Enhancing Genomic Subtyping Resolution: Strategies for Superior Pathogen Discrimination and Precision Medicine
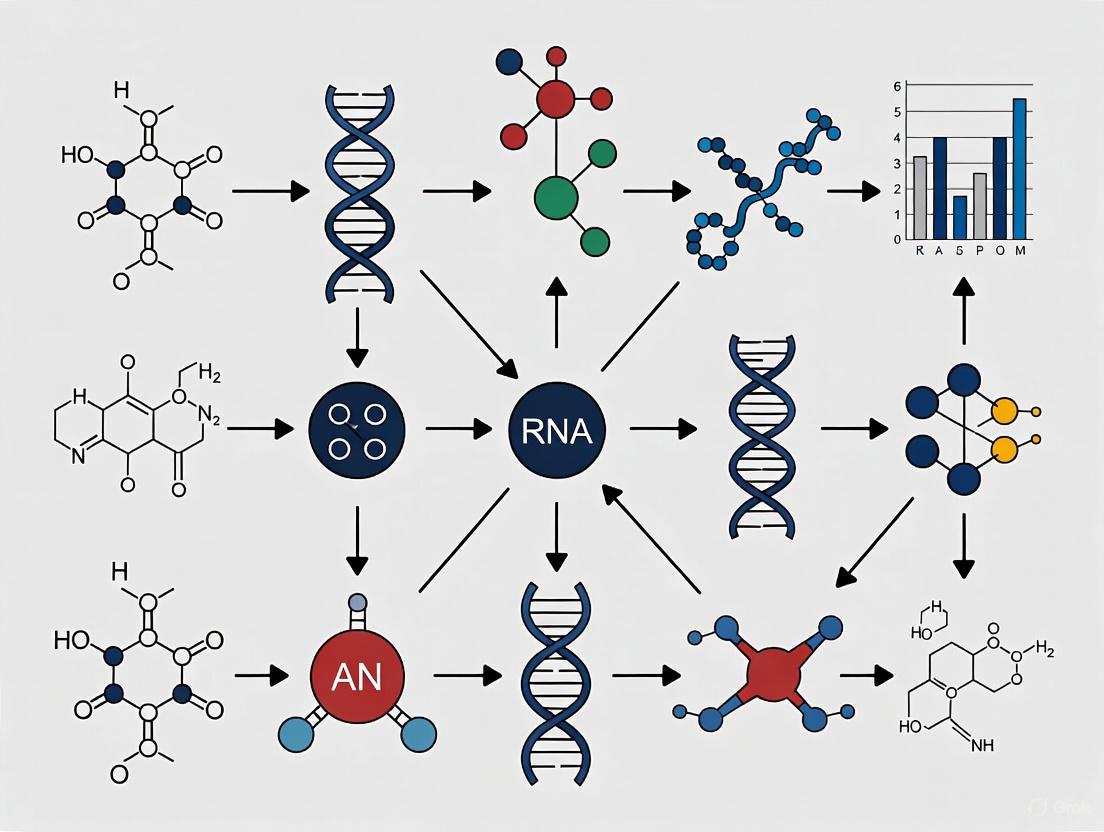
This article provides a comprehensive exploration of modern approaches for enhancing the discriminatory power of genomic subtyping methods, a critical need for researchers and drug development professionals.
Enhancing Genomic Subtyping Resolution: Strategies for Superior Pathogen Discrimination and Precision Medicine
Abstract
This article provides a comprehensive exploration of modern approaches for enhancing the discriminatory power of genomic subtyping methods, a critical need for researchers and drug development professionals. It covers foundational principles, from transitioning beyond traditional methods like PFGE to advanced whole-genome sequencing (WGS) techniques. The scope includes a detailed analysis of current methodologies like cgMLST and wgMLST, tackles optimization challenges such as mobile genetic element interference, and presents rigorous validation frameworks for comparing statistical and deep learning-based integration. By synthesizing insights from bacterial epidemiology and cancer genomics, this resource aims to equip scientists with the knowledge to achieve higher resolution in strain discrimination and disease subtyping for improved outbreak detection and personalized therapies.
From Phenotypes to Base Pairs: The Evolution and Core Principles of High-Resolution Subtyping
In genomic epidemiology, discriminatory power refers to the ability of a subtyping method to distinguish between epidemiologically unrelated bacterial strains. This fundamental characteristic determines the effectiveness of outbreak investigations, source tracking, and pathogen surveillance. The transition from traditional methods like pulsed-field gel electrophoresis (PFGE) to whole-genome sequencing (WGS) has fundamentally transformed our approach to bacterial subtyping, offering unprecedented resolution for differentiating bacterial pathogens. However, this advanced capability comes with significant technical challenges that can impact the consistency and reliability of laboratory results. This technical support center addresses the specific issues researchers encounter when implementing these sophisticated genomic subtyping methods, providing practical troubleshooting guidance framed within the broader research objective of optimizing discriminatory power.
Table: Evolution of Key Subtyping Methods and Their Resolutions
| Subtyping Method | Genetic Basis | Discriminatory Power | Primary Use Case |
|---|---|---|---|
| PFGE [1] [2] | Restriction fragment patterns | Moderate (Gold standard for outbreak investigation) | Outbreak investigations, source tracking |
| MLST [1] | Sequences of 2-10 genes | Low to Moderate (Phylogenetic subtyping) | Phylogenetic studies, population genetics |
| Whole-Genome Sequencing (WGS) [1] | Full genomic sequence | High (Can be tailored for low or high resolution) | Outbreak detection, transmission tracing, comprehensive characterization |
Technical Support Center: Troubleshooting Genomic Subtyping Methods
Frequently Asked Questions (FAQs)
FAQ 1: Why does our WGS analysis yield different cluster results compared to other laboratories when analyzing the same bacterial isolates?
Differences in cluster results between laboratories typically stem from pipeline heterogeneity rather than data quality issues. Recent multi-country assessments revealed that different bioinformatics pipelines can generate varying cluster compositions, particularly at the outbreak detection level [3]. This inconsistency primarily occurs because:
- Schema Differences: Laboratories use different cgMLST or wgMLST schemas with varying numbers and selections of loci
- Algorithm Variations: Clustering may be performed with single-linkage hierarchical clustering (HC) or Minimum-Spanning Tree (MST) generation through MSTreeV2 (GT) [3]
- Threshold Discrepancies: Lack of standardized genetic distance thresholds for defining clusters
Solution: Implement threshold flexibilization strategies and participate in continuous pipeline comparability assessments, as demonstrated by the BeONE consortium, which found that adjusting thresholds improved detection of similar outbreak signals across different laboratories [3].
FAQ 2: Why does discriminatory power vary significantly across different pathogens when using the same cgMLST approach?
Different traditional typing groups (e.g., serotypes) exhibit remarkably different genetic diversity profiles, which directly impacts how effectively cgMLST can discriminate between strains [3]. For example:
- Listeria monocytogenes shows clear stability plateaus that correspond to sequence types (STs) [3]
- Campylobacter jejuni demonstrates marked discrepancies between pipelines due to different resolution powers of allele-based schemas [3]
- The genetic heterogeneity within a species affects how many allele differences constitute an outbreak cluster
Solution: Develop species-specific and sequence-type-specific thresholds rather than applying uniform criteria across all pathogens.
FAQ 3: Why is our config file update not being recognized during the allele calling process?
This common bioinformatics issue typically relates to caching of previous configurations. To resolve this, you must overwrite the collection of terms that were cached for older versions of your config file by specifying --no-cache in your command [4]. Always verify that:
- File paths in the config are correctly specified
- The schema version matches your reference database
- All dependencies have been updated compatibly
Troubleshooting Guides
Issue: Low Discriminatory Power with cgMLST for Certain Pathogens
Problem: cgMLST analysis fails to provide sufficient resolution to distinguish between epidemiologically unrelated isolates of Campylobacter jejuni.
Investigation:
- Verify that your schema includes an adequate number of core genome loci (typically 500-3,000 depending on the pathogen)
- Check the genetic diversity of your dataset - some clonal pathogens naturally exhibit limited diversity
- Compare your results with traditional typing methods like MLST to ensure biological relevance
Resolution:
- Transition to wgMLST (whole-genome MLST), which includes both core and accessory genomes, providing higher resolution power [3]
- Implement a SNP-based approach for high-resolution analysis of closely related isolates [1] [3]
- For C. jejuni, consider using a standardized, higher-resolution schema specifically validated for this pathogen
Issue: Inconsistent Cluster Composition Between Analytical Pipelines
Problem: Your WGS pipeline identifies different outbreak clusters compared to collaborative laboratories using the same raw data.
Investigation:
- Document the specific parameters of each pipeline:
- Allele-calling algorithm
- Schema version and source
- Clustering algorithm (HC vs. MST/GT)
- Distance threshold criteria
- Analyze a standardized dataset with known epidemiological relationships
Resolution:
- Apply ReporTree [3] to harmonize clustering information across different distance thresholds
- Perform an inter-pipeline clustering congruence assessment [3]
- Establish internal validation protocols using reference strains with known relationships
- Implement threshold flexibilization to identify optimal outbreak detection parameters [3]
Troubleshooting Inconsistent Cluster Results Between Pipelines
Experimental Protocols for Assessing Discriminatory Power
Protocol: Inter-Pipeline Congruence Assessment
Purpose: To evaluate the congruence of clustering results between different WGS bioinformatics pipelines used for genomic surveillance of foodborne bacterial pathogens [3].
Materials:
- WGS datasets of target pathogen (e.g., Listeria monocytogenes, Salmonella enterica, Escherichia coli, Campylobacter jejuni)
- Multiple bioinformatics pipelines (e.g., cg/wgMLST schemas, allele/SNP-callers)
- ReporTree software [3]
- Computing infrastructure with adequate storage and processing capacity
Methodology:
- Dataset Preparation:
- Select a diverse collection of bacterial isolates with known epidemiological relationships
- Include reference strains where genetic relationships are well-established
- Ensure sequence quality meets minimum requirements (completeness, coverage)
Multi-Pipeline Analysis:
- Analyze the same dataset using each participating laboratory's standard pipeline
- Include both allele-based (cgMLST, wgMLST) and SNP-based pipelines
- Apply both hierarchical clustering (HC) and Minimum-Spanning Tree (MST) generation where possible
Cluster Comparison:
- Use ReporTree to harmonize clustering information across all possible distance thresholds
- Identify stability regions where cluster composition remains consistent across threshold ranges
- Calculate congruence scores between pipelines at different threshold levels
Threshold Optimization:
- Identify threshold ranges where different pipelines detect similar outbreak signals
- Determine pathogen-specific thresholds that maximize discriminatory power while maintaining epidemiological relevance
Expected Results: This protocol will identify pipeline-specific biases and establish optimal thresholds for cluster detection, directly contributing to improved discriminatory power in genomic subtyping methods.
Protocol: Validation of Discriminatory Power Against Known Epidemiological Relationships
Purpose: To validate the discriminatory power of a subtyping method by comparing genetic relationships with established epidemiological links [1].
Materials:
- Bacterial isolates from documented outbreaks (known related isolates)
- Environmental or sporadic isolates (known unrelated isolates)
- Reference subtyping method (e.g., PFGE, MLST)
- WGS platform and bioinformatics pipeline
Methodology:
- Strain Selection:
- Include isolates from confirmed outbreak events with epidemiological links
- Include spatially and temporally distinct isolates with no known epidemiological connections
- Balance the dataset to include diverse genetic backgrounds
Blinded Analysis:
- Perform WGS and subtyping analysis without knowledge of epidemiological relationships
- Apply appropriate genetic distance thresholds for cluster definition
- Construct phylogenetic trees to visualize genetic relationships
Concordance Assessment:
- Compare genetic clustering with known epidemiological links
- Calculate sensitivity and specificity for detecting known relationships
- Compare resolution with reference subtyping methods
Discriminatory Power Quantification:
- Calculate Simpson's index of diversity to quantify discriminatory power
- Determine the number of types identified and the frequency of each type
- Assess the ability to distinguish between epidemiologically unrelated isolates
Experimental Validation of Discriminatory Power
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table: Key Research Reagent Solutions for Genomic Subtyping
| Tool/Platform | Type | Function | Application in Discriminatory Power Research |
|---|---|---|---|
| ReporTree [3] | Software | Harmonizes clustering information across distance thresholds | Enables comparison of cluster results between different pipelines and laboratories |
| cg/wgMLST Schemas [3] | Bioinformatics Resource | Defines loci for allele-based typing | Provides framework for standardized strain comparison; different schemas offer varying resolution |
| ResFinder [5] | Web Tool | Identifies antimicrobial resistance genes from WGS data | Adds functional characterization to genetic subtyping, enhancing epidemiological investigation |
| SNP-based Pipelines [1] [3] | Bioinformatics Method | Detects single-nucleotide polymorphisms across genomes | Offers highest resolution subtyping for outbreak investigation and transmission tracing |
| INNUENDO [3] | Analytical Platform | Integrated WGS data analysis and visualization | Supports standardized bioinformatic analyses for cross-laboratory comparisons |
| PFGE [1] [2] | Laboratory Method | Separates large DNA fragments to generate fingerprints | Gold standard reference method for validating new subtyping approaches |
The pursuit of enhanced discriminatory power in genomic epidemiology requires continuous methodological refinement and standardization. As the field transitions from traditional to genomic subtyping methods, researchers must address the challenges of pipeline heterogeneity, threshold optimization, and species-specific validation. The protocols and troubleshooting guides presented here provide a framework for overcoming these obstacles, enabling more accurate cluster detection and outbreak investigation. By implementing standardized congruence assessments, validating against known epidemiological relationships, and selecting appropriate reagents and platforms, researchers can significantly improve the reliability and discriminatory power of their genomic subtyping methods, ultimately strengthening public health responses to infectious disease threats.
For decades, public health and clinical microbiology laboratories relied on pulsed-field gel electrophoresis (PFGE) and multi-locus sequence typing (MLST) as cornerstone methods for bacterial strain typing and outbreak investigation. While these methods served as crucial public health tools, they presented significant limitations in resolution, speed, and reproducibility. The emergence of whole-genome sequencing (WGS) has fundamentally transformed microbial surveillance by providing unprecedented resolution for distinguishing bacterial strains. WGS-based methods represent a paradigm shift in molecular epidemiology, offering superior discriminatory power that enables public health officials to detect outbreaks with greater precision, trace transmission pathways more accurately, and distinguish between truly related cases and sporadic infections with remarkable clarity [6] [7].
Traditional methods like PFGE and the 7-locus MLST scheme provided initial frameworks for strain differentiation but lacked the resolution needed for fine-scale outbreak investigations. PFGE, while widely used in networks like PulseNet USA for over two decades, offered limited discriminatory power for certain pathogens and produced results that were challenging to standardize across laboratories [7]. Similarly, MLST schemes based on only seven housekeeping genes often failed to differentiate between closely related isolates, particularly for monomorphic species or widespread sequence types like Legionella pneumophila ST1 or Clostridioides difficile RT027 [8] [6]. The transition to WGS-based typing methods addresses these limitations by examining genetic variation across thousands of loci or the entire genome, providing a resolution that has redefined our approach to outbreak detection and microbial population genetics.
Technical Foundations: Understanding WGS-Based Typing Methods
Whole-genome sequencing enables several analytical approaches for strain typing, each with distinct methodologies and applications in public health and research settings. The primary WGS-based typing methods include core genome MLST (cgMLST), whole genome MLST (wgMLST), and single nucleotide polymorphism (SNP) analysis.
Core Genome MLST (cgMLST) analyzes genetic variation in a standardized set of core genes present in nearly all isolates of a species. This approach typically examines 500-2,000 genes that are conserved across the bacterial population, providing a balance between standardization and discriminatory power. For example, a cgMLST scheme for Legionella pneumophila may utilize 1,521 core genes, while a simplified 50-loci scheme has been proposed for easier standardization between laboratories [6]. cgMLST forms the backbone of national surveillance systems, such as PulseNet 2.0 in the United States, which uses a threshold of 0-10 allelic differences to define clusters of Shiga-toxin-producing E. coli (STEC) infections [7].
Whole Genome MLST (wgMLST) extends the analysis beyond the core genome to include accessory genes that may be present or absent in different isolates. This method typically analyzes thousands of genes (e.g., 4,000-6,000 loci) and provides higher resolution by capturing strain-specific genetic elements. Studies have shown high concordance between wgMLST and SNP-based analyses for outbreak detection, with wgMLST (chromosome-associated loci) demonstrating nearly equivalent performance to high-quality SNP analysis for clustering related STEC isolates [7].
High-Quality SNP (hqSNP) Analysis identifies single nucleotide polymorphisms by comparing isolate genomes to a closely related reference sequence. This method provides the highest possible resolution for distinguishing closely related isolates and is particularly valuable for investigating outbreaks involving highly clonal pathogens. Regression analyses have demonstrated strong correlations between hqSNP differences and cgMLST allelic differences, though the relationship varies by bacterial species and outbreak context [7].
Table 1: Comparison of Major Genomic Typing Methods
| Method | Genetic Targets | Discriminatory Power | Standardization Potential | Primary Applications |
|---|---|---|---|---|
| PFGE | Whole genome restriction fragments | Moderate | Limited due to technical variability | Historical outbreak investigation |
| MLST | 7-8 housekeeping genes | Low to moderate | High for sequence-based comparison | Population structure analysis |
| cgMLST | 500-2,000 core genes | High | High with standardized schemes | Routine surveillance & outbreak detection |
| wgMLST | All chromosomal genes | Very high | Moderate with standardized schemes | High-resolution outbreak investigation |
| hqSNP | Single nucleotide variants | Highest | Low due to reference dependence | Fine-scale transmission mapping |
Comparative Advantages: Quantitative Evidence of WGS Superiority
Multiple studies have demonstrated the superior performance of WGS-based methods compared to traditional typing techniques across various bacterial pathogens. The transition to WGS represents not merely an incremental improvement but a fundamental advancement in discriminatory power, throughput, and epidemiological concordance.
For Legionella pneumophila outbreak investigations, WGS has proven particularly valuable for discriminating within common sequence types that were previously challenging to differentiate using conventional methods. Research comparing WGS typing tools for Belgian L. pneumophila outbreaks found that all three WGS approaches (cgMLST, wgMLST, and 50-loci cgMLST) provided concordant results that aligned with traditional sequence-based typing, but with significantly improved resolution. This enhanced discrimination is especially crucial for widespread sequence types like ST1, where standard 7-locus MLST often lacks sufficient resolution to distinguish related from unrelated isolates [6]. The study demonstrated that a simplified 50-loci cgMLST scheme successfully classified isolates into subtypes while maintaining epidemiological concordance, offering a practical solution for standardizing WGS analysis across public health laboratories.
In the context of Clostridioides difficile infections, WGS has revealed important insights into population structures that were obscured by traditional ribotyping methods. A 2025 study analyzing C. difficile isolates from hospitals in Berlin-Brandenburg found that cgMLST analysis revealed very close genetic relatedness between RT027 isolates despite their epidemiological unrelatedness, suggesting a monomorphic population structure. Similar patterns were observed for RT078 isolates, while other ribotypes showed more heterogeneous populations [8]. These findings have important implications for outbreak investigations, suggesting that for monomorphic strains like RT027 and RT078, new definitions of clonal relatedness may be necessary when using high-resolution WGS methods.
The analytical performance of WGS typing methods has been systematically validated in national surveillance systems. For STEC outbreak detection, a comprehensive evaluation of PulseNet 2.0's WGS-based approaches demonstrated high concordance between hqSNP, cgMLST, and wgMLST methods. The regression slope for hqSNP versus cgMLST allele differences was 0.432, while the slope for hqSNP versus wgMLST (chromosomal loci) was 0.966, indicating a nearly 1:1 relationship for the latter comparison [7]. K-means analysis using the Silhouette method showed clear separation of outbreak groups with average silhouette widths ≥0.87 across all methods, confirming the robust clustering performance of WGS-based typing approaches.
Table 2: Performance Metrics of WGS Typing Methods for STEC Outbreak Detection
| Method | Comparison to hqSNP (Regression Slope) | Average Silhouette Width | Typical Analysis Time | Technical Complexity |
|---|---|---|---|---|
| hqSNP | Reference | ≥0.87 | Longer | High |
| wgMLST | 0.966 | ≥0.87 | Moderate | Moderate |
| cgMLST | 0.432 | ≥0.87 | Faster | Lower |
Implementation and Workflow Integration
The integration of WGS into public health and clinical laboratories has been facilitated by the development of automated platforms and standardized bioinformatics pipelines. These advancements have addressed earlier challenges related to workflow complexity, turnaround time, and technical expertise requirements.
Automated WGS platforms have demonstrated significant improvements in efficiency compared to manual methods. A 2025 evaluation of the Clear Dx WGS platform for bacterial strain typing found that the automated workflow reduced turnaround time by 16–19 hours and eliminated 3 hours of manual labor while decreasing costs by an estimated 34%–57% depending on the number of isolates processed [9]. Despite these efficiency gains, the analytical performance remained statistically similar to manual methods, with 99% concordance in isolate groupings across 224 bacterial isolates representing 18 species. This demonstrates that automation can substantially improve workflow efficiency without compromising data quality.
National genomic surveillance networks have developed sophisticated infrastructure to support WGS implementation. France's Genomic Medicine Initiative (PFMG2025) has established a comprehensive framework including reference centers, clinical laboratories, and data analysis facilities [10]. Similarly, PulseNet USA's transition to PulseNet 2.0 implemented a cloud-based, modular platform that performs end-to-end analysis including sequence quality assessment, de novo assembly, speciation, allele calling, and genotyping tasks using standardized workflows [7]. These standardized systems enable comparable results across different laboratories and facilitate rapid cluster detection.
The development of novel MLST schemes based on WGS data represents another advancement in the field. For Staphylococcus capitis, researchers applied a hierarchical filtering strategy to core genome analysis of 603 high-quality genomes to develop an optimized MLST scheme with superior discriminatory power [11]. This approach identified seven target genes (mntC, phoA, atpB_2, hisS, rluB, carB, and clpP) that provided an optimal balance between cluster resolution and discrimination, successfully distinguishing clinically relevant lineages like the NRCS-A clone (ST1) and linezolid-resistant L clone (ST6). This methodology demonstrates how WGS data can inform the development of more effective typing schemes even for traditionally challenging organisms.
Troubleshooting Guide: Addressing Common WGS Implementation Challenges
Frequently Asked Questions
Q: Our NGS library yields are consistently low, leading to failed runs or insufficient coverage for reliable typing. What are the primary causes and solutions? A: Low library yield can result from multiple factors in the preparation process:
- Poor input DNA quality: Degraded DNA or contaminants (phenol, salts, EDTA) inhibit enzymatic reactions. Check 260/280 and 260/230 ratios and re-purify if necessary [12].
- Inaccurate quantification: UV spectrophotometry (NanoDrop) often overestimates concentration. Use fluorometric methods (Qubit) for accurate DNA quantification [12] [13].
- Fragmentation issues: Over- or under-shearing creates suboptimal fragment sizes. Optimize fragmentation parameters for your specific instrument [12].
- Adapter ligation inefficiency: Incorrect adapter-to-insert ratios reduce yield. Titrate adapter concentrations and ensure fresh ligase reagents [12].
Q: We observe high rates of adapter dimers in our sequencing results, reducing useful sequence data. How can we minimize this? A: Adapter dimers (sharp ~70-90 bp peaks in electropherograms) indicate ligation issues:
- Optimize purification: Increase bead cleanup ratios to better exclude small fragments [12].
- Adjust adapter concentration: Excess adapters promote dimer formation; titrate to find optimal concentration [12].
- Verify fragment size: Ensure your insert DNA is properly sized before adapter ligation [12].
Q: How do we handle plasmid mixtures or contaminated samples that complicate assembly and analysis? A: Sample purity is critical for reliable WGS:
- Validate sample quality: Run uncut plasmid on gel or BioAnalyzer to detect multiple species or concatemers [13].
- Linearize plasmids: Distinguish monomers from multimers by running linearized preparations [13].
- Size selection: Gel extraction can isolate the target plasmid from contaminants [13].
- Note: Automated pipelines typically only return consensus for the most abundant species, potentially missing minor variants [13].
Q: What coverage depth is sufficient for reliable cgMLST calling in bacterial isolates? A: Coverage requirements vary by application:
- Manual WGS: Typically targets 100× coverage for most species, though 200× may be needed for difficult genomes like C. difficile [9].
- Automated WGS: Can achieve reliable results with lower coverage (30-80× depending on genome size), with actual coverage often averaging 88× [9].
- Quality metrics: For Oxford Nanopore sequencing, ~20× coverage generally produces highly accurate consensus sequences [13].
Q: How do we validate that our WGS typing results are epidemiologically relevant? A: Validation requires multiple approaches:
- Compare with known outbreaks: Test methods on previously characterized outbreaks to establish thresholds [6] [7].
- Use multiple schemes: Compare cgMLST, wgMLST, and hqSNP results for concordance [7].
- Establish allele difference thresholds: For STEC, PulseNet uses 0-10 cgMLST allele differences to define clusters [7].
- Epidemiological correlation: Always correlate genetic relatedness with epidemiological data [8] [6].
Technical Issue Resolution Table
Table 3: Troubleshooting Common WGS Preparation Issues
| Problem | Primary Indicators | Root Causes | Corrective Actions |
|---|---|---|---|
| Low Library Yield | Low molar concentration; faint electropherogram peaks | Input DNA degradation; contaminants; quantification errors | Re-purify DNA; use fluorometric quantification; optimize fragmentation [12] |
| High Adapter Dimer Rate | Sharp ~70-90 bp peak in BioAnalyzer | Excessive adapters; inefficient ligation; incomplete cleanup | Titrate adapter:insert ratio; optimize bead cleanup; verify fragment size [12] |
| Insufficient Coverage | <20× average coverage; poor assembly metrics | Low input DNA; sequencing failures; poor library quality | Verify DNA concentration fluorometrically; check library quality metrics; repeat preparation [9] [13] |
| Poor Assembly Quality | Low N50; many contigs; missing genes | Mixed samples; high fragmentation; repetitive elements | Check sample purity; optimize DNA extraction; use appropriate assembler [6] [11] |
| Discordant Typing Results | Inconsistent cluster assignments between methods | Different analytical schemes; quality thresholds | Standardize scheme; validate against reference isolates; establish QC metrics [6] [7] |
Essential Reagents and Research Solutions
Successful implementation of WGS for molecular typing requires careful selection of reagents and platforms optimized for specific applications. The following solutions represent key components of robust WGS workflows for public health and research laboratories.
Table 4: Essential Research Reagents and Platforms for WGS Typing
| Reagent/Platform | Function | Application Notes | Performance Characteristics |
|---|---|---|---|
| Clear Dx WGS Platform | Automated nucleic acid extraction and sequencing | Fully automated solution for bacterial strain typing; integrates liquid handling, thermocyclers, and sequencers | Reduces turnaround time by 16-19h; decreases costs by 34-57%; 99% concordance with manual methods [9] |
| Nextera XT DNA Library Prep Kit | Manual library preparation | Fragment DNA and attach adapters in single-tube reaction | Compatible with Illumina sequencing; used in multiple validation studies [9] [8] |
| Kapa HyperPlus Library Prep Kit | Manual library preparation | High-performance kit for challenging samples | Used in Legionella WGS studies; provides uniform coverage [6] |
| SeqSphere+ Software | cgMLST analysis | Commercial platform for allele calling and cluster analysis | Supports standardized cgMLST schemes; used in multiple validation studies [9] [8] [6] |
| BioNumerics wgMLST | Whole genome analysis | Integrated platform for wgMLST analysis | Used in PulseNet validation; demonstrates high concordance with hqSNP [7] |
| SKESA Assembler | De novo assembly | Optimized for bacterial genome assembly | Used in multiple public health pipelines including PulseNet 2.0 [9] [7] |
The revolution in molecular typing brought by whole-genome sequencing represents a fundamental shift in how public health laboratories detect and investigate disease outbreaks. The superior discriminatory power of WGS-based methods like cgMLST and wgMLST has enabled investigators to distinguish between related and unrelated isolates with precision that was previously unattainable with PFGE or traditional MLST. As standardization improves and costs continue to decline, WGS is poised to become the universal method for pathogen characterization in public health, clinical, and research settings.
The implementation of automated WGS platforms and streamlined bioinformatics pipelines will further accelerate this transition, making high-resolution typing accessible to a broader range of laboratories. Future developments will likely focus on real-time analysis during outbreaks, integration of antimicrobial resistance prediction, and direct sequencing from clinical samples to bypass culture requirements. As these advancements mature, WGS will continue to enhance our ability to track disease transmission, identify emerging threats, and implement targeted control measures with unprecedented speed and accuracy.
Frequently Asked Questions (FAQs)
1. What is the key difference between Simpson's Index and the Shannon Index? Simpson's Index and the Shannon Index respond differently to the abundance of species or types in a community. The Shannon Index is more sensitive to the presence of rare species, while Simpson's Index is more sensitive to changes in the abundance of the most common species [14] [15]. This means that in communities with the same richness but different evenness, these two indices can sometimes show opposite trends [15].
2. My Simpson's Index value decreased after a treatment, but my Shannon Index increased. Is this possible? Yes, this is a possible scenario and highlights why choosing the correct index is critical. This opposite response occurs because the indices weight different aspects of the population. An increase in the Shannon Index suggests an increase in the number of rare types, to which it is sensitive. A simultaneous decrease in Simpson's Index suggests a reduction in evenness, likely through an increased dominance of one or a few common types, to which Simpson's Index is sensitive [15]. You should interpret this result based on which component—rare types or dominant types—is more relevant to your research question.
3. When should I use Simpson's Index over the Shannon Index in my genomic research? The choice depends on your research focus:
- Use Simpson's Index (or its reciprocal/inverse, Simpson's Diversity,
1/D) when your primary interest is in understanding the dominance and evenness of common subtypes, for instance, when tracking the spread of a dominant pathogen strain in an outbreak [15]. - Use the Shannon Index when your study is concerned with the full diversity profile, particularly the presence and importance of rare subtypes. This is often crucial in ecological studies and for conservation purposes, where rare species provide critical habitats [15].
4. How do I calculate Simpson's Diversity Index from my data? Simpson's Index can be calculated in a few related ways. A common formula used in ecology is: Simpson's Index of Diversity = 1 - D, where D = Σ n(n-1) / N(N-1) [16].
n= the total number of organisms of a particular species/typeN= the total number of organisms of all species/typesΣ= the sum of the calculations for each species/type [16]
This calculation yields a value between 0 and 1, where 1 represents infinite diversity and 0 represents no diversity [16].
5. What are "Hill's numbers" and how do they relate to common diversity indices?
Hill's numbers provide a unified framework for diversity indices, known as the effective number of species or "true diversity" [17] [14]. They are represented by qD, where the parameter q defines the sensitivity to species abundances. Common diversity indices are special cases of Hill's numbers [17]:
0D(q=0): Species Richness (S). Sensitive to rare species.1D(q=1): Exponential of Shannon entropy (exp(H')). Equally sensitive to all species.2D(q=2): Inverse Simpson index (1/D). Sensitive to common species. Using Hill's numbers allows for a more consistent and intuitive comparison across communities [17] [14].
Troubleshooting Guides
Issue: Low Discriminatory Power in My Multilocus Sequence Typing (MLST) Scheme
Problem: Your current MLST scheme is not providing enough resolution to distinguish between closely related bacterial isolates, leading to an unclear picture of transmission dynamics.
Solution:
- Re-evaluate Locus Selection: The core of a high-resolution MLST scheme is the selection of highly variable genes. Follow this validated workflow for designing a new scheme:
This workflow is adapted from a study that developed a high-resolution MLST scheme for *Treponema pallidum [18].*
- Increase the Number of Loci: If you are using an older scheme with fewer than seven loci, consider expanding it. A seven-gene MLST scheme is a standard and robust approach that has been successfully applied to various pathogens like Staphylococcus aureus and Treponema pallidum to achieve high discriminatory power [18].
- Consider Alternative Typing Methods: If optimizing MLST fails, transition to a Multi-Locus Variable Number Tandem Repeat Analysis (MLVA). MLVA typically offers higher resolution than MLST because it targets rapidly evolving VNTR regions. This method has been shown to subdivide common Cryptosporidium parvum gp60 subtypes into multiple distinct MLVA profiles, greatly enhancing outbreak investigation [19].
Issue: Choosing the Wrong Diversity Index Leading to Misinterpretation
Problem: The diversity index you selected is giving counter-intuitive results or is not aligned with your research question, potentially leading to incorrect conclusions.
Solution: Follow this decision pathway to select the most appropriate index:
This guide synthesizes insights from ecological studies comparing index behavior [14] [15].
Verification: After selecting an index, validate your results by calculating a second, complementary index. For example, if you use Simpson's Index, also calculate the Shannon Index. If they show opposite trends, investigate the species abundance distribution in your data to understand why, as this is a known phenomenon [15].
Comparative Tables of Key Metrics
Table 1: Core Diversity Indices and Their Properties
| Index Name | Formula | Sensitivity | Interpretation | Common Use Case |
|---|---|---|---|---|
| Species Richness (S) | S = Count of types [17] |
Rare species [14] | The total number of different types/species present. | Quick assessment of variety; detecting impacts of disturbance [14]. |
| Shannon Index (H') | H' = -∑(p_i * ln(p_i)) [17] |
Equally sensitive to rare and abundant species [14] | Measures the uncertainty in predicting the identity of a randomly chosen individual. A higher H' indicates greater diversity [17] [14]. | General-purpose diversity assessment; emphasizes overall heterogeneity [15]. |
| Simpson's Index (D) | D = ∑(p_i²) [17] |
Abundant species [14] | The probability that two randomly chosen individuals belong to the same type. | Emphasizes the dominance of common types [15]. |
| Simpson's Index of Diversity | 1 - D [16] |
Abundant species | The probability that two randomly chosen individuals belong to different types. Ranges from 0-1 [16]. | More intuitive interpretation of diversity; used in ecology [16]. |
| Inverse Simpson Index | 1 / D [17] |
Abundant species | Equivalent to Simpson's Diversity in Hill's numbers (²D) [17] [14]. Represents the effective number of common species. |
Used in population genetics and community ecology. |
| Berger-Parker Index | 1 / p_max [14] |
Most abundant species only | The reciprocal of the proportion of the most abundant type. Measures dominance [14]. | Assessing the dominance of a single type in a community. |
Table 2: Research Reagent Solutions for Genomic Subtyping
| Reagent / Material | Function in Experiment | Specification / Notes |
|---|---|---|
| Target Genomic DNA | The template for PCR amplification in MLST or MLVA. | For best results, use DNA extracted from clinical/environmental samples with sufficient pathogen burden. Sample concentration and purity are critical [18]. |
| Primers (Oligonucleotides) | To amplify specific, highly variable genetic loci for sequencing or fragment analysis. | Should be designed to anneal to conserved regions flanking variable sites. Follow design criteria: 18-22 bp length, 45-60% GC content, amplicon size of 400-700 bp [18]. |
| PCR Master Mix | Enzymatic amplification of the target loci. | Must be high-fidelity to minimize errors during amplification, especially when Sanger sequencing is the next step. |
| Sanger Sequencing Kit | Determining the nucleotide sequence of the amplified MLST loci. | Required for traditional MLST. The workflow is suitable for laboratories with standard Sanger sequencing resources [18]. |
| Capillary Electrophoresis System | For fragment size analysis in MLVA protocols. | Used to separate and size the amplified VNTR fragments from an MLVA reaction, generating the profile data [19]. |
| PubMLST Database | A public repository for curating and comparing allele profiles and sequence types. | Enables standardization and global comparison of your typing data with other isolates [18]. |
Troubleshooting Guides and FAQs
Guide 1: Addressing Multi-Omics Data Integration Challenges
Problem: My multi-omics subtyping results are unstable and fail to capture biologically meaningful patterns.
Root Cause: This often stems from relying on a single distance metric that cannot capture the complex relationships in your molecular data. Euclidean distance alone may miss important directional patterns in feature vectors [20].
Solution: Implement a multi-metric consensus approach.
Actionable Steps:
- Calculate both Euclidean and Angular distance matrices for each omics data type [20].
- Convert distances to affinity matrices using a scaling parameter
σ, typically set as the median of all pairwise Euclidean distances [20]. - Construct separate consensus matrices for Euclidean affinity, Angular affinity, and overall connectivity.
- For small datasets (<200 samples), average full affinity matrices. For larger datasets, employ stability-driven approaches to mitigate sensitivity to data size [20].
Validation: Compare cluster stability using internal validation metrics (silhouette width, Dunn index) across different metric combinations. Biologically validate subtypes using known pathway enrichment.
Problem: I have significant missing data across omics types, leading to substantial sample loss.
Solution: Utilize methods specifically designed for incomplete multi-omics data.
- Actionable Steps:
- Implement frameworks like DSCC or NEMO that can handle missing modalities [20].
- Apply gene-level aggregation to create a consistent framework across mRNA, miRNA, DNA methylation, and protein data when possible [20].
- For metabolomics data, apply log2 transformation and replace missing values with zero after confirming this is appropriate for your data structure [20].
Guide 2: Improving Subtyping Discriminatory Power
Problem: My current subtyping method lacks directional awareness and fails to differentiate subtle molecular patterns.
Root Cause: Traditional magnitude-based metrics neglect angular relationships between feature vectors, which can be particularly important for capturing distinct molecular signatures [20].
Solution: Incorporate angular distance metrics to enhance pattern discrimination.
Technical Implementation:
Expected Improvement: Studies show combining angular and Euclidean affinity captures complementary views of each omics type, significantly improving subtyping performance [20].
Problem: I need to incorporate biological knowledge but lack pathway information for non-transcriptomic data.
Solution: Map diverse molecular features to gene-level representations compatible with existing pathway databases.
- Actionable Steps:
- For miRNA data: Map miRNA IDs to target genes using miRTarBase or similar databases [20].
- For DNA methylation: Map CpG sites to genes using manufacturer-provided annotations and calculate median methylation per gene.
- For protein data: Average measurements of all proteins encoded by the same gene.
- Remove genes not associated with KEGG or Reactome pathways to focus on biologically interpretable features [20].
Guide 3: Validating Clinical Relevance of Subtypes
Problem: My molecular subtypes don't correlate with clinical outcomes or treatment response.
Root Cause: Subtypes may reflect technical artifacts rather than biologically distinct groups with clinical relevance.
Solution: Integrate multiple clinical endpoints into subtyping validation.
Methodology: Implement multi-endpoint frameworks like MuTATE that simultaneously model overall survival, progression-free survival, and tumor-free survival during subtype discovery [21].
Clinical Validation Protocol:
- Use subtype information as a covariate in prognostic models to test if it improves survival prediction accuracy [20].
- In umbrella trial designs (like FUTURE for TNBC), assign different targeted therapies based on molecular subtypes and compare outcomes across arms [22].
- Evaluate if subtypes show differential response to specific drug classes in preclinical models.
Success Metrics: Look for statistically significant separation in survival curves (p < 0.05) and objective response rates that differ by ≥20% between subtypes receiving matched versus unmatched therapies [22].
Experimental Protocols for Enhanced Discriminatory Power
Protocol 1: DSCC Multi-Omics Subtyping Workflow
Objective: Identify disease subtypes from diverse molecular data using spectral clustering and community detection.
Materials: Processed multi-omics data (gene expression, miRNA, methylation, CNV, mutations, protein, metabolites)
Methodology:
Data Processing:
- Perform gene-level aggregation for all possible data types (mRNA, miRNA, methylation, protein)
- Map features to KEGG-compatible representations
- Apply log2 transformation to metabolomics data, replace missing values with zero
Network Construction:
- Calculate both Euclidean and Angular affinity matrices for each data matrix
- Set scaling parameter σ as median of pairwise Euclidean distances
- Construct three consensus matrices: Euclidean affinity, Angular affinity, connectivity
Ensemble Clustering:
- Apply both spectral clustering (captures global structure) and Louvain community detection (captures local patterns)
- Integrate results from multiple algorithms and metrics
- Validate cluster stability using bootstrapping approaches
Validation: Compare against 13 state-of-the-art methods using 43 cancer datasets with >11,000 patients [20].
Protocol 2: Multi-Endpoint Decision Tree Optimization
Objective: Generate interpretable molecular subtypes that optimize multiple clinical endpoints.
Materials: Molecular feature matrix with associated clinical outcomes (overall survival, progression-free survival, treatment response)
Methodology:
Data Preparation:
- Curate molecular features from sequencing, proteomic, or epigenetic profiling
- Annotate with multiple clinical endpoints
- Split data into training (60%) and validation (40%) sets
MuTATE Framework Application:
- Implement multi-target decision tree algorithm that jointly models all clinical endpoints
- Compare against single-endpoint CART models
- Optimize tree depth and partitioning parameters via grid search
Clinical Interpretation:
- Analyze reassignment of cases between risk categories compared to established models
- Validate novel subtypes using external datasets when available
- Perform biomarker discovery from splitting rules in decision trees
Performance Metrics: In simulations, MuTATE showed significantly lower test error (2.97 vs. >3.0 for CART) and lower false discovery rate (5.7% for 5-target vs. 11.0% for CART) [21].
Table 1: Performance Comparison of Advanced Subtyping Methods
| Method | Key Innovation | Validation Scale | Accuracy Improvement | Clinical Utility |
|---|---|---|---|---|
| DSCC | Multi-distance metrics + ensemble clustering | 43 cancer datasets (>11,000 patients) | Superior to 13 state-of-art methods [20] | Improves survival prediction as covariate [20] |
| MuTATE | Multi-endpoint decision trees | 682 patients across 3 cancers | Reclassified 13-72% of cases [21] | Enhanced risk stratification accuracy [21] |
| FUTURE Trial | Subtype-guided targeted therapy | 141 metastatic TNBC patients | 29.8% objective response rate in heavily pretreated patients [22] | 4/7 arms achieved efficacy boundaries [22] |
Table 2: Troubleshooting Common Subtyping Experimental Failures
| Failure Mode | Root Cause | Diagnostic Signals | Corrective Actions |
|---|---|---|---|
| Low discriminatory power | Single distance metric limitations | Poor cluster separation, unstable assignments | Implement multi-metric consensus (Euclidean + Angular) [20] |
| Poor biological relevance | Lack of pathway context | Subtypes not enriched for known pathways | Map multi-omics features to KEGG-compatible gene representations [20] |
| Weak clinical correlation | Single-endpoint optimization | Subtypes don't predict multiple outcomes | Implement multi-endpoint frameworks like MuTATE [21] |
| Missing data bias | Exclusion of samples with incomplete omics | Reduced sample size, selection bias | Use methods that handle missing data (DSCC, NEMO) [20] |
Pathway and Workflow Visualizations
Research Reagent Solutions
Table 3: Essential Research Reagents for Genomic Subtyping Experiments
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| KEGG Pathway Database | Biological pathway reference for gene aggregation | Enables consistent multi-omics framework; focus on pathway-associated genes [20] |
| miRTarBase | miRNA-to-gene mapping resource | Critical for incorporating miRNA data into gene-level framework [20] |
| PharmGKB/CPIC Guidelines | Pharmacogenomic clinical implementation | Essential for translating subtypes to treatment recommendations [23] |
| TCGA/Public Data Portals | Validation datasets and benchmarking | Required for method comparison across >11,000 patients [20] |
| Custom Gene Panels | Targeted sequencing for validation | Balance coverage depth with cost; useful for subclonal mutation detection [24] |
| Imaging Mass Cytometry | Spatial proteomic profiling | Reveals tumor microenvironment context of molecular subtypes [24] |
| DEPICT/MAGMA Tools | Gene prioritization and pathway analysis | Supports functional interpretation of subtype-discriminating features [25] |
A Toolkit for Modern Biology: Core Genomic Subtyping Methods and Their Applications
Core Genome Multilocus Sequence Typing (cgMLST) is a high-resolution, whole-genome sequencing (WGS)-based method that characterizes bacterial isolates by indexing genetic variation across hundreds to thousands of core genes—those shared by all or nearly all isolates of a species [26]. This technique extends the principles of traditional multilocus sequence typing (MLST), which typically analyzes only six to eight housekeeping genes, by utilizing a much larger portion of the genome. This expansion offers a powerful tool for standardized genomic surveillance, providing the discriminatory power necessary for detailed epidemiological investigations while ensuring global comparability of results [27].
The primary advantage of cgMLST lies in its ability to provide a universal nomenclature for bacterial typing. Unlike traditional methods such as pulsed-field gel electrophoresis (PFGE), which produces results that can be subjective and difficult to interpret, cgMLST generates portable, unambiguous data that can be directly compared across laboratories worldwide [1] [28]. This is crucial for tracking the global spread of pathogens, investigating outbreaks, and understanding bacterial population dynamics. Furthermore, cgMLST is less affected by the confounding effects of horizontal gene transfer and recombination compared to methods based on single nucleotide polymorphisms (SNPs) for some species, as it treats all allelic changes as single events, making it particularly suitable for analyzing highly recombining organisms like Haemophilus influenzae and Moraxella catarrhalis [26] [27].
cgMLST Workflow: From Scheme Definition to Isolate Analysis
Developing and implementing a cgMLST scheme is a multi-stage process that requires careful planning and validation. The workflow can be broadly divided into two main phases: (1) the initial development and evaluation of the typing scheme itself, and (2) the application of the scheme to analyze and type new bacterial isolates. The following diagram illustrates the key stages involved in creating a stable cgMLST scheme.
Diagram Title: cgMLST Scheme Development Workflow
Defining the cgMLST Scheme
The process begins with the careful selection of a seed genome. This genome must be complete, well-annotated, and publicly accessible (e.g., from NCBI). Ideally, the seed isolate should be a type strain or another well-characterized strain available from a culture collection [29]. For example, in developing a scheme for Neisseria meningitidis, the FAM18 strain (accession NC_008767) can serve as the seed genome [29].
Next, a diverse set of penetration query genomes is added to represent the full genetic variation within the species. These genomes should span different sequence types (STs) and clonal complexes (CCs). A good starting point is to select all available finished genomes from NCBI, perform an MLST analysis, and then choose genomes that differ by ST and/or CC [29]. The example for N. meningitidis uses a list of 13 NCBI accession numbers. It is also possible to incorporate assembled sequence data from other sources, such as NCBI SRA or your own sequenced isolates, if sufficient complete genomes are not available [29].
A critical quality control step involves removing outlier genomes. Software tools can compare all query genomes against the seed genome's genes. Genomes where a significantly lower percentage (e.g., only 76% in an example with Pseudomonas aeruginosa) of the non-homologous seed genes are found should be considered taxonomic outliers and excluded from the scheme definition process [29].
To ensure the scheme focuses on chromosomal genes, it is advisable to exclude genes from mobile genetic elements. This can be done by adding plasmid sequences from the same species to an "exclude" list. For instance, the N. meningitidis scheme development incorporated two known plasmid sequences to prevent plasmid-borne genes from being included in the cgMLST targets [29].
Finally, the calculation of the scheme is performed using specialized software. This process categorizes every gene from the seed genome into one of three groups [29]:
- cgMLST: Genes that are non-homologous, have valid start/stop codons in the seed genome, appear uniquely in all query genomes, and do not have invalid stop codons in most queries. These form the targets for typing.
- Accessory: Genes that are non-homologous but may overlap with others, not appear in all queries, or have invalid stop codons in many queries. These are not part of the core scheme but can be used to increase discriminatory power.
- Discarded: Genes that are homologous or have invalid start/stop codons in the seed genome. These are not used.
Evaluating and Validating the cgMLST Scheme
Once a scheme is defined, it must be rigorously evaluated. A pragmatic first test is to re-sequence the seed strain using a modern NGS platform (e.g., Illumina) and analyze the data with the new scheme. The expectation is that 98.5% or more of the cgMLST targets should be found and pass all automated checks. If not, the reasons for failure must be investigated, and problematic targets might be moved to the accessory genome [29].
The most comprehensive evaluation involves testing the scheme against a well-characterized and diverse collection of isolates that represents the entire population genetic background of the species. The scheme is considered stable if most genomes in this collection have at least 95% good cgMLST targets. If some genomes fall below this threshold, the scheme definition process should be iterated by adding more representative isolates as query genomes [29].
After successful validation, the scheme can be finalized and implemented on public platforms like PubMLST to ensure global accessibility [26] [27]. For example, the cgMLST scheme for Haemophilus influenzae was developed using a dataset of over 2,200 genomes and subsequently implemented in PubMLST, providing a standardized tool for public health authorities worldwide [26].
Performance Comparison of Bacterial Typing Methods
Different typing methods offer varying levels of resolution, which must be matched to the specific epidemiological question. The table below summarizes the key advantages and disadvantages of the most common methods, highlighting the position of cgMLST.
Table 1: Comparison of Bacterial Subtyping Methods
| Subtyping Method | Advantages | Disadvantages |
|---|---|---|
| Whole Genome Sequencing (WGS) | - Can be tailored for low or high discriminatory power- Provides phylogenetically relevant data- High reproducibility if standardized- High typability- Broadly applicable to any species | - High cost (though decreasing)- Requires significant technical and bioinformatics expertise- Long turn-around time in some settings- Complex data interpretation [1] |
| Core Genome MLST (cgMLST) | - High discriminatory power and reproducibility- Standardized nomenclature for global surveillance- Mitigates effects of recombination- Easier data interpretation and comparison than WGS SNP analysis | - Requires a pre-defined, validated scheme- Dependent on quality of genome assemblies- May miss recent outbreaks in highly clonal populations without accessory genome |
| Pulsed-Field Gel Electrophoresis (PFGE) | - Historical gold standard for outbreak investigations- High reproducibility when standardized- High typability- Relatively inexpensive | - Labor-intensive- Results can be subjective and difficult to interpret- Does not produce phylogenetically relevant information [1] |
| Multilocus Sequence Typing (MLST) | - Used for phylogenetic studies- High repeatability and reproducibility- High typability- Portable data | - Low to moderate discriminatory power (little use in outbreaks)- Moderately expensive and labor-intensive- Requires adaptation/validation for each species [1] |
The superior discriminatory power of cgMLST is evident in a study of Clostridium difficile, where WGS (using an SNV approach) revealed that among patient pairs whose isolates matched by MLST and were on the same hospital ward, 28% of the pairs were actually highly genetically distinct (with >10 SNVs difference). This demonstrates that MLST, which queries only a small fraction of the genome, can group together genetically unrelated isolates, whereas cgMLST provides the resolution needed for accurate transmission mapping [1].
cgMLST in Action: Key Applications and Experimental Findings
Case Study: Resolving the Population Structure ofMoraxella catarrhalis
A recent study developed a cgMLST scheme comprising 1,319 core genes to investigate the population structure of nearly 2,000 M. catarrhalis genomes [27]. The scheme confirmed the existence of two divergent lineages, seroresistant (SR) and serosensitive (SS), with distinct evolutionary paths. The SR genomes were more conserved, while the SS genomes showed greater genetic variability. The cgMLST data, combined with a Life Identification Number (LIN) code system, provided a robust framework for characterizing lineages and identifying variations in virulence genes and antimicrobial resistance elements, such as the bro β-lactamase, which was more common in SR lineages [27].
Case Study: Tracking OXA-48-ProducingKlebsiella pneumoniae
A study of OXA-48-producing K. pneumoniae compared cgMLST using two different schemes (SeqSphere+ with 2,365 genes and Institut Pasteur's BIGSdb-Kp with 634 genes) with whole-genome MLST (wgMLST) and core-genome SNP (cgSNP) analysis [28]. For the predominant sequence type, ST405, cgMLST using SeqSphere+ found 0–10 allele differences between isolates, while wgMLST found 0–14 differences. The cgSNP analysis showed 6–29 SNPs even in isolates with identical cgMLST profiles. This highlights that while different high-resolution methods may yield slightly different results, they generally lead to the same epidemiological conclusions. The study emphasized that threshold parameters for defining relatedness must be applied cautiously and in conjunction with clinical data [28].
Table 2: Key Research Reagents and Resources for cgMLST
| Item | Function in cgMLST Analysis |
|---|---|
| Seed Genome | A complete, annotated reference genome from a well-characterized strain (e.g., type strain) that serves as the foundation for defining the core gene set. [29] |
| Penetration Query Genomes | A diverse panel of genomes spanning the genetic breadth of the species, used to identify a stable set of core genes present in most isolates. [29] |
| BIGSdb (PubMLST Platform) | A widely used open-source platform for hosting and curating cgMLST schemes and allele databases, enabling standardized global analysis and nomenclature. [26] [30] |
| Ridom SeqSphere+ Software | A commercial software application that facilitates the entire cgMLST workflow, from scheme development and data analysis to visualization and cluster detection. [29] [28] |
| chewBBACA | An open-source bioinformatics tool for pangenome analysis and cgMLST scheme development, used to identify core genes and call alleles. [26] |
| Pathogenwatch | A free, web-based platform that uses cgMLST schemes from PubMLST and other sources to rapidly genotype uploaded genomes and identify close relatives. [31] [32] |
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: My newly developed cgMLST scheme fails to call a large number of targets in my evaluation dataset. What could be wrong? A1: A high rate of failure to call targets often indicates an unstable scheme. This typically occurs when the initial set of penetration query genomes was not diverse enough to capture the full genetic variation of the species. The solution is an iterative process: acquire additional representative isolates, produce high-quality draft genomes, and add them as new query genomes to re-calculate and refine the cgMLST scheme [29].
Q2: How do I determine the threshold for considering two isolates as part of the same outbreak cluster using cgMLST? A2: There is no universal threshold. The number of allele differences that defines a cluster is species-specific and context-dependent. Thresholds should be established based on retrospective analysis of well-defined outbreaks and population genetic studies of the species. For example, a study on K. pneumoniae suggested a genetic distance threshold of 0.0035 for cgMLST to discriminate between related and unrelated isolates. It is critical to use such thresholds in combination with epidemiological data [28].
Q3: What is the difference between a "stable" and an "ad hoc" cgMLST scheme? A3: A stable scheme provides a public, expandable nomenclature and is laborious to define, evaluate, and calibrate. Once approved, it is available for immediate use by the global community. In contrast, an ad hoc scheme provides a local nomenclature and can be established quickly by individual users for specific, limited analyses [29].
Q4: How does cgMLST handle the issue of homologous genes and paralogs? A4: The presence of paralogs (duplicated genes) can mislead genetic relationships. During scheme development, software pipelines (e.g., chewBBACA, Panaroo) include steps to identify and filter out paralogous loci. Furthermore, a robust scheme should be developed and validated using a large dataset (e.g., >500 genomes), which has been identified as a threshold for stable paralogous locus detection [26].
Q5: My assembly quality is good, but the cgMLST analysis flags many missing genes. What should I check? A5: First, verify that the assembly pipeline has not introduced systemic errors. Differences in assembly methods can sometimes lead to fragmented genes or missing regions, particularly in repetitive areas. Check the "Stats" table in your analysis platform for quality metrics. If the quality is confirmed, investigate whether the missing genes are part of a known difficult-to-assemble gene family (e.g., the PPE & PE gene family in M. tuberculosis). If problems are repeatedly observed for certain targets, they might need to be manually removed from the core scheme and added to the accessory genome [29] [31].
Frequently Asked Questions (FAQs)
1. What is the primary advantage of wgMLST over traditional molecular typing methods?
wgMLST provides significantly higher discriminatory power compared to traditional methods like pulsed-field gel electrophoresis (PFGE) or conventional multilocus sequence typing (MLST). While standard MLST targets only 7-8 housekeeping genes, wgMLST extends this to thousands of core and accessory genes across the entire genome, enabling detection of even minor genetic variations between closely related isolates. This enhanced resolution is particularly valuable for precise outbreak investigations and transmission tracking [33] [34].
2. How does wgMLST differ from cgMLST?
Whole genome MLST (wgMLST) analyzes both the core genome (genes present in all isolates of a species) and the accessory genome (genes variably present among isolates). In contrast, core genome MLST (cgMLST) focuses only on the core genome. The inclusion of accessory genes in wgMLST provides additional discriminatory power, especially for distinguishing closely related bacterial strains that may have acquired or lost specific genetic elements [35] [36].
3. What are typical allele difference thresholds for distinguishing outbreak-related isolates?
The acceptable number of allele differences for considering isolates as part of the same outbreak varies by bacterial species. For Pseudomonas aeruginosa, epidemiologically linked isolates typically show 0-13 allele differences in wgMLST analysis. However, these thresholds should be established for each specific pathogen and validated with epidemiological data [36].
4. What software tools are available for wgMLST analysis?
Several bioinformatics tools support wgMLST analysis, including:
- chewBBACA: For schema creation and allele calling [37]
- BioNumerics: Provides integrated wgMLST and cgMLST schemes [36]
- EnteroBase: Enables accessory genome analysis [35]
- pymlst: A Python-based workflow for wgMLST analysis [38]
5. How should I handle paralogous genes in wgMLST analysis?
Paralogous genes (homologous sequences within the same genome resulting from gene duplication) should be identified and removed from your analysis as they can cause uncertainty in allele assignment. The chewBBACA pipeline includes a paralog detection step that outputs a list of potentially paralogous loci, which should be excluded from the final schema [37].
Troubleshooting Guides
Issue 1: Low Number of Loci in cgMLST Schema
Problem: After running ExtractCgMLST, the number of loci in your core genome is unexpectedly low.
Solutions:
- Check genome assembly quality using metrics like N50 value, number of contigs, and assembly size
- Apply quality filters: exclude genomes with >150 contigs, abnormal genome sizes, or >5% missing loci from the cgMLST
- Recompute cgMLST after excluding low-quality assemblies [37]
Example Quality Control Metrics: Table: Recommended Genome Assembly Quality Thresholds
| Metric | Threshold Value | Rationale |
|---|---|---|
| Number of Contigs | <150 | Ensures sufficient assembly continuity |
| Genome Size | Within expected species range | Identifies anomalous assemblies |
| N50 Value | As high as possible (varies by species) | Indicator of assembly fragmentation |
| Missing Loci | <5% of cgMLST | Ensures adequate gene detection |
Issue 2: Discrepancies Between wgMLST and SNP-Based Phylogenies
Problem: Your wgMLST analysis produces clustering results that conflict with SNP-based phylogenies.
Solutions:
- Investigate potential homologous recombination events, which can affect tree topology
- For highly recombinant species like Pseudomonas aeruginosa, consider using cgMLST instead of wgMLST
- Exclude identified recombinant regions from your analysis [36]
Issue 3: Poor Schema Creation or Allele Calling Performance
Problem: chewBBACA schema creation or allele calling fails or produces suboptimal results.
Solutions:
- Ensure you're using the appropriate Prodigal training file for your species
- Verify that input genomes meet quality requirements
- For allele calling, use the correct BLAST Score Ratio (BSR) value (default is 0.6)
- Check that the schema seed and input files are properly formatted [37]
Experimental Protocols
Protocol 1: Creating a wgMLST Schema with chewBBACA
Purpose: Develop a novel wgMLST schema for a bacterial species.
Materials:
- Representative genome assemblies (complete genomes preferred)
- Species-specific Prodigal training file
- Computational resources (minimum 6 CPU cores recommended)
Methodology:
- Install chewBBACA and download necessary datasets
- Run schema creation command:
- Perform allele calling on the same genomes:
- Identify and remove paralogous loci:
- Determine core genome using ExtractCgMLST module with desired threshold (e.g., 95%) [37]
Protocol 2: Accessory Genome Analysis in EnteroBase
Purpose: Identify and visualize accessory genome elements across a set of bacterial isolates.
Materials:
- Assembled genomes with pre-called wgMLST loci
- EnteroBase account with appropriate permissions
Methodology:
- Navigate to "Tasks > Accessory Genome" in EnteroBase
- Click "View Accessory Genome" and select your workspace/tree
- Analyze the visualization interface with three main sections:
- Phylogenetic tree (left panel)
- Presence/absence heatmap of accessory loci (middle panel)
- Strain labels (right panel)
- Use controls to zoom, scroll, and explore specific loci
- Click on loci of interest to view detailed information in genome browser
- Export data as allele matrix or create custom sub-schemes for specific research questions [35]
Table: Comparison of Typing Methods for Pseudomonas aeruginosa Outbreak Investigation [36]
| Typing Method | Epidemiologically Linked Isolate Range | Coefficient of Correlation with SNP (R²) | Discriminatory Power |
|---|---|---|---|
| wgMLST | 0-13 allele differences | 0.78-0.99 | High |
| cgMLST | Not specified | 0.92-0.99 | High |
| SNP calling | 0-26 SNPs | Reference method | Highest |
Table: Effect of Quality Control on cgMLST Schema Size [37]
| Analysis Scenario | Number of Genomes | cgMLST Loci (95% threshold) |
|---|---|---|
| Initial 32 complete genomes | 32 | 1,271 |
| All 712 assemblies (no QC) | 712 | 1,194 |
| After quality filtering | 645 | 1,248 |
Workflow Visualization
wgMLST Analysis Workflow
Core vs. Accessory Genome Analysis
Research Reagent Solutions
Table: Essential Materials for wgMLST Analysis
| Reagent/Resource | Function/Application | Example Sources |
|---|---|---|
| Prodigal Training Files | Gene prediction parameters optimized for specific species | chewBBACA included files [37] |
| wgMLST Schemes | Pre-defined locus sets for specific genera/species | BioNumerics, EnteroBase [35] [36] |
| Quality Control Tools | Assess genome assembly quality before analysis | CLC Genomics Workbench, SPAdes [33] [39] |
| Reference Genomes | Basis for gene presence/absence calls and schema creation | NCBI RefSeq, GenBank [33] [39] |
| Allele Calling Algorithms | Identify known and novel alleles in sequenced genomes | chewBBACA, BioNumerics [37] [36] |
Whole-genome sequencing (WGS) has revolutionized microbial infectious disease surveillance by providing nucleotide-level resolution for investigating outbreaks. Single nucleotide variant (SNV)-based phylogenomic methods have emerged as a powerful approach for classifying microbial samples, offering superior discriminatory power compared to traditional subtyping methods like pulsed-field gel electrophoresis (PFGE) or multilocus sequence typing (MLST) [40] [1]. High-quality core genome SNV (hqSNV) analysis represents a refined methodology that focuses on identifying high-quality variants present in the core genome across a population of isolates, providing a robust foundation for phylogenetic inference. This technical support document details the implementation of hqSNV analysis using the SNVPhyl pipeline, a bioinformatics tool specifically designed for identifying high-quality SNVs and constructing whole-genome phylogenies within the user-friendly Galaxy framework [40].
Framed within broader research to improve discriminatory power in genomic subtyping, hqSNV analysis addresses a critical need in public health microbiology. While traditional MLST methods might classify distantly related isolates as the same sequence type, studies have demonstrated that WGS can reveal significant genetic divergence (e.g., >10 SNVs) within these same MLST-matched pairs, highlighting previously undetected transmission chains and diverse infection sources [1]. The SNVPhyl pipeline operationalizes this enhanced discriminatory capability through an integrated, validated workflow that combines reference mapping, sophisticated variant filtering, and phylogeny construction, making high-resolution outbreak investigation accessible to researchers and public health laboratories [40].
Pipeline Architecture and Key Stages
The SNVPhyl pipeline integrates both pre-existing and custom-developed bioinformatics tools into a cohesive workflow within the Galaxy platform [40]. This integration provides a scalable environment that can be deployed on everything from a local server to a high-performance computing cluster. The workflow proceeds through several critical stages:
- Data Preparation and Quality Control: Input data, consisting of sequence reads and a reference genome, are prepared and validated.
- Sequence Mapping: Reads are mapped to the reference genome using the SMALT aligner.
- Variant Calling: High-quality variants are identified using FreeBayes, with parallel processing by SAMtools/mpileup/BCFtools for verification.
- Variant Filtering: A multi-stage filtering process removes low-quality variants, including those in repetitive regions, recombinant regions, or positions with insufficient coverage.
- Phylogenetic Tree Construction: A maximum-likelihood phylogeny is generated from the filtered SNV alignment using PhyML.
The entire workflow is designed with quality assurance in mind, generating extensive diagnostic outputs that allow researchers to verify each analysis step and troubleshoot potential issues [40] [41].
Workflow Visualization
The following diagram illustrates the logical flow and key stages of the SNVPhyl pipeline:
Essential Research Reagents and Computational Tools
Successful implementation of hqSNV analysis requires specific computational tools and resources. The following table details the essential components of the "research reagent kit" for SNVPhyl-based phylogenomics:
Table 1: Essential Research Reagents and Computational Tools for hqSNV Analysis
| Item Name | Type/Format | Primary Function in Workflow |
|---|---|---|
| Whole-Genome Sequence Reads [42] | FASTQ format (fastqsanger) |
Input data containing sequencing reads from microbial isolates for analysis. |
| Reference Genome [42] [43] | FASTA format | Reference sequence for read mapping and coordinate-based variant identification. |
| Invalid Positions Masking File [42] | BED-like format (tab-delimited) | Optional file to exclude problematic regions (e.g., phage, plasmids) from analysis. |
| SNVPhyl Pipeline [40] [42] | Galaxy Workflow / Docker Image | Core bioinformatics pipeline for hqSNV discovery and phylogeny construction. |
| PHASTER [43] | Web Service / Tool | Used for pre-analysis to identify phage regions in the reference genome for masking. |
Critical Parameters for High-Quality SNV Calling
The discriminatory power of SNVPhyl analysis depends on appropriate parameter settings. These parameters control the stringency for variant calling and filtering, directly impacting the quality and epidemiological relevance of the resulting phylogeny.
Table 2: Key SNVPhyl Parameters for Optimizing hqSNV Detection
| Parameter | Default/Recommended Value | Impact on Analysis |
|---|---|---|
min_coverage [42] [43] |
10-15× | Lower values may include false positives; higher values may exclude valid variants in low-coverage regions. |
min_mean_mapping [42] |
30 | Ensures only reads mapping with high confidence to unique genomic regions are considered. |
relative_snv_abundance(also snv_abundance_ratio, alternative_allele_proportion) [42] [43] |
0.75 | Critical for mixed infections; requires 75% of reads to support variant, reducing false positives. |
min_percent_coverage [44] |
Varies (e.g., 90) | Minimum percentage of reference genome that must meet min_coverage for sample inclusion. |
| Density Threshold & Window Size [44] | Varies (e.g., 5 SNVs in 100bp window) | Identifies/rejects hyper-variable regions indicative of recombination or horizontal gene transfer. |
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Common Error Messages and Resolutions
Error: "No valid phylip alignment" / SNV Alignment file is empty [42]
- Explanation: This indicates no valid SNVs passed all filtering criteria. The most common cause is that one or more samples failed mapping or coverage requirements.
- Solution:
- Check the
filterStats.txtoutput file to see how many SNVs were filtered at each stage. - Examine the
mappingQuality.txtfile to verify all samples met the minimum coverage and percent coverage thresholds. A sample with very low coverage or poor mapping will cause positions to be filtered out as "filtered-coverage" [41]. - Ensure the reference genome is appropriately related to your samples. A distantly related reference will yield too few mapped reads for reliable variant calling.
- Check the
Error: "Tool [...] missing" in Galaxy [45]
- Explanation: The Galaxy instance is missing a specific tool or tool version required by the SNVPhyl workflow.
- Solution:
- A system administrator must log into Galaxy and install the missing tool from the Galaxy ToolShed.
- Ensure the tool version specified in the error message matches the version required by the SNVPhyl workflow.
Error: "Timeout while uploading" to Galaxy [45]
- Explanation: File transfer from the analysis client (e.g., IRIDA) to the Galaxy instance took longer than the configured time limit.
- Solution: A system administrator must increase the timeout limit (e.g.,
galaxy.library.upload.timeoutin the configuration file) and restart the service.
Interpretation of Output Files
How do I interpret the different statuses in the
snvTable.tsvfile? [41] The status column indicates why a particular genomic position was included or excluded from the final phylogeny.valid: Position passed all filters and was used to build the tree.filtered-invalid: Position was in a repeat region, high-SNV density region, or a user-defined invalid position.filtered-coverage: Position had insufficient coverage in at least one sample (marked as-in the table).filtered-mpileup: A variant call mismatch occurred between FreeBayes and SAMtools (marked asNin the table). This often relates to parameters like mapping quality orrelative_snv_abundance.
What does the
vcf2core.tsvfile tell me about my analysis? [41] This file provides a summary of the "core genome" used for phylogenetic analysis. Key columns include:- Total valid and included positions in core genome: The number of genomic positions that were evaluable across all samples.
- Percentage of valid and included positions in core genome: The percentage of the reference genome that is included in the core. A low percentage may indicate a poor choice of reference genome or significant contamination in some samples.
Experimental Design and Best Practices
How do I choose an appropriate reference genome? Select a closed, high-quality genome that is phylogenetically close to your isolates. Using an inappropriate reference (e.g., from a different serotype or lineage) can lead to poor mapping and sparse SNV data. The reference can be the type strain for the species or a high-quality assembly from a previous outbreak.
Should I mask parts of the genome, and why? Yes, masking is a recommended best practice. Mobile genetic elements like phages, plasmids, and genomic islands are often subject to horizontal gene transfer, which does not reflect the vertical evolutionary history of the core genome. Including these regions can introduce homoplasy and distort the phylogenetic tree. You can identify phage regions using tools like PHASTER and provide their coordinates in an
invalid_positions.bedfile [42] [43]. SNVPhyl also has a built-in step to find and mask repetitive regions.What is a sufficient SNV threshold to define an outbreak cluster? There is no universal threshold, as SNV accumulation rates vary by organism and evolutionary time scale. A study on Clostridium difficile used a threshold of 0-2 SNVs to define recent transmission [1]. Thresholds must be established for each organism based on known evolutionary rates and the timeframe of the investigation. SNVPhyl provides the high-quality data necessary to make these distinctions.
Multilevel Genome Typing (MGT) is an advanced genomic framework designed to provide a universal and stable nomenclature for bacterial pathogen typing at multiple resolutions [46]. It addresses a critical need in public health microbiology by enabling both long-term tracking of bacterial clones and short-term, high-resolution outbreak detection within a single, standardized system [46] [47]. Traditional typing methods often operate at a fixed resolution—for example, classic seven-gene Multilocus Sequence Typing (MLST) for broad population studies or core genome MLST (cgMLST) for outbreak investigations. MGT innovatively bridges this gap by employing a series of consecutive MLST schemes of increasing sizes, from a few genes up to the entire core genome [46]. This allows researchers to examine genetic relatedness with a scalable level of detail, making it a powerful tool for improving the discriminatory power in genomic subtyping methods research [48].
Frequently Asked Questions (FAQs)
1. What is the core principle behind MGT? MGT operates on the principle of using multiple, methodologically connected MLST schemes, called "levels" [46]. Each level uses a different number of genetic loci, providing a gradient of resolutions. Lower levels (with fewer loci) are suitable for long-term, global epidemiology, while higher levels (with more loci) offer the fine-scale resolution needed for detecting recent transmission chains and outbreaks [46] [47].
2. How does MGT improve upon existing methods like cgMLST or SNP-based phylogenetics? While cgMLST provides high resolution, it lacks flexibility for broader epidemiological questions and often requires setting arbitrary allele thresholds for clustering, which can lack stability [47]. SNP-based methods, though highly discriminatory, can suffer from issues of stability and founder effects when new data is added [46]. MGT provides a stable, standardized nomenclature at each level without relying on variable thresholds. It integrates the stability of traditional MLST with the high resolution of WGS, creating a unified system for all epidemiological time scales [46] [47].
3. For which pathogens has MGT been successfully developed? The MGT framework has been successfully applied to several key bacterial pathogens. It was first established for Salmonella enterica serovar Typhimurium, featuring a nine-level scheme [46] [48]. More recently, an eight-level MGT scheme was developed for Staphylococcus aureus and used to analyze over 50,000 genomes, demonstrating its utility in tracking globally disseminated clones like ST8-USA300 and local hospital transmissions [47].
4. What is a "Genome Type" (GT)? A Genome Type is the unique identifier for a strain within the MGT system. It is a string of Sequence Types (STs), each derived from a different MGT level, concatenated and separated by hyphens (e.g., GT 19-2-11-27-115-274-365-435-501) [46]. This provides a precise and communicable definition of a strain's identity across multiple resolutions.
5. My research involves a pathogen without an established MGT scheme. Can I develop one? Yes. The methodology suggests that MGT can form the basis for typing systems in other microorganisms beyond those for which it has already been established [46]. Development involves defining a series of MLST schemes based on the genetic diversity and evolutionary rate of the target pathogen, typically starting with the classic MLST as the first level and culminating in a cgMLST scheme at the highest level [46] [47].
Troubleshooting Common MGT Workflow Challenges
Problem 1: Inadequate Discriminatory Power at Lower MGT Levels
Symptoms: Inability to distinguish between known, distinct lineages when using lower MGT levels (e.g., MGT1-MGT4). Root Causes:
- The genetic diversity among the isolates in question is too recent to be captured by the smaller number of loci in lower levels.
- The isolates are genuinely closely related, belonging to the same broad clone. Solutions:
- Proceed to Higher MGT Levels: The MGT framework is designed for this scenario. Move your analysis to MGT5 or higher, which incorporate more loci and provide greater resolution [46].
- Confirm with cgMLST: Use the highest MGT level (e.g., MGT8 or MGT9, which represents the cgMLST) to validate the true relatedness of the isolates [46].
- Context is Key: Lower levels are ideal for long-term epidemiology. If your question involves recent outbreak detection, higher levels should be your default [47].
Problem 2: Data Quality and Assembly Issues Affecting ST Calling
Symptoms: A high number of loci are reported as "missing" or "problematic" during the allele calling process, leading to an incomplete GT. Root Causes:
- Poor quality of raw sequencing reads (e.g., contamination, low coverage) [47].
- Inefficient DNA fragmentation or adapter ligation during library preparation [12].
- Assembly errors due to problematic genomic regions (e.g., high GC content, repeats) [47]. Solutions:
- Pre-process Reads Rigorously: Implement robust read trimming and quality control steps. One study used Kraken to screen for contamination, removing samples with >20% non-target reads [47].
- Optimize Library Prep: Ensure accurate quantification of input DNA using fluorometric methods (e.g., Qubit) over UV absorbance to prevent enzyme inhibition from contaminants. Titrate adapter-to-insert ratios to avoid adapter dimer formation [12].
- Use a Standardized Pipeline: Employ a dedicated MGT pipeline (e.g., MGTdb) that includes reference-based assembly with tools like Shovill and SKESA, followed by quality filtering based on metrics like N50 and total assembly size [47].
Problem 3: Interpreting and Communicating Complex MGT Results
Symptoms: Difficulty in conveying the relationships between multiple GTs or describing a cluster of related but non-identical isolates. Root Causes:
- The full GT is too long for concise communication when the highest resolution is not needed.
- A cluster of isolates shares STs at lower levels but differs at higher levels. Solutions:
- Use Partial GTs: You can use a truncated GT to describe a broader group. For example,
GT 19-2-11-27-115-274-X-X-Xcan be shortened toGT 19-2-11-27-115-274to represent all isolates sharing that profile, regardless of the higher-level types [46]. - Use Degenerate GTs: To communicate related GTs, employ a degenerate format. For example,
GT 19-2-11-(27/32)-115-274-365-435-501indicates two sub-lineages that differ only at the MGT4 level [46]. - Reference Specific Levels: Describe a clone by its ST at a specific MGT level (e.g., "MGT4 ST27"), similar to traditional MLST [46].
Experimental Protocol: Implementing an MGT Analysis
The following workflow details the steps for applying an established MGT scheme to a set of bacterial whole-genome sequences, based on the methodologies used in published studies [46] [47].
Workflow Diagram
Step-by-Step Protocol
1. Sample Preparation and Sequencing
- Principle: Generate high-quality whole-genome sequencing data, typically using Illumina short-read platforms [47].
- Procedure:
- Extract genomic DNA from pure bacterial cultures.
- Prepare a sequencing library, ensuring careful fragmentation and adapter ligation. Avoid over-amplification to prevent biases [12].
- Sequence the library on an appropriate Illumina platform (e.g., MiSeq, NextSeq) to achieve sufficient coverage (>50x is typical).
2. Bioinformatic Processing and Quality Control (QC)
- Principle: Ensure that only high-quality genomic data proceeds to typing to prevent erroneous ST calls [47].
- Procedure:
- Trim Raw Reads: Use tools like Trimmomatic to remove adapter sequences and low-quality bases [47].
- Screen for Contamination: Classify reads with a tool like Kraken. Discard samples where more than 20% of reads are classified as non-target organisms [47].
- Assemble Genomes: Perform reference-based assembly using pipelines like Shovill (which utilizes SKESA) [47].
- Quality Filter Assemblies: Calculate assembly metrics (e.g., total length, N50, number of contigs) with Quast. Filter out assemblies that do not meet predefined thresholds for size and contiguity [47].
3. MGT Allele Calling and Genome Type Assignment
- Principle: For each quality-filtered genome, determine the allele numbers for every locus in each MGT level [46].
- Procedure:
- Use the species-specific MGT database and analysis platform (e.g., https://mgtdb.unsw.edu.au/).
- Upload assembled genomes to the platform or run the MGT software locally.
- The tool will map the assembled sequences against the defined loci for each MGT level.
- For each level, the combination of allele numbers defines the Sequence Type (ST) at that level.
- The final output is the Genome Type (GT), a concatenation of all STs from MGT1 to the highest level.
4. Data Interpretation and Epidemiological Analysis
- Principle: Use the hierarchical GT information to answer specific epidemiological questions [46] [47].
- Procedure:
- Long-term/Global Analysis: Use lower MGT levels (e.g., MGT1-MGT3) to identify major lineages and their geographic distribution over decades.
- Outbreak Detection: Use higher MGT levels (e.g., MGT7-MGT9) to cluster isolates from a suspected outbreak and distinguish them from background cases.
- Communication: Report findings using standardized GT nomenclature, employing partial or degenerate GTs as needed for clarity [46].
The table below summarizes the MGT scheme for Salmonella enterica serovar Typhimurium, demonstrating how the number of loci and resolution increase with each level [46].
| MGT Level | Number of Loci | Total Sequence Length | Proportion of Reference Genome (%) | Average Isolates per ST | Utility and Resolution |
|---|---|---|---|---|---|
| MGT1 | 7 | 3.3 kb | 0.07% | 115 | Classical 7-gene MLST; identifies major, long-lived clones [46]. |
| MGT2 | 18 | 10.8 kb | 0.22% | 37.4 | Broad population structure; ~1 new allele per 100 years [46]. |
| MGT3 | 77 | 53.2 kb | 1.10% | 8.3 | Intermediate resolution for tracking clones over years to decades [46]. |
| MGT4 | 156 | 105.6 kb | 2.17% | 4.6 | Higher resolution for regional epidemiology [46]. |
| MGT5 | 241 | 210.4 kb | 4.33% | 2.9 | Distinguishes closely related lineages [46]. |
| MGT6 | 682 | 525.8 kb | 10.82% | 1.9 | Suitable for short-term epidemiology (~1-2 years) [46]. |
| MGT7 | 1,044 | 1.05 Mb | 21.67% | 1.5 | High resolution for outbreak investigation [46]. |
| MGT8 | 2,956 | 2.79 Mb | 57.40% | 1.2 | Species core genome MLST (cgMLST); very high resolution [46]. |
| MGT9 | 5,293 | 4.01 Mb | 82.62% | 1.2 | Serovar/core genome & intergenic cgMLST; highest resolution for outbreak detection [46]. |
The following table lists key reagents, software, and data resources essential for conducting MGT analysis.
| Item | Category | Function / Application |
|---|---|---|
| Illumina DNA Prep Kit | Wet-lab Reagent | For preparing high-quality sequencing libraries from bacterial genomic DNA [47]. |
| Qubit Fluorometer | Laboratory Instrument | Accurate quantification of DNA concentration for library preparation, superior to UV absorbance for this purpose [12]. |
| Trimmomatic | Bioinformatics Tool | Removes adapter sequences and trims low-quality bases from raw sequencing reads [47]. |
| Kraken | Bioinformatics Tool | Fast taxonomic classification of sequencing reads to screen for sample contamination [47]. |
| Shovill Pipeline | Bioinformatics Tool | Rapid and efficient pipeline for bacterial genome assembly, often using SKESA [47]. |
| QUAST | Bioinformatics Tool | Quality Assessment Tool for evaluating genome assemblies against quality thresholds [47]. |
| Species-Specific MGT Database | Data Resource | Web-accessible database (e.g., MGTdb) for assigning STs and GTs and for comparing isolates globally [47]. |
MGT Resolution Hierarchy and Application
This diagram illustrates the conceptual relationship between MGT levels, resolution, and their primary applications in epidemiology.
FAQs: Core Concepts and Experimental Design
FAQ 1: What is the primary advantage of multi-omics subtyping over traditional single-omics approaches?
Multi-omics subtyping provides a holistic view of cancer biology by integrating data from various molecular layers, such as the genome, transcriptome, proteome, and epigenome. This approach addresses the significant limitation of single-omics studies, which often ignore molecular heterogeneity at other (epi-)genetic levels of gene regulation [49]. By capturing these dynamic, multi-layered interactions, multi-omics integration identifies biologically coherent subgroups with greater clinical relevance. For instance, in ovarian cancer, multi-omics subtyping has identified subtypes with significant associations to overall survival, whereas taxonomies based on single-omics data did not [49].
FAQ 2: How can machine learning (ML) improve multi-omics data integration and subtyping?
Machine learning algorithms are powerful tools for handling the high-dimensionality and complexity of multi-omics datasets. They can capture non-linear relationships and identify subtle patterns often missed by traditional statistics [50]. Specific applications include:
- High-Dimensional Data Handling: ML models, particularly with GPU acceleration, can manage the data-intensive nature of omics-driven computations [51].
- Prognostic Model Development: Algorithms like
plsRcoxcan integrate diverse data types to create robust prognostic scores (e.g., MCMLS) that predict patient survival and immunotherapy response more effectively than models based on clinical factors alone [50]. - Dimensionality Reduction and Fusion: Techniques like sparse Canonical Correlation Analysis (SCCA) project different omics data types onto a unified space, facilitating effective data fusion for subsequent clustering analysis [49].
FAQ 3: What are the common computational challenges in multi-omics integration, and how can they be addressed?
Researchers often face several hurdles, which can be mitigated through specific strategies:
- Data Harmonization: Disparate data types, scales, and dimensionality complicate integration. Using advanced statistical, network-based, and ML methods like MOVICS can model these interdependencies [52] [50].
- Interpretability: Complex ML models can be "black boxes." Employing network-based approaches that incorporate prior biological knowledge can enhance interpretability and predictive power [52].
- Generalization Gap: Models trained on one cohort may not perform well on others. Employing cross-validation and testing on independent, multi-site datasets is crucial for ensuring generalizability [51] [53].
Troubleshooting Guides
Issue 1: Suboptimal Clustering Results from Multi-Omics Data
Problem: The identified cancer subtypes lack biological coherence, clinical relevance, or are not reproducible.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Poor Feature Selection | Check if features with low variance or no prognostic value dominate the analysis. | Apply rigorous feature selection. For example, select top features based on Median Absolute Deviation (MAD) and filter using Cox regression with appropriate p-value cutoffs (e.g., 0.01 for mRNA) [50]. |
| Incorrect Cluster Number | The chosen number of clusters (k) does not reflect the true underlying data structure. | Perform cluster prediction analysis (e.g., using silhouette analysis) to determine the optimal k within a reasonable range (e.g., 2-8) [50]. |
| Failure to Integrate Genetic Data | Subtypes are derived solely from phenotypic data (e.g., imaging), limiting biological interpretability. | Use methods like Gene-SGAN that jointly model phenotypic and genetic data to confer genetic correlations to the derived disease subtypes [53]. |
| Algorithm Limitations | The clustering method is not capturing complex relationships between omics layers. | Employ or compare multiple clustering algorithms (e.g., via the MOVICS package) or use methods specifically designed for integration, such as SCCA-CC or iCluster [50] [49]. |
Issue 2: Poor Performance of a Multi-Omics Prognostic Classifier
Problem: A developed prognostic model (e.g., MCMLS) shows high accuracy on training data but fails to predict outcomes in validation cohorts.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Overfitting | The model is overly complex and has learned noise from the training data. | Implement regularization techniques (e.g., LASSO penalty in SCCA), use simpler models, and ensure the training dataset is large enough relative to the number of features [49]. |
| Batch Effects | Technical artifacts from different data processing batches confound the biological signal. | Use the sva package or similar tools to remove batch effects before merging datasets from different sources (e.g., TCGA and GEO) [50]. |
| Inadequate Validation | The model was not rigorously tested on independent, external datasets. | Validate the model on multiple, independent cohorts from repositories like GEO. Use methods like Nearest Template Prediction (NTP) to assign subtype labels in new datasets [50]. |
Experimental Protocols for Key Methodologies
Protocol 1: Multi-Omics Integrative Clustering using MOVICS
This protocol outlines the process for identifying cancer subtypes from multiple omics data types using the MOVICS R package [50].
1. Data Acquisition and Preprocessing
- Obtain multi-omics data (e.g., mRNA, lncRNA, miRNA, DNA methylation, mutation) from databases like TCGA.
- Ensure all data types are available for the same patient set and have linked clinical survival information.
- Critical Step: For DNA methylation data, convert beta values to M-values for improved statistical performance in downstream analyses.
2. Feature Selection
- Apply strict, data-type-specific criteria to select the most informative features:
- mRNA/lncRNA: Select top 3,000 features by Median Absolute Deviation (MAD), then filter via Cox regression (p < 0.01).
- miRNA: Select top 500 features by MAD, then filter via Cox regression (p < 0.001).
- DNA Methylation: Select top 3,000 features by MAD, then filter via Cox regression (p < 0.05).
- Mutation Data: Select genes mutated in >15% of the cohort.
- Microbiome Data: Select top 15 features by standard deviation.
3. Multi-Omics Clustering
- Determine the optimal number of clusters (k) using cluster prediction analysis (k=2 to 8).
- Run at least ten different clustering algorithms (e.g., COCA, NEMO, PINSPlus) implemented in MOVICS.
- Evaluate clustering quality using silhouette analysis.
- Critical Step: Perform consensus clustering to integrate results from the multiple algorithms and derive stable subtypes.
4. Subtype Validation and Characterization
- Validate the identified subtypes on independent datasets (e.g., from GEO) after removing batch effects.
- Use Nearest Template Prediction (NTP) to assign subtype labels in validation cohorts.
- Characterize subtypes by performing survival analysis (Kaplan-Meier curves with log-rank test) and analyzing their immune landscape (e.g., with CIBERSORT, ESTIMATE).
Protocol 2: Sparse CCA for Multi-Omics Classification (SCCA-CC)
This protocol describes using Sparse Canonical Correlation Analysis (SCCA) to fuse two types of omics data (e.g., mRNA and miRNA) for cancer subtyping and classification [49].
1. Data Input and Normalization
- Collect two matched omics datasets (e.g., mRNA and miRNA expression matrices) for the same set of patient samples.
- Ensure data matrices are properly normalized. SCCA-CC does not require non-negative matrices, unlike NMF.
2. Sparse Projection and Data Fusion
- Use the
PMAR package and itsCCAfunction with lasso penalty (parameterstypexandtypezset to "standard"). - Set the sparsity penalty parameters (e.g., default value of 0.3) to control the number of features used from each omics type.
- Project both omics datasets onto a unified, lower-dimensional space using SCCA. The number of canonical vectors (K) is determined by the lower dimension of the two input data types.
- Fuse the projected data matrices (
APandBP) into a single integrated matrix, for example, by weighted average.
3. Clustering and Classifier Training
- Perform unsupervised clustering (e.g., k-means, hierarchical clustering) on the fused data matrix to identify cancer subtypes.
- Train a classifier (e.g., SVM, random forest) using the fused data and the assigned subtype labels.
- Key Advantage: The trained projection matrices and classifier can be applied to classify new samples, even if only a single type of omics data is available.
Table 1: Performance Comparison of Multi-Omics Prognostic Models in Colorectal Cancer (CRC). This table summarizes the predictive performance of a novel ML model (MCMLS) against clinical factors [50].
| Prognostic Model / Factor | Cohort | Concordance Index (C-index) / Area Under Curve (AUC) | Notes |
|---|---|---|---|
| MCMLS (ML Model) | Training (TCGA) | C-index: Not Specified (Higher than alternatives) | Developed from multi-omics & microbiome data. |
| Validation (Meta-dataset) | C-index: Not Specified (Higher than alternatives) | Consistently outperformed existing signatures. | |
| Clinical Risk Factors | AUC < 0.7 | Includes tumor stage, T stage, N stage, M stage, and gender. | |
| Radiomics (CT) for Lymph Node Metastasis | Multicenter (N=730) | C-index: 0.797 (External Validation) | Outperformed conventional clinical N staging [51]. |
| CNN for Survival Prediction | GC Cohort (N=1061) | C-index: 0.849 | Based on CT images and clinical data [51]. |
Table 2: Deep Learning Performance in Gastric Cancer (GC) Image Analysis. This table compiles the accuracy of various deep learning models applied to endoscopic and CT images for GC diagnosis [51].
| Task | Imaging Modality | Model / Approach | Performance | Study Context |
|---|---|---|---|---|
| Early GC Detection | ME-NBI | CNN (Meta-analysis) | Sensitivity: 0.95, Specificity: 0.95 | Pooled from 15 studies [51]. |
| Early GC Detection | WLI | CNN (Meta-analysis) | Sensitivity: 0.80, Specificity: 0.95 | Pooled from 15 studies [51]. |
| Predict Invasion Depth | Endoscopy | CNN-CAD | AUC: 0.94 | Surpassed expert endoscopists' accuracy by 17.25% [51]. |
| Differentiate Mucosal/Submucosal GC | Endoscopy | CNN-based Network | Accuracy: 77% | - [51]. |
| Lesion Detection | Endoscopy | YOLO_v3 CNN | Detection Rate: 95.6% | Internal validation [51]. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools and Databases for Multi-Omics Subtyping.
| Item | Function / Application | Brief Explanation |
|---|---|---|
| MOVICS R Package | Multi-omics Clustering | An integrated pipeline for performing multi-omics clustering and visualization using multiple algorithms [50]. |
| TCGA (The Cancer Genome Atlas) | Data Source | A public repository containing multi-dimensional maps of key genomic changes in over 30 types of cancer, essential for training and discovery [54] [50]. |
| GEO (Gene Expression Omnibus) | Data Source / Validation | A public functional genomics data repository, crucial for obtaining independent datasets to validate derived subtypes [50] [49]. |
| CIBERSORT / ESTIMATE | Immune Microenvironment Analysis | Computational algorithms for characterizing immune cell composition from tumor transcriptome data, vital for subtype characterization [50]. |
| SCCA (Sparse CCA) | Data Fusion and Dimensionality Reduction | A statistical method for projecting two types of high-dimensional omics data onto a unified, lower-dimensional space for integration [49]. |
| UNCSeq Custom Capture | Targeted Sequencing | A custom bait set (Agilent SureSelect) encompassing ~1200 genes commonly altered in cancer, used for focused genomic studies [54]. |
Navigating Technical Challenges: Strategies to Overcome Limits in Subtyping Resolution
Frequently Asked Questions (FAQs)
Q1: Why is filtering for Mobile Genetic Elements (MGEs) like plasmids and prophages important in genomic subtyping?
MGEs are independent, highly transferable genetic units that can be shared between unrelated bacterial strains. If not filtered out, their sequences can obscure the true evolutionary relationship between isolates, making distinct lineages appear closely related and vice versa. This confounds outbreak detection and source attribution. One study on Shigella surveillance found that MGEs were a primary confounding factor in long-term outbreak analysis, complicating the interpretation of standard subtyping methods [55].
Q2: What is the key difference in the analysis workflow when MGEs are filtered?
The core principle is to separate the analysis of the core genome (chromosomal, vertically inherited) from the accessory genome (including MGEs). Subtyping based solely on the core genome provides a clearer picture of evolutionary lineage, while MGE analysis can reveal independent acquisition of traits like virulence or antibiotic resistance. As one review notes, methods like core genome MLST (cgMLST) that focus on stable chromosomal genes are central to this approach for outbreak investigations [56].
Q3: Which bioinformatics tools are essential for identifying prophages and plasmids?
A robust toolkit is necessary for comprehensive MGE identification. The table below summarizes key research reagents and their functions.
Table 1: Essential Research Reagents and Tools for MGE Filtering
| Tool Name | Function | Brief Description & Utility |
|---|---|---|
| VirSorter2 [57] | Prophage Prediction | Identifies prophage sequences within bacterial genomes and plasmids; used in prophage discovery studies with configurable score thresholds. |
| PHASTER [58] | Prophage Analysis | A user-friendly web server for rapid identification and annotation of prophage sequences; useful for quick analysis and visualization. |
| MOB-suite [59] | Plasmid Typing & Mobility | Predicts plasmid mobility (conjugative, mobilizable, non-mobilizable) and assigns them to clusters and subclusters based on sequence similarity. |
| PlasmidScope [59] | Plasmid Database & Analysis | A comprehensive database of plasmids with rich annotations, supporting online analysis and interactive visualization of custom sequences. |
| cgMLST Schemes [56] | Core Genome Subtyping | Species-specific schemes of hundreds to thousands of core genes used for high-resolution phylogenetic analysis after MGE filtration. |
Q4: What quantitative impact does MGE filtering have on genomic studies?
Large-scale genomic studies demonstrate the significant contribution of MGEs to the total gene pool and their role in horizontal gene transfer. The following table summarizes quantitative findings from a prophage study in the porcine gut, illustrating their abundance and functional impact.
Table 2: Quantitative Data on Prophages from a Porcine Gut Microbiota Study [57]
| Metric | Value | Context / Implication |
|---|---|---|
| Prophages Identified | 10,742 | From 7,524 high-quality prokaryotic genomes. |
| Prophage Prevalence | - | Distribution was heterogeneous across host species. |
| Broad Host Range | 1.70% (183/10,742) | Prophages with potential for inter-species infectivity. |
| Prophages with Host Defense Genes | 5.07% (545/10,742) | Prophages enhancing the host's adaptive immune capabilities (e.g., CRISPR-Cas). |
| Common Prophage Genes | Integrases, tail tube proteins | Identified as critical determinants of phage host specificity. |
Troubleshooting Guides
Issue 1: Inconsistent Subtyping Results in an Outbreak Investigation
Problem: Your whole-genome sequencing (WGS) data of bacterial isolates from a suspected outbreak is giving conflicting results. Some clustering methods show a tight outbreak cluster, while others suggest high genetic diversity.
Diagnosis: This is a classic symptom of MGE-generated "noise." The presence or absence of highly mobile plasmids and prophages in different isolates is distorting the phylogenetic signal [55].
Solution: Implement a core genome-based subtyping workflow to filter out MGEs.
Step 1: Identify and Mask Prophages.
- Protocol: Use VirSorter2 [57] to scan your assembled genomes.
- Command example:
- Interpretation: Regions identified as prophage (categories 1-4 for lysogenic phages) should be masked or removed from the genome file before subtyping.
Step 2: Identify and Mask Plasmids.
- Protocol: Use MOB-suite [59] to reconstruct and classify contigs from your assembly.
- Command example:
- Interpretation: All contigs identified as plasmid-derived should be separated from the chromosomal contigs.
Step 3: Perform Core Genome Analysis.
- Protocol: Use a species-specific cgMLST scheme [56] on the filtered, chromosomal genomes.
- Workflow: Upload your MGE-filtered genomes to a platform like Enterobase or Ridom SeqSphere+ that supports cgMLST. The allele calling will be performed against a defined set of core genes.
- Expected Outcome: Isolates truly part of the outbreak will form a tight cluster with a low number of allele differences (e.g., 0-10), while unrelated isolates will be clearly separated, providing a reliable result for surveillance.
The following diagram illustrates this core workflow for de-noising genomic data.
Issue 2: Differentiating Between Vertical Inheritance and Horizontal Transfer of a Virulence Gene
Problem: You have identified a key virulence factor (e.g., a toxin gene) in your bacterial pathogen but cannot determine if it is chromosomally inherited (stable) or located on a plasmid/prophage (mobile and a higher risk for spread).
Diagnosis: The genomic context of the gene has not been established. A gene on an MGE indicates potential for horizontal transfer and may be a recent acquisition unrelated to the core phylogeny [60].
Solution: Conduct a local genomic context analysis to pinpoint the gene's location.
Step 1: Annotate the Genomes.
- Use an annotation tool like Prokka [59] to identify all open reading frames (ORFs) and their functions in your assembled genomes.
Step 2: Map the Gene of Interest.
- Protocol: Use BLAST to find the exact contig and position of your virulence gene within each genome.
Step 3: Characterize the Flanking Region.
- Protocol: Check if the contig containing the gene was identified as a plasmid by MOB-suite [59].
- Protocol: Check if the flanking genes are typical MGE markers (e.g., integrases, transposases, plasmid replication genes). The presence of these is a strong indicator of an MGE.
- Protocol: Use PHASTER [58] to see if the region is part of a prophage. The tool will provide a visual annotation of the prophage region, including its attachment sites.
Step 4: Correlate with Phylogeny.
- Protocol: Build a core genome phylogeny (see Issue 1). Then, overlay the presence/absence pattern of the virulence gene.
- Expected Outcome: If the gene is on a plasmid or prophage, its distribution will not match the core phylogeny—it will appear in distantly related strains, confirming horizontal acquisition.
The logical process for this analysis is outlined below.
Addressing Homoplasy and Convergent Evolution in Microbial Genomes
Frequently Asked Questions
What is homoplasy and why is it important in microbial genomics? Homoplasy occurs when the same genetic trait is present in two or more lineages but was not inherited from their common ancestor. Instead, it arises through independent evolutionary events such as convergent evolution, parallel evolution, or evolutionary reversals [61] [62]. In microbial genomes, homoplasic SNPs are considered important signatures of strong positive selective pressure, potentially indicating adaptive evolution for clinically relevant traits like antibiotic resistance and virulence [61]. This makes homoplasy detection crucial for understanding pathogen adaptation.
How does homoplasy affect phylogenetic analysis and discriminatory power? Homoplasies can obscure the true evolutionary history of sequences by suggesting greater genetic similarity than actually exists [63]. When present in large numbers, they can obscure true phylogenetic relationships, potentially reducing the accuracy of phylogenetic trees and the discriminatory power of subtyping methods [63]. However, when properly identified, homoplasic sites provide valuable signals of adaptive evolution in response to selective pressures [61].
What are the main types of homoplasy? Homoplasic SNPs arise through different series of mutation events [61]:
- Parallel homoplasic SNPs: The same substitution occurs independently at the same site in multiple diverged lineages
- Convergent homoplasic SNPs: The same nucleotide arises in diverged lineages through distinct series of substitution events
- Revertant homoplasic SNPs: A derived nucleotide mutates back to the ancestral nucleotide
What tools are available for homoplasy detection? Several specialized tools have been developed for homoplasy detection in genomic datasets [61] [63]:
- SNPPar: Uses ancestral state reconstruction to assign mutation events to branches and identify homoplasies
- HomoplasyFinder: Uses consistency index to identify sites inconsistent with the phylogeny
- TreeTime: Provides ancestral state reconstruction and homoplasy identification functions
Troubleshooting Guides
Issue: Poor Discrimination Between Known Epidemiologically Unrelated Strains
Problem: Your phylogenetic analysis fails to distinguish between strains that are known to be epidemiologically unrelated based on clinical or field data.
Solution:
- Verify data quality: Ensure your genome assemblies meet quality standards and contamination has been properly addressed [64]
- Increase resolution: Shift from traditional 7-gene MLST to core genome MLST (cgMLST) or whole genome MLST (wgMLST) schemes [56]
- Check for excessive homoplasy: Use HomoplasyFinder to identify homoplasic sites that might be obscuring true relationships [63]
- Consider alternative phylogenetic methods: If using maximum parsimony, try model-based methods that might be less sensitive to homoplasy
Prevention: Implement standardized quality control protocols for sequencing data and validate the discriminatory power of your typing method for your specific bacterial species [56].
Issue: Unexpected Homoplasy Patterns in Analysis
Problem: Homoplasy detection tools identify an unusually high number of homoplasic sites, potentially indicating problems with data quality or phylogenetic reconstruction.
Solution:
- Verify phylogenetic tree quality: Ensure the input tree is well-resolved and properly rooted [63]
- Check for recombination: In species with high recombination rates, remove recombined regions before analysis as they can create homoplasies [61]
- Validate with simulated data: Test your analysis pipeline with simulated datasets containing known homoplasies to verify performance [61] [63]
- Examine specific homoplasic sites: Use tools like SNPPar to annotate mutations and determine if they cluster in specific genes or genomic regions [61]
Prevention: Establish negative controls in your sequencing workflow and implement routine monitoring of sequencing error rates.
Issue: Computational Limitations with Large Datasets
Problem: Homoplasy analysis becomes computationally intractable with datasets of thousands of genomes.
Solution:
- Use optimized tools: SNPPar has been specifically designed for large datasets (>1000 isolates and/or >100,000 SNPs) and uses efficient algorithms to minimize computational requirements [61]
- Implement filtering strategies: Reduce the dataset to variable sites only before analysis
- Leverage ancestral state reconstruction efficiently: SNPPar requires ASR for only a small percentage of SNPs (approximately 1.25% in testing), significantly reducing computation time [61]
- Optimize workflow: For initial screening, use faster methods like consistency index calculation before applying more computationally intensive ASR approaches
Performance Benchmark: In testing, SNPPar analyzed ~64,000 genome-wide SNPs from 2000 Mycobacterium tuberculosis genomes in approximately 23 minutes using ~2.6 GB of RAM on a laptop [61].
Homoplasy Detection Tool Comparison
Table: Comparison of Homoplasy Detection Tools and Methods
| Tool/Method | Key Features | Data Requirements | Performance | Output Information |
|---|---|---|---|---|
| SNPPar [61] | - Uses ancestral state reconstruction (ASR)- Annotates mutations at codon/gene level- Differentiates homoplasy types | SNP alignment, tree, and annotated reference genome | ~23 min for 2000 genomesHigh specificity (zero false-positives) | Homoplasic SNPs, mutation branches, convergence at codon/gene level |
| HomoplasyFinder [63] | - Calculates consistency index- Java-based with R package available- Multiple access methods (R, CLI, GUI) | Newick tree and FASTA alignment | Fast processing on standard computers | Inconsistent sites, annotated tree, alignment without inconsistent sites |
| TreeTime [61] | - Ancestral state reconstruction- Homoplasy identification function- Molecular dating capabilities | Tree and alignment | Approximately linear time increase with sample size | Homoplasic sites, mutation placement on tree |
| cgMLST/wgMLST [56] | - Gene-by-gene approach- Uses hundreds to thousands of loci- Scheme-dependent | Genome assemblies and appropriate scheme | Varies by scheme and implementation | Allele profiles, genetic distances, phylogenetic trees |
Experimental Protocols
Protocol 1: Homoplasy Detection Using SNPPar
Purpose: To efficiently detect and analyze homoplasic SNPs from large whole genome sequencing datasets, including identification of convergent evolution at codon and gene levels.
Input Requirements:
- SNP alignment in accepted format
- Phylogenetic tree corresponding to alignment
- Annotated reference genome
Procedure:
- Prepare input files: Generate SNP alignment from WGS data, reconstruct phylogenetic tree using preferred method (e.g., RAxML-NG, IQ-TREE), and obtain properly annotated reference genome
- Run SNPPar analysis: Execute with appropriate parameters for your dataset
- Interpret results: Examine output files for:
- Homoplasic SNPs with their locations
- Assignment of mutation events to specific tree branches
- Classification of homoplasy type (parallel, convergent, revertant)
- Annotation of convergent evolution at codon and gene levels
Validation: Test with simulated datasets to verify sensitivity and specificity. In validation studies, SNPPar demonstrated zero false-positives in all tests and zero false-negatives in 89% of tests [61].
Protocol 2: Homoplasy Screening with HomoplasyFinder
Purpose: To automatically identify homoplasies present in phylogenetic data using consistency index calculations.
Input Requirements:
- Newick formatted phylogenetic tree (must be rooted)
- FASTA formatted multiple sequence alignment
Procedure:
- Install HomoplasyFinder: Available as Java application or R package
- Provide input data: Ensure tree and alignment correspond properly
- Execute analysis: Run with default or customized parameters
- Review outputs:
- Report of inconsistent sites (consistency index <1)
- Annotated Newick tree
- Alignment with inconsistent sites removed (optional)
Algorithm Details: The tool uses an algorithm adapted from Swofford et al. that calculates the minimum number of state changes required on a phylogenetic tree to explain the characters observed at the tips [63]. The consistency index is then calculated by dividing this minimum number by the number of different nucleotides observed at that site minus one.
Workflow Visualization
Homoplasy Detection and Analysis Workflow
Research Reagent Solutions
Table: Essential Resources for Homoplasy Analysis
| Resource Type | Specific Examples | Function/Purpose |
|---|---|---|
| Bioinformatics Tools | SNPPar, HomoplasyFinder, TreeTime, ClonalFrameML | Detect and analyze homoplasies using different algorithms and approaches |
| Reference Databases | NCBI GenBank, European Nucleotide Archive (ENA), PubMLST | Provide reference genomes and curated schemes for analysis |
| Computational Resources | High-performance computing clusters, adequate RAM (>8GB recommended for large datasets) | Handle computationally intensive phylogenetic and homoplasy analyses |
| Quality Control Tools | FastQC, CheckM, Kraken | Verify sequence quality, assembly completeness, and contamination status |
| Phylogenetic Software | RAxML-NG, IQ-TREE, BEAST2 | Reconstruct accurate phylogenetic trees essential for homoplasy detection |
Benchmarking and calibration are critical for validating and refining genomic subtyping methods, ensuring they provide biologically meaningful and reproducible categorizations of disease. This process involves the systematic comparison of computational tools against benchmark datasets and known biological truths to establish species-specific or context-specific interpretation guidelines. For genomic subtyping, this is essential for improving discriminatory power—the ability of a method to correctly distinguish between distinct molecular subtypes.
Frequently Asked Questions
Q1: What are the primary challenges when benchmarking cancer subtyping methods? Current disease subtyping approaches face several key challenges [20]:
- Over-reliance on Magnitude-Based Metrics: Many methods use metrics like Euclidean distance and neglect directional differences between feature vectors, which can capture more discriminative patterns.
- Lack of Algorithmic Integration: Each clustering algorithm has unique strengths and weaknesses. Failing to combine them means missing opportunities to identify both global and local patterns in the data.
- Inadequate Use of Pathway Information: Many methods overlook crucial pathway information (e.g., from KEGG, Reactome) that can reveal functional similarities between different genetic alterations.
- Handling of Missing Data: Most tools require perfectly matched samples across all omics types, leading to substantial data loss when some data modalities are unavailable.
Q2: How is performance typically quantified in subtyping method benchmarks? Performance is assessed using multiple metrics on datasets where some "ground truth" is known or inferred. A comprehensive benchmark of 13 subtyping methods across 43 cancer datasets with over 11,000 patients utilized the following criteria to evaluate the identified subtypes [20]:
- Clinical Relevance: Assessing significant differences in survival outcomes (e.g., log-rank test p-value) between the proposed subtypes.
- Biological Coherence: Analyzing the enrichment of known pathway signals, mutational signatures, and other molecular characteristics within the subtypes.
- Stability: Measuring the reproducibility of the results.
Q3: What is a key consideration for calibrating genetic interaction scores from CRISPR screens? When calibrating scores for synthetic lethality (SL) detection from combinatorial CRISPR screens, no single scoring method universally performs best. A comprehensive analysis of five scoring methods across five different datasets revealed that performance is dataset-dependent [65]. Therefore, it is a recommended calibration strategy to test multiple algorithms. For instance, one analysis identified that Gemini-Sensitive performed well across most datasets and is available as an R package, making it a reasonable first choice [65].
Q4: What are common sequence-related errors in genomic submissions and how are they resolved? Sequence validation often flags errors that require recalibration of analytical pipelines [66]:
- Internal Stop Codons: The presence of a stop codon within a predicted coding region often indicates errors in the nucleotide sequence or insufficient trimming of low-quality sequence ends. Resolution: Review and trim low-quality data from the sequences [66].
- Low-Complexity Sequences: Sequences with an unusual composition (e.g., "AAATAAAAAAAATAAAAAAT") can cause artefactual hits in similarity searches like BLAST. Resolution: Filter low-complexity sequences before analysis to prevent spurious alignments [67].
- PCR Primer Sequence Errors: Providing a primer sequence in the
primer-namefield, or including non-IUPAC nucleotides in theprimer-sequencefield, will trigger an error. Resolution: Ensure primer names are labels and primer sequences contain only valid IUPAC characters. Format inosines as<i>[66].
Experimental Protocols for Benchmarking
Protocol 1: Comprehensive Benchmarking of a Novel Subtyping Method
This protocol is based on the validation strategy for the DSCC (Disease subtyping using Spectral clustering and Community detection from Consensus networks) method [20].
- 1. Dataset Curation: Collect a large number of multi-omics datasets (e.g., 43 cancer datasets from TCGA). Include various data types: gene expression, miRNA, DNA methylation, copy number variation, somatic mutations, protein, and metabolite levels.
- 2. Data Pre-processing:
- Perform gene-level aggregation for mRNA, miRNA, DNA methylation, and protein data.
- Map features to genes using authoritative databases (e.g., miRTarBase for miRNA).
- Remove genes not associated with KEGG pathways to incorporate biological knowledge.
- For metabolomics, apply log2 transformation and replace missing values with zero.
- 3. Network Construction and Clustering:
- For each molecular data matrix, compute two patient affinity matrices: Euclidean and Angular.
- Combine affinity matrices into three consensus matrices: consensus Euclidean, consensus Angular, and consensus connectivity.
- Apply multiple clustering algorithms (e.g., spectral clustering and Louvain community detection) to the consensus networks to identify disease subtypes.
- 4. Performance Benchmarking:
- Compare the novel method against a panel of state-of-the-art approaches (e.g., SNF, NEMO, MOVICS, etc.).
- Evaluate subtypes based on clinical relevance (survival analysis), biological coherence (pathway enrichment), and stability.
- Incorporate subtype information as a covariate in prognostic models to test for improved survival prediction accuracy.
The following workflow diagram illustrates the key steps of the DSCC method:
Protocol 2: Benchmarking Genetic Interaction Scoring Methods
This protocol outlines the steps for evaluating methods that score synthetic lethality from combinatorial CRISPR screens [65].
- 1. Data Collection: Gather multiple combinatorial CRISPR screen datasets where two genes are perturbed simultaneously and the fitness impact is measured.
- 2. Method Application: Apply a set of different genetic interaction scoring methods (e.g., five different algorithms) to each dataset to infer synthetic lethality.
- 3. Benchmarking against a Gold Standard: Use a known set of true positive interactions to evaluate the methods. A common benchmark is a set of known synthetic lethal paralog pairs.
- Paralog-based Benchmark: Utilize pairs of paralog genes known to be synthetic lethal as a positive reference set.
- 4. Performance Evaluation: Assess each method's ability to recover the known positive interactions across the different screen datasets. Identify the top-performing methods that show consistent results.
Table 1: Summary of Subtyping Method Benchmarking Results This table summarizes the findings from a large-scale benchmark of subtyping methods across 43 cancer datasets. [20]
| Method Category | Example Methods | Key Strengths | Key Limitations |
|---|---|---|---|
| Consensus-Based | MOVICS, ClustOmics | Integrates multiple clustering algorithms | Often relies on specific omics with large sample sizes |
| Shared Representation | intNMF, iClusterPlus | Generates a shared representation across data types | Can struggle with very heterogeneous data |
| Similarity-Based | SNF, NEMO, DSCC | Combines patient similarity networks; some handle missing data | Network construction can be sensitive to parameters |
Table 2: Performance of Genetic Interaction Scoring Methods This table provides a generalized summary from a benchmark of five scoring methods for synthetic lethality detection. Performance is dataset-dependent, and no single method is universally best. [65]
| Scoring Method | Reported Performance | Availability / Notes |
|---|---|---|
| Gemini-Sensitive | Performed well across most datasets | Available as an R package; reasonable first choice |
| Other Methods (4) | Performance varied significantly by dataset | Highlights need for method calibration on specific data |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Genomic Subtyping & Benchmarking
| Item / Reagent | Function / Application |
|---|---|
| Combinatorial CRISPR Library | Enables simultaneous perturbation of two genes in a pool to screen for synthetic lethal genetic interactions [65]. |
| Multi-omics Datasets (TCGA, etc.) | Provide the foundational molecular data (genomics, transcriptomics, epigenomics, etc.) required for discovering and validating disease subtypes [20]. |
| KEGG Pathway Database | A crucial knowledge base used to map multi-omics features into biologically meaningful pathways during data pre-processing and result interpretation [20]. |
| miRTarBase | A curated database of miRNA-target interactions used to map miRNA expression data to target genes for gene-level aggregation in multi-omics analyses [20]. |
| Standalone BLAST Suite | Command-line tools for performing local or large-scale batch sequence similarity searches, which is essential for functional annotation and quality control [67]. |
| ClusteredNR Database | A clustered version of the NCBI nr protein database. Faster searches and easier-to-interpret results, as each cluster is represented by a single lead protein [67]. |
Troubleshooting Common Experimental Issues
Issue: Inconsistent or Biased Subtyping Results
- Potential Cause 1: The method is overly sensitive to a single data type or fails to integrate information effectively.
- Solution: Consider using an ensemble method like DSCC that leverages multiple distance metrics (Euclidean and Angular) and combines spectral clustering with community detection. This captures both global and local data structures for more robust subtypes [20].
- Potential Cause 2: Poor data quality or incorrect pre-processing.
- Solution: Rigorously pre-process data. Perform gene-level aggregation for consistency, map features to pathways, and handle missing values appropriately (e.g., log2 transformation and zero-imputation for metabolomics data) [20].
Issue: Poor Sequence Alignment Results or Validation Errors
- Potential Cause 1: Low-complexity sequences causing artefactual BLAST hits.
- Solution: Enable the low-complexity sequence filter (on by default in web BLAST) or use the
-segparameter for standalone BLASTp. This substitutes low-complexity regions to prevent spurious matches [67]. - Potential Cause 2: Sequences contain lowercase nucleotides or illegal characters.
- Solution: Convert all sequence characters to uppercase using a command like
tr 'acgt' 'ACGT' < input.fa > output.fnabefore importing into analysis pipelines [68]. - Potential Cause 3: Incorrectly formatted primer sequences in submission files.
- Solution: Ensure primer sequences are provided in the
fwd-primer-sequenceandrev-primer-sequencesource modifiers and contain only IUPAC nucleotides. Remove any extra text like "5'-" or "3'-" [66].
The following diagram outlines a logical workflow for troubleshooting benchmarked subtyping results, helping to diagnose where the process may be breaking down.
Frequently Asked Questions (FAQs)
Q1: My multi-omics data comes from different batches. How do MOFA+ and MOGCN handle batch effects, and what pre-processing is required?
- MOFA+ does not automatically correct for batch effects. It requires you to perform batch effect correction as a separate pre-processing step before integration. Common methods include ComBat or Harman [69].
- MoGCN, by constructing a patient similarity network, can be more robust to some technical variations. However, for best practices, it is also recommended to apply pre-processing to minimize batch effects [70]. The model's performance is enhanced with cleaner input data.
Q2: I need to understand which specific genes or pathways are driving my subtype classification. Which tool offers better interpretability?
- MOFA+ is highly regarded for its strong interpretability. It provides feature loadings for each latent factor, allowing you to directly identify the top-weighted genes, miRNAs, or methylation sites. These can be easily linked to downstream pathway enrichment analyses [69] [71].
- MoGCN, while a powerful classifier, has a more complex relationship between input features and the output. You can extract features based on the model's importance scores, but the interpretability is less straightforward than MOFA+'s direct loading scores [69] [70].
Q3: I have a small dataset (n<100). Which method is more suitable for my project?
- MOFA+, as a statistical framework, is generally more robust for smaller sample sizes. Its Bayesian probabilistic model with sparsity constraints is designed to handle high-dimensional data where the number of features far exceeds the number of samples [69] [72].
- MoGCN, as a deep learning model, typically requires a larger amount of data to train effectively and avoid overfitting. Its performance may be suboptimal on very small datasets [73] [70].
Q4: My samples are not perfectly matched across all omics layers. Can these tools handle missing data?
- MOFA+ has a key strength in handling missing data. It can naturally integrate datasets where some omics data is missing for a subset of samples, as it models the shared variation from the available data [74] [72].
- MoGCN typically requires a common set of samples across all input omics layers to construct a unified patient similarity network. Using it with unmatched samples requires additional methodological considerations [70].
Troubleshooting Guides
Problem: MOFA+ model fails to converge or has a long runtime.
- Potential Cause & Solution:
- Check Data Scaling: Ensure all data views are properly normalized (e.g., z-scored) before integration. Large differences in scale between omics types can hinder convergence.
- Adjust Training Parameters: Increase the number of iterations. MOFA+ uses a convergence threshold; allowing it to run longer may resolve the issue. Consider using the stochastic variational inference (SVI) option for very large datasets to speed up computation [72].
- Review Factor Number: An excessively high number of requested factors can increase runtime and complexity. Use the model selection criteria to choose an appropriate number.
Problem: MoGCN model is overfitting, showing high training accuracy but poor test performance.
- Potential Cause & Solution:
- Increase Regularization: Apply stronger regularization techniques (e.g., Dropout, L2 regularization) within the graph convolutional and fully connected layers to reduce overfitting [70].
- Simplify Model Architecture: Reduce the number of layers or neurons in the network. A complex model is more prone to overfitting, especially with limited data.
- Data Augmentation: While challenging with omics data, techniques using generative models like VAEs to synthesize minority-class samples have been proposed to address class imbalance and overfitting [73].
Problem: Biological results from MOFA+ are difficult to interpret.
- Potential Cause & Solution:
- Inspect Factor-Trait Associations: Correlate the inferred latent factors with known clinical features (e.g., tumor stage, survival). This can ground the statistical factors in biological or clinical reality [69] [72].
- Focus on High-Loading Features: For a factor of interest, extract the features (e.g., genes) with the highest absolute loadings. Use these features for functional enrichment analysis (e.g., GO, KEGG) to identify relevant biological pathways [69].
Experimental Protocols for Genomic Subtyping
The following workflow and protocol are based on a comparative analysis of MOFA+ and MoGCN for breast cancer subtype classification [69].
Title: Multi-omics Integration and Subtyping Workflow
1.0 Data Collection and Processing
- 1.1 Data Source: Download multi-omics data (e.g., transcriptomics, epigenomics, microbiome) from public repositories like The Cancer Genome Atlas (TCGA) via cBioPortal [69].
- 1.2 Data Cleaning: Filter out features with zero expression in more than 50% of samples.
- 1.3 Batch Effect Correction: This is a critical step. Apply batch correction methods appropriate for each data type.
- 1.4 Data Normalization: Normalize the data within each omics layer (e.g., z-score normalization) to make features comparable.
2.0 Multi-Omics Data Integration
- 2.1 MOFA+ Integration (Statistical Approach)
- Tool: MOFA+ R package (v 4.3.2).
- Method: Apply unsupervised multi-omics factor analysis. Use the
prepare_mofaandrun_mofafunctions to train the model. Specify the number of factors or allow the model to estimate them based on variance explained. - Key Parameters: Train the model over a sufficient number of iterations (e.g., 400,000) to ensure convergence [69].
- 2.2 MoGCN Integration (Deep Learning Approach)
- Tool: Implement the MoGCN model, available from its GitHub repository [70].
- Method:
- Step 1: Use a multi-modal autoencoder to reduce noise and dimensionality of each omics dataset.
- Step 2: Construct a Patient Similarity Network (PSN) for each omics layer and fuse them into a single network using Similarity Network Fusion (SNF).
- Step 3: Train the Graph Convolutional Network (GCN) using the fused network and the latent features from the autoencoder for subtype classification [70].
3.0 Feature Selection for Subtype Classification
- 3.1 MOFA+ Feature Selection: For a fair comparison, select the top 100 features from each omics layer based on the absolute loadings from the latent factor that explains the highest shared variance [69].
- 3.2 MoGCN Feature Selection: Similarly, select the top 100 features per omics layer based on an importance score calculated by multiplying the absolute encoder weights by the standard deviation of each input feature [69].
4.0 Subtype Classification & Evaluation
- 4.1 Classifier Training: Use the selected features from each method to train supervised classifiers.
- Models: Use both linear (e.g., Logistic Regression with L2 regularization) and non-linear (e.g., Support Vector Classifier with linear kernel) models.
- Training: Perform a grid search with five-fold cross-validation to find the best hyperparameters. Use the F1 score as the evaluation metric to handle class imbalance [69].
- 4.2 Clustering Evaluation (Unsupervised): Evaluate the latent representations from MOFA+ and MoGCN using clustering metrics.
- Methods: Apply t-SNE for visualization.
- Metrics: Calculate the Calinski-Harabasz index (higher is better) and the Davies-Bouldin index (lower is better) [69].
5.0 Biological Validation
- 5.1 Pathway Enrichment Analysis: Input the top transcriptomic features identified by each method into tools like OmicsNet 2.0 for network construction and IntAct database for pathway enrichment analysis (significance threshold P-value < 0.05) [69].
- 5.2 Clinical Association: Correlate the identified key features with clinical data (e.g., survival, tumor stage) using databases like OncoDB to assess clinical relevance [69].
Performance Comparison for Breast Cancer Subtyping
The table below summarizes key quantitative findings from a study comparing MOFA+ and MoGCN on 960 breast cancer samples [69].
| Evaluation Metric | MOFA+ (Statistical) | MoGCN (Deep Learning) |
|---|---|---|
| Subtype Classification (F1 Score) | 0.75 (Non-linear model) | Lower than MOFA+ (Exact value not specified) |
| Number of Enriched Pathways Identified | 121 | 100 |
| Key Pathways Identified | Fc gamma R-mediated phagocytosis, SNARE pathway | Not Specified |
| Clustering Quality (Calinski-Harabasz Index) | Higher | Lower |
| Clustering Quality (Davies-Bouldin Index) | Lower | Higher |
| Strengths | Superior feature selection, better interpretability, handles missing data | Integrates network topology, potential for capturing complex non-linearities |
The Scientist's Toolkit: Essential Research Reagents
The table lists key computational tools and data resources essential for conducting multi-omics integration studies as discussed.
| Tool / Resource | Function & Explanation |
|---|---|
| MOFA+ | A statistical framework for unsupervised integration of multi-omics data. It identifies latent factors that represent key sources of biological and technical variation across datasets [72] [75]. |
| MoGCN | A deep learning model that uses Graph Convolutional Networks to integrate multi-omics data for cancer subtype classification by combining patient similarity networks and feature vectors [70]. |
| TCGA (The Cancer Genome Atlas) | A public database that provides a large collection of multi-omics data from various cancer types, serving as a primary data source for development and validation [69] [70]. |
| Similarity Network Fusion (SNF) | A method used to construct a fused patient similarity network from multiple omics data types, which is a key input for the MoGCN model [70]. |
| Autoencoder (AE) | A type of neural network used for dimensionality reduction. In MoGCN, it is used to compress each omics dataset and extract meaningful latent features [70]. |
| cBioPortal | A web resource for visualizing, analyzing, and downloading cancer genomics datasets, often used to access TCGA data [69]. |
Benchmarks and Real-World Performance: Validating and Comparing Subtyping Methods
FAQs on Epidemiological Concordance
What is epidemiological concordance and why is it important for genomic research?
Epidemiological concordance refers to the agreement between different methodological approaches when assessing the same biological or clinical question. In genomic research, it serves as a critical benchmark for validating new subtyping methods. When different research designs—such as observational studies and randomized controlled trials—produce concordant findings, it increases confidence in the results' validity [76] [77]. For genomic subtyping, this means that molecular classifications should align with clinical outcomes and epidemiological patterns to be considered biologically meaningful and clinically useful.
How can I assess concordance when validating a new subtyping method?
Researchers can assess concordance through multiple approaches. One method involves comparing the summary findings from different research designs that are statistically significant and in the same direction [76]. Another approach evaluates genetic linkage alongside epidemiological transmission patterns, where genomic relatedness (e.g., SNP distances) should correlate with epidemiological assessments of transmission probability [78]. A third strategy examines whether identified subtypes demonstrate consistent clinical behavior across different patient populations and data sources [79].
What are common causes of discordance in molecular subtyping?
Several factors can lead to discordant results in subtyping studies. Technical variability in sample processing, library preparation, or sequencing can introduce artifacts [12]. Biological heterogeneity within tumors may cause sampling bias, especially when different regions of the same tumor show distinct molecular profiles [20]. Methodological limitations arise when subtyping tools prioritize certain data types over others or fail to capture complementary biological information [20]. Data source inconsistencies occur when different surveillance systems or databases report varying case counts for the same condition [79].
Troubleshooting Guide: Addressing Discordance in Subtyping Studies
Problem: Poor Concordance Between Molecular Subtypes and Clinical Outcomes
| Symptoms | Potential Causes | Corrective Actions |
|---|---|---|
| Subtypes lack prognostic significance | Method overlooks clinically relevant features; Inadequate feature selection | Incorporate direction-aware metrics like angular distance; Use multi-omics integration [20] |
| Poor cross-dataset reproducibility | Overfitting to dataset-specific noise; Limited biological knowledge incorporation | Apply ensemble clustering (e.g., spectral clustering + community detection); Include pathway information [20] |
| Inconsistent treatment response prediction | Tumor heterogeneity not captured; Subtypes don't reflect biological mechanisms | Leverage complementary data types; Analyze at gene-level with KEGG pathways [20] |
Problem: Technical Discordance in Sequencing Data
| Symptoms | Potential Causes | Corrective Actions |
|---|---|---|
| Low library yield | Input quality issues; Contaminants; Fragmentation inefficiency | Re-purify input; Verify quantification; Optimize fragmentation parameters [12] |
| High duplicate rates | Overamplification; Insufficient input material | Reduce PCR cycles; Use two-step indexing; Validate with qPCR [12] |
| Adapter dimer contamination | Improper adapter ratios; Inefficient cleanup | Titrate adapter:insert ratios; Adjust bead cleanup parameters [12] |
| Sample call rate below threshold | DNA inhibitors; Array performance issues | Ethanol precipitation cleanup; Verify array suitability for sample type [80] |
| Symptoms | Potential Causes | Corrective Actions |
|---|---|---|
| Varying case counts across sources | Different reporting standards; Geographic resolution limitations | Understand source limitations; Use multiple sources for triangulation [79] |
| Unidentified transmissions in outbreak | Limited epidemiological resolution; Asymptomatic cases | Supplement with genomic linkage analysis (SNP cut-offs) [78] |
| Implausibly high case counts | Billing data artifacts; Surveillance biases | Cross-validate with clinical data; Assess source suitability for disease context [79] |
Experimental Protocols for Concordance Assessment
Protocol 1: Evaluating Subtyping Method Performance Using DSCC Framework
The Disease Subtyping using Spectral Clustering and Community detection from Consensus networks (DSCC) protocol provides a robust framework for achieving concordant subtyping [20]:
Data Processing: Aggregate multi-omics data (mRNA, miRNA, DNA methylation, CNVs, somatic mutations, protein, metabolite levels) into gene-level features. Map features to KEGG pathways for biological consistency.
Patient Network Construction: For each data matrix, compute both Euclidean and Angular affinity matrices to capture magnitude and directional relationships:
- Euclidean affinity:
A_ij = exp(-d_euclidean²/μ²) - Angular affinity:
A_ij = exp(-d_angular²/μ²) - Use median of pairwise distances for scaling parameter μ
- Euclidean affinity:
Consensus Network Formation: Combine affinity matrices into three consensus matrices: consensus Euclidean affinity, consensus Angular affinity, and consensus connectivity.
Ensemble Clustering: Apply both spectral clustering (to identify global structures) and community detection methods like Louvain (to capture local patterns) for robust subtype identification.
Concordance Validation: Validate subtypes against clinical outcomes (survival analysis) and biological pathways (enrichment analysis).
Protocol 2: Assessing Transmission Concordance in Infectious Diseases
This protocol evaluates concordance between epidemiological and genomic transmission assessment [78]:
Study Population: Include consecutive carriers of the pathogen during the study period in an endemic setting.
Epidemiological Assessment: Prospectively investigate patient contacts and exposures. Classify transmission probability into four categories: no suspected transmission, low, moderate, and high probability.
Genomic Analysis: Perform whole-genome sequencing of isolates. Calculate single nucleotide polymorphism (SNP) distances between isolates. Establish SNP cut-off to define genetically related strains (e.g., 80 SNPs).
Concordance Measurement: Compare epidemiological and genetic linkage across all patient-isolate pairs. Test for trend in genomic linkage across increasing levels of epidemiological transmission probability.
Statistical Analysis: Use chi-square test for trend to assess significance of concordance pattern.
Research Reagent Solutions
| Item | Function | Application Notes |
|---|---|---|
| NH4OAc/Ethanol DNA Cleanup | Removes inhibitors from gDNA preparations | Use 0.5 volumes 7.5M NH4OAc + 2.5 volumes absolute ethanol; Incubate 1hr at -20°C [80] |
| Axiom Genotyping Arrays | High-density genotyping | Mendelian consistency rate: 99.96%; Average sample call rate: 99.62% [80] |
| Reduced EDTA TE Buffer | DNA resuspension after cleanup | Maintains DNA stability while reducing EDTA interference (10mM Tris-HCl pH 8.0, 0.1mM EDTA) [80] |
| Multi-omics Data Matrices | Comprehensive molecular profiling | Includes mRNA, miRNA, methylation, CNV, mutations, protein, metabolites; Enables cross-validation [20] |
Quantitative Data on Method Concordance
| Concordance Measure | Results (n=34 Associations) |
|---|---|
| Same direction findings | 23/34 associations (67.6%) |
| Statistically significant same direction | 6/23 associations (26.1%) |
| Opposite direction findings | 11/34 associations (32.4%) |
| Statistically significantly different | 12/34 associations (35.3%) |
| Epidemiological Probability | Genomic Linkage (80 SNP cut-off) |
|---|---|
| No transmission suspected | 115/708 (16.2%) |
| Low probability | 27/319 (8.5%) |
| Moderate probability | 11/26 (42.3%) |
| High probability | 64/76 (84.2%) |
Workflow Visualization
DSCC Method Workflow
Transmission Concordance Assessment
Multi-Omics Integration for Subtyping
Molecular subtyping of bacterial pathogens is an indispensable tool for public health surveillance, outbreak investigations, and source tracking in foodborne disease. For pathogens like Salmonella and Listeria monocytogenes, subtyping methods determine the genetic relatedness between isolates, enabling researchers to distinguish strains beyond the species level. This capability is crucial for identifying contamination sources during food safety incidents and implementing effective control measures [81]. The central thesis of this technical evaluation is that while multiple subtyping methodologies are available, their discriminatory power—the ability to differentiate between unrelated strains—varies significantly. The selection of an appropriate method must therefore be guided by the specific organism, the epidemiological context, and the required resolution [1] [82]. The field is currently undergoing a major transition, with whole-genome sequencing (WGS) rapidly emerging as the new gold standard due to its superior resolution, despite ongoing utility of established techniques for specific applications [81].
Technical Comparison of Major Subtyping Methods
This section provides a detailed, side-by-side comparison of the most widely used subtyping techniques, summarizing their key characteristics to guide method selection.
Comparative Performance of Subtyping Assays
Table 1: Overview of Key Subtyping Methods for Bacterial Pathogens
| Method | Discriminatory Power | Ability for Serovar Prediction | Time to Result (from single colony) | Estimated Service Cost per Isolate (USD) | Primary Advantages | Primary Disadvantages |
|---|---|---|---|---|---|---|
| Classical Serotyping | Very Poor [81] | Directly identifies serovar [81] | 2–17 days [81] | ~$175 [81] | Provides historical epidemiological context [81] | Time-consuming, labor-intensive, low resolution, requires extensive antisera [81] |
| Pulsed-Field Gel Electrophoresis (PFGE) | Good [81] | Intermediate [81] | 4–6 days [81] | $130–$200 [81] | Gold standard for outbreak investigation; highly reproducible [1] | Labor-intensive; does not produce phylogenetically relevant data [1] |
| Multilocus Sequence Typing (MLST) | Low to Moderate [1] | Intermediate [81] | 1–2 days [81] | ~$280 [81] | Excellent for phylogenetic studies; highly reproducible [1] | Low discriminatory power limits use in outbreak investigations [1] |
| Whole-Genome Sequencing (WGS) | Best [81] [1] | High (via in silico prediction) [81] | 3–17 days (depends on workflow) [81] | $100–>$500 [81] | Ultimate discriminatory power; enables in silico serotyping, resistance, and virulence profiling [81] [1] | High informatics burden; requires bioinformatics expertise; cost of instrumentation [1] |
Workflow Diagram: From Sample to Subtype
The following diagram illustrates the general workflow for molecular subtyping, from sample collection to data interpretation, which is common across different methodologies.
Detailed Experimental Protocols
This section outlines standard operating procedures for three key molecular subtyping techniques, providing a foundation for laboratory implementation.
Pulsed-Field Gel Electrophoresis (PFGE) Protocol
PFGE remains a widely used method for high-resolution subtyping of bacterial isolates [83] [82].
- Step 1: Preparation of Agarose-Embedded DNA. Grow a pure culture of the isolate overnight. Suspend bacterial cells to a specific optical density (e.g., 4.0 McFarland standard). Mix the cell suspension with molten, clean-cut agarose and dispense into plug molds. Solidify the plugs on ice or at 4°C [82].
- Step 2: Cell Lysis and DNA Restriction. Incubate the plugs in a lysis buffer containing proteinase K to lyse the cells and digest proteins, releasing intact genomic DNA. Following lysis, wash the plugs thoroughly with Tris-EDTA (TE) buffer to remove cellular debris and enzyme residues. Incubate a slice of the purified plug with a rare-cutting restriction enzyme (e.g., XbaI for Salmonella, ApaI or AscI for Listeria) to generate large DNA fragments [82].
- Step 3: Electrophoresis and Analysis. Place the restricted plug slice into an agarose gel. Perform electrophoresis using a contour-clamped homogeneous electric field (CHEF) apparatus under standardized conditions (e.g., in 0.5X TBE buffer at 14°C, with pulse times optimized for the pathogen). Stain the gel with ethidium bromide and visualize the banding pattern under UV light. Analyze the fingerprint patterns using specialized software (e.g., BioNumerics) to determine isolate relatedness [82].
Multilocus Sequence Typing (MLST) Protocol
MLST provides a standardized approach for characterizing bacterial isolates based on DNA sequence data [82].
- Step 1: DNA Extraction and Target Amplification. Extract genomic DNA from a pure bacterial culture. Design and utilize PCR primers to amplify internal fragments (typically 450-500 bp) of seven housekeeping genes. The selection of genes is standardized for each bacterial species [82].
- Step 2: DNA Sequencing and Allele Assignment. Purify the PCR products and perform Sanger sequencing for each of the seven gene fragments from both directions. Compare the obtained sequences against the curated MLST database for the specific pathogen (e.g.,
pubmlst.org). Assign an allele number for each gene fragment based on its unique sequence [82]. - Step 3: Sequence Type (ST) Determination. The combination of the seven assigned allele numbers defines the Sequence Type (ST) for the isolate. For example, an isolate with the allele profile
(2, 5, 12, 7, 9, 3, 1)would be assigned a unique ST number. Closely related STs are grouped into Clonal Complexes (CCs) [82].
Whole-Genome Sequencing (WGS) Data Analysis Workflows
WGS data can be analyzed using two primary computational approaches for subtyping, each with distinct strengths.
- cg/wgMLST (Gene-by-Gene Approach). This method involves comparing the sequenced isolate against a curated scheme of core genome (cgMLST) or whole genome (wgMLST) genes. The analysis identifies differences in the allele profiles of these genes. It is relatively robust to evolutionary events like homologous recombination and allows for easy data standardization and portability between laboratories [84].
- Single Nucleotide Polymorphism (SNP)-Based Analysis. This method identifies single nucleotide differences across the entire genome. It can be performed by mapping sequencing reads to a reference genome or by comparing de novo assemblies. SNP-based methods offer very high resolution but require careful bioinformatics processing, often including filtering of recombinant genomic regions to avoid misleading distance estimates [84].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful subtyping requires high-quality reagents and specialized materials. The following table lists key components for establishing these methods in the laboratory.
Table 2: Essential Research Reagents and Materials for Subtyping
| Item Name | Function/Application | Specific Examples & Notes |
|---|---|---|
| Selective & Non-Selective Enrichment Media | Isolation and growth of target pathogens from complex samples. | Buffered Listeria Enrichment Broth (BLEB), Fraser Broth, Rappaport-Vassiliadis Soy Broth. Different media can bias which strains are isolated [85]. |
| Immunomagnetic Separation (IMS) Beads | Specific capture and concentration of target bacteria from enrichment cultures. | Anti-Listeria or anti-Salmonella antibody-coated magnetic beads (e.g., Dynal beads) for purification prior to subtyping [85]. |
| Restriction Enzymes | Digesting genomic DNA to generate fragments for banding pattern analysis. | XbaI (for Salmonella PFGE) [82]; ApaI and AscI (for Listeria PFGE) [83] [86]. |
| Molecular Biology Kits | Standardized protocols for DNA extraction, purification, and PCR setup. | Commercial kits for plasmid purification [82], genomic DNA extraction (e.g., guanidinium thiocyanate method for Rep-PCR) [82], and PCR clean-up. |
| PCR Primers | Amplification of specific genetic targets for sequence-based typing. | Primers for MLST housekeeping genes [82]; Rep-PCR primers (e.g., Uprime-RI set) [82]; primers for virulence gene confirmation (e.g., hlyA for L. monocytogenes) [85]. |
| Bioinformatics Software | Analysis of sequencing data, phylogenetic tree construction, and cluster analysis. | Tools for cg/wgMLST (e.g., BioNumerics), SNP calling (e.g., CFSAN SNP Pipeline, Gubbins), and recombination detection (e.g., ClonalFrameML) [84]. |
Troubleshooting Guide & FAQs
This section addresses common technical challenges and questions researchers face when performing subtyping studies.
Frequently Asked Questions (FAQs)
Q1: My PFGE results show faint or smeared bands. What could be the cause? A: Smeared PFGE patterns are often a result of incomplete DNA restriction or DNA degradation. To resolve this, ensure that the restriction enzyme is active and that the reaction conditions (buffer, temperature, incubation time) are optimal. Also, verify that the proteinase K digestion step was complete and that all inhibitors were removed during the plug wash steps [82].
Q2: When should I use MLST over WGS for my subtyping needs? A: MLST remains a cost-effective and standardized method for long-term phylogenetic studies and population genetics, where high discriminatory power is not the primary goal. It is also useful as a rapid screening tool or in laboratories without access to high-throughput sequencing capabilities. However, for high-resolution outbreak investigations where distinguishing between very closely related isolates is critical, WGS is the superior choice [81] [1].
Q3: We found different Listeria subtypes when using two different enrichment methods on the same sample. Which result is correct? A: Both results are likely valid. Different enrichment protocols, particularly those with varying selective pressures (e.g., Fraser Broth vs. a non-selective enrichment with IMS), can select for different subpopulations of bacteria present in the original sample. This phenomenon, known as enrichment bias, means that using a single method may not capture the full diversity of strains present. The use of multiple enrichment methods can provide a more comprehensive picture of the contamination [85].
Q4: What is the major hurdle to adopting WGS in a routine public health laboratory? A: The primary challenge is no longer the cost of sequencing itself, but the bioinformatics burden. This includes the need for significant technical expertise in data analysis, high-capacity computing infrastructure, specialized software, and the lack of a universal, standardized analysis method that fits all organisms and epidemiological questions [1] [84].
Troubleshooting Common Experimental Issues
- Problem: Low Discriminatory Power with MLST. If MLST fails to distinguish between isolates that are suspected to be unrelated, it is a limitation of the method's inherent resolution. Solution: Move to a higher-resolution method such as cgMLST (which analyzes hundreds of genes) or WGS-based SNP analysis to achieve the necessary discrimination for outbreak investigation [1].
- Problem: Poor Reproducibility in Band-Based Methods (e.g., Rep-PCR). Slight variations in electrophoresis conditions, reagent quality, or DNA concentration can lead to pattern shifts. Solution: Strictly standardize all protocols. Always include reference size standards in every gel run and use software that normalizes band positions based on these standards to ensure inter-gel comparability [82].
- Problem: Inconsistent WGS Phylogenetic Results. Different analysis workflows (e.g., cgMLST vs. SNP-based trees) or parameter settings can produce varying phylogenetic trees. Solution: This highlights the need for benchmarking and validation of bioinformatics pipelines. For a given organism and study context, consistently apply a single, validated workflow. Be aware that the choice of reference genome in SNP analysis can impact the results [84].
Technical Support Center: Troubleshooting Guides & FAQs
This technical support center is designed for researchers working on enhancing the discriminatory power of genomic subtyping methods for lymphoma and breast cancer. The following guides address common experimental challenges, supported by recent breakthroughs and quantitative evidence.
Frequently Asked Questions
Q1: Our DLBCL subtyping model using whole slide images (WSIs) is overfitting despite data augmentation. What robust architectures can improve generalization?
A: Overfitting in WSI analysis is common due to high image resolution and limited labeled datasets. We recommend a vision transformer-based framework with knowledge distillation [87].
- Recommended Solution: Implement a teacher-student knowledge distillation framework. Train a multi-modal teacher model on all available WSI modalities (e.g., HES, IHC-BCL6, IHC-CD10, IHC-MUM1). Then, use this teacher to guide the training of a mono-modal student model that uses only HES stains. This transfers knowledge from multiple modalities to a simpler model, significantly improving its generalization on a single modality [87].
- Key Experimental Protocol:
- Teacher Model Training: Develop a multi-modal architecture with a Vision Transformer (ViT) encoder to process high-resolution WSIs as sequences of patches. Implement a feature fusion mechanism to combine information from the four input modalities.
- Knowledge Distillation: Use the trained teacher model to generate soft labels (probability distributions) for the training dataset.
- Student Model Training: Train a mono-modal ViT-based student model on HES stains only. The loss function should combine the standard cross-entropy loss with a distillation loss (e.g., Kullback-Leibler divergence) that measures the difference between the student's predictions and the teacher's soft labels.
- Expected Outcome: This approach has shown to outperform six state-of-the-art methods, effectively leveraging multi-modal data to create a highly accurate mono-modal classifier, thus reducing overfitting [87].
Q2: For lymphoma histopathological classification, how can we achieve high accuracy with a small, labeled dataset?
A: Small datasets hinder deep learning models. An autoencoder-assisted stacked ensemble learning (SEL) framework effectively addresses this by leveraging unsupervised feature learning [88].
- Recommended Solution: Employ a convolutional autoencoder (CAE) for unsupervised deep feature extraction, followed by a stacked ensemble of classifiers.
- Key Experimental Protocol:
- Feature Extraction: Train a CAE on your histopathological images (labeled or unlabeled) to learn compressed, high-level feature representations. Use Principal Component Analysis (PCA) for further dimensionality reduction.
- Base Model Training: Train multiple machine learning classifiers (e.g., Random Forest, Support Vector Machine, Multi-Layer Perceptron) on the extracted deep features.
- Stacked Ensemble: Use the predictions from these base classifiers as input features to a meta-classifier (e.g., a Gradient Boosting Machine) for final prediction.
- Expected Outcome: This hybrid pipeline has achieved 99.04% accuracy, 0.9998 AUC, and 0.9996 Average Precision in lymphoma subtype identification, demonstrating superior performance with limited data by reducing overfitting and enhancing feature discrimination [88].
Q3: How can we validate the discriminatory power of new HRQoL instruments in specific cancer populations like DLBCL?
A Direct comparison of utility scores and statistical analysis of measurement properties between established instruments is required [89].
- Recommended Solution: Conduct a cross-sectional study using both the new and standard instruments (e.g., EQ-5D-5L and SF-6Dv2) in the same patient cohort. Analyze the correlation and agreement between the derived utility scores.
- Key Experimental Protocol:
- Data Collection: Administer both HRQoL instruments to a defined patient population (e.g., DLBCL patients). Collect demographic and clinical characteristics.
- Statistical Analysis:
- Calculate mean utility scores for each instrument.
- Assess correlation between instrument dimensions using Spearman's correlation and between utility scores using Pearson's correlation.
- Evaluate agreement using a Bland-Altman plot.
- Compare utility scores across clinical subgroups (e.g., initial-treatment vs. relapsed/refractory) using ANOVA or t-tests.
- Use the Graded Response Model (GRM) to analyze the discrimination ability of each dimension.
- Expected Outcome: The study will reveal if the two instruments can be used interchangeably. For example, in Chinese DLBCL patients, the correlation was high (0.787) but agreement was not strong, and EQ-5D-5L had suboptimal discriminative power in patients with good health, indicating the instruments are not interchangeable [89].
Q4: We are exploring combination therapies in lymphoma. How can we design models to predict patient response to immunotherapy combinations?
A Move beyond monotherapy models by integrating multimodal data that reflects the tumor immune microenvironment and mechanisms of action of combined therapies [90].
- Recommended Solution: Develop machine learning models that incorporate clinical, pathological, and molecular baseline data to predict outcomes like survival or treatment response. Ensemble methods have shown high performance in this context.
- Key Experimental Protocol:
- Data Curation: Collect baseline patient data including demographics, disease stage, ECOG performance status, LDH levels, IPI score, extranodal involvement, and molecular subtype (e.g., GCB/ABC).
- Model Training and Validation: Train multiple supervised machine learning models, such as Random Forest (RF), XGBoost, and multilayer perceptron (MLP). Use a held-out test set for validation. Address class imbalance with techniques like class-weight adjustment.
- Performance Assessment: Evaluate models using AUC, accuracy, F1-score, and Brier score. For time-to-event outcomes, use Random Survival Forests (RSF) or Cox models and assess with C-index and Integrated Brier Score.
- Expected Outcome: Studies have shown that ML models like Random Forest can achieve high discrimination (AUC = 0.906) in predicting mortality in DLBCL, outperforming traditional statistical approaches like the Cox model (C-index = 0.55) [91].
Table 1: Performance Comparison of Lymphoma Subtyping and Prognostication Models
| Model/Approach | Application | Key Performance Metrics | Reference |
|---|---|---|---|
| Vision Transformer with Knowledge Distillation | DLBCL ABC/GCB Subtyping from WSIs | Outperformed 6 state-of-the-art methods | [87] |
| Autoencoder-Assisted Stacked Ensemble | Lymphoma Subtype Classification | Accuracy: 99.04%, AUC: 0.9998, Average Precision: 0.9996 | [88] |
| Random Forest (RF) | DLBCL Mortality Prediction (26 months) | AUC: 0.9060, Accuracy: 0.833, F1-score: 0.902 | [91] |
| Extreme Gradient Boosting (XGBoost) | DLBCL Mortality Prediction (26 months) | AUC: 0.8335 | [91] |
| Multilayer Perceptron (MLP) | DLBCL Mortality Prediction (26 months) | AUC: 0.7861, Accuracy: 0.849 | [91] |
| Cox Proportional Hazards Model | DLBCL Mortality Prediction | Time-dependent AUC: 0.5561, C-index: 0.55 | [91] |
Table 2: Health Utility Scores and Instrument Properties in DLBCL Patients
| Metric | EQ-5D-5L | SF-6Dv2 | Notes |
|---|---|---|---|
| Mean (SD) Utility Score | 0.828 (0.222) | 0.641 (0.220) | Scores are not directly comparable [89] |
| Correlation between Utility Scores | Pearson's correlation: 0.787 [89] | ||
| Correlation between Dimensions | Spearman's correlation ranged from 0.299 to 0.680 [89] | ||
| Discriminatory Power | Suboptimal among patients with good health | Valid properties shown | As per Graded Response Model (GRM) analysis [89] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Advanced Cancer Subtyping workflows
| Item | Function in the Experiment |
|---|---|
| HES-stained Whole Slide Images (WSIs) | Standard histological staining for primary morphological analysis; used as the input modality for mono-modal deep learning models [87]. |
| IHC Markers (e.g., BCL6, CD10, MUM1) | Protein markers for immunohistochemistry used to determine cell-of-origin (e.g., Hans algorithm) and provide multi-modal data for teacher models [87]. |
| EQ-5D-5L Questionnaire | A generic preference-based measure (GPBM) with 5 dimensions (MO, SC, UA, P/D, AD) to assess Health-Related Quality of Life (HRQoL) and generate utility scores for QALY calculations [89]. |
| SF-6Dv2 Questionnaire | A GPBM derived from SF-36, with 6 dimensions (PF, RL, SF, PA, MH, VA), used to assess HRQoL and provide an alternative utility score for health economic evaluations [89]. |
| RNA-seq Data | Used for transcriptomic analysis, crucial for understanding molecular subtypes (e.g., Luminal A, Basal-like in breast cancer) and identifying differentially expressed genes [92]. |
| Target Region Sequencing (TRS) Panels | For focused sequencing of genes or genomic regions with specific functions, allowing detection of variants at low allele frequencies for biomarker discovery [92]. |
| Patient-Derived Cells | Used in microengineered models (e.g., Breast Cancer-on-a-Chip) to create physiologically relevant systems for studying tumor dynamics and personalized drug responses [93]. |
Experimental Workflow & Pathway Visualizations
ViT DLBCL Subtyping Flow
Ensemble Learning Workflow
PD-1/PD-L1 Pathway
FAQs on Inter-laboratory Reproducibility
What defines the "discriminatory power" of a subtyping method, and why is it critical for inter-laterboratory studies?
Discriminatory power is a method's ability to differentiate between epidemiologically unrelated strains of bacteria. Methods with higher discriminatory power reduce the chance of falsely linking unrelated strains or failing to link related ones. This is fundamental for accurate outbreak detection and surveillance, as it ensures that conclusions about transmission pathways are based on true genetic relationships rather than methodological limitations [1].
What are the primary sources of inter-laboratory variability in genomic subtyping, and how can they be minimized?
Key sources of variability include:
- Reagent Quality: Sensitive molecular biology reagents can be compromised by improper storage or bad batches from vendors [94].
- Protocol Deviations: Minor inconsistencies in sample processing, such as fixation times or antibody concentrations, can significantly impact results [94].
- Data Analysis: The interpretation of whole genome sequencing (WGS) data is complex. Without standardized bioinformatic pipelines and parameters, different labs may draw different conclusions from the same data [1]. Minimization strategies include using standardized, validated protocols; implementing rigorous controls; and sharing raw data and analysis parameters between collaborating laboratories.
How does Whole Genome Sequencing (WGS) compare to traditional methods for ensuring reproducibility across labs?
WGS offers superior discriminatory power compared to traditional methods like PFGE or MLST because it interrogates the entire genome rather than a small fraction of it [1]. However, this power introduces complexity. While WGS data itself is highly reproducible, the analytical approaches require standardization. In contrast, methods like PFGE are well-standardized and inexpensive but are less discriminatory and do not provide phylogenetically relevant information [1]. The high reproducibility and typability of WGS make it a powerful tool for inter-laboratory studies, provided the analytical hurdles are addressed [1].
Troubleshooting Guides
Guide 1: Troubleshooting Low Discriminatory Power in Subtyping Assays
Problem: Your subtyping method fails to distinguish between isolates that are known to be epidemiologically unrelated.
Steps to Resolve:
- Repeat the Experiment: Rule out simple human error or technical mistakes during a single run [94].
- Verify Method Selection: Ensure you are using a method with sufficiently high discriminatory power for your investigation. For outbreak investigations, WGS is often required over lower-resolution methods like MLST [1].
- Check Reagents and Equipment:
- Confirm all reagents have been stored at the correct temperature and have not expired [94].
- Verify that equipment, such as sequencers or thermocyclers, is properly calibrated.
- Systematically Change Variables: Isolate and test one variable at a time [94]. Key variables to test include:
- DNA extraction method: Inefficient lysis or shearing can affect downstream analysis.
- Sequencing coverage: Low coverage in NGS methods may miss true genetic variations. The UMA panel, for instance, achieved a median coverage of 233X [95].
- Bioinformatic parameters: Adjust the thresholds for calling genetic variants, such as single nucleotide variants (SNVs). Defining the number of SNVs that constitute a different subtype is critical [1].
Guide 2: Troubleshooting Inter-laboratory Inconsistencies
Problem: Different laboratories generate inconsistent subtyping results when analyzing splits of the same sample.
Steps to Resolve:
- Establish a Common Reference: Use a shared reference material or a "Panel of Normal" samples across all labs to calibrate assays and normalize results [95].
- Standardize the Protocol: Implement a common, validated protocol across all sites. The UMA panel, for example, was designed as a targeted NGS approach specifically validated across two laboratories for clinical-grade accuracy and reproducibility [95].
- Implement a Rigorous Quality Control (QC) System: Define and monitor QC metrics at every step, from DNA quality/quantity to final data output.
- Cross-Validate with an Orthogonal Method: Compare results with a different, established method. The UMA panel was validated against traditional FISH and SNP arrays, achieving a balanced accuracy of over 93% [95].
- Document Everything: Maintain detailed, standardized documentation of all procedures, including any deviations from the protocol. This is essential for identifying the source of discrepancies [94].
Data Presentation
| Subtyping Method | Discriminatory Power | Key Advantages | Key Disadvantages for Inter-laboratory Use |
|---|---|---|---|
| Whole Genome Sequencing (WGS) | Very High | Analysis can be tailored; provides phylogenetic data; high typability. | Requires high technical and bioinformatics expertise; analytical approach not yet standardized; expensive. |
| Pulse Field Gel Electrophoresis (PFGE) | High (Gold Standard) | Well-standardized for many species; inexpensive. | Does not produce phylogenetic data; fairly labor-intensive. |
| Multilocus Sequence Typing (MLST) | Low to Moderate | High repeatability and reproducibility; good for phylogenetics. | Little use in outbreak investigations; requires adaptation for each species. |
| Validation Parameter | Result | Technical Detail |
|---|---|---|
| Concordance with FISH | >93% Balanced Accuracy | Demonstrated for Copy Number Alterations (CNA) and immunoglobulin heavy chain translocations (t-IgH). |
| Sequencing Coverage | Median 233X | With a minimum requirement of ≥4 million reads per sample. |
| Panel Design Efficiency | 92.5% reduction in IgH target size | Targeted 170 regions (92.9 kbp) vs. full IgH locus (1235.3 kbp). |
| Targeted Genomic Aberrations | t-IgH, CNA, mutations in 82 genes | Total panel footprint of 460.4 kbp. |
Experimental Protocols
Objective: To validate the robustness and reproducibility of a customized next-generation sequencing panel across multiple laboratory sites.
Key Materials:
- Patient Samples: DNA extracted from BM-CD138+ cells from patients (e.g., 150 NDMM and SMM patients) and healthy donors for a "Panel of Normal" [95].
- Custom NGS Panel: A designed panel (e.g., UMA: 0.46 Mbp footprint) targeting relevant genomic aberrations [95].
- Reference Methods: Traditional methods for cross-validation, such as FISH panels and SNP arrays [95].
Methodology:
- Sample Distribution: Distribute aliquots of the same DNA samples to participating laboratories.
- Library Preparation: Each lab performs library preparation following the same standardized protocol (e.g., using the SureSelect Agilent Design System) [95].
- Sequencing: Sequence the libraries on respective NGS platforms, ensuring a minimum of 4 million reads per sample is achieved [95].
- Bioinformatic Analysis: Analyze the raw sequencing data (Fastq files) using a unified, customized bioinformatic pipeline to call variants, CNA, and translocations [95].
- Cross-Validation: Compare the NGS results with data generated from the reference methods (FISH, SNP arrays) to calculate concordance metrics [95].
- Inter-lab Comparison: Perform pairwise comparisons of the genomic alteration calls between all participating laboratories to assess reproducibility.
Visualizations
Diagram 1: UMA Panel Inter-lab Validation Workflow
Diagram 2: Troubleshooting Low Discriminatory Power
The Scientist's Toolkit
Research Reagent Solutions for Genomic Subtyping
| Item | Function |
|---|---|
| Custom NGS Capture Panel | Targeted enrichment of genomic regions of interest (e.g., mutations, translocations) for cost-effective and deep sequencing [95]. |
| Panel of Normal (PON) | DNA from healthy donors used to establish a baseline and filter out common polymorphisms and sequencing artifacts during bioinformatic analysis [95]. |
| Orthogonal Validation Methods | Traditional techniques like FISH and SNP arrays used to cross-validate and confirm findings from novel NGS assays [95]. |
| Standardized DNA Extraction Kits | Ensure consistent yield, purity, and fragment size of DNA across all samples and laboratories, a critical first step for reproducibility. |
| Reference Genomic DNA | A well-characterized control sample used across runs and labs to monitor assay performance and technical variability. |
Conclusion
Enhancing the discriminatory power of genomic subtyping is not a one-size-fits-all endeavor but requires a nuanced, method-aware strategy. The journey from low-resolution phenotypic methods to high-fidelity whole-genome techniques has unlocked unprecedented detail for tracking outbreaks and understanding disease heterogeneity. Success hinges on selecting the right tool—whether cgMLST for standardized surveillance, wgMLST for high-resolution outbreak detection, or multi-omic integration for complex diseases—while proactively managing technical confounders like mobile genetic elements. Future directions will be shaped by the widespread adoption of scalable frameworks like Multilevel Genome Typing, the refined application of AI for data integration, and the development of robust, species-specific validation standards. These advances will solidify genomic subtyping as the cornerstone of next-generation public health defense and precision medicine, enabling tailored interventions from the population level down to the individual patient.
References
- 1. What's Your Subtype? The Epidemiologic Utility of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5697907/]
- 2. Assessment and Comparison of Molecular Subtyping ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.01591/full]
- 3. Multi-country and intersectoral assessment of cluster ... [https://www.nature.com/articles/s41467-025-59246-8]
- 4. Troubleshooting - Genomic Epidemiology Ontology [https://genepio.org/lexmapr/lexmapr-documentation/troubleshooting/]
- 5. Center for Genomic Epidemiology [https://www.genomicepidemiology.org/]
- 6. Comparison of whole genome sequencing typing tools for ... [https://link.springer.com/article/10.1007/s10096-024-05013-4]
- 7. Validation of Core and Whole-Genome Multi-Locus ... [https://www.mdpi.com/2076-2607/13/6/1310]
- 8. Whole genome sequence analysis reveals limited diversity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12121276/]
- 9. Automated whole genome sequencing platform for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077132/]
- 10. PFMG2025–integrating genomic medicine into the national ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910791/]
- 11. A new approach for establishing multilocus sequence typing ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-04339-z]
- 12. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 13. Troubleshooting & result interpretation [https://eurofinsgenomics.eu/en/custom-dna-sequencing/eurofins-services/whole-plasmid-sequencing/wps-data-interpretation/]
- 14. Choosing and using diversity indices: insights for ecological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4224527/]
- 15. Opposite trends in response for the Shannon and Simpson ... [https://www.sciencedirect.com/science/article/abs/pii/S0143622802000024]
- 16. Simpson's Diversity Index [https://geographyfieldwork.com/Simpson'sDiversityIndex.htm]
- 17. Diversity index [https://en.wikipedia.org/wiki/Diversity_index]
- 18. A new typing scheme demonstrates high discriminatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12265546/]
- 19. Investigating genetic diversity within Cryptosporidium ... [https://www.sciencedirect.com/science/article/pii/S2667114X25000925]
- 20. DSCC: disease subtyping using spectral clustering and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611214/]
- 21. MuTATE: an interpretable multi-endpoint machine learning ... [https://www.nature.com/articles/s44401-025-00025-4]
- 22. The FUTURE phase II umbrella clinical trial | Cell Research [https://www.nature.com/articles/s41422-023-00795-2]
- 23. Pharmacogenomics in practice: a review and implementation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10233068/]
- 24. Functional genomics and tumor microenvironment analysis ... [https://www.nature.com/articles/s41467-025-64666-7]
- 25. A practical guideline of genomics-driven drug discovery in ... [https://www.sciencedirect.com/science/article/pii/S2666979X22001392]
- 26. Development and implementation of a core genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11315579/]
- 27. Investigating the population structure of Moraxella ... [https://www.nature.com/articles/s41467-025-64487-8]
- 28. Core/Whole Genome Multilocus Sequence Typing and ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.02961/full]
- 29. Tutorial for Stable cgMLST Scheme [https://www.ridom.de/u/Tutorial_for_Stable_cgMLST_Scheme.html]
- 30. Administrator's guide — BIGSdb 1.52.0 documentation [https://bigsdb.readthedocs.io/en/latest/administration.html]
- 31. FAQ | Pathogenwatch - GitBook [https://cgps.gitbook.io/pathogenwatch/faq]
- 32. cgMLST | next.pathogen.watch docs [https://next-docs.pathogen.watch/technical-descriptions-of-analysis-tools/lineage-and-genotyping/cgmlst]
- 33. Whole-Genome Multilocus Sequence Typing of Extended- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5121380/]
- 34. Whole Genome Multilocus Sequence Typing [https://www.cd-genomics.com/bmb/whole-genome-multilocus-sequence-typing.html]
- 35. Searching the Accessory Genome - EnteroBase - Read the Docs [https://enterobase.readthedocs.io/en/latest/features/accessory-genome.html]
- 36. Comparison of Whole Genome (wg-) and Core ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2020.01729/full]
- 37. Step-by-step Tutorial - chewBBACA's documentation! [https://chewbbaca.readthedocs.io/en/latest/user/tutorials/chewie_step_by_step.html]
- 38. cg/wgMLST analysis — pymlst 2.2 documentation [https://pymlst.readthedocs.io/en/stable/documentation/cgmlst.html]
- 39. Whole-genome sequencing and ad hoc shared ... [https://www.nature.com/articles/s41598-021-99080-8]
- 40. SNVPhyl: a single nucleotide variant phylogenomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5628696/]
- 41. Output - SNVPhyl - Read the Docs [https://snvphyl.readthedocs.io/en/latest/user/output/]
- 42. Usage - SNVPhyl [https://snvphyl.readthedocs.io/en/latest/user/usage/]
- 43. High quality core genome single nucleotide variant ... [https://bio-protocol.org/exchange/minidetail?id=6465001&type=30]
- 44. Parameters - SNVPhyl - Read the Docs [https://snvphyl.readthedocs.io/en/latest/user/parameters/]
- 45. Troubleshooting Pipelines Guide - GitHub Pages [https://phac-nml.github.io/irida-documentation/user/administrator/troubleshooting/pipelines/]
- 46. Multilevel genome typing: genomics-guided scalable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7262494/]
- 47. Characterizing Staphylococcus aureus genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542621/]
- 48. genomics-guided scalable resolution typing of microbial ... [https://pubmed.ncbi.nlm.nih.gov/32458794/]
- 49. Multi-Omics Data Fusion for Cancer Molecular Subtyping ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.607817/full]
- 50. Integrative analysis of multi-omics data and gut microbiota ... [https://www.nature.com/articles/s41598-025-08915-1]
- 51. Beyond Biomarkers: Machine Learning-Driven Multiomics ... [https://www.mdpi.com/2075-4426/15/5/166]
- 52. Navigating Cancer Complexity: Integrative Multi-Omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553891/]
- 53. Gene-SGAN: discovering disease subtypes with imaging ... [https://www.nature.com/articles/s41467-023-44271-2]
- 54. Genomic Analysis Reveals Racial and Age-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12034101/]
- 55. Evaluation of whole-genome sequencing-based subtyping ... [https://pubmed.ncbi.nlm.nih.gov/34730485/]
- 56. Typing methods based on whole genome sequencing data [https://onehealthoutlook.biomedcentral.com/articles/10.1186/s42522-020-0010-1]
- 57. Comprehensive discovery and functional characterization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12454387/]
- 58. PHASTER [https://phaster.ca/]
- 59. PlasmidScope: a comprehensive plasmid database with rich ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11701673/]
- 60. De novo virulence feature discovery and risk assessment ... [https://www.nature.com/articles/s42003-025-07678-9]
- 61. SNPPar: identifying convergent evolution and other ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8767352/]
- 62. Homoplasy as an Evolutionary Process: An Optimistic View ... [https://link.springer.com/article/10.1007/s13752-024-00470-8]
- 63. HomoplasyFinder: a simple tool to identify homoplasies on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6412054/]
- 64. MicrobesNG - Frequently Asked Questions [https://microbesng.com/microbesng-faq/]
- 65. Benchmarking genetic interaction scoring methods for ... [https://pubmed.ncbi.nlm.nih.gov/41018953/]
- 66. Validation and Discrepancy Report Error Explanations - NCBI [https://www.ncbi.nlm.nih.gov/genbank/validation/]
- 67. Frequently Asked Questions — BLASTHelp documentation - NIH [https://blast.ncbi.nlm.nih.gov/doc/blast-help/FAQ.html]
- 68. Troubles importing FASTA file - User Support [https://forum.qiime2.org/t/troubles-importing-fasta-file/2546]
- 69. Comparative analysis of statistical and deep learning-based multi-omics integration for breast cancer subtype classification | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06662-5]
- 70. MoGCN: A Multi-Omics Integration Method Based on ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.806842/full]
- 71. Multi-Omics: Challenges and Solutions [https://bigomics.ch/blog/key-challenges-in-multi-omics-data-integration/]
- 72. MOFA+: a statistical framework for comprehensive integration of multi-modal single-cell data | Genome Biology | Full Text [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-020-02015-1]
- 73. Challenges in AI-driven multi-omics data analysis for ... [https://www.sciencedirect.com/science/article/pii/S2352914825000681]
- 74. A technical review of multi-omics data integration methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC12315550/]
- 75. MOFA | Multi-Omics Factor Analysis [https://biofam.github.io/MOFA2/]
- 76. Concordance Between the Findings of Epidemiological ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK138246/]
- 77. Vol 6: Concordance Between the Findings of ... [https://www.ahrq.gov/research/findings/evidence-based-reports/nutritn6tp.html]
- 78. Concordance between epidemiological evaluation of ... [https://www.sciencedirect.com/science/article/pii/S1198743X20302238]
- 79. Measuring concordance of data sources used for infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9980358/]
- 80. Genotyping Support - Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/microarray-analysis-support-center/genotyping-support/genotyping-support-troubleshooting.html]
- 81. Assessment and Comparison of Molecular Subtyping and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6639432/]
- 82. Comparison of Subtyping Methods for Differentiating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1594788/]
- 83. Comparison of three molecular subtyping techniques for ... [https://pubmed.ncbi.nlm.nih.gov/31023493/]
- 84. Detailed Evaluation of Data Analysis Tools for Subtyping ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.02897/full]
- 85. Comparison of Subtypes of Listeria monocytogenes Isolates ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0092467]
- 86. Comparison of three molecular subtyping techniques for ... [https://www.sciencedirect.com/science/article/pii/S0325754119300045]
- 87. A vision transformer-based framework for knowledge ... [https://arxiv.org/html/2308.01328v3]
- 88. Autoencoder-Assisted Stacked Ensemble Learning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389832/]
- 89. EQ-5D-5L and SF-6Dv2 health utilities scores of diffuse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11414240/]
- 90. Beyond monotherapy: multimodal strategies integrating ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1713199/full]
- 91. Mortality Prediction in Diffuse Large B-Cell Lymphoma ... [https://www.mdpi.com/2077-0383/14/22/8216]
- 92. Bioinformatics Strategies in Breast Cancer Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563043/]
- 93. Microengineered Breast Cancer Models: Shaping the ... [https://www.mdpi.com/2072-6694/17/19/3160]
- 94. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 95. Unique molecular assay (UMA): a next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485320/]