Evolutionary Arms Race: Comparative Mechanisms of Toxin Resistance in Prokaryotes and Eukaryotes
This review provides a systematic comparison of the fundamental and applied aspects of toxin resistance mechanisms across the prokaryotic and eukaryotic domains.
Evolutionary Arms Race: Comparative Mechanisms of Toxin Resistance in Prokaryotes and Eukaryotes
Abstract
This review provides a systematic comparison of the fundamental and applied aspects of toxin resistance mechanisms across the prokaryotic and eukaryotic domains. We explore the foundational principles, from enzymatic inactivation and efflux pumps in bacteria to target-site insensitivity and immune responses in complex organisms. The article assesses modern methodological approaches for studying these systems, including in silico analyses and database resources, and addresses key challenges such as antimicrobial resistance (AMR). By validating and contrasting these divergent evolutionary strategies, we highlight their direct implications for overcoming current bottlenecks in drug development, offering a roadmap for novel therapeutic and biotechnological applications.
Core Defense Strategies: From Bacterial Enzymes to Eukaryotic Target-Site Mutations
In the continuous struggle for survival, organisms across all kingdoms of life produce a diverse arsenal of natural toxins. These compounds serve as key mediators of interference competition, defense, and pathogenesis by targeting fundamental cellular processes. The evolutionary arms race between toxin producers and their intended targets has shaped intricate resistance mechanisms at the molecular level. This comparative analysis examines the cellular targets of natural toxins and the corresponding resistance strategies evolved by prokaryotic and eukaryotic organisms, providing a framework for understanding these ancient biological battles and their applications in drug development and biotechnology.
Classification and Mechanisms of Natural Toxins
Natural toxins can be systematically categorized based on their origin, chemical structure, and molecular mechanisms of action. The following sections provide a detailed overview of the major toxin classes and their cellular targets.
Bacterial Toxins: Precision Molecular Weapons
Bacterial toxins represent sophisticated weaponry developed through evolutionary time to disrupt cellular function. They are broadly classified into pore-forming toxins and toxins with enzymatic activity, each employing distinct strategies to compromise target cells.
Pore-Forming Toxins disrupt cellular integrity by creating pores in the plasma membrane of target cells. Water-soluble monomers released by pathogenic bacteria bind to specific cellular receptors (lipids, glycolipids, glycoproteins, or proteins) and undergo oligomerization in the membrane [1]. This process is accompanied by remarkable conformational changes leading to the formation of water-filled pores, alteration of membrane potential, and eventual cell death due to ion imbalance and osmotic lysis [1]. Notable examples include:
- Cholesterol-Dependent Cytolysins (CDCs): These β-pore forming toxins, including streptolysin O and perfringolysin O, bind to cholesterol-rich membrane domains and create large pores ranging from 1-100 nm in diameter [1].
- Cytolysin A (ClyA): An α-pore-forming toxin produced by Escherichia coli and Salmonella enterica that forms pores via membrane-spanning α-helices [1].
Toxins with Enzymatic Activity function as precision tools that enter target cells and modify specific intracellular components. Their enzymatic activities are diverse and highly specific:
- ADP-Ribosyltransferases (e.g., Cholera toxin, Pertussis toxin, Diphtheria toxin) modify target proteins by transferring ADP-ribose groups, altering their function [1].
- Proteases (e.g., Botulinum neurotoxin, Anthrax Lethal Factor) cleave specific cellular proteins essential for neuronal function or signaling pathways [1].
- Adenylyl Cyclases (e.g., Anthrax Edema Factor, Bordetella pertussis CyaA) dramatically increase intracellular cAMP levels, disrupting cellular signaling [1].
- Glycosyltransferases (e.g., Clostridioides difficile Toxins A and B) modify Rho GTPases through glucosylation, disrupting cytoskeletal organization [1].
- Deamidases (e.g., Cytotoxic necrotizing factors from E. coli) deamidate Rho GTPases, leading to constitutive activation and cellular dysfunction [1].
Table 1: Major Bacterial Toxin Classes and Their Mechanisms of Action
| Toxin Class | Representative Examples | Bacterial Source | Molecular Target | Enzymatic Activity |
|---|---|---|---|---|
| Pore-forming | Streptolysin O, Perfringolysin O | Streptococcus pyogenes, Clostridium perfringens | Plasma membrane cholesterol | Forms membrane pores (25-30 nm diameter) |
| ADP-Ribosyltransferases | Cholera toxin, Diphtheria toxin | Vibrio cholerae, Corynebacterium diphtheriae | G-proteins, Elongation Factor 2 | NAD-dependent ADP-ribosylation |
| Proteases | Botulinum neurotoxin, Anthrax Lethal Factor | Clostridium botulinum, Bacillus anthracis | SNARE proteins, MAPKKs | Zinc-dependent metalloprotease |
| Adenylyl Cyclases | Edema Factor, CyaA | Bacillus anthracis, Bordetella pertussis | intracellular ATP | Calcium/calmodulin-dependent adenylate cyclase |
| Glycosyltransferases | Toxin A, Toxin B | Clostridioides difficile | Rho GTPases | UDP-glucose-dependent glycosyltransferase |
| Deamidases | Cytotoxic necrotizing factor | Escherichia coli | Rho GTPases | Glutamine deamidation |
Plant Toxins: Diverse Chemical Defenses
Plants have evolved numerous toxic proteins as defense mechanisms against herbivores, insects, and pathogens. These compounds target essential biological processes and represent powerful chemical deterrents [2].
Ribosome-Inactivating Proteins (RIPs) are cytotoxic enzymes that inhibit protein synthesis by catalytically inactivating ribosomes. They are classified into three types based on their structure:
- Type I RIPs (e.g., pokeweed antiviral protein, trichosanthin, saporin) are single-chain proteins of approximately 30 kDa with RNA N-glycosidase activity [2].
- Type II RIPs (e.g., ricin, abrin) consist of an enzymatic A-chain and a lectin-like B-chain that facilitates cellular entry through binding to galactose residues on cell surfaces [2].
- Type III RIPs (e.g., maize b32) contain an N-terminal domain with glycosidase activity and a C-terminal domain of uncertain function [2].
The primary mechanism of RIP toxicity involves the enzymatic removal of a specific adenine residue (A-4324) from the 28S rRNA of the large ribosomal subunit, which inhibits the binding of elongation factors and consequently blocks protein synthesis [2]. Additionally, many RIPs exhibit polynucleotide adenine glycosylase (PAG) activity on various nucleic acid substrates and may possess other enzymatic activities including chitinase, lipase, and superoxide dismutase functions [2].
Other Plant Toxic Proteins include:
- Lectins: Carbohydrate-binding proteins that can agglutinate cells and disrupt cellular recognition.
- Protease Inhibitors: Interfere with digestive enzymes in herbivores.
- α-Amylase Inhibitors: Block carbohydrate digestion.
- Ureases and Arcelins: Exhibit insecticidal and defensive properties.
- Antimicrobial Peptides: Broad-spectrum defense molecules against microorganisms [2].
Trans-Kingdom Toxin Systems
Recent research has identified sophisticated toxin delivery systems that operate across kingdom boundaries. The Type VI Secretion System (T6SS) functions as a molecular syringe that injects effector proteins directly into both prokaryotic and eukaryotic target cells [3]. For example, Yersinia pseudotuberculosis secretes TseR, a trans-kingdom T6SS RNase effector that contains an Ntox44 domain and exhibits divalent cation-dependent RNase activity [3]. This effector preferentially cleaves single-stranded RNA and can mediate bacterial killing through both contact-dependent and contact-independent mechanisms, with OmpC facilitating its entry during contact-independent killing [3]. During infection, TseR alters the host gut microbiome and directly targets eukaryotic host cells, demonstrating how single toxin effectors can function across biological kingdoms [3].
Figure 1: Trans-kingdom toxin mechanism of T6SS RNase effector TseR in Yersinia pseudotuberculosis
Cellular Targets of Natural Toxins
Fundamental Processes as Toxin Targets
Natural toxins have evolved to target conserved cellular components and processes essential for life. The most critical targets include:
Protein Synthesis Machinery: Multiple toxins directly target the translation apparatus. RIPs depurinate specific adenine residues in the α-sarcin/ricin loop (α-SRL) of 28S rRNA, preventing elongation factor binding and inhibiting protein synthesis [2]. Diphtheria toxin ADP-ribosylates elongation factor 2 (EF-2), rendering it inactive and halting polypeptide chain elongation [1].
Membrane Integrity: Pore-forming toxins directly compromise the plasma membrane's barrier function by creating aqueous channels. The size of these pores varies significantly, with cholesterol-dependent cytolysins forming particularly large pores (25-30 nm) that allow uncontrolled passage of ions and small molecules [1].
Signal Transduction Pathways: Many bacterial toxins modulate key signaling molecules. Cytotoxic necrotizing factors (CNF1, CNF2, CNF3) from E. coli and CNFY from Yersinia pseudotuberculosis deamidate Rho GTPases, leading to constitutive activation and disruption of cytoskeletal dynamics [1]. Similarly, Pasteurella multocida toxin and Bordetella bronchiseptica dermonecrotic toxin target Rho GTPases through deamidation and transglutamination, respectively [1].
Ion Homeostasis: Plant-derived cardenolides from milkweed and foxglove target the sodium-potassium pump (Na+/K+-ATPase) in animal cells [4]. These compounds bind to a specific site on the pump protein, turning it off and disrupting the critical ion gradient necessary for numerous cellular functions, including neuronal transmission and muscle contraction [4].
Gene Expression: The newly discovered T6SS RNase effector TseR from Y. pseudotuberculosis targets RNA molecules in both bacterial and eukaryotic cells [3]. This divalent cation-dependent RNase preferentially cleaves single-stranded RNA, disrupting gene expression globally and mediating pathogenesis through alteration of the host gut microbiome [3].
Comparative Target Vulnerability
The essential nature of certain cellular processes makes them vulnerable targets for toxin action across biological systems. Protein synthesis, being universally essential and highly conserved, represents the most frequently targeted process. Membrane integrity represents another fundamental target, as all cells require intact membranes to maintain homeostasis. Signaling pathways show more kingdom-specific targeting, with eukaryotic-specific signaling components (e.g., heterotrimeric G proteins) being targeted by certain bacterial toxins, while conserved GTPases (Rho family) are targeted across kingdoms.
Table 2: Cellular Targets of Natural Toxins Across Biological Kingdoms
| Target Category | Specific Target | Toxin Examples | Producer Organisms | Effect on Target |
|---|---|---|---|---|
| Translation Machinery | 28S rRNA | Ricin, Abrin | Plants (Ricinus communis, Abrus precatorius) | Adenine depurination, inhibits EF binding |
| Elongation Factor 2 | Diphtheria toxin | Corynebacterium diphtheriae | ADP-ribosylation, inhibits function | |
| Membrane Integrity | Plasma membrane cholesterol | Streptolysin O, Perfringolysin O | Streptococcus pyogenes, Clostridium perfringens | Forms large pores (25-30 nm), osmotic lysis |
| General membrane lipids | Cytolysin A (ClyA) | Escherichia coli, Salmonella enterica | Forms α-helical pores, membrane disruption | |
| Signaling Molecules | Rho GTPases | Cytotoxic necrotizing factor, Toxin B | Escherichia coli, Clostridioides difficile | Deamidation/glucosylation, constitutive activation |
| G-proteins | Cholera toxin, Pertussis toxin | Vibrio cholerae, Bordetella pertussis | ADP-ribosylation, altered signaling | |
| MAP Kinase Kinases | Anthrax Lethal Factor | Bacillus anthracis | Proteolytic cleavage, disrupts signaling | |
| Ion Transport | Na+/K+ ATPase | Cardenolides | Plants (milkweed, foxglove) | Inhibits pump function, disrupts ion gradients |
| Gene Expression | Cellular RNA | TseR RNase effector | Yersinia pseudotuberculosis | RNA cleavage, disrupts gene expression |
Defense and Resistance Mechanisms
Prokaryotic Resistance Strategies
Bacteria have evolved sophisticated mechanisms to resist toxins from competitors and environmental challenges:
Toxin-Antitoxin (TA) Systems: These abundant genetic elements encode a toxin protein that inhibits cell growth and an antitoxin that counteracts the toxin [5]. The majority of toxins are enzymes that interfere with translation or DNA replication, but a wide variety of molecular activities and cellular targets have been described [5]. Antitoxins are proteins or RNAs that often control their cognate toxins through direct interactions and, in conjunction with other signaling elements, through transcriptional and translational regulation of TA module expression [5]. These systems function in post-segregational killing ("plasmid addiction"), abortive infection (bacteriophage immunity through altruistic suicide), and persister formation (antibiotic tolerance through dormancy) [5].
Second Messenger Signaling: Bacteria utilize various low-molecular-weight non-proteinaceous molecules, called alarmones or second messengers, to coordinate cellular responses to stress and toxin exposure [6]. These include:
- (p)ppGpp: The effector of the stringent response, activated upon nutrient limitation and various stresses, which reprograms cellular metabolism toward survival [6].
- c-di-GMP: Generally known to regulate bacterial lifestyle transition from motile to sedentary, biofilm formation, cell cycle, and virulence [6].
- c-di-AMP: Involved in potassium and cell wall homeostasis [6].
- cAMP: Governs carbon source utilization in Gram-negative bacteria through binding to the CRP regulator [6].
DNA Repair and Genomic Integrity: Bacteria maintain genome stability through control of DNA replication and repair processes, which is indispensable for maintaining cellular functions under toxin-induced stress [6].
Arsenic-Specific Resistance: Prokaryotes have evolved elaborate mechanisms for arsenic resistance involving dedicated pathways for detoxification and extrusion [7] [8]. These include:
- Arsenite extrusion via ArsB and ACR3 membrane transporters [7] [8].
- Arsenate reduction to arsenite by arsenate reductases (ArsC) [8].
- Arsenite methylation to less toxic forms by arsenite methyltransferases (ArsM) [7].
Eukaryotic Resistance Strategies
Eukaryotes have developed distinct countermeasures against natural toxins:
Target Site Insensitivity: Some herbivores evolve resistant versions of target proteins through mutations that prevent toxin binding while maintaining normal function [4]. For example, insects feeding on milkweed and foxglove plants make versions of the sodium-potassium pump with amino acid substitutions in the cardenolide-binding site, rendering them insensitive to these toxins while maintaining ion transport function [4].
Detoxification Enzymes: Eukaryotes employ specialized enzyme systems, particularly cytochrome P450 enzymes (CYPs), to metabolize and neutralize toxins [4]. These enzymes begin the process by which cells turn toxic compounds into harmless molecules that the body can use or excrete [4]. Most insects have a large collection of CYP genes (some over 150), each coding for proteins that interact with different sets of molecules [4].
Horizontal Gene Transfer: Some eukaryotes have acquired resistance genes from bacterial sources through horizontal gene transfer [9] [7]. For example, the alga Galdieria sulphuraria, which lives in highly acidic environments rich in arsenic, acquired the arsenic efflux protein ArsB through HGT from bacteria, facilitating niche adaptation [7]. Multiple transfers of arsenite methyltransferases (ArsM) have also increased arsenic tolerance in various eukaryotic lineages [7].
Vacuolar Sequestration: Plants and fungi can compartmentalize toxins away from sensitive cellular components. In response to arsenic exposure, both prokaryotes and higher plants reduce cytosolic arsenic concentration through transporters that operate either in arsenite extrusion out of cells or by sequestering arsenic into vacuoles [8].
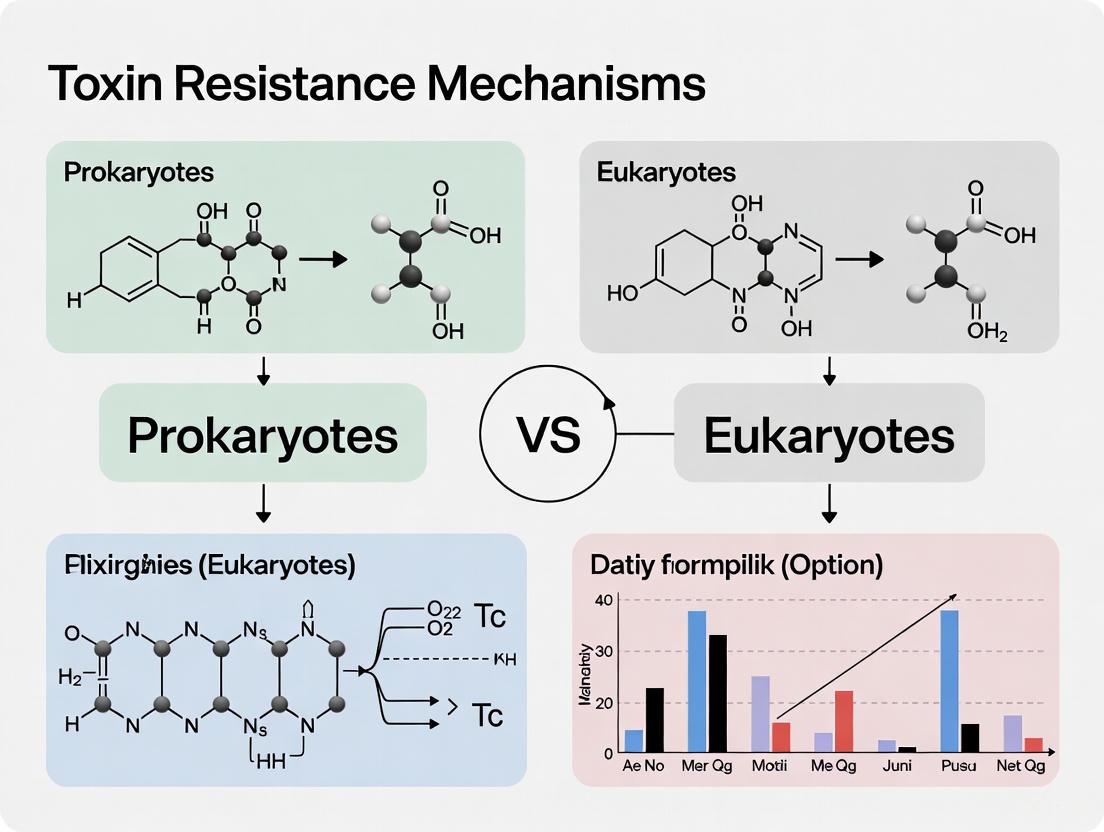
Figure 2: Comparative resistance mechanisms in prokaryotes and eukaryotes
Experimental Approaches and Methodologies
Key Experimental Protocols
Research on toxin mechanisms and resistance employs specialized methodologies:
Bacterial Competition Assays: For studying T6SS-mediated toxicity, researchers employ both contact-dependent and contact-independent competition assays [3]. In contact-dependent assays, donor and recipient bacterial strains are co-cultured on solid media for direct physical interaction, while contact-independent assays use culture supernatants or purified toxins added to recipient cultures, with OmpC facilitating toxin entry in some systems [3]. Viability is measured through colony-forming unit counts or fluorescent viability stains.
RNA-Seq Analysis of Toxin Targets: To identify global RNA targets of RNase effectors like TseR, researchers perform RNA sequencing on toxin-treated cells [3]. The protocol involves: (1) treatment of E. coli cultures with purified TseR effector, (2) RNA extraction at multiple time points, (3) library preparation and sequencing, (4) bioinformatic analysis to identify cleavage sites and preferential targets [3].
Membrane Permeabilization Measurements: Pore-forming toxin activity is quantified using black lipid membrane (BLM) experiments that determine biophysical properties including ion selectivity and channel size [1]. Additional methods include dye release assays from lipid vesicles, and measurement of ion flux in eukaryotic cells using patch-clamp electrophysiology [1].
Arsenic Resistance Phenotyping: Comprehensive assessment of arsenic tolerance involves growth assays under arsenic stress, measurement of intracellular arsenic accumulation via atomic absorption spectroscopy, and speciation analysis of arsenic compounds using HPLC-ICP-MS [7] [8].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Toxin Studies
| Reagent/Category | Specific Examples | Research Applications | Function in Experiments |
|---|---|---|---|
| Pore-Forming Toxins | Streptolysin O, Perfringolysin O | Membrane permeabilization studies | Creates controlled pores for intracellular delivery of small molecules, peptides, or drugs [1] |
| Engineered Toxin Systems | Modified Anthrax Protective Antigen | Targeted drug delivery | Engineered to recognize specific cell surface markers (e.g., EGFR, Her2) for cancer cell targeting [1] |
| Toxin Domains as Biosensors | Domain 4 of Perfringolysin O (PFO) | Cholesterol domain visualization | Binds specifically to cholesterol-rich membrane nanodomains for imaging [1] |
| Plant RIPs | Ricin, Abrin, Saporin | Ribosome function studies, anticancer research | Inhibits protein synthesis; studied for apoptotic effects on cancer cells [2] |
| Second Messenger Analogs | (p)ppGpp, c-di-GMP, cAMP | Bacterial stress response studies | Modulates transcriptional networks in bacterial homeostasis and stress response [6] |
| Detoxification Enzyme Assays | CYP enzyme substrates | Insecticide resistance research | Measures metabolic capability against plant toxins and synthetic pesticides [4] |
The comparative analysis of natural toxins and their cellular targets reveals fundamental principles of biological conflict and adaptation. The evolutionary arms race between toxin producers and target organisms has generated remarkable molecular diversity in both offensive weapons and defensive countermeasures. Understanding these intricate interactions provides valuable insights for therapeutic development, including the engineering of toxins for targeted cancer therapies [1] [10], the development of novel antibiotics targeting bacterial-specific systems [6], and strategies to overcome pesticide resistance in agriculture [4]. The continued study of these natural molecular battles will undoubtedly yield new tools for medicine and biotechnology while enhancing our understanding of fundamental biological processes across the kingdoms of life.
Prokaryotes have evolved a sophisticated arsenal of molecular mechanisms to manage toxins, including antibiotics, environmental stressors, and metabolic by-products. This guide provides a comparative assessment of three core mechanisms—enzymatic degradation, efflux pumps, and toxin-antitoxin (TA) systems—contrasting their operation in prokaryotic cells with the fundamentally different biology of eukaryotic cells. Understanding these mechanisms is critical for drug development, as they contribute significantly to bacterial pathogenicity and antibiotic resistance [11] [12]. For researchers, appreciating the distinct structural and functional biology of prokaryotes versus eukaryotes is the first step in designing targeted therapeutic strategies [13]. This comparison lays the groundwork for developing novel antibacterial agents that exploit unique prokaryotic pathways while minimizing off-target effects in human hosts.
Comparative Analysis of Core Resistance Mechanisms
The table below summarizes the key characteristics of the three primary toxin resistance mechanisms in prokaryotes, providing a direct comparison of their functions and components.
Table 1: Comparative Overview of Prokaryotic Toxin Resistance Mechanisms
| Mechanism | Primary Function | Key Components | Energy Source | Key Experimental Substrates/Assays |
|---|---|---|---|---|
| Enzymatic Degradation | Chemical modification or breakdown of toxic molecules [12] | Bacterial enzymes (e.g., β-lactamases) [12] | Chemical energy from reaction | Antibiotic susceptibility testing, HPLC/MS for degradation products [12] |
| Efflux Pumps | Active transport of toxins out of the cell [14] [15] | Membrane transport proteins (e.g., AcrB, TolC) [14] | Proton motive force or ATP [15] | Ethidium bromide accumulation assays, MIC determination with EPIs [14] |
| Toxin-Antitoxin Systems | Stress response, persistence formation, phage defense [11] [16] | Toxic protein and its cognate antitoxin (RNA or protein) [17] | N/A (Constitutive or stress-induced expression) | Bacterial two-hybrid assays, spot dilution assays, microscopy for persistence [17] [18] |
Mechanism 1: Enzymatic Degradation
Functional and Comparative Analysis
Enzymatic degradation involves the production of specific bacterial enzymes that inactivate toxic compounds, most notably antibiotics, through modification or hydrolysis [12]. A classic example is the production of β-lactamases, enzymes that hydrolyze the β-lactam ring of penicillin and related antibiotics, rendering them ineffective [12]. This mechanism is highly efficient and specific, but its major limitation is that each enzyme typically targets a single class or a limited range of antibiotic structures.
From a comparative perspective, this mechanism is largely unique to prokaryotes as a defense against antibiotics. While eukaryotes possess vast arrays of detoxifying enzymes (e.g., cytochrome P450 family), these generally target environmental toxins or metabolic waste and do not confer resistance to classical antibiotics. The fundamental difference lies in the targets: prokaryotic enzymes often directly attack the core chemical structure of synthetic or semi-synthetic antibacterial compounds, whereas eukaryotic detoxification systems are adapted to a different set of natural products and xenobiotics.
Experimental Protocols for Identification and Characterization
Protocol 1: Measuring Antibiotic Degradation Kinetics
- Culture the bacterial strain of interest to mid-log phase in an appropriate broth.
- Incubate a standardized inoculum with a known concentration of the antibiotic in a liquid medium.
- Sample the supernatant at regular intervals (e.g., 0, 30, 60, 120 minutes).
- Assay for remaining antibiotic activity using a bioassay with a susceptible indicator strain or via analytical methods like High-Performance Liquid Chromatography (HPLC) to detect the intact antibiotic and its breakdown products [12].
- Calculate the degradation rate based on the reduction of antibiotic concentration or activity over time.
Protocol 2: Confirmatory Disk Diffusion Assay for Enzyme Production
- Spread a lawn of a standardized, antibiotic-susceptible indicator strain on an agar plate.
- Place an antibiotic-impregnated disk in the center.
- Apply the bacterial culture supernatant or a purified enzyme preparation adjacent to the disk.
- Incubate and observe for a distortion or indentation in the zone of inhibition around the disk, indicating enzymatic inactivation of the antibiotic diffusing from the disk [12].
Mechanism 2: Multidrug Efflux Pumps
Functional, Structural, and Comparative Analysis
Multidrug efflux pumps are membrane-spanning transporter proteins that actively export a wide range of structurally unrelated toxic compounds from the bacterial cell, thereby reducing the intracellular concentration to sub-lethal levels [14] [15]. These pumps are major contributors to intrinsic and acquired multidrug resistance (MDR) in bacteria. They are classified into several families based on their structure and energy source, with the Resistance-Nodulation-Division (RND) family being particularly clinically significant in Gram-negative bacteria [14] [15].
Table 2: Classification and Characteristics of Major Bacterial Efflux Pump Families
| Efflux Pump Family | Representative Example | Primary Energy Source | Typical Substrate Profile |
|---|---|---|---|
| ABC (ATP-binding cassette) | MacAB (E. coli) [14] | ATP Hydrolysis | Macrolides, peptides [14] |
| MFS (Major Facilitator Superfamily) | EmrB (E. coli) [15] | Proton Motive Force | Various antibiotics, dyes, detergents [15] |
| RND (Resistance-Nodulation-Division) | AcrB (E. coli), MexB (P. aeruginosa) [14] [15] | Proton Motive Force | Broad range: β-lactams, quinolones, macrolides, dyes, detergents [14] |
| MATE (Multidrug and Toxic Compound Extrusion) | NorM (V. parahaemolyticus) [14] | Proton/Sodium Ion Gradient | Fluoroquinolones, aminoglycosides [14] |
| SMR (Small Multidrug Resistance) | EmrE (E. coli) [14] | Proton Motive Force | Small, hydrophobic cations, disinfectants [14] |
The RND-type pumps in Gram-negative bacteria, such as the AcrAB-TolC system in E. coli, form complex tripartite structures that span the entire cell envelope. The inner membrane component (e.g., AcrB) captures substrates from the cytoplasm and periplasm, the periplasmic adapter protein (e.g., AcrA) forms a bridge, and the outer membrane protein (e.g., TolC) forms a channel to the exterior [14]. This architecture allows them to expel drugs directly into the external medium, bypassing the permeability barrier of the outer membrane.
In contrast, eukaryotic cells possess their own set of efflux pumps, most notably the P-glycoprotein (MDR1), which is an ABC transporter that contributes to MDR in cancer cells [14]. While the function of expelling toxins is analogous, the prokaryotic and eukaryotic pumps are structurally and evolutionarily distinct. They exhibit no sequence homology and utilize different energy-coupling mechanisms. This divergence presents a drug development opportunity, as inhibitors can be designed to specifically target prokaryotic pumps without cross-reacting with human counterparts.
Experimental Protocols for Functional Analysis
Protocol 1: Ethidium Bromide Accumulation Assay
- Prepare a bacterial suspension in a suitable buffer with a known OD600.
- Load the cells with Ethidium Bromide (EtBr), a fluorescent efflux pump substrate.
- Add an energy source (e.g., glucose) to initiate active efflux.
- Monitor fluorescence over time in a spectrofluorometer. A decrease in fluorescence indicates active efflux of EtBr. The assay can be repeated in the presence and absence of an efflux pump inhibitor (EPI) like Carbonyl Cyanide m-Chlorophenylhydrazone (CCCP) to confirm the energy-dependent nature of the efflux [15].
- Calculate accumulation ratios by comparing fluorescence levels with and without an energy source or inhibitor.
Protocol 2: Minimum Inhibitory Concentration (MIC) Profiling with Inhibitors
- Determine the MIC of various antibiotics against the target strain using standard broth microdilution methods.
- Repeat the MIC determination in the presence of a sub-inhibitory concentration of a known EPI (e.g., Phe-Arg-β-naphthylamide for RND pumps).
- A significant reduction (e.g., ≥4-fold) in the MIC of an antibiotic in the presence of the EPI is indicative of that antibiotic being a substrate for the efflux pump system [14].
Diagram 1: RND-type efflux pump mechanism. The diagram illustrates the tripartite structure and proton-driven export of antibiotics.
Mechanism 3: Toxin-Antitoxin Systems
Functional, Genetic, and Comparative Analysis
Toxin-antitoxin (TA) systems are genetic modules composed of a stable toxin protein that disrupts essential cellular processes and a labile antitoxin that neutralizes the toxin [17]. Under normal growth conditions, the antitoxin is produced in excess, forming a complex that represses the TA operon. Under stress (e.g., nutrient starvation, antibiotic exposure), the labile antitoxin is degraded, freeing the toxin to act on its target and induce a state of growth arrest or persistence, which is thought to promote survival under adverse conditions [11] [17] [16]. These systems are categorized into six types (I-VI) based on the nature and mode of action of the antitoxin.
Table 3: Classification of Major Toxin-Antitoxin System Types
| TA System Type | Antitoxin Nature | Mechanism of Antitoxin Action | Example |
|---|---|---|---|
| Type I | Non-coding RNA [17] | Binds toxin mRNA, preventing translation [17] | hok/sok (Plasmid R1) [17] |
| Type II | Protein [17] | Binds toxin protein, neutralizes activity [17] | RelB/RelE (E. coli), Kid/Kis (Plasmid R1) [17] [18] |
| Type III | Non-coding RNA [17] | Directly binds toxin protein [17] | ToxN/ToxI (B. subtilis) [17] |
| Type IV | Protein [17] | Binds toxin target, preventing toxin action [17] | CbtA/CbeA (E. coli) [17] |
| Type V | Protein [17] | Cleaves toxin mRNA [17] | GhoS/GhoT (E. coli) [17] |
The physiological role of TA systems is complex and includes functions in phage defense, stabilization of genomic parasites, and stress response [16]. Recent research suggests that TA systems do not induce uniform growth stasis across a population but rather create phenotypic heterogeneity, leading to subpopulations of cells with different metabolic states and stress tolerance levels [16].
Strikingly, some prokaryotic TA systems have been shown to function efficiently in eukaryotes. The Kid toxin from the parD system of plasmid R1 inhibits cell proliferation and induces apoptosis in human cells, while its cognate antitoxin Kis neutralizes this effect [18]. This cross-kingdom functionality highlights the conservation of some fundamental cellular targets and pathways. For drug development, TA systems represent attractive targets for novel antibacterial strategies that could disrupt the toxin-antitoxin balance to trigger bacterial cell death or sensitize persistent cells to conventional antibiotics.
Experimental Protocols for Characterization
Protocol 1: Bacterial Two-Hybrid Assay for Protein-Protein Interaction
- Clone the toxin and antitoxin genes into the appropriate two-hybrid vectors (e.g., encoding complementary fragments of adenylate cyclase in the BACTH system).
- Co-transform the constructs into an E. coli reporter strain.
- Plate transformants on selective media containing X-Gal.
- A positive protein-protein interaction between the toxin and antitoxin is indicated by the restoration of adenylate cyclase activity, leading to β-galactosidase production and blue colonies [17].
Protocol 2: Spot Dilution Assay for Toxicity and Neutralization
- Clone the toxin gene under a tightly regulated, inducible promoter (e.g., araBAD, rhamnose) on a plasmid.
- Clone the antitoxin gene under a constitutive or independently inducible promoter on a compatible plasmid.
- Transform the plasmids into the appropriate bacterial strain.
- Induce toxin expression in serial dilutions of the culture spotted on agar plates.
- Assess cell growth: Toxicity is evidenced by lack of growth upon induction, which is rescued by co-expression of the antitoxin [18].
Diagram 2: Type II TA system regulation. The diagram shows stress-induced antitoxin degradation leading to toxin activation.
The Scientist's Toolkit: Essential Research Reagents
The table below lists key reagents and their applications for studying the prokaryotic toxin resistance mechanisms discussed in this guide.
Table 4: Essential Research Reagents for Studying Prokaryotic Defense Mechanisms
| Reagent / Tool | Primary Function/Application | Specific Use-Case Example |
|---|---|---|
| Carbonyl Cyanide m-Chlorophenylhydrazone (CCCP) | Protonophore; dissipates proton motive force [15] | Positive control in efflux pump assays to inhibit energy-dependent efflux [15]. |
| Phe-Arg-β-naphthylamide (PAβN) | Broad-spectrum efflux pump inhibitor (EPI) for RND pumps [14] | Used in MIC assays to potentiate antibiotic activity and identify pump substrates [14]. |
| pBAD or pRham Vectors | Tightly regulated, inducible expression systems | Controlled expression of toxin genes for toxicity assays in bacteria and eukaryotes [18]. |
| Bacterial Adenylate Cyclase-Based Two-Hybrid (BACTH) System | In vivo detection of protein-protein interactions [17] | Validation of direct binding between Type II toxin and antitoxin proteins [17]. |
| Fluorescent Dyes (e.g., Ethidium Bromide) | Substrates for many multidrug efflux pumps [15] | Used in real-time fluorometric assays to quantify efflux pump activity. |
| Anti-Serial Dilution Plating | Method for quantifying bacterial persistence | Measuring the fraction of persister cells surviving antibiotic treatment, a phenotype linked to TA systems [16]. |
The comparative assessment of enzymatic degradation, efflux pumps, and toxin-antitoxin systems reveals a multi-layered defensive strategy in prokaryotes. Enzymatic degradation offers high specificity, efflux pumps provide broad-spectrum protection, and TA systems contribute to population survival under extreme stress. The functional conservation of some systems, like TA modules, in eukaryotes [18] underscores the presence of ancient, fundamental cellular pathways, while the structural divergence of others, like efflux pumps [14], highlights unique evolutionary paths. For researchers and drug development professionals, this comparative framework is invaluable. It identifies vulnerable nodes—such as the protein-protein interface in Type II TA systems, the energy-coupling mechanism of RND efflux pumps, and the active sites of inactivating enzymes—that can be targeted for the rational design of next-generation antimicrobials and potentiators capable of overcoming multidrug resistance.
The continuous exposure to environmental toxins, antimicrobial compounds, and chemical weapons produced by competitors has driven the evolution of sophisticated defense mechanisms across the tree of life. Eukaryotes and prokaryotes have developed distinct yet sometimes convergent strategies to detect, neutralize, and eliminate these toxic threats. Eukaryotic systems have evolved complex, multi-layered defenses that integrate transcriptional regulation, protein trafficking, and immune surveillance pathways to maintain cellular integrity against toxic assaults. Meanwhile, prokaryotes employ more direct mechanisms centered on toxin-immunity protein pairs and efflux transporters. Understanding these divergent strategies provides crucial insights for addressing pressing challenges in drug development, pesticide resistance, and antimicrobial therapy. This review comprehensively compares the molecular machinery underlying toxin resistance, highlighting both the fundamental distinctions and remarkable convergences between eukaryotic and prokaryotic systems, with emphasis on the clinical and agricultural applications of these findings.
Eukaryotic Detoxification Pathways: Multi-Layered Defense Systems
Transcriptional Regulation of Detoxification Genes
Eukaryotic cells employ sophisticated transcriptional programs to regulate detoxification genes, allowing them to rapidly adapt to xenobiotic challenges. Key transcriptional pathways identified in insects and fungi demonstrate remarkable evolutionary convergence with mammalian systems. In insects, several well-characterized transcriptional pathways regulate the expression of detoxification enzymes, including cytochrome P450 monooxygenases (CYPs), glutathione S-transferases (GSTs), carboxyl esterases (CarE), and ATP-binding cassette (ABC) transporters [19] [20]. The principal transcriptional regulators include:
- AhR/ARNT Pathway: Aryl hydrocarbon receptor and its partner ARNT that bind xenobiotic response elements
- CncC/Keap1 Pathway: Conserved cap'n'collar transcription factor and its negative regulator Keap1 that responds to oxidative stress
- Nuclear Receptors: Ligand-activated transcription factors that directly bind xenobiotics
- MAPK/CREB and GPCR/cAMP/PKA Pathways: Signal transduction cascades that connect extracellular signals to transcriptional activation [19] [20]
Similar regulatory mechanisms operate in fungi. Research on the filamentous fungus Sclerotinia homoeocarpa revealed that a fungus-specific transcription factor, ShXDR1, coordinately regulates both phase I (CYPs) and phase III (ABC transporters) detoxification genes [21]. A gain-of-function mutation (M853T) in ShXDR1 causes constitutive overexpression of these genes, resulting in multidrug resistance to various fungicidal chemicals [21]. This system represents a functional analog to the mammalian pregnane X receptor (PXR) pathway, demonstrating convergent evolution between fungal and mammalian lineages in regulating xenobiotic detoxification [21].
Figure 1: Transcriptional regulation of detoxification genes in eukaryotic systems. Insects utilize the CncC/Keap1 pathway where xenobiotics inactivate Keap1, releasing Nrf2/CncC to activate gene expression. Fungi employ XDR1 transcription factors, with gain-of-function mutations leading to constitutive detoxification gene expression.
Post-Transcriptional Regulation by Non-Coding RNAs
Eukaryotes employ extensive post-transcriptional regulatory mechanisms mediated by non-coding RNAs that fine-tune detoxification responses. MicroRNAs (miRNAs) have emerged as crucial regulators of insecticide resistance in various insect species [19] [20]. These small non-coding RNAs, typically 18-25 nucleotides in length, regulate gene expression by binding to complementary sequences in target mRNAs, leading to translational repression or mRNA degradation [20]. miRNAs typically bind to the 3'-untranslated regions (UTRs) of target mRNAs through imperfect base pairing, with the "seed" sequence (nucleotides 2-8 at the 5' end) playing a critical role in target recognition [19].
In resistant insect populations, specific miRNAs have been shown to target detoxification genes, including P450 enzymes, GSTs, and esterases [19]. The expression of these miRNAs is influenced by oxidative and cellular stress, creating a dynamic regulatory network that allows insects to rapidly adapt to insecticide exposure [20]. Beyond miRNAs, long non-coding RNAs (lncRNAs) and epitranscriptomic modifications such as RNA methylation also contribute to insecticide resistance, although their mechanisms are less well-characterized [19].
Protein Trafficking and Cellular Defense Mechanisms
Eukaryotic cells have evolved sophisticated protein trafficking systems that contribute to toxin defense. Recent research in yeast has revealed that the conserved oligomeric Golgi (COG) complex is essential for resistance to the AB toxin K28 [22]. The COG complex mediates the retrograde trafficking of the defense factor Ktd1, which surveys endolysosomal compartments for toxins and provides protection [22]. In cog mutants, mis-localization of Ktd1 results in hypersensitivity to K28 toxin, demonstrating the critical importance of precise cellular trafficking in toxin defense [22].
Eukaryotic cells also employ ribosome-mediated stress surveillance systems. Recent research has revealed that ribosomes not only synthesize proteins but also function as sophisticated stress sensors. When ribosomes stall and collide due to cellular stress—such as limited amino acids, damaged mRNA, or viral infections—they activate the ribotoxic stress response (RSR) [23]. This response is mediated by the kinase ZAK, which detects ribosome collisions and initiates signaling cascades that trigger protective responses, including DNA repair mechanisms or programmed cell death [23]. The discovery of this "hidden alarm system" reveals how eukaryotic cells quickly detect trouble at the translational level and mount an appropriate defense.
Prokaryotic Defense Mechanisms: Direct and Efficient Countermeasures
Toxin-Immunity Protein Systems
Prokaryotes employ primarily toxin-immunity protein systems as their fundamental defense strategy against antimicrobial toxins produced by competitors. These systems consist of antimicrobial toxins that inhibit the growth of competing strains and cognate immunity proteins that protect the producer cells from self-intoxication [24]. The genes encoding toxin-immunity pairs are typically located adjacent to each other in bacterial genomes, ensuring coordinated expression [24]. The Prokaryotic Antimicrobial Toxin database (PAT) currently contains 441 experimentally validated antimicrobial toxin proteins from 70 prokaryotic genera, with over 40% reported in the past five years, reflecting the rapid expansion of this field [24].
Prokaryotic antimicrobial toxins exhibit remarkable functional diversity, including:
- Nucleases that target DNA or RNA of competitor cells
- Phospholipases or pore-forming toxins that disrupt cell membranes
- Glycoside hydrolases or proteases that degrade cell walls
- NADases that disrupt cellular energy balance
- ADP-ribosyltransferases that target tubulin-like proteins to prevent cell division [24]
These toxin-immunity systems are distributed across diverse secretion mechanisms, including contact-dependent systems like T6SS, T4SS, and T7SS, as well as contact-independent secretion of bacteriocins [24].
Complement-Like Killing Mechanisms in Bacteria
Recent research has revealed unexpected complexity in prokaryotic toxin systems, including mechanisms that resemble eukaryotic immune effectors. In the Gram-negative Bacteroidota, a family of two-component CDC-like (CDCL) toxins functions similarly to the mammalian membrane attack complex (MAC) [25]. Unlike their CDC relatives that target eukaryotic cells, CDCLs bind to and kill closely related bacterial species [25].
The CDCL system requires proteolytic activation of two components (CDCLL and CDCLS) that then interact to form a pore, resulting in bacterial cell death [25]. The producing bacteria protect themselves from their own CDCL toxins through surface lipoproteins that block pore formation [25]. Genomic analyses reveal that these CDCL genes are widespread in human gut Bacteroidales species and are often located on mobile genetic elements, facilitating their distribution across diverse bacterial populations [25].
Table 1: Comparative Analysis of Toxin Resistance Mechanisms in Prokaryotes and Eukaryotes
| Feature | Prokaryotic Systems | Eukaryotic Systems |
|---|---|---|
| Primary Defense Strategy | Toxin-immunity protein pairs | Transcriptional regulation of detoxification enzymes |
| Key Regulatory Components | Adjacent gene organization | Transcription factors (CncC/Keap1, XDR1, nuclear receptors) |
| Detoxification Phases | Limited phase variation | Coordinated phase I-III detoxification |
| Cellular Surveillance | Restriction-modification systems | Ribotoxic stress response (ZAK kinase) |
| Export Mechanisms | Specialized secretion systems (T6SS, T4SS) | ABC transporters, membrane trafficking |
| Intercellular Signaling | Contact-dependent inhibition | Hormonal signaling, paracrine factors |
| Evolutionary Adaptation | Horizontal gene transfer | Gene duplication, alternative splicing |
Experimental Approaches and Methodologies
Key Experimental Protocols in Toxin Resistance Research
RNA Sequencing for Detoxification Gene Profiling: Next-generation RNA sequencing (RNA-seq) has been instrumental in identifying detoxification genes involved in multidrug resistance. The protocol typically involves treating sensitive and resistant strains with sublethal concentrations of the toxic compound (e.g., 0.1 µg/ml propiconazole for fungi) for short periods (1 hour), followed by RNA extraction, library preparation, and sequencing [21]. Bioinformatics analyses then identify differentially expressed genes, particularly focusing on detoxification enzyme families such as CYPs, GSTs, and ABC transporters [21]. This approach revealed the coordinated overexpression of phase I and III detoxification genes in multidrug-resistant fungal strains [21].
Molecular Docking for Detoxification Enzyme Discovery: Computational approaches, particularly molecular docking, have become valuable tools for identifying potential detoxification enzymes. Reverse molecular docking platforms screen a given ligand (e.g., a toxin) against numerous potential protein targets [26]. Software such as AutoDock, VINA, GOLD, and FRED use conformation search algorithms and scoring functions to predict binding modes and affinities [26]. A consensus strategy employing multiple docking algorithms often provides more reliable predictions than single software approaches [26]. These methods have been successfully used to identify key residues in enzymes that interact with toxins, such as the interaction between QDDH and deoxynivalenol (DON) [26].
Cryo-Electron Microscopy for Structural Analysis: Structural biology techniques, particularly cryo-electron microscopy (cryo-EM), have been crucial for understanding the mechanisms of toxin resistance and defense. In the study of ZAK kinase activation by ribosome collisions, researchers combined biochemical experiments with cryo-EM to demonstrate how ZAK attaches to collided ribosomes and identified the structural features necessary for its activation [23]. This approach revealed that ZAK interacts with specific ribosomal proteins, causing dimerization that initiates cellular signaling cascades [23].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents and Their Applications in Toxin Resistance Studies
| Reagent/Solution | Function/Application | Experimental Context |
|---|---|---|
| Propiconazole | Demethylation inhibitor fungicide | Used to induce detoxification gene expression in fungal strains [21] |
| Carboxyfluorescein | Fluorescent dye for pore formation assays | Loaded into liposomes to monitor CDCL toxin activity [25] |
| Trypsin | Proteolytic enzyme for toxin activation | Required for proteolytic activation of CDCL toxins [25] |
| POPC Liposomes | Artificial membrane systems | Used to study pore-forming activity of toxins in controlled environments [25] |
| α-rhamnosidase/β-glucosidases | Detoxification enzymes | Sequentially hydrolyze antifungal saponins in plant-pathogen interactions [26] |
| iKIX1 | Protein-protein interaction inhibitor | Disrupts PDR1-mediator interaction to combat multidrug resistance in fungi [21] |
Comparative Analysis and Evolutionary Perspectives
The comparative analysis of toxin resistance mechanisms reveals both striking divergences and remarkable convergences between prokaryotic and eukaryotic strategies. Prokaryotes employ direct, efficient systems centered on toxin-immunity protein pairs that provide immediate protection against specific threats [24]. These systems are often encoded on mobile genetic elements, facilitating rapid horizontal transfer through microbial communities [24]. In contrast, eukaryotes have evolved multi-layered regulatory networks that integrate transcriptional, post-transcriptional, and protein trafficking mechanisms to provide flexible, inducible responses to diverse toxic challenges [19] [20].
Despite these fundamental differences, examples of convergent evolution are evident. The fungal XDR1 regulatory system shows functional analogy to the mammalian PXR pathway, though these transcription factors share no sequence homology [21]. Similarly, the CDCL toxin system in Bacteroidota has evolved a pore-forming mechanism strikingly similar to the eukaryotic complement membrane attack complex, despite originating from a completely different phylogenetic background [25]. These convergent solutions highlight the power of natural selection to arrive at similar mechanistic answers to the universal challenge of toxin defense.
The evolutionary trajectories of these systems also differ significantly. Prokaryotes primarily rely on horizontal gene transfer to acquire new resistance traits, allowing rapid adaptation but potentially costing more cellular resources to maintain numerous specific immunity proteins [24] [27]. Eukaryotes tend to employ gene duplication and regulatory network expansion, creating layered systems that can be fine-tuned to specific threats while minimizing fitness costs [19] [20]. This fundamental difference in evolutionary strategy has profound implications for addressing toxin resistance in clinical and agricultural settings.
Figure 2: Evolutionary pathways of toxin defense strategies. Prokaryotes rely on horizontal gene transfer and mobile genetic elements to disseminate toxin-immunity pairs, while eukaryotes utilize gene duplication and regulatory network expansion to create layered defense systems, with convergent evolution leading to similar solutions.
Applications and Future Directions
The comparative understanding of toxin resistance mechanisms has significant implications for addressing pressing challenges in medicine and agriculture. In antifungal drug development, targeting the interaction between transcription factors like ShXDR1 and mediator complexes represents a promising strategy for overcoming multidrug resistance in fungal pathogens [21]. The discovery of iKIX1, a compound that disrupts the PDR1-mediator interaction in yeast, provides a proof-of-concept for this approach [21].
In agriculture, understanding the transcriptional regulation of detoxification genes in insect pests enables the development of novel pest management strategies. RNA interference (RNAi) technology can be employed to silence specific resistance-related genes, potentially restoring insecticide sensitivity in resistant populations [19] [20]. Similarly, modulating the CncC/Keap1 pathway could alter the expression of multiple detoxification genes simultaneously, providing a broader approach to insecticide resistance management [19].
The discovery of complement-like killing mechanisms in bacteria opens new avenues for developing narrow-spectrum antimicrobials that target specific bacterial species while preserving beneficial microbiota [25]. As our understanding of these diverse defense mechanisms continues to grow, so too will our ability to manipulate them for human health and agricultural productivity.
The evolutionary arms race between organisms and toxins has driven the development of sophisticated resistance mechanisms. This comparative guide examines two fundamental processes underpinning resistance: horizontal gene transfer (HGT), which enables rapid dissemination of genetic traits across contemporary populations, and natural selection, which acts on vertical inheritance and mutation over generational timescales. While HGT dominates as the primary mechanism for rapid resistance acquisition in prokaryotes, particularly against antibiotics, eukaryotes rely more heavily on natural selection acting on existing genetic variation and rare beneficial mutations. Through analysis of experimental data and emerging research, we demonstrate how these distinct pathways shape resistance landscapes across the tree of life, with critical implications for antimicrobial development, cancer therapeutics, and managing treatment resistance.
The capacity to withstand toxic compounds represents a fundamental survival challenge that has shaped evolutionary pathways across all life forms. In prokaryotes, resistance mechanisms primarily emerge through horizontal gene transfer (HGT), the non-sexual movement of genetic information between organisms, enabling virtually instantaneous acquisition of resistance traits across species boundaries [28] [29]. This process stands in stark contrast to the slower, generational process of natural selection acting on random mutations and vertical inheritance—a mechanism that dominates in eukaryotic resistance evolution [30]. The distinction between these pathways has profound implications for how resistance develops and spreads in different biological contexts.
The clinical and ecological significance of understanding these mechanisms cannot be overstated. In prokaryotic systems, HGT facilitates the rapid spread of antibiotic resistance genes among bacterial pathogens, contributing to the global health crisis of multidrug-resistant infections [28] [31]. In eukaryotic systems, natural selection drives the emergence of treatment resistance in contexts ranging from cancer therapeutics to antifungal applications, though through fundamentally different genetic mechanisms [31]. This comparative analysis examines the genetic foundations, operational mechanisms, and experimental evidence for these distinct resistance pathways, providing researchers with a structured framework for understanding and investigating resistance evolution across biological systems.
Horizontal Gene Transfer: The Prokaryotic Paradigm
Mechanisms and Molecular Processes
Horizontal gene transfer encompasses three primary mechanisms that enable prokaryotes to acquire genetic material from contemporary organisms in their environment. Transformation involves the uptake and incorporation of exogenous DNA fragments from the environment, a process facilitated by competence factors that allow bacterial cells to bind and internalize extracellular DNA [32]. Naturally competent bacteria like Neisseria gonorrhoeae and Streptococcus pneumoniae exemplify this mechanism, which typically involves homologous recombination of DNA fragments approximately 10 genes in length [32].
Conjugation represents the most common form of HGT, particularly between distantly related bacterial species, involving direct cell-to-cell contact and transfer of mobile genetic elements [32] [31]. This process is mediated by conjugative plasmids, integrative conjugative elements (ICEs), and conjugative transposons that encode the necessary machinery for DNA transfer between cells. The clinical significance of conjugation is profound, as it enables cross-species transfer of antibiotic resistance genes, with certain plasmids capable of transferring across genera, phyla, and even domains [31].
Transduction involves the transfer of bacterial DNA via bacteriophages (bacterial viruses), which occasionally package host DNA instead of viral DNA during infection cycles [32] [29]. When these transducing particles infect new bacterial cells, they inject the previous host's DNA, which may then recombine into the recipient's genome. Both generalized transduction (where any bacterial DNA fragment can be transferred) and specialized transduction (where specific bacterial genes adjacent to prophage integration sites are transferred) contribute to this process [32].
Table 1: Primary Mechanisms of Horizontal Gene Transfer in Prokaryotes
| Mechanism | Genetic Material Transferred | Key Elements | Transfer Range |
|---|---|---|---|
| Transformation | Environmental DNA fragments | Competence proteins, DNA uptake systems | Typically within same or closely related species |
| Conjugation | Plasmids, conjugative transposons | Conjugative pilus, transfer genes | Broad range, including distant species |
| Transduction | Bacterial DNA via viruses | Bacteriophages, pac sites | Usually within same bacterial species |
| Gene Transfer Agents | Random DNA fragments | Virus-like particles encoded by host | Primarily within alphaproteobacteria |
Mobile Genetic Elements as HGT Vehicles
Mobile genetic elements (MGEs) serve as the primary vehicles for HGT, functioning as natural genetic engineering systems that facilitate the movement and reorganization of DNA within and between genomes. Plasmids are extrachromosomal DNA elements that replicate independently and frequently carry accessory genes conferring selective advantages, such as antibiotic resistance and toxin production [33] [31]. The ability of plasmids to transfer between bacteria via conjugation makes them particularly effective in spreading resistance traits through microbial populations.
Transposons (jumping genes) are DNA sequences that can change position within a genome, sometimes carrying additional genes such as those encoding antibiotic resistance [29]. Horizontal transposon transfer (HTT) represents a specialized form of HGT that enables these mobile elements to colonize new genomes, with DNA transposons and LTR retroelements being most likely to undergo HTT due to their stable double-stranded DNA intermediates [29]. Integrons are genetic systems that capture and express gene cassettes, frequently accumulating multiple antibiotic resistance genes in clinical isolates [31]. These platforms significantly contribute to the assembly of multidrug resistance clusters in pathogenic bacteria.
The mobilome—the collective mobile genetic elements within a genome—provides prokaryotes with access to a shared gene pool, enabling extremely rapid adaptation to selective pressures like antibiotic exposure. This dynamic genetic reservoir stands in stark contrast to the relatively static chromosomal background, highlighting the dual nature of prokaryotic genomes as both inherited and acquired genetic entities.
Natural Selection: The Eukaryotic Foundation
Vertical Inheritance and Mutation Accumulation
In contrast to prokaryotes, eukaryotic resistance primarily emerges through natural selection acting on genetic variation generated through vertical inheritance and mutation. The sexual reproduction cycle in eukaryotes provides a mechanism for generating genetic diversity through meiotic recombination and gamete fusion, creating novel genetic combinations upon which natural selection can act [31]. This process, while slower than HGT, enables the gradual accumulation of beneficial mutations that enhance resistance to toxins and other environmental stressors.
Eukaryotes employ sophisticated epigenetic modifications as rapid-response mechanisms to environmental challenges, including toxin exposure. These include DNA methylation, histone modifications, and non-coding RNA-mediated regulation that can alter gene expression patterns without changing the underlying DNA sequence [31]. While not permanent genetic changes, these epigenetic adjustments can provide provisional protection while slower genetic adaptations evolve through selection on random mutations.
The expansion of gene families through duplication and divergence represents another key mechanism by which eukaryotes evolve resistance through natural selection. Gene duplication creates genetic redundancy that allows one copy to maintain original function while others accumulate mutations that may confer novel protective functions [31]. This process has been instrumental in the evolution of detoxification systems like cytochrome P450 enzymes, which play crucial roles in metabolizing various toxins and drugs.
Limited Horizontal Gene Transfer in Eukaryotes
While HGT is less prevalent in eukaryotes than in prokaryotes, growing evidence indicates that it does occur and contributes to eukaryotic evolution, including resistance traits [30] [29]. Documented cases of HGT in eukaryotes include the transfer of mitochondrial genes between parasitic plants and their hosts [30], the acquisition of bacterial genes for toxin degradation in some arthropods [31], and the integration of Agrobacterium T-DNA into the genome of sweet potato (Ipomoea batatas) and other plants [30].
The barriers to HGT in eukaryotes include the nuclear envelope, which separates the genome from the cytoplasm; the presence of germline-soma separation in multicellular organisms, which requires foreign DNA to enter germ cells to be heritable; and RNA interference pathways that silence foreign genetic elements [30]. Despite these barriers, some eukaryotic lineages have experienced significant HGT, such as tardigrades, in which approximately 17.5% of genes originate from foreign sources like bacteria, fungi, and plants [31].
The functional domains of transferred genes in eukaryotes often involve toxin resistance and metabolic adaptation, suggesting that HGT may provide selective advantages similar to those in prokaryotes, albeit through different mechanistic pathways. The investigation of these rare transfer events provides valuable insights into the potential for engineering HGT-based solutions for eukaryotic disease management.
Comparative Analysis: Experimental Data and Evidence
Quantitative Resistance Patterns Across Organisms
Recent genomic studies reveal distinct patterns in how resistance genes are distributed and maintained across prokaryotic and eukaryotic systems. Analysis of 24,102 complete bacterial genomes shows that duplicated antibiotic resistance genes (ARGs) are highly enriched in bacteria isolated from humans and livestock—environments with high antibiotic exposure—with further enrichment in antibiotic-resistant clinical isolates [33]. This pattern demonstrates how HGT, combined with strong selection, rapidly amplifies resistance genes in prokaryotic populations facing toxin pressure.
In contrast, eukaryotic resistance typically emerges through the selection of pre-existing genetic variations or rare beneficial mutations. For instance, the Fhb7 resistance gene in wheat, which provides resistance to Fusarium head blight, originated from an HGT event between the Epichloë fungus and Thinopyrum elongatum, but this represents a rare exception rather than the norm [30]. Most eukaryotic resistance evolves through selection on standing variation or new mutations within the species' own gene pool.
Table 2: Comparative Analysis of Resistance Mechanisms in Prokaryotes vs. Eukaryotes
| Characteristic | Prokaryotes | Eukaryotes |
|---|---|---|
| Primary Mechanism | Horizontal Gene Transfer | Natural Selection on Mutations |
| Timescale | Immediate to days | Generational to evolutionary |
| Genetic Source | Global gene pool | Species gene pool |
| Key Elements | Plasmids, transposons, integrons | Gene duplications, regulatory changes |
| Spread Pattern | Epidemic, network-based | Clonal, tree-based |
| Environmental Response | Gene acquisition | Gene expression changes, epigenetics |
| Experimental Evidence | Duplicated ARGs in clinical isolates [33] | Fhb7 transfer in wheat [30] |
Molecular and Biochemical Distinctions
Prokaryotic and eukaryotic resistance systems show fundamental differences at the molecular level. Bacterial toxins used in interference competition are often encoded within gene cassettes on mobile elements and exhibit distinctive amino acid compositions, with over-representation of histidine and arginine compared to non-toxic secreted proteins [34]. Eukaryotic toxin resistance systems frequently involve enzyme families like cytochrome P450s and glutathione S-transferases that have expanded through gene duplication and divergence.
The two-component CDC-like (CDCL) toxins produced by Gram-negative Bacteroidota illustrate how prokaryotic systems employ horizontally transferred toxin genes in bacterial antagonism [25]. These CDCL genes are distributed on mobile genetic elements among gut microbiota species and function similarly to the mammalian complement membrane attack complex, representing an HGT-dependent armory system [25]. Eukaryotic systems lack such portable toxin arsenals, instead relying on immune recognition and programmed cell death pathways.
The empirical data reveal that HGT provides prokaryotes with a rapid-response capability to novel toxins, while eukaryotes depend on selection acting on existing genetic toolkits—a fundamental distinction with profound implications for clinical practice and resistance management.
Experimental Approaches and Methodologies
Key Experimental Protocols
Investigating HGT-mediated resistance typically involves experimental evolution studies where bacteria are exposed to sublethal antibiotic concentrations, followed by genomic analysis of evolved populations. One such protocol exposed E. coli strains containing a minimal transposon with a tetracycline resistance gene to 50 μg/mL tetracycline for 9 days, with control populations propagated without antibiotics [33]. Whole-genome sequencing of resistant colonies revealed tetA duplications through intragenomic transposition in selected populations, while control populations showed no such duplications.
A modified short-term protocol using wild-type E. coli K-12 MG1655 demonstrated that just one day (~10 bacterial generations) of tetracycline selection was sufficient to drive resistance gene duplications to observable frequencies across all replicate populations [33]. Replacement of the tetA gene with genes conferring resistance to spectinomycin, kanamycin, carbenicillin, and chloramphenicol yielded similar results, with antibiotic resistance gene (ARG) duplications observed in 8 out of 8 evolved populations across all four antibiotics [33].
For studying natural selection-based resistance in eukaryotes, mutation accumulation lines combined with whole-genome sequencing provide insights into the rate and spectrum of spontaneous mutations. These approaches typically involve propagating multiple independent lines through single-organism bottlenecks for hundreds of generations, followed by genomic sequencing to identify accumulated mutations and phenotypic assays to assess their functional consequences.
Detection and Analysis Methods
Bioinformatic detection of HGT events employs both parametric methods (identifying atypical sequence signatures like GC content, codon usage bias) and phylogenetic methods (identifying discrepancies between gene trees and species trees) [29]. The availability of thousands of complete bacterial genomes enables robust detection of recently transferred genes, particularly those associated with mobile genetic elements.
Shotgun metagenomics provides a powerful approach for identifying HGT events in complex microbial communities without cultivation. This method involves fragmenting and sequencing all DNA in a sample, then assembling contiguous regions and searching for phylogenetic mismatches that indicate horizontal transfer [29]. For eukaryotes, detecting HGT requires additional safeguards to exclude contamination and account of the complexity of eukaryotic genomes with abundant repeat-rich regions [30].
Functional validation of candidate resistance genes involves heterologous expression in model organisms followed by toxin sensitivity assays. For example, cloning putative resistance genes into susceptible strains and measuring changes in minimum inhibitory concentration (MIC) provides direct evidence of resistance function. For eukaryotic systems, RNA interference or CRISPR-based gene editing can establish whether candidate genes confer resistance through loss-of-function experiments.
Table 3: Essential Research Reagents for Investigating Resistance Mechanisms
| Reagent/Resource | Function/Application | Examples/Sources |
|---|---|---|
| PAT Database | Catalog of experimentally validated antimicrobial toxins | 441 toxins with delivery mechanisms [24] |
| Tn5 Transposase System | Experimental evolution of HGT | tetA-Tn5 transposition assay [33] |
| Long-read Sequencers | Resolving duplicated resistance genes | PacBio, Oxford Nanopore [33] |
| Mobile Genetic Elements | HGT mechanism analysis | Plasmids, conjugative transposons [31] |
| Antibiotic Selection Media | Experimental evolution | Tetracycline, carbenicillin [33] |
| Competent Bacterial Strains | Transformation studies | E. coli DH5α, MG1655 [33] [32] |
| Phage Lysates | Transduction experiments | P1, λ phage [32] |
| Metagenomic Datasets | Natural HGT detection | Earth Microbiome Project [24] |
The comparative analysis of horizontal gene transfer and natural selection as resistance mechanisms reveals a fundamental dichotomy in evolutionary strategy between prokaryotes and eukaryotes. HGT provides prokaryotes with a rapid-response system to immediately address novel toxin threats through gene acquisition from a global genetic commons. In contrast, eukaryotes primarily rely on natural selection acting on existing genetic variation, resulting in slower but potentially more stable resistance evolution.
These distinctions have profound implications for clinical practice and drug development. The HGT-driven spread of antibiotic resistance necessitates approaches that target the mobile genetic elements themselves, such as compounds that disrupt conjugation or plasmid maintenance. For eukaryotic resistance, as seen in cancer chemotherapy and antifungal treatments, combination therapies that target multiple pathways simultaneously may help overcome the slower but inevitable emergence of resistance through selection.
Future research directions should include developing HGT-inhibiting therapeutics that specifically target conjugation machinery or plasmid replication, thus preserving antibiotic efficacy. For eukaryotic systems, leveraging rare natural HGT events, such as the Fhb7 transfer in wheat, might inspire novel biotechnological approaches to engineer resistance in crops and animals. The continued development of databases like PAT (Prokaryotic Antimicrobial Toxin database) provides essential resources for tracking the evolution and spread of resistance elements across microbial ecosystems [24].
Understanding these complementary evolutionary pathways—horizontal gene transfer's rapid gene sharing versus natural selection's gradual optimization—provides researchers with a comprehensive framework for addressing the growing challenge of treatment resistance across medical, agricultural, and environmental contexts.
From Discovery to Therapy: Methodologies and Biomedical Applications
This guide provides an objective comparison of computational tools for molecular docking and genomic analysis, with experimental data framed within research on toxin resistance mechanisms across prokaryotes and eukaryotes.
Molecular Docking Tools: Performance and Precision
Molecular docking is a cornerstone of computational drug design, simulating how small molecules (ligands) interact with biological targets like proteins. This is crucial for understanding toxin resistance mechanisms, as it can reveal how certain proteins neutralize toxic compounds or how mutations confer resistance [35].
Comparative Performance of Docking Methodologies
A 2025 comprehensive benchmark evaluated traditional and deep learning (DL)-based docking methods across multiple dimensions, including pose prediction accuracy and physical validity [36]. The results reveal a clear performance stratification.
Table 1: Performance Benchmark of Molecular Docking Tools (Success Rate %)
| Method Category | Specific Tool | Pose Accuracy (RMSD ≤ 2 Å) | Physical Validity (PB-Valid) | Combined Success (RMSD ≤ 2 Å & PB-Valid) |
|---|---|---|---|---|
| Traditional Methods | Glide SP | Data Not Provided | >94% | Data Not Provided |
| Generative Diffusion Models | SurfDock | 91.76 (Astex) | 63.53 (Astex) | 61.18 (Astex) |
| DiffBindFR | 75.30 (Astex) | 46.73 (Astex) | 34.58 (PoseBusters) | |
| Regression-Based Models | KarmaDock, GAABind, QuickBind | Data Not Provided | Data Not Provided | Data Not Provided |
| Hybrid Methods | Interformer | Data Not Provided | Data Not Provided | Data Not Provided |
Key Findings:
- Traditional methods like Glide SP consistently excel in producing physically plausible poses, with validity rates above 94% across diverse datasets [36].
- Generative diffusion models, such as SurfDock, achieve superior pose accuracy but often generate structures with steric clashes or incorrect bond lengths, leading to moderate combined success rates [36].
- Regression-based models frequently fail to produce physically valid poses and generally occupy the lowest performance tier [36].
Experimental Protocol for Docking Evaluation
The benchmark data in Table 1 was derived from a rigorous, multi-dataset evaluation protocol [36]:
- Datasets: The Astex diverse set (known complexes), the PoseBusters benchmark set (unseen complexes), and the DockGen dataset (novel protein binding pockets) were used to test generalization.
- Evaluation Metrics:
- Pose Accuracy: Measured by Root-Mean-Square Deviation (RMSD). A prediction with RMSD ≤ 2 Å relative to the experimental structure is considered successful.
- Physical Validity: Assessed using the PoseBusters toolkit, which checks for chemical and geometric consistency, including bond lengths, angles, and absence of steric clashes.
- System Environment: Benchmarks were conducted in a controlled Docker environment restricted to a single CPU core and a maximum of 12GB memory to ensure a fair and reproducible evaluation [36].
Genomic Analysis Tools for Comparative Genomics
Comparative genomics relies on efficient tools to query and analyze genomic intervals, which is fundamental for identifying genetic elements involved in toxin production and resistance across different species [37].
Benchmarking Genomic Interval Query Tools
A systematic evaluation of genomic interval query tools assessed their runtime performance and memory efficiency using simulated datasets of varying sizes [37].
Table 2: Benchmark of Genomic Interval Query Tools
| Tool | Core Data Structure | Indexing Required? | Data Sorting Required? | Supported Formats |
|---|---|---|---|---|
| BEDTools | Hierarchical binning | No | No | BED, GFF, VCF |
| tabix | Binning & linear index | Yes | Yes | BED, GTF, VCF |
| BEDOPS | Flat interval set | No | Yes | BED (.starch) |
| GIGGLE | B+ tree | Yes | Yes | BED, VCF (.bgz) |
| bedtk | Implicit interval tree | No | No | BED (.gz) |
| gia | Flat interval set | No | No (for unsorted data) | BED (.gz, .bgz) |
Key Findings:
- Tools like BEDTools and bedtk offer flexibility as they do not require pre-sorted or pre-indexed data, making them suitable for rapid, ad-hoc analyses [37].
- tabix and GIGGLE, which require indexing, can provide faster query speeds on large, static datasets but incur an upfront computational cost [37].
- The benchmarking framework, segmeter, is publicly available, facilitating reproducibility and custom comparative analyses [37].
Application to Toxin Resistance Research
The curated computational toolkit enables a comparative assessment of toxin resistance mechanisms in prokaryotes versus eukaryotes. Key differences in toxin proteins can be leveraged to design selective inhibitors.
Curated Toxin Datasets for Robust Modeling
Research highlights the importance of using high-quality, segregated datasets for bacterial and animal toxins, as they possess intrinsic biophysical differences [34]:
- Amino Acid Composition: Animal toxins are significantly enriched in cysteine (which contributes to stability), while bacterial toxins show higher prevalence of histidine and arginine [34].
- Sequence Length: Animal toxins are, on average, significantly shorter than bacterial toxins [34].
- Isoelectric Point (pI): Bacterial toxin distributions are shifted toward acidic pI values, with about a third having pI below 5, potentially related to their mechanism of action in acidic endosomes [34].
Mixing these distinct toxin groups in bioinformatics models can introduce noise and compromise predictive performance. Therefore, using specialized, curated datasets is critical for reliability [34].
Workflow for Toxin Resistance Mechanism Investigation
The following diagram illustrates a generalized experimental workflow that integrates the discussed tools for studying toxin resistance.
This section details key databases, software, and computational resources essential for conducting research in this field.
Table 3: Essential Research Reagent Solutions for Computational Toxicology
| Resource Name | Type | Primary Function | Relevance to Toxin Research |
|---|---|---|---|
| Protein Data Bank (PDB) | Database | Repository for 3D structural data of proteins and nucleic acids. | Source of protein-toxin complex structures for analysis and docking template [35]. |
| UniProtKB/Swiss-Prot | Database | Expertly curated protein sequence and functional information. | Foundational resource for obtaining accurate sequences of toxins and resistance-related proteins [34]. |
| Curated Toxin Datasets | Dataset | Specialized collections of bacterial exotoxins and animal toxins. | Provides high-quality, non-redundant data for training predictive models and comparative studies [34]. |
| segmeter | Software | Benchmarking framework for genomic interval query tools. | Enables reproducible performance comparison of genomics tools on custom datasets [37]. |
| PoseBusters | Software | Validation toolkit for molecular docking predictions. | Checks physical plausibility of predicted docking poses, critical for avoiding false positives [36]. |
The comparative assessment of toxin resistance mechanisms in prokaryotes and eukaryotes is a cornerstone of modern microbiology and toxicology, with profound implications for drug development and understanding infectious diseases. Bacteria employ a vast arsenal of protein toxins to attack competing prokaryotic or eukaryotic cells, or to inhibit self-growth during stress [38]. These toxins operate through diverse mechanisms, targeting essential cellular processes such as DNA replication, translation, and cell envelope integrity [39] [38]. To systematically organize knowledge on these molecular weapons, several specialized database resources have been developed. This guide provides an objective comparison of these databases, with a focus on the prokaryotic antimicrobial toxin database (PAT) and other key resources, supporting experimental data on their application, and detailed protocols for their use in cross-kingdom comparative research.
Comparative Analysis of Major Toxin and Resistance Databases
Researchers have several databases at their disposal, each with a specific focus. The table below provides a quantitative comparison of their scope and content.
Table 1: Comparative Overview of Toxin and Resistance Mechanism Databases
| Database Name | Primary Focus | Number of Toxins/ Antitoxins Cataloged | Key Features | Organismal Focus |
|---|---|---|---|---|
| Toxinome [38] | Comprehensive bacterial protein toxins and antitoxins | 1,483,028 toxins; 491,345 antitoxins | Integrates data from multiple resources; identifies "Toxin Islands"; maps to 59,475 bacterial genomes | Bacteria |
| PAT (Prokaryotic Antimicrobial Toxin Database) [38] | Bacterial and archaeal toxins from select classes | 441 toxins (from 7 classes) | Focus on bacteriocins and T6SS effectors; contains predicted toxins | Prokaryotes (Bacteria & Archaea) |
| TADB [39] [38] | Type II Toxin-Antitoxin Systems | Not explicitly stated in results | Dedicated to a specific, widespread class of TA systems; well-curated | Prokaryotes |
| SecRet6 [38] | Type VI Secretion System (T6SS) effectors | Not explicitly stated in results | Specialized database for toxins delivered via the T6SS | Mostly Proteobacteria |
| BACTIBASE/BAGEL4 [38] | Bacteriocins | Not explicitly stated in results | Resources focused on ribosomally synthesized antimicrobial peptides | Bacteria |
The Toxinome database represents the most comprehensive effort, cataloging nearly two million toxins and antitoxins from across the bacterial tree of life [38]. In contrast, the PAT database is more focused, containing a smaller, curated set of toxins from specific classes, with a notable emphasis on bacteriocins and T6SS effectors found in proteobacteria [38]. Specialized resources like TADB and SecRet6 offer deep curation for specific toxin mechanisms, namely Type II toxin-antitoxin systems and T6SS effectors, respectively [39] [38]. A critical functional insight from Toxinome is the identification of 5,161 Toxin Islands—genomic loci densely clustered with toxin and antitoxin genes, which serve as hotspots for discovering novel toxin-associated genes [38].
Experimental Applications: Comparing Toxin Effects Across Kingdoms
Specialized databases provide the foundational data for designing experiments that elucidate differential resistance mechanisms. A key study on iodinated X-ray contrast media (ICM) exemplifies this approach, directly comparing toxicity mechanisms in prokaryotic (E. coli) and eukaryotic (yeast) models [40].
Detailed Experimental Protocol for Cross-Kingdom Toxicity Assessment
Objective: To compare the toxicity mechanisms of chemical stressors (e.g., ICM) between prokaryotic and eukaryotic cells, quantifying molecular and phenotypic endpoints [40].
Materials:
- Test Organisms: Prokaryote: Escherichia coli; Eukaryote: Saccharomyces cerevisiae (yeast).
- Stressors: Ionic and non-ionic iodinated contrast media.
- Key Reagents: Microarray kits for transcriptomics, ROS detection assays, cytotoxicity assay kits.
Methodology:
- Exposure: Expose log-phase cultures of E. coli and yeast to a range of concentrations of the ICM compounds for defined durations.
- Phenotypic Endpoint Analysis:
- Cytotoxicity: Measure conventional endpoints such as cell viability or growth inhibition using metabolic assays.
- Reactive Oxygen Species (ROS): Quantify intracellular ROS levels using fluorescent probes.
- Molecular Endpoint Analysis (Toxicogenomics):
- Microarray Assay: Extract total RNA from control and exposed cells.
- Data Quantification: Hybridize labeled cDNA to genome-wide microarray chips.
- Index Calculation: Compute a Transcriptional Effect Level Index (TELI) for E. coli and a Protein Effect Level Index (PELI) for yeast from the altered gene/protein expression profiles. These indices integrate the magnitude and significance of changes across multiple biomarkers [40].
- Data Correlation and Analysis: Statistically correlate molecular indices (TELI, PELI) with phenotypic endpoints (cytotoxicity, ROS) to establish a quantitative relationship between gene/protein expression changes and observable damage [40].
The application of this protocol yielded clear, quantitative differences in how prokaryotes and eukaryotes respond to the same toxins.
Table 2: Summary of Experimental Findings from ICM Exposure Study [40]
| Parameter | Prokaryote (E. coli) | Eukaryote (Yeast) |
|---|---|---|
| Overall Susceptibility | Lower | Higher |
| Stress Intensity | Significantly lower | Significantly higher |
| Diversity of Stress Types | Less diverse | More diverse |
| Toxicity of Ionic vs Non-Ionic ICM | Ionic ICM is more toxic than non-ionic | Ionic ICM is more toxic than non-ionic |
| Correlation between Molecular & Phenotypic Endpoints | Extremely high | Extremely high |
The study demonstrated that the toxic mechanisms are concentration-dependent and relevant to the cellular structure and defense systems inherent to each domain of life [40]. Crucially, the high correlation between molecular and phenotypic endpoints validates the use of toxicogenomic data from databases to predict tangible biological outcomes.
Visualization of Core Concepts and Workflows
Toxin-Antitoxin System Regulation and Function
The following diagram illustrates the genetic structure and functional regulation of a typical Type II Toxin-Antitoxin (TA) system, a key element in prokaryotic biology and a major component of many toxin databases [39].
Toxin-Antitoxin System Regulation
Cross-Kingdom Toxicity Assessment Workflow
This workflow outlines the experimental protocol for comparing toxin effects and resistance mechanisms in prokaryotic and eukaryotic models, as described in Section 3.1.
Cross-Kingdom Toxicity Workflow
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials essential for conducting experiments in toxin biology and resistance mechanism research, as inferred from the cited methodologies.
Table 3: Essential Reagents for Toxin and Resistance Mechanism Research
| Reagent/Material | Function in Research | Example Application |
|---|---|---|
| Bacterial & Eukaryotic Model Cells | Serve as test organisms for toxicity and resistance assays. | Using E. coli (prokaryote) and S. cerevisiae (yeast) for comparative studies [40]. |
| Clustered Toxin Gene Sequences | Act as references for identifying novel toxins via homology and domain analysis. | Identifying unannotated genes in Toxin Islands as potential novel toxins [38]. |
| Microarray or RNA-seq Kits | Enable transcriptomic profiling to determine molecular toxicity endpoints. | Quantifying changes in gene expression to compute a Transcriptional Effect Level Index (TELI) [40]. |
| ROS Detection Assay Kits | Measure reactive oxygen species generation, a common phenotypic response to toxin-induced stress. | Correlating molecular changes with oxidative stress in cells exposed to iodinated contrast media [40]. |
| Cytotoxicity/Cell Viability Assays | Quantify the overall phenotypic effect of a toxin on cell health and proliferation. | Measuring growth inhibition in E. coli and yeast as a conventional phenotypic endpoint [40]. |
| Protein Domain Databases (e.g., Pfam) | Provide curated models (HMMs) to identify toxin and antitoxin domains in genomic data. | Expanding the Toxinome database by mapping 219 toxin and 94 antitoxin domains to bacterial genes [38]. |
The evolving landscape of toxin databases, from specialized resources to comprehensive platforms like Toxinome, provides researchers with powerful tools to catalog and understand the complex interplay of microbial toxins and host resistance mechanisms. The supporting experimental data clearly demonstrates fundamental differences in how prokaryotic and eukaryotic cells perceive and respond to toxic insults, a critical consideration for drug development. These database resources, when used in conjunction with the detailed experimental protocols and reagents outlined in this guide, empower scientists to systematically decode the logic of toxin resistance across the tree of life.
Toxin-antitoxin (TA) modules are simple genetic elements ubiquitous in bacteria and archaea, composed of a stable toxin protein that inhibits essential cellular processes and a labile antitoxin that neutralizes its cognate toxin [41]. Originally discovered as "addiction modules" ensuring plasmid maintenance in bacterial populations, these systems are now recognized as versatile stress-response switches that modulate bacterial physiology, impacting biofilm formation, persistence, and multidrug tolerance [41] [5]. The abundance of TA modules in major bacterial pathogens, coupled with their central role in antibiotic tolerance, positions them as compelling targets for novel antibacterial strategies [41] [42]. This guide provides a comparative assessment of TA systems, focusing on their mechanisms, functions, and therapeutic potential, framed within the broader context of prokaryotic toxin resistance mechanisms.
Comparative Classification and Mechanisms of TA Systems
TA systems are classified into eight types (I-VIII) based on the molecular nature of the antitoxin and its mode of toxin inhibition [41] [43]. Among these, Type II systems are the most extensively characterized and will be the primary focus of this comparative analysis.
Table 1: Classification of Toxin-Antitoxin Systems
| Type | Toxin | Antitoxin | Mechanism of Antitoxin Action | Key Features |
|---|---|---|---|---|
| I | Protein | Antisense RNA | Binds toxin mRNA, inhibiting translation [44] | Toxins often small, membrane-targeting proteins [44] |
| II | Protein | Protein | Forms complex with toxin, inhibiting its activity [41] [45] | Most diverse and well-studied class; toxins are enzymes [41] [42] |
| III | Protein | RNA | Directly binds and neutralizes toxin protein [43] | Antitoxin RNA does not require translation to function [43] |
| IV | Protein | Protein | Competes with toxin for the same cellular target [45] | Antitoxin does not directly interact with the toxin [45] |
| V | Protein | Protein | Cleaves toxin mRNA, preventing toxin synthesis [43] | Antitoxin acts as an RNAse [43] |
| VI | Protein | Protein | Mediates proteolytic degradation of the toxin [43] | Direct elimination of the toxin component [43] |
| VII | Protein | Protein | Enzymatically neutralizes toxin activity [43] | Newly described system [43] |
| VIII | RNA | Antisense RNA | Binds and neutralizes toxin RNA [43] | Only known system where the toxin is RNA [43] |
Type II toxins exhibit remarkable diversity, primarily targeting the central dogma of molecular biology, with translation being a favorite target.
Table 2: Mechanisms of Action of Type II Toxins
| Cellular Target | Toxin Family Examples | Molecular Mechanism | Physiological Outcome |
|---|---|---|---|
| Translation | MazF, RelE, VapC, HigB | mRNA cleavage at specific sequences; tRNA cleavage; rRNA damage [45] | Global inhibition of protein synthesis; growth arrest [41] [45] |
| DNA Replication | CcdB, ParE | Inhibition of DNA gyrase, blocking DNA replication [44] [46] | Inhibition of cell division; cell death [44] |
| Cell Division | - | Interference with cytoskeleton formation [41] | Disruption of cell division [41] |
| Membrane Integrity | Hok | Membrane binding, inhibiting respiration [47] | Loss of membrane potential; cell death [47] |
| tRNA Machinery | HipA | Phosphorylation of glutamyl-tRNA synthetase or EF-Tu [44] [45] | Inhibition of translation via tRNA charging/delivery [45] |
The following diagram illustrates the general genetic structure and regulatory logic of a Type II TA module.
Figure 1: Regulatory Logic of a Type II TA Module. Under normal conditions, the toxin-antitoxin complex represses its own transcription. Stress conditions activate proteases (Lon/ClpP) that degrade the labile antitoxin, freeing the stable toxin to inhibit growth.
Experimental Analysis of TA System Function
Key Experimental Models and Workflows
Research on TA systems employs both genetic/molecular biology techniques and competitive fitness assays to elucidate function and potential. A common workflow for validating TA system activation and its physiological impact is outlined below.
Figure 2: General Workflow for TA System Experimental Analysis.
Intracellular Plasmid Competition Assay
A pivotal experiment demonstrating the fitness advantage conferred by TA systems, particularly when combined with partitioning systems, involves intracellular plasmid competition [47].
Protocol:
- Strain and Plasmid Construction: Engineer two competing plasmids with identical backbones but differing stability traits (e.g., one with a TA system like hok/sok, another with a partition system like parMRC, and a third with both), and different antibiotic resistance markers (e.g., Kanamycin vs. Chloramphenicol) [47].
- Co-transformation: Co-transform a recipient bacterial strain (e.g., E. coli) with the two competing plasmids and plate under double antibiotic selection to ensure all colonies harbor both plasmids [47].
- Competition Passage: Inoculate co-transformants into liquid media and serially passage for approximately 50 generations in the absence of antibiotic selection, allowing for plasmid loss and competition [47].
- Outcome Analysis: Plate the final population on non-selective and selective media to determine the frequency of hosts homoplasmic for each plasmid, heteroplasmic hosts, and plasmid-free cells. The plasmid found in a higher frequency of homoplasmic hosts is considered more fit [47].
Key Data: This method directly showed that plasmids harboring both a TA system and an active partition system have superior fitness compared to those with either system alone, explaining their prevalence in large, low-copy-number plasmids [47].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for TA System Research
| Reagent / Solution | Function in Research | Example Application |
|---|---|---|
| Inducible Expression Plasmids | Allows controlled, high-level expression of toxin genes to study their effects in the absence of antitoxin [42]. | Functional characterization of a putative toxin's cellular target and phenotypic outcome. |
| Gene Deletion Mutants | Enables the study of phenotypic changes (e.g., persistence, biofilm) upon removal of specific TA loci from the chromosome [41] [45]. | Assessing the contribution of a specific TA system to antibiotic tolerance. |
| Lon Protease Inhibitors | Chemical tools to block the primary protease pathway for antitoxin degradation, preventing TA system activation [46]. | Probing the role of Lon-mediated activation in stress response. |
| Fluorescent Reporter Fusions | Reporters fused to TA promoters allow real-time monitoring of TA system activation at the single-cell level [45]. | Investigating stochastic activation and heterogeneity in persister formation. |
| Antisense Oligonucleotides | Synthetic oligos designed to target and block the translation of antitoxin mRNA, artificially activating the toxin [42] [43]. | Validation of TA systems as antibacterial targets. |
Comparative Assessment of Therapeutic Strategies
Targeting TA modules for antibacterial therapy involves strategies to artificially trigger toxin activation in pathogens, leading to growth arrest or death. These approaches can be directly compared based on their mechanism and stage of development.
Table 4: Comparison of Therapeutic Strategies Targeting TA Systems
| Therapeutic Strategy | Molecular Mechanism | Experimental Evidence | Advantages & Challenges |
|---|---|---|---|
| Peptide Inhibitors | Short peptides mimicking the toxin's binding site on the antitoxin, disrupting the TA complex and freeing the toxin [42]. | Proof-of-concept studies showing induced bacterial growth inhibition in culture [42]. | Advantage: High specificity. Challenge: Delivery into bacterial cells. |
| Antisense Oligonucleotides | Synthetic oligonucleotides that bind antitoxin mRNA, blocking its translation and preventing synthesis of new antitoxin [42] [43]. | Demonstrated activation of toxin lethality in the absence of antitoxin in model bacteria [43]. | Advantage: Rational design against any target. Challenge: Stability and delivery in vivo. |
| Protease Activation | Small molecules that enhance the activity of cellular proteases (e.g., Lon), accelerating the natural degradation of antitoxins [46]. | RNA-Seq data shows TA upregulation under conditions of Lon induction (e.g., rifampicin treatment) [46]. | Advantage: Exploits native bacterial pathways. Challenge: Risk of off-target effects. |
| TA System Delivery | Delivery of cloned toxin genes into bacteria via phage or plasmid vectors to intoxicate target cells from within [43]. | Successful killing of P. aeruginosa using recombinant toxin genes [43]. | Advantage: Potent, direct lethality. Challenge: Specific delivery mechanism required. |
The following diagram synthesizes these strategies into a unified view of the therapeutic targeting pathways.
Figure 3: Pathways for Therapeutically Activating TA Systems. Multiple strategies can artificially induce toxin activation by preventing antitoxin synthesis, disrupting the TA complex, or introducing new toxin genes.
The comprehensive comparative assessment presented in this guide underscores the potential of TA systems as novel therapeutic targets. The data reveals that Type II systems, with their diverse enzymatic activities and central role in bacterial persistence, are particularly promising. The experimental evidence from plasmid competition assays confirms the potent fitness advantage provided by TA systems, explaining their prevalence in pathogenic genomes [47]. While challenges remain—particularly in drug delivery and understanding the nuanced biology of chromosomal systems—the strategic artificial activation of these "intracellular molecular bombs" represents a paradigm shift in combating multidrug-resistant bacterial infections [42]. Future work should focus on optimizing delivery mechanisms for TA-targeting therapeutics and further elucidating the complex regulatory networks that govern TA activation in different bacterial pathogens.
The engineering of toxin resistance represents a frontier in biotechnology, offering solutions for protecting crops against pests and improving the safety of medical therapies. The strategies employed, however, differ profoundly depending on whether the target is a prokaryote (bacteria, archaea) or a eukaryote (plants, animals, fungi). This divergence stems from fundamental biological differences. Prokaryotes often utilize horizontal gene transfer for rapid adaptation, possess efflux pump complexes in their cell envelopes to remove toxins, and have simpler genetic systems that can be directly targeted [48] [49]. In contrast, eukaryotes rely more on vertical inheritance of resistance traits, possess complex internal membrane systems and organelles for sequestration, and can employ sophisticated mechanisms like RNA interference (RNAi) to silence genes critical for toxin action [7] [50]. This guide provides a comparative assessment of the experimental approaches, performance data, and reagent toolsets used to engineer toxin resistance in these two domains of life.
Engineering Resistance in Agricultural Systems
Prokaryotic Toxins in Plant Protection
A major application of prokaryotic toxins in agriculture is the use of Bt (Bacillus thuringiensis) proteins in genetically modified crops like corn and cotton. These bacterial toxins are lethal to specific insect pests but safe for humans and wildlife [51] [52].
Experimental Protocol for Monitoring Field-Evolved Resistance: The efficacy of Bt crops is routinely assessed through long-term field monitoring.
- Sample Collection: Millions of target pests (e.g., corn rootworm, pink bollworm) are collected from georeferenced fields across agricultural regions over multiple growing seasons [51] [50].
- Bioassay: Insects are exposed to artificial diet or plant tissue containing a range of Bt toxin concentrations.
- Resistance Assessment: Mortality rates are recorded and compared to susceptible control populations. A significant decrease in mortality indicates field-evolved resistance [52].
- Molecular Analysis (in some cases): Genomic DNA from resistant insects is sequenced to identify mutations in genes coding for toxin-binding sites in the insect midgut.
Performance Data: The table below summarizes the performance of successive generations of Bt crops and the corresponding pest resistance.
Table 1: Evolution of Bt Crop Performance Against Pest Resistance
| Technology Generation | Toxin Mechanism | Target Pests | Initial Efficacy | Emergence of Field-Resistant Pests | Key Evidence |
|---|---|---|---|---|---|
| First-Generation Bt Crops | Single Bt protein (e.g., Cry1Ac) | Lepidopteran pests (bollworms), Coleopteran pests (rootworms) | Highly effective, >99% control | ~5-8 years | Survival of pink bollworm on Bt cotton in India; corn rootworm in the U.S. Corn Belt [51] [52] |
| Pyramided Bt Crops | Two or more distinct Bt proteins (e.g., Cry1Ac + Cry2Ab) | Same as above | High, intended to delay resistance | ~15 years | Resistance to both Cry1Ac and Cry2Ab in pink bollworm in India [52] |
| Bt + RNAi Stack | Bt protein + RNA interference | Corn rootworm | High in lab conditions | Reduced efficacy in fields with pre-existing Bt resistance | University of Arizona analysis of multi-state field data showed less root protection where Bt resistance existed [51] [50] |
Eukaryotic RNA Interference (RNAi) as a Novel Strategy
RNAi is a eukaryotic defense mechanism that has been co-opted for engineering pest resistance in crops. It works by producing double-stranded RNA (dsRNA) that, when ingested by a pest, silences a gene essential for its survival [50].
- Experimental Protocol for RNAi-Based Pest Control:
- Target Gene Identification: Select an essential pest gene (e.g., for growth, development, or detoxification) with low similarity to non-target organism genes.
- dsRNA Synthesis: Synthesize a dsRNA fragment complementary to a portion of the target gene mRNA.
- Efficacy Testing:
- In vitro: Feed the dsRNA to pests in an artificial diet and observe mortality or growth inhibition.
- In planta: Genetically engineer crop plants to express the pest-specific dsRNA.
- Field Trials: Assess the protection of the engineered crop from pest damage and yield loss under natural conditions.
The following diagram illustrates the logical workflow and mechanism of this RNAi-based strategy.
Engineering Resistance in Medical contexts
Prokaryotic Toxins as Therapeutic Agents and Targets
In medicine, prokaryotic toxins are both a threat and a tool. Pathogenic bacteria use toxin-efflux pumps to develop antibiotic resistance, while engineered toxins can be used to target cancer cells.
Experimental Protocol: Disrupting Bacterial Efflux Pumps with Physical Force A novel approach to countering toxin resistance in bacteria involves targeting the mechanical integrity of their efflux systems [49].
- Device Fabrication: Create a microfluidic device with channels narrower than the bacteria.
- Bacterial Stressing: Flow bacteria (e.g., E. coli) through the constricted channels, subjecting them to known mechanical shear forces and deformation.
- Pump Function Assay: Use single-molecule fluorescence imaging (e.g., with a tagged pump component) to monitor the assembly and disassembly of efflux pump complexes like AcrAB-TolC in real-time.
- Viability Assay: Expose mechanically stressed bacteria to toxins (antibiotics) and measure the resulting cell death compared to unstressed controls.
Performance Data: The study found that mechanical stress alone compromised efflux complexes, making bacteria more susceptible to toxins. This demonstrates that mechanobiology is a new tool to combat prokaryotic toxin resistance [49].
Engineering Eukaryotic Cells for Therapeutic Safety
A key challenge in drug development is that many potent therapeutic proteins, derived from prokaryotes, are toxic to human cells. Engineering resistance into human cells is therefore crucial.
- Experimental Protocol: Universal Toxin-Based Selection in Human Cells
This method selects for human cells that have been successfully genome-edited by making them resistant to Diphtheria Toxin (DT) [53].
- Target Identification: Identify the human gene encoding the DT receptor, heparin-binding EGF-like growth factor (HBEGF).
- Precise Genome Editing: Use CRISPR-based base editors (CBE or ABE) to introduce a single nucleotide change in HBEGF that disrupts DT binding (e.g., Glu141Lys or Tyr123Cys).
- Co-selection: Co-transfect cells with the HBEGF-targeting editor and a second editor targeting a separate therapeutic gene of interest.
- DT Application: Treat the cell population with a lethal dose of DT. Only cells with a successfully edited HBEGF locus (and a high likelihood of also having the second edit) survive.
- Validation: Sequence the genomic DNA of the DT-resistant population to quantify the enrichment of edits at the second, therapeutic locus.
The workflow and molecular mechanism of this powerful selection strategy are detailed below.
- Performance Data: This DT-based selection method robustly enriches for precise genome edits.
Table 2: Efficacy of Diphtheria Toxin Selection for Enriching Genome Edits
| Editor System | Target Locus | Editing Type | Enrichment in DT-Selected vs. Non-Selected Cells | Key Application |
|---|---|---|---|---|
| CBE3/sgRNA10 | HBEGF (selection) | C-to-T (Glu141Lys) | N/A (Primary selection event) | Creates DT-resistant phenotype [53] |
| CBE3/sgRNA10 | DPM2, EGFR, EMX1, PCSK9, DNMT3B (co-selection) | C-to-T substitution | 4 to 7-fold increase | Enriches for precise base edits at unrelated loci [53] |
| ABE7.10/sgRNA5 | EMX1, CTLA4, IL2RA, AAVS1 (co-selection) | A-to-G substitution | 6 to 13-fold increase | Enriches for precise base edits at unrelated loci [53] |
| SpCas9/sgRNA10 | DPM2, EMX1, PCSK9, DNMT3B (co-selection) | Insertions/Deletions (Indels) | >90% indel rate in selected cells | Enriches for nuclease-mediated gene disruption [53] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Engineering Toxin Resistance
| Reagent / Tool | Function | Application Context |
|---|---|---|
| Bt Toxins (Cry proteins) | Prokaryotic endotoxins that disrupt insect gut membranes. | Selective agent in bioassays; transgene for pest-resistant crops [51] [52]. |
| dsRNA / siRNA | Triggers RNA interference by silencing complementary mRNA sequences. | Molecular reagent for functional genetics in pests; transgene for RNAi crops [50]. |
| Diphtheria Toxin (DT) | Bacterial exotoxin that inhibits eukaryotic protein synthesis. | Selective agent in cell culture to eliminate non-engineered human cells [53]. |
| CRISPR Base Editors (CBE, ABE) | Engineered fusion proteins that catalyze precise point mutations without double-strand breaks. | Tool for installing toxin-resistance mutations (e.g., in HBEGF) in eukaryotic cells [53]. |
| Microfluidic Shear Device | Applies controlled mechanical forces to single cells. | Tool to study mechanobiology of prokaryotic efflux pumps and disrupt their function [49]. |
| Toxinome Database | A comprehensive database of nearly 1.5 million bacterial toxins and antitoxins. | In silico resource for identifying novel toxin targets and understanding resistance evolution [38]. |
The comparative assessment of toxin resistance engineering reveals a clear paradigm: success hinges on a deep understanding of the fundamental biology of the target organism. In prokaryotes, strategies often focus on disrupting physical structures like efflux pumps or exploiting horizontal gene transfer networks. In eukaryotes, precision is paramount, leveraging sophisticated cellular machinery like RNAi and employing base editors to install protective mutations with single-nucleotide resolution. The experimental data show that while these technologies are powerful—enabling multi-fold enrichment of edited cells or durable crop protection—they are not impervious to evolutionary counter-strategies. The ongoing arms race with resistant pests and the need for safer cell and gene therapies will continue to drive innovation, likely through the combination of the approaches outlined in this guide, such as stacking Bt with RNAi in crops or using multiple selection pressures in medical applications.
Overcoming Resistance: Addressing AMR and Therapeutic Failures
Antimicrobial resistance (AMR) represents one of the most pressing global health threats of the 21st century, undermining the effectiveness of life-saving treatments and placing populations at heightened risk from common infections and routine medical interventions. The World Health Organization (WHO) has documented that approximately one in six laboratory-confirmed bacterial infections is now caused by bacteria resistant to antibiotics, with annual deaths attributable to AMR predicted to rise from 4.71 million in 2021 to 8.22 million by 2050 [54] [55]. This "silent pandemic" constitutes a profound evolutionary response by microorganisms to the widespread, and often indiscriminate, use of antimicrobial compounds [56]. From a clinical perspective, the rise of multidrug-resistant (MDR) and extensively drug-resistant (XDR) phenotypes in pathogens like methicillin-resistant Staphylococcus aureus (MRSA), carbapenem-resistant Klebsiella pneumoniae, and drug-resistant Pseudomonas aeruginosa has created major concerns for healthcare systems worldwide [57] [58].
The comparative analysis of resistance mechanisms between prokaryotic and eukaryotic microorganisms reveals both convergent evolutionary strategies and distinct molecular pathways shaped by fundamental biological differences. While prokaryotes (bacteria) and eukaryotes (fungi, protozoa) share common resistance strategies such as efflux pumps and target modification, their genetic regulation, cellular machinery, and evolutionary trajectories differ significantly. Understanding these distinctions is critical for developing next-generation antimicrobials that can overcome resistance. This review provides a comprehensive comparative assessment of toxin resistance mechanisms in prokaryotic and eukaryotic microorganisms, examining their molecular basis, experimental methodologies for investigation, and emerging therapeutic approaches to combat the escalating AMR crisis.
Molecular Mechanisms of Multidrug Resistance: A Comparative Analysis
Prokaryotic Resistance Mechanisms
Bacterial pathogens have evolved sophisticated genetic and biochemical mechanisms to withstand antimicrobial pressure. The primary molecular strategies include enzymatic inactivation of drugs, overexpression of efflux systems, target site modification, and reduced permeability. β-lactamases (such as blaNDM and blaKPC) represent one of the most clinically significant resistance mechanisms, enabling bacteria to hydrolyze β-lactam antibiotics before they can reach their targets [57]. These enzymes work in concert with mobile genetic elements that facilitate the rapid horizontal transfer of resistance genes between bacterial species, accelerating the dissemination of MDR phenotypes.
Efflux pump systems constitute another major resistance mechanism in prokaryotes. Transporters such as MexAB-OprM in Pseudomonas aeruginosa actively export multiple antibiotic classes from the cell, reducing intracellular concentrations to sublethal levels [57]. These pumps often exhibit broad substrate specificity, enabling resistance to unrelated antimicrobial compounds simultaneously. From an evolutionary perspective, the genes encoding these resistance mechanisms are often ancient, having originally evolved in response to natural antimicrobial producers in the environment, but their proliferation and diversification have been dramatically accelerated by human antibiotic use [56].
Eukaryotic Resistance Mechanisms
Eukaryotic microbial pathogens, including fungi like Candida auris and protozoa like Plasmodium falciparum, employ parallel but distinct resistance strategies. The therapeutic challenges for eukaryotic pathogens are particularly acute, as the restricted pipeline of new drug therapies poses considerable risks to global health, especially in the developing world [59]. Antifungal resistance mechanisms in fungi include alterations in drug targets (e.g., mutations in ERG11 for azole resistance), overexpression of efflux pumps (CDR and MDR genes), and biofilm formation that creates physical barriers and phenotypic heterogeneity conferring tolerance [59].
In parasitic protozoa, resistance mechanisms are equally diverse. Plasmodium falciparum, the causative agent of malaria, has developed resistance to nearly all antimalarials, including artemisinin, through mutations in the Kelch13 (K13) protein that likely regulate the parasite's stress response [59]. The pace of resistance emergence in eukaryotic pathogens has been rapid, with the time taken for resistance phenotypes to appear in clinical settings steadily decreasing [56]. This acceleration mirrors trends observed in prokaryotic resistance but is particularly concerning given the more limited arsenal of antifungal and antiparasitic drugs available.
Table 1: Comparative Analysis of Primary Resistance Mechanisms in Prokaryotic and Eukaryotic Microorganisms
| Resistance Mechanism | Prokaryotic Examples | Eukaryotic Examples | Key Features |
|---|---|---|---|
| Enzymatic Inactivation | β-lactamases (blaNDM, blaKPC) [57] | Not commonly reported | Rapid hydrolysis of antibiotics; often plasmid-encoded |
| Efflux Pumps | MexAB-OprM [57]; ATP-binding cassette (ABC) transporters [60] | CDR, MDR genes in Candida [59]; PfCRT in Plasmodium [59] | Broad substrate specificity; energy-dependent transport |
| Target Modification | Mutated DNA gyrase (fluoroquinolone resistance) [58] | ERG11 mutations (azole resistance) [59]; K13 mutations (artemisinin resistance) [59] | Altered drug-binding sites; maintained physiological function |
| Reduced Permeability | Porin mutations in Gram-negatives [57] | Altered membrane sterols in fungi | Decreased intracellular drug accumulation |
| Horizontal Gene Transfer | Plasmid-mediated resistance genes [57] [39] | Limited in eukaryotes; some parasexual exchange in fungi | Rapid dissemination of resistance traits across species |
Evolutionary and Ecological Perspectives
The global dissemination of AMR represents a massive, inadvertent experiment in evolutionary biology, demonstrating how intense selective pressure can drive rapid adaptation in microbial populations [56]. The selection coefficient (s), which measures the relative fitness advantage of resistant strains compared to susceptible ones under antimicrobial pressure, helps explain the rapid proliferation of resistance. However, the concept of "selective efficiency" provides a more nuanced framework that considers not just the advantage of resistance but also its genetic, metabolic, ecological, and evolutionary costs to the microorganism [56].
From this perspective, resistance mechanisms that provide protection with minimal fitness cost (such as upregulation of existing efflux systems) are particularly likely to persist and spread. The contrast between the widespread global distribution of resistance genes and the apparent rarity of therapeutically useful antimicrobial production phenotypes highlights the evolutionary efficiency of resistance mechanisms [56]. Furthermore, environmental factors, including the use of antimicrobials in agriculture and inappropriate waste management, create complex ecological networks that facilitate the emergence and dissemination of resistance across human, animal, and environmental reservoirs [58].
Experimental Approaches for Investigating Resistance Mechanisms
Genomic and Transcriptomic Methodologies
Advanced genomic technologies have revolutionized our understanding of AMR mechanisms in both prokaryotic and eukaryotic microorganisms. Comparative genomic analyses enable researchers to identify mutations associated with resistance phenotypes, while transcriptomic approaches reveal how microorganisms regulate gene expression in response to antimicrobial challenge.
For prokaryotes, the comprehensive comparative-genomic analysis of toxin-antitoxin (TA) systems has provided insights into their role in stress response and potential persistence mechanisms [39]. Type II toxin-antitoxin systems, in which both toxin and antitoxin are proteins, are particularly widespread in prokaryotes and represent selfish genetic elements that can affect cell fate under stress conditions [39]. Experimental protocols for identifying these systems involve sensitive methods for distant sequence similarity searches, genome context analysis, and specialized approaches for identifying mobile two-component systems.
For eukaryotic pathogens, studies of artemisinin resistance in Plasmodium falciparum have employed population transcriptomics to identify the molecular mechanisms underlying resistance [59]. The identification of K13-propeller mutations as markers of artemisinin resistance demonstrated how genomic approaches can reveal resistance mechanisms even when the precise biochemical pathway is not fully understood. These methodologies typically involve parasite isolation from patient blood samples, RNA extraction, sequencing library preparation, and computational analysis to identify differentially expressed genes or mutations associated with resistance.
Table 2: Key Experimental Methodologies for Investigating AMR Mechanisms
| Methodology | Application in Prokaryotes | Application in Eukaryotes | Key Outputs |
|---|---|---|---|
| Whole Genome Sequencing | Identification of resistance mutations and mobile genetic elements [39] | Detection of single nucleotide polymorphisms (e.g., K13 in Plasmodium) [59] | Comprehensive mutational landscape; phylogenetic relationships |
| RNA Sequencing | Analysis of efflux pump and β-lactamase expression regulation [57] | Assessment of stress response and resistance gene expression [59] | Transcriptional profiles; differentially expressed genes |
| Toxicogenomics Microarrays | E. coli microarray assays for toxicity mechanisms [40] | Yeast microarray assays for comparative toxicology [40] | Gene/protein biomarker levels; damage/repair pathway regulation |
| Protein Structure Analysis | β-lactamase enzyme characterization [57] | Drug target modeling (e.g., fungal CYP51) [59] | Drug-target interactions; resistance-associated conformational changes |
| Phenotypic Assays | MIC determination; efflux pump activity assays [57] | Growth inhibition assays; persistence quantification [59] | Resistance levels; susceptibility profiles |
Phenotypic and Functional Assays
Complementing genomic approaches, phenotypic assays provide critical functional validation of suspected resistance mechanisms. For both prokaryotes and eukaryotes, minimum inhibitory concentration (MIC) determinations remain the gold standard for assessing resistance levels. However, more sophisticated assays have been developed to investigate specific mechanisms.
For efflux pump activity, assays using fluorescent substrates with and without pump inhibitors can quantify transport activity in both bacterial and fungal pathogens [57]. For enzyme-mediated resistance, biochemical assays directly measure antibiotic modification or degradation. In eukaryotic pathogens, specialized assays have been developed to measure phenomena like antifungal tolerance in Candida albicans biofilms, which produce antifungal-tolerant persister cells through mechanisms that may differ from genetic resistance [59].
A particularly informative approach involves comparative toxicology studies using prokaryotic and eukaryotic model systems. Recent research compared the toxicity mechanisms of iodinated contrast media on E. coli (prokaryote) and yeast (eukaryote) using microarray assays, conventional phenotypic endpoint cytotoxicity, and reactive oxygen species (ROS) measurements [40]. This study demonstrated that eukaryotes are generally more susceptible to toxicity than prokaryotes, with significantly higher stress intensity and diverse stress types observed in yeast cells compared to E. coli when exposed to the same compounds [40]. The correlation between molecular toxicity endpoints (Transcriptional Effect Level Index and Protein Effect Level Index) and phenotypic endpoints was extremely high, validating the integration of multiple assay types for comprehensive resistance mechanism characterization.
Research Reagent Solutions for AMR Investigations
The experimental investigation of antimicrobial resistance mechanisms requires specialized reagents and tools tailored to the distinct biology of prokaryotic and eukaryotic microorganisms. The following table details essential research materials for AMR research, their applications, and considerations for use in different microbial systems.
Table 3: Essential Research Reagents for Investigating Antimicrobial Resistance Mechanisms
| Reagent/Tool | Function | Prokaryotic Applications | Eukaryotic Applications |
|---|---|---|---|
| Growth Media & Supplements | Culture maintenance and experimental propagation | Mueller-Hinton broth/agar for standardized AST [58] | RPMI 1640 for fungal susceptibility testing [59] |
| Antimicrobial Compounds | Selective pressure for resistance studies | WHO-recommended antibiotics for surveillance [55] | Clinical antifungals (azoles, echinocandins) [59] |
| DNA/RNA Extraction Kits | Nucleic acid isolation for molecular analyses | Protocols optimized for bacterial cell wall lysis | Methods for fungal cell wall disruption or parasite isolation |
| Whole Genome Sequencing Kits | Comprehensive genetic characterization | Pan-bacterial sequencing; plasmid isolation [39] | Parasite or fungal genome sequencing [59] |
| qPCR Reagents & Primers | Gene expression quantification | Efflux pump and β-lactamase gene expression [57] | Resistance gene expression (ERG11, K13) [59] |
| Efflux Pump Substrates & Inhibitors | Functional analysis of transport activity | Ethidium bromide; carbonyl cyanide m-chlorophenyl hydrazone (CCCP) [57] | Rhodamine 6G; cyclosporine A for fungal ABC transporters [59] |
| Antibodies for Western Blot | Protein detection and quantification | β-lactamase enzyme detection [57] | Detection of resistance markers (PfCRT, CYP51) [59] |
| Cell Viability Assays | Quantification of microbial survival | Live/dead staining; resazurin reduction assays | MTT/XTT assays for fungal viability [40] |
| ROS Detection Probes | Oxidative stress measurement | DCFH-DA for bacterial oxidative stress [40] | Dihydroethidium for fungal ROS detection [40] |
Visualization of Experimental Workflows and Signaling Pathways
Comparative Experimental Workflow for AMR Mechanism Investigation
The following diagram illustrates an integrated experimental workflow for investigating antimicrobial resistance mechanisms in prokaryotic and eukaryotic microorganisms, highlighting parallel approaches and key decision points.
Diagram 1: Integrated workflow for AMR mechanism investigation in prokaryotic and eukaryotic pathogens.
Comparative Resistance Mechanism Pathways
This diagram compares the primary molecular resistance pathways in prokaryotic and eukaryotic microorganisms, highlighting convergent strategies and distinct features.
Diagram 2: Comparative resistance pathways in prokaryotic and eukaryotic microorganisms.
Emerging Solutions and Future Directions
The escalating AMR crisis has stimulated innovative approaches to combat resistance in both prokaryotic and eukaryotic pathogens. Artificial intelligence (AI) and machine learning are revolutionizing antimicrobial discovery and resistance monitoring. At IDWeek 2025, researchers highlighted AI multi-agent systems that mine pathogen genomes for novel essential targets, generate first-pass inhibitor scaffolds, and evaluate pharmacologic liabilities before wet-lab experimentation [61]. These approaches are being applied to both antibacterial and antifungal development, with the goal of designing compounds that target resistance-proof pathways.
Novel therapeutic modalities are also emerging. Bacteriophage therapy, CRISPR-based genome editing to selectively eliminate resistance genes, and antimicrobial peptides represent promising alternatives to conventional antibiotics [57]. For eukaryotic pathogens, combination therapies have proven successful in slowing resistance emergence, as demonstrated by artemisinin combination therapy for malaria and nifurtimox-eflornithine combination for African trypanosomiasis [59]. The Fleming Initiative, a groundbreaking collaboration between Imperial College London and GSK, exemplifies the large-scale, coordinated effort needed to address AMR, with research programs targeting WHO priority pathogens using advanced AI and novel therapeutic approaches [54].
Surveillance and stewardship remain critical components of AMR management. The WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS) supports standardized data collection from member countries, providing essential information to guide public health action [55]. The integration of AI-driven resistance dashboards that continuously learn from antibiograms, culture data, and prescribing patterns offers the potential for real-time resistance monitoring and more targeted intervention strategies [61].
The global AMR crisis represents a complex evolutionary and ecological challenge that demands a comprehensive understanding of resistance mechanisms across both prokaryotic and eukaryotic microorganisms. While these pathogen classes employ conceptually similar resistance strategies—efflux, target modification, enzymatic inactivation, and reduced permeability—their distinct cellular biologies and genetic architectures result in different mechanistic implementations and evolutionary trajectories. The comparative assessment of these mechanisms reveals both universal principles of microbial adaptation and unique features that must be considered in therapeutic development.
The future of AMR management will require integrated approaches combining basic science, clinical practice, public health policy, and innovative technology. AI-driven discovery platforms, enhanced surveillance systems, novel therapeutic modalities, and improved stewardship practices offer promising pathways forward. As emphasized by the Fleming Initiative, addressing the AMR crisis will require sustained collaboration across academic, industrial, clinical, and public health sectors globally [54]. The coordinated application of scientific innovation, economic investment, and political will is essential to prevent the feared "post-antibiotic era" from becoming a reality.
The perpetual struggle between hosts and pathogens represents one of the most powerful evolutionary forces shaping biological systems across all domains of life. Pathogens, including bacteria, viruses, and eukaryotic parasites, employ sophisticated strategies to detect, evade, subvert, and ultimately bypass the sophisticated defense mechanisms of their eukaryotic hosts. This ongoing co-evolutionary arms race has driven the diversification of immune systems in eukaryotes and the corresponding development of evasion mechanisms in pathogens [62] [63]. The fundamental imperative for survival has selected for an astonishing array of molecular weaponry on both sides, with pathogens devising methods to overcome everything from physical barriers to complex adaptive immune responses. Understanding these evasion strategies provides not only fundamental insights into host-pathogen interactions but also reveals potential therapeutic targets for combating infectious diseases. This comparative analysis examines the principal mechanisms through which pathogens circumvent eukaryotic defenses, highlighting the convergent evolutionary solutions that have emerged across diverse pathogen taxa and the experimental approaches driving their discovery.
Eukaryotic Defense Systems: The Targets of Subversion
Layered Immunity in Eukaryotes
Eukaryotes possess a multi-layered defense system comprising innate and adaptive components that pathogens must overcome to establish successful infection. The innate immune system serves as the first line of defense, featuring physical barriers like skin and mucous membranes, chemical defenses such as antimicrobial peptides, and cellular components including phagocytes and pattern recognition receptors (PRRs) that detect conserved pathogen-associated molecular patterns (PAMPs) [64] [65]. PRRs include diverse protein families such as Toll-like receptors (TLRs), NOD-like receptors (NLRs), and various cytosolic DNA and RNA sensors that initiate inflammatory responses upon pathogen detection [62] [66]. The more recently evolved adaptive immune system, found in vertebrates, provides highly specific, long-lasting protection through antigen-specific B and T lymphocytes, generating immunological memory that enables rapid response upon re-exposure to previously encountered pathogens [67].
Core Defense Mechanisms Across Eukaryotes
Despite tremendous diversity among eukaryotic organisms, several defense mechanisms are deeply conserved across evolutionary history. Pattern recognition receptors that detect bacterial signatures often utilize a limited set of protein domains that have been reused and repurposed throughout eukaryotic evolution [62]. Core microbicidal strategies include production of reactive oxygen species via NADPH oxidases, antimicrobial peptides that disrupt microbial membranes, lysozymes that degrade bacterial cell walls, and autophagy mechanisms that sequester and destroy intracellular invaders [62]. Comparative genomic analyses reveal that many components of eukaryotic immune systems have origins in prokaryotic defense mechanisms, with structural homologs of human innate immune proteins identified in bacterial anti-phage systems [66] [64]. For instance, the cGAS-STING pathway, crucial for cytosolic DNA sensing in mammals, shares evolutionary roots with bacterial cGAS/DncV-like nucleotidyltransferases (CD-NTases) that function in anti-phage defense [66].
Table 1: Evolutionarily Conserved Eukaryotic Defense Mechanisms
| Defense Mechanism | Key Components | Evolutionary Origin | Pathogen Targets |
|---|---|---|---|
| Pattern Recognition | TLRs, NLRs, Lectins | Present in LECA*; some domains reused across lineages | Bacterial surfaces, viral nucleic acids, fungal cell walls |
| Antimicrobial Peptides | Defensins, Cathelicidins | Present in LECA; independently evolved in multiple groups | Bacterial membranes, fungal membranes |
| Reactive Oxygen Species | NADPH oxidases | Present in LECA | Broad-spectrum antimicrobial activity |
| Phagocytosis | Actin cytoskeleton, phagosomes | Early eukaryotic innovation | Bacteria, large particles, apoptotic cells |
| Autophagy | ATG proteins, autophagosomes | Present in LECA | Intracellular bacteria, viruses |
| RNA Interference | Dicer, Argonaute, RISC | Prokaryotic Argonaute ancestry | Viral RNA, transposable elements |
LECA: Last Eukaryotic Common Ancestor [62]
Pathogen Evasion Strategies: Mechanisms and Examples
Pathogens have evolved a remarkable diversity of strategies to overcome eukaryotic defenses, often targeting multiple components of the immune system simultaneously. These evasion mechanisms can be categorized based on their molecular targets and functional consequences.
Antigenic Variation: Staying Ahead of Recognition
One of the most sophisticated evasion strategies is antigenic variation, wherein pathogens alter their surface antigens to evade antibody recognition and immune memory. This strategy takes several forms across different pathogen types. The influenza virus employs both antigenic drift, caused by accumulation of point mutations in surface proteins hemagglutinin and neuraminidase, and antigenic shift, resulting from reassortment of genomic segments between different viral strains, leading to major pandemic outbreaks [67]. African trypanosomes, which cause sleeping sickness, utilize a more complex system involving approximately 1000 variant surface glycoprotein (VSG) genes, with only one expressed at a time through programmed DNA rearrangements that switch expression to a new VSG gene when immune pressure mounts [67]. Bacterial pathogens including Neisseria gonorrhoeae and Salmonella typhimurium also employ antigenic variation through DNA rearrangements that alter surface structures like pili and flagellin, enabling persistence within infected hosts despite robust immune responses [67].
Latency and Persistence: Hiding from Immune Surveillance
Many pathogens establish long-term infections by entering dormant states that minimize their visibility to the immune system. Herpesviruses, including herpes simplex virus (HSV) and varicella zoster virus (VZV), establish latency in neuronal cells where viral gene expression is largely silenced, eliminating production of viral peptides that would otherwise flag infected cells for T-cell recognition [67]. The low expression of MHC class I molecules on neurons further enhances this hiding strategy. Epstein-Barr virus (EBV) establishes latency in B cells, expressing only a limited set of viral proteins, including EBNA-1, which cleverly avoids proteasomal degradation and thus prevents presentation of viral peptides to CD8+ T cells [67]. Bacterial pathogens can form persister populations that survive antibiotic treatment without genetic resistance, a phenomenon observed in Plasmodium falciparum malaria parasites and fungal biofilms of Candida albicans [68]. These persister cells may result from stochastic gene expression changes that prepare subpopulations for survival under stress conditions, or from environmental signals that induce dormancy.
Direct Interference with Immune Function
Many pathogens actively disrupt immune signaling and effector mechanisms through molecular sabotage. Leishmania parasites directly suppress host immunity by inhibiting transcription of the pro-inflammatory cytokine IL-12, blunting the development of protective immune responses [65]. Bacterial pathogens like Escherichia coli, Shigella flexnerii, and Yersinia pestis employ specialized secretion systems (Type III secretion) that inject bacterial effector proteins directly into host cells, disrupting signaling pathways and inducing apoptosis [65]. Bacillus anthracis produces lethal factor (LF) and edema factor (EF) toxins that enter host cells via protective antigen (PA), with LF cleaving mitogen-activated protein kinase kinases (MAPKKs) to disrupt cellular signaling and protein synthesis, while EF acts as a calmodulin-dependent adenylate cyclase that disrupts cellular physiology [65]. HIV directly targets CD4+ T-cells, gradually depleting these central coordinators of adaptive immunity and compromising the host's ability to mount effective immune responses against other pathogens [65].
Table 2: Major Pathogen Evasion Strategies and Representative Examples
| Evasion Strategy | Molecular Mechanism | Pathogen Examples | Experimental Evidence |
|---|---|---|---|
| Antigenic Variation | Surface protein alteration through mutation or DNA rearrangement | Influenza virus, African trypanosomes, Neisseria gonorrhoeae | Serological typing, genomic sequencing, animal models [67] |
| Latency/Persistence | Reduced metabolic activity, limited gene expression | Herpesviruses, Plasmodium falciparum, Candida albicans | Cell culture models, animal infection models, patient samples [67] [68] |
| Immune Suppression | Inhibition of cytokine production, immune cell depletion | Leishmania spp., HIV, Bacillus anthracis | Cytokine assays, flow cytometry, transcriptional analysis [65] |
| Intracellular Sequestration | Residence within protective cellular niches | Mycobacterium tuberculosis, Listeria monocytogenes | Cell culture infection models, microscopy, intracellular survival assays [63] |
| Molecular Mimicry | Imitation of host structures to avoid detection | Streptococcal M protein, various viral proteins | Structural biology, antibody cross-reactivity studies [63] |
| Secretion System Effectors | Injection of virulence proteins into host cells | Yersinia pestis, Pseudomonas aeruginosa | Bacterial genetics, protein interaction studies, cell biology [65] |
Comparative Experimental Analysis: Methodologies and Findings
Experimental Models for Studying Immune Evasion
Research into pathogen evasion mechanisms employs diverse experimental systems ranging from prokaryotic models to complex eukaryotic hosts. Studies of bacterial anti-phage systems have revealed unexpected similarities with eukaryotic innate immunity, including structural homologs of human cGAS and STING proteins that function in bacterial defense against viruses [66]. The discovery of these systems was facilitated by bioinformatic analyses of "defense islands" in microbial genomes and functional screening approaches [66]. Zebrafish embryo models have been used to study conserved defense responses, revealing that both prokaryotes and eukaryotes can recognize and respond to specific DNA sequences such as 5′-GTTTGTT-3′ found in plasmids and viral genomes [69]. Injection of plasmid pEGFP-N1 into zebrafish zygotes triggered upregulation of immune response genes including isg15, while mutation of the core recognition sequence abolished this response, demonstrating a conserved nucleic acid sensing mechanism [69]. Cell culture models using human cell lines (HEK 293T, HCT116) have confirmed these findings, showing similar sequence-specific responses to foreign DNA [69].
Signaling Pathways in Host-Pathogen Interactions
The complex interplay between host defenses and pathogen countermeasures revolves around key signaling pathways that detect infection and coordinate responses. The following diagram illustrates central pathways in eukaryotic anti-pathogen defense and major points of pathogen subversion:
Diagram 1: Eukaryotic Immune Signaling and Pathogen Evasion Points. This diagram illustrates the core signaling pathway activated by pathogen detection in eukaryotic cells (green nodes) and the major strategies pathogens employ to disrupt these signals (red nodes).
The Scientist's Toolkit: Essential Research Reagents
Investigating host-pathogen interactions requires specialized reagents and tools designed to probe specific aspects of immune recognition and evasion. The following table summarizes key research solutions used in this field:
Table 3: Essential Research Reagents for Studying Immune Evasion Mechanisms
| Research Reagent | Composition/Type | Experimental Function | Example Applications |
|---|---|---|---|
| Pattern Recognition Receptor Agonists | Synthetic lipids, carbohydrates, nucleic acids | Activate specific PRRs to study downstream signaling | TLR4 activation by LPS, cGAS activation by dsDNA [66] |
| Cytokine ELISA Kits | Antibody pairs, standards, detection reagents | Quantify cytokine production in response to infection | Measure IFN-β, IL-6, TNF-α in cell supernatants [69] |
| Reporter Cell Lines | Genetically engineered cells with promoter-reporter constructs | Monitor activation of specific signaling pathways | IFN-stimulated response element (ISRE) reporters [69] |
| Neutralizing Antibodies | Monoclonal antibodies against immune components | Block specific immune molecules to assess function | Anti-IFNAR antibodies to block type I IFN signaling [67] |
| CRISPR/Cas9 Gene Editing Systems | Cas9 nuclease, guide RNAs, repair templates | Generate knockout cell lines of immune genes | Create PRR-deficient cells to study pathway requirements [64] |
| Pathogen-associated Molecular Patterns | Purified microbial components (LPS, flagellin, CpG DNA) | Stimulate immune responses in experimental systems | Study PRR signaling in isolation [66] |
| Protein Translation Inhibitors | Small molecules (cycloheximide, anisomycin) | Block host protein synthesis to study requirements | Distinguish direct vs. indirect pathogen effects [68] |
Discussion: Evolutionary Patterns and Therapeutic Implications
Convergent Evolution of Evasion Mechanisms
The struggle between hosts and pathogens has led to remarkable examples of convergent evolution, where distantly related pathogens have developed similar solutions to the challenge of eukaryotic immunity. The independent evolution of NLR-like proteins in both plants and animals demonstrates how similar immune sensing architectures can arise separately in different eukaryotic lineages [62]. Similarly, bacterial and eukaryotic innate immune systems show striking thematic parallels despite vast evolutionary distance, with both employing cytosolic nucleic acid sensors and pore-forming proteins that induce cell death upon infection [64]. The discovery that components of the human cGAS-STING pathway share evolutionary roots with bacterial anti-phage defense systems illustrates how ancient mechanisms can be repurposed across domains of life [66] [70]. This evolutionary conservation provides opportunities for developing broad-spectrum therapeutic approaches that target fundamental mechanisms of immune recognition or pathogen evasion.
Experimental Challenges and Future Directions
Studying pathogen evasion mechanisms presents significant methodological challenges, including the species-specificity of many host-pathogen interactions and the technical limitations of accurately modeling complex immune environments in vitro [68] [69]. The phenomenon of persister cell populations that survive treatment without genetic resistance poses particular difficulties for experimental analysis and therapeutic development [68]. Future research directions include developing more sophisticated organoid and tissue culture systems that better recapitulate the tissue microenvironment, applying single-cell technologies to analyze heterogeneous pathogen and host cell populations, and employing structural biology approaches to understand the molecular details of pathogen effector proteins and their host targets [68] [63]. Additionally, comparative studies across broader evolutionary ranges may reveal novel evasion strategies and deepen our understanding of the fundamental principles governing host-pathogen interactions.
Pathogens have evolved an extraordinary diversity of mechanisms to bypass eukaryotic defenses, ranging from antigenic variation and latency to direct interference with immune signaling components. These evasion strategies highlight the powerful selective pressures exerted by host immune systems and demonstrate remarkable examples of convergent evolution across pathogen taxa. The experimental investigation of these mechanisms relies on sophisticated tools including animal models, cell culture systems, and molecular biology techniques that enable researchers to dissect the complex interplay between host and pathogen. Understanding these evasion strategies not only provides fundamental insights into host-pathogen co-evolution but also identifies potential vulnerabilities that could be exploited therapeutically. As pathogens continue to evolve new ways to circumvent host defenses, ongoing research into these mechanisms remains essential for developing next-generation antimicrobial therapies and vaccine strategies.
The relentless emergence of resistance constitutes the most significant challenge in modern therapeutic development, particularly in oncology and anti-infective fields. This arms race between therapeutic intervention and adaptive biological systems demands strategies that anticipate and circumvent resistance mechanisms before they undermine clinical efficacy. The fundamental differences in cellular organization between prokaryotes and eukaryrates have profound implications for how resistance evolves, necessitating distinct yet complementary therapeutic approaches. In prokaryotic systems like bacteria, resistance often emerges through rapid horizontal gene transfer and high mutation rates, enabling swift population-level adaptation to environmental toxins. Conversely, eukaryotic resistance in human cancers frequently arises through clonal evolution and genomic instability, selecting for survival advantages within heterogeneous tumor populations. Understanding these divergent evolutionary trajectories provides the conceptual foundation for designing next-generation therapeutics that proactively address resistance rather than reactively responding to its emergence.
This comparative assessment examines innovative strategies being deployed to overcome resistance across biological domains, with particular focus on structural optimization of therapeutic molecules, exploitation of synthetic lethality, and manipulation of bacterial virulence pathways. The following analysis synthesizes experimental data and clinical evidence to objectively evaluate competing approaches for extending therapeutic durability against adaptive biological systems increasingly skilled at evading targeted interventions.
Comparative Analysis of Resistance Mechanisms: Prokaryotic vs. Eukaryotic Systems
Fundamental Divergence in Resistance Evolution
The structural and functional dichotomy between prokaryotic and eukaryotic cells establishes fundamentally different landscapes for resistance development. Prokaryotic resistance typically employs efficient efflux systems, enzymatic inactivation of therapeutics, and target modification through mutation or enzymatic alteration. The simpler cellular architecture of prokaryotes, while potentially offering fewer defensive options, enables more rapid generational turnover and consequently faster evolutionary adaptation. This is particularly evident in antibiotic resistance, where horizontal gene transfer allows resistance determinants to spread rapidly through bacterial populations independent of reproductive cycles.
In contrast, eukaryotic resistance mechanisms in human cancers exploit complex cellular machinery, including enhanced DNA repair pathways, drug efflux pumps, apoptotic evasion, and activation of alternative signaling cascades. The regulatory sophistication of eukaryotic cells provides more potential nodes for therapeutic intervention but simultaneously creates more numerous bypass routes for resistant clones. Cancer therapeutics face the additional challenge of tumor heterogeneity, where pre-existing resistant subclones undergo selective expansion under therapeutic pressure.
Table 1: Comparative Analysis of Primary Resistance Mechanisms in Prokaryotic vs. Eukaryotic Systems
| Characteristic | Prokaryotic Systems | Eukaryotic Systems |
|---|---|---|
| Primary Resistance Mechanisms | Enzymatic inactivation, Target modification, Efflux pumps, Reduced permeability | Target mutation, Bypass signaling pathways, Efflux transporters, Apoptotic evasion, Epigenetic adaptation |
| Genetic Flexibility | High (rapid division, horizontal gene transfer) | Moderate (genomic instability, clonal selection) |
| Cellular Compartmentalization | Limited (no organelles) | Extensive (membrane-bound organelles) |
| Key Adaptive Advantage | Speed of adaptation | Diversity of escape routes |
| Representative Therapeutic Challenge | MRSA resistance to multiple antibiotics | EGFR-mutant NSCLC resistance to tyrosine kinase inhibitors |
Quantitative Assessment of Resistance-Overcoming Therapeutics
Recent therapeutic advances have produced several clinical candidates specifically designed to address established resistance mechanisms. The following table synthesizes performance data for selected therapeutics that have demonstrated efficacy against resistant pathogens or malignancies in preclinical and clinical studies.
Table 2: Experimental Performance Data of Selected Therapeutics Against Resistant Models
| Therapeutic Agent | Target | Resistance Mechanism Addressed | Experimental Model | Key Efficacy Metric | Result |
|---|---|---|---|---|---|
| Streptoclipamide A [71] | ClpP protease | MRSA virulence regulation | MRSA-infected mouse pneumonia model | Host survival rate | Significant improvement vs. control |
| HLX97 [72] | KAT6A/B | Hormone resistance in breast cancer | ZR-75-1 xenograft model | Tumor growth inhibition | Dose-dependent efficacy with minimal weight loss |
| AK112 (PD-1/VEGF双抗) [73] | PD-1/VEGF | PD-L1 low expression in NSCLC | Phase III clinical (1L sqNSCLC) | mPFS in PD-L1 TPS<1% | 8.7 months |
| Sac-TMT (TROP2 ADC) [73] | TROP2 | EGFR-TKI resistance in NSCLC | Phase III clinical (3L EGFRm NSCLC) | mPFS vs. standard care | 13.4 months vs. 4.3 months |
| Iza-bren (EGFR/HER3 ADC) [73] | EGFR/HER3 | EGFR C797S, T790M, Exon20ins | I/II clinical (EGFRm NSCLC) | ORR in resistance mutations | 100% |
| HLX43 (PD-L1 ADC) [74] | PD-L1 | PD-1/PD-L1 therapy resistance | Preclinical models | Tumor growth inhibition | Significant activity in resistant models |
Experimental Protocols: Methodologies for Evaluating Resistance Interventions
Protocol 1: Assessment of Anti-Virulence Compounds Against MRSA
Objective: To evaluate the efficacy of ClpP protease inhibitors in reducing MRSA virulence and restoring antibiotic susceptibility [71].
Materials and Methods:
- Bacterial Strains: MRSA clinical isolates with confirmed virulence phenotypes
- Test Compound: Streptoclipamide A (480 nM IC₅₀ against ClpP)
- Control Interventions: Vancomycin (standard care), Vehicle control
- In Vitro Assays:
- Fluorescence-Based Protease Activity: ClpP protease inhibition measured using fluorogenic substrates
- Virulence Factor Quantification: α-hemolysin expression via immunoblotting
- Gene Expression Analysis: RNAIII, agrA, saeR transcript levels by qRT-PCR
- In Vivo Models:
- G. mellonella Infection Model: Larvae infected with MRSA, treated with compound alone or in combination
- Mouse Pneumonia Model: Immunocompetent mice infected intranasally with MRSA, therapeutic administration at 6h post-infection
Experimental Workflow:
- In vitro determination of IC₅₀ against purified ClpP protease
- Assessment of impact on bacterial growth kinetics (OD₆₀₀)
- Quantification of virulence factor suppression (hemolysin production)
- Evaluation of transcriptomic changes in virulence regulons
- Therapeutic efficacy assessment in animal infection models
- Histopathological analysis of tissue damage and inflammatory infiltration
Protocol 2: Evaluating ADC Efficacy in EGFR-TKI Resistant NSCLC
Objective: To determine the activity of novel ADC constructs against EGFR-mutant NSCLC with acquired resistance to tyrosine kinase inhibitors [73].
Materials and Methods:
- Cell Models:
- EGFR-mutant NSCLC lines with confirmed TKI resistance (including C797S, T790M, MET amplification)
- Patient-derived organoids (PDOs) from TKI-resistant patients
- Test Articles:
- Iza-bren (EGFR/HER3 ADC with novel microtubule inhibitor payload)
- Control ADCs (DS-8201 analog)
- In Vitro Assays:
- Cell Viability: ATP-based quantification after 72h drug exposure
- Apoptosis Assessment: Annexin V/PI flow cytometry
- Mechanism Studies: Immunoblotting for pHER3, total HER3, and downstream signaling
- In Vivo Models:
- CDX Models: HCC827-OR (osimertinib-resistant) xenografts
- PDX Models: Clinically relevant resistance variants
- Metastasis Models: Intracardiac injection for brain metastasis assessment
Experimental Endpoints:
- In vitro IC₅₀ determination across resistance variants
- Bystander killing effects in co-culture systems
- In vivo tumor growth inhibition (T/C ratio) at multiple dose levels
- Biomarker analysis of target expression and pathway modulation
- Toxicity assessment (body weight, hematology, histopathology)
Visualizing Resistance Pathways and Therapeutic Interventions
Prokaryotic Resistance: MRSA Virulence Regulation by ClpP Protease
Eukaryotic Resistance: ADC Bypass of EGFR-TKI Resistance
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Resistance Mechanism Investigation
| Reagent/Platform | Primary Function | Application Context | Key Features |
|---|---|---|---|
| Dual-Promoter Single Plasmid System [75] | Coordinated heavy/light chain expression | Complex antibody production (bispecifics) | Reduces chain mispairing, improves yield |
| Expi293-F/ExpiCHO-S Cells [75] | Eukaryotic protein expression host | Recombinant antibody production | High-density transient expression, human-like glycosylation |
| Patient-Derived Organoids (PDOs) [73] | Patient-specific disease modeling | ADC efficacy testing in resistant tumors | Preserves tumor heterogeneity, predicts clinical response |
| Fluorogenic Peptide Substrates [71] | Protease activity quantification | ClpP inhibitor screening | High sensitivity, real-time kinetic measurements |
| WGCNA Algorithm [76] | Gene co-expression network analysis | Transcriptomic profiling under toxin stress | Identifies key regulatory modules and hub genes |
| MetaPhlAn4 Tool [77] | Microbiome composition analysis | Strain-level microbial tracking | High taxonomic precision, database comprehensiveness |
Despite the fundamental differences between prokaryotic and eukaryotic resistance mechanisms, several convergent therapeutic principles emerge from this comparative analysis. First, successful resistance-countering strategies increasingly employ multi-target approaches that simultaneously engage primary targets and resistance pathways, exemplified by bispecific antibodies and dual-target ADCs. Second, the strategic deployment of combination therapies that attack cellular vulnerabilities from multiple angles demonstrates superior durability compared to sequential monotherapies, as evidenced by the synergy between anti-virulence compounds and conventional antibiotics. Third, diagnostic-forward therapeutic development that anticipates resistance through comprehensive molecular profiling enables more proactive rather than reactive intervention strategies.
The most promising developments recognize that resistance is not merely a technical hurdle but an evolutionary inevitability under selective therapeutic pressure. Consequently, the next generation of anti-resistance strategies must incorporate evolutionary principles into therapeutic design, employing approaches that minimize selective advantages for resistant subpopulations while maximizing therapeutic durability. This paradigm shift from reactive to proactive resistance management represents the most promising frontier in therapeutic optimization across both prokaryotic and eukaryotic domains.
Diagnostic and Regulatory Hurdles in Developing Anti-Toxin Therapies
Anti-toxin therapies, which include antitoxins and antivenoms, are specialized biologics designed to neutralize toxins produced by pathogens or delivered by venomous creatures. These therapies function primarily as passive immunotherapies, introducing pre-formed antibodies or antibody fragments that bind with high specificity to target toxins, preventing their interaction with cellular receptors and subsequent pathogenic cascades [78]. The development landscape for these therapies presents a unique set of diagnostic and regulatory challenges that distinguish them from conventional drug development pathways. These hurdles stem from the acute nature of toxin exposures, the rarity of many toxin-mediated conditions, and the complex biological origins of therapeutic agents themselves [78] [79].
Framing this discussion within a comparative assessment of toxin resistance mechanisms reveals a fundamental dichotomy: prokaryotes and eukaryotes have evolved dramatically different defensive strategies. Prokaryotes employ primarily genetic and enzymatic resistance mechanisms, often encoded on mobile genetic elements that facilitate rapid horizontal transfer of toxin-neutralizing capabilities [80]. In contrast, eukaryotes have developed sophisticated adaptive immune systems capable of producing highly specific neutralizing antibodies, which form the basis for all current anti-toxin therapies [78] [79]. This distinction underpins both the therapeutic approach and the developmental challenges in creating effective anti-toxin treatments.
Current FDA-Approved Anti-Toxins and Their Characteristics
The United States Food and Drug Administration (FDA) maintains stringent approval requirements for biologics, including anti-toxins. The regulatory pathway involves an Investigational New Drug (IND) application followed by extensive clinical trials and a Biologics License Application (BLA) that scrutinizes manufacturing processes, safety profiles, and demonstrated efficacy [78]. Within this rigorous framework, only a select number of anti-toxin products have received FDA approval, as detailed in Table 1.
Table 1: Currently FDA-Approved Anti-Toxin Therapies
| Product Name | Target Toxin | Manufacturer | First FDA Approval | Indication | Key Characteristics |
|---|---|---|---|---|---|
| Botulism Antitoxin Heptavalent (A, B, C, D, E, F, G) - (Equine) | Botulinum neurotoxin serotypes A-G | Emergent BioSolutions Canada, Inc. | March 2013 | Treatment of suspected botulism | Broad-spectrum coverage against all seven known botulinum toxin serotypes; equine-derived [78] |
| Centruroides (Scorpion) Immune F(ab′)₂ | Venom of Centruroides scorpions | Rare Disease Therapeutics, Inc. | August 2011 | Treatment of scorpion envenomation | Uses F(ab′)₂ antibody fragments; orphan drug designation [78] |
The approval process for these products faced unique challenges compared to conventional therapeutics. For conditions like botulism and scorpion envenomation, the low incidence of cases makes large-scale randomized controlled trials impractical [78]. Regulatory evaluations therefore relied heavily on animal models and surrogate endpoints, with the FDA adopting flexible approaches to assess clinical outcomes without compromising safety standards [78]. Additionally, manufacturing consistency presents particular challenges for biologics derived from biological sources like equine serum, requiring meticulous oversight to ensure batch-to-batch consistency in neutralization capacity [78].
Diagnostic Hurdles in Anti-Toxin Development
Toxin Identification and Characterization Challenges
The initial diagnostic hurdle in anti-toxin development involves comprehensive toxin identification and characterization. Toxins exist in diverse structural variants with different mechanisms of pathogenicity, complicating the design of broadly effective therapeutics. For example, botulinum toxin has seven distinct serotypes (A-G) with varying prevalence and pathological effects [78] [81]. Similar diversity exists among scorpion venoms and bacterial exotoxins, requiring sophisticated analytical techniques for proper characterization [79].
Advanced methods being employed include high-throughput screening (HTS) combined with next-generation sequencing (NGS) to rapidly identify and characterize antibody candidates from combinatorial libraries [79]. Structural biology techniques such as cryo-electron microscopy (cryo-EM) and X-ray crystallography enable detailed mapping of epitope-paratope interactions, ensuring engineered neutralizing molecules are precisely targeted [79]. These methodologies allow researchers to address the fundamental challenge of toxin diversity while developing therapeutics with appropriate specificity profiles.
Preclinical Assessment Methodologies
Table 2: Key Experimental Protocols in Anti-Toxin Development
| Methodology | Application | Technical Approach | Output Metrics |
|---|---|---|---|
| Neutralization Assays | Efficacy assessment of antitoxin candidates | In vitro exposure of toxins to antitoxins followed by cell-based viability assays | IC50 values; percentage neutralization at specific concentrations |
| Affinity Measurement | Binding characterization | Surface plasmon resonance (SPR) and isothermal titration calorimetry (ITC) | Binding constants (KD), association/dissociation rates |
| Structural Characterization | Epitope mapping | X-ray crystallography; cryo-electron microscopy | Atomic-resolution structures of toxin-antitoxin complexes |
| Animal Challenge Models | In vivo efficacy | Controlled administration of toxin followed by antitoxin treatment at varying timepoints | Survival rates; symptom progression; minimum effective dose |
The transition from in vitro characterization to in vivo models presents significant methodological challenges. Animal models must recapitulate human toxin exposure and pathophysiology, yet many toxins act rapidly with narrow therapeutic windows [79]. This necessitates carefully timed administration protocols and precise dosing regimens. For botulinum toxin, which causes flaccid paralysis by blocking acetylcholine release at neuromuscular junctions, animal models typically monitor time to onset and progression of paralysis following toxin challenge and subsequent antitoxin administration [81]. These models must account for serotype-specific differences in toxin potency and mechanism [78] [81].
Regulatory Framework and Hurdles
Unique Regulatory Challenges for Anti-Toxins
The regulatory pathway for anti-toxin therapies faces distinctive challenges that stem from both scientific and practical considerations. Unlike chronic conditions where therapeutic effects can be measured over time, anti-toxins must demonstrate efficacy in acute scenarios where timely intervention is critical [78]. This creates evidentiary challenges, as traditional randomized controlled trials are often ethically and practically impossible for acute toxin exposures [78]. Regulatory agencies like the FDA must therefore evaluate applications based on animal model data, in vitro neutralization studies, and sometimes historical controls rather than large-scale human trials [78].
Manufacturing consistency represents another significant regulatory hurdle. Anti-toxins derived from biological sources (such as equine serum for botulism antitoxin) face inherent batch-to-batch variability [78]. Regulatory reviews therefore meticulously scrutinize manufacturing processes, purification protocols, and quality control measures to ensure consistent potency, purity, and safety across production batches [78]. The application of Good Manufacturing Practice (GMP) guidelines to these biologically-derived products requires specialized expertise and rigorous oversight [79].
Economic and Market Barriers
Beyond scientific and regulatory challenges, anti-toxin development faces substantial economic barriers. The relatively rare incidence of many toxin exposures compared to chronic diseases limits market incentives for development [78] [79]. Development costs for anti-toxins are comparable to other biologics, with similar manufacturing complexities and regulatory requirements, yet the potential return on investment is significantly constrained by the limited patient populations [79]. This economic reality has led to many anti-toxin products receiving orphan drug designation, which provides certain incentives but doesn't fully address the market limitations [78].
The economic challenges are particularly pronounced given the high costs of clinical development. One attempted clinical trial for a novel antibiotic (not an antitoxin) was estimated to cost approximately $1 million per recruited patient when targeting a resistant infection [80]. While this example comes from the antibiotic field, it illustrates the extreme costs associated with developing therapies for conditions with limited patient populations. Similar economic pressures affect anti-toxin development, creating a situation where the societal value of these therapies may far exceed their commercial potential [79] [80].
Emerging Solutions and Innovative Approaches
Technological Innovations in Anti-Toxin Design
Novel technological approaches are helping to address some traditional hurdles in anti-toxin development. Recombinant DNA technology enables production of monoclonal antibodies with defined epitopes and optimized neutralizing properties, moving away from animal-derived sera toward more consistent manufactured products [79]. Engineering techniques such as antibody humanization reduce immunogenicity risks, while nanobody technology (using antibody fragments derived from camelids) offers advantages of small molecular size, high stability, and rapid tissue penetration [79].
Advanced engineering approaches include bispecific and multispecific antibodies that can neutralize multiple toxin variants simultaneously or engage immune effector functions to enhance toxin clearance [79]. Some innovative constructs are being designed not only to bind toxins but to catalytically degrade them or sequester them away from critical cellular targets [79]. These technological advances address key limitations of traditional anti-toxins while potentially streamlining regulatory approval through improved safety and consistency profiles.
Diagnostic and Regulatory Pathway Innovations
The integration of rapid diagnostic tests with anti-toxin therapies represents a promising approach to addressing both therapeutic and regulatory challenges. Development of diagnostics that can quickly identify specific toxins involved in an exposure would allow for more targeted antitoxin use and potentially support narrower indications in regulatory submissions [79]. Such companion diagnostics could help address the challenge of toxin variant diversity while providing a more personalized approach to toxin exposure treatment.
From a regulatory perspective, initiatives to streamline approval processes for rare disease therapies have benefitted anti-toxin development [78]. Orphan drug designations, fast-track programs, and the FDA's flexible approaches to efficacy demonstration for acute, rare conditions have helped bring anti-toxins to market despite the challenges of traditional clinical trial designs [78]. Enhanced post-marketing surveillance systems then provide ongoing safety monitoring that complements the pre-approval data package [78] [79].
Research Toolkit for Anti-Toxin Development
Table 3: Essential Research Reagents and Platforms for Anti-Toxin Development
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| Toxin Standards | Reference materials for assays | Purified botulinum serotypes for neutralization assays; standardized venom extracts |
| Immune Libraries | Source of neutralizing antibodies | Phage display libraries; hybridoma collections from immunized animals |
| Cell-Based Assay Systems | In vitro efficacy assessment | Neuronal cell cultures for botulinum toxin; engineered reporter cell lines |
| Animal Models | In vivo efficacy and safety testing | Mouse neutralization models; larger animal models for pharmacokinetic studies |
| Protein Engineering Tools | Antibody optimization | Directed evolution platforms; humanization workflows; affinity maturation systems |
| Analytical Instruments | Characterization | SPR for binding kinetics; HPLC/MS for purity assessment; cryo-EM for structural biology |
The research toolkit for anti-toxin development continues to evolve with technological advancements. Traditional reagents like toxin standards and animal models remain essential, but are now complemented by sophisticated protein engineering platforms and high-resolution analytical instruments [79]. The integration of computational approaches with experimental methods has created a more rational design process for anti-toxin therapies, moving beyond empirical discovery toward engineered solutions [79].
The development of anti-toxin therapies will continue to face significant diagnostic and regulatory hurdles stemming from the acute nature of toxin exposures, the diversity of toxin structures, and the limited commercial incentives for development. However, technological innovations in antibody engineering, diagnostic approaches, and manufacturing processes are creating new pathways to address these challenges [79]. The evolving regulatory landscape for rare disease therapies and biologics also provides a more adaptable framework for evaluating these critical but commercially challenging products [78].
The comparative assessment of toxin resistance mechanisms between prokaryotes and eukaryotes highlights both the biological constraints and opportunities in anti-toxin development. Eukaryotes have evolved the sophisticated immune machinery that provides the foundation for current anti-toxin approaches, but the rapid adaptability of prokaryotic resistance mechanisms presents an ongoing challenge [80]. Future advances will likely need to incorporate elements from both biological strategies—harnessing eukaryotic antibody diversity while embracing the adaptability more characteristic of prokaryotic systems—to create next-generation anti-toxin therapies that can overcome current diagnostic and regulatory hurdles.
Visual Appendix
Anti-Toxin Mechanism of Action
Diagram 1: Anti-Toxin Mechanism of Action. Antitoxins (green) neutralize toxins (red) before they can bind to cellular targets and cause pathogenic effects.
Anti-Toxin Development Workflow
Diagram 2: Anti-Toxin Development Workflow. The multi-stage process from initial toxin characterization through regulatory approval, highlighting key activities at each development phase.
Direct Comparison and Validation of Divergent Evolutionary Paths
The capacity to withstand toxins, antimicrobial compounds, and other stressors is a fundamental characteristic of living organisms, yet the underlying mechanisms differ profoundly across the tree of life. This guide provides a systematic comparison of resistance paradigms in prokaryotic and eukaryotic organisms, framing the analysis within the broader context of evolutionary adaptation to environmental threats. For researchers and drug development professionals, understanding these distinct and convergent strategies is critical for combating antimicrobial resistance and developing novel therapeutic interventions. Resistance mechanisms are broadly categorized into two types: innate resistance, which is an intrinsic, inherited property of a species or strain, and acquired resistance, which is gained through genetic mutations or horizontal gene transfer. This analysis examines the molecular basis, key mechanisms, and experimental approaches for characterizing resistance across these biological domains, leveraging the most current data to inform future research and development.
Molecular Mechanisms of Resistance: A Comparative Analysis
The fundamental structural and genetic differences between prokaryotes and eukaryotes have led to the evolution of distinct resistance strategies. Prokaryotes (e.g., bacteria) utilize mechanisms that often directly counteract the drug's structure or function. In contrast, eukaryotes (including fungi, parasites, and human cells) employ sophisticated systems rooted in their complex cellular biology and immune capabilities [68] [64]. The following sections break down these core mechanisms.
Table 1: Core Resistance Mechanisms in Prokaryotes and Eukaryotes
| Mechanism Category | Prokaryotic Paradigm | Eukaryotic Paradigm |
|---|---|---|
| Target Modification | Alteration of drug-binding sites on bacterial targets (e.g., ribosomes, enzymes) [82]. | Mutations in parasite enzymes (e.g., DHFR for pyrimethamine resistance in Plasmodium) or human kinase targets in cancer [68]. |
| Efflux Pumps | Proton motive force-dependent (e.g., Major Facilitator Superfamily transporter LmrP) or ATP-binding cassette (ABC) transporters (e.g., LmrA) [83]. | ATP-binding Cassette (ABC) transporters and Major Facilitator Superfamily (MFS) transporters in fungal pathogens (e.g., Candida, Aspergillus) [68] [83]. |
| Enzymatic Inactivation | Production of hydrolytic enzymes (e.g., β-lactamases) or modifying enzymes (e.g., aminoglycoside acetyltransferases) [82]. | Parasite-mediated activation of prodrugs into inactive compounds, though less common than in bacteria [68]. |
| Reduced Permeability | Downregulation of porin channels in the outer membrane of Gram-negative bacteria, reducing drug uptake [82]. | Reduced uptake of drugs via transporters in parasitic membranes; not a major mechanism in fungi [68]. |
| Toxin Sequestration/Scavenging | Not commonly reported as a primary mechanism. | Serum-based toxin scavenging (e.g., SVMP Inhibitors in mammals neutralizing snake venom metalloproteinases) [84]. |
| Cellular Persistence | Formation of metabolically dormant persister cells, distinct from genetic resistance [68]. | Parasite dormancy (e.g., Plasmodium hypnozoites) and fungal biofilms contributing to relapsing infections [68]. |
Key Mechanistic Insights
- Efflux Systems are Evolutionarily Conserved: One of the most significant parallels between prokaryotes and eukaryotes is the widespread use of efflux pumps from similar families, such as the ATP-binding cassette (ABC) transporters and the Major Facilitator Superfamily (MFS) [83]. While the energy-coupling mechanisms may differ—proton motive force in some prokaryotes versus ATP hydrolysis in many eukaryotes—the functional outcome of expelling toxic compounds is convergent [83] [82].
- The Persistence Phenomenon: Both domains exhibit persister populations, which are subpopulations of cells that survive antibiotic exposure without acquiring genetic resistance. In bacteria, this is linked to dormancy; in eukaryotic pathogens like Plasmodium falciparum and Candida albicans, it is associated with biofilms and stochastic "bet-hedging" strategies, presenting a major challenge for treatment [68].
- The Innate Immune Bridge: Eukaryotes leverage their innate immune system as a resistance mechanism against toxins, a strategy absent in prokaryotes. This includes mechanical barriers, pattern recognition receptors, and cellular components like phagocytes [85] [86]. Recent research reveals surprising evolutionary links, showing that eukaryotes and prokaryotes share conceptual strategies, such as employing pattern recognition receptors (PRRs) and inducing programmed cell death in response to viral/phage infections [64].
Experimental Protocols for Characterizing Resistance
A systematic approach to studying resistance is vital for accurate diagnosis and research. Below are detailed protocols for key experiments cited in resistance literature.
Protocol 1: Genomic SELEX for Mapping Transcription Factor Binding Sites
This protocol is used to identify the complete set of DNA binding sites for a specific transcription factor, crucial for understanding regulatory networks in prokaryotic resistance [87].
- Library Preparation: Extract and fragment the entire genome of the target prokaryote (e.g., E. coli). Ligate adapters to the fragments for amplification and sequencing.
- Transcription Factor Purification: Clone and express the transcription factor of interest with an affinity tag (e.g., His-tag). Purify the protein using affinity chromatography.
- SELEX Cycle:
- Incubation: Mix the purified transcription factor with the genomic DNA library in a binding buffer.
- Partitioning: Pass the mixture through a nitrocellulose filter. Protein-bound DNA fragments will be retained on the filter, while unbound fragments will pass through.
- Elution and Amplification: Recover the protein-bound DNA fragments from the filter. Amplify the eluted DNA using PCR with primers complementary to the adapters.
- Iteration: Repeat the SELEX cycle (steps a-c) for 5-10 rounds under increasingly stringent conditions (e.g., higher salt concentration, competitor DNA) to enrich for high-affinity binding sites.
- Sequencing and Analysis: Subject the final enriched DNA pool to high-throughput sequencing. Map the sequences back to the reference genome to identify the genomic locations of transcription factor binding sites.
Protocol 2: Assessment of Efflux Pump Activity
This protocol determines the contribution of efflux pumps to resistance in both prokaryotic and eukaryotic cells.
- Sample Preparation:
- Grow bacterial or fungal cells to mid-log phase.
- Divide the culture into two aliquots.
- Efflux Pump Inhibition: Treat one aliquot with a sub-lethal concentration of an efflux pump inhibitor (EPI; e.g., PaβN for Gram-negative bacteria, verapamil for fungi). The other aliquot serves as an untreated control.
- Drug Accumulation Assay:
- Expose both aliquots to a fluorescent substrate of efflux pumps (e.g., ethidium bromide, rhodamine 123).
- Incubate in the dark for a defined period (e.g., 60 minutes).
- Measurement:
- For fluorometry: Wash the cells, resuspend them in buffer, and measure the intracellular fluorescence using a fluorometer.
- For flow cytometry: Analyze the cells directly using a flow cytometer to measure fluorescence on a per-cell basis.
- Data Interpretation: A significant increase in fluorescence in the EPI-treated sample compared to the control indicates active efflux of the substrate. The fold-change in fluorescence is proportional to the efflux pump activity.
Protocol 3: In Vitro Determination of Toxin Resistance (LD50 Shift Assay)
This protocol is used to quantify resistance to a toxin, such as snake venom, in predator-prey systems [84].
- Toxin Preparation: Obtain and lyophilize the crude toxin (e.g., snake venom). Reconstitute in a suitable buffer and determine protein concentration.
- Serum/Plasma Collection: Collect blood from resistant and non-resistant (control) animal models. Allow it to clot and centrifuge to isolate serum, which contains potential resistance factors like neutralizing proteins.
- Pre-incubation: Mix a fixed quantity of the toxin with serial dilutions of the resistant serum or control serum. Incubate the mixtures for 30-60 minutes at 37°C.
- Bioassay:
- Inject the pre-incubated toxin-serum mixtures into a model organism (e.g., laboratory mice) or apply them to a cell culture model.
- For each dilution, record the mortality or cell viability at a predetermined time point.
- Dose-Response Analysis: Calculate the median lethal dose (LD50) of the toxin after pre-incubation with resistant serum and control serum. The ratio of the LD50 (Resistant) to LD50 (Control) represents the fold-increase in resistance conferred by the serum components.
The following workflow summarizes the logical relationship and progression of these key experimental protocols:
Research Reagent Solutions and Essential Materials
A well-equipped toolkit is fundamental for resistance research. The table below details key reagents, their functions, and applicability across prokaryotic and eukaryotic systems.
Table 2: Essential Research Reagents for Resistance Studies
| Reagent/Material | Function in Research | Example Application |
|---|---|---|
| Efflux Pump Inhibitors (EPIs) | Blocks transporter activity to confirm its role in resistance. | PaβN for RND pumps in Gram-negative bacteria; Verapamil for MDR pumps in fungi [82]. |
| Fluorescent Efflux Substrates | Visualizing and quantifying efflux pump activity. | Ethidium bromide, Rhodamine 123 used in fluorometry/flow cytometry assays [82]. |
| Affinity Chromatography Kits | Rapid purification of tagged proteins (e.g., transcription factors). | His-tag purification kits for isolating proteins for Genomic SELEX [87]. |
| Pattern Recognition Receptor (PRR) Agonists | Activating innate immune pathways to study defensive responses. | Synthetic lipopeptides (TLR2 agonists), CpG oligonucleotides (TLR9 agonists) in eukaryotic cells [64]. |
| Defined Genetic Mutant Libraries | Linking genes to resistance phenotypes through systematic screening. | Keio collection (E. coli knockout mutants) or yeast gene deletion collections [87]. |
| Cell Viability/Cytotoxicity Assays | Quantifying the lethal effects of toxins or antimicrobials. | MTT, AlamarBlue, or LDH release assays to determine IC50/LD50 values [68] [84]. |
| High-Quality Reference Toxins | Standardized positive controls for resistance assays. | Lyophilized snake venoms for serum neutralization studies; purified antibiotic standards [84]. |
| CRISPR-Cas9 Gene Editing Systems | Precise knockout or modification of genes to validate resistance mechanisms. | Validating the role of a specific ion channel or enzyme in toxin resistance [64]. |
Visualization of Key Signaling Pathways in Innate Immunity
The innate immune system in eukaryotes and anti-phage defense systems in bacteria show evolutionary parallels. The cGAS-STING pathway, a cornerstone of eukaryotic innate immunity, has functional ancestors in bacterial anti-phage systems. The diagram below illustrates this conserved signaling logic.
This systematic comparison elucidates that while prokaryotic and eukaryotic resistance paradigms are shaped by divergent cellular architectures, they exhibit both fundamental differences and remarkable convergent evolution. Prokaryotes excel in direct, molecular-level countermeasures such as enzymatic inactivation and target modification. Eukaryotes, conversely, integrate resistance with complex organismal defenses, including adaptive immunity and systemic toxin scavenging. The critical convergence on mechanisms like efflux pumps and persistence highlights universal evolutionary pressures. For researchers, the future lies in exploiting these insights—by developing efflux pump inhibitors effective across domains, or by designing combination therapies that target both genetic resistance and persister populations. The experimental frameworks and tools detailed here provide a foundation for such innovative approaches, which are urgently needed to address the escalating global crisis of antimicrobial and chemotherapeutic resistance.
The interaction between predators and prey, or herbivores and their toxic food sources, represents a relentless evolutionary arms race. A quintessential example of this dynamic is the development of resistance to cardiotonic steroids (CTS), a class of potent toxins that includes cardenolides and bufadienolides. These toxins, produced by plants like milkweed and toads as a chemical defense, function by binding to and inhibiting the Na+/K+-ATPase (NKA), an essential transmembrane protein responsible for maintaining electrochemical gradients across cell membranes [88] [89]. The inhibition of this "sodium pump" is fatal to most animals. However, across diverse and phylogenetically divergent species, a remarkable pattern of convergent evolution has emerged: the repeated evolution of resistance through nearly identical molecular solutions. This guide provides a comparative assessment of two primary resistance mechanisms—target site insensitivity via Na+/K+-ATPase mutations and enzymatic inactivation—contrasting their occurrence and experimental characterization in prokaryotic and eukaryotic systems.
Core Mechanisms of Toxin Resistance
Organisms have evolved two primary strategic paradigms to circumvent the action of natural toxins.
- Target Site Insensitivity: This mechanism involves evolutionary alterations to the toxin's molecular target within the organism, reducing the toxin's binding affinity. Resistance to cardiotonic steroids (CTS) via mutations in the Na+/K+-ATPase α-subunit (ATP1A) is a classic example of convergent evolution, documented across insects, amphibians, reptiles, birds, and mammals [90] [88] [89]. Specific amino acid substitutions in the toxin-binding pocket prevent inhibition while preserving the enzyme's essential physiological function.
- Enzymatic Inactivation: This strategy employs enzymes to chemically modify the toxin, rendering it inert. This is a widespread mechanism of antibiotic self-resistance in antibiotic-producing bacteria and a major contributor to clinical antibiotic resistance [91] [92]. The modifications can include detoxification, sequestration, or efflux of the toxic compound.
The following diagram illustrates the logical relationship and key examples of these core resistance mechanisms.
Case Study 1: Na+/K+-ATPase Target Site Insensitivity
The Molecular Basis of Resistance
The Na+/K+-ATPase is a highly conserved enzyme, yet its extracellular H1-H2 loop, which forms part of the CTS-binding pocket, is a hotspot for convergent evolution. Specific amino acid substitutions in this region, particularly at positions 111 and 122 (numbering based on the mature pig enzyme), sterically hinder CTS binding without completely disrupting the pump's ion-transport function [90] [89]. The table below summarizes key resistance-conferring substitutions observed across the animal kingdom.
Table 1: Convergent Amino Acid Substitutions in Na+/K+-ATPase Conferring Cardiotonic Steroid Resistance
| Amino Acid Position | Ancestral (Sensitive) State | Resistant State(s) | Observed In | Key Experimental Findings |
|---|---|---|---|---|
| 111 | Glutamine (Q) | Glutamic Acid (E), Threonine (T), Histidine (H), Leucine (L), Valine (V), Arginine (R) | Insects, Birds, Amphibians, Mammals [90] [88] [93] | Q111V/N122H combination in Drosophila conferred >12-fold resistance compared to wild type [90]. Q111E found in toxin-resistant Crested Serpent-eagle [88]. |
| 122 | Asparagine (N) | Histidine (H), Aspartic Acid (D) | Lepidoptera, Coleoptera, Heteroptera, Diptera, Amphibians [90] [93] | N122H substitution alone increases resistance; effect is synergistic with substitutions at position 111 [90]. |
Experimental Workflow for Characterizing ATP1A Mutations
Research on ATP1A-mediated resistance typically combines evolutionary genetics with functional molecular biology techniques to confirm the phenotypic effect of identified mutations. The standard workflow is summarized below.
Diagram Title: Workflow for Characterizing ATP1A Resistance
Key Research Reagents and Experimental Platforms
The functional characterization of ATP1A mutations relies on a standardized toolkit of molecular biology reagents and experimental platforms.
Table 2: Essential Research Reagents for Investigating ATP1A-Mediated Resistance
| Reagent / Platform | Function in Research | Specific Examples from Literature |
|---|---|---|
| Heterologous Expression Systems | Provides a standardized cellular background to test the function of wild-type and mutant proteins without interference from the native organism's other systems. | HEK293 cells: Used to express mutant Drosophila melanogaster ATP1A, demonstrating 12-fold increased ouabain resistance [90]. |
| Site-Directed Mutagenesis Kits | Enables precise introduction of candidate resistance mutations (e.g., Q111E, N122H) into expression vectors for functional testing. | Used in protein-engineering experiments across tetrapod backgrounds to test effects of substitutions [89] [93]. |
| Cardiotonic Steroids (CTS) | Selective agents used in viability assays and inhibitors used in enzyme kinetics studies to quantify resistance levels. | Ouabain: A standard reference cardenolide used in selection regimes and binding assays [90] [89]. Bufalin: Used in structural studies (PDB 4RES) [89]. |
| Tethered Cell Rotation Assay | Allows direct observation and measurement of flagellar motor function and ion pumping in engineered bacteria. | Used to confirm H+-powered motility in evolved E. coli stator mutant potB G20V [94]. |
Case Study 2: Enzymatic Inactivation in Prokaryotes
The Molecular Basis of Resistance
In prokaryotes, enzymatic inactivation is a dominant and highly diverse resistance mechanism, particularly against antibiotics. Microbes produce a wide array of enzymes that chemically modify antibiotics, rendering them ineffective before they can reach their cellular targets [91] [92]. The table below summarizes major classes of these enzymes.
Table 3: Major Mechanisms of Enzymatic Antibiotic Inactivation in Bacteria
| Antibiotic Class | Resistance Enzyme(s) | Mechanism of Inactivation | Key Experimental Findings |
|---|---|---|---|
| Aminoglycosides | Acetyltransferases (AAC), Nucleotidyltransferases (ANT), Phosphotransferases (APH) [92] | Chemical modification (acetylation, adenylation, phosphorylation) of specific hydroxyl or amino groups on the antibiotic molecule. | Over 50 enzyme variants documented. Modification prevents antibiotic binding to the ribosomal target [92]. |
| β-Lactams | β-Lactamases (e.g., ESBLs, Carbapenemases) [92] | Hydrolysis of the β-lactam ring, the core structural element essential for antibiotic activity. | Genes (e.g., blaCTX-M, blaKPC) are often plasmid-mediated, facilitating rapid horizontal spread. Deletion of blaKPC-2 abolished carbapenem resistance in K. pneumoniae [92]. |
| Chloramphenicol | Chloramphenicol acetyltransferases (CATs) [92] | Acetylation of the antibiotic, preventing its binding to the 50S ribosomal subunit. | A major mechanism of acquired resistance; cat genes are frequently plasmid-encoded [92]. |
| Macrolides | Ere enzymes, Phosphotransferases, Glycosyltransferases | Erythromycin esterase (Ere) hydrolyzes the macrolide lactone; other enzymes phosphorylate or glycosylate the antibiotic [92]. | EreA and EreB are Zn2+-dependent hydrolases that open the macrolide ring, abolishing antibacterial activity [92]. |
Advanced Resistance Models: Temporal-Spatial Shielding
Beyond simple enzymatic degradation, some antibiotic producers employ sophisticated resistance strategies that separate the timing and location of toxic antibiotic activation from the site of biosynthesis, a model known as temporal-spatial shielding [91].
A prime example is the biosynthesis of naphthyridinomycin (NDM). The producer organism utilizes a dual-enzyme system for self-protection:
- Intracellular Detoxification (NapW): The cytosolic enzyme NapW reduces the hemiaminal pharmacophore of the biosynthetic intermediate, maintaining it in a non-toxic form during synthesis [91].
- Extracellular Activation & Control (NapU): The matured prodrug is exported from the cell. The secreted enzyme NapU then oxidizes it into the active antibiotic NDM. NapU can also overoxidize and inactivate NDM, controlling its extracellular concentration and protecting the producer from re-entry of the toxin [91].
This mechanism is summarized in the following pathway diagram.
Diagram Title: Temporal-Spatial Shielding in NDM Biosynthesis
Comparative Analysis: Eukaryotes vs. Prokaryotes
The choice between target site modification and enzymatic inactivation is not random but is influenced by fundamental biological constraints.
Prevalence of Mechanism:
- Target Site Insensitivity is a dominant strategy for eukaryotes facing environmental toxins like CTS, where the target is a self-protein. This is likely because altering a fundamental, highly conserved housekeeping protein like Na+/K+-ATPase is constrained by severe pleiotropy. Mutations must confer resistance without destroying function, limiting the number of viable evolutionary paths [89] [95].
- Enzymatic Inactivation is overwhelmingly the strategy of choice for prokaryotic antibiotic resistance. The ability to horizontally acquire genes encoding efficient modifying enzymes provides a rapid and versatile response to environmental toxins and antibiotics [92].
Genetic and Evolutionary Dynamics:
- Eukaryotes often rely on point mutations in existing genes, leading to convergent evolution at the same amino acid positions in distant lineages (e.g., N122H in insects and mammals) [90] [93]. In some cases, gene duplication and neofunctionalization occur, as seen in Leptodactylus frogs, where one ATP1A1 paralog evolved toxin resistance while the other maintained ancestral function [95].
- Prokaryotes heavily utilize horizontal gene transfer (conjugation, transformation, transduction). Resistance genes, often located on mobile genetic elements like plasmids, transposons, and integrons, can spread rapidly within and across bacterial species, creating a vast and shared "resistome" [92].
Implications for Drug Discovery and Human Health
Understanding these evolutionary mechanisms has direct applications in combating two major health challenges: antibiotic resistance and cancer.
Combating Antibiotic Resistance: The bacterial resistome is the evolutionary precursor to clinical antibiotic resistance genes [91] [92]. Studying self-resistance mechanisms in environmental bacteria can predict future resistance threats in clinics and guide the development of next-generation antibiotics that are less susceptible to existing inactivation enzymes, or inhibitors that can protect existing antibiotics (e.g., β-lactamase inhibitors).
Drug Discovery and Toxicology: The principle of target site insensitivity informs toxicology and pharmacology. For instance, the specific amino acid differences in Na+/K+-ATPase between resistant predators (like the Crested Serpent-eagle) and sensitive species explain differential vulnerability to toxins [88]. Similarly, understanding these mechanisms can aid in the design of drugs that selectively target pathogenic enzymes or pest proteins while sparing the host's orthologs.
The escalating crisis of antimicrobial resistance necessitates robust experimental models to accurately evaluate the efficacy of novel therapeutic agents. The choice between in vitro and in vivo validation systems represents a critical juncture in the drug development pipeline, with each approach offering distinct advantages and limitations for assessing resistance mechanisms in prokaryotic and eukaryotic pathogens. While in vitro models provide controlled, high-throughput screening platforms, they often fail to replicate the complex physiological microenvironments where infections establish. Conversely, in vivo models incorporate host-pathogen interactions but face challenges with translational relevance and ethical considerations. This guide provides a comparative analysis of contemporary experimental models, detailing their applications, methodologies, and data outputs to inform strategic decisions in antimicrobial resistance research.
In Vitro Model Systems
In vitro models serve as the foundational first step for antimicrobial efficacy testing, offering reproducibility, scalability, and controlled conditions for initial screening.
Standard Susceptibility Testing
Conventional in vitro models utilize microtiter plate assays and flow cells to determine minimum inhibitory concentrations (MICs) and assess antimicrobial susceptibility. These systems are cost-effective and amenable to automation but often poorly correlate with in vivo outcomes due to their simplified environments [96]. Standardized antifungal susceptibility testing (AFST) methods from EUCAST and CLSI provide clinical breakpoints for resistance classification, though these may not fully capture tolerance or persistence phenotypes [97].
Table 1: In Vitro Model Comparisons for Resistance Assessment
| Model Type | Key Applications | Advantages | Limitations |
|---|---|---|---|
| Microtiter Plate Assays | MIC determination, high-throughput compound screening | Low cost, standardized, automated | Static conditions, lacks host factors [96] |
| Flow Cell Systems | Biofilm formation, antimicrobial penetration studies | Dynamic fluid flow, mimics some physiological conditions | Complex setup, limited throughput [96] |
| Experimental Evolution | Resistance mechanism mapping, fitness trade-off analysis | Controlled monitoring of adaptation, highly repeatable | Simplified environment lacks host complexity [97] |
| Continuous Culture (Chemostats) | Study of resistance evolution under constant selection pressure | Maintains steady-state growth, controls mutation rates | Equipment intensive, artificial conditions [97] |
Experimental Evolution Models
Experimental evolution has emerged as a powerful methodology for studying resistance dynamics through controlled long-term microbial propagation under selective pressure. This approach allows researchers to monitor the acquisition of resistance in real-time, map associated fitness trade-offs, and identify collateral sensitivity patterns [97]. In pathogenic fungi, serial batch transfer methods have successfully generated numerous resistant replicates to investigate resistance dynamics in Candida glabrata and C. auris, revealing that multidrug resistance often occurs at moderate fitness costs and is mediated by mutations in a limited set of genes [97].
Experimental Protocol: Serial Batch Transfer for Experimental Evolution
- Inoculum Preparation: Start with a susceptible founder strain of known genotype, preferably tagged with a selective marker (e.g., antibiotic resistance, fluorescent protein) for competitive fitness assays.
- Drug Exposure: Propagate replicate populations in media containing sub-inhibitory concentrations of the antimicrobial agent. Include drug-free controls.
- Serial Transfer: At regular intervals (typically 24-72 hours, during mid-log phase), transfer a small aliquot (usually 1:100-1:1000 dilution) of each population to fresh media with identical or escalating drug concentrations.
- Monitoring: Regularly sample and cryopreserve populations to create an evolutionary archive for retrospective analysis.
- Phenotypic Assessment: Periodically determine MIC values and measure competitive fitness against the ancestral strain.
- Genomic Analysis: Sequence endpoint populations or individual clones to identify mutations underlying resistance.
Fitness can be quantified through competitive assays where differentially marked resistant and susceptible strains are co-cultured, with population densities tracked via selective plating, flow cytometry (for fluorescent markers), or quantitative PCR of strain-specific genetic markers [97].
In Vivo Model Systems
In vivo models provide essential physiological context for resistance assessment but face challenges in standardization and clinical translatability.
Animal Infection Models
Mammalian models, particularly murine systems, remain the gold standard for preclinical evaluation of antimicrobial efficacy against resistant pathogens. These models incorporate pharmacokinetic/pharmacodynamic (PK/PD) parameters, host immune responses, and tissue-specific microenvironments that significantly influence resistance development and treatment outcomes [96]. For instance, in vivo experimental evolution in a systemic mouse model demonstrated that even amphotericin B resistance mechanisms with severe fitness trade-offs can fixate in vivo, though resistance development was relatively limited compared to parallel in vitro approaches, likely due to lower selective drug pressure in living systems [97].
Table 2: In Vivo Model Characteristics for Resistance Studies
| Model System | Infection Types | Key Parameters Measured | Translational Limitations |
|---|---|---|---|
| Murine Thigh Infection | Soft tissue infections, efficacy against resistant bacteria | Bacterial burden reduction, PK/PD indices | Interspecies immune differences [98] [96] |
| Mouse Systemic Infection | Sepsis, disseminated fungal infections | Survival rates, organ burden | Different drug pharmacokinetics [96] |
| Rabbit Endocarditis | Biofilm-associated infections, device-related infections | Vegetation bacterial counts, treatment duration | Cost, ethical considerations [99] |
| Mouse Lung Infection | Pneumonia, respiratory infections | Lung bacterial load, inflammatory markers | Anatomical differences in respiratory tract [96] |
Specialized In Vivo Applications
Advanced in vivo applications include testing combination therapies against persister cells and biofilm-associated infections. For example, the anti-persister drug pyrazinamide plays a crucial role in shortening tuberculosis therapy and reducing relapse rates by targeting dormant bacterial populations [99]. Similarly, phage lysin CF-301 (Exebacase) demonstrated significantly enhanced efficacy against methicillin-resistant Staphylococcus aureus (MRSA) bacteremia when combined with standard antibiotics in animal models, leading to its advancement to clinical trials [100].
Comparative Analysis: Prokaryotic vs. Eukaryotic Pathogens
Fundamental biological differences between prokaryotic and eukaryotic pathogens necessitate specialized approaches for resistance assessment across experimental models.
Toxin Resistance Mechanisms
Bacterial and eukaryotic pathogens employ distinct molecular strategies for toxin resistance that reflect their evolutionary relationships and cellular architectures. Bacterial toxins exhibit preferential amino acid usage, with histidine (H) and arginine (R) being overrepresented, while animal toxins show significant cysteine (C) and lysine (K) enrichment [34]. These compositional differences correlate with functional specialization, as the high cysteine content in animal toxins often contributes to structural stability through disulfide bonding [34].
Table 3: Model Performance Against Different Pathogen Types
| Experimental Model | Prokaryotic Pathogens | Eukaryotic Pathogens | Notable Pathogen-Specific Adaptations |
|---|---|---|---|
| In Vitro: Microtiter | Standardized for bacteria (CLSI/EUCAST) | Standardized for yeasts (CLSI/EUCAST) | Filamentous fungi require specialized methods [97] |
| In Vitro: Experimental Evolution | Study of efflux pumps, horizontal gene transfer | Analysis of aneuploidy, chromosomal rearrangements | Fungal sexual reproduction slows deleterious mutation accumulation [97] |
| In Vivo: Systemic Infection | Effective for sepsis models with Gram-negative bacteria | Limited utility for dimorphic fungi | Host temperature affects fungal dimorphism [97] |
| In Vivo: Biofilm Models | Catheter-associated UTI, endocarditis models | Candida biofilm on medical devices | Fungal biofilms have distinct matrix composition [96] |
Technical Considerations by Pathogen Type
Experimental evolution reveals distinctive resistance patterns between prokaryotic and eukaryotic systems. While bacteria frequently acquire resistance through plasmid-borne genes and horizontal gene transfer, fungal pathogens more commonly develop resistance through chromosomal mutations, aneuploidy formation, and overexpression of efflux pumps [97]. For instance, experimentally evolved Candida albicans populations exposed to fluconazole demonstrated resistance development through mutations in four key genes, with chaperone Hsp90 identified as a critical facilitator of resistance evolution [97].
Visualization of Experimental Workflows
The following diagrams illustrate core methodologies for resistance assessment in prokaryotic and eukaryotic systems.
Experimental Evolution Workflow
In Vivo Validation Pipeline
The Scientist's Toolkit: Research Reagent Solutions
Successful resistance assessment requires specialized reagents and tools tailored to specific experimental approaches.
Table 4: Essential Research Reagents for Resistance Studies
| Reagent/Tool | Function | Application Examples |
|---|---|---|
| Fluorescent Markers (GFP, RFP) | Strain labeling for competitive fitness assays | Tracking population dynamics in experimental evolution [97] |
| Selective Markers (NTC, HYG) | Differential strain selection | Quantifying subpopulation sizes in co-culture experiments [97] |
| DNA Barcodes | High-throughput population tracking | Deep sequencing-based quantification of strain fitness [97] |
| pLM Embeddings (ProtT5) | Protein sequence representation | Training specialized predictors like Exo-Tox for bacterial toxin identification [101] |
| Specialized Databases (Swiss-Prot, PSORTb) | Curated protein sequences and localizations | Building training datasets for machine learning predictors [34] [101] |
| Signal Peptide Prediction Tools | Identification of secreted proteins | Differentiating exotoxins from intracellular proteins [101] |
The comparative assessment of in vitro and in vivo models for resistance evaluation reveals a necessary complementarity rather than superiority of either approach. While in vitro systems, particularly experimental evolution, offer unparalleled control for deconstructing resistance mechanisms and fitness trade-offs, in vivo models provide essential physiological context for therapeutic validation. The emerging integration of artificial intelligence with traditional microbiological methods represents a promising frontier for predictive resistance modeling. Researchers should strategically select models based on specific experimental questions, recognizing that a hierarchical approach combining controlled in vitro screening with physiologically relevant in vivo validation provides the most comprehensive framework for addressing the escalating antimicrobial resistance crisis.
The evolutionary arms race between hosts and pathogens has led to the development of sophisticated defense mechanisms across life's domains. Prokaryotes (bacteria and archaea) and eukaryotes (plants, animals, fungi, and protists) have evolved fundamentally distinct strategies for achieving toxin and pathogen resistance. Prokaryotes typically employ population-wide innate immune mechanisms that operate through restricted modification systems and CRISPR adaptive immunity, focusing on horizontal gene transfer and rapid evolution at the population level [102] [103]. In contrast, eukaryotes have developed complex somatic resistance mechanisms within an individual's lifetime, and remarkably, some have also evolved the capacity for heritable resistance that can be transmitted to subsequent generations, a phenomenon known as transgenerational inheritance [104] [105]. This comparative guide objectively analyzes the experimental evidence, methodologies, and outcomes defining these divergent defensive strategies, providing a framework for researchers investigating microbial pathogenesis, evolutionary biology, and therapeutic development.
Core Concepts and Definitions
Prokaryotic Defense Systems
Prokaryotes utilize several intracellular immune strategies to combat phage infection and plasmid invasion:
- Restricted Modification (RM) System: An innate immune system that recognizes and cleaves foreign, unmodified DNA sequences, present in over 90% of sequenced bacterial and archaeal genomes [102].
- CRISPR System: An adaptive immune system that provides sequence-specific immunity against foreign genetic elements by incorporating short sequences from invaders into the host genome.
- Prokaryotic Argonaute (pAgo) System: A RNA-guided system that provides defense against mobile genetic elements [102].
- Population-wide Immunity: Emerges from rapid horizontal gene transfer of resistance traits and the collective survival of resistant clones within microbial communities.
Eukaryotic Defense Modalities
Eukaryotes employ multi-layered defense strategies operating at different biological scales:
- Somatic Resistance: Acquired within an organism's lifetime through epigenetic reprogramming, immunological memory, or somatic adaptations without alteration of the germline DNA sequence.
- Heritable Induced Resistance (h-IR): Environmentally induced resistance traits that are stably transmitted to subsequent generations through epigenetic mechanisms, including DNA methylation changes and histone modifications [104] [105].
Comparative Analysis of Resistance Mechanisms
Table 1: Fundamental Characteristics of Prokaryotic vs. Eukaryotic Resistance
| Characteristic | Prokaryotic Population-wide Immunity | Eukaryotic Somatic Resistance | Eukaryotic Heritable Resistance |
|---|---|---|---|
| Temporal Scale | Rapid (hours to days) | Medium (days to weeks) | Long-term (multiple generations) |
| Inheritance Pattern | Horizontal gene transfer | Non-heritable | Vertical transmission |
| Molecular Basis | DNA restriction enzymes, CRISPR spacers | Epigenetic modifications, immune memory | Stable epialleles, DNA methylation patterns |
| Specificity | Sequence-specific (CRISPR) or broad (RM) | Pathogen-specific (adaptive immunity) or broad (priming) | Primarily broad-spectrum priming |
| Key Regulatory Elements | Cas proteins, restriction-modification enzymes | NPR1 protein, salicylic acid, jasmonic acid | DDM1, MET1, CMT3 chromatin remodelers [104] |
| Evolutionary Impact | Rapid population adaptation | Individual survival advantage | Multi-generational adaptation |
Experimental Evidence and Methodologies
Prokaryotic Immunity: Plasmid Invasion and Core Sequence Recognition
Experimental Protocol 1: Identification of a Conserved Defense Response Core Sequence
- Objective: To determine whether a conserved defense response allows identification and degradation of foreign plasmids containing specific sequence motifs in both prokaryotic and eukaryotic cells [102].
- Materials: Plasmid pEGFP-N1, E. coli cells, zebrafish embryos, mammalian cell lines (HEK 293T, HCT116).
- Methodology:
- Transform E. coli with pEGFP-N1 plasmid containing or lacking the 5ʹ-GTTTGTT-3ʹ core sequence
- Microinject circular and linear forms of pEGFP-N1 into zebrafish zygotes
- Transfert mammalian cell lines with plasmids containing wild-type or mutant core sequences
- Perform transcriptome sequencing and qPCR to measure immune gene activation (isg15)
- Conduct chromatin immunoprecipitation (ChIP) to assess H3K4me3 levels
- Key Findings: Plasmids containing the 5ʹ-GTTTGTT-3ʹ core sequence activated defense gene isg15 and were degraded more rapidly in both prokaryotic and eukaryotic systems. Mutation to 5ʹ-CAAACAA-3ʹ greatly reduced plasmid degradation and immune activation [102].
Figure 1: Conserved Defense Pathway for Foreign DNA Recognition. The 5ʹ-GTTTGTT-3ʹ core sequence triggers immune activation and plasmid degradation in both prokaryotes and eukaryotes, while mutated sequences enable plasmid persistence.
Eukaryotic Heritable Resistance: Arabidopsis thaliana Model
Experimental Protocol 2: Multi-Generational Analysis of Heritable Induced Resistance
- Objective: To investigate the prevalence, stability, and predictability of environment-induced heritable changes in Arabidopsis thaliana [105].
- Materials: 14 natural accessions (genotypes) of A. thaliana, treatments: jasmonic acid, nutrient variations, leaf removal, drought, cadmium, salinity.
- Methodology:
- Subject ancestral generation to control and 10 environmental treatments
- Cultivate four successive offspring generations in control environment
- Measure phenotypes: flowering time, plant height, fruit number, aboveground biomass
- Perform genome-wide gene expression analysis
- Analyze transposon abundance and correlation with induced variation susceptibility
- Key Findings: All environmental treatments caused heritable phenotypic and gene expression changes transmissible over four generations. Susceptibility to environmental induction correlated with transposon abundance in the Gypsy and MuDR superfamilies [105].
Table 2: Heritable Resistance Outcomes in Arabidopsis thaliana Under Various Treatments
| Environmental Treatment | Phenotypic Changes in Offspring | Generational Stability | Epigenetic Markers |
|---|---|---|---|
| Jasmonic Acid | Slight enhancement of fruit production | Up to 4 generations | H3K4me3 modification |
| High Cadmium | Significant reduction in plant size and fruit number | Stable transmission | Reduced DDM1 expression [104] |
| High Salinity | Shorter plants with fewer fruits | Persistent across generations | MET1 and CMT3 repression [104] |
| Nutrient Addition | Increased aboveground biomass | Heritable changes observed | DNA methylation changes |
| Drought | Reduced fruit production | Genotype-dependent stability | Transposon activation |
Molecular Mechanisms and Signaling Pathways
Prokaryotic Immune Signaling
Prokaryotic immunity operates through direct DNA recognition and cleavage mechanisms. The restricted modification system distinguishes self from non-self DNA based on methylation patterns, while CRISPR systems incorporate foreign DNA spacers that guide Cas proteins to cleave complementary invading sequences [102]. These systems provide population-level protection through the selective survival of resistant individuals and horizontal transfer of defense elements.
Eukaryotic Signaling for Somatic and Heritable Resistance
Figure 2: Eukaryotic Resistance Signaling Pathways. Somatic resistance involves signaling molecules and defense priming within a generation, while heritable resistance requires chromatin remodeling and creates stable epialleles transmitted across generations.
Eukaryotic somatic resistance employs complex signaling networks:
- Systemic Acquired Resistance (SAR): Regulated by NPR1 protein with salicylic acid (SA) and N-hydroxy-pipecolic acid (Pip) as key signaling metabolites [104].
- Priming: Enhanced capacity to activate defense responses upon challenge, involving histone modifications and DNA methylation [104].
- Heritable Resistance: Involves stable reduction in expression of chromatin remodelers DDM1, MET1, and CMT3, which is maintained in the apical meristem and transmitted to progeny [104].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Resistance Mechanisms
| Reagent / Solution | Function | Application Examples |
|---|---|---|
| Plasmid pEGFP-N1 | Foreign DNA containing viral-derived sequences with 5ʹ-GTTTGTT-3ʹ core | Prokaryotic and eukaryotic defense activation studies [102] |
| Zebrafish (Danio rerio) model | Vertebrate model with innate immunity detectable at zygote stage | Transgenerational immune studies, transcriptome sequencing [102] |
| Arabidopsis thaliana accessions | Plant model with 14+ natural genotypes varying in transposon abundance | Heritable induced resistance studies across generations [105] |
| Chromatin Immunoprecipitation (ChIP) | Analyzes histone modifications (H3K4me3) at target genes | Epigenetic regulation of defense genes [102] |
| Jasmonic Acid (JA) | Plant hormone signaling molecule | Inducing heritable resistance against herbivores [105] |
| β-aminobutyric acid (BABA) | Chemical priming agent | Inducing resistance against biotrophic pathogens [104] |
| CRISPR/Cas9 systems | Targeted genome editing | Testing gene function in immune responses [102] |
The distinct outcomes of population-wide immunity in prokaryotes versus somatic and heritable resistance in eukaryotes represent fundamental evolutionary adaptations to environmental challenges. Prokaryotic strategies emphasize rapid population evolution through horizontal gene transfer and simple sequence recognition systems, while eukaryotic approaches employ complex multi-generational strategies incorporating epigenetic memory and transgenerational inheritance. For researchers and drug development professionals, these differences highlight the importance of considering temporal scales and inheritance patterns when designing therapeutic interventions. Understanding conserved elements, such as the 5ʹ-GTTTGTT-3ʹ core sequence recognized by both domains [102], may reveal universal principles of immune recognition, while domain-specific mechanisms offer targeted opportunities for manipulating resistance pathways in agricultural, environmental, and biomedical contexts.
Conclusion
The comparative assessment of toxin resistance mechanisms reveals a fundamental dichotomy: prokaryotes rely heavily on rapid, transferrable genetic solutions like enzymatic inactivation and efflux pumps, while eukaryotes often depend on evolutionary adaptations such as target-site mutations and complex immune responses. This divergence offers critical insights for biomedical research. Understanding prokaryotic systems, such as toxin-antitoxin modules, opens avenues for novel antibacterial strategies to combat the escalating AMR crisis. Conversely, elucidating eukaryotic resistance, exemplified by target-site insensitivity, informs the development of protective therapies against toxigenic threats and enables the prediction of evolutionary outcomes in response to environmental toxins. Future research must leverage cross-disciplinary approaches, integrating computational biology, structural analysis, and functional genomics to translate these foundational mechanisms into next-generation therapeutics and diagnostic tools, ultimately turning the principles of natural defense into powerful medical weapons.
References
- 1. Some Examples of Bacterial Toxins as Tools - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11125981/]
- 2. Plant Toxic Proteins: Their Biological Activities, Mechanism of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10303728/]
- 3. A trans-kingdom T6SS RNase effector targeting both ... [https://www.sciencedirect.com/science/article/pii/S2211124725008459]
- 4. How Herbivores Overcome Toxins [https://learn.genetics.utah.edu/content/herbivores/toxins/]
- 5. An Overview of Toxin-Antitoxin Biology [https://www.sciencedirect.com/science/article/pii/S1097276518300030]
- 6. Prokaryotic homeostasis – a solution to thrive and survive [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1704789/full]
- 7. A comparative study indicates vertical inheritance and ... [https://www.sciencedirect.com/science/article/abs/pii/S1055790322000926]
- 8. Comparative Analysis of Arsenic Transport and Tolerance ... [https://www.mdpi.com/2073-4409/11/17/2741]
- 9. A comparative study indicates vertical inheritance and ... [https://pubmed.ncbi.nlm.nih.gov/35533945/]
- 10. Researchers Discover Gut Bacteria 'Weapon,' Redirect It ... [http://www.ou.edu/news/articles/2025/may/researchers-discover-gut-bacteria-weapon-redirect-tt-toward-cancer.html]
- 11. Prokaryotic homeostasis – a solution to thrive and survive - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593503/]
- 12. The Mechanism of Bacterial Resistance and Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495013/]
- 13. Understanding antibiotic resistance: Week 2: 1.1 | OpenLearn [https://www.open.edu/openlearn/ocw/mod/oucontent/view.php?id=75460§ion=1.1]
- 14. Function and Inhibitory Mechanisms of Multidrug Efflux Pumps [https://pmc.ncbi.nlm.nih.gov/articles/PMC8678522/]
- 15. Exploring molecular mechanisms of drug resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11883354/]
- 16. Bacterial toxin-antitoxin systems: Novel insights on ... [https://www.sciencedirect.com/science/article/pii/S2666517423000251]
- 17. Toxin–antitoxin systems: Biology, identification, and application [https://pmc.ncbi.nlm.nih.gov/articles/PMC3827094/]
- 18. Regulatable killing of eukaryotic cells by the prokaryotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC140101/]
- 19. Enthralling genetic regulatory mechanisms meddling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10511911/]
- 20. Enthralling genetic regulatory mechanisms meddling ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2023.1257859/full]
- 21. A Xenobiotic Detoxification Pathway through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6050962/]
- 22. Killer toxin K28 resistance in yeast relies on COG complex ... [https://pubmed.ncbi.nlm.nih.gov/40557545/]
- 23. Scientists reveal a hidden alarm system inside your cells [https://www.sciencedaily.com/releases/2025/11/251124094323.htm]
- 24. a comprehensive database of prokaryotic antimicrobial toxins [https://pmc.ncbi.nlm.nih.gov/articles/PMC9825508/]
- 25. Distant relatives of a eukaryotic cell-specific toxin family ... [https://www.nature.com/articles/s41467-024-49103-5]
- 26. Detoxification Enzyme - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/detoxification-enzyme]
- 27. Mechanisms of bacterial immunity, protection, and survival ... [https://www.sciencedirect.com/science/article/pii/S1931312824001781]
- 28. Horizontal Gene Transfer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4536854/]
- 29. Horizontal gene transfer [https://en.wikipedia.org/wiki/Horizontal_gene_transfer]
- 30. Horizontal Gene Transfers in Plants - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8401529/]
- 31. Gene transfer: Types, mechanisms, and methods [https://www.abcam.com/en-us/knowledge-center/dna-and-rna/gene-transfer-types-mechanisms-and-methods]
- 32. 3.1: Horizontal Gene Transfer in Bacteria [https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_(Kaiser)/Unit_2%3A_Bacterial_Genetics_and_the_Chemical_Control_of_Bacteria/3%3A_Bacterial_Genetics/3.1%3A_Horizontal_Gene_Transfer_in_Bacteria]
- 33. Duplicated antibiotic resistance genes reveal ongoing ... [https://www.nature.com/articles/s41467-024-45638-9]
- 34. a critical examination of bacterial exotoxins and animal toxins [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-025-07438-2]
- 35. Assessing molecular docking tools: understanding drug ... [https://fjps.springeropen.com/articles/10.1186/s43094-025-00862-y]
- 36. Decoding the limits of deep learning in molecular docking for ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc05395a]
- 37. A Comprehensive Benchmark of Tools for Efficient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11888206/]
- 38. Toxinome—the bacterial protein toxin database - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10790787/]
- 39. Comprehensive comparative-genomic analysis of Type 2 toxin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2701414/]
- 40. Comparing the toxicity of iodinated X-ray contrast media on ... [https://www.sciencedirect.com/science/article/pii/S0147651322005188]
- 41. Bacterial toxin-antitoxin modules: classification, functions, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8610362/]
- 42. Targeting Type II Toxin-Antitoxin Systems as Antibacterial ... [https://pubmed.ncbi.nlm.nih.gov/32899634/]
- 43. Characterization of toxin-antitoxin systems from public ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.951774/full]
- 44. Comprehensive comparative-genomic analysis of Type 2 toxin ... [https://biologydirect.biomedcentral.com/articles/10.1186/1745-6150-4-19]
- 45. The Variety in the Common Theme of Translation Inhibition ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.00262/full]
- 46. Toxin-Antitoxin Modules Are Pliable Switches Activated by ... [https://www.mdpi.com/2072-6651/8/7/214]
- 47. The combination of active partitioning and toxin-antitoxin ... [https://www.nature.com/articles/s41467-025-62473-8]
- 48. Discrepancies between prokaryotes and eukaryotes need ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9790305/]
- 49. Physical forces affect bacteria's toxin resistance, study finds [https://chemistry.cornell.edu/news/physical-forces-affect-bacterias-toxin-resistance-study-finds]
- 50. New Study Highlights Threat of Pest Resistance to Corn's ... [https://bioengineer.org/new-study-highlights-threat-of-pest-resistance-to-corns-latest-biotech-defenses/]
- 51. Study warns pest resistance threatens corn industry's ... [https://news.arizona.edu/news/study-warns-pest-resistance-threatens-corn-industrys-newest-biotech-defense]
- 52. Emerging technological developments to address pest ... [https://jcottonres.biomedcentral.com/articles/10.1186/s42397-024-00192-z]
- 53. Universal toxin-based selection for precise genome ... [https://www.nature.com/articles/s41467-020-20810-z]
- 54. GSK and Fleming Initiative scientists unite to target AMR ... [https://www.gsk.com/en-gb/media/press-releases/gsk-and-fleming-initiative-scientists-unite-to-target-amr-with-advanced-ai/]
- 55. Global antibiotic resistance surveillance report 2025 [https://www.who.int/publications/i/item/9789240116337]
- 56. The Antimicrobial Resistance Crisis: An Inadvertent ... [https://www.frontiersin.org/journals/ecology-and-evolution/articles/10.3389/fevo.2021.692674/full]
- 57. Antimicrobial resistance: Linking molecular mechanisms to ... [https://www.sciencedirect.com/science/article/pii/S2472555225000255]
- 58. Antimicrobial Resistance: A Growing Serious Threat for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10340576/]
- 59. Drug resistance in eukaryotic microorganisms [https://www.nature.com/articles/nmicrobiol201692]
- 60. Multidrug resistance: molecular mechanisms and clinical ... [https://pubmed.ncbi.nlm.nih.gov/9272126/]
- 61. Key Takeaways from IDWeek 2025: AI, AMR Strategies ... [https://www.medpace.com/blog/key-takeaways-from-idweek-2025-ai-amr-strategies-next-generation-anti-viral-development-converging/]
- 62. The origin and evolution of cell-intrinsic antibacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9275444/]
- 63. Anti-Immunology: Evasion of the Host Immune System by ... [https://www.sciencedirect.com/science/article/pii/S0092867406001322]
- 64. Exploring the evolutionary links: Innate immunity in ... [https://www.sciencedirect.com/science/article/abs/pii/S1359511324002897]
- 65. Host − Pathogen interactions and immune evasion [https://www.immunology.org/public-information/bitesized-immunology/pathogens-disease/host-pathogen-interactions-and-immune]
- 66. Conservation and similarity of bacterial and eukaryotic innate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11389603/]
- 67. Pathogens have evolved various means of evading or ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK27176/]
- 68. Drug resistance in eukaryotic microorganisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5215055/]
- 69. Both prokaryotes and eukaryotes produce an immune ... [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-022-00825-3]
- 70. Evolution of RNA- and DNA-guided antivirus defense systems ... [https://biologydirect.biomedcentral.com/articles/10.1186/s13062-017-0177-2]
- 71. 张帆课题组在新型抗毒力药物研究领域取得新进展 [https://www.pharm.whu.edu.cn/info/1069/41241.htm]
- 72. 2025 AACR | 复宏汉霖多项创新管线临床前研究数据首次发布 [https://www.henlius.com/NewsDetails-4986-26.html]
- 73. 国产新药“全球新”突围:2025年FIC/BIC潜力品种临床数据解析 [https://www.phirda.com/artilce_40759.html?module=trackingCodeGenerator]
- 74. 2025 ASCO | 复宏汉霖创新药矩阵近20项最新研究结果即将 ... [https://www.henlius.com/NewsDetails-4977-26.html]
- 75. 复杂抗体表达平台化策略探析:从质粒设计到系统优化 [https://www.bioworkshops.com/cn/html/news/3732.html]
- 76. 真核小球藻与原核铜绿微囊藻对磺胺胁迫的响应机制比较 [https://www.ebiotrade.com/newsf/2025-9/20250919083409660.htm]
- 77. 2024-2025微生物组70篇必读论文和中国十大研究 [https://www.chinagut.cn/articles/ss/b8d0a2bcd28c4bc8b53aacee5c360c72]
- 78. How many FDA approved Antitoxin are there? [https://synapse.patsnap.com/article/how-many-fda-approved-antitoxin-are-there]
- 79. What Antitoxin are being developed? [https://synapse.patsnap.com/article/what-antitoxin-are-being-developed]
- 80. Antibiotics re-booted—time to kick back against drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125309/]
- 81. Analyzing the Landscape of Botulinum Toxin Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533941/]
- 82. Overview of antimicrobial resistance and mechanisms [https://www.sciencedirect.com/science/article/pii/S2950194624000505]
- 83. Towards the molecular mechanism of prokaryotic and ... [https://pubmed.ncbi.nlm.nih.gov/11428916/]
- 84. Convergent evolution of toxin resistance in animals - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9543476/]
- 85. In brief: The innate and adaptive immune systems - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK279396/]
- 86. Immune system [https://en.wikipedia.org/wiki/Immune_system]
- 87. Prokaryotic genome regulation: A revolutionary paradigm - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3511978/]
- 88. Evolutionary insights into Na+/K+-ATPase-mediated toxin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257717/]
- 89. Constraints on the evolution of toxin-resistant Na,K-ATPases ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1010323]
- 90. Community-wide convergent evolution in insect adaptation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3420205/]
- 91. Newly Discovered Mechanisms of Antibiotic Self- ... [https://www.mdpi.com/2079-6382/12/1/35]
- 92. Antibiotics, Resistome and Resistance Mechanisms [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2018.02066/full]
- 93. Constraints on the evolution of toxin-resistant Na,K- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9462791/]
- 94. The rapid evolution of flagellar ion selectivity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9683732/]
- 95. Concerted evolution reveals co-adapted amino acid ... [https://www.sciencedirect.com/science/article/pii/S0960982221004620]
- 96. In vitro and ex vivo systems at the forefront of infection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7172914/]
- 97. Unlocking the potential of experimental evolution to study ... [https://www.nature.com/articles/s44259-024-00064-1]
- 98. A generative artificial intelligence approach for the ... [https://www.nature.com/articles/s41564-025-02114-4]
- 99. Bacterial persisters: molecular mechanisms and ... [https://www.nature.com/articles/s41392-024-01866-5]
- 100. Next-generation antimicrobials: A review of phage lysins as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452485/]
- 101. Exo-Tox: Identifying Exotoxins from secreted bacterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333140/]
- 102. Both prokaryotes and eukaryotes produce an immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9188160/]
- 103. Prokaryotes Versus Eukaryotes: Who is Hosting Whom? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4668860/]
- 104. Heritable induced resistance in Arabidopsis thaliana [https://pmc.ncbi.nlm.nih.gov/articles/PMC10457550/]
- 105. Environment-induced heritable variations are common in ... [https://www.nature.com/articles/s41467-024-49024-3]