High-Resolution Subtyping with Multiplex PCR: A Comprehensive Guide for Pathogen Characterization and Drug Development
This article provides a comprehensive overview of multiplex PCR assays for high-resolution subtyping, a critical methodology for researchers and drug development professionals.
High-Resolution Subtyping with Multiplex PCR: A Comprehensive Guide for Pathogen Characterization and Drug Development
Abstract
This article provides a comprehensive overview of multiplex PCR assays for high-resolution subtyping, a critical methodology for researchers and drug development professionals. It covers the foundational principles that enable discrimination between closely related pathogen strains, details cutting-edge methodological approaches including high-resolution melting curve analysis and digital PCR multiplexing, and offers solutions for common design and optimization challenges. The content further explores rigorous validation frameworks and comparative performance against other molecular techniques, synthesizing insights from recent applications in bacteriology, virology, and respiratory pathogen detection. This resource aims to equip scientists with the knowledge to implement robust subtyping assays that enhance epidemiological surveillance, therapeutic development, and clinical diagnostics.
The Fundamentals of High-Resolution Subtyping: Principles and Diagnostic Power
Defining High-Resolution Subtyping in Pathogen Surveillance and Outbreak Investigation
High-resolution subtyping represents a critical advancement in molecular epidemiology, enabling researchers to differentiate pathogen strains beyond the species or serovar level. This granularity is fundamental for effective outbreak investigation, transmission tracking, and pathogen surveillance. In the context of a broader thesis on multiplex PCR assays, this document details how these techniques provide the resolution, speed, and throughput necessary for modern public health responses. These methods allow for the precise identification of genetic variants, facilitating the detection of outbreak clusters and informing targeted control measures. This Application Note provides a structured comparison of subtyping methods, detailed protocols for key assays, and a strategic framework for their application in outbreak settings.
Comparative Analysis of Subtyping Methods
The choice of subtyping method is dictated by the required resolution, throughput, cost, and available laboratory infrastructure. A systematic comparison of 12 typing methods for Salmonella along the poultry production chain demonstrated varying discriminatory powers [1]. The evaluation used the Discrimination Index (DI) to quantify each method's ability to distinguish between closely related isolates [1].
Table 1: Comparison of Key Pathogen Subtyping Methods
| Method | Discrimination Index (DI) | Resolution | Key Application | Throughput |
|---|---|---|---|---|
| CRISPR-MVLST | 0.9628 [1] | High | Traceability and virulence assessment [1] | Medium |
| cgMLST (Core Genome MLST) | 0.8541 [1] | High (Gold Standard) | Long-term epidemiological surveillance [1] | High (with WGS) |
| Serotyping | Not Quantified | Low | Basic serogroup identification [1] | High |
| AMR Gene Profile Typing | Not Quantified | Variable | Tracking antimicrobial resistance [1] | High |
| HRM-PCR | 100% Sensitivity & Specificity [2] | High | Differentiation of closely related strains [2] | High |
| Multiplex RT-PCR | 100% Correlation with Serotyping [3] | Medium to High | Simultaneous detection and subtyping of multiple viruses [3] | High |
The data show that CRISPR-MVLST exhibited a higher discriminatory power (DI = 0.9628) than the gold-standard cgMLST method (DI = 0.8541) for the studied Salmonella isolates, making it a powerful tool for traceability along the food chain [1]. Meanwhile, techniques like HRM-PCR and multiplex RT-PCR offer high resolution and are ideally suited for rapid response scenarios.
Experimental Protocols for High-Resolution Subtyping
Protocol: CRISPR-MVLST forSalmonellaSubtyping
This protocol is adapted from a study assessing subtyping methods for tracking Salmonella transmission [1].
1. Principle: Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) regions and Multi-Virulence Locus Sequence Typing (MVLST) are sequenced and analyzed. The combination of fast-evolving CRISPR arrays with virulence gene loci provides high discriminatory power for distinguishing closely related bacterial strains [1].
2. Reagents and Equipment:
- DNA extraction kit (e.g., QIAamp DNA Blood Mini Kit [4])
- PCR reagents: primers for CRISPR and virulence loci, DNA polymerase, dNTPs, buffer
- Thermal cycler
- Sanger or next-generation sequencing platform
- Bioinformatics software for sequence assembly and type assignment
3. Procedure:
- Step 1: DNA Extraction. Extract genomic DNA from pure bacterial cultures using a standardized kit. Quantify DNA concentration and assess purity via spectrophotometry.
- Step 2: PCR Amplification. Perform multiplex PCR to amplify the target CRISPR arrays and specific virulence genes. Use published primer sequences and cycling conditions [1].
- Step 3: Sequencing. Purify PCR amplicons and subject them to Sanger or next-generation sequencing.
- Step 4: Data Analysis. Assemble sequence reads and align them to reference databases. Assign a CRISPR-MVLST Sequence Type (CST) based on the combined profile of CRISPR spacers and virulence gene alleles [1].
4. Interpretation: Isolates with identical CSTs are considered closely related and likely part of the same transmission chain. The close correlation between CSTs and the presence of specific antimicrobial resistance (AMR) or virulence factor (VF) genes can also provide functional insights into the characterized strains [1].
Protocol: Multiplex HRM-PCR for DiarrheagenicE. coli(DEC) Subtyping
This protocol is based on a method developed for subtyping five diarrheagenic E. coli pathotypes in a single well [2].
1. Principle: Target genes specific to different DEC pathotypes are co-amplified in a single multiplex PCR reaction. Following amplification, High-Resolution Melting (HRM) curve analysis distinguishes the different amplicons based on their unique melting temperature (Tm) values and curve profiles [2].
2. Reagents and Equipment:
- HRM-capable real-time PCR instrument
- HRM master mix (including saturating DNA intercalating dye)
- Forward and reverse primers for each DEC pathotype target gene
- Template DNA (limit of detection: 0.5 to 1 ng/μL [2])
3. Procedure:
- Step 1: Reaction Setup. Prepare a single PCR reaction mix containing all primer sets and the template DNA. The study demonstrated that different DNA concentrations do not influence the subtyping results, confirming reliability [2].
- Step 2: Amplification and Melting. Run the combined multiplex PCR and HRM analysis on a real-time PCR system. The typical cycling and melting conditions are:
- PCR Amplification: 40-45 cycles of denaturation, annealing, and extension.
- HRM Analysis: Denature at 95°C, cool to a pre-defined temperature (e.g., 60°C), and then slowly increase the temperature (e.g., 0.1°C/sec to 95°C) while continuously monitoring fluorescence.
- Step 3: Analysis. Analyze the resulting melting curves. Different pathotypes are identified by their characteristic peak profiles and distinct Tm values on the derivative melt curve plot [2].
4. Interpretation: The assay demonstrated 100% sensitivity and specificity for subtyping the five DEC pathotypes [2]. Each pathotype produces a unique HRM signature, allowing for definitive identification from a single reaction.
Protocol: Dual-Target qRT-PCR for Influenza A(H5) Subtyping
This protocol describes an internally controlled, dual-target assay for specific detection of influenza A(H5) viruses, crucial for pandemic preparedness [5].
1. Principle: Two distinct regions of the influenza A(H5) hemagglutinin (HA) gene are targeted simultaneously in a multiplex qRT-PCR. This dual-target design reduces the likelihood of false negatives due to viral evolution and point mutations [5]. The assay includes primers/probes for the influenza A matrix (M) gene for pan-influenza A detection and RNase P as an internal control for sample adequacy.
2. Reagents and Equipment:
- RNA extraction kit (e.g., EZ1 virus mini kit 2.0 [5])
- One-step qRT-PCR master mix
- Primer-probe sets for H5 Target 1, H5 Target 2, influenza A M gene, and RNase P
- Real-time PCR instrument
Table 2: Research Reagent Solutions for Influenza A(H5) Subtyping
| Reagent | Function | Example | Specifications |
|---|---|---|---|
| Primer-Probe Set 1 | Detects first region of H5 HA gene | GDR4, GDR5, GDR6 [4] [5] | Designed for conserved regions of clade 2.3.4.4b |
| Primer-Probe Set 2 | Detects second region of H5 HA gene | Custom designed [5] | Reduces false negatives via dual-target design |
| Pan-Influenza A Primers-Probe | Broad influenza A detection | Targets M gene [5] | Confirms influenza A virus presence |
| Internal Control | Monitors extraction & inhibition | RNase P primers-probe [5] | Ensures sample quality and reaction validity |
| Nucleic Acid Extraction Kit | Purifies RNA from specimens | EZ1 virus mini kit 2.0 [5] | Ensures high-quality template for PCR |
3. Procedure:
- Step 1: RNA Extraction. Extract total nucleic acids from 400 μL of clinical upper respiratory specimen (e.g., swab in viral transport media). Elute in 60 μL of elution buffer [5].
- Step 2: qRT-PCR Setup. Combine eluted RNA with the master mix and the multiplexed primer-probe sets. The final reaction contains primers and probes for the two H5 targets, the influenza A M gene, and RNase P.
- Step 3: Amplification. Run the qRT-PCR with the following cycling conditions: 50°C for 10 min (reverse transcription), 95°C for 2 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min [5].
- Step 4: Analysis. A sample is considered positive for influenza A(H5) if one or both H5 targets amplify with a cycle threshold (Ct) value below the validated cutoff, and the influenza A M gene is also detected. The RNase P signal confirms adequate nucleic acid extraction and absence of significant PCR inhibitors.
4. Interpretation: The assay showed a 95% lower limit of detection (LLOD) of <0.5 to 2.5 copies/μL for different H5 clades and demonstrated 100% specificity with no cross-reactivity against non-H5 influenza A viruses [5]. Continuous sequence surveillance is recommended to ensure primer-probe sets remain matched to circulating strains.
Strategic Implementation in Outbreak Investigation
Integrating high-resolution subtyping into field epidemiology requires a structured approach. The following workflow aligns with the CDC's Field Epidemiology Manual, illustrating how these methods are embedded in the investigative process [6].
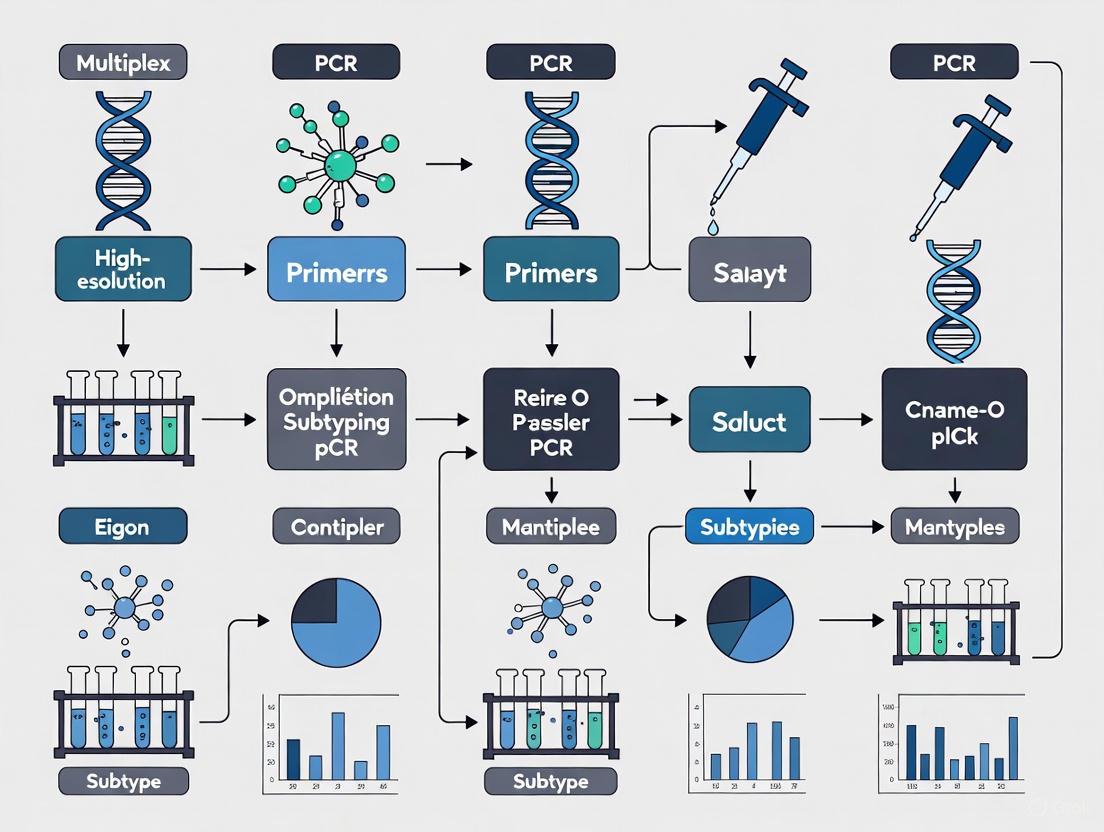
Diagram 1: Integration of high-resolution subtyping into the field investigation workflow. The process begins with standard epidemiological steps (yellow) [6], leading to analytics where subtyping (blue) is applied to define clusters and guide targeted control measures (red).
The utility of subtyping is maximized when it directly informs public health action. As shown in Diagram 1, data from methods like CRISPR-MVLST or HRM-PCR are critical for defining an outbreak cluster with precision, moving beyond temporal and spatial associations to genetic relatedness [1] [6]. This high-resolution confirmation enables the implementation of more targeted and effective control measures, potentially interrupting transmission with greater efficiency.
High-resolution subtyping methods, particularly advanced multiplex PCR assays and next-generation sequencing techniques, are indispensable tools in the modern molecular epidemiology toolkit. As demonstrated, methods like CRISPR-MVLST, HRM-PCR, and dual-target qRT-PCR provide the discriminatory power necessary for precise pathogen tracking, source attribution, and resistance profiling. Their integration into a structured field investigation framework ensures that molecular data translates directly into actionable public health interventions, ultimately strengthening global health security and pandemic preparedness.
Multiplex PCR assays represent a significant advancement in molecular diagnostics, enabling the simultaneous detection and subtyping of multiple pathogens or genetic markers in a single reaction. For high-resolution subtyping research, the core of a successful multiplex assay lies in the careful selection of target genes, including conserved regions for broad detection and strain-specific markers for precise differentiation [7]. This protocol details the application of these core components through a pan-genome analysis approach for the specific detection of Bacillus anthracis, a critical pathogen for public health and biodefense [8]. The methodologies described herein provide a framework for developing robust, specific, and informative multiplex PCR assays suitable for demanding applications in research and drug development.
Key Research Reagent Solutions
The following table catalogues essential reagents and their functions for the development and execution of multiplex PCR assays as discussed in this application note.
Table 1: Essential Research Reagents for Multiplex PCR Assay Development
| Reagent Category | Specific Example | Function in the Assay |
|---|---|---|
| Primer/Probe Sets | BA1698, BA5354, BA5361 primers [8] | Target strain-specific chromosomal markers for precise identification. |
| Detection Probes | 6-FAM, ROX-labeled TaqMan probes [9] [5] | Enable multiplexed, real-time detection of different targets via distinct fluorescent signals. |
| Enzyme Master Mix | Hot Start Taq DNA Polymerase [7] | Enhances specificity by preventing non-specific amplification during reaction setup. |
| PCR Additives | Betaine, Dimethyl Sulfoxide (DMSO) [7] | Destabilize GC-rich secondary structures, improving amplification efficiency of complex templates. |
| Nucleic Acid Controls | Synthesized ssDNA/ssRNA targets [5] | Act as quantitative standards for determining the limit of detection (LOD) and assay validation. |
Core Genetic Components for Subtyping
The discriminatory power of any multiplex PCR assay is founded on the strategic choice of genetic targets. These can be broadly classified into conserved regions and variable, strain-specific markers.
Conserved Genetic Regions
Conserved genes are typically housekeeping genes or essential functional genes that are present across all members of a species or genus. In multiplex assays, they serve as indispensable internal controls, confirming the presence of the target organism's DNA and the success of the amplification reaction itself. For instance, in an influenza A subtyping assay, the matrix (M) gene is a classic conserved target used for pan-influenza A detection, ensuring that all typeable influenza A viruses are captured before subtyping is attempted [5].
Strain-Specific Markers and Virulence Determinants
Strain-specific markers are genetic sequences unique to a particular strain, clade, or serotype. They are the key to high-resolution subtyping and are often located on pathogenicity islands, virulence plasmids, or prophage regions.
Table 2: Strain-Specific Targets for Pathogen Subtyping
| Pathogen | Assay Purpose | Strain-Specific Targets | Genetic Location |
|---|---|---|---|
| Bacillus anthracis [8] | Specific detection | BA1698, BA5354, BA5361 | Chromosome (novel and prophage regions) |
| Salmonella Typhimurium [9] | Virulence & Resistance Genotyping | spvC (virulence), sul1, blaTEM (resistance), DT104 spacer | Virulence plasmid (pSLT), SGI1, Chromosome |
| Influenza A Virus (Swine) [10] | Hemagglutinin (HA) Subtyping | H1, H3 | Viral RNA genome |
| Influenza A Virus (Swine) [10] | Neuraminidase (NA) Subtyping | N1, N2 | Viral RNA genome |
| Avian Influenza A(H5) [5] | Dual-Target Subtyping | Two distinct regions of the H5 Hemagglutinin gene | Viral RNA genome |
The selection of these markers requires comprehensive genomic analysis. In the case of B. anthracis, a pan-genome analysis of 151 genomes identified 30 chromosome-encoded genes exclusive to this species, overcoming the challenge of genetic similarity with B. cereus and B. thuringiensis [8]. For Salmonella, targets were chosen from Salmonella Pathogenicity Islands (SPIs) like SPI-2 (ssaQ), SPI-5 (sopB), and the Salmonella Genomic Island 1 (SGI1), which harbors antimicrobial resistance genes [9].
Experimental Protocol: Pan-Genome Analysis for Marker Discovery
This protocol outlines the methodology for identifying strain-specific chromosomal markers, as demonstrated for Bacillus anthracis [8].
The following diagram illustrates the primary workflow for the identification and validation of strain-specific genetic markers.
Detailed Methodology
Step 1: Genome Dataset Curation
- Obtain a diverse set of complete genome sequences from public databases like NCBI. For the referenced study, this included 50 genomes each of B. anthracis, B. cereus, and B. thuringiensis, plus one B. weihenstephanensis as an outgroup [8].
- Ensure metadata (e.g., strain, source, date) is recorded for downstream analysis.
Step 2: De Novo Genome Annotation
- Annotate all genomes uniformly using a tool such as Prokka version 1.11 [8].
- Prokka rapidly annotates prokaryotic genomes, identifying genes, RNAs, and other features, producing standard output files (GFF, GBK) for each genome.
Step 3: Pan-Genome Analysis
- Input the Prokka-generated annotation files into Roary version 3.13.0 [8].
- Roary constructs the pan-genome, classifying genes into core (present in all strains), soft core, shell, and cloud (strain-specific) genes.
- The key output is a gene presence/absence matrix (CSV file) that details which genes are found in which strains.
Step 4: Identification of Exclusive Genes
- Parse the gene presence/absence matrix using a custom script (e.g., Perl script as used in the study) [8].
- The script flags genes that are present in all B. anthracis strains but completely absent from all B. cereus and B. thuringiensis strains in the dataset.
Step 5: In silico Specificity Validation
- Perform a nucleotide BLAST (BLASTn) search for each candidate exclusive gene against the entire NCBI database, excluding B. anthracis [8].
- Confirm that the sequences have no significant homology to genes from any other organism to ensure specificity.
Step 6: Confirmatory Local BLAST Alignment
- Perform a local BLAST alignment against a larger, independent set of B. anthracis genomes (e.g., 132 chromosomally complete genomes from GenBank) [8].
- This step verifies that the identified marker genes are consistently present and well-conserved across a wide population of the target strain.
Step 7: Functional Analysis (Optional)
- Use databases like STRING v.12.0 to predict physical and functional protein-protein interactions among the proteins encoded by the newly identified genes [8].
- This can provide insights into the potential biological roles and pathways these genes are involved in.
Experimental Protocol: Multiplex PCR Assay Validation
Once candidate markers are identified, they must be incorporated into a validated multiplex PCR assay.
The subsequent workflow details the critical steps for establishing and validating the multiplex PCR assay.
Detailed Methodology
Step 1: Primer and Probe Design
- Design primers and probes to have similar melting temperatures (Tm) to ensure uniform amplification efficiency [7].
- Aim for primers 18-30 bp long with a GC content of 35-60% [7].
- For real-time PCR, select fluorophores with non-overlapping emission spectra (e.g., FAM, HEX/VIC, ROX, Cy5) [11] [9].
- Critical: Check for self-complementarity and primer-primer interactions to minimize dimer formation.
Step 2: Reaction Optimization and Setup
- Use a hot-start Taq DNA polymerase to minimize non-specific amplification and primer-dimer formation [7].
- Optimize the concentration of MgCl₂, primers, and probes. Multiplex reactions may require higher enzyme concentrations than uniplex PCR [7].
- Consider adding PCR enhancers like betaine or DMSO to assist in the amplification of templates with secondary structures or high GC content [7].
- The final reaction mix typically includes:
- 1X PCR Buffer
- Hot-start Taq DNA Polymerase
- dNTPs (e.g., 200 µM each)
- Optimized concentrations of MgCl₂, primers, and probes
- Template DNA (2-5 µL)
- Nuclease-free water to volume.
Step 3: Determine Analytical Sensitivity (Limit of Detection)
- Serially dilute quantified target nucleic acid (e.g., synthesized single-stranded DNA [5] or genomic RNA from cultured isolates [10]).
- Test a high number of replicates (e.g., 20 replicates per dilution) to statistically determine the 95% LOD.
- For the B. anthracis study, multiplex PCR was established using three identified genes (BA1698, BA5354, BA5361) [8].
Step 4: Determine Analytical Specificity
- Test the assay against a panel of genomic DNA or RNA from closely related non-target strains and other common flora.
- For the avian influenza A(H5) assay, specificity was confirmed using non-H5 influenza A viruses and clinical samples positive for other respiratory pathogens [5].
Step 5: Assay Evaluation with Clinical or Environmental Specimens
- Validate the assay's performance using a collection of well-characterized strains or clinical samples.
- The B. anthracis multiplex PCR was tested on 17 strains, including vaccine and virulent strains from diverse geographic and temporal origins [8].
Quantitative Data from Multiplex Assay Applications
Table 3: Performance Metrics of Representative Multiplex PCR Assays
| Assay Description | Targets | Analytical Sensitivity (LOD) | Specificity / Key Findings | Reference |
|---|---|---|---|---|
| B. anthracis Chromosomal Detection | BA1698, BA5354, BA5361 | Established | 30 exclusive genes identified; assay differentiated B. anthracis from B. cereus/thuringiensis. | [8] |
| Influenza A(H5) Subtyping (qRT-PCR) | H5 (dual-target), M gene, RNase P | Clade 1: 2.5 copies/µLClade 2.3.4.4b: <0.5 copies/µL | 100% specificity on non-H5 panel (n=16); no false positives in 155 clinical samples. | [5] |
| Swine IAV Subtyping (RT-qPCR) | H1, H3, N1, N2 | 5.09 × 10¹ to 5.09 × 10³ copies/µL | 100% diagnostic sensitivity on 85 IAVs; subtyped 74% of clinical samples. | [10] |
| S. Typhimurium Virulence/Resistance | 10 markers (e.g., ssaQ, sopB, sul1, blaTEM) | Established | Distinguished 34 genotypes; detected markers in 538 strains with varying prevalence. | [9] |
In the evolving landscape of molecular diagnostics and research, multiplex polymerase chain reaction (PCR) has emerged as a transformative methodology, particularly for high-resolution subtyping research. This technique enables the simultaneous amplification of multiple DNA or RNA targets in a single reaction, using multiple primer sets in one tube. For researchers and drug development professionals focused on detailed genetic characterization, multiplex PCR offers a powerful tool for uncovering complex biological signatures that singleplex methods cannot efficiently reveal.
The fundamental distinction lies in the reaction design: where singleplex PCR amplifies one target per reaction, multiplex PCR can simultaneously detect numerous targets—from a handful to dozens—within the same sample volume. This capability is particularly valuable for comprehensive profiling of pathogens, genetic variants, and expression patterns, which forms the cornerstone of advanced research in oncology, infectious diseases, and personalized medicine. As research demands more data from limited samples, multiplex PCR provides an efficient solution that conserves precious materials while accelerating discovery timelines.
Comparative Advantages of Multiplex PCR
Quantitative Performance Metrics
Multiplex PCR delivers significant advantages across key performance parameters essential for research efficiency and data quality. The table below summarizes the core benefits quantified from recent market analyses and technical studies:
Table 1: Performance advantages of multiplex PCR over singleplex approaches
| Parameter | Multiplex PCR Advantage | Impact on Research Workflows |
|---|---|---|
| Sample Consumption | Up to 80% reduction in sample volume required [12] | Enables more tests from biobanked/rare samples |
| Data Point Cost | Significant reduction in cost per data point [12] | Makes large-scale studies more economically viable |
| Throughput Time | 50% faster procedure compared to running multiple singleplex reactions [12] | Accelerates research timelines and data generation |
| Workflow Efficiency | Fewer pipetting steps and reduced hands-on time [13] | Minimizes manual errors and increases reproducibility |
| Information Yield | Multiple data points from a single sample [12] | Provides more comprehensive profiling from limited material |
Applications in High-Resolution Subtyping
The advantages of multiplex PCR translate directly into enhanced capabilities for specific research applications critical to drug development and molecular characterization:
Pathogen Subtyping and Co-infection Detection: Multiplex PCR enables simultaneous identification of multiple pathogen strains or species from a single sample, providing comprehensive profiles that singleplex methods cannot efficiently generate. During the SARS-CoV-2 pandemic, this capability was leveraged to differentiate between SARS-CoV-2, Influenza A/B, and other respiratory pathogens in a single test, demonstrating its utility for syndromic testing and surveillance [13].
Genetic Variant Profiling: In oncology research, multiplex PCR facilitates the simultaneous detection of multiple single nucleotide variants (SNVs), copy number variations, and fusion genes. For example, the USE-PCR approach enables 32 single nucleotide variants to be called simultaneously with up to 86.5% accuracy in cancer cell lines, making it invaluable for comprehensive tumor genotyping [14].
Avirulence Gene Monitoring: In plant pathogen research, tools combining multiplex PCR with high-throughput sequencing enable characterization of allelic variants for eight avirulence genes in fungal populations. This approach allows large-scale monitoring of pathogen evolution and early detection of resistance breakdowns in agricultural settings [15].
Figure 1: Workflow comparison showing efficiency gains with multiplex PCR
Experimental Design and Protocol Optimization
Critical Considerations for Multiplex Assay Development
Designing effective multiplex PCR assays requires addressing several technical challenges that are less pronounced in singleplex formats:
Primer Compatibility: All primers in the reaction must function efficiently under identical thermal cycling conditions and buffer composition without forming primer-dimers or cross-hybridizing. This requires careful in silico analysis of potential interactions before experimental validation [13].
Reagent Competition: Multiple targets compete for shared reagents (dNTPs, enzymes, magnesium ions), which can lead to imbalanced amplification. Without optimization, this may result in preferential amplification of certain targets and reduced sensitivity for others [16].
Detection System Capacity: Multiplex assays require advanced fluorescence detection systems and non-overlapping fluorophores to accurately distinguish multiple signals. The number of targets is ultimately limited by the instrument's optical channels and the availability of spectrally distinct fluorophores [13].
Protocol for Multiplex PCR in Avirulence Gene Subtyping
The MPSeqM protocol exemplifies a sophisticated application of multiplex PCR for high-resolution subtyping in plant pathology research [15]. This method enables characterization of eight avirulence genes in the fungal pathogen Leptosphaeria maculans through pooled sample analysis:
Table 2: Key research reagents for multiplex PCR subtyping
| Reagent Category | Specific Examples | Function in Multiplex PCR |
|---|---|---|
| Polymerase Master Mix | NUHI Pro NGS PCR Mix [17] | Provides optimized enzyme blend for balanced multi-target amplification |
| Primer Design Tools | ecoPrimers software [18] | Enables in silico design of compatible primer sets |
| Universal Probe Systems | USE-PCR color-coded tags [14] | Decouples detection from target amplification for standardized signal generation |
| Sample Preservation Kits | DNeasy Blood & Tissue Kit [18] | Maintains DNA integrity from limited or precious samples |
| Library Preparation | Hieff NGS DNA Selection Beads [17] | Enables efficient target enrichment for downstream sequencing |
Procedure:
DNA Extraction: Grind pathogen samples (e.g., fungal-infected leaf tissue) with homogenization beads. Extract DNA using a DNeasy Blood & Tissue Kit with modified elution (75µL initial elution, 15-minute incubation, followed by 100µL second elution, 1-minute incubation) [18].
Multiplex PCR Assembly: Prepare 25µL reactions containing:
- 50ng template DNA
- 4µL primer mix (containing 8 AvrLm gene primer pairs and Actin control)
- 12.5µL PCR master mix
- Optimized primer concentrations to balance amplification efficiency
Thermal Cycling: Execute amplification with parameters:
- Initial denaturation: 95°C for 10-15 minutes
- 30-35 cycles of:
- Denaturation: 98°C for 10-20 seconds
- Annealing: Optimized temperature (e.g., 63°C) for 45-60 seconds
- Extension: 72°C for 1-5 minutes
- Final extension: 72°C for 5-10 minutes
Pooling and Sequencing: Combine PCR products from multiple samples, then sequence using Illumina MiSeq technology. Analyze reads by mapping to an AvrLm sequence database with thresholds defined from control samples [15].
Figure 2: End-to-end workflow for multiplex PCR-based subtyping
Technical Considerations and Limitations
Performance Trade-offs in Multiplexing
While multiplex PCR offers substantial benefits, researchers must acknowledge and address its limitations through careful experimental design:
Detection Sensitivity Disparities: Comparative studies between singleplex and multiplex approaches have revealed performance variations across target types. In vector-host-parasite detection systems, singleplex clearly outperformed multiplex for the parasite component, despite similar performances for host and vector detection [18]. This suggests that lower-abundance targets may require special optimization in multiplex formats.
Primer Competition Effects: When multiple targets are amplified in a single reaction, they compete for dNTPs, enzymes, and other reaction components. If one target amplifies more efficiently, it may deplete reagents needed for other targets, potentially leading to poor amplification of less abundant sequences [16].
Initial Development Investment: Developing and validating a multiplex PCR assay involves greater time and resource investment compared to singleplex assays. However, these upfront efforts yield significant time and cost savings once the assay is optimized and routinely implemented [13].
Mitigation Strategies for Multiplex PCR Challenges
Several approaches can address the technical challenges associated with multiplex PCR:
Primer Limiting: For targets that outcompete others for reagents, significantly reducing the primer concentration causes early plateauing, preserving reagents for other targets in the reaction [16].
Universal Probe Systems: Technologies like USE-PCR employ universal hydrolysis probes with amplitude modulation and multispectral encoding, enabling higher-order multiplexing while standardizing data analysis across platforms [14].
Comprehensive Validation: Always compare multiplex results with singleplex configurations using 5-6 samples from both experimental and control groups. If results are comparable between configurations, it is safe to proceed with multiplexing; if not, further optimization is required [16].
Emerging Applications in Research and Diagnostics
Multiplex PCR continues to evolve with technological advancements, opening new possibilities for high-resolution subtyping research:
Universal Signal Encoding PCR (USE-PCR): This novel approach combines universal hydrolysis probes, amplitude modulation, and multispectral encoding to overcome traditional limitations in multiplexing. USE-PCR has demonstrated 92.6% ± 10.7% mean target identification accuracy at high template copy and 97.6% ± 4.4% at low template copy, with a dynamic range spanning four orders of magnitude [14].
High-Resolution HLA Genotyping: Optimized multiplex PCR combined with next-generation sequencing enables comprehensive HLA genotyping across six loci (HLA-A, -B, -C, -DPB1, -DQB1, -DRB1) with ≥95% accuracy at four-digit resolution. This approach offers a reliable, cost-effective method for donor-recipient matching in transplantation medicine [17].
Multiplexed Pathogen Surveillance: The combination of multiplex PCR with high-throughput sequencing enables large-scale monitoring of pathogen populations. The MPSeqM tool successfully characterized eight avirulence genes in field populations of Leptosphaeria maculans, with proportions of virulent isolates perfectly correlating with phenotypic data [15].
The integration of artificial intelligence and machine learning further enhances multiplex PCR applications, improving classification accuracy of experiments utilizing synthetic DNA templates by combining ML algorithms with real-time digital PCR systems [19]. These advancements position multiplex PCR as an increasingly powerful tool for high-resolution subtyping across diverse research domains.
Application Note: Multiplex PCR for Antimicrobial Resistance Gene Profiling
Antimicrobial resistance (AMR) poses a significant global health threat, necessitating robust surveillance methods. Multiplex PCR has emerged as a powerful tool for high-throughput screening and identification of antibiotic resistance genes (ARGs) across diverse samples, from clinical isolates to environmental microbiomes [20].
Protocol: Standard Uniplex PCR for Antibiotic Resistance Determinants
This protocol details the detection of four key antibiotic resistance determinants: sul1 (sulfonamide resistance), erm(B) (erythromycin resistance), ctx-m-32 (cefotaxime resistance, an extended-spectrum beta-lactamase), and intI1 (class 1 integron integrase, a marker associated with human-impacted samples and mobile genetic elements) [21].
- Sample Preparation: Extract genomic DNA from samples (e.g., bacterial cultures, environmental biomass) using a commercial kit. Ensure DNA purity (1.8 < OD260/280 < 2.0) and absence of degradation [20].
- Primer Design: Utilize specific primers with known sequences and melting temperatures (Tm) as listed in [21].
- PCR Master Mix Preparation: For a 20 µL reaction, combine components as specified in the table below. Prepare a master mix sufficient for all reactions, including positive and negative controls.
Table 1: PCR Master Mix Recipe for Uniplex ARG Detection
| Component | Description | Volume/RXN (µL) | Final Concentration |
|---|---|---|---|
| Primer 1 | Forward Primer (100µM) | 0.4 | 2µM |
| Primer 2 | Reverse Primer (100µM) | 0.4 | 2µM |
| TAQ | JumpStart RedTaq ReadyMix | 10 | 1X |
| PCR Water | Nuclease-free Water | 4.2 | N/A |
| Sample | Template DNA | 5.0 | - |
| Total Volume | 20.0 |
- Thermal Cycling: Perform amplification in a thermal cycler under the following conditions, optimized for each gene [21]:
- Initial Denaturation: 94°C for 2 minutes.
- Amplification (35 cycles): Denature at 94°C for 30 seconds, anneal at the primer-specific Tm (see Table 2) for 30 seconds, and extend at 72°C for 2 minutes.
- Final Extension: 72°C for 5 minutes.
- Analysis: Resolve PCR products by agarose gel electrophoresis (e.g., 3.5% gel) and visualize under UV light after staining with SYBR SAFE or ethidium bromide. Compare amplicon sizes to a DNA ladder and positive controls for confirmation.
Table 2: Primer Sequences and Amplicon Sizes for ARG Detection
| Gene | Sequence (5' to 3') | Tm (°C) | Amplicon Size (bp) |
|---|---|---|---|
| sul1 | F: GACGAGATTGTGCGGTTCTTR: GAGACCAATAGCGGAAGCC | 64 | 185 |
| erm(B) | F: GATACCGTTTACGAAATTGGR: GAATCGAGACTTGAGTGTGC | 58 | 364 |
| ctx-m-32 | F: CGTCACGCTGTTGTTAGGAAR: CGCTCATCAGCACGATAAAG | 63 | 156 |
| intI1 | F: ACATGCGTGTAAATCATCGTCGR: CTGGATTTCGATCACGGCACG | 60 | 473 |
Performance and Comparison with Alternative Methods
Multiplex and uniplex PCR are highly sensitive for targeted ARG detection. A 2023 study comparing quantitative PCR (qPCR) and metagenomics for AMR screening found that qPCR (a fluorescence-based multiplexable PCR method) offers superior sensitivity and quantitative accuracy for specific, low-abundance targets in complex samples like wastewater and animal faeces [22]. In contrast, metagenomics provides a much broader, untargeted overview of the resistome but with lower sensitivity for individual genes [22]. This makes multiplex PCR ideal for focused surveillance of priority resistance genes.
Application Note: Family-Wide Multiplex PCR for Viral Evolution and Discovery
Tracking viral evolution and identifying novel zoonotic pathogens require assays that can detect both known and unknown viruses. Family-wide multiplex PCR targets highly conserved regions within viral families (e.g., Coronaviridae, Orthomyxoviridae), enabling the detection of known members and the discovery of novel variants through subsequent sequencing [23].
Protocol: Multiplex RT-PCR and Nanopore Sequencing (FP-NSA)
This protocol, termed Family-wide PCR and Nanopore Sequencing of Amplicons (FP-NSA), is designed for surveillance of zoonotic respiratory viruses like influenza and coronaviruses [23].
- Target Selection and Primer Design: Identify conserved genomic regions (e.g., RNA-dependent RNA polymerase ORF1ab for coronaviruses, matrix M gene for influenza viruses) from a diverse set of reference sequences. Design primers to these regions to ensure broad reactivity within the target viral family [23].
- Nucleic Acid Extraction: Extract total RNA from clinical specimens (e.g., nasopharyngeal swabs) using a kit such as the RNeasy Mini Kit (Qiagen). Include a DNase treatment step to remove contaminating genomic DNA.
- Multiplex RT-PCR:
- Prepare a 20 µL reaction containing:
- 4 µL of One-Step RT-PCR Buffer 5X
- 0.8 µL One-Step RT-PCR Enzyme Mix
- Primers at optimized concentrations (e.g., 900 nM for coronavirus primers, 100 nM for influenza virus primers)
- 2 µL of RNA template
- Perform amplification with the following cycling conditions [23]:
- Reverse Transcription: 50°C for 30 minutes
- Initial Denaturation: 95°C for 15 minutes
- 40 Cycles: 94°C for 30 seconds, 52°C for 30 seconds, 72°C for 30 seconds
- Final Extension: 72°C for 10 minutes
- Prepare a 20 µL reaction containing:
- Nanopore Sequencing and Analysis: Sequence the multiplex PCR amplicons using a portable MinION device. The resulting data can be analyzed in real-time for pathogen identification and used for phylogenetic analysis to track viral evolution and identify novel strains, such as the novel γ-coronavirus discovered using this method [23].
Research Reagent Solutions for Viral Surveillance
Table 3: Essential Reagents for Viral Surveillance Workflows
| Item | Function | Example |
|---|---|---|
| One-Step RT-PCR Kit | Combined reverse transcription and PCR amplification | Qiagen One-Step RT-PCR Kit [23] |
| Family-Wide Primers | Broadly target conserved regions of viral families | Custom primers for CoV ORF1ab, IAV M gene [23] |
| Nanopore Sequencing Kit | Library preparation and barcoding for multiplex sequencing | Oxford Nanopore Rapid Barcoding Kit [23] [24] |
| Portable Sequencer | Real-time, long-read sequencing in field settings | MinION device (Oxford Nanopore) [23] [24] |
| Bioinformatics Tools | Taxonomic classification and phylogenetic analysis | Centrifuge, BLAST, autoMLST [23] [25] |
Application Note: High-Resolution Subtyping of Bacterial Clones
Strain-level typing of bacterial pathogens is critical for hospital infection control and outbreak investigation. Multiplex PCR-based methods offer a rapid, cost-effective, and high-resolution alternative to traditional techniques like Pulsed-Field Gel Electrophoresis (PFGE) for discerning bacterial clones [26] [25].
Protocol: XbaI-based Multiplex PCR forKlebsiella pneumoniaeTyping
This novel method exploits single-nucleotide polymorphism (SNP) variations in and around XbaI-restriction sites within bacterial genomes to generate strain-specific amplification profiles, integrating the discrimination power of PFGE with the simplicity of PCR [25].
- In Silico Analysis and Primer Design: Analyze whole genome sequences of target species (e.g., K. pneumoniae) to map XbaI-restriction sites (5'...T↓CTAGA...3'). Identify syntenic regions (conserved gene neighborhoods) around these sites and design primers that flank these regions. Select a set of primers that provide high discriminatory power [25].
- DNA Extraction: Extract high-quality genomic DNA from a pure bacterial culture. A protocol involving mechanical lysis (e.g., using a TissueLyser with glass beads) followed by purification with a kit like the DNeasy Blood and Tissue Kit (Qiagen) is suitable [25].
- Multiplex PCR Amplification:
- Prepare a 25 µL reaction containing [25]:
- 5 µL of 5X Taq DNA Polymerase Buffer
- 200 µM of each dNTP
- 1 mM MgCl₂
- 0.5 µM of each primer
- 2.5 U of Taq DNA Polymerase
- 2.5 µL of DNA template
- Perform amplification with the following cycling conditions [25]:
- Initial Denaturation: 95°C for 2 minutes
- 40 Cycles: 93°C for 30 seconds, 57°C for 40 seconds, 72°C for 40 seconds
- Final Extension: 72°C for 5 minutes
- Prepare a 25 µL reaction containing [25]:
- Data Analysis: Resolve PCR products on a high-percentage agarose gel (e.g., 3.5%). Create a dendrogram based on the banding pattern using software like PyElph 1.3. The resulting clusters can be compared to known sequence types (STs) for validation, demonstrating concordance with established typing methods like MLST [25].
Advanced Technique: Melting Curve Analysis for Plasmid Replicon Typing
For rapid identification of plasmids carrying AMR genes, real-time PCR with melting curve analysis can be employed. This method uses SYBR Green dye and primers specific to plasmid replicon types. Post-amplification, the amplicon is melted, generating a unique melting temperature (Tm) peak for each replicon type. This technique is fast, sensitive, and reduces contamination risk by eliminating the need for gel electrophoresis [27].
Table 4: Comparison of Bacterial Typing Methods
| Method | Principle | Discriminatory Power | Turnaround Time | Key Advantage |
|---|---|---|---|---|
| XbaI-multiplex PCR [25] | Amplification of genomic regions flanking XbaI sites | High (clusters with MLST) | 4-6 hours | Cost-effective, high resolution, simple equipment |
| rep-PCR [26] | Amplification of repetitive intergenic sequences | High | ~1 hour (automated) | High-throughput, automated (DiversiLab system) |
| Melting Curve Analysis [27] | Tm analysis of plasmid replicon amplicons | Targeted (plasmid typing) | ~2 hours | Closed-tube system, high sensitivity, no gel needed |
| PFGE [25] | Macrorestriction digestion and pulsed-field electrophoresis | Very High (Gold Standard) | 2-4 days | High discrimination, well-established |
| Whole Genome Sequencing [25] | Determination of complete DNA sequence | Highest | Days to weeks, plus bioinformatics | Ultimate resolution, identifies all genetic variation |
Advanced Methodologies and Real-World Applications in Research and Diagnostics
High-Resolution Melting (HRM) Curve Analysis for Genotype Discrimination
High-Resolution Melting (HRM) analysis is a powerful, post-polymerase chain reaction (PCR) technique that enables precise genotyping, species identification, and sequence variant detection based on the disassociation characteristics of double-stranded DNA. This method leverages the fact that DNA melting behavior is determined by its nucleotide sequence, length, and GC content, allowing even single nucleotide polymorphisms (SNPs) to be distinguished through their unique melting profiles [28]. The technique involves amplifying target DNA in the presence of a saturating DNA-binding fluorescent dye, followed by gradual heating while monitoring fluorescence loss as double-stranded DNA denatures [29]. The resulting melting curves provide distinctive fingerprints that can discriminate between different genotypes, species, or strains with high accuracy and resolution.
Within multiplex PCR assays for high-resolution subtyping research, HRM analysis offers significant advantages as a rapid, closed-tube, cost-effective approach that requires no additional probes or processing steps after amplification. This makes it particularly valuable for applications requiring high-throughput screening, such as microbial pathogen detection, species authentication, and genetic variation studies [30]. The technology has proven effective across diverse fields, from clinical diagnostics to food authenticity testing, providing researchers with a robust tool for precise genotype discrimination.
Principles of HRM Technology
Fundamental Mechanism
HRM analysis operates on the principle that the melting temperature (Tm) of a DNA fragment—the temperature at which half of the duplex DNA dissociates into single strands—is determined by its length, GC content, and nucleotide sequence. During the HRM process, amplified PCR products are subjected to a temperature gradient while fluorescence is continuously monitored using specialized instruments capable of precise temperature control and sensitive detection [31]. The intercalating dye fluoresces strongly when bound to double-stranded DNA but loses fluorescence as the DNA strands separate, generating characteristic melting curves for each genetic variant.
The discriminatory power of HRM stems from its ability to detect minute differences in melting behavior between amplicons with variant sequences. These differences manifest as shifts in melting temperature or alterations in curve shape when compared to reference samples [29]. Normalization algorithms enhance these differences by setting pre- and post-melting regions to defined values, while difference plots further amplify distinctions by subtracting a control curve from all samples, facilitating visual interpretation of variants [28].
Critical Design Considerations
Successful HRM assay design requires careful consideration of several factors. Amplicon length typically ranges from 50-300 base pairs, with shorter fragments often providing better resolution [31]. Primer design must avoid secondary structures and ensure specificity, while GC content significantly influences melting temperature and curve shape [32]. The choice of saturating DNA dye is crucial, with EvaGreen and SYTO9 being commonly used options that provide uniform binding without inhibiting PCR amplification [30].
Table 1: Key Factors Influencing HRM Assay Performance
| Factor | Impact on HRM Analysis | Optimal Range/Selection |
|---|---|---|
| Amplicon Length | Determines melting transition sharpness | 50-300 bp (shorter preferred) |
| GC Content | Affects melting temperature | Varies by application |
| Sequence Composition | Influences curve shape and Tm | Target regions with diagnostic SNPs |
| DNA Dye | Affects resolution and PCR efficiency | Saturating dyes (EvaGreen, SYTO9) |
| DNA Quality/Quantity | Impacts reproducibility | 5-8 ng/μL typical sensitivity [28] |
| Instrument Precision | Determines data quality | High-resolution real-time PCR systems |
Applications in Genotype Discrimination and Species Identification
HRM analysis has been successfully implemented across diverse research fields for genotype discrimination and species identification, demonstrating particular utility in multiplex assay formats.
Microbial Pathogen Detection
In clinical microbiology, HRM enables simultaneous detection and differentiation of multiple pathogens from complex samples. A multiplex HRM assay developed for urinary tract infections simultaneously detects five bacterial pathogens (Escherichia coli, Klebsiella pneumoniae, Staphylococcus saprophyticus, Enterococcus faecalis, and group B streptococci) directly from urine samples with sensitivity of 100% and specificity ranging from 99.3-100% for all test pathogens [31]. The assay generates five distinct melt curves with detection limits of 1.5 × 10³ CFU/ml for E. coli and K. pneumoniae and 1.5 × 10² CFU/ml for the other targets, providing results within 5 hours compared to 24-48 hours for conventional culture.
For zoonotic abortifacient agents, a novel multiplex qPCR-HRM assay simultaneously detects Brucella spp., Coxiella burnetii, Leptospira spp., and Listeria monocytogenes in cattle, sheep, and goats [29]. The assay generates four well-separated melting peaks with Tm values of 83.2°C, 80.6°C, 77.4°C, and 75.6°C, respectively, enabling identification of individual and co-infections. The method demonstrated high analytical sensitivity with detection limits between 4.26-10.20 copies per reaction across the different targets.
Food Authenticity and Species Authentication
HRM analysis has proven valuable for enforcing food labeling regulations and preventing species substitution. For mussel authentication, a panel of 10 highly informative SNPs genotyped by PCR-HRM accurately identifies M. chilensis, M. edulis, M. galloprovincialis, and M. trossulus in fresh, frozen, and canned products [28]. The method demonstrated high robustness against variations in DNA quality, annealing time and temperature, primer concentration, and reaction volume, with zero false-positive and false-negative rates and sensitivity ranging between 5-8 ng/μL.
In food safety applications, a multiplex HRM assay targeting invA, stn, and fimA genes reliably detects Salmonella with three specific, well-separated melting peaks at average Tm values of 77.21°C, 81.43°C, and 85.44°C, respectively [30]. This multi-target approach reduces false negatives from strains lacking one target gene and minimizes false positives from non-Salmonella strains possessing only one gene, achieving detection of 10³ CFU/g in most food samples after 6-hour enrichment.
Parasite Identification and Genetic Variation
HRM facilitates rapid discrimination of medically important parasites, including Plasmodium species causing malaria. An HRM assay targeting the 18S SSU rRNA region differentiates Plasmodium falciparum and Plasmodium vivax with a significant Tm difference of 2.73°C [33]. The method demonstrated high sensitivity and specificity, with complete agreement with sequencing results in tested samples, providing a cost-effective alternative for species identification in endemic regions.
Viral genotyping also benefits from HRM analysis, as demonstrated by an assay differentiating variant groups of Grapevine leafroll-associated virus 3 (GLRaV-3), a significant plant pathogen [32]. The universal primer set targeting the Hsp70h gene detected and differentiated GLRaV-3 variant groups I, II, III, and VI, though groups I and II required a subsequent real-time RT-PCR HRM with a different primer set for discrimination due to their similar melting temperatures.
Table 2: Representative HRM Applications in Genotype Discrimination
| Application Field | Targets Discriminated | Performance Metrics | Reference |
|---|---|---|---|
| Urinary Tract Infections | 5 bacterial pathogens | Sensitivity: 100%, Specificity: 99.3-100% | [31] |
| Zoonotic Abortifacients | 4 bacterial pathogens | Detection limit: 4.26-10.20 copies/reaction | [29] |
| Mussel Authentication | 4 Mytilus species | False-positive/negative rates: 0%, Sensitivity: 5-8 ng/μL | [28] |
| Salmonella Detection | 3 target genes | Detects 10³ CFU/g after 6h enrichment | [30] |
| Malaria Diagnosis | 2 Plasmodium species | Complete agreement with sequencing | [33] |
| Plant Virus Typing | 4 GLRaV-3 variant groups | Successful differentiation of groups I, II, III, VI | [32] |
Experimental Protocols
Protocol 1: Multiplex HRM for Bacterial Pathogen Detection
This protocol adapts the methodology for simultaneous detection of four zoonotic abortifacient agents (Brucella spp., Coxiella burnetii, Leptospira spp., and Listeria monocytogenes) [29].
Reagent Preparation
- Reaction Mix: 4 μL of 5x HOT FIREPol EvaGreen HRM Mix (no ROX)
- Primers: 0.5 μL of each primer (10 pmol) for all four targets
- Template DNA: 1 μL (10-20 ng/μL)
- Nuclease-free water: to 20 μL total reaction volume
PCR Amplification and HRM Conditions
- Initial Denaturation: 95°C for 15 minutes
- Amplification (45 cycles):
- Denaturation: 95°C for 15 seconds
- Annealing: 63°C for 20 seconds
- Extension: 72°C for 25 seconds
- HRM Analysis:
- Denaturation: 95°C for 15 seconds
- Renaturation: 60°C for 1 minute
- Melting: Continuous monitoring from 60°C to 95°C with 0.2°C increments
Data Analysis
- Normalize melting curves by pre- and post-melting regions
- Generate difference plots by subtracting reference curve
- Identify pathogens based on characteristic Tm values:
- Brucella spp.: ~83.2°C
- Coxiella burnetii: ~80.6°C
- Listeria monocytogenes: ~77.4°C
- Leptospira spp.: ~75.6°C
Protocol 2: SNP-Based Species Identification
This protocol follows the approach for mussel species identification using informative SNPs [28].
Assay Design and Validation
- SNP Selection: Identify highly informative SNPs using FST outlier and MAFMAX criteria
- Primer Design: Design primers flanking target SNPs (amplicons <150 bp)
- In Silico Validation: Predict Tm differences using uMelt or similar software
- Experimental Validation: Test specificity with reference samples
HRM Reaction Setup
- Reaction Mix: 10 μL 2x HRM Master Mix
- Primers: 0.5 μL each (10 μM)
- DNA Template: 2 μL (5-20 ng/μL)
- Total Volume: 20 μL with nuclease-free water
Thermal Cycling Conditions
- Activation: 95°C for 10 minutes
- Amplification (40 cycles):
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 1 minute
- HRM Step:
- Denaturation: 95°C for 15 seconds
- Renaturation: 60°C for 1 minute
- Melting: 60°C to 95°C with 0.1°C/s ramp rate
Genotype Calling
- Analyze normalized melting curves
- Use cluster analysis to group samples by genotype
- Assign species based on reference genotype profiles
- Apply threshold (typically >95% probability) for species assignment
HRM Analysis Workflow: This diagram illustrates the sequential steps in HRM analysis from sample collection to result interpretation.
Research Reagent Solutions
Table 3: Essential Reagents and Materials for HRM Analysis
| Reagent/Material | Function/Purpose | Example Products/Alternatives |
|---|---|---|
| Saturating DNA Dye | Fluorescent detection of dsDNA during melting | EvaGreen, SYTO9, LCGreen PLUS |
| HRM Master Mix | Optimized buffer system for amplification and melting | HOT FIREPol EvaGreen HRM Mix, Type-It HRM PCR Kit |
| Species-Specific Primers | Target amplification with discrimination capability | Custom-designed primers (10-20 bp, Tm ~60°C) |
| DNA Extraction Kit | High-quality DNA isolation from various samples | Qiagen DNA Mini Kit, Favorgen DNA Extraction Kit |
| Positive Controls | Reference samples for melting curve comparison | Genomic DNA from target species/variants |
| Optical Plates/Stripes | Reaction vessels compatible with HRM instruments | White/clear 96-well plates with optical seals |
| Quantitation Standard | DNA concentration measurement | NanoDrop spectrophotometer, Qubit dsDNA HS assay |
Method Validation and Quality Assurance
Robust validation is essential for implementing HRM assays in research and diagnostic settings. Key performance parameters must be established to ensure reliable genotype discrimination.
Analytical Sensitivity and Specificity
The limit of detection (LOD) should be determined using serial dilutions of target DNA. For multiplex HRM assays, LOD typically ranges from 4-10 copies/reaction for each target [29]. Specificity must be verified against closely related non-target species and potential cross-reactants. The mussel authentication assay demonstrated zero false-positive and false-negative rates through extensive validation [28].
Repeatability and Reproducibility
Intra-assay and inter-assay variability should be assessed using multiple replicates across different runs. Coefficients of variation for Tm values are typically below 2% for well-optimized assays [29]. Inter-laboratory transferability strengthens validation, as demonstrated by the "almost perfect agreement" (κ = 0.925, p < 0.001) achieved for the mussel identification assay across different laboratories [28].
Robustness Testing
Assay performance should be evaluated under varying conditions, including:
- DNA quality and concentration
- Annealing temperature and time variations
- Primer concentration fluctuations
- Different reaction volumes
- Various HRM kit lots
The mussel identification method demonstrated robustness against all these variables, maintaining accurate species identification across conditions [28].
HRM Validation Parameters: This diagram outlines the key validation components required for implementing robust HRM assays in research and diagnostic settings.
Troubleshooting and Technical Considerations
Successful implementation of HRM analysis requires addressing several technical challenges that may impact assay performance and result interpretation.
Common Issues and Solutions
- Poor Curve Separation: Optimize amplicon design to increase Tm differences; target regions with higher GC content variation; reduce amplicon length for sharper transitions.
- Low Sensitivity: Verify DNA quality and concentration; optimize primer concentrations; increase cycle number for low-abundance targets; include PCR enhancers if needed.
- Irreproducible Melting Profiles: Standardize DNA extraction methods; ensure consistent thermal cycling conditions; use fresh dye preparations; verify instrument calibration.
- Non-Specific Amplification: Redesign primers with stricter parameters; optimize annealing temperature using gradient PCR; incorporate touchdown PCR protocols; increase stringency with additives like DMSO or betaine.
Multiplex Assay Optimization
For multiplex HRM applications, careful balancing of primer concentrations is essential to ensure uniform amplification of all targets. Primer pairs should be tested individually before combining, with adjustments made to concentrations to achieve balanced amplification [31]. The annealing temperature should be optimized to work efficiently with all primer sets, potentially requiring compromise between ideal temperatures for individual assays.
Cross-Platform Compatibility
HRM results may vary between different real-time PCR instruments due to differences in thermal uniformity, optical detection systems, and data collection algorithms [29]. When transferring methods between platforms, re-optimization may be necessary, and platform-specific Tm value ranges should be established. For clinical applications, establish confidence intervals for melting points that include at least 90% of observed melting points for each variant [32].
High-Resolution Melting analysis represents a versatile, robust, and cost-effective technology for genotype discrimination and species identification in multiplex PCR assays. Its closed-tube nature, minimal reagent requirements, and rapid turnaround time make it particularly valuable for high-throughput applications across diverse research fields. The continuing refinement of HRM methodologies, coupled with advances in real-time PCR instrumentation and saturating DNA dyes, promises to further expand its applications in both basic research and diagnostic settings. As evidenced by the successful implementations across microbiology, food authentication, and parasitology, HRM analysis has established itself as an indispensable tool in the molecular researcher's toolkit for high-resolution subtyping research.
Multiplex Polymerase Chain Reaction (PCR) is a powerful molecular biology technique that enables the simultaneous amplification of multiple target DNA sequences in a single reaction tube. By incorporating multiple primer sets specific to different DNA targets, this method allows researchers to gain more information from limited starting materials, making it substantially more cost-effective and time-efficient than performing multiple uniplex PCR reactions [34] [35]. First described in 1988 for detecting deletion mutations in the dystrophin gene, multiplex PCR has evolved into an indispensable tool for applications ranging from pathogen identification and genotyping to mutation analysis and forensic studies [34] [35].
The technique is particularly valuable in high-resolution subtyping research, where distinguishing between closely related pathogens or genetic variants is essential. For instance, during the SARS-CoV-2 pandemic, real-time PCR multiplex assays were designed to increase diagnostic capabilities by combining multiple gene targets into a single reaction [34]. The success of multiplex PCR hinges on careful experimental design, particularly in primer selection and reaction optimization, to ensure uniform amplification of all targets while minimizing unwanted interactions between the numerous primer pairs sharing the same reaction environment [36].
Multiplex PCR Primer Design
Fundamental Principles and Parameters
The design of specific primer sets is the most critical factor determining the success of a multiplex PCR reaction. Effective primer design must balance several competing parameters to ensure all primers function harmoniously under a single set of reaction conditions [36]. The key considerations for multiplex primer design include:
- Primer Length: Primers are typically 18-22 bases long, providing an optimal balance between specificity and binding efficiency [34] [35].
- Melting Temperature (Tm): Primers should have similar Tm values, preferably between 55°C-60°C. For sequences with high GC content, primers with a higher Tm (75°C-80°C) may be required. A Tm variation of 3°C-5°C between primers is generally acceptable [35].
- Specificity: Primers must be highly specific to their intended targets to avoid cross-hybridization, especially given the competition when multiple target sequences are present in a single reaction [35].
- Dimer Formation: Primers should be checked for potential dimer formation with all other primers in the reaction mixture. Primer dimers consist of two primer molecules that hybridize to each other and can be amplified by DNA polymerase, competing for reagents and potentially inhibiting target DNA amplification [34].
Table 1: Key Parameters for Multiplex PCR Primer Design
| Parameter | Optimal Range | Importance |
|---|---|---|
| Primer Length | 18-22 bases | Balances specificity and binding efficiency |
| Melting Temperature (Tm) | 55-60°C (standard); 75-80°C (high GC content) | Ensures all primers function at common annealing temperature |
| GC Content | 25-75% | Prevents overly stable or unstable hybrids |
| Amplicon Size | Varying lengths (e.g., 100-500 bp) | Allows clear differentiation by electrophoresis |
| ΔG° of Binding | -10.5 to -12.5 kcal/mol | Optimizes amplification efficiency and uniformity |
Advanced Computational Design Approaches
As the level of multiplexing increases, the complexity of primer design grows exponentially. For highly multiplexed panels, manual primer design becomes impractical, necessitating sophisticated computational approaches. The number of potential primer dimer interactions grows quadratically with the number of primers, while the sequence selection choices grow exponentially [37].
The Simulated Annealing Design using Dimer Likelihood Estimation (SADDLE) algorithm represents a significant advancement in highly multiplexed primer design. This stochastic algorithm systematically minimizes primer dimer formation by evaluating a loss function that estimates the severity of primer dimer interactions across the entire primer set [37]. In practice, SADDLE has demonstrated remarkable efficacy, reducing the fraction of primer dimers from 90.7% in a naively designed 96-plex primer set (192 primers) to just 4.9% in an optimized set. The approach remains effective even when scaling to 384-plex (768 primers) reactions [37].
Specialized software tools like PrimerPlex and FastPCR incorporate these principles to facilitate multiplex primer design. These programs automatically check oligos for cross-reactivity, minimize Tm mismatches, and identify compatible primer sets from millions of possible combinations [35] [38]. FastPCR can calculate multiplex PCR primer pairs for given target sequences or different targets inside a sequence, with the speed of calculation depending on the amount of target sequence and primer pairs required [38].
Experimental Protocol and Workflow
Reaction Setup and Optimization
Establishing a robust multiplex PCR protocol requires careful optimization of several reaction components. The following protocol provides a general framework that can be adapted for specific applications:
Table 2: Typical Multiplex PCR Reaction Components
| Component | Final Concentration | Notes |
|---|---|---|
| PCR Buffer | 1X | May require optimization of salt concentrations |
| MgCl₂ | 1.5-4.0 mM | Must be balanced with dNTP concentration |
| dNTPs | 200-400 µM each | Concentration proportional to MgCl₂ |
| Primers | 0.1-1.0 µM each | Often requires individual concentration optimization |
| DNA Polymerase | 0.5-2.5 U/µL | Use enzymes validated for multiplex applications |
| Template DNA | 1-100 ng | Quality and quantity affect amplification efficiency |
| BSA or Betaine | Optional | Can improve amplification of GC-rich targets |
A standardized thermal cycling protocol for multiplex PCR includes:
- Initial Denaturation: 94-95°C for 2-5 minutes
- Amplification Cycles (30-40 cycles):
- Denaturation: 94-95°C for 30-60 seconds
- Annealing: 55-65°C for 30-90 seconds (requires optimization)
- Extension: 72°C for 60-90 seconds (adjust based on amplicon size)
- Final Extension: 72°C for 5-10 minutes
- Hold: 4-10°C indefinitely [39] [36]
The annealing temperature is particularly critical and must be optimized to ensure specific binding of all primer pairs. Gradient PCR is recommended during optimization to identify the temperature that provides the best balance of specificity and efficiency for all targets [36].
Multiplex qPCR and Advanced Detection Methods
Multiplex quantitative PCR (qPCR) extends the capabilities of conventional multiplex PCR by enabling real-time detection and quantification of multiple targets. In multiplex qPCR, two or more target genes are amplified in the same reaction using the same reagent mix, with each target detected using probes labeled with distinct fluorescent dyes [40].
The simplest and most common form is duplexing, where two genes are amplified in a single reaction. With careful optimization, it is possible to measure the expression of three or four genes simultaneously, providing substantial savings in cost, reagents, and time [40]. Successful multiplex qPCR requires:
- Selection of dyes with minimal spectral overlap (e.g., FAM, VIC, ABY, JUN)
- Matching dye intensity with target abundance (brightest dyes with low-abundance targets)
- Using master mixes specifically formulated for multiplex applications
- Potential implementation of primer limitation for highly abundant targets [40]
Fluorescence Melting Curve Analysis (FMCA) has emerged as a versatile detection method for multiplex PCR. This technique leverages the unique melting temperatures (Tm) of specific hybridization probes bound to their complementary DNA sequences to differentiate between multiple pathogens in a single reaction tube [41]. Recent advancements have demonstrated FMCA-based multiplex assays capable of simultaneously detecting six respiratory pathogens with limits of detection between 4.94 and 14.03 copies/μL and exceptional precision (intra-/inter-assay CVs ≤ 0.70% and ≤ 0.50%) [41].
Multiplex PCR Workflow: This diagram illustrates the comprehensive workflow for multiplex PCR experiments, from initial primer design through reaction optimization to final amplification and analysis.
Research Reagent Solutions
Successful implementation of multiplex PCR requires careful selection of reagents and specialized kits designed to address the unique challenges of amplifying multiple targets simultaneously. The following table outlines essential research reagent solutions for multiplex PCR applications:
Table 3: Essential Research Reagent Solutions for Multiplex PCR
| Reagent/Kits | Function | Application Examples |
|---|---|---|
| Multiplex PCR Kits (e.g., Qiagen, Agilent) | Pre-optimized master mixes with enhanced specificity | Qiagen's kit works with up to 16 primer pairs; Agilent's hybrid capture amplifies >100 fragments [34] |
| Specialized DNA Polymerases | Engineered for robust amplification in multiplex conditions | Reduced primer dimer formation; improved processivity |
| dNTP Mixes | Balanced nucleotides for efficient incorporation | Prevents biased amplification of certain targets |
| MgCl₂ Solutions | Cofactor for DNA polymerase activity | Concentration must be balanced with dNTPs [36] |
| PCR Additives (BSA, Betaine, DMSO) | Enhance amplification efficiency | Reduce secondary structure; improve GC-rich target amplification [36] |
| Multiplex qPCR Master Mixes | Optimized for real-time multiplex detection | Contains passive reference dyes; balanced for multiple probe types [40] |
| Fluorescent Probes/Dyes (FAM, VIC, ABY, JUN) | Enable multiplex detection in real-time PCR | Distinct emission spectra allow target discrimination [40] |
Commercial multiplex PCR kits provide significant advantages for researchers, as they typically include pre-optimized reaction components and validated primer sets for specific applications. These ready-to-use solutions can dramatically reduce development time and improve reproducibility. For instance, Qiagen's multiplex PCR kit is useful for typing transgenic organisms or microsatellite analysis, while Agilent has optimized a hybrid capture-based target enrichment approach that amplifies more than 100 fragments simultaneously [34].
For qPCR applications, TaqMan Multiplex Master Mix, TaqPath 1-Step Multiplex Master Mix, and TaqPath ProAmp Master Mixes are all specifically optimized for multiplexing reactions. These formulations typically include Mustang Purple dye as a passive reference dye instead of ROX to accommodate the use of JUN dye in high-level multiplexing [40].
Applications in High-Resolution Subtyping Research
Multiplex PCR has proven particularly valuable in high-resolution subtyping research, where distinguishing between closely related pathogens or genetic variants is essential for both clinical management and public health surveillance. The technique's ability to simultaneously detect multiple targets in a single reaction makes it ideal for comprehensive pathogen identification and characterization.
In respiratory virus surveillance, a multiplex reverse transcription (RT)-PCR method has been developed that can detect and subtype influenza A (H1N1 and H3N2) and B viruses as well as respiratory syncytial virus (RSV) types A and B in clinical samples. This approach enables the differentiation of five distinct amplification products of different sizes on agarose gels, providing critical information for epidemiological monitoring and vaccine development [3]. More recently, FMCA-based multiplex PCR assays have been designed to simultaneously detect six respiratory pathogens (SARS-CoV-2, influenza A and B, RSV, adenovirus, and Mycoplasma pneumoniae), demonstrating 98.81% agreement with reference methods in clinical validation studies [41].
In food safety applications, a rapid multiplex real-time PCR high-resolution melt curve assay has been developed for the simultaneous detection of Bacillus cereus, Listeria monocytogenes, and Staphylococcus aureus in food matrices. The assay successfully distinguishes these pathogens based on their distinct melting temperatures (76.23°C, 80.19°C, and 74.01°C, respectively), providing an efficient tool for food safety monitoring [42].
For bacterial subtyping, multiplex PCR assays have been developed to detect CRISPR-Cas subtypes I-F1 and I-F2 in Acinetobacter baumannii, an important ESKAPE pathogen. This method achieved a 100% detection rate for isolates containing these Cas subtypes, providing a valuable tool for monitoring CRISPR-Cas systems and developing novel strategies to manage multidrug-resistant A. baumannii [39].
Multiplex PCR Challenges and Solutions: This diagram illustrates common challenges in multiplex PCR experiments and corresponding optimization strategies to address them.
Troubleshooting and Optimization Strategies
Despite careful planning, multiplex PCR assays often require extensive optimization to achieve balanced amplification of all targets. Common challenges include spurious amplification products, uneven or no amplification of some target sequences, and difficulties in reproducing results [36].
Addressing Amplification Biases
Several factors can lead to preferential amplification of certain targets in multiplex reactions:
- Primer Concentration Optimization: The relative concentration of primers for each target often needs individual adjustment. While standard singleplex PCR typically uses primer concentrations of 900nM each, multiplex reactions may require reduction to 150nM for highly abundant targets to prevent them from dominating the reaction (primer limitation) [40].
- Magnesium Concentration: Magnesium chloride concentration needs to be proportional to the amount of dNTPs in the reaction. Increasing magnesium concentration can improve yields but may decrease specificity [36].
- Thermal Cycling Parameters: An optimal combination of annealing temperature and buffer concentration is essential. Gradient PCR is recommended to determine the optimal annealing temperature that provides specific amplification for all targets [36].
- Template Quality and Quantity: The quality of the template may be determined more effectively in multiplex than in simple PCR reactions. Degraded templates may show preferential amplification of smaller targets [35].
Validation and Quality Control
Rigorous validation is essential for any new multiplex PCR procedure. The sensitivity and specificity must be thoroughly evaluated using standardized purified nucleic acids [36]. Validation should include:
- Comparison with singleplex reactions to ensure multiplexing doesn't alter Ct values
- Assessment of precision (intra- and inter-assay variability)
- Evaluation of limits of detection for each target
- Testing against panels of non-target organisms to confirm specificity
Where available, full use should be made of external and internal quality controls, which must be rigorously applied. For clinical applications, this is particularly important to ensure reliable results that can inform patient management decisions [36].
Multiplex PCR represents a powerful approach for high-throughput genetic analysis in research and diagnostic settings. While the development of robust multiplex assays requires significant optimization, the benefits in terms of efficiency, cost-effectiveness, and comprehensive data generation make it an indispensable tool in modern molecular biology. As computational design methods continue to advance and reagent formulations improve, the scalability and applications of multiplex PCR will undoubtedly expand, further solidifying its role in high-resolution subtyping research and beyond.
The detection and identification of foodborne pathogens represent a critical challenge in ensuring food safety. Diarrheagenic Escherichia coli (DEC) constitutes a group of foodborne pathogens that pose a significant threat to both food safety and human health, with milk and dairy products serving as potential transmission vehicles [2]. Traditional methods for subtyping DEC are often time-consuming, labor-intensive, and require multiple separate reactions, presenting challenges for laboratories handling large sample volumes.
This application note details a case study utilizing an innovative method that combines multiplex polymerase chain reaction (PCR) with high-resolution melting (HRM) analysis to subtype five major DEC pathotypes in a single reaction well directly from milk samples [2] [43]. This methodology aligns with the broader thesis that advanced multiplex PCR assays provide powerful tools for high-resolution subtyping in microbiological research, offering streamlined procedures, reduced detection time, and enhanced reliability for food safety testing.
Key Findings and Performance Data
The developed single-well HRM assay demonstrated exceptional performance characteristics, making it suitable for implementation in food safety testing laboratories. The key analytical performance data are summarized in the table below.
Table 1: Performance Characteristics of the Single-Well HRM Assay for DEC Subtyping
| Performance Parameter | Result | Experimental Details |
|---|---|---|
| Sensitivity | 100% | Correctly identified all positive samples of the five DEC pathotypes [2] |
| Specificity | 100% | Correctly excluded all non-target organisms; no cross-reactivity observed [2] |
| Detection Limit | 0.5 to 1 ng/μL | Determined using serial dilutions of target DNA [2] [44] |
| Reproducibility | High reliability and stability | Results were unaffected by variations in DNA concentration [43] [44] |
| Sample Matrix | Milk | Successfully detected and subtyped DEC directly in spiked milk samples [2] |
The assay leverages the principle that DNA amplicons with distinct sequences (in this case, from different DEC pathotypes) exhibit characteristic melting temperatures ((Tm)) and curve profiles when subjected to a controlled temperature gradient [2]. This enables the discrimination of different DEC types based on characteristic peaks and distinct (Tm) values in the differential melting curve plot [43].
Experimental Protocol
The following diagram illustrates the comprehensive workflow for subtyping DEC in milk using the single-well HRM assay.
Detailed Methodology
3.2.1 DNA Extraction
- Procedure: Extract genomic DNA from milk samples using a commercial bacterial DNA extraction kit. For artificially contaminated milk, incubate the sample in an enrichment broth prior to extraction to increase bacterial load [2].
- Quality Control: Determine DNA concentration and purity using a spectrophotometer. Adjust the DNA concentration to a working range suitable for PCR amplification.
3.2.2 Multiplex PCR Amplification
- Reaction Setup: Prepare a single PCR reaction mixture containing:
- Template DNA: 0.5 to 1 ng/μL in final volume [44].
- Primer Mix: A multiplexed set of primers specific for the target virulence genes of the five DEC pathotypes.
- PCR Master Mix: Contains DNA polymerase, dNTPs, and optimized buffer components with MgCl₂.
- Saturating DNA Dye: A dsDNA-binding dye, such as EvaGreen or SYTO9, which is essential for HRM analysis [2].
- Amplification Protocol: Perform PCR in a real-time thermal cycler capable of HRM analysis. A typical cycling program includes:
- Initial denaturation: 95°C for 10 minutes.
- 40 cycles of:
- Denaturation: 95°C for 15 seconds.
- Annealing: 60°C for 30 seconds.
- Extension: 72°C for 30 seconds.
3.2.3 High-Resolution Melting Analysis
- Melting Data Collection: Immediately after amplification, heat the amplicons from 65°C to 95°C with incremental temperature increases as small as 0.1°C to 0.2°C per step, while continuously monitoring fluorescence [2].
- Data Processing: Convert the raw fluorescence data into melting curves (fluorescence vs. temperature) and subsequently into differential melting curves (-dF/dT vs. temperature) to accentuate differences between samples.
3.2.4 Data Interpretation and Subtyping
- Identification: Identify DEC pathotypes by comparing the (T_m) values and curve shapes of unknown samples to those of known reference strains. Each DEC pathotype produces a distinct melting peak due to differences in the GC content, length, and sequence of its amplified product [2].
- Analysis Software: Utilize the software provided with the real-time PCR instrument to automatically cluster samples based on their melting profiles.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs the key reagents and materials required to implement this single-well HRM assay.
Table 2: Essential Research Reagents for HRM-Based DEC Subtyping
| Reagent/Material | Function | Specific Example/Note |
|---|---|---|
| Pathotype-Specific Primers | Amplifies unique virulence gene sequences from five DEC pathotypes in a single reaction. | Targets must be selected to generate amplicons with distinct melting temperatures ((T_m)). |
| DNA Polymerase | Catalyzes the amplification of target DNA sequences during PCR. | Use a high-fidelity enzyme with appropriate buffer. |
| Saturating DNA Dye | Binds double-stranded DNA and fluoresces, enabling melting curve analysis. | EvaGreen, SYTO9 [2]. Do not use SYBR Green I as it is not suitable for HRM. |
| DNA Extraction Kit | Isolates high-quality genomic DNA from complex food matrices like milk. | Includes lysis buffers, proteases, and purification columns. |
| Optical Plates/Tubes | Holds reactions for real-time PCR and HRM analysis. | Must be compatible with the real-time thermal cycler and prevent evaporation. |
| Reference DNA Controls | Provides known melting profiles for each DEC pathotype for assay calibration and validation. | Genomic DNA from certified reference strains. |
| Real-Time PCR Instrument with HRM Capability | Performs thermal cycling and precise temperature ramping for fluorescence data collection during melting. | Requires ability to measure fluorescence with high precision at small temperature increments. |
Principles of HRM Analysis for Subtyping
The fundamental principle of this subtyping method is that the melting behavior of a DNA amplicon is a unique function of its nucleotide sequence. The following diagram outlines the logical process of discrimination.
The sequence-specific melting is detected by monitoring the release of a saturating DNA-binding dye from the double-stranded DNA as it denatures (melts) with increasing temperature. Differences of even a single base pair can be sufficient to cause a measurable shift in the (T_m), allowing for precise discrimination between subtypes [2] [45].
This application note demonstrates that the single-well HRM assay for DEC subtyping is a robust, reliable, and efficient method for detecting and differentiating five major DEC pathotypes directly in milk. The assay achieves 100% sensitivity and specificity, with a detection limit of 0.5-1 ng/μL, and its performance is not influenced by variations in DNA concentration [2] [43].
This methodology exemplifies the power of integrating multiplex PCR with HRM analysis within the broader context of high-resolution subtyping research. It significantly streamlines operational procedures, shortens total detection time, and provides a novel, powerful tool for food safety surveillance, quality control laboratories, and public health agencies tasked with ensuring the safety of dairy products.
Escherichia coli sequence type 131 (ST131) is a globally dominant multidrug-resistant clone responsible for a significant proportion of extraintestinal infections, including urinary tract infections and bloodstream infections [46] [47]. Its clear clinical and epidemiological importance, combined with a complex clonal substructure composed of multiple distinctive subclones, has driven the need for sophisticated molecular typing assays [48] [49]. This case study details the application and protocol for a novel 36-plex PCR assay that provides high-resolution subclonal assignment of ST131 isolates, surpassing the discriminatory power of existing methods [48].
The assay's design is motivated by the understanding that ST131 subclones differ in their O and H antigens (rfb and fliC alleles), type-1 fimbriae adhesin (fimH allele), antimicrobial resistance profiles, and clinical associations [48]. This method enables any laboratory equipped for conventional endpoint PCR to perform detailed molecular characterization, which was previously achievable only through resource-intensive whole genome sequencing (WGS) [48] [49].
Background
The E. coli ST131 Clonal Group
ST131 belongs to phylogenetic group B2 and is predominantly associated with extraintestinal pathogenic E. coli (ExPEC) [46]. It emerged dramatically around the year 2000 and now accounts for the greatest share of multidrug-resistant human ExPEC infections globally [48] [46]. A key to its success lies in its complex clonal architecture, which includes major clades A, B, and C, the latter being the most extensively expanded and associated with fluoroquinolone resistance and the fimH30 allele [48] [47].
Clade C (H30) is further subdivided into a fluoroquinolone-susceptible component (C0 or H30S) and fluoroquinolone-resistant components (C1/H30R1 and C2/H30Rx), with C2 frequently carrying the blaCTX-M-15 extended-spectrum beta-lactamase gene [48]. Clade A (H41 subclone) is associated with trimethoprim-sulfamethoxazole resistance and younger patients, while clade B (H22 subclone) is often less resistant and linked to food animals [48].
The Need for Enhanced Subclonal Resolution
Existing PCR assays for ST131 offered limited characterization of this substructure [48]. High-resolution subtyping is crucial for * molecular epidemiological studies*, surveillance, and understanding the specific traits and transmission patterns of dominant subclones [49]. The 36-plex assay was developed to fill this technological gap, providing a rapid and portable method for extensive ST131 characterization without the immediate need for WGS [48].
The 36-Plex PCR Assay: Design and Workflow
Assay Design and Target Selection
The assay combines 22 novel and 14 published primers into a multiplex PCR targeting 20 distinct genetic markers [48] [49]. These markers were strategically selected to provide comprehensive subclonal resolution and are categorized as follows:
- ST131 Identification:
mdh36,gyrB47,trpA72 - Clade/Subclone Markers:
sbmA,plsB,nupC,rmuC,kefC,ybbW - Surface Antigen Genes: O16 and O25b
rfbvariants; H4 and H5fliCalleles - Adhesin Alleles: Five
fimHalleles (fimH22,fimH27,fimH30,fimH35,fimH41) - Resistance & Accessory Markers: A fluoroquinolone resistance-associated
parCallele (E84V) and a subclone-specific prophage marker [48]
This combination of targets resolves ST131 into 15 distinct molecular subsets: 3 within clade A (H41), 5 within clade B (H22), and 7 within clade C (H30), the latter encompassing subclones C0 (H30S), C1, C1-M27 (H30R1), and C2 (H30Rx) [48].
Experimental Workflow
The complete experimental process, from sample preparation to data interpretation, is outlined below.
Research Reagent Solutions
The following table details the key reagents and materials required to implement the 36-plex PCR assay.
Table 1: Essential Research Reagents for the 36-Plex PCR Assay
| Reagent/Material | Function/Description | Key Characteristics |
|---|---|---|
| Primer Pools 1-3 | Core detection mix for amplification of 20 genetic targets | Contains 36 primers (22 novel, 14 published); specific combination per pool [48] |
| DNA Polymerase | Enzymatic amplification of target sequences | Must be suitable for multiplex endpoint PCR |
| Thermal Cycler | Precise temperature cycling for PCR | Validated on Eppendorf Mastercycler x50, Bio-Rad MyCycler, and Bio-Rad T1000 [48] |
| Agarose Gel Electrophoresis System | Separation and visualization of amplicons | Standard equipment for endpoint PCR analysis |
| ST131Typer (Software) | In silico subclonal assignment from WGS data | Command-line executable; provides 87.8% accuracy vs. PCR [48] [49] |
Detailed Experimental Protocol
DNA Extraction and Primer Preparation
- DNA Extraction: Extract genomic DNA from pure cultured E. coli isolates using a standard commercial bacterial DNA extraction kit, following the manufacturer's instructions. Elute the DNA in nuclease-free water or the provided elution buffer. Quantify the DNA and adjust the concentration to a uniform working solution (e.g., 10-20 ng/μL).
- Primer Reconstitution: Resuspend lyophilized primers in sterile TE buffer or nuclease-free water to create concentrated stock solutions (e.g., 100 μM). Prepare the three working primer pools by combining the appropriate volumes of each primer from the stock solutions to achieve the predetermined optimal concentration for the multiplex reaction [48].
Multiplex PCR Amplification
- Reaction Setup: Prepare the PCR master mix on ice. A sample reaction formulation for a 25 μL total volume is shown below. Optimize volumes and concentrations based on specific polymerase requirements.
Table 2: Multiplex PCR Reaction Setup
| Component | Final Concentration/Amount |
|---|---|
| PCR-Grade Water | To 25 μL |
| 2X Multiplex PCR Master Mix | 12.5 μL |
| Primer Pool (1, 2, or 3) | Optimized concentration (e.g., 0.1–0.5 μM each primer) |
| DNA Template | 2–5 μL (e.g., 50-100 ng total DNA) |
- Thermal Cycling: Perform amplification in a thermal cycler. The following protocol is a generalized starting point and must be optimized, particularly the annealing temperature, which was found to vary by instrument [48].
- Initial Denaturation: 95°C for 5 minutes.
- Amplification (35 cycles):
- Denature: 95°C for 30 seconds.
- Anneal: 60–61°C for 45 seconds. Note: A 1°C higher temperature was required for the Bio-Rad T1000 cycler to avoid nonspecific amplification [48].
- Extend: 72°C for 60 seconds.
- Final Extension: 72°C for 7 minutes.
- Hold: 4°C.
Amplicon Analysis and Data Interpretation
- Gel Electrophoresis: Separate the PCR products by loading 5–10 μL of each reaction mixture into the wells of a 2–3% agarose gel containing a safe DNA intercalating dye. Include an appropriate DNA ladder. Run the gel at a constant voltage until sufficient separation is achieved.
- Visualization and Profiling: Visualize the gel under UV light. Document the banding pattern for each isolate.
- Subclonal Assignment: Compare the observed amplicon sizes and presence/absence profile against the reference data to assign the isolate to one of the 15 molecular subsets of ST131 [48]. The key for interpretation, as detailed in the original publication, links specific banding patterns to subclones.
Table 3: Example Subclonal Assignment Based on PCR Profile
| ST131 Clade | Subclone | Key PCR Profile Characteristics |
|---|---|---|
| A | H41 | fimH41+, O16+, H5+ [48] |
| B | H22 | fimH22+, O25b+, H4+ [48] [46] |
| C (H30) | C0 / H30S | fimH30+, parC E84V- (fluoroquinolone-susceptible) [48] |
| C (H30) | C1 / H30R1 | fimH30+, parC E84V+, lacks C2-specific prophage [48] |
| C (H30) | C2 / H30Rx | fimH30+, parC E84V+, possesses C2-specific prophage [48] |
Validation and Performance
The 36-plex PCR assay was validated across three independent laboratories, demonstrating high accuracy and reproducibility [48].
- Specificity: The assay correctly identified all 146 non-ST131 control isolates as negative, yielding a specificity of 100% (95% CI, 97.5–100%) for ST131 [48].
- Concordance with WGS: When applied to a collection of 105 ST131 strains with a known WGS phylogeny, the assay classified all 100% correctly by subclone (95% CI, 96.6% – 100%) [48].
- Detection of Resistance Markers: The assay demonstrated 100% accuracy (95% CI, 96.6–100%) in detecting the
parCE84V mutation associated with fluoroquinolone resistance when compared to WGS data [48].
For laboratories with WGS capability, the in silico tool ST131Typer was developed as a direct analog of the multiplex PCR assay. It achieved an accuracy of 87.8%, with most discrepancies attributed to incomplete or fragmented genome assemblies rather than errors in the tool itself [48] [49].
Technical Considerations and Troubleshooting
- Thermal Cycler Calibration: The annealing temperature is critical. Performance was consistent across different thermal cyclers, but required a 1°C increase on the Bio-Rad T1000 model. It is advisable to perform initial optimization when using a new instrument [48].
- Primer Pool Balancing: The assay's success relies on careful balancing of primer concentrations in each pool to ensure uniform amplification of all targets. The published primer sequences and concentrations should be followed precisely [48].
- Amplicon Resolution: Use high-quality agarose gels at an appropriate concentration (≥2%) to ensure clear resolution of similarly sized amplicons for accurate scoring.
- Template Quality: While the assay is robust, using high-quality, non-degraded DNA will minimize the risk of amplification failure.
The 36-plex PCR assay represents a significant advancement in the molecular typing of E. coli ST131. It provides a high-resolution, accessible, and cost-effective method for detailed subclonal characterization, enabling any laboratory with standard PCR capabilities to perform sophisticated analyses that were previously in the domain of specialized sequencing centers. This assay is a powerful tool for enhancing global surveillance, understanding the epidemiology and evolution of this successful multidrug-resistant clone, and potentially informing clinical management strategies [48] [49].
Digital PCR (dPCR) represents the third generation of PCR technology, enabling the absolute quantification of nucleic acids with a sensitivity that allows for the detection of single molecules. This is achieved by partitioning a PCR reaction into thousands to millions of individual compartments, so that each contains either zero, one, or a few target molecules. After end-point amplification, the fraction of positive partitions is counted, and the absolute concentration of the target is calculated using Poisson statistics, without the need for a standard curve [50]. Multiplexed digital PCR (mdPCR) builds upon this foundation by allowing for the simultaneous detection and quantification of multiple nucleic acid targets in a single reaction. This capability is crucial for complex diagnostic and research scenarios, such as detecting multiple resistance mutations in oncology or subtyping various pathogens, where the genetic material is limited, and comprehensive information is required rapidly [51] [2]. The evolution of dPCR from a research tool to a clinical asset is driven by its superior sensitivity, accuracy, and the growing need for multiplexed solutions in precision medicine.
Key Applications and Quantitative Performance
Multiplexed dPCR is pushing the boundaries in fields that demand high sensitivity and the ability to quantify multiple targets concurrently. Its application is particularly impactful in oncology and infectious disease diagnostics.
Table 1: Performance Metrics of Multiplexed dPCR Assays in Clinical Research
| Application Area | Specific Targets | Multiplexing Level | Limit of Detection | Key Performance Findings |
|---|---|---|---|---|
| BTK Inhibitor Resistance [51] | BTK (C481S, C481F, C481R) and PLCG2 (R665W) mutations | 3 assays covering 96% of resistant cases | Superior to NGS at low allelic frequencies | Detected 68 mutations vs. 49 by NGS in a 28-patient cohort; more suitable for small clone detection. |
| Pancreatic Cancer Precursors [52] | KRAS mutations, GNAS mutations, Copy Number Alterations (CNA) | 14-plex (including wild-type sequences & reference) | <0.2% Variant Allele Frequency | Simultaneously quantified single nucleotide mutations and CNAs in liquid biopsy and tissue samples. |
| Viral Pathogen Subtyping [2] | Five diarrheagenic E. coli subtypes | 5-plex in a single well | 0.5 to 1 ng/μL | 100% sensitivity and specificity; different DNA concentrations did not influence subtyping. |
| Blood-borne Virus Detection [53] | HCV, HIV-1, HHpgV-1 | 3-plex in a single tube | 100 copies/mL | 100% specificity; successfully identified single and co-infections in clinical serum samples. |
The data in Table 1 demonstrates the versatility of mdPCR. In monitoring resistance to Bruton's tyrosine kinase (BTK) inhibitors in hematologic malignancies, mdPCR proved to be a more sensitive and rapid alternative to next-generation sequencing (NGS), making it ideal for guiding therapeutic decisions at relapse [51]. Furthermore, the development of a 14-plex dPCR assay for pancreatic cancer precursors showcases a significant leap in multiplexing capability. This assay can simultaneously detect low-frequency mutations (below 0.2% variant allele frequency) and copy number alterations, providing a comprehensive molecular profile from minimal sample material, such as liquid biopsies [52].
Detailed Experimental Protocols
Protocol 1: Multiplex dPCR for BTK Inhibitor Resistance Mutation Detection
This protocol is adapted from a study demonstrating the sensitive detection of mutations conferring resistance to BTK inhibitors in chronic lymphocytic leukemia [51].
1. Sample Preparation and DNA Extraction
- Obtain peripheral blood or bone marrow aspirate from patients.
- Extract genomic DNA using a commercial kit suitable for blood samples (e.g., QIAamp DNA Blood Mini Kit). Quantify DNA using a spectrophotometer and adjust the concentration to a working range of 10-50 ng/μL.
2. Multiplex Digital PCR Assay Setup
- Primers and Probes: Design and validate three separate multiplex dPCR assays. Each assay uses a combination of TaqMan hydrolysis probes labeled with distinct fluorophores (e.g., FAM, HEX/VIC) to differentiate between wild-type and mutant sequences for BTK (C481S, C481F, C481R) and PLCG2 (R665W).
- Reaction Mixture (per reaction):
- 10 μL of 2X dPCR Supermix (for probes)
- 1.0 μL of 20X primer-probe mix for each mutation target
- 5-50 ng of template DNA
- Nuclease-free water to a final volume of 20 μL
3. Partitioning and Amplification
- Load the reaction mixture into a droplet generator (e.g., Bio-Rad QX200 Droplet Generator) to create ~20,000 nanodroplets per sample.
- Transfer the emulsified samples to a 96-well PCR plate and seal.
- Perform PCR amplification on a thermal cycler using the following cycling conditions:
- Enzyme activation: 95°C for 10 minutes
- 40 cycles of:
- Denaturation: 95°C for 30 seconds
- Annealing/Extension: 60°C for 60 seconds
- Enzyme deactivation: 98°C for 10 minutes
- Hold at 4°C (Ensure the ramp rate is set to 2°C/second for optimal performance).
4. Post-PCR Analysis
- Read the droplets using a droplet reader (e.g., Bio-Rad QX200 Droplet Reader).
- Analyze the data with associated software (e.g., QuantaSoft). Set thresholds to distinguish positive and negative droplets for each fluorescence channel based on negative and positive controls.
- The software will automatically calculate the absolute concentration (copies/μL) and variant allele frequency for each mutation using Poisson statistics.
Protocol 2: Highly Multiplexed dPCR with Melting Curve Analysis for Pancreatic Cancer
This protocol outlines a method for a 14-plex dPCR assay that combines mutation detection with copy number analysis via melting curves [52].
1. Sample and Primers
- Samples: DNA from formalin-fixed paraffin-embedded (FFPE) tissue, liquid biopsy (cfDNA), or frozen tissue. For cfDNA, use 5-20 ng per reaction.
- Primer Design: Design primers to amplify wild-type and mutant sequences for KRAS and GNAS, along with the reference gene RPP30. Primers are designed to generate amplicons with distinct melting temperatures (Tm).
2. Multiplex dPCR Reaction Setup
- Reaction Mixture (per reaction):
- 10 μL of 2X Evagreen or similar saturating DNA dye master mix
- 2.0 μL of a custom 7X primer mix (containing all 14 primer pairs)
- 5 μL of template DNA (1-10 ng)
- Nuclease-free water to a final volume of 20 μL
3. Partitioning, Amplification, and Melting
- Partition the reaction mixture into a minimum of 20,000 partitions using a chip-based system (e.g., Sniper DQ24, Qiagen QIAcuity, or Optolane LOAA).
- Perform PCR amplification with standard cycling conditions suitable for the primer sets.
- Following amplification, perform a high-resolution melting (HRM) curve analysis:
- Denature at 95°C for 2 minutes.
- Cool to the starting temperature (e.g., 60°C).
- Gradually increase temperature to 95°C at a slow ramp rate (e.g., 0.1°C/second) while continuously monitoring fluorescence.
4. Data Analysis
- The endpoint fluorescence is used for initial absolute quantification of each target.
- The melting curve data is analyzed to generate derivative melt plots (-dF/dT vs. Temperature). Each specific amplicon will produce a distinct peak at its characteristic Tm.
- Variant allele frequencies are calculated from the ratio of mutant to wild-type sequences. Copy number alterations are determined by comparing the concentration of the target gene to the reference gene (RPP30).
Workflow Visualization
The following diagram illustrates the core workflow of a multiplexed digital PCR experiment, from sample preparation to final data analysis.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of multiplexed dPCR relies on a suite of specialized reagents and instruments. The table below lists essential components and their functions.
Table 2: Essential Reagents and Tools for Multiplexed dPCR
| Item | Function/Description | Examples/Considerations |
|---|---|---|
| dPCR Master Mix | A chemical formulation optimized for partition stability and robust amplification. | Probe-based supermix (for target-specific detection); Evagreen master mix (for melting curve analysis) [52]. |
| Primers & Probes | Oligonucleotides designed to specifically bind and amplify target sequences. | For multiplexing, TaqMan probes with non-overlapping fluorophores (FAM, HEX, Cy5) or primers for amplicons with distinct Tm are used [51] [52]. |
| Partitioning Device | Creates thousands of nanoscale reactions for single-molecule amplification. | Droplet generators (Bio-Rad QX series, Sniper DQ24); Chip-based systems (Qiagen QIAcuity, Optolane LOAA) [50] [54]. |
| Thermal Cycler | Instrument that drives PCR through precise temperature cycles. | Often integrated with the partitioning/reading platform (e.g., QIAcuity integrated cycler) [54]. |
| Droplet/Chip Reader | Measures endpoint fluorescence in each partition to determine positivity. | Fluorescence-capable readers (e.g., Bio-Rad QX200 Reader, Sniper DQ24 imager) [50] [54]. |
| Analysis Software | Interprets fluorescence data, applies Poisson statistics, and provides absolute quantification. | Vendor-specific software (e.g., QuantaSoft, QIAcuity Software) is critical for accurate data interpretation [54]. |
Technology Platform Comparison
The mdPCR landscape features several commercial platforms, each with unique strengths in partitioning, multiplexing capacity, and workflow integration.
Table 3: Comparison of Select Digital PCR Platforms with Multiplexing Capabilities
| Platform / Company | Partitioning Technology | Key Multiplexing Feature | Representative Use Case |
|---|---|---|---|
| QX700/Stilla (Bio-Rad) [54] [55] | Droplet-based (6 colors) | Ease of use, cost benefits for broader adoption. | Oncology diagnostics, rare mutation detection. |
| QIAcuity (Qiagen) [54] [55] | Chip-based (nanoplates) | Up to 12-plex per reaction; integrated, automated workflow. | Infectious disease testing, wastewater monitoring, gene expression. |
| LOAA (Optolane) [54] | Chip-based ("lab-on-an-array") | Real-time absolute quantification in each partition; wide dynamic range. | HER2 status testing in cancer [54]. |
| DQ24 (Sniper) [54] | Droplet-based (VibroJect technology) | 6-plex + reference; no microfluidic chip required. | Gene fusions, MRD, infectious disease testing. |
| Absolute Q (Thermo Fisher) [55] | Chip-based (Counting plates) | High-resolution counting technology; AI-powered software. | General research and clinical applications. |
Solving Multiplex PCR Challenges: A Guide to Robust Assay Design and Optimization
False negatives in multiplex PCR assays present a significant challenge in molecular diagnostics and high-resolution subtyping research, potentially leading to missed detections and inaccurate conclusions. These errors primarily stem from two technical obstacles: the formation of stable secondary structures in nucleic acid targets that limit primer accessibility, and primer-dimer interactions that efficiently consume reagents without generating target amplicons [56]. In the context of high-resolution subtyping research, such as distinguishing between classical, hypervirulent, and convergent Klebsiella pneumoniae pathotypes, false negatives can obscure critical phenotypic differences and compromise study validity [57].
The financial and temporal costs of false negatives are substantial, requiring repeated experiments, additional validation, and potentially delaying research progress. This application note provides detailed strategies and protocols to overcome these challenges through advanced primer design, optimized reaction conditions, and robust validation methodologies specifically tailored for researchers engaged in pathogen subtyping and characterization.
Computational Design Strategies
In Silico Assay Design and Evaluation
Modern assay development leverages comprehensive computational approaches to preemptively address factors contributing to false negatives. The traditional iterative design-test-optimize cycle is being replaced by data-driven workflows that utilize extensive sequence databases and sophisticated algorithms to predict assay performance before laboratory validation [58].
Figure 1: Computational workflow for multiplex PCR assay design with iterative primer optimization
The Simulated Annealing Design using Dimer Likelihood Estimation (SADDLE) algorithm represents a significant advancement in multiplex primer design. This approach systematically minimizes primer-dimer formation by evaluating a loss function that estimates dimer severity between all possible primer pairs in a set. For a 96-plex PCR primer set (192 primers), SADDLE reduces the fraction of primer dimers from 90.7% in naive designs to just 4.9% in optimized sets [37].
Target Selection and Signature Validation
Effective target selection requires identifying unique genomic regions with minimal potential for secondary structure formation. This process involves:
- Comprehensive database curation: Assembling whole genome sequences from public repositories like NCBI Pathogen Detection to capture genetic diversity [57] [58].
- Multiple sequence alignment: Identifying conserved regions across target pathogens while highlighting variable regions useful for subtyping.
- Secondary structure prediction: Using tools like mfold or UNAFold to evaluate potential folding in target regions that might limit primer accessibility.
- In silico PCR validation: Computational testing against inclusivity panels (target organisms) and exclusivity panels (near-neighbor organisms) to predict false negatives and false positives [58].
Table 1: Key Bioinformatics Tools for Multiplex PCR Assay Design
| Tool Category | Specific Tools/Approaches | Application in Assay Design | Performance Benefit |
|---|---|---|---|
| Sequence Database | NCBI Pathogen Detection, Institut Pasteur MLST | Access to comprehensive genomic data for target and near-neighbor organisms | Identifies genetic diversity to prevent false negatives due to sequence variation [57] [58] |
| Primer Design | Thermo Fisher OligoPerfect, SADDLE Algorithm | Optimizes primer characteristics and minimizes dimer formation | Reduces primer-dimer formation from 90.7% to 4.9% in 96-plex assays [57] [37] |
| Specificity Validation | NCBI Primer-BLAST, in silico PCR | Checks primer specificity against entire databases | Predicts potential cross-reactivity and false positives before wet lab testing [57] [58] |
| Secondary Structure Prediction | mfold, UNAFold | Models target sequence folding and primer accessibility | Identifies problematic targets with stable secondary structures that cause false negatives |
Experimental Optimization Protocols
Multiplex PCR Assay Protocol for Pathogen Subtyping
This optimized protocol enables simultaneous detection of Klebsiella pneumoniae pathotypes (classical, hypervirulent, and convergent strains) while minimizing false negatives [57].
Materials and Reagents
- Template DNA (minimal input: 1 ng/μL) [57]
- PCR master mix with optimized buffer components
- Primers (sequences detailed in Table 2)
- Thermocycler with gradient capability
- Agarose gel electrophoresis equipment or capillary electrophoresis system
Primer Design Specifications Primers should target key biomarkers with the following characteristics:
- Length: 18-22 bases
- G+C content: Approximately 50 mol%
- Melting temperature (Tm): <2°C ΔTm across all primers in the multiplex
- Dimer potential: Minimized using computational design tools [57] [37]
Table 2: Example Primer Panel for K. pneumoniae Pathotyping [57]
| Target Type | Specific Genes | Amplicon Size (bp) | Primary Function |
|---|---|---|---|
| Hypervirulence Markers | rmpA, rmpA2, iucA, peg344, iroB | Varies by design | Differentiation of hypervirulent (hvKp) from classical (cKp) strains |
| Carbapenem Resistance | blaNDM, blaOXA-48-like, blaKPC | Varies by design | Identification of carbapenem-resistant (CR-Kp) strains |
| Extended-spectrum β-lactamase | blaCTX-M | Varies by design | Detection of ESBL-producing strains |
| Internal Control | ABL1 mRNA | 104 bp | Verification of RNA isolation, reverse transcription, and PCR amplification [59] |
Step-by-Step Procedure
- Reaction Setup
- Prepare 25 μL reactions containing:
- 1X PCR buffer with additional MgCl2 (optimize between 2-4 mM)
- 200 μM of each dNTP
- 0.2-0.4 μM of each primer (optimize concentration for each primer pair)
- 1.0-1.5 U of DNA polymerase with high processivity
- 1-5 μL template DNA (minimum 1 ng/μL)
- Include positive controls (characterized reference strains) and negative controls (no template) in each run.
- Prepare 25 μL reactions containing:
Thermocycling Conditions
- Initial denaturation: 95°C for 5 minutes
- 35-45 cycles of:
- Denaturation: 95°C for 10-30 seconds
- Annealing: 58-62°C (optimize using gradient PCR) for 10-30 seconds
- Extension: 72°C for 20-60 seconds (adjust based on amplicon size)
- Final extension: 72°C for 5-7 minutes
- Hold: 4°C indefinitely
Amplicon Analysis
- Separate PCR products by capillary electrophoresis or agarose gel electrophoresis
- Analyze amplification patterns against expected band sizes for pathotype classification
- For quantitative applications, use real-time PCR with hydrolysis probes
Addressing Secondary Structure and Primer Dimers
Secondary Structure Mitigation
- Thermal optimization: Incorporate a hot start activation step (95°C for 5 minutes) to ensure complete denaturation before cycling begins.
- Chemical additives: Include DMSO (2-5%), betaine (1-1.5 M), or formamide (1-3%) in reaction mixtures to disrupt secondary structures [57].
- Denaturant conditions: Use 7-deaza-dGTP (partial substitution for dGTP) to reduce base pairing strength in GC-rich targets.
Primer-Dimer Prevention
- Co-Primers technology: Implement primers with two target recognition sequences linked together—a short primer and a longer capture sequence—to dramatically reduce primer-dimer formation while increasing specific signal generation [56].
- Touchdown PCR: Implement a touchdown approach where the annealing temperature is gradually decreased (e.g., from 65°C to 55°C over 10 cycles) to favor specific amplification during early cycles.
- Primer concentration titration: Systematically vary primer concentrations (0.1-0.5 μM) to find the optimal balance between sensitivity and dimer formation.
Validation and Quality Control
Comprehensive Assay Validation
Robust validation is essential to identify and eliminate sources of false negatives in multiplex PCR assays:
Internal Controls Incorporate the human ABL1 gene as an internal control to verify successful RNA isolation, reverse transcription, and PCR amplification. Primers should be designed to span exon-exon junctions to ensure amplification of cDNA rather than genomic DNA [59].
Analytical Sensitivity Testing
- Determine the limit of detection (LOD) using serial dilutions of characterized control templates.
- For the K. pneumoniae multiplex PCR, the assay demonstrated high sensitivity with efficient amplification from DNA inputs as low as 1 ng/μL [57].
- Compare against reference methods like digital droplet PCR (ddPCR), which can detect single copies of target genes [60].
Inclusivity and Exclusivity Testing
- Test against a panel of well-characterized target strains (inclusivity) and near-neighbor organisms (exclusivity).
- For the K. pneumoniae assay, validation against whole-genome sequencing data demonstrated 100% specificity without cross-amplification in ATCC control strains [57].
Table 3: Troubleshooting Guide for False Negatives in Multiplex PCR
| Problem | Potential Causes | Solutions | Expected Outcomes |
|---|---|---|---|
| Consistent false negatives across targets | Enzyme inhibition, inefficient lysis, reaction setup errors | Implement internal controls (e.g., ABL1), add BSA (0.1-0.5 μg/μL), verify reagent concentrations | Internal control amplification confirms successful RNA isolation and reverse transcription; identifies failed reactions [59] |
| Target-specific false negatives | Sequence polymorphisms, secondary structure, primer binding issues | Redesign primers using SADDLE algorithm, optimize annealing temperature, add DMSO (2-5%) or betaine (1-1.5 M) | Uniform amplification across all targets; computational prediction of primer dimer reduction to 4.9% [57] [37] |
| Variable sensitivity between replicates | Primer-dimer formation, stochastic effects at low template concentration | Use Co-Primers technology, increase template input, optimize primer concentrations | 2.5-fold increase in fluorescent signal with Co-Primers; consistent detection at low template concentrations [56] |
| Reduced amplification efficiency in multiplex | Enzyme limitation, substrate competition, buffer incompatibility | Increase polymerase concentration (1.5-2.0 U/reaction), optimize MgCl2 concentration (2-4 mM), balance primer concentrations | Successful simultaneous detection of all targets with uniform efficiency [57] |
Figure 2: Diagnostic decision pathway for troubleshooting false negatives in multiplex PCR assays
Research Reagent Solutions
Table 4: Essential Research Reagents for Overcoming False Negatives
| Reagent Category | Specific Examples | Function in Assay Optimization | Application Notes |
|---|---|---|---|
| Specialized Primers | Co-Primers | Two target recognition sequences linked to reduce primer-dimer formation | Increases fluorescent signal 2.5-fold; critical for highly multiplexed reactions [56] |
| Polymerase Systems | Hot-start DNA polymerases | Prevents non-specific amplification during reaction setup | Reduces primer-dimer formation; improves specificity in complex multiplex reactions |
| Secondary Structure Suppressants | DMSO (2-5%), betaine (1-1.5 M), 7-deaza-dGTP | Disrupts stable secondary structures in GC-rich targets | Enhances amplification efficiency; particularly valuable for targets with high GC content |
| Buffer Additives | BSA (0.1-0.5 μg/μL), trehalose, glycerol | Stabilizes enzymes, neutralizes inhibitors in complex matrices | Improves robustness with clinical samples; enhances resistance to inhibitors |
| Internal Control Templates | ABL1 mRNA primers, synthetic gBlocks | Verifies successful RNA isolation, reverse transcription, and amplification | Distinguishes true negatives from assay failure; gBlocks provide quantifiable standards [60] [59] |
Effective management of false negatives in multiplex PCR requires an integrated approach addressing both computational design and experimental optimization. The strategies outlined herein—including the SADDLE algorithm for primer design, Co-Primers technology for dimer suppression, and comprehensive validation protocols—enable researchers to achieve highly sensitive and specific detection in complex subtyping applications. Implementation of these methods supports the generation of reliable, reproducible data essential for high-resolution pathogen characterization and drug development research.
In the context of high-resolution subtyping research, the integrity of multiplex PCR data is paramount. False positive results, arising primarily from primer-amplicon interactions and various forms of cross-reactivity, represent a significant threat to data reliability, potentially leading to erroneous conclusions in pathogen subtyping, genotyping, and gene expression analysis. A false positive occurs when a sample does not contain the target sequence, but the amplification test incorrectly signals its presence [61]. In multiplex assays, where numerous primer pairs coexist, the probability of such non-specific interactions increases dramatically. These interactions can deplete reaction components, inhibit target amplification, and generate spurious amplification products that are detected as genuine signals [7] [61]. For researchers and drug development professionals, understanding and mitigating these sources of error is not merely a technical exercise but a fundamental requirement for generating reproducible and clinically actionable data. This document outlines the mechanisms behind these false positives and provides detailed, actionable protocols for their elimination.
Mechanisms and Impacts of Non-Specific Interactions
Primer-Amplicon Interactions
One of the most insidious sources of false positives in multiplex PCR is the interaction between a primer and a non-target amplicon. This occurs when a primer sequence, designed for a specific target, finds a fortuitous but imperfect binding site on an amplicon generated by a different primer pair in the same reaction [61].
- Mechanism: A primer binds to a secondary site on a non-target amplicon. The polymerase then extends the primer, generating a shorter, unexpected product. If this product falls within the detection range of the assay (e.g., is flanked by probe-binding sites or is of a detectable size), it will be recorded as a false positive signal.
- Impact: This not only produces a false positive for the primer's intended target but can also deplete primers and dNTPs, potentially causing false negatives for other targets and distorting the overall quantitative profile of the assay [61].
Other Forms of Cross-Reactivity
- Primer-Dimer Formation: Two primers hybridize to each other, typically via a few complementary bases at their 3' ends, and are extended by the polymerase. This consumes reagents and can produce a detectable amplification signal, especially in probe-based assays where dye release is non-specific [7] [61].
- Cross-Hybridization with Non-Target Genomic Sequences: Primers may bind to and amplify homologous sequences from related but non-target organisms or from different regions of the same genome. This is a critical issue in subtyping, where distinguishing between highly similar sequences (e.g., viral clades) is the goal [5].
The following diagram illustrates the primary mechanisms that lead to false positives in a multiplex PCR reaction.
Strategic Primer and Assay Design for Prevention
The most effective approach to managing false positives is through meticulous in silico design, which prevents problems before costly wet-lab experiments begin.
Comprehensive Primer Design Criteria
- Homology and Specificity Checks: Design primers with minimal homology to non-target sequences, including all other primers in the pool and non-target genomic regions. This requires using tools like primer-BLAST that perform comprehensive off-target binding checks against entire genome databases [62].
- Consensus Design for Broad Coverage: In subtyping applications, account for known sequence diversity within the target. For instance, in designing an influenza A(H5) subtyping assay, researchers analyzed circulating clade 2.3.4.4b sequences to ensure primer-probe sets had a maximum of one mismatch to over 97% of known variants [5].
- Harmonized Thermodynamic Properties: Ensure all primers in a multiplex have similar and high annealing temperatures (e.g., 65–68°C). This allows the use of a two-step PCR protocol with a combined annealing/extension step, which improves specificity and reduces spurious initiation [63].
- Optimized Primer Length and Concentration: Use primers 18–30 nucleotides in length. In the pool, the concentration of each primer may need to be reduced (e.g., to 0.015 μM) to minimize interaction potential while maintaining efficient amplification [63].
Advanced Computational Tools and Pooling Strategies
Sophisticated software platforms are indispensable for managing the complexity of multiplex design.
Table 1: Computational Tools for Multiplex PCR Design
| Tool/Platform | Primary Function | Key Feature | Application in Subtyping |
|---|---|---|---|
| PrimerPooler [63] | Allocates primers into optimized subpools | Minimizes cross-hybridization via comprehensive inter-/intra-primer analysis | Manages large panels of primers for pathogen strain identification |
| Primal Scheme [63] | Develops multiplex primer schemes | Generates overlapping amplicons; uses pairwise alignment for universal candidates | Designing tiling amplicon schemes for whole-genome sequencing of variants |
| NGS-PrimerPlex [63] | High-throughput primer design | Non-target amplicon prediction and SNP overlap assessment | Designing targeted NGS panels for high-resolution genotyping |
| DNA Software Tools [61] | Models complex interactions | Uses N-state thermodynamic models to predict secondary structure & binding | Overcoming false negatives/positives caused by folded DNA targets |
The workflow for employing these strategies is methodical, progressing from sequence analysis to experimental validation.
Experimental Optimization and Validation Protocols
Even with perfect in silico design, rigorous wet-lab validation is essential.
Reagent and Cycling Condition Optimization
- Hot Start PCR: This technique is critical. By preventing polymerase activity until the first high-temperature denaturation step, it drastically reduces primer-dimer formation and other non-specific extensions that occur during reaction setup [7].
- PCR Additives: Cosolvents like betaine, DMSO, or glycerol can help destabilize secondary structures in GC-rich templates, promoting uniform primer binding across all targets and reducing amplification bias [7].
- Cycling Parameters:
- Extended Annealing/Empirical Testing: A systematic study on qPCR optimization recommends a stepwise approach to optimize primer sequences, annealing temperatures, and primer concentrations for each target to achieve maximum efficiency and specificity [62].
- Cycle Number: Keep the number of cycles to the minimum necessary for detection, as spurious products accumulate in later cycles.
Comprehensive Controls and Validation Experiments
- Specificity Testing with Non-Target Templates: Validate the assay using genomic RNA or DNA from closely related non-target strains. For example, the H5 subtyping qRT-PCR was validated against non-H5 influenza A viruses to confirm no cross-reactivity [5].
- Limit of Detection (LLOD) and Efficiency Determination: Perform dilution series with known copy numbers of the target to establish the detection limit and amplification efficiency. The ideal primer pair should achieve an R² ≥ 0.9999 and an efficiency (E) of 100 ± 5% [62].
- Dual-Target Design: For critical subtyping applications, design two independent primer-probe sets for the same target. This drastically reduces the chance of a false negative due to sequence variation and provides internal confirmation, making a false positive from cross-reactivity highly unlikely [5].
Table 2: Key Research Reagent Solutions for False Positive Management
| Reagent / Material | Function | Optimization Consideration |
|---|---|---|
| Hot-Start DNA Polymerase [7] | Suppresses non-specific amplification during reaction setup by requiring heat activation. | Essential for all complex multiplex assays. Reduces primer-dimer and mis-priming. |
| PCR Additives (e.g., Betaine, DMSO) [7] | Destabilizes secondary structure, homogenizes melting temperatures of different amplicons. | Concentration must be titrated; typically 0.5-1M Betaine or 1-5% DMSO. |
| Photoactive DNA-Intercalating Dyes (PMA, EMA) [64] | Distinguishes viable from dead cells by penetrating compromised membranes and blocking DNA amplification. | Critical for viability testing; requires optimization of dye concentration and light exposure. |
| Synthesized Nucleic Acid Standards (gBlocks) [65] [5] | Provides absolute quantitation standards and allows for determination of assay LOD and efficiency without cultured pathogens. | Designed to match primer binding regions; used to create standard curves. |
| Multiplex PCR Kits | Provides pre-optimized buffers with balanced salt concentrations for multiple primer pairs. | A starting point, but primer-specific optimization is often still required. |
Eliminating false positives in multiplex PCR is an achievable goal that demands a rigorous, multi-faceted strategy. By understanding the mechanisms of primer-amplicon interactions and cross-reactivity, researchers can implement robust in silico design principles using advanced computational tools. This must be followed by systematic experimental optimization that includes stringent thermal cycling protocols, the use of specialized reagents, and comprehensive validation with appropriate controls. For high-resolution subtyping research, where the accurate discrimination of closely related sequences has direct implications for diagnostics and therapeutic development, such rigorous attention to assay design and validation is not just best practice—it is fundamental to generating reliable and meaningful scientific data.
Multiplex polymerase chain reaction (PCR) is a cornerstone technique in molecular biology, enabling the simultaneous amplification of multiple DNA targets in a single reaction. Its value in high-resolution subtyping research is immense, allowing for the discrimination of closely related pathogen strains, detailed genetic profiling, and comprehensive analysis of complex samples. However, the development of a robust multiplex PCR assay is a multifaceted process that requires careful optimization to avoid preferential amplification and to achieve balanced, specific, and sensitive detection of all targets. Among the most critical parameters to optimize are primer concentration and annealing temperature. This application note provides detailed protocols and strategies for systematically balancing primer efficiencies and establishing optimal annealing conditions to ensure the success of multiplex PCR assays in advanced research and diagnostic contexts.
Core Principles of Multiplex PCR Optimization
The simultaneous amplification of multiple targets introduces technical challenges not typically encountered in singleplex PCR. Primers for different targets compete for reaction components and can interact with each other, leading to primer-dimer formation, off-target amplification, and significant disparities in amplification efficiency [66]. These issues can severely compromise the accuracy of high-resolution subtyping, where the faithful representation of all targets is paramount.
Two foundational principles govern the optimization process:
- Primer Concentration Balancing: Adjusting the concentration of each primer pair to ensure uniform amplification efficiency across all targets, thereby preventing bias towards amplicons with more efficient primers [66] [67].
- Annealing Temperature Optimization: Establishing a temperature that promotes specific and simultaneous binding of all primer pairs to their respective targets, while minimizing non-specific binding and primer-dimer artifacts [68].
The following sections provide detailed, step-by-step protocols for addressing these critical parameters.
Protocol 1: Primer Concentration Balancing Using Standardized DNA Templates
Balancing primer concentrations with total DNA extracts can be problematic when targeting multi-copy genes or different species due to the unknown number of template molecules present [66]. The following protocol overcomes this limitation by using standardized DNA templates, which are PCR products encompassing the primer-binding sites for each target.
Materials and Reagents
- Primer Pairs: Desalted or HPLC-purified primers for all targets and internal control.
- Template DNA: Genomic DNA from positive control samples or reference strains.
- PCR Reagents: Thermostable DNA polymerase (e.g., standard or multiplex master mix), dNTPs, PCR buffer (with and without MgCl₂).
- Agarose Gel Electrophoresis System or automated capillary electrophoresis system (e.g., QIAxcel).
- Spectrophotometer or fluorometer for nucleic acid quantification.
- Thermal Cycler.
Step-by-Step Procedure
Step 1: Generate Standardized DNA Templates
- For each target, perform a singleplex PCR using a generic primer pair that flanks the region of your specific primers. For example, use universal primers like LCO1490/HCO2198 for mitochondrial COI genes [66].
- Purify the resulting PCR products using a commercial PCR purification kit.
- Quantify the concentration of each purified amplicon using a spectrophotometer and normalize all to the same concentration (e.g., 10-20 ng/μL). These normalized amplicons are your standardized DNA templates, each containing a known, accessible binding site for one of your specific primer pairs.
Step 2: Initial Multiplex Setup with Equal Primer Concentrations
- Prepare a multiplex PCR master mix containing all primer pairs at an equal, low concentration (e.g., 0.1 μM each) [68] [53].
- Aliquot the master mix into separate tubes.
- To each tube, add one of the standardized DNA templates as the sole template source. Include a negative control (no template).
- Run the PCR using a thermal profile with an estimated, conservative annealing temperature.
Step 3: Analyze Amplification Efficiency
- Analyze the PCR products by capillary electrophoresis (e.g., QIAxcel) or agarose gel electrophoresis.
- Compare the signal strength (e.g., peak height in RFU or band intensity) for the target amplicon across all reactions. The signal strength reflects the primer pair's efficiency under the given conditions [66].
Step 4: Iterative Primer Adjustment
- Identify primer pairs yielding disproportionately high or low signals.
- Prepare a new multiplex master mix, systematically increasing the concentration of low-efficiency primers and/or decreasing the concentration of high-efficiency primers. Adjustments are typically made in 0.05 μM increments.
- Repeat steps 2 and 3 using a mixture of all standardized DNA templates until all targets are amplified with relatively even signal strength.
Step 5: Validation with Complex Template
- Once balanced with standardized templates, validate the multiplex PCR using a more complex, biologically relevant template, such as genomic DNA from a sample with a known profile, to ensure performance is maintained.
Data Interpretation and Troubleshooting
- Uneven Amplification Persists: Consider re-designing primers with consistently high melting temperatures (Tms) or investigate potential secondary structures. The use of a hot-start polymerase can improve specificity.
- Non-specific Bands or Primer-Dimers: Further optimize the annealing temperature (see Protocol 2) and consider reducing primer concentrations further if possible.
Table 1: Example Primer Concentration Adjustment During Optimization
| Target Gene | Initial Concentration (μM) | Adjusted Concentration (μM) | Relative Signal Strength (Pre/Post) |
|---|---|---|---|
| nuc | 0.1 | 0.15 | Low → Balanced |
| mecA | 0.1 | 0.08 | High → Balanced |
| hla | 0.1 | 0.1 | Balanced → Balanced |
| sea | 0.1 | 0.12 | Low → Balanced |
| IAC | 0.1 | 0.05 | High → Balanced |
Protocol 2: Annealing Temperature Optimization Using Gradient PCR
The annealing temperature (Ta) is critical for specificity in multiplex PCR. Using a predicted Tm is often insufficient, as buffer composition and primer interactions can alter effective Ta [68]. A gradient PCR is the most reliable method for empirical determination.
Materials and Reagents
- Optimized Primer Mix: The balanced primer concentrations from Protocol 1.
- Template DNA: A positive control template containing all targets, such as a mix of genomic DNA from known positive samples or the standardized template mix.
- PCR Reagents: As in Protocol 1.
- Thermal Cycler with Gradient Functionality.
Step-by-Step Procedure
Step 1: Reaction Setup
- Prepare a single master mix containing the balanced primer concentrations and the positive control template.
- Aliquot the same master mix into each well of the PCR plate or tube strip.
Step 2: Gradient PCR Execution
- In the thermal cycler software, set a gradient across the block that spans a wide temperature range (e.g., 50°C to 65°C). The range should bracket the calculated average Tm of the primer sets.
- Program the cycling conditions, using a combined annealing/extension step is often beneficial in multiplex PCR to shorten cycle times, especially when using primers with harmonized, high Tms (e.g., 65-68°C) [63].
- Start the PCR run.
Step 3: Post-PCR Analysis
- Analyze the results using gel or capillary electrophoresis.
- Evaluate for the following criteria at each temperature:
- Specificity: Presence of only the desired amplicons and absence of non-specific bands or primer-dimers.
- Yield: Strong, balanced signal intensity for all target amplicons.
- Reproducibility: The chosen temperature should be in the middle of a range that produces robust and specific amplification for all targets.
Data Interpretation and Troubleshooting
- No Amplification at Any Temperature: Check primer and template quality. Consider lowering the annealing temperature range or reviewing primer design for secondary structures.
- Non-specific Products at Lower Temperatures: The optimal Ta is likely the highest temperature that still yields strong, specific amplification of all targets.
- Loss of Larger Amplicons at Higher Temperatures: A compromise Ta may be necessary, or the primer design for the missing target may need to be re-evaluated.
Table 2: Example Annealing Temperature Gradient Results
| Annealing Temperature (°C) | Specificity Score (1-5) | Yield Score (1-5) | Notes |
|---|---|---|---|
| 55.0 | 2 | 5 | High yield but non-specific bands present |
| 57.5 | 3 | 5 | Faint non-specific bands |
| 58.8 | 5 | 5 | Optimal: High yield and high specificity |
| 60.1 | 5 | 4 | Good specificity, slightly reduced yield |
| 61.5 | 5 | 3 | Specific, but yield for two targets is low |
| 63.0 | 5 | 1 | Specific, but very low yield for most targets |
Integrated Workflow for Multiplex PCR Assay Development
The following diagram illustrates the systematic workflow for developing and optimizing a multiplex PCR assay, integrating both primer balancing and annealing temperature optimization.
The Scientist's Toolkit: Essential Reagents and Materials
The successful implementation of these optimization protocols relies on a set of key reagents and tools. The following table details these essential components.
Table 3: Research Reagent Solutions for Multiplex PCR Optimization
| Item | Function/Description | Application Notes |
|---|---|---|
| Multiplex PCR Master Mix | A specialized buffer containing optimized salt concentrations, dNTPs, and a thermostable DNA polymerase. | Often includes MgCl2 at a concentration that supports simultaneous amplification of multiple targets. Hot-start enzymes are recommended to enhance specificity [68]. |
| Standardized DNA Templates | Purified, concentration-normalized amplicons containing the primer binding sites for each target. | Crucial for unbiased primer balancing, as they provide a known quantity of accessible template, independent of genomic complexity and gene copy number variation [66]. |
| Internal Amplification Control (IAC) | A non-target DNA sequence spiked into the reaction and amplified with its own primer pair. | Essential for distinguishing true negative results from PCR failure due to inhibition or reaction setup errors [67]. |
| Capillary Electrophoresis System | An automated system (e.g., QIAxcel) for separating and quantifying PCR products. | Provides high-resolution analysis of amplicon size and yield (in Relative Fluorescence Units, RFU), which is superior to gel electrophoresis for quantitative optimization [66]. |
| Gradient Thermal Cycler | A PCR instrument that allows different tubes to run at different temperatures within the same cycle. | Indispensable for empirically determining the optimal annealing temperature without requiring multiple separate runs [68]. |
| Primer Design Software | Computational tools (e.g., Primer Premier, Primer3, NGS-PrimerPlex) for in silico primer design and analysis. | Used to design primers with compatible Tms, check for primer-dimer potential, and ensure specificity against relevant databases [66] [63]. |
The systematic optimization of primer concentration and annealing temperature is not merely a recommendation but a necessity for developing a reliable multiplex PCR assay capable of high-resolution subtyping. The protocols outlined here—utilizing standardized DNA templates for unbiased primer balancing and empirical gradient PCR for temperature determination—provide a robust framework for researchers. By adhering to this structured approach and leveraging the essential tools described, scientists can overcome the inherent challenges of multiplexing, thereby ensuring the generation of accurate, reproducible, and meaningful data for advanced research and diagnostic applications.
In the field of molecular diagnostics and pathogen surveillance, genetic diversity presents a significant challenge for assay developers. Target sequence variation—single nucleotide polymorphisms (SNPs), insertions, deletions, and recombination events—can critically compromise detection efficiency in multiplex PCR assays. These variations, particularly in primer and probe binding regions, lead to false-negative results, reduced sensitivity, and inaccurate subtyping, ultimately undermining the reliability of diagnostic conclusions. This application note addresses strategic approaches to design robust multiplex assays that maintain comprehensive coverage across diverse genetic variants, with particular focus on high-resolution melting analysis and probe-based detection systems.
The emergence of novel viral variants and the natural genetic drift of pathogens necessitate diagnostic tools capable of adapting to evolution. Conventional assays designed against conserved sequences often fail when faced with unexpected mutations in primer binding sites. Furthermore, in multiplexed systems intended to detect numerous targets simultaneously, the challenge is magnified as variations can affect different targets to varying degrees, potentially creating blind spots in detection capabilities. The strategies outlined herein provide methodologies to anticipate, accommodate, and validate against such variations, ensuring consistent performance across known genetic diversity and resilience against future evolutionary changes.
Strategic Approaches for Variant-Inclusive Assay Design
Probe Modification with Abasic Site Mimics
Incorporating synthetic nucleotides at polymorphic positions within hybridization probes represents an advanced strategy for maintaining detection efficiency across divergent sequences. Recent research has demonstrated the successful use of tetrahydrofuran (THF) residues,
which function as abasic site mimics within molecular probes [69]. This modification strategically eliminates base-pairing interactions at highly variable nucleotide positions, thereby minimizing the impact of known or potential base mismatches on the probe's melting temperature (Tm).
The implementation of this approach requires:
- Identification of polymorphic sites through comprehensive analysis of sequence databases
- Strategic replacement of standard nucleotides with THF residues at these variable positions
- Validation of hybridization stability across known variant spectra
This design enhancement allows a single probe to hybridize efficiently with multiple variant sequences, as the non-pairing abasic site does not destabilize the duplex through mismatch formation. Consequently, assays maintain uniform melting temperatures and detection sensitivity across different subtypes, significantly improving the robustness of variant detection [69].
Bioinformatics-Driven Conservative Design
A foundational approach to ensuring broad variant coverage begins with comprehensive bioinformatic analysis of target sequences across available databases. This process involves:
- Pan-genomic alignment of target sequences to identify conserved regions
- Variant frequency analysis to prioritize commonly occurring polymorphisms
- Epitope masking to avoid regions with known high variability
- Cross-reactivity screening against non-target sequences
Advanced tools such as the NCBI BLAST database provide essential resources for specificity checking during assay design [70]. Similarly, pathogen-specific databases collecting global isolate sequences enable designers to identify truly conserved regions across geographical and temporal distributions. The selection of amplification targets from highly conserved genomic regions—such as structural protein genes or housekeeping genes—forms the first line of defense against variant-induced detection failures.
Table 1: Strategic Comparison of Variant-Inclusive Assay Design Approaches
| Design Strategy | Mechanism of Action | Best Application Context | Technical Limitations |
|---|---|---|---|
| Abasic Site Probes | THF residues at polymorphic positions minimize Tm variance | Detection of highly variable targets with predictable variation | Requires prior knowledge of variable positions; synthetic probe cost |
| Conserved Region Targeting | Amplification from genomic regions with minimal natural diversity | Broad-spectrum pathogen detection; surveillance of stable targets | Limited applicability for rapidly evolving organisms |
| Asymmetric PCR | Unequal primer ratio favors single-stranded DNA production | Enhancing hybridization efficiency in melting curve analysis | Requires optimization of primer ratios; potential reduced efficiency |
| Multiplex HRM | Distinguishes variants by differential melting behavior | Subtyping of closely related strains; discrimination of variants | Requires high-resolution instruments; complex data interpretation |
Multiplex HRM for Subtyping Resolution
High-resolution melting (HRM) analysis provides a powerful platform for distinguishing sequence variants without requiring specialized probes. This technique capitalizes on the fact that DNA melting behavior is highly sensitive to sequence composition, including single nucleotide changes. In a demonstrated application for subtyping five diarrheagenic Escherichia coli strains, HRM enabled discrimination based on characteristic peaks and distinct Tm values in the derivative melting curve [2].
The implementation workflow includes:
- Multiplex PCR amplification of target sequences in a single reaction well
- Precise temperature ramping with high-resolution fluorescence monitoring
- Differentiation of variants based on unique melting profiles
- Cluster analysis of melting curves for subtype classification
This approach proved 100% specific and sensitive with a detection limit of 0.5 to 1 ng/μL, demonstrating that different DNA concentrations did not influence subtyping results—a critical advantage for clinical samples with variable pathogen loads [2]. The method streamlined operational procedures, reduced detection time, and provided a novel tool for subtyping diverse pathogens.
Experimental Validation Protocols
Analytical Sensitivity and Specificity Testing
Comprehensive validation against a panel of reference strains is essential to confirm variant coverage. The following protocol outlines the evaluation of assay inclusivity:
Reference Strain Selection: Obtain reference materials representing known genetic diversity (e.g., 47 reference strains across different subtypes as used in a respiratory pathogen panel) [69]
Limit of Detection (LOD) Determination:
- Prepare serial dilutions of each target
- Test each dilution in at least 20 replicates
- Calculate LOD through probit analysis as the concentration detectable with ≥95% probability
- Record results in copies/μL for standardized comparison
Cross-Reactivity Assessment:
- Test against a panel of non-target organisms (e.g., 10 respiratory viruses and 4 bacteria for respiratory panels)
- Confirm absence of signal in non-target reactions
- Validate specificity under multiplex conditions
Inclusivity Documentation:
- Create a comprehensive table of detected variants
- Note any polymorphisms in primer/probe regions
- Document performance characteristics for each variant
Table 2: Exemplary Analytical Performance of a Variant-Inclusive Multiplex Assay
| Performance Parameter | Experimental Result | Method of Determination | Acceptance Criterion |
|---|---|---|---|
| Limit of Detection | 4.94-14.03 copies/μL across targets | Probit analysis (≥95% hit rate) | ≤20 copies/μL for clinical relevance |
| Intra-Assay Precision | Coefficient of variation ≤0.70% | 5 replicates at 5×LOD and 2×LOD | CV ≤1.5% for Tm values |
| Inter-Assay Precision | Coefficient of variation ≤0.50% | 5 separate runs on different days | CV ≤2.0% for Tm values |
| Inclusivity | Detection of 47/47 reference strains | Testing against diverse subtypes | ≥95% of known variants |
| Cross-Reactivity | No detection of non-target organisms | Panel of 14 non-target pathogens | 100% specificity |
Melting Temperature Optimization Workflow
For assays employing melting curve analysis, precise determination of Tm values is critical for variant discrimination. The following protocol ensures accurate Tm measurement:
Step 1: Asymmetric PCR Setup
- Implement unequal primer ratios (e.g., 50:1 ratio of limiting:excess primer)
- Use 20 μL reaction volumes containing:
- 5× One Step U* Mix
- One Step U* Enzyme Mix
- Limiting and excess primers
- Fluorescently labeled probes
- 10 μL template [69]
Step 2: Thermocycling Conditions
- Reverse transcription: 50°C for 5 minutes
- Initial denaturation: 95°C for 30 seconds
- 45 cycles of:
- Denaturation: 95°C for 5 seconds
- Annealing/extension: 60°C for 13 seconds
Step 3: Melting Curve Analysis
- Denaturation: 95°C for 60 seconds
- Hybridization: 40°C for 3 minutes
- Temperature ramp: 40°C to 80°C at 0.06°C/s
- Continuous fluorescence acquisition
Step 4: Data Interpretation
- Plot negative derivative of fluorescence (-dF/dT) versus temperature
- Identify peak Tm values for each target
- Establish Tm ranges for each variant with acceptable variance (e.g., ±0.5°C)
- Validate separation between variant-specific Tm clusters
This protocol yielded intra-assay and inter-assay coefficients of variation ≤0.70% and ≤0.50%, respectively, demonstrating highly reproducible differentiation of targets based on Tm values [69].
Implementation Workflow for Variant-Inclusive Assays
The diagram below illustrates the comprehensive workflow for developing and implementing variant-inclusive multiplex assays:
Research Reagent Solutions
Table 3: Essential Reagents for Variant-Inclusive Multiplex Assays
| Reagent Category | Specific Examples | Function in Variant-Inclusive Assays |
|---|---|---|
| Specialized Probes | THF-modified probes [69] | Accommodate sequence variations while maintaining uniform Tm |
| PCR Master Mixes | 5× One Step U* Mix [69] | Provide optimized buffer for multiplex amplification |
| Enzyme Systems | One Step U* Enzyme Mix [69] | Support reverse transcription and PCR in unified systems |
| Fluorescent Dyes | SYBR Green, TaqMan probes [71] | Enable real-time monitoring and melting curve analysis |
| Reference Materials | Plasmid controls, reference strains [69] | Validate assay performance across known variants |
| Nucleic Acid Controls | RNase P [69] | Monitor extraction efficiency and sample quality |
Proactive management of target sequence variation is fundamental to developing robust multiplex PCR assays for high-resolution subtyping. Through integrated implementation of bioinformatic conservation analysis, strategic probe engineering with abasic site mimics, and validation against diverse variants, assays can achieve comprehensive coverage while maintaining discrimination power. The experimental protocols and reagent systems described provide a roadmap for researchers to future-proof their detection platforms against the challenge of genetic diversity, ultimately strengthening diagnostic capabilities in both clinical and public health contexts.
Validation Frameworks and Comparative Analysis with Next-Generation Sequencing
In the evolving field of molecular diagnostics, multiplex PCR assays have become indispensable for high-resolution subtyping research, enabling the simultaneous detection and differentiation of multiple pathogens or genetic variants in a single reaction [41] [72]. The ability to accurately identify co-infections and genetically distinct subtypes is crucial for understanding disease dynamics, guiding therapeutic interventions, and developing targeted treatments [41] [73]. However, the development and implementation of these sophisticated assays require rigorous analytical validation to ensure their reliability, accuracy, and reproducibility in both research and clinical settings.
This application note provides a detailed framework for establishing the core analytical performance parameters of multiplex PCR assays, with a specific focus on sensitivity, specificity, and limit of detection (LOD). The protocols and data interpretation guidelines presented herein are designed to support researchers, scientists, and drug development professionals in validating assays for high-resolution subtyping applications, thereby contributing to robust and reproducible research outcomes.
Core Analytical Performance Parameters
Defining Key Validation Metrics
The analytical validation of a multiplex PCR assay rests on three fundamental pillars. Diagnostic sensitivity refers to the assay's ability to correctly identify true positive samples, calculated as (True Positives/(True Positives + False Negatives)) × 100. Diagnostic specificity measures the assay's capacity to correctly identify true negative samples, calculated as (True Negatives/(True Negatives + False Positives)) × 100. The limit of detection (LOD) represents the lowest concentration of the target analyte that can be reliably detected by the assay, typically defined as the concentration detectable in ≥95% of replicates [41] [72]. These parameters must be established for each target in the multiplex panel to ensure comprehensive assay validation.
Experimental Design Considerations
When designing validation experiments, it is crucial to incorporate appropriate controls and replicates to account for experimental variability. Each target should be tested in a minimum of 20 replicates at concentrations near the expected LOD to establish robust detection limits [41] [72]. For specificity testing, a panel of non-target organisms that are genetically similar or commonly found in the same sample matrix should be included to demonstrate minimal cross-reactivity and ensure the assay's ability to discriminate between closely related subtypes [41] [73] [74].
Experimental Protocols for Analytical Validation
Protocol 1: Determining Limit of Detection (LOD)
Sample Preparation and Dilution Series
- Prepare reference materials: Use quantified synthetic oligonucleotides, in vitro transcribed RNA, or cultured pathogens with known concentrations. For nucleic acids, determine copy number/μL using spectrophotometric measurement and the formula: Copy number (molecules) = [X(ng) × (6.0221 × 10^23)] / [(N × 660 g/mol) + (10^9 ng/g)] where X is the mass of DNA in ng and N is the length of the DNA in base pairs [73].
- Create serial dilutions: Prepare a 5-10 fold dilution series in the appropriate buffer, spanning concentrations both above and below the expected LOD. Include negative template controls consisting of molecular grade water or negative sample matrix.
- Extract nucleic acids: Process dilution series using the same automated or manual extraction method intended for clinical or research samples. For nasopharyngeal swabs, centrifugation at 13,000 × g for 10 minutes to remove debris, followed by a wash step in sterile normal saline (13,000 × g, 5 minutes) and resuspension in 200 μL saline prior to extraction may be necessary [41].
PCR Amplification and Data Analysis
- Perform amplification: Run all dilution samples in a minimum of 20 replicates [41] [72] using optimized PCR conditions. For melting curve-based assays, include a post-PCR melting curve analysis beginning with denaturation at 95°C for 60s, hybridization at 40°C for 3min, then temperature increase from 40°C to 80°C at a rate of 0.06°C/s [41].
- Analyze results: Calculate the percentage of positive replicates at each dilution. The LOD is defined as the lowest concentration at which ≥95% of replicates test positive [41] [72]. Probit analysis can be used for statistical confirmation.
Protocol 2: Establishing Analytical Specificity
Cross-Reactivity Testing
- Prepare specificity panel: Collect a comprehensive panel of non-target organisms including closely related genetic variants, common commensals, and pathogens that may be present in the sample matrix. For respiratory assays, this should include other respiratory viruses and bacteria; for HPV genotyping, include different HPV genotypes and other microorganisms that may be present in genital specimens [73] [74].
- Extract and amplify: Process all panel members using the same nucleic acid extraction and amplification protocols as for target samples. Use appropriate positive controls for each non-target organism to ensure nucleic acid quality.
- Analyze results: Evaluate amplification plots and melting curves (for melt-based assays) for any cross-reactivity. The assay should demonstrate no amplification or distinct, non-overlapping melting peaks for all non-target organisms [41] [72].
Inclusivity Testing
- Test strain diversity: Include multiple strains, subtypes, or genetic variants of each target to ensure the assay can detect the full spectrum of intended targets. For respiratory pathogen detection, test 47 reference strains of different subtypes [41]; for malaria detection, ensure primers target conserved regions of the msp1 gene across different isolates [72].
- Evaluate performance: Confirm that all target variants are detected with comparable efficiency. For melting curve assays, verify that Tm values are consistent across variants or that any variations don't lead to misclassification [41] [72].
Protocol 3: Assessing Precision and Reproducibility
Intra-assay and Inter-assay Precision
- Prepare samples: Use reference materials at two concentrations (e.g., 2× LOD and 5× LOD) for each target [41].
- Intra-assay precision: Test each concentration in 5 replicates within the same run [41]. Calculate mean Cq values, melting temperatures (if applicable), and standard deviations/coefficients of variation (CV).
- Inter-assay precision: Test each concentration in 5 replicates across different runs performed by different operators on different days [41]. Calculate mean values and CVs across all runs.
- Acceptance criteria: For melt curve assays, intra-assay and inter-assay CVs for Tm values should be ≤0.70% and ≤0.50%, respectively [41]. For Cq values, CVs should typically be <3% [74].
Data Presentation and Analysis
Quantitative Validation Data from Representative Studies
Table 1: Analytical Sensitivity and Precision Data from Multiplex PCR Validation Studies
| Target Pathogen | LOD (copies/μL) | Intra-assay CV (Tm) | Inter-assay CV (Tm) | Reference |
|---|---|---|---|---|
| SARS-CoV-2 | 4.94-14.03* | ≤0.70% | ≤0.50% | [41] |
| Influenza A/B | 4.94-14.03* | ≤0.70% | ≤0.50% | [41] |
| P. knowlesi | 10 | 0.34% | 0.34% | [72] |
| P. cynomolgi | 10 | 0.37% | 0.37% | [72] |
| P. inui | 10 | 0.35% | 0.35% | [72] |
| CHIKV | 2064 copies/mL | - | - | [75] |
| DENV1 | 3587 copies/mL | - | - | [75] |
| ZIKV | 30249 copies/mL | - | - | [75] |
| RVFV | 73 PFU/mL | - | - | [75] |
Range represents variation across different targets in the multiplex panel [41]
Table 2: Clinical Performance of Validated Multiplex PCR Assays
| Assay Type | Sample Size | Sensitivity | Specificity | Agreement with Reference | Co-infections Detected | Reference |
|---|---|---|---|---|---|---|
| Respiratory Pathogen FMCA | 1005 | 98.81%* | 98.81%* | 98.81% | 6.07% | [41] |
| Simian Malaria msp1 assay | 191 | 100% | 100% | 100% | Not specified | [72] |
| HPV Genotyping | 190 | 98% | 100% | High concordance | Not specified | [73] |
| Arbovirus RDCZ-multiplex | 48 | 75-100%* | 100% | Variable at low viral loads | Not specified | [75] |
Calculated based on resolution of discordant results by sequencing [41] Based on detection of confirmed positive samples [72] *Dependent on target and viral load; some loss of sensitivity at low concentrations [75]
Workflow Visualization
Figure 1: Comprehensive Workflow for Multiplex PCR Assay Validation
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Multiplex PCR Validation
| Reagent/Material | Function | Optimization Guidelines | Application Examples |
|---|---|---|---|
| High-Fidelity Polymerase | Catalyzes DNA amplification with proofreading activity | Use for complex templates or long amplicons; error rate as low as 1×10^-6 [76] | Cloning, sequencing [76] |
| Hot Start Polymerase | Prevents non-specific amplification by requiring heat activation | Reduces primer-dimer formation; improves specificity [76] | All multiplex PCR applications [76] |
| MgCl₂ | Essential cofactor for polymerase activity | Titrate between 1.5-4.0 mM; optimal typically 2-3 mM [77] | Critical for assay efficiency and specificity [76] [77] |
| dNTPs | Building blocks for DNA synthesis | Use balanced solutions at 200-250 μM each; avoid degradation [77] | Standard component in all PCR reactions [77] |
| Buffer Additives (DMSO, Betaine) | Improves amplification efficiency of difficult templates | DMSO (2-10%) for GC-rich templates; Betaine (1-2 M) for long amplicons [76] | GC-rich targets, long-range PCR [76] |
| Fluorophore-Labeled Probes | Target detection in real-time PCR | Design with appropriate quenchers; optimize concentration (0.1-0.3 μM) [41] [73] | Multiplex real-time PCR, FMCA [41] [73] |
| Primer Pairs | Target-specific amplification | Design for similar Tm (55-65°C); length 18-24 bp; GC content 40-60% [76] [77] | All PCR applications [41] [72] [76] |
Troubleshooting Common Validation Challenges
Addressing Sensitivity Issues
When an assay fails to achieve the desired sensitivity, several factors should be investigated. Suboptimal primer design is a common culprit; primers should target conserved regions and be designed with appropriate melting temperatures (55-65°C) and GC content (40-60%) [76] [77]. Insufficient PCR efficiency can be improved by optimizing Mg2+ concentration (typically 1.5-4.0 mM) and adjusting annealing temperature through gradient PCR [76] [77]. For targets with secondary structures or high GC content, additives such as DMSO (2-10%) or betaine (1-2 M) can significantly improve amplification efficiency [76].
Improving Specificity and Reducing Cross-Reactivity
Specificity challenges in multiplex assays often manifest as cross-reactivity between targets or non-specific amplification. High annealing temperature is one of the most effective strategies; for most applications, the optimal annealing temperature (Ta) is 3-5°C below the primer Tm [76]. Asymmetric primer ratios can be employed in melting curve-based assays to favor production of single-stranded DNA, reducing competition from the complementary strand and facilitating more efficient probe-target hybridization during melting curve analysis [41]. Reduced primer concentrations (0.2-1.0 μM) can help minimize primer-dimer formation and non-specific amplification while maintaining efficient target amplification [77].
Comprehensive analytical validation is the cornerstone of reliable multiplex PCR assays for high-resolution subtyping research. The systematic approach to establishing sensitivity, specificity, and LOD described in this application note provides researchers with a framework for developing robust assays capable of accurately differentiating between closely related pathogens or genetic variants. By adhering to these detailed protocols and leveraging the appropriate research reagents, scientists can ensure their multiplex PCR assays generate reproducible, high-quality data suitable for both basic research and drug development applications. As molecular diagnostics continue to evolve, these validation principles will remain essential for advancing our understanding of disease heterogeneity and developing targeted therapeutic interventions.
Multiplex PCR (mPCR) assays represent a significant advancement in molecular diagnostics, enabling the simultaneous detection and subtyping of multiple pathogens in a single reaction. Within high-resolution subtyping research, the clinical utility of these assays is fundamentally determined by their diagnostic accuracy compared to established reference standards, primarily conventional culture and sequencing methods. This application note provides a structured evaluation of mPCR assay performance, detailing key experimental protocols for conducting robust concordance studies. The data and methodologies presented herein are framed to support researchers and drug development professionals in validating novel mPCR panels for respiratory pathogens, ensuring results are reliable, reproducible, and clinically actionable.
The diagnostic accuracy of multiplex PCR assays is typically quantified against culture and sequencing through standard statistical measures. The following table summarizes performance data from recent concordance studies, highlighting the sensitivity, specificity, and predictive values of various mPCR platforms.
Table 1: Diagnostic Performance of Multiplex PCR Assays Against Reference Standards
| Multiplex PCR Assay / Platform | Target Pathogens | Reference Standard | Sensitivity (95% CI) | Specificity (95% CI) | Positive Predictive Value (95% CI) | Negative Predictive Value (95% CI) | Citation |
|---|---|---|---|---|---|---|---|
| Multiplex Probe Amplification (MPA) | 18 Respiratory pathogens (SARS-CoV-2, Influenza A/B, RSV, etc.) | Next-Generation Sequencing (NGS) | 95.00% (N/A) | 93.75% (N/A) | 98.96% (N/A) | 75.00% (N/A) | [78] |
| EvaGreen-based multiplex qPCR | Six bacterial LRTI pathogens (K. pneumoniae, A. baumannii, etc.) | Conventional Culture | 100% (for 4/6 pathogens) | 87.5% - 97.6% | N/A | N/A | [79] |
| One-step RV Real-time PCR | Multiple Respiratory Viruses | Sequencing | 94.1% (88.3% - 97.6%) | 96.6% (92.2% - 98.9%) | N/A | N/A | [80] |
| BioFire FilmArray Pneumonia Panel | Bacteria and Viruses causing Pneumonia | Bacterial Culture | Significantly higher positivity rate (60.3% vs. 52.8%) | N/A | N/A | N/A | [81] |
| Unyvero A50 (Tissue Biopsies) | Various PJI pathogens | Microbiological Culture | 30.0% (12.0% - 62.0%) | 100% (87.0% - 100%) | 100% (48.0% - 100%) | 73.0% (56.0% - 86.0%) | [82] |
Experimental Protocols for Concordance Studies
A robust clinical performance evaluation requires carefully designed experiments to compare the mPCR assay against reference methods. The following protocols outline the key steps for conducting these studies.
Protocol for Specimen Collection and Processing
Proper specimen handling is critical to prevent degradation of nucleic acids and ensure the validity of comparative results.
Materials:
- Sterile swabs, universal containers, or nucleic acid preservation solution (e.g., containing viral inactivators).
- Cold chain equipment (e.g., -80°C freezer, cold packs).
Procedure:
- Collection: Collect respiratory specimens (e.g., nasopharyngeal swabs, sputum, bronchoalveolar lavage) from patients with suspected infections using a uniform protocol [78]. For non-respiratory infections, such as periprosthetic joint infection (PJI), collect multiple periprosthetic tissue biopsies [82].
- Transport and Storage: Immediately after collection, place specimens in nucleic acid preservation solution. Store temporarily at 4°C and transport on cold packs to the laboratory. Aliquot and store specimens at -80°C until nucleic acid extraction to preserve integrity [78].
- Homogenization (for viscous samples): For sputum or tracheal aspirates, homogenize an aliquot with 0.1% dithiothreitol (DTT) for 15 minutes at room temperature. Centrifuge at 8000 rpm for 10 minutes, discard the supernatant, and resuspend the pellet in PBS or TE buffer for DNA extraction [79].
Protocol for Nucleic Acid Extraction
This protocol ensures the simultaneous purification of high-quality DNA and RNA, which is essential for detecting a broad range of pathogens.
Materials:
- Commercial nucleic acid extraction kit (e.g., Easy Pure Viral DNA/RNA Kit, Wizard Genomic DNA Extraction Kit, or automated systems like MagNA Pure 96).
- RNase-free water.
- Centrifuge and microcentrifuge tubes.
Procedure:
- Input Volume: Use 200 μL of clinical specimen or resuspended pellet for extraction [78] [79].
- Extraction: Perform nucleic acid extraction according to the manufacturer's instructions. This typically involves lysis, binding to a silica membrane, washing, and elution.
- Elution: Elute the purified total nucleic acid (DNA and RNA) in 50-60 μL of DNase-free and RNase-free water [78].
- Quality Control: Assess the concentration and purity of the extracted nucleic acids using a spectrophotometer (e.g., NanoDrop). Store eluates at -80°C if not used immediately.
Protocol for Multiplex PCR Setup and Amplification
This protocol is adapted for a TaqMan probe-based real-time PCR system, which offers high specificity and is suitable for multiplexing.
Materials:
- Primer and probe mixes for target pathogens (e.g., FAM, HEX/VIC, ROX, and Cy5 channels).
- PCR master mix (containing buffer, dNTPs, Mg2+, Taq polymerase, Uracil-DNA Glycosylase (UNG) to prevent carryover contamination).
- Real-time PCR instrument (e.g., ABI 7500 Fast System, Bio-Rad CFX96).
Procedure:
- Reaction Preparation: On ice, prepare a total reaction volume of 25 μL per test. Combine the master mix with the specific primer-probe working mix. For example, the MPA assay uses two separate tubes to accommodate 18 targets [78]. Use 1-5 μL of extracted DNA/RNA as template.
- Thermal Cycling: Run the PCR on the real-time instrument using a protocol similar to the following:
- Stage 1 (UDG Incubation): 50°C for 10 min [80] or 55°C for 10 min [78].
- Stage 2 (Initial Denaturation & Enzyme Activation): 95°C for 3-15 min.
- Stage 3 (Amplification): 40-46 cycles of:
- Denaturation: 95°C for 10-15 s.
- Annealing/Extension & Fluorescence Acquisition: 60-62°C for 45 s.
- Stage 4 (Melting Curve Analysis, if applicable): For dye-based methods like EvaGreen, include a melting curve step (e.g., 95°C for 10 s, 25°C for 1 min, 68°C for 15 s) to distinguish amplicons by their melting temperature (Tm) [79] [2].
- Result Interpretation: Analyze fluorescence emission data using the instrument's software. A sample is considered positive for a specific pathogen if the cycle threshold (Ct) value is below a validated cut-off (e.g., Ct < 35) [78].
Protocol for Reference Standard Testing
A. Microbiological Culture:
- Inoculate processed samples onto appropriate agar media (e.g., blood agar, MacConkey agar, chocolate agar) and into liquid broth [82].
- Incubate aerobically and anaerobically at 37°C for 24-48 hours, evaluating for growth at 24-hour intervals.
- Identify bacterial growth using standard techniques (e.g., MALDI-TOF MS) and perform antimicrobial susceptibility testing (e.g., Vitek2) [79]. For quantitative cultures, consider a growth threshold of ≥ 10^5 CFU/mL for positivity in respiratory samples [79].
B. Sequencing (NGS or Sanger):
- Use sequencing to resolve discrepancies or confirm all positive results from mPCR and culture.
- For Sanger sequencing, purify PCR products (e.g., using exonuclease I and shrimp alkaline phosphatase), then sequence with a cycle sequencing kit [80].
- Analyze sequences using the Basic Local Alignment Search Tool (BLAST) for pathogen identification [80]. Targeted NGS (tNGS) can also serve as a high-resolution reference [83].
Experimental Workflow and Data Analysis
The following diagram illustrates the logical workflow for a comprehensive clinical concordance study, from specimen collection to final data analysis.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of mPCR concordance studies relies on a suite of specialized reagents and tools. The table below details essential materials and their functions.
Table 2: Essential Research Reagents for mPCR Concordance Studies
| Research Reagent / Tool | Function / Application | Examples / Notes |
|---|---|---|
| Nucleic Acid Preservation Solution | Stabilizes DNA/RNA in clinical specimens immediately after collection, preventing degradation during transport and storage. | Often contains viral inactivators for biosafety [78]. |
| Total Nucleic Acid Extraction Kits | Simultaneously purifies DNA and RNA from diverse sample matrices; critical for detecting both viral and bacterial pathogens. | Easy Pure Viral DNA/RNA Kit; automated systems like MagNA Pure 96 enhance reproducibility [78] [79]. |
| TaqMan Probes & Primers | Provide high specificity in real-time mPCR assays by binding to unique pathogen gene sequences. Fluorescent labels allow multiplexing. | Designed against conserved, unique genes (e.g., lytA for S. pneumoniae, copB for M. catarrhalis) [83]. |
| PCR Master Mix with UNG | Contains enzymes, dNTPs, and buffers optimized for efficient amplification. Uracil-N-Glycosylase (UNG) prevents amplicon carryover contamination. | Includes dUTP in the reaction; essential for maintaining assay integrity in high-throughput settings [78]. |
| Fluorescent Dyes (e.g., EvaGreen) | A saturating dye that binds double-stranded DNA, enabling multiplex real-time PCR with melting curve analysis without the need for probes. | More cost-effective than probe-based assays; allows detection of more targets; requires careful optimization to avoid non-specific signals [79]. |
| Commercial Multiplex PCR Panels | Integrated, standardized tests for the simultaneous detection of numerous pathogens and antimicrobial resistance markers. | BioFire FilmArray Pneumonia Panel; Unyvero A50; useful as a benchmark or for labs developing their own assays [79] [82] [81]. |
The advancement of molecular diagnostics has positioned Multiplex PCR and Next-Generation Sequencing (NGS) as two pivotal technologies for genomic variant detection and pathogen surveillance. While multiplex PCR allows for the simultaneous, targeted detection of a predefined set of genetic markers with high sensitivity, NGS offers a broader, hypothesis-free approach capable of discovering novel variants and conducting comprehensive genomic analyses. Selecting the appropriate method hinges on the specific application requirements, including the need for discovery versus routine monitoring, resolution, cost, and turnaround time. This Application Note provides a detailed comparative analysis of these technologies, supported by experimental data and tailored protocols, to guide researchers and drug development professionals in optimizing their genomic surveillance strategies.
Performance and Diagnostic Accuracy Comparison
Quantitative Performance Metrics in Clinical Oncology
Direct comparisons in clinical settings reveal distinct performance profiles for each technology. The following table summarizes key findings from studies in metastatic breast cancer (MBC) and non-small cell lung cancer (NSCLC).
Table 1: Performance comparison of multiplex PCR and NGS in detecting genomic variants in cancer.
| Metric | Multiplex PCR | Targeted NGS | Context and Notes |
|---|---|---|---|
| Overall Concordance | Benchmark | 95% (90/95) [84] | Compared to multiplex dPCR for ERBB2, ESR1, PIK3CA in MBC plasma [84] |
| Correlation (R²) | Benchmark | 0.9786 [84] | For mutant allele frequencies in MBC [84] |
| Success Rate | 100% [85] [86] | 98% [85] [86] | On lung cancer biopsy samples [85] [86] |
| Detection Rate | 35.9% [85] [86] | 37.3% [85] [86] | Proportion of NSCLC samples with a driver mutation detected [85] [86] |
| Sensitivity (Pooled) | 62.2% [87] | 88.6% [87] | For bacterial detection in prosthetic joint infections (mPCR vs. mNGS) [87] |
| Specificity (Pooled) | 96.2% [87] | 93.2% [87] | For bacterial detection in prosthetic joint infections (mPCR vs. mNGS) [87] |
| Key Strengths | High sensitivity for low-frequency variants; Rapid turnaround [84] | Discovery of novel/atypical variants; Multigene analysis [84] |
Operational and Economic Considerations
Beyond analytical performance, operational factors are critical for platform selection. A cost-effectiveness analysis in Spanish reference centers for NSCLC demonstrated that despite higher initial costs, NGS was a cost-effective strategy compared to single-gene testing (including multiplex PCR), with an incremental cost-utility ratio of €25,895 per Quality-Adjusted Life-Year (QALY) gained. This was driven by the detection of more actionable alterations, leading to better-targeted therapies and improved patient outcomes [88].
Table 2: Operational characteristics of multiplex PCR versus NGS.
| Characteristic | Multiplex PCR | Targeted NGS |
|---|---|---|
| Typical Turnaround Time | Faster (e.g., 12-14 hours for pneumonia diagnosis) [89] | Slower (e.g., 48+ hours including library prep and bioinformatics) [88] |
| Multiplexing Capacity | Moderate (dozens of targets) | High (hundreds to thousands of targets) |
| Variant Discovery | Limited to predefined variants | Excellent for novel variant discovery [84] |
| Cost per Sample | Lower | Higher, but cost-effective in comprehensive genomic profiling [88] |
| Handling of Low-Quality/Quantity Samples | Robust performance reported [85] [90] | Requires sufficient DNA/RNA quality and quantity [85] |
| Workflow & Infrastructure | Standard molecular biology lab; simpler bioinformatics | Specialized equipment and extensive bioinformatics support required [91] |
Experimental Protocols
Protocol A: Multiplex PCR for Liquid Biopsy Analysis in Metastatic Breast Cancer
This protocol is adapted from a study comparing multiplex digital PCR (dPCR) with targeted NGS for detecting mutations in plasma circulating tumor DNA (ctDNA) [84].
1. Principle: Multiplex dPCR assays are designed to simultaneously detect specific hotspot mutations in genes like ESR1 and PIK3CA. The "drop-off" system allows for the detection of mutations within a specific region by using a probe that binds to the wild-type sequence; the absence of signal indicates a potential mutation, which is then confirmed with specific probes [84].
2. Reagents:
- Plasma samples from patients.
- cfDNA extraction kit (e.g., QIAamp Circulating Nucleic Acid Kit).
- Multiplex dPCR assay mix (containing mutation-specific and drop-off probes).
- dPCR Supermix for Probes (Bio-Rad or Thermo Fisher).
- Droplet generation oil.
3. Procedure:
- cfDNA Extraction: Extract cell-free DNA from 2-4 mL of plasma using a commercial kit. Elute in a low TE buffer.
- Assay Preparation:
- Prepare a 20 µL reaction mix containing 1X dPCR Supermix, the multiplexed primer/probe assay, and approximately 5-20 ng of cfDNA.
- The multiplex assay for ESR1 may include a drop-off probe covering codons 536-538 and a specific probe for the p.D538G mutation [84].
- Droplet Generation: Transfer the reaction mix to a droplet generator cartridge along with 70 µL of droplet generation oil. Generate droplets.
- PCR Amplification:
- Transfer the emulsified droplets to a 96-well PCR plate.
- Seal the plate and run the PCR on a thermal cycler with the following conditions:
- Enzyme activation: 95°C for 10 minutes.
- 40-45 cycles of: Denaturation at 94°C for 30 seconds, Annealing/Extension at 55-60°C for 60 seconds.
- Enzyme deactivation: 98°C for 10 minutes.
- Hold at 4°C.
- Droplet Reading: Read the plate on a droplet reader. Analyze the data using the manufacturer's software to determine the mutant allele frequency (MAF) for each target.
Protocol B: Targeted NGS for Comprehensive Variant Profiling from Liquid Biopsy
This protocol utilizes a commercially targeted NGS panel, such as the Plasma-SeqSensei BREAST Cancer CA assay, for the sensitive detection of somatic mutations across multiple genes [84].
1. Principle: Targeted NGS uses a multiplex PCR approach to amplify regions of interest from cfDNA, followed by high-throughput sequencing. This allows for the simultaneous detection of a wide spectrum of mutations across several genes, including single nucleotide variants (SNVs) and insertions/deletions (indels).
2. Reagents:
- Purified cfDNA (as in Protocol A, step 1).
- Targeted NGS Panel (e.g., PSS BC NGS Assay, Sysmex Inostics).
- Library Preparation Master Mix.
- Barcoding Adapters.
- Solid-phase reversible immobilization (SPRI) beads.
- Sequencing Kit (e.g., for Illumina NextSeq 500).
3. Procedure:
- Library Preparation:
- Amplify 4-43 ng of input cfDNA using the targeted NGS panel, which contains multiple primer pairs designed to amplify mutational hotspots in genes like ERBB2, ESR1, and PIK3CA.
- The initial amplification is typically performed on a thermal cycler with a program optimized for the specific panel.
- Indexing and Barcoding: Add sample-specific barcodes (indexes) to the amplified products via a second, limited-cycle PCR. This enables the multiplexing of multiple samples in a single sequencing run.
- Library Purification: Clean up the final library using SPRI beads to remove primers, dimers, and other contaminants.
- Library Quantification: Quantify the purified library using a fluorometric method (e.g., Qubit) and assess the size distribution with a bioanalyzer or tape station.
- Sequencing: Pool the barcoded libraries at equimolar concentrations and load onto a sequencer (e.g., Illumina NextSeq 500) for sequencing with a 2x150 bp paired-end run.
- Bioinformatic Analysis:
- Demultiplexing: Assign reads to individual samples based on their unique barcodes.
- Alignment: Map sequencing reads to the human reference genome (e.g., hg19).
- Variant Calling: Use specialized algorithms (e.g., MuTect, VarScan2) to identify somatic mutations relative to the reference and filter out technical artifacts.
- Annotation: Annotate called variants for functional impact and population frequency.
Technology Selection Workflows
The choice between multiplex PCR and NGS depends on the clinical or research question. The following diagram illustrates the decision-making pathway.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogs essential reagents and kits cited in the referenced studies for implementing the described protocols.
Table 3: Key research reagents and kits for multiplex PCR and NGS applications.
| Reagent/Kits | Function/Application | Specific Example/Note |
|---|---|---|
| AmoyDx Pan Lung Cancer PCR Panel | Multiplex PCR-based detection of 9 driver mutations in NSCLC [85] [86] | Designed for real-time PCR; covers EGFR, ALK, ROS1, KRAS, BRAF, MET, RET, HER2, NTRK [85] [86]. |
| Plasma-SeqSensei Breast Cancer NGS Assay | Targeted NGS for somatic mutations in liquid biopsy [84] | Ready-to-use panel for ERBB2, ESR1, PIK3CA; demonstrated high concordance with dPCR [84]. |
| Oncomine Dx Target Test (ODxTT-M) | Targeted NGS panel for solid tumors (NSCLC) [85] [86] | Covers 46 cancer-related genes; requires sufficient nucleic acid quality and tumor content (≥30%) [85]. |
| Custom Multiplex dPCR Assays | Ultrasensitive quantification of specific mutations in liquid biopsy [84] | Often require in-house development and validation; use "drop-off" systems for mutation clusters [84]. |
| Ion PGM / Illumina Systems | Next-generation sequencing platforms | Used for high-throughput sequencing of NGS libraries [91] [90]. |
| SPRI Beads | Solid-phase reversible immobilization for NGS library purification | Used for size selection and clean-up of NGS libraries post-amplification. |
Multiplex PCR and NGS are complementary, not competing, technologies in the modern molecular laboratory. Multiplex PCR is the tool of choice for rapid, sensitive, and cost-effective monitoring of a predefined set of targets, making it ideal for high-throughput routine screening and minimal residual disease detection. In contrast, NGS provides an unparalleled breadth of analysis, enabling comprehensive genomic profiling, discovery of novel variants, and hypothesis-free exploration in pathogen surveillance and oncology. The decision framework and detailed protocols provided herein empower researchers to make an informed selection based on their specific application, ensuring optimal resource utilization and scientific rigor.
Within high-resolution subtyping research, the adoption of multiplex PCR assays represents a paradigm shift, enabling the simultaneous interrogation of numerous pathogenic or genetic targets. The core value proposition of this technology lies in its profound impact on key operational parameters: it drastically reduces assay turnaround time, significantly increases laboratory throughput, and optimizes the consumption of valuable resources. This application note provides a detailed, data-driven cost-benefit analysis to guide researchers and drug development professionals in the strategic implementation of these assays. The quantitative data and protocols herein are framed to support informed decision-making for research programs requiring precise pathogen or genetic variant subtyping.
Quantitative System Comparison
The selection of a multiplex PCR system is contingent upon the specific throughput and turnaround time requirements of the research or diagnostic laboratory. The table below summarizes the performance characteristics of several established and emerging multiplex technologies, illustrating the trade-offs between speed, multiplexing capacity, and operational complexity.
Table 1: Performance Comparison of Multiplex PCR Technologies
| Test System | Pathogens/Targets Detected | Degree of Multiplexity | Time for Result (Hours) | Throughput | Testing Location | Integrated System |
|---|---|---|---|---|---|---|
| FilmArray [92] | Viruses and Bacteria | >15 targets | ~1 | Low | Near-patient facility and/or laboratory | Yes |
| Jaguar [92] | Viruses | 2–6 targets | 1.5–2 | Moderate | Near-patient facility and/or laboratory | Yes |
| RespPlex [92] | Viruses and Bacteria | >15 targets | 5-6 | Moderate to High | Laboratory | No |
| Infiniti [92] | Viruses | >15 targets | 6.5–10 | Moderate to High | Laboratory | No |
| PLEX-ID [92] | Viruses and Bacteria | >15 targets | 6-8 | Moderate to High | Laboratory | No |
| BioCode MDx-3000 [93] | Syndromic Panels | Up to 3 panels in parallel | N/S | 188 samples per 8-hour shift | Laboratory | N/S |
| cobas liat [94] | Respiratory/STI Panels | Multiple targets | ~0.33 (20 mins) | N/S | Point of Care | Yes |
Abbreviation: N/S, Not Specified in the source material.
Experimental Protocols for Multiplex Assays
Protocol 1: Multiplex Real-Time PCR with Melt-Curve Analysis for Viral Detection
This protocol details a method for simultaneous detection and differentiation of multiple viruses using a SYBR Green-based multiplex real-time PCR assay, adapted from a study detecting HCV, HIV-1, and HHpgV-1 [53]. It is ideal for co-infection studies and blood-borne pathogen screening.
Sample Preparation and Nucleic Acid Extraction:
- Collect serum samples and extract RNA using a commercial kit (e.g., QIAamp Viral RNA Mini Kit, Qiagen) under RNase-free conditions.
- Synthesize cDNA from the extracted RNA using a reverse transcription kit (e.g., RevertAid First Strand cDNA Synthesis Kit, Thermo Scientific). Store cDNA at -20°C.
Primer Design Criteria:
- Retrieve multiple sequences for each target virus from GenBank and align them to identify conserved regions (e.g., 5' UTR).
- Design primers with similar melting temperatures (Tm), typically between 59–62°C.
- Ensure amplicon lengths are distinct enough to be resolved by melt-curve analysis (e.g., 84 bp, 94 bp, 133 bp).
- Verify primer specificity in silico using BLAST and check for dimers or secondary structures using software like GeneRunner.
Multiplex Real-Time PCR Reaction Setup:
- Reaction Mix: 12.5 µL of SYBR Green master mix (containing buffer, dNTPs, MgCl₂, and hot-start Taq polymerase), 0.25–0.4 µM of each primer pair, and 5 µL of cDNA template. Adjust the final volume to 25 µL with nuclease-free water.
- Cycling Conditions:
- PCR Activation: 95°C for 15 minutes.
- Amplification (45 cycles): Denature at 95°C for 30 seconds, anneal at 57°C for 35 seconds, and extend at 72°C for 35 seconds.
- Melt-Curve Analysis: Perform immediately after amplification to distinguish amplicons based on their unique melting temperatures (Tm).
Analysis and Validation:
- Generate standard curves using serially diluted plasmids (e.g., 10⁶ to 10¹ copies/mL) to determine the limit of detection (LOD) and enable quantification.
- Validate assay specificity by testing against other common pathogens to rule out cross-reactivity.
Protocol 2: Highly Multiplexed PCR Primer Design Using SADDLE
For research applications requiring massive multiplexing, such as targeted sequencing for genetic subtyping, the SADDLE algorithm enables the design of primer sets with minimal dimer formation [37].
Primer Candidate Generation:
- Identify "pivot" nucleotides in the genomic sequence that must be included in the amplicon.
- Generate "proto-primers" with 3' ends flanking the pivot. Systematically truncate these from the 3' end until the calculated standard free energy (ΔG°) of binding is between -10.5 and -12.5 kcal/mol.
- Apply filters to remove candidates with GC content <25% or >75%.
Stochastic Primer Set Optimization:
- Initialization: Randomly select one primer pair candidate for each target to form an initial set, S₀.
- Loss Function Evaluation: Calculate the total "Badness" score L(S) for the set, which sums the potential for dimer formation between every possible pair of primers.
- Simulated Annealing:
- Generate a new temporary primer set (T) by randomly swapping one or more primers with other candidates from the pool.
- Compute L(T). If L(T) < L(Sg), accept the new set. If L(T) is worse, accept it with a probability that decreases over "generations" to escape local minima.
- Repeat for thousands of iterations to converge on a final, optimized primer set S_final with minimal dimer potential.
Experimental Validation:
- The optimized primer set can be used for next-generation sequencing (NGS) library preparation or in a single-tube qPCR assay, as demonstrated for the detection of 56 gene fusions in lung cancer [37].
Workflow and Logical Diagrams
The following diagram illustrates the core operational logic and workflow optimization achieved by implementing a multiplex PCR system, compared to traditional singleplex testing.
Diagram 1: Workflow comparison of singleplex versus multiplex testing.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of the protocols described above relies on key reagents and instruments. The following table details essential materials and their functions in a multiplex PCR workflow for subtyping research.
Table 2: Key Research Reagent Solutions for Multiplex PCR Assays
| Item | Function/Application | Example Use Case/Note |
|---|---|---|
| Hot-Start Taq DNA Polymerase [7] | Reduces non-specific amplification and primer-dimer formation by requiring heat activation. | Critical for improving specificity in complex multiplex reactions. |
| SYBR Green Master Mix [53] | Intercalating dye for real-time PCR amplification and subsequent melt-curve analysis. | Enables cost-effective multiplexing with Tm-based target differentiation. |
| Barcoded Magnetic Beads (BMB) [93] | Solid-phase support for post-PCR hybridization, allowing highly multiplexed detection. | Used in systems like BioCode for digital encoding and target capture. |
| Primer Design Software | Computational tool for generating and evaluating primer candidates against multiple parameters. | Essential for implementing algorithms like SADDLE to minimize primer dimers [37]. |
| Automated Nucleic Acid Extractor | Standardizes and accelerates the isolation of DNA/RNA from clinical samples. | Improves throughput and reduces hands-on time for sample preparation. |
| Batch Panel Testing System [93] | Instrument that automates amplification, capture, and detection for multiple samples. | Enables high walk-away time (e.g., 3.5 hours) and running multiple panels in parallel. |
The strategic integration of multiplex PCR assays into high-resolution subtyring research pipelines offers a compelling cost-benefit profile. The quantitative data and detailed protocols provided demonstrate that this technology directly addresses the core challenges of modern laboratories by delivering faster results, higher sample throughput, and more efficient utilization of reagents and personnel. By carefully selecting the appropriate system and optimization strategies, researchers and drug developers can significantly accelerate the pace of discovery and diagnostics while maintaining rigorous scientific standards.
Conclusion
Multiplex PCR for high-resolution subtyping has emerged as a powerful, accessible, and cost-effective technology that bridges the gap between single-pathogen tests and more complex whole-genome sequencing. By enabling the simultaneous detection and precise characterization of multiple pathogen strains or variants in a single reaction, it provides critical insights for epidemiology, drug development, and clinical management. Future directions will likely involve integration with portable platforms for point-of-care use, expansion of panels to include emerging variants and resistance markers, and the development of standardized bioinformatic tools for in silico subtyping. As the demand for precise pathogen surveillance grows, these refined multiplex assays will play an increasingly vital role in global health security and personalized medicine.
References
- 1. Comprehensive Assessment of Subtyping Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9602514/]
- 2. High-resolution melting real-time polymerase chain ... [https://www.sciencedirect.com/science/article/pii/S0022030224005691]
- 3. Multiplex PCR for Typing and Subtyping Influenza and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC105099/]
- 4. A real-time PCR approach for rapid high resolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1899167/]
- 5. Multiplex Dual-Target Reverse Transcription PCR for ... [https://wwwnc.cdc.gov/eid/article/30/8/24-0785_article]
- 6. Conducting a Field Investigation | Field Epi Manual [https://www.cdc.gov/field-epi-manual/php/chapters/field-investigation.html]
- 7. Multiplex PCR: Optimization and Application in Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC88949/]
- 8. Pan- genome analysis reveals novel chromosomal markers ... for [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-09817-9]
- 9. A multiplex real-time PCR virulence and resistance... assay targeting [https://pmc.ncbi.nlm.nih.gov/articles/PMC3150258/]
- 10. One-step multiplex RT-qPCR for the detection and ... [https://www.sciencedirect.com/science/article/abs/pii/S0166093419300552]
- 11. Five tips on how to design your first or 15th dPCR multiplex ... [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/science-matters/pcr-solutions/five-tips-on-how-to-design-your-first-or-15th-dpcr-multiplex-assay]
- 12. Multiplex Assays Market Size to Hit USD 6.75 Billion by 2034 [https://www.precedenceresearch.com/multiplex-assays-market]
- 13. Evolution of Multiplex PCR: Benefits, Challenges & Key ... [https://www.eurogentec.com/en/news/111_evolution-of-multiplex-pcr-benefits-challenges-key-applications]
- 14. Multiplexed, universal probe-based rare variant detection ... [https://www.nature.com/articles/s41598-025-08814-5]
- 15. MPSeqM, a tool combining multiplex PCR and high ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-03855-2]
- 16. Multiplex vs. Singleplex qPCR: What Do I Need To Know? [https://www.thermofisher.com/blog/behindthebench/multiplex-vs-singleplex-qpcr-what-do-i-need-to-know/]
- 17. Optimized multiplex PCR-NGS for comprehensive HLA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12240775/]
- 18. Multiplex vs. singleplex assay for the simultaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11927560/]
- 19. Multiplex PCR Assay Market CAGR, Segments and ... [https://www.towardshealthcare.com/insights/multiplex-pcr-assay-market-sizing]
- 20. PCR-based Microbial Antibiotic Resistance Gene Analysis [https://www.cd-genomics.com/microbioseq/pcr-based-microbial-antibiotic-resistance-gene-analysis.html]
- 21. 4-Gene Standard Uniplex PCR Protocol for Antibiotic ... [https://www.protocols.io/view/4-gene-standard-uniplex-pcr-protocol-for-antibioti-dne85bhw.html]
- 22. Quantitative PCR versus metagenomics for monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10117749/]
- 23. Novel multiplex family-wide PCR and Nanopore sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535105/]
- 24. Multiplex metagenomic sequencing for rapid viral pathogen ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11952-w]
- 25. A novel XbaI multiplex PCR method for rapid typing of ... [https://www.nature.com/articles/s41598-025-99308-x]
- 26. Microbial DNA Typing by Automated Repetitive-Sequence- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC540112/]
- 27. Rapid plasmid replicon typing by real time PCR melting curve ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/1471-2180-13-83]
- 28. Development and Validation of a Multi-Locus PCR-HRM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8391999/]
- 29. A novel multiplex qPCR‑HRM assay for the simultaneous ... [https://www.nature.com/articles/s41598-023-39447-1]
- 30. Multiplex high resolution melt-curve real-time PCR assay ... [https://www.sciencedirect.com/science/article/abs/pii/S0956713518301506]
- 31. Multiplex high-resolution melting assay for simultaneous ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.1049178/full]
- 32. Real-time RT-PCR high-resolution melting curve analysis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3519601/]
- 33. Optimization of the real-time PCR platform method using ... [https://www.nature.com/articles/s41598-025-16972-9]
- 34. What is multiplex PCR? [https://frontlinegenomics.com/what-is-multiplex-pcr/]
- 35. An overview of multiplex PCR assay, primer design ... [http://www.premierbiosoft.com/tech_notes/multiplex-pcr.html]
- 36. Multiplex polymerase chain reaction: a practical approach [https://pubmed.ncbi.nlm.nih.gov/11835531/]
- 37. Designing highly multiplex PCR primer sets with Simulated ... [https://www.nature.com/articles/s41467-022-29500-4]
- 38. Multiplex primer design [https://primerdigital.com/fastpcr/m12.html]
- 39. Development and optimization of multiplex PCR for rapid ... [https://www.sciencedirect.com/science/article/abs/pii/S1045105625000156]
- 40. What is multiplex qPCR? [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/what-is-multiplex-qpcr.html]
- 41. Development and clinical validation of a novel multiplex ... [https://www.nature.com/articles/s41598-025-16434-2]
- 42. A Rapid Multiplex Real-Time PCR High-Resolution Melt ... [https://www.sciencedirect.com/science/article/pii/S0362028X22077122]
- 43. High-resolution melting real-time polymerase chain ... [https://pubmed.ncbi.nlm.nih.gov/38490558/]
- 44. High-resolution melting real-time PCR assays for subtyping ... [https://scispace.com/papers/high-resolution-melting-real-time-pcr-assays-for-subtyping-4lcinmubll]
- 45. Development and validation of high-resolution melting ... [https://www.sciencedirect.com/science/article/abs/pii/S0956713522002882]
- 46. Escherichia coli ST131, an Intriguing Clonal Group - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4135899/]
- 47. Population dynamics of an Escherichia coli ST131 lineage ... [https://www.nature.com/articles/s41467-019-11571-5]
- 48. Novel Multiplex PCR Method and Genome Sequence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9241916/]
- 49. Novel Multiplex PCR Method and Genome Sequence ... [https://pubmed.ncbi.nlm.nih.gov/35604132/]
- 50. Digital PCR: from early developments to its future application ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00055f]
- 51. Multiplex digital PCR enables sensitive detection of ... [https://pubmed.ncbi.nlm.nih.gov/39849159/]
- 52. Highly multiplexed digital PCR assay for simultaneous ... [https://pubmed.ncbi.nlm.nih.gov/40077847/]
- 53. Design and optimization of a multiplex real-time PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535783/]
- 54. Digital PCR Market Opportunities Growing for Legacy ... [https://www.genomeweb.com/pcr/digital-pcr-market-opportunities-growing-legacy-developers-amid-emerging-competition-asia]
- 55. Top Companies Shaping the Digital PCR dPCR Industry ... [https://www.intellectualmarketinsights.com/blogs/top-companies-shaping-the-digital-pcr-dpcr-industry-in-2025]
- 56. Overcoming the challenge of primer-dimers in multiplexed ... [https://blog.biosearchtech.com/overcoming-the-challenge-of-primer-dimers-in-multiplexed-pcr-assays]
- 57. Multiplex PCR assay for the rapid detection of Klebsiella ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578128/]
- 58. Appendix Q: Recommendations for Developing Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8370429/]
- 59. How to Avoid False-Negative and False-Positive COVID-19 ... [https://www.mdpi.com/2673-8937/2/2/18]
- 60. Development of a novel strategy to reduce diagnostic ... [https://www.nature.com/articles/s41598-024-78654-2]
- 61. The Four Most Common Problems in Multiplex pcr Design [https://www.dnasoftware.com/common-problems-in-multiplex-panel-design/]
- 62. An optimized protocol for stepwise optimization of real-time ... [https://www.nature.com/articles/s41438-021-00616-w]
- 63. Primer Pool Design Strategies for Multiplex PCR Success [https://www.dynegene.com/en/detail-416.html]
- 64. Optimization of the viability PCR for accurate detection of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0324819]
- 65. Optimization and validation of a consolidated Set ... [https://www.sciencedirect.com/science/article/pii/S2215016125004443]
- 66. Advances in multiplex PCR: balancing primer efficiencies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3573865/]
- 67. Optimization and evaluation of a multiplex PCR assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9944222/]
- 68. Optimization of Annealing Temperature and other PCR ... [https://www.genaxxon.com/shop/en/blog/optimization-of-annealing-temperature-and-other-pcr-parameters]
- 69. Development and clinical validation of a novel multiplex ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368015/]
- 70. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 71. rtpcr: a package for statistical analysis and graphical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530193/]
- 72. Development and validation of a multiplex PCR assay with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12216036/]
- 73. Development and validation of a multiplex qPCR method for ... [https://infectagentscancer.biomedcentral.com/articles/10.1186/s13027-024-00633-z]
- 74. Performance of three multiplex real-time PCR assays for ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2024.1421427/full]
- 75. Technical validation of a multiplex real-time PCR for ... [https://www.sciencedirect.com/science/article/pii/S0166093425000679]
- 76. Optimizing PCR Reaction Conditions for High Fidelity and ... [https://www.labx.com/resources/optimizing-pcr-reaction-conditions-for-high-fidelity-and-yield/5579]
- 77. PCR Optimization: Factors Affecting Reaction Specificity ... [https://www.mybiosource.com/learn/pcr-optimization-factors-affecting-reaction-specificity-and-efficien/]
- 78. Clinical Evaluation of a Multiplex PCR Assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9862116/]
- 79. Development and validation of multiplex real-time PCR for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10848345/]
- 80. Comparison of two multiplex PCR assays for the detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7162222/]
- 81. Pathogen detection by multiplex PCR: A comparative study ... [https://www.sciencedirect.com/science/article/pii/S2212534525001212]
- 82. Diagnostic accuracy of multiplex polymerase chain ... [https://www.nature.com/articles/s41598-021-99076-4]
- 83. Methodological establishment and diagnostic value of a ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0328651]
- 84. Comparative performance of a targeted next-generation ... [https://www.sciencedirect.com/science/article/abs/pii/S1525157825002375]
- 85. Comparison between next‐generation sequencing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10993699/]
- 86. Comparison between next-generation sequencing and ... [https://pubmed.ncbi.nlm.nih.gov/38572952/]
- 87. Diagnostic accuracy of 16S rDNA PCR, multiplex PCR and ... [https://www.sciencedirect.com/science/article/pii/S1198743X25000837]
- 88. Cost-Effectiveness of Next-Generation Sequencing Versus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10309530/]
- 89. Rapid, season-specific PCR testing versus traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318422/]
- 90. Cost-efficient multiplex PCR for routine genotyping of up to ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-015-1514-4]
- 91. A comparison of high-throughput SARS-CoV-2 sequencing ... [https://www.nature.com/articles/s41598-022-16549-w]
- 92. Multiplex PCR and Emerging Technologies for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7107927/]
- 93. A Guide to Sample Throughput for Labs [https://www.apbiocode.com/sample-throughput/]
- 94. Multiplexing technology for efficiency [https://diagnostics.roche.com/global/en/article-listing/diagnostics-insights/multiplex-testing-efficiency-efficacy.html]