Intrinsic Antibiotic Resistance: Mechanisms, Key Bacterial Pathogens, and Research Strategies
This article provides a comprehensive analysis of bacterial species possessing intrinsic (natural) antibiotic resistance, a critical challenge in antimicrobial resistance (AMR).
Intrinsic Antibiotic Resistance: Mechanisms, Key Bacterial Pathogens, and Research Strategies
Abstract
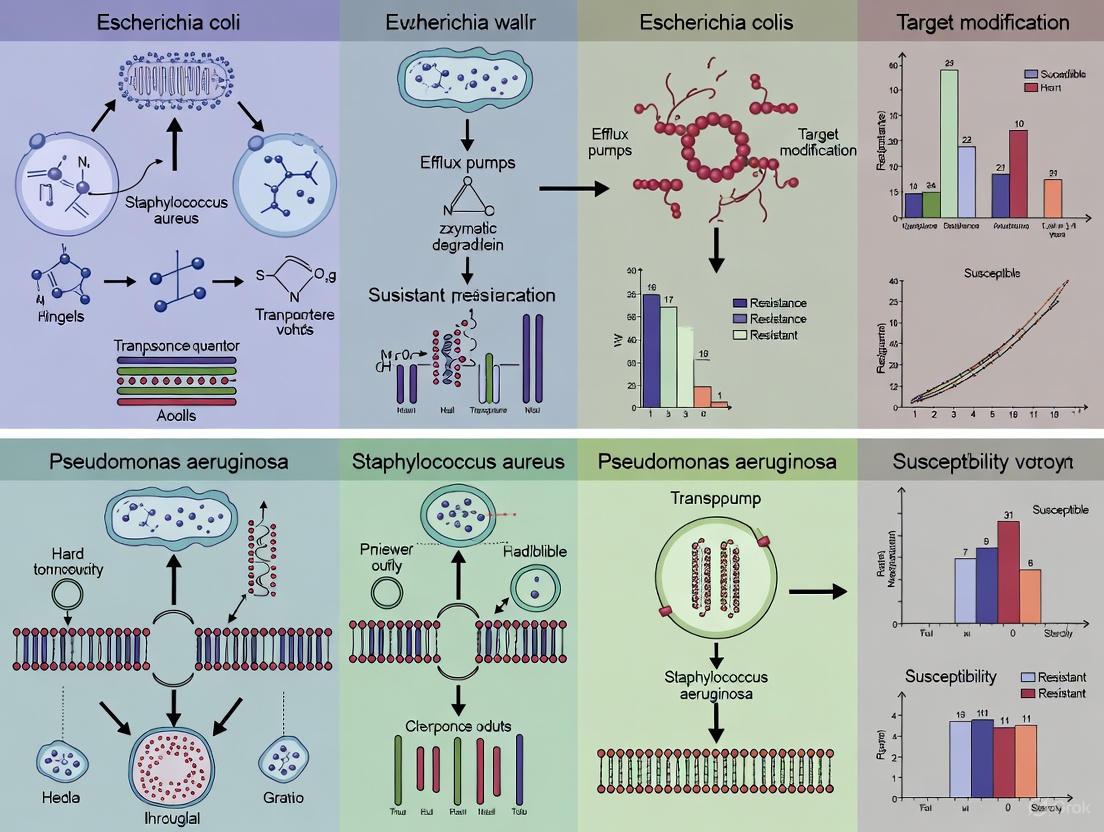
This article provides a comprehensive analysis of bacterial species possessing intrinsic (natural) antibiotic resistance, a critical challenge in antimicrobial resistance (AMR). Aimed at researchers, scientists, and drug development professionals, it explores the foundational mechanisms of innate resistance, details high-priority pathogens from the WHO 2024 list, and examines advanced methodological approaches for studying these bacteria. The content further addresses troubleshooting for R&D hurdles, validates surveillance and comparative analysis frameworks, and synthesizes key strategies to guide the development of novel therapeutics against inherently resistant infections.
The Innate Shield: Unraveling the Core Mechanisms of Natural Antibiotic Resistance
Antimicrobial resistance (AMR) represents one of the most pressing global health crises of the 21st century, threatening to undermine the foundations of modern medicine [1]. In 2019 alone, bacterial infections accounted for 13.6% of all global deaths, with more than 7.7 million fatalities directly attributable to 33 bacterial pathogens [1]. Projections indicate that by 2050, AMR could be responsible for over 10 million deaths annually unless effective countermeasures are developed [1] [2].
Within this crisis, understanding the fundamental distinction between intrinsic and acquired antibiotic resistance is paramount for directing drug discovery efforts. Intrinsic resistance refers to innate capabilities of a bacterial species to withstand antibiotic action, while acquired resistance emerges through genetic changes in previously susceptible strains [3] [4]. This distinction is not merely academic; it shapes diagnostic approaches, therapeutic decisions, and research priorities. For drug development professionals, targeting the immutable mechanisms of intrinsic resistance requires different strategies than countering the adaptable nature of acquired resistance. This whitepaper delineates these critical resistance categories, their molecular foundations, and their implications for developing next-generation antimicrobial therapies.
Defining the Fundamental Resistance Paradigms
Intrinsic Resistance: The Innate Bacterial Armor
Intrinsic resistance, also termed innate or natural resistance, is chromosomally encoded and universally present across all strains of a bacterial species [3]. It is a hereditary trait independent of horizontal gene transfer or previous antibiotic exposure [5] [3]. This form of resistance delineates the natural spectrum of activity for an antibiotic class and is consequently predictable for given bacterial species [3].
Table 1: Mechanisms and Examples of Intrinsic Resistance
| Mechanism | Description | Representative Examples |
|---|---|---|
| Reduced Permeability | Structural barriers prevent antibiotic entry into the cell | Gram-negative outer membrane confers resistance to glycopeptides (e.g., vancomycin) [3] [4] |
| Efflux Pumps | Constitutively expressed pumps export antibiotics | Pseudomonas aeruginosa MexAB-OprM system exports multiple drug classes [3] |
| Enzymatic Inactivation | Chromosomally encoded enzymes degrade or modify antibiotics | P. aeruginosa AmpC β-lactamase hydrolyzes cephalosporins [3] |
| Target Modification | Native antibiotic targets exhibit low drug affinity | Enterococci low-affinity PBP5 confers cephalosporin resistance [3] |
| Absence of Target | Bacteria lack the structure or pathway targeted by the antibiotic | Mycoplasmas lack cell walls, making them resistant to β-lactams [3] |
Acquired Resistance: The Adaptable Bacterial Response
Acquired resistance emerges in previously susceptible bacterial strains through genetic changes that confer the ability to survive antibiotic exposure [6]. This form of resistance is unpredictable, strain-specific, and results from two primary processes: mutations in chromosomal genes or acquisition of foreign genetic material through horizontal gene transfer [5] [6].
Table 2: Mechanisms of Acquired Resistance
| Mechanism | Genetic Basis | Clinical Example |
|---|---|---|
| Enzymatic Inactivation | Acquisition of plasmid-encoded genes | β-lactamase (ESBL) production in E. coli [1] [4] |
| Target Modification | Mutations in chromosomal genes | MRSA via mecA gene encoding alternative PBP2a [1] [4] |
| Enhanced Efflux | Mutation in regulatory genes | Overexpression of efflux pumps in K. pneumoniae [1] |
| Target Bypass | Acquisition of alternative metabolic pathways | Vancomycin-resistant enterococci produce D-Ala-D-Lac instead of D-Ala-D-Ala [4] |
| Reduced Permeability | Mutations in porin genes | Carbapenem resistance in Enterobacterales via porin loss [1] |
Methodologies for Investigating Resistance Mechanisms
Experimental Workflow for Differentiating Resistance Types
Core Experimental Protocols
Protocol for Identifying Intrinsic Resistance Mechanisms
Objective: Systematically characterize the molecular basis of intrinsic antibiotic resistance in a bacterial species.
Methodology:
- Comparative Genomic Analysis:
- Perform whole-genome sequencing of multiple type strains using Illumina NovaSeq and Oxford Nanopore platforms
- Identify conserved chromosomal genes encoding resistance determinants through pan-genome analysis
- Annotate putative efflux pump regulators, permeability barriers, and innate enzymatic systems
Membrane Permeability Assessment:
- Utilize nitrocefin diffusion assays to quantify outer membrane permeability
- Employ ethidium bromide accumulation assays with and without efflux pump inhibitors
- Conduct proteomic analysis of membrane fractions via LC-MS/MS to characterize porin profiles
Target Site Characterization:
- Express and purify putative target proteins (e.g., PBPs, DNA gyrase)
- Determine antibiotic binding affinity using surface plasmon resonance (SPR)
- Compare target gene sequences across related susceptible and resistant species
Validation: Create targeted knockout mutants of identified resistance genes using CRISPR-Cas9 systems and confirm hypersusceptibility phenotype through broth microdilution MIC testing [3].
Protocol for Tracking Acquisition of Resistance
Objective: Elucidate genetic mechanisms underlying acquired resistance in clinical isolates.
Methodology:
- Horizontal Gene Transfer Detection:
- Perform plasmid conjugation assays with resistant donor and susceptible recipient strains
- Conduct natural transformation experiments with genomic DNA from resistant strains
- Use PCR-based replicon typing to classify resistance plasmids
Mutation Analysis:
- Sequence candidate resistance genes from pre- and post-treatment isolates
- Identify single nucleotide polymorphisms (SNPs) through variant calling pipelines
- Correlate mutation patterns with resistance phenotype trajectories
Expression Profiling:
- Quantify mRNA expression of efflux pumps and resistance enzymes via RT-qPCR
- Assess regulatory gene mutations through promoter sequence analysis
- Profile global gene expression changes using RNA-seq under antibiotic stress
Validation: Conduct complementation experiments by introducing wild-type genes into mutant backgrounds and assess restoration of susceptibility [5] [6].
The Researcher's Toolkit: Essential Reagents and Platforms
Table 3: Essential Research Reagents for Resistance Mechanism Studies
| Reagent/Platform | Application | Key Function in Resistance Research |
|---|---|---|
| CRISPR-Cas9 Systems | Gene knockout/editing | Functional validation of resistance genes through targeted mutagenesis [3] |
| Broth Microdilution Panels | MIC determination | Gold standard quantification of resistance levels according to CLSI/EUCAST guidelines |
| Long-read Sequencers (Nanopore) | Whole genome assembly | Resolution of mobile genetic elements and complex resistance loci [1] |
| Efflux Pump Inhibitors | Mechanism elucidation | Differentiation between efflux-mediated and other resistance mechanisms |
| β-lactamase Substrates | Enzyme detection | Characterization of extended-spectrum β-lactamases and carbapenemases [4] |
| Surface Plasmon Resonance | Binding affinity studies | Quantification of drug-target interactions in intrinsic resistance [3] |
| Conjugation Assay Systems | HGT monitoring | Tracking plasmid-mediated dissemination of resistance genes [5] |
Implications for Drug Development and Therapeutic Innovation
The strategic distinction between intrinsic and acquired resistance mechanisms directly informs multiple facets of antibiotic drug development. For pathogens exhibiting primarily intrinsic resistance, such as P. aeruginosa and A. baumannii, effective therapeutic approaches must circumvent constitutive barriers like impermeable membranes and multidrug efflux systems [3]. This might involve designing smaller compounds that exploit rare porins, developing efflux pump inhibitors as combination therapies, or creating novel agents that bypass the need to cross certain membrane barriers entirely.
In contrast, combating acquired resistance requires strategies focused on preventing resistance emergence and spread. This includes developing compounds with multiple targets within the same pathogen, creating drugs less susceptible to common enzymatic inactivation mechanisms, and employing stewardship approaches that limit selective pressure [6]. The WHO's critical priority pathogens list, dominated by Gram-negative bacteria with both intrinsic and acquired resistance mechanisms, highlights the clinical urgency of these targeted approaches [1] [7].
Emerging therapeutic avenues include novel antibiotic classes such as lasso peptides and macrocyclic peptides (e.g., zosurabalpin), naturally derived compounds (e.g., corallopyronin, clovibactin), and targeted inhibitors that circumvent existing resistance mechanisms [1]. Additionally, non-antibiotic approaches including bacteriophage therapy, monoclonal antibodies, and virulence factor inhibitors offer promise for overcoming both intrinsic and acquired resistance by targeting bacterial pathogens through alternative mechanisms [8].
The critical distinction between intrinsic and acquired antibiotic resistance provides an essential conceptual framework for directing antimicrobial drug development. Intrinsic resistance, being inherent and predictable, demands pathogen-specific strategies that circumvent constitutive protection mechanisms. Acquired resistance, characterized by its genetic plasticity and transferability, necessitates approaches that forestall evolutionary adaptation and horizontal dissemination. As resistance continues to escalate globally—with current reports indicating that one in six laboratory-confirmed bacterial infections worldwide are now resistant to antibiotic treatments—the strategic allocation of research resources guided by this fundamental distinction becomes increasingly imperative [7]. Future progress against the AMR crisis will depend on integrating this understanding with innovative chemical entities, novel therapeutic modalities, and improved diagnostic precision to preserve the efficacy of antimicrobial therapies for future generations.
Antimicrobial resistance (AMR) poses a critical threat to global health, with intrinsic resistance mechanisms in Gram-negative bacteria presenting particularly formidable challenges. This whitepaper examines the sophisticated cellular fortifications conferred by reduced membrane permeability and active efflux pumps, which function synergistically to limit intracellular antibiotic accumulation. Within the context of bacterial species exhibiting natural antibiotic resistance, we delineate the molecular architecture and operational mechanisms of these barrier systems, present quantitative assessments of their contributions to resistance profiles, and detail experimental methodologies for their investigation. The interplay between these systems not only defines current treatment limitations but also illuminates pathways for novel therapeutic strategies aimed at circumventing resistance in multidrug-resistant pathogens.
The outer membrane (OM) of Gram-negative bacteria constitutes a highly selective permeability barrier that, in synergy with active efflux systems, confers intrinsic resistance to a broad spectrum of antimicrobial agents [9]. This asymmetric bilayer, composed of phospholipids in the inner leaflet and lipopolysaccharides (LPS) in the outer leaflet, provides protection without compromising essential exchange functions [9]. The OM's effectiveness as a barrier stems from its unique structural organization. The LPS molecules, particularly their lipid A components, feature six saturated fatty acid chains (compared to two in typical phospholipids), creating a densely packed, hydrophobic membrane with low fluidity [9]. Strong lateral interactions between LPS molecules, stabilized by divalent cations that bridge anionic groups, further reduce permeability to hydrophobic compounds [9].
Simultaneously, bacteria employ active efflux pumps—proteinaceous transporters that expel toxic substances, including antibiotics, from the cell [10]. These energy-dependent systems recognize substrates based on physicochemical properties rather than defined chemical structures, enabling them to handle remarkably diverse compounds [11]. The combination of these passive and active barrier mechanisms creates a robust defense system that this review will explore in detail, focusing on molecular mechanisms, experimental approaches, and therapeutic implications for drug development professionals.
Molecular Architecture of the Outer Membrane
Lipopolysaccharide Structure and Barrier Function
The structural complexity of LPS is fundamental to the OM's barrier properties. A typical LPS molecule consists of three domains: lipid A, a core oligosaccharide, and the O-antigen polysaccharide [9]. Lipid A, a glucosamine-based phospholipid, forms the membrane-anchoring segment, while the O-antigen extends externally, contributing to serum resistance and immune evasion. Mutants with truncated LPS cores ("deep rough" mutants) exhibit dramatically increased sensitivity to hydrophobic antibiotics, detergents, and bile salts, underscoring the importance of an intact LPS structure for barrier function [9]. The barrier effectiveness is further modulated by LPS modifications, such as the addition of 4-aminoarabinose or phosphoethanolamine to lipid A phosphates in polymyxin-resistant strains. These substitutions reduce the net negative charge of LPS, potentially enabling closer packing of LPS molecules and decreasing binding of cationic antimicrobial peptides [9].
Porin-Mediated Permeation Pathways
Hydrophilic antibiotics, including β-lactams and fluoroquinolones, primarily traverse the OM through porin channels—β-barrel proteins that form aqueous diffusion pores [9]. General diffusion porins, such as OmpF and OmpC in Escherichia coli, permit the passive passage of small hydrophilic molecules based on size, charge, and hydrophobicity. The molecular basis for porin selectivity involves constriction zones lined with acidic and basic residues that create an electric field, influencing the passage of charged molecules [9]. Modifications to porin expression, sequence, or structure represent common resistance strategies. For instance, clinical isolates of Klebsiella pneumoniae frequently show alterations in ompK35 and ompK36 porin genes, contributing to resistance against β-lactams and other hydrophilic antibiotics [12]. Similarly, Pseudomonas aeruginosa can downregulate its major porin OprF to reduce antibiotic uptake [9].
Table 1: Primary Antibiotic Permeation Pathways Across the Gram-Negative Outer Membrane
| Permeation Pathway | Antibiotic Classes | Molecular Determinants | Resistance Mechanisms |
|---|---|---|---|
| Lipid-mediated diffusion | Aminoglycosides, Macrolides, Rifamycins, Novobiocin, Fusidic acid | LPS core structure, Hydrophobicity, Cationic bridges | LPS modifications (e.g., 4-aminoarabinose addition), Increased LPS packing density |
| Porin-mediated diffusion | β-Lactams, Fluoroquinolones, Tetracyclines, Chloramphenicol | Porin expression (OmpF, OmpC, OprF), Size exclusion limit, Charge selectivity | Porin downregulation, Porin mutations altering channel properties, Loss-of-function mutations |
| Self-promoted uptake | Polymyxins, Cationic antimicrobial peptides | Lipid A charge, LPS packing density | Lipid A modifications reducing negative charge, Addition of phosphoethanolamine |
Active Efflux Systems: Architecture and Function
Classification and Energy Coupling
Bacterial efflux pumps are categorized into five major superfamilies based on amino acid sequence, energy coupling mechanism, and structural organization [10] [11]. An understanding of their distinct properties is essential for designing inhibition strategies.
ATP-binding cassette (ABC) superfamily: These primary active transporters utilize ATP hydrolysis to drive substrate translocation across the membrane. ABC transporters typically consist of two transmembrane domains (TMDs) that form the translocation pathway and two nucleotide-binding domains (NBDs) that hydrolyze ATP [10]. They function via an 'alternate access' mechanism, switching between inward-facing and outward-facing conformations [10].
Resistance-nodulation-division (RND) superfamily: Particularly important in Gram-negative bacteria, RND pumps are secondary active transporters that utilize the proton motive force (pmf) for energy. They form sophisticated tripartite complexes spanning the entire cell envelope, consisting of an inner membrane RND transporter (e.g., AcrB), a periplasmic adapter protein (e.g., AcrA), and an outer membrane factor (e.g., TolC) [10] [11].
Major facilitator superfamily (MFS): The largest superfamily of secondary active transporters, MFS pumps utilize proton gradients to extrude substrates and primarily handle single classes of antimicrobials in bacterial pathogens [10].
Multidrug and toxic compound extrusion (MATE) family: These secondary transporters use either proton or sodium ion gradients to export diverse drugs [10].
Small multidrug resistance (SMR) family: Compact secondary transporters with four transmembrane segments that form homotrimers to create a functional efflux channel [11].
Table 2: Major Bacterial Efflux Pump Superfamilies and Their Properties
| Superfamily | Energy Source | Typical Architecture | Representative Systems | Substrate Profile |
|---|---|---|---|---|
| ABC | ATP hydrolysis | 2 TMDs + 2 NBDs | MacAB (multiple species) | Macrolides, peptides, LPS |
| RND | Proton motive force | 12 TMDs; tripartite complex | AcrAB-TolC (E. coli), MexAB-OprM (P. aeruginosa) | Extremely broad: β-lactams, fluoroquinolones, tetracyclines, dyes, detergents |
| MFS | Proton motive force | 12 or 14 TMDs | MdfA (E. coli), NorA (S. aureus) | Fluoroquinolones, tetracyclines, chloramphenicol |
| MATE | Proton/sodium motive force | 12 TMDs | NorM (V. cholerae), PmpM (P. aeruginosa) | Fluoroquinolones, aminoglycosides, dyes |
| SMR | Proton motive force | 4 TMDs (homotrimer) | EmrE (E. coli), QacC (S. aureus) | Disinfectants, dyes, some β-lactams |
RND Pumps: The Gram-Nigh Tripartite Assemblies
The RND-type efflux pumps represent the most clinically significant efflux systems in Gram-negative pathogens due to their extraordinarily broad substrate specificity [10]. The AcrAB-TolC system of E. coli serves as a paradigm for understanding these complex molecular machines. The inner membrane component AcrB (an RND transporter) acts as the substrate recognition and energy transduction module, undergoing conformational changes that facilitate drug transport [11]. The periplasmic adapter protein AcrA forms a bridge between AcrB and the outer membrane channel TolC, creating a continuous conduit from the cytoplasm to the extracellular space [10]. Structural studies have revealed that AcrB functions as a trimer, with each monomer cycling through consecutive loose, tight, and open states in a coordinated rotational mechanism that extrudes substrates [11].
Beyond antibiotic resistance, RND pumps serve fundamental physiological functions. The AcrAB-TolC system in E. coli pumps out bile acids and fatty acids, providing protection in hostile environments like the intestinal tract [11]. In pathogens like Erwinia amylovora, AcrAB homologs contribute to virulence, host colonization, and resistance to plant toxins [11]. The multifunctionality of these systems complicates therapeutic targeting, as complete inhibition may adversely affect bacterial viability or virulence in ways that could potentially be exploited.
Synergistic Barrier Function: Permeability and Efflux
The intrinsic resistance of Gram-negative bacteria emerges not merely from the independent action of the OM barrier and efflux systems, but from their powerful synergy [13]. This cooperative relationship fundamentally defines the resistance profiles of significant pathogens including Acinetobacter baumannii, Pseudomonas aeruginosa, and Burkholderia species [13]. The OM restricts the initial influx of antibiotics, thereby reducing the intracellular concentration that efflux pumps must manage. Simultaneously, efflux systems actively extrude compounds that penetrate the OM, preventing their accumulation to effective levels [13].
This synergy universally protects bacteria from structurally diverse antibiotics, with the OM and efflux pumps selecting compounds based on distinct physicochemical properties [13]. Research indicates that antibiotics can be categorized into specific clusters based on their interactions with these permeability barriers, with each cluster following intrinsic rules of intracellular penetration [13]. For instance, hydrophobic antibiotics that traverse the lipid bilayer are vulnerable to efflux, while hydrophilic antibiotics relying on porins for entry face both reduced influx through porin downregulation and active extrusion.
Diagram 1: Synergy between membrane barriers and efflux. The outer membrane limits initial antibiotic influx, while efflux pumps actively remove compounds that penetrate this barrier, creating a cooperative defense system.
Quantitative analyses reveal that the relative contribution of each component varies significantly across bacterial species. In P. aeruginosa, the exceptionally low permeability of its OM (approximately 100-fold lower than E. coli) combines with potent RND efflux systems to create an extraordinarily robust barrier system [13]. This interspecies variation in permeability barriers explains the differential antibiotic susceptibility patterns observed clinically and highlights the need for pathogen-specific therapeutic approaches.
Quantitative Assessment of Resistance Contributions
The individual and combined contributions of the OM barrier and efflux pumps to antibiotic resistance can be quantified through carefully designed experiments. Comparative studies measuring antibiotic accumulation in wild-type strains versus isogenic mutants with hyperporinated membranes or deleted efflux pump genes have been instrumental in decoupling these effects [13].
Table 3: Quantitative Contributions of Barrier Mechanisms to Antibiotic Resistance
| Bacterial Species | Antibiotic | OM Contribution (Fold Resistance) | Efflux Contribution (Fold Resistance) | Synergistic Effect |
|---|---|---|---|---|
| E. coli | Ciprofloxacin | 2-4x | 4-8x | 8-32x (combined) |
| P. aeruginosa | Levofloxacin | 16-32x | 8-16x | 128-512x (combined) |
| A. baumannii | Carbapenems | 8-16x | 2-4x | 16-64x (combined) |
| K. pneumoniae | β-lactams | 4-8x (porin loss) | 4-8x (AcrAB) | 16-64x (combined) |
Recent clinical data from K. pneumoniae isolates demonstrate the real-world impact of these mechanisms. Among clinical isolates, the prevalence of the AcrAB efflux system reached 94.54%, while the porin genes ompK35 and ompK36 were present in 96.36% and 98.18% of strains, respectively [12]. Strains simultaneously possessing efflux and porin modifications were significantly associated with extensively drug-resistant (XDR) and pandrug-resistant (PDR) phenotypes, highlighting the clinical consequences of combined barrier mechanisms [12].
The quantitative understanding of these resistance contributions is increasingly leveraged through systems biology approaches that integrate multiscale data to predict AMR evolution. These models incorporate factors such as mutation rates, fitness costs, and selection pressures to forecast resistance trajectories [14]. The predictability of resistance evolution varies across temporal, biological, and complexity scales, with short-term microevolution exhibiting greater predictability than long-term macroevolution [14].
Experimental Methodologies for Analysis
Assessing Outer Membrane Permeability
Lipid Bilayer Permeability Assay: This method evaluates the diffusion rates of antimicrobial compounds across model membrane systems. Synthetic liposomes incorporating purified LPS or specific phospholipid compositions are created to mimic the native OM environment [9]. A gradient of the test antibiotic is established across the liposome membrane, and uptake is quantified over time using techniques such as fluorescence spectroscopy (for intrinsically fluorescent or labeled antibiotics) or liquid chromatography-mass spectrometry (LC-MS) for direct quantification [9]. This approach allows systematic examination of how specific LPS modifications (e.g., core oligosaccharide truncations, lipid A alterations) influence permeability independent of cellular context.
Porin Permeability Profiling: The role of specific porins in antibiotic uptake can be delineated through multiple approaches. Genetic methods involve creating isogenic strains with deleted or modified porin genes and comparing antibiotic susceptibility profiles and accumulation rates [12]. Electrophysiological approaches incorporate purified porins into planar lipid bilayers and measure ionic currents in the presence of antibiotics, providing information on translocation rates and channel selectivity [9]. Molecular exclusion assays using reconstituted porins in proteoliposomes can directly quantify the diffusion of radiolabeled or fluorescent antibiotics through specific porin channels [9].
Efflux Pump Functional Analysis
Efflux Inhibition Assays: The contribution of active efflux to antibiotic resistance can be quantified using efflux pump inhibitors (EPIs) such as phenylalanine-arginine β-naphthylamide (PAβN) for RND pumps or verapamil for MFS pumps [10] [11]. Minimum inhibitory concentration (MIC) reduction assays compare antibiotic susceptibility in the presence and absence of subinhibitory concentrations of EPIs. A significant reduction (typically ≥4-fold) in MIC with EPI treatment indicates substantial efflux contribution [10]. Ethidium bromide accumulation assays directly measure efflux activity using fluorescent substrates, where increased intracellular fluorescence in the presence of EPIs or in efflux-deficient mutants demonstrates functional efflux [10].
Real-time Efflux Kinetics: Advanced methodologies enable direct quantification of antibiotic efflux kinetics. Intracellular antibiotic concentrations can be monitored in real-time using LC-MS/MS sampling from bacterial suspensions, providing direct measurement of accumulation and efflux rates [13]. Fluorescent antibiotic derivatives or probes enable continuous monitoring of efflux kinetics through fluorescence spectroscopy or flow cytometry, allowing high-throughput screening of efflux activity across multiple conditions [10].
Diagram 2: Experimental workflow for analyzing resistance mechanisms. The integrated approach combines phenotypic screening with genetic and functional characterization to delineate the contributions of specific resistance components.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Membrane Permeability and Efflux Studies
| Reagent/Category | Specific Examples | Research Application | Mechanistic Insight Provided |
|---|---|---|---|
| Efflux Pump Inhibitors | PAβN, CCCP, Verapamil, Reserpine | Functional efflux characterization | Distinguishes efflux-mediated resistance; identifies pump substrates |
| Membrane Permeabilizers | Polymyxin B nonapeptide (PMBN), EDTA, Tris | Barrier function assessment | Evaluates OM integrity; distinguishes intracellular vs. extracellular targets |
| Genetic Tools | Knockout strains (ΔacrB, ΔtolC), Plasmid complementation, Reporter fusions | Mechanism dissection | Isolates contribution of specific genes; studies regulation |
| Chemical Probes | Ethidium bromide, Hoechst 33342, N-phenylnaphthylamine | Membrane integrity and fluidity | Measures passive diffusion; monitors membrane organization |
| Antibody Reagents | Anti-OmpA, Anti-LPS core, Anti-AcrA | Protein localization and expression | Quantifies membrane component abundance; visualizes spatial distribution |
| Analytical Standards | (^{14})C-labeled antibiotics, Fluorescent antibiotic derivatives | Uptake and efflux kinetics | Enables precise quantification of antibiotic accumulation |
Therapeutic Implications and Future Directions
The sophisticated understanding of cellular fortifications provided by reduced membrane permeability and efflux pumps informs several promising therapeutic strategies. Efflux pump inhibitors (EPIs) represent a logical approach to counteract efflux-mediated resistance, with the goal of rejuvenating existing antibiotics [10]. Despite significant research investment, no EPI has yet achieved clinical approval, reflecting the challenges of achieving potent inhibition without host toxicity and the redundancy of efflux systems [10]. Innovative approaches include the exploration of natural product inhibitors such as carotenoids, flavonoids, and alkaloids, which may provide novel chemical scaffolds with improved therapeutic indices [11]. Additionally, nanoparticles, particularly zinc oxide, have shown promise as efflux inhibitors, potentially through simultaneous disruption of multiple resistance mechanisms [11].
An alternative strategy involves designing antibiotics that bypass conventional permeability barriers. This includes developing compounds that exploit native uptake systems, such as siderophore-antibiotic conjugates that "hijack" iron acquisition pathways [9]. Another approach focuses on creating molecules with optimized physicochemical properties that evade efflux recognition, potentially through machine learning analysis of pump substrate preferences [10]. The emerging understanding of antibiotic clustering based on permeation rules provides a framework for such rational design approaches [13].
The growing appreciation for the ecological and evolutionary dynamics of resistance development highlights additional intervention points. Within-patient AMR emergence occurs through multiple mechanisms: spontaneous resistance mutations, in situ horizontal gene transfer, selection of pre-existing resistance, and immigration of resistant lineages [15]. The relative importance of each mechanism varies across bacterial species and infection sites, suggesting that personalized approaches considering both pathogen and infection context may be necessary [15]. Quantitative systems-based modeling of resistance evolution, incorporating multiscale data from microbial evolution experiments, offers promise for predicting resistance trajectories and informing antibiotic stewardship paradigms [14].
The cellular fortifications comprising the Gram-negative outer membrane permeability barrier and active efflux systems represent sophisticated defense mechanisms that collectively determine intrinsic antibiotic resistance. Their synergistic action creates a formidable barrier that limits the efficacy of existing antibiotics and complicates the development of new therapeutic agents. A comprehensive understanding of the molecular architecture, functional coordination, and evolutionary dynamics of these systems provides essential insights for overcoming bacterial resistance. Future advances will require integrated approaches combining structural biology, chemical biology, and systems-based modeling to develop innovative strategies that circumvent or neutralize these ancient bacterial defense systems. The application of this knowledge to therapeutic design, coupled with prudent antimicrobial stewardship, offers the best hope for addressing the escalating crisis of antimicrobial resistance.
Antimicrobial resistance (AMR) represents one of the most pressing global public health threats, with drug-resistant infections causing approximately 1.27 million deaths worldwide annually [16]. Among the diverse strategies employed by bacterial pathogens, structural evasion through innate drug target modifications and enzymatic inactivation of antibiotics constitutes a primary defense mechanism that significantly compromises therapeutic efficacy. These resistance mechanisms are particularly concerning in Gram-negative bacteria, which possess a complex cell envelope that acts as an additional permeability barrier, working in concert with enzymatic and target-based resistance strategies [17].
The relentless evolutionary arms race between bacteria and antimicrobial compounds has selected for sophisticated resistance mechanisms that are often encoded on mobile genetic elements, enabling rapid dissemination among bacterial populations [18] [19]. Structural evasion strategies encompass two fundamental approaches: (1) the physical alteration or protection of antimicrobial targets within the bacterial cell, and (2) the enzymatic destruction or chemical modification of antibiotic molecules before they reach their cellular targets. Understanding these mechanisms at molecular and structural levels is crucial for developing novel therapeutic approaches to combat multidrug-resistant pathogens, particularly within the framework of bacterial species exhibiting natural antibiotic resistance [20] [17].
Molecular Mechanisms of Enzymatic Inactivation
β-Lactamases: Diversity and Classification
β-lactamases represent the most prevalent and diverse family of antibiotic-inactivating enzymes, capable of hydrolyzing the β-lactam ring essential to the antibacterial activity of penicillins, cephalosporins, carbapenems, and monobactams [21] [17]. These enzymes are classified into four molecular classes (A, B, C, and D) based on their amino acid sequences and catalytic mechanisms. Classes A, C, and D are serine hydrolases that utilize an active-site serine residue to catalyze hydrolysis of the β-lactam ring, while class B enzymes are zinc-dependent metallo-β-lactamases that employ metal ions for catalysis [21].
The Ambler classification system categorizes β-lactamases according to their molecular structure and mechanism:
- Class A (Serine-based): Includes TEM, SHV, and CTX-M enzymes, often with extended-spectrum activity (ESBLs)
- Class B (Metallo-β-lactamases): Requires zinc ions for activity, capable of hydrolyzing carbapenems
- Class C (Serine-based): Primarily cephalosporinases (AmpC enzymes)
- Class D (Serine-based): Oxacillinases (OXA-type) with variable activity against carbapenems
Table 1: Major β-Lactamase Classes and Their Properties
| Class | Catalytic Mechanism | Representative Enzymes | Key Substrates | Inhibitors |
|---|---|---|---|---|
| A | Serine hydrolase | TEM-1, SHV-1, CTX-M-15 | Penicillins, early cephalosporins | Clavulanic acid, sulbactam, tazobactam |
| B | Zinc-dependent metallo-enzyme | NDM-1, VIM, IMP | Carbapenems, penicillins, cephalosporins | EDTA, but no clinically available inhibitors |
| C | Serine hydrolase | AmpC, CMY-2 | Cephalosporins, cephamycins | Boronic acid derivatives, avibactam |
| D | Serine hydrolase | OXA-48, OXA-23 | Oxacillin, carbapenems (variable) | NaCl, but limited clinical inhibition |
Aminoglycoside-Modifying Enzymes (AMEs)
Aminoglycoside-modifying enzymes (AMEs) represent another major group of antibiotic-inactivating enzymes that catalyze the chemical modification of aminoglycoside antibiotics through three primary mechanisms: N-acetylation (acetyltransferases), O-adenylylation (adenylyltransferases), and O-phosphorylation (phosphotransferases) [21] [17]. These modifications occur at key amino or hydroxyl groups essential for antibiotic binding to the bacterial 16S ribosomal RNA, thereby reducing drug affinity for its target and diminishing antibacterial activity.
The genetic encoding of these enzymes varies, with many found on mobile genetic elements such as plasmids and transposons, facilitating horizontal gene transfer between bacterial strains and species. This mobility has contributed to the widespread distribution of AMEs across clinically important pathogens, significantly limiting the therapeutic utility of aminoglycoside antibiotics [17].
Drug Target Modification Mechanisms
Alteration of Penicillin-Binding Proteins (PBPs)
Bacteria can evade β-lactam antibiotics through modifications to penicillin-binding proteins (PBPs), which are the molecular targets for this drug class. These alterations include mutations that reduce antibiotic binding affinity, acquisition of low-affinity PBPs from other bacterial species, and overexpression of native PBPs [18]. Methicillin-resistant Staphylococcus aureus (MRSA) represents the most clinically significant example, possessing the mecA gene that encodes PBP2a, a transpeptidase with markedly reduced affinity for β-lactam antibiotics [19].
In Gram-negative bacteria, PBP modifications contribute to resistance, though often to a lesser extent than β-lactamase production. In E. coli, mutations in PBP3 can confer resistance to specific β-lactams like ceftazidime and aztreonam, while maintaining susceptibility to other β-lactam antibiotics. This specificity highlights the precise structural relationship between PBPs and their antibiotic inhibitors [18].
Ribosomal Protection and Modification
Bacteria employ several strategies to protect or alter ribosomal targets from antibiotic inhibition. Methylation of specific nucleotides within the ribosomal RNA represents a particularly effective mechanism, as exemplified by Erm methylases that add methyl groups to the A2058 residue in 23S rRNA, conferring resistance to macrolide, lincosamide, and streptogramin B antibiotics (MLSᵦ phenotype) [19].
Another significant mechanism involves mutations in genes encoding ribosomal proteins or rRNA, which can reduce antibiotic binding affinity without compromising essential ribosomal functions. For instance, mutations in the L4 and L22 ribosomal proteins or in 23S rRNA can confer resistance to macrolide antibiotics by altering the drug-binding pocket in the ribosomal tunnel [19].
Table 2: Bacterial Antibiotic Target Modification Mechanisms
| Target Site | Antibiotic Class | Resistance Mechanism | Key Genetic Determinants | Example Pathogens |
|---|---|---|---|---|
| Ribosomal subunit (30S) | Aminoglycosides | rRNA methylation | ArmA, RmtA-E | K. pneumoniae, P. aeruginosa |
| Ribosomal subunit (50S) | Macrolides | rRNA methylation | Erm family | S. aureus, S. pneumoniae |
| Dihydrofolate reductase | Trimethoprim | Mutated enzyme | dfrA, dfrB | UPEC, S. aureus |
| RNA polymerase | Rifampicin | Mutated β-subunit | rpoB mutations | M. tuberculosis, MRSA |
| DNA gyrase/Topoisomerase IV | Fluoroquinolones | Mutated enzymes | gyrA, gyrB, parC, parE | E. coli, K. pneumoniae |
Experimental Methodologies for Investigation
Enzyme Kinetics and Inhibition Assays
Characterizing antibiotic-inactivating enzymes requires robust biochemical assays to determine kinetic parameters and inhibition profiles. The following protocol outlines a standardized approach for β-lactamase activity assessment:
Protocol: β-Lactamase Kinetic Assay Using Nitrocefin Hydrolysis
Reagent Preparation:
- Prepare assay buffer: 50 mM phosphate buffer (pH 7.0) containing 0.1 mg/mL BSA
- Prepare nitrocefin stock solution: 10 mM in DMSO (store protected from light)
- Prepare purified β-lactamase enzyme: Serial dilutions in assay buffer
Kinetic Measurements:
- Add 980 μL assay buffer to spectrophotometer cuvette
- Add 10 μL nitrocefin stock (final concentration 100 μM)
- Initiate reaction by adding 10 μL enzyme preparation
- Immediately monitor absorbance at 482 nm for 5 minutes (ε₄₈₂ = 15,000 M⁻¹cm⁻¹)
Data Analysis:
- Calculate initial velocity from linear portion of progress curve
- Determine kcₐₜ and Kₘ using Michaelis-Menten equation
- For inhibition studies, pre-incubate enzyme with inhibitor for 10 minutes before substrate addition
This spectrophotometric method leverages the chromogenic shift of nitrocefin from yellow (λₘₐₓ = 390 nm) to red (λₘₐₓ = 482 nm) upon β-lactam ring hydrolysis, enabling real-time monitoring of enzyme activity [18] [17].
Molecular Docking and Structural Analysis
Computational approaches provide insights into the structural basis of drug target modifications:
Protocol: Molecular Docking of Antibiotics to Modified Targets
Protein Preparation:
- Obtain crystal structures of wild-type and mutant target proteins from PDB
- Remove water molecules and add hydrogen atoms using molecular modeling software
- Assign partial charges and protonation states appropriate for physiological pH
Ligand Preparation:
- Obtain 3D structures of antibiotic compounds from PubChem or similar databases
- Perform energy minimization using molecular mechanics force fields
- Generate multiple conformations for flexible docking
Docking Simulation:
- Define binding site based on known catalytic residues or co-crystallized ligands
- Perform rigid receptor/flexible ligand docking using AutoDock Vina or similar software
- Run multiple simulations (≥20) with different random seeds to ensure reproducibility
- Analyze binding poses, interaction energies, and hydrogen bonding patterns
This approach enables quantitative comparison of antibiotic binding affinities to wild-type versus modified targets, identifying specific structural alterations responsible for resistance [18] [17].
Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Antibiotic Resistance Mechanisms
| Reagent/Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Chromogenic β-lactam substrates | Nitrocefin, CENTA | β-lactamase activity detection | Colorimetric change upon hydrolysis enables real-time kinetic measurements |
| Recombinant resistance enzymes | Purified β-lactamases, aminoglycoside-modifying enzymes | Biochemical characterization | Enables detailed kinetic studies without bacterial culture requirements |
| Gene expression systems | Inducible plasmids (pET, pBAD) | Heterologous expression | Allows controlled production of resistance proteins in model organisms |
| Antibiotic analogs | Fluorescently-labeled antibiotics, biotin-conjugated drugs | Cellular localization and binding studies | Permits visualization of drug distribution and target engagement |
| Chemical inhibitors | Clavulanic acid, avibactam, boronic acids | Enzyme inhibition profiling | Differentiates between β-lactamase classes and determines inhibition potency |
| Bacterial strain panels | ESKAPE pathogen sets, isogenic mutant collections | Comparative resistance studies | Provides standardized platforms for evaluating resistance mechanisms |
Signaling Pathways and Regulatory Networks
The expression of antibiotic resistance mechanisms is often tightly regulated through complex signaling pathways that sense antibiotic exposure and environmental stresses. The following diagram illustrates the regulatory network controlling the WhiB7-mediated antibiotic resistance in mycobacteria, a key pathway in intrinsic drug resistance:
Regulatory Pathway of WhiB7-Mediated Resistance
This regulatory cascade demonstrates how Mycobacterium abscessus and related species coordinate resistance to multiple antibiotic classes. When ribosome-targeting antibiotics induce ribosomal stress, the transcription factor WhiB7 becomes activated and transactivates a regulon of over 100 genes involved in antimicrobial resistance [20]. Among these genes, Eis2 encodes a protein that modifies aminoglycoside antibiotics through acetylation, rendering them ineffective. Recent research has exploited this pathway by developing prodrug antibiotics that are activated by Eis2, effectively "hacking" the resistance mechanism to enhance drug efficacy [20].
The following experimental workflow outlines a comprehensive approach for investigating antibiotic target modifications:
Workflow for Investigating Target Modifications
Quantitative Analysis of Resistance Prevalence
Surveillance data and clinical studies provide crucial insights into the prevalence and distribution of specific resistance mechanisms across bacterial populations and geographic regions. The following table summarizes key quantitative findings from recent investigations:
Table 4: Prevalence of Key Resistance Mechanisms in Clinical Isolates
| Resistance Mechanism | Pathogen | Antibiotic Affected | Prevalence Rate | Geographic Variation | Source |
|---|---|---|---|---|---|
| ESBL production | Uropathogenic E. coli (UPEC) | β-lactams | 14.6-60% | Significant regional variation | [18] |
| Plasmid-mediated dfrA genes | UPEC | Trimethoprim | Up to 32.1% in U.S. | Higher in recurrent UTIs | [18] |
| Sul gene acquisition | UPEC | Sulfamethoxazole | Correlates with TMP resistance | Regional patterns observed | [18] |
| QRDR mutations | UPEC | Fluoroquinolones | >30% in most regions | Increasing globally | [18] |
| WhiB7 regulon activation | M. abscessus | Ribosomal-targeting | Intrinsic resistance | Consistent across isolates | [20] |
| AcrAB-TolC efflux (overexpression) | UPEC | Multiple classes | High in biofilm-forming isolates | Associated with persistence | [21] |
These quantitative findings highlight the substantial burden of target modification and enzymatic inactivation mechanisms across clinically important pathogens. The data demonstrate significant geographic variation in resistance prevalence, underscoring the need for localized surveillance to inform empirical therapy guidelines and stewardship interventions [18] [22].
Structural evasion through drug target modifications and enzymatic inactivation represents a formidable challenge in clinical management of bacterial infections. The sophisticated molecular mechanisms underlying these resistance strategies, coupled with their rapid dissemination via mobile genetic elements, have contributed significantly to the global AMR crisis. Future research directions should focus on leveraging structural biology insights to design novel antibiotics less susceptible to these evasion strategies, developing combination therapies that target resistance mechanisms directly, and exploring innovative approaches such as resistance "hacking" that repurpose bacterial defense systems for therapeutic benefit [20]. As our understanding of these fundamental resistance mechanisms deepens, so too will our capacity to develop effective countermeasures against multidrug-resistant pathogens.
Antimicrobial resistance (AMR) represents one of the most severe threats to global public health, with drug-resistant bacterial infections causing over 1 million deaths annually and posing a critical challenge to modern medicine [23]. The World Health Organization (WHO) has identified a group of bacterial pathogens of global priority, highlighting the acute threat posed by species with intrinsic and acquired multidrug resistance [24]. These "critical priority" pathogens, primarily Gram-negative bacteria such as Acinetobacter baumannii, Pseudomonas aeruginosa, and carbapenem-resistant Enterobacteriaceae, exhibit a remarkable capacity to resist the effects of most available antibiotics, including the last-resort treatments like carbapenems [23]. Understanding the molecular mechanisms, epidemiology, and research methodologies for these bacteria is fundamental to developing novel countermeasures. This whitepaper provides an in-depth technical profile of these clinically critical intrinsically resistant bacteria within the context of ongoing global research efforts to combat the AMR crisis.
The WHO Priority Pathogens List: A Framework for Threat Assessment
The WHO released its first list of priority bacterial pathogens in 2017, categorizing 12 families of bacteria into critical, high, and medium priority tiers based on urgency for new research and development [24]. This list was designed to guide and encourage the development of new antibiotics. The criteria for this classification included the pathogen's mortality rates, prevalence in community and healthcare settings, ease of transmission, the availability of effective treatments, and whether prevention strategies are possible [23].
In 2024, a second alert was released, regrettably listing almost the same set of bacterial species, underscoring the lack of sufficient progress in developing effective treatments over the intervening years [24]. The critical priority pathogens, which represent the gravest threat, are multidrug-resistant bacteria that primarily cause severe and often fatal infections in hospitalized patients, the elderly, and those using medical devices such as ventilators and blood catheters [23] [25]. These include:
- Acinetobacter baumannii (carbapenem-resistant)
- Pseudomonas aeruginosa (carbapenem-resistant)
- Enterobacteriaceae (e.g., Klebsiella pneumoniae, Escherichia coli, carbapenem-resistant, third-generation cephalosporin-resistant)
The persistence of these pathogens on the WHO list highlights the fragility of the current antibacterial research and development (R&D) ecosystem. As of 2025, the clinical pipeline remains insufficient, with only 90 antibacterial agents in clinical development, a decrease from 97 in 2023. Of these, a mere 5 are effective against at least one of the "critical" priority bacteria [26].
Profiles of Critical Priority Pathogens and Their Resistance Mechanisms
The bacteria designated as critical priority by the WHO are characterized by a formidable array of intrinsic and acquired resistance mechanisms. The following section details the profiles and molecular strategies of the most threatening pathogens.
Table 1: Clinical Impact and Resistance Profiles of Critical WHO Pathogens
| Pathogen | Common Infection Types | Key Intrinsic/Acquired Resistance Mechanisms | Noteworthy Resistance Rates |
|---|---|---|---|
| Acinetobacter baumannii | Bloodstream infections, ventilator-associated pneumonia, wound infections | Production of all four classes of β-lactamases (A, B, C, D); expression of efflux pumps; altered target sites [23]. | Over 80% of isolates were carbapenem-non-susceptible in a 2023-2024 study [25]. |
| Pseudomonas aeruginosa | Pneumonia (especially in CF patients), bloodstream infections, urinary tract infections | Low membrane permeability; constitutive expression of efflux pumps; production of β-lactamases and carbapenemases; biofilm formation [23]. | A leading drug-resistant Gram-negative bacterium in bloodstream infections [7]. |
| Klebsiella pneumoniae | Bloodstream infections, pneumonia, urinary tract infections, intra-abdominal infections | Production of extended-spectrum β-lactamases (ESBLs) and carbapenemases (e.g., KPC, NDM) [7] [23]. | >55% globally resistant to 3rd-gen cephalosporins; >40% of isolates in a recent study were MDR/XDR [7] [25]. |
| Escherichia coli | Urinary tract infections, gastrointestinal infections, bloodstream infections | Production of ESBLs and carbapenemases; plasmid-mediated resistance gene transfer [7] [23]. | >40% globally resistant to 3rd-gen cephalosporins; a leading cause of resistant community and hospital-acquired infections [7]. |
Molecular Mechanisms of Resistance
The resilience of these critical pathogens stems from their diverse and often synergistic resistance strategies, which can be categorized into four main groups:
- Enzymatic Inactivation of Antibiotics: This is a primary mechanism for resistance to β-lactam antibiotics. Pathogens like A. baumannii and K. pneumoniae produce a wide variety of β-lactamase enzymes, including extended-spectrum β-lactamases (ESBLs) and carbapenemases (e.g., KPC, NDM, OXA), which hydrolyze and inactivate the antibiotic molecules [23].
- Reduced Drug Permeability and Efflux Pumps: Gram-negative bacteria have a low-permeability outer membrane that intrinsically restricts the entry of many antibiotics. Furthermore, they express efflux pumps (e.g., in A. baumannii) that actively export multiple classes of antibiotics—such as aminoglycosides, tetracyclines, and fluoroquinolones—from the cell, conferring a multidrug-resistant phenotype [23].
- Target Site Modification: Bacteria can alter the molecular targets of antibiotics through mutation or enzymatic modification. For example, mutations in DNA gyrase and topoisomerase IV reduce the efficacy of fluoroquinolones, while modification of the ribosomal target site can confer resistance to aminoglycosides and macrolides [23] [27].
- Biofilm Formation and Collective Tolerance: Within polymicrobial infections, bacterial communities can form biofilms that provide collective tolerance. The biofilm matrix limits antibiotic diffusion and creates nutrient and oxygen gradients that reduce the metabolic activity of cells in the interior, increasing the proportion of persister cells that survive treatment [28].
The following diagram illustrates the synergistic interplay of these core resistance mechanisms within a bacterial cell.
Advanced Methodologies for Resistance Surveillance and Profiling
Tracking the emergence and spread of AMR requires sophisticated surveillance methods that extend beyond clinical settings into the environment. Key experimental approaches for monitoring antibiotic resistance genes (ARGs) are detailed below.
Protocol: Environmental Surveillance of ARGs via Concentration and qPCR/ddPCR
Wastewater and biosolids are hotspots for the accumulation and potential dissemination of ARGs. This protocol outlines a comparative approach for concentrating and quantifying ARGs from these complex matrices [29].
- Objective: To compare the efficiency of two concentration methods—Filtration–Centrifugation (FC) and Aluminum-based Precipitation (AP)—coupled with two detection techniques—quantitative PCR (qPCR) and droplet digital PCR (ddPCR)—for quantifying specific ARGs in secondary treated wastewater and biosolids.
- Sample Collection: Collect 1L samples of secondary treated wastewater and biosolids from urban wastewater treatment plants (WWTPs). Store at 4°C until analysis.
- Concentration Methods:
- Filtration–Centrifugation (FC): Filter 200 mL of wastewater through a 0.45 µm sterile filter. The filter is then placed in buffered peptone water, agitated, and sonicated. The resulting suspension is centrifuged (3000× g for 10 min), and the pellet is resuspended in PBS [29].
- Aluminum-based Precipitation (AP): Adjust the pH of 200 mL of wastewater to 6.0. Add AlCl₃ to a final concentration of 0.9 N, shake, and centrifuge (1700× g for 20 min). The pellet is reconstituted in 3% beef extract and centrifuged again, with the final pellet resuspended in PBS [29].
- DNA Extraction: Extract and purify DNA from the concentrated samples and biosolids using a commercial kit (e.g., Maxwell RSC Pure Food GMO and Authentication Kit).
- ARG Quantification:
- qPCR: Perform using standard curves for absolute or relative quantification. It is highly sensitive but can be impaired by matrix-associated inhibitors [29] [30].
- ddPCR: Partition the sample into thousands of nanoliter-sized droplets for absolute quantification without a standard curve. This method reduces the impact of inhibitors and offers enhanced sensitivity for low-abundance ARGs [29].
- Key Findings: The AP method generally provides higher ARG concentrations than FC, particularly in wastewater. ddPCR demonstrates greater sensitivity than qPCR in wastewater, whereas in biosolids, both methods perform similarly [29].
Protocol: Comparative ARG Profiling via HT-qPCR and Metagenomics
This protocol describes a systematic comparison of High-Throughput qPCR (HT-qPCR) and metagenomic sequencing for ARG profiling in environmental samples, such as aquaculture water and sediments [30].
- Objective: To evaluate the performance of HT-qPCR and metagenomic sequencing in characterizing ARG profiles and to develop a risk assessment model for ARGs detected by HT-qPCR.
- Sample Processing: Extract total DNA from environmental samples (water, sediment).
- Parallel Analysis:
- HT-qPCR: Analyze DNA using pre-designed primer sets targeting specific ARGs (e.g., 31-40 targets). This method provides absolute quantification of ARG abundance and is highly sensitive for low-abundance targets [30].
- Metagenomic Sequencing: Sequence the same DNA extracts on an Illumina or similar platform. Process raw sequences to profile the microbial community and identify ARG subtypes and their genetic contexts (e.g., proximity to mobile genetic elements) via alignment to reference databases [30].
- Data Integration and Risk Assessment:
- A novel risk assessment model can be developed for HT-qPCR data by integrating the absolute abundance of ARGs, their detection frequency, the co-occurrence with mobile genetic elements (inferring horizontal gene transfer potential), and the pathogenicity of the bacterial hosts identified via 16S rRNA sequencing [30].
- This model allows for the prioritization of high-risk ARG subtypes, such as mexF, ereA, and sul2, facilitating targeted control measures [30].
The workflow for this comparative analysis and risk assessment is outlined below.
Research into intrinsically resistant bacteria relies on a suite of specialized reagents and platforms. The following table catalogues key solutions for critical experimental procedures in AMR research.
Table 2: Essential Research Reagents and Platforms for AMR Studies
| Category / Reagent | Specific Example(s) | Function / Application |
|---|---|---|
| Automated ID & AST Systems | Vitek 2 Compact System (Biomerieux) with GN cards and AST-N233/XNO5 cards [25] | Automated bacterial identification and antimicrobial susceptibility testing (AST) by Minimum Inhibitory Concentration (MIC). |
| Standardized AST Methods | Broth microdilution (e.g., ComASP Colistin Test Panel); CLSI guidelines [25] | Reference methods for confirming resistance, especially for last-resort antibiotics like colistin. |
| DNA Extraction Kits | Maxwell RSC Pure Food GMO and Authentication Kit (Promega) [29] | Automated extraction of high-quality, inhibitor-free DNA from complex matrices like biosolids and wastewater. |
| qPCR/ddPCR Platforms | Quantitative PCR (qPCR); Droplet Digital PCR (ddPCR) [29] | Sensitive detection and absolute quantification of specific antibiotic resistance genes (ARGs). |
| High-Throughput PCR | WaferGen SmartChip for HT-qPCR [30] | Simultaneous quantification of hundreds to thousands of ARG targets across many samples. |
| Priority ARG Targets | blaCTX-M, blaNDM, blaKPC, blaOXA, mecA, vanA, mcr, tet(A) [29] [30] | Key resistance genes against critical antibiotics (β-lactams, glycopeptides, colistin, tetracyclines) for surveillance. |
| Concentration Reagents | Aluminum Chloride (AlCl₃); Buffered Peptone Water with Tween [29] | Concentrating bacterial cells and viral particles (including phages) from large-volume water samples for downstream analysis. |
The WHO critical priority pathogens, with their formidable array of intrinsic and acquired resistance mechanisms, represent a persistent and evolving threat to global health. The continued dominance of Gram-negative bacteria like carbapenem-resistant Acinetobacter baumannii and Klebsiella pneumoniae on the WHO list, coupled with an insufficient and fragile antibacterial R&D pipeline, underscores the urgent need for a paradigm shift in how we approach this crisis. A comprehensive strategy is required, one that integrates robust national and international surveillance using advanced molecular methods, a deeper ecological understanding of resistance gene flow through the "One Health" continuum, and sustained investment in the discovery of innovative therapeutics and rapid diagnostics. Without coordinated global action to address the scientific, economic, and public health challenges of AMR, the prospect of a post-antibiotic era becomes increasingly imminent.
Antimicrobial resistance (AMR) represents one of the most pressing global public health challenges of our time, directly threatening the efficacy of modern medicine. The One Health approach recognizes that the health of humans, animals, and ecosystems is interconnected and that AMR emergence and dissemination must be understood through this integrated lens [31]. Resistant bacteria and antimicrobial resistance genes (ARGs) circulate continuously between human, animal, and environmental reservoirs through complex transmission pathways, making containment through human healthcare measures alone impossible [32].
The environmental and agricultural dimensions of AMR are particularly critical as they represent often overlooked amplifiers of resistance. This whitepaper provides a technical examination of these reservoirs, focusing on their role in the broader context of bacterial species with natural antibiotic resistance. We synthesize current scientific understanding of reservoir dynamics, transmission mechanisms, and surveillance methodologies to inform research and drug development initiatives aimed at mitigating AMR spread.
The Scope of the Antimicrobial Resistance Crisis
The global burden of AMR continues to escalate at an alarming rate. According to recent World Health Organization (WHO) surveillance data from over 100 countries, one in six laboratory-confirmed bacterial infections in 2023 were resistant to standard antibiotic treatments [7]. Between 2018 and 2023, antibiotic resistance increased in over 40% of the pathogen-antibiotic combinations monitored, with an average annual increase of 5-15% [7] [33].
Regional disparities in resistance patterns highlight the complex interplay of socioeconomic and healthcare factors. The WHO South-East Asian and Eastern Mediterranean Regions report the highest resistance rates, with approximately one in three reported infections demonstrating resistance, compared to one in five in the African Region [7] [33]. Gram-negative bacteria pose a particularly severe threat, with more than 40% of Escherichia coli and over 55% of Klebsiella pneumoniae isolates globally now resistant to third-generation cephalosporins, first-line treatments for serious infections [7].
In the United States, specific resistant pathogens have demonstrated dramatic increases. Infections caused by NDM-producing carbapenem-resistant Enterobacterales (NDM-CRE) surged by more than 460% between 2019 and 2023 [34]. These pathogens produce the New Delhi metallo-β-lactamase (NDM) enzyme that confers resistance to nearly all available antibiotics, including last-resort carbapenems [34].
Table 1: Global Prevalence of Antibiotic Resistance in Key Bacterial Pathogens
| Bacterial Pathogen | Antibiotic Class | Resistance Rate | Notes |
|---|---|---|---|
| Klebsiella pneumoniae | Third-generation cephalosporins | >55% globally, >70% in some regions | Leading cause of drug-resistant bloodstream infections [7] |
| Escherichia coli | Third-generation cephalosporins | >40% globally | Major pathogen in urinary and gastrointestinal infections [7] |
| Acinetobacter spp. | Carbapenems | Increasing frequency | Narrowing treatment options, rising resistance to last-resort antibiotics [7] |
| Enterobacterales | Carbapenems (NDM-producing) | 460% increase (2019-2023) | Particularly NDM-CRE strains; few effective treatments available [34] |
Environmental Reservoirs of Antimicrobial Resistance
Aquatic Environments and Biofilms
Aquatic ecosystems serve as critical reservoirs and conduits for the dissemination of antibiotic-resistant bacteria (ARB) and ARGs. The continuous discharge of wastewater treatment plant (WWTP) effluents, agricultural runoff, and other anthropogenic sources introduces antibiotics, biocides, heavy metals, and resistant bacteria into aquatic systems [35]. Although antibiotic concentrations in these environments are typically sub-inhibitory (ng/L to μg/L), they function as signaling molecules that promote horizontal gene transfer (HGT) and maintain a persistent pool of resistance genes in native microbial communities [35] [36].
Biofilms represent particularly efficient environmental reservoirs for AMR. These structured multicellular communities embedded in a self-produced extracellular polymeric substance (EPS) matrix exhibit intrinsic physiological characteristics that enhance resistance dissemination [35]. The EPS matrix acts as a protective barrier that limits antibiotic penetration while maintaining high bacterial density and proximity that facilitates genetic exchange [35] [36]. Biofilms demonstrate 10 to 1,000 times reduced susceptibility to antimicrobial agents compared to their planktonic counterparts [35].
Table 2: Mechanisms of Enhanced Antibiotic Resistance in Environmental Biofilms
| Mechanism | Functional Significance | Research Findings |
|---|---|---|
| Physical barrier | EPS matrix limits antibiotic diffusion | Creates chemical gradients and protected niches [35] |
| Metabolic heterogeneity | Includes dormant "persister" cells | Non-growing cells tolerate antibiotic exposure [35] |
| HGT facilitation | High cell density promotes genetic exchange | Conjugation rates 2-5 times higher under sub-MIC antibiotics [35] |
| Stress response activation | Sub-MIC antibiotics induce defense mechanisms | Antibiotics function as signaling molecules [35] |
| e-DNA retention | Extracellular DNA concentrated in matrix | Provides raw material for natural transformation [36] |
The genetic mobilome within biofilms—including plasmids, transposons, insertion sequences, bacteriophages, integrons, and extracellular DNA—creates an efficient infrastructure for HGT [36]. Clinical studies have demonstrated that sub-minimum inhibitory concentrations (sub-MIC) of antibiotics significantly increase the prevalence of mobile genetic elements, particularly Class 1 integrons, in freshwater biofilms exposed to treated sewage effluent [36]. This enhanced gene transfer capacity, combined with the constant selective pressure of environmental antibiotics, establishes biofilms as hotspots for the evolution and dissemination of novel resistance combinations.
Soil and Agricultural Environments
Agricultural systems represent profound amplifiers of AMR through the application of livestock manure, dairy lagoon effluent, and treated wastewater to farmland [37]. These practices introduce ARBs, ARGs, and selective agents (antibiotics, biocides, heavy metals) directly into soil ecosystems, where they can persist and transfer resistance to indigenous soil bacteria [37] [38].
Metagenomic analyses of livestock waste have revealed distinct resistance profiles dominated by specific antibiotic classes. In swine manure, aminoglycoside resistance genes represent 40-55% of the identified resistome, followed by tetracycline (30-45%), beta-lactam (20-35%), and macrolide (18-30%) resistance genes [37]. Network analyses demonstrate co-occurrence patterns between transporter genes, regulator genes, efflux pumps, and specific ARGs, with phyletic affiliations primarily with Bacteroidetes fragilis and Enterobacter aerogenes [37].
The diagram below illustrates the complex interactions and transmission pathways of AMR within the One Health framework:
Agricultural Reservoirs and Transmission Pathways
Livestock Production Systems
The use of antibiotics in livestock production constitutes a significant driver of AMR emergence. Prophylactic and growth-promoting applications in food animals create sustained selective pressures that enrich for resistant bacteria and ARGs within animal microbiomes [31]. Comparative studies demonstrate dramatically increased AMR abundance in the gut of farm animals (chicken, turkey, pig) compared to wild animals (boars, foxes, rodents) [31]. Longitudinal research in swine and broiler operations has documented concomitant increases in AMR in Enterococcus spp. following antibiotic administration [31].
The impact of antibiotic use extends beyond pathogenic bacteria to encompass commensal organisms that serve as ARG reservoirs. Investigations into the poultry resistome reveal that optimized doses of enrofloxacin cause significant perturbations in the gut microbiota and increase ARG diversity, while synbiotic supplementation can reduce the number of enriched ARGs [39]. This suggests that nutritional interventions may partially mitigate antibiotic-induced resistome expansion.
Transmission to Humans
The transmission of AMR from agricultural operations to humans occurs through multiple exposure routes:
Foodborne transmission: Resistant bacteria from food animals contaminate products throughout the supply chain. Studies have identified multidrug-resistant Salmonella from poultry, cephalosporin-resistant Escherichia coli from veal calves, and carbapenem-resistant E. coli from pigs [31]. Additionally, diverse carbapenem-resistant bacteria (Pseudomonas, Stenotrophomonas, Myroides) have been detected in seafood products, highlighting that non-pathogenic bacteria regularly excluded from surveillance programs may serve as resistance reservoirs [31].
Occupational exposure: Direct contact with food animals represents a significant transmission risk. Livestock-associated methicillin-resistant Staphylococcus aureus (LA-MRSA) has been identified in workers at industrial livestock operations but not in workers at antibiotic-free operations [31]. Genomic studies confirm that MRSA ST398 strains can spread among swine, humans, and the environment, with potential international transmission [39].
Environmental dissemination: Agricultural runoff and manure application contaminate waterways and soils with ARBs and ARGs, creating extended exposure pathways for surrounding communities. This is particularly problematic in low- and middle-income countries (LMICs) where high population density, poorer sanitation, and intensive animal farming practices create conditions conducive to inter-reservoir transmission [38].
Methodologies for AMR Surveillance and Analysis
Experimental Approaches for Reservoir Tracking
Understanding AMR dynamics across One Health reservoirs requires integrated surveillance methodologies that combine cultivation-dependent and molecular approaches. The following experimental workflow outlines a comprehensive approach to characterizing AMR in environmental and agricultural reservoirs:
The Scientist's Toolkit: Key Research Reagents and Methodologies
Table 3: Essential Research Reagents and Methodologies for AMR Reservoir Studies
| Category | Specific Reagents/Methods | Application and Function |
|---|---|---|
| Selective Media | Chromogenic agar with antibiotics; MacConkey agar with cephalosporins | Isolation and presumptive identification of resistant Enterobacterales [39] |
| Molecular Biology | PCR primers for blaNDM, blaCTX-M, mcr-1; Sanger sequencing | Targeted detection and confirmation of specific resistance genes [39] [34] |
| Genomic Sequencing | Illumina short-read; PacBio SMRT sequencing; Metagenomic libraries | Comprehensive resistome characterization; plasmid reconstruction [37] [39] |
| Bioinformatic Tools | CARD; ResFinder; MLST; Prokka | ARG annotation; strain typing; genome annotation [37] [39] |
| Culture Supplements | Sub-MIC antibiotics; Synbiotic formulations | Simulation of environmental conditions; mitigation studies [35] [39] |
Protocol for Resistome Analysis in Environmental Samples
Sample Collection and Processing:
- Collect environmental samples (water, soil, biofilm) using sterile containers and maintain cold chain during transport
- For biofilms, gently scrape submerged surfaces with sterile implements and homogenize in buffer
- Process samples within 24 hours of collection
Metagenomic DNA Extraction:
- Use commercial soil or water DNA extraction kits with bead-beating step for comprehensive cell lysis
- Include negative extraction controls to monitor contamination
- Assess DNA quality and quantity using fluorometric methods
Library Preparation and Sequencing:
- Prepare metagenomic sequencing libraries using Illumina-compatible protocols
- Sequence to a minimum depth of 10-20 million reads per sample
- Include positive controls with known ARG composition for quality assessment
Bioinformatic Analysis:
- Perform quality control of raw reads using FastQC and Trimmomatic
- Conduct assembly using metaSPAdes or Megahit
- Annotate ARGs using the Comprehensive Antibiotic Resistance Database (CARD) with RGI
- Perform taxonomic classification using Kraken2 or MetaPhlAn
- Conduct statistical analysis in R with vegan and phyloseq packages
This protocol enables comprehensive characterization of resistomes and identifies co-occurrence patterns between ARGs, mobile genetic elements, and taxonomic markers, providing critical insights into AMR dissemination pathways.
The environmental and agricultural dimensions of AMR represent critical components of the resistance lifecycle that demand increased research attention. The One Health perspective provides an essential framework for understanding the complex interactions between human, animal, and environmental reservoirs that drive the emergence and dissemination of resistant strains [31] [32]. Current evidence unequivocally demonstrates that interventions focused solely on human healthcare settings cannot adequately address the global AMR crisis.
Future research priorities should include:
- Enhanced surveillance integrating genomic and metagenomic approaches across all One Health sectors
- Elucidation of the ecological and evolutionary dynamics driving HGT in environmental hotspots
- Development of interventional strategies to disrupt AMR transmission at the human-animal-environment interface
- Innovation in wastewater treatment and agricultural waste processing to reduce AMR dissemination
The role of environmental bacteria as sources of novel ARGs that can transfer to pathogenic species under antibiotic selection pressure necessitates a fundamental reexamination of AMR containment strategies [38]. Reducing the environmental burden of AMR will require improved waste treatment, restricted antibiotic use in humans and animals, prioritization of less environmentally persistent antibiotics, and better control of pharmaceutical manufacturing discharges [38]. Through coordinated, transdisciplinary approaches aligned with One Health principles, the scientific community can develop effective strategies to mitigate this escalating global health threat.
Advanced Research Tools: Profiling and Combatting Innate Bacterial Defenses
Genomic and Metagenomic Approaches for Decoding Intrinsic Resistomes
The intrinsic resistome encompasses all innate, chromosomal genes that contribute to a bacterium's natural resistance to antibiotics, a phenomenon independent of horizontal gene transfer or prior antibiotic exposure [40]. This concept fundamentally expands our understanding of antibiotic resistance beyond acquired mechanisms to include a complex network of inherent genetic factors. The intrinsic resistome is universally present within bacterial species and predates the clinical use of antibiotics, representing a natural defense arsenal that dramatically limits therapeutic options, particularly for Gram-negative pathogens [40].
Understanding the intrinsic resistome is crucial for addressing the global antimicrobial resistance (AMR) crisis. Infections caused by antibiotic-resistant bacteria are associated with significant increases in morbidity and mortality rates, longer hospital stays, and higher treatment costs [41]. The intrinsic resistance of Gram-negative bacteria, mediated by their outer membrane and active efflux systems, presents a particularly pressing clinical challenge that restricts available treatments [40]. Decoding these innate resistance mechanisms through genomic and metagenomic approaches provides the foundational knowledge needed to develop novel therapeutic strategies to combat multidrug-resistant pathogens.
Fundamental Mechanisms of Intrinsic Resistance
Bacteria employ multiple sophisticated mechanisms to achieve intrinsic antibiotic resistance, with the most well-characterized being permeability barriers and efflux systems.
Outer Membrane Permeability
The Gram-negative outer membrane serves as a formidable permeability barrier that effectively excludes many antimicrobial compounds. This protective structure is composed of an asymmetric lipid bilayer containing lipopolysaccharides (LPS) in the outer leaflet and phospholipids in the inner leaflet [40]. The limited fluidity of this membrane, compared to the cytoplasmic membrane, significantly reduces its permeability to hydrophobic compounds. Integral outer membrane proteins (porins) form water-filled channels that permit the passive diffusion of small hydrophilic molecules, but their size selectivity and charge characteristics restrict the passage of many antibiotics [40]. This selective permeability represents a primary intrinsic resistance mechanism in Gram-negative bacteria.
Active Efflux Systems
Bacteria encode numerous multidrug efflux pumps that actively transport antibiotics out of the cell, thereby reducing intracellular concentrations to subtoxic levels. These systems are classified into several families based on their structure and energy coupling mechanisms:
- Resistance-Nodulation-Division (RND) family: These tripartite systems span both the inner and outer membranes in Gram-negative bacteria and exhibit broad substrate specificity [40].
- Major Facilitator Superfamily (MFS): Single-component transporters that utilize the proton motive force for energy [42].
- ATP-Binding Cassette (ABC) transporters: Utilize ATP hydrolysis to drive antibiotic extrusion [42].
- Multidrug and Toxic Compound Extrusion (MATE) family: Exchange intracellular drugs for extracellular sodium or hydrogen ions [42].
- Small Multidrug Resistance (SMR) family: Small homotrimeric transporters that handle a variety of lipophilic cations [42].
The combined activity of these efflux systems with the permeability barrier creates a synergistic defense that confers intrinsic resistance to multiple antibiotic classes.
Additional Genetic Determinants
Beyond the classic permeability and efflux mechanisms, genome-wide studies have revealed a surprising array of additional genetic loci that contribute to intrinsic resistance. Systematic screening of gene inactivation and transposon insertion libraries has identified numerous genes unrelated to these traditional mechanisms that nonetheless modulate antibiotic susceptibility [40]. These findings illustrate that intrinsic resistance represents a complex phenotype involving metabolic pathways, stress response systems, and other cellular processes that indirectly influence antibiotic susceptibility.
Table 1: Core Mechanisms of Intrinsic Antibiotic Resistance
| Mechanism | Key Components | Antibiotic Classes Affected | Representative Examples |
|---|---|---|---|
| Permeability Barrier | Outer membrane, Lipopolysaccharides, Porins | β-lactams, Glycopeptides, Macrolides | Gram-negative outer membrane [40] |
| Active Efflux | RND, MFS, ABC, MATE, SMR transporters | Multiple classes including tetracyclines, quinolones, β-lactams | AcrAB-TolC system in E. coli [40] |
| Target Modification | rRNA methyltransferases, Altered PBPs | Aminoglycosides, β-lactams | 23S rRNA methylation in Streptomyces [42] |
| Antibiotic Inactivation | Hydrolytic enzymes, Modification enzymes | β-lactams, Aminoglycosides | β-lactamases, Aminoglycoside-modifying enzymes [42] |
Genomic Methodologies for Resistome Analysis
Whole Genome Sequencing of Bacterial Isolates
Whole Genome Sequencing (WGS) of bacterial isolates provides a powerful approach for comprehensively characterizing resistance determinants. The standard workflow begins with bacterial isolation and culture, followed by DNA extraction, library preparation, and high-throughput sequencing [43]. Advances in next-generation sequencing (NGS) technologies have enabled relatively inexpensive and fast WGS, making it accessible for both research and diagnostic microbiology [43].
The resulting genomic data allows for accurate identification of strain phylogeny, single nucleotide polymorphisms (SNPs), and specific resistance determinants. This approach is particularly valuable for tracking outbreaks and understanding the genetic basis of resistance in clinical pathogens [43]. For example, WGS analyses have been instrumental in reclassifying misidentified Klebsiella variicola isolates and characterizing their distinct resistance profiles compared to K. pneumoniae [43].
WGS workflow for intrinsic resistome characterization
Comparative Genomic Analyses
Comparative genomics enables researchers to identify resistance determinants across different bacterial strains and species. By comparing genomes of resistant and susceptible isolates, researchers can pinpoint genetic variations associated with resistance phenotypes. This approach has revealed that intrinsic resistance is more complex than initially thought, involving numerous genes beyond those encoding obvious resistance mechanisms like efflux pumps or permeability barriers [40].
Comparative analyses between antibiotic-producing Streptomyces species and pathogenic bacteria have uncovered surprising similarities in resistance mechanisms, suggesting potential evolutionary connections between self-resistance in producers and clinical resistance [42]. These comparisons provide insights into the origins and evolution of resistance determinants.
Metagenomic Frameworks for Environmental Resistome Profiling
Shotgun Metagenomic Sequencing
Shotgun metagenomics enables comprehensive analysis of resistance genes in complex microbial communities without the need for cultivation. This approach involves extracting total DNA directly from environmental samples, followed by sequencing and computational analysis to identify and quantify resistance determinants [44]. The term "metagenomics" was first used by Handelsman et al. (1998) and reflects the fact that pure cultures are not required for sequencing [44].
Metagenomic analysis provides global snapshots of bacterial community composition and ARG distribution in environmental samples containing numerous nonculturable microorganisms [45]. This powerful tool facilitates high-throughput identification and quantification of ARGs in diverse habitats, revealing the extensive diversity and distribution of resistance elements in natural environments [44].
Table 2: Metagenomic Approaches for Resistome Analysis
| Approach | Methodology | Advantages | Limitations |
|---|---|---|---|
| Shotgun Metagenomics | Random sequencing of all DNA in a sample | Culture-independent, comprehensive gene cataloging | Computational complexity, DNA extraction biases |
| Functional Metagenomics | Cloning environmental DNA into host organisms followed by functional screening | Identifies novel genes without prior sequence knowledge | Low throughput, host expression biases |
| Targeted Metagenomics | Amplification or capture of specific resistance gene families | High sensitivity for known genes, cost-effective | Limited to known target sequences |
| Co-assembly | Pooling and assembling multiple related metagenomic samples | Improved gene detection, longer contigs | Potential misassemblies, computational demands [46] |
Metagenomic Co-assembly Strategies
Metagenomic co-assembly involves pooling and assembling sequencing reads from multiple related samples to improve gene detection and assembly quality. This approach is particularly valuable for low-biomass environments like atmospheric samples, where individual assemblies may yield fragmented results [46]. Co-assembly consistently outperforms individual assembly in key metrics including genome fraction, duplication ratio, and misassemblies [46].
In a study of airborne microbiomes, co-assembly of 45 air samples produced significantly longer contigs (762,369 contigs ≥500 bp, totaling 555.79 million bp) compared to individual assembly (455,333 contigs and 334.31 million bp) [46]. This improved assembly facilitated the identification of resistance genes against clinically important antibiotics, including aminoglycosides, beta-lactams, fosfomycin, glycopeptides, quinolones, and tetracyclines in atmospheric samples [46].
Resistome Analysis Frameworks
Comprehensive resistome characterization requires integrated frameworks that examine multiple aspects of resistance potential. A proposed metagenomic framework for environmental samples includes five key categories [45]:
- ARG potential: Identification and quantification of antibiotic resistance genes
- ARG hosts: Tracking microbial taxa carrying resistance determinants
- Pathogenicity potential: Detection of pathogenic bacteria carrying ARGs
- Co-selection potential: Identification of biocide/metal resistance genes (B/MRGs) that may co-select for antibiotic resistance
- Gene transfer potential: Detection of mobile genetic elements (MGEs) that facilitate horizontal transfer
Application of this framework to urban river sediments revealed 203 ARG subtypes dominated by multidrug, macrolide-lincosamide-streptogramin, bacitracin, quinolone, and sulfonamide resistance genes [45]. Host-tracking analysis identified Dechloromonas, Pseudoxanthomonas, Arenimonas, Lysobacter, and Pseudomonas as major ARG hosts, while co-occurrence analysis showed strong associations between ARGs, B/MRGs, and MGEs, indicating high potential for co-selection and horizontal gene transfer [45].
Bioinformatics Tools and Databases
Resistance Gene Identification Pipelines
Specialized bioinformatics tools are essential for identifying and characterizing resistance genes in genomic and metagenomic datasets. These include:
- ResFinder: Identifies acquired antimicrobial resistance genes in bacterial genomes [41]
- CARD-RGI: The Comprehensive Antibiotic Resistance Database with Resistance Gene Identifier provides curated information on resistance mechanisms and detection tools [41]
- VirulenceFinder: Detects virulence-related genes in bacterial genomes [41]
- MobileElementFinder: Identifies mobile genetic elements associated with resistance genes [41]
- PlasmidFinder: Detects plasmid replicons in bacterial genomes [41]
These tools are often integrated into comprehensive analysis pipelines that process sequencing data from quality control through to resistance gene annotation and visualization.
Metagenomic Assembly and Annotation
Assembly and annotation of metagenomic data present unique computational challenges due to the genetic heterogeneity and unknown composition of microbial communities. Common approaches include:
- De novo assembly: Tools like Flye [41], SPAdes [41], and Canu [41] reconstruct longer contigs from short sequencing reads
- Gene prediction: Identification of open reading frames (ORFs) in assembled contigs or directly from sequencing reads
- Functional annotation: Assignment of predicted genes to functional categories using homology-based searches against reference databases
- Taxonomic classification: Bin contigs into taxonomic groups based on sequence composition and marker genes
The quality of metagenomic assemblies significantly impacts downstream analyses, with co-assembly approaches demonstrating superior performance for complex environmental samples [46].
Advanced Sequencing Technologies and Protocols
Rapid Nanopore Sequencing
Oxford Nanopore Technologies (ONT) offers rapid sequencing capabilities that are particularly valuable for clinical applications requiring timely results. A rapid nanopore-based protocol (ONT20h) demonstrated comparable or superior performance in AMR gene detection compared to slower sequencing methods, while achieving equivalent virulence factor identification [41]. This protocol maintained a high level of agreement with phenotypic antimicrobial susceptibility testing, supporting its potential as an efficient diagnostic tool in clinical microbiology [41].
The implementation of rapid WGS protocols could significantly improve infection control strategies and therapeutic decision-making by providing timely information about resistance profiles [41]. However, further studies are needed to optimize clinical application of this technology, considering costs, availability of bioinformatics tools, and reference database quality [41].
Table 3: Comparison of Sequencing Protocols for Resistome Analysis
| Protocol | Technology/Platform | Sequencing Time | Assembly Software | Key Applications |
|---|---|---|---|---|
| ONT20h | Oxford Nanopore - GridION | 20 hours | Flye v.2.7.1 with Medaka polishing | Rapid clinical diagnostics, outbreak investigation [41] |
| ONT48hA | Oxford Nanopore - GridION | 48 hours | Canu v.1.9 without polishing | Research applications requiring longer reads [41] |
| ONT48hB | Oxford Nanopore - GridION | 48 hours | Flye v.2.9 with Medaka polishing | High-quality genome assembly [41] |
| IT | Illumina - MiSeq | 56 hours | SPAdes v.3.13.0 | Reference-quality sequencing, variant detection [41] |
| Hybrid | ONT GridION/Illumina MiSeq | 20/56 hours | Unicycler v.0.5.0 | Complete genome assembly, resolving repetitive regions [41] |
Hybrid Sequencing Approaches
Hybrid sequencing strategies combining multiple technologies leverage the complementary strengths of different platforms. For example, combining long-read technologies (such as Oxford Nanopore or PacBio) with short-read technologies (such as Illumina) can produce more complete genome assemblies by leveraging the accuracy of short reads with the contiguity of long reads [41].
The hybrid protocol included in the comparison table used Unicycler v.0.5.0 for assembly, utilizing raw data from both ONT20h and IT sequencing [41]. This approach is particularly valuable for resolving complex genomic regions and repetitive elements that challenge single-technology assemblies.
Table 4: Essential Research Reagents and Computational Tools for Resistome Analysis
| Category | Item/Resource | Specification/Function | Application Notes |
|---|---|---|---|
| Sequencing Technologies | Oxford Nanopore GridION | Long-read sequencing platform | Enables rapid 20h protocol for clinical applications [41] |
| Illumina MiSeq | Short-read sequencing platform | Provides high-accuracy reads for hybrid assemblies [41] | |
| Assembly Tools | Flye v.2.7.1-2.9 | De novo assembler for long reads | Used with Medaka polishing in ONT protocols [41] |
| SPAdes v.3.13.0 | Genome assembler for short reads | Suitable for Illumina data assembly [41] | |
| Unicycler v.0.5.0 | Hybrid assembler | Combines ONT and Illumina data for improved assemblies [41] | |
| Resistance Databases | ResFinder | Identifies acquired antimicrobial resistance genes | Critical for ARG annotation [41] |
| CARD-RGI | Comprehensive Antibiotic Resistance Database | Provides curated resistance gene information [41] | |
| Specialized Tools | VirulenceFinder | Detects virulence factors | Links resistance with pathogenicity [41] |
| MobileElementFinder | Identifies mobile genetic elements | Assesses horizontal transfer potential [41] | |
| PlasmidFinder | Detects plasmid replicons | Tracks plasmid-mediated resistance spread [41] |
Data Interpretation and Translational Applications
From Genomic Data to Therapeutic Strategies
Decoding intrinsic resistomes enables the development of novel therapeutic strategies that target resistance mechanisms directly. One promising approach involves identifying vulnerabilities in the intrinsic resistome that could be exploited to rejuvenate existing antibiotics [40]. Studies have shown that deletion of certain intrinsic resistance elements renders bacteria hyper-susceptible to antibiotics, suggesting that pharmacological inhibition of these targets could potentiate current antibacterial agents [40].
The most promising targets for intervention include:
- Permeabilization of the Gram-negative outer membrane to increase antibiotic penetration
- Inhibition of active efflux systems to enhance intracellular antibiotic accumulation
- Disruption of regulatory networks that coordinate resistance mechanisms
- Interference with stress response pathways that contribute to intrinsic resistance
These approaches could expand the therapeutic arsenal against multidrug-resistant pathogens by counteracting their innate defense systems.
Environmental Surveillance and One Health Perspectives
Genomic and metagenomic approaches reveal extensive connections between environmental resistomes and clinical resistance, supporting a One Health framework that integrates human, animal, and environmental health. Monitoring intrinsic resistomes in diverse ecosystems provides early warning systems for emerging resistance threats and reveals transmission pathways between environmental and clinical settings [45] [46].
Atmospheric monitoring has identified resistance genes in airborne microbiomes, suggesting potential for long-range dispersal of resistance determinants [46]. Similarly, aquatic environments serve as significant reservoirs and mixing pots for resistance genes from diverse sources [45]. Implementing comprehensive surveillance networks that track intrinsic resistomes across these interconnected ecosystems is essential for understanding and mitigating the global spread of antibiotic resistance.
Interconnectivity between environmental and clinical resistomes
Genomic and metagenomic approaches have revolutionized our understanding of intrinsic resistomes, revealing them to be complex networks of genetic determinants that extend far beyond simple permeability barriers and efflux systems. The integration of advanced sequencing technologies, sophisticated bioinformatics tools, and comprehensive analytical frameworks enables researchers to decode these innate resistance arsenals across diverse bacterial species and environments.
As the threat of antimicrobial resistance continues to grow, leveraging these approaches to develop novel therapeutic strategies—such as inhibitors that target vulnerabilities in intrinsic resistance mechanisms—becomes increasingly urgent. Furthermore, implementing comprehensive surveillance systems that track resistomes across human, animal, and environmental compartments through a One Health lens is essential for mitigating the global spread of resistance determinants. The continued refinement of genomic and metagenomic methodologies will play a pivotal role in addressing one of the most pressing public health challenges of our time.
High-Throughput Screening for Novel Compounds Targeting Resistant Pathogens
The escalating crisis of antimicrobial resistance (AMR) necessitates transformative approaches in antibiotic discovery. High-throughput screening (HTS) has emerged as a pivotal strategy for rapidly identifying novel compounds against resistant pathogens. By enabling the testing of hundreds of thousands of compounds against bacterial targets, HTS platforms overcome the historical "innovation gap" where no new classes of antibacterial agents were discovered for decades [47]. These approaches are particularly valuable for targeting priority pathogens identified by the World Health Organization, including multi-drug resistant Shigella, ESKAPE pathogens, and other organisms exhibiting resistance to current therapeutics [47] [48].
Modern HTS platforms have evolved beyond traditional growth inhibition assays to incorporate sophisticated models that better mimic infection contexts. This includes intracellular infection models, whole-organism screens, and computational prescreening methods that enhance hit identification. The integration of quantitative systems biology with experimental HTS has further advanced predictive capabilities for resistance evolution, enabling more strategic compound selection [14]. This technical guide examines current methodologies, experimental protocols, and emerging frameworks in HTS for antimicrobial discovery, with particular emphasis on overcoming resistance mechanisms in bacterial pathogens.
HTS Platforms and Methodologies
Phenotypic Screening Platforms
3D Intracellular Infection Models
Traditional monolayer cell cultures have limitations in simulating the intestinal environment for enteric pathogens. A recently developed three-dimensional (3D) high-throughput assay incorporates Shigella invasion into Caco-2 cells cultured on Cytodex 3 beads, scaled into a 384-well platform for screening chemical compound libraries [47].
Key Optimization Parameters:
- Multiplicity of Infection (MOI): 150 optimized for robust infection coverage
- Invasion Time: 6 hours determined as optimal for intracellular replication
- Bead Concentration: 4,000 beads/ml provided suitable screening density
- Quality Metrics: Z' factor > 0.4 and signal-to-background (S/B) values > 2-fold ensured assay robustness [47]
This platform demonstrated high reproducibility, with intra-assay coefficient of variation (CV) < 10% and inter-assay CV ranging from 1.43% to 14.82% across 11 reference antimicrobials [47]. The model confirmed functionality through biomarkers including sucrase activity (3.5-fold increase in 3D model), alkaline phosphatase production (5.5-fold increase), and ZO-1 tight junction formation [47].
Whole-Organism Screening with C. elegans
The nematode C. elegans provides a complete living system for anti-infective screening, allowing identification of compounds that boost host innate immunity or disrupt bacterial virulence mechanisms without direct bactericidal activity [48].
Platform Advantages:
- Capacity for high-throughput screening in 384-well plates
- In-assay counterscreen against generally toxic compounds
- Infection with multiple human pathogens possible
- Identification of immunostimulatory compounds and virulence disruptors [48]
Automation and Readouts:
- Automated dispensing of infected nematodes using modified flow cytometry
- Robot-assisted compound pinning into assay wells
- Cell-permeable dyes for quantification of live/dead nematodes via image analysis [48]
In seminal studies, this platform identified anti-infective compounds that protected C. elegans from enterococcal infection at concentrations far below their minimal inhibitory concentration (MIC), suggesting host-directed mechanisms rather than direct antibacterial activity [48].
Target-Based Screening Approaches
Computational Prescreening and Virtual Libraries
Computational approaches enable preliminary screening of extensive compound libraries before experimental validation. In one workflow, researchers screened 3,601 chemical compounds from the ChemDiv database against the trimethoprim-resistant DfrA1 protein through molecular docking [49].
Screening Methodology:
- Library Preparation: Compounds optimized with electronegative atoms (O, N, F, S, Cl) to facilitate binding interactions
- Binding Site Identification: Central binding pocket targeted in DfrA1 protein
- Interaction Analysis: Hydrogen bonds, π-stacking, π-alkyl, π-sigma, and van der Waals interactions evaluated
- Free Energy Calculations: MM/GBSA calculations estimated binding affinities [49]
This approach identified six promising drug candidates (DC1-DC6) with binding free energies lower than -9 kcal/mol, superior to the control drug Iclaprim [49].
Electronic Structure-Based Screening
For bimetallic catalyst systems, electronic density of states (DOS) similarity has served as an effective descriptor for identifying compounds with catalytic properties comparable to palladium for hydrogen peroxide synthesis [50].
Similarity Quantification:
where g(E;σ) represents a Gaussian distribution function focusing comparison near Fermi energy [50].
This DOS similarity screening of 4350 bimetallic alloy structures identified eight candidates, four of which demonstrated catalytic properties comparable to palladium in experimental validation [50].
Table 1: Comparison of HTS Platform Capabilities
| Platform Type | Throughput Capacity | Key Applications | Hit Validation Rate | Primary Advantages |
|---|---|---|---|---|
| 3D Intracellular Model [47] | 384-well format, >500,000 compounds | Intracellular pathogens (Shigella, Mycobacteria) | 12 hits from >500,000 compounds | Physiologically relevant intracellular environment |
| C. elegans Whole-Organism [48] | 384-well format, 10-20 nematodes/well | ESKAPE pathogens, host-directed therapies | 28 anti-infectives from 37,200 compounds | Identifies immunostimulatory compounds and virulence disruptors |
| Computational Prescreening [49] | 3,601 compounds in library | Specific resistance targets (DfrA1) | 6 hits from 3,601 compounds | Cost-effective; provides binding mechanism data |
| Electronic Structure Screening [50] | 4,350 alloy structures | Catalyst discovery, enzyme mimics | 4 hits from 4,350 structures | Based on fundamental electronic properties |
Experimental Protocols and Workflows
3D Intracellular Infection Assay Protocol
Cell Culture and Differentiation:
- Culture Caco-2 cells on Cytodex 3 beads in spinner flasks or rotating wall vessel bioreactors
- Maintain in humid atmosphere of 5% CO₂ at 37°C for 21 days to ensure full differentiation
- Verify differentiation through biomarkers:
- Sucrase activity (2.8-3.5-fold increase from baseline)
- Alkaline phosphatase production (increasing trend from day 8 to 21)
- ZO-1 tight junction protein formation [47]
Infection and Screening:
- Harvest 3D cells and transfer to 384-well cell-culture plates
- Infect with nanoluciferase-producing Shigella flexneri at MOI of 150
- Incubate for 6 hours to establish intracellular infection
- Add compound libraries and incubate for predetermined treatment period
- Quantify intracellular bacterial load using nanoluciferase activity [47]
Validation and QC Metrics:
- Calculate Z' factor (>0.4 indicates robust assay)
- Determine signal-to-background ratio (>2-fold acceptable)
- Assess invasion efficiency (target: 0.083% for S. flexneri SF_nanoluc)
- Estimate bacterial load (~15 S. flexneri per bead) [47]
Computational Screening Protocol for DfrA1 Inhibitors
Structure Preparation:
- Obtain 3D structure of target protein (DfrA1) from PDB or homology modeling
- Prepare protein structure through energy minimization and binding site identification
- Curate compound library (3,601 compounds) with structural optimization using Gaussian software [49]
Virtual Screening Workflow:
- Perform molecular docking of all compounds against binding pocket
- Analyze interaction profiles (hydrogen bonds, hydrophobic interactions, π-effects)
- Calculate binding free energies using MM/GBSA method
- Select top candidates based on:
- Binding free energy (< -9 kcal/mol)
- Number and quality of binding interactions
- Drug-likeness parameters (Rule of Five compliance) [49]
Experimental Validation:
- Conduct molecular dynamics simulations (100-200 ns) to assess complex stability
- Analyze thermodynamic properties (solvent-accessible surface area, polarity, binding site interactions)
- Evaluate residence time and inhibitory efficacy [49]
PBMC-Based Immunomodulator Screening
While primarily used for vaccine adjuvant discovery, PBMC screening protocols offer valuable methodology for identifying host-directed anti-infectives [51].
Cell Preparation and Compound Exposure:
- Thaw cryopreserved PBMCs in autologous platelet-poor plasma (PPP)
- Centrifuge at 3000 × g for 8 minutes (high acceleration/medium deceleration)
- Resuspend in DMEM with 10% PPP
- Incubate with compound libraries for 72 hours in 384-well plates [51]
Multiplexed Readouts:
- Harvest supernatants for cytokine secretion analysis via AlphaLISA:
- Tumor necrosis factor alpha (TNF-α)
- Interferon gamma (IFN-γ)
- Interleukin 10 (IL-10)
- Fix cells for immunophenotyping via flow cytometry:
- CD80, CD86, HLA-DR, OX40 expression [51]
Data Analysis and Hit Validation
Quantitative Assessment of Screening Results
Table 2: Key Metrics for HTS Hit Validation
| Validation Parameter | Calculation Method | Acceptance Criteria | Application Example | ||
|---|---|---|---|---|---|
| Assay Robustness | Z' factor = 1 - (3×σₚ + 3×σₙ)/ | μₚ - μₙ | Z' > 0.4 [47] | 3D intracellular assay (Z' = 0.57) [47] | |
| Binding Affinity | Binding free energy (ΔG) via MM/GBSA | ΔG < -9 kcal/mol [49] | DfrA1 inhibitors (DC1-DC6: -9 to -11 kcal/mol) [49] | ||
| Specificity Index | Cytotoxic concentration50 (CC₅₀)/ effective concentration50 (EC₅₀) | SI > 10 [48] | C. elegans anti-infectives (EC₅₀ << MIC) [48] | ||
| Drug-Likeness | Rule of Five compliance | MW ≤ 500 Da, MLogP ≤ 4.15, HBD ≤ 5, HBA ≤ 10 [49] | DfrA1 inhibitors DC4 and DC6 [49] | ||
| Resistance Prediction | Evolutionary entropy analysis | Lower entropy favors repeatability [14] | Predictable resistance mutations [14] |
Counter-Screening and Selectivity Assessment
Effective hit validation requires comprehensive counter-screening to exclude non-specific or generally toxic compounds:
Cytotoxicity Profiling:
- Assess mammalian cell viability in parallel with antimicrobial activity
- Determine selectivity indices (CC₅₀/EC₅₀) for prioritized hits
- C. elegans platforms provide built-in toxicity assessment [48]
Specificity Testing:
- Evaluate activity against related bacterial targets
- Test against structurally similar human enzymes
- Assess spectrum of activity against commensal bacteria [49]
Resistance Propensity Evaluation:
- Apply quantitative systems biology models to predict resistance evolution
- Quantify evolutionary predictability and repeatability using entropy measures [14]
- Assess mutation rates in presence of sub-inhibitory compound concentrations
Visualization of Screening Workflows
HTS Platform Selection and Application
3D Intracellular Infection Model
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Antimicrobial HTS Platforms
| Reagent/Resource | Function in HTS | Example Application | Specifications/Alternatives |
|---|---|---|---|
| Cytodex 3 Beads [47] | Microcarrier for 3D cell culture | Caco-2 intestinal model for Shigella infection | 4000 beads/mL concentration optimized |
| Caco-2 Cell Line [47] | Human intestinal epithelial model | Intracellular pathogen screening | 21-day differentiation protocol required |
| Nanoluciferase Reporter [47] | Bacterial load quantification | Intracellular replication measurement | S. flexneri SF_nanoluc strain |
| C. elegans Nematodes [48] | Whole-organism infection model | ESKAPE pathogen screening | 10-20 nematodes/well in 384-well format |
| PBMCs with Autologous Plasma [51] | Human immune response modeling | Immunomodulator screening | Cryopreserved for longitudinal studies |
| AlphaLISA Assay Kits [51] | Cytokine secretion quantification | TNF-α, IFN-γ, IL-10 measurement | 5000 assay point capacity |
| Flow Cytometry Antibodies [51] | Immune activation marker detection | CD80, CD86, HLA-DR, OX40 staining | Diluted 1:200 with dPBS |
| Molecular Docking Software [49] | Virtual compound screening | DfrA1 inhibitor identification | Maestro (Schrödinger LLC), Gaussian |
Emerging Frontiers and Future Directions
Integration of Quantitative Systems Biology
Predictive modeling of resistance evolution enhances HTS strategic planning. Key advances include:
Evolutionary Predictability Assessment:
- Quantification of evolutionary entropy to assess mutation repeatability
- Stochastic systems-based population models to predict resistance appearance
- Analysis of epistatic interactions that constrain evolutionary trajectories [14]
Multiscale Data Integration:
- Incorporation of genomic, transcriptomic, and proteomic data
- Mapping of genotype to phenotype in resistance mechanisms
- Modeling of nongenetic resistance facilitation of genetic evolution [14]
Chemical Diversity and Compound Prioritization
Expanding chemical space exploration requires sophisticated prioritization strategies:
Electronegative Atom Enrichment:
- Strategic inclusion of oxygen, nitrogen, fluorine, sulfur, and chlorine
- Enhanced nucleophilic attraction to binding pockets
- Improved prediction of drug-protein interactions [49]
DOS Similarity Screening:
- Electronic structure matching to known effective compounds
- Quantitative similarity metrics (ΔDOS_{2-1}) for catalyst discovery
- Extension to enzyme inhibitor identification [50]
Resistance-Informed Compound Selection
Future HTS platforms will increasingly incorporate resistance propensity assessment during early screening:
Evolutionary Vulnerability Scoring:
- Prediction of resistance mutation likelihood
- Assessment of fitness costs associated with resistance
- Selection of compounds with higher genetic barriers to resistance [14] [52]
Sanitation-Transmission Modeling:
- Quantitative biology of resistance transmission in various settings
- Relative weighting of selection pressure versus transmission dynamics
- Location-specific intervention planning based on sanitation infrastructure [52]
These advanced approaches position HTS as a cornerstone in the global response to antimicrobial resistance, enabling more strategic and effective antibiotic discovery against increasingly resistant pathogens.
The escalating crisis of antimicrobial resistance (AMR) represents one of the most severe global health threats of the 21st century, with antibiotic-resistant bacteria directly causing approximately 1.27 million deaths worldwide in 2019 alone [53]. The ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) have become particularly problematic, demonstrating resistance rates exceeding 90% to last-resort carbapenem antibiotics in some settings [53]. This whitepaper examines three innovative therapeutic avenues—phage therapy, CRISPR-Cas9 systems, and anti-virulence strategies—that offer promising alternatives to conventional antibiotics for combating drug-resistant bacterial infections. These approaches represent a paradigm shift from broad-spectrum antimicrobial activity to targeted, precision medicine that disrupts bacterial pathogenesis while minimizing damage to beneficial microbiota and reducing selective pressure for resistance development.
Phage Therapy: Harnessing Bacterial Viruses
Scientific Foundations and Mechanisms
Bacteriophages (phages) are naturally occurring viruses that specifically infect and replicate within bacterial cells, serving as the most abundant biological entities on Earth [54]. Their typical structure includes a protein capsid enclosing genetic material (double or single-stranded DNA or RNA) and a tail apparatus that recognizes and binds to specific receptors on the bacterial cell surface [54]. Phages exhibit two primary replication pathways: the lytic cycle, which results in immediate bacterial lysis and viral particle release, and the lysogenic cycle, where phage DNA integrates into the bacterial chromosome as a prophage without immediately killing the host [54]. Therapeutic applications predominantly utilize lytic phages due to their direct bactericidal activity.
Phages demonstrate exceptional specificity, typically targeting only particular bacterial strains within a species, which enables precise pathogen elimination while preserving commensal microbiota [53]. This specificity contrasts sharply with broad-spectrum antibiotics that disrupt diverse microbial communities. The primary families of therapeutic interest include Myoviridae (long contractile tails), Siphoviridae (long non-contractile tails), and Podoviridae (short non-contractile tails) [54].
Advanced Technical Approaches
Overcoming Evolutionary Limitations
A significant challenge in phage therapy involves addressing the natural evolutionary arms race between phages and bacteria. Two sophisticated approaches have emerged to counter bacterial resistance mechanisms:
Adaptive Evolution (Appelmans Protocol): This method involves experimentally co-evolving phages with bacterial populations under controlled conditions that simulate resistance development [53]. Through repeated exposure to both sensitive and resistant bacterial strains, phages evolve enhanced infectivity through mutations in receptor-binding proteins (tail fibers, baseplate proteins, or spikes), enabling them to recognize modified or alternative bacterial receptors [53]. This process can yield phages with expanded host ranges, improved lytic activity, and the ability to overcome bacterial defense systems like CRISPR-Cas and restriction-modification systems [53].
Exploiting Bacterial Fitness Trade-offs: This strategic approach selects phages that target bacterial structures serving dual functions in virulence and essential physiology [53] [55]. When bacteria evolve resistance to these phages through receptor modification, they frequently incur fitness costs that diminish pathogenicity. Notable examples include phages targeting:
Table 1: Clinical Outcomes of Personalized Inhaled Phage Therapy for Multidrug-Resistant Pseudomonas aeruginosa in Cystic Fibrosis Patients (2025 Study)
| Parameter | Pre-Therapy Values | Post-Therapy Values (5-18 days) | Statistical Significance |
|---|---|---|---|
| Sputum Pseudomonas CFU/mL | Median: 2.6 × 10⁸Mean: 3.0 × 10⁸ (±1.0 × 10⁸ SEM) | Median: 2.6 × 10⁴Mean: 7.7 × 10⁶ (±6.9 × 10⁶ SEM) | P = 0.006(Two-way ANOVA with Dunnett's test) |
| Percent Predicted FEV1 (ppFEV1) | Median: 36Mean: 37 (±5.5 SEM) | Median: 42Mean: 45 (±6.9 SEM) | P = 0.004(Wilcoxon signed-rank test) |
| Patient Population | 9 adults with cystic fibrosis (8 female, 1 male)Median age: 32 years (range 22-46) | 7-10 days of nebulized phage therapy(1 × 10¹⁰ PFU twice daily for inpatients, daily for outpatients) | No adverse events reported |
Phage-Antibiotic Synergy (PAS)
Emerging evidence demonstrates potent synergistic effects between phages and conventional antibiotics [54]. Phages can disrupt bacterial biofilms, enhancing antibiotic penetration to previously inaccessible bacterial populations. Additionally, phage-induced stress responses can alter bacterial metabolism, increasing susceptibility to specific antibiotic classes. This approach enables the use of previously ineffective antibiotics at lower concentrations, reducing toxicity and resistance selection pressure.
Experimental Protocol: Adaptive Phage Evolution
Objective: Generate phage variants with expanded host range against antibiotic-resistant bacterial strains through directed evolution.
Materials:
- Bacterial target strains (including antibiotic-resistant clinical isolates)
- Natural phage isolates from environmental sources (water, soil, wastewater)
- Growth media (LB broth, agar plates)
- Phage buffer (SM buffer)
- Norgen Biotek's Phage DNA Isolation Kit (Cat. 46800) [54]
- Oxford Nanopore Technologies and Illumina sequencing platforms
Methodology:
- Phage Isolation and Characterization: Isolate phages from environmental samples using the double-agar overlay method against target bacterial strains. Purify phage DNA using commercial kits for genomic sequencing and analysis to confirm lytic potential and absence of virulence or antibiotic resistance genes [54].
- Serial Passaging: Co-culture phages with evolving bacterial populations in liquid media. Each passage involves:
- Infecting log-phase bacterial cultures with phage stock at multiplicity of infection (MOI) of 0.1-1
- Incubating with aeration until lysis occurs (typically 4-24 hours)
- Filtering supernatant through 0.22μm membrane to remove bacteria
- Using filtrate to infect fresh bacterial culture for subsequent passage
- Selection Pressure Application: Introduce increasingly resistant bacterial populations through:
- Alternating between different bacterial strains with varied resistance mechanisms
- Incorporating antibiotics at sub-inhibitory concentrations to select for phages that work synergistically
- Using biofilm-grown bacteria to select for enhanced penetration capability
- Plaque Assay and Isolation: Periodically plate phage samples using the double-agar overlay method. Select individual plaques with desired characteristics (clearer plaques, larger zones of lysis) for further amplification and characterization.
- Characterization of Evolved Phages: Evaluate evolved phages for:
- Host range expansion against original and novel bacterial strains
- Burst size and latent period through one-step growth curves
- Genomic stability through resequencing
- Synergy with antibiotics through checkerboard assays
Validation: Assess therapeutic efficacy in relevant infection models (e.g., biofilm models, animal infection models) comparing evolved versus ancestral phages.
Research Reagent Solutions for Phage Therapy
Table 2: Essential Research Reagents for Phage Therapy Development
| Reagent/Category | Specific Examples | Research Function |
|---|---|---|
| Phage DNA Isolation Kits | Norgen Biotek Phage DNA Isolation Kit (Cat. 46800) [54] | High-quality viral DNA purification for genomic sequencing and analysis |
| Bacterial Culture Media | LB Broth, LB Agar, Soft Agar | Cultivation of bacterial hosts and phage propagation |
| Sequencing Platforms | Oxford Nanopore Technologies, Illumina Systems | Complete phage genome assembly and annotation |
| Animal Infection Models | Murine wound infection, Pulmonary infection models | In vivo efficacy and safety testing of phage preparations |
| Biofilm Models | Static biofilm assays, Flow cell systems | Assessment of phage penetration and biofilm disruption capability |
CRISPR-Cas Systems: Precision Gene Targeting
Molecular Mechanisms and System Diversity
The CRISPR-Cas (Clustered Regularly Interspaced Short Palindromic Repeats-CRISPR associated) system constitutes an adaptive immune system in prokaryotes that provides sequence-specific protection against foreign genetic elements, including plasmids and phages [57]. This system has been harnessed as a powerful genetic engineering tool with specific applications in combating antimicrobial resistance.
CRISPR-Cas systems are categorized into two primary classes:
- Class 1 (Types I, III, IV): Utilize multi-protein complexes for target interference [57]
- Class 2 (Types II, V, VI): Employ single effector proteins (e.g., Cas9, Cas12, Cas13) for simplified genome editing applications [57]
The Type II CRISPR-Cas9 system, derived from Streptococcus pyogenes, represents the most extensively characterized and utilized system for antimicrobial applications. Its mechanism involves three functional stages:
- Adaptation: Cas1 and Cas2 proteins facilitate the acquisition of foreign DNA spacers into the CRISPR array [58]
- Expression: Transcription and processing of the CRISPR array into mature CRISPR RNA (crRNA) [58]
- Interference: crRNA guides the Cas9 nuclease to complementary DNA sequences, resulting in double-strand breaks at sites adjacent to a Protospacer Adjacent Motif (PAM, 5'-NGG for Cas9) [58] [57]
Antimicrobial Applications and Delivery Strategies
CRISPR-Cas systems can be programmed to target specific antimicrobial resistance genes for selective elimination from bacterial populations. Successful applications include:
- Resensitization to Carbapenems: CRISPR-Cas9 delivery to eliminate carbapenemase genes (e.g., blaNDM, oxa23) in Enterobacteriaceae [56]
- Reversal of Plasmid-Mediated Resistance: Targeting mobile resistance genes (e.g., mcr-1 for colistin resistance, tet(X4) for tigecycline resistance) on conjugative plasmids [56]
- Chromosomal Resistance Ablation: Disruption of chromosomally-encoded resistance mechanisms through targeted mutation
A particularly innovative application involves engineering probiotic bacteria with CRISPR-Cas systems that prevent the acquisition of antibiotic resistance genes through horizontal gene transfer. A 2025 study demonstrated that an engineered CRISPR-Cas9 system could protect E. coli MG1655 and the probiotic strain E. coli Nissle 1917 from acquiring targeted resistance genes via transformation, transduction, and conjugation with 2-3 logs of protection efficiency [58].
Table 3: CRISPR-Cas Delivery Platforms for Antimicrobial Applications
| Delivery Platform | Mechanism | Advantages | Limitations |
|---|---|---|---|
| Engineered Bacteriophages | Phagemids, temperate phages, or modified virulent phages deliver CRISPR components | High target specificity, natural injection mechanism | Limited packaging capacity, host range restrictions |
| Conjugative Plasmids | Bacterial conjugation machinery transfers CRISPR-bearing plasmids | Broad host range potential, self-propagation | Slidespread dissemination concerns, regulatory challenges |
| Nanoparticles | Lipid or polymer-based nanoparticles encapsulate CRISPR components | Protection from degradation, tunable targeting | Variable delivery efficiency, potential cytotoxicity |
| Natural Transformation | Direct DNA uptake by competent bacteria | Simplicity for laboratory strains | Limited to naturally transformable species |
Experimental Protocol: Engineering Probiotics with CRISPR-Cas Protection
Objective: Create a probiotic strain resistant to horizontal acquisition of antibiotic resistance genes using a synthetic CRISPR-Cas9 system.
Materials:
- Bacterial strains: E. coli MG1655, E. coli Nissle 1917
- Plasmid vectors: pWEB-TNC, pBAD18-kan, pMM441-kan
- CRISPR components: synthesized CRISPR array targeting specific AMR genes, Cas9, tracrRNA
- Antibiotics: Kanamycin, Chloramphenicol, Ampicillin, Cefotaxime
- Molecular biology reagents: Restriction enzymes, Gibson Assembly mix, PCR reagents
Methodology:
- CRISPR-Cas9 Plasmid Construction:
- Amplify tracrRNA under BioBrick promoter pJ23104 and Cas9 under pJ23101 using specific primers
- Clone into pWEB-TNC vector using SalI/SmaI and SalI/BglII restriction sites, respectively
- Synthesize and clone a synthetic CRISPR array containing spacers targeting 8 specific AMR genes (e.g., tetM, ermB, VanA, aph-3, aac3, oxa23, blaNDM) [58]
- Verify final construct (pCRISPR+) using sequencing and diagnostic PCR
Bacterial Transformation:
- Introduce pCRISPR+ and control plasmids (pCRISPR-) into recipient strains via electroporation or heat shock
- Select transformants on appropriate antibiotic-containing media
Protection Efficiency Assessment:
- Transformation Assay: Introduce donor plasmids carrying targeted AMR genes via transformation; quantify protection by comparing transformation efficiencies
- Transduction Assay: Use phage-mediated transduction to transfer AMR genes; assess reduction in transductant formation
- Conjugation Assay: Co-culture with donor strains carrying conjugative plasmids with targeted AMR genes; enumerate transconjugants to measure conjugation blockade
Functional Validation:
- Challenge protected strains with antibiotics to confirm maintained susceptibility
- Perform genomic DNA extraction and sequencing to verify absence of acquired resistance genes
- Assess potential fitness costs through growth curve analysis
Validation: Demonstrate protection in complex microbial communities and animal infection models to evaluate performance under physiologically relevant conditions.
Anti-Virulence Strategies: Pathoblockers
Conceptual Framework and Molecular Targets
Anti-virulence therapeutics, termed "pathoblockers," represent a fundamentally different approach from traditional bactericidal agents. Rather than killing bacteria or inhibiting growth, these compounds selectively disrupt virulence factors essential for pathogenesis while leaving bacterial viability intact [59]. This approach minimizes selective pressure for resistance development and preserves beneficial commensal microbiota.
Promising molecular targets for anti-virulence strategies include:
- Adhesins and Biofilm Formation: Inhibition of initial attachment and biofilm development through targeting of microbial surface components recognizing adhesive matrix molecules (MSCRAMMs) in Gram-positive pathogens, or sortase A (SrtA), a membrane transpeptidase essential for surface protein anchoring [59]
- Toxin Production and Secretion: Neutralization of pore-forming toxins (e.g., LtxA in Aggregatibacter actinomycetemcomitans, α-hemolysin in S. aureus) using monoclonal antibodies or small molecule inhibitors [59]
- Quorum Sensing (QS) Systems: Disruption of bacterial cell-to-cell communication through degradation of autoinducers or blockade of their receptors, preventing coordinated virulence gene expression [59]
- Type III Secretion Systems (T3SS): Inhibition of needle complex assembly or effector protein translocation in Gram-negative pathogens like P. aeruginosa and Salmonella enterica [59]
Clinical Development and Approved Agents
The anti-virulence approach has transitioned from concept to clinical reality with several advanced candidates:
- Bezlotoxumab: First FDA-approved anti-virulence agent that neutralizes Clostridioides difficile toxin B (TcdB) [59]
- MEDI4893 (Suvratoxumab): Monoclonal antibody against S. aureus α-hemolysin that has completed Phase 2 clinical trials for pneumonia prevention [59]
- AR-301: Anti-α-hemolysin antibody that has entered Phase 3 trials for S. aureus pneumonia treatment [59]
Small molecule pathoblockers have also demonstrated promise in preclinical studies. Catechins (plant-derived flavonoids) can inhibit LtxA-mediated cytotoxicity by altering toxin structure and reducing cholesterol affinity [59]. INP0341, a salicylidene acylhydrazide, exhibits broad-spectrum T3SS inhibition across multiple Gram-negative pathogens [59].
Experimental Protocol: Anti-Virulence Compound Screening
Objective: Identify and characterize compounds that inhibit quorum sensing or toxin activity in multidrug-resistant pathogens.
Materials:
- Bacterial strains: P. aeruginosa PAO1, S. aureus MRSA strains
- Reporter constructs: Plasmid-based QS biosensors (e.g., lasB-gfp, rhlA-gfp)
- Cell culture lines: Human lung epithelial cells (A549), macrophages (THP-1)
- Compounds: Natural product libraries, synthetic small molecules
- Analytical tools: HPLC for autoinducer quantification, cytotoxicity assays
Methodology:
- Primary Screening - Quorum Sensing Inhibition:
- Transform P. aeruginosa with GFP reporter plasmids fused to QS-controlled promoters (lasB, rhlA)
- Grow reporter strains in presence of test compounds at sub-inhibitory concentrations
- Measure fluorescence intensity as indicator of QS activity
- Identify hits showing significant reduction in QS without affecting growth
Secondary Screening - Virulence Factor Quantification:
- Culture pathogens with and without active compounds
- Quantify extracellular virulence factors:
- Protease activity using azocasein degradation assays
- Pyocyanin production via chloroform extraction and absorbance measurement
- Hemolysin activity through erythrocyte lysis assays
- Assess biofilm formation using crystal violet staining and confocal microscopy
Mechanistic Studies:
- Extract and quantify autoinducer molecules (AHLs) using HPLC and mass spectrometry
- Perform RNA sequencing to analyze virulence gene expression patterns
- Conduct electrophoretic mobility shift assays to examine LuxR-type receptor binding
Efficacy Validation in Infection Models:
- Assess toxin neutralization in cell culture models using lactate dehydrogenase release assays
- Evaluate protection in Galleria mellonella infection models
- Validate efficacy in murine pneumonia or skin infection models
Validation Criteria: Compounds demonstrating significant reduction in virulence factor production or activity without bactericidal effects advance to further development.
Comparative Analysis and Future Directions
Integrated Therapeutic Approaches
The most promising applications of these innovative antimicrobial strategies involve their integration in complementary combinations:
- Phage-CRISPR Synergy: Engineered phages can deliver CRISPR-Cas systems specifically to target pathogens, creating "predator-prey" dynamics that selectively eliminate resistant subpopulations [56]
- Phage-Anti-Virulence Combinations: Phages that select for resistance trade-offs can be paired with anti-virulence compounds that exploit resulting vulnerabilities [53] [55]
- CRISPR-Enhanced Probiotics: Engineered probiotic strains with CRISPR systems that defend against horizontal gene transfer could prevent resistance dissemination in microbiome environments [58]
Regulatory and Commercialization Landscape
The regulatory framework for these novel antimicrobials is evolving to accommodate their unique characteristics. France recently authorized the first personalized phage therapy platform for veterinary use, establishing a validated framework for producing tailored phage combinations without requiring lengthy review cycles for each new formulation [60]. This platform approach represents a fundamental shift from traditional single-formulation approvals toward adaptable, evolving biological medicines.
However, significant challenges remain in the economic sustainability of antimicrobial development. Large pharmaceutical companies have largely abandoned antibiotic research due to unfavorable economics, with most innovation now occurring in small biotech companies and academic settings [61]. New economic models that recognize the societal value of antimicrobials are essential to support the development of these innovative therapies.
The escalating antimicrobial resistance crisis demands innovative approaches that move beyond traditional antibiotic paradigms. Phage therapy, CRISPR-Cas systems, and anti-virulence strategies each offer distinct mechanisms for addressing drug-resistant infections through targeted, evolution-informed approaches. Phages provide adaptable biological weapons that can co-evolve with bacterial defenses, CRISPR-Cas systems enable precise elimination of resistance genes, and anti-virulence compounds disarm pathogens without invoking strong selective pressure. The integration of these approaches, supported by evolving regulatory frameworks and sustainable economic models, represents the most promising path forward for addressing the global AMR threat. As research advances, these innovative therapeutic avenues will likely transform our approach to bacterial infections, shifting from broad-spectrum eradication to precision manipulation of microbial populations.
Exploiting Natural Products and Phytocompounds to Overcome Resistance Mechanisms
Antimicrobial resistance (AMR) represents one of the most pressing global public health threats of our time, with the World Health Organization (WHO) reporting that one in six laboratory-confirmed bacterial infections in 2023 were resistant to antibiotic treatments [7]. Between 2018 and 2023, antibiotic resistance rose in over 40% of the pathogen-antibiotic combinations monitored, with an average annual increase of 5–15% [7]. This crisis is particularly acute for Gram-negative pathogens such as Escherichia coli and Klebsiella pneumoniae, with more than 40% of E. coli and over 55% of K. pneumoniae globally now resistant to third-generation cephalosporins, the first-choice treatment for these infections [7]. The development of new antibiotics has stagnated due to scientific challenges and lack of economic incentives, with large pharmaceutical companies largely exiting antibiotic research and development [61]. In this context, natural products and phytocompounds derived from plants, fungi, and other biological sources offer a promising reservoir of novel antimicrobial agents and resistance-modifying compounds [62] [63]. This technical guide provides a comprehensive overview of current research on exploiting natural products to overcome bacterial resistance mechanisms, with specific methodologies and resources for researchers and drug development professionals.
Bacterial Resistance Mechanisms and WHO Priority Pathogens
Fundamental Antibiotic Resistance Mechanisms
Bacteria employ diverse biochemical strategies to circumvent antibiotic action, which can be broadly categorized into several core mechanisms as illustrated in Figure 1 and detailed in Table 1 [16].
Figure 1: Major bacterial antibiotic resistance mechanisms and phytocompound targeting
Table 1: Core antibiotic resistance mechanisms in bacteria
| Resistance Mechanism | Biochemical Basis | Example Genes/Proteins | Antibiotics Affected |
|---|---|---|---|
| Enzymatic Inactivation | Antibiotic modification or destruction via hydrolytic enzymes or transferases | β-lactamases (bla genes), Aminoglycoside-modifying Enzymes (AMEs) | β-lactams, Aminoglycosides [64] [65] |
| Efflux Pump Systems | Active transport of antibiotics out of bacterial cells | RND family (AcrAB-TolC), MFS family (NorA), MATE family | Multiple classes including fluoroquinolones, β-lactams [65] |
| Target Modification | Alteration of antibiotic binding sites to reduce drug affinity | Altered PBPs (mecA), methylated rRNA, mutated DNA gyrase | β-lactams, Macrolides, Fluoroquinolones [66] [65] |
| Reduced Permeability | Decreased antibiotic entry via porin loss or membrane alteration | OmpF/C porin loss, LPS modifications | β-lactams, Carbapenems, Quinolones [65] |
| Biofilm Formation | Structured communities embedded in extracellular matrix providing physical barrier | Polysaccharide synthesis genes (algD, psl), quorum-sensing systems | Multiple antibiotic classes [66] |
WHO Priority Pathogens and Resistance Patterns
The WHO has categorized antibiotic-resistant bacteria into critical, high, and medium priority groups based on the urgency for new antibiotics [62]. The critical priority group includes carbapenem-resistant Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacterales, which represent the most significant threats due to their resistance profiles and association with healthcare-associated infections [62] [64]. The global distribution of resistance shows concerning patterns, with the WHO South-East Asian and Eastern Mediterranean Regions experiencing the highest resistance rates, where 1 in 3 reported infections were resistant in 2023 [7]. Particularly alarming is the emergence and spread of carbapenem resistance, which was once rare but is becoming more frequent, narrowing treatment options and forcing reliance on last-resort antibiotics [7].
Phytocompound Classes and Their Antimicrobial Activities
Major Bioactive Phytocompound Classes
Plants produce a diverse array of secondary metabolites with demonstrated antimicrobial properties. Systematic reviews of research conducted between 2014 and 2024 have identified key phytocompound classes with efficacy against multidrug-resistant pathogens [62]. The distribution of these compound classes and their relative prevalence in antimicrobial research is summarized in Table 2.
Table 2: Major phytocompound classes with demonstrated antimicrobial activity against resistant pathogens
| Phytocompound Class | Chemical Structure | Primary Antimicrobial Mechanisms | Extraction Solvents (by efficiency) | Representative Active Compounds |
|---|---|---|---|---|
| Flavonoids (24.8% of derivatives studied) | C6-C3-C6 skeleton with phenolic structure | Membrane disruption, efflux pump inhibition, β-lactamase interference, biofilm reduction | Ethanol, Methanol, Ethyl acetate, Aqueous | Quercetin, Naringenin, Catechin [62] [64] |
| Alkaloids | Nitrogen-containing heterocyclic compounds | Nucleic acid intercalation, enzyme inhibition, membrane disruption | Ethanol, Methanol, n-Butanol | Piperine, Berberine, Sanguinarine [62] |
| Terpenoids | Isoprene polymer derivatives (C5H8)n | Membrane fluidity disruption, permeability alteration | Ethyl acetate, n-Hexane, Methanol | Thymol, Carvacrol, Artemisinin [62] [65] |
| Phenolic Compounds | Hydroxylated aromatic rings | Protein binding, enzyme inhibition, oxidative stress | Methanol, Acetone, Ethanol | Gallic acid, Ellagic acid, Curcumin [62] |
| Tannins | Polymerized phenolics | Protein precipitation, enzyme inhibition, membrane interaction | Acetone-Water, Methanol, Aqueous | Tannic acid, Ellagitannins [62] |
| Saponins | Steroid or triterpenoid glycosides | Membrane cholesterol complexation, pore formation | Methanol, Ethanol, Aqueous | α-Hederin, Dioscin [62] |
Quantitative Analysis of Phytocompound Efficacy
Recent systematic analysis of 4371 articles published between 2014 and 2024 identified 290 studies meeting rigorous inclusion criteria for evaluating natural products against antibiotic-resistant pathogens [62]. The research geography shows significant concentrations of studies in regions with rich biodiversity and traditional medicinal knowledge, including India (n=58), Cameroon (n=18), Brazil (n=19), Nigeria (n=14), Egypt (n=13), and China (n=12) [62]. The most frequently studied pathogens reflect the WHO priority list, with Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, Salmonella typhi, and Staphylococcus aureus emerging as the predominant targets due to their clinical significance and resistance profiles [62].
Experimental Methodologies for Evaluating Phytocompound Efficacy
Standardized Screening Protocols
Plant Material Collection and Extraction:
- Plant Selection and Authentication: Select plant materials based on ethnobotanical knowledge or chemotaxonomic relationships. Collect plant parts (leaves, bark, roots, flowers) and authenticate by trained botanists. Voucher specimens should be deposited in herbariums [63].
- Drying and Powdering: Air-dry plant materials in shade (25-28°C) or using freeze-dryers. Grind to fine powder (20-40 mesh) using mechanical grinders to increase surface area for extraction [62].
- Extraction Methods: Employ sequential extraction using solvents of increasing polarity (n-hexane → ethyl acetate → methanol → water). Standardized protocols recommend solvent-to-material ratio of 10:1 (v/w), with extraction times of 24-72 hours using orbital shakers (120 rpm) at room temperature, or using Soxhlet apparatus for non-polar solvents [62] [64].
- Extract Concentration: Filter extracts through Whatman No. 1 filter paper and concentrate under reduced pressure at 40°C using rotary evaporators. Preserve extracts at -20°C until use [64].
Antimicrobial Susceptibility Testing:
- Initial Screening - Disk Diffusion Assay: Prepare Mueller-Hinton agar plates. Swab standardized inoculum (0.5 McFarland, ~1.5 × 10^8 CFU/mL) of test pathogens. Apply sterile filter paper disks (6 mm diameter) impregnated with 10-20 μL of plant extracts (10-100 mg/mL in appropriate solvent). Include solvent controls and standard antibiotic controls. Incubate at 37°C for 18-24 hours. Measure zones of inhibition in millimeters [63].
- Minimum Inhibitory Concentration (MIC) Determination: Employ broth microdilution method in 96-well plates according to CLSI guidelines. Prepare two-fold serial dilutions of plant extracts (typically 0.5-512 μg/mL) in cation-adjusted Mueller-Hinton broth. Inoculate with 5 × 10^5 CFU/mL of test organisms. Include growth controls and sterility controls. Incubate at 37°C for 18-24 hours. Add resazurin indicator (0.02%) for visual detection of growth. MIC defined as lowest concentration showing no visible growth [64] [65].
- Minimum Bactericidal Concentration (MBC) Determination: Subculture 10 μL from wells showing no growth in MIC assay onto fresh Mueller-Hinton agar plates. Incubate at 37°C for 18-24 hours. MBC defined as lowest concentration showing 99.9% killing of initial inoculum [65].
Mechanism-Specific Assay Protocols
Efflux Pump Inhibition Assays:
- Ethidium Bromide Accumulation Assay: Grow bacteria to mid-log phase. Wash and resuspend in PBS with glucose (0.4%). Divide suspension into aliquots with and without potential efflux pump inhibitors. Add ethidium bromide (1 μg/mL). Monitor fluorescence (excitation 530 nm, emission 600 nm) over time using fluorometer. Increased fluorescence indicates efflux pump inhibition [65].
- Checkerboard Synergy Assays: Prepare two-dimensional serial dilutions of antibiotic and phytocompound in 96-well plates. Inoculate with standardized bacterial suspension. Calculate Fractional Inhibitory Concentration (FIC) index: FIC index = (MIC of antibiotic in combination/MIC of antibiotic alone) + (MIC of phytocompound in combination/MIC of phytocompound alone). Synergy defined as FIC index ≤0.5 [64] [65].
Biofilm Inhibition and Eradication Assays:
- Crystal Violet Biofilm Assay: Grow biofilms in 96-well plates for 24-48 hours. Treat with sub-MIC concentrations of phytocompounds. Fix biofilms with methanol, stain with 0.1% crystal violet, solubilize in acetic acid (30%), measure absorbance at 595 nm [66].
- Confocal Microscopy of Biofilms: Grow biofilms on glass coverslips. Treat with phytocompounds. Stain with LIVE/DEAD BacLight Bacterial Viability Kit (SYTO9 and propidium iodide). Visualize using confocal laser scanning microscopy to determine bactericidal activity and biofilm architecture changes [66].
Time-Kill Kinetics Assay: Prepare bacterial suspension (~10^6 CFU/mL) in Mueller-Hinton broth. Treat with phytocompounds at 1×, 2×, and 4× MIC. Remove aliquots at 0, 2, 4, 6, 8, 12, and 24 hours. Perform serial dilutions and plate on Mueller-Hinton agar. Count colonies after incubation. Plot log10 CFU/mL versus time. Bactericidal activity defined as ≥3 log10 reduction in CFU/mL from initial inoculum [65].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential research reagents and materials for phytocompound antimicrobial research
| Category | Specific Reagents/Materials | Function/Application | Technical Notes |
|---|---|---|---|
| Extraction Solvents | Ethanol, Methanol, Ethyl Acetate, n-Hexane, n-Butanol, Aqueous solutions | Phytocompound extraction based on polarity | Ethanol and methanol most effective for broad-spectrum extraction; ethanol preferred for its lower toxicity [62] |
| Culture Media | Mueller-Hinton Agar/Broth, Tryptic Soy Broth, Luria-Bertani Medium | Bacterial cultivation and antimicrobial susceptibility testing | Mueller-Hinton recommended by CLSI for standardized susceptibility testing [63] |
| Reference Strains | ATCC 25922 (E. coli), ATCC 27853 (P. aeruginosa), ATCC 29213 (S. aureus), ATCC 25923 (S. aureus) | Quality control and assay standardization | Essential for validating experimental conditions and comparing results across studies [64] |
| Resistance Indicators | Ethidium bromide, Rhodamine 6G, Resazurin, Crystal violet | Assessment of efflux pump activity, viability, and biofilm formation | Resazurin used for visual MIC determination; ethidium bromide for efflux studies [65] |
| Synergy Testing Materials | 96-well microtiter plates, Multipipettes, Plate readers | Checkerboard assays for combination therapy assessment | Automated systems improve reproducibility for high-throughput screening [64] |
| Analytical Standards | Reference antibiotics (Ciprofloxacin, Vancomycin, Imipenem), Phytochemical standards (Quercetin, Berberine) | Method validation and compound quantification | Essential for HPLC calibration and activity comparison [62] [63] |
Research Workflow and Data Analysis Framework
The standard experimental workflow for evaluating phytocompounds against resistant pathogens follows a systematic progression from initial screening to mechanistic studies, as illustrated in Figure 2.
Figure 2: Standardized research workflow for phytocompound evaluation
Data Interpretation Guidelines
- MIC Value Classification: MIC ≤ 100 μg/mL considered promising for crude extracts; MIC ≤ 10 μg/mL considered promising for purified compounds [64]
- Synergy Interpretation: FIC index ≤0.5 = synergy; 0.5-4.0 = indifference; >4.0 = antagonism [65]
- Time-Kill Kinetics: Bactericidal = ≥3 log10 CFU/mL reduction; Bacteriostatic = <3 log10 reduction [65]
- Statistical Analysis: Minimum triplicate experiments with appropriate controls; statistical significance determined by ANOVA with post-hoc tests (p<0.05) [62]
The systematic investigation of natural products and phytocompounds represents a promising strategy to address the escalating crisis of antimicrobial resistance. The rich chemical diversity of plant-derived compounds provides multiple mechanisms to counter bacterial resistance, including efflux pump inhibition, biofilm disruption, and enzyme interference. Standardized methodologies for extraction, screening, and mechanism elucidation are essential for generating comparable and reproducible data across research laboratories. As resistance continues to evolve, integrating modern technologies such as artificial intelligence for resistance prediction and natural product screening, along with advanced analytical techniques for compound identification, will accelerate the discovery and development of novel antimicrobial agents from natural sources [66] [14]. The continued exploration of phytocompounds, particularly in combination with conventional antibiotics, offers a viable pathway to extend the utility of existing antibiotics and address the critical threat of multidrug-resistant pathogens identified by the WHO.
The escalating global crisis of antimicrobial resistance (AMR) represents one of the most pressing challenges to modern medicine. Bacterial species with innate antibiotic resistance deploy sophisticated defense mechanisms, including biofilm formation, efflux pumps, enzymatic inactivation of drugs, and target modification, rendering conventional monotherapies increasingly ineffective [67] [68]. This has catalyzed a paradigm shift toward combinatorial therapeutic strategies that simultaneously target multiple bacterial vulnerabilities, thereby bypassing innate defenses and restoring therapeutic efficacy. The World Health Organization reports alarming resistance rates, with over 40% of Escherichia coli and 55% of Klebsiella pneumoniae isolates now resistant to third-generation cephalosporins, highlighting the critical need for innovative approaches [68].
This technical guide examines the scientific foundation and practical application of synergistic combination therapies against multidrug-resistant (MDR) pathogens. By integrating insights from advanced therapy medicinal products (ATMPs), nanotechnology, natural products, and evolved biologics, we provide researchers and drug development professionals with a comprehensive framework for designing and implementing next-generation antimicrobial regimens. These approaches collectively aim to outmaneuver bacterial resistance through multi-mechanistic actions that overwhelm bacterial adaptive capabilities and reduce the emergence of resistant subpopulations [67] [69].
Advanced Therapeutic Modalities
Resistance Mechanism Exploitation
A groundbreaking "resistance hacking" approach strategically turns a bacterium's own defense systems against itself. Recent proof-of-concept research demonstrates that structurally modified florfenicol can exploit the WhiB7 resistome in Mycobacterium abscessus, converting drug resistance mechanisms into vulnerabilities [20].
Table 1: Key Components of the WhiB7 Resistance Exploitation System
| Component | Function | Therapeutic Exploitation |
|---|---|---|
| WhiB7 | Master regulator of ribosomal stress response | Activation perpetuates antibiotic cascade |
| Eis2 | Drug resistance protein | Converts prodrug to active form |
| Modified Florfenicol | Prodrug design | Inactive until converted by bacterial enzymes |
| Ribosomal Targeting | Primary antibiotic mechanism | Enhanced by continuous WhiB7 activation |
The engineered florfenicol prodrug is selectively activated by Eis2, a resistance protein induced by WhiB7. As WhiB7 activates, more Eis2 proteins are produced, generating increased active drug, which further inhibits the ribosome and activates WhiB7 in a perpetual cascade that continuously amplifies the antibiotic effect [20]. This approach demonstrates exceptional specificity for M. abscessus and closely related species, minimizing mitochondrial toxicity and microbiome disruption associated with long-term conventional antibiotic regimens.
Diagram 1: Resistance Hacking Cascade. This diagram illustrates the perpetual amplification cycle where bacterial resistance mechanisms are exploited to enhance antibiotic efficacy.
Nanotechnology-Enhanced Delivery Systems
Nanotechnology-based delivery platforms significantly improve the stability, targeting, and bioavailability of antimicrobial agents while enabling controlled release profiles [67]. These systems are particularly effective against biofilm-associated infections, which traditionally demonstrate heightened resistance to conventional antibiotics.
Table 2: Advanced Nanotechnology-Based Delivery Systems for Combating AMR
| Nanocarrier System | Active Component | Key Properties | Efficacy Metrics |
|---|---|---|---|
| Vancomycin-loaded multivesicular liposomes | Vancomycin HCl | >90% encapsulation efficiency | Sustained release up to 19 days (vs. 6-8h for free drug) [67] |
| Silver-poly(ionic liquid) nanocomposite | Silver nanoparticles | Intrinsic antibacterial properties | Effective against E. coli and S. aureus [67] |
| Cs@Pyc.SOF hybrid nanocomposite | Sofosbuvir, pycnogenol, chitosan | 83% drug-loading efficiency | Controlled release up to 94% over 48h [67] |
| Self-nanomicellizing solid dispersion (Soluplus) | Narasin | 100-fold solubility increase | Superior skin penetration, strong antibacterial activity [67] |
| Garlic-derived AgNPs | Silver nanoparticles, ciprofloxacin | 15-20 nm particle size | 28±0.5 mm inhibition zone, MIC 100 mg/mL, synergistic with ciprofloxacin (FIC index=0.37) [69] |
These nanocarriers overcome multiple bacterial defense mechanisms through enhanced biofilm penetration, efflux pump evasion, and targeted intracellular delivery. The hybrid nanocomposite Cs@Pyc.SOF demonstrates particularly impressive controlled release kinetics, achieving 94% drug release over 48 hours while maintaining therapeutic concentrations at the infection site [67]. Similarly, the SabiWhite-loaded ethosomal topical delivery system exhibits sustained release (93.12% over 24 hours) with significant in-vivo edema reduction (36.17%) comparable to Diclofenac gel (41.92%) [69].
Evolved Biologics and Phage Therapy
Experimental evolution techniques have enabled significant advances in bacteriophage therapy, overcoming the traditional limitation of extreme strain specificity. Researchers at UC San Diego successfully "trained" phages to adapt against Klebsiella pneumoniae defenses through a 30-day co-evolution protocol [70].
Experimental Evolution Protocol:
- Initial phage selection: Identify baseline phages with partial activity against target bacterial strains
- Serial co-culture: Iterative cycles of phage-bacteria co-incubation under controlled laboratory conditions
- Selective pressure: Periodic isolation and amplification of phages demonstrating improved lytic capability
- Genetic characterization: Whole-genome sequencing of evolved phages to identify adaptive mutations
- Efficacy validation: Testing evolved phages against multidrug-resistant and extensively drug-resistant strains
This process yielded phages with acquired mutations in genes responsible for bacterial cell recognition and binding, resulting in expanded host range and enhanced bacterial growth suppression over extended periods [70]. The evolved phages demonstrated efficacy against drug-resistant K. pneumoniae, a pathogen responsible for severe hospital-acquired infections including pneumonia and sepsis.
Diagram 2: Phage Experimental Evolution Workflow. This protocol enables bacteriophages to overcome bacterial defenses through directed evolution, resulting in expanded host range against drug-resistant pathogens.
Natural Product Synergy
Natural products and plant-derived compounds offer rich sources of antimicrobial agents with novel mechanisms of action that can synergize with conventional antibiotics. These combinations are particularly valuable against multidrug-resistant pathogens where standard treatments have failed.
Table 3: Natural Product-Antibiotic Synergistic Combinations
| Natural Product | Synergistic Antibiotic | Target Pathogens | Key Findings |
|---|---|---|---|
| Indian Borage extract | Amikacin | Resistant isolates | >50% of resistant isolates became sensitive; reduced pulmonary lesions and splenic damage in mouse models [69] |
| δ-Carene (from Cissampelos oppositifolia) | Amoxicillin, Erythromycin | MRSA, E. coli | MIC 0.04 mg/mL (MRSA), 0.05 mg/mL (E. coli); rapid killing (2-4h) in time-kill assays [69] |
| Propolis and essential oils | Various antibiotics | Multiple MDR pathogens | Enhanced efficacy in nanotechnology delivery systems; disruption of bacterial membranes [67] |
| Tea tree essential oils | Conventional antibiotics | Biofilm-forming pathogens | Incorporation into novel drug delivery systems enhances antibiofilm activity [67] |
The molecular basis for these synergistic effects includes bacterial membrane disruption, efflux pump inhibition, and structural modifications to antibiotic targets. FTIR/UV spectral data confirm structural changes in bacterial cells following combination treatment, while molecular docking studies demonstrate favorable binding interactions between natural compounds and antibiotics [69]. For instance, Indian Borge extract combined with amikacin demonstrated significantly reduced pulmonary lesions and splenic damage in mouse models compared to antibiotic therapy alone [69].
Computational and Immunological Approaches
Computational Drug Discovery and Epitope Mapping
Artificial intelligence and computational screening methods are accelerating the identification of novel antimicrobial compounds and therapeutic targets. Virtual screening of natural products against the metallo-β-lactamase VIM-1 of Pseudomonas aeruginosa identified four inhibitors (CNP0390322, CNP03905695, CNP0079056, CNP0338283) with superior docking scores and stable interactions in one-microsecond molecular dynamics simulations [69]. These inhibitors show potential for restoring β-lactam activity against resistant strains.
In immunotherapeutic development, computational mapping of Staphylococcal Protein A (SpA) epitopes has enabled the construction of multi-epitope vaccines demonstrating high binding affinities to HLA and TLR-4 interactions, representing promising vaccine candidates against MRSA [69]. Similarly, analysis of non-structural proteins of hepatitis C virus identified 27 CTL epitopes, three with >90% conservation and strong immunogenic responses after docking to HLA-A*02:01 and TLR-3 [69].
Immunomodulatory Combinations
Strategic immunomodulation represents a promising approach for enhancing antimicrobial efficacy while minimizing collateral damage to protective immunity. Research comparing thymoglobulin (START trial), teplizumab (AbATE trial), and alefacept (T1DAL trial) revealed that successful therapies induce T cell exhaustion phenotypes rather than broad depletion [71].
Key Immunomodulatory Protocol:
- Agent Selection: Prefer partial agonists over broad depletors (e.g., teplizumab, alefacept)
- Phenotypic Monitoring: Track PD1/TIGIT/KLRG1 and EOMES markers indicating T cell exhaustion
- Regulatory Cell Preservation: Avoid therapies that deplete regulatory T cells (e.g., abatacept in ACCESS trial)
- Combination Timing: Administer pro-regulatory therapies during remission windows when tissue environment supports reprogramming
Notably, alefacept treatment generated CD8 T cells with two beneficial states: one characterized by TIGIT/PD1/EOMES (exhaustion markers) and another with CD57/KIR induction (regulatory markers), both correlating with positive clinical outcomes [71]. This approach highlights the importance of balancing effector inhibition with regulatory support for durable treatment responses.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Investigating Combination Therapies
| Reagent/Category | Specific Examples | Research Application | Key Characteristics |
|---|---|---|---|
| Click Chemistry Reagents | Thiol-maleimide, 1,2,3-triazole | Antimicrobial dendrimeric peptide synthesis | Enables di-branched and tetra-branched analogues with enhanced activity [67] |
| Nanocarrier Systems | PLGA-cholesterol hybrid NPs, Liponiosomes (LNs) | Intracellular drug delivery | Anionic NPs show enhanced trypanocidal activity against intracellular amastigotes [67] |
| Zwitterionic Polymers | Poly(sulfur ylides) | Anti-biofilm surface coatings | Disrupts bacterial membranes without human cell toxicity [67] |
| Metal-Organic Frameworks | NG-MOF-5@LNs | Targeted antimicrobial delivery | Monodispersed spherical particles with IC50 21 µg/mL against MCF-7 cells [67] |
| Biosurfactant Nanoemulsions | Various formulations | Broad-spectrum antibiofilm applications | Significant effects against E. coli and S. aureus biofilms [67] |
| IL-2 Agonist Formulations | Selective IL-2 receptor targeting | Regulatory T cell expansion | Preferential targeting of high-affinity IL-2 receptor on Tregs [71] |
These research tools enable the development and testing of innovative combination approaches. Click chemistry reagents, for instance, have been used to create di-branched analogues of battacin that demonstrate up to 40-fold higher selectivity for bacteria and fungi, with improved membrane lysis, faster killing kinetics, and strong antibiofilm activity [67]. Similarly, zwitterionic polymers like poly(sulfur ylides) offer safer alternatives to polyethylene glycol for preventing bacterial biofilms on medical devices and protective coatings [67].
The strategic integration of multiple therapeutic modalities represents the most promising approach to overcoming the formidable defense mechanisms of naturally resistant bacterial species. By simultaneously targeting disparate bacterial processes—through mechanisms such as resistance hacking, nanoparticle-enhanced delivery, evolved phage therapy, and natural product synergy—these combination approaches create a multi-front assault that overwhelms bacterial adaptive capacity.
The future of antimicrobial development lies in this combinatorial paradigm, which demands continued innovation in delivery platforms, computational prediction tools, and mechanistic understanding of resistance pathways. As bacterial evolution continues to outpace traditional antibiotic development, these sophisticated synergistic strategies offer the best hope for restoring therapeutic efficacy against even the most recalcitrant pathogens. Success will require collaborative efforts across disciplines—from structural biology and nanotechnology to computational science and immunology—to design the next generation of intelligent combination therapies that can stay ahead of bacterial resistance evolution.
Navigating R&D Roadblocks: From Diagnostic Gaps to Economic Hurdles
The pipeline for novel antibiotics is critically underfunded, not due to a lack of scientific capability, but because of profound and persistent market failures. This innovation gap poses a dire threat to global public health, especially as antimicrobial resistance (AMR) continues to rise. This technical guide examines the economic structures that disincentivize antibiotic development, analyzes the scientific complexities that underpin the value of novel agents, and details emerging economic models and innovative research strategies designed to bridge this gap. Understanding the confluence of these factors is essential for researchers, scientists, and drug development professionals aiming to navigate and rectify the broken antimicrobial development ecosystem.
The Economic Case: Analyzing the Market Failure
The core problem facing antibiotic development is not scientific but economic. The traditional profit-driven pharmaceutical model struggles to deliver new antibiotics due to a combination of misaligned incentives and market dynamics [72].
Root Causes of the Economic Disincentive
- Low Financial Returns: Antibiotics are inherently less profitable than drugs for chronic conditions. They are typically used for short-course treatments and are often held in reserve as drugs of last resort due to antimicrobial stewardship principles, deliberately limiting their volume of use [72] [73].
- The "Fire Extinguisher" Problem: New antibiotics are seen as critical infrastructure—essential to have but undesirable to use frequently. This stewardship imperative directly conflicts with the traditional volume-based sales model, destroying the economic incentive for development [72].
- Crowding Out by Generics: The market is saturated with cheap, effective generic antibiotics, which makes it difficult for newer, more expensive ones to achieve significant market share and recoup development costs [72].
- High Development Costs and Risk: The cost of meeting regulatory requirements is high, and the probability of success in the drug development pipeline remains low. This creates a high-risk, low-reward scenario for investors [72].
The consequences of this market failure are stark. Between 2016 and 2019, several major pharmaceutical companies, including Novartis, Sanofi, AstraZeneca, and GSK, moved away from antimicrobial research [72]. Furthermore, multiple small and medium-sized enterprises (SMEs), which account for 81% of antibacterial programs, have faced bankruptcy even after successfully gaining regulatory approval for novel antibiotics [72].
The Scale of the Financial Gap
Recent economic analyses have quantified the investment required to create a viable pull incentive. The table below summarizes the "fair share" annual revenue targets needed from G7+EU27 countries to support a sustainable antibiotic pipeline, based on their relative Gross Domestic Product (GDP) [74].
Table 1: Annual Global Revenue Targets for Effective Antibacterial Pull Incentives (G7+EU27)
| Target Scenario | Annual Global Revenue Target (USD 2024) | Contextual Benchmark |
|---|---|---|
| Low-End | $258 million | Consistently over ten years [74] |
| Mid-Range | $363 million | Would rank ~230th globally among drugs by revenues [74] |
| High-End | $562 million | Consistently over ten years [74] |
A 2021 analysis suggested that the discounted net present value of a new antibiotic is approximately $240 million, which is considerably below its probable development costs [72]. Other estimates indicate that a reward of $2 billion to $4 billion per new antibiotic is needed to cover development costs and the cost of failed attempts across the portfolio [73].
The Scientific Basis: Intrinsic Resistance and the Value of Innovation
The economic challenges exist alongside formidable scientific hurdles. Bacteria possess a vast arsenal of natural and acquired defense mechanisms, making the discovery of agents with novel targets exceptionally difficult.
Fundamental Mechanisms of Antimicrobial Resistance
Bacterial resistance can be intrinsic (a natural trait of a species) or acquired through genetic mutation or horizontal gene transfer [5] [75]. The primary biochemical resistance mechanisms are summarized below.
Table 2: Core Mechanisms of Antimicrobial Resistance in Bacteria
| Mechanism | Functional Description | Example |
|---|---|---|
| Limiting Uptake | Reduces drug permeability, particularly through the outer membrane in Gram-negative bacteria [5]. | The LPS layer in Gram-negatives provides intrinsic resistance to many agents [75]. |
| Drug Inactivation | Enzymatic destruction or modification of the antibiotic molecule [5]. | Production of β-lactamases that hydrolyze β-lactam antibiotics [5]. |
| Target Modification | Alteration of the bacterial target site to reduce antibiotic binding [5]. | Mutation in DNA gyrase conferring resistance to quinolones [5]. |
| Active Efflux | Energy-dependent pumping of antibiotics out of the cell [5]. | Upregulation of multidrug-efflux pumps in Pseudomonas aeruginosa [5]. |
The Special Case of Biofilms
Biofilms represent a critical challenge in treating persistent infections. These structured microbial communities are encased in an extracellular polymeric substance (EPS) matrix and exhibit intrinsic tolerance to antibiotics, which is distinct from genetic resistance [76] [77]. The biofilm matrix acts as a physical barrier, limiting antibiotic penetration. Furthermore, biofilms contain metabolically heterogeneous populations, including dormant persister cells, which are unaffected by antibiotics targeting active cellular processes [76] [5]. The dense, structured environment of a biofilm also accelerates horizontal gene transfer (HGT), making these communities hotspots for the dissemination of resistance genes [76].
Emerging Solutions: Economic and Scientific Innovation
Pioneering Economic Models: Delinked Payments
To address the market failure, "delinked" payment models are being piloted. In this system, a government or health service provides a payment to the manufacturer that is disconnected from the volume of antibiotic sold [73]. This model directly addresses the core conflict between stewardship and profit.
- How it Works: A health technology assessment body determines the lifetime value of a new antibiotic to the healthcare system. A payment is then negotiated, often an annual "subscription," that reflects a proportion of this value during the patent period [73].
- Key Benefits:
- Removes incentive for over-promotion: Companies are not driven to maximize sales, aligning with stewardship goals.
- Rewards innovation, not volume: The payment is based on the drug's value as a health security asset.
- Brings revenue forward: Provides a return on investment during the exclusivity period [73].
The UK's NHS is a pioneer in this area, having piloted a delinked subscription model. The pilot initially offered up to £10 million annually per antibiotic, with revised proposals increasing this to £20 million per year [73].
The STEDI Value Framework
A critical component of delinked models is the "STEDI" framework, used to quantify the full population-level value of a new antibiotic beyond direct patient benefit [73]:
- Spectrum: Value of having a narrow-spectrum agent to target specific resistant pathogens.
- Transmission: Value of reducing the spread of resistant pathogens.
- Enablement: Value of enabling modern medicine (e.g., surgery, chemotherapy) that relies on effective antibiotics.
- Diversity: Value of having a diverse arsenal of antibiotics to slow resistance.
- Insurance: Value of having an effective antibiotic available for a future catastrophic AMR outbreak [73].
The insurance value is particularly noteworthy, as it represents a premium society is willing to pay to mitigate the risk of a low-probability, high-impact AMR catastrophe, analogous to purchasing fire insurance [73].
Innovative Research Methodologies and Reagents
Scientific innovation is compressing the discovery timeline and opening new avenues for antibiotic development.
Table 3: Research Reagent Solutions for Modern Antibiotic Discovery
| Research Tool / Reagent | Primary Function in Antibiotic Discovery |
|---|---|
| Machine Learning (ML) Models | Parse biological and chemical data to identify patterns predictive of antimicrobial activity; generate novel molecular structures [78]. |
| Genomic & Proteomic Databases | Provide the raw "blueprints" of life (from both modern and extinct organisms) for mining potential antimicrobial peptides [78]. |
| Synthetic Chemical Libraries (Building Blocks) | Enable generative AI models to design billions of novel, yet synthetically feasible, antibiotic candidates [78]. |
| High-Throughput Robotic Screening Systems | Automate the testing of thousands of synthesized molecule candidates against bacterial targets [78]. |
| Standardized Bacterial Panels (e.g., ESKAPE pathogens) | Provide consistent, clinically relevant targets for in vitro evaluation of compound efficacy [76]. |
| Biofilm Reactors & Models | Facilitate the study of antibiotic efficacy against biofilms, which is crucial for assessing activity against persistent infections [76] [77]. |
Experimental Workflow: AI-Driven Antibiotic Discovery
The following diagram visualizes a modern, AI-accelerated workflow for discovering novel antibiotics, integrating methodologies from multiple pioneering labs [78].
Protocol: Mining Genomic Data for Antimicrobial Peptides
This protocol outlines the process of using public data to discover natural antimicrobial peptides, a strategy exemplified by the work of de la Fuente et al. [78].
- Objective: To identify novel Antimicrobial Peptides (AMPs) from genomic and proteomic sequencing data.
- Materials:
- Hardware: High-performance computing cluster.
- Software: Machine learning frameworks (e.g., TensorFlow, PyTorch), sequence alignment tools (BLAST).
- Data: Publicly available proteomic/genomic databases (e.g., NCBI, ancient organism proteomes).
- Reagents: Solid-phase peptide synthesizer, reagents for peptide synthesis, bacterial culture media, standard bacterial strains (e.g., ESKAPE pathogens).
- Methodology:
- Data Acquisition & Curation: Download and rigorously curate proteomic datasets. This includes standardizing data formats and integrating experimentally determined Minimum Inhibitory Concentration (MIC) data for known AMPs to serve as a training set.
- Model Training: Train a machine learning model (e.g., a neural network) to recognize sequence features and patterns associated with antimicrobial activity using the curated training data.
- Prediction & In Silico Screening: Deploy the trained model to screen the entire proteomic database. The model will output a ranked list of peptide sequences predicted to have high antimicrobial potential.
- Peptide Synthesis: Select top candidate peptides for chemical synthesis using standard solid-phase peptide synthesis (SPPS) techniques.
- In Vitro Validation:
- Resuspend the synthesized peptides and determine concentration.
- Perform broth microdilution assays according to CLSI guidelines against a panel of target bacteria to determine experimental MICs.
- Evaluate cytotoxicity against mammalian cell lines to assess selective toxicity.
- In Vivo Validation: Progress lead candidates with favorable in vitro profiles to animal infection models (e.g., mouse skin abscess or thigh infection models) [78].
Addressing the innovation gap in antibiotic development requires a fundamental shift from a purely market-driven model to a public health-driven, collaboratively financed framework. The scientific tools—from AI to genomics—are increasingly powerful. The primary barrier is now economic and political. Widespread global adoption of delinked pull incentives that meet "fair share" targets, coupled with continued robust funding for push initiatives like CARB-X, is essential to create a sustainable ecosystem. For researchers and drug developers, success will depend on engaging with these new economic models while leveraging cutting-edge scientific methodologies to efficiently deliver the next generation of antimicrobial therapies that our healthcare system desperately needs.
Overcoming Diagnostic Challenges for Rapid Identification of Resistant Infections
Antimicrobial resistance (AMR) represents one of the most severe global public health threats, projected to cause 10 million deaths annually by 2050 with an estimated economic loss of $100 trillion [79] [80]. In the United States alone, healthcare providers face 2.8 million antibiotic-resistant infections each year, resulting in 35,000 deaths [79]. The core of this crisis lies in the diagnostic dilemma that clinicians face: without rapid pathogen identification and resistance profiling, treatment decisions are incorrect in 30-50% of cases [79]. This leads to prescription of unwarranted antibiotics, incorrect antibiotic selection, overuse of broad-spectrum agents, or dangerous treatment delays—scenarios that violate fundamental bioethical principles of beneficence and non-maleficence [79].
The COVID-19 pandemic has further exacerbated the global AMR crisis, highlighting critical weaknesses in our diagnostic infrastructure [79]. For researchers investigating bacterial species with intrinsic antibiotic resistance, such as Mycobacterium abscessus (dubbed the "antibiotic nightmare") [20], the challenges are particularly acute. These organisms possess complex sets of intrinsic resistance mechanisms that act as gauntlets for antibiotics to surpass, requiring sophisticated diagnostic approaches that can rapidly identify both the pathogen and its unique resistance profile to guide targeted therapeutic interventions.
Current Diagnostic Landscape and Technological Limitations
Conventional Methods and Their Constraints
Traditional diagnostic approaches for pathogen identification and antimicrobial susceptibility testing (AST) remain largely dependent on culture-based techniques that have changed little in decades. These methods, while cost-effective and thoroughly validated, are "very slow" according to clinical microbiology laboratory perspectives [79]. The standard workflow involves specimen inoculation onto culture media, followed by 1-3 days (or longer) for colony formation, subsequent morphological and metabolic characterization, and finally phenotypic susceptibility testing [80].
Table 1: Comparison of Current Diagnostic Methods for Pathogen Identification
| Method | Time Required | Key Advantages | Major Limitations |
|---|---|---|---|
| Culture-based Techniques | 1-3+ days | Cost-effective, extensive clinical validation, reproducible | Labor-intensive, requires expertise, slow growth of some pathogens |
| Immunological Techniques (ELISA) | Hours | High-throughput, low cost, can detect multiple pathogens simultaneously | Limited selectivity/sensitivity, shared antigens between species |
| MALDI-TOF MS | Minutes after colony isolation | Fast, accurate identification | High equipment costs, limited application for AMR detection, similar spectra for related species |
| Nucleic-acid-based Techniques (PCR) | Hours | High sensitivity/specificity, culture-independent | Requires prior knowledge of pathogens, limited multiplexing in conventional formats |
Phenotypic susceptibility testing continues to play a crucial role in detecting AMR through methods including broth dilution tests, antimicrobial gradient methods, and disc diffusion tests [80]. These approaches provide valuable quantitative data, particularly the minimum inhibitory concentration (MIC), which represents the lowest antibiotic concentration that inhibits bacterial growth [80]. However, the fundamental drawback remains that these phenotypic methods require up to several days due to the essential culturing step, leaving clinicians without critical guidance during the initial, most critical hours of infection management.
The Bioethical Imperative for Rapid Diagnostics
From a bioethical perspective, the current diagnostic delays create untenable situations for both providers and patients. Tracey L. Cohen from the University of Miami Miller School of Medicine emphasizes that when clinicians lack rapid pathogen identification, patients cannot provide truly informed consent because they cannot be accurately informed about risks, benefits, and alternatives [79]. This infringes on the principle of respect for patient autonomy. Additionally, the prescription of inappropriate antibiotics increases the risk of resistance development within the individual patient, potentially leading to treatment failure and violating the provider's duty of non-maleficence ("do no harm") [79].
The ethical obligations extend beyond the clinician-patient relationship to include pharmaceutical and biotechnology companies, which must ensure that rapid diagnostics do not sacrifice accuracy for speed. Furthermore, governments and third-party payers have ethical obligations to subsidize and cover these tests to ensure just distribution and financial accessibility in conformity with the principle of social justice [79].
Emerging Technologies and Innovative Approaches
Advanced Molecular Detection Systems
Molecular diagnostics, particularly quantitative PCR (qPCR) and reverse transcription PCR (RT-PCR), have revolutionized pathogen identification by providing rapid, sensitive detection of specific DNA targets. qPCR offers significant advantages through its ability to amplify and quantify microbial targets with fast turnaround times, as it requires no post-reaction processing [81]. This technology enables precise identification of specific bacterial serogroups or serotypes that can provide actionable information about antibiotic susceptibility, informing appropriate, timely treatment decisions [81].
The latest innovations in qPCR master mixes, such as the TaqPath BactoPure Microbial Detection qPCR Master Mix, offer enhanced sensitivity through formulations that minimize extraneous background DNA, enabling reliable detection from as low as 1 copy/μL through 2×10^8 copies/μL [81]. This wide dynamic range allows for accurate diagnostics even at low pathogen concentrations that might be missed by conventional methods. The exceptional lot-to-lot consistency achieved through cGMP manufacturing practices in ISO 13485-certified facilities further enhances the reliability of molecular diagnostics for antimicrobial resistance surveillance [81].
Novel Antimicrobial Discovery Platforms
Archaea-Derived Antimicrobial Peptides
The exploration of previously untapped biological reservoirs has revealed promising new avenues for antimicrobial discovery. Recent research leveraging deep learning to systematically mine archaeal proteomes has identified 12,623 molecules with potential antimicrobial activity, termed "archaeasins" [82]. These peptide compounds demonstrate unique compositional features that differentiate them from traditional antimicrobial peptides, including a distinct amino acid profile enriched in glutamic acid residues while maintaining a prevalence of cationic residues [82].
Experimental validation of 80 synthesized archaeasins revealed that 93% showed antimicrobial activity in vitro against clinically relevant pathogens including Acinetobacter baumannii, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus aureus, and Enterococcus spp. [82]. Notably, archaeasin-73 emerged as a lead candidate, significantly reducing A. baumannii loads in mouse infection models with effectiveness comparable to established antibiotics like polymyxin B [82]. The successful identification of these compounds highlights the power of integrating deep learning with experimental validation to accelerate antibiotic discovery from unconventional sources.
Exploiting Bacterial Resistance Mechanisms
Innovative approaches are emerging that strategically exploit bacterial resistance mechanisms rather than attempting to overcome them. Scientists at St. Jude Children's Research Hospital have demonstrated a proof-of-concept wherein a structurally modified version of the drug florfenicol exploits drug resistance mechanisms in Mycobacterium abscessus to amplify the antibiotic's effect perpetually [20]. This "resistance hacking" approach represents a new frontier in combating intrinsically resistant bacteria.
The engineered florfenicol functions as a prodrug—a chemically inactive compound that converts to its active form within the bacterium through the action of Eis2, a protein that the bacterial resistance mechanism WhiB7 induces [20]. As WhiB7 activates, more Eis2 proteins are produced, which in turn generate more of the antibiotic's active form. The activated florfenicol analog then inhibits the ribosome, subsequently activating WhiB7 further and creating a perpetual cascade that continuously amplifies the antibiotic effect [20]. This approach demonstrates significantly reduced mitochondrial toxicity compared to conventional phenicol derivatives, offering a larger safety window for treating these challenging infections.
Immune Molecule Repurposing
Research from the NIH Intramural Research Program has revealed that chemokines—immune proteins primarily known for directing immune cell movement—can directly kill bacteria without triggering antimicrobial resistance [83]. This discovery emerged from investigating how chemokines interact with bacterial cell membranes, particularly their binding to negatively charged phospholipids like cardiolipin and phosphatidylglycerol [83].
The antimicrobial mechanism involves chemokines binding to and breaking apart the bacterial cell membrane, which bacteria cannot easily modify to develop resistance, unlike specific protein targets of conventional antibiotics [83]. Experimental data demonstrated that treating bacteria with the chemokine CCL20 did not cause microbes to become resistant even after multiple generations, whereas conventional antibiotics required increasingly higher doses to achieve the same effect [83]. This approach offers promising avenues for developing new antimicrobials that bypass traditional resistance mechanisms.
Chemokine Antimicrobial Mechanism: This diagram illustrates how chemokines kill bacteria by targeting anionic phospholipids in cell membranes, a mechanism that does not trigger resistance development.
Experimental Workflows and Research Methodologies
Standardized Antimicrobial Susceptibility Testing Protocol
For researchers characterizing novel antimicrobial compounds or resistance profiles in bacterial species with intrinsic resistance, a standardized protocol encompassing MIC determination, minimum bactericidal concentration (MBC) assessment, antibiotic susceptibility profiling, and phenotype stability testing provides a comprehensive approach [84]. The protocol below has been validated for assessing resistance development risk following exposure to antimicrobial formulations:
Broth Microdilution MIC Determination
- Prepare doubling dilutions of the antimicrobial compound in a 96-well microtiter plate using appropriate broth medium [84]
- Standardize bacterial inoculum to 1×10^8 CFU/mL from overnight culture
- Add 50μL of standardized culture to each well of the microtiter plate
- Incubate for 24 hours at 37°C
- Visually determine MIC as the lowest concentration showing no bacterial growth [84]
Minimum Bactericidal Concentration Assessment
- Remove 20μL from wells showing no bacterial growth and from wells containing the two lowest concentrations showing growth
- Add to 180μL of appropriate neutralizer to stop antimicrobial action
- Transfer to solid culture media and incubate for 24-48 hours at 37°C
- Determine MBC as the lowest concentration showing ≥99.9% kill compared to initial inoculum [84]
Table 2: Key Research Reagent Solutions for Antimicrobial Resistance Studies
| Reagent/Kit | Primary Function | Key Features | Application in AMR Research |
|---|---|---|---|
| TaqPath BactoPure Microbial Detection qPCR Master Mix | Pathogen DNA detection and quantification | Virtually free of background DNA; wide dynamic range (1-2×10^8 copies/μL); lot-to-lot consistency | Rapid identification of pathogens and resistance genes in clinical samples |
| API Test Strips | Biochemical profiling of bacterial isolates | Standardized, miniaturized biochemical tests; species-specific databases | Complementary identification of cultured pathogens with intrinsic resistance |
| Cation-Adjusted Mueller-Hinton Broth | Antimicrobial susceptibility testing | Standardized composition for reproducible MIC results | Gold-standard medium for broth microdilution assays according to CLSI guidelines |
| Neutralizer Solution (e.g., Tween 80 + Asolectin) | Stopping antimicrobial action | Quenches activity of diverse antimicrobial agents without bacterial toxicity | Essential for accurate MBC determinations following antimicrobial exposure |
Computational Prediction of Resistance Evolution
Quantitative systems-based approaches are emerging to predict AMR evolution by integrating mathematical models with multiscale data from microbial evolution experiments [14]. These approaches quantify evolutionary predictability (the existence of a probability distribution for resistance outcomes) and evolutionary repeatability (the likelihood of specific resistance events occurring) [14]. Shannon entropy and other variability measures can quantify repeatability, with uniform distributions representing maximum uncertainty/entropy and Dirac delta functions representing minimum uncertainty in predictable evolutionary processes [14].
Metabolic fitness landscapes have been successfully utilized to predict antibiotic resistance by modeling the complex interactions between mutations, gene expression changes, and environmental factors [14]. For instance, in yeast, mutations emerging during evolution experiments with synthetic drug resistance gene networks were computationally predicted beforehand based on the costs and benefits of expressing the synthetic network under specific drug conditions [14]. Similarly, in bacteria, the same resistance mutations have been found to repeatedly fix in independently evolving populations, suggesting predictable and repeatable evolutionary patterns under specific selective pressures [14].
Resistance Prediction Workflow: This diagram outlines the computational approach for predicting antimicrobial resistance evolution by integrating experimental data with systems biology models.
Future Directions and Implementation Challenges
Overcoming Barriers to Diagnostic Adoption
Despite the promising technological advances, significant barriers impede the widespread development and uptake of rapid diagnostics for resistant infections. Lengthy and unpredictable pathways for coverage, coding, and payment represent substantial obstacles for diagnostic developers [79]. Additionally, survey data indicates that up to 70% of clinical laboratories in the United States are not using current Clinical and Laboratory Standards Institute (CLSI) criteria for resistance determination, creating a critical patient safety issue [79].
The implementation of rapid diagnostics must be accompanied by comprehensive stewardship programs that ensure appropriate test utilization and interpretation. As Karen C. Carroll emphasized, quality antimicrobial susceptibility testing is fundamental for infection control and national surveillance efforts [79]. Emerging evidence suggests that cycling different antibiotic classes or combining rapid diagnostics with novel therapeutic approaches that exploit resistance mechanisms may provide the "one-two knockout punch" needed to tackle drug-resistant infections [20].
Integrating Multi-Omics Approaches
The future of rapid diagnostics lies in integrating multi-omics data—genomic, transcriptomic, proteomic, and metabolomic—to create comprehensive resistance profiles. Machine learning algorithms are increasingly being applied to MALDI-TOF MS data to improve prediction of antibiotic resistance, overcoming one of the major limitations of this rapid identification technology [80]. Similarly, deep learning frameworks like APEX 1.1 are demonstrating remarkable capability in identifying encrypted antimicrobial peptides within proteomic data, with significant correlations between predicted and experimentally validated minimum inhibitory concentrations [82].
Direct, culture-independent sequencing approaches offer potential to complement current culture-based methods in routine clinical settings, though standardization of analysis pipelines and result interpretation remains challenging [80]. As these technologies mature, they promise to transform the diagnostic landscape for resistant infections, potentially reducing turnaround times from days to hours while providing comprehensive resistance profiling that guides targeted therapeutic interventions.
The challenges in rapidly identifying resistant infections demand a multifaceted approach that combines technological innovation, ethical consideration, and implementation science. Rapid diagnostics represent not just technological improvements but fundamental tools for upholding bioethical principles in patient care, enabling providers to fulfill their duties of beneficence, non-maleficence, and respect for patient autonomy. The emergence of novel strategies—from deep learning-guided antibiotic discovery to resistance mechanism exploitation and immune molecule repurposing—offers promising avenues for addressing the escalating threat of antimicrobial resistance.
For researchers focused on bacterial species with natural antibiotic resistance, the evolving diagnostic landscape presents both challenges and opportunities. By leveraging advanced molecular techniques, computational approaches, and innovative therapeutic strategies, the scientific community can work toward a future where rapid, accurate identification of resistant infections enables targeted, effective treatments that curb the global AMR crisis. The integration of these approaches within ethical frameworks that ensure equitable access and appropriate use will be essential for maximizing their impact on individual patient outcomes and public health.
Optimizing Antimicrobial Stewardship to Preserve Existing Treatment Options
Antimicrobial resistance (AMR) represents one of the most pressing challenges to global public health, undermining the efficacy of antibiotics and complicating the treatment of infectious diseases. With drug-resistant infections contributing to 4.95 million deaths globally in 2019 and projections suggesting this number could rise to 10 million annually by 2050, the need for effective antimicrobial stewardship is critical [85]. Antimicrobial stewardship programs (ASPs) are coordinated interventions designed to improve and measure the appropriate use of antimicrobial agents by promoting the selection of the optimal drug regimen, including dosing, duration, and route of administration [86]. The core mission of stewardship is to optimize patient outcomes while minimizing toxicity and curbing the emergence of resistance, thereby preserving the utility of existing treatments [87]. This technical guide examines evidence-based stewardship strategies within the broader context of bacterial species with natural and acquired antibiotic resistance, providing researchers and drug development professionals with a framework for implementing and advancing these crucial programs.
Core Elements of Antimicrobial Stewardship Programs
Foundational Principles and Frameworks
The Centers for Disease Control and Prevention (CDC) has established Core Elements for Antibiotic Stewardship that provide healthcare facilities with a flexible framework for implementing programs tailored to their specific resources and needs [88]. These principles recognize that there is no "one-size-fits-all" approach, but all successful ASPs share common foundational elements. The complexity of medical decision-making surrounding antibiotic use requires programs that can adapt to varied facility sizes and types of care. The core elements encompass leadership commitment, accountability, drug expertise, action, tracking, reporting, and education, creating a comprehensive structure for stewardship activities [88]. These frameworks complement existing guidelines from key healthcare partner organizations, including the Infectious Diseases Society of America (IDSA) and the Society for Healthcare Epidemiology of America (SHEA), which strongly recommend that ASPs be led by infectious disease physicians with additional stewardship training [86].
Fundamental Stewardship Interventions
Prospective Audit and Feedback
Prospective audit and feedback (PAF) allows the ASP to review patient encounters and identify opportunities where antimicrobial management can be optimized. This review can result in recommendations to change the agent, adjust the dose or duration, convert intravenous to oral formulations, and evaluate drug interactions [89]. When deployed effectively, PAF can reduce overall antibiotic use, cost, and length of stay. This intervention can be initiated based on the antimicrobial prescribed or by clinical results obtained from the microbiology laboratory [89].
- Postprescription Review: A comprehensive patient review occurs after antimicrobial prescription to optimize treatment. This can be performed immediately after prescribing or within 24-72 hours when more clinical information is available [89].
- Microbiology-Laboratory Initiated PAF: ASPs can focus on reviewing sterile site cultures that pose high morbidity and mortality risks if treated inappropriately. The clinical impact of molecular rapid diagnostic tests (mRDTs) is most pronounced when reviewed and acted upon by the ASP in real time [89].
Facility-Specific Treatment Guidelines
The establishment of facility-specific treatment guidelines for common infectious disease syndromes is fundamental to optimizing empiric antimicrobial selection, de-escalation, and duration of therapy [89]. These guidelines should be developed collaboratively in multidisciplinary teams, incorporating clinical stakeholders to increase the likelihood of acceptance. Lower respiratory tract infections, urinary tract infections, and skin and soft-tissue infections account for most antibiotic use in hospitals and should be a high priority for hospital-based ASPs [89]. Integration of these guidelines into the clinician's workflow can be achieved by leveraging the electronic health record to incorporate recommendations into order sets and clinical decision support systems.
Prior Authorization
Prior authorization requires certain agents to be approved before initiation, typically based on policies jointly established by the facility's ASP and the pharmacy and therapeutics committee [89]. This intervention allows direct control over specific agents and has been shown to decrease designated antimicrobial use, reduce costs, and improve antibiotic resistance among gram-negative pathogens. Common reasons for restriction include drug cost, complexity in dosing and monitoring, and broad-spectrum agents that should only be used to treat specific pathogens [89].
Table 1: Comparison of Fundamental Stewardship Interventions
| Intervention | Key Features | Evidence Strength | Impact Measures |
|---|---|---|---|
| Prospective Audit & Feedback | Post-prescription review, laboratory-initiated review | Strong recommendation, moderate-quality evidence [86] | Reduced antibiotic use, cost, and length of stay [89] |
| Facility-Specific Guidelines | Based on local epidemiology and susceptibilities, multidisciplinary development | Weak recommendation, low-quality evidence [86] | Standardized prescribing, improved empiric selection [89] |
| Prior Authorization | Restriction of specific agents, pre-approval required | Strong recommendation, moderate-quality evidence [86] | Decreased use of targeted agents, cost reduction [89] |
Advanced Diagnostic and Technological Approaches
Diagnostic Stewardship and Rapid Testing
Diagnostic stewardship aims to improve the appropriate use and interpretation of diagnostic tests to guide therapeutic decisions and avoid the consequences of false-positive results [89]. Unnecessarily testing patients without infectious symptoms or with low pre-test probability of infection increases the likelihood of false-positive results, which may lead to treatment with unnecessary antibiotics. Common targets for diagnostic stewardship include inappropriate urine cultures or C. difficile tests, where positive results may lead to incorrect diagnosis and delayed identification of the true cause of symptoms [89].
Molecular rapid diagnostic tests (mRDTs) have emerged as a key technology to decrease the time to identification and antimicrobial susceptibility of pathogens. These tests can decrease the time to effective therapy and antimicrobial optimization, while also reducing length of stay in patients with bloodstream infections [89]. The successful implementation of mRDTs is dependent on workflows that support antimicrobial stewardship review of results and communication of recommendations to frontline clinicians. Incorporating mRDTs into the ASP workflow should be a high priority in hospitals utilizing this technology.
Clinical Decision Support and Technology Integration
Computerized clinical decision support systems integrated into the electronic health record at the time of prescribing can significantly enhance ASP efforts. The IDSA/SHEA guidelines suggest incorporating computerized clinical decision support at the time of prescribing into ASPs, particularly when information technology resources are readily available [86]. Computerized surveillance systems that synthesize data from the electronic health record and other sources can streamline the work of ASPs by identifying opportunities for interventions. These systems can facilitate the implementation of facility-specific guidelines, provide alerts for antibiotic time-outs, and support appropriate duration of therapy through automatic stop orders.
Diagram: Diagnostic Stewardship Workflow - This diagram illustrates the integration of rapid diagnostic testing with antimicrobial stewardship program review to optimize antibiotic regimens and improve outcomes.
Experimental Protocols for Stewardship Research
Environmental Surveillance for Resistance Patterns
Understanding the environmental dimension of antibiotic resistance is crucial within the One Health framework, which highlights the interconnectedness of human, animal, and environmental health in the emergence and spread of AMR [90]. The following protocol outlines methods for surveillance of antibiotic-resistant bacteria in wastewater environments:
- Sample Collection: Collect sewage samples (500mL) from strategic locations such as sewage outlets receiving hospital wastewater. Samples should be transferred to sterile amber glass bottles, with pH checked on site, and immediately transported to the laboratory for isolation while storing at -20°C for further analysis [90].
- Liquid-Liquid Extraction: Perform extraction by adding EDTA salt (0.5g) to 10ml of each sample, shaking for 2 minutes, sonicating for 1 minute in an ultrasonic water bath, and vortexing for 2 minutes. Transfer the sample solution with 20ml of dichloromethane to a separating funnel, shake for 5 minutes, collect the DCM layer, and repeat with additional DCM. Pass the collected DCM through sodium sulfate to absorb moisture, then evaporate to dryness under nitrogen. Reconstitute the dried extract with 2ml of methanol and water (20:80) and filter through a 0.22μm nylon syringe filter [90].
- Bacterial Isolation and Characterization: Subject sewage samples to serial dilution (up to 10⁻⁶), and spread 100μL of each diluted sample onto minimal salt medium agar plates. Isolate and purify antibiotic-resistant colonies through streaking on nutrient agar. Perform phenotypic characterization through gram staining and virulence tests (hemolysis assay, biofilm formation assay, protease, amylase and lipase activity assays) [90].
- Antibiotic Susceptibility Testing: Determine minimum inhibitory concentrations (MICs) using both antibiotic gradient strips and broth microdilution methods following EUCAST guidelines. Test against clinically relevant antibiotics such as amoxicillin, meropenem, and vancomycin [90].
- Molecular Identification: Perform 16S rRNA gene sequencing for species identification and investigate resistance mechanisms through genetic analysis [90].
Phage Training Experimental Protocol
Novel approaches to combat antibiotic-resistant bacteria include using bacteriophages (phages) as an alternative to traditional antibiotics. The following protocol for experimental evolution of phages was developed by UC San Diego researchers:
- Phage-Bacteria Co-culture: Initiate controlled laboratory co-culture of phages with target bacterial strains (e.g., Klebsiella pneumoniae) for extended periods (30 days) to allow for evolutionary adaptation [70].
- Selection Pressure Application: Apply selective pressure by serial passage of phages in the presence of progressively more resistant bacterial strains, including multidrug-resistant and extensively drug-resistant pathogens.
- Genetic Analysis: Sequence evolved phages to identify mutations in genes responsible for recognizing and binding to bacterial cells. Correlate genetic changes with phenotypic improvements in host range and killing efficiency [70].
- Efficacy Assessment: Evaluate evolved phages for enhanced ability to suppress bacterial growth over extended periods and against a wider variety of bacterial strains compared to ancestral phages.
Table 2: Research Reagent Solutions for Antimicrobial Resistance Studies
| Reagent/Equipment | Specification | Application/Function |
|---|---|---|
| Minimal Salt Medium Agar | Composition: 2 g/L NH₄Cl, 1.5 g/L K₂HPO₄, 0.5 g/L KH₂PO₄ [90] | Isolation of antibiotic-resistant bacteria from environmental samples |
| Antibiotic Standards | Amoxicillin trihydrate, meropenem trihydrate, vancomycin hydrochloride [90] | MIC determination and resistance profiling |
| LC/MS System | Thermo Scientific TSQ Quantis plus LCMS/MS or Agilent 6460 Triple Quad, ESI+ mode [90] | Quantification of antibiotic residues in environmental samples |
| Molecular Biology Reagents | 16S rRNA sequencing primers, PCR components, electrophoresis equipment [90] | Bacterial identification and resistance gene detection |
| Cell Culture Media | Mueller-Hinton agar, Brain Heart Infusion, nutrient agar [90] | Bacterial cultivation and virulence assays |
Integration with Broader Resistance Research
The One Health Perspective
Antimicrobial resistance operates within a One Health framework, recognizing the interconnectedness of human, animal, and environmental health [91]. Environmental reservoirs, particularly wastewater systems, play a critical role in the dissemination of resistant bacteria. Studies have shown that sewage receiving hospital wastewater harbors multidrug-resistant bacterial populations, with isolates demonstrating significant resistance even when antibiotic concentrations are below quantification limits [90]. Research has identified diverse bacterial strains in sewage samples, including Stenotrophomonas, Sphingobium, Brucella, Agrobacterium, Ochrobactrum, Acinetobacter, Klebsiella, and Pandoraea, with most exhibiting multidrug resistance [90]. Notably, Pandoraea sp. strain VITSA19 displayed exceptionally high resistance to all tested antibiotics (≥4,096 μg/mL for amoxicillin, ≥512 μg/mL for meropenem and ≥4,096 μg/mL for vancomycin) [90]. These findings underscore sewage as a reservoir of multidrug-resistant bacteria and highlight the urgent need for integrated environmental AMR surveillance and improved wastewater treatment practices to mitigate resistance transmission to human and ecological health.
Novel Therapeutic Approaches
Research into bacterial species with natural antibiotic resistance has spurred the development of innovative therapeutic strategies. Phage therapy represents a promising alternative, with recent advances demonstrating that experimental evolution of phages can enhance their effectiveness against drug-resistant pathogens [70]. UC San Diego researchers successfully "trained" phages to adapt to bacterial defenses through 30 days of co-evolution, resulting in significant improvements in their ability to kill a wide variety of bacterial strains, including multidrug-resistant and extensively drug-resistant K. pneumoniae [70]. Genetic analysis revealed that the evolved phages acquired mutations to specific genes responsible for recognizing and binding to bacterial cells, likely contributing to their improved effectiveness [70]. This approach highlights the potential of leveraging evolutionary principles to develop powerful tools against the antibiotic resistance crisis.
Additionally, the discovery of new antibiotic molecules from unconventional sources offers promising avenues for treatment. Researchers have recently discovered a new antibiotic molecule in a technician's garden that targets a broad range of disease-causing bacteria—even strains resistant to commercial drugs—and is not toxic to human cells [92]. This molecule targets bacteria in a way that other drugs don't, potentially offering a new mechanism to combat resistance.
Optimizing antimicrobial stewardship requires a multifaceted approach that integrates fundamental interventions with advanced diagnostic technologies and novel therapeutic strategies. The core elements of prospective audit and feedback, facility-specific treatment guidelines, and prior authorization provide a foundation for effective stewardship programs. When enhanced through diagnostic stewardship, technological support, and integration with broader resistance research, these programs can significantly preserve existing treatment options. The connection between environmental resistance surveillance and clinical stewardship highlights the importance of a One Health approach to addressing the AMR crisis. As research continues to evolve, leveraging novel approaches such as phage therapy and discovering new antibiotic molecules from diverse sources will be essential to complement stewardship efforts. For researchers, scientists, and drug development professionals, implementing and advancing these evidence-based stewardship strategies is crucial to mitigating the impact of antimicrobial resistance and preserving the efficacy of existing treatments for future generations.
Strategies for Biofilm Disruption and Tackling Persistent Bacterial Populations
Within the broader context of research on bacterial species with natural antibiotic resistance, the phenomena of biofilms and bacterial persistence represent a critical frontier. Biofilms, which are structured communities of microorganisms encased in a self-produced extracellular matrix, and bacterial persisters, a subpopulation of transiently dormant, non-growing cells, are major contributors to chronic infections and therapeutic failure [93] [94]. These survival states are intrinsically tolerant to conventional antibiotics, not through acquired genetic resistance, but via physical and physiological mechanisms that shield them from drug action [5] [95].
The clinical and economic impacts are profound. Biofilms are implicated in approximately 65% of all bacterial infections and nearly 80% of chronic wounds [93]. Globally, the financial burden of biofilm-associated infections is estimated to exceed $280 billion annually, reflecting the extended treatments, device failures, and increased morbidity they cause [93] [96]. Similarly, persister cells are the primary culprits behind relapsing infections such as tuberculosis, recurrent urinary tract infections, and Lyme disease, as they survive antibiotic exposure only to regenerate the infection once treatment ceases [94]. For researchers and drug development professionals, understanding and disrupting these bacterial defenses is paramount to overcoming the limitations of current antimicrobial therapies.
Biofilm Biology and Mechanisms of Antimicrobial Tolerance
The Biofilm Lifecycle
The formation of a biofilm is a complex, multi-stage process that transitions bacteria from a free-swimming, planktonic lifestyle to a sessile, community-based one [96]. The lifecycle can be broadly summarized in five key stages, as illustrated in the diagram below.
Diagram 1: Biofilm Development Cycle
- Initial Reversible Attachment: Planktonic bacteria use attachment structures like flagella, pili, and fimbriae to loosely adhere to a biotic or abiotic surface. This attachment is initially reversible [93] [96].
- Irreversible Attachment: Cells commit to the surface by upregulating adhesion molecules and glycoproteins, forming a stable association [93].
- Microcolony Formation: Attached cells undergo division and begin to form three-dimensional clusters. Quorum sensing (QS), a cell-cell communication system, becomes active, coordinating group behavior [93] [96].
- Biofilm Maturation: The community secretes a robust extracellular polymeric substance (EPS) matrix, which can constitute over 90% of the biofilm's dry mass [93] [96]. This creates a protected environment with structured, mushroom-like towers and fluid channels [97].
- Active Dispersal: In response to environmental cues such as nutrient depletion, sub-populations of cells detach to seed new niches, completing the lifecycle and spreading the infection [96].
Intrinsic Resistance Mechanisms in Biofilms
The organized structure and altered physiology of biofilms confer tolerance through several concurrent mechanisms, detailed in the table below.
Table 1: Key Mechanisms of Biofilm-Mediated Antimicrobial Tolerance
| Mechanism | Functional Description | Impact on Antimicrobial Efficacy |
|---|---|---|
| Physical Barrier (EPS) | The EPS matrix, composed of polysaccharides, proteins, and extracellular DNA (eDNA), physically limits drug penetration and can inactivate drugs via binding or enzymatic degradation [93] [96]. | The Minimum Inhibitory Concentration (MIC) for biofilm cells can be 100-800 times greater than for planktonic cells [93]. |
| Metabolic Heterogeneity | Gradients of nutrients and oxygen create zones with different metabolic activities. Cells in deep, nutrient-depleted layers enter a slow-growing or dormant state [93] [96]. | Most antibiotics target active cellular processes and are ineffective against dormant cells, leaving a reservoir of surviving bacteria [93]. |
| Persister Cell Enrichment | The harsh conditions within biofilms (e.g., starvation, hypoxia) promote the formation of dormant persister cells that are highly tolerant to antibiotics [94] [95]. | Persisters are not killed by bactericidal antibiotics, leading to regrowth and relapse of the infection after the end of therapy [94]. |
| Efflux Pump Upregulation | Expression of multidrug efflux pumps can be heightened in specific regions of the biofilm, actively extruding antibiotics from the cells [93]. | Increases the required antibiotic concentration at the intracellular target site, contributing to treatment failure [93]. |
The following diagram synthesizes how these mechanisms interact to protect a mature biofilm from antimicrobial attack.
Diagram 2: Biofilm Resistance Mechanisms
Bacterial Persistence: A Distinct Phenotype of Survival
Defining Persisters and Their Clinical Role
It is crucial to distinguish bacterial persistence from genetic antibiotic resistance. Persisters are a subpopulation of genetically susceptible, non-growing or slow-growing bacteria that survive lethal doses of antibiotics. Once the antibiotic pressure is removed, these cells can resume growth and produce a new population that remains susceptible to the same drug [94] [95]. In contrast, resistant bacteria possess stable genetic mutations that allow them to grow in the presence of the antibiotic, and this resistance is inherited by their progeny [5].
Persisters are a major underlying cause of relapsing and chronic infections [94]. They were first identified in 1944 by Joseph Bigger, who observed that a small fraction of Staphylococcus populations survived penicillin treatment [94]. Today, they are recognized as key players in the persistence of diseases like tuberculosis, where they necessitate prolonged multi-drug therapy [94].
Molecular Mechanisms of Persister Formation
The formation of persister cells is regulated by a network of interconnected biochemical pathways that induce a dormant state. Key mechanisms include:
- Toxin-Antitoxin (TA) Modules: These genetic modules are ubiquitous in bacteria and consist of a stable toxin that inhibits essential cellular processes (e.g., translation) and a labile antitoxin that neutralizes the toxin. Under stress conditions, proteases degrade the antitoxin, freeing the toxin to induce dormancy. The HipA toxin in E. coli was one of the first genes linked to high persistence [94] [95].
- The Stringent Response: Nutrient starvation triggers the rapid synthesis of the alarmone (p)ppGpp. High levels of (p)ppGpp lead to a global reprogramming of cellular metabolism, shuttling resources away from growth and division and toward maintenance and survival, thereby promoting dormancy [95].
- Other Metabolic Triggers: Downregulation of the tricarboxylic acid (TCA) cycle in response to antibiotic-induced oxidative stress has been shown to protect persisters by preventing the production of lethal reactive oxygen species [95]. Epigenetic modifications and the activity of small non-coding RNAs also contribute to the persister phenotype [94].
The relationship between these pathways is illustrated below.
Diagram 3: Persister Cell Formation Pathways
Experimental Approaches for Studying Biofilms and Persisters
Advanced Imaging and Cultivation Systems
Understanding the dynamic nature of biofilms requires sophisticated imaging technologies. Light Sheet Fluorescence Microscopy (LSFM) integrated with microfluidic cultivation systems represents a state-of-the-art approach [97].
Protocol: Imaging Polymicrobial Biofilm Dynamics with LSFM
- Objective: To visualize the real-time, three-dimensional structural development and species interaction within a polymicrobial biofilm.
- Materials:
- Microfluidic cultivation chamber (e.g., commercial or PDMS-made chips).
- Light Sheet Fluorescence Microscope.
- Bacterial strains (e.g., P. aeruginosa and S. aureus) transformed with constitutively expressed fluorescent proteins (e.g., GFP, mCherry).
- Conditioned media from mono- or co-cultures.
- Methodology:
- Inoculation: Introduce a suspension of fluorescently tagged bacteria into the microfluidic chamber at a desired ratio (e.g., 1:1 or skewed to favor one species).
- Continuous Perfusion: Maintain a continuous flow of nutrient medium to mimic in vivo shear forces and provide nutrients.
- Multidirectional Imaging: Capture images of the growing biofilm using LSFM from multiple angles over a time course (e.g., 24-72 hours).
- 3D Reconstruction: Use computational software to combine the multidirectional images into an isotropic 3D model of the biofilm structure.
- Intervention Studies: Introduce conditioned media or antimicrobial compounds via the microfluidic system and continue imaging to monitor dispersion or killing effects [97].
- Key Application: This protocol was used to demonstrate that P. aeruginosa can invade and disperse pre-formed, mushroom-shaped S. aureus biofilms, and that conditioned media from the co-culture alone is sufficient to induce dispersion [97].
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Biofilm and Persister Research
| Research Reagent | Function in Experimental Design |
|---|---|
| Microfluidic Cultivation Chambers | Provides a controlled, dynamic environment for growing biofilms under fluid shear stress, enabling high-resolution, real-time imaging [97]. |
| Conditioned Media | Cell-free supernatant from bacterial cultures used to investigate the role of secreted chemical signals and virulence factors in biofilm formation and dispersal [97]. |
| Fluorescent Protein Tags (e.g., GFP, mCherry) | Allows for visual distinction and tracking of different bacterial species or genetic variants within a polymicrobial biofilm using microscopy [97]. |
| Efflux Pump Inhibitors (e.g., PaβN) | Chemical tools used to block the activity of multidrug efflux pumps, allowing researchers to delineate their contribution to biofilm-specific antibiotic tolerance [93]. |
| Quorum Sensing Inhibitors | Molecules that interfere with bacterial cell-to-cell communication, used to study the role of QS in biofilm maturation and virulence [93]. |
Emerging Strategies for Disruption and Eradication
Bacteriophages and Phage-Derived Enzymes
Bacteriophages (phages), viruses that infect and kill bacteria, offer a highly specific and evolving weapon against biofilms and persisters [98].
- Mechanism of Action: Lytic phages infect bacterial cells, replicate inside them, and produce endolysins that break down the cell wall, causing lysis and death. Phages can penetrate biofilms by producing depolymerases, enzymes that degrade specific polysaccharides, eDNA, or proteins within the EPS matrix, thus breaking down the biofilm's structural integrity [98].
- Targeting Persisters: A significant challenge is that persisters are metabolically inactive, which typically prevents phage infection. Innovative solutions include:
- Phage Engineering: Genetically modifying phages to express biofilm-degrading enzymes on their capsid or to recognize receptors on dormant cells [98].
- Combination Therapy: Using phages in conjunction with resuscitation-promoting factors or specific antibiotics that can trigger a return to metabolic activity in persisters, making them vulnerable to phage attack [98].
Exploiting Resistance Mechanisms: "Resistance Hacking"
A novel, proof-of-concept strategy involves turning a bacterium's own resistance machinery against itself. Researchers at St. Jude Children's Research Hospital demonstrated this with Mycobacterium abscessus, an "antibiotic nightmare" [20].
Protocol: A Proof-of-Concept for Resistance Hacking
- Objective: To exploit the WhiB7 resistance regulon to perpetually amplify the effect of a prodrug antibiotic.
- Materials:
- Engineered florfenicol prodrug (a modified version of the antibiotic florfenicol).
- Wild-type M. abscessus and a mutant strain lacking the whiB7 gene.
- Standard microbiological culture equipment and MIC determination assays.
- Methodology:
- Sensitivity Testing: Confirm that the engineered florfenicol prodrug has strong antibiotic activity against wild-type M. abscessus but no effect on the ΔwhiB7 mutant.
- Mechanism Elucidation:
- The prodrug is imported into the bacterium.
- The WhiB7-regulated enzyme Eis2 activates the prodrug into its toxic form.
- The active drug inhibits the ribosome, which further activates the WhiB7 stress response.
- This leads to increased production of Eis2, which in turn activates more prodrug, creating a perpetual, self-amplifying cycle of antibiotic production within the bacterium [20].
- Outcome: This cycle leads to continuous amplification of the antibiotic's effect, effectively "hacking" the resistance pathway to cause bacterial suicide. This approach also showed a reduced toxicity profile towards human mitochondria [20].
Adjunctive Therapies and Combination Strategies
Given the multifactorial nature of biofilm and persister tolerance, combination therapies are often the most promising.
- Matrix Disrupting Agents: Enzymes like glycoside hydrolases that break down polysaccharides in the EPS matrix can be used alongside conventional antibiotics to improve drug penetration [96]. Dornase alfa, a recombinant human DNase, degrades eDNA in the matrix and in neutrophil extracellular traps (NETs), and is used in cystic fibrosis care [96].
- Energy-Wasting Approaches: Some studies suggest that stimulating bacterial metabolism, for instance by adding metabolites like mannitol or glucose, can wake persister cells, making them susceptible to killing by aminoglycoside antibiotics [94].
The challenges posed by bacterial biofilms and persister populations are central to the crisis of antibiotic failure. Moving beyond traditional antibiotic discovery, the future of treating these resilient bacterial states lies in a multi-pronged strategy: leveraging a deep understanding of their underlying biology to develop targeted anti-biofilm agents, harnessing the power of natural predators like bacteriophages, and designing innovative "smart" molecules that can exploit bacterial stress responses. For the research community, the priority must be to translate these promising in vitro concepts and proofs-of-concept into safe and effective clinical therapies that can finally address the root cause of chronic and relapsing infections.
The escalating global antimicrobial resistance (AMR) crisis demands urgent innovation in antibiotic development. This whitepaper examines the critical policy frameworks and economic incentives required to re-engage pharmaceutical research and development (R&D) in combating naturally resistant bacterial pathogens. With one in six bacterial infections globally now resistant to antibiotic treatments and resistance rising at 5-15% annually for many pathogen-drug combinations, the pipeline for novel antibiotics remains dangerously weak [7]. This paper analyzes push, pull, and hybrid incentive models designed to overcome market failures that stifle antibiotic investment, with particular focus on their application to pathogens with intrinsic resistance mechanisms. We provide technical guidance for researchers and policymakers on implementing these models effectively, supported by quantitative analyses, experimental methodologies for evaluating novel approaches, and visualization of key biological pathways being targeted.
The AMR Crisis and the Market Failure in Antibiotic R&D
The Growing Burden of Antimicrobial Resistance
The World Health Organization reports alarming trends in antibiotic resistance worldwide. Gram-negative bacteria, including Klebsiella pneumoniae and Escherichia coli, pose particularly severe threats, with over 40% of E. coli and 55% of K. pneumoniae isolates resistant to third-generation cephalosporins—first-line treatments for serious bloodstream infections [7]. In some regions, these resistance rates exceed 70%, while carbapenem resistance, once rare, is increasingly reported, severely limiting treatment options [7]. Recent hospital data from 2020-2022 reveals carbapenem-resistant Enterobacteriaceae (CRE) detection rates increased from 7.2% to 14.4%, highlighting the rapid expansion of this crisis [99].
Economic Disincentives for Antibiotic Development
The antibiotics market suffers from fundamental characteristics that make investment financially unattractive compared to other therapeutic areas [100]:
- Conservation Imperatives: Effective antibiotics must be used sparingly to preserve efficacy, directly limiting sales volume
- Generic Competition: Established generics markets with multiple substitutes create price pressure
- Brief Treatment Duration: Antibiotics are typically prescribed for short courses versus chronic medications
- Pricing and Reimbursement Systems: Systems often encourage use of cheapest available options
- Rapid Obsolescence: Resistance development can quickly diminish drug effectiveness
These market dynamics have led major pharmaceutical companies to redirect scientific talent and R&D capacity toward more profitable therapeutic areas, creating a critical innovation gap [100].
Incentive Models: Theory and Implementation
Push, Pull, and Hybrid Incentive Mechanisms
Investment in antibiotics can be incentivized through complementary strategies known as push and pull mechanisms, with hybrid approaches combining elements of both [100].
Table 1: Comparison of Antibiotic R&D Incentive Mechanisms
| Mechanism | Definition | Examples | Advantages | Disadvantages |
|---|---|---|---|---|
| Push Incentives | Reduce developers' R&D costs by distributing expenditures across multiple parties [100] | Research grants, tax incentives, public-private partnerships, direct funding of research personnel [100] | Lowers barriers for SME entry; supports early-stage research; allows targeted priority-setting [100] | Funds may go to failed projects; information asymmetry between developers and funders; may reduce operational efficiency [100] |
| Pull Incentives | Reward successful development by ensuring future revenue [100] | Market entry rewards, advanced market commitments, patent buyouts, transferable exclusivity vouchers [100] | Payment only for successful products; aligns with public health goals; can be delinked from volume sold [100] | Requires large financial commitments; uncertain which products will succeed; may not support early-stage R&D [100] |
| Hybrid Incentives | Combine push and pull elements [100] | Purchase commitments with cost-sharing; milestone-based funding with market rewards [101] | Balances risk reduction with success rewards; can be designed for optimal social benefit [101] | Increased implementation complexity; requires careful design to avoid inefficiencies [100] |
Quantitative Analysis of Pull Incentive Requirements
Recent analyses have quantified the "fair share" investments required from high-income countries to establish effective pull incentives. Updated 2024 calculations indicate a global annual need of approximately $4.01 billion (2024 USD) over 10 years, distributed across higher-income countries based on their economic capacity [102].
Table 2: Global Pull Incentive Requirements (Updated to 2024 USD)
| Estimate Type | Annual Value (2019 USD) | Annual Value (2024 USD) |
|---|---|---|
| Lower Bound | $220 million | $284 million |
| Mid-point | $310 million | $401 million |
| Upper Bound | $480 million | $621 million |
Analysis of two representative antibiotics (cefiderocol and ceftazidime-avibactam) reveals that most G7 countries and the EU27 have substantial gaps between actual sales revenue and fair-share targets [102]. For example, the EU27 collectively showed an $800 million gap, while Canada had gaps of $58 million and $104 million for the two drugs, respectively [102]. Notably, this analysis demonstrates that the cost to governments for pull incentives would be reduced by actual revenues, making the net investment significantly lower than the headline guarantee figures [102].
Implementing Pull Incentives: Current Global Progress
National and Regional Implementation Models
Several jurisdictions have begun implementing pull incentives with varying structures:
- United Kingdom: Has established a "subscription-style" model that provides upfront payments for access to innovative antibiotics, delinking payment from volume sold [102]
- Italy: Has recently launched its pull incentive program, with data showing it has already met fair-share targets for certain antibiotics through needed use [102]
- United States: The proposed PASTEUR Act would create a subscription-style model, though it has not yet been enacted [102]
- Other Initiatives: Canada, Japan, Australia, and the European Union are at various stages of developing pull incentive programs [102]
Analysis of Implementation Effectiveness
Economic modeling demonstrates that pure pull subsidies or hybrid models generally outperform pure push mechanisms across multiple dimensions. One analysis found that hybrid subsidy contracts "slightly outperform pure purchase commitment contracts which in turn, significantly outperform sponsor cost-sharing contracts" when measured by sponsor cost, development probability, consumer surplus, and cost per individual successfully vaccinated [101].
Crucially, analysis of actual antibiotic revenues reveals that three instances (Italy for two test drugs, the US for ceftazidime-avibactam) have achieved fair-share targets through routine sales, demonstrating that meeting targets does not always represent extra cost at the country level [102]. This finding underscores that revenue guarantees are most critical in the early years following market introduction when sales are typically insufficient to support commercialization costs [102].
Research and Methodologies for Targeting Resistant Pathogens
Innovative Approaches to Combat Natural Resistance
Novel strategies are emerging that exploit bacterial resistance mechanisms themselves. One proof-of-concept study demonstrates an approach called "resistance hacking" against Mycobacterium abscessus, a species with intrinsic multidrug resistance [20].
Experimental Protocol: Resistance Hacking in M. abscessus
- Conceptual Foundation: Engineer a prodrug version of florfenicol that lacks antibiotic activity until activated by bacterial resistance machinery
- Identification of Resistance Pathway: Target the WhiB7 "resistome," a master regulator of ribosomal stress that controls over 100 proteins involved in antimicrobial resistance
- Prodrug Design: Structural modification of florfenicol to create a compound activated by Eis2, a protein induced by WhiB7 for drug resistance
- Mechanism Validation:
- Compare activity against normal M. abscessus versus WhiB7-knockout strains
- Measure Eis2 activation and conversion rates of prodrug to active form
- Assess ribosomal inhibition and subsequent WhiB7 activation
- Efficacy and Safety Assessment:
- Determine minimum inhibitory concentrations (MIC)
- Evaluate specificity against closely related bacterial species
- Assess mitochondrial toxicity in eukaryotic cells
- Measure impact on healthy microbiome composition
Diagram 1: Resistance hacking mechanism in M. abscessus (Chars: 98)
Essential Research Reagents and Methodologies
Table 3: Key Research Reagents for Antibiotic Resistance Studies
| Reagent/Resource | Function/Application | Example/Specification |
|---|---|---|
| Vitek 2-Compact System | Automated antimicrobial susceptibility testing and bacterial identification | bioMérieux; using AST-N335, AST-N334, and AST-GN639 cards [99] |
| WHONET Software | Data processing and analysis of bacterial resistance patterns | 2023 version for analyzing specimen sources, species composition, and antimicrobial susceptibility results [99] |
| CLSI Guidelines | Standardized methodologies for antimicrobial susceptibility testing | CLSI M100 guidelines for disk diffusion and MIC determination [99] |
| Modified Florfenicol Prodrug | Proof-of-concept compound that exploits bacterial resistance mechanisms | Structurally modified version of florfenicol activated by Eis2 in M. abscessus [20] |
| WhiB7-knockout Strains | Control strains for validating resistance pathway targeting | M. abscessus with deleted WhiB7 gene to confirm mechanism of action [20] |
Implementation Framework and Evaluation Metrics
Measuring Policy Implementation Success
Effective implementation of pull incentives requires robust monitoring and evaluation frameworks. Research identifies key implementation outcomes that should be measured [103]:
- Acceptability: Perception among stakeholders that the incentive is agreeable
- Adoption: Initial uptake and implementation of the incentive mechanism
- Appropriateness: Perceived fit and relevance for addressing AMR
- Feasibility: Practicality of implementation within specific contexts
- Fidelity: Degree to which the incentive is implemented as designed
- Penetration: Integration within the targeted market or ecosystem
- Sustainability: Maintenance of the incentive mechanisms over time
- Costs: Resources required for implementation and maintenance
Determinants of Successful Implementation
Implementation success depends on multiple determinants across different domains [103]:
- External Setting: Policy environment, inter-organizational networks, patient needs and resources
- Internal Setting: Structural characteristics, implementation climate, available resources
- Characteristics of Individuals: Knowledge and beliefs, self-efficacy
- Process of Implementation: Planning, engaging, executing, reflecting, and evaluating
Quantitative measures for these determinants enable policymakers to assess readiness for implementation and identify potential barriers before rollout.
Path Forward: Integrated Strategies for Sustainable Antibiotic Innovation
The declining antibiotic pipeline demands urgent implementation of coordinated pull incentives across high-income countries. Based on our analysis, we recommend:
Immediate Implementation of Pull Incentives: Countries should establish delinked subscription-style models with minimum annual revenue guarantees of $401 million globally to create a predictable market [102]
Hybrid Approaches for Maximum Impact: Combine push funding for early-stage research with pull incentives for late-stage development and commercialization to balance risk and reward [101]
Coordinated International Action: Implement complementary pull incentives across G7 and EU27 countries based on fair-share calculations to prevent free-rider problems [102]
Novel Mechanism Targeting: Support research on innovative approaches, such as resistance hacking, that exploit bacterial resistance pathways rather than simply overcoming them [20]
Robust Monitoring and Evaluation: Establish standardized metrics to assess implementation outcomes and determinants, enabling iterative improvement of incentive designs [103]
The $401 million annual global investment represents a modest 0.02% of global pharmaceutical revenue yet would position a new antibiotic at only #230 in global revenue rankings—demonstrating both feasibility and proportionality of the required investment [102]. With bacterial resistance escalating rapidly, coordinated action using these evidence-based models represents our best strategy for revitalizing the antibiotic pipeline and addressing the growing threat of naturally resistant bacterial pathogens.
Data-Driven Defense: Surveillance, Trends, and Pathogen Prioritization
The World Health Organization's (WHO) Global Antimicrobial Resistance and Use Surveillance System (GLASS) stands as a cornerstone in the global effort to understand and combat antimicrobial resistance (AMR). Established in 2015, GLASS provides a standardized framework for the collection, analysis, and interpretation of AMR data, enabling cross-national comparisons and informing public health policy [104]. This technical guide analyzes the core trends in antibiotic resistance prevalence from 2018 to 2023, a period marked by significant global challenges including the COVID-19 pandemic. The data, contributed by over 110 countries and drawn from more than 23 million bacteriologically confirmed infections, provides an unprecedented view of the evolving AMR landscape [105] [106]. For researchers focused on bacterial species with innate or natural resistance mechanisms, this surveillance data is invaluable. It not only highlights the clinical consequences of resistance but also helps identify priority pathogens and geographical hotspots where the discovery of novel natural antibiotic compounds is most critically needed.
Key Global Resistance Trends from WHO GLASS (2018-2023)
The 2025 GLASS report reveals a consistent and worrying increase in resistance across many common bacterial pathogens. The core finding is that, in 2023, one in six laboratory-confirmed bacterial infections globally was resistant to antibiotic treatments [7] [107]. The trend data is even more alarming: between 2018 and 2023, antibiotic resistance rose in over 40% of the pathogen-antibiotic combinations under continuous monitoring, with these combinations showing an average relative annual increase of 5% to 15% [7] [106]. This persistent rise underscores the rapid pace at which AMR is evolving and outpacing conventional treatment options.
Regional Variation in Resistance Prevalence
The burden of AMR is not uniformly distributed across the globe. The GLASS data identifies significant regional disparities, with the highest prevalence rates observed in health systems that are often under-resourced.
Table 1: Regional Antibiotic Resistance Prevalence in Common Bacterial Infections (2023)
| WHO Region | Resistance Prevalence | Key Contextual Notes |
|---|---|---|
| South-East Asia & Eastern Mediterranean | 1 in 3 infections (approx. 33%) | Highest regional prevalence |
| African Region | 1 in 5 infections (approx. 20%) | |
| Global Average | 1 in 6 infections (approx. 16.7%) | |
| Region of the Americas | 1 in 7 infections (approx. 14%) | Slightly better than global average |
Resistance is more common and worsening in areas where health systems lack the capacity for robust diagnosis and treatment of bacterial pathogens [7] [106]. This highlights a critical feedback loop: regions with weaker health infrastructure are both more severely affected by AMR and less able to generate the surveillance data needed to combat it.
The Growing Threat of Resistant Gram-Negative Pathogens
The data solidifies the status of drug-resistant Gram-negative bacteria as one of the most dangerous threats. Among these, Escherichia coli and Klebsiella pneumoniae are particularly concerning, especially in the context of life-threatening bloodstream infections [7] [107].
Table 2: Resistance in Key Gram-Negative Pathogens to First-Line Antibiotics (2023)
| Pathogen | Antibiotic Class (Example) | Global Resistance Rate | Noteworthy Regional Data |
|---|---|---|---|
| Escherichia coli | Third-generation cephalosporins | > 40% | |
| Klebsiella pneumoniae | Third-generation cephalosporins | > 55% | Resistance exceeds 70% in the African Region |
| E. coli, K. pneumoniae, Salmonella, Acinetobacter | Carbapenems and Fluoroquinolones | Increasing | Carbapenem resistance, once rare, is becoming more frequent |
The rise of resistance to last-resort antibiotics like carbapenems is especially troubling, as it severely narrows treatment options. This often forces a reliance on older, more toxic, or costly antibiotics, which may be unavailable in low- and middle-income countries [7] [107]. For researchers, these pathogens represent a critical target for the development of new therapeutic agents, particularly those with novel mechanisms of action that can circumvent existing resistance pathways.
Experimental Protocols for Natural Product Research Informed by Surveillance Data
Surveillance data from GLASS directly informs the strategic direction of research into natural antibiotics. The following protocols outline a standardized methodology for screening and evaluating natural products against priority pathogens identified in GLASS reports.
Protocol 1: In-vitro Screening of Natural Products against WHO Priority Pathogens
Objective: To evaluate the antibacterial activity of natural product extracts against a panel of WHO priority bacterial pathogens, including multidrug-resistant (MDR) strains.
Materials:
- Bacterial Strains: A panel including Methicillin-resistant Staphylococcus aureus (MRSA), Carbapenem-resistant Escherichia coli and Klebsiella pneumoniae, and others from the WHO priority list [108].
- Natural Product Extracts: Lyophilized extracts dissolved in an appropriate solvent (e.g., DMSO, ethanol, or aqueous buffer) with sterility filtration (0.22 µm).
- Culture Media: Mueller-Hinton Broth (MHB) and Agar (MHA), as per CLSI guidelines.
- Equipment: Microplate reader, incubator, sterile 96-well microtiter plates.
Methodology:
- Preparation of Inoculum: Adjust the turbidity of overnight bacterial cultures in MHB to a 0.5 McFarland standard, then dilute to a final concentration of approximately 5 × 10^5 CFU/mL in fresh MHB.
- Microbroth Dilution Assay:
- Dispense 100 µL of the diluted inoculum into each well of a 96-well plate.
- Serially dilute the natural product extract across the plate (e.g., two-fold dilutions) to achieve a range of concentrations. Include a growth control (inoculum without extract) and a sterility control (media only).
- Seal the plate and incubate at 37°C for 16-20 hours.
- Determination of Minimum Inhibitory Concentration (MIC):
- Following incubation, visually inspect the plate for turbidity. The MIC is defined as the lowest concentration of the extract that completely inhibits visible growth.
- For a more objective endpoint, add a resazurin indicator (0.02% w/v) and incubate for an additional 2-4 hours. A color change from blue to pink indicates metabolic activity and thus, bacterial growth.
- Biofilm Inhibition Assay: For biofilm-forming pathogens like Pseudomonas aeruginosa and Staphylococcus aureus:
- Incubate the bacteria with sub-MIC concentrations of the natural extract in a sterile, flat-bottom plate for 24-48 hours.
- Gently remove the planktonic cells and wash the adhered biofilm.
- Fix with methanol and stain with 0.1% crystal violet for 15 minutes.
- Destain with 33% glacial acetic acid and measure the absorbance at 570 nm. A reduction in absorbance indicates inhibition of biofilm formation [109].
Protocol 2: Checkerboard Synergy Assay for Combination Therapy
Objective: To determine the synergistic effect between a natural product and a conventional antibiotic against a multidrug-resistant bacterial isolate.
Materials: The same as Protocol 1, with the addition of a standard antibiotic (e.g., a cephalosporin or carbapenem).
Methodology:
- Plate Setup:
- Prepare a solution of the natural product at 4× the starting concentration and the antibiotic at 4× its starting concentration.
- Dispense the natural product in a series of descending concentrations along the y-axis of the 96-well plate.
- Dispense the antibiotic in a series of descending concentrations along the x-axis.
- Add the bacterial inoculum to all wells, resulting in a final volume of 200 µL and 1× concentrations of both agents in each well.
- Incubation and Analysis:
- Incubate the plate at 37°C for 16-20 hours.
- Determine the MIC of each agent alone and in combination.
- Calculate the Fractional Inhibitory Concentration (FIC) Index:
FIC Index = (MIC of Drug A in combination / MIC of Drug A alone) + (MIC of Drug B in combination / MIC of Drug B alone) - Interpretation: Synergy is typically defined as an FIC Index ≤ 0.5. This approach can help "rescue" the efficacy of existing antibiotics [109] [108].
Diagram 1: Experimental workflow for evaluating natural products against resistant bacteria.
Visualization of Research Workflows and Resistance Mechanisms
Understanding the workflow for evaluating natural products and the mechanisms by which they overcome resistance is critical for research and development. The following diagram illustrates a multi-target mechanism, a key advantage of many natural compounds.
Diagram 2: Multi-target mechanisms of natural antimicrobial compounds.
The Scientist's Toolkit: Key Research Reagent Solutions
Translating GLASS data into actionable research requires a specific toolkit. The table below details essential reagents and their functions for conducting the experimental protocols outlined in this guide.
Table 3: Essential Research Reagents for Antimicrobial Resistance Studies
| Reagent / Material | Function / Application | Examples / Notes |
|---|---|---|
| Defined Natural Product Extracts | Source of novel antimicrobial compounds for primary screening. | Standardized extracts from plants (e.g., Aloe vera, Psidium guajava), algae; rich in alkaloids, flavonoids, phenols [109] [108]. |
| WHO Priority Pathogen Panel | Representative target strains for in-vitro and in-vivo assays. | MDR strains of Acinetobacter baumannii, Pseudomonas aeruginosa, Escherichia coli, Klebsiella pneumoniae, MRSA [108]. |
| Cell Viability Indicators | Objective measurement of bacterial growth inhibition in microtiter assays. | Resazurin (AlamarBlue); MTT; Tetrazolium salts. |
| Biofilm Staining Reagents | Quantification of biofilm mass and assessment of anti-biofilm activity. | Crystal Violet (total biomass); SYTO stains (confocal microscopy). |
| Synergy Assay Matrix | High-throughput screening of natural product-antibiotic interactions. | 96-well or 384-well plates for checkerboard assays. |
| Permeabilization & Efflux Assays | Elucidate mechanism of action, specifically membrane integrity and efflux pump activity. | Ethidium bromide uptake assays; N-phenylnaphthylamine (NPN) for outer membrane permeability; efflux pump inhibitors like PAβN. |
The WHO GLASS data from 2018 to 2023 paints a clear and urgent picture: antibiotic resistance is a pervasive and growing global crisis. The trends show steady annual increases, with Gram-negative pathogens like E. coli and K. pneumoniae posing a particularly severe threat, especially in regions with developing health systems. This surveillance intelligence is not merely a warning; it is a strategic roadmap for the research community. It directs efforts towards the most critical pathogens and highlights the need for innovative solutions. Natural products, with their inherent multi-target mechanisms and synergistic potential with conventional antibiotics, represent a promising frontier in this fight. The experimental frameworks and tools detailed in this guide provide a foundation for systematically exploring this potential, offering a path forward to discover the next generation of therapeutics against drug-resistant bacterial infections.
Comparative Analysis of Resistance Mechanisms Across Gram-negative and Gram-positive Species
Antimicrobial resistance (AMR) represents one of the most pressing global health crises of our time, with drug-resistant bacterial infections contributing to approximately 4.95 million deaths annually worldwide [85]. The World Health Organization (WHO) has classified various bacterial pathogens as critical priorities based on their resistance profiles and clinical impact, emphasizing the urgent need for research and development of novel therapeutic strategies [110] [111]. This whitepaper provides a comprehensive technical analysis of the distinct resistance mechanisms employed by Gram-positive and Gram-negative bacterial species, framed within the context of natural antibiotic resistance research.
The fundamental structural differences between Gram-positive and Gram-negative bacteria establish the foundation for their divergent resistance strategies. Gram-positive bacteria possess a thick peptidoglycan layer exterior to the cell membrane, which retains the crystal violet dye in Gram staining [112]. In contrast, Gram-negative bacteria feature a more complex, multi-layered cell envelope consisting of an outer membrane (containing lipopolysaccharides), a thinner peptidoglycan layer, and an inner cytoplasmic membrane [110] [113]. This outer membrane serves as a formidable permeability barrier that intrinsically protects Gram-negative bacteria from many antimicrobial agents [113].
Structural Foundations of Resistance
Gram-Positive Cell Wall Architecture
The cell wall of Gram-positive bacteria is characterized by a thick, multi-layered peptidoglycan (PG) scaffold that provides structural integrity and protection from environmental stresses [112]. This peptidoglycan matrix consists of linear glycan strands formed from alternating residues of N-acetylmuramic acid (MurNAc) and N-acetylglucosamine (GlcNAc), cross-linked via short peptide bridges to create a dense mesh-like sacculus [111]. Embedded within this peptidoglycan layer are anionic polymers called teichoic acids, which serve as sensors and facilitate the movement of molecules [112]. The substantial thickness of the Gram-positive cell wall (20-80 nm) represents the primary interface with the extracellular environment and constitutes the first line of defense against antimicrobial agents [111].
Gram-Negative Cell Envelope Complexity
The Gram-negative cell envelope presents a more sophisticated barrier system with three distinct components [110] [113]. The outer membrane (OM) is an asymmetric lipid bilayer with phospholipids in the inner leaflet and lipopolysaccharides (LPS) in the outer leaflet. This OM contains protein channels called porins that regulate the passage of hydrophilic molecules, including many antibiotics [110]. Beneath the OM lies a thin, single-layer peptidoglycan cell wall that provides structural support but offers minimal barrier function. The innermost layer is the symmetric phospholipid inner membrane (IM), which hosts numerous proteins involved in transport, biosynthesis, and energy production [113]. This complex envelope structure makes Gram-negative bacteria intrinsically resistant to many antibiotic classes that can effectively target Gram-positive pathogens [113].
Table 1: Comparative Cell Envelope Characteristics
| Feature | Gram-Positive Bacteria | Gram-Negative Bacteria |
|---|---|---|
| Outer Membrane | Absent | Present (with LPS) |
| Peptidoglycan Layer | Thick (20-80 nm), multi-layered | Thin (2-7 nm), single-layered |
| Teichoic Acids | Present | Absent |
| Periplasmic Space | Absent | Present |
| Porins | Absent | Present in outer membrane |
| Permeability Barrier | Peptidoglycan and capsule | Outer membrane and porins |
Molecular Mechanisms of Antibiotic Resistance
Bacteria employ four principal biochemical strategies to circumvent antibiotic activity, though the specific implementations differ significantly between Gram-positive and Gram-negative species [110] [111].
Enzymatic Inactivation or Modification
Gram-positive bacteria frequently produce β-lactamases that hydrolyze the β-lactam ring of penicillin and related antibiotics, rendering them ineffective [112] [111]. Additionally, they utilize transferase enzymes that modify antibiotics through phosphorylation, acetylation, or adenylation—a strategy particularly effective against aminoglycosides, chloramphenicol, and fluoroquinolones [111].
Gram-negative bacteria similarly employ a diverse array of β-lactamases, including extended-spectrum β-lactamases (ESBLs) and carbapenemases (KPC, NDM, VIM, OXA-48), which hydrolyze advanced-generation cephalosporins and carbapenems [110] [113]. The location of these enzymes in the periplasmic space of Gram-negative bacteria enhances their protective efficacy by intercepting antibiotics before they reach their cellular targets [113].
Target Site Modification
Alteration of antibiotic binding sites represents a common resistance mechanism across bacterial types. Gram-positive pathogens such as MRSA express an alternative penicillin-binding protein (PBP2a) with reduced affinity for β-lactam antibiotics [112]. Similarly, vancomycin-resistant Enterococcus faecium (VRE) modifies the D-Ala-D-Ala target to D-Ala-D-Lac, dramatically reducing vancomycin binding affinity [112].
Gram-negative bacteria develop mutations in genes encoding target enzymes, including DNA gyrase (gyrA/B) and topoisomerase IV (parC/E) for fluoroquinolones, and ribosomal RNA for aminoglycosides [113]. These target modifications occur without compromising essential bacterial functions, demonstrating the precision of evolutionary adaptation.
Enhanced Efflux Systems
Efflux pumps represent a formidable resistance mechanism, actively exporting antibiotics from the bacterial cell. Gram-positive bacteria utilize proton motive force-dependent transporters such as NorA, which confers resistance to fluoroquinolones [112].
Gram-negative bacteria deploy sophisticated multi-component efflux systems, particularly those in the Resistance-Nodulation-Division (RND) family (e.g., AcrAB-TolC in Escherichia coli) [110] [114]. These systems span the entire cell envelope, efficiently extruding diverse antibiotic classes from the periplasmic space and cytoplasm directly to the extracellular environment [114].
Reduced Permeability
While Gram-positive bacteria may alter their thick peptidoglycan structure to limit antibiotic penetration, this strategy is less significant compared to their other resistance mechanisms [111].
In contrast, Gram-negative bacteria excel at regulating membrane permeability by modifying porin expression (channel closure) or mutating porin genes to reduce antibiotic influx [110] [114]. They may also alter lipopolysaccharide structure to reduce binding of cationic antimicrobial peptides and antibiotics like colistin [113].
Table 2: Comparative Analysis of Primary Resistance Mechanisms
| Mechanism | Gram-Positive Examples | Gram-Negative Examples |
|---|---|---|
| Enzymatic Inactivation | β-lactamases (Staphylococcus), VanA (Enterococcus) | ESBLs (E. coli, Klebsiella), Carbapenemases (KPC, NDM) |
| Target Modification | PBP2a (MRSA), D-Ala-D-Lac (VRE) | gyrA/parC mutations (Fluoroquinolone resistance), 16S rRNA methylation (Aminoglycoside resistance) |
| Efflux Pumps | NorA (S. aureus), Mef(A)/Msr(A) (Macrolides) | RND pumps (AcrAB-TolC), MexAB-OprM (P. aeruginosa) |
| Reduced Permeability | Peptidoglycan remodeling | Porin loss/mutations (OmpF/C), LPS modification (mcr genes) |
Experimental Methodologies for Resistance Mechanism Analysis
Gene Network Analysis for Resistance Investigation
Objective: To identify key genetic determinants and molecular pathways associated with antibiotic resistance through comprehensive gene network analysis [115].
Protocol:
- Selection of Differentially Expressed Genes (DEGs): Retrieve gene expression data from drug-resistant bacterial strains using publicly available databases (e.g., GEO, SRA). Select up-regulated genes with fold change >2 (p<0.05) associated with drug-resistance mechanisms [115].
- Protein-Protein Interaction (PPI) Network Construction: Input significantly up-regulated genes into the STRING database (version 12.0+) using organism-specific reference genomes. Select significant interactions with medium confidence value >0.4 [115].
- PPI Network Analysis: Import network data into Cytoscape (v3.9.1+). Use CytoHubba plugin to identify hub genes through topological algorithms (MNC, DMNC, MCC, Degree). Perform cluster analysis using Cytocluster plugin with IPCA algorithm (Tin threshold=0.5, shortest path length=2, complex size threshold=10) [115].
- Pathway Enrichment and Gene Ontology Analysis: Conduct functional enrichment analysis of hub genes and their interactions using STRING database. Categorize genes according to cellular components, molecular functions, and biological processes [115].
- Promoter Analysis: Examine 200 bp upstream flanking regions of hub genes to identify putative regulatory elements and transcription factor binding sites [115].
- miRNA-gene Interaction Prediction: Predict interactions between bacterial milRNAs and up-regulated genes to identify post-transcriptional regulatory mechanisms [115].
Graph 1: Gene Network Analysis Workflow. This workflow outlines the computational pipeline for identifying key genetic elements in antibiotic resistance.
Morbidostat-Based Experimental Evolution
Objective: To investigate resistance development dynamics under controlled antibiotic selection pressure using continuous culturing technology [116].
Protocol:
- Bacterial Strain Preparation: Obtain reference strains from certified culture collections (e.g., ATCC). Prepare microbial suspensions from isolated colonies cultivated on appropriate agar media. Standardize growth in liquid broth (e.g., Mueller-Hinton) to ensure uniform conditions [116].
- Morbidostat Operation: Utilize a computer-controlled continuous culturing bioreactor that automatically monitors bacterial density via optical density (OD600) measurements. The system employs an algorithm that switches between drug-containing media (increasing selective pressure when bacterial growth exceeds dilution rate) and drug-free media (decreasing pressure when growth is inhibited) [116].
- Experimental Evolution: Inoculate the morbidostat with the bacterial strain of interest. Program the system to maintain a defined dilution rate while automatically adjusting antibiotic concentration to exert selective pressure. Continue evolution experiments for predetermined generations (typically 200-500) [116].
- Clonal Analysis and Whole Genome Sequencing: Periodically sample evolving populations throughout the experiment. Isolate individual clones for comprehensive analysis. Extract genomic DNA from evolved isolates and subject to whole genome sequencing to identify mutations associated with resistance development [116].
- Phenotypic Characterization: Determine MIC values for evolved clones using broth macrodilution methods according to CLSI/EUCAST guidelines. Assess cross-resistance patterns to other antibiotic classes [116].
- Resistance Mechanism Validation: Clone identified mutated genes into susceptible parental strains to confirm causal relationship to resistance [116].
Graph 2: Morbidostat Experimental Evolution Pipeline. This diagram illustrates the workflow for studying resistance development under controlled antibiotic selection.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Antibiotic Resistance Studies
| Reagent/Platform | Application | Technical Specifications |
|---|---|---|
| Cytoscape (v3.9.1+) | Network analysis and visualization | Open-source platform with CytoHubba and Cytocluster plugins for hub gene identification and cluster analysis [115] |
| STRING Database | Protein-protein interaction network construction | Comprehensive resource with medium confidence cutoff >0.4 for significant interactions; organism-specific reference datasets [115] |
| Morbidostat Device | Experimental evolution under antibiotic pressure | Computer-controlled continuous culturing system with OD600 monitoring and automated drug concentration adjustment [116] |
| Mueller-Hinton Broth | Standardized antimicrobial susceptibility testing | CLSI-approved medium for broth macrodilution MIC determinations; ensures reproducible growth conditions [116] |
| CLSI/EUCAST Guidelines | Standardized antimicrobial susceptibility testing | Definitive protocols for MIC determination and resistance breakpoint definitions [116] |
| Whole Genome Sequencing Platforms | Identification of resistance mutations | Illumina, Nanopore, or PacBio platforms for comprehensive genomic analysis of evolved isolates [116] |
Emerging Therapeutic Approaches Against Resistant Pathogens
Novel Antimicrobial Agents and Adjuvants
The development of new antimicrobial chemical entities continues to be a critical strategy, though the pipeline remains limited. Recent advances include β-lactam/β-lactamase inhibitor combinations such as ceftazidime-avibactam and meropenem-vaborbactam, which effectively target carbapenem-resistant Enterobacteriaceae [114]. Additionally, siderophore-cephalosporin conjugates like cefiderocol exploit bacterial iron uptake systems to enhance penetration through the outer membrane of Gram-negative pathogens [114]. For Gram-positive infections, next-generation oxazolidinones and tetracycline derivatives show promise against resistant strains, though resistance emergence remains a concern [112] [111].
Non-Traditional Antimicrobial Therapies
Bacteriophage Therapy: Lytic bacteriophages offer a highly specific approach against multidrug-resistant bacterial infections. Phages can be administered as customized cocktails tailored to individual patient isolates or as fixed-composition products targeting specific pathogens [117]. Clinical applications have demonstrated efficacy against various Gram-negative infections, including those caused by Pseudomonas aeruginosa, Acinetobacter baumannii, and Escherichia coli, particularly in biofilm-associated conditions where conventional antibiotics fail [117].
Antimicrobial Peptides (AMPs): These naturally occurring molecules, such as the newly developed TGV-49, disrupt microbial membranes through interactions with phospholipids and fatty acids, leading to rapid cell lysis [116]. Their mechanism of action makes them less susceptible to conventional resistance mechanisms, though bacterial adaptation remains possible [116].
Anti-virulence Strategies: Compounds that target bacterial virulence factors rather than essential growth processes represent an innovative approach to circumventing resistance. These agents disarm pathogens without imposing strong selective pressure for resistance development [117].
Graph 3: Emerging Therapeutic Strategies. This diagram outlines innovative approaches to combat antibiotic-resistant infections.
The comparative analysis of resistance mechanisms across Gram-positive and Gram-negative species reveals both shared strategies and distinct adaptations reflecting their fundamental structural differences. Gram-positive bacteria rely heavily on target modification and enzymatic inactivation, while Gram-negative pathogens exploit their complex envelope structure to limit drug access while deploying sophisticated efflux systems. Understanding these mechanistic differences is essential for developing targeted therapeutic strategies that address the unique vulnerabilities of each bacterial type.
The escalating global AMR crisis demands innovative approaches that move beyond traditional antibiotic discovery. Advanced methodologies such as gene network analysis and experimental evolution provide powerful tools for deciphering resistance mechanisms and identifying novel targets. Furthermore, non-traditional therapies including bacteriophages, antimicrobial peptides, and anti-virulence agents offer promising alternatives that may help break the cycle of resistance development. As research continues, a multifaceted approach combining these diverse strategies will be essential for addressing the growing threat of multidrug-resistant bacterial infections across both Gram-positive and Gram-negative species.
Evaluating the Clinical and Economic Burden of Key Resistant Pathogens
Antimicrobial resistance (AMR) represents one of the most pressing global public health challenges of the 21st century, undermining the efficacy of life-saving treatments and escalating both clinical complications and economic costs worldwide. The World Health Organization (WHO) has declared AMR a top global public health threat, with bacterial antibiotic resistance (ABR) contributing significantly to the estimated 4.95 million deaths annually associated with drug-resistant infections [118] [119]. This whitepaper provides a comprehensive technical evaluation of the clinical and economic burdens imposed by key resistant pathogens, contextualized within broader research on bacterial species possessing natural antibiotic resistance. For researchers and drug development professionals, understanding these multifaceted burdens is fundamental to guiding therapeutic innovation, surveillance efforts, and investment priorities in an era of diminishing treatment options.
The escalating AMR crisis has been further exacerbated by the COVID-19 pandemic, which led to substantial constraints in antibiotic treatment options and increased resistance rates [62]. In response, international surveillance systems like the WHO's Global Antimicrobial Resistance and Use Surveillance System (GLASS) have been established to generate standardized data and guide public health action [105]. This analysis synthesizes the most current surveillance data, economic modeling studies, and emerging research tools to provide a foundational resource for scientific efforts aimed at mitigating the AMR threat.
Global Prevalence and Health Impact of Key Resistant Pathogens
Surveillance data reveals alarming trends in the prevalence and mortality associated with key resistant pathogens globally. According to the 2025 WHO GLASS report, which draws on more than 23 million bacteriologically confirmed cases from 110 countries between 2016 and 2023, AMR is undermining effective treatment for a wide spectrum of infections including bloodstream infections, urinary tract infections, gastrointestinal infections, and urogenital gonorrhoea [105]. This extensive dataset provides critical insights into the adjusted global and regional estimates of AMR for 93 infection type–pathogen–antibiotic combinations, representing the most comprehensive surveillance effort to date.
In the United States, CDC data indicates that more than 2.8 million antimicrobial-resistant infections occur each year, resulting in more than 35,000 deaths annually. When Clostridioides difficile infections are included, the U.S. toll exceeds 3 million infections and 48,000 deaths each year [120]. The global distribution of resistant pathogens follows distinct patterns, with a 2022 meta-analysis of food samples from Italy and Thailand between 2012-2021 revealing regional variations in resistance profiles. In Italy, the highest microbial prevalence was associated with β-lactam and tetracycline resistance, while Thailand reported predominantly cephalosporin and aminoglycoside resistance among isolated pathogens [121].
Table 1: Global Prevalence and Impact of Priority Resistant Pathogens
| Pathogen | Resistance Profile | Key Infections Caused | WHO Priority Category | Notable Regional Prevalence |
|---|---|---|---|---|
| Acinetobacter baumannii | Carbapenem-resistant | Bloodstream infections, pneumonia | Critical | Increasing globally in healthcare settings |
| Enterobacterales | Third-generation cephalosporin & carbapenem-resistant | Urinary tract, bloodstream infections | Critical | High prevalence in hospitals worldwide |
| Pseudomonas aeruginosa | Carbapenem-resistant | Healthcare-associated infections, pneumonia | High | MDR strains detected in Italy & Thailand |
| Staphylococcus aureus | Methicillin-resistant (MRSA) | Skin infections, pneumonia, bacteremia | High | Community and healthcare-associated spread |
| Enterococcus faecium | Vancomycin-resistant (VRE) | Surgical site infections, bacteremia | High | Increasing hospital-onset infections in U.S. |
| Escherichia coli | 3rd-gen cephalosporin & carbapenem-resistant | Urinary tract, gastrointestinal infections | Critical | Most prevalent in food samples in Italy & Thailand [121] |
| Klebsiella pneumoniae | Carbapenem-resistant | Pneumonia, bloodstream infections | Critical | Major contributor to global AMR burden |
| Mycobacterium tuberculosis | Rifampicin-resistant | Tuberculosis | Separate WHO listing | High cost-per-case across income settings [118] |
The WHO Bacterial Priority Pathogens List (WHO BPPL) serves as a critical guide for directing research and development efforts toward the most threatening resistant pathogens [62]. The 2024 list categorizes pathogens into three priority groups (Critical, High, and Medium) based on criteria including mortality, community and healthcare burden, prevalence of resistance, and transmissibility. This classification system helps align scientific resources with the most pressing public health needs, particularly for bacterial species exhibiting natural antibiotic resistance mechanisms.
Quantitative Economic Burden Analysis
The global economic burden of antibiotic-resistant infections is staggering, with recent comprehensive modeling studies quantifying both direct healthcare costs and broader productivity losses. A 2025 analysis published in BMJ Global Health calculated that ABR was associated with a median value of US$693 billion (IQR: US$627–768 billion) in hospital costs globally, with an additional US$194 billion in productivity losses due to premature mortality and morbidity [118] [122]. These figures underscore the massive economic implications of AMR that extend far beyond direct medical expenses to encompass significant macroeconomic impacts.
Table 2: Economic Burden of Antibiotic-Resistant Infections by Pathogen Category
| Pathogen/Resistance Type | Attributable Hospital Cost Per Case (US$) | Key Drivers of Economic Burden | Potential Avertable by Vaccines (US$) |
|---|---|---|---|
| Multidrug-resistant Tuberculosis | $3,000 (LICs) – $41,000 (HICs) | Extended hospitalization, specialized drug regimens, isolation requirements | Substantial portion of total $207B hospital costs avertable [118] |
| Carbapenem-resistant Infections | $3,000 – $7,000 (depending on syndrome) | High mortality, prolonged ICU stays, limited treatment options | Significant proportion with E. coli & K. pneumoniae vaccines [118] |
| Methicillin-resistant S. aureus (MRSA) | Varies by healthcare setting & country income level | Surgical site infections, bacteremia, increased length of stay | Up to 30-40% of associated costs with effective vaccination [122] |
| Third-generation cephalosporin-resistant Enterobacterales | Significant cost increments vs. susceptible infections | Complicated urinary tract & bloodstream infections | Major proportion avertable with E. coli vaccination [118] |
| Vancomycin-resistant Enterococcus (VRE) | Notable cost increases in hospital settings | Healthcare-associated infections in immunocompromised | Potential reduction through infection control & future vaccines |
The economic burden varies substantially across pathogens and healthcare settings. Multidrug-resistant tuberculosis demonstrated the highest mean hospital cost attributable to ABR per patient, ranging from US$3,000 in lower-income settings to US$41,000 in high-income settings [118]. Carbapenem-resistant infections were also associated with exceptionally high costs-per-case, estimated between US$3,000–US$7,000 depending on the specific infection syndrome. In the United States specifically, treatment for six frequent antimicrobial-resistant healthcare-associated pathogens contributes to more than $4.6 billion in healthcare costs annually [123], with this figure representing only direct hospitalization costs rather than comprehensive economic impact.
From a healthcare system perspective, it is crucial to distinguish between the incremental cost of an ABR infection compared to a susceptible infection (the attributable burden of ABR) versus the incremental cost of an ABR infection compared to no infection (the associated burden of ABR) [118]. This distinction has important implications for evaluating different intervention strategies, with stewardship programs requiring attributable burden metrics while preventive measures like vaccination require associated burden data for economic assessments.
Methodologies for Studying Resistance Mechanisms and Compound Efficacy
Fluorescent Antibiotic Probes for Resistance Visualization
The use of fluorescent antibiotics represents a powerful methodological advancement for studying antimicrobial resistance mechanisms, offering significant advantages over traditional approaches. The experimental protocol involves several key stages [124]:
Synthesis of Azide Derivatives: Azide derivatives of target antibiotics are first synthesized through chemical modification, creating a reactive handle for subsequent fluorophore attachment.
Click Chemistry Conjugation: The azide-functionalized antibiotics are coupled with alkyne-fluorophores using copper-catalyzed azide-alkyne cycloaddition, a specific form of click chemistry that enables efficient conjugation under mild conditions.
Purification and Validation: The resulting fluorescent antibiotic probes undergo thorough purification to remove unreacted components, followed by validation of their antimicrobial activity through minimum inhibitory concentration (MIC) assessment against both susceptible and resistant bacterial strains.
Bacterial Accumulation Studies: Bacterial accumulation of the fluorescent probes can be quantified using either spectrophotometry for population-level measurements or flow cytometry for single-cell analysis, providing insights into permeability differences between resistant and susceptible strains.
Subcellular Localization: Confocal microscopy enables examination of the spatial distribution of fluorescent antibiotics within bacterial cells, affording valuable information about drug target engagement and alterations that occur in resistant species.
This methodology enables researchers to directly visualize antibiotic uptake, retention, and localization in ways that traditional susceptibility testing cannot provide, particularly for understanding intrinsic resistance mechanisms in bacterial species with natural antibiotic resistance.
Natural Product Screening Against Priority Pathogens
Systematic screening of natural products represents a promising approach for discovering novel antimicrobial compounds effective against resistant pathogens. A 2025 systematic review conducted comprehensive searches across PUBMED/MEDLINE, WEB OF SCIENCE, and SCOPUS databases, identifying 4371 articles published between 2014 and 2024, from which 290 studies were selected for detailed analysis [62]. The methodology followed these key stages:
Search Strategy Implementation: Comprehensive literature searches employed primary search terms and MeSH phrases including ("natural product" OR "natural compound") AND (antibacteri* OR antimicrobial*) AND (MDR OR "multi-drug resistant *"), with Boolean operators customized for each database's requirements.
Strict Inclusion Criteria Application: Studies were selected based on four criteria: (1) original research design; (2) investigation of antimicrobial effects of natural products; (3) measurement of antimicrobial effects against resistant pathogens; and (4) publication in English.
Quality Assessment: Methodological rigor was evaluated using the Newcastle-Ottawa Scale for observational studies and the Cochrane Risk of Bias tool for randomized controlled trials.
Data Extraction and Synthesis: Information on plant habitats, active compound classes, extraction solvents, and antimicrobial efficacy was systematically extracted and categorized.
This rigorous methodology identified several key classes of plant-derived compounds with significant antioxidant and antimicrobial activity against WHO priority pathogens, including alkaloids, flavonoids, phenols, saponins, tannins, and terpenoids [62]. These bioactive compounds were typically extracted using varied solvents including ethanol, methanol, aqueous solutions, benzoate, ethyl acetate, n-butanol, and methanolic preparations obtained from different plant parts such as leaves, bark, flowers, and roots.
Emerging Solutions and Research Frontiers
Novel Antibiotic Discovery
The urgent need for new antimicrobial agents has spurred innovative approaches to antibiotic discovery, with several promising developments emerging recently. Researchers at McMaster University have identified a new class of antibiotics called lariocidin from a soil bacterium (Paenibacillus) collected from a residential garden [119]. This discovery is particularly significant as it represents the first new class of antibiotics to reach the market in nearly three decades. Lariocidin demonstrates several ideal characteristics for a drug candidate: it exhibits a novel mechanism of action by binding directly to the bacterial protein synthesis machinery in a previously unreported way; it shows activity against otherwise drug-resistant bacteria; it demonstrates low toxicity to human cells; and it performs effectively in animal infection models.
Concurrently, other research teams have discovered additional promising antibiotic molecules that target broad ranges of drug-resistant bacteria through novel mechanisms [92]. These discoveries highlight the continued value of exploring diverse environmental niches, including common sources like soil samples, for identifying microorganisms that produce antimicrobial compounds with activity against resistant pathogens.
Vaccine Development to Mitigate Economic Burden
Vaccination represents a promising strategy for reducing the substantial economic burden associated with antibiotic-resistant infections. Modeling studies indicate that bacterial vaccines could avert 30-40% of hospital costs and productivity losses attributable to AMR [118] [122]. Specifically, vaccines targeting Staphylococcus aureus, Escherichia coli, and Klebsiella pneumoniae could prevent a substantial portion of the economic burden across diverse geographic and economic settings. The 2025 economic burden study quantified that approximately US$207 billion (IQR: US$186-229 billion) in hospital costs and US$76 billion in productivity losses could be potentially avertable through vaccination [118].
These findings provide strong economic justification for increased investment in vaccine development as part of a comprehensive strategy to combat antimicrobial resistance. From a policy perspective, vaccines offer the dual benefit of directly preventing resistant infections while simultaneously reducing antibiotic consumption through decreased incidence of susceptible infections, thereby slowing the emergence of new resistance mechanisms.
Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents for Antimicrobial Resistance Studies
| Research Reagent/Tool | Primary Function | Application in AMR Research |
|---|---|---|
| Fluorescent Antibiotic Probes | Visualizing antibiotic uptake and localization | Studying permeability barriers & efflux pump activity in resistant strains [124] |
| Click Chemistry Components | Covalent conjugation of fluorophores to antibiotics | Generating customized molecular probes for specific antibiotic classes |
| Minimum Inhibitory Concentration (MIC) Panels | Determining bacterial susceptibility thresholds | Standardized assessment of resistance levels across pathogen collections |
| Natural Product Libraries | Screening bioactive plant extracts | Identifying novel compounds with activity against priority pathogens [62] |
| Solvent Extraction Systems | Isolating active compounds from natural sources | Preparing plant-derived antimicrobials for mechanism of action studies |
| Confocal Microscopy | High-resolution spatial imaging | Subcellular localization of antibiotics in bacterial cells [124] |
| Flow Cytometry | Single-cell analysis of bacterial populations | Quantifying heterogeneous responses to antibiotics within cultures |
| Animal Infection Models | In vivo efficacy assessment | Evaluating novel compound performance in physiologically relevant systems [119] |
The clinical and economic burdens imposed by key resistant pathogens continue to escalate globally, necessitating coordinated and innovative responses from the research community. Comprehensive surveillance data from WHO GLASS reveals the alarming prevalence of resistance across essential pathogen-antibiotic combinations, while economic analyses quantify the staggering financial implications approaching US$700 billion annually in hospital costs alone [105] [118]. Methodological advances in fluorescent probe technology, natural product screening, and novel compound discovery provide powerful tools for investigating resistance mechanisms and developing new therapeutic options. For researchers focused on bacterial species with natural antibiotic resistance, these integrated approaches—combining basic science investigation with translational development of vaccines and novel antibiotics—represent the most promising pathway toward mitigating the growing threat of antimicrobial resistance. The significant economic burden avertable through vaccination (approximately 30-40% of total costs) underscores the importance of maintaining diversified research portfolios that address both treatment and prevention strategies in parallel [118] [122].
Benchmarking Novel Compounds Against Standard-of-Care Therapies
Within the urgent global effort to combat antimicrobial resistance (AMR), the discovery and validation of novel antibacterial compounds have become paramount. However, the translation of promising candidates from the laboratory to the clinic hinges on rigorous, standardized benchmarking against established standard-of-care therapies. Such benchmarking is essential for assessing the comparative efficacy, safety, and potential resistance profiles of new agents, thereby guiding strategic decisions in the drug development pipeline. This whitepaper provides a comprehensive technical guide for researchers and drug development professionals on the design and execution of robust benchmarking studies, contextualized within the rapidly advancing field of research on bacterial species with natural antibiotic resistance. It synthesizes contemporary strategies, data from recent discoveries, and detailed experimental protocols to establish a framework for the accurate evaluation of novel therapeutic compounds.
Foundational Principles of Benchmarking in Drug Discovery
Benchmarking novel compounds is a multifaceted process that extends beyond simple efficacy comparisons. It involves a systematic assessment of a compound's performance against a validated ground truth, utilizing protocols that are aligned with best practices to ensure reliability and generalizability [125].
A core component of benchmarking is the establishment of a ground truth mapping, which typically consists of a curated set of known drug-indication associations against which new predictions are measured. Commonly used sources for this include the Comparative Toxicogenomics Database (CTD) and the Therapeutic Targets Database (TTD). The choice of database can influence outcomes; for instance, one study reported that performance was better observed when using TTD instead of CTD when assessing drug-indication associations appearing in both mappings [125].
Data splitting is another critical step to avoid over-optimism and ensure model generalizability. Several methods are employed:
- K-fold cross-validation: Very commonly used, it involves partitioning the dataset into 'k' subsets, training the model on k-1 folds, and validating on the remaining fold [125].
- Temporal splits: This method splits data based on approval dates, testing the model's ability to predict newer drugs based on older data, which can provide a more realistic assessment of predictive power [125].
- Leave-one-out protocols: A special case of k-fold cross-validation where 'k' equals the number of data points [125].
Finally, the selection of appropriate performance metrics is crucial for correct interpretation. While Area Under the Receiver-Operating Characteristic Curve (AUC-ROC) and Area Under the Precision-Recall Curve (AUC-PR) are widely used, their relevance to drug discovery has been questioned [125]. More interpretable metrics such as recall at k (e.g., the proportion of known drugs ranked in the top 10 candidates), precision, and accuracy above a specific threshold are frequently reported and can offer more tangible insights for decision-making [125].
Contemporary Case Studies in Novel Compound Discovery
The following case studies illustrate the application of advanced technologies in discovering novel antimicrobials and the critical importance of benchmarking their activity against established treatments and controls.
Deep Learning-Driven Discovery of Archaeasins
The exploration of underexplored biological domains, such as archaea, represents a promising frontier for antibiotic discovery. In a landmark 2025 study, researchers leveraged a deep learning framework, APEX 1.1, to systematically mine 233 archaeal proteomes for encrypted antimicrobial peptides [82].
The workflow and key validation steps for these novel peptides, termed "archaeasins," are summarized below. This benchmarking process involved a series of in vitro and in vivo experiments to compare the novel archaeasins against established standard-of-care antibiotics.
The study provided quantitative benchmarking data essential for evaluating the potential of archaeasins. The table below summarizes the key efficacy results from the experimental validation phase.
Table 1: Benchmarking Data for Archaeasin-73 and Controls [82]
| Compound / Metric | In Vitro MIC (μmol/L) - Range across pathogens | In Vivo Efficacy (Mouse Model) - Reduction in A. baumannii load | Hit Rate (Synthesized Peptides) |
|---|---|---|---|
| Archaeasin-73 | ≤ 64 μmol/L (active against multiple strains) | Significant reduction | N/A |
| Polymyxin B (Control) | N/A (established antibiotic) | Comparable effectiveness to Archaeasin-73 | N/A |
| All Tested Archaeasins | 93% showed activity (MIC ≤ 64 μmol/L) against ≥1 strain | N/A | 93% (75 out of 80 synthesized) |
Exploiting Bacterial Resistance Mechanisms
A novel "resistance hacking" approach was demonstrated in a proof-of-concept study targeting Mycobacterium abscessus, an "antibiotic nightmare" intrinsically resistant to many drugs [20]. Researchers developed a structurally modified version of the antibiotic florfenicol that acts as a prodrug. This prodrug is converted to its active form by Eis2, a protein that the bacterium's master resistance regulator, WhiB7, induces for defense. This creates a perpetual cascade where WhiB7 activation leads to more Eis2, which generates more active antibiotic, further activating WhiB7, thereby continuously amplifying the antibiotic's effect [20].
The key benchmark for success in this study was the demonstration that the engineered florfenicol analog had strong activity against normal M. abscessus but no effect on a strain lacking WhiB7—the opposite of what is expected with conventional antibiotics [20]. This unique mechanism also resulted in a significantly improved safety profile by avoiding the mitochondrial toxicity associated with conventional phenicol antibiotics, a critical benchmark for therapeutic index [20].
Chemokines as Innate Antimicrobials
NIH IRP research has rediscovered the direct antimicrobial properties of certain chemokines, immune system molecules traditionally studied for their role in directing cell movement [83]. The study established that chemokines like CCL20 kill bacteria by binding to negatively charged phospholipids (cardiolipin and phosphatidylglycerol) in the bacterial cell membrane and disrupting it [83].
A crucial part of benchmarking these compounds was assessing the propensity to induce resistance. When bacteria were repeatedly exposed to sublethal doses of CCL20 over multiple generations, the dose needed to kill them remained constant. In contrast, bacteria exposed to conventional antibiotics required progressively higher doses, demonstrating that chemokines do not readily trigger antimicrobial resistance—a significant advantage over many standard-of-care therapies [83]. Furthermore, two such chemokines were benchmarked as being better at killing E. coli than the body's own specialized antimicrobial peptide, beta-defensin 3 [83].
Essential Experimental Protocols for Benchmarking
This section details specific methodologies cited in the case studies, providing a reproducible framework for benchmarking novel antimicrobial compounds.
Protocol: Minimum Inhibitory Concentration (MIC) Assays
The MIC assay is a fundamental benchmark for in vitro efficacy. The following protocol is adapted from the archaeasin study [82].
- Objective: To determine the lowest concentration of an antimicrobial agent that inhibits the visible growth of a microorganism.
- Materials:
- Cation-adjusted Mueller-Hinton Broth (CAMHB): Standard culture medium for antimicrobial susceptibility testing.
- Sterile 96-well microtiter plates.
- Test Compounds: Novel compounds (e.g., archaeasins) and control antibiotics (e.g., Polymyxin B, Levofloxacin) serially diluted in appropriate solvent/buffer [82].
- Bacterial Strains: Clinically relevant pathogens (e.g., Acinetobacter baumannii, Escherichia coli, Staphylococcus aureus, etc.) prepared to a standardized inoculum density (e.g., 5 × 10^5 CFU/mL) [82].
- Microplate reader (for optical density measurement).
- Procedure:
- Prepare two-fold serial dilutions of the test and control compounds in CAMHB across the wells of the microplate.
- Inoculate each well with the standardized bacterial suspension. Include growth control (bacteria, no compound) and sterility control (medium only) wells.
- Incubate the plates at 35±2°C for 16-20 hours.
- Determine the MIC visually or spectrophotometrically (e.g., at 600 nm) as the lowest concentration of compound that completely inhibits visible growth.
- Benchmarking Analysis: Compare the MIC values of novel compounds directly against those of standard-of-care antibiotics for the same bacterial strains under identical conditions.
Protocol:In VivoEfficacy in Murine Infection Models
In vivo models are critical for benchmarking therapeutic potential in a whole-organism context.
- Objective: To evaluate the efficacy of a novel compound in reducing bacterial load in a live animal infection model.
- Materials:
- Mouse model (e.g., immunocompromised or neutropenic mice for infection studies).
- Pathogen Strain: A bioluminescent or standard strain of a target bacterium (e.g., A. baumannii).
- Test and Control Compounds: Formulated for delivery (e.g., intravenous, intraperitoneal).
- In vivo imaging system (IVIS) if using bioluminescent strains, or materials for homogenizing tissue for CFU counts.
- Procedure:
- Infect mice via an appropriate route (e.g., intramuscular, intravenous) with a predetermined lethal dose of the bacterium.
- Randomize mice into treatment groups (novel compound, vehicle control, standard-of-care antibiotic control).
- Administer treatments at a specific time post-infection, with a defined dosing regimen.
- Monitor survival and/or quantify bacterial burden at endpoint. For burden, euthanize animals, harvest target organs (e.g., spleen, liver), homogenize, and plate serial dilutions for CFU enumeration. Alternatively, track bioluminescence signal intensity over time using IVIS [82].
- Benchmarking Analysis: Compare the reduction in bacterial load (log10 CFU/organ) or the improvement in survival rates in the novel compound group versus the standard-of-care and vehicle control groups. Statistical tests (e.g., t-test, ANOVA) are used to determine significance.
Protocol: Resistance Induction Assay
Benchmarking the potential for resistance development is a key differentiator for novel compounds.
- Objective: To assess if bacteria develop resistance upon repeated, sublethal exposure to a novel compound compared to a standard antibiotic.
- Materials:
- Bacterial strain (e.g., E. coli).
- Test Compound (e.g., chemokine CCL20) and Control Antibiotics with known resistance induction profiles [83].
- Culture media (e.g., LB broth).
- Procedure:
- Expose a bacterial population to a concentration of the compound that kills a substantial portion but not all of the population (sub-MIC).
- Allow the surviving bacteria to regrow in fresh medium without compound.
- Repeat steps 1 and 2 for multiple passages (e.g., 20+ cycles), each time challenging the regrown population with the same compound.
- Periodically (e.g., every 5 passages), perform an MIC assay to determine if the inhibitory concentration has increased [83].
- Benchmarking Analysis: Plot the MIC values over the number of passages for the novel compound and the control antibiotics. A flat line indicates no resistance development (a positive result for compounds like CCL20), while an upward slope indicates escalating resistance [83].
The Scientist's Toolkit: Key Reagent Solutions
The following table outlines essential reagents and their functions for the core experiments described in this whitepaper.
Table 2: Research Reagent Solutions for Key Antibacterial Benchmarking Experiments
| Reagent / Material | Function in Benchmarking | Example Use Case |
|---|---|---|
| Cation-adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for reproducible MIC assays, ensuring cation concentrations do not interfere with compound activity. | Used in MIC assays for archaeasins and control antibiotics [82]. |
| Polymyxin B | Standard-of-care control antibiotic for Gram-negative infections; serves as a benchmark for efficacy. | Used as a positive control in in vitro and in vivo validation of archaeasin-73 [82]. |
| Liposomes (composed of Cardiolipin/Phosphatidylglycerol) | Tool to mechanistically validate membrane-targeting action of antimicrobials via binding studies. | Used to demonstrate chemokines bind to anionic phospholipids to break bacterial membranes [83]. |
| Whole-Genome Sequencing (WGS) Services | Provides comprehensive analysis of resistance genes (resistome) and mechanisms in bacterial isolates. | Used to characterize multidrug-resistant bacteria from wastewater, identifying β-lactamase genes and efflux pumps [126]. |
| Curcumin & Emodin | Natural compounds used as benchmark inhibitors for screening alternative antimicrobial strategies. | Showed consistent inhibitory activity against multi-drug-resistant wastewater isolates like Microbacterium spp. [126]. |
The relentless rise of antimicrobial resistance demands a disciplined and rigorous approach to the development of new therapeutic agents. Benchmarking novel compounds against standard-of-care therapies is not merely a regulatory checkbox but a critical, iterative process that de-risks drug development and ensures that new candidates provide a genuine advance over existing options. By adopting the structured frameworks, contemporary case studies, and detailed experimental protocols outlined in this technical guide—from advanced computational mining and mechanistic in vitro assays to robust in vivo models and resistance induction studies—researchers can generate high-quality, comparable data. This disciplined approach is fundamental to identifying the most promising candidates, such as archaeasins and resistance-hacking prodrugs, and steering them successfully through the development pipeline, ultimately expanding our arsenal in the fight against drug-resistant bacteria.
Assessing the Impact of Global Initiatives and Public-Private Partnerships like CARB-X
The relentless rise of antimicrobial resistance (AMR) represents one of the most pressing challenges to modern medicine, directly responsible for approximately 1.27 million global deaths annually [127] [128]. Gram-negative bacteria, including Escherichia coli and Klebsiella pneumoniae, now exhibit particularly alarming resistance rates, with over 40% of E. coli and 55% of K. pneumoniae resistant to first-choice treatments like third-generation cephalosporins [7]. This crisis demands a coordinated global response, spurring the creation of public-private partnerships (PPPs) designed to accelerate the development of novel antibacterial solutions. Among these, the Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator (CARB-X) has emerged as a pivotal non-profit partnership dedicated to reinvigorating the early-stage antibacterial pipeline. This whitepaper assesses the strategic impact, operational methodologies, and scientific advancements driven by CARB-X, framing its role within the broader research landscape of intrinsically resistant bacterial species such as Mycobacterium abscessus.
Recent data from the World Health Organization (WHO) illuminates the accelerating pace of the AMR crisis. In 2023, approximately one in six laboratory-confirmed bacterial infections globally were resistant to antibiotic treatment [7] [129]. Between 2018 and 2023, antibiotic resistance increased in over 40% of the pathogen-antibiotic combinations monitored by WHO, with an average annual increase of 5-15% [7]. The burden of AMR is not distributed equally, with the WHO South-East Asian and Eastern Mediterranean Regions reporting the highest resistance levels, where one in three reported infections were resistant [7].
Table 1: Global Antibiotic Resistance Profile for Key Pathogens (2023)
| Bacterial Pathogen | Infection Type | First-Line Antibiotic | Global Resistance Rate | Key Regional Concern |
|---|---|---|---|---|
| Escherichia coli | Bloodstream, Urinary Tract | Third-generation cephalosporins | >40% [7] | African Region (>70%) [7] |
| Klebsiella pneumoniae | Bloodstream, Lower Respiratory | Third-generation cephalosporins | >55% [7] | African Region (>70%) [7] |
| Acinetobacter spp. | Bloodstream, Wound | Carbapenems | Increasing [7] | Widespread carbapenem resistance [7] |
| Staphylococcus aureus | Bloodstream, Skin/Soft Tissue | Oxacillin (Methicillin) | Data Included in Report [7] | Not Specified |
This escalating threat underscores the critical need for global initiatives like CARB-X that focus on delivering new therapeutics, preventatives, and diagnostics to outpace the evolution of resistant bacteria.
CARB-X: Strategic Framework and Operational Model
CARB-X is a global non-profit PPP established in 2016 with a mission to accelerate the development of innovative antibacterial products targeting the world's most dangerous drug-resistant bacteria [128] [130]. Its strategy is built on four core pillars: funding, comprehensive support, global scope, and a commitment to stewardship and access.
Funding and Portfolio Strategy
CARB-X operates by pooling funds from a global consortium of governments and foundations. As of 2023, this includes significant multi-year commitments from the UK government (£24 million), the German government (€39 million), and the Canadian government (CAD $6.3 million), alongside funding from the US government, Wellcome Trust, and the Bill & Melinda Gates Foundation [128]. This funding is deployed as non-dilutive grants to product developers worldwide, with 95% of the funding directed to these developers rather than operational overhead [128].
The portfolio is strategically curated to address gaps in the antibacterial pipeline. CARB-X funds products—including antibiotics, vaccines, and rapid diagnostics—that target bacteria on the CDC's Antibiotic Resistant Threats list or the WHO's Priority Bacterial Pathogens list [127] [130]. A key strategic focus is on performance characteristics that enable broad global use, such as developing oral antibiotics to replace intravenous formulations, which can reduce healthcare costs and increase access in low-resource settings [127].
Table 2: CARB-X Funding and Portfolio Impact (2016-2025)
| Metric | Pre-2024 Figure | 2024-2025 Developments |
|---|---|---|
| Total Projects Funded | 96 projects [127] | 118 R&D projects (as of 2025) [130] |
| Projects in Clinical Trials | 18 projects advanced to or completed clinical trials [127] | 22 projects entered or completed first-in-human trials [130] |
| Products on the Market | 2 diagnostics reached the market [127] | 3 products on the market [130] |
| Global Reach | Applications from 41 countries [130] | 2025 funding round open for Gram-negative therapeutics and typhoid diagnostics [131] |
Comprehensive Support and Portfolio Acceleration
Beyond funding, CARB-X provides awardees with extensive scientific, business, and regulatory support through its "Comprehensive Support" model [130]. This is augmented by Portfolio Acceleration Tools (PATs), which are initiatives designed to identify and overcome common development roadblocks across multiple projects, creating efficiencies that benefit the entire AMR R&D community [130].
Commitment to Global Access
A foundational requirement for all CARB-X funding is the development of a Stewardship & Access Plan [128] [130]. These plans ensure that successful products are made available and appropriate for use by patients worldwide, including those in low- and middle-income countries (LMICs) who bear the highest burden of AMR [128].
Case Study: Exploiting Bacterial Resistance Mechanisms inM. abscessus
The "antibiotic nightmare" bacterium Mycobacterium abscessus exemplifies the intrinsic resistance that complicates treatment, particularly in immunocompromised patients [20]. Its resistance is orchestrated by the WhiB7 resistome, a master genetic regulator that controls the expression of over 100 proteins involved in antimicrobial resistance in response to ribosomal stress [20].
Experimental Protocol: "Resistance Hacking" with a Florfenicol Prodrug
A proof-of-concept study from St. Jude Children's Research Hospital demonstrated a novel strategy to turn this resistance mechanism against the bacterium itself [20]. The following workflow and subsequent diagram outline the key experimental steps and the mechanism of action.
Experimental Workflow:
- Compound Screening & Anomalous Observation: Researchers screened structurally modified analogs of chloramphenicol/florfenicol against wild-type M. abscessus and a WhiB7-knockout strain. The lead florfenicol analog showed strong activity against the wild-type but no effect on the ΔWhiB7 mutant, indicating its activity was dependent on the resistance system [20].
- Mode of Action Elucidation: Biochemical assays and genetic analyses confirmed the analog was a prodrug, inactive until modified within the bacterial cell. The enzyme Eis2, whose production is directly induced by WhiB7, was identified as the activator of the prodrug [20].
- Validation of Perpetual Cascade: Researchers validated the self-amplifying cycle. The activated drug inhibits the ribosome, which further activates WhiB7, leading to increased Eis2 production and, consequently, even more drug activation [20].
- Safety and Specificity Profiling: The prodrug's lack of initial activity was tested against mammalian mitochondria, revealing avoided mitochondrial toxicity, a common side effect of phenicol antibiotics, and confirming specificity to mycobacterial species [20].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating Resistance Mechanisms in M. abscessus
| Research Reagent / Tool | Function in the Experimental Protocol |
|---|---|
| WhiB7-Knockout Mutant Strain | Serves as a critical control to confirm that the antibiotic's activity is dependent on the WhiB7-mediated resistance pathway. Its use revealed the anomalous prodrug activation [20]. |
| Structurally Modified Florfenicol Prodrug | The inactive investigational compound that is selectively activated by the bacterial resistance enzyme Eis2, forming the basis of the "resistance hacking" strategy [20]. |
| Eis2 Enzyme Assays | In vitro biochemical kits or purified components used to demonstrate that the Eis2 enzyme directly metabolizes the prodrug into its active, ribosome-inhibiting form [20]. |
| Ribosomal Stress Assays | Methods (e.g., rRNA expression analysis, reporter gene assays) to quantify the activation level of the WhiB7 regulon in response to the active antibiotic [20]. |
Analysis of Impact and Future Directions
Quantifiable Impact on the Antibacterial Pipeline
CARB-X has demonstrably altered the early-stage R&D landscape for AMR. From its inception in 2016 through 2025, CARB-X has supported 118 R&D projects, of which 22 have entered or completed first-in-human clinical trials, and 3 have reached the market [130]. This represents a significant contribution to a global pipeline that was described as "dangerously thin" just a decade ago [128]. Its model of funding and comprehensive support has proven attractive to innovators, with the program receiving over 1,773 expressions of interest from 41 countries [130].
Future Research and Funding Priorities
The strategic focus of global AMR initiatives continues to evolve. CARB-X's 2025 funding round prioritizes two key areas: direct-acting small molecule therapeutics for Gram-negative bacteria (specifically Pseudomonas aeruginosa) and rapid diagnostics for typhoid fever in low-resource settings [131]. This aligns with the WHO report highlighting Gram-negative pathogens as the greatest threat [7]. Furthermore, the 2025 launch of the "Gram-Negative Antibiotic Discovery Innovator (Gr-ADI)" by the Novo Nordisk Foundation, Wellcome, and the Gates Foundation seeks to fund foundational research on new chemical start points and target selection, indicating a growing emphasis on overcoming the fundamental scientific challenges in antibiotic discovery [131].
Global public-private partnerships like CARB-X represent a formidable and essential response to the complex challenge of antimicrobial resistance. By providing targeted funding, expert support, and enforcing global access principles, CARB-X has successfully accelerated a diverse portfolio of innovative antibacterial products toward clinical use. The concurrent advancement of novel scientific strategies, such as "resistance hacking" demonstrated in M. abscessus, illustrates how a deeper understanding of bacterial resistance mechanisms can be leveraged to develop smarter, more effective therapeutics. The continued success of these initiatives depends on sustained global investment and scientific ingenuity to ensure the pipeline of life-saving antibacterial products can outpace the relentless evolution of resistance.
Conclusion
Intrinsic antibiotic resistance represents a formidable and escalating global health threat, underscored by the WHO's 2024 report of a 40% jump in resistant infections. Confronting this 'silent pandemic' demands a multifaceted, global strategy that integrates foundational research into resistance mechanisms with innovative methodological approaches for drug discovery. Success hinges on overcoming significant economic and diagnostic hurdles through enhanced surveillance, robust policy interventions, and international collaboration. Future efforts must prioritize the development of a sustainable pipeline for novel antimicrobials and rapid diagnostics, firmly guided by a One Health framework that connects human, animal, and environmental health. The engagement of researchers, policymakers, and funders is paramount to mitigate the profound clinical and economic impacts projected for the coming decades.
References
- 1. An Overview of the Epidemiology of Multidrug Resistance and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472688/]
- 2. Antimicrobial resistance [https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance]
- 3. Intrinsic Resistance - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/intrinsic-resistance]
- 4. Resistance mechanisms – Antibiotic resistance – ReAct [https://www.reactgroup.org/toolbox/understand/antibiotic-resistance/resistance-mechanisms-in-bacteria/]
- 5. An overview of the antimicrobial resistance mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604941/]
- 6. Antibiotic Resistance - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK513277/]
- 7. WHO warns of widespread resistance to common ... [https://www.who.int/news/item/13-10-2025-who-warns-of-widespread-resistance-to-common-antibiotics-worldwide]
- 8. Addressing the global challenge of bacterial drug resistance [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1517772/full]
- 9. Outer Membrane Permeability and Antibiotic Resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2696358/]
- 10. Role of bacterial efflux pumps in antibiotic resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10268834/]
- 11. Efflux pump [https://en.wikipedia.org/wiki/Efflux_pump]
- 12. The influence of efflux pump, outer membrane permeability ... [https://www.sciencedirect.com/science/article/pii/S1876034124002788]
- 13. Synergy between Active Efflux and Outer Membrane ... [https://pubmed.ncbi.nlm.nih.gov/29089426/]
- 14. Quantitative systems-based prediction of antimicrobial ... [https://www.nature.com/articles/s41540-023-00304-6]
- 15. Ecological and evolutionary mechanisms driving within- ... [https://www.nature.com/articles/s41579-024-01041-1]
- 16. About Antimicrobial Resistance [https://www.cdc.gov/antimicrobial-resistance/about/index.html]
- 17. Evaluation of Antibiotic Resistance Mechanisms in Gram ... [https://www.mdpi.com/2079-6382/12/11/1590]
- 18. Molecular Mechanisms of Antibiotic Resistance in ... [http://www.euti.org/journal/view.php?number=441]
- 19. Antimicrobial Multidrug Resistance and Mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12646968/]
- 20. Approach to combat antibiotic resistance turns bacterium's ... [https://www.stjude.org/media-resources/news-releases/2025-medicine-science-news/approach-to-combat-antibiotic-resistance-turns-bacteriums-genes-against-it.html]
- 21. Bioinspired Nanoplatforms: Polydopamine and Exosomes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12197175/]
- 22. Analysis of multiple bacterial species and antibiotic classes ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3001579]
- 23. Bacterial Antibiotic Resistance: The Most Critical Pathogens [https://pmc.ncbi.nlm.nih.gov/articles/PMC8541462/]
- 24. The WHO's critical bacteria list: scientific response eight ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1633382/full]
- 25. Trends in the Antimicrobial Resistance Pattern of Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566077/]
- 26. WHO releases new reports on new tests and treatments in ... [https://www.who.int/news/item/02-10-2025-who-releases-new-reports-on-new-tests-and-treatments-in-development-for-bacterial-infections]
- 27. Origins and Evolution of Antibiotic Resistance - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2937522/]
- 28. Ecology and evolution of antimicrobial resistance in ... [https://www.nature.com/articles/s41396-020-00832-7]
- 29. Comparative Analysis of Concentration and Quantification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566704/]
- 30. Quantitative comparison of HT-qPCR/16S rRNA ... [https://www.sciencedirect.com/science/article/abs/pii/S0304389425028237]
- 31. Reservoirs of antimicrobial resistance in the context of One Health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10265130/]
- 32. Reservoirs of antimicrobial resistance in the context of One Health - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1369527423000280]
- 33. Antibiotic resistance surges globally, UN health agency warns [https://news.un.org/en/story/2025/10/1166087]
- 34. CDC Report Finds Sharp Rise in Dangerous Drug ... [https://www.cdc.gov/media/releases/2025/2025-cdc-report-finds-sharp-rise-in-dangerous-drug-resistant-bacteria.html]
- 35. The role of biofilms as environmental reservoirs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4628128/]
- 36. Environmental Biofilms as Reservoirs for Antimicrobial ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.766242/full]
- 37. Potential reservoirs of antimicrobial resistance in livestock ... [https://pubmed.ncbi.nlm.nih.gov/36781130/]
- 38. Environment, animals, and food as reservoirs of antibiotic- ... [https://pubmed.ncbi.nlm.nih.gov/38548016/]
- 39. Frontiers | Editorial: “One Health” approach for revealing reservoirs and transmission of antimicrobial resistance, volume II [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1170407/full]
- 40. Intrinsic antibiotic resistance: Mechanisms, origins ... [https://www.sciencedirect.com/science/article/abs/pii/S1438422113000246]
- 41. Evaluation of whole-genome sequencing protocols for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11923095/]
- 42. Antibiotic Resistance Mechanisms in Bacteria [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.02928/full]
- 43. Genomic and metagenomic approaches for predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6692204/]
- 44. Metagenomic Approaches to Analyze Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC7848172/]
- 45. Application to an urban river in Beijing [https://www.sciencedirect.com/science/article/pii/S0269749118341083]
- 46. Metagenomic co-assembly uncovers mobile antibiotic ... [https://www.nature.com/articles/s43247-025-02381-3]
- 47. A three-dimensional high assay identifies throughput ... novel [https://www.nature.com/articles/s44259-025-00110-6?error=cookies_not_supported&code=e2e4418f-4127-4ccb-8c8c-c50b77aa9128]
- 48. C. elegans in high - throughput for anti-infective screens ... compounds [https://pmc.ncbi.nlm.nih.gov/articles/PMC6463281/]
- 49. High throughput screening identifies potential inhibitors ... [https://www.nature.com/articles/s41598-025-91410-4]
- 50. High-throughput computational-experimental screening ... [https://www.nature.com/articles/s41524-021-00605-6]
- 51. A protocol for high-throughput screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10365952/]
- 52. Quantitative and organismic biology in antibiotic resistance [https://pubmed.ncbi.nlm.nih.gov/38768878/]
- 53. Phage Therapy as a Novel Alternative to Antibiotics Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562026/]
- 54. Phage Therapy: The Future of Fighting Antibiotic Resistance [https://norgenbiotek.com/blog/phage-therapy-future-fighting-antibiotic-resistance?srsltid=AfmBOor37e7Wz_g94EK-ZyvdjR2GaXwT3dicL9_f_AX_ggaQ5rf1uk8j]
- 55. Personalized inhaled bacteriophage therapy for treatment ... [https://www.nature.com/articles/s41591-025-03678-8]
- 56. CRISPR-Cas mediated targeting of resistance genes for ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025097375]
- 57. Harnessing bacterial immunity: CRISPR-Cas system as a ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1588446/full]
- 58. A CRISPR-Cas9 system protecting E. coli against ... [https://www.nature.com/articles/s41598-025-85334-2]
- 59. Anti-Virulence Therapeutic Strategies Against Bacterial ... [https://www.mdpi.com/2248-2997/12/2/262]
- 60. Alternatives to antibiotics in the fight against superbugs [https://www.weforum.org/stories/2025/10/this-regulatory-shift-is-unlocking-alternatives-to-antibiotics-in-the-fight-against-superbugs/]
- 61. Antibiotics re-booted—time to kick back against drug ... [https://www.nature.com/articles/s44259-025-00096-1]
- 62. A systematic review on natural products with antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12211454/]
- 63. Natural Products in the Fight Against Antibiotic Resistance [https://www.frontiersin.org/research-topics/59102/natural-products-in-the-fight-against-antibiotic-resistance-addressing-the-who-priority-pathogens]
- 64. Exploring Phytochemicals for Combating Antibiotic Resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8334005/]
- 65. Review on plant antimicrobials: a mechanistic viewpoint [https://aricjournal.biomedcentral.com/articles/10.1186/s13756-019-0559-6]
- 66. Antibiotic Resistance: A Genetic and Physiological Perspective [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579171/]
- 67. Combining Advanced Therapies with Alternative Treatments [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114861/]
- 68. 世卫组织警告称全球普遍存在常用抗生素耐药性 [https://www.who.int/zh/news/item/13-10-2025-who-warns-of-widespread-resistance-to-common-antibiotics-worldwide]
- 69. Editorial: Advances in new combinational therapies for ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1709379/full]
- 70. UC San Diego Researchers Expand Virus-Based Treatment ... [https://today.ucsd.edu/story/uc-san-diego-researchers-expand-virus-based-treatment-options-for-antibiotic-resistant-infections]
- 71. Synergistic targeting of immunologic pathways to empower ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9478166/]
- 72. There is no market for new antibiotics: this allows an open ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8237369/]
- 73. Delinked Payment Systems and Insurance Value [https://link.springer.com/article/10.1007/s41669-025-00591-1]
- 74. Bridging the fair share gap for antibacterial innovation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452676/]
- 75. Acquired Bacterial Resistance to Antibiotics and ... [https://www.mdpi.com/2079-6382/14/3/222]
- 76. Biofilms and multidrug resistance: an emerging crisis and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12237878/]
- 77. Biofilms: structure, resistance mechanism, emerging control ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00094g]
- 78. Harnessing AI to Revolutionize Antibiotic Discovery [https://asm.org/articles/2025/august/ai-next-frontier-antibiotic-discovery]
- 79. Exploring the Need for Rapid Diagnostics - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK593538/]
- 80. Clinical Diagnostics of Bacterial Infections and Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10135054/]
- 81. Molecular Diagnostics for Fighting Antibiotic Resistance [https://www.thermofisher.com/blog/clinical-conversations/molecular-daignostics-precision-medicine-antibiotic-resistance/]
- 82. Deep learning reveals antibiotics in the archaeal proteome [https://www.nature.com/articles/s41564-025-02061-0]
- 83. A Promising New Tool to Combat Antibiotic-Resistant ... [https://irp.nih.gov/blog/post/2025/08/a-promising-new-tool-to-combat-antibiotic-resistant-bacteria]
- 84. Development of a Protocol for Predicting Bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4375328/]
- 85. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 86. SHEA/IDSA Clinical Practice Guidelines for Implementing ... [https://www.idsociety.org/practice-guideline/implementing-an-ASP/]
- 87. Antimicrobial Stewardship Program [https://www.unmc.edu/intmed/divisions/id/asp/index.html]
- 88. Core Elements of Antibiotic Stewardship [https://www.cdc.gov/antibiotic-use/hcp/core-elements/index.html]
- 89. Interventions to optimize antimicrobial stewardship - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495515/]
- 90. Antibiotic resistance patterns of environmental bacteria ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1640369/full]
- 91. Antimicrobial resistance: Impacts, challenges, and future ... [https://www.sciencedirect.com/science/article/pii/S2949916X24000343]
- 92. New antibiotic that kills drug-resistant bacteria discovered ... [https://www.nature.com/articles/d41586-025-00945-z]
- 93. Strategies for combating antibiotic resistance in bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10846525/]
- 94. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 95. Recent Advances in Bacterial Persistence Mechanisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10531727/]
- 96. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 97. Dynamics of bacterial biofilm development imaged using ... [https://www.sciencedirect.com/science/article/pii/S2405580825002146]
- 98. Targeting bacterial persistence with bacteriophages [https://www.sciencedirect.com/science/article/abs/pii/S0042682225002624]
- 99. Distribution and Antibiotic Resistance Analysis of 13,048 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11869759/]
- 100. A systematic review and critical assessment of incentive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4775540/]
- 101. A model of R&D valuation and the design of research ... [https://www.sciencedirect.com/science/article/abs/pii/S0167668708000577]
- 102. Progress (at least some!) towards a global pull incentive [https://amr.solutions/2025/09/15/progress-at-least-some-towards-a-global-pull-incentive/]
- 103. Quantitative measures of health policy implementation ... [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-020-01007-w]
- 104. Global Antimicrobial Resistance and Use Surveillance ... [https://www.who.int/initiatives/glass]
- 105. Global antibiotic resistance surveillance report 2025 [https://www.who.int/publications/i/item/9789240116337]
- 106. ICARS welcomes the new WHO GLASS report on global ... [https://icars-global.org/glass-report-2025/]
- 107. WHO warns of widespread resistance to common ... [https://www.paho.org/en/news/13-10-2025-who-warns-widespread-resistance-common-antibiotics-worldwide]
- 108. A systematic review on natural products with antimicrobial ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02717-x]
- 109. Natural antibiotics against antimicrobial resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11405619/]
- 110. Evaluation of Antibiotic Resistance Mechanisms in Gram ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10668847/]
- 111. Evaluation of Antibiotic Resistance Mechanisms in Gram ... [https://www.mdpi.com/2079-6382/13/12/1197]
- 112. Resistance of Gram-Positive Bacteria to Current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7356343/]
- 113. Resistance of Gram-Negative Bacteria to Current Antibacterial Agents and Approaches to Resolve It - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7144564/]
- 114. Newly developed antibiotics against multidrug-resistant ... [https://pubmed.ncbi.nlm.nih.gov/40172627/]
- 115. Comparison of the antibiotic resistance mechanisms in a gram-positive and a gram-negative bacterium by gene networks analysis | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0311434]
- 116. Susceptibility and resistance of Gram-negative bacteria to ... [https://www.frontiersin.org/journals/antibiotics/articles/10.3389/frabi.2025.1615821/full]
- 117. Emerging antimicrobial therapies for Gram-negative ... [https://www.nature.com/articles/s44259-025-00087-2]
- 118. The global economic burden of antibiotic-resistant infections ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182023/]
- 119. McMaster researchers discover new class of antibiotics [https://healthsci.mcmaster.ca/a-breakthrough-moment-mcmaster-researchers-discover-new-class-of-antibiotics/]
- 120. Antimicrobial Resistance Facts and Stats [https://www.cdc.gov/antimicrobial-resistance/data-research/facts-stats/index.html]
- 121. Comparative meta-analysis of antimicrobial resistance from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9803827/]
- 122. The global economic burden of antibiotic-resistant ... [https://immunizationeconomics.org/recent-activity/2025/6/23/the-global-economic-burden-of-antibiotic-resistant-infections-and-the-potential-impact-of-bacterial-vaccines-a-modelling-study/]
- 123. CDC Partners Estimate Healthcare Cost of Antimicrobial ... [https://www.cdc.gov/antimicrobial-resistance/stories/partner-estimates.html]
- 124. Visualization of Bacterial Resistance using Fluorescent ... [https://pubmed.ncbi.nlm.nih.gov/32176211/]
- 125. Strategies for robust, accurate, and generalizable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12607264/]
- 126. From wastewater to resistance: characterization of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1612534/full]
- 127. CARB-X funds the Myers Research Group to develop ... [https://carb-x.org/carb-x-news/carb-x-funds-myers-research-group/]
- 128. CARB-X Receives Global Funding in Fight Against ... [https://www.bu.edu/law/record/articles/2023/carb-x-fight-against-antimicrobial-resistance/]
- 129. Study: Antibiotic resistance is rising at an alarming rate [https://www.npr.org/sections/goats-and-soda/2025/10/15/g-s1-93449/antibiotic-resistance-bacteria]
- 130. Our Strategy [https://carb-x.org/about/our-strategy/]
- 131. CARB-X announces its 2025 funding round [https://amr.solutions/2025/02/26/carb-x-announces-its-2025-funding-round/]