Intrinsic Antibiotic Resistance: Core Mechanisms, Research Methodologies, and Therapeutic Breakthroughs
This article provides a comprehensive analysis of the fundamental mechanisms underpinning intrinsic antibiotic resistance, a critical and growing challenge in clinical microbiology and drug development.
Intrinsic Antibiotic Resistance: Core Mechanisms, Research Methodologies, and Therapeutic Breakthroughs
Abstract
This article provides a comprehensive analysis of the fundamental mechanisms underpinning intrinsic antibiotic resistance, a critical and growing challenge in clinical microbiology and drug development. Aimed at researchers, scientists, and pharmaceutical professionals, it explores the innate, chromosomally encoded defenses that render bacterial species impervious to certain antimicrobial agents from the outset. The scope ranges from foundational concepts—detailing the roles of impermeable membranes, constitutive efflux pumps, and innate enzymatic inactivation—to advanced methodological approaches for studying these barriers. It further investigates innovative strategies to circumvent resistance, including antibiotic potentiators and structure-based drug design, and concludes with a comparative evaluation of resistance across priority pathogens and future directions for revitalizing the antibacterial pipeline. By synthesizing current research and emerging trends, this review serves as a vital resource for navigating the complexities of intrinsic resistance and developing next-generation therapeutics.
The Innate Fortress: Deconstructing Fundamental Mechanisms of Intrinsic Resistance
Antimicrobial resistance (AMR) represents a severe global health threat, projected to cause 10 million deaths annually by 2050 if left unaddressed [1]. A comprehensive understanding of resistance mechanisms is fundamental to combating this crisis. This whitepaper provides an in-depth technical analysis of the core distinctions between intrinsic and acquired resistance, with particular focus on the interplay between constitutive and inducible traits. We explore the genetic basis, molecular mechanisms, and experimental approaches for investigating these resistance forms, framing our discussion within the context of intrinsic antibiotic resistance research. For researchers and drug development professionals, we present quantitative data, detailed methodologies, and essential research tools to advance the development of novel therapeutic strategies against resistant pathogens.
Antibiotic resistance occurs when bacteria evolve mechanisms to evade the effect of antimicrobial agents [2]. This multidrug-resistant (MDR) phenotype undermines decades of progress in infectious disease control and threatens modern medical procedures [1]. Resistance mechanisms are broadly categorized as either intrinsic or acquired, based on their genetic origin and evolutionary history.
Simultaneously, resistance traits can be classified by their expression patterns as constitutive (always expressed) or induced (expressed only upon encountering specific stimuli, such as an antibiotic) [2]. Understanding the relationship between these classifications is crucial for designing effective countermeasures. The intrinsic resistome—the collection of all chromosomally encoded elements that contribute to intrinsic resistance—has emerged as a promising target for novel antibiotics and resistance breakers [3] [4].
Defining Resistance Categories
Intrinsic vs. Acquired Resistance
Table 1: Fundamental Characteristics of Intrinsic and Acquired Resistance
| Feature | Intrinsic Resistance | Acquired Resistance |
|---|---|---|
| Genetic Basis | Chromosomal genes present in all strains of a bacterial species [2] [4] | Horizontal gene transfer (plasmids, transposons) or chromosomal mutations [5] [2] |
| Prevalence | Universal within a species; independent of antibiotic exposure [4] | Variable; depends on selective pressure and transmission [5] |
| Evolutionary Origin | Predates antibiotic chemotherapy; ancient [4] | Arises during antibiotic therapy or through contact with resistant bacteria [2] |
| Examples | Gram-negative outer membrane; efflux pumps in Pseudomonas aeruginosa [5] [4] | MRSA (mecA gene); ESBL-producing E. coli [1] [5] |
Intrinsic resistance refers to the innate ability of a bacterial species to withstand antibiotic action due to its inherent structural or functional characteristics [2] [6]. This resistance is genetically hardwired, independent of horizontal gene transfer or previous antibiotic exposure [4]. The conventional example is the multi-drug resistant phenotype exhibited by Gram-negative bacteria, attributed to the presence of a protective outer membrane and constitutive expression of efflux pumps [4].
Acquired resistance develops when previously susceptible bacteria gain the ability to survive antibiotic treatment through genetic changes [2] [6]. This can occur via spontaneous mutations in chromosomal genes or through horizontal acquisition of resistance genes on mobile genetic elements such as plasmids, transposons, or integrons [5] [2]. A prominent example is methicillin-resistant Staphylococcus aureus (MRSA), which acquires the mecA gene encoding an altered penicillin-binding protein (PBP2a) with low affinity for β-lactam antibiotics [1] [5].
Constitutive vs. Induced Resistance
Table 2: Comparison of Constitutive and Induced Resistance Traits
| Characteristic | Constitutive Resistance | Induced Resistance |
|---|---|---|
| Expression Pattern | Constant, baseline expression [2] | Triggered by environmental signals (e.g., antibiotic presence) [2] |
| Genetic Regulation | Not subject to conditional regulation | Tightly regulated by specific inducer systems |
| Energy Cost | Constant metabolic burden [7] | Temporary burden only during induction |
| Response Time | Immediate protection | Delayed protection until induction occurs |
| Examples | Porins in Gram-negative outer membrane [4] | WhiB7 regulon in Mycobacterium abscessus [8] |
Constitutive resistance traits are consistently expressed at a baseline level, providing constant protection regardless of environmental conditions [2]. From an evolutionary perspective, constitutive expression is maintained when the threat of antibiotic exposure is constant or unpredictable, justifying the continuous metabolic expenditure [7].
Induced resistance traits are expressed only when triggered by specific environmental signals, such as antibiotic exposure [2]. This inducible expression provides an adaptive advantage by minimizing metabolic costs in the absence of threats while enabling rapid protection when challenged [7]. A sophisticated example is the WhiB7 "resistome" in Mycobacterium abscessus, a master regulator activated by ribosomal stress that controls over 100 proteins involved in antimicrobial resistance when antibiotics target the ribosome [8].
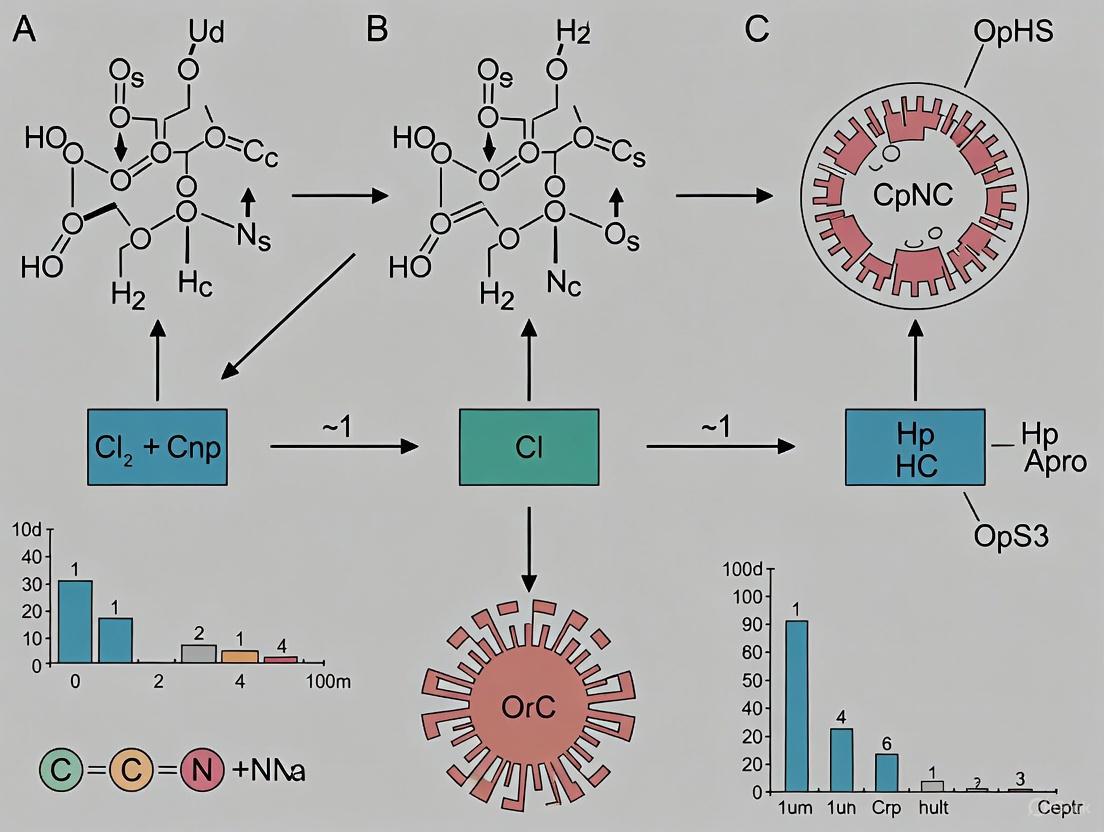
Diagram 1: Relationship between resistance classification systems. The conceptual frameworks of intrinsic/acquired and constitutive/induced represent different axes for classifying resistance mechanisms, with significant overlap between categories.
Molecular Mechanisms of Resistance
Fundamental Resistance Mechanisms
Bacteria employ four primary biochemical strategies to circumvent antibiotic activity, which can operate through either constitutive or induced systems:
Enzymatic Inactivation or Modification: Production of enzymes that degrade or modify antibiotics, rendering them ineffective [1] [5]. β-lactamases represent the most prominent example, with extended-spectrum β-lactamases (ESBLs) constituting a major clinical concern [5]. Expression can be constitutive or induced upon antibiotic exposure.
Target Site Modification: Alteration of antibiotic binding sites through mutation or enzymatic modification [1] [5]. In MRSA, the acquired mecA gene constitutively produces PBP2a, an alternative penicillin-binding protein with low affinity for β-lactams [5].
Reduced Permeability or Enhanced Efflux: Decreased antibiotic accumulation via impaired uptake or active efflux [1] [5] [4]. Gram-negative bacteria intrinsically resist many antibiotics due to their outer membrane barrier and constitutively expressed efflux pumps like AcrAB-TolC in E. coli [3] [4].
Bypass Pathways or Target Protection: Development of alternative metabolic pathways or production of proteins that protect antibiotic targets [1].
The Intrinsic Resistome of Gram-Negative Bacteria
The intrinsic resistome of Gram-negative pathogens presents a formidable clinical challenge due to its multi-layered architecture:
Outer Membrane Permeability Barrier: The Gram-negative outer membrane, with its asymmetric lipid bilayer containing lipopolysaccharide (LPS), functions as a formidable constitutive barrier to many antibiotics [4]. The flexibility and packing of LPS molecules determine membrane fluidity and permeability, with tighter packing reducing penetration of hydrophobic compounds [4]. Porins facilitate selective uptake of nutrients and small molecules, but their expression and characteristics can limit antibiotic penetration [4].
Active Efflux Systems: Resistance-nodulation-division (RND) superfamily efflux pumps, such as AcrAB-TolC in E. coli and MexAB-OprM in P. aeruginosa, contribute substantially to intrinsic resistance through constitutive expression [5] [4]. These tripartite systems span both membrane layers and actively extrude diverse antibiotics, often exhibiting broad substrate specificity [4]. Research demonstrates that knocking out efflux pump genes like acrB creates hypersusceptibility to multiple antibiotic classes [3].
Table 3: Quantitative Impact of Intrinsic Resistance Mechanisms in E. coli
| Genetic Modification | Antibiotic Tested | Effect on Susceptibility | Key Findings | Experimental Method |
|---|---|---|---|---|
| ΔacrB (efflux pump) | Trimethoprim | Hypersusceptibility | Most compromised in evolving resistance; promising for "resistance proofing" [3] | Genome-wide knockout screen |
| ΔrfaG (cell envelope biogenesis) | Trimethoprim | Hypersusceptibility | High drug regimes drove knockout to extinction more frequently than wild type [3] | Genome-wide knockout screen |
| ΔlpxM (cell envelope biogenesis) | Trimethoprim | Hypersusceptibility | Adapted at sub-inhibitory concentrations via target mutations [3] | Genome-wide knockout screen |
Experimental Approaches and Methodologies
Genome-Wide Screening for Intrinsic Resistance Factors
Objective: Identify chromosomal genes contributing to intrinsic antibiotic resistance through systematic screening of mutant libraries.
Protocol (adapted from Balachandran et al., 2025 [3]):
- Library Preparation: Utilize a comprehensive single-gene knockout collection (e.g., Keio collection for E. coli with ~3,800 mutants).
- Growth Conditions: Culture knockout strains in duplicate in LB media supplemented with antibiotic at predetermined IC₅₀ values alongside antibiotic-free controls.
- Phenotypic Assessment: Measure optical density at 600 nm (OD₆₀₀) after incubation period to quantify growth inhibition.
- Data Analysis:
- Calculate fold growth relative to wild type for each knockout.
- Generate Gaussian distribution of drug susceptibilities with mean ≈1.
- Classify hypersensitive mutants as those showing growth lower than two standard deviations from the median in antibiotic media but normal growth in control media.
- Functional Enrichment: Categorize identified genes into functional pathways (e.g., cell envelope biogenesis, membrane transport, information transfer) using databases such as Ecocyc.
Key Outputs: Identification of drug-specific and drug-agnostic gene targets; revelation of network interactions within the intrinsic resistome.
Experimental Evolution for Resistance Proofing
Objective: Evaluate the potential of intrinsic resistance targets to prevent or delay evolution of antibiotic resistance.
Protocol (adapted from Balachandran et al., 2025 [3]):
- Strain Selection: Compare wild-type and knockout strains (e.g., ΔacrB, ΔrfaG, ΔlpxM) hypersusceptible to target antibiotic.
- Evolution Conditions: Propagate strains in serial passages under high and sub-inhibitory antibiotic concentrations.
- Monitoring: Track population survival and extinction events across passages.
- Genomic Analysis: Sequence adapted strains to identify resistance-conferring mutations (e.g., in folA for trimethoprim resistance).
- Comparison: Assess differential adaptability between wild-type and knockout strains.
Key Outputs: Determination of which intrinsic resistance mechanisms, when targeted, most effectively constrain evolutionary pathways to resistance; identification of compensatory mutations.
Diagram 2: Experimental workflow for identifying and validating intrinsic resistance targets. The pipeline integrates genome-wide screening with experimental evolution to pinpoint targets with potential for resistance-proofing therapeutic strategies.
Research Tools and Reagents
Table 4: Essential Research Reagent Solutions for Intrinsic Resistance Studies
| Reagent / Tool | Function / Application | Example Use Case | Key Features |
|---|---|---|---|
| Keio Knockout Collection | Genome-wide single-gene knockout library for E. coli | Systematic identification of intrinsic resistance genes [3] | ~3,800 non-essential gene knockouts; systematic coverage |
| Conditional Expression Systems | Inducible control of gene expression | Study essential resistance genes; mimic induction [3] | Tight regulation; tunable expression levels |
| Efflux Pump Inhibitors | Chemical inhibition of efflux activity | Potentiate antibiotic efficacy; study efflux contributions [3] | e.g., Chlorpromazine, Piperine; mechanism validation |
| High-Throughput Screening | Automated susceptibility testing | Parallel assessment of mutant libraries [3] | 96-well/384-well formats; robotic automation |
| Genome Sequencing | Identification of resistance mutations | Track evolutionary adaptation [3] | Whole-genome or targeted sequencing |
| Transcriptomic Analysis | Global gene expression profiling | Identify induced resistance regulons [8] | RNA-seq; microarray analysis |
Emerging Concepts and Research Directions
Resistance Hacking: Exploiting Resistance Mechanisms
A groundbreaking approach termed "resistance hacking" involves structurally modifying antibiotics to exploit bacterial resistance mechanisms against themselves [8]. Proof-of-concept research demonstrates that a modified version of florfenicol exploits the WhiB7-induced Eis2 protein in Mycobacterium abscessus to perpetually amplify the antibiotic effect [8]. Specifically, the prodrug is activated by Eis2, whose expression increases as WhiB7 is activated, creating a perpetual cascade that continuously amplifies antibiotic concentration [8].
This approach represents a paradigm shift from circumventing resistance to weaponizing the resistance machinery itself, offering species-specific targeting that minimizes collateral damage to the host microbiome and reduces toxicity [8].
Evolutionary Constraints and Resistance Proofing
Research increasingly focuses on "resistance proofing" strategies that target intrinsic resistance mechanisms to constrain bacterial evolvability [3]. Studies comparing different hypersusceptible E. coli knockouts reveal that ΔacrB (efflux-deficient) strains are most compromised in their ability to evolve resistance, establishing efflux inhibition as a promising resistance-proofing strategy [3].
However, at sub-inhibitory antibiotic concentrations, hypersusceptible knockouts can adapt through mutations in drug-specific resistance pathways rather than compensatory evolution, frequently involving upregulation of the drug target [3]. This highlights the importance of considering evolutionary dynamics when targeting intrinsic resistance mechanisms.
Quantitative Prediction of Resistance Evolution
Systems biology approaches integrating quantitative models with multiscale data from microbial evolution experiments show promise for predicting AMR evolution [9]. The predictability of an evolutionary process can be defined by the existence of a probability distribution of outcomes, while repeatability relates to the likelihood of specific events within that distribution [9].
Measures such as Shannon entropy can quantify evolutionary repeatability, with higher entropy indicating greater uncertainty in evolutionary outcomes [9]. Research indicates that larger selection pressures generate more repeatable evolution, and resistance evolution demonstrates considerable predictability at the phenotypic level despite genetic heterogeneity [9].
The distinction between intrinsic and acquired resistance, coupled with the constitutive versus induced expression of resistance traits, provides essential frameworks for understanding bacterial adaptation to antibiotics. The intrinsic resistome represents a complex network of chromosomal elements that contribute to baseline resistance, extending beyond the traditional concepts of permeability barriers and efflux pumps.
Experimental approaches combining genome-wide screens with experimental evolution offer powerful methodologies for identifying and validating targets within the intrinsic resistome. Emerging strategies such as resistance hacking and resistance proofing leverage these insights to develop novel therapeutic interventions that constrain evolutionary pathways to resistance.
For researchers and drug development professionals, targeting the intrinsic resistome offers the promise of rejuvenating existing antibiotics against resistant pathogens while imposing evolutionary constraints that delay the emergence of new resistance mechanisms. As our understanding of the intricate relationships between constitutive and induced resistance deepens, so too will our capacity to develop innovative solutions to the antimicrobial resistance crisis.
The outer membrane (OM) of Gram-negative bacteria constitutes a formidable and sophisticated barrier that is fundamental to the organism's intrinsic resistance to many antimicrobial agents [10] [11]. This membrane operates as a highly selective filter, permitting the influx of essential nutrients while effectively excluding a wide array of harmful substances, including antibiotics [10]. The permeability properties of this barrier are therefore a critical determinant of bacterial susceptibility to antibiotics, a significant challenge in modern healthcare as underscored by the World Health Organization, which identifies antimicrobial resistance (AMR) as a top global health threat [12] [13]. Understanding the molecular basis of the OM's barrier function, encompassing both lipid-mediated and porin-mediated pathways, is essential for researching resistance mechanisms and developing strategies to overcome them [10] [11]. This whitepaper provides an in-depth technical analysis of the OM's role in antibiotic resistance, framed within the broader context of intrinsic resistance research, and is intended for an audience of researchers, scientists, and drug development professionals.
Structural Organization of the Gram-Negative Outer Membrane
The Gram-negative bacterial outer membrane is an asymmetric bilayer, a unique characteristic that is central to its barrier function [10] [11]. The inner leaflet is composed primarily of phospholipids (approximately 80% phosphatidylethanolamine, 15% phosphatidylglycerol, and 5% cardiolipin), while the outer leaflet is predominantly constituted by lipopolysaccharides (LPS) [10]. This asymmetry is a key determinant of the membrane's low permeability.
A typical LPS molecule consists of three domains:
- Lipid A: A glucosamine-based phospholipid that anchors the LPS into the membrane.
- Core Oligosaccharide: A relatively short, branched carbohydrate chain.
- O-Antigen: A distal polysaccharide of variable length that contributes to serotype specificity [10].
The LPS layer is stabilized by strong lateral interactions between molecules and by divalent cations (e.g., Mg²⁺, Ca²⁺) that cross-bridge the anionic groups on adjacent LPS molecules, creating a dense, tightly packed surface [10]. The resulting structure is markedly less fluid and more hydrophobic than a typical phospholipid bilayer, presenting a formidable physical and chemical barrier.
Embedded within this membrane is a diverse array of outer membrane proteins (Omps). Some of the most abundant, such as murein lipoprotein (Lpp) and OmpA, play crucial structural roles in maintaining membrane integrity and cell shape [10] [12]. Among the most functionally significant Omps for antibiotic permeability are the porins, which form water-filled channels for the passive diffusion of hydrophilic molecules [10] [14].
Pathways of Antibiotic Permeation and Associated Resistance Mechanisms
The Lipid Bilayer Pathway and Hydrophobic Antibiotic Resistance
Hydrophobic antibiotics, such as macrolides (e.g., erythromycin), rifamycins, novobiocin, and fusidic acid, traverse the OM by passive diffusion through the lipid bilayer itself [10]. The integrity of the LPS layer is therefore critical in determining resistance to these compounds.
Table 1: Antibiotics Utilizing Lipid-Mediated Uptake and Associated Resistance Modifications
| Antibiotic Class | Examples | Primary Resistance Mechanism | Molecular Consequence |
|---|---|---|---|
| Macrolides | Erythromycin | LPS core truncation; cationic substitution on Lipid A | Altered membrane packing; reduced affinity for cationic agents |
| Rifamycins | Rifampin | Addition of 4-aminoarabinose to Lipid A | Reduction of net negative charge on LPS; tighter packing |
| Aminoglycosides | Gentamicin, Kanamycin | Not fully detailed in search results; likely involves reduced uptake | Likely reduced passive diffusion through bilayer |
| Polymyxins | Polymyxin B, Colistin | Esterification of lipid A phosphates with 4-aminoarabinose or phosphoethanolamine [10] | Decreased negative charge; reduced initial binding and uptake |
Key Resistance Mechanisms:
- Deep Rough LPS Mutants: Mutants with truncated core oligosaccharides ("deep rough" or Re chemotypes) exhibit heightened sensitivity to hydrophobic antibiotics and detergents because their OM is destabilized. This destabilization can lead to the incorporation of phospholipid patches in the outer leaflet, which are significantly more permeable to lipophilic compounds [10].
- Cationic Substitutions: Polymyxin-resistant mutants of Salmonella typhimurium and E. coli modify their Lipid A by adding 4-aminoarabinose or phosphoethanolamine. This modification reduces the net negative charge of the LPS, decreasing electrostatic interactions with cationic antibiotics like polymyxin B and promoting a more closely packed LPS layer, thereby enhancing resistance [10].
- Permeabilizer Action: Compounds like polymyxin B nonapeptide (PMBN) and Tris/EDTA compete with divalent cations for LPS binding sites. Their action disrupts the LPS lattice, destabilizes the membrane, and creates pathways for hydrophobic antibiotics to penetrate, effectively sensitizing the bacteria [10].
The Porin Pathway and Hydrophilic Antibiotic Resistance
Hydrophilic antibiotics, including β-lactams, fluoroquinolones, tetracyclines, and some carbapenems, rely on porin channels to cross the OM [10] [15] [11]. Porins are β-barrel proteins that form trimeric, water-filled pores, facilitating the passive diffusion of small, hydrophilic molecules [14]. Resistance via this pathway often involves alterations that reduce porin-mediated influx.
Table 2: Major Porins and Their Role in Antibiotic Permeability and Resistance
| Porin | Structural Features | Role in Antibiotic Uptake | Documented Resistance Mechanism |
|---|---|---|---|
| OmpF | Larger channel, cation-selective [15] | Major route for β-lactams, fluoroquinolones [15] | Downregulation; mutation of charged residues altering conductance [15] |
| OmpC | Smaller channel, cation-selective [15] | Uptake of β-lactams, fluoroquinolones [15] | Downregulation; mutation of charged periplasmic residues [15] |
| OmpA | Monomeric β-barrel, small channel [10] [12] | Diffusion of small hydrophilic molecules (e.g., β-lactams) [12] | Loss-of-function mutations; altered expression [12] |
| OmpW | Monomeric β-barrel | Implicated in drug transport [12] | Not fully detailed in search results |
| OmpX | Small β-barrel | May contribute to reduced permeability [12] | Overexpression linked to resistance [12] |
Key Resistance Mechanisms:
- Porin Loss or Downregulation: Complete loss or reduced expression of major porins like OmpF and OmpC is a common clinical resistance mechanism. This directly decreases the number of available channels for antibiotic entry [12] [11].
- Porin Mutation: Mutations can alter the physicochemical properties of the porin channel. For instance, mutations in charged residues on the periplasmic surface of OmpC can affect its conductance and ion selectivity, thereby modulating antibiotic permeability [15].
- Ionic Regulation of Porin Permeability: Recent research reveals that porin permeability is dynamically regulated by periplasmic ions. Acidification of the periplasm reduces porin conductance, while an increase in periplasmic K⁺ concentration enhances it. This metabolic control directly impacts antibiotic uptake, explaining, for example, increased ciprofloxacin resistance in bacteria catabolizing lipids [15].
Experimental Methodologies for Assessing Outer Membrane Permeability
Protocol 1: Quantifying Porin Permeability Using Fluorescent Tracers
This protocol utilizes fluorescent probes to measure porin-mediated uptake in real-time, adapted from single-cell imaging studies [15].
Objective: To measure the permeability of the outer membrane via porins in live E. coli cells using the fluorescent glucose analogue 2-NBDG. Principle: 2-NBDG is a hydrophilic molecule whose entry into the cell is mediated by porins. Its accumulation, quantified by fluorescence, serves as a proxy for porin permeability [15].
Materials:
- Bacterial Strain: Wild-type and porin mutant (e.g., ΔompCΔompF) E. coli.
- Growth Medium: Appropriate broth (e.g., LB, M9).
- Fluorescent Tracer: 100 µM 2-NBDG (from a 20 mM stock in DMSO) [15].
- Ionophores: 50 µM Carbonyl cyanide m-chlorophenyl hydrazone (CCCP, protonophore) and 10 µM Valinomycin (K⁺ ionophore) to manipulate internal ion concentrations [15].
- Equipment: Microfluidic perfusion system for single-cell imaging or flow cytometer; fluorescence microscope; temperature-controlled incubator.
Procedure:
- Culture Preparation: Grow bacterial cultures to mid-exponential phase (OD₆₀₀ ≈ 0.5) in the desired medium.
- Cell Loading: Wash and resuspend the cells in an appropriate buffer (e.g., potassium phosphate buffer) to an OD₆₀₀ of ~0.1.
- Ionophore Pre-treatment (Optional): Incubate aliquots of the cell suspension with CCCP or valinomycin for 10 minutes at 37°C with shaking.
- Tracer Uptake: Add 2-NBDG to the cell suspension to a final concentration of 10-100 µM. Immediately transfer the mixture to a microfluidic chamber for imaging or load into a flow cytometer.
- Real-Time Imaging/Acquisition:
- For single-cell imaging: Perfuse the cells with buffer containing 2-NBDG and acquire time-lapse fluorescence images every 30-60 seconds for 20-30 minutes using a 488 nm laser for excitation and a 525/50 nm emission filter [15].
- For flow cytometry: Take samples at specific time points (e.g., 0, 5, 15, 30 min), wash, and resuspend in ice-cold buffer to stop uptake. Analyze fluorescence immediately using flow cytometry (FITC channel).
- Data Analysis: Quantify the mean fluorescence intensity (MFI) per cell over time. Compare the initial rates of uptake and the plateau MFI between wild-type and mutant strains or between treated and untreated conditions.
Protocol 2: Assessing LPS-Mediated Barrier Function via Sensitivity Assays
Objective: To evaluate the integrity of the LPS barrier by measuring bacterial sensitivity to hydrophobic antibiotics and detergents. Principle: Mutations that truncate the LPS core (rough mutants) destabilize the OM, increasing its permeability to hydrophobic compounds and thereby increasing susceptibility [10].
Materials:
- Bacterial Strains: Wild-type (smooth LPS) and isogenic deep-rough mutant (e.g., lpcA or rfaC mutant).
- Antimicrobials: Novobiocin (10 mg/mL stock), Erythromycin (10 mg/mL stock), Sodium deoxycholate (10% w/v stock).
- Growth Medium: Cation-adjusted Mueller-Hinton Broth (CAMHB).
- Equipment: 96-well microtiter plates, plate reader, multichannel pipette.
Procedure:
- Culture Standardization: Grow overnight cultures of test strains and dilute to ~1 x 10⁶ CFU/mL in CAMHB.
- Broth Microdilution: In a 96-well plate, perform two-fold serial dilutions of the antimicrobials (e.g., novobiocin: 0.5-256 µg/mL; deoxycholate: 0.001%-1%).
- Inoculation: Add an equal volume of the standardized bacterial inoculum to each well. Include growth control (bacteria + medium) and sterility control (medium only).
- Incubation: Incubate the plate at 37°C for 16-20 hours without shaking.
- Analysis: Determine the Minimum Inhibitory Concentration (MIC) as the lowest concentration of antimicrobial that completely inhibits visible growth. A ≥4-fold decrease in the MIC of the rough mutant compared to the wild-type strain indicates a compromised LPS barrier function.
Regulatory Pathways and Metabolic Control of Porin Permeability
Recent research has unveiled a sophisticated regulatory network where bacterial metabolism dynamically controls porin permeability via changes in periplasmic ion concentrations [15]. This represents a novel, rapid response mechanism that complements traditional transcriptional regulation.
Diagram 1: Metabolic Control of Porin Permeability. This diagram illustrates how bacterial metabolic states influence periplasmic ion concentrations (H⁺ and K⁺) to dynamically regulate porin conductance, thereby balancing nutrient uptake with energy conservation and impacting antibiotic resistance [15].
Genetic Regulation of Porin Expression
Beyond immediate metabolic control, porin expression is regulated at the transcriptional level. Key regulatory systems include:
- SmpB Protein: In Aeromonas veronii, the SmpB protein binds to specific regions of the OmpA promoter, acting as a positive regulator of ompA expression, particularly during the stationary phase [12].
- Anti-Repressors: In A. baumannii, the A1S_0316 protein acts as an anti-repressor by binding the OmpA promoter with higher affinity than the global repressor H-NS, preventing H-NS-mediated repression [12].
- Sigma Factor Circuits: In Stenotrophomonas maltophilia, peptidoglycan stress triggered by the loss of OmpA-peptidoglycan interaction upregulates sigma factor σP, leading to a cascade that ultimately modulates β-lactamase expression and antibiotic resistance [12].
Diagram 2: Genetic Regulation of Resistance. This diagram outlines the sigma(P)-NagA regulatory circuit that connects outer membrane integrity to β-lactamase expression, illustrating a multi-layer resistance response [12].
The Scientist's Toolkit: Key Research Reagents and Methodologies
Table 3: Essential Research Reagents for Studying Outer Membrane Permeability
| Reagent / Tool | Category | Primary Function in Research | Example Application |
|---|---|---|---|
| 2-NBDG | Fluorescent Tracer | Porin-permeable glucose analog for tracking OM permeability [15] | Quantifying real-time porin-mediated uptake using flow cytometry or microscopy [15] |
| Bocillin FL | Fluorescent Tracer | Penicillin-based fluorescent probe for β-lactam uptake studies [15] | Visualizing and quantifying penetration of β-lactam-like molecules [15] |
| Ionophores (CCCP, Valinomycin) | Chemical Modulator | Disrupts H⁺ or K⁺ gradients across membranes [15] | Manipulating periplasmic ion concentrations to study their effect on porin conductance [15] |
| pHuji & pHluorin | Genetically Encoded Sensor | Fluorescent proteins for ratiometric measurement of periplasmic and cytoplasmic pH, respectively [15] | Real-time monitoring of pH changes in specific cellular compartments in single cells [15] |
| GINKO1 & GINKO2 | Genetically Encoded Sensor | Fluorescent biosensors for monitoring cytoplasmic and periplasmic K⁺ levels [15] | Tracking dynamic changes in potassium ion concentration in response to metabolic shifts [15] |
| ArchT | Optogenetic Tool | Light-activated proton pump expressed in the inner membrane [15] | Precisely and reversibly acidifying the periplasm to directly test its effect on porin permeability [15] |
| Microfluidic Perfusion System | Equipment | Enables high-resolution imaging of single cells under controlled conditions [15] | Conducting long-term, real-time imaging of ion fluctuations and tracer uptake in individual bacteria [15] |
The outer membrane of Gram-negative bacteria is a dynamic and complex barrier whose permeability is a cornerstone of intrinsic antibiotic resistance. Its function is determined by the intricate interplay between the LPS layer and a diverse set of porin channels. Resistance arises not only from classic genetic mutations that alter the abundance or structure of these components but also from a newly appreciated layer of metabolic regulation that dynamically controls porin permeability in response to the cell's energetic state. Overcoming this barrier requires a deep and nuanced understanding of these pathways. Future research and drug development must account for this complexity, potentially targeting the regulatory systems themselves (e.g., Kch channel) or designing novel agents that can bypass or disrupt the barrier, thereby revitalizing our arsenal in the fight against multidrug-resistant Gram-negative infections.
Constitutive efflux pumps represent a fundamental component of intrinsic antibiotic resistance in bacteria, enabling survival amid antimicrobial agents from the earliest exposure. These membrane-associated transport proteins, expressed at baseline levels across bacterial species, function as frontline defenses by actively extruding toxic compounds from bacterial cells. This whitepaper examines the structural classification, regulatory mechanisms, and physiological roles of constitutively expressed efflux systems, with particular focus on their clinical significance in multidrug-resistant pathogens such as Acinetobacter baumannii and Pseudomonas aeruginosa. The document further details experimental methodologies for investigating efflux pump activity and provides a strategic framework for developing efflux pump inhibitors as therapeutic adjuvants. Within the broader context of intrinsic resistance mechanisms research, understanding these constitutive systems provides critical insights for overcoming treatment failures and designing novel antimicrobial strategies.
Constitutive efflux pumps are transport proteins consistently expressed at baseline levels in bacterial cells, providing inherent protection against antimicrobial compounds without requiring prior exposure or genetic adaptation [16] [17]. Unlike inducible resistance mechanisms that activate only under antibiotic pressure, these pumps maintain a constant vigilance system, contributing significantly to what is termed intrinsic resistance - the innate ability of a bacterial species to resist antibiotic classes due to its core genomic makeup [18]. This fundamental defense mechanism predates clinical antibiotic use, suggesting these pumps evolved primarily for physiological functions beyond antibiotic extrusion [16] [17].
The clinical significance of constitutive efflux extends beyond providing baseline protection. When overexpressed, often through mutations in regulatory genes, these same pumps can confer elevated multidrug resistance (MDR) phenotypes in clinical isolates, expelling chemically diverse antibiotics and contributing to treatment failures [16] [17] [19]. The Resistance-Nodulation-Division (RND) family efflux pumps in Gram-negative pathogens represent particularly effective constitutive systems due to their tripartite structure that spans both inner and outer membranes, allowing direct extrusion of antibiotics to the extracellular environment [16] [19]. For opportunistic pathogens like Acinetobacter baumannii and Pseudomonas aeruginosa, which possess numerous chromosomal efflux pump genes, this intrinsic resistance mechanism presents a major therapeutic challenge, especially in healthcare settings where carbapenem resistance rates continue to rise globally [16].
Classification and Mechanisms of Major Efflux Pump Families
Bacterial efflux pumps are categorized into superfamilies based on their structural characteristics, energy coupling mechanisms, and phylogenetic relationships. The table below summarizes the key features of major efflux pump families with constitutive expression profiles.
Table 1: Major Families of Bacterial Efflux Pumps with Constitutive Expression
| Family | Energy Source | Typical Structure | Primary Substrates | Representative Examples |
|---|---|---|---|---|
| RND (Resistance-Nodulation-Division) | Proton motive force | Tripartite complex (inner membrane transporter, periplasmic adapter, outer membrane factor) | Broad spectrum: β-lactams, fluoroquinolones, tetracyclines, macrolides, chloramphenicol, dyes, detergents | AdeABC, AdeIJK in A. baumannii; AcrAB-TolC in E. coli; MexAB-OprM in P. aeruginosa |
| MFS (Major Facilitator Superfamily) | Proton motive force | Single component (12-14 transmembrane segments) | Tetracyclines, chloramphenicol, fluoroquinolones, β-lactams | TetA, Tet(B) in A. baumannii; NorA in S. aureus |
| MATE (Multidrug and Toxic Compound Extrusion) | Proton/sodium motive force | Single component (12 transmembrane segments) | Fluoroquinolones, aminoglycosides, dyes | AbeM in A. baumannii |
| SMR (Small Multidrug Resistance) | Proton motive force | Small tetramer (4 transmembrane segments) | Disinfectants, dyes, fluoroquinolones | AbeS in A. baumannii; EmrE in E. coli |
| ABC (ATP-Binding Cassette) | ATP hydrolysis | Two transmembrane domains + two nucleotide binding domains | Aminoglycosides, macrolides, glycopeptides | MsbA in E. coli |
| PACE (Proteobacterial Antimicrobial Compound Efflux) | Proton motive force | Four transmembrane segments | Chlorhexidine, acriflavine, propanol | AceI in A. baumannii |
The RND family represents the most clinically significant constitutive efflux system in Gram-negative pathogens due to its broad substrate profile and efficient extrusion mechanism [16] [19]. These pumps form sophisticated tripartite architectures that traverse the entire cell envelope: an inner membrane RND transporter (e.g., AdeB, AdeI), a periplasmic membrane fusion protein (MFP, e.g., AdeA, AdeJ), and an outer membrane factor (OMF, e.g., AdeC, AdeK) [16]. This continuous conduit allows direct antibiotic extrusion from the cell interior or periplasm to the external environment, effectively reducing intracellular drug concentrations below inhibitory levels [16] [19].
The operational mechanism involves a proton antiport process where the influx of protons down their electrochemical gradient provides energy for substrate extrusion [16]. RND transporters typically contain 12 transmembrane segments with two large loops between transmembrane segments 1-2 and 7-8, forming proximal and distal binding pockets that accommodate structurally diverse compounds [16] [19]. These pumps cycle through loose, tight, and open conformations to capture and expel substrates, with some evidence suggesting they can directly efflux compounds from the cytoplasm despite primarily functioning in the periplasm [16].
Diagram 1: RND family efflux pump structure and mechanism
Regulation and Expression of Efflux Pumps
Constitutive efflux pump expression is governed by sophisticated regulatory networks that maintain baseline levels while allowing adaptive responses to environmental stresses. These systems integrate local regulators specific to individual pump operons with global regulators that coordinate multiple cellular responses [17].
In Acinetobacter baumannii, the clinically significant AdeABC pump is regulated by the AdeRS two-component system, where AdeS acts as a sensor kinase and AdeR as a response regulator [16]. Under normal conditions, this system maintains modest expression levels sufficient for intrinsic resistance functions. Mutations in adeRS, particularly in AdeS, can lead to constitutive overexpression, resulting in significantly enhanced multidrug resistance phenotypes in clinical isolates [16]. Similarly, the AdeIJK pump, which demonstrates substantial basal activity even without induction, is regulated by the AdeN repressor and the BaeSR two-component system [16]. The AdeFGH system is controlled by the AdeL LysR-type transcriptional regulator, with additional modulation by quorum sensing molecules such as the abaI autoinducer [16].
The evolutionary conservation of efflux pumps across bacterial species indicates they serve fundamental physiological roles beyond antibiotic resistance [17]. Research suggests constitutive efflux activity contributes to:
- Virulence modulation: Export of virulence factors and toxins
- Stress response: Protection against oxidative stress, bile salts, and host-derived antimicrobial peptides
- Cell-to-cell communication: Transport of quorum sensing molecules and intercellular signals
- Metabolic waste removal: Elimination of toxic metabolic byproducts
- Homeostasis maintenance: Regulation of internal pH and ion concentrations [16] [17] [19]
The tight integration of efflux pump regulation with stress response pathways explains why antibiotic exposure often selects for mutants with constitutively overexpressed pumps, as these adaptations provide simultaneous resistance to multiple drug classes while maintaining bacterial fitness in hostile environments [17].
Experimental Methodologies for Efflux Pump Investigation
Efflux Pump Activity Assays
Minimum Inhibitory Concentration (MIC) Determination with EPIs
- Principle: Compare MIC values of antibiotics with and without efflux pump inhibitors (EPIs) to detect efflux-mediated resistance [20] [21]
- Protocol:
- Prepare serial dilutions of test antibiotic in Mueller-Hinton broth
- Inoculate with standardized bacterial suspension (~5×10^5 CFU/mL)
- Add subinhibitory concentrations of EPI (e.g., Phe-Arg-β-naphthylamide, carbonyl cyanide m-chlorophenyl hydrazone, or plant-derived inhibitors like berberine or curcumin) [21]
- Incubate at 35°C for 16-20 hours
- Determine MIC as lowest antibiotic concentration inhibiting visible growth
- Interpret results: ≥4-fold MIC reduction with EPI indicates significant efflux contribution [20] [21]
Ethidium Bromide Accumulation and Efflux Assays
- Principle: Measure fluorescence changes as ethidium bromide (EtBr) accumulates in cells or is actively extruded [16]
- Protocol:
- Grow bacterial culture to mid-logarithmic phase (OD600 ≈ 0.5)
- Harvest cells by centrifugation and wash with phosphate-buffered saline (PBS)
- Resuspend in PBS with glucose (0.2% w/v) as energy source
- Load cells with EtBr (0.5-2 μg/mL) and incubate 30 minutes
- Measure baseline fluorescence (excitation 530 nm, emission 600 nm)
- Add energy inhibitor (e.g., carbonyl cyanide m-chlorophenyl hydrazone) or EPI
- Monitor fluorescence increase (accumulation) or decrease (efflux) over time
- Calculate initial efflux rates from fluorescence decay curves [16]
Gene Expression Analysis
Quantitative Reverse Transcription PCR (qRT-PCR)
- Principle: Quantify efflux pump mRNA levels to assess constitutive expression and regulatory responses [22]
- Protocol:
- Extract total RNA from bacterial cultures using guanidinium thiocyanate-phenol-chloroform method
- Treat with DNase I to remove genomic DNA contamination
- Synthesize cDNA using reverse transcriptase and random hexamers
- Perform qPCR with gene-specific primers for target efflux pumps (e.g., adeB, adeJ, adeG)
- Include housekeeping gene controls (e.g., rpoB, gyrB)
- Calculate relative expression using 2^(-ΔΔCt) method [22]
RNA Sequencing (RNA-seq)
- Principle: Comprehensive transcriptome profiling to identify differentially expressed genes in efflux pump mutants [23]
- Protocol:
- Extract high-quality total RNA (RIN > 8.0)
- Deplete ribosomal RNA using target-specific probes
- Prepare sequencing libraries with polyA selection or rRNA depletion
- Sequence on high-throughput platform (Illumina)
- Map reads to reference genome and quantify transcript abundance
- Identify differentially expressed genes with statistical significance (FDR < 0.05) [23]
Genetic Approaches for Functional Characterization
Gene Knockout Construction
- Principle: Create isogenic mutants to directly assess efflux pump contribution to resistance [23]
- Protocol:
- Amplify upstream and downstream flanking regions of target gene
- Clone fragments into suicide vector with selectable marker
- Introduce plasmid into target strain via conjugation or transformation
- Select for single-crossover integrants using appropriate antibiotics
- Counter-select for double-crossover events yielding gene deletions
- Verify mutants by PCR and sequencing [23]
Complementation Studies
- Principle: Restore gene function in mutants to confirm phenotype linkage [23]
- Protocol:
- Amplify complete target gene with native promoter
- Clone into stable expression vector
- Introduce recombinant plasmid into knockout mutant
- Verify complementation by restored gene expression and phenotypic reversal [23]
Research Reagent Solutions
Table 2: Essential Research Reagents for Efflux Pump Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Efflux Pump Inhibitors | Phe-Arg-β-naphthylamide (PAβN), carbonyl cyanide m-chlorophenyl hydrazone (CCCP), verapamil, reserpine | Functional characterization of efflux activity, EPI development | Varying specificity for different pump families; potential cytotoxicity at high concentrations |
| Fluorescent Substrates | Ethidium bromide, Hoechst 33342, rhodamine 6G, Nile red | Real-time efflux kinetics, pump activity quantification | Differential substrate preferences among pumps; fluorescence properties affect detection sensitivity |
| Plant-Derived EPIs | Berberine, curcumin, palmatine, piperine, capsaicin | Natural product screening, combination therapy development | Dual antibacterial and EPI activity; potential Sortase A inhibition; lower cytotoxicity profiles |
| Gene Expression Tools | RT-PCR primers for efflux pump genes, RNA extraction kits, RNA-seq library prep kits | Expression profiling, regulatory mechanism studies | Primer specificity critical for homologous pump genes; RNA quality affects results |
| Antibiotic Substrates | Ciprofloxacin, levofloxacin, tetracycline, chloramphenicol, erythromycin, β-lactams | Susceptibility testing, substrate range determination | Use clinical isolates with defined resistance profiles; include EPI controls |
| Bacterial Strains | ATCC type strains, clinical isolates with characterized efflux mutations, isogenic knockout mutants | Mechanistic studies, comparative analyses | Verify genetic background; include appropriate controls for mutant studies |
Connection to Virulence and Pathogenesis
Emerging evidence demonstrates that constitutive efflux pumps function at the intersection of antibiotic resistance and bacterial virulence, influencing host-pathogen interactions through multiple mechanisms [17] [23]. Research on Pseudomonas aeruginosa reveals that mutations inactivating the MexEF-OprN efflux pump unexpectedly increase virulence during infection through enhanced quorum sensing (QS) signaling [23]. These efflux pump mutants exhibit elevated production of QS-regulated virulence factors including elastase and rhamnolipids, leading to more severe infection outcomes in murine models [23].
Efflux pumps also contribute to virulence through:
- Biofilm formation: Export of biofilm matrix components and signaling molecules
- Stress adaptation: Protection against host immune effectors like antimicrobial peptides
- Toxin secretion: Extrusion of cytolytic compounds and exoenzymes
- Metabolic fitness: Maintenance of cellular homeostasis during infection [17] [19]
The relationship between efflux and virulence displays pathogen-specific characteristics. In Salmonella enterica, the AcrAB-TolC system facilitates adhesion and invasion of host cells, while in Escherichia coli, efflux pumps contribute to colonization competence [19]. This functional integration suggests that therapeutic targeting of efflux pumps may simultaneously restore antibiotic susceptibility and attenuate virulence, providing dual therapeutic benefits [17] [23].
Diagram 2: Efflux pump modulation of virulence and resistance
Therapeutic Targeting and Future Directions
Efflux Pump Inhibitor Development
The strategic inhibition of constitutive efflux pumps represents a promising approach to revitalizing existing antibiotics and overcoming multidrug resistance [16] [20] [21]. Current EPI development strategies include:
Natural Product Screening Plant-derived compounds including berberine, curcumin, and palmatine demonstrate dual antibacterial and efflux inhibition activity, potentially acting as both antimicrobials and resistance breakers [21]. These compounds exhibit effects on bacterial growth kinetics and morphology while inhibiting efflux function, making them attractive candidates for combination therapies [21].
Synthetic Chemistry Approaches Structure-based drug design targeting conserved regions of efflux pumps, particularly the binding pockets and proton translocation domains, enables development of potent inhibitors with improved pharmacological properties [16] [19]. Recent efforts have identified specific binding boxes in the periplasmic adapter proteins of RND pumps as promising therapeutic targets [19].
Dual-Target Inhibitors Compounds capable of inhibiting both bacterial efflux pumps and mammalian MDR transporters (e.g., P-glycoprotein) offer potential for concurrent treatment of infectious diseases and cancer, though selectivity considerations remain challenging [20].
Technological Innovations
Advanced methodologies are enhancing EPI discovery and development:
Machine Learning Applications Computational approaches analyze chemical libraries to predict EPI activity, identify structural features associated with efflux inhibition, and optimize lead compounds, accelerating the discovery pipeline [19].
Structural Biology Techniques Cryo-electron microscopy and X-ray crystallography provide high-resolution structures of efflux pumps, enabling rational drug design through detailed understanding of substrate binding and transport mechanisms [16] [19].
Chemical Informatics Database development systematizes known EPI structures and activities, facilitating quantitative structure-activity relationship (QSAR) modeling and virtual screening of compound libraries [20] [19].
The continued investigation of constitutive efflux pumps remains essential for addressing the growing threat of multidrug-resistant infections. By integrating fundamental knowledge of pump structure-function relationships with innovative therapeutic approaches, researchers can develop effective strategies to counteract this primordial bacterial defense mechanism and preserve the efficacy of existing antimicrobial agents.
Antimicrobial resistance represents one of the most pressing challenges to modern healthcare, contributing significantly to global morbidity and mortality [18]. While acquired resistance through horizontal gene transfer often dominates clinical concerns, intrinsic resistance mechanisms encoded by chromosomal genes provide a fundamental "enzymatic armor" that enables bacterial survival against antimicrobial agents. This innate resistance predates antibiotic chemotherapy and is present in all bacterial species [24].
The concept of the "resistome" encompasses all antibiotic resistance genes, both intrinsic and acquired, within bacterial populations. Within this framework, chromosomal genes encoding enzymatic inactivation systems represent a sophisticated first line of defense that does not require external genetic acquisition [25]. These intrinsic mechanisms are particularly problematic in clinical settings as they are ubiquitous within specific bacterial species and not dependent on the selective pressures that drive the spread of acquired resistance.
This review examines the chromosomal gene-encoded enzymatic systems that confer intrinsic antibiotic resistance, with a focus on their biochemical mechanisms, genetic regulation, and experimental characterization. Understanding these native resistance elements is paramount for developing novel therapeutic strategies to overcome treatment failures and combat the escalating antimicrobial resistance crisis.
Core Mechanisms of Enzymatic Antibiotic Inactivation
Bacteria employ several sophisticated enzymatic strategies to neutralize antibiotics, including modification of the drug molecule itself, target site alterations, and protection of vulnerable cellular components. The major enzymatic mechanisms encoded by chromosomal genes include:
Antibiotic-Modifying Enzymes
Chromosomal genes encode various enzymes that chemically modify antibiotics, rendering them ineffective against their cellular targets. These modifications include:
- Hydrolytic inactivation: Enzymes such as β-lactamases cleave critical bonds in antibiotic structures. The AmpC β-lactamase, chromosomally encoded in many Gram-negative bacteria, hydrolyzes the β-lactam ring of penicillins and cephalosporins [18].
- Group transfer reactions: Transferases catalyze the covalent attachment of chemical groups to antibiotics. This includes aminoglycoside-modifying enzymes such as acetyltransferases, phosphotransferases, and nucleotidyltransferases [26].
- Redox-based inactivation: Some enzymes catalyze redox reactions that alter essential components of antibiotic molecules.
Target Modification Systems
Beyond direct antibiotic modification, bacteria utilize enzymatic systems to alter the molecular targets of antibiotics:
- Enzyme mutation and evolution: Chromosomal genes encoding target proteins can mutate to reduce antibiotic binding affinity while maintaining cellular function. Mutations in genes for DNA gyrase (gyrA, gyrB) and topoisomerase IV (parC, parE) confer resistance to quinolones by altering the quinolone resistance-determining region (QRDR) [25].
- Target protection proteins: Some chromosomal genes encode proteins that physically protect antibiotic targets without modifying them, such as the Qnr proteins that protect DNA gyrase from quinolones [26].
Efflux Pump Systems
While not direct inactivation mechanisms, efflux pumps function as enzymatic armor by reducing intracellular antibiotic concentrations. Chromosomal multidrug efflux systems like AcrAB-TolC in Enterobacteriaceae provide intrinsic resistance to multiple antibiotic classes [27] [18].
Table 1: Major Chromosomal Enzymatic Systems for Antibiotic Inactivation
| Enzyme Class | Representative Enzymes | Antibiotic Targets | Mechanism of Action |
|---|---|---|---|
| β-Lactamases | AmpC, SHV | β-Lactams | Hydrolysis of β-lactam ring |
| Aminoglycoside-Modifying Enzymes | AAC, APH, ANT | Aminoglycosides | Acetylation, phosphorylation, adenylation |
| Target-Altering Enzymes | Mutated PBP2a, Altered DNA gyrase | β-Lactams, Quinolones | Reduced drug-target binding affinity |
| Drug-Modifying Enzymes | Chloramphenicol acetyltransferase | Chloramphenicol | Acetylation |
| Ribosomal Methyltransferases | Erm family | Macrolides, Lincosamides, Streptogramins | Methylation of 23S rRNA |
Key Chromosomal Resistance Genes and Their Regulation
mecA/mecC-Mediated Resistance in Staphylococcus aureus
The mecA gene represents a paradigm of chromosomal antibiotic resistance, encoding the alternative penicillin-binding protein PBP2a in methicillin-resistant Staphylococcus aureus (MRSA) [28]. This protein possesses low affinity for β-lactam antibiotics due to structural differences in its active site, allowing it to maintain bacterial cell wall synthesis when native PBPs are inhibited [28] [25].
The mecA gene is part of the staphylococcal cassette chromosome mec (SCCmec), a mobile genetic element that integrates into the bacterial chromosome [28]. Its expression is regulated by the mecA regulatory system (mecR1-mecI) and the β-lactamase regulatory system (blaR1-blaI), which respond to the presence of β-lactam antibiotics [28]. A homologous gene, mecC, has also been identified and encodes PBP2c with similar function [28].
Auxiliary Factor Genes (fem Factors)
The expression of methicillin resistance in MRSA requires the coordinated activity of auxiliary factors encoded by fem (factor essential for methicillin resistance) genes [28]. These chromosomal genes, including femA, femB, femC, femD, femE, and femF, participate in cell wall biosynthesis and synergistically regulate resistance levels without directly affecting PBP2a production [28].
Insertional inactivation of femA and femB results in complete loss of methicillin resistance, demonstrating their essential role in the resistance phenotype [28]. These genes are dispersed throughout the bacterial chromosome and represent potential targets for novel anti-MRSA therapies aimed at disrupting the native enzymatic armor.
Enzymatic Targets and Modifications
Chromosomal genes encoding antibiotic targets can develop mutations that confer resistance while maintaining essential cellular functions:
- RNA polymerase mutations: Mutations in the rpoB gene, particularly in codons 507-533, alter the β-subunit of RNA polymerase and confer resistance to rifamycins [25].
- DNA gyrase and topoisomerase IV mutations: Mutations in gyrA/gyrB and parC/parE genes reduce binding affinity for fluoroquinolones while maintaining enzymatic function [25].
- Ribosomal RNA methyltransferases: Chromosomal erm genes encode methyltransferases that modify 23S rRNA, preventing binding of macrolides, lincosamides, and streptogramins [18].
Table 2: Experimentally Characterized Chromosomal Resistance Genes
| Gene | Bacterial Species | Encoded Enzyme/Protein | Resistance Profile |
|---|---|---|---|
| mecA | Staphylococcus aureus | PBP2a | β-lactams |
| mecC | Staphylococcus aureus | PBP2c | β-lactams |
| femA | Staphylococcus aureus | Fem factor A | β-lactams (auxiliary) |
| blaA | Bacteroides fragilis | β-lactamase | β-lactams |
| ampC | Enterobacteriaceae, Pseudomonas | β-lactamase | β-lactams |
| vanA | Enterococcus faecium | D-Ala-D-Lac ligase | Glycopeptides |
| erm(B) | Various Gram-positives | rRNA methyltransferase | Macrolides |
| aac(6')-Ib | Various Gram-negatives | Aminoglycoside acetyltransferase | Aminoglycosides |
| gyrA | Multiple species | DNA gyrase subunit A | Quinolones |
| rpoB | Multiple species | RNA polymerase subunit B | Rifamycins |
Experimental Approaches and Methodologies
Gene Inactivation and Functional Analysis
Understanding chromosomal resistance genes requires robust methods for genetic manipulation. The one-step inactivation method using PCR products provides an efficient approach for disrupting chromosomal genes in Escherichia coli and other bacteria [29]. This technique employs the phage λ Red recombinase system to facilitate homologous recombination between the chromosome and PCR products containing selectable markers flanked by homology regions [29].
Protocol: One-Step Chromosomal Gene Inactivation
- Amplify a selectable antibiotic resistance cassette (e.g., kanamycin or chloramphenicol) using primers with 36-50 nucleotide extensions homologous to the target gene.
- Introduce the PCR product into bacteria expressing the λ Red recombinase system (encoded on a temperature-sensitive plasmid).
- Select for transformants on appropriate antibiotic-containing media.
- Verify gene disruption by PCR analysis using primers flanking the target region and internal cassette primers.
- Eliminate the antibiotic resistance cassette using FLP recombinase acting on FRT sites if desired [29].
This method allows for systematic functional analysis of chromosomal genes suspected to contribute to intrinsic resistance, including fem factors and regulatory elements.
Experimental Evolution for Studying Resistance Emergence
Experimental evolution approaches allow direct observation of how chromosomal genes contribute to resistance development under selective pressure:
Protocol: Experimental Evolution of Antibiotic Resistance
- Initiate multiple independent bacterial lineages in subinhibitory concentrations of antibiotics.
- Propagate cultures through serial passages (typically 28+ days) with increasing antibiotic concentrations.
- Monitor population dynamics through regular sampling and determination of minimum inhibitory concentrations (MICs).
- Identify genetic changes through whole-genome sequencing of isolates from different time points.
- Validate causal mutations by reintroducing specific changes into naive backgrounds [30].
This approach has demonstrated how chromosomal genes facilitate adaptation, such as the integration of carbapenemase genes into the chromosome of E. coli ST38 under antibiotic selection [30].
Molecular Characterization of Resistance Mechanisms
Protocol: Characterization of β-Lactam Resistance Mechanisms
- Determine MICs to various β-lactams using broth microdilution according to CLSI guidelines.
- Detect PBP2a production using immunoassays or latex agglutination tests.
- Amplify mecA and mecC genes by PCR with specific primers.
- Assess expression levels of mecA and regulatory genes using quantitative RT-PCR.
- Evaluate the impact of auxiliary factors through gene inactivation and complementation studies [28].
Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Chromosomal Resistance Genes
| Reagent/Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Gene Inactivation Systems | λ Red recombinase system [29], FLP/FRT system | Targeted gene disruption | Temperature-sensitive replicon, high efficiency |
| Selective Markers | Kanamycin resistance (kan), Chloramphenicol resistance (cat) | Selection of recombinants | FRT-flanked for excision, various resistance profiles |
| Expression Vectors | pANTSγ, pINT-ts, pBAD18 | Complementation, heterologous expression | Inducible promoters, temperature-sensitive replication |
| PCR Enzymes | Taq polymerase, Pfu polymerase | Amplification of disruption cassettes | High fidelity, proofreading activity |
| Antibiotics for Selection | Ampicillin, Kanamycin, Chloramphenicol | Selective pressure, mutant selection | Various concentrations for different bacterial species |
| Bacterial Strains | E. coli BW25113, S. aureus strains with SCCmec | Host for genetic manipulations | Defined genetic background, recA+ for recombination |
| Sequencing Primers | Custom oligonucleotides with homology extensions | Verification of constructs | 36-50 nt homology regions, verification primers |
| Growth Media | SOB, SOC media | Transformation efficiency | High transformation efficiency, recovery after electroporation |
Visualization of Key Concepts
PBP2a-Mediated Resistance Mechanism
Experimental Workflow for Resistance Gene Analysis
Chromosomal genes encoding enzymatic armor represent a fundamental component of bacterial defense systems against antibiotics. The mecA/mecC-mediated production of PBP2a in MRSA exemplifies how native genetic elements can be co-opted or modified to provide robust resistance mechanisms. Together with auxiliary factors and regulatory systems, these chromosomal genes create sophisticated networks that enable bacterial survival under antimicrobial pressure.
Understanding these intrinsic resistance mechanisms at molecular, genetic, and biochemical levels provides critical insights for developing next-generation antimicrobial agents and combination therapies that can bypass or inhibit these native defense systems. As the antimicrobial resistance crisis continues to escalate, decoding the complexities of chromosomal resistance genes will be essential for preserving the efficacy of existing antibiotics and informing the design of novel therapeutic approaches.
Intrinsic resistance is the innate, chromosomally encoded ability of a bacterial species to withstand the action of a particular antibiotic class without prior exposure or horizontal gene transfer [31] [32]. This phenomenon is a cornerstone of the natural phenotype of susceptibility in bacteria and is distinct from acquired resistance. The World Health Organization (WHO) has prioritized antibiotic-resistant bacterial pathogens into critical, high, and medium priority groups to guide research and development of new strategies to combat antimicrobial resistance (AMR) [33]. Understanding the intrinsic resistome—the full complement of chromosomal elements that contribute to intrinsic resistance—is vital for developing novel therapeutic interventions and is the focus of this technical guide for researchers and drug development professionals [31].
The clinical and ecological impact of intrinsic resistance is profound. Bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to nearly 5 million more [34]. The WHO's 2024 Bacterial Priority Pathogens List (WHO BPPL) updates the prioritization of antibiotic-resistant pathogens to address these evolving challenges, categorizing 24 pathogens across 15 families [33]. This guide delves into the intrinsic resistance mechanisms of the most critical pathogens on this list, providing structured data and methodologies to advance research in this field.
The WHO Critical Priority Pathogens List
The 2024 WHO BPPL is a critical tool in the global fight against antimicrobial resistance [33]. Building on the 2017 edition, the list refines the prioritization of antibiotic-resistant bacteria to guide research and public health interventions. The pathogens categorized as critical priority are of utmost concern due to their global impact in terms of disease burden, transmissibility, treatability, and gaps in the R&D pipeline for new effective treatments [33] [35]. These bacteria are often multidrug-resistant, posing severe threats in healthcare settings.
The critical priority group primarily encompasses Gram-negative bacteria resistant to last-resort antibiotics, including carbapenem-resistant Acinetobacter baumannii and carbapenem-resistant Pseudomonas aeruginosa [33]. Also included are Enterobacteriaceae—such as Klebsiella pneumoniae, Escherichia coli, and Enterobacter spp.—that are resistant to both third-generation cephalosporins and carbapenems [35]. These pathogens are frequently associated with hospital-acquired infections like pneumonia, bloodstream infections, and infections in critically ill patients requiring medical devices such as ventilators and blood catheters [35].
Table 1: WHO Critical Priority Bacterial Pathogens and Key Intrinsic Resistances
| Bacterial Pathogen | Family | Key Intrinsic Resistance Profiles [32] [35] |
|---|---|---|
| Acinetobacter baumannii | Moraxellaceae | Intrinsic resistance to many beta-lactams (e.g., ampicillin, amoxicillin-clavulanate, 1st/2nd gen. cephalosporins), aminoglycosides, tetracyclines, macrolides. Often displays multi- or pan-drug resistance. |
| Pseudomonas aeruginosa | Pseudomonadaceae | Intrinsic resistance to many beta-lactams (e.g., ampicillin, amoxicillin-clavulanate, 1st/2nd gen. cephalosporins, many tetracyclines, chloramphenicol, and trimethoprim/sulfamethoxazole. |
| Enterobacteriaceae (Klebsiella pneumoniae, Escherichia coli, Enterobacter spp.) | Enterobacteriaceae | K. pneumoniae: Intrinsic resistance to ampicillin. E. coli: Intrinsic resistance to ampicillin, amoxicillin-clavulanate, some 1st-gen. cephalosporins. Enterobacter spp.: Intrinsic resistance to ampicillin, amoxicillin-clavulanate, 1st-gen. cephalosporins. |
Core Mechanisms of Intrinsic Resistance
The intrinsic resistance phenotype is an emergent property resulting from the concerted action of several chromosomal elements [31]. The primary mechanisms include reduced antibiotic permeability, efflux pump activity, and enzymatic inactivation.
Figure 1: Core mechanisms conferring intrinsic antibiotic resistance in bacterial pathogens.
Impermeability and Efflux Pumps
The synergy between low outer membrane permeability and broad-spectrum efflux pumps is a fundamental mechanism of intrinsic resistance in Gram-negative bacteria, particularly in critical pathogens like P. aeruginosa and A. baumannii [31]. The Gram-negative outer membrane acts as a formidable barrier, limiting the penetration of many antibiotic classes, including beta-lactams, macrolides, and glycopeptides [32]. This innate impermeability is powerfully complemented by multidrug efflux pumps.
These efflux systems, which often have a wide range of substrates, actively transport antibiotics out of the cell, preventing intracellular accumulation to effective concentrations [35]. In A. baumannii, for instance, several efflux pump families—including the Resistance Nodulation Division (RND) superfamily (e.g., AdeABC), the Major Facilitator Superfamily (MFS), and the Small Multidrug Resistance (SMR) family—contribute to resistance against aminoglycosides, tetracyclines, fluoroquinolones, and beta-lactams [35]. The AdeABC pump, in particular, has been linked to tigecycline resistance [35]. Similarly, in E. coli, the AcrAB efflux system is a major contributor to its intrinsic resistance to macrolides and other drug classes [31].
Enzymatic Inactivation and Target Modification
The production of chromosomally encoded antibiotic-inactivating enzymes is another key strategy. Many bacteria possess innate genes for enzymes that chemically modify or degrade antibiotics [31]. A classic example is the intrinsic production of various β-lactamases, such as the AmpC cephalosporinase found in A. baumannii and P. aeruginosa, which hydrolyzes and inactivates a broad range of penicillin and cephalosporin antibiotics [35].
Furthermore, intrinsic resistance can arise from the lack of a specific target or structural modifications to the target site that reduce antibiotic binding. For example, the absence of a cell wall in Mycoplasma pneumoniae makes it intrinsically resistant to all beta-lactam antibiotics, which target cell wall synthesis [32]. Enterococcus species exhibit intrinsic low-level resistance to aminoglycosides due to impaired drug uptake, though this can be overcome by synergism with cell-wall active agents [32].
Experimental Analysis of the Intrinsic Resistome
Elucidating the components of the intrinsic resistome requires high-throughput, genome-wide approaches. These methodologies allow for the systematic identification of genes that, when inactivated or overexpressed, alter the bacterial susceptibility profile.
Genome-Wide Mutagenesis and Phenotypic Screening
The most direct method for analyzing the intrinsic resistome involves screening comprehensive gene knockout or insertion libraries (e.g., transposon mutant libraries) [31]. This approach determines the contribution of each individual gene to the baseline antibiotic susceptibility of a bacterium. Mutants are arrayed in multi-well plates and screened for changes in the Minimum Inhibitory Concentration (MIC) to a panel of antibiotics. Genes whose inactivation leads to a decreased MIC (hypersusceptibility) are classified as components of the intrinsic resistome, as they are necessary for the wild-type level of resistance [31].
Figure 2: Workflow for identifying intrinsic resistome genes via mutant library screening.
Resistance Induction Through In Vitro Selection Pressures
Experimental induction of resistance under sustained laboratory selection pressure can reveal potential pathways for resistance development and identify genes that may become relevant in a clinical setting over time. This involves serially passaging bacteria in the presence of sub-inhibitory and progressively increasing concentrations of an antimicrobial agent [36].
For example, a 2016 study successfully induced resistance to the antimicrobial peptide Tachyplesin I in Aeromonas hydrophila, Pseudomonas aeruginosa, and Escherichia coli through two methods: long-term exposure to escalating drug concentrations and UV mutagenesis followed by selection on peptide-containing plates [36]. The study noted that resistance was stable and observed cross-resistance to other antimicrobials in some mutants, highlighting the potential risks associated with the clinical use of even potent antimicrobial peptides [36].
Table 2: Key Research Reagents and Methodologies for Intrinsic Resistance Studies
| Reagent / Method | Function & Application in Resistance Research |
|---|---|
| Transposon Mutant Library | Genome-wide collection of random gene knockouts for identifying genes that confer hypersusceptibility when inactivated. |
| CRISPR-Cas9 / RNAi Libraries | Functional genomics tools for targeted or systematic gene knockout/knockdown to validate resistance genes. |
| Standard Broth Microdilution | CLSI-standardized method for determining Minimum Inhibitory Concentration (MIC), the gold standard for susceptibility testing. |
| Conditional Expression Plasmids | For controlled overexpression (gain-of-function) of candidate genes to confirm their role in elevating MIC. |
| LC-MS/MS (Liquid Chromatography-Mass Spectrometry) | To quantify intracellular antibiotic accumulation and assess efflux pump activity or membrane permeability. |
Correlative Genomics and Transcriptomics
Leveraging large-scale pharmacogenomic datasets is a powerful computational and experimental approach. By integrating genomic, transcriptomic, and drug sensitivity data from hundreds of bacterial isolates or cell lines, researchers can identify correlations between basal gene expression levels and antibiotic potency [37]. This method hinges on the hypothesis that the overexpression of an intrinsic resistance driver (e.g., an efflux pump component) is inversely correlated with drug sensitivity.
A key advancement in this area involves applying stringent filters to these correlations to distinguish specific, mechanistic drivers from general, non-specific correlates. This includes removing genes that are mere proxies for co-expressed gene networks and filtering for gene-drug relationships with high selectivity, thereby excluding genes that simply mark tissue lineage or general metabolic state [37]. Candidate genes identified through this bioinformatic analysis must then be functionally validated through gene knockout (to enhance susceptibility) or overexpression (to confer resistance) in model bacterial strains [37].
Research Gaps and Future Directions
Despite advances in understanding the intrinsic resistome, significant challenges remain. A major hurdle is the distinction between genes that specifically confer resistance and those that indirectly affect susceptibility through broad impacts on cellular fitness and metabolism [31] [37]. Furthermore, the interplay between intrinsic resistance mechanisms and the acquisition of mobile genetic elements carrying resistance genes is complex and not fully elucidated.
Future research should prioritize:
- Defining the Resistome-Phenotype Link: Systematically linking specific genetic elements within the intrinsic resistome to measurable phenotypic resistance outcomes across different genetic backgrounds and environmental conditions.
- Exploring Inhibitors of Intrinsic Resistance: Targeting components of the intrinsic resistome, such as efflux pumps or regulatory proteins, to re-sensitize bacteria to existing antibiotics [31]. This approach could revitalize older drugs and enhance the efficacy of new ones.
- Integrating Multi-Omics Data: Combining genomic, transcriptomic, proteomic, and metabolomic data to build a holistic model of how intrinsic resistance emerges from networked cellular systems, rather than from isolated genes.
Overcoming these challenges requires a sustained global commitment. AMR demands a coordinated "One Health" approach that integrates surveillance and control strategies across human health, animal health, agriculture, and the environment [34]. The WHO's BPPL serves as a critical guide for focusing these research efforts and investments on the most threatening pathogens, aiming to mitigate the global public health crisis of antimicrobial resistance [33].
From Bench to Insight: Advanced Techniques for Profiling and Targeting Intrinsic Barriers
Genomic and Metagenomic Mining for Predicting Intrinsic Resistomes
The intrinsic resistome encompasses all chromosomally encoded elements in a bacterial species that contribute to its natural, baseline level of antibiotic resistance, independent of horizontal gene acquisition. Understanding and identifying these determinants is critical for combating antimicrobial resistance (AMR), a global health threat projected to cause 10 million deaths annually by 2050 [1]. This whitepaper provides an in-depth technical guide for researchers and drug development professionals on the core concepts, computational methodologies, and experimental protocols for mining intrinsic resistomes from genomic and metagenomic data. We detail state-of-the-art bioinformatics tools, machine learning pipelines, and functional validation strategies, framing this within the broader thesis that targeting intrinsic resistance mechanisms offers a promising avenue for developing novel therapeutic adjuvants and resistance-breaking strategies.
The clinical definition of antibiotic resistance is often based on breakpoints of minimal inhibitory concentrations (MICs). In contrast, an ecological definition uses the ecological cut-off (ECOFF) value, which identifies the upper limit of the wild-type population's MIC [31]. Intrinsic resistance falls at the intersection of these definitions. A bacterium is considered intrinsically resistant from a clinical perspective if infections cannot be treated with a given antibiotic. The major mechanisms underlying this phenotype include:
- Lack of the drug target
- Activity of chromosomally encoded antibiotic-inactivating enzymes
- Reduced drug uptake due to cellular envelope impermeability and the activity of multidrug efflux pumps [31]
From a genetic perspective, the intrinsic resistome is defined as the set of all chromosomally encoded elements that contribute to antibiotic resistance, irrespective of prior antibiotic exposure and not acquired via horizontal gene transfer (HGT) [31]. This concept reframes intrinsic resistance from being solely dependent on a few well-known mechanisms to an emergent property of the bacterial cell, arising from the concerted action of numerous genes involved in basic cellular processes and metabolism [31].
Table 1: Key Characteristics of the Intrinsic Resistome
| Feature | Description |
|---|---|
| Genetic Basis | Chromosomally encoded; not acquired via horizontal gene transfer. |
| Independence | Presence is independent of previous antibiotic exposure. |
| Composition | Includes classical resistance genes (e.g., efflux pumps) and genes involved in basic bacterial metabolism. |
| Phenotypic Impact | Determines the characteristic baseline susceptibility of a bacterial species. |
| Evolutionary Role | Serves as a reservoir of genes from which high-level, clinically relevant resistance can evolve. |
Studying the intrinsic resistome is vital for several reasons: it helps predict the evolution of resistance, reveals links between core metabolism and antibiotic susceptibility, and identifies novel targets for drug development. Inhibiting elements of the intrinsic resistome can re-sensitize bacteria to existing antibiotics, a strategy known as "resistance proofing" [3].
Computational Identification and Prediction
The foundation of modern intrinsic resistome mining is computational analysis of genomic and metagenomic data. This process involves specialized databases, diverse toolsets, and increasingly, machine learning models.
Selecting the appropriate database is critical, as they vary in curation methods, scope, and annotation depth [38].
Table 2: Key Databases for Antibiotic Resistance Gene Analysis
| Database Name | Type & Curation | Key Features | Strengths | Limitations |
|---|---|---|---|---|
| CARD [38] | Manually curated; relies on experimental validation and peer-reviewed publications. | Antibiotic Resistance Ontology (ARO); Resistance Gene Identifier (RGI) tool. | High-quality, structured data; detailed mechanistic information. | Potential gaps for emerging genes without validation; manual curation can delay updates. |
| ResFinder/ PointFinder [38] | Manually curated. | Focuses on acquired AMR genes and chromosomal point mutations; integrated analysis. | Rapid analysis from raw reads; detailed mutation insights. | Scope is primarily on acquired resistance and specific mutations. |
| MEGARes [38] | Manually curated. | Structured hierarchical classification of ARGs. | Facilitates accurate analysis of metagenomic data. | --- |
| NDARO [38] | Consolidated (integrates multiple sources). | Integrates data from CARD, Lahey Clinic, and other resources. | Broad coverage. | Potential challenges with consistency and redundancy. |
Bioinformatics Tools and Workflows
A typical workflow for intrinsic resistome mining involves sequence annotation, analysis, and visualization.
- Gene Cluster Annotation: Tools like antiSMASH are versatile platforms for genome mining of secondary metabolite biosynthetic gene clusters, including those for antibiotics [39]. Its plug-and-play architecture allows for the detection of a wide range of cluster types.
- ARG Identification from WGS and Metagenomes: Tools like AMRFinderPlus and DeepARG are widely used. AMRFinderPlus relies on homology-based searches against curated databases, while DeepARG uses a machine learning model to predict ARGs from sequence data, making it suitable for identifying novel or divergent genes [38].
- Specialized Prediction Pipelines: GraphAMR is a novel computational pipeline that improves read mapping technology for discovering ARGs from fragmented metagenomic assemblies [40]. AMRLearn is a dedicated machine learning pipeline for predicting AMR phenotypes associated with single-nucleotide polymorphism (SNP) genotypes from whole-genome sequence data [41].
Diagram 1: Computational Resistome Mining Workflow
Machine Learning for Resistance Prediction
Machine learning (ML) is increasingly used to predict AMR phenotypes directly from genomic or transcriptomic data [42]. These are typically supervised learning models that use features like gene presence/absence, single-nucleotide variants (SNVs), k-mers, or gene expression data to predict resistance labels (e.g., susceptible/resistant or MIC values) [42].
A key advancement is the use of ML to identify minimal, predictive gene signatures. For example, a study on Pseudomonas aeruginosa used a genetic algorithm (GA) coupled with automated ML (AutoML) on transcriptomic data from 414 clinical isolates. This approach identified minimal gene sets (~35-40 genes) that could predict resistance to meropenem, ciprofloxacin, tobramycin, and ceftazidime with accuracies of 96-99% [43]. Notably, these predictive gene sets showed limited overlap (2-10%) with known resistance markers in CARD, highlighting significant knowledge gaps and the potential of ML to uncover novel elements of the intrinsic resistome [43].
Experimental Validation and Functional Analysis
Computational predictions require rigorous experimental validation to confirm the role of identified genes in intrinsic resistance.
Genome-Wide Mutant Screens
A primary method for mapping the intrinsic resistome is through systematic screening of mutant libraries [31]. The Keio collection, an E. coli knockout library of ~3,800 non-essential genes, is a key resource [3].
Protocol: High-Throughput Susceptibility Screening of a Knockout Library
- Culture Preparation: Grow individual knockout strains in 96-well or 384-well plates in a rich medium like LB.
- Antibiotic Exposure: Inoculate duplicate plates containing growth media supplemented with an antibiotic at a predetermined concentration (e.g., the IC₅₀ for the wild-type strain) and a control plate without antibiotic.
- Phenotypic Measurement: Measure optical density (OD₆₀₀) after a standardized incubation period to quantify growth.
- Data Analysis: Calculate growth inhibition for each knockout relative to the wild-type control. Knockouts exhibiting significantly lower growth in antibiotic-containing media than in control media, but with normal growth in control media, are classified as hypersusceptible. A common threshold is growth lower than two standard deviations from the median of the distribution [3].
- Functional Enrichment: Analyze the list of hypersusceptible mutants for enrichment of specific biological pathways (e.g., cell envelope biogenesis, membrane transport) using databases like Ecocyc [3].
This approach in E. coli has identified hypersusceptible knockouts in genes involved in efflux (acrB), cell envelope biogenesis (rfaG, lpxM), and information transfer pathways [3].
Experimental Evolution and Resistance Proofing
To evaluate if disrupting intrinsic resistance mechanisms can limit the evolution of high-level resistance ("resistance proofing"), experimental evolution under antibiotic pressure is used.
Protocol: Laboratory Evolution of Hypersusceptible Mutants
- Strain Selection: Select hypersusceptible knockout strains (e.g., ΔacrB, ΔrfaG) and the wild-type progenitor.
- Passaging Under Selection: Propagate replicate populations in liquid culture or on solid media containing a high, inhibitory concentration of antibiotic over multiple generations.
- Monitoring Adaptation: Regularly monitor population density and survival. Populations that drive to extinction are considered to have a compromised ability to evolve resistance.
- Characterizing Mutations: Sequence the genomes of evolved populations that recover growth to identify resistance-conferring mutations (e.g., in target enzymes like folA for trimethoprim) [3].
This method has shown that while inhibiting efflux pumps like AcrB compromises the ability to evolve resistance, bacteria can sometimes adapt via mutations in drug-specific pathways, bypassing the need for the missing intrinsic resistance element [3].
The Researcher's Toolkit
Table 3: Essential Reagents and Resources for Intrinsic Resistome Research
| Category | Item/Reagent | Function & Application |
|---|---|---|
| Biological Resources | Keio E. coli Knockout Collection [3] | Genome-wide library of single-gene deletions for high-throughput functional screening. |
| Clinical Isolate Libraries (e.g., 414 P. aeruginosa isolates [43]) | Diverse strain collections for training and validating ML models and studying resistance epidemiology. | |
| Computational Tools | CARD & RGI [38] | Reference database and tool for homology-based identification of known ARGs. |
| antiSMASH [39] | Platform for identifying biosynthetic gene clusters in genomic and metagenomic data. | |
| DeepARG & AMRLearn [41] [38] | ML-based tools for predicting novel ARGs and linking genotypes to resistance phenotypes. | |
| Laboratory Reagents | Trimethoprim, Chloramphenicol, etc. [3] | Broad-spectrum antibiotics for phenotypic screening and selection pressure in evolution experiments. |
| Efflux Pump Inhibitors (e.g., Chlorpromazine, Piperine) [3] | Chemical inhibitors used to pharmacologically mimic genetic knockout of efflux systems. | |
| Analysis Software | Genetic Algorithm (GA) & AutoML Frameworks [43] | For feature selection and model building from high-dimensional transcriptomic or genomic data. |
| MultiGeneBlast/ClusterBlast [39] | For comparative analysis of gene clusters across different genomes. |
Diagram 2: From Resistome Discovery to Application
The mining of intrinsic resistomes through genomic and metagenomic approaches has fundamentally expanded our understanding of antibiotic resistance. It reveals that baseline resistance is a complex phenotype orchestrated by a network of genes far beyond a few canonical efflux pumps or permeability barriers. The integration of sophisticated bioinformatics databases, machine learning models capable of discovering novel predictive signatures, and robust experimental validation protocols provides a powerful framework for continued discovery. This field holds immense promise for addressing the AMR crisis, not only by improving our ability to predict resistance but also by identifying novel, high-value targets for combination therapies. Inhibiting elements of the intrinsic resistome, particularly those like efflux pumps that are difficult for bacteria to bypass evolutionarily, offers a viable path to "resistance-proof" existing antibiotics and revitalize our antimicrobial arsenal [3]. Future efforts must focus on expanding these analyses across a wider range of bacterial pathogens and translating these foundational insights into clinically effective adjuvant therapies.
Structural Biology and OM Permeability Assays to Quantify Drug Uptake
Within the framework of intrinsic antibiotic resistance research, the bacterial outer membrane (OM) stands as a primary defensive barrier. Many bacterial species are classified as intrinsically resistant to a range of antimicrobial agents due to the innate low permeability of their cellular envelopes, which severely limits drug uptake [24] [44]. This reduced uptake, often coupled with the activity of multidrug efflux pumps, prevents many therapeutic compounds from reaching their intracellular targets at effective concentrations [18]. The study of the intrinsic resistome—the set of chromosomally encoded elements that contribute to the natural, baseline level of antibiotic resistance in a bacterial species—has revealed that permeability is a cornerstone of this phenotype [44]. Understanding and quantifying drug penetration through the OM is therefore not merely a technical exercise but a fundamental pursuit in overcoming a major mechanism of treatment failure.
Structural biology provides the essential tools to deconstruct this barrier at an atomic level. By elucidating the three-dimensional structures of OM proteins, such as porins and transporters, researchers can visualize the molecular sieves and gates that control the influx of compounds [18]. When these structural insights are integrated with functional OM permeability assays, a powerful pipeline emerges. This combination allows scientists to move beyond correlative observations and establish causative links between molecular architecture and drug permeation rates, thereby providing a quantitative framework for assessing a compound's potential efficacy against intrinsically resistant pathogens.
Core Concepts: The Outer Membrane and the Intrinsic Resistome
The Gram-Negative Outer Membrane as a Selective Barrier
The Gram-negative bacterial outer membrane is an asymmetric bilayer that serves as a formidable physical and functional obstacle to hydrophobic molecules and large antibiotics. Its inner leaflet is composed of phospholipids, while the outer leaflet is made up of lipopolysaccharide (LPS), whose dense, negatively charged carbohydrate core presents a formidable hurdle to the passive diffusion of many antimicrobials [18]. The passage of small, hydrophilic molecules, including many antibiotics, is largely governed by porins—beta-barrel protein channels that form water-filled pores across the membrane. The specificity, size, and abundance of these porins are thus critical determinants of intrinsic resistance. Variations in porin expression and structure between bacterial species contribute significantly to their characteristic susceptibility profiles [44].
Defining the Intrinsic Resistome
The intrinsic resistome encompasses all chromosomal genes that contribute to the baseline level of antibiotic resistance in a bacterium, independent of acquired resistance mechanisms [44]. As illustrated in the search results, this includes not only classical resistance genes but also a wide array of elements involved in basic bacterial metabolism and physiology. The major mechanisms constituting the intrinsic resistome include:
- Reduced Uptake: Mediated by the impermeability of the OM and the selectivity of porins.
- Active Efflux: The activity of constitutively expressed multidrug efflux pumps that expel toxins from the cell.
- Lack of Target: The absence or structural incompatibility of the drug's target within the organism.
- Antibiotic Inactivation: The presence of chromosomally encoded enzymes that modify or destroy the drug [24] [44] [18].
The following table summarizes key examples of intrinsic resistance and their underlying causes, highlighting the central role of permeability.
Table 1: Examples of Intrinsic Antibiotic Resistance in Bacterial Pathogens
| Bacterial Species | Intrinsic Resistance To | Primary Mechanism(s) |
|---|---|---|
| Pseudomonas aeruginosa | Aminoglycosides, many β-lactams | Low OM permeability, efflux pumps [18] |
| Escherichia coli | Macrolides (e.g., erythromycin) | Efflux (AcrAB-TolC) [44] |
| Enterococci | Aminoglycosides, cephalosporins | Low-affinity drug targets, impermeability [18] |
| Klebsiella spp. | Ampicillin | Production of chromosomally encoded β-lactamase [18] |
| Stenotrophomonas maltophilia | Aminoglycosides, carbapenems | Enzymatic inactivation, efflux, permeability [18] |
Structural Biology Techniques for OM Permeability Assays to Visualize Molecular Sieves
Structural biology techniques provide atomic-resolution blueprints of the components that govern molecular transit across the outer membrane. The primary goal is to characterize the architecture of porins and other channels to understand the physico-chemical rules of permeation.
Key Structural Biology Methods
X-ray Crystallography has been the workhorse for determining the first high-resolution structures of major porins like OmpF and OmpC, revealing the precise dimensions of the pore and the intricate "eyelet" region that dictates selectivity. Cryo-Electron Microscopy (Cryo-EM) is increasingly valuable for solving structures of larger complexes, such as full efflux pumps embedded in membranes, which are often difficult to crystallize. Nuclear Magnetic Resonance (NMR) Spectroscopy offers unique insights into the dynamics and conformational flexibility of these proteins in a near-native lipid environment.
The structural parameters derived from these techniques are directly relevant to permeability. These include the pore diameter and electrostatic potential of the channel lumen, which filter molecules by size and charge, respectively. Furthermore, visualizing antibiotics bound within these pores (e.g., via co-crystallization) can reveal specific molecular interactions that either facilitate or hinder passage [18].
Integrating Structure with Function: A Workflow
The power of structural biology is fully realized when its findings are integrated with functional permeability data. The following diagram illustrates the cyclical workflow of hypothesis, experimentation, and validation that defines this integrative approach.
Workflow for Integrating Structural and Permeability Data
Experimental Protocols: Quantitative OM Permeability Assays
To translate structural insights into quantitative metrics, robust functional assays are required. The following sections provide detailed methodologies for key experiments.
Liposome Swelling Assay
This classic assay measures the passive diffusion of compounds through purified porins reconstituted into artificial liposomes.
Detailed Protocol:
- Liposome Preparation: Dissolve phospholipids (e.g., DPhPC) in chloroform and dry under nitrogen to form a thin film. Rehydrate the film in a buffer containing a high concentration of a test solute (e.g., 100 mM potassium phosphate, pH 7.2).
- Porin Reconstitution: Purify the porin of interest (e.g., OmpF) via detergent extraction and chromatography. Mix the purified porin with the pre-formed liposomes. Remove detergent via dialysis or adsorption beads to form proteoliposomes with incorporated porin channels.
- Osmotic Response Measurement: Dilute the proteoliposomes into an iso-osmotic solution of the test antibiotic. The rapid diffusion of the small antibiotic through the porins creates a transient osmotic imbalance, causing water to enter and the liposomes to swell.
- Data Acquisition and Analysis: Monitor the change in light scattering (absorbance at 400-600 nm) over time using a stopped-flow apparatus or a standard spectrophotometer. The initial rate of decrease in absorbance is proportional to the permeability coefficient of the antibiotic through the porin. Compare rates against controls with empty liposomes (no porin) and with reference solutes of known permeability.
Microfluidics and Single-Cell Analysis
Advanced techniques now allow for the quantification of drug uptake at the single-cell level, capturing population heterogeneity.
Detailed Protocol (based on quantitative Single-Cell Mass Spectrometry principles [45]):
- Cell Preparation and Loading: Culture bacterial cells to mid-log phase. Load a dilute cell suspension into a custom microfluidic chip or glass chip with microwells designed to trap individual cells.
- Drug Exposure and Uptake: Perfuse the chip with a defined concentration of the antibiotic dissolved in growth medium. Control the exposure time precisely.
- Single-Cell Sampling: For mass spectrometry-based quantification, a specialized sampling probe (e.g., a "Single-probe" with a tip diameter of ~10 µm) is inserted into a single cell within its microwell. A sampling solvent containing an internal standard is continuously delivered into the cell, extracting cellular contents.
- Mass Spectrometry Analysis: The extract is immediately ionized at the nano-ESI emitter of the probe and analyzed by a high-sensitivity mass spectrometer. The internal standard allows for absolute quantification of the intracellular drug concentration.
- Data Analysis: Calculate the drug accumulation in each individual cell (moles/cell). The distribution of accumulation levels across hundreds of cells reveals heterogeneity in permeability and efflux activity within the population.
Data Integration and Analysis
The quantitative data generated from these assays are critical for building predictive models. The table below summarizes key parameters and their significance.
Table 2: Key Quantitative Parameters from OM Permeability Assays
| Parameter | Description | Assay Type | Significance for Resistance |
|---|---|---|---|
| Permeability Coefficient (P) | Rate of solute flux across the membrane per unit concentration gradient. | Liposome Swelling | Direct measure of the intrinsic permeability of a compound via a specific pathway. Low P indicates a strong permeability barrier. |
| Half-Time of Swelling (t₁/₂) | Time for liposome absorbance to decrease by half. | Liposome Swelling | Indirect measure of permeability; inversely related to P. A longer t₁/₂ indicates slower diffusion. |
| Intracellular Concentration ([C]in) | Moles of drug per cell or per unit cell volume at a given time. | Single-Cell MS, LC/MS of Lysates | Reflects the net effect of influx (permeability) and efflux. Low [C]in is indicative of either poor uptake or active efflux. |
| Accumulation Ratio | Ratio of intracellular to extracellular drug concentration ([C]in/[C]out). | Various | A ratio <1 often suggests active efflux is dominating; a ratio >1 suggests active uptake or trapping. |
| Minimum Inhibitory Concentration (MIC) | The lowest concentration of drug that inhibits visible growth. | Broth Microdilution | The ultimate functional readout. Correlating MIC with permeability parameters validates their biological relevance. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the described protocols relies on a suite of specialized reagents and tools. The following table catalogs essential items for researchers in this field.
Table 3: Research Reagent Solutions for OM Permeability Studies
| Category | Item / Reagent | Function / Application | Key Considerations |
|---|---|---|---|
| Biological Models | E. coli OmpF/OmpC knockout strains | Isogenic hosts for porin reconstitution studies to define specific channel contributions. | Ensures clean background for functional assays. |
| P. aeruginosa clinical isolates | Models for studying complex, clinically relevant intrinsic resistance. | High intrinsic resistance due to low permeability and potent efflux. | |
| Caco-2 cell line [46] | In vitro model of intestinal epithelium for parallel studies on drug absorption. | Not a bacterial model, but useful for ADME/Tox context in drug development. | |
| Assay Kits & Reagents | BD Cytofix/Cytoperm Buffer [47] | Fixation and permeabilization of cells for intracellular staining; can be optimized for OM studies. | Requires optimization to minimize impact on RNA/protein integrity [47]. |
| Liposome Kits (e.g., from Avanti Polar Lipids) | Pre-formed lipids for creating consistent, defined model membranes. | Saves time and improves reproducibility in liposome swelling assays. | |
| Dodecyl Maltoside (DDM) [48] | Mild detergent for solubilizing membrane proteins while preserving native structure. | Critical for the purification of stable, functional porins. | |
| Tools & Equipment | Single-probe MS Device [45] | Microscale sampling and ionization device for live, single-cell mass spectrometry. | Enables absolute quantification of drugs in individual live cells. |
| Stopped-Flow Spectrophotometer | Apparatus for measuring rapid kinetic events, such as liposome swelling (millisecond resolution). | Essential for obtaining accurate initial rates in swelling assays. | |
| HiseqX / NextSeq Sequencing Platforms [47] | High-throughput sequencing to monitor global transcriptional responses to permeabilization. | Identifies compensatory changes in the resistome upon membrane disruption. |
Data Interpretation and Integration with the Broader Resistome
Interpreting permeability data requires a holistic view of the bacterial cell. A low accumulation ratio from a single-cell MS experiment, for instance, does not automatically imply poor permeability. It could be the result of highly efficient efflux. Therefore, conditional experiments are essential. Repeating the assay in the presence of an efflux pump inhibitor (e.g., PaβN for RND-type pumps) can disentangle the contributions of influx and efflux. A significant increase in drug accumulation upon inhibitor addition indicates that efflux was masking a reasonably permeable OM.
The relationship between the OM and other elements of the intrinsic resistome can be visualized as an interconnected network, as shown below.
Interplay of OM Permeability with Broader Resistome
This systems-level understanding is crucial for designing effective therapeutic strategies. For example, the discovery that the global regulator Crc in P. aeruginosa modulates both carbon metabolism and susceptibility to antibiotics underscores the deep connection between central metabolism and the intrinsic resistome [44]. Inhibiting such a regulator could simultaneously increase membrane permeability and decrease efflux pump expression, sensitizing the bacterium to existing drugs.
Future Directions and Therapeutic Applications
The ultimate goal of quantifying drug uptake is to inform the design of novel antibiotics or adjuvant therapies that circumvent the permeability barrier. Structural insights are directly feeding into structure-based drug design. For instance, knowing the exact diameter and electrostatics of the primary porins in a pathogen like P. aeruginosa allows medicinal chemists to tailor drug properties (e.g., molecular weight, hydrophobicity, charge) to favor uptake, as demonstrated in computational studies targeting tubulin [49].
A particularly promising avenue is the development of efflux pump inhibitors. These adjuvants, administered alongside conventional antibiotics, aim to neutralize a key component of the intrinsic resistome. By blocking the pump, they allow the antibiotic to accumulate inside the cell, effectively resensitizing the bacterium to treatment [44]. This approach could "re-purpose" antibiotics that are currently ineffective against intrinsically resistant pathogens.
Furthermore, the integration of machine learning with high-throughput permeability and structural data is poised to revolutionize the field. As shown in a study on tubulin inhibitors, ML models can be trained to predict the activity of compounds based on their chemical features and potential for uptake, dramatically accelerating the virtual screening of millions of compounds before synthesis [49]. This powerful combination of structural biology, quantitative assays, and computational prediction represents the future of overcoming intrinsic antibiotic resistance.
Characterizing Efflux Pump Kinetics and Regulation in Model Pathogens
Efflux pumps are transmembrane transporter proteins that actively extrude toxic substrates, including antibiotics, from bacterial cells. They are fundamental components of the cell envelope and play a critical role in intrinsic antibiotic resistance by significantly reducing intracellular drug concentrations [50] [51]. In many bacterial pathogens, the constitutive expression of these systems provides a baseline level of resistance, which can be further amplified through regulatory mutations leading to pump overexpression, thereby contributing to multidrug-resistant (MDR) phenotypes [19] [52]. The study of efflux pump kinetics—quantifying the rates of drug influx and efflux—is essential for understanding their contribution to resistance and for developing strategies to overcome it, such as the discovery of efflux pump inhibitors (EPIs) [50] [51].
This guide focuses on characterizing these systems in model pathogens like Escherichia coli and Acinetobacter baumannii. E. coli, particularly the K-12 strain and its derivatives, serves as a primary model for Gram-negative bacteria due to its well-characterized efflux systems, such as the major tripartite pump AcrAB-TolC [50] [51]. The nosocomial pathogen A. baumannii is another critical model organism, as it often carries numerous chromosomally encoded efflux pumps, making it a classic example of a pathogen that can exhibit MDR to pan-drug resistance [52].
Efflux Pump Families and Their Molecular Mechanisms
Bacterial efflux pumps are categorized into several families based on their structure, energy coupling, and phylogenetic relationships. The most clinically significant families, particularly in Gram-negative bacteria, are detailed below.
Resistance-Nodulation-Division (RND) Family: These are the most potent multidrug efflux systems in Gram-negative bacteria. They form tripartite complexes that span the entire cell envelope. The complex consists of an inner membrane RND transporter (e.g., AcrB in E. coli, AdeB in A. baumannii), a periplasmic adapter protein (PAP or MFP; e.g., AcrA, AdeA), and an outer membrane factor (OMF; e.g., TolC, AdeC) [19] [52]. These pumps use the proton motive force as an energy source and can transport a wide array of substrates directly from the periplasm or cytoplasm to the external environment [51] [52].
Major Facilitator Superfamily (MFS): This is the largest known superfamily of secondary active transporters. MFS pumps typically possess 12 or 14 transmembrane segments and function as secondary transporters, utilizing ion gradients to drive substrate efflux [19] [51].
ATP-Binding Cassette (ABC) Superfamily: These are primary active transporters that derive energy from ATP hydrolysis. They consist of two nucleotide-binding domains (NBDs) and two transmembrane domains (TMDs) [19]. While some ABC transporters are involved in multidrug resistance, others have specific physiological functions, such as the MacAB system involved in pathogenicity [51].
Other Families: Additional families include the Multidrug and Toxic Compound Extrusion (MATE) family, which exchange protons or sodium ions; the Small Multidrug Resistance (SMR) family, characterized by small size and four transmembrane segments; and the more recently identified Proteobacterial Antimicrobial Compound Efflux (PACE) family, involved in biocide resistance [19] [51].
Table 1: Major Efflux Pump Families in Model Pathogens
| Family | Energy Source | Typical Architecture | Key Examples in Model Pathogens |
|---|---|---|---|
| RND | Proton Motive Force | Tripartite (IM-PAP-OM) | AcrAB-TolC (E. coli), AdeABC (A. baumannii) |
| MFS | Ion Gradients | Single-component (12-14 TMS) | TetA (E. coli), MefA (A. baumannii) |
| ABC | ATP Hydrolysis | Single or multi-component (2 NBDs, 2 TMDs) | MacAB (E. coli, Salmonella) |
| MATE | H+/Na+ Antiport | Single-component (12 TMS) | NorM (V. parahaemolyticus) |
| SMR | Proton Motive Force | Homotrimer (4 TMS each) | EmrE (E. coli) |
| PACE | Proton Motive Force | Single-component (4 TMS) | AceI (A. baumannii) |
Experimental Protocols for Kinetic Analysis
A critical step in understanding efflux-mediated resistance is the accurate quantification of transport activity. The following protocol describes a semi-automated fluorometric method for determining the kinetics of ethidium bromide (EtBr) efflux, a common efflux pump substrate.
Fluorometric Determination of Efflux Kinetics
Principle: This method leverages the fluorescent properties of EtBr, which exhibits weak fluorescence in aqueous solution but becomes strongly fluorescent upon binding to cellular components like DNA. The real-time monitoring of fluorescence allows for the discrimination between accumulation (net result of influx and efflux) and active efflux [50].
Materials and Reagents:
- Bacterial Strains: Use isogenic strains differing in efflux pump expression. A recommended set includes:
- Wild-type strain (e.g., E. coli AG100).
- Efflux pump knockout mutant (e.g., E. coli AG100A, ΔacrAB).
- Efflux pump overexpressing mutant (e.g., E. coli AG100TET) [50].
- Growth Media: Luria-Bertani (LB) broth and agar.
- Buffers and Solutions: Phosphate Buffered Saline (PBS), glucose solution.
- Substrates and Inhibitors: Ethidium bromide (EtBr) stock solution, efflux pump inhibitor such as Chlorpromazine (CPZ) or Phe-Arg-β-naphthylamide (PAβN).
- Equipment: Real-time fluorometer (e.g., Rotor-Gene 3000) or a fluorescence plate reader, spectrophotometer for measuring optical density, microcentrifuge, and water bath.
Procedure:
- Cell Preparation and Loading:
- Grow bacterial strains to mid-exponential phase (OD600 ~0.5) in LB broth under appropriate conditions.
- Harvest cells by centrifugation (e.g., 5,000 x g for 10 minutes) and wash twice with PBS to remove residual media.
- To load the cells with the fluorescent substrate, resuspend the cell pellet in PBS containing a sub-inhibitory concentration of EtBr (e.g., 2-10 µg/mL) and incubate for 30-60 minutes to allow for accumulation. The presence of glucose (e.g., 0.4%) during this loading step can enhance accumulation by providing energy that may be co-opted for efflux [50].
- Efflux Assay:
- After loading, harvest the cells by centrifugation and wash thoroughly with PBS to remove extracellular EtBr.
- Resuspend the cell pellet in PBS. Distribute the cell suspension into aliquots in the fluorometer tubes or plate.
- To establish a baseline, measure fluorescence for 1-2 minutes (λex ~530 nm, λem ~590 nm).
- Initiate efflux by adding a source of energy. This is typically done by adding glucose (e.g., 0.4% final concentration) to the cell suspension. Continuously monitor the decrease in fluorescence over time (e.g., 30-60 minutes) as EtBr is actively extruded from the cells.
- Inhibitor Controls: For specific aliquots, add a known EPI (e.g., 100 µg/mL CPZ) simultaneously with glucose. The inhibitor should cause a significant reduction in the rate of fluorescence decrease, confirming that the signal is due to active efflux.
- Energy Depletion Control: Perform the assay in the absence of glucose or at a low temperature (e.g., 4°C) to confirm that efflux is an energy-dependent process [50].
Data Analysis and Kinetic Modeling: The raw fluorescence data is processed to calculate the rate of efflux. A simple experimental model can be applied to describe the transport kinetics, integrating passive influx and active efflux of EtBr [50].
- The efflux rate constant (k_- ) can be determined by fitting the fluorescence decay curve to a first-order exponential decay model.
- Comparing the k_- values between the wild-type, knockout, and overexpressing strains quantitatively demonstrates the contribution of the specific efflux system to the overall efflux capacity. For example, the calculated efflux rate for an AcrAB-overexpressing strain (AG100TET) was found to be approximately twice that of the wild-type strain [50].
Quantitative Analysis of Efflux Kinetics and Regulation
The kinetic parameters derived from experiments like the fluorometric assay above provide a quantitative framework for comparing efflux capacity across different genetic backgrounds or under inhibitory conditions.
Table 2: Experimental Efflux Rates of Ethidium Bromide in E. coli Strains
| E. coli Strain | Relevant Genotype/Phenotype | Calculated Efflux Rate (min⁻¹) | Implication |
|---|---|---|---|
| AG100 | Wild-type (functional AcrAB-TolC) | 0.0173 ± 0.0057 | Baseline efflux activity |
| AG100A | ΔacrAB::Tn903 (AcrAB inactivated) | 0.0106 ± 0.0033 | Significantly reduced efflux, confirming AcrAB's major role |
| AG100TET | Tetracycline-induced AcrAB overexpression | 0.0230 ± 0.0075 | Enhanced efflux capacity, demonstrating inducible resistance |
The regulation of efflux pump expression is complex and often involves local repressors and global regulatory networks. Key regulatory mechanisms include:
- Local Regulators: Many efflux pump operons are controlled by adjacent genes encoding transcriptional regulators. For example, the adeABC operon in A. baumannii is regulated by the AdeRS two-component system, where mutations can lead to pump overexpression and consequent multidrug resistance [52].
- Global Regulators: Efflux pumps are also integrated into broader cellular responses. They can be under the control of global transcription factors like MarA, SoxS, and Rob in E. coli, which are activated in response to antibiotic stress and other environmental signals, leading to the coordinated upregulation of multiple resistance mechanisms [50] [51].
Diagram 1: Simplified regulatory pathway of efflux pump expression. Antibiotic stress activates both local and global regulators, which bind to the promoter regions of efflux pump operons, leading to increased production and a multidrug-resistant phenotype.
Advanced and Computational Approaches
Modern research extends beyond basic kinetics to incorporate advanced computational and data-driven methods.
Machine Learning (ML) in AMR Prediction: Unsupervised learning techniques, such as K-means clustering and Principal Component Analysis (PCA), are being applied to analyze patterns in large genomic datasets of antimicrobial resistance genes (ARGs). These methods can identify inherent structures and relationships, such as clustering of genes by length or resistance class, offering novel insights into potential resistance mechanisms and informing predictive models [53].
Molecular Docking and EPI Screening: Computational approaches are invaluable for identifying potential EPIs. Homology modeling can be used to construct 3D models of efflux pumps based on known structures. Molecular docking simulations, using protocols like CDOCKER, can then predict the binding interactions and affinities of thousands of compounds from chemical libraries (e.g., Traditional Chinese Medicine libraries) against these models, prioritizing candidates for experimental validation [54].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Efflux Pump Studies
| Reagent / Tool | Function / Purpose | Example Use Case |
|---|---|---|
| Ethidium Bromide (EtBr) | Model fluorescent substrate for efflux pumps. | Kinetic assays to measure real-time efflux activity [50]. |
| Chlorpromazine (CPZ) | Broad-spectrum efflux pump inhibitor. | Positive control to confirm efflux-mediated signal in inhibition assays [50]. |
| Phe-Arg-β-naphthylamide (PAβN) | Broad-spectrum EPI for RND pumps. | Restoring antibiotic susceptibility in Gram-negative bacteria [52]. |
| Glucose | Energy source for proton motive force-dependent pumps. | Used to energize cells and initiate active efflux in assays [50]. |
| Isogenic Strain Panel | Genetically defined strains (WT, knockout, overexpressor). | Directly linking efflux pump genotype to phenotypic output [50]. |
| Verapamil | Known EPI for mammalian P-glycoprotein, also inhibits some bacterial pumps. | Used as a positive control in EPI screening studies [54]. |
Diagram 2: Core workflow for kinetic characterization of efflux pumps, from cell preparation to data analysis.
In conclusion, the precise characterization of efflux pump kinetics and their regulatory mechanisms is a cornerstone of intrinsic antibiotic resistance research. The methodologies outlined here, from robust experimental protocols to emerging computational tools, provide a framework for researchers to quantify efflux activity, elucidate regulatory pathways, and identify novel inhibitors, thereby contributing to the global effort to combat multidrug-resistant bacterial pathogens.
AI-Driven Discovery of Antibiotics Bypassing Intrinsic Resistance
The escalating global antimicrobial resistance (AMR) crisis poses a formidable challenge to modern medicine, with drug-resistant infections contributing to approximately 4.95 million deaths annually and projected to reach 10 million by 2050 if unaddressed [1]. A fundamental barrier in treating infections, particularly those caused by Gram-negative pathogens, is intrinsic antibiotic resistance—a naturally occurring phenomenon universal within bacterial species and independent of horizontal gene transfer [4]. This resistance dramatically limits therapeutic options and is primarily mediated by the Gram-negative outer membrane, which exhibits limited permeability, and the expression of multidrug efflux pumps that effectively reduce intracellular drug concentrations [18] [4]. Traditional antibiotic discovery approaches, reliant on prospecting in nature or modifying existing compounds, have struggled to overcome these barriers, with no new antibiotic class discovered in decades [55].
The advent of artificial intelligence (AI) represents a paradigm shift in antibiotic discovery, offering powerful tools to design compounds that bypass intrinsic resistance mechanisms. By leveraging machine learning (ML) and generative AI, researchers can now explore previously inaccessible chemical spaces to identify or create molecules capable of penetrating bacterial membranes or disrupting essential cellular processes that are not targeted by conventional antibiotics [56] [55]. This technical guide examines the core mechanisms of intrinsic resistance, details AI methodologies being deployed against them, and provides experimental frameworks for validating novel anti-infectives, contextualized within the broader research landscape of intrinsic resistance mechanisms.
Core Mechanisms of Intrinsic Antibiotic Resistance
Permeability Barriers and Efflux Systems
Intrinsic resistance in bacteria is primarily orchestrated by two key physiological features: the permeability barrier of the outer membrane and the activity of efflux pumps. In Gram-negative bacteria, the outer membrane serves as a formidable obstacle due to its asymmetric structure containing lipopolysaccharide (LPS) in the outer leaflet, which reduces fluidity and creates a hydrophilic surface that repels many antibiotics [4]. The passage of molecules across this membrane is largely governed by porin proteins, which form water-filled channels with molecular size and charge selectivity. The intrinsic resistance profiles of many Gram-negative pathogens, including Pseudomonas aeruginosa and Acinetobacter baumannii, are directly attributable to their low outer membrane permeability and specific porin characteristics [18] [4].
Complementing the permeability barrier, active efflux systems provide a second layer of intrinsic resistance by pumping toxic compounds, including antibiotics, out of the bacterial cell. These multidrug efflux pumps, particularly the Resistance-Nodulation-Division (RND) family in Gram-negative bacteria, can transport a broad spectrum of structurally unrelated antimicrobials, conferring a multidrug-resistant (MDR) phenotype [4] [57]. The synergistic action of reduced permeability and active efflux creates an exceptionally effective defense system, as the slowed influx through the membrane allows efflux pumps to maintain low intracellular antibiotic concentrations [4]. This combination presents a critical challenge that conventional antibiotic discovery approaches have largely failed to overcome, necessitating innovative strategies that can bypass these intrinsic resistance mechanisms.
Additional Genetic Components of the Intrinsic Resistome
Beyond the classical permeability and efflux mechanisms, genome-wide studies have revealed that the intrinsic resistome comprises a surprisingly complex network of genetic determinants. Screening of gene inactivation and transposon insertion libraries has identified numerous chromosomal genes that contribute to intrinsic resistance levels, even in the absence of acquired resistance mechanisms [4]. These elements include various housekeeping genes, metabolic enzymes, and regulatory factors that indirectly influence antibiotic susceptibility through diverse physiological pathways.
The molecular basis of intrinsic resistance predates the clinical use of antibiotics and is abundantly present in environmental organisms. Soil-dwelling bacteria, for instance, possess extensive intrinsic resistomes containing resistance determinants identical to those circulating in clinical pathogens, highlighting the environmental origins of many resistance elements [4]. This observation suggests that intrinsic resistance represents an ancient bacterial defense strategy that has evolved over millennia rather than a recent response to anthropogenic antibiotic use. The complexity of the intrinsic resistome presents both a challenge and an opportunity—while it complicates treatment options, targeting non-essential components of this network could potentially rejuvenate existing antibiotics by inducing hyper-susceptibility in otherwise resistant pathogens [4].
AI Methodologies for Bypassing Intrinsic Resistance
Generative AI for Novel Compound Design
Generative AI approaches have emerged as powerful tools for designing structurally novel antibiotics that can circumvent intrinsic resistance mechanisms. Researchers at MIT employed two distinct generative AI strategies to design compounds effective against resistant pathogens: a fragment-based approach for targeting Neisseria gonorrhoeae and an unconstrained design method against methicillin-resistant Staphylococcus aureus (MRSA) [56]. For the fragment-based approach, researchers began with a library of approximately 45 million chemical fragments, which were screened using ML models trained to predict antibacterial activity against N. gonorrhoeae. After applying filters for cytotoxicity and similarity to existing antibiotics, they identified a promising fragment (F1) that served as the foundation for generating additional compounds using two generative algorithms: Chemically Reasonable Mutations (CReM) and Fragment-Based Variational Autoencoder (F-VAE) [56].
The unconstrained design approach demonstrated even greater innovation by allowing generative models to freely design molecules based solely on the general rules of chemical plausibility, without being constrained to specific fragments. Using the same algorithms (CReM and VAE), researchers generated over 29 million compounds, which were then filtered for synthetic feasibility and predicted activity against MRSA [56]. This strategy resulted in the identification of compound DN1, which demonstrated efficacy in clearing MRSA skin infections in a mouse model. Both approaches yielded compounds structurally distinct from existing antibiotics and appearing to work through novel mechanisms, primarily involving disruption of bacterial membrane integrity—a target that bypasses traditional resistance pathways [56].
Machine Learning for Mining Biological and Chemical Space
Beyond generative design, ML algorithms are being deployed to mine vast biological and chemical datasets for novel antimicrobial candidates. A prominent strategy involves mining ancient proteomes for antimicrobial peptides (AMPs) with potent activity against contemporary pathogens. Researchers at the University of Pennsylvania have developed ML models that parse through genomic and proteomic sequencing data spanning the Tree of Life, including extinct organisms such as Neanderthals, Denisovans, and woolly mammoths [55]. These models identify snippets encoding products with predicted antimicrobial potential, particularly focusing on AMPs—short amino acid sequences with attractive antibiotic properties.
The underlying AI architectures for these discovery approaches vary based on the data type and discovery goal. For chemical compound screening, random forest models and neural networks are frequently employed to predict antibacterial activity based on structural features [58]. For peptide discovery, recurrent neural networks (RNNs) and Hidden Markov models can identify and classify antimicrobial sequences based on patterns in amino acid distribution [58]. The effectiveness of these models hinges on the quality and volume of training data, with researchers increasingly assembling rigorously curated datasets that standardize biological measurements such as minimum inhibitory concentrations (MICs) across diverse bacterial strains to ensure comparability and predictive accuracy [55].
Table 1: AI Approaches in Antibiotic Discovery
| AI Method | Key Features | Applications | Output Examples |
|---|---|---|---|
| Generative AI (CReM, F-VAE) | Starts with fragments or free generation; creates novel molecular structures | MRSA, N. gonorrhoeae | NG1, DN1 compounds |
| Proteome Mining ML | Analyzes genomic/proteomic data from extant and extinct organisms | AMP discovery against Gram-negative pathogens | Mammothisins, elephasins |
| Random Forest Models | Screens chemical libraries for predicted activity | β-lactamase inhibitor identification | 74 hit compounds |
| Neural Networks | Pattern recognition in chemical structures or amino acid sequences | Antimicrobial peptide identification | Novel AMPs with membrane disruption |
Experimental Protocols for Validation
Compound Screening and Mechanism of Action Studies
The transition from AI-predicted compounds to validated antibiotic candidates requires rigorous experimental protocols. For initial antibacterial activity screening, researchers employ standardized broth microdilution methods following Clinical and Laboratory Standards Institute (CLSI) guidelines to determine minimum inhibitory concentrations (MICs) against a panel of bacterial pathogens, including reference strains and clinically isolated multidrug-resistant variants [1] [18]. This initial screening should include both Gram-positive and Gram-negative species to assess spectrum of activity and potential intrinsic resistance bypass. For compounds showing promising MIC values, time-kill kinetics assays are performed to determine whether the antibacterial effect is bactericidal or bacteriostatic [18].
Mechanism of action studies are crucial for confirming novel targets and bypass of intrinsic resistance. For membrane-targeting compounds, researchers employ fluorescent membrane potential-sensitive dyes (e.g., DiSC₃(5)) to monitor membrane depolarization in real-time [56]. Additionally, transmission electron microscopy (TEM) can visualize ultrastructural changes in bacterial membranes following compound treatment. For compounds targeting specific proteins like LptA (involved in LPS transport), pull-down assays using biotinylated compound variants can confirm direct binding, while complementation experiments with plasmid-borne gene copies can verify target specificity [56]. To assess resistance bypass capability specifically, assays comparing compound accumulation in wild-type versus efflux pump-deficient strains can determine whether the compound is affected by major efflux systems [4].
Assessing Intrinsic Resistance Bypass
Specific protocols are required to evaluate how effectively novel compounds bypass intrinsic resistance mechanisms. For permeability assessment, researchers compare compound activity in wild-type strains versus those with genetically modified outer membranes, such as LPS-deficient mutants [4]. The N-phenyl-1-naphthylamine (NPN) uptake assay provides a quantitative measure of outer membrane permeability, with increased NPN fluorescence indicating enhanced penetration [4]. For efflux pump evasion, compounds are tested in the presence and absence of efflux pump inhibitors like phenylalanine-arginine β-naphthylamide (PAβN), with minimal differences in MIC indicating poor efflux pump recognition [4].
The intracellular accumulation of promising compounds can be directly quantified using liquid chromatography-mass spectrometry (LC-MS/MS) in bacterial cell lysates, providing definitive evidence of penetration capability [4]. For compounds predicted to target essential cellular processes behind permeability barriers, genetic approaches such as constructing conditional knockdown mutants of target genes can confirm essentiality and mechanism specificity [56]. These comprehensive validation workflows ensure that AI-discovered compounds truly bypass intrinsic resistance mechanisms rather than merely exhibiting moderate activity against resistant pathogens.
Table 2: Key Assays for Validating Bypass of Intrinsic Resistance
| Assay Type | Experimental Approach | Interpretation |
|---|---|---|
| MIC Determination | Broth microdilution per CLSI guidelines | Baseline activity against resistant strains |
| Membrane Depolarization | DiSC₃(5) fluorescence monitoring | Confirmation of membrane targeting |
| Outer Membrane Permeability | NPN uptake assay | Quantification of penetration in Gram-negatives |
| Efflux Pump Interaction | MIC with/without efflux pump inhibitors | Assessment of efflux recognition |
| Intracellular Accumulation | LC-MS/MS of bacterial lysates | Direct measurement of compound penetration |
| Target Engagement | Pull-down assays with biotinylated compounds | Verification of direct target binding |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for AI-Driven Antibiotic Discovery
| Reagent/Category | Function in Research | Examples/Specifications |
|---|---|---|
| Chemical Fragment Libraries | Basis for fragment-based generative AI design | Enamine's REAL space; 45+ million fragments [56] |
| Bacterial Strain Panels | In vitro validation of compound activity | Reference strains + MDR clinical isolates (e.g., CRKP, XDR Salmonella) [1] |
| Efflux Pump Inhibitors | Assessing efflux-mediated resistance | PAβN; CCCP for proton motive force disruption [4] |
| Membrane Permeability Probes | Quantifying outer membrane penetration | N-phenyl-1-naphthylamine (NPN); 1-N-phenylnaphthylamine [4] |
| Antimicrobial Peptide Databases | Training data for ML models | APD3; CAMP; curated natural and synthetic AMPs [55] |
| Molecular Probes for Viability | Distinguishing bactericidal vs. bacteriostatic activity | Resazurin; SYTOX Green; propidium iodide [18] |
| Genomic DNA from Extinct Species | Mining ancient biological diversity | Woolly mammoth; Neanderthal; Denisovan [55] |
Visualizing AI-Driven Antibiotic Discovery Workflows
AI-Driven Discovery Pipeline
AI-Driven Antibiotic Discovery Pipeline
Intrinsic Resistance Mechanisms and AI Bypass Strategies
Resistance Mechanisms and AI Bypass Strategies
The integration of AI methodologies into antibiotic discovery represents a transformative approach to addressing the persistent challenge of intrinsic resistance. By leveraging generative models to explore vast chemical spaces and machine learning to mine biological data across evolutionary timescales, researchers can now identify and design compounds that bypass traditional resistance mechanisms [56] [55]. These approaches have yielded promising candidates, such as the MIT-discovered compounds NG1 and DN1, which exhibit novel mechanisms of action targeting bacterial membrane integrity [56]. The continued refinement of these AI tools, coupled with robust experimental validation frameworks, offers renewed hope for overcoming the intrinsic resistance barriers that have limited antibiotic development for decades.
Looking forward, the success of AI-driven antibiotic discovery will depend on addressing several critical challenges. The economic barriers to antibiotic development remain substantial, with insufficient financial incentives for pharmaceutical companies despite the clear public health need [55] [59]. Additionally, the data quality used to train AI models requires continued standardization and expansion to improve predictive accuracy [55]. Future directions should focus on integrating AI across the entire drug development pipeline, from initial discovery through clinical trial optimization, and developing models that can simultaneously predict efficacy, toxicity, and synthetic feasibility [58]. As these technologies mature, they offer the potential to fundamentally reshape our approach to combating antimicrobial resistance, moving from reactive modifications of existing compounds to proactive design of novel therapeutics that preempt resistance mechanisms.
Application of the One Health Framework to Track Environmental Resistance Reservoirs
The global health crisis of antimicrobial resistance (AMR) necessitates innovative surveillance strategies that transcend traditional clinical settings. The One Health framework provides a holistic approach, recognizing the intricate interconnectedness of human, animal, and environmental health in the evolution and dissemination of resistant microorganisms [60] [61]. Environmental compartments function as critical reservoirs and amplifiers for antimicrobial resistance genes (ARGs) and resistant bacteria, facilitating their circulation back to humans and animals through water, soil, and food systems [60]. This technical guide details the application of the One Health framework for tracking environmental resistance reservoirs, providing researchers and drug development professionals with advanced methodologies to elucidate the complex dynamics of AMR. Focusing on mechanisms of intrinsic antibiotic resistance, this review synthesizes current experimental and computational approaches for resistome surveillance, essential for developing effective interventions against drug-resistant infections.
The One Health Perspective on Environmental AMR Reservoirs
The environment acts as a pivotal component in the AMR lifecycle, serving as a recipient of antimicrobial residues from agricultural, pharmaceutical, and municipal waste, and as a bioreactor where selection pressures favor the emergence and persistence of resistance [60]. Within the One Health triad, the environmental domain is characterized by several key features:
Resistance Hotspots: Specific environments, such as wastewater from pharmaceutical manufacturing, agricultural runoff, and untreated sewage, are recognized as significant AMR hotspots [60]. These locations introduce exceptionally high concentrations of active pharmaceutical ingredients (APIs) into ecosystems, creating intense selective pressure that favors resistant microbial populations and promotes horizontal gene transfer (HGT) [60].
Interconnected Transmission Pathways: AMR drivers are not sector-specific; wastewater effluents, agricultural runoff, and foodborne transmission create interconnected loops that facilitate the persistence of ARGs and HGT across human, animal, and environmental interfaces [60]. This interconnectedness underscores the necessity of a unified One Health strategy rather than compartmentalized approaches.
Climate Change as an Amplifier: Emerging evidence indicates that climate change accelerates AMR through increased temperatures, altered rainfall patterns, and extreme weather events [60]. These climatic factors create favorable conditions for the spread and persistence of resistant organisms and can disrupt water and sanitation infrastructure, particularly in vulnerable low- and middle-income countries (LMICs) [60].
Table 1: Major Environmental Sources and Pathways of AMR Dissemination
| Source Category | Specific Examples | Key Resistance Elements | Primary Exposure Pathways |
|---|---|---|---|
| Industrial Effluents | Pharmaceutical manufacturing discharge | High concentrations of APIs, ARBs, ARGs | Contaminated rivers, irrigation water, aquatic sediments [60] |
| Agricultural Systems | Manure amendment, aquaculture, runoff | ARGs (e.g., macrolide-lincosamide-streptogramin [MLS], tetracycline) | Soil contamination, food crops, groundwater [60] [62] |
| Municipal Wastewater | WWTP effluents, combined sewer overflows | Diverse ARGs, mobile genetic elements (MGEs) | Recreational water, drinking water sources, shellfish [63] |
| Food Systems | Animal products, produce irrigation | Zoonotic pathogens with ARGs (e.g., Salmonella, E. coli) | Food consumption, food handling [64] |
The conceptual foundation of the One Health approach to environmental AMR is visualized in Figure 1, which illustrates the interconnected pathways and intervention points.
Figure 1: One Health Framework for Environmental AMR Tracking. This diagram illustrates the interconnected pathways of AMR transmission between human, animal, and environmental domains, highlighting key reservoirs, drivers, and intervention points within the One Health approach.
Advanced Methodologies for Environmental Resistome Surveillance
Tracking environmental resistance reservoirs requires sophisticated techniques capable of detecting and quantifying diverse ARGs, often present at low abundances within complex microbial communities. This section details established and emerging methodologies for comprehensive resistome analysis.
Molecular Detection and Quantification Approaches
High-Throughput Quantitative PCR (HT-qPCR)
HT-qPCR enables simultaneous quantification of hundreds of predefined ARG targets across multiple samples, providing sensitive and quantitative data on resistome composition.
- Protocol Overview: DNA is extracted from environmental samples (water, sediment, soil) using commercial kits optimized for complex matrices. Primer sets targeting specific ARG classes (e.g., β-lactam, tetracycline, vancomycin resistance genes) and mobile genetic elements (MGEs) are used in multiplexed qPCR reactions performed on platforms such as the WaferGen SmartChip [63].
- Data Normalization: Results are typically normalized to both sample volume (for water) or mass (for solids) and to the 16S rRNA gene copy number to account for variations in bacterial biomass [63].
- Application Example: A recent study applied HT-qPCR to profile ARGs in wastewater and receiving environments, calculating an Antibiotic Resistance Gene Index (ARGI) as a standardized metric for comparing AMR levels across different wastewater treatment plants (WWTPs). The ARGI of the studied WWTPs ranged from 2.0 to 2.3, indicating higher relative ARG levels than the mean European ARGI of 2.0, but lower than the global mean of 2.4 [63].
Diversity of Antibiotic Resistance Genes and Transfer Elements-Quantitative Monitoring (DARTE-QM)
DARTE-QM represents an advanced amplicon sequencing approach that implements TruSeq high-throughput sequencing to simultaneously sequence thousands of antibiotic resistance gene targets.
- Primer Design: The method employs 796 primer pairs designed to target 67 antibiotic-resistant families and 662 ARGs, in addition to the 16S rRNA gene, in a multiplexed amplicon library preparation [62].
- Library Preparation and Sequencing: Following targeted amplification, libraries are prepared with Illumina adapters and barcodes, allowing for multiplexing of hundreds of samples in a single sequencing run on platforms such as the Illumina MiSeq [62].
- Performance Characteristics: Evaluation using a mock-community microbiome demonstrated high specificity (98.2%) and sensitivity (94.7%), with the method successfully identifying 55 of 56 ARGs known to be present in the reference genomes [62].
Table 2: Comparison of Methodologies for Environmental Resistome Surveillance
| Method | Key Features | Targets | Throughput | Limitations | Best Applications |
|---|---|---|---|---|---|
| HT-qPCR | Quantitative, high sensitivity | Predefined ARGs and MGEs | High (hundreds of targets) | Limited to known targets; primer bias | Time-series monitoring; source tracking [63] |
| DARTE-QM | Quantitative, broad spectrum | 662 ARGs across multiple classes | Very High (thousands of targets) | Artifact reads in complex samples; requires specialized bioinformatics | Comprehensive resistome profiling; comparative studies [62] |
| Shotgun Metagenomics | Untargeted, discovers novel genes | All genetic material in sample | Moderate (limited by sequencing depth) | High cost; computational intensity; low-abundance genes may be missed | Discovery of novel ARGs and mechanisms [65] |
| Water-Based Epidemiology | Population-level surveillance, early warning | Pathogens and ARGs in wastewater | High for population coverage | Limited spatial resolution; complex data interpretation | Community-level AMR burden assessment [66] |
Computational and Modeling Approaches
Mathematical modeling provides powerful tools for understanding AMR dynamics and predicting resistance evolution, complementing experimental approaches.
- Gene Network Models: Stochastic models of gene expression can elucidate how fluctuations in gene expression (non-genetic heterogeneity) contribute to drug resistance. These models have demonstrated that gene network motifs, such as feedforward and positive feedback loops—commonly found in natural resistance networks—can enhance drug resistance by modulating gene expression noise within cell populations [67].
- Population Dynamics Models: These models incorporate the multi-scale nature of AMR, combining stochastic gene expression with population simulation algorithms to investigate the evolution of resistance. Such models predict that non-genetic heterogeneity can facilitate the evolution of permanent, genetic drug resistance by increasing population size under drug treatment, thereby enhancing the probability of acquiring resistance mutations [67].
- Resistome Data Analysis: Specialized bioinformatics pipelines are required for processing data from targeted sequencing approaches like DARTE-QM. These pipelines must handle high heterogeneity in sequencing data and distinguish true ARG signals from amplification artifacts, which can account for up to 47% of reads in environmental samples [62].
The experimental workflow for implementing a comprehensive One Health surveillance strategy for environmental AMR is detailed in Figure 2.
Figure 2: Workflow for One Health AMR Surveillance in Environmental Reservoirs. This diagram outlines the comprehensive process for tracking environmental resistance, from sample collection through computational analysis to One Health interpretation.
The Scientist's Toolkit: Essential Reagents and Materials
Implementing environmental AMR surveillance requires specialized reagents and materials optimized for complex sample matrices and diverse analytical approaches.
Table 3: Research Reagent Solutions for Environmental AMR Studies
| Reagent/Material | Function | Application Notes | Key Considerations |
|---|---|---|---|
| DNA Extraction Kits | Isolation of high-quality microbial DNA from complex matrices | Soil, water, sediment, and wastewater samples | Select kits with effective inhibitor removal; include bead-beating for comprehensive lysis [62] |
| ARG-Targeted Primer Sets | Amplification of specific resistance genes | HT-qPCR, DARTE-QM, and other targeted approaches | Design or select panels covering major antibiotic classes; include MGE targets for mobility assessment [62] [63] |
| 16S rRNA Gene Primers | Quantification of total bacterial load | Normalization of ARG abundance | Essential for accounting for variations in bacterial biomass across samples [63] |
| Mock Community Standards | Quality control and quantification calibration | Method validation and cross-study comparisons | Composed of DNA from sequenced isolates with known ARG content [62] |
| High-Fidelity Polymerases | Accurate amplification for sequencing applications | DARTE-QM and amplicon sequencing | Critical for minimizing amplification errors in complex multiplex reactions [62] |
| Bioinformatics Pipelines | Processing and analysis of sequencing data | ARG classification, quantification, and statistical analysis | Customized pipelines required for novel methods like DARTE-QM [62] |
| Mobile Genetic Element Probes | Detection of horizontal gene transfer potential | Understanding ARG dissemination mechanisms | Include plasmids, integrons, transposons in analysis [63] |
Data Interpretation and Integration into One Health Surveillance
Translating environmental AMR data into actionable insights requires careful interpretation within the One Health context, considering the interconnectedness of reservoirs.
Spatiotemporal Patterns: Environmental resistomes demonstrate significant variation across locations and time. Studies have shown clear separation of resistome profiles between different environmental sources (e.g., agricultural soils vs. swine manure), with the first two eigenvalues in principal coordinate analysis accounting for nearly 80% of the total variation [62]. Temporal monitoring reveals fluctuations in ARG abundance related to antibiotic usage patterns, rainfall events, and agricultural practices.
Source Apportionment: Identifying contributions from different AMR sources is critical for targeted interventions. Computational approaches, including machine learning and statistical modeling, can help distinguish human, agricultural, and wildlife contributions to environmental resistomes. Network analysis, as demonstrated in zoonotic interaction studies, can identify key interfaces for spillover events, with human-cattle and human-food interfaces showing increased probability of zoonotic transmission [64].
Risk Assessment Framework: Evaluating the public health risk associated with environmental ARG detection involves multiple factors:
- ARG Mobility: Presence of MGEs co-located with ARGs increases dissemination potential [63].
- Pathogen Association: Detection of ARGs in known human pathogens elevates risk.
- Environmental Persistence: ARGs that persist post-treatment (e.g., in WWTP effluents) represent ongoing contamination sources [63].
- Exposure Pathways: Identification of critical exposure routes (recreational water, food, aerosols) completes the risk assessment.
The application of the One Health framework to track environmental resistance reservoirs represents a paradigm shift in AMR surveillance, moving beyond clinical settings to encompass the complex ecological context of resistance evolution and dissemination. Advanced methodological approaches, including HT-qPCR, DARTE-QM, and sophisticated computational models, provide researchers with powerful tools to decipher the intricate dynamics of environmental resistomes. Integration of data across human, animal, and environmental domains enables identification of critical transmission interfaces and prioritization of interventions. As AMR continues to pose a grave threat to global health, the holistic perspective offered by the One Health framework, supported by the methodologies detailed in this guide, will be essential for developing effective strategies to mitigate the spread of resistant microorganisms and safeguard the efficacy of antimicrobial agents for future generations.
Breaching the Walls: Strategic Disruption of Intrinsic Defense Systems
Antibiotic Potentiators and Adjuvants to Inhibit Efflux and Enzymes
The rising tide of antimicrobial resistance (AMR) represents one of the most pressing challenges to global public health, with multidrug-resistant (MDR) pathogens associated with nearly 5 million global deaths annually [68] [69]. Intrinsic resistance, an innate and heritable trait universally present within a bacterial species, forms the foundational core of this problem [18]. Unlike acquired resistance, which develops through horizontal gene transfer or mutation, intrinsic resistance is largely conferred by constitutive mechanisms such as expression of efflux pumps and production of antibiotic-inactivating enzymes [18] [70]. These systems pre-date the clinical use of antibiotics and play essential roles in bacterial physiology, including detoxification, virulence, and intercellular communication [19] [71] [51]. The overuse and misuse of antibiotics have exerted immense selective pressure, amplifying these inherent defenses and rendering many conventional therapeutics ineffective [72] [69].
The antibiotic discovery pipeline has significantly dwindled, making the development of entirely new drug classes an increasingly unsustainable strategy alone [72] [70]. In response, the scientific community has pivoted towards innovative approaches that rejuvenate existing antibiotics. Among these, antibiotic adjuvants (also termed potentiators) have emerged as a promising therapeutic paradigm [72] [68]. These compounds, which possess little or no inherent antibacterial activity, are co-administered with antibiotics to counteract specific resistance mechanisms [72] [70]. By targeting the very machinery that confers resistance—such as efflux pumps and hydrolytic enzymes—adjuvants can restore the efficacy of an antibiotic to which a pathogen has become resistant [68]. This approach extends the lifespan of existing antibiotics, potentially slows the development of new resistance, and represents a synergistic tool essential for combating multi-drug resistant pathogens like the critical-priority ESKAPE organisms (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) [72] [68].
Core Mechanisms of Intrinsic Antibiotic Resistance
Bacteria deploy a sophisticated array of defense strategies to survive antibiotic exposure. For intrinsic resistance, the most significant mechanisms involve limiting intracellular antibiotic accumulation and inactivating the drug before it can reach its target.
Antibiotic Efflux Pumps
Efflux pumps are transmembrane transporter proteins that actively extrude toxic substrates, including a wide range of antibiotics, from the bacterial cell. This process reduces the intracellular concentration of the drug, preventing it from reaching its therapeutic threshold [19] [57]. These pumps are classified into families based on their structure and energy source, as detailed in Table 1 [19] [52] [51].
Table 1: Major Families of Bacterial Efflux Pumps
| Family | Energy Source | Structural Characteristics | Key Examples | Representative Substrates |
|---|---|---|---|---|
| RND (Resistance-Nodulation-Division) | Proton Motive Force (Secondary Active Transport) | Tripartite complex (Inner membrane RND pump, Periplasmic Adapter Protein, Outer Membrane Factor) [19] [52] | AcrAB-TolC (E. coli), AdeABC (A. baumannii), MexAB-OprM (P. aeruginosa) [19] [52] [51] | Tetracyclines, β-lactams, fluoroquinolones, chloramphenicol, macrolides, dyes, detergents [52] [51] |
| MFS (Major Facilitator Superfamily) | Proton Motive Force (Secondary Active Transport) | Typically 12 or 14 transmembrane segments; functions as symporters, antiporters, or uniporters [19] | NorA (S. aureus), MefA (S. pneumoniae) [70] | Fluoroquinolones, macrolides, tetracyclines [70] |
| ABC (ATP-Binding Cassette) | ATP Hydrolysis (Primary Active Transport) | Two transmembrane domains and two nucleotide-binding domains [19] | MacAB (E. coli, S. enterica) [19] [51] | Macrolides, polypeptides [19] [51] |
| MATE (Multidrug and Toxic Compound Extrusion) | Proton or Sodium Ion Gradient (Secondary Active Transport) | Typically 12 transmembrane segments [19] [51] | NorM (V. parahaemolyticus) [51] | Fluoroquinolones, aminoglycosides, ethidium bromide [51] |
| SMR (Small Multidrug Resistance) | Proton Motive Force (Secondary Active Transport) | Small size; four transmembrane α-helical domains forming homodimers or heterodimers [19] [51] | EmrE (E. coli) [51] | Disinfectants, dyes, some antibiotics [51] |
The RND family pumps are particularly consequential for intrinsic resistance in Gram-negative bacteria. Their tripartite structure forms a conduit that spans both the inner and outer membranes, allowing them to eject drugs directly into the external environment [19] [52]. Furthermore, efflux pumps have fundamental physiological roles beyond antibiotic resistance. They are involved in virulence, biofilm formation, stress response, and quorum sensing, which explains their conservation and constitutive expression in many pathogens [19] [71] [51]. For instance, the AcrAB-TolC system in E. coli plays a role in pumping out bile acids and fatty acids, while its homolog in Erwinia amylovora is critical for virulence and host colonization [71].
Enzymatic Inactivation of Antibiotics
A second major pillar of intrinsic resistance is the production of enzymes that inactivate antibiotics through degradation or modification [18] [70]. The most prominent among these are the β-lactamases, a diverse group of enzymes that hydrolyze the β-lactam ring, a structural component essential to the activity of penicillins, cephalosporins, carbapenems, and other β-lactam antibiotics [72] [18] [57]. The emergence of extended-spectrum β-lactamases (ESBLs) and carbapenemases (e.g., KPC, NDM) has severely compromised the efficacy of last-resort antibiotics [18] [68]. Other enzymatic resistance mechanisms include:
- Aminoglycoside-modifying enzymes (AMEs) that catalyze the acetylation, phosphorylation, or adenylation of amino or hydroxyl groups on aminoglycoside drugs [70].
- Enzymatic modification of chloramphenicol via acetylation, preventing its binding to the ribosome [70].
Table 2: Key Antibiotic-Inactivating Enzymes and Their Mechanisms
| Enzyme Class | Antibiotic Target | Mechanism of Action | Clinical Impact |
|---|---|---|---|
| β-Lactamases (e.g., TEM, SHV, CTX-M, KPC) | β-lactams (Penicillins, Cephalosporins, Carbapenems) | Hydrolysis of the β-lactam ring, rendering the antibiotic inert [18] [57] | Major cause of resistance in Gram-negative bacteria; ESBLs and carbapenemases limit treatment options [72] [68] |
| Aminoglycoside Modifying Enzymes (e.g., AAC, APH, ANT) | Aminoglycosides (Gentamicin, Amikacin) | Acetylation (AAC), phosphorylation (APH), or adenylation (ANT) of drug molecules [70] | Widespread resistance in both Gram-positive and Gram-negative pathogens [70] |
| Chloramphenicol Acetyltransferases (CAT) | Chloramphenicol | Acetylation of hydroxyl groups, blocking ribosomal binding [70] | Confers resistance to chloramphenicol [70] |
The following diagram illustrates how these core mechanisms of efflux and enzymatic inactivation collectively confer intrinsic resistance to an antibiotic.
Diagram 1: Core mechanisms of intrinsic antibiotic resistance. Antibiotics entering the cell via porins can be (2a) inactivated by enzymes or (2b) extruded by efflux pumps, preventing them from reaching their essential target (2c).
Antibiotic Adjuvants: Mechanisms and Experimental Assessment
Antibiotic adjuvants restore the efficacy of antibiotics by directly targeting the resistance mechanisms described above. The two primary classes relevant to this guide are Efflux Pump Inhibitors (EPIs) and Enzyme Inhibitors.
Efflux Pump Inhibitors (EPIs)
EPIs are compounds that block the function of multidrug efflux pumps, thereby increasing the intracellular concentration of co-administered antibiotics [19] [52]. They can act through various mechanisms:
- Competitive Inhibition: Binding directly to the substrate-binding pocket of the pump, thereby blocking antibiotic binding [52] [51].
- Uncompetitive Inhibition: Interfering with the functional assembly or energy coupling of the efflux complex (e.g., disrupting the proton motive force or interactions between the tripartite components in RND pumps) [52].
- Depleting Energy Sources: Reducing the cellular energy (e.g., ATP or proton gradient) required to power the transport cycle [71].
Promising EPIs include natural products like the alkaloid lysergol and the flavonoid rotenone, as well as synthetic compounds like Phe-Arg-β-naphthylamide (PAβN) [19] [71]. However, clinical translation of EPIs has been hampered by issues of toxicity, poor stability, and unfavorable pharmacokinetics [19] [52] [70].
Experimental Protocol: Assessing Efflux Pump Inhibition
This protocol outlines a standard methodology for evaluating the efficacy of a putative EPI.
Objective: To determine if a test compound (potential EPI) restores the susceptibility of a bacterial strain to a known antibiotic by inhibiting efflux pump activity.
Materials:
- Bacterial Strain: A characterized strain that overexpresses a specific efflux pump (e.g., Acinetobacter baumannii overexpressing AdeABC).
- Antibiotics: Standard antibiotics known to be substrates of the target pump (e.g., tetracycline, ciprofloxacin).
- Putative EPI: The test compound (e.g., PAβN or a novel inhibitor).
- Control Compounds: A known EPI (positive control) and a compound with no EPI activity (negative control).
- Dye: Ethidium bromide (EtBr) or another fluorescent substrate of efflux pumps.
- Growth Medium: Appropriate broth and agar (e.g., Mueller-Hinton).
- Equipment: Microplate reader, fluorometer, incubator.
Procedure:
Checkerboard Broth Microdilution Assay:
- Prepare a two-dimensional matrix of serial dilutions of the antibiotic and the putative EPI in a 96-well microtiter plate.
- Inoculate each well with a standardized bacterial suspension.
- Incubate the plate at 37°C for 16-20 hours.
- Determine the Minimum Inhibitory Concentration (MIC) of the antibiotic in the presence and absence of the EPI.
- Calculate the Fractional Inhibitory Concentration (FIC) Index to quantify synergy:
- FIC Index = (MIC of antibiotic combined/MIC of antibiotic alone) + (MIC of EPI combined/MIC of EPI alone)
- Interpretation: FIC Index ≤ 0.5 indicates synergy; >0.5 to 4 indicates no interaction; >4 indicates antagonism [72].
Ethidium Bromide Accumulation Assay:
- Grow bacterial cells to mid-log phase.
- Wash and resuspend the cells in an appropriate buffer.
- Divide the suspension into aliquots: one treated with the putative EPI and an untreated control.
- Add EtBr to all aliquots and monitor fluorescence over time using a fluorometer.
- Interpretation: An increase in fluorescence intensity in the EPI-treated sample compared to the control indicates inhibition of efflux activity, as more EtBr is retained inside the cells [52].
Enzyme Inhibitors
These adjuvants inhibit the activity of antibiotic-inactivating enzymes. The most successful clinical examples are β-lactamase inhibitors, which are co-formulated with β-lactam antibiotics [72] [68] [70].
- Mechanism: They often act as suicide substrates—molecules that structurally resemble the β-lactam antibiotic and are recognized and bound by the β-lactamase. The enzyme then irreversibly catalyzes its own inactivation by forming a stable, covalent complex with the inhibitor [68].
- Clinical Examples: Clavulanic acid (combined with amoxicillin), sulbactam, tazobactam, and the newer agents avibactam and vaborbactam (combined with meropenem) [68] [70].
Experimental Protocol: Evaluating β-Lactamase Inhibition
Objective: To determine the kinetic parameters of β-lactamase inhibition and assess the restoration of antibiotic activity.
Materials:
- Purified β-lactamase Enzyme (e.g., TEM-1, KPC-2).
- Antibiotic Substrate: Nitrocefin, a chromogenic β-lactam that changes color upon hydrolysis.
- β-lactam Antibiotic: The drug to be protected (e.g., ampicillin, ceftazidime).
- Inhibitor: The test compound (e.g., clavulanic acid).
- Spectrophotometer.
Procedure:
Enzyme Kinetic Assay:
- Prepare a solution of nitrocefin and purified β-lactamase.
- Measure the rate of nitrocefin hydrolysis (increase in absorbance at 482 nm) to establish the baseline enzyme activity (V₀).
- Pre-incubate the enzyme with varying concentrations of the inhibitor for a set time.
- Add nitrocefin and measure the initial rate of hydrolysis (Vᵢ).
- Plot the residual enzyme activity (Vᵢ/V₀) against inhibitor concentration to determine the IC₅₀ (concentration that inhibits 50% of enzyme activity).
Antibiotic Potentiation Assay:
- Perform a checkerboard broth microdilution assay as described in section 3.1.1, using the β-lactam antibiotic and the inhibitor.
- Determine the MIC of the antibiotic alone and in combination with the inhibitor.
- A significant (e.g., ≥4-fold) reduction in the MIC of the antibiotic in the presence of the inhibitor confirms potentiation and effective enzyme inhibition [68].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Research on Efflux and Enzyme Inhibition
| Reagent / Tool | Function / Application | Example Compounds / Kits |
|---|---|---|
| Reference Efflux Pump Inhibitors | Positive controls for EPI assays; used to validate experimental systems. | Phe-Arg-β-naphthylamide (PAβN/ MC-207,110) [19] [70], Carbonyl cyanide m-chlorophenyl hydrazone (CCCP) [52] |
| Reference Enzyme Inhibitors | Positive controls for β-lactamase inhibition assays. | Clavulanic Acid, Tazobactam, Avibactam [68] [70] |
| Fluorescent Efflux Substrates | Probes for direct measurement of efflux pump activity via accumulation assays. | Ethidium Bromide (EtBr), Hoechst 33342 [52] |
| Chromogenic β-Lactamase Substrates | Probes for measuring β-lactamase enzyme kinetics and inhibition. | Nitrocefin [68] |
| Characterized Bacterial Strains | Essential for studying specific efflux pumps or enzymes in a relevant genetic background. | E. coli K-12 with AcrAB-TolC; A. baumannii with AdeABC overexpression; Isogenic pairs (e.g., wild-type vs. efflux pump knockout) [52] [51] |
| Cell Lysis & Protein Purification Kits | For obtaining purified enzymes (e.g., β-lactamases) for in vitro biochemical assays. | Commercial kits for His-tag protein purification from cytoplasmic or periplasmic fractions |
The strategic use of antibiotic adjuvants to inhibit efflux pumps and resistance enzymes represents a powerful and necessary approach to overcome intrinsic resistance. By targeting the root causes of treatment failure, this paradigm extends the utility of our existing antibiotic arsenal. While significant challenges remain—particularly in developing safe, effective, and pharmacokinetically compatible EPIs—ongoing research into novel compounds and their mechanisms holds immense promise. For researchers and drug development professionals, a deep understanding of these resistance mechanisms and the experimental tools to evaluate inhibitors is paramount. Integrating adjuvant therapy into our antimicrobial toolkit is not merely an alternative strategy but a critical component of a sustainable defense against the relentless evolution of multidrug-resistant pathogens.
Structure-Activity Relationship (SAR) to Design Membrane-Penetrating Compounds
The escalating crisis of antimicrobial resistance (AMR) represents a profound threat to global public health, with drug-resistant bacterial infections causing an estimated 1.27 million deaths annually [73]. A fundamental challenge in combating Gram-negative pathogens, in particular, lies in their formidable outer membrane (OM), which acts as a highly effective permeability barrier that restricts antibiotic entry [74]. This intrinsic resistance mechanism, coupled with acquired resistance strategies, has rendered many conventional antibiotics ineffective, creating an urgent need for novel therapeutic strategies. The design of compounds capable of penetrating the bacterial membrane has thus emerged as a critical frontier in antibiotic discovery [74] [75].
The Structure-Activity Relationship (SAR) provides a methodological framework for understanding how the chemical structure of a molecule influences its biological activity, particularly its ability to traverse complex biological membranes. By systematically analyzing how specific structural modifications affect permeability and antibacterial efficacy, researchers can rationally design compounds optimized to overcome the formidable barriers presented by bacterial envelopes [76]. This technical guide examines the core principles of SAR for membrane-penetrating compounds within the context of intrinsic antibiotic resistance mechanisms, providing researchers with strategic insights and experimental methodologies to advance this crucial field.
Bacterial Membrane Structure and Resistance Mechanisms
Anatomical Barriers to Permeation
The effectiveness of membrane-penetrating compounds is intrinsically linked to the structural complexity of their bacterial targets. Gram-negative bacteria possess a unique asymmetrical outer membrane with an inner leaflet composed of phospholipids and an outer leaflet consisting of densely packed lipopolysaccharides (LPS) [74]. The LPS layer is stabilized by divalent cations (Mg²⁺, Ca²⁺), creating a low-fluidity barrier that severely restricts the penetration of hydrophobic compounds [77] [74]. This outer membrane contains protein channels called porins, which act as size-exclusion filters for hydrophilic molecules, while efflux pumps actively remove compounds that successfully penetrate [74] [78].
In contrast, Gram-positive bacteria lack this outer membrane but possess a thick peptidoglycan layer that can still impede molecular access. The cytoplasmic membranes of both bacterial classes are rich in phosphatidylglycerol (PG) and cardiolipin, which confer a net negative charge that can be exploited for selective targeting [77] [79]. The compositional differences between bacterial and mammalian membranes—specifically the prevalence of phosphatidylcholine and sphingomyelin in mammalian systems—provide a foundational principle for designing selectively toxic compounds [79].
Key Resistance Determinants
Bacteria employ multiple sophisticated mechanisms to evade antibiotic action, with the outer membrane serving as the first line of defense [74]. Beyond this physical barrier, resistance mechanisms include:
- Efflux Systems: Resistance-nodulation-division (RND) family efflux pumps, unique to Gram-negative bacteria, recognize and extrude a wide spectrum of antibiotics before they reach intracellular targets [74] [78].
- Enzyme-Mediated Inactivation: Bacteria produce antibiotic-inactivating enzymes such as β-lactamases (including ESBLs and carbapenemases), aminoglycoside-modifying enzymes, and colistin-resistant phosphoethanolamine transferases [74] [78].
- Target Modification: Alteration of antibiotic binding sites through genetic mutations or post-translational modifications reduces drug affinity, as exemplified by PBP2a in methicillin-resistant Staphylococcus aureus (MRSA) [80] [78].
- Membrane Vesicle Production: Gram-negative bacteria release outer membrane vesicles that sequester antibiotics and remove them from the cellular environment [74].
Table 1: Major Bacterial Resistance Mechanisms Affecting Compound Permeation
| Resistance Mechanism | Representative Examples | Impact on Membrane Penetration |
|---|---|---|
| Outer Membrane Barrier | LPS in Gram-negative bacteria | Restricts hydrophobic compound entry; porins limit hydrophilic compound size |
| Efflux Pumps | RND family (AcrAB-TolC in E. coli) | Extrudes diverse antibiotics; major contributor to multidrug resistance |
| Enzymatic Inactivation | β-lactamases, aminoglycoside-modifying enzymes | Chemically modifies antibiotics before cellular engagement |
| Target Modification | PBP2a in MRSA; altered peptidoglycan precursors in VRE | Reduces antibiotic binding affinity without affecting penetration |
| Membrane Vesicles | OMVs in Gram-negative bacteria | Sequester antibiotics extracellularly |
Fundamental SAR Principles for Membrane Penetration
Core Structural Determinants of Permeation
The permeation capacity of antibacterial compounds across bacterial membranes is governed by specific physicochemical properties that can be optimized through structural design:
- Cationic Charge: The majority of natural antimicrobial peptides (AMPs) exhibit a net positive charge (typically +2 to +9) due to an excess of basic residues (lysine, arginine, histidine) [76] [79]. This cationicity facilitates initial electrostatic interactions with negatively charged bacterial surface components such as lipopolysaccharides (LPS) in Gram-negatives and teichoic acids in Gram-positives [79].
- Amphipathicity: Optimal membrane disruption requires a balanced spatial segregation of hydrophobic and hydrophilic domains within the molecular structure. This amphipathic character enables simultaneous interaction with both lipid acyl chains and polar head groups of membrane phospholipids [76] [79].
- Hydrophobicity: A sufficient hydrophobic content (typically 30-50% of residues) is essential for integration into the lipid bilayer core. However, excessive hydrophobicity often correlates with increased mammalian cell toxicity, creating a narrow therapeutic window [76].
- Molecular Conformation: Secondary structures such as α-helices and β-sheets promote optimal orientation and insertion into biological membranes. Structural rigidity from disulfide bridges or cyclic constraints can enhance stability without compromising activity [76] [79].
Table 2: Key Physicochemical Parameters for Membrane-Penetrating Compounds
| Parameter | Optimal Range | Structural Influence | Biological Impact |
|---|---|---|---|
| Net Charge | +2 to +9 | Ratio of basic (Lys, Arg) to acidic (Asp, Glu) residues | Electrostatic attraction to anionic bacterial surfaces |
| Hydrophobicity | 30-50% | Proportion of non-polar residues (Ala, Val, Ile, Phe, Trp) | Membrane partitioning and depth of penetration |
| Amphipathicity | Hydrophobic moment >0.5 | Spatial segregation of polar and non-polar faces | Membrane disruption efficiency and selectivity |
| Polar Surface Area | <200 Ų | Number and distribution of hydrogen bond donors/acceptors | Transmembrane permeability and efflux susceptibility |
SAR-Guided Molecular Design Strategies
Strategic structural modifications can significantly enhance the membrane-penetrating capabilities of lead compounds while minimizing undesirable properties:
- Charge Distribution: Localized rather than uniform distribution of cationic residues often enhances membrane activity. Clustering basic residues at molecular termini or in discrete domains can create regions of high charge density that more effectively disrupt membrane integrity [76].
- Hydrophobic Core Optimization: Systematic replacement of aliphatic residues with aromatic amino acids (tryptophan, tyrosine) can strengthen membrane anchoring via cation-π and π-π stacking interactions with lipid head groups [76].
- Backbone Cyclization: Macrocyclization or side-chain crosslinking (e.g., via disulfide bridges) reduces conformational flexibility, enhances proteolytic stability, and can improve the spatial organization of functional groups for optimal membrane interaction [76].
- Steric Modulation: Incorporation of β-amino acids, D-enantiomers, or N-methylated residues can disrupt protease recognition sites while maintaining or enhancing membrane activity. These modifications also alter hydrogen-bonding potential, which affects traversal across the outer membrane [76] [79].
Compound Class-Specific SAR Analysis
Antimicrobial Peptides (AMPs)
Antimicrobial peptides represent nature's solution to membrane penetration, with over 3000 identified examples providing a rich source of SAR insights [76] [79]. These typically short (12-50 amino acids), cationic peptides employ diverse mechanisms of membrane interaction:
- Pore-Forming Mechanisms: AMPs can disrupt membrane integrity through various models including:
- Barrel-Stave: Peptides oligomerize to form transmembrane channels where hydrophobic regions face lipids and hydrophilic regions line the pore interior [79].
- Toroidal: Peptides induce lipid monolayers to bend continuously through the pore, creating mixed lipid-peptide channels [79].
- Carpet: Peptides cover the membrane surface in a detergent-like manner, causing mass disruption at threshold concentrations [79].
The specific mechanism employed depends on peptide structure, concentration, and membrane composition. For example, α-helical peptides like magainin often utilize the toroidal pore model, while β-sheet peptides like protegrins may function via barrel-stave mechanisms [79].
- Key SAR Considerations for AMPs:
- Helical hydrophobicity directly correlates with antimicrobial activity but also with hemolytic potential
- Proline and glycine residues introduce structural kinks that can facilitate pore formation
- Cationic charge density governs interaction kinetics with anionic membrane surfaces
- Amphipathic moment determines the efficiency of membrane partitioning and disruption
Non-Peptidic Small Molecules
Small molecule antibiotics face distinct permeability challenges, particularly in traversing the Gram-negative outer membrane. SAR studies have revealed critical structural requirements:
- Molecular Weight and Rigidity: Compounds under 600 Da generally demonstrate improved penetration through porin channels, while conformational flexibility aids adaptation to membrane environments [74] [78].
- Ionization State: Zwitterionic compounds with balanced acidic and basic moieties often show enhanced accumulation in Gram-negative bacteria, potentially due to improved porin permeability and reduced efflux recognition [74].
- Hydrogen Bonding Capacity: Reduced numbers of hydrogen bond donors (<5) and acceptors (<10) correlate with improved membrane penetration by minimizing hydration energy penalties during membrane partitioning [74].
Experimental Protocols for SAR Determination
Membrane Permeability and Localization Assays
Diagram 1: Experimental workflow for evaluating compound-membrane interactions
Protocol 1: Outer Membrane Permeability Assessment (N-Phenyl-1-naphthylamine Assay)
Principle: The NPN fluorescence assay quantifies outer membrane disruption by measuring the uptake of the hydrophobic fluorophore N-phenyl-1-naphthylamine, which exhibits enhanced fluorescence in phospholipid environments [74].
Procedure:
- Grow Gram-negative bacteria (e.g., E. coli MG1655) to mid-log phase (OD₆₀₀ ≈ 0.5) in appropriate medium.
- Harvest cells by centrifugation (5,000 × g, 10 min), wash twice, and resuspend in buffer (5 mM HEPES, pH 7.2) to OD₆₀₀ ≈ 0.5.
- Add NPN to a final concentration of 10 μM and incubate for 5 minutes in the dark.
- Distribute 100 μL aliquots of cell suspension into black 96-well plates.
- Add test compounds at serial concentrations (typically 0.5-64 μg/mL) and immediately measure fluorescence (excitation 350 nm, emission 420 nm) every 30 seconds for 15 minutes.
- Calculate percentage outer membrane disruption relative to positive control (10 mM EDTA, 100% disruption) and negative control (buffer alone, 0% disruption).
SAR Application: Correlate structural features (charge, hydrophobicity) with permeability kinetics. Compounds causing rapid NPN uptake typically possess strong membrane-disrupting properties.
Protocol 2: Cytoplasmic Membrane Depolarization (DiSC₃(5) Assay)
Principle: The carbocyanine dye DiSC₃(5) partitions into polarized membranes and exhibits self-quenching; membrane depolarization results in dye release and fluorescence dequenching [79].
Procedure:
- Prepare bacterial cells as described in Protocol 1, resuspend in buffer containing 20 mM glucose.
- Load cells with DiSC₃(5) (final concentration 0.4 μM) and incubate 30 minutes in the dark.
- Add potassium chloride (100 mM) to equilibrate cytoplasmic and external K⁺ concentrations.
- Distribute 100 μL aliquots into black 96-well plates, add test compounds, and monitor fluorescence (excitation 622 nm, emission 670 nm) for 20 minutes.
- Calculate percentage depolarization relative to positive control (10 μM gramicidin D, 100% depolarization).
SAR Application: Quantitate the relationship between structural modifications and membrane-disrupting potency. Compounds causing rapid depolarization typically have bactericidal mechanisms.
Structural Analysis and Bioinformatics Approaches
Protocol 3: Surface Plasmon Resonance (SPR) for Membrane Binding Kinetics
Principle: SPR measures real-time binding interactions between compounds and membrane models immobilized on a sensor chip [76].
Procedure:
- Prepare liposomes mimicking bacterial membranes (composition: POPG/POPE 3:1 for Gram-negative; POPG/cardiolipin 4:1 for Gram-positive).
- Immobilize liposomes on L1 sensor chip using standard amine coupling chemistry.
- Flow compounds at various concentrations (0.5-50 μM) in running buffer (10 mM HEPES, 150 mM NaCl, pH 7.4) at 30 μL/min.
- Monitor association (120 s) and dissociation (180 s) phases.
- Determine kinetic parameters (kₐ, kḍ, K_D) using appropriate binding models.
SAR Application: Precisely quantify how structural modifications affect membrane binding affinity and kinetics.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Membrane Penetration Studies
| Reagent/Category | Specific Examples | Research Application | SAR Relevance |
|---|---|---|---|
| Membrane Models | POPG, POPE, Cardiolipin, LPS | Artificial membrane systems for binding and permeation studies | Determines structural requirements for interaction with specific membrane components |
| Fluorescent Probes | NPN, DiSC₃(5), SYTOX Green, Propidium Iodide | Membrane integrity and permeability assessment | Quantitates relationship between compound structure and membrane disruption efficacy |
| Bacterial Strains | E. coli ATCC 25922, P. aeruginosa PAO1, A. baumannii ATCC 19606 | Standard and clinical isolates for activity testing | Reveals structure-dependent activity against different membrane architectures |
| Efflux Pump Mutants | E. coli ΔacrB, P. aeruginosa ΔmexB | Differentiating intrinsic activity from efflux susceptibility | Identifies structural features that avoid efflux recognition |
| Analytical Standards | Polymyxin B, Colistin, Nisin | Comparator membrane-active compounds | Benchmark for optimizing structure-based activity |
| Liposome Preparation Kits | Mini-Extruder systems, commercial lipid kits | Creating uniform membrane models for biophysical studies | Enables standardized assessment of membrane-compound interactions |
Visualization of Membrane Interaction Pathways
Diagram 2: Pathways of compound-membrane interactions and disruption mechanisms
The strategic application of Structure-Activity Relationship principles to the design of membrane-penetrating compounds represents a promising avenue for addressing the critical challenge of antimicrobial resistance. By systematically elucidating the complex relationships between chemical structure and membrane interaction dynamics, researchers can develop compounds capable of overcoming the sophisticated barrier systems of multidrug-resistant pathogens. The integration of robust experimental methodologies with computational approaches and high-throughput screening will accelerate the discovery of novel membrane-active agents. As the AMR crisis continues to escalate, evidenced by the WHO's report of increasing resistance patterns globally [81], the rational design of compounds targeting the fundamental permeability barrier of bacteria remains an essential component of comprehensive antibiotic discovery efforts. Through continued refinement of SAR models and collaborative interdisciplinary research, the scientific community can develop the next generation of therapeutic agents to combat resistant infections and safeguard modern medicine.
Combination Therapies to Overcome Multifactorial Intrinsic Resistance
Antimicrobial resistance (AMR) represents a defining global health crisis of our time, severely undermining the effectiveness of antibiotics that form the foundation of modern medicine [82]. In 2019 alone, bacterial infections accounted for 13.6% of all global deaths, with more than 7.7 million fatalities directly attributable to 33 bacterial pathogens [82]. The most significant concern is represented by multidrug-resistant (MDR) pathogens, particularly the ESKAPEE group—Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, Enterobacter spp., and Escherichia coli [82]. Without rapid intervention, annual AMR-attributable deaths are projected to climb to 10 million by 2050 [82] [1].
Intrinsic resistance in bacteria arises through multifactorial mechanisms operating individually or in combination, including enzymatic degradation of antimicrobials (e.g., β-lactamases), target site modification, efflux pump overexpression, reduced membrane permeability, and biofilm formation [82] [1]. This complexity necessitates innovative therapeutic approaches, particularly combination therapies that simultaneously target multiple resistance pathways to restore treatment efficacy. This review synthesizes current knowledge on combination strategies to overcome multifactorial intrinsic resistance, providing researchers and drug development professionals with experimental frameworks and quantitative data to guide future therapeutic development.
Molecular Mechanisms of Intrinsic Resistance
Understanding the fundamental mechanisms underlying intrinsic resistance is essential for developing effective combination therapies. Bacteria employ four primary resistance strategies, often in combination, to survive antibiotic exposure.
Enzymatic Inactivation
Antibiotics can be degraded or modified by bacterial enzymes, rendering them ineffective before reaching their cellular targets [1]. β-lactamases represent the most clinically significant family of resistance enzymes, capable of hydrolyzing β-lactam antibiotics. The extended-spectrum β-lactamases (ESBLs) and carbapenemases (e.g., KPC, NDM, OXA-48) in Enterobacteriaceae have dramatically limited treatment options for common pathogens [1].
Target Site Modification
Bacteria can alter antibiotic targets through mutation or enzymatic modification, reducing drug binding affinity. Methicillin-resistant Staphylococcus aureus (MRSA) exemplifies this mechanism through acquisition of the mecA gene, which encodes PBP2a—a modified penicillin-binding protein with low affinity for β-lactams [1]. Similarly, mutations in DNA gyrase and topoisomerase IV confer resistance to fluoroquinolones [1].
Efflux Pump Overexpression
Bacterial efflux systems actively transport antibiotics out of the cell, reducing intracellular concentrations below inhibitory levels. These pumps often exhibit broad substrate specificity, contributing to multidrug resistance phenotypes. Pseudomonas aeruginosa utilizes the MexAB-OprM efflux system, among others, to resist multiple antibiotic classes including β-lactams, fluoroquinolones, and tetracyclines [82].
Reduced Membrane Permeability
Modifications to outer membrane porins or lipid composition can limit antibiotic penetration into bacterial cells. Porin loss or mutation in Klebsiella pneumoniae and Escherichia coli significantly reduces permeability to carbapenems and other β-lactams, contributing to resistance [1]. Gram-negative bacteria inherently exhibit greater resistance to many antibiotics due to their impermeable outer membrane [82].
Table 1: Major Resistance Mechanisms in Priority Bacterial Pathogens
| Pathogen | Primary Resistance Mechanisms | Key Genetic Determinants | Antibiotic Classes Affected |
|---|---|---|---|
| Acinetobacter baumannii (carbapenem-resistant) | Enzymatic degradation, Efflux pumps, Porin mutations | blaOXA-23, blaNDM, AdeABC efflux system | Carbapenems, Cephalosporins, Aminoglycosides |
| Klebsiella pneumoniae (carbapenem-resistant) | Enzymatic degradation, Porin loss, Biofilm formation | blaKPC, blaNDM, OmpK35/36 mutations | Carbapenems, Cephalosporins, Fluoroquinolones |
| Pseudomonas aeruginosa (carbapenem-resistant) | Efflux pumps, Enzymatic degradation, Target modification | MexAB-OprM efflux, blaPDC, gyrA/parC mutations | Carbapenems, Cephalosporins, Fluoroquinolones |
| Staphylococcus aureus (methicillin-resistant) | Target modification, Enzymatic inactivation, Efflux | mecA (PBP2a), blaZ, msrA | β-lactams, Macrolides, Fluoroquinolones |
| Escherichia coli (ESBL-producing) | Enzymatic degradation, Efflux pumps | blaCTX-M, blaTEM, blaSHV, AcrAB-TolC | Cephalosporins, Fluoroquinolones, Tetracyclines |
Current Landscape of Combination Therapies
Combination approaches simultaneously target bacterial viability and resistance mechanisms, creating synergistic effects that restore antibiotic efficacy. The World Health Organization's 2024 Bacterial Priority Pathogen List categorizes resistant pathogens into critical, high, and medium priorities to guide research and resource allocation [82].
Novel Antibiotic Combinations
Traditional antibiotics combined with novel agents represent a promising strategy against multidrug-resistant pathogens. Zosurabalpin, a novel macrocyclic peptide, has demonstrated efficacy against carbapenem-resistant Acinetobacter baumannii by inhibiting lipopolysaccharide transport [82]. When combined with existing carbapenems, it exhibits synergistic activity against previously pan-resistant strains. Similarly, the combination of ceftazidime-avibactam with aztreonam has shown success against metallo-β-lactamase-producing Enterobacteriaceae by simultaneously inhibiting serine β-lactamases (avibactam) while maintaining aztreonam's activity against metallo-β-lactamases [82].
Antibiotic-Potentiator Combinations
Potentiator approaches enhance the activity of existing antibiotics without direct antibacterial effects. Efflux pump inhibitors like phenylalanine-arginine β-naphthylamide (PAβN) restore susceptibility to multiple antibiotic classes in resistant Pseudomonas aeruginosa and Escherichia coli strains [1]. Similarly, β-lactamase inhibitors (clavulanic acid, avibactam, vaborbactam) protect companion β-lactam antibiotics from enzymatic degradation, extending their spectrum against ESBL-producing and carbapenem-resistant Enterobacteriaceae [82] [1].
Table 2: Quantitative Efficacy of Selected Combination Therapies Against Resistant Pathogens
| Combination Therapy | Pathogen Target | Resistance Mechanism Addressed | Fold Change in MIC | Synergy Rate (%) |
|---|---|---|---|---|
| Ceftazidime-Avibactam + Aztreonam | MBL-producing Enterobacteriaceae | Metallo-β-lactamase enzymatic degradation | 16-64× reduction | 85-92% |
| Meropenem-Vaborbactam | KPC-producing K. pneumoniae | Serine carbapenemase degradation | 32-128× reduction | 78-88% |
| Colistin + Carbapenems | XDR A. baumannii | Membrane permeability, Efflux pumps | 4-16× reduction | 65-75% |
| Fosfomycin + Aminoglycosides | MRSA, VRE | Target modification, Enzymatic inactivation | 8-32× reduction | 70-82% |
| Novel Lasso Peptides + β-lactams | ESKAPE pathogens | Biofilm formation, Efflux pumps | 16-64× reduction | Under investigation |
Experimental Protocols for Combination Therapy Development
Robust experimental methodologies are essential for evaluating potential combination therapies. The following protocols provide standardized approaches for assessing synergistic activity.
Checkerboard Synergy Assay
The checkerboard broth microdilution method quantitatively measures drug interactions through Fractional Inhibitory Concentration (FIC) indices [82] [1].
Materials and Reagents:
- Cation-adjusted Mueller-Hinton broth (CAMHB)
- 96-well sterile polystyrene microtiter plates
- Antibiotic stock solutions at 10× highest test concentration
- Bacterial suspension adjusted to 0.5 McFarland standard (~1.5 × 10^8 CFU/mL)
- Multichannel pipettes and sterile tips
- Automated plate reader (OD600 nm)
Procedure:
- Prepare serial two-fold dilutions of Antibiotic A in CAMHB along the x-axis of the microtiter plate, with concentrations typically ranging from 4× to 1/64× the MIC.
- Prepare serial two-fold dilutions of Antibiotic B in CAMHB along the y-axis.
- Dilute the bacterial suspension to approximately 5 × 10^5 CFU/mL in CAMHB.
- Add 100 μL of the inoculated broth to each well, resulting in a final bacterial density of 5 × 10^4 CFU/mL.
- Include growth control (no antibiotic) and sterility control (no inoculum) wells.
- Seal plates and incubate at 35±2°C for 16-20 hours.
- Determine the MIC of each antibiotic alone and in combination visually or spectrophotometrically.
Interpretation: Calculate FIC indices using the formula: FIC index = (MICA in combination/MICA alone) + (MICB in combination/MICB alone). Synergy is defined as FIC index ≤0.5; additivity as 0.5-1.0; indifference as 1.0-4.0; and antagonism as >4.0.
Time-Kill Kinetics Assay
Time-kill studies provide dynamic assessment of bactericidal activity and can detect synergistic interactions that static MIC methods may miss [1].
Materials and Reagents:
- Cation-adjusted Mueller-Hinton broth (CAMHB)
- Sterile plastic tubes (e.g., 15 mL Falcon tubes)
- Antibiotic stock solutions
- Phosphate-buffered saline (PBS) for serial dilutions
- Agar plates for viable counting
- Bacterial suspension adjusted to 0.5 McFarland standard
Procedure:
- Prepare antibiotic solutions in CAMHB at predetermined concentrations (typically 0.5×, 1×, and 2× MIC for single agents and combinations).
- Inoculate tubes with bacteria to a final density of approximately 5 × 10^5 CFU/mL.
- Incubate at 35±2°C with shaking (200 rpm).
- Remove aliquots (100 μL) at 0, 4, 8, and 24 hours.
- Perform serial 10-fold dilutions in PBS and plate 100 μL onto appropriate agar media.
- Incubate plates for 16-20 hours at 35±2°C and enumerate colonies.
Interpretation: Synergy is defined as a ≥2-log10 decrease in CFU/mL between the combination and its most active constituent after 24 hours. Bactericidal activity is defined as a ≥3-log10 decrease in CFU/mL from the initial inoculum.
The following diagram illustrates the strategic framework for developing combination therapies that target multiple resistance mechanisms simultaneously:
The Scientist's Toolkit: Essential Research Reagents and Materials
Advancing combination therapy research requires specialized reagents and tools for evaluating compound interactions and efficacy against resistant pathogens.
Table 3: Essential Research Reagents for Combination Therapy Development
| Reagent/Tool | Primary Function | Application Examples | Key Considerations |
|---|---|---|---|
| WHOnet Software | Management and analysis of antimicrobial susceptibility test data | Trend analysis of resistance patterns, Phenotypic correlation | Free WHO-provided software, Supports data standardization [83] |
| BacLink Software | Conversion of laboratory data formats to WHONET-compatible formats | Integration of diverse laboratory instrument outputs | Essential for multi-center surveillance studies [83] |
| R Statistical Software | Advanced statistical analysis and data visualization | Synergy index calculation, Resistance trend modeling, Publication-quality graphics | Open-source platform with specialized packages for microbiology [83] |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for susceptibility testing | Broth microdilution assays, Checkerboard synergy testing | Cation concentration critical for aminoglycoside and polymyxin testing [1] |
| EUCAST/CLSI Breakpoint Tables | Interpretation criteria for susceptibility testing | Standardized categorization of resistant/intermediate/susceptible isolates | Regular updates required to reflect current resistance trends [83] |
| Resazurin Cell Viability Assay | Fluorometric/colorimetric assessment of bacterial viability | High-throughput screening of compound libraries | Alternative to labor-intensive colony counting methods |
| Biofilm Assay Kits (crystal violet, ATP-based) | Quantification of biofilm formation and eradication | Evaluation of anti-biofilm agents in combination with antibiotics | Multiple measurement methodologies provide complementary data |
| Genomic DNA Extraction Kits | Isolation of high-quality bacterial DNA | Whole-genome sequencing of resistant isolates, Resistance gene identification | Essential for correlating phenotypic resistance with genetic determinants |
Emerging Therapeutic Approaches and Future Directions
The pipeline of novel agents targeting resistance mechanisms provides new opportunities for combination approaches.
Naturally-Derived Compounds and Antimicrobial Peptides
Naturally derived compounds offer novel scaffolds that can circumvent existing resistance mechanisms. Corallopyronin, clovibactin, and chlorotonil A represent promising natural products with activity against multidrug-resistant pathogens [82]. Antimicrobial peptides (AMPs) from commensal bacteria demonstrate synergistic activity with conventional antibiotics against biofilms of Acinetobacter baumannii and other ESKAPE pathogens [84]. These AMPs exhibit unique mechanisms of action, including membrane disruption and inhibition of cell wall synthesis, making them less susceptible to conventional resistance mechanisms.
Targeted Inhibitors and Precision Approaches
Molecular targeted therapies represent an emerging frontier in combating resistance. Debio 1453 specifically targets Neisseria gonorrhoeae through FabI inhibition, demonstrating efficacy against extensively drug-resistant strains [82]. Similarly, phage-derived lysins and engineered bacteriocins offer pathogen-specific approaches that can be combined with broader-spectrum antibiotics to enhance activity while minimizing collateral damage to the microbiota.
Alternative Therapeutic Modalities
Non-antibiotic approaches are being investigated as potentiators of conventional treatments. Gemmotherapy extracts from medicinal plants like dog rose, lingonberry, and sea buckthorn have demonstrated variable antimicrobial effects against resistant pathogens [84]. Nanoparticle-based drug delivery systems enhance antibiotic penetration through bacterial membranes and biofilms, potentially overcoming permeability-based resistance mechanisms [84].
The continued evolution of multifactorial intrinsic resistance demands innovative combination strategies that simultaneously target multiple vulnerability points in bacterial pathogens. By integrating mechanistic insights with robust experimental approaches and novel therapeutic agents, researchers can develop effective combinations to address the escalating AMR crisis.
The escalating crisis of antimicrobial resistance (AMR) represents one of the most severe threats to global public health, with multidrug-resistant (MDR) pathogens already responsible for over 700,000 deaths annually and projections suggesting this number could rise to 10 million by 2050 without effective interventions [85]. Traditional antibiotics, which typically target specific bacterial processes, are increasingly compromised by sophisticated bacterial resistance mechanisms including enzymatic inactivation, efflux pumps, decreased membrane permeability, and target modification [86] [85]. The limitations of conventional antibiotics are further exacerbated by their inability to penetrate protective biofilms—structured microbial communities that can exhibit up to 1000-fold increased resistance compared to planktonic bacteria [85]. This dire landscape has accelerated the development of novel antimicrobial strategies that operate through fundamentally different mechanisms, offering promise in overcoming resistant pathogens. Among the most promising are antimicrobial peptides (AMPs), nanoparticles, and phage therapy, each presenting unique advantages for circumventing traditional resistance pathways and providing new therapeutic options against infections that have become refractory to conventional antibiotics [87] [88] [85].
Antimicrobial Peptides (AMPs): Mechanism and Therapeutic Potential
Mechanisms of Action and Biological Activities
Antimicrobial peptides are naturally occurring molecules that constitute an essential component of the innate immune response across all biological domains. These peptides exhibit a distinctive mechanism of action that centers primarily on targeting bacterial membranes, significantly reducing the likelihood of resistance development compared to conventional antibiotics [89] [90]. The amphiphilic structure of AMPs—featuring a hydrophilic N-terminus rich in cationic amino acids and a hydrophobic C-terminus—enables them to interact electrostatically with negatively charged bacterial membrane components [90]. This interaction leads to membrane disruption through several models, including the barrel-stave pore model, toroidal pore model, carpet model, and detergent-like model, all ultimately resulting in membrane permeability and cell death [90].
Beyond their direct membrane-disrupting activity, AMPs also employ non-membrane targeting mechanisms. They can inhibit cell wall synthesis by binding to essential components like lipid II, creating a spatial barrier that obstructs synthesis processes, as demonstrated by daptomycin and Nisin [90]. Additionally, AMPs can exert intracellular effects by interfering with vital components such as nucleic acids and proteins; for instance, indolicidin embeds within DNA to inhibit topoisomerase activity, while PR-39 degrades proteins associated with DNA replication [90]. This multi-target approach makes AMPs particularly valuable against MDR pathogens. Furthermore, AMPs exhibit diverse biological activities including antibiofilm, antiviral, antifungal, and immunomodulatory properties, positioning them as versatile therapeutic agents [87] [90]. Their ability to work synergistically with conventional antibiotics has been suggested as a key weapon against multi-antibiotic-resistant bacteria, potentially restoring efficacy to existing treatments [87].
Experimental Approaches and Research Reagents
Table 1: Key Research Reagents for Antimicrobial Peptide Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Natural AMPs | NaD1 (tobacco defensin), Nisin, Polymyxin B | Study innate defense mechanisms; reference compounds for activity comparisons |
| Synthetic AMPs | C18G & truncated forms, BiF2_5K7K, A-11, AP19, MV6, Omiganan | Investigate structure-activity relationships; optimize stability and efficacy |
| Model Lipid Membranes/Vesicles | Various phospholipid compositions | Study membrane interaction mechanisms, including pore formation and disruption |
| Bacterial Strains | Drug-resistant P. aeruginosa, K. pneumonia, MRSA, E. coli | Evaluate spectrum of activity and efficacy against clinically relevant pathogens |
| Mammalian Cell Lines | Standard cytotoxicity models (e.g., hemolysis assays) | Assess selectivity and safety profiles |
| Algorithmic Prediction Tools | α-hairpin prediction algorithms | Design novel AMPs with enhanced properties |
Advanced methodologies in AMP research include the use of model lipid membranes and vesicles to study peptide-membrane interactions, with recent work by Meier et al. demonstrating that peptide length and ensuing hydrophobic matching are critical factors in the evolution and design of membrane-disrupting AMPs [87]. Synthetic biology approaches enable the creation of optimized AMP variants, as exemplified by BiF2_5K7K, which demonstrated superior activity against Gram-positive and Gram-negative bacteria isolated from boar semen and sow vaginal discharge, achieving improved pregnancy and farrowing rates in artificial insemination tests at pig farms [87]. Similarly, synthetic AMPs A-11 and AP19 restricted the growth of Gram-negative bacteria in boar semen without harming sperm motility, acrosomal integrity, or viability, suggesting their potential as alternatives to conventional antibiotics in semen extenders [87]. Algorithmic approaches are also emerging, with Slavokhotova et al. developing predictive algorithms for α-hairpins based on characteristic motifs containing four or six cysteines, discovering that AMPs with six cysteines exhibited more potent antimicrobial activity than those with four [87].
Nanoparticle-Based Antimicrobial Strategies
Mechanisms of Antimicrobial Action
Nanoparticles represent a paradigm shift in antimicrobial therapy, offering unique physicochemical properties that enable multi-modal mechanisms of action distinct from conventional antibiotics. Metallic nanoparticles, particularly silver nanoparticles (AgNPs), exhibit broad-spectrum antimicrobial activity through several simultaneous pathways: generation of reactive oxygen species (ROS) that cause oxidative damage to cellular components; direct disruption of bacterial membranes; and interference with DNA replication and protein synthesis [91] [88] [85]. The high surface area-to-volume ratio of nanoparticles enhances their interaction with bacterial membranes, while their tunable surface chemistry allows for functionalization that improves targeting and efficacy [88] [85]. This multi-mechanistic approach is particularly advantageous against MDR pathogens as it circumvents traditional resistance pathways that typically involve specific molecular targets.
Nanoparticles also demonstrate exceptional efficacy against biofilms, a major challenge in treating chronic infections. Their small size enables penetration through the extracellular polymeric substance that characterizes biofilms, while their functionalizable surfaces can be engineered to deliver antimicrobial payloads directly to embedded bacteria [85]. This capability addresses a critical limitation of conventional antibiotics, which often fail to eradicate biofilm-associated infections. The versatility of nanoparticle systems extends to their composition diversity, including metal-based nanoparticles (silver, zinc oxide, gold), carbon-based nanomaterials, and polymeric nanostructures, each offering distinct advantages for specific therapeutic applications [88] [85].
Experimental Approaches and Research Reagents
Table 2: Research Reagents for Nanoparticle Antimicrobial Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Metal Nanoparticles | AgNPs, ZnONPs, AuNPs | Intrinsic antimicrobial activity; antibiotic delivery vehicles |
| Polymeric Nanoparticles | Cationic polymers, PLGA nanoparticles | Membrane disruption; controlled release of antimicrobials |
| Carbon-Based Nanomaterials | Graphene oxide, carbon nanotubes | Enhanced drug loading; photothermal therapy |
| Functionalization Ligands | Antibodies, peptides, carbohydrates | Target-specific delivery to pathogens or infected cells |
| Bacterial Strains | MRSA, CRAB, VRE, MDR P. aeruginosa | Evaluate efficacy against priority pathogens |
| Biofilm Models | Static, flow-cell, in vivo biofilm models | Assess penetration and anti-biofilm activity |
Critical to nanoparticle research is the comprehensive characterization of physicochemical properties, including size, shape, surface charge, and stability, all of which significantly influence antimicrobial efficacy [91] [88]. Synthesis methods—whether physical, chemical, or biological—must be carefully optimized as they directly impact these critical parameters [91]. Research protocols typically involve in vitro susceptibility testing against planktonic and biofilm-embedded MDR pathogens, with particular emphasis on ESKAPE pathogens that pose the greatest clinical threat [88]. Synergistic studies combining nanoparticles with conventional antibiotics represent a particularly promising area, with numerous reports demonstrating that such combinations can restore antibiotic efficacy against resistant strains by enhancing drug uptake or inhibiting resistance pathways [85]. For instance, gold nanoparticles have been shown to potentiate vancomycin activity against MRSA by facilitating its interaction with bacterial membranes [85]. Assessment of cytotoxicity using mammalian cell lines and evaluation of in vivo toxicity profiles are essential components of the development pipeline, addressing concerns about potential adverse effects [86].
Nanoparticle Antimicrobial Mechanisms and Applications
Phage Therapy: Bacteriophage-Based Interventions
Mechanisms and Evolutionary Approaches
Bacteriophage therapy utilizes viruses that specifically infect and lyse bacterial hosts, offering a highly targeted approach to combating MDR pathogens. Phages initiate infection through receptor-binding proteins that recognize specific bacterial surface structures such as outer membrane proteins, teichoic acids, lipopolysaccharides, capsules, pili, and flagella [92]. Following attachment, lytic phages inject their genetic material and hijack the host's cellular machinery to replicate, ultimately causing bacterial lysis and release of progeny virions [93]. This precise mechanism enables phages to target pathogenic bacteria while preserving beneficial microbiota, a significant advantage over broad-spectrum antibiotics [92].
A key innovation in modern phage therapy involves harnessing evolutionary principles to overcome bacterial resistance. Adaptive evolution strategies, such as the Appelmans protocol, accelerate phage-bacteria coevolution under controlled conditions to generate phages with expanded host ranges and enhanced lytic capabilities [92]. This approach simulates natural evolutionary pressures, selecting for phages that can overcome bacterial defense mechanisms including receptor modification, CRISPR-Cas systems, restriction-modification systems, and biofilm formation [92]. Furthermore, researchers are exploiting the concept of evolutionary trade-offs, wherein bacterial resistance to phages coincides with reduced antibiotic resistance or attenuated virulence [92] [94]. For instance, phage OMKO1 infects Pseudomonas aeruginosa through the Mex efflux pump system, and bacterial mutations conferring phage resistance often compromise efflux function, thereby resensitizing the bacteria to antibiotics [94]. This strategic approach transforms the inevitable emergence of phage resistance into a therapeutic advantage.
Experimental Approaches and Research Reagents
Table 3: Research Reagents for Phage Therapy Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Lytic Phages | T4 (Myoviridae), T7 (Podoviridae), lambda (Siphoviridae) | Therapeutic agents; models for host interaction studies |
| Phage DNA Isolation Kits | Norgen Biotek's Phage DNA Isolation Kit (Cat. 46800) | High-quality viral DNA purification for genomic characterization |
| Bacterial Host Strains | MDR clinical isolates, biofilm-forming strains | Phage host range determination; efficacy testing |
| Evolutionary Models | Appelmans protocol, co-culture systems | Host range expansion; overcoming bacterial resistance |
| Delivery Systems | Liposomes, hydrogels, nebulizers | Enhanced phage stability and targeted delivery |
| Sequencing Platforms | Illumina, Oxford Nanopore Technologies (ONT) | Genomic characterization; safety assessment |
Phage therapy research requires specialized methodologies for phage isolation, characterization, and application. Critical initial steps include environmental sampling from appropriate niches and phage purification through plaque assays [93]. Genomic characterization using high-quality DNA extraction methods, such as Norgen Biotek's Phage DNA Isolation Kit, enables comprehensive analysis to confirm lytic capability and absence of virulence or antibiotic resistance genes [93]. Host range determination against panels of clinically relevant bacterial strains is essential for assessing therapeutic potential [92]. Advanced approaches include adaptive evolution experiments to expand host range and overcome resistance, and encapsulation strategies using liposomes or hydrogels to enhance phage stability and delivery [86]. For respiratory infections, such as those in cystic fibrosis patients, specialized nebulization systems are employed for inhaled phage delivery, as demonstrated in a recent clinical study where personalized inhaled phage therapy significantly reduced P. aeruginosa density and improved lung function in patients [94]. Combination therapies phages with antibiotics are also a major research focus, investigating synergistic effects that enhance bacterial killing and suppress resistance development [86].
Phage Therapy Mechanisms and Delivery Strategies
Comparative Analysis and Future Perspectives
Technical Comparison of Antimicrobial Modalities
Table 4: Comparative Analysis of Novel Antimicrobial Modalities
| Characteristic | Antimicrobial Peptides | Nanoparticles | Phage Therapy |
|---|---|---|---|
| Primary Mechanism | Membrane disruption; intracellular targeting | ROS generation; membrane damage; drug delivery | Bacterial lysis through viral replication |
| Spectrum of Activity | Broad-spectrum typically | Broad-spectrum typically | Narrow, strain-specific typically |
| Resistance Potential | Low due to multi-target mechanisms | Low due to multi-mechanistic action | Moderate (requires cocktails/evolutionary approaches) |
| Biofilm Activity | Moderate to high (disruptive) | High (penetration + delivery) | Variable (phage-dependent) |
| Clinical Status | 12 FDA-approved peptides; several in trials [87] [90] | Preclinical and early clinical development | Compassionate use; clinical trials ongoing [94] |
| Key Advantages | Immunomodulatory properties; rapid killing | Multifunctional; tunable properties; synergistic potential | Self-amplifying; high specificity; evolutionary trade-offs |
| Major Challenges | Cytotoxicity; proteolytic degradation; production cost | Toxicity concerns; scalability; regulatory frameworks | Host range limitations; bacterial resistance; standardization |
Integration and Future Directions
The future of antimicrobial development likely lies in strategic integration of these complementary modalities rather than relying on any single approach. Promising integrative strategies include nanoparticle-based AMP delivery systems that enhance stability and bioavailability [90], phage-antibiotic synergy (PAS) combinations that enhance efficacy and suppress resistance [86], and nanotechnology-enabled phage delivery systems that improve targeting and intracellular reach [86]. The synergistic potential of these combinations represents a paradigm shift from monotherapy to multi-target approaches that address the complexity of bacterial resistance.
Significant challenges remain in the clinical translation of these novel modalities. For AMPs, issues of cytotoxicity, proteolytic degradation, and production costs must be addressed through structural optimization and advanced delivery systems [90]. Nanoparticle therapies require comprehensive toxicity assessment, standardization of characterization protocols, and scalable manufacturing processes [88] [85]. Phage therapy faces hurdles in host range limitations, standardization of production, and regulatory approval pathways [92] [86]. Ongoing research is addressing these challenges through bioengineering approaches, computational design tools including artificial intelligence, and development of appropriate regulatory frameworks that accommodate the unique characteristics of these biological and nanomaterial-based therapeutics [87] [88].
The emergence of these novel antimicrobial modalities signals a transformative period in infectious disease treatment. By leveraging fundamentally different mechanisms of action compared to conventional antibiotics, AMPs, nanoparticles, and phage therapy offer promising pathways to overcome multidrug resistance. Their continued development, alone and in strategic combinations, represents our best hope for addressing the escalating crisis of antimicrobial resistance and safeguarding the future of infectious disease treatment.
Overcoming Biofilm-Associated Enhanced Intrinsic Resistance
Biofilms are structured communities of microbial cells encased within a self-produced extracellular polymeric substance (EPS) and are a primary mode of growth for bacteria in both natural and clinical environments [95] [96]. The biofilm lifestyle confers a remarkable level of intrinsic tolerance and resistance to antimicrobial agents, creating significant challenges in treating associated infections [97]. This intrinsic resistance is a multifaceted phenomenon, distinct from acquired genetic resistance, and is a major contributor to the persistence of chronic infections and the global antimicrobial resistance (AMR) crisis [96]. Within the broader context of intrinsic antibiotic resistance research, understanding the specific mechanisms that biofilms employ to withstand antibiotic therapy is paramount for developing effective countermeasures. This whitepaper delineates the core mechanisms underlying biofilm-associated enhanced intrinsic resistance and synthesizes current experimental and strategic approaches to overcome this formidable defensive barrier, providing a technical guide for researchers and drug development professionals.
Core Mechanisms of Biofilm-Mediated Intrinsic Resistance
The intrinsic resistance of biofilms is not attributable to a single mechanism but arises from a complex interplay of physical, physiological, and adaptive traits of the biofilm community [95] [96].
The Biofilm Matrix as a Physical and Chemical Barrier
The extracellular matrix is a hallmark of biofilms, comprising polysaccharides, proteins, extracellular DNA (eDNA), and lipids [95] [98]. This matrix acts as a formidable barrier to antimicrobial penetration. The anionic components of the matrix, particularly eDNA, can bind to cationic antimicrobials such as aminoglycosides, effectively trapping them and preventing their diffusion to the cellular targets [95]. Furthermore, the matrix harbors extracellular enzymes such as β-lactamases that can inactivate antibiotics before they reach their targets [97]. The matrix can constitute over 90% of the biofilm's dry mass, creating a significant diffusive barrier that contributes to the requirement for antibiotic concentrations that can be 100 to 800 times higher than the minimum inhibitory concentration (MIC) for their planktonic counterparts to be effective [97].
Physiological Heterogeneity and Persister Cell Formation
Biofilms are physiologically heterogeneous environments. Gradients of nutrients, oxygen, and waste products create distinct metabolic niches within the biofilm structure [97] [99]. Cells in the deeper layers of the biofilm often experience nutrient limitation, leading to slow growth or a dormant state [97]. Since many antibiotics are most effective against rapidly dividing cells, these dormant populations exhibit heightened tolerance [99]. A sub-population of these dormant cells, known as persisters, are transiently tolerant to high concentrations of antibiotics and can repopulate the biofilm once antibiotic pressure is removed, leading to recurrent infections [96]. This heterogeneity is often modeled in terms of "zones," where each bacterial cell responds to its immediate microenvironment, leading to a mosaic of physiological states [97].
Altered Microenvironment and Stress Responses
The metabolic activity of biofilm cells alters the local microenvironment, which can further impact antibiotic efficacy. For example, the accumulation of acidic waste products in the biofilm core can reduce the efficacy of antibiotics whose activity is pH-dependent [97]. Additionally, the biofilm mode of growth is associated with an upregulation of general stress responses, which can contribute to a non-specific increase in tolerance [95]. Hypoxic conditions within dense biofilm microcolonies have been shown to enhance antibiotic resistance by altering the composition and function of multidrug efflux pumps [97].
Enhanced Mutation Rates and Horizontal Gene Transfer
Biofilms provide a hotspot for genetic exchange and diversification. The rate of point mutations has been documented to be 4 to over 100-fold higher in biofilms compared to planktonic cultures, which is often linked to oxidative stress within the biofilm microenvironment [99]. This elevated mutation rate accelerates the emergence of resistant mutants. Moreover, the dense, structured nature of biofilms and the presence of eDNA facilitate horizontal gene transfer (HGT) through conjugation and transformation, enabling the spread of resistance genes within the biofilm community [99] [96].
Table 1: Key Mechanisms of Biofilm-Associated Intrinsic Resistance and Their Functional Consequences
| Mechanism | Key Components | Functional Consequence |
|---|---|---|
| Matrix-Mediated Resistance | Exopolysaccharides, eDNA, Proteins [95] [98] | Traps & inactivates antibiotics; impedes diffusion [95] [97] |
| Physiological Heterogeneity | Nutrient/Oxygen gradients; Slow-growing cells; Persisters [97] [99] | Reduces efficacy of cidal antibiotics; enables re-population [97] [96] |
| Efflux Pump Activity | Upregulated multidrug efflux pumps (e.g., in P. aeruginosa) [97] | Active extrusion of multiple antibiotic classes from cells |
| Genetic Diversification | High mutation rate; Horizontal Gene Transfer (HGT) [99] [96] | Accelerates emergence and spread of resistance genes |
Experimental Approaches for Investigating Biofilm Resistance
A critical step in overcoming biofilm resistance is its accurate detection and quantification in the laboratory. A range of methodologies is employed to study biofilm formation, structure, and susceptibility.
Standardized Biofilm Detection and Quantification Methods
Phenotypic methods remain the cornerstone for identifying and quantifying biofilm formation. The Tissue Culture Plate Method (TCPM) is widely considered the gold standard for quantitative assessment of biofilm formation [100]. This method involves growing biofilms in 96-well plates, staining with crystal violet, and measuring the absorbance to quantify biomass. Alternative methods include the Tube Method (TM) and Congo Red Agar (CRA) method, which are less quantitative but useful for initial screening [100]. A comparative analysis of these methods found that for catheter-derived bacterial isolates, the CRA method showed higher sensitivity (81.8%) and specificity (61.5%) than the Tube method (72.7% and 46.2%, respectively) [100]. Strong biofilm formation has been directly correlated with higher antimicrobial resistance profiles in clinical isolates, underscoring the importance of accurate detection [100].
Determining Biofilm Antimicrobial Susceptibility
Evaluating the susceptibility of biofilms to antimicrobial agents requires specialized approaches distinct from standard planktonic MIC tests. The Minimal Biofilm Eradication Concentration (MBEC) assay is a commonly used method that measures the lowest concentration of an antibiotic required to eradicate a biofilm grown on a peg lid [99]. Another key metric is the Minimal Duration for Killing (MDK), which quantifies the time required to kill a specific fraction (e.g., 99% or 99.99%) of the biofilm population [99]. This is particularly relevant for capturing tolerance phenotypes, where biofilms can survive prolonged exposure to high antibiotic concentrations without a change in the conventional MIC [99]. Experimental evolution, where biofilm populations are repeatedly exposed to antimicrobial treatments, has proven invaluable for shedding light on the evolutionary trajectories and genetic adaptations that lead to reduced susceptibility in biofilms [99] [101].
Table 2: Key Metrics for Assessing Biofilm Antimicrobial Susceptibility
| Metric | Definition | Significance in Biofilms |
|---|---|---|
| Minimum Inhibitory Concentration (MIC) | Lowest antibiotic concentration that prevents visible growth of planktonic cells [99] | Often irrelevant for biofilms; does not predict efficacy [97] |
| Minimum Biofilm Eradication Concentration (MBEC) | Lowest antibiotic concentration that eradicates a biofilm [99] | More clinically relevant; can be 100-800x higher than planktonic MIC [97] |
| Minimum Duration for Killing (MDK) | Time required to kill a defined fraction (e.g., 99.99%) of the biofilm population [99] | Quantifies tolerance; key for determining treatment duration |
Diagram 1: Biofilm Susceptibility Testing Workflow. This flowchart outlines the general process for determining the Minimum Biofilm Eradication Concentration (MBEC) and Minimal Duration for Killing (MDK).
Strategic Pathways for Overcoming Biofilm Resistance
The complexity of biofilm resistance necessitates innovative therapeutic strategies that extend beyond conventional antibiotic treatments. These approaches aim to disrupt the protective architecture of the biofilm, target its unique physiology, or prevent its formation.
Matrix-Targeting Dispersal Agents
A primary strategy is to degrade the EPS matrix to sensitize the biofilm to antibiotics and host immune responses. Enzymes such as glycoside hydrolases (which break down polysaccharides), dispersin B, and DNase I (which degrades eDNA) have shown efficacy in disrupting the biofilm matrix and enhancing the activity of co-administered antibiotics in in vitro models [95] [98]. For instance, the use of glycoside hydrolases has been demonstrated to induce dispersal in monospecies and multispecies P. aeruginosa and S. aureus biofilm models, suggesting potential for treating chronic wound infections [95].
Quorum Sensing Inhibition
Quorum sensing (QS) is a cell-cell communication system that regulates biofilm formation, virulence, and resistance in a cell-density-dependent manner [97] [98]. Quorum Sensing Inhibitors (QSIs) interfere with this signaling, potentially attenuating biofilm development and pathogenicity without exerting a lethal selective pressure. Gram-negative bacteria use acyl-homoserine lactones (AHLs), while Gram-positive bacteria use autoinducing peptides [97] [98]. QSIs can function by degrading these autoinducer signals or blocking their receptors. This disruption has been shown to downregulate the expression of efflux pumps and other virulence factors, making the biofilm more susceptible to antibiotic treatment [97] [98].
Targeting Intracellular Signaling: c-di-GMP
The secondary messenger bis-(3'-5')-cyclic dimeric guanosine monophosphate (c-di-GMP) is a central regulator of the switch between motile planktonic and sessile biofilm lifestyles in bacteria [95] [98]. High intracellular levels of c-di-GMP promote biofilm formation by upregulating matrix production and suppressing motility. Consequently, inhibiting diguanylate cyclases (DGCs), the enzymes that synthesize c-di-GMP, presents a promising strategy to prevent biofilm formation or trigger its dispersal [98]. Mutations in genes regulating c-di-GMP breakdown, such as rpfR in Burkholderia cenocepacia, lead to increased biofilm mass, underscoring the therapeutic potential of modulating this pathway [95].
Diagram 2: Biofilm Lifecycle and Therapeutic Targets. This diagram illustrates the stages of biofilm development and highlights key regulatory systems (Quorum Sensing and c-di-GMP signaling) that are targets for anti-biofilm strategies.
Eradication of Persister Cells
Targeting the dormant persister cell subpopulation is crucial for preventing biofilm relapse. While persisters are tolerant to most conventional antibiotics, they can be killed by certain compounds that remain active against non-growing cells. These include bacterial metabolite analogs that disrupt energy production, membrane-targeting agents such as cationic antimicrobial peptides, and some newer-generation fluoroquinolones [98]. Combining these agents with matrix-disrupting agents or antibiotics can lead to more complete eradication of the biofilm community.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Biofilm Research
| Reagent / Material | Function in Biofilm Research | Example Application |
|---|---|---|
| Polystyrene Microtiter Plates | Substrate for high-throughput biofilm growth and quantification [100] | Tissue Culture Plate Method (TCPM) for biofilm biomass measurement [100] |
| Crystal Violet Stain | Dye that binds to biofilm biomass (cells and matrix) [100] | Staining and semi-quantification of biofilms in the TCPM [100] |
| Silicone Coupons / Pegs | Medical-grade material to mimic biofilm growth on implants [101] | MBEC assay systems and experimental evolution studies [99] [101] |
| Dispersin B & DNase I | Enzymes for selective degradation of matrix components [95] [98] | Studying matrix function and as a potential anti-biofilm agent [95] |
| Congo Red Agar (CRA) | Differential medium for phenotypic identification of biofilm producers [100] | Initial screening and characterization of bacterial isolates [100] |
| Quorum Sensing Inhibitors (QSIs) | Small molecules that block bacterial cell-cell communication [97] [98] | Investigating QS role in virulence and testing combination therapies [98] |
Overcoming biofilm-associated enhanced intrinsic resistance requires a paradigm shift from traditional antibiotic therapies toward a multi-targeted approach. The synergistic combination of matrix-disrupting agents, quorum sensing inhibitors, antipersister compounds, and conventional antibiotics represents the most promising avenue for effective biofilm eradication. Future research must leverage advanced models, such as experimental evolution in biofilms and multispecies community analyses, to better predict therapeutic outcomes and resistance evolution. By deepening our understanding of the fundamental mechanisms that underpin biofilm resilience and strategically targeting its vulnerabilities, the scientific community can develop the next generation of anti-biofilm therapeutics to address this critical component of the AMR crisis.
Pathogen Prioritization and Pipeline Analysis: Validating Targets and Novel Agents
Comparative Analysis of Intrinsic Resistance in ESKAPE Pathogens
The ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter spp.) represent a critical group of multidrug-resistant bacteria capable of "escaping" the biocidal action of antimicrobial agents. This comprehensive analysis examines the intrinsic resistance mechanisms that render these pathogens particularly challenging in clinical settings. By integrating recent experimental data on resistance development, comparative resistance profiles across healthcare and environmental settings, and detailed mechanistic studies, this review provides a framework for understanding the evolutionary and molecular basis of treatment failure. The findings highlight the urgent need for innovative therapeutic strategies that anticipate and counter resistance mechanisms from the earliest stages of drug development.
Antimicrobial resistance (AMR) represents one of the most formidable challenges in modern infectious disease therapy, with the ESKAPE pathogens standing as particularly concerning culprits in hospital-acquired infections (HAIs) worldwide [102]. These pathogens are characterized by their enhanced capacity to develop multidrug resistance (MDR) and extensively drug-resistant (XDR) profiles through diverse genetic and phenotypic adaptations [103]. The World Health Organization (WHO) has classified these bacteria as priority pathogens for which new antibiotics are urgently needed, with carbapenem-resistant A. baumannii, P. aeruginosa, and Enterobacteriaceae listed as critical priorities [104].
Intrinsic resistance refers to the innate ability of a bacterial species to resist antibiotic classes through its inherent structural or functional characteristics, as opposed to acquired resistance gained through mutation or horizontal gene transfer. This analysis systematically compares these intrinsic resistance mechanisms across the ESKAPE spectrum, examining how limitations in drug uptake, production of antibiotic-degrading enzymes, alterations in drug target sites, and enhanced drug efflux systems collectively contribute to treatment failures [103]. Understanding these pathways is vital for formulating innovative therapeutic strategies against these resilient pathogens.
Comparative Resistance Profiles Across ESKAPE Pathogens
Global Resistance Prevalence in Clinical Settings
Table 1: Pooled Antibiotic Resistance Proportions in Hospital-Acquired ESKAPE Infections from Low- and Lower-Middle-Income Countries [105]
| Pathogen | Antibiotic Class | Resistance Proportion (%) | 95% Confidence Interval |
|---|---|---|---|
| Staphylococcus aureus | Methicillin | 48.4 | 41.7-55.2 |
| Acinetobacter baumannii | Carbapenem | 72.4 | 62.1-81.7 |
| Pseudomonas aeruginosa | Carbapenem | 37.1 | 24.6-45.9 |
| Klebsiella pneumoniae | Carbapenem | 34.9 | 24.6-45.9 |
| Klebsiella pneumoniae | Third-generation cephalosporins | 78.7 | 71.5-85.2 |
| Escherichia coli | Carbapenem | 16.6 | 10.7-23.4 |
| Escherichia coli | Third-generation cephalosporins | 78.5 | 72.1-84.2 |
| Enterobacter spp. | Carbapenem | 51.2 | 27.5-74.7 |
| Enterobacter spp. | Third-generation cephalosporins | 83.5 | 71.9-92.8 |
Recent meta-analyses reveal alarming resistance patterns among ESKAPE pathogens in healthcare settings, particularly in resource-constrained regions. As shown in Table 1, Gram-negative ESKAPE pathogens exhibit exceptionally high resistance to last-line antibiotics, with carbapenem-resistant A. baumannii surpassing 70% in pooled analyses [105]. The high between-study heterogeneity (I² > 80%) indicates substantial variation in resistance patterns across different geographical regions, possibly reflecting disparities in antibiotic stewardship, infection control practices, and surveillance systems.
Resistance Development to Novel Antibiotic Candidates
Table 2: Laboratory Evolution of Resistance to Recent Antibiotics in Gram-Negative ESKAPE Pathogens [106]
| Parameter | Finding | Clinical Relevance |
|---|---|---|
| Timeframe for resistance development | 60 days (∼120 generations) | Rapid resistance emergence |
| Median resistance level increase | 64-fold MIC increase | Substantial reduction in efficacy |
| Populations reaching peak plasma concentration MIC | 87% of ALE-adapted lines | Likely treatment failure |
| Populations surpassing clinical breakpoints | 88.3% of ALE-adapted lines | Exceeds resistance thresholds |
| Frequency of resistance emergence | No significant difference between recent and control antibiotics | New candidates as prone to resistance as existing drugs |
Concerningly, even antibiotic candidates in development show susceptibility to resistance evolution. Laboratory evolution experiments demonstrate that clinically relevant resistance emerges within 60 days of antibiotic exposure in Escherichia coli, K. pneumoniae, A. baumannii, and P. aeruginosa [106]. As detailed in Table 2, recent antibiotics in development demonstrate similar susceptibility to resistance emergence compared to established antibiotics, with median resistance levels increasing approximately 64-fold during experimental evolution. This indicates that intrinsic resistance mechanisms provide a foundation for rapid adaptation even to novel compounds.
Molecular Mechanisms of Intrinsic Resistance
Comparative Analysis of Resistance Mechanisms Across ESKAPE Pathogens
The intrinsic resistance of ESKAPE pathogens stems from four primary mechanisms that operate individually or in combination:
3.1.1 Limitations in Drug Uptake Gram-negative ESKAPE pathogens possess an outer membrane that serves as a formidable permeability barrier, particularly in A. baumannii, P. aeruginosa, and K. pneumoniae [103]. This membrane structure, complemented by selective porin channels, intrinsically restricts antibiotic penetration. Porin modifications and loss-of-function mutations further enhance resistance by reducing intracellular antibiotic accumulation to sub-inhibitory concentrations.
3.1.2 Antibiotic-Inactivating Enzymes ESKAPE pathogens produce a diverse array of antibiotic-degrading enzymes that confer class-specific resistance. Extended-spectrum β-lactamases (ESBLs) and carbapenemases are particularly prevalent in K. pneumoniae, A. baumannii, and Enterobacter spp., conferring resistance to last-resort β-lactam antibiotics [102]. The genes encoding these enzymes are frequently located on mobile genetic elements, facilitating horizontal transfer within and between species.
3.1.3 Target Site Modifications Alterations in antibiotic target sites represent another fundamental resistance strategy. Methicillin-resistant S. aureus (MRSA) exhibits modified penicillin-binding proteins (PBP2a) with reduced affinity for β-lactam antibiotics [102]. Similarly, target protection and replacement mechanisms confer resistance to other antibiotic classes across ESKAPE pathogens.
3.1.4 Efflux Pump Systems Multidrug efflux pumps actively export antibiotics from the bacterial cell, maintaining intracellular concentrations below effective levels. These systems often exhibit broad substrate specificity, contributing to MDR phenotypes. The RND-type efflux pumps in Gram-negative ESKAPE pathogens are particularly effective against multiple antibiotic classes [103].
Diagram 1: Comprehensive Resistance Mechanisms in ESKAPE Pathogens. This diagram illustrates the four primary intrinsic resistance mechanisms employed by ESKAPE pathogens and their progression from multidrug resistance (MDR) to extensively drug-resistant (XDR) phenotypes.
Species-Specific Resistance Profiles
The distribution and predominance of resistance mechanisms vary significantly across ESKAPE pathogens:
Acinetobacter baumannii has emerged as one of the most challenging ESKAPE pathogens due to its remarkable capacity to acquire and disseminate resistance genes through mobile genetic elements, including plasmids, resistance islands, and insertion sequences [104]. This pathogen additionally employs biofilm formation as a complementary resistance mechanism, providing physical protection against antibiotics and host immune factors.
Pseudomonas aeruginosa exhibits exceptional intrinsic resistance due to its low-permeability outer membrane and constitutive expression of multiple efflux pump systems. These native characteristics are frequently complemented by acquired resistance mechanisms, resulting in difficult-to-treat XDR strains, particularly in healthcare settings [102].
Klebsiella pneumoniae and Enterobacter spp. are notable for their high prevalence of ESBL and carbapenemase production, with resistance proportions exceeding 75% for third-generation cephalosporins in some settings [105]. The mobility of the genetic elements carrying these resistance genes facilitates rapid inter-species dissemination within healthcare environments.
Staphylococcus aureus employs distinct resistance strategies, with methicillin resistance mediated by the mecA gene encoding PBP2a in MRSA strains [102]. The continued evolution of MRSA, including the emergence of vancomycin-resistant strains (VRSA), underscores the adaptive capacity of this pathogen.
Enterococcus faecium exhibits intrinsic resistance to multiple antibiotic classes, with vancomycin resistance (VRE) representing a particularly serious concern in healthcare settings, limiting available treatment options [102].
Experimental Models for Studying Resistance Development
Laboratory Evolution Protocols
Understanding the trajectory of resistance development requires well-established experimental models that simulate the evolutionary pressures of clinical antibiotic exposure:
4.1.1 Spontaneous Frequency-of-Resistance (FoR) Analysis
- Methodology: Approximately 10¹⁰ bacterial cells are exposed to each antibiotic on agar plates for 2 days at concentrations to which the given strain is susceptible [106].
- Detection threshold: Mutants with at least a 4-fold increase in MIC are selected as resistant.
- Application: This approach identifies first-step resistance mutations and estimates their initial frequencies within populations.
4.1.2 Adaptive Laboratory Evolution (ALE)
- Duration: Up to 120 generations (typically 60 days) of continuous exposure to increasing antibiotic concentrations [106].
- Population design: Ten parallel-evolving populations for each bacterial strain-antibiotic combination.
- Endpoint analysis: Comparison of MICs in evolved lines versus ancestral strains to quantify resistance development.
4.1.3 Functional Metagenomics
- Objective: Identification of mobile resistance genes present in clinical isolates, soil, and human gut microbiomes [106].
- Application: Assesses the potential for horizontal transfer of resistance determinants from environmental reservoirs to clinical pathogens.
Diagram 2: Experimental Workflow for Analyzing Antibiotic Resistance Development. This diagram outlines the integrated methodological approach for studying resistance emergence in ESKAPE pathogens, combining short-term and evolutionary analyses with functional genetic assessments.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagent Solutions for ESKAPE Resistance Studies
| Category | Specific Reagents/Assays | Function and Application |
|---|---|---|
| Susceptibility Testing | CLSI/EUCAST guidelines, Broth microdilution, Agar dilution | Standardized MIC determination for resistance classification |
| Molecular Analysis | PCR for resistance genes (e.g., mecA, blaKPC, vanA), Whole-genome sequencing | Identification of genetic determinants of resistance |
| Strain Collections | Clinical isolates (SEN, MDR, XDR), Reference strains (ATCC) | Comparative analysis of resistance mechanisms and evolution |
| Evolution Experiments | Mueller-Hinton agar, Cation-adjusted broth, 96-well plates | Media and materials for FoR and ALE studies |
| Antibiotic Solutions | Recent antibiotics (SPR-206, cefiderocol), Control antibiotics (carbapenems, fluoroquinolones) | Comparative resistance development studies |
| Bioinformatic Tools | Resistance gene databases (CARD, ResFinder), Phylogenetic analysis software | Analysis of evolutionary trajectories and resistance gene dissemination |
This comprehensive toolkit enables researchers to systematically investigate intrinsic resistance mechanisms and their evolution under antibiotic pressure. The combination of standardized phenotypic assays with advanced genomic analyses provides multidimensional insights into the resistance potential of ESKAPE pathogens [106] [102].
Discussion and Future Perspectives
The comparative analysis of intrinsic resistance in ESKAPE pathogens reveals several critical insights with profound implications for antibiotic development and clinical practice. First, the overlapping resistance mechanisms between established antibiotics and novel candidates indicate that current compound optimization approaches may be insufficient to overcome evolutionary resistance pathways [106]. Second, the environmental persistence of ESKAPE pathogens creates reservoirs for community-acquired infections and resistance gene dissemination, extending the challenge beyond traditional healthcare settings [107] [104].
Strategic Approaches to Counteract Intrinsic Resistance
Future efforts to combat ESKAPE pathogens should prioritize several key strategies:
Narrow-Spectrum Therapeutics: The significant heterogeneity in resistance development across antibiotic-strain combinations suggests potential for narrow-spectrum antibacterial therapies that could remain effective against specific ESKAPE pathogens [106]. Such targeted approaches may reduce selective pressure and delay resistance emergence.
Combination Therapies: The simultaneous use of multiple therapeutic agents with complementary mechanisms represents a promising strategy to overcome intrinsic resistance. Antibiotic-adjuvant combinations that inhibit resistance mechanisms (e.g., β-lactam/β-lactamase inhibitor combinations) have demonstrated clinical utility and may extend the lifespan of existing antibiotics [102].
Alternative Therapeutic Modalities: Non-traditional approaches, including bacteriophage therapy, antimicrobial peptides, nanoparticles, and photodynamic therapy, offer potential pathways to circumvent conventional resistance mechanisms [102]. These modalities typically employ distinct molecular targets that may bypass existing intrinsic resistance pathways.
Implications for Antibiotic Development
The finding that resistance mutations to antibiotic candidates are already present in natural populations indicates that clinical resistance can emerge rapidly through selection of pre-existing bacterial variants [106]. This underscores the critical importance of incorporating resistance forecasting from the earliest stages of drug development, including comprehensive assessment of resistance mutational backgrounds and mobile resistance genes in diverse microbial populations.
Furthermore, the environmental dimension of ESKAPE resistance necessitates a "One Health" approach that recognizes the interconnectedness of human, animal, and environmental reservoirs in the dissemination of resistance determinants [104]. Effective antimicrobial stewardship must therefore extend beyond clinical settings to encompass agricultural, veterinary, and environmental management practices.
This comparative analysis demonstrates that intrinsic resistance in ESKAPE pathogens stems from a sophisticated interplay of reduced drug permeability, enzymatic inactivation, target modification, and efflux mechanisms. The rapid evolution of resistance to even the most promising antibiotic candidates highlights the remarkable adaptability of these pathogens and the limitations of current developmental paradigms.
Moving forward, successful management of ESKAPE infections will require innovative approaches that anticipate and counter resistance mechanisms from the earliest stages of drug design. This includes enhanced surveillance of resistance determinants in clinical and environmental settings, development of companion diagnostics to guide targeted therapy, and exploration of non-traditional treatment modalities that operate outside conventional resistance pathways. By integrating these multidimensional strategies, the scientific community can work toward reversing the evolutionary trajectory that currently favors these master escapers of antimicrobial action.
The escalating crisis of antimicrobial resistance (AMR) underscores an urgent need for innovative antibiotics. This whitepaper evaluates the pronounced innovation gap between novel classes of antibiotics and derivative agents within the developmental pipeline. Analysis reveals that despite a global health threat claiming millions of lives annually, the current antibacterial pipeline is dominated by analogues of existing classes, particularly β-lactamase inhibitor combinations, which offer only incremental advances. The development of agents with new chemical classes or novel mechanisms of action—essential for overcoming intrinsic resistance mechanisms in priority Gram-negative pathogens—remains critically low. Framed within the context of intrinsic antibiotic resistance, this review synthesizes quantitative pipeline data, details experimental methodologies for resistome analysis, and proposes a strategic roadmap to revitalize antibiotic innovation, arguing that overcoming scientific and economic hurdles is imperative to secure the future of infectious disease treatment.
The relentless rise of antimicrobial resistance (AMR) poses a catastrophic threat to global health. Current estimates indicate that bacterial AMR was directly responsible for 1.3 million deaths globally in 2019 and associated with approximately 5 million fatalities, a burden that is projected to grow without intervention [108]. The World Health Organization (WHO) has declared AMR a top-tier global health threat, highlighting an urgent need for new therapeutic agents [109].
Antibiotic discovery experienced a "golden age" between the 1940s and 1960s, leading to the introduction of more than 20 new antibiotic classes. However, this period was followed by a stark "discovery void." Since 1987, only five novel antibiotic classes have reached the market [110]. This innovation drought is particularly alarming as bacteria develop resistance to existing drugs, rendering many infections untreatable. The core of this crisis is the innovation gap: the disconnect between the urgent need for antibiotics with new mechanisms of action and the predominance of derivative agents in development, which are often susceptible to pre-existing cross-resistance mechanisms [110].
This challenge is intrinsically linked to the concept of the intrinsic resistome. Defined as the set of chromosomally encoded elements that contribute to natural, non-acquired antibiotic resistance, the intrinsic resistome encompasses factors like the impermeability of cellular envelopes, the activity of multidrug efflux pumps, and the absence of drug targets [24] [44]. Gram-negative pathogens, in particular, are shielded by a formidable outer membrane and express efflux systems that collectively limit the penetration of many antibiotics, making them naturally resistant to a broad spectrum of drugs [24]. Deriving new agents from existing classes often fails to overcome these intrinsic barriers. Therefore, a deep understanding of the intrinsic resistome is not merely an academic exercise but a prerequisite for the rational design of truly novel antibiotics that can circumvent these inherent bacterial defenses [44].
Quantitative Analysis of the Current Antibiotic Pipeline
A quantitative assessment of the antibacterial development pipeline reveals a critical deficit of innovation. According to a 2024 WHO analysis, the current pipeline, while active, is insufficient to address the rapid spread of resistant infections [110].
Table 1: Analysis of the Traditional Antibacterial Clinical Pipeline (Adapted from WHO Data)
| Pipeline Category | Number of Agents | Key Observations | Implication for Innovation |
|---|---|---|---|
| Total Traditional Antibacterial Agents | 97 | Includes 57 traditional antibiotics and 40 non-traditional agents. | Pipeline is diversified but still insufficient. |
| Agents Targeting WHO BPPL | 32 | Pathogens listed on the WHO Bacterial Priority Pathogen List. | Focus remains on critical threats. |
| Agents Meeting WHO Innovation Criteria | 12 | Criteria include: no cross-resistance, new target, new MoA, and/or new chemical class. | Only ~21% of traditional agents are considered innovative. |
| Innovative Agents Targeting Critical Pathogens | 4 | These are agents with new MoAs or classes against critical-tier pathogens. | Severe gap for the most urgent threats. |
The data underscores a concerning trend: the pipeline is heavily populated with analogues of existing classes, especially β-lactam/β-lactamase inhibitor combinations [110]. While these derivatives can be effective in the short term and are less risky to develop, they represent incremental improvements. A vast majority (>80%) of antibiotics approved since 2017 belong to existing classes, with only two—vaborbactam (a β-lactamase inhibitor) and lefamulin—representing a new chemical class [110]. This lack of novelty is a fundamental vulnerability in the global strategy to combat AMR, as pathogens with intrinsic or acquired resistance to a parent antibiotic class will often exhibit cross-resistance to its derivatives.
Table 2: Categorization of Antibiotics in Clinical Development (2023 Data)
| Antibiotic Category | Representative Examples | Stage of Development (Number of Candidates) | Key Characteristics & Challenges |
|---|---|---|---|
| Traditional Antibiotics | Cephalosporins, Carbapenems, Macrolides | 57 candidates in total [110]. | Primarily derivatives; face pre-existing cross-resistance. |
| Non-Traditional Antibacterials | Phage-derived, Monoclonal Antibodies, Live Biotherapeutics | 40 candidates in total [110]. | Novel therapeutic modalities; regulatory pathways less defined. |
| Phage-derived Therapies | Exebacase (CF-301), Bacteriophage cocktails | Phase 1 to Phase 3 [109]. | High specificity; potential to overcome resistance via new MoAs. |
| Monoclonal Antibodies | Tosatoxumab (AR-301), Suvratoxumab (AR-302) | Phase 2 to Phase 3 [109]. | Target bacterial toxins or surface structures; can enhance immune clearance. |
The exit of major pharmaceutical companies from antibiotic research and development (R&D) has exacerbated this innovation gap. Since the 1990s, 18 major pharmaceutical firms have left the field, with the remaining few significantly scaling back their investments [110]. This exodus is largely driven by economic realities: the high cost of development (estimated at ~US$1.4 billion per approved drug), coupled with the low return on investment because antibiotics are typically used for short durations and are often held as reserves [108] [110]. The innovation void is, therefore, not solely a scientific failure but a market failure as well.
The Scientific Hurdle: Intrinsic Resistance and the Gram-Negative Challenge
The scientific challenge of developing novel antibiotics is profoundly linked to bacterial intrinsic resistance, a phenomenon that predates human antibiotic use and is present in all bacterial species [24]. The intrinsic resistome comprises a network of genes and pathways that contribute to a bacterium's innate ability to withstand antibiotics, extending beyond the classic barriers of outer membrane impermeability and efflux pumps to include fundamental metabolic processes [44].
For Gram-negative pathogens—which dominate the WHO's "Critical Priority" list, including Acinetobacter baumannii, Pseudomonas aeruginosa, and carbapenem-resistant Enterobacteriaceae—the intrinsic resistome presents a formidable obstacle. Their complex cell envelope structure, featuring an outer membrane with low permeability, acts as a primary barrier. This is synergistically supported by constitutively expressed multidrug efflux pumps (e.g., AcrAB-TolC in E. coli and MexAB-OprM in P. aeruginosa) that actively export a wide range of antibiotics, reducing their intracellular concentration [24] [44]. Consequently, many promising drug candidates active against Gram-positive bacteria fail to penetrate Gram-negative cells.
The following diagram illustrates the key components of the intrinsic resistome in a model Gram-negative bacterium and the strategic approach to counter it.
Diagram Title: Intrinsic Resistome and Therapeutic Strategies.
This multi-faceted nature of intrinsic resistance means that the susceptibility phenotype of a bacterium is an emergent property resulting from the concerted action of numerous elements [44]. Therefore, disabling key nodes of the intrinsic resistome through adjunct therapies (e.g., efflux pump inhibitors) represents a promising strategy to "re-purpose" existing antibiotics and enhance the efficacy of novel drugs against intrinsically resistant pathogens [24] [44].
Experimental Methodologies for Resistome Research and Novel Compound Identification
Bridging the innovation gap requires sophisticated experimental protocols to identify novel targets and compounds. Research into the intrinsic resistome and the discovery of new antibiotics leverage a suite of high-throughput genomic and culturing techniques.
Genome-Wide Analysis of the Intrinsic Resistome
Identifying the genetic basis of intrinsic resistance is crucial for target discovery. Two primary high-throughput methods are employed:
Transposon Mutagenesis and Screening (Tn-Seq): This approach involves generating a large library of random transposon insertion mutants across the bacterial genome. This library is then exposed to sub-inhibitory concentrations of an antibiotic. Mutants with insertions in genes that are part of the intrinsic resistome will show altered fitness (either enriched or depleted) compared to the control population. High-throughput sequencing of the transposon insertion sites before and after antibiotic exposure identifies these candidate genes [44].
- Procedure:
- Library Creation: Generate a saturated transposon-insertion mutant library in the target pathogen (e.g., P. aeruginosa).
- Selection Pressure: Incubate the library in the presence of the antibiotic of interest and a no-antibiotic control.
- DNA Extraction & Amplification: Harvest genomic DNA from both populations and amplify the transposon-insertion junctions via PCR.
- Sequencing & Analysis: Perform next-generation sequencing and map the reads to the reference genome. Calculate the relative abundance of each mutant. Genes for which insertions are depleted after antibiotic exposure are considered part of the core intrinsic resistome, as their inactivation increases susceptibility [44].
- Procedure:
Overexpression Libraries: This complementary method involves creating a genomic library where fragments of the bacterial chromosome are cloned into a multi-copy plasmid, leading to overexpression of the encoded genes. This library is then transformed into a susceptible host (like E. coli) and screened for clones that confer resistance upon overexpression. This technique is powerful for identifying genes that, when amplified, contribute directly to acquired resistance, such as efflux pumps or inactivating enzymes [44].
Exploring Novel Chemical Space
Over-reliance on traditional soil culturing techniques (the Waksman platform) led to the repeated rediscovery of the same compounds. Newer approaches are expanding the accessible chemical space:
- Unconventional Culturing and Bioprospecting: This involves isolating and cultivating previously "unculturable" bacteria from diverse and extreme environments (e.g., marine sediments, caves). These microbes often produce unique secondary metabolites with novel antibiotic activities [108].
- Genome Mining and Metabolic Engineering: With the proliferation of bacterial genome sequences, bioinformatics tools can identify "silent" biosynthetic gene clusters (BGCs) that are not expressed under laboratory conditions. By activating these BGCs through genetic engineering or chemical elicitors, researchers can discover new antibiotic compounds [111].
- Synthetic Biology and Deep Machine Learning: Modular chemical synthesis allows for the creation of synthetic antibiotic candidates not found in nature. Furthermore, deep learning models can now be trained to predict molecules with antibacterial activity, design novel structures that inhibit specific targets, or even predict resistance evolution by analyzing fitness landscapes [108] [9].
The following workflow diagram integrates these modern discovery approaches.
Diagram Title: Integrated Antibiotic Discovery Workflow.
The Scientist's Toolkit: Essential Reagents and Methodologies
Research into intrinsic resistance and novel antibiotic development relies on a specific toolkit of reagents, assays, and model systems. The table below details key resources essential for experimental work in this field.
Table 3: Key Research Reagent Solutions for Antibiotic Resistance R&D
| Reagent / Material | Primary Function | Application in Research |
|---|---|---|
| Transposon Mutagenesis Kits | Facilitates random insertion of transposons into bacterial chromosomes for gene disruption. | Construction of genome-wide mutant libraries for Tn-Seq analysis of the intrinsic resistome [44]. |
| Specialized Growth Media | Supports the cultivation of fastidious or previously unculturable bacteria. | Bioprospecting for novel antibiotic-producing microorganisms from diverse environments [108]. |
| Liposome-Based Permeation Assays | Synthetic models of bacterial outer membranes. | Quantitative measurement of a compound's ability to penetrate the Gram-negative permeability barrier [112]. |
| Recombinant Efflux Pump Proteins | Purified components of multidrug efflux systems (e.g., AcrB). | High-throughput screening for efflux pump inhibitors and structural studies for rational drug design [44]. |
| Genome-Mined BGC Cloning Kits | Tools for the heterologous expression of silent biosynthetic gene clusters. | Activation and production of cryptic antibiotic compounds in tractable host strains like Streptomyces [111]. |
| Microfluidic Chemostats | Devices for maintaining microbial cultures under constant conditions with high temporal control. | High-replicate evolution experiments to study and predict the paths of antimicrobial resistance [9]. |
The innovation gap between novel and derivative antibiotics represents a critical vulnerability in global public health defense. The scientific challenges, particularly the robust intrinsic resistome of Gram-negative pathogens, are significant, yet they are compounded by a more formidable obstacle: a failed economic model that discourages private investment [111] [110]. The analysis confirms that the current pipeline, while containing a reasonable number of agents, suffers from a stark lack of diversity and novelty, with only a handful of candidates representing new classes or mechanisms of action against the most critical threats.
To bridge this gap, a multi-pronged strategic roadmap is essential:
- Augmented Push and Pull Incentives: "Push" funding (e.g., from public-private partnerships like CARB-X and GARDP) must be expanded to de-risk the early-stage discovery and lead optimization phases, particularly in academia and SMEs. Concurrently, robust "pull" incentives, such as market entry rewards and subscription models (e.g., the UK and proposed PASTEUR Act in the US), are required to ensure a viable market for novel antibiotics, guaranteeing a return on investment upon successful development [111] [110].
- Integration of Advanced Discovery Platforms: The field must fully embrace and fund innovative approaches, including genetic resistance modulation (inhibiting the intrinsic resistome), phage-derived therapies, monoclonal antibodies, and AI-driven drug design. These non-traditional modalities offer the best hope for circumventing existing resistance mechanisms [109] [108].
- Global Commitment and One Health Approach: As reinforced by the 2024 UN High-level Meeting on AMR, combating this crisis requires a coordinated "One Health" effort across human, animal, and environmental sectors. Catalytic funding and strong political will are needed to implement national action plans and foster international collaboration [110].
Overcoming the innovation gap is not insurmountable, but it demands a concerted, global effort that aligns scientific ambition with sustainable economic policies. The tools and knowledge exist; what is now required is the collective will to invest in the present to secure the future of modern medicine.
Antimicrobial resistance (AMR) represents one of the most pressing global health challenges of the 21st century, projected to cause 10 million deaths annually by 2050 if current trends continue [53]. Research into the mechanisms of intrinsic antibiotic resistance is crucial for developing effective countermeasures against resistant pathogens. This technical guide provides a comprehensive framework for validating antimicrobial efficacy and resistance mechanisms through integrated experimental approaches, from fundamental in vitro susceptibility testing to complex in vivo infection models. The validation models described herein are particularly focused on addressing the sophisticated resistance mechanisms employed by gram-negative bacteria and mycobacteria, which possess extensive intrinsic resistance capabilities that dramatically limit treatment options [113] [114]. By establishing robust, standardized methodologies across the research continuum, scientists can generate translatable, reproducible data that effectively bridges basic research and clinical application.
Minimum Inhibitory Concentration (MIC) Determinations
Fundamental Principles and Methodologies
The minimum inhibitory concentration (MIC) assay serves as the gold standard for determining bacterial susceptibility to antimicrobial agents, defining the lowest concentration of an antibiotic that prevents visible bacterial growth in vitro [115]. Reliable MIC assessment significantly impacts therapeutic strategy choice, directly influencing infection therapy efficiency [116]. The clinical utility of MIC values is realized through comparison with established clinical breakpoints, which categorize bacterial strains as susceptible, resistant, or intermediate based on pharmacokinetic and pharmacodynamic parameters [115].
International standards for MIC determination are maintained by two primary organizations: the European Committee on Antimicrobial Susceptibility Testing (EUCAST) and the Clinical & Laboratory Standards Institute (CLSI) [115]. Although both are recommended by the World Health Organization, significant methodological variations exist between them, necessitating clear specification of which guidelines were followed when reporting results [115]. As of January 2024, EUCAST recommends broth microdilution for most routine testing, with agar dilution reserved for specific antibiotics like fosfomycin and mecillinam [116] [115].
Table 1: Standardized Methods for MIC Determination
| Method Type | Recommended Applications | Standardized Guidelines | Key Considerations |
|---|---|---|---|
| Broth Microdilution | Non-fastidious organisms, most antibiotics | EUCAST, CLSI | Uses Mueller-Hinton broth; 96-well format enables high-throughput testing [116] [115] |
| Agar Dilution | Fosfomycin, mecillinam, anaerobic bacteria | EUCAST, CLSI | Uses Mueller-Hinton agar; suitable for testing multiple strains simultaneously [116] |
| Gradient Method | When precise MIC values needed for individual isolates | EUCAST | Commercial strips with antibiotic gradients; flexible for small batches [115] |
| Cation-Adjusted Broth | Polymyxin antibiotics (e.g., colistin) | EUCAST | Requires adjustment of divalent cation concentrations for accurate results [115] |
Detailed Protocol: Broth Microdilution Method
The broth microdilution method represents the reference standard for MIC determinations and is comprehensively outlined in EUCAST and ISO 20776-1 guidelines [115] [117]. The following protocol details the essential steps for reliable MIC determination:
Bacterial Strain Preparation:
- Day 1: Using a sterile 1 μL loop, streak all test strains on LB agar (or appropriate rich medium supplemented with necessary antibiotics) and incubate statically overnight at 37°C [115].
- Day 2: Inoculate 5 mL of LB broth with a single colony of each test strain and incubate overnight at 37°C with agitation at 220 RPM [115].
Inoculum Standardization:
- Gently vortex the overnight cultures to ensure homogeneity [115].
- Mix 100 μL of overnight culture with 900 μL of growth media, transfer to a UV-Vis cuvette, and measure OD600 using a spectrophotometer [115].
- Calculate the volume of overnight culture required to prepare standardized inoculum using the formula:
Volume (μL) = 1000 μL ÷ (10 × OD600 measurement) / (target OD600)[115]. - Pipette the calculated volume into a sterile 1.5 mL microtube and add 0.85% w/v sterile saline solution to 1 mL total volume [115].
- Use the inoculum within 30 minutes of preparation [115].
Quality Control and CFU Enumeration:
- For broth microdilution methods, verify the inoculum by diluting 10 μL of positive growth-control wells in 10 mL of 0.85% w/v sterile saline and plating 100 μL on non-selective agar medium [115].
- Incubate plates statically for 18-24 hours at 37°C and enumerate colonies to confirm inoculum density of approximately 5 × 10^5 CFU/mL [115].
- Include quality control strains with well-characterized genotypes and resistance mechanisms in each experiment [115]. For E. coli, the ATCC 25922 strain is recommended by EUCAST as a quality control reference [115].
MIC Interpretation and Reporting:
- Incubate microdilution plates at 37°C for 16-20 hours before reading results [115].
- The MIC value is identified as the lowest antibiotic concentration that completely inhibits visible bacterial growth [115].
- Report both the MIC value and the assessment system used (e.g., "EUCAST 2024") to ensure proper interpretation [115].
Advanced In Vitro Models for Investigating Intrinsic Resistance
Genetic Approaches to Resistance Mechanism Identification
Genetic screening approaches provide powerful tools for identifying intrinsic resistance mechanisms. Genome-wide knockout libraries, such as the Keio collection of E. coli knockouts (~3,800 single-gene deletions), enable systematic identification of genes involved in antibiotic resistance [113]. Screening methodologies typically involve:
Hypersensitivity Screening:
- Grow knockout strains in media supplemented with antibiotics at IC50 values alongside non-supplemented controls [113].
- Measure optical density at 600 nm and calculate fold growth compared to wild type [113].
- Classify knockouts with growth lower than two standard deviations from the median as hypersensitive [113].
- Validate hits by analyzing growth on solid media supplemented with MIC, MIC/3, and MIC/9 antibiotic concentrations [113].
Functional Analysis of Resistance Mechanisms:
- Introduce validated gene deletions into clean genetic backgrounds (e.g., E. coli K-12 MG1655) to confirm phenotypes [113].
- Test susceptibility of knockouts against sub-MIC concentrations of multiple antibiotics to determine spectrum of hypersensitivity [113].
- For gram-negative bacteria, key intrinsic resistance pathways typically include efflux pumps (e.g., acrB), cell envelope biogenesis (e.g., rfaG, lpxM), and information transfer pathways [113].
Table 2: Key Intrinsic Resistance Mechanisms and Research Applications
| Resistance Mechanism | Genetic Determinants | Experimental Applications | Research Implications |
|---|---|---|---|
| Efflux Pumps | acrB (E. coli), tap, tetV (M. abscessus) | Hypersensitivity screening, efflux inhibition studies [113] [114] | Target for resistance-breaking adjuvants; ΔacrB shows compromised resistance evolution [113] |
| Cell Envelope Biogenesis | rfaG, lpxM (E. coli), WhiB7 regulon (M. abscessus) | Membrane permeabilization studies, LPS biosynthesis analysis [113] [114] | Increased antibiotic permeation; potential for combination therapies [113] |
| Drug Modification Enzymes | eis2 (M. abscessus), cat (M. abscessus) | Prodrug activation studies, enzyme kinetics [114] | Exploitable for targeted activation; eis2 activates FF-NH2 prodrug [114] |
| Ribosomal Protection | erm(41) (M. abscessus) | Ribosomal footprinting, translation inhibition assays [114] | Understanding target site modifications; circumvention through analog design [114] |
Exploiting Resistance Mechanisms for Therapeutic Development
Innovative approaches to combating antibiotic resistance involve leveraging bacterial resistance mechanisms against themselves. This "resistance hacking" strategy is exemplified by recent work with Mycobacterium abscessus, where the engineered florfenicol prodrug (FF-NH2) exploits the WhiB7 resistome for selective activation [114] [8]. Key findings demonstrate:
Prodrug Activation via Intrinsic Resistance:
- FF-NH2 is converted to its active form (FF-ac) by Eis2, a WhiB7-dependent N-acetyltransferase normally involved in antibiotic resistance [114].
- Activated florfenicol inhibits the ribosome, further activating WhiB7 and creating a feed-forward bioactivation loop that continuously amplifies antibiotic effect [114] [8].
- This approach results in narrow-spectrum activity specifically against M. abscessus-chelonae complex species, minimizing microbiome disruption and mitochondrial toxicity [114] [8].
Resistance Evolution Studies:
- Experimental evolution under antibiotic pressure reveals differential adaptation capabilities of hypersensitive strains [113].
- High drug selection regimes drive hypersensitive knockouts (e.g., ΔacrB) to extinction more frequently than wild type [113].
- At sub-inhibitory concentrations, hypersensitive strains can adapt through mutations in drug-specific resistance pathways rather than compensatory evolution [113].
Animal Infection Models for Validation
Model Selection Considerations
Animal models are vital for understanding infectious disease pathogenesis, host immune responses, and for evaluating therapeutic efficacy in vivo [118]. Prior to selecting an animal model, researchers must ensure sufficient in vitro and ex vivo data justify animal use and that the experimental design addresses ethical considerations through a harm-benefit analysis [118]. Key factors in model selection include:
Phylogenetic Scale and Species Characteristics:
- Use the appropriate species lowest on the phylogenetic scale in accordance with replacement principles of the 3Rs (Replacement, Reduction, Refinement) [118].
- Lower-order organisms (C. elegans, D. melanogaster, G. mellonella) offer ethical advantages, lower costs, and reduced regulatory scrutiny while maintaining utility for specific research questions [118].
- Smaller animals typically cost less to purchase and house, require less space, and generate less waste, particularly important when working with limited ABSL housing capacity [118].
Pathophysiological Relevance:
- Evaluate the model animal's physiological response to infection and similarity to human disease progression [118].
- Assess morbidity through empirical measurements (body temperature, weight changes) and clinical observations (attitude, appetite, activity level) [118].
- Identify organ or tissue tropism and analyze pathophysiology of targeted organs to provide insight into molecular mechanisms of infection [118].
Murine Model of M. abscessus Infection
Murine models of M. abscessus infection have demonstrated utility for evaluating novel therapeutic approaches, including the florfenicol prodrug strategy [114]. These models effectively recapitulate key aspects of human disease and enable assessment of treatment efficacy in vivo. Critical considerations for model implementation include:
Infection Parameters:
- Utilize immunocompromised mouse strains to model infections in susceptible populations [114] [8].
- Establish infection via relevant routes (e.g., pulmonary, intravenous) depending on research objectives [118].
- Monitor disease progression through bacterial burden quantification, histopathological analysis, and clinical scoring [118].
Therapeutic Evaluation:
- Administer test compounds at clinically relevant doses and routes (e.g., oral, intraperitoneal) [114].
- Compare treatment efficacy against standard regimens and untreated controls [114].
- Assess both microbiological (bacterial load) and pathological (tissue damage, inflammation) endpoints [118].
- Evaluate toxicity through monitoring of weight loss, clinical signs, and histological examination of tissues [114] [8].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Intrinsic Resistance Studies
| Reagent/Material | Specifications | Research Applications | Quality Control |
|---|---|---|---|
| Mueller-Hinton Medium | Broth (MHB) or Agar (MHA); with supplements for fastidious organisms | Standardized growth medium for MIC determinations [116] [115] | Performance testing with QC strains; check cation concentrations [115] |
| Antibiotic Stock Solutions | Proper solvent/diluent combinations; water, alcohol, or phosphate buffer depending on antibiotic [116] | Preparation of dilution series for MIC assays | Verify potency through routine QC; proper storage conditions [115] |
| Quality Control Strains | Species-specific reference strains (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853) [115] | Validation of MIC procedure accuracy and reagent performance | Regular monitoring of QC results using statistical methods [115] |
| Knockout Library Collections | Comprehensive sets (e.g., Keio collection: ~3,800 E. coli knockouts) [113] | Genome-wide screening for resistance determinants | Verify genotype and growth characteristics of individual strains [113] |
| Efflux Pump Inhibitors | Chemical inhibitors (e.g., chlorpromazine, piperine, verapamil) [113] | Studying efflux-mediated resistance; combination therapies | Confirm activity and specificity in relevant systems [113] |
| Specialized Animal Models | Immunocompromised strains, specific pathogen-free animals | In vivo efficacy testing for compounds active in vitro | Health monitoring; verification of immune status [118] |
The escalating crisis of antimicrobial resistance demands rigorous, standardized validation models that effectively bridge in vitro findings and in vivo efficacy. This technical guide has outlined integrated experimental approaches for characterizing intrinsic resistance mechanisms and evaluating novel therapeutic strategies, with particular emphasis on exploiting these very resistance pathways for therapeutic development. The emerging paradigm of "resistance hacking" – exemplified by the florfenicol prodrug that leverages M. abscessus's WhiB7 resistome for activation – represents a promising frontier in anti-infective development [114] [8]. As resistance mechanisms continue to evolve, so too must our validation methodologies, ensuring that preclinical data robustly predicts clinical utility and accelerates the development of effective countermeasures against multidrug-resistant pathogens.
Economic and Regulatory Hurdles in Developing Drugs for Resistant Gram-Negatives
The challenge of developing new antibiotics against Gram-negative bacteria is profoundly influenced by the sophisticated intrinsic resistance mechanisms inherent to this class of pathogens. Their complex cell envelope, comprising an outer membrane that acts as a formidable permeability barrier, synergizes with constitutive efflux pumps and innate enzymatic defenses to drastically reduce the intracellular concentration of antimicrobial agents [119] [120]. This intrinsic resilience is a key reason why Gram-negative pathogens, such as Acinetobacter baumannii, Pseudomonas aeruginosa, and Klebsiella pneumoniae, dominate the World Health Organization's (WHO) Bacterial Priority Pathogens List (BPPL) and are responsible for a significant portion of the nearly 5 million annual deaths associated with antimicrobial resistance (AMR) [121] [122]. The "antibiotic discovery void" since the 1980s, marked by a stark decline in new antibiotic classes, has occurred alongside bacteria rapidly acquiring new resistance traits, creating a critical public health crisis [122].
This whitepaper delves into the economic and regulatory landscape that continues to hinder the development of novel therapeutics, framing this challenge within the broader context of overcoming intrinsic bacterial defenses. Understanding these hurdles is paramount for researchers and drug development professionals aiming to revitalize the pipeline.
Economic Challenges and the Dwindling Pipeline
The development of new antibiotics, particularly for Gram-negative infections, is plagued by significant economic disincentives that have caused major pharmaceutical companies to exit the field.
Market Failures and Scientific Hurdles
The core economic problem is a misalignment between the high societal value of effective antibiotics and their low commercial return on investment. Antibiotics are typically used for short-duration treatments, unlike chronic medications for conditions like hypertension or diabetes, which generate sustained revenue [122]. Furthermore, to preserve efficacy, new agents are often reserved as last-line treatments, deliberately limiting their use and sales volume [122]. This creates a market failure where the high costs of development cannot be recouped.
Scientifically, the intrinsic resistance of Gram-negatives presents a formidable barrier. The outer membrane of Gram-negative bacteria acts as a physical barrier, while efflux pumps actively remove toxic compounds, including antibiotics [120] [123]. The diversity of intrinsic beta-lactamases (e.g., AmpC) further inactivates a broad range of antibiotics, making target identification and compound penetration exceptionally difficult [123]. Overcoming these interconnected mechanisms requires substantial investment in basic research with a high risk of failure.
The Clinical Pipeline and Industry Exodus
The clinical pipeline for new antibacterial agents remains insufficient. As of a 2023 WHO analysis, the pipeline included 97 antibacterial agents, with only 12 meeting at least one of the WHO's innovation criteria (e.g., new mechanism of action) [122]. This lack of novelty is a direct consequence of economic realities. Since the 1990s, 18 major pharmaceutical companies have exited antibacterial research and development (R&D), with the remaining few also scaling back their efforts [122]. This corporate exodus has led to a dangerous reliance on smaller entities and academia, which often lack the capital to shepherd a drug through late-stage clinical trials and global marketing.
The table below summarizes the key economic barriers and their impacts.
Table 1: Key Economic Hurdles in Antibiotic Development for Gram-Negative Pathogens
| Hurdle Category | Specific Challenge | Impact on Drug Development |
|---|---|---|
| Market Dynamics | Short treatment duration & stewardship-driven low usage | Low sales volume & inability to recoup R&D costs; unattractive ROI |
| Financial Models | High development cost (~$1.5B per new drug) with low price point | Major pharma exit; lack of sustained investment capital |
| Scientific Complexity | Intrinsic resistance (outer membrane, efflux pumps, enzymes) | High failure rate in early-stage discovery and development |
| Pipeline Health | Dominance of analogues vs. novel chemical classes; limited agents for critical BPPL pathogens | Inadequate therapeutic options for worst-case MDR infections |
Regulatory Landscape and Evolving Pathways
Regulatory agencies have recognized the public health emergency posed by AMR and are creating specialized pathways to encourage antibiotic development. However, navigating this landscape presents its own set of challenges.
Incentive Programs and Adaptive Pathways
In the United States, the GAIN (Generating Antibiotic Incentives Now) Act provides incentives such as a five-year extension of market exclusivity for Qualified Infectious Disease Products (QIDPs) [124]. The LPAD (Limited Population Pathway for Antibacterial and Antifungal Drugs) pathway allows for smaller, faster trials for drugs targeting limited populations of patients with unmet needs [124].
In the European Union, the PRIME (Priority Medicines) scheme offers enhanced support and accelerated assessment for medicines that target an unmet medical need [125]. The Innovation Task Force (ITF) provides a platform for early, informal dialogue with regulators, which is particularly valuable for academics and SMEs working on novel approaches [125]. For example, the approval of Emblaveo (aztreonam/avibactam) demonstrated regulatory flexibility, as the EMA accepted limited clinical data based on the drug's activity against metallo-β-lactamase (MBL)-producing Gram-negative bacteria [125].
New Regulatory Requirements
A significant new regulatory requirement is the Stewardship and Access Plan (SAP), which mandates that developers outline how they will ensure both appropriate use (stewardship) and adequate patient access post-approval [125]. These plans must include prescribing guidelines, resistance monitoring, supply guarantees, and pricing transparency. Furthermore, Environmental Risk Assessments (ERAs) have gained importance for antimicrobials, requiring an evaluation of the risk that manufacturing and patient excretion of the drug could select for environmental AMR [125].
Table 2: Key Regulatory Pathways and Tools for Antimicrobial Development
| Region | Initiative/Pathway | Key Features & Purpose |
|---|---|---|
| United States | GAIN (Generating Antibiotic Incentives Now) Act | Grants QIDP designation: 5-year market exclusivity extension & fast-track review [124]. |
| LPAD (Limited Population Pathway) | Allows for smaller, focused clinical trials for drugs targeting limited, high-unmet-need populations [124]. | |
| European Union | PRIME (Priority Medicines) | Enhanced regulatory guidance, accelerated assessment (150-day review), and iterative scientific advice [125]. |
| Innovation Task Force (ITF) | Early, informal dialogue for novel products/technologies before formal scientific advice [125]. | |
| Scientific Advice | Formal procedure to get agency feedback on development plans to meet regulatory expectations [125]. | |
| Global | Stewardship & Access Plan (SAP) | Mandatory strategic document at marketing authorization outlining prudent use and broad, fair access plans [125]. |
Experimental Approaches to Overcome Intrinsic Resistance
To combat the intrinsic resistance of Gram-negatives, researchers are employing advanced experimental models and exploring non-traditional therapeutic avenues.
Morbidostat-Driven Resistomics Workflow
Understanding and pre-empting resistance development is crucial. The morbidostat is a sophisticated continuous-culture device that dynamically adjusts antibiotic concentration to maintain a constant selective pressure, driving bacterial evolution in a controlled environment [126]. This tool is vital for a "resistomics" workflow, which aims to identify resistance mechanisms early in drug development.
The following diagram and table detail the application of the morbidostat in profiling novel compounds.
Table 3: Research Reagent Solutions for Morbidostat-Based Resistance Profiling
| Research Reagent / Material | Function in Experimental Protocol |
|---|---|
| Morbidostat Device | Computer-controlled continuous culturing bioreactor that automatically adjusts antibiotic pressure to maintain a constant bacterial growth inhibition [126]. |
| Target Bacterial Strains | Clinical isolates and reference strains (e.g., ATCC) of priority Gram-negative pathogens such as A. baumannii, K. pneumoniae, and P. aeruginosa [126]. |
| Novel Investigational Agent (e.g., TGV-49) | The compound being evaluated; its chemical structure (e.g., poly-N1-hydrazino(imino)methyl-1,6-hexanediamine) dictates its initial mechanism of action (membrane disruption) [126]. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for antimicrobial susceptibility testing, ensuring reproducible and comparable results [126]. |
| Whole Genome Sequencing (WGS) Platforms | Used to identify genetic mutations (SNPs, indels) in evolved bacterial clones that confer resistance to the investigational agent [126]. |
Emerging Non-Traditional Therapies
Beyond traditional small molecules, several innovative therapeutic classes are being advanced to circumvent intrinsic resistance mechanisms.
- Bacteriophage Therapy (PT): Lytic bacteriophages are viruses that infect and lyse specific bacteria. They can penetrate biofilms and their mechanism of action—targeting bacterial cell wall structures—bypasses traditional antibiotic resistance pathways [120]. Two development models exist: personalized Magistral preparations from large phage banks and traditional fixed-composition products. Phage therapy has been successfully used in compassionate cases for infections like those in cystic fibrosis and osteomyelitis [120].
- Anti-Virulence Agents: These compounds target bacterial pathogenicity factors (e.g., toxins, secretion systems) rather than essential growth pathways. By disarming the pathogen instead of killing it, they exert less selective pressure for resistance and can preserve the host microbiome [120].
- Antimicrobial Peptides (AMPs) and Immunotherapy: AMPs are part of the innate immune system and often target the bacterial membrane. Immunotherapies, including monoclonal antibodies, enhance the host's immune clearance of bacterial pathogens [120].
The economic and regulatory hurdles in developing drugs for resistant Gram-negative bacteria are deeply intertwined with the fundamental biology of intrinsic resistance. While regulatory pathways have evolved to support innovation, the underlying market failure remains largely unaddressed, stifling the pipeline despite urgent global need. Future success depends on a multi-pronged strategy: implementing pull incentives that delink profitability from sales volume, deepening mechanistic research on intrinsic resistance to identify new targets, and fully leveraging novel regulatory tools like PRIME and LPAD. Furthermore, a collaborative "One Health" approach that coordinates efforts across human health, animal health, and environmental sectors is essential to manage the AMR crisis holistically [122] [75]. For researchers and developers, focusing on non-traditional therapies and employing robust experimental evolution models early in development will be critical to outmaneuver bacterial resistance and secure the future of infectious disease treatment.
Antimicrobial resistance (AMR) poses a critical threat to global health, directly causing an estimated 1.27 million deaths globally in 2019 and contributing to 4.95 million deaths [34]. The World Health Organization's 2025 report, drawing from over 23 million bacteriologically confirmed cases across 110 countries, reveals that one in six bacterial infections is now resistant to standard antibiotic treatments [81] [127]. This crisis is exacerbated by intrinsic antibiotic resistance, a natural and chromosomally encoded phenotype present in all bacterial species that predates human antibiotic use [24]. This inherent resistance, mediated by mechanisms such as reduced outer membrane permeability and constitutive efflux pumps, fundamentally shapes treatment outcomes and the global burden of AMR by limiting therapeutic options from the outset [24] [18]. Understanding the link between the intrinsic bacterial resistome and treatment failure rates is therefore essential for guiding public health action, informing drug development, and optimizing therapeutic strategies to combat resistant infections.
Global Surveillance Data on Antibiotic Resistance
The WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS) provides standardized data to track the scale and trends of AMR globally. Country participation has grown substantially, from 25 countries in 2016 to 104 in 2023, yet nearly half of all countries did not report data in 2023, indicating significant surveillance gaps [81] [127]. The burden is not evenly distributed, with the highest resistance rates observed in the WHO South-East Asian and Eastern Mediterranean Regions, where one in three reported infections were resistant. In the African Region, one in five infections was resistant, while the Americas Region fared slightly better than the global average with one in seven infections resistant [127].
Resistance in Key Bacterial Pathogens
The following table summarizes the adjusted global resistance estimates for key pathogen-antibiotic combinations, which illustrate the severe clinical challenges posed by intrinsic and acquired resistance mechanisms.
Table 1: Global Antibiotic Resistance Estimates for Key Pathogens (2023)
| Pathogen | Antibiotic Class | Global Resistance Prevalence | Clinical Significance |
|---|---|---|---|
| Escherichia coli | Third-generation cephalosporins | >40% [127] | First-choice treatment for bloodstream infections and UTIs is increasingly ineffective [127]. |
| Klebsiella pneumoniae | Third-generation cephalosporins | >55% [127] | A leading cause of drug-resistant sepsis; resistance exceeds 70% in the African Region [127]. |
| Klebsiella pneumoniae | Carbapenems | Increasing, specifics not provided [127] | Narrowing treatment options, forcing reliance on last-resort antibiotics [127]. |
| Staphylococcus aureus | Methicillin (MRSA) | Median rate of 35% [34] | A major cause of healthcare and community-associated resistant infections. |
| Acinetobacter spp. | Carbapenems | Increasing, specifics not provided [127] | Notorious for multi-drug resistance, including intrinsic resistance to many drug classes [18]. |
| Pseudomonas aeruginosa | Multiple (Ampicillin, 1st/2nd Gen. Cephalosporins, etc.) | Intrinsically Resistant [18] | Native outer membrane permeability and efflux pumps confer broad resistance [24] [18]. |
| Stenotrophomonas maltophilia | Aminoglycosides, β-lactams, Carbapenems | Intrinsically Resistant [18] | Possesses innate resistance to multiple major antibiotic classes [18]. |
Trends and Drivers of Resistance
Between 2018 and 2023, antibiotic resistance rose in over 40% of the monitored antibiotics, with an average annual increase of 5-15% [127]. This trend is accelerated by the misuse and overuse of antimicrobials in humans, animals, and plants [34]. The economic costs are staggering, with the World Bank estimating that AMR could result in US $1 trillion in additional healthcare costs by 2050 and US $1 trillion to US $3.4 trillion in annual GDP losses by 2030 [34]. The rise of resistance, particularly to last-resort drugs like carbapenems, underscores the urgent need for novel therapeutic strategies that can overcome intrinsic resistance mechanisms [18] [127].
Intrinsic Resistance Mechanisms and the Resistome
The intrinsic antibiotic resistome is a universal and natural feature of bacterial species, mediated by a complex network of genes and genetic loci beyond the well-characterized barriers of the outer membrane and active efflux [24].
Core Mechanisms of Intrinsic Resistance
The primary mechanisms that contribute to intrinsic resistance are summarized in the table below.
Table 2: Core Mechanisms of Intrinsic Antibiotic Resistance
| Mechanism | Function | Example Pathogens |
|---|---|---|
| Reduced Permeability (Outer Membrane) | Acts as a physical barrier, particularly in Gram-negative bacteria due to lipopolysaccharide (LPS), limiting drug uptake [18]. | All Gram-negative bacteria (e.g., E. coli, P. aeruginosa) [18]. |
| Constitutive Efflux Pumps | Actively transport a wide range of antibiotics out of the cell, reducing intracellular concentration [24] [18]. | P. aeruginosa, S. maltophilia [18]. |
| Natural Enzymatic Inactivation | Production of innate, chromosomally-encoded enzymes that inactivate antibiotics [18]. | Beta-lactamases in many species [18]. |
| Drug Target Modification | Innate structural properties of the target site (e.g., ribosome, enzyme) that reduce antibiotic binding affinity [18]. | Enterococci (aminoglycosides) [18]. |
Gram-negative bacteria are particularly formidable due to their intrinsic resistance, which is largely attributed to their outer membrane, which acts as a barrier to many antibiotic classes. Furthermore, multidrug efflux pumps like AcrAB-TolC in E. coli can export a diverse range of compounds, conferring resistance to β-lactams, fluoroquinolones, macrolides, tetracycline, and chloramphenicol [18]. The synergy between the low-permeability membrane and these broad-specificity efflux pumps creates a highly effective defense system [24].
Linking Intrinsic Traits to Treatment Failure
Intrinsic resistance directly impacts treatment failure rates by rendering entire classes of antibiotics ineffective against specific pathogens. For example, the intrinsic resistance of all Gram-negative bacteria to glycopeptides (like vancomycin) and lipopeptides means these drugs are never a consideration for treating such infections [18]. Similarly, the intrinsic resistance of Klebsiella spp. to ampicillin and Serratia marcescens to macrolides dictates that alternative therapies must be chosen from the start [18]. This limitation of the available arsenal increases the reliance on broader-spectrum antibiotics, which in turn drives the selection for acquired resistance in these and other bacteria. When treatment guidelines are not aligned with local resistance patterns, or when first-line antibiotics fail due to unrecognized intrinsic resistance, the risk of poor patient outcomes and mortality increases significantly [127].
Methodologies for Surveillance and Analysis
Robust surveillance and standardized laboratory methodologies are the bedrock for understanding AMR and linking intrinsic traits to treatment outcomes.
WHO GLASS Surveillance Framework
The WHO GLASS system supports countries in building national surveillance systems to generate standardized, comparable AMR data [81]. The protocol involves:
- Case Ascertainment: Collecting isolates from specified infection types (bloodstream, urinary tract, gastrointestinal, and gonorrhoea) from a network of sentinel laboratories [81].
- Laboratory Analysis: Conducting bacteriogical confirmation and antimicrobial susceptibility testing (AST) for a core list of antibiotics against priority pathogens [81] [127]. The Minimum Inhibitory Concentration (MIC) is determined, which is the lowest concentration of an antibiotic that inhibits visible bacterial growth [18].
- Data Reporting and Analysis: Countries report aggregate data or isolate-level data to GLASS. The data is analyzed to generate national and regional resistance prevalence estimates for specific pathogen-antibiotic combinations, which are then published in global reports [81].
Experimental Protocols for Characterizing Intrinsic Resistance
For researchers investigating the intrinsic resistome, the following detailed methodologies are essential.
Protocol 1: Determining the Minimum Inhibitory Concentration (MIC) The broth microdilution method is the gold standard for AST.
- Materials: Cation-adjusted Mueller-Hinton broth, sterile 96-well plates, logarithmic-phase bacterial inoculum (standardized to ~5 x 10^5 CFU/mL), serial two-fold dilutions of the antibiotic.
- Procedure:
- Prepare serial dilutions of the antibiotic across the plate.
- Inoculate each well with the standardized bacterial suspension.
- Incubate the plate at 35±2°C for 16-20 hours.
- Read the MIC visually as the lowest antibiotic concentration that completely inhibits growth. Compare results to clinical breakpoints (e.g., EUCAST or CLSI standards) to categorize isolates as susceptible, intermediate, or resistant [18].
Protocol 2: Assessing the Role of Efflux Pumps
- Materials: Antibiotic substrates, efflux pump inhibitors (e.g., Phe-Arg-β-naphthylamide, PABN), Mueller-Hinton agar.
- Procedure:
- Perform standard disk diffusion or MIC testing with and without a sub-inhibitory concentration of an efflux pump inhibitor.
- A significant increase in the zone of inhibition or a ≥4-fold decrease in MIC in the presence of the inhibitor indicates active efflux contributing to resistance [18].
Protocol 3: Genetic Analysis of Resistance Determinants
- Materials: Bacterial genomic DNA, primers for PCR, sequencing reagents.
- Procedure:
- Extract genomic DNA from the target strain and a control strain.
- Use PCR to amplify genes known to be associated with intrinsic resistance (e.g., genes encoding efflux pump components, porins, or innate enzymes).
- Sequence the amplified products and perform comparative genomic analysis to identify mutations or differential expression patterns that may explain the resistance phenotype [24] [18].
Data Integration and Visualization Framework
Integrating complex data on resistance prevalence, bacterial genetics, and treatment outcomes requires a structured visualization framework. The following diagram illustrates the conceptual workflow from data collection to clinical impact.
Diagram 1: AMR Data to Clinical Impact Workflow
For analyzing the complex networks of genetic determinants and their relationships, graph visualization is a powerful technique. Tools like Cytoscape and Gephi allow researchers to map nodes (e.g., resistance genes, bacterial species) and links (e.g., genetic transfer, co-occurrence) to uncover hidden patterns and key influencers in the resistome [128] [129].
The following table lists key reagents, tools, and databases essential for research into intrinsic resistance and treatment failure.
Table 3: Essential Research Reagents and Resources for Intrinsic AMR Research
| Item Name | Function/Application | Specific Example/Notes |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth | Standardized medium for antimicrobial susceptibility testing (AST). | Essential for reproducible MIC determination per CLSI/EUCAST guidelines. |
| Efflux Pump Inhibitors | Chemical agents to probe the contribution of efflux to resistance. | Phe-Arg-β-naphthylamide (PABN) for RND-type pumps in Gram-negative bacteria [18]. |
| PCR Reagents & Primers | Amplification of intrinsic resistance genes for genetic analysis. | Used to target genes encoding efflux pump components (e.g., acrB, mexB), porins (e.g., ompF, ompC), and innate enzymes [18]. |
| Graph Visualization Software | Visualizing complex networks in resistance gene ecology and molecular pathways. | Cytoscape (open-source) or KeyLines/ReGraph (commercial SDKs) for creating interactive network diagrams [128] [129]. |
| WHO GLASS Data Dashboard | Accessing global and regional AMR surveillance data. | Provides open-access data on resistance prevalence for key pathogen-drug combinations to inform research hypotheses [81] [127]. |
| Bioinformatics Suites | Analysis of genomic and transcriptomic data to identify resistance markers. | Tools like igraph (R/Python) for network analysis; whole-genome sequencing pipelines for resistome prediction [128]. |
The integration of global surveillance data with a deep mechanistic understanding of intrinsic resistance is paramount to addressing the AMR crisis. The WHO reports provide a stark picture of the increasing burden, with intrinsic resistance mechanisms forming a foundational layer that limits therapeutic options and contributes to treatment failures. Focusing research on inhibiting elements of the intrinsic resistome, such as efflux pumps, offers a promising strategy for "re-sensitizing" bacteria to existing antibiotics [24]. Achieving this requires a concerted global effort, including strengthening laboratory capacity for surveillance, fostering innovation in drug discovery, and promoting the rational use of antibiotics through robust stewardship programs aligned with the One Health approach [34] [127].
Conclusion
Intrinsic antibiotic resistance represents a formidable and innate barrier in the fight against multidrug-resistant infections, governed by a limited set of core mechanisms including restrictive membrane permeability, constitutive efflux pumps, and chromosomal resistance genes. Understanding these foundational principles is not merely an academic exercise but a critical prerequisite for rational drug design. The methodologies to study these barriers are increasingly sophisticated, leveraging genomics, structural biology, and artificial intelligence. While the therapeutic pipeline has been historically slow, promising strategies centered on antibiotic potentiation and novel modalities offer pathways to breach these innate defenses. A concerted, cross-disciplinary effort that integrates basic mechanistic research, innovative development, and supportive economic policies is essential. Future success will depend on our ability to translate this integrated understanding of intrinsic resistance into clinically effective agents that secure our therapeutic arsenal for the future.
References
- 1. The Global Challenge of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12284435/]
- 2. Antibiotic Resistance - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK513277/]
- 3. Impeding pathways of intrinsic resistance in Escherichia coli ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003443]
- 4. Intrinsic antibiotic resistance: Mechanisms, origins ... [https://www.sciencedirect.com/science/article/abs/pii/S1438422113000246]
- 5. Understanding Antimicrobial Resistance [https://www.uspharmacist.com/article/understanding-antimicrobial-resistance]
- 6. Antimicrobial Resistance: Definition, Causes & Prevention [https://my.clevelandclinic.org/health/articles/16142-antimicrobial-resistance]
- 7. Tradeoffs associated with constitutive and induced plant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3078369/]
- 8. Approach to combat antibiotic resistance turns bacterium's ... [https://www.stjude.org/media-resources/news-releases/2025-medicine-science-news/approach-to-combat-antibiotic-resistance-turns-bacteriums-genes-against-it.html]
- 9. Quantitative systems-based prediction of antimicrobial ... [https://www.nature.com/articles/s41540-023-00304-6]
- 10. Outer Membrane Permeability and Antibiotic Resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2696358/]
- 11. Understanding antibiotic resistance via outer membrane ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5903844/]
- 12. Outer Membrane Porins Contribute to Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10385648/]
- 13. Antibiotic Resistance: A Genetic and Physiological Perspective [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579171/]
- 14. Porin (protein) [https://en.wikipedia.org/wiki/Porin_(protein)]
- 15. Metabolic control of porin permeability influences antibiotic ... [https://www.nature.com/articles/s41564-025-02175-5]
- 16. Types and Mechanisms of Efflux Pump Systems and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10974122/]
- 17. Multidrug Efflux Pumps at the Crossroad between Antibiotic ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2016.01483/full]
- 18. An overview of the antimicrobial resistance mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6604941/]
- 19. Role of bacterial efflux pumps in antibiotic resistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10268834/]
- 20. Identification of Compounds With Potential Dual Inhibitory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12179561/]
- 21. Efflux pump inhibitors from plant compounds: A new ... [https://www.sciencedirect.com/science/article/pii/S0926669025009240]
- 22. Regulation and expression of multidrug resistance (MDR) ... [https://www.nature.com/articles/6690475]
- 23. Evolutionary loss of an antibiotic efflux pump increases ... [https://www.nature.com/articles/s41467-025-63284-7]
- 24. Intrinsic antibiotic resistance: mechanisms, origins ... [https://pubmed.ncbi.nlm.nih.gov/23499305/]
- 25. Bacterial Enzymes and Antibiotic Resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6351036/]
- 26. Mechanisms of Antibiotic Resistance - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4888801/]
- 27. Mechanism of antibacterial resistance, strategies and next- ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1444781/full]
- 28. Unmasking MRSA's Armor: Molecular Mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388575/]
- 29. One-step inactivation of chromosomal genes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC18686/]
- 30. An antiplasmid system drives antibiotic resistance gene ... [https://www.nature.com/articles/s41467-024-48219-y]
- 31. The intrinsic resistome of bacterial pathogens - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3639378/]
- 32. Intrinsic Resistance Patterns | MI - Microbiology [https://microbiology.mlsascp.com/intrinsic-resistance-patterns.html]
- 33. WHO bacterial priority pathogens list, 2024 [https://www.who.int/publications/i/item/9789240093461]
- 34. Antimicrobial resistance [https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance]
- 35. Bacterial Antibiotic Resistance: The Most Critical Pathogens [https://www.mdpi.com/2076-0817/10/10/1310]
- 36. Experimental Induction of Bacterial Resistance to the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5038303/]
- 37. Drivers of intrinsic resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9149149/]
- 38. Identification of antibiotic genes from whole genome and... resistance [https://onehealthadv.biomedcentral.com/articles/10.1186/s44280-025-00079-x]
- 39. antiSMASH 2.0—a versatile platform for genome mining of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3692088/]
- 40. Editorial: Computational Predictions , Dynamic Tracking, and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9014298/]
- 41. AMRLearn: Protocol for a machine learning pipeline ... [https://www.sciencedirect.com/science/article/pii/S266616672500139X]
- 42. Machine Learning for Antimicrobial Resistance Prediction [https://pmc.ncbi.nlm.nih.gov/articles/PMC9491192/]
- 43. Minimal gene signatures enable high-accuracy prediction ... [https://www.nature.com/articles/s41540-025-00584-0]
- 44. The intrinsic resistome of bacterial pathogens [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2013.00103/full]
- 45. Quantification of Drug Molecules in Live Single Cells Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6677389/]
- 46. Advancements in techniques for analyzing cell permeability [https://www.sciencedirect.com/science/article/pii/S2405844025022236]
- 47. Assessing the Influence of Selected Permeabilization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11843891/]
- 48. The mitochondrial permeability transition: Recent progress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9787756/]
- 49. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 50. Fluorometric determination of ethidium bromide efflux kinetics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2774284/]
- 51. Function and Inhibitory Mechanisms of Multidrug Efflux ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.737288/full]
- 52. Types and Mechanisms of Efflux Pump Systems and the ... [https://www.mdpi.com/2076-0817/13/3/197]
- 53. Data-Driven Approaches in Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11590962/]
- 54. An undergraduate experimental research program, involving ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-07340-2]
- 55. Harnessing AI to Revolutionize Antibiotic Discovery [https://asm.org/articles/2025/august/ai-next-frontier-antibiotic-discovery]
- 56. Using generative AI, researchers design compounds that ... [https://news.mit.edu/2025/using-generative-ai-researchers-design-compounds-kill-drug-resistant-bacteria-0814]
- 57. Resistance mechanisms – Antibiotic resistance – ReAct [https://www.reactgroup.org/toolbox/understand/antibiotic-resistance/resistance-mechanisms-in-bacteria/]
- 58. Artificial Intelligence and Antibiotic Discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8614913/]
- 59. AI has designed thousands of potential antibiotics. Will any ... [https://www.nature.com/articles/d41586-025-03201-6]
- 60. A One-Health Perspective of Antimicrobial Resistance (AMR) [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565658/]
- 61. Antibiotic Resistance: One Health One World Outlook - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8656695/]
- 62. Diversity of Antibiotic Resistance genes and Transfer ... [https://www.nature.com/articles/s42003-022-03155-9]
- 63. High-throughput qPCR profiling of antimicrobial resistance ... [https://www.sciencedirect.com/science/article/pii/S0269749125004695]
- 64. A One Health framework for exploring zoonotic interactions ... [https://www.nature.com/articles/s41467-024-49967-7]
- 65. Current Trends in Experimental and Computational ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7677515/]
- 66. A water-focused one-health approach for early detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6501061/]
- 67. Advancing Antimicrobial Resistance Research Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7530828/]
- 68. Antibiotic potentiators as a promising strategy for ... [https://www.nature.com/articles/s44259-025-00112-4]
- 69. About Antimicrobial Resistance [https://www.cdc.gov/antimicrobial-resistance/about/index.html]
- 70. Antibiotic Potentiators Against Multidrug-Resistant Bacteria [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.887251/full]
- 71. Efflux pump [https://en.wikipedia.org/wiki/Efflux_pump]
- 72. Antibiotic adjuvants: synergistic tool to combat multi-drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10765517/]
- 73. Antimicrobial Resistance: A Growing Serious Threat for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10340576/]
- 74. Tackling the outer membrane: facilitating compound entry ... [https://www.nature.com/articles/s44259-023-00016-1]
- 75. Antimicrobial resistance: Impacts, challenges, and future ... [https://www.sciencedirect.com/science/article/pii/S2949916X24000343]
- 76. Structure–activity relationships of antibacterial peptides [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034643/]
- 77. Molecular mechanisms of membrane targeting antibiotics [https://www.sciencedirect.com/science/article/pii/S0005273615003582]
- 78. Small-molecule strategies to combat antibiotic resistance [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra04047g?page=search]
- 79. the various mechanisms of action of antimicrobial peptides ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3856679/]
- 80. Antimicrobial resistance: the example of Staphylococcus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC154455/]
- 81. Global antibiotic resistance surveillance report 2025 [https://www.who.int/publications/i/item/9789240116337]
- 82. An Overview of the Epidemiology of Multidrug Resistance and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472688/]
- 83. A Six-Step Protocol for Monitoring Antimicrobial Resistance ... [https://www.mdpi.com/2409-9279/8/5/115]
- 84. Antibiotics, Volume 14, Issue 10 (October 2025) – 97 articles [https://www.mdpi.com/2079-6382/14/10]
- 85. Nanomaterial-Based Strategies to Combat Antibiotic Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11852044/]
- 86. Phage-antibiotics synergy and nanotechnology ... [https://www.sciencedirect.com/science/article/pii/S0378517325011366]
- 87. Antimicrobial Peptides: An Emerging Hope in the Era of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189473/]
- 88. A Comprehensive Review of Nanoparticles in the Fight ... [https://www.mdpi.com/2076-0817/14/11/1090]
- 89. The role of antimicrobial peptides in overcoming antibiotic ... [https://www.sciencedirect.com/science/article/pii/S2950194625001050]
- 90. Antimicrobial peptide biological activity, delivery systems ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06321-9]
- 91. Combating Multi-Drug Resistance with Silver Nanoparticles [https://www.sciencedirect.com/science/article/pii/S2950194625003760]
- 92. Phage Therapy as a Novel Alternative to Antibiotics Through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562026/]
- 93. Phage Therapy: The Future of Fighting Antibiotic Resistance [https://norgenbiotek.com/blog/phage-therapy-future-fighting-antibiotic-resistance?srsltid=AfmBOopVTQgXP3cIAkbS0XmmxDe6i6z6mIPE0u8vbay6KlbPq1oX09IZ]
- 94. Personalized inhaled bacteriophage therapy for treatment ... [https://www.nature.com/articles/s41591-025-03678-8]
- 95. Mechanisms of antimicrobial resistance in biofilms [https://www.nature.com/articles/s44259-024-00046-3]
- 96. The Association between Biofilm Formation and Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9312340/]
- 97. Strategies for combating antibiotic resistance in bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10846525/]
- 98. Development of Antibiofilm Therapeutics Strategies to ... [https://www.mdpi.com/2076-2607/10/2/303]
- 99. Biofilm antimicrobial susceptibility through an experimental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9579162/]
- 100. Comparative analysis of biofilm detection methods and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625357/]
- 101. Intermittent antibiotic treatment of bacterial biofilms favors ... [https://www.nature.com/articles/s42003-023-04601-y]
- 102. Emerging Strategies to Combat ESKAPE Pathogens in the Era ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6452778/]
- 103. Mechanisms of Multidrug Antimicrobial Resistance in Gram ... [https://pubmed.ncbi.nlm.nih.gov/39858349/]
- 104. The Prevalence of ESKAPE Pathogens and Their Drug ... [https://www.mdpi.com/2036-7481/16/9/201]
- 105. Antibiotic resistance in hospital-acquired ESKAPE-E ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8820817/]
- 106. ESKAPE pathogens rapidly develop resistance against ... [https://www.nature.com/articles/s41564-024-01891-8]
- 107. Prevalence of ESKAPE pathogens in the environment [https://www.sciencedirect.com/science/article/pii/S143846392200089X]
- 108. The antibiotic resistance crisis and the development of new ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11226406/]
- 109. Three Innovations of Next-Generation Antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC9952447/]
- 110. Current economic and regulatory challenges in developing ... [https://www.nature.com/articles/s44259-025-00123-1]
- 111. Towards the sustainable discovery and development of ... [https://www.nature.com/articles/s41570-021-00313-1]
- 112. Important challenges to finding new leads for new antibiotics [https://www.sciencedirect.com/science/article/pii/S1369527424001383]
- 113. Impeding pathways of intrinsic resistance in Escherichia coli ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12543169/]
- 114. Prodrug florfenicol amine is activated by intrinsic resistance ... [https://www.nature.com/articles/s41564-025-02147-9]
- 115. Antibiotic susceptibility testing using minimum inhibitory ... [https://www.nature.com/articles/s44259-024-00051-6]
- 116. The Minimum Inhibitory Concentration of Antibiotics [https://pmc.ncbi.nlm.nih.gov/articles/PMC7913839/]
- 117. MIC Determination [https://www.eucast.org/bacteria/methodology-and-instructions/mic-determination/]
- 118. Considerations for Infectious Disease Research Studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5482514/]
- 119. , adaptive and acquired antimicrobial Intrinsic in... resistance [https://pubmed.ncbi.nlm.nih.gov/28258229/]
- 120. Emerging antimicrobial therapies for Gram-negative ... [https://www.nature.com/articles/s44259-025-00087-2]
- 121. WHO warns of widespread resistance to common ... [https://www.who.int/news/item/13-10-2025-who-warns-of-widespread-resistance-to-common-antibiotics-worldwide]
- 122. Current economic and regulatory challenges in developing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159177/]
- 123. of antimicrobial Mechanisms in resistance - Gram bacilli negative [https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-015-0061-0]
- 124. Antimicrobial Resistance [https://www.fda.gov/emergency-preparedness-and-response/mcm-issues/antimicrobial-resistance]
- 125. Antimicrobial Resistance: Key Regulatory Updates [https://www.dlrcgroup.com/antimicrobial-resistance-key-regulatory-updates/]
- 126. Frontiers | Susceptibility and resistance of Gram - negative to... bacteria [https://www.frontiersin.org/journals/antibiotics/articles/10.3389/frabi.2025.1615821/full]
- 127. WHO warns of widespread resistance to common ... [https://www.paho.org/en/news/13-10-2025-who-warns-widespread-resistance-common-antibiotics-worldwide]
- 128. Network Visualization - Data Visualization [https://guides.library.jhu.edu/datavisualization/network]
- 129. Graph Visualization Explained: Tools, Techniques & Use ... [https://cambridge-intelligence.com/graph-visualization-software/]