-resistant (MDR) Gram-negative pathogens presenting particular therapeutic challenges. Efflux pumps of the Resistance-Nodulation-Division (RND) family constitute a primary mechanism of intrinsic and acquired resistance in these pathogens by actively extruding diverse antibiotics from the bacterial cell [86] [15]. This review provides a comparative analysis of RND-type efflux systems in three clinically significant pathogens—Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae—framed within the context of intrinsic resistance research. Understanding the specific efflux machinery, their regulatory networks, and complementary functions in these high-priority pathogens is fundamental to developing novel therapeutic strategies to counteract multidrug resistance.
The RND-type efflux pumps in Gram-negative bacteria function as tripartite complexes that span the entire cell envelope. These complexes typically consist of an inner membrane RND transporter (which provides substrate specificity and energy-coupled transport), a periplasmic membrane fusion protein (MFP), and an outer membrane factor (OMF) channel [86] [87]. This assembly forms a continuous conduit that allows for the direct extrusion of substrates from the cell interior or the periplasm to the external environment, effectively reducing intracellular antibiotic concentrations [86].
Table 1: Major RND Efflux Pumps in A. baumannii, P. aeruginosa, and K. pneumoniae
| Pathogen | Major RND Efflux Pumps | Key Regulatory Elements | Primary Antibiotic Substrates | Clinical & Physiological Relevance |
|---|---|---|---|---|
| A. baumannii | AdeABC, AdeIJK, AdeFGH [88] [26] | AdeRS (TCS) for AdeABC [26] | β-lactams, FQs, TCN, TGC, CHL, ML, aminoglycosides [89] [88] [26] | Most common in MDR clinical isolates; contributes to carbapenem resistance [89] [26] |
| P. aeruginosa | MexAB-OprM, MexXY-OprM, MexCD-OprJ, MexEF-OprN [87] | MexR, NfxB, MexT, MexZ [87] | FQs, β-lactams, AG, TCN, CHL, ML [13] [87] | Major role in intrinsic resistance; MexAB-OprM is constitutively expressed [87] |
| K. pneumoniae | AcrAB-TolC, OqxAB, KexEF, EefABC [90] [91] | AcrR, RamA, OqxR [90] [91] | FQs, β-lactams, TCN, CHL, TPP [90] [91] | Contributes to MDR and virulence in respiratory infections [90] [91] |
Abbreviations: FQs (Fluoroquinolones), TCN (Tetracycline), TGC (Tigecycline), CHL (Chloramphenicol), ML (Macrolides), AG (Aminoglycosides), TPP (Tetraphenylphosphonium), TCS (Two-Component System)
Table 2: Quantitative Data from Key Efflux Pump Studies
| Study Focus / Pathogen | Experimental Finding | Quantitative Result | Citation |
|---|---|---|---|
| A. baumannii (CnSAB vs CSAB) | Relative adeB gene expression | 6.1-fold higher in CnSAB (p=0.002) [89] | [89] |
| A. baumannii (CnSAB vs CSAB) | Biofilm formation (OD₅₅₀) | 1.3-fold higher in CSAB (p=0.021) [89] | [89] |
| K. pneumoniae (Mutant Selection) | Isolation frequency of hyper-MDR mutants | 10⁻⁷ to 10⁻⁹ [91] | [91] |
| K. pneumoniae (AcrAB in Virulence) | Bacterial load in murine pneumonia model (ΔacrB vs WT) | Significantly reduced for mutant [90] | [90] |
Pathogen-Specific Deep Dives
1Acinetobacter baumannii
A. baumannii exemplifies the critical role of RND efflux pumps in clinical antibiotic resistance. Its genome encodes for several RND systems, with AdeABC, AdeIJK, and AdeFGH being the most clinically significant [88] [26]. These systems exhibit functional complementarity, where the deletion of one pump can be partially compensated by the increased activity of another, underscoring the robustness of its efflux defense network [88].
The AdeABC pump, often overexpressed in MDR clinical isolates, has a remarkably broad substrate spectrum that includes fluoroquinolones, β-lactams, tetracyclines (including tigecycline), chloramphenicol, and aminoglycosides [89] [26]. Its expression is tightly controlled by the AdeRS two-component system, where mutations in adeS or adeR are frequently linked to pump overexpression and consequent multidrug resistance [26]. The AdeIJK system is considered the ancestral efflux pump in the Acinetobacter genus and is present in the core genome of all species [26]. Even at its basal, constitutive expression level, it contributes to intrinsic resistance, and its overexpression leads to a broad-spectrum MDR phenotype [26]. The AdeFGH pump, while less prevalent, confers resistance to chloramphenicol, fluoroquinolones, clindamycin, and particularly trimethoprim [88]. Recent structural biology advances, including cryo-EM structures of AdeB, AdeJ, and now AdeG, are revealing the molecular determinants of drug binding and translocation, paving the way for structure-informed inhibitor design [88].
2Pseudomonas aeruginosa
P. aeruginosa possesses a complex and well-characterized efflux pump network that is a major determinant of its high intrinsic resistance to diverse antimicrobial classes [13] [87]. Its low outer membrane permeability works synergistically with active efflux to create a powerful barrier against antibiotics [13].
The four primary RND systems in P. aeruginosa are MexAB-OprM, MexXY-OprM, MexCD-OprJ, and MexEF-OprN [87]. Among these, MexAB-OprM is constitutively expressed and is a key player in intrinsic resistance to β-lactams, fluoroquinolones, and chloramphenicol [87]. Its expression is negatively regulated by the MexR repressor. The MexXY-OprM system is notable for its contribution to aminoglycoside resistance and is inducible by sub-inhibitory concentrations of its substrates, such as ribosome-targeting antibiotics [87]. The MexCD-OprJ and MexEF-OprN pumps are not typically expressed in wild-type strains but their overexpression in mutant isolates leads to resistance to several drug classes, including fluoroquinolones and carbapenems [87]. The complex regulatory hierarchy governing these pumps makes P. aeruginosa highly adaptable to antibiotic pressure.
3Klebsiella pneumoniae
K. pneumoniae leverages its RND efflux pumps not only for antibiotic resistance but also for pathogenesis and survival within the host. The pathogen's genome harbors a rich repertoire of at least 12 RND-type efflux pump genes, underscoring their importance in its physiology and resistance profile [91].
The AcrAB-TolC system is the best-characterized pump in K. pneumoniae. It contributes to resistance against fluoroquinolones, β-lactams, and other compounds [90] [91]. Its expression can be upregulated by mutations in the local repressor acrR or through global regulators like RamA [90]. Beyond resistance, AcrAB-TolC has a demonstrated role in virulence. Isogenic acrB knockouts exhibit increased susceptibility to antimicrobial peptides present in human bronchoalveolar lavage fluid and show a significantly reduced capacity to cause pneumonia in a murine model [90]. Other important pumps include OqxAB, which confers resistance to fluoroquinolones and chlorhexidine, and the more recently characterized KexEF and EefABC systems, which have been identified as powerful exporters in hyper-MDR mutants selected in vitro [91]. These findings highlight that the overexpression of various RND pumps can be a common pathway to the multidrug-resistant phenotype in K. pneumoniae.
Essential Research Tools and Methodologies
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for Efflux Pump Studies
| Reagent / Material | Function / Application | Specific Example(s) |
|---|---|---|
| Strain Panels (Clinical & Reference) | Comparative analysis of gene expression, resistance prevalence, and pump activity across different genetic backgrounds. | A. baumannii ATCC 19606 [88], K. pneumoniae ATCC 10031 (hypersusceptible strain for mutant selection) [91], P. aeruginosa PAO1 [87]. |
| Isogenic Knockout Mutants | Directly determine the contribution of a specific efflux pump gene to resistance and virulence phenotypes. | K. pneumoniae 52145ΔacrB and 52145ΔacrR [90], A. baumannii with deletions in adeB, adeJ, or adeG [88]. |
| Gene Expression Analysis Tools | Quantify relative mRNA levels of efflux pump genes and their regulators. | qRT-PCR primers for adeB, adeG, adeJ in A. baumannii [89]; RT-PCR for acrB and acrR in K. pneumoniae [90]. |
| Fluorescent Substrate Efflux Assays | Functionally measure the real-time activity of efflux pumps in live bacteria. | Ethidium bromide efflux assay [91]; accumulation assays using carbonyl cyanide m-chlorophenyl hydrazone (CCCP) as a proton motive force uncoupler [13]. |
| Cryo-Electron Microscopy (Cryo-EM) | Determine high-resolution 3D structures of efflux pump components to understand substrate binding and transport mechanisms. | Structural determination of AdeB, AdeJ, and AdeG from A. baumannii [88]. |
Standard Experimental Protocols
Protocol 1: Quantitative Real-Time PCR (qRT-PCR) for Efflux Pump Gene Expression
- RNA Extraction: Harvest bacterial cells from cultures grown under conditions of interest (e.g., with/without antibiotic exposure). Use a commercial kit (e.g., Qiagen RNeasy Mini Kit) to isolate total cellular RNA. Treat samples with DNase to remove genomic DNA contamination [89].
- cDNA Synthesis: Reverse transcribe the purified RNA into complementary DNA (cDNA) using a reverse transcriptase enzyme and random hexamer or gene-specific primers.
- qRT-PCR Amplification: Perform quantitative PCR using gene-specific primers for the target efflux pump genes (e.g., adeB, adeG, adeJ) and for a stable reference gene (e.g., 16S rRNA) [89]. Use a SYBR Green or TaqMan-based system to monitor amplification in real-time.
- Data Analysis: Calculate the relative gene expression using a comparative method (e.g., 2^(-ΔΔCt) method), normalizing the expression of the target gene to the reference gene and comparing it to a control strain or condition [89].
Protocol 2: Ethidium Bromide Efflux Assay
- Cell Preparation: Grow bacterial strains to mid-logarithmic phase. Harvest, wash, and resuspend the cells in an appropriate buffer (e.g., phosphate-buffered saline) [91].
- Loading and Energy Depletion: Incubate the cell suspension with ethidium bromide (EtBr). To allow dye influx, pre-treat the cells with a proton motive force uncoupler like CCCP, which inhibits energy-dependent efflux. This step loads the cells with EtBr.
- Efflux Initiation and Measurement: Remove the uncoupler by washing the cells. Resuspend the cells in fresh buffer containing glucose (to re-energize the cells and re-activate efflux pumps). Immediately monitor fluorescence over time using a spectrofluorometer (excitation ~530 nm, emission ~600 nm). A rapid decrease in fluorescence indicates active efflux of EtBr [91].
- Data Interpretation: Compare the initial rates of fluorescence decrease between different strains (e.g., wild-type vs. overexpressing mutant) to assess relative efflux pump activity.
Protocol 3: Analysis of Efflux Pump Regulators via Mutant Selection
- Mutant Isolation: Plate a high-density culture of a susceptible bacterial strain (e.g., ~10^9 CFU) onto agar plates containing an antimicrobial agent at the MIC or a slightly higher concentration. Incubate and count the resulting colonies to determine the mutation frequency [91].
- Phenotypic Screening: Test the resistant mutants for cross-resistance to other antimicrobial agents (e.g., dyes, disinfectants, antibiotics of different classes) to identify those with a multidrug-resistant phenotype suggestive of efflux pump overexpression [91].
- Genotypic Characterization: Sequence the genes encoding the efflux pumps and their known local and global regulators (e.g., adeRS in A. baumannii, acrR or ramA in K. pneumoniae) in the hyper-MDR mutants to identify mutations responsible for the phenotype [91] [26].
- Functional Validation: Quantify the expression level of the efflux pump operon in the mutant via qRT-PCR and confirm its role by constructing an isogenic knockout to see if the hyper-resistance is abolished [91].
Regulatory Networks and Visualization
The expression of RND efflux pumps is controlled by a sophisticated interplay of dedicated local regulators and global regulatory networks. In A. baumannii, the expression of the critical adeABC operon is primarily governed by the AdeRS two-component system. The histidine kinase, AdeS, senses environmental stimuli (e.g., antibiotics) and autophosphorylates. The phosphate group is then transferred to the response regulator, AdeR, which binds to the intercistronic region between adeR and adeA to activate transcription [26]. Mutations in adeRS are a common mechanism of pump overexpression in clinical isolates. In K. pneumoniae, the expression of acrAB can be repressed by the local repressor AcrR, and derepression occurs through mutations in acrR or via activation by global regulators like RamA [90] [91]. The regulatory pathways for these pumps can be visualized in the following diagram.
Diagram Title: Efflux Pump Regulatory Pathways
The experimental workflow for investigating the role of efflux pumps in resistance, from mutant selection to mechanistic validation, integrates several core protocols as shown below.
Diagram Title: Experimental Workflow for MDR Mutant Analysis
The comparative analysis of A. baumannii, P. aeruginosa, and K. pneumoniae reveals both shared and pathogen-specific strategies for employing RND efflux pumps as a primary defense mechanism. While all three utilize tripartite RND systems to achieve multidrug resistance, key differences exist in their predominant pumps, regulatory circuits, and the integration of efflux with other physiological processes like virulence. The functional complementarity among pumps within a single pathogen, as seen in A. baumannii, and the role of pumps in virulence, as in K. pneumoniae, highlight the complexity of this resistance mechanism.
Future research should focus on exploiting this knowledge to develop novel therapeutic agents. The detailed cryo-EM structures of pumps like AdeB, AdeJ, and AdeG provide a blueprint for the rational design of efflux pump inhibitors (EPIs) that could block substrate binding or transport [88]. An alternative approach is to target the regulatory pathways that control pump overexpression; inhibiting the AdeRS system in A. baumannii, for instance, could prevent the upregulation of AdeABC and re-sensitize the bacterium to existing antibiotics [26]. Combining such EPIs or regulatory disruptors with conventional antibiotics represents a promising strategy to break through efflux-mediated resistance and restore the efficacy of our antimicrobial arsenal against these formidable pathogens.
The rise of multidrug-resistant (MDR) Escherichia coli represents a critical global health threat, significantly complicating the treatment of common infections. Among the various mechanisms driving this resistance, the overexpression of efflux pumps, particularly the AcrAB-TolC system, has emerged as a fundamental contributor. This tripartite efflux system actively exports a wide range of antimicrobial agents from bacterial cells, reducing intracellular drug concentrations and diminishing treatment efficacy. A comprehensive understanding of the correlation between acrAB overexpression and antibiotic resistance is essential for developing novel therapeutic strategies to combat MDR pathogens. This whitepaper synthesizes evidence from systematic reviews and meta-analyses to elucidate this critical relationship, providing researchers and drug development professionals with consolidated insights into efflux pump-mediated resistance mechanisms.
The AcrAB-TolC Efflux Pump: Structure and Function
The AcrAB-TolC efflux pump is a tripartite system that spans the entire cell envelope of Gram-negative bacteria like E. coli. This complex consists of three primary components: AcrB, an inner membrane transporter that belongs to the Resistance-Nodulation-Division (RND) family; AcrA, a periplasmic adaptor protein that structurally links AcrB to TolC; and TolC, an outer membrane channel that serves as the final exit pathway for substrates [42] [92]. The system functions as a proton antiporter, utilizing the proton motive force to energize the extrusion of diverse antimicrobial compounds from the cell interior to the external environment [15].
This efflux system demonstrates remarkably broad substrate specificity, encompassing multiple classes of antibiotics including fluoroquinolones, β-lactams, aminoglycosides, tetracyclines, and macrolides [42] [92]. The operational mechanism involves a sophisticated rotational cycle within the AcrB trimer, which recognizes and binds substrates within its transmembrane domains, subsequently undergoing conformational changes that facilitate substrate translocation through the TolC channel [37]. This versatile extrusion capability positions AcrAB-TolC as a primary determinant of intrinsic and adaptive resistance in E. coli.
Table 1: Components of the AcrAB-TolC Efflux Pump
| Component | Location | Function | Family |
|---|---|---|---|
| AcrB | Inner membrane | Substrate recognition and transport; energy transduction | RND transporter |
| AcrA | Periplasmic space | Structural adaptor; connects AcrB to TolC | Membrane fusion protein (MFP) |
| TolC | Outer membrane | Outer membrane channel; final exit pathway | Outer membrane factor (OMF) |
Regulatory Mechanisms Governing acrAB Expression
The expression of the acrAB-tolC operon is tightly regulated by complex transcriptional networks that respond to various environmental stressors. Key regulatory proteins include MarA, SoxS, and Rob, which activate acrAB transcription in response to antibiotic exposure, oxidative stress, and other toxic insults [42] [92]. These global regulators bind to specific sequences in the acrAB promoter region, initiating transcription and enhancing the bacterium's capacity to expel harmful compounds.
The MarA protein, encoded by the multiple antibiotic resistance (mar) operon, serves as a master regulator of the bacterial stress response. Early research demonstrated that mar mutants incapable of functional AcrAB expression failed to develop significant antibiotic resistance, establishing the central role of AcrAB in the Mar phenotype [93]. Similarly, SoxS activates acrAB expression under conditions of oxidative stress, while Rob contributes to regulation during stationary phase growth [42]. This multilayered regulatory architecture allows fine-tuned control of efflux pump expression in response to diverse environmental challenges, facilitating bacterial adaptation and survival under antibiotic pressure.
Diagram 1: Transcriptional Regulation of acrAB Expression. Environmental stressors activate transcriptional regulators that bind the acrAB promoter, leading to efflux pump expression and antibiotic resistance.
Meta-Analysis Methodology: Systematic Review Approach
Recent systematic reviews and meta-analyses have employed rigorous methodologies to quantitatively assess the relationship between acrAB overexpression and antibiotic resistance. The predominant approach follows Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to ensure comprehensive literature searching, transparent study selection, and robust data synthesis [42] [92].
Search Strategy and Study Selection
Electronic databases including PubMed, Scopus, Google Scholar, and EBSCO are systematically searched using structured queries combining Medical Subject Headings (MeSH) terms and keywords related to "acrAB," "efflux pump," "Escherichia coli," and "gene expression." The search typically encompasses studies published over several decades to capture historical and contemporary evidence. Following initial identification, studies undergo sequential screening based on predefined inclusion and exclusion criteria.
Table 2: Study Selection Criteria in Systematic Reviews
| Category | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Study Design | Experimental studies quantifying acrAB expression | Review articles, case reports, editorials |
| Methodology | qPCR, RNA-seq, or microarray analysis | Studies without molecular expression data |
| Organism | Escherichia coli isolates | Non-E. coli species |
| Intervention | Antibiotic exposure with controls | Genetically modified strains with artificial overexpression |
| Data Reporting | Quantifiable gene expression data | Studies without control groups or specific exposure details |
Data Extraction and Quality Assessment
Eligible studies undergo systematic data extraction using standardized forms, capturing information on bacterial strains, antibiotic exposure conditions, expression measurement techniques, and resistance phenotypes. Quality assessment typically evaluates methodological rigor, including appropriate controls, technical replicates, and statistical analyses. Data synthesis employs random-effects meta-analysis models to account for heterogeneity across studies, with effect sizes expressed as standardized mean differences (SMD) for continuous outcomes and risk ratios (RR) for dichotomous outcomes [42] [92] [94].
Quantitative Evidence: Meta-Analysis Findings
The most recent comprehensive meta-analysis published in 2025 incorporated data from 10 high-quality studies meeting stringent inclusion criteria. The pooled analysis demonstrated a significant increase in acrAB expression in MDR E. coli isolates compared to susceptible strains, with a substantial effect size (SMD: 3.5, 95% CI: 2.1–4.9) [42] [92] [94]. This quantitative synthesis provides robust evidence supporting the central role of acrAB overexpression in clinical antibiotic resistance.
The meta-analysis further revealed that efflux pump inhibition resulted in a ≥4-fold reduction in minimum inhibitory concentrations (MICs) for fluoroquinolones and β-lactams across multiple studies, indicating restoration of antibiotic susceptibility [42]. Risk ratio analysis showed that efflux pump inhibitors significantly restored antibiotic susceptibility (RR: 4.2, 95% CI: 3.0–5.8), underscoring the therapeutic potential of targeting this resistance mechanism [42] [92]. Despite substantial heterogeneity among studies attributed to methodological variations in bacterial strains, antibiotic exposure conditions, and expression measurement techniques, the consistent direction and magnitude of effects strengthen the evidence base.
Table 3: Meta-Analysis Results of acrAB Expression and Resistance Correlation
| Outcome Measure | Effect Size | 95% Confidence Interval | Interpretation |
|---|---|---|---|
| acrAB Expression in MDR vs. Susceptible Strains | SMD: 3.5 | 2.1 – 4.9 | Large, significant increase in MDR isolates |
| Restoration of Susceptibility with EPIs | RR: 4.2 | 3.0 – 5.8 | Significant restoration of antibiotic efficacy |
| MIC Reduction with EPIs | ≥4-fold decrease | N/A | Clinically relevant reversal of resistance |
Experimental Approaches for Assessing Efflux Pump Activity
Molecular Techniques for Expression Analysis
Research on acrAB expression employs sophisticated molecular techniques to quantify transcript levels under various conditions. Quantitative PCR (qPCR) represents the most widely utilized method, offering sensitivity, specificity, and reproducibility for measuring gene expression differences between antibiotic-exposed and control strains [42] [92]. RNA sequencing (RNA-seq) provides a comprehensive, unbiased approach for transcriptome-wide expression profiling, enabling simultaneous assessment of acrAB and related regulatory genes [42]. Microarray analysis, though less frequently employed in recent studies, has contributed historical data on efflux pump expression patterns.
Functional Assays for Efflux Activity
Beyond expression measurement, functional assessment of efflux pump activity provides critical complementary data. Minimum inhibitory concentration (MIC) determination in the presence and absence of efflux pump inhibitors (EPIs) such as phenylalanine-arginine beta-naphthylamide (PAβN) or carbonyl cyanide m-chlorophenylhydrazone (CCCP) offers indirect evidence of efflux-mediated resistance [42] [95]. A ≥4-fold reduction in MIC following EPI exposure signifies substantial efflux contribution to the resistance phenotype. More direct approaches include fluorometric assays using substrate analogs like ethidium bromide to visualize real-time efflux activity, though these are more common in mechanistic studies than clinical isolates.
Diagram 2: Experimental Workflow for Assessing acrAB-Mediated Resistance. Integrated approach combining molecular expression analysis with functional susceptibility testing.
Research Reagent Solutions for Efflux Pump Studies
Table 4: Essential Research Reagents for acrAB Expression and Function Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Efflux Pump Inhibitors | PAβN, CCCP | Functional assessment of efflux contribution to resistance |
| Molecular Kits | RNA extraction kits, cDNA synthesis kits, qPCR master mixes | acrAB expression quantification |
| Antibiotic Standards | Fluoroquinolones, β-lactams, aminoglycosides | Resistance phenotype characterization |
| Reference Strains | E. coli K-12 strains, isogenic mutant sets | Controlled genetic background studies |
| Bioinformatics Tools | RNA-seq analysis pipelines, statistical packages | Expression data processing and meta-analysis |
Therapeutic Implications and Future Directions
The compelling evidence linking acrAB overexpression to clinically significant antibiotic resistance has stimulated active research into efflux pump inhibitors (EPIs) as potential therapeutic adjuvants. These compounds aim to restore antibiotic susceptibility by blocking efflux activity, thereby increasing intracellular drug concentrations [42] [15]. Promising EPI candidates include both synthetic compounds like PAβN and naturally occurring substances such as plant-derived polyphenols [42]. Advances in structure-based drug design have yielded AcrB-targeted inhibitors with refined mechanisms, though clinical translation remains challenging due to toxicity concerns and pharmacokinetic limitations [42] [61].
Future research directions should prioritize the development of safer efflux inhibitors with optimized pharmacological properties, standardization of expression assays to facilitate cross-study comparisons, and exploration of combination therapies that simultaneously target efflux pumps and other resistance mechanisms [42] [15]. Additionally, investigating the interplay between efflux-mediated resistance and other adaptive responses, such as biofilm formation and persister cell development, may reveal novel therapeutic opportunities. The integration of computational approaches, including molecular dynamics simulations to study pump-substrate interactions [37] and machine learning to identify novel EPI candidates [15], represents a promising frontier in overcoming efflux-mediated resistance.
Systematic reviews and meta-analyses provide conclusive evidence that acrAB overexpression significantly correlates with multidrug resistance in E. coli, establishing this efflux pump as a major contributor to treatment failures. The quantitative synthesis of available studies demonstrates substantial effect sizes for both expression differences and susceptibility restoration with EPIs, underscoring the clinical relevance of this resistance mechanism. While methodological variations across studies introduce heterogeneity, the consistent direction of effects strengthens confidence in these findings. For research and drug development professionals, these insights highlight the critical importance of considering efflux activity in antibiotic development programs and resistance management strategies. Future progress in combating multidrug-resistant infections will likely depend on successfully translating this knowledge into effective therapeutic approaches that neutralize efflux-mediated resistance.
1 Introduction
In the ongoing battle against antimicrobial resistance (AMR), efflux pump inhibitors (EPIs) represent a promising therapeutic strategy to restore the efficacy of existing antibiotics. Efflux pumps, membrane-bound transporter proteins that actively extrude toxic compounds, are a major component of intrinsic resistance in many clinically relevant bacterial species [8]. By expelling a wide range of antibiotics, they significantly reduce intracellular drug concentrations, leading to treatment failure [92]. The benchmarking of EPI efficacy across different bacterial species is therefore a critical endeavor in antimicrobial research and development. This guide provides a technical framework for assessing EPI performance, detailing core experimental protocols, data analysis methods, and the essential reagents required for standardized evaluation. This work is situated within the broader thesis that targeting intrinsic resistance mechanisms, particularly efflux, is fundamental to overcoming multidrug-resistant (MDR) infections.
2 Efflux Pump Diversity and Functional Mechanisms
Bacterial efflux systems are categorized into several superfamilies based on their structure and energy source. The most clinically significant in Gram-negative bacteria are the Resistance-Nodulation-Division (RND) family pumps, such as E. coli's AcrAB-TolC and P. aeruginosa's MexAB-OprM, which form tripartite complexes spanning both the inner and outer membranes to expel substrates directly into the external environment [8]. Other major families include the ATP-Binding Cassette (ABC) superfamily, which uses ATP hydrolysis, and the Major Facilitator Superfamily (MFS), which utilizes the proton motive force [8] [96].
A key concept in efflux-mediated resistance is the peristaltic pump mechanism of RND transporters like AcrB. This process involves conformational changes across three protomers—Loose (L), Tight (T), and Open (O)—that collectively bind and extrude substrates [8]. EPIs can disrupt this process by binding to the transporter and blocking substrate recognition or extrusion.
The following diagram illustrates the functional cycle of a typical RND efflux pump and the potential inhibition sites for EPIs.
Diagram: Functional Cycle and Inhibition of an RND Efflux Pump. The pump cycles through Loose (access), Tight (binding), and Open (extrusion) states to expel substrates (e.g., antibiotics). EPIs can block this process by binding to the Tight or Open states.
3 Quantitative Benchmarking of EPI Efficacy
The efficacy of an EPI is quantitatively assessed by its ability to lower the Minimum Inhibitory Concentration (MIC) of a co-administered antibiotic and to increase intracellular drug accumulation. The table below summarizes key quantitative findings from recent studies, highlighting the variable performance of EPIs across different bacterial species and efflux systems.
Table 1: Benchmarking EPI Efficacy Across Bacterial Species and Efflux Systems
| Bacterial Species | Efflux Pump(s) | EPI Tested | Antibiotic Potentiated | Key Efficacy Metric | Reference |
|---|---|---|---|---|---|
| Escherichia coli | AcrAB-TolC | Various (Meta-analysis) | Fluoroquinolones, β-lactams | ≥4-fold MIC reduction; Susceptibility Restoration (RR: 4.2) [92] | |
| Staphylococcus aureus | NorA (MFS) | Flupentixol | Ciprofloxacin | Synergy in vitro & in vivo; Stable docking with NorA [97] | |
| Pseudomonas aeruginosa | MexEF-OprN | (Genetic inactivation studied) | (Intrinsic resistance) | Altered virulence & QS; 90% mortality in murine model (∆mexEF) [46] | |
| Nocardia farcinica | Nfa56470 (MFS) | CCCP, other EPIs | Ciprofloxacin | 4- to 64-fold MIC reduction [96] | |
| Mycobacterium abscessus | Multiple (e.g., MmpL/S) | (Genetic study) | Linezolid, others | >1000-fold variation in drug accumulation identified [4] |
Abbreviations: RR: Risk Ratio; MIC: Minimum Inhibitory Concentration; QS: Quorum Sensing.
4 Core Experimental Protocols for EPI Assessment
A robust assessment of EPI efficacy requires a multi-faceted experimental approach, combining phenotypic, genotypic, and functional assays.
4.1 Minimum Inhibitory Concentration (MIC) Reduction Assay This is the primary phenotypic assay for evaluating an EPI's ability to restore antibiotic susceptibility.
- Method: A standard broth microdilution is performed according to CLSI guidelines [97]. Briefly, a 96-well microtiter plate is prepared with a serial two-fold dilution of the antibiotic. The EPI is added to the wells at a sub-inhibitory concentration. Each well is then inoculated with a standardized bacterial suspension (e.g., 5 × 10^5 CFU/mL). After incubation (e.g., 24 h at 37°C), the MIC is determined as the lowest antibiotic concentration that prevents visible growth. The addition of a redox indicator like resazurin can aid in visualizing bacterial growth [97].
- Data Analysis: The MIC in the presence of the EPI is compared to the MIC of the antibiotic alone. A ≥4-fold reduction in MIC is typically considered indicative of significant efflux pump inhibition [92].
4.2 Intracellular Antibiotic Accumulation Assay This assay directly measures the EPI's functional impact on drug concentration inside the cell.
- Method: Bacterial cultures are exposed to the antibiotic in the presence or absence of the EPI. After incubation, the cells are extensively washed to remove extracellular drug. The bacterial pellet is then lysed, and the intracellular antibiotic is quantified. While fluorometry is common, Liquid Chromatography-Mass Spectrometry (LC-MS) offers superior specificity and sensitivity for direct antibiotic quantification, as demonstrated in M. abscessus [4].
- Data Analysis: Accumulation is expressed as the ratio of intracellular to extracellular drug concentration or as a relative increase compared to the no-EPI control. A significant increase in accumulation confirms that the EPI is blocking drug efflux.
4.3 Gene Expression Analysis via Quantitative PCR (qPCR) This protocol assesses whether an EPI acts by downregulating efflux pump gene expression.
- Method: Bacterial RNA is extracted from cultures treated with the EPI, an antibiotic, or a combination, and an untreated control. The RNA is reverse-transcribed into cDNA. qPCR is performed using primers specific to the target efflux pump genes (e.g., acrB, norA) and housekeeping genes (e.g., rpoB, gyrB) for normalization [92] [96].
- Data Analysis: Gene expression levels are calculated using the comparative Ct (ΔΔCt) method. Significant downregulation of efflux pump genes in the presence of the EPI suggests a transcriptional-level mechanism of action.
The workflow below illustrates how these core protocols are integrated to provide a comprehensive assessment of EPI performance.
Diagram: Integrated Workflow for Comprehensive EPI Efficacy Assessment. The workflow combines phenotypic (MIC), functional (accumulation), and genotypic (qPCR) assays to benchmark EPI performance from multiple angles.
5 The Scientist's Toolkit: Key Research Reagents
Successful execution of EPI benchmarking studies requires a suite of reliable reagents and tools.
Table 2: Essential Research Reagents for EPI Studies
| Reagent / Solution | Function and Application | Examples / Specifications |
|---|---|---|
| Reference Bacterial Strains | Provide a standardized genetic background for consistent, reproducible assays. | ATCC strains (e.g., S. aureus ATCC 25923, P. aeruginosa ATCC 9027) [97]. |
| Clinical/MDR Isolates | Evaluate EPI efficacy against relevant, hard-to-treat resistance phenotypes. | Genetically characterized isolates from biobanks [92]. |
| Validated EPIs | Serve as positive controls to validate experimental systems. | PAβN, CCCP [96]. |
| Candidate EPIs | Novel or repurposed compounds under investigation. | Flupentixol, plant-derived compounds (e.g., berberine) [97] [98]. |
| Culture Media | Support bacterial growth under standardized conditions for susceptibility testing. | Mueller-Hinton Broth (MHB) and Agar (MHA) [97]. |
| Detection Reagents | Enable quantification of bacterial growth or intracellular antibiotic accumulation. | Resazurin dye (for MIC) [97]; LC-MS instrumentation & solvents [4]. |
| Nucleic Acid Kits | Isolate and prepare genetic material for expression analysis. | RNA extraction kits, reverse transcription kits, qPCR master mixes [96]. |
6 Data Analysis and Interpretation
Interpreting data from EPI studies requires careful consideration of several factors. The degree of MIC reduction (e.g., 4-fold vs. 64-fold) directly correlates with the potency of the EPI [96]. However, it is critical to rule out inherent antibacterial activity of the EPI itself by testing it alone. Furthermore, the correlation between efflux pump gene expression and phenotypic resistance is not always straightforward, as post-transcriptional regulation and pump activity also play major roles [92]. The ultimate goal is to establish a clear chain of evidence: the EPI increases antibiotic accumulation and reduces MIC, ideally without affecting bacterial viability on its own, thereby demonstrating targeted efflux inhibition.
7 Conclusion and Future Perspectives
Benchmarking EPI performance is a complex but essential process for revitalizing our antibiotic arsenal. The standardized protocols and benchmarking data outlined in this guide provide a roadmap for researchers to systematically evaluate potential inhibitors. The future of this field lies in overcoming the pharmacological challenges that have hindered the clinical translation of EPIs, such as toxicity and poor pharmacokinetics [8] [92]. Advances in structure-based drug design, informed by a deeper understanding of efflux pump architecture and function, along with the repurposing of existing drugs with known safety profiles, offer promising avenues for developing effective EPI-antibiotic combination therapies to combat multidrug-resistant infections.
Multidrug resistance (MDR) mediated by efflux pumps represents a critical challenge in both antibacterial and anticancer chemotherapy. This whitepaper explores the emerging frontier of dual-function inhibitors capable of targeting efflux systems in both bacteria and cancer cells. These compounds offer a promising strategy to overcome intrinsic resistance by blocking the transporter proteins responsible for extruding antimicrobial and chemotherapeutic agents from cells. The convergence of resistance mechanisms between these disparate cell types presents a unique opportunity for therapeutic intervention, potentially revitalizing obsolete drugs and enhancing treatment efficacy across medical domains. This technical guide synthesizes current research, experimental methodologies, and structural insights to provide a foundation for rational drug design in this innovative field.
Efflux pumps are transmembrane transporter proteins that actively export toxic substances, including antibiotics and chemotherapeutic agents, from cellular interiors. This extrusion mechanism significantly reduces intracellular drug accumulation, conferring a multidrug resistance (MDR) phenotype that diminishes treatment efficacy across diverse medical contexts [99] [15]. In bacteria, efflux pump overexpression contributes substantially to antimicrobial resistance (AMR), identified by the World Health Organization as a critical global health threat associated with millions of deaths annually [99]. Similarly, in cancer cells, induced resistance to chemotherapeutic agents mediated by efflux pumps contributes significantly to treatment failure and disease progression [99].
The intrinsic resistance conferred by efflux pumps stems from their broad substrate specificity. Individual pumps can recognize and extrude multiple structurally unrelated compounds, creating a formidable cellular defense mechanism. Six major families of efflux pumps have been characterized: ATP-binding cassette (ABC), resistance-nodulation-division (RND), major facilitator superfamily (MFS), multidrug and toxic compound extrusion (MATE), small multidrug resistance (SMR), and proteobacterial antimicrobial compound efflux (PACE) [8] [15] [61]. Of these, RND pumps in Gram-negative bacteria and P-glycoprotein (an ABC transporter) in cancer cells represent particularly challenging therapeutic targets due to their central role in clinical multidrug resistance [99] [61].
Scientific Basis for Dual-Function Inhibition
Structural and Functional Similarities
The fundamental premise underlying dual-function inhibitor development is the conserved mechanisms and structural homology between bacterial and mammalian efflux transporters. Despite their evolutionary divergence, both bacterial and cancer cell efflux pumps perform analogous functions—recognizing and extruding diverse xenobiotics—often through similar architectural principles [99]. Notably, some bacterial and mammalian efflux pumps share the same or structurally similar ligands, creating opportunities for cross-domain inhibition [99].
RND transporters in bacteria and P-glycoprotein in human cells represent particularly compelling targets for dual inhibition approaches. Both function as polyspecific transporters with broad substrate recognition capabilities, both utilize energy-dependent extrusion mechanisms (proton motive force for RND pumps, ATP hydrolysis for P-glycoprotein), and both contribute significantly to clinical drug resistance when overexpressed [99] [61]. Molecular dynamics simulations have revealed detailed conformational cycling during substrate transport in RND pumps like AcrB, providing structural blueprints for targeted inhibition [12].
Therapeutic Potential and Applications
The identification of compounds with dual reversal activity offers strategic advantages for combating both antibacterial and cancer multidrug resistance simultaneously [99]. From a therapeutic perspective, dual inhibitors could potentially:
- Resensitize resistant pathogens to conventional antibiotics when administered in combination
- Enhance chemosensitivity of resistant cancer cells to existing antineoplastic agents
- Reduce complexity in co-treatment regimens targeting co-morbid infections and cancers
- Provide insights for rational drug design through comparative structural biology
Conversely, identifying dual inhibitors also helps characterize selective inhibitors for specific pumps by understanding structural features to avoid during targeted development [99]. For instance, selective NorA (S. aureus efflux pump) inhibitors would ideally avoid concomitant P-glycoprotein inhibition to prevent potential adverse effects on drug metabolism and distribution [99].
Promising Compound Classes and Structural Features
Pyranopyridine Derivatives
The pyranopyridine scaffold represents a novel structural class with demonstrated efficacy against RND-type efflux pumps in Enterobacteriaceae. MBX2319 (3,3-dimethyl-5-cyano-8-morpholino-6-(phenethylthio)-3,4-dihydro-1H-pyrano[3,4-c]pyridine) emerged from high-throughput screening as a potent inhibitor of AcrB, the major efflux pump in E. coli [100]. Structure-activity relationship (SAR) studies of 60 MBX2319 analogs identified key modifications that enhance potency, metabolic stability, and solubility:
- The morpholinyl group at position 8 can be replaced with various amine functionalities while maintaining activity
- The phenethylthio moiety at position 6 tolerates significant structural variation, with certain aromatic and heteroaromatic enhancements improving potency
- The gem-dimethyl functionality at position 3 is critical for maintaining efflux inhibitory activity
- The nitrile group at position 5 is sterically hindered but can be modified to carboxamide or N-hydroxyamidine derivatives [100]
Several optimized pyranopyridine derivatives (22d-f, 22i, and 22k) demonstrated significantly improved efficacy compared to MBX2319 in potentiating antibacterial activity of levofloxacin and piperacillin against E. coli [100].
Piperine Analogs and QSAR Insights
Piperine analogs have shown notable activity as efflux pump inhibitors against NorA in Staphylococcus aureus. Quantitative structure-activity relationship (QSAR) analysis of these compounds identified three critical descriptors governing inhibition efficacy:
- Partial negative surface area (Jurs_PNSA-1): Positively correlates with inhibitory activity
- Molecular shadow in the XZ plane (Shadow_XZ): Inversely proportional to inhibitory activity
- Heat of formation: Related to molecular stability and inhibitory potential [101]
The resulting QSAR model (r² = 0.962, q² = 0.917) demonstrated excellent predictive power for NorA inhibition, providing valuable insights for designing natural product-derived efflux pump inhibitors [101].
Table 1: Key Compound Classes with Dual-Target Potential
| Compound Class | Primary Target | Potential Secondary Target | Key Structural Features |
|---|---|---|---|
| Pyranopyridine derivatives | AcrB (E. coli) | P-glycoprotein (indicated by systematic review) [99] | Sterically hindered nitrile, morpholinyl group, phenethylthio moiety, gem-dimethyl groups [100] |
| Piperine analogs | NorA (S. aureus) | P-glycoprotein (theoretical potential) [99] [101] | Partial negative surface area, planar molecular shadow, optimized heat of formation [101] |
| MBX2319 analogs | RND pumps (Enterobacteriaceae) | Undetermined cancer MDR pumps | Modified amine groups at position 8, varied thioether moieties at position 6 [100] |
Experimental Approaches and Methodologies
Systematic Identification Protocols
A rigorous systematic review approach has been developed to identify compounds with demonstrated activity against both antimicrobial and cancer MDR efflux pumps. The protocol follows PRISMA-P guidelines and includes the following methodological elements:
- Database interrogation: Comprehensive searching of PubMed and Scopus for peer-reviewed literature published between January 2012 and September 2024
- Eligibility criteria: Inclusion limited to in vitro studies employing methods to detect changes in antibiotic sensitivity of resistant bacteria and chemosensitivity of resistant cancer cells upon treatment with efflux pump inhibitors
- Data extraction: Structured capture of chemical identifiers, bacterial strains, cancer cell lines, methodological approaches, half-maximal inhibitory concentrations (IC₅₀), and other quantitative measures of reversal activity
- Analysis framework: Narrative synthesis with content curation in tabular and graphical formats to facilitate cross-compound comparisons [99]
This systematic approach identified 763 unique records, with 246 selected for full-text review based on eligibility criteria, representing the most comprehensive assessment of dual-function efflux inhibitors to date [99].
Efflux Inhibition Assay Methodologies
Bacterial Efflux Inhibition Assessment
Fluorometric accumulation assays provide direct measurement of efflux pump activity using fluorescent substrate dyes like Hoechst 33342 [102]. Standardized protocols include:
- Cell preparation: Exponential phase bacterial cultures harvested and washed with appropriate buffer
- Dye loading: Incubation with fluorescent substrate in presence and absence of putative inhibitors
- Inhibition quantification: Measurement of intracellular fluorescence accumulation using plate readers or flow cytometry
- Control normalization: Comparison to negative controls (no inhibitor) and positive controls (established EPIs) [102]
Checkerboard susceptibility testing determines the potentiation effect of efflux pump inhibitors on antibiotic activity:
- Serial dilutions of antibiotics and putative EPIs prepared in 96-well microtiter plates
- Bacterial inoculation and incubation under standard growth conditions
- MIC determination for antibiotics alone and in combination with EPIs
- Calculation of fractional inhibitory concentration (FIC) indices to quantify synergy [101]
Cancer MDR Reversal Assessment
Chemosensitivity restoration assays evaluate the ability of compounds to reverse cancer MDR:
- Resistant cancer cell lines treated with chemotherapeutic agents in presence and absence of putative EPIs
- Cell viability assessment using colorimetric (MTT, XTT) or fluorometric assays
- Quantification of reversal fold by comparing IC₅₀ values of chemotherapeutics with and without EPIs
- Specificity verification using sensitive cell lines to confirm MDR-selective reversal [99]
Cellular accumulation studies directly measure chemotherapeutic agent retention:
- Radiolabeled or fluorescent chemotherapeutic drugs incubated with cells
- Intracellular drug quantification using scintillation counting, fluorescence measurement, or mass spectrometry
- Kinetic analysis of drug accumulation over time with and without EPI treatment [99]
Visualization of Key Mechanisms and Workflows
Diagram 1: Comprehensive screening workflow for dual-function efflux pump inhibitors
Diagram 2: Tripartite RND efflux pump structure and inhibition mechanism
Research Reagent Solutions
Table 2: Essential Research Reagents for Efflux Pump Studies
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Fluorescent Substrates | Hoechst 33342, Ethidium Bromide | Efflux activity quantification via accumulation assays | Signal intensity, substrate specificity, cellular toxicity limits [102] |
| Reference EPIs | Phe-Arg-β-naphthylamide (PAβN), 1-(1-Naphthylmethyl)-piperazine (NMP) | Positive controls for inhibition studies | Solubility, stability, specificity for target pumps [100] |
| Model Bacterial Strains | E. coli ATCC, S. aureus 1199B (NorA overexpressing) | Standardized efflux assessment | Growth characteristics, pump expression levels, genetic stability [100] [101] |
| Cancer Cell Models | P-glycoprotein overexpressing lines (e.g., KB-V1, MCF-7/ADR) | MDR reversal assessment | Doubling time, pump expression verification, phenotypic stability [99] |
| QSAR Software | Cerius2, Molecular descriptor packages | Structural optimization and prediction | Descriptor selection, model validation, computational requirements [101] |
Challenges and Future Directions
The development of dual-function efflux pump inhibitors faces several significant challenges that must be addressed to advance this promising field:
Pharmacological Hurdles
Optimal concentration thresholds and tissue distribution represent critical pharmacological barriers. Effective dual inhibitors must achieve therapeutic concentrations at both infection sites and tumor locations, which may have dramatically different microenvironments [8]. Additionally, the structural complexity and substrate promiscuity of efflux mechanisms complicate targeted inhibitor design, as modifications to enhance activity against one pump may diminish efficacy against others [8].
Specificity and Toxicity Concerns
A fundamental challenge lies in achieving sufficient selectivity to avoid disruption of physiological efflux functions. Inhibition of mammalian P-glycoprotein can adversely affect drug metabolism, distribution, and elimination, potentially causing unintended drug-drug interactions [99]. Similarly, broad-spectrum bacterial efflux inhibition may disrupt microbiome homeostasis by compromising native bacterial defense mechanisms [99] [61].
Innovative Screening Approaches
Emerging technologies offer promising avenues to accelerate dual inhibitor discovery:
- Machine learning and QSAR: Advanced computational models can predict dual inhibitory activity based on chemical descriptors, reducing reliance on high-throughput physical screening [15] [101]
- Molecular dynamics simulations: All-atom simulations provide insights into inhibitor binding modes and conformational effects on pump function [12]
- High-content screening platforms: Automated systems enabling parallel assessment of antibacterial and anticancer efflux inhibition
- Natural product exploration: Phylogenetic analysis of archaeal efflux pumps reveals novel structural motifs that could inspire inhibitor design [102]
The systematic review protocol outlined in this whitepaper represents a crucial step in consolidating existing knowledge and establishing a curated database of compounds with demonstrated dual inhibitory activity [99]. This structured approach will facilitate pattern recognition and guide rational design of next-generation efflux pump inhibitors with enhanced efficacy and optimized pharmacological properties.
As research progresses, the integration of structural biology, computational modeling, and sophisticated screening methodologies will be essential to overcome current limitations and realize the therapeutic potential of dual-function efflux pump inhibitors in combating multidrug resistance across medical domains.
Conclusion
Efflux pumps stand as a formidable cornerstone of intrinsic bacterial resistance, profoundly impacting the efficacy of existing antibiotics and complicating the development of new ones. A synthesized understanding from foundational biology to advanced troubleshooting reveals that overcoming this barrier requires a multi-pronged approach. Future directions must prioritize the rational design of novel antibiotics that evade efflux recognition, coupled with the development of safe and effective, clinically viable efflux pump inhibitors. Furthermore, standardizing diagnostic methods to detect efflux-mediated resistance in clinical isolates is crucial for informing stewardship and treatment strategies. Successfully dismantling this intrinsic defense system through integrated research and innovation is essential for restoring the power of our antimicrobial arsenal against multidrug-resistant pathogens.
References
- 1. An overview of the antimicrobial resistance mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604941/]
- 2. Mechanism of antibacterial resistance, strategies and next- ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1444781/full]
- 3. The Three Bacterial Lines of Defense against Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4613276/]
- 4. Efflux pumps and membrane permeability contribute to ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1013027]
- 5. Types and Mechanisms of Efflux Pump Systems and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10974122/]
- 6. Resistance mechanisms – Antibiotic resistance – ReAct [https://www.reactgroup.org/toolbox/understand/antibiotic-resistance/resistance-mechanisms-in-bacteria/]
- 7. Multidrug efflux pumps: structure, function and regulation [https://www.nature.com/articles/s41579-018-0048-6]
- 8. Efflux-Mediated Resistance in Enterobacteriaceae [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382670/]
- 9. Efflux pump [https://en.wikipedia.org/wiki/Efflux_pump]
- 10. Tripartite efflux pumps of the RND superfamily - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10191380/]
- 11. Tripartite assembly of RND multidrug efflux pumps [https://www.nature.com/articles/ncomms10731]
- 12. Molecular Dynamics Computer Simulations of Multidrug RND ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3962194/]
- 13. Role of efflux pump(s) in intrinsic resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC284630/]
- 14. Efflux pump-mediated resistance to new beta lactam ... [https://www.nature.com/articles/s43856-024-00591-y]
- 15. Role of bacterial efflux pumps in antibiotic resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10268834/]
- 16. Understanding the role of drug efflux pumps in biofilms ... [https://www.sciencedirect.com/science/article/abs/pii/S0924857925001396]
- 17. Bacterial Efflux Pumps (null) [https://gosset.ai/targets/bacterial-efflux-pumps/]
- 18. Efflux-Mediated Resistance in Enterobacteriaceae [https://www.mdpi.com/2079-6382/14/8/778]
- 19. Efflux-linked Accelerated Evolution of Antibiotic Resistance at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9699456/]
- 20. Efflux pumps and microbial biofilm formation [https://www.sciencedirect.com/science/article/pii/S1567134823000576]
- 21. Role of bacterial efflux pumps in biofilm formation [https://pubmed.ncbi.nlm.nih.gov/29506149/]
- 22. Modulation of Bacterial Multidrug Resistance Efflux Pumps of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4347946/]
- 23. Integrative review on Acinetobacter baumannii as a multidrug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626374/]
- 24. The Art of War with Pseudomonas aeruginosa [https://www.mdpi.com/2079-6382/12/8/1304]
- 25. Bacterial Multidrug Efflux Pumps at the Frontline of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9032748/]
- 26. Targeting Acinetobacter baumannii resistance-nodulation ... [https://www.nature.com/articles/s44259-024-00074-z]
- 27. MexXY multidrug efflux system of Pseudomonas aeruginosa [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2012.00408/full]
- 28. Multidrug efflux pumps of Pseudomonas aeruginosa show ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1512472/full]
- 29. Inhibition of efflux pumps by FDA-approved drugs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406663/]
- 30. Antimicrobial and Anti-Efflux Machinery of FDA-Approved ... [https://www.mdpi.com/2076-2607/13/6/1227]
- 31. Unveiling the potential of a novel drug efflux pump inhibitor ... [https://www.sciencedirect.com/science/article/abs/pii/S0882401025002384]
- 32. Evaluation of Multidrug Efflux Pump Inhibitors by a New ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0018547]
- 33. Impeding pathways of intrinsic resistance in Escherichia coli ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003443]
- 34. Determination of Drug Efflux Pump Efficiency in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7598683/]
- 35. Heterogeneous efflux pump expression underpins ... [https://elifesciences.org/articles/99752]
- 36. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 37. Escherichia coli resistance mechanism AcrAB-TolC efflux ... [https://www.nature.com/articles/s41598-024-52536-z]
- 38. Efflux MexAB-Mediated Resistance in P. aeruginosa ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7350317/]
- 39. The AcrAB efflux pump contributes to the virulence of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12367648/]
- 40. Decoding MexB efflux pump genes: structural, molecular ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2024.1519737/full]
- 41. Efflux pump gene expression study using RNA-seq in ... [https://pubmed.ncbi.nlm.nih.gov/34886926/]
- 42. Expression of multidrug efflux pump gene acrAB in ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11778-6]
- 43. Gene expression analysis by quantitative PCR [https://bio-protocol.org/exchange/minidetail?id=19104639&type=30]
- 44. Overexpression of efflux pump genes is one of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10783012/]
- 45. Identification of Natural Compound Inhibitors for Multidrug Efflux Pumps of Escherichia coli and Pseudomonas aeruginosa Using In Silico High-Throughput Virtual Screening and In Vitro Validation | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0101840]
- 46. Evolutionary loss of an antibiotic efflux pump increases ... [https://www.nature.com/articles/s41467-025-63284-7]
- 47. A high throughput flow cytometric assay platform targeting transporter inhibition - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4101541/]
- 48. Quantitative high-throughput screening data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4375054/]
- 49. Rapid multiplexed phenotypic screening identifies drug ... [https://pubmed.ncbi.nlm.nih.gov/26832750/]
- 50. Screening Compounds with a Novel High-Throughput ABCB1 ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0060334]
- 51. Cryo-EM as a tool to study bacterial efflux systems and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7946387/]
- 52. Multidrug efflux pumps as main players in intrinsic and ... [https://www.sciencedirect.com/science/article/abs/pii/S136876461630019X]
- 53. Crystal structures of multidrug efflux pump MexB bound ... [https://www.nature.com/articles/s41598-019-40232-2]
- 54. Cryo-EM structure of the Pseudomonas aeruginosa MexY ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11980583/]
- 55. Effectiveness of Efflux Pump Inhibitors as Biofilm Disruptors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6963839/]
- 56. Machine Learning Modeling for ABC Transporter Efflux and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587445/]
- 57. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 58. Towards an interpretable machine learning model for ... [https://www.sciencedirect.com/science/article/pii/S221371652500195X]
- 59. Harnessing machine learning to predict antibiotic ... [https://www.nature.com/articles/s41522-025-00833-4]
- 60. Opportunities and Challenges of Efflux Pump Inhibitors as ... [https://www.glasgowunisrc.org/news/article/10186/Opportunities-and-Challenges-of-Efflux-Pump-Inhibitors-as-a-Solution-for-Antimicrobial-Resistance/]
- 61. Function and Inhibitory Mechanisms of Multidrug Efflux ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.737288/full]
- 62. Bacterial multidrug efflux pumps: Mechanisms, physiology ... [https://www.sciencedirect.com/science/article/pii/S0006291X14009711]
- 63. Efflux pump inhibitors for bacterial pathogens: From bench ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6563736/]
- 64. Multidrug efflux in Gram-negative bacteria: structural ... [https://www.nature.com/articles/s44259-024-00023-w]
- 65. Efflux Resistance Breakers: A New Technology to ... [https://chemrxiv.org/engage/chemrxiv/article-details/68d56baa3e708a764940b12b]
- 66. Fluorescent substrates for flow cytometric evaluation of efflux ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3785545/]
- 67. Fluorescent substrates for flow cytometric evaluation of efflux ... [https://pubmed.ncbi.nlm.nih.gov/23470221/]
- 68. Multidrug efflux in Gram-negative bacteria - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11721645/]
- 69. A historical perspective on the multifunctional outer membrane ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762307/]
- 70. Exploring the principles behind antibiotics with limited ... [https://www.nature.com/articles/s41467-025-56934-3]
- 71. Conformational plasticity across phylogenetic clusters of ... [https://www.nature.com/articles/s41467-025-66751-3]
- 72. Mutations in the proximal binding site and F-loop of AdeJ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12326959/]
- 73. Kinetic control of TolC recruitment by multidrug efflux complexes [https://pmc.ncbi.nlm.nih.gov/articles/PMC2752513/]
- 74. Advances in the Discovery of Efflux as Novel... Pump Inhibitors [https://pmc.ncbi.nlm.nih.gov/articles/PMC10525980/]
- 75. Synergistic effects of antibiotics and efflux pump inhibitors ... [https://pubmed.ncbi.nlm.nih.gov/40613831/]
- 76. The Challenge of Efflux-Mediated Antibiotic Resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4402952/]
- 77. (PDF) The development of efflux to... - Academia.edu pump inhibitors [https://www.academia.edu/90931200/The_development_of_efflux_pump_inhibitors_to_treat_Gram_negative_infections]
- 78. Microbial efflux : tactics and pump inhibition strategies [https://pubmed.ncbi.nlm.nih.gov/21470111/]
- 79. sciencedirect.com/topics/engineering/ efflux - pump [https://www.sciencedirect.com/topics/engineering/efflux-pump]
- 80. JMIR Research Protocols - Identification of Compounds With Potential... [https://www.researchprotocols.org/2025/1/e66197]
- 81. Discovery and implementation of transcriptional biomarkers of ... [https://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-6-59]
- 82. Efflux-linked accelerated evolution of antibiotic resistance ... [https://www.sciencedirect.com/science/article/pii/S1097276522010243]
- 83. Quantitative real-time analysis of the efflux by the MacAB- ... [https://www.nature.com/articles/s42003-021-01997-3]
- 84. The crosstalk between efflux pump and resistance gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11275522/]
- 85. Quantitative contribution of efflux to multi-drug resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6443642/]
- 86. Acinetobacter baumannii Efflux Pumps and Antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7024869/]
- 87. Role of Efflux Pumps on Antimicrobial Resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9779380/]
- 88. Cryo-EM structure and complementary drug efflux activity ... [https://www.sciencedirect.com/science/article/abs/pii/S0969212624005446]
- 89. Comparative analysis of carbapenemases, RND family efflux ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8377947/]
- 90. Klebsiella pneumoniae AcrAB Efflux Pump Contributes to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2798511/]
- 91. The role of RND-type efflux pumps in multidrug-resistant ... [https://www.nature.com/articles/s41598-020-67820-x]
- 92. Expression of multidrug efflux pump gene acrAB in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539121/]
- 93. AcrAB efflux pump plays a major role in the antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC177656/]
- 94. Expression of multidrug efflux pump gene acrAB in ... [https://pubmed.ncbi.nlm.nih.gov/41120967/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1R3QZIpFgeaXQJt8K9w8_oRDFOUkgIho18PKxDpWTR1UFZLoNX&fc=None&ff=20251023005157&v=2.18.0.post22+67771e2]
- 95. of Efflux Pumps Overexpression and OqxAB Contributes to... AcrAB [https://pubmed.ncbi.nlm.nih.gov/35786184/]
- 96. Overexpression of the Major Facilitator Superfamily Efflux ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1708290/full]
- 97. Evaluating the ciprofloxacin potentiation efficacy of ... [https://www.nature.com/articles/s41598-025-24167-5]
- 98. Efflux pump inhibitors from plant compounds: A new ... [https://www.sciencedirect.com/science/article/pii/S0926669025009240]
- 99. Identification of Compounds With Potential Dual Inhibitory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12179561/]
- 100. Structure-Activity Relationships of a Novel Pyranopyridine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4398657/]
- 101. Quantitative structure activity relationship (QSAR) of ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523409002967]
- 102. Identification and characterisation of two functional ... [https://www.nature.com/articles/s44259-024-00036-5]