Breaking the Bottleneck: Strategies to Overcome NGS Data Analysis Challenges in Chemogenomics
Next-generation sequencing (NGS) has become indispensable in chemogenomics for uncovering the genetic basis of drug response and toxicity.
Breaking the Bottleneck: Strategies to Overcome NGS Data Analysis Challenges in Chemogenomics
Abstract
Next-generation sequencing (NGS) has become indispensable in chemogenomics for uncovering the genetic basis of drug response and toxicity. However, the transition from raw sequence data to clinically actionable insights is hampered by significant bottlenecks, including data deluge, rare variant interpretation, and analytical inconsistencies. This article provides a comprehensive guide for researchers and drug development professionals, addressing these challenges from foundational principles to advanced applications. We explore the unique data analysis demands in chemogenomics, detail cutting-edge methodological approaches leveraging AI and automation, provide proven optimization strategies for robust workflows, and discuss validation frameworks to ensure reliable, clinically translatable results. By synthesizing current best practices and emerging technologies, this resource aims to equip scientists with the knowledge to accelerate drug discovery and development through more efficient and accurate NGS data analysis.
The Chemogenomics Data Deluge: Understanding the Scale and Source of NGS Bottlenecks
The Unique Data Analysis Demands of Chemogenomics
Core Concepts of Chemogenomics
What is chemogenomics and what kind of data does it generate?
Chemogenomics is a powerful approach that studies cellular responses to chemical perturbations. In the context of genome-wide CRISPR/Cas9 knockout screens, it identifies genes whose knockout sensitizes or suppresses growth inhibition induced by a compound [1]. This generates a genetic signature that can decipher a compound's mechanism of action (MOA), identify off-target effects, and reveal chemo-resistance or sensitivity genes [1].
What are the primary goals of a chemogenomic screen?
The primary goals are to:
- Confirm the mechanism of action (MOA) of a compound.
- Identify potential secondary off-target effects.
- Discover genetic vulnerabilities suggesting innovative drug combination strategies.
- Identify novel gene functions involved in the cellular mechanism targeted by a compound [1].
Troubleshooting NGS Data Analysis in Chemogenomics
How do I address low sequencing library yield from my chemogenomic screen?
Low library yield can halt progress. The following table outlines common causes and corrective actions based on established NGS troubleshooting guidelines [2].
| Cause | Mechanism of Yield Loss | Corrective Action |
|---|---|---|
| Poor Input Quality / Contaminants | Enzyme inhibition from residual salts, phenol, or EDTA [2]. | Re-purify input sample; ensure wash buffers are fresh; target high purity (260/230 > 1.8) [2]. |
| Inaccurate Quantification | Under-estimating input concentration leads to suboptimal enzyme stoichiometry [2]. | Use fluorometric methods (Qubit) over UV absorbance; calibrate pipettes; use master mixes [2]. |
| Fragmentation Inefficiency | Over- or under-fragmentation reduces adapter ligation efficiency [2]. | Optimize fragmentation parameters (time, energy); verify fragmentation profile before proceeding [2]. |
| Suboptimal Adapter Ligation | Poor ligase performance or incorrect molar ratios reduce adapter incorporation [2]. | Titrate adapter:insert molar ratios; ensure fresh ligase and buffer; maintain optimal temperature [2]. |
My chemogenomic data shows high duplicate reads and potential batch effects. How can I fix this?
Over-amplification during library prep is a common cause of high duplication rates, which reduces library complexity and statistical power [2]. Batch effects from processing samples across different days or operators can also introduce technical variation.
Solutions:
- Optimize PCR Cycles: Use the minimum number of PCR cycles necessary for library amplification to avoid over-amplification artifacts [2].
- Randomize Samples: Process samples randomly across batches to prevent confounding technical effects with biological conditions.
- Automate Library Prep: Consider automated liquid handlers to improve reproducibility. For example, the ExpressPlex kit requires only two pipetting steps prior to thermocycling, significantly reducing manual error [3].
- Use Multiplexing Kits: Employ kits with high auto-normalization capabilities to achieve consistent read depths across samples without individual normalization, reducing preparation variability [3].
What are the best practices for ensuring my bioinformatics workflows are robust and reproducible?
Inefficient or error-prone bioinformatics pipelines can become a major bottleneck, leading to delays, increased costs, and inconsistent results [4].
Methodology for Robust Workflow Development:
- Adopt Modern Frameworks: Migrate legacy in-house workflows to modern, cloud-friendly frameworks like Nextflow and utilize community resources like nf-core for standardized, version-controlled pipelines [4].
- Implement Continuous Integration/Deployment (CI/CD): Set up automated testing for your bioinformatics pipelines to ensure any changes do not break existing functionality and to guarantee reproducibility [4].
- Enable Cross-Platform Deployment: Design workflows to be portable across different computing environments (e.g., Local HPC, Cloud like AWS/Azure) without modification for scalable and flexible analysis [4].
- Utilize Workflow Automation: Implement automatic pipeline triggers upon data arrival to reduce manual intervention and tracking errors, ensuring a consistent analysis path for every dataset [4].
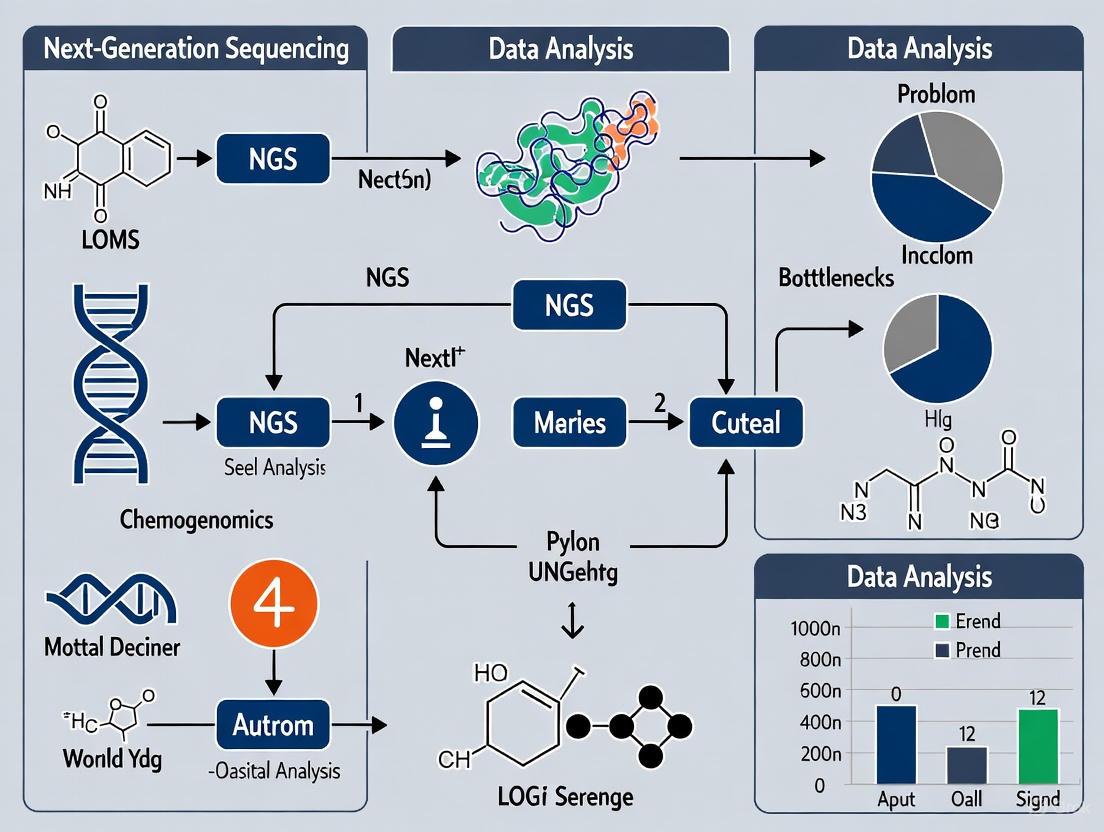
Chemogenomic NGS Analysis Pipeline
FAQs on Experimental Design & Interpretation
What defines a high-quality chemical probe for a chemogenomic screen?
A high-quality chemical probe is a selective small-molecule modulator – usually an inhibitor – of a protein’s function that allows mechanistic and phenotypic questions about its target in cell-based or animal research [5]. Unlike drugs, probes prioritize selectivity over pharmacokinetics.
Key criteria include [5]:
- Selectivity: Demonstrated activity against the intended target with minimal interaction against a panel of related targets.
- Potency: Sufficient cellular activity at the intended dose.
- Target Engagement: Validation that the probe binds to its intended target in the model system used.
- Negative Controls: Availability of an inactive, structurally related control compound.
Why is the use of orthogonal probes and negative controls critical?
The use of two structurally distinct chemical probes (orthogonal probes) is critical because they are unlikely to share the same off-target activities. If both probes produce the same phenotypic result, confidence increases that the effect is due to on-target modulation [5]. Negative controls help distinguish specific on-target effects from non-specific or off-target effects inherent to the chemical scaffold [5].
How do I determine the correct concentration for my compound in a cellular screen?
For a chemogenomic screen in NALM6 cells, the platform typically performs a dose-response curve to determine the IC50 (the concentration that inhibits 50% of cell growth). An intermediate dose close to the IC50 is often used to capture both genes that confer resistance (enriched) and sensitivity (depleted) in a single screen [1]. It is crucial to re-validate target engagement when moving a probe to a new cellular system, as protein expression and accessibility can differ [5].
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function | Example / Key Feature |
|---|---|---|
| CRISPR/Cas9 Knockout Library | Enables genome-wide screening of gene knockouts. | Designed for human cancer cells; contains sgRNAs targeting genes. |
| Chemical Probe | Selectively modulates a protein's function to study its role. | Must be selective, potent, and have a demonstrated negative control compound [5]. |
| NALM6 Cell Line | A standard cellular model for suspension cell screens. | Derived from human pre-B acute lymphoblastic leukemia; features high knockout efficiency and easy lentiviral infection [1]. |
| High-Throughput Library Prep Kit | Prepares sequencing libraries from amplified sgRNA pools. | Kits like ExpressPlex enable rapid, multiplexed preparation with minimal hands-on time and auto-normalization for consistent coverage [3]. |
| Nextflow Pipeline | Orchestrates the bioinformatics analysis of NGS data. | A workflow management system that ensures portability and reproducibility across computing environments [4]. |
From Compound to Genetic Signature
Next-generation sequencing (NGS) has revolutionized chemogenomics research, enabling comprehensive analysis of genomic variations that influence drug response. However, the journey from raw sequencing data to clinically actionable insights is fraught with technical challenges. Two primary bottlenecks dominate this landscape: persistent sequencing errors that risk confounding downstream analysis and increasing computational limitations as data volumes grow exponentially. This technical support center provides troubleshooting guidance to help researchers navigate these critical roadblocks in their pharmacogenomics workflows.
Section 1: Understanding and Correcting Sequencing Errors
Sequencing errors originate from multiple sources throughout the NGS workflow. During sample preparation, artifacts may be introduced via polymerase incorporation errors during amplification. The sequencing process itself introduces approximately 0.1-1% of errors, which are more common in reads with poor-quality bases where sequencers misinterpret signals. Additional errors accumulate during library preparation stages. These errors manifest as base substitutions, insertions, or deletions, with error profiles varying significantly across sequencing platforms. Illumina platforms typically produce approximately one error per thousand nucleotides, primarily substitutions, while third-generation technologies like Oxford Nanopore and PacBio historically had higher error rates (>5%) distributed across substitution, insertion, and deletion types [6] [7].
How can I computationally correct sequencing errors in heterogeneous datasets?
Computational error correction employs specialized algorithms to identify and fix sequencing errors. The performance of these methods varies substantially across different dataset types, with no single method performing best on all data. For highly heterogeneous datasets like T-cell receptor repertoires or viral quasispecies, the following correction methods have been benchmarked:
Table: Computational Error-Correction Methods for NGS Data [6]
| Method | Best Application Context | Key Characteristics |
|---|---|---|
| Coral | Whole genome sequencing data | Balanced precision and sensitivity |
| Bless | Various dataset types | k-mer based approach |
| Fiona | Diverse applications | Good performance across datasets |
| Pollux | Experimental datasets | Effective error correction |
| BFC | Multiple data types | Efficient computational correction |
| Lighter | Large-scale data | Fast processing capability |
| Musket | General purpose | High accuracy correction |
| Racer | Recommended replacement for HiTEC | Improved error correction |
| RECKONER | Sequencing reads | Sensitivity-focused approach |
| SGA | Assembly applications | Effective for genomic assembly |
Evaluation metrics for these tools include:
- Gain: Quantifies overall performance (1.0 = perfect correction)
- Precision: Proportion of proper corrections among all corrections performed
- Sensitivity: Proportion of fixed errors among all existing errors [6]
What experimental protocols can eliminate sequencing errors?
Unique Molecular Identifier (UMI)-based high-fidelity sequencing protocols (safe-SeqS) can eliminate sequencing errors from raw reads. This method:
- Attaches UMIs to DNA fragments prior to amplification
- Groups reads into clusters based on UMI tags after sequencing
- Generates consensus sequences within each UMI cluster
- Requires at least 80% of reads to support a nucleotide call, otherwise disregards the cluster [6]
This approach is particularly valuable for creating gold standard datasets to benchmark computational error-correction methods, especially for highly heterogeneous populations like immune repertoires and viral quasispecies [6].
Section 2: Computational and Analytical Limitations
Why has computation become a major bottleneck in NGS analysis?
Computational analysis has transformed from a negligible cost to a significant bottleneck due to several converging trends. While sequencing costs have plummeted to approximately $100-600 per genome, computational advances have not kept pace with Moore's Law. Analytical pipelines are now overwhelmed by massive data volumes from single-cell sequencing and large-scale re-analysis of public datasets. This shift means researchers must now explicitly consider trade-offs between accuracy, computational resources, storage, and infrastructure complexity that were previously insignificant when sequencing costs dominated budgets [7].
What strategies address computational bottlenecks in genomic analysis?
Several innovative approaches help mitigate computational limitations:
Data Sketching: Uses lossy approximations that sacrifice perfect fidelity to capture essential data features, providing orders-of-magnitude speedups [7]
Hardware Acceleration: Leverages FPGAs and GPUs for significant speed improvements, though requires additional hardware investment [7]
Domain-Specific Languages: Enables programmers to handle complex genomic operations more efficiently [7]
Cloud Computing: Provides flexible resource allocation, allowing researchers to make hardware choices for each analysis rather than during technology refresh cycles [7]
Table: Computational Trade-offs in NGS Analysis [7]
| Approach | Advantages | Trade-offs |
|---|---|---|
| Data Sketching | Orders of magnitude faster | Loss of perfect accuracy |
| Hardware Accelerators (FPGAs/GPUs) | Significant speed improvements | Expensive hardware requirements |
| Domain-Specific Languages | Reproducible handling of complex operations | Steep learning curve |
| Cloud Computing | Flexible resource allocation | Ongoing costs, data transfer issues |
How can I extract accurate pharmacogenotypes from clinical NGS data?
The Aldy computational method can extract pharmacogenotypes from whole genome sequencing (WGS) and whole exome sequencing (WES) data with high accuracy. Validation studies demonstrate:
- Aldy v3.3 achieved 99.5% concordance with panel-based genotyping for 14 major pharmacogenes using WGS
- Aldy v4.4 reached 99.7% concordance for WGS and similar accuracy for WES data
- The method identified additional clinically actionable star alleles not covered by targeted genotyping in CYP2B6, CYP2C19, DPYD, SLCO1B1, and NUDT15 [8]
Key challenges in clinical NGS data include low read depth, incomplete coverage of pharmacogenetically relevant loci, inability to phase variants, and difficulty resolving large-scale structural variations, particularly for CYP2D6 copy number variation [8].
Section 3: Troubleshooting Common Experimental Issues
How do I troubleshoot low library yield in NGS preparations?
Low library yield stems from several root causes with specific corrective actions:
Table: Troubleshooting Low NGS Library Yield [2]
| Root Cause | Mechanism of Yield Loss | Corrective Action |
|---|---|---|
| Poor input quality/contaminants | Enzyme inhibition from salts, phenol, or EDTA | Re-purify input sample; ensure 260/230 >1.8, 260/280 ~1.8 |
| Inaccurate quantification | Suboptimal enzyme stoichiometry | Use fluorometric methods (Qubit) instead of UV; calibrate pipettes |
| Fragmentation inefficiency | Reduced adapter ligation efficiency | Optimize fragmentation parameters; verify size distribution |
| Suboptimal adapter ligation | Poor adapter incorporation | Titrate adapter:insert ratios; ensure fresh ligase/buffer |
| Overly aggressive purification | Desired fragment loss | Optimize bead:sample ratios; avoid bead over-drying |
What are the most common sequencing preparation failures and their solutions?
Frequent sequencing preparation issues fall into distinct categories:
Sample Input/Quality Issues
- Failure signals: Low starting yield, smear in electropherogram, low library complexity
- Root causes: Degraded DNA/RNA, sample contaminants, inaccurate quantification, shearing bias
- Solutions: Re-purify input samples, use fluorometric quantification, optimize fragmentation [2]
Fragmentation/Ligation Failures
- Failure signals: Unexpected fragment size, inefficient ligation, adapter-dimer peaks
- Root causes: Over/under-shearing, improper buffer conditions, suboptimal adapter-to-insert ratio
- Solutions: Optimize fragmentation parameters, titrate adapter ratios, maintain optimal temperature [2]
Amplification/PCR Problems
- Failure signals: Overamplification artifacts, bias, high duplicate rate
- Root causes: Too many PCR cycles, inefficient polymerase, primer exhaustion
- Solutions: Reduce cycle number, use high-efficiency polymerase, optimize primer design [2]
Section 4: The Scientist's Toolkit
Research Reagent Solutions for NGS Workflows
Table: Essential Materials for NGS Experiments [6] [2] [8]
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Unique Molecular Identifiers (UMIs) | Error correction via molecular barcoding | Attached prior to amplification for high-fidelity sequencing |
| High-fidelity polymerases | Accurate DNA amplification | Reduces incorporation errors during PCR |
| Fluorometric quantification reagents | Accurate nucleic acid measurement | Superior to absorbance methods for template quantification |
| Size selection beads | Fragment purification | Critical for removing adapter dimers; optimize bead:sample ratio |
| Commercial NGS libraries | Standardized sequencing preparation | CLIA-certified options for clinical applications |
| TaqMan genotyping assays | Orthogonal variant confirmation | Validates computationally extracted pharmacogenotypes |
| KAPA Hyper prep kit | Library construction | Used in clinical WGS workflows |
Section 5: Workflow Diagrams
NGS Error Correction and Analysis Workflow
Computational Bottlenecks and Solutions Framework
Section 6: Frequently Asked Questions
How do I choose between computational error correction and UMI-based methods?
The choice depends on your research objectives and resources. Computational correction offers a practical solution for routine analyses where perfect accuracy isn't critical, with tools like Fiona and Musket providing a good balance of precision and sensitivity. UMI-based methods are preferable when creating gold standard datasets or working with highly heterogeneous populations like viral quasispecies or immune repertoires, where error-free reads are essential for downstream interpretation. For clinical applications requiring the highest accuracy, combining both approaches provides optimal results [6].
What are the key considerations for implementing NGS in clinical pharmacogenomics?
Clinical NGS implementation requires addressing several critical factors:
- Validation: Computational genotype extraction methods must demonstrate >99% accuracy compared to reference standards, as shown with Aldy for major pharmacogenes [8]
- Coverage: Ensure mean read depth >30x for all pharmacogenetically relevant variant regions [8]
- Variant Phasing: Utilize tools that can resolve haplotype phases for accurate star allele calling [8]
- Structural Variants: Implement methods capable of detecting copy number variations, particularly for challenging genes like CYP2D6 [8]
- Actionability: Focus on pharmacogenes with established clinical guidelines (CPIC) and FDA-recognized associations [9] [8]
How can I optimize computational workflows for large-scale NGS data?
Optimization strategies include:
- Performance Profiling: Identify bottlenecks in your specific analysis pipeline (alignment, variant calling, etc.)
- Tool Selection: Choose algorithms with appropriate speed-accuracy tradeoffs for your research question
- Resource Allocation: Leverage cloud computing for burst capacity and specialized hardware (FPGAs/GPUs) for repetitive tasks
- Data Management: Implement efficient storage solutions for intermediate files and final results
- Pipeline Parallelization: Design workflows to process samples independently when possible to maximize throughput [7]
Impact of Pharmacogenetic Complexity on Analysis Pipelines
Troubleshooting Guides
Pipeline Configuration & Validation
Issue: Inconsistent variant calling across different sample batches.
- Potential Cause: Inadequate pipeline validation or batch effects.
- Solution: Adhere to joint AMP/CAP recommendations for NGS bioinformatics pipeline validation [10]. Implement a rigorous quality control (QC) protocol that includes:
- Using validated reference materials with known variants for each batch.
- Regularly re-running control samples to monitor pipeline drift.
- Establishing and monitoring key performance metrics like sensitivity, specificity, and precision for variant detection [10].
Issue: High number of variants of uncertain significance (VUS) in pharmacogenes.
- Potential Cause: Standard computational prediction tools trained on pathogenic datasets perform poorly on pharmacogenes, which are under less evolutionary constraint [11].
- Solution: Utilize pharmacogenomics-specific functional prediction pipelines. This involves:
- High-Throughput Experimental Data: Incorporate data from large-scale functional assays that characterize the consequences of rare variants in genes like CYP450 family members [11].
- Specialized Computational Tools: Use tools designed for pharmacogenomic (PGx) variants, as traditional tools like SIFT and PolyPhen-2 may misclassify functionally important but non-pathogenic variants [11].
- Leverage TDM Data: Correlate genetic findings with large, retrospective therapeutic drug monitoring (TDM) datasets to validate the clinical impact of VUS [11].
Data Analysis & Interpretation
Issue: Difficulty analyzing complex gene loci (e.g., CYP2D6, HLA).
- Potential Cause: Short-read NGS platforms struggle with highly homologous regions, segmental duplications, and copy number variations (CNVs) [11].
- Solution: Implement a multi-technology approach.
- Targeted Long-Read Sequencing: Use technologies like Single-Molecule Real-Time (SMRT) sequencing or Nanopore sequencing for targeted haplotyping and accurate CNV profiling of complex loci [11].
- Specialized Bioinformatics Pipelines: Employ variant calling pipelines specifically designed and validated for these complex regions to accurately resolve star (*) alleles [11].
Issue: Algorithm fails to predict a known drug-response phenotype.
- Potential Cause: The analysis may be missing key rare or structural variants, or the model may not account for population-specific alleles [12] [11].
- Solution:
- Ensure your variant calling pipeline includes comprehensive coverage of rare variants and CNVs, as recommended by the Association for Molecular Pathology (AMP) [13].
- For dose prediction algorithms (e.g., for warfarin), verify that the model includes alleles relevant to your patient's ancestry. For example, the CYP2C9*8 allele is important for patients of African ancestry but is often missing from standard algorithms [12].
Clinical Implementation & Reporting
Issue: Challenges integrating PGx results into the Electronic Health Record (EHR) for clinical decision support.
- Potential Cause: Lack of standardized data formats for genomic information and insufficiently designed clinical decision support (CDS) tools [13].
- Solution:
- Advocate for the adoption of data and application standards for genomic information (e.g., HL7 FHIR) to improve data portability and EHR integration [13].
- Design CDS tools that are seamlessly integrated into clinician workflows and provide clear, actionable recommendations, not just raw genetic data [13].
Frequently Asked Questions (FAQs)
Q1: What are the key differences between validating a germline pipeline versus a somatic pipeline for pharmacogenomics?
A: The primary focus in PGx is on accurate germline variant calling to predict an individual's inherent drug metabolism capacity. The validation must ensure high sensitivity and specificity for a predefined set of clinically relevant PGx genes and their known variant types, including single nucleotide variants (SNVs), insertions/deletions (indels), and complex variants like hybrid CYP2D6/CYP2D7 alleles [10] [11]. Somatic pipelines, used in oncology, are optimized for detecting low-frequency tumor variants and often require different validation metrics.
Q2: Our pipeline works well for European ancestry populations but has poor performance in other groups. How can we fix this?
A: This is a common issue due to the underrepresentation of diverse populations in genomic research [13] [12]. Solutions include:
- Utilize Pan-Ethnic Allele Frequency Databases: Use reference databases like the All of Us Research Program, which has enrolled a diverse cohort, to ensure your pipeline and interpretation tools are informed by global genetic diversity [13].
- Incorporate Population-Specific Alleles: Actively curate and include alleles with higher frequency in underrepresented populations (e.g., CYP2C9*8 in African ancestry) into your genotyping panels and interpretation algorithms [12].
- Validate Pipeline Performance: Specifically validate your bioinformatics pipeline's performance across diverse ancestral backgrounds to identify and correct for biases [13].
Q3: What is the most effective way to handle the thousands of rare variants discovered by NGS in pharmacogenes?
A: Adopt a two-pronged interpretation strategy [11]:
- For characterized variants: Rely on curated knowledgebases like PharmGKB and CPIC guidelines for which there is existing clinical or functional evidence.
- For uncharacterized rare variants: Combine high-throughput experimental characterization data (when available) with computational predictions from tools specifically tuned for pharmacogenes. Correlating findings with large-scale TDM data can provide retrospective clinical validation for these variants.
Q4: How can Artificial Intelligence (AI) help overcome PGx analysis bottlenecks?
A: AI and machine learning (ML) are revolutionizing PGx by [14]:
- Improving Variant Calling: Tools like DeepVariant use deep learning to identify genetic variants with higher accuracy than traditional methods.
- Predicting Drug Response: ML models can integrate multi-omics data (genomic, transcriptomic) to predict whether a patient will be a responder or non-responder to a specific drug.
- Interpreting Complex Patterns: AI can help interpret the combined effect of multiple variants across different genes to predict complex drug response phenotypes, moving beyond single gene-drug pairs.
Experimental Protocols & Methodologies
High-Throughput Functional Characterization of PGx Variants
Purpose: To experimentally determine the functional impact of numerous rare variants in a pharmacogene (e.g., CYP2C9) discovered via NGS. Methodology:
- Variant Selection: Select missense and loss-of-function variants from NGS data with a focus on rare variants (MAF < 1%) of uncertain significance.
- Site-Directed Mutagenesis: Create plasmid constructs for each variant allele.
- Heterologous Expression: Express the variant proteins in a standardized cell system (e.g., mammalian cell lines).
- Enzyme Kinetics Assay: Measure the enzymatic activity (e.g., V~max~, K~m~) for each variant against a model substrate and compare to the wild-type enzyme.
- Data Integration: Classify variants based on functional impact (e.g., normal, decreased, or no function) and integrate this data into a curated database for clinical interpretation [11].
NGS Bioinformatics Pipeline Validation
Purpose: To establish the performance characteristics of a clinical NGS pipeline for PGx testing as per professional guidelines [10]. Methodology:
- Sample Selection: Use a validation set of samples with known variants, confirmed by an orthogonal method (e.g., Sanger sequencing). This set should include a range of variant types (SNVs, indels, CNVs) across all relevant PGx genes.
- Sequencing & Analysis: Process the validation samples through the entire NGS workflow, from library preparation to bioinformatics analysis.
- Performance Calculation: Calculate the following metrics for each variant type and each gene:
- Accuracy: (True Positives + True Negatives) / Total Samples
- Precision (Positive Predictive Value): True Positives / (True Positives + False Positives)
- Analytical Sensitivity (Recall): True Positives / (True Positives + False Negatives)
- Specificity: True Negatives / (True Negatives + False Positives)
- Establish Reportable Range: Define the minimum coverage and quality thresholds for confidently calling a variant [10].
Data Presentation
Table 1: Common Pharmacogenomic Analysis Bottlenecks and Strategic Solutions
| Bottleneck Category | Specific Challenge | Impact on Research | Proposed Solution |
|---|---|---|---|
| Variant Interpretation | High volume of rare variants & VUS [11] | Delays in determining clinical relevance; inconclusive reports. | Integrate high-throughput functional data and PGx-specific computational tools [11]. |
| Pipeline Accuracy | Inconsistent performance across complex loci (CYP2D6, HLA) [11] | Mis-assignment of star alleles; incorrect phenotype prediction. | Supplement with long-read sequencing for targeted haplotyping [11]. |
| Population Equity | Underrepresentation in reference data [13] [12] | Algorithmic bias; reduced clinical utility for non-European populations. | Utilize diverse biobanks (e.g., All of Us); include population-specific alleles in panels [13] [12]. |
| Clinical Integration | Lack of standardized EHR integration [13] | PGx data remains siloed; fails to inform point-of-care decisions. | Adopt data standards (HL7 FHIR); develop workflow-integrated CDS tools [13]. |
| Evidence Generation | Difficulty proving clinical utility [13] [12] | Sparse insurance coverage; slow adoption by clinicians. | Leverage real-world data (RWD) and therapeutic drug monitoring (TDM) for retrospective studies [11]. |
Table 2: Essential Research Reagent Solutions for PGx Studies
| Reagent / Material | Function in PGx Analysis | Key Considerations |
|---|---|---|
| Reference Standard Materials | Provides a truth set for validating NGS pipeline accuracy and reproducibility [10]. | Must include variants in key PGx genes (e.g., CYP2C19, DPYD, TPMT) and complex structural variants. |
| Targeted Long-Read Sequencing Kits | Resolves haplotypes and accurately calls variants in complex genomic regions (e.g., CYP2D6) [11]. | Higher error rate than short-reads requires specialized analysis; ideal for targeted enrichment. |
| Pan-Ethnic Genotyping Panels | Ensures inclusive detection of clinically relevant variants across diverse ancestral backgrounds [13]. | Panels must be curated with population-specific alleles (e.g., CYP2C9*8) to avoid healthcare disparities. |
| Functional Assay Kits | Provides experimental characterization of variant function for VUS resolution [11]. | Assays should be high-throughput and measure relevant pharmacokinetic parameters (e.g., enzyme activity). |
| Curated Knowledgebase Access | Provides essential, evidence-based clinical interpretations for drug-gene pairs [13]. | Reliance on frequently updated resources like PharmGKB and CPIC guidelines is critical. |
Workflow and Pathway Visualizations
PGx NGS Analysis Pipeline
Pharmacogenomic Variant Interpretation
Drug Metabolism Pathway Impact
The Challenge of Rare and Structural Variants in Drug Response
Frequently Asked Questions
Why is my PGx genotyping pipeline failing on complex pharmacogenes like CYP2D6? Complex pharmacogenes often contain high sequence homology with non-functional pseudogenes (e.g., CYP2D6 and CYP2D7) and tandem repeats, which cause misalignment of short sequencing reads [15] [16]. This leads to inaccurate variant calling and haplotype phasing. To resolve this, consider supplementing your data with long-read sequencing (e.g., PacBio or Oxford Nanopore) for the problematic loci. Long-read technologies can span repetitive regions and resolve full haplotypes, significantly improving accuracy [15].
How can I accurately determine star allele haplotypes from NGS data? Accurate haplotyping requires statistical phasing of observed small variants followed by matching to known star allele definitions [16]. Use specialized PGx genotyping tools like PyPGx, which implements a pipeline to phase single nucleotide variants and insertion-deletion variants, and then cross-references them against a haplotype translation table for the target gene. The tool combines this with a machine learning-based approach to detect copy number variations and other structural variants that define critical star alleles [16].
My variant calling workflow is running out of memory. How can I fix this?
Genes with a high density of variants or very long genes can cause memory errors during aggregation steps [17]. This can be mitigated by increasing the memory allocation for specific tasks in your workflow definition file (e.g., a WDL script). For example, you may increase the memory for first_round_merge from 20GB to 32GB, and for second_round_merge from 10GB to 48GB [17].
What is the most cost-effective sequencing strategy for comprehensive PGx profiling? The choice involves a trade-off between cost, completeness, and accuracy [7].
- Targeted Panels: Cost-effective for focused analysis of a predefined set of ADME genes but miss novel variants and complex structural variations outside the targeted regions [15].
- Whole Genome Sequencing (WGS): Provides a comprehensive view of coding and non-coding regions, capturing known and novel variants. With costs now as low as $100 per genome, WGS is an increasingly viable option for population-level PGx studies [16] [7].
- Hybrid Approach: Use short-read WGS for broad variant discovery and supplement with long-read sequencing for complex loci to resolve haplotypes accurately [15].
How do I interpret a hemizygous genotype call on an autosome? A haploid (hemizygous-like) call for a variant on an autosome (e.g., genotype '1' instead of '0/1') typically indicates that the variant is located within a heterozygous deletion on the other chromosome [17]. This is not an error but a correct representation of the genotype. You should inspect the gVCF file for evidence of a deletion call spanning the variant's position on the other allele [17].
Troubleshooting Guides
Guide 1: Resolving Structural Variants in Complex Pharmacogenes
Problem: Inaccurate detection of star alleles due to structural variants (SVs) like gene deletions, duplications, and hybrids in genes such as CYP2A6, CYP2D6, and UGT2B17.
Investigation & Solution:
- Confirm Data Quality: Check alignment (BAM) files around the gene of interest. Look for low mapping quality scores and dropped coverage, which signal alignment ambiguity in complex regions [15] [16].
- Employ SV-aware Tools: Standard variant callers often miss SVs. Use PGx-specialized tools like PyPGx, which uses a support vector machine (SVM) to detect SVs from read depth and copy number variation data [16].
- Validate with Long-Read Sequencing: If possible, use long-read sequencing (10–40 kb reads) to span repetitive regions and resolve the haplotype structure unambiguously. Studies show this method can fully resolve haplotypes for the majority of guideline pharmacogenes [15].
Guide 2: Managing Computational Bottlenecks in Population-Scale PGx Analysis
Problem: Processing whole-genome sequencing data for thousands of samples is computationally prohibitive, causing long delays.
Investigation & Solution:
- Profile Your Pipeline: Identify which steps (e.g., read alignment, variant calling, joint genotyping) consume the most time and memory [7] [18].
- Leverage Hardware Acceleration: For standard secondary analysis (alignment and variant calling), consider using hardware-accelerated solutions like the Illumina Dragen system, which can process a 30x genome in under an hour, though at a higher compute cost [7].
- Utilize Data Sketching: For specific analyses like comparative k-mer studies, use efficient "sketching" algorithms (e.g., Mash) that sacrifice perfect fidelity for massive speed-ups, enabling rapid initial surveys [7].
- Optimize Memory Allocation: As detailed in the FAQ, manually adjust memory for specific tasks in your workflow scripts to prevent crashes on large genes [17].
Table 1: Comparison of Genotyping Technologies for PGx
| Technology | Key Principle | Advantages | Limitations in PGx SV Detection |
|---|---|---|---|
| PCR/qPCR | Amplification of specific DNA sequences | Cost-effective, fast, high-throughput [15] | Limited to known, pre-defined variants; cannot detect novel SVs [15] |
| Microarrays | Hybridization to predefined oligonucleotide probes | Simultaneously genotypes hundreds to thousands of known SNVs and CNVs [15] | Cannot detect novel variants or balanced SVs (e.g., inversions); poor resolution for small CNVs [15] [19] |
| Short-Read NGS (Illumina) | Parallel sequencing of millions of short DNA fragments | Detects known and novel SNVs/indels; high accuracy [15] [7] | Struggles with phasing, large SVs, and highly homologous regions due to short read length [15] [20] |
| Long-Read NGS (PacBio, Nanopore) | Sequencing of single, long DNA molecules | Resolves complex loci, fully phases haplotypes, detects all SV types [15] | Higher raw error rates and cost per sample, though improving [7] |
Table 2: Essential Research Reagent Solutions
| Item | Function in PGx Analysis |
|---|---|
| PyPGx | A Python package for predicting PGx genotypes (star alleles) and phenotypes from NGS data. It integrates SNV, indel, and SV detection using a machine-learning model [16]. |
| PharmVar Database | The central repository for curated star allele nomenclature, providing haplotype definitions essential for accurate genotype-to-phenotype translation [16]. |
| PharmGKB | The Pharmacogenomics Knowledgebase, a resource that collects, curates, and disseminates knowledge about the impact of genetic variation on drug response [16]. |
| Burrows-Wheeler Aligner (BWA) | A widely used software package for aligning sequencing reads against a reference genome, a critical first step in most NGS analysis pipelines [15]. |
| 1000 Genomes Project (1KGP) Data | A public repository of high-coverage whole-genome sequencing data from diverse populations, serving as a critical resource for studying global PGx variation [16]. |
Experimental Protocols
Protocol 1: Population-Level Star Allele and Phenotype Calling with PyPGx
Objective: To identify star alleles and predict metabolizer phenotypes from high-coverage whole-genome sequencing data across a diverse cohort.
Methodology:
- Data Input: Obtain high-coverage WGS data (BAM/FASTQ) aligned to GRCh37 or GRCh38 [16].
- Variant Phasing: Use the PyPGx pipeline, which employs the Beagle program to statistically phase observed small variants (SNVs and indels) into two haplotypes per sample [16].
- Star Allele Matching: Cross-reference the phased haplotypes against the target gene's haplotype translation table. The pipeline selects the final star allele based on priority: allele function, number of core variants, protein impact, and reference allele status [16].
- SV Detection: Compute per-base copy number from read depth via intra-sample normalization. Detect SVs (deletions, duplications) from this data using a pre-trained support vector machine (SVM) classifier [16].
- Diplotype Assignment: Combine the candidate star alleles and SV results to make the final diplotype call (e.g.,
CYP2D6*1/*4) and translate it to a predicted phenotype (e.g., Poor Metabolizer) using database guidelines [16].
Protocol 2: Validating SVs with Long-Read Sequencing
Objective: To confirm the structure and phase of complex SVs identified in pharmacogenes by short-read WGS.
Methodology:
- Sample Selection: Select samples where short-read analysis suggests a complex or ambiguous SV (e.g., a hybrid gene or duplication with uncertain breakpoints) [15].
- Library Preparation & Sequencing: Prepare high molecular weight DNA libraries. Sequence using a long-read platform (PacBio HiFi or Oxford Nanopore) to generate reads of 10 kb or longer [15].
- Variant Calling & Phasing: Align long reads and call variants. The length of the reads will allow for direct observation of the co-occurrence of variants on a single DNA molecule, providing unambiguous haplotype phasing and precise SV breakpoint identification [15] [19].
Workflow and Process Diagrams
Analysis Workflow for PGx Variants
Technology Selection Logic
Understanding the 40 Exabyte Challenge
In the era of large-scale chemogenomics studies, the management of Next-Generation Sequencing (NGS) data has become a critical bottleneck. By 2025, an estimated 40 exabytes of storage capacity will be required to handle the global accumulation of human genomic data [21] [22]. This unprecedented volume presents significant challenges for storage, transfer, and computational analysis, particularly in drug discovery pipelines where rapid iteration is essential.
Quantifying the NGS Data Challenge
| Data Metric | Scale & Impact |
|---|---|
| Global Genomic Data Volume (2025) | 40 Exabytes (EB) [21] [22] |
| NGS Data Storage Market (2024) | USD 1.6 Billion [23] |
| Projected Market Size (2034) | USD 8.5 Billion [23] |
| Market Growth Rate (CAGR) | 18.6% [23] |
| Primary Data Type | Short-read sequencing data dominates the market [23] |
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: What are the primary factors contributing to the massive data volumes in NGS-based chemogenomics?
The 40 exabyte challenge stems from multiple, concurrent advances in sequencing technology and its application:
- Throughput of Modern Sequencers: Platforms like Illumina's NovaSeq X generate terabytes of data per run, enabling large-scale projects but creating immediate storage pressures [24].
- Shift to Multiomic Analyses: Modern chemogenomics does not rely on genomics alone. Integrating epigenomic (e.g., methylation), transcriptomic (RNA expression), and proteomic data from the same sample multiplies the data volume and complexity for a more comprehensive view of drug response [25] [26] [24].
- Population-Scale Studies: Initiatives like the UK Biobank and the Alliance for Genomic Discovery are sequencing hundreds of thousands of genomes to discover therapeutic targets, generating petabytes of raw data [25].
- Advanced Applications: Techniques like single-cell sequencing and spatial transcriptomics, which profile gene expression at the individual cell level within a tissue context, are exceptionally data-intensive but critical for understanding tumor heterogeneity and drug resistance [25] [24].
FAQ 2: Our lab is experiencing severe bottlenecks in transferring and sharing large NGS datasets. What are the best solutions?
Data transfer is a common physical bottleneck. The following strategies and tools can help mitigate this issue:
- Implement Data Compression: Use specialized tools like
CRAMfor raw sequencing data (which offers better compression than BAM) andBGZFfor compressed, indexed genomic files to minimize the physical size of datasets for transfer. - Leverage Cloud-Based Platforms: Utilize secure, cloud-based bioinformatics platforms like DNAnexus, Terra, or Illumina BaseSpace [26] [24]. These platforms allow collaborators to access and analyze data in a centralized location, eliminating the need for repeated large-scale transfers. They comply with security frameworks like HIPAA and GDPR, ensuring data privacy [24].
- Aspera or Similar High-Speed Transfer Protocols: For moving data to and from the cloud, use high-speed transfer protocols that bypass the inherent latency of standard TCP/IP, significantly accelerating upload/download times.
FAQ 3: How can we ensure the quality and integrity of our NGS data when dealing with such large datasets?
Maintaining data quality at scale requires a robust Quality Management System (QMS). The Next-Generation Sequencing Quality Initiative (NGS QI) provides essential tools for this purpose [27].
- Use NGS QI Resources: Implement the NGS QMS Assessment Tool and the Identifying and Monitoring NGS Key Performance Indicators (KPIs) SOP to establish a framework for continuous quality monitoring [27].
- Establish Key Performance Indicators (KPIs): Track metrics like read depth (coverage), base call quality scores (Q-score), alignment rates, and duplication rates for every run. A sudden shift in these KPIs can indicate issues with library preparation, the sequencer, or the analysis pipeline [27].
- Validate and Lock Down Workflows: Once an NGS method is validated for a specific chemogenomics assay, it is crucial to "lock down" the entire workflow—from library prep to bioinformatics analysis—to ensure reproducibility. Any change (e.g., new reagent lot, software update) requires careful revalidation [27].
FAQ 4: What computational strategies are most effective for analyzing large-scale chemogenomics data?
Traditional computing methods often fail at this scale. The key is to leverage scalable, automated, and intelligent solutions.
- Adopt AI/ML for Variant Calling: Replace traditional heuristic methods with AI-powered tools like DeepVariant, which uses deep learning to identify genetic mutations with superior accuracy, reducing false positives and manual review time [26] [24].
- Utilize Cloud and High-Performance Computing (HPC): Cloud platforms (AWS, Google Cloud, Microsoft Azure) offer scalable computational power on demand. They are essential for running resource-intensive tasks like genome-wide association studies (GWAS) and multi-omics integration without local infrastructure bottlenecks [24].
- Automate Bioinformatics Pipelines: Use workflow management systems (e.g., Nextflow, Snakemake) to create reproducible, scalable, and portable analysis pipelines. This automates the data flow from raw fastq files to final variant calls, minimizing manual intervention and human error [28].
FAQ 5: How can our research group cost-effectively store and manage 40 exabytes of data?
The economic burden of data storage is significant. A strategic approach is required.
- Evaluate Hybrid Storage Models: A combination of on-premises storage for active projects and low-cost cloud storage (e.g., Amazon S3 Glacier, Google Cloud Coldline) for archiving infrequently accessed data can be highly cost-effective [29].
- Implement Data Lifecycle Policies: Not all data needs to be kept forever. Establish clear policies that define which data must be retained (e.g., final variant calls, analysis-ready BAMs) and which can be deleted (e.g., raw intermediate files) after a defined period and project completion.
- Leverage Vendor Solutions: Explore vendors specializing in NGS data storage, such as Qumulo for scalable file storage or DNAnexus and Illumina for integrated analysis platforms that manage storage and computation together [29] [23].
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item / Solution | Function in NGS Workflow |
|---|---|
| Illumina NovaSeq X Series | High-throughput sequencing platform for generating whole-genome data at a massive scale, foundational for large chemogenomics screens [24]. |
| Oxford Nanopore Technologies | Provides long-read sequencing capabilities, crucial for resolving complex genomic regions, detecting structural variations, and direct RNA/epigenetic modification detection [27] [24]. |
| DNAnexus/Terra Platform | Cloud-based bioinformatics platforms that provide secure, scalable environments for storing, sharing, and analyzing NGS data without advanced computational expertise [26] [22]. |
| DeepVariant | An AI-powered tool that uses a deep neural network to call genetic variants from NGS data, dramatically improving accuracy over traditional methods [26] [24]. |
| NGS QI Validation Plan SOP | A standardized template from the NGS Quality Initiative for planning and documenting assay validation, ensuring data quality and regulatory compliance (e.g., CLIA) [27]. |
| CRISPR Design Tools (e.g., Synthego) | AI-powered platforms for designing and validating CRISPR guides in functional genomics screens to identify drug targets [26]. |
| Nextflow | Workflow management software that enables the creation of portable, reproducible, and scalable bioinformatics pipelines, automating data analysis from raw data to results [28]. |
Advanced Analytical Frameworks: AI and Machine Learning Solutions for Chemogenomics Data
Technical Foundation: Understanding AI-Based Variant Calling
Variant calling is a fundamental step in genomic analysis that involves the identification of genetic variations, such as single nucleotide polymorphisms (SNPs), insertions/deletions (InDels), and structural variants, from high-throughput sequencing data [30]. Artificial Intelligence (AI), particularly deep learning (DL), has revolutionized this field by introducing tools that offer higher accuracy, efficiency, and scalability compared to traditional statistical methods [30].
Performance Comparison of AI-Powered Variant Callers
The table below summarizes the key characteristics of prominent AI-based variant calling tools.
| Tool Name | Primary AI Methodology | Key Strengths | Common Sequencing Data Applications | Notable Limitations |
|---|---|---|---|---|
| DeepVariant [30] [31] | Deep Convolutional Neural Networks (CNNs) | High accuracy; automatically produces filtered variants; supports multiple technologies [30]. | Short-read, PacBio HiFi, Oxford Nanopore [30] | High computational cost [30] |
| DeepTrio [30] | Deep CNNs | Enhances accuracy for family trios; improved performance in challenging genomic regions [30]. | Short-read, various technologies [30] | Designed for trio analysis, not single samples [30] |
| DNAscope [30] | Machine Learning (ML) | High computational speed and accuracy; reduced memory overhead [30]. | Short-read, PacBio HiFi, Oxford Nanopore [30] | Does not leverage deep learning architectures [30] |
| Clair/Clair3 [30] [31] | Deep CNNs | High speed and accuracy, especially at lower coverages; optimized for long-read data [30] [31]. | Short-read and long-read data [30] | Predecessor (Clairvoyante) was inaccurate with multi-allelic variants [30] |
| Medaka [30] | Neural Networks | Designed for accurate variant calling from Oxford Nanopore long-read data [30]. | Oxford Nanopore [30] | Specialized for one technology (ONT) [30] |
| NeuSomatic [31] | Convolutional Neural Networks (CNNs) | Specialized for detecting somatic mutations in heterogeneous cancer samples [31]. | Tumor and normal paired samples [31] | Focused on somatic, not germline, variants [31] |
Troubleshooting Guides and FAQs
FAQ 1: What are the key differences between traditional and AI-powered variant callers, and why should I switch?
Answer: Traditional variant callers rely on statistical and probabilistic models that use hand-crafted rules to distinguish true variants from sequencing errors [31]. In contrast, AI-powered tools use deep learning models trained on large genomic datasets to automatically learn complex patterns and subtle features associated with real variants [30]. This data-driven approach typically results in superior accuracy, higher reproducibility, and a significant reduction in false positives, especially in complex genomic regions where conventional methods often struggle [30] [31]. The switch is justified when your research demands higher precision, such as in clinical diagnostics or the identification of low-frequency somatic mutations in cancer [31] [32].
FAQ 2: My AI variant caller is extremely slow and resource-intensive. How can I improve its performance?
Answer: High computational demand is a common bottleneck, particularly with deep learning models. To mitigate this:
- Check Hardware Compatibility: Ensure you are using a GPU-equipped system. While some tools like DeepVariant can run on a CPU, a GPU drastically accelerates computation [30]. Note that some efficient tools, like DNAscope, are optimized for multi-threaded CPU processing and do not require a GPU [30].
- Optimize Input Data: For tools like DeepVariant that use pileup images, verify that the input region is not excessively large. Consider processing the genome in smaller, parallelized chunks if supported by the workflow.
- Evaluate Alternatives: If runtime is critical, benchmark alternative tools. For instance, DNAscope and Clair3 are noted for their computational efficiency and faster runtimes compared to other deep learning methods [30].
FAQ 3: I am working with long-read sequencing data (Oxford Nanopore/PacBio). Which AI caller is most suitable?
Answer: Long-read technologies have specific error profiles that require specialized tools. The most recommended AI-based callers for long-read data are:
- Clair3: Specifically designed for long-read data, it integrates pileup and full-alignment information to achieve high speed and accuracy, even at lower coverages [30] [31].
- Medaka: Developed by Oxford Nanopore, it employs neural networks to perform haploid-aware variant calling, accounting for the inherent error rates of ONT sequencing [30].
- DeepVariant: Its ongoing development includes support for both PacBio HiFi and Oxford Nanopore data, maintaining high accuracy across platforms [30].
- PEPPER-Margin-DeepVariant: A comprehensive pipeline that combines AI-powered components for long-read data, addressing challenges in structural variant detection [31].
FAQ 4: How do I handle variant calling for family-based or cancer somatic mutation studies?
Answer: The study design dictates the choice of the variant caller.
- For Family Trios (e.g., child and parents): Use DeepTrio. It is an extension of DeepVariant that jointly analyzes sequencing data from all three family members. This familial context allows it to better distinguish sequencing errors from true de novo mutations, significantly enhancing accuracy [30].
- For Somatic Mutations in Cancer: Use a tool specifically designed for somatic calling, such as NeuSomatic. These tools use CNN architectures trained to detect low variant allele frequencies in a background of tumor heterogeneity, which is a common challenge in cancer genomics [31].
FAQ 5: What is the role of Transformer models in variant calling and NGS analysis?
Answer: While many established variant callers are based on CNNs, Transformer models represent the next wave of AI innovation in genomics. Drawing parallels between biological sequences and natural language, Transformers are now being applied to critical tasks in the NGS pipeline [33] [34]. Their powerful self-attention mechanism allows them to understand long-range contextual relationships within DNA or protein sequences. In genomics, Transformers are currently making a significant impact in:
- Neoantigen Detection: Predicting how peptides (potential neoantigens) bind to the Major Histocompatibility Complex (MHC), a crucial step for developing personalized cancer vaccines [33].
- Basecalling: Tools like Bonito and Dorado from Oxford Nanopore are beginning to use transformer architectures to improve the accuracy of converting raw electrical signals into nucleotide sequences [26] [31].
- Nucleotide Sequence Analysis: More broadly, Transformer-based language models are being adapted for a wide range of tasks in bioinformatics, including the analysis of DNA and RNA sequences [34].
Detailed Experimental Protocols
Protocol 1: Germline Variant Calling with DeepVariant
This protocol outlines the steps for identifying germline SNPs and small InDels from whole-genome sequencing data using the DeepVariant pipeline [30].
1. Input Preparation:
- Input File: A coordinate-sorted BAM file containing reads aligned to a reference genome. The BAM file should be generated following standard preprocessing steps (quality control, adapter trimming, alignment, and duplicate marking) [32].
- Reference Genome: The same reference genome (in FASTA format) used for read alignment.
2. Variant Calling Execution:
- Run the DeepVariant command, specifying the input BAM, reference genome, and output directory.
- DeepVariant will process the aligned reads, creating "pileup images" of the data. These images represent the sequencing data at each potential variant site.
- The pre-trained deep convolutional neural network (CNN) then analyzes these images to distinguish true genetic variants from sequencing artifacts [30].
3. Output and Filtering:
- Output File: The primary output is a VCF (Variant Call Format) file containing the identified variants and their genotypes.
- A key strength of DeepVariant is that it outputs high-quality, filtered calls directly, often eliminating the need for additional hard-filtering steps that are common with traditional callers [30].
Protocol 2: Somatic Variant Calling with an AI-Based Workflow
This protocol describes a workflow for identifying somatic mutations from paired tumor-normal samples, which is essential in cancer genomics [31] [32].
1. Sample and Input Preparation:
- Sample Pairs: Obtain matched BAM files from a tumor tissue sample and a normal (e.g., blood) sample from the same patient.
- Data Preprocessing: Ensure both BAM files have undergone identical and rigorous preprocessing, including local realignment and base quality score recalibration (BQSR), as per best practices (e.g., GATK Best Practices) [32].
2. Somatic Variant Calling:
- Use a specialized somatic caller like NeuSomatic.
- Provide the tool with the paired tumor and normal BAM files. The model, often a CNN, is trained to identify the subtle signals of somatic mutations against the complex background of tumor heterogeneity and sequencing noise [31].
3. Output and Annotation:
- The output is a VCF file containing the somatic variants.
- Prioritization: Annotate the VCF file using databases (e.g., dbSNP, ClinVar) to filter common polymorphisms and identify variants with potential clinical or functional impact [32]. This is critical for narrowing down candidate driver mutations in chemogenomics research.
Workflow Visualization
AI Variant Calling in Chemogenomics
NGS Data to Variant Discovery
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and tools required for implementing AI-powered variant calling in a research pipeline.
| Item Name | Function/Brief Explanation | Example Tools/Formats |
|---|---|---|
| High-Quality NGS Library | The starting material for sequencing. Library preparation quality directly impacts variant calling accuracy [35]. | Kits for DNA/RNA extraction, fragmentation, and adapter ligation. |
| Sequencing Platform | Generates the raw sequencing data. Platform choice (e.g., Illumina, ONT, PacBio) influences the selection of the optimal AI caller [30] [36]. | Illumina, Oxford Nanopore, PacBio systems. |
| Computational Infrastructure | Essential for running computationally intensive AI models. A GPU significantly accelerates deep learning inference [30]. | High-performance servers with GPUs. |
| Reference Genome | A standardized genomic sequence used as a baseline for aligning reads and calling variants [32]. | FASTA files (e.g., GRCh38/hg38). |
| Aligned Read File (BAM) | The standard input file for variant callers. Contains sequencing reads mapped to the reference genome [32]. | BAM or CRAM file format. |
| AI Variant Calling Software | The core tool that uses a trained model to identify genetic variants from the aligned reads. | DeepVariant, Clair3, DNAscope, NeuSomatic [30] [31]. |
| Variant Call Format (VCF) File | The standard output file containing the list of identified genetic variants, their genotypes, and quality metrics [30] [32]. | VCF file format. |
| Annotation Databases | Used to add biological and clinical context to raw variant calls, helping prioritize variants for further study [32]. | dbSNP, ClinVar, COSMIC, gnomAD. |
Overcoming Rare Variant Interpretation with Computational Prediction Tools
Technical Support Center
Troubleshooting Guides
Issue 1: Low Diagnostic Yield in Rare Disease Analysis
- Problem: Exome or genome sequencing of a rare disease patient has been completed, but no clinically relevant variants were identified in known disease-associated genes.
- Diagnosis: The analysis likely failed to correctly prioritize a rare, pathogenic missense variant. This is a common bottleneck, as affected individuals often carry multiple variations in disease-associated genes, with only a fraction being truly pathogenic [37].
- Solution:
- Re-analyze with updated databases: The sheer re-analysis of exomic data after 1–3 years, updating major disease variant and disease-gene association databases, is reported to increase diagnosed cases by over 10% [37].
- Reanalyze in collaboration with the clinician: A further improvement in yields could be obtained by reanalyzing the data with the clinical context provided by the diagnosing physician [37].
- Employ a high-performing predictor: Use a top-tier computational variant effect predictor like AlphaMissense to re-score all rare missense variants. Recent unbiased benchmarking in population cohorts has shown it outperforms many other tools in correlating rare variants with human traits [38].
Issue 2: High Computational Cost and Slow Analysis Times
- Problem: Secondary analysis of whole-genome sequencing data (alignment, variant calling) is taking too long, becoming a significant bottleneck and cost center.
- Diagnosis: Traditional analytical pipelines can be overwhelmed by the massive amount of data produced by modern sequencers. With sequencing costs falling, computation is now a considerable part of the total cost [7].
- Solution:
- Evaluate trade-offs: Consider the trade-offs between accuracy, compute time, and infrastructure complexity [7].
- Utilize hardware acceleration: Leverage hardware-accelerated solutions (e.g., Illumina Dragen on cloud platforms like AWS) which can reduce analysis time from tens of hours to under an hour, though at a higher compute cost [7].
- Consider targeted analysis: For specific clinical questions, a more targeted analysis (e.g., looking for specific marker genes) using faster, alignment-free methods might be sufficient, trading some accuracy for speed [7].
Issue 3: Adapter Contamination in Sequencing Data
- Problem: Sequencing run returns data with abnormal adapter dimer signals, impacting data quality and variant calling accuracy.
- Diagnosis: Inefficient ligation or an imbalance in the adapter-to-insert molar ratio during library preparation, leading to adapter-dimers being sequenced [2].
- Solution:
- Bioinformatic trimming: Reanalyze the run with the correct barcode settings selected (e.g., "RNABarcodeNone") to automatically trim the adapter sequence from the reads [39].
- Wet-lab optimization: For future runs, titrate the adapter-to-insert ratio to find the optimal balance. Excess adapters promote adapter dimers, while too few reduce ligation yield [2]. Ensure thorough purification and size selection to remove small fragments.
Frequently Asked Questions (FAQs)
Q: After initial analysis fails, what is the most effective first step to identify a causative variant? A: The most effective first step is the periodic re-analysis of sequencing data. Re-analyzing exome data after updating disease and variant databases can increase diagnostic yields by over 10%. Collaboration with the diagnosing clinician to incorporate updated clinical findings further enhances this process [37].
Q: Which computational variant effect predictor should I use for rare missense variants? A: Based on recent unbiased benchmarking using population cohorts like the UK Biobank and All of Us, AlphaMissense was the top-performing predictor, outperforming 23 other tools in inferring human traits from rare missense variants [38]. It was either the best or tied for the best predictor in 132 out of 140 gene-trait combinations evaluated [38].
Q: My NGS library yield is unexpectedly low. What are the primary causes? A: The primary causes and their fixes are summarized in the table below [2]:
| Cause | Mechanism of Yield Loss | Corrective Action |
|---|---|---|
| Poor Input Quality | Enzyme inhibition from contaminants (phenol, salts). | Re-purify input sample; ensure high purity (260/230 > 1.8). |
| Quantification Errors | Overestimating usable material. | Use fluorometric methods (Qubit) over UV absorbance (NanoDrop). |
| Fragmentation Issues | Over- or under-fragmentation reduces ligation efficiency. | Optimize fragmentation time/energy; verify fragment distribution. |
| Suboptimal Ligation | Poor ligase performance or wrong adapter:insert ratio. | Titrate adapter ratios; ensure fresh ligase/buffer. |
Q: What amount of sequencing data is recommended for Hi-C genome scaffolding? A: For genome scaffolding using Hi-C data (e.g., with the Proximo platform), the recommended amount of sequencing data (2x75 bp or longer) is [40]:
- Genome size <400 Mb: 100 million read-pairs
- Genome size 400 Mb – 1.5 Gb: 150 million read-pairs
- Genome size 1.5 Gb – 3 Gb: 250 million read-pairs For larger genomes or assemblies with low contiguity, scale accordingly.
Experimental Protocols
Protocol: Benchmarking Variant Effect Predictors using a Population Cohort
This protocol outlines a method for the unbiased evaluation of computational variant effect predictors, avoiding the circularity and bias that can limit traditional benchmarks that use clinically classified variants [38].
Cohort and Gene-Trait Set Curation:
- Assemble a set of established gene-trait combinations from rare-variant burden association studies (e.g., from published literature or biobank studies).
- Obtain whole-exome or whole-genome sequencing data and corresponding phenotype data for a large population cohort (e.g., UK Biobank, All of Us) that was not used in the training of the predictors being evaluated.
Variant Extraction and Filtering:
- Extract all missense variants for the trait-associated genes from the cohort data.
- Filter variants to include only those with a minor allele frequency (MAF) < 0.1% to focus on rare variants with potentially larger phenotypic effects.
Computational Prediction:
- Collect predicted functional scores for all extracted missense variants from the computational predictors being benchmarked (e.g., AlphaMissense, CADD, ESM1-v, etc.).
Performance Measurement:
- For each gene-trait combination, evaluate the correlation between the summed predicted variant scores for each participant and their trait value.
- For binary traits (e.g., medication use), calculate the Area Under the Balanced Precision-Recall Curve (AUBPRC).
- For quantitative traits (e.g., LDL cholesterol levels), calculate the Pearson Correlation Coefficient (PCC).
- Use bootstrap resampling (e.g., 10,000 iterations) to estimate the uncertainty (mean and 95% CI) for each performance measure.
Statistical Comparison:
- Perform pairwise statistical comparisons between predictors across all gene-trait combinations using a Wilcoxon signed-rank test, adjusting for false discovery rate (FDR) with Storey's q-value. A predictor is considered superior if the FDR < 10% [38].
Workflow and Relationship Diagrams
Rare Variant Analysis Workflow
Predictor Benchmarking Logic
Research Reagent Solutions
Essential computational tools and resources for rare variant interpretation in chemogenomics research.
| Tool/Resource Name | Function/Brief Explanation | Application Context |
|---|---|---|
| AlphaMissense | A computational variant effect predictor that outperforms others in inferring human traits from rare missense variants in unbiased benchmarks [38]. | Prioritizing pathogenic missense variants in patient cohorts. |
| Human Phenotype Ontology (HPO) | A standardized vocabulary of phenotypic abnormalities, structured as a directed acyclic graph, containing over 13,000 terms for describing patient phenotypes [37]. | Standardizing phenotype data for genotype-phenotype association studies. |
| Paraphase | A computational tool for haplotype-resolved variant calling in homologous genes (e.g., SMN1/SMN2) from both WGS and targeted sequencing data [41]. | Analyzing genes with high sequence homology or pseudogenes. |
| pbsv | A suite of tools for calling and analyzing structural variants (SVs) in diploid genomes from HiFi long-read sequencing data [41]. | Comprehensive detection of SVs, which are often involved in rare diseases. |
| Online Mendelian Inheritance in Man (OMIM) | A comprehensive, authoritative knowledgebase of human genes and genetic phenotypes, freely available and updated daily [37]. | Curating background knowledge on gene-disease relationships. |
| Prokrustean graph | A data structure that allows rapid iteration through all k-mer sizes from a sequencing dataset, drastically reducing computation time for k-mer-based analyses [42]. | Optimizing k-mer-based applications like metagenomic profiling or genome assembly. |
Integrating Multi-Omics Data for Comprehensive Drug Response Profiling
Integrating multi-omics data is imperative for studying complex biological processes holistically. This approach combines data from various molecular levels—such as genome, epigenome, transcriptome, proteome, and metabolome—to highlight interrelationships between biomolecules and their functions. In chemogenomics research, this integration helps bridge the gap from genotype to phenotype, providing a more comprehensive understanding of how tumors respond to therapeutic interventions. The advent of high-throughput techniques has made multi-omics data increasingly available, leading to the development of sophisticated tools and methods for data integration that significantly enhance drug response prediction accuracy and provide deeper insights into the biological mechanisms underlying treatment efficacy [43].
Analysis of multi-omics data alongside clinical information has taken a front seat in deriving useful insights into cellular functions, particularly in oncology. For instance, integrative approaches have demonstrated superior performance over single-omics analyses in identifying driver genes, understanding molecular perturbations in cancers, and discovering novel biomarkers. These advancements are crucial for addressing the challenges of tumor heterogeneity, which often reduces the efficacy of anticancer pharmacological therapy and results in clinical variability in patient responses [43] [44]. Multi-omics integration provides an additional perspective on biological systems, enabling researchers to develop more accurate predictive models for drug sensitivity and resistance.
Technical Support & Troubleshooting Hub
Frequently Asked Questions (FAQs)
Q: Why should I integrate multi-omics data instead of relying on single-omics analysis for drug response prediction? A: Integrated multi-omics approaches provide a more holistic view of biological systems by revealing interactions between different molecular layers. Studies have consistently shown that combining omics datasets yields better understanding and clearer pictures of the system under study. For example, integrating proteomics data with genomic and transcriptomic data has helped prioritize driver genes in colon and rectal cancers, while combining metabolomics and transcriptomics has revealed molecular perturbations underlying prostate cancer. Multi-omics integration can significantly improve the prognostic and predictive accuracy of disease phenotypes, ultimately aiding in better treatment strategies [43].
Q: What are the primary technical challenges in preparing sequencing libraries for multi-omics studies? A: The most common challenges fall into four main categories: (1) Sample input and quality issues including degraded nucleic acids or contaminants that inhibit enzymes; (2) Fragmentation and ligation failures leading to unexpected fragment sizes or adapter-dimer formation; (3) Amplification problems such as overcycling artifacts or polymerase inhibition; and (4) Purification and cleanup errors causing incomplete removal of small fragments or significant sample loss. These issues can result in poor library complexity, biased representation, or complete experimental failure [2].
Q: Which computational approaches show promise for integrating heterogeneous multi-omics data? A: Gene-centric multi-channel (GCMC) architectures that transform multi-omics profiles into three-dimensional tensors with an additional dimension for omics types have demonstrated excellent performance. These approaches use convolutional encoders to capture multi-omics profiles for each gene, yielding gene-centric features for predicting drug responses. Additionally, multi-layer network theory and artificial intelligence methods are increasingly being applied to dissect complex multi-omics datasets, though these approaches require large, systematic datasets to be most effective [44] [45].
Q: What public data repositories are available for accessing multi-omics data? A: Several rich resources exist, including:
- The Cancer Genome Atlas (TCGA): One of the largest collections of multi-omics data for over 33 cancer types.
- International Cancer Genomics Consortium (ICGC): Coordinates large-scale genome studies from 76 cancer projects.
- Cancer Cell Line Encyclopedia (CCLE): Contains gene expression, copy number, and sequencing data from 947 human cancer cell lines.
- Clinical Proteomic Tumor Analysis Consortium (CPTAC): Hosts proteomics data corresponding to TCGA cohorts.
- Omics Discovery Index: A consolidated resource providing datasets from 11 repositories in a uniform framework [43].
Troubleshooting Guide: NGS Library Preparation
Table: Common NGS Library Preparation Issues and Solutions
| Problem Category | Typical Failure Signals | Common Root Causes | Corrective Actions |
|---|---|---|---|
| Sample Input/Quality | Low starting yield; smear in electropherogram; low library complexity | Degraded DNA/RNA; sample contaminants (phenol, salts); inaccurate quantification | Re-purify input sample; use fluorometric quantification (Qubit) instead of UV only; ensure high purity (260/230 > 1.8) [2] |
| Fragmentation & Ligation | Unexpected fragment size; inefficient ligation; adapter-dimer peaks | Over- or under-shearing; improper buffer conditions; suboptimal adapter-to-insert ratio | Optimize fragmentation parameters; titrate adapter:insert molar ratios; ensure fresh ligase and optimal temperature [2] |
| Amplification/PCR | Overamplification artifacts; bias; high duplicate rate | Too many PCR cycles; inefficient polymerase; primer exhaustion | Reduce cycle number; use high-fidelity polymerases; optimize primer design and concentration [2] |
| Purification & Cleanup | Incomplete removal of small fragments; sample loss; carryover of salts | Wrong bead ratio; bead over-drying; inefficient washing; pipetting error | Calibrate bead:sample ratios; avoid over-drying beads; implement pipette calibration [2] |
Case Study: Troubleshooting Sporadic Failures in a Core Facility A core laboratory performing manual NGS preparations encountered inconsistent failures across different operators. The issues included samples with no measurable library or strong adapter/primer peaks. Root cause analysis identified deviations in protocol execution, particularly in mixing methods, timing differences between operators, and degradation of ethanol wash solutions. The implementation of standardized operating procedures with highlighted critical steps, master mixes to reduce pipetting errors, operator checklists, and temporary "waste plates" to catch accidental discards significantly reduced failure frequency and improved consistency [2].
Diagnostic Strategy Flow: When encountering NGS preparation problems, follow this systematic approach:
- Examine electropherograms for sharp 70-90 bp peaks (indicating adapter dimers) or abnormal size distributions.
- Cross-validate quantification using both fluorometric (Qubit) and qPCR methods rather than relying solely on absorbance measurements.
- Trace backwards through each preparation step—if ligation failed, examine fragmentation and input quality.
- Run appropriate controls to detect contamination or reagent issues.
- Review protocol details including reagent logs, kit lots, enzyme expiry dates, and equipment calibration records [2].
Experimental Protocols & Methodologies
Gene-Centric Multi-Channel (GCMC) Integration Protocol
Objective: To integrate multi-omics profiles for enhanced cancer drug response prediction using a gene-centric deep learning approach.
Background: Tumor heterogeneity reduces the efficacy of anticancer therapies, creating variability in patient treatment responses. The GCMC methodology addresses this by transforming multi-omics data into a structured format that captures gene-specific information across multiple molecular layers, enabling more accurate drug response predictions [44].
Table: Research Reagent Solutions for Multi-Omics Integration
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| TCGA Multi-omics Data | Provides genomic, transcriptomic, epigenomic, and proteomic profiles | Use controlled access data for 33+ cancer types; ensure proper data use agreements [43] |
| CCLE Pharmacological Profiles | Drug sensitivity data for 479 cancer cell lines | Screen against 24 anticancer drugs; correlate with multi-omics features [43] |
| CPTAC Proteomics Data | Protein-level information corresponding to TCGA samples | Integrate with genomic data to identify functional protein alterations [43] |
| GCMC Computational Framework | Deep learning architecture for multi-omics integration | Transform data to 3D tensors; implement convolutional encoders per gene [44] |
Methodology:
- Data Acquisition and Preprocessing:
- Collect multi-omics data (genomic, transcriptomic, epigenomic, proteomic) from relevant sources such as TCGA, GDSC, or in-house experiments.
- Perform quality control, normalization, and batch effect correction for each omics dataset separately.
- Align all omics data to a common gene-centric coordinate system.
Tensor Construction:
- Transform the preprocessed multi-omics profiles into a three-dimensional tensor structure with dimensions: [Genes × Features × Omics Types].
- Include an additional dimension to represent different omics types, creating a multi-channel input structure.
Model Architecture and Training:
- Implement convolutional encoders to capture patterns within each gene's multi-omics profile.
- Design the network to process each gene independently initially, then integrate information across genes in later layers.
- Train the model using drug response data (IC50 values, AUC measurements, or binary sensitivity indicators) as the target variable.
- Employ appropriate regularization techniques to prevent overfitting, given the high-dimensional nature of multi-omics data.
Validation and Interpretation:
- Evaluate model performance using cross-validation and independent test sets from different sources (e.g., TCGA patients, PDX models).
- Analyze feature importance to identify which omics types and specific genes contribute most to predictions for different drug classes.
- Validate biological insights through experimental follow-up or comparison with known mechanisms of action [44].
Validation Results: The GCMC approach has demonstrated superior performance compared to single-omics models and other integration methods. In comprehensive evaluations, it achieved better performance than baseline models for more than 75% of 265 drugs from the GDSC cell line dataset. Furthermore, it showed excellent clinical applicability, achieving the best performance on TCGA and patient-derived xenograft (PDX) datasets in terms of both area under the precision-recall curve (AUPR) and area under the receiver operating characteristic curve (AUC) [44].
Workflow Visualization: Multi-Omics Drug Response Profiling
Multi-Omics Drug Response Profiling Workflow
Cross-Omics Integration Analysis Protocol
Objective: To identify interactions between different molecular layers that influence drug response.
Methodology:
- Data Generation:
- Generate or acquire matched multi-omics data from the same samples, ensuring at least partial overlap between omics datasets.
- Include appropriate controls and replicates to account for technical variability.
Multi-Layer Network Construction:
- Build individual networks for each omics type (e.g., co-expression networks, protein-protein interaction networks).
- Create cross-omics edges based on known biological relationships (e.g., gene-protein, protein-metabolite interactions).
- Use statistical methods to identify significant correlations between different molecular layers.
Integrative Analysis:
- Apply multi-omics clustering algorithms to identify molecular subtypes that may respond differentially to treatments.
- Use pathway enrichment analysis across omics layers to identify activated or suppressed biological processes.
- Integrate with drug response data to identify multi-omics signatures predictive of sensitivity or resistance [43] [45].
Interpretation Guidelines:
- Prioritize consistent patterns across multiple omics layers over single-omics findings.
- Validate identified pathways using experimental approaches such as chemical biology techniques.
- Consider the biological context and known mechanisms of drug action when interpreting results.
- Account for the different coverage and precision levels of each omics technology [45].
Advanced Integrative Approaches
Multi-Layer Network Analysis for Biological Insight
Biological mechanisms typically operate across multiple biomolecule types rather than being confined to a single omics layer. Multi-layer network approaches provide a powerful framework for representing and analyzing these complex interactions. These methods integrate information from genome, transcriptome, proteome, metabolome, and ionome to create a more comprehensive understanding of cellular responses to therapeutic interventions [45].
Table: Characteristics of Different Omics Technologies
| Omics Layer | Coverage | Quantitative Precision | Key Challenges |
|---|---|---|---|
| Genomics | High | High | Static information; limited functional insights |
| Transcriptomics | High | Medium-High | Does not directly reflect protein abundance |
| Proteomics | Medium | Medium | Low throughput; complex post-translational modifications |
| Metabolomics | Low-Medium | Variable | Extreme chemical diversity; rapid turnover |
| Ionomics | High | High | Biologically complex interpretation |
The complexity of biological systems presents significant challenges for multi-omics integration. The genome, while being effectively digital and relatively straightforward to sequence, provides primarily static information. The transcriptome offers dynamic functional information but may not accurately reflect protein abundance. The proteome exhibits massive complexity due to post-translational modifications, cellular localization, and protein-protein interactions. The metabolome represents a phenotypic readout but features enormous chemical diversity. The ionome reflects the convergence of physiological changes across all layers but can be challenging to interpret biologically [45].
Chemical Biology Approaches for Validation
Chemical biology techniques provide powerful methods for validating multi-omics findings. For example, photo-cross-linking-based chemical approaches can be used to examine enzymes that recognize specific post-translational modifications. These methods involve designing chemical probes that incorporate photoreactive amino acids to capture enzymes that recognize specific modifications, converting transient protein-protein interactions into irreversible covalent linkages [46].
One successful application of this approach identified human Sirt2 as a robust lysine de-fatty-acylase. Researchers used a chemical probe based on a Lys9-myristoylated histone H3 peptide, in which residue Thr6 was replaced with a diazirine-containing photoreactive amino acid (photo-Leu). The probe also included a terminal alkyne-containing amino acid at the peptide C-terminus to enable bioorthogonal conjugation of fluorescence tags for detecting captured proteins. This approach enabled the discovery of previously unrecognized cellular functions of Sirt2, which had been considered solely as a deacetylase [46].
Relationship Visualization: Multi-Omics Data Integration Concepts
Multi-Omics Integration Conceptual Framework
Automated Workflows for High-Throughput Compound Screening
Troubleshooting Guides
Why is my screening data inconsistent with high variability between replicates?
Problem: High inter-assay and intra-assay variability in high-throughput screening (HTS) results, leading to unreliable data and difficulties in identifying true hits [47].
Causes and Solutions:
| Cause | Solution | Preventive Measure |
|---|---|---|
| Manual liquid handling | Implement automated liquid handlers | Use non-contact dispensers (e.g., I.DOT Liquid Handler) with integrated volume verification [47] |
| Inter-operator variability | Standardize protocols across users | Develop detailed SOPs and use automated workflow orchestration software [48] |
| Uncalibrated equipment | Regular instrument validation | Schedule routine maintenance and calibration checks |
Experimental Protocol for Variability Assessment:
- Prepare Control Plates: Use a control compound with known effect at EC80 concentration and a negative control (DMSO only) distributed across three 384-well plates [47].
- Automated Dispensing: Dispense controls and reagents using an automated non-contact liquid handler. Enable DropDetection technology to verify dispensed volumes [47].
- Assay Execution: Run the assay under standard conditions.
- Data Analysis: Calculate the Z'-factor for each plate using the formula: Z' = 1 - (3σc+ + 3σc-)/|μc+ - μc-|, where σc+ and σc- are the standard deviations of the positive and negative controls, and μc+ and μc- are their means. A Z' factor > 0.5 indicates a robust assay suitable for HTS [47].
How do I troubleshoot low library yield in NGS-based screening?
Problem: Low final library yield following NGS library preparation for chemogenomic assays, resulting in insufficient material for sequencing [2].
Causes and Solutions:
| Cause | Diagnostic Clues | Corrective Action |
|---|---|---|
| Poor Input Sample Quality | Degraded DNA/RNA; low 260/230 ratios (e.g., <1.8) indicating contaminants [2] | Re-purify input sample; use fluorometric quantification (e.g., Qubit) instead of UV absorbance [2] |
| Inefficient Adapter Ligation | Sharp peak at ~70-90 bp on Bioanalyzer (adapter dimers) [2] | Titrate adapter-to-insert molar ratio; ensure fresh ligase buffer; verify reaction temperature [2] |
| Overly Aggressive Purification | High sample loss after bead-based cleanups [2] | Optimize bead-to-sample ratio; avoid over-drying beads; use shallow annealing temperatures during PCR [2] |
Experimental Protocol for Yield Optimization:
- Quality Control: Assess input DNA/RNA quality using an automated electrophoresis system (e.g., BioAnalyzer). Accept only samples with RIN > 8 or DIN > 7 [2].
- Quantification: Use a fluorometric method for accurate nucleic acid quantification.
- Automated Library Prep: Use a robotic liquid handler for all purification and normalization steps to minimize bead handling and pipetting errors [48].
- QC Checkpoint: After library amplification, quantify yield using a fluorescence-based method and check the fragment size distribution on a BioAnalyzer. A successful library will show a clear peak at the expected size with minimal adapter-dimer contamination [2].
Frequently Asked Questions (FAQs)
What are the key considerations when implementing automation in my screening workflow?
Successful implementation requires more than just purchasing equipment [48].
- How do I justify the ROI for automation? Automation ROI extends beyond speed. For 1,000 scientists saving 15 minutes daily, over 62,000 hours are recovered annually. Additional ROI comes from reduced reagent consumption (up to 90% through miniaturization), improved data quality, and higher staff satisfaction as scientists focus on analysis over repetitive tasks [49] [47].
- Which steps should I automate first? Conduct a workflow audit to identify key bottlenecks. Start small by automating a single, repetitive process like DNA extraction or compound dilution before scaling to full workflows [48].
- How can I ensure my team adopts the new automated systems? Engage end-users early in the design and testing phase. Invest in comprehensive training and change management to encourage buy-in. Select systems with intuitive software interfaces [48].
How can I manage and analyze the large volumes of data generated by HTS?
The data management challenge is as critical as the wet-lab workflow [47].
- What is the best way to handle multiparametric HTS data? Implement an automated data pipeline using specialized software (e.g., GeneData Screener). This replaces error-prone manual spreadsheet cleansing and enables streamlined analysis for faster insights [50] [49].
- How can I improve the quality of my hit selection? Use automated systems to screen compounds at multiple concentrations to generate comprehensive dose-response data. This helps eliminate false positives and provides quantitative data on compound potency and efficacy [50] [47].
- Can automation help with data integrity and compliance? Yes. Automated data pipelines log every action, control access, and generate automatic audit trails. This embeds compliance into the workflow, reduces documentation burden, and lowers the risk of data integrity violations [49].
Workflow Visualization
Automated HTS and Data Analysis Workflow
Troubleshooting Logic for Common HTS and NGS Issues
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function | Application Note |
|---|---|---|
| Non-Contact Liquid Handler (e.g., I.DOT) [47] | Precisely dispenses sub-microliter volumes without tip contact, minimizing carryover and variability. | Essential for assay miniaturization in 384- or 1536-well formats. Integrated DropDetection verifies every dispense [47]. |
| Automated NGS Library Prep Station | Robotic system that performs liquid handling for library construction, normalization, and pooling [48]. | Reduces batch effects and hands-on time. Can increase sample throughput from 200 to over 600 per week while cutting hands-on time by 65% [48]. |
| High-Sensitivity DNA/RNA QC Kit | Fluorometric-based assay for accurate quantification of nucleic acid concentration. | Critical for quantifying input material for NGS library prep, as UV absorbance can overestimate concentration [2]. |
| HTS Data Analysis Software (e.g., GeneData Screener) [50] | Automates data processing, normalization, and hit identification from multiparametric screening data. | Replaces manual spreadsheet analysis; enables rapid, error-free processing of thousands of data points and generation of dose-response curves [50] [49]. |
| Laboratory Information Management System (LIMS) | Tracks samples, reagents, and associated metadata throughout the entire workflow [48]. | Provides chain-of-custody and traceability, which is critical for reproducibility and regulatory compliance [48]. |
Structural Variant Detection for Understanding Complex Drug-Gene Interactions
Troubleshooting Guides
FAQ: Addressing Common Structural Variant Detection Challenges
Q1: Why does my SV detection tool fail to identify known gene deletions or duplications in pharmacogenes?
This is a common problem often rooted in the high sequence homology between functional genes and their non-functional pseudogenes, which causes misalignment of sequencing reads [16]. This is particularly prevalent in genes like CYP2D6, which has a homologous pseudogene (CYP2D7) [16].
- Solution: Implement a specialized computational tool that uses a machine learning-based approach to estimate copy number and detect SVs from read depth data, rather than relying solely on sequence alignment [16]. The PyPGx pipeline, for example, employs a support vector machine (SVM)-based classifier trained on both GRCh37 and GRCh38 genome builds to address this [16]. Always manually inspect the copy number and allele fraction profiles output by the tool to verify the quality of SV calls [16].
Q2: How can I resolve the high rate of false positive SVs in my NGS data from chemogenomic studies?
False positives frequently arise from sequencing errors introduced during library preparation or from using suboptimal bioinformatics parameters [51].
- Solution:
- Implement Robust QC: Execute rigorous quality control (QC) at every stage of your NGS workflow, from library prep to sequencing, to minimize inaccuracies [51].
- Standardize Your Pipeline: Use standardized, well-documented bioinformatics pipelines to reduce inconsistencies caused by variable alignment algorithms or variant calling methods [51].
- Validation: Confirm putative SVs using an orthogonal method, such as PCR-based validation or, ideally, long-read sequencing, which is more adept at resolving complex regions [16].
Q3: What is the best way to handle the "cold start" problem when predicting targets for new drugs with no known interactions?
Network-based inference (NBI) methods often suffer from a "cold start" problem, where they cannot predict targets for new drugs that lack existing interaction data [52].
- Solution: Transition from pure network-based methods to feature-based methods or matrix factorization techniques. Feature-based methods can predict interactions by learning from the chemical structure and other features of a drug, and the sequence and features of a target, even in the absence of known interactions [52]. Random walk-based methods have also shown an ability to address the cold start problem for drugs by traversing transitive relationships in a sparse drug-target interaction network [52].
Q4: Our lab struggles with the computational intensity of SV detection on large whole-genome datasets. How can we optimize this?
Large-scale NGS analyses, including WGS for pharmacogenetics, are computationally demanding and can slow down or fail without proper resources [51].
- Solution:
- Utilize High-Performance Computing (HPC): Perform analyses on powerful servers or clusters with sufficient memory and processing cores [51].
- Parallel Computing: Divide samples into non-overlapping batches to facilitate parallel computing, as demonstrated in large-scale studies like those analyzing the 2504 samples from the 1000 Genomes Project [16].
- Cloud-Based Solutions: Consider using cloud computing platforms for scalable and flexible computational resources for NGS data analysis [53].
Common Structural Variant Detection Bottlenecks and Solutions
Table 1: Troubleshooting common issues in structural variant detection for pharmacogenes.
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Failure to detect known SVs (e.g., in CYP2D6) | High sequence homology with pseudogenes leading to read misalignment [16] | Use ML-based tools (e.g., PyPGx's SVM classifier) on read depth data; manually inspect output [16] |
| High false positive SV calls | Sequencing errors; suboptimal bioinformatics tool parameters [51] | Implement rigorous QC; use standardized workflows; validate with orthogonal methods [51] |
| Inability to predict targets for new drugs ("Cold Start") | Reliance on network-based methods that require existing interaction data [52] | Adopt feature-based machine learning models or matrix factorization techniques [52] |
| Long analysis times & computational failures | Large dataset size (e.g., WGS); insufficient computational resources [51] | Use HPC clusters; implement parallel computing by batching samples; leverage cloud platforms [16] [53] |
| Difficulty interpreting functional impact of SVs | Lack of annotation for novel SVs in standard databases [54] | Cross-reference with PharmVar and PharmGKB; assess cumulative impact of multiple variants [55] [54] |
Experimental Protocols
Detailed Methodology: Population-Level Pharmacogene SV Detection using PyPGx
This protocol is adapted from large-scale studies, such as the pharmacogenetic analysis of the 1000 Genomes Project using whole-genome sequences [16].
1. Sample Preparation and Sequencing
- Input Material: High molecular weight genomic DNA.
- Sequencing Technology: High-coverage (e.g., ~30x) Whole Genome Sequencing (WGS) using short-read Illumina platforms.
- Output: Paired-end FASTQ files for each sample.
2. Data Preprocessing and Alignment
- Tool: Use alignment tools like BWA-MEM.
- Reference Genome: Align reads to the human reference genome (e.g., GRCh37 or GRCh38).
- Command (example from
fucpackage):ngs-fq2bamto convert FASTQ to aligned BAM files [16].
3. Structural Variant Detection with PyPGx
- Tool: PyPGx (v0.16.0 or higher) [16].
- Input Files for Pipeline: For each batch of samples, generate:
- A multi-sample VCF file (
create-input-vcfcommand). - A depth of coverage file (
prepare-depth-of-coveragecommand). - A control statistics file (
compute-control-statisticscommand).
- A multi-sample VCF file (
- Core SV Detection Workflow:
- Phasing: Statistically phase small variants (SNVs, indels) into haplotypes using a tool like Beagle with a reference panel [16].
- Copy Number Calculation: Compute per-base copy number from read depth data via intra-sample normalization using a stable control gene (e.g., VDR) as an anchor [16].
- SV Classification: Detect SVs (deletions, duplications, hybrids) from the copy number data using the pre-trained Support Vector Machine (SVM) classifier [16].
- Command: Execute the
run-ngs-pipelinecommand from PyPGx for each target pharmacogene.
4. Genotype Calling and Phenotype Prediction
- Star Allele Assignment: Combine candidate star alleles from phased small variants with the SV results to make the final diplotype assignment (e.g.,
CYP2D6*1/*4) [16]. - Phenotype Translation: Use translation tables from resources like PharmGKB or CPIC to assign predicted phenotypes (e.g., Poor Metabolizer, Ultrarapid Metabolizer) based on the called diplotypes [16].
Workflow Visualization
The Scientist's Toolkit
Key Research Reagent Solutions
Table 2: Essential materials and tools for SV analysis in pharmacogenomics.
| Item | Function / Explanation |
|---|---|
| High-Coverage WGS Data | Provides the raw sequencing reads necessary for detecting a wide range of genetic variants, including SVs, across the entire genome [16]. |
| Control Gene Locus (e.g., VDR) | Used for intra-sample normalization during copy number calculation, serving as a stable baseline for read depth comparison [16]. |
| Reference Haplotype Panel (e.g., 1KGP) | Used for statistical phasing of small variants, helping to determine which variants are co-located on the same chromosome [16]. |
| PyPGx Pipeline | A specialized bioinformatics tool for predicting PGx genotypes and phenotypes from NGS data, with integrated machine learning-based SV detection capabilities [16]. |
| PharmGKB/PharmVar Databases | Core resources for clinical PGx annotations, providing information on star allele nomenclature, functional impact, and clinical guidelines [54]. |
| GRCh37/GRCh38 Genome Builds | Standardized reference human genome sequences required for read alignment, variant calling, and training SV classifiers [16]. |
Logical Framework for SV Analysis Challenges
Streamlining Chemogenomics Workflows: Practical Strategies for Enhanced Efficiency
Quality Control Pitfalls and Proven Mitigation Strategies
Within chemogenomics research, next-generation sequencing (NGS) has become an indispensable tool for uncovering the complex interactions between small molecules and biological systems. However, the path from sample to insight is fraught with technical challenges that can compromise data integrity. Quality control (QC) pitfalls at any stage of the NGS workflow can introduce biases, reduce sensitivity, and lead to erroneous biological conclusions, ultimately creating significant bottlenecks in data analysis. This guide addresses the most common QC challenges and provides proven mitigation strategies to ensure the generation of reliable, high-quality NGS data for chemogenomics applications.
Frequently Asked Questions (FAQs)
What are the most critical quality control checkpoints in an NGS workflow?
The most critical QC checkpoints occur at multiple stages: (1) Sample Input/Quality Assessment to ensure nucleic acid integrity and purity; (2) Post-Library Preparation to verify fragment size distribution and concentration; and (3) Post-Sequencing to evaluate raw read quality, complexity, and potential contamination before beginning formal analysis [2].
How can I distinguish true biological signals from PCR amplification artifacts in my data?
PCR duplicates, identified as multiple reads with identical start and end positions, are a primary artifact of over-amplification [56]. These artifacts falsely increase homozygosity and can be identified and marked using tools like Picard's MarkDuplicates or samtools rmdup [57]. To minimize these artifacts, use the minimum number of PCR cycles necessary (often 6-10 cycles) and consider PCR-free library preparation methods for sufficient starting material [56] [57].
My NGS data shows unexpected low complexity. What are the potential causes?
Low library complexity, indicated by high rates of duplicate reads, often stems from:
- Insufficient or degraded starting material, requiring excessive PCR amplification [2].
- Biased fragmentation during library prep, where certain genomic regions (e.g., high-GC content) are under-represented [58] [2].
- Enzymatic cleavage biases, as enzymes like MNase and DNase I have sequence-specific cleavage preferences that can skew representation [58].
- Overly aggressive purification or size selection leading to significant sample loss [2].
What steps can I take to identify and remove contaminating sequences?
Contaminant removal is crucial, especially in metagenomic studies. A effective strategy involves:
- Creating a contaminant reference database containing sequences from known contaminants (e.g., host genome, PhiX control sequence, or common laboratory contaminants) [59].
- Alignment-based filtering using tools like Bowtie2 to align your reads against this database [59].
- Removing all reads that align to the contaminant references. Software suites like KneadData, which integrate Trimmomatic for quality filtering and Bowtie2 for contaminant alignment, streamline this process [59].
How does chromatin structure influence NGS assays like ChIP-seq, and how can this bias be mitigated?
Chromatin structure itself is a significant source of bias. Heterochromatin is more resistant to sonication shearing than euchromatin, leading to under-representation [58]. Furthermore, enzymatic digestion (e.g., with MNase) has strong sequence preferences, which can create false patterns of nucleosome occupancy [58]. Mitigation strategies include using input controls that are sonicated or digested alongside the experimental samples and applying analytical tools that account for these known enzymatic sequence biases [58].
Troubleshooting Guide: Common NGS QC Failures
Table 1: Common NGS Quality Control Issues and Solutions
| Problem Category | Typical Failure Signals | Root Causes | Proven Mitigation Strategies |
|---|---|---|---|
| Sample Input & Quality | Low library yield; smeared electrophoregram; low complexity [2] | Degraded DNA/RNA; contaminants (phenol, salts); inaccurate quantification [2] | Re-purify input; use fluorometric quantification (Qubit); check 260/230 and 260/280 ratios [2] |
| Fragmentation & Ligation | Unexpected fragment size; high adapter-dimer peaks [2] | Over-/under-shearing; improper adapter-to-insert molar ratio; poor ligase performance [2] | Optimize fragmentation parameters; titrate adapter ratios; ensure fresh ligase and optimal reaction conditions [2] |
| PCR Amplification | High duplicate rate; over-amplification artifacts; sequence bias [2] | Too many PCR cycles; polymerase inhibitors; primer exhaustion [56] [2] | Minimize PCR cycles; use robust polymerases; consider unique molecular identifiers (UMIs) [56] |
| Contaminant Sequences | High proportion of reads align to non-target organisms (e.g., host) [60] [59] | Impure samples (e.g., host DNA in metagenomic samples); cross-contamination during prep [60] | Use alignment tools (Bowtie2) against contaminant databases; employ careful sample handling [59] |
| Read Mapping Issues | Low mapping rate; uneven coverage; "sticky" peaks in certain regions [58] | Repetitive elements; high genomic variation; poor reference genome quality [58] | Use longer or paired-end reads; apply specialized mapping algorithms for repeats; use updated genome assemblies [58] |
Experimental Protocols for Key QC Experiments
Protocol 1: Removal of Contaminating Sequences Using KneadData
This protocol is designed to systematically remove common contaminants, such as host DNA, from metagenomic or transcriptomic sequencing data, which is a frequent requirement in chemogenomics studies involving host-associated samples [59].
Gather Reference Sequences: Compile all contaminant sequences (e.g., human genome, PhiX, common lab contaminants) into a single FASTA file.
Index the Reference Database using Bowtie2.
Run KneadData, which internally uses Trimmomatic for quality trimming and Bowtie2 for contaminant alignment.
Output Interpretation: The main output file (
*_kneaddata.fastq) contains the cleaned reads. The log file provides statistics on the proportion of reads removed as contaminants [59].
Protocol 2: Accurate Quantification and Assessment of PCR Duplication Rates
Accurate quantification of duplication rates is essential for evaluating library complexity and the potential for false homozygosity calls, which can impact variant analysis in chemogenomics.
Alignment: Map your sequencing reads to a reference genome using an aligner like BWA or Bowtie2 [56].
Duplicate Marking: Process the aligned BAM file with a duplicate identification tool. Samblaster is one option used in RAD-seq studies [56].
Rate Calculation: The duplication rate is calculated as the proportion of marked duplicates in the file. Most duplicate marking tools provide this summary statistic.
Troubleshooting High Duplicate Rates:
- Cause: High duplicate rates often correlate with higher total read counts, as sequencing a greater fraction of the library increases the chance of sampling the same molecule multiple times [56].
- Investigation: If the rate is abnormally high, investigate the starting material quantity and the number of PCR cycles used during library prep. Higher PCR cycle numbers can lead to higher duplicate rates [56] [57].
- Mitigation: For future experiments, if high depth is required, consider splitting the library prep over multiple independent reactions to maintain complexity [56].
Workflow Visualization
NGS Quality Control Checkpoints
Contaminant Screening Workflow
The Scientist's Toolkit: Essential Reagents & Software
Table 2: Key Research Reagent Solutions for NGS Quality Control
| Item Name | Function/Benefit | Example Use Case |
|---|---|---|
| SPRISelect Beads | Size selection and clean-up; removal of short fragments and adapter dimers [61] | Purifying long-read sequencing libraries to remove fragments < 3-4 kb [61] |
| Fluorometric Assays (Qubit) | Accurate quantification of double-stranded DNA using fluorescence; superior to UV absorbance for NGS prep [2] | Measuring input DNA/RNA concentration without overestimation from contaminants [2] |
| High-Fidelity Polymerase | Reduces PCR errors and maintains representation during library amplification [2] | Generating high-complexity libraries with minimal amplification bias |
| Unique Molecular Identifiers (UMIs) | Short random nucleotide sequences that tag individual molecules before amplification [56] | Enabling bioinformatic correction for PCR amplification bias and accurate quantification |
| QC-Chain Software | A holistic QC package offering de novo contamination screening and fast processing for metagenomic data [60] | Rapid quality assessment and contamination identification in complex microbial community samples [60] |
| KneadData Software | An integrated pipeline that performs quality trimming (via Trimmomatic) and contaminant removal (via Bowtie2) [59] | Systematic cleaning of metagenomic or host-derived sequencing data in a single workflow [59] |
Automation Solutions for Library Preparation and Data Processing
Frequently Asked Questions (FAQs)
Q1: What are the key benefits of automated NGS library preparation compared to manual methods? Automated NGS library preparation systems like the MagicPrep NGS provide several advantages: they reduce manual hands-on time to approximately 10 minutes, achieve a demonstrated success rate exceeding 99%, and offer true walk-away automation that eliminates costly errors during library preparation [62]. This enables researchers to focus on other experimental work while the system processes libraries.
Q2: Can automated library preparation systems be used with fewer than a full batch of samples? Yes, systems like MagicPrep NGS can run with fewer than 8 samples. However, the reagents and consumables are designed for single use only, and any unused reagents cannot be recovered or saved for future experiments, which may impact cost-efficiency for small batches [62].
Q3: What environmental conditions are required for optimal operation of automated NGS library preparation systems? Automated NGS systems require specific environmental conditions for reliable operation: room temperature between 20-26°C, relative humidity of 30-60% (non-condensing), and installation at altitudes around 500 meters above sea level. Adequate airflow must be maintained by leaving at least 15cm (6 inches) of clear space on all sides of the instrument [62].
Q4: How does automated library preparation address GC bias in samples? Advanced automated systems utilize pre-optimized reagents and protocols that minimize GC bias. Testing with bacterial genomes of varying GC content (32%-68% GC) has demonstrated uniform DNA fragmentation and consistent coverage regardless of GC content, providing more reliable data across diverse sample types [62].
Q5: What are the common error sources in automated NGS workflows and how can they be troubleshooted? For touchscreen responsiveness issues or system errors, performing a power cycle (completely shutting down the system until LED indicators turn off, then restarting) often resolves the problem. For barcode scanning errors, ensure reagents are new and unused, and remove any moisture obstructing the barcode reader. If errors persist, contact technical support [62].
Troubleshooting Guides
Library Preparation Issues
Problem: Low Library Yield or Failed Library Construction
Table: Troubleshooting Low Library Yield
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Insufficient DNA/RNA Input | Verify sample concentration and quality using fluorometry or spectrophotometry | Adjust input amount to system recommendations (e.g., 50-500 ng for DNA, 10 ng-1 μg for total RNA) [62] |
| Sample Quality Issues | Check degradation levels (e.g., RNA Integrity Number) | Implement quality control measures and use high-quality extraction methods [63] |
| Reagent Handling Problems | Confirm proper storage and handling of reagents | Ensure complete thawing and mixing of reagents before use [64] |
Prevention Strategies:
- Implement rigorous nucleic acid quality control protocols before library preparation
- Ensure proper storage conditions for all reagents and consumables
- Regularly maintain and calibrate automated systems according to manufacturer specifications
- Use integrated solutions with pre-optimized scripts and reagents designed specifically for your automated system [62]
Data Processing Bottlenecks
Problem: Slow Data Analysis Pipeline
Table: NGS Informatics Market Solutions to Data Bottlenecks
| Bottleneck Type | Solution Approach | Impact/ Benefit |
|---|---|---|
| Variant Calling Speed | AI/ML-accelerated tools (Illumina DRAGEN, NVIDIA Parabricks) | Reduces run times from hours to minutes while improving accuracy [65] |
| Data Storage Costs | Cloud and hybrid computing architectures | Enables scaling without capital expenditure; complies with data sovereignty laws [65] |
| Bioinformatician Shortage | Commercial platforms with intuitive interfaces | Reduces dependency on specialized bioinformatics expertise [65] |
Implementation Guidance for Chemogenomics:
- Deploy cloud-native platforms that bundle workflow management, compliance dashboards, and pay-per-use computing
- Consider hybrid models that keep raw read files on-premises while outsourcing compute-intensive secondary analysis to regional clouds
- Utilize containerized workflows to ensure reproducibility across research teams [65]
Table: Performance Metrics of Automated NGS Solutions
| Parameter | MagicPrep NGS System | Traditional Manual Methods | Measurement Basis |
|---|---|---|---|
| Success Rate | >99% [62] | Variable (user-dependent) | Library recovery ≥200ng with expected fragment distribution [62] |
| Hands-on Time | ~10 minutes [62] | Several hours to days | Time from sample ready to run initiation [62] |
| Batch Consistency | 5.8%-16.8% CV [62] | Typically higher variability | Coefficient of variation across multiple runs and batches [62] |
| Post-Run Stability | Up to 65 hours [62] | Limited (evaporation concerns) | Time libraries can be held in system without degradation [62] |
Experimental Protocols
Automated Library Preparation Using Integrated Systems
Methodology: The Tecan MagicPrep NGS system provides a complete automated workflow for Illumina-compatible library preparation. The system integrates instrument, software, pre-optimized scripts, and reagents in a single platform [62].
Procedure:
- System Setup (~5 minutes): Place the reagent card into the instrument and ensure all components are properly seated
- Sample Loading (~5 minutes): Transfer samples to the sample plate according to the platform specifications
- Run Initiation: Start the automated protocol through the touchscreen interface
- Library Recovery: Collect finished libraries after run completion (typically several hours)
Key Considerations:
- The system performs all library preparation steps automatically, including fragmentation, adapter ligation, and amplification where applicable
- No pre-mixing of reagents is required, minimizing potential for pipetting errors
- The walk-away automation enables unattended operation once initiated [62]
Library Quantification Protocol for Quality Control
Methodology: KAPA Library Quantification Kit using qPCR-based absolute quantification, compatible with Illumina platforms with P5 and P7 flow cell oligo sequences [64].
Detailed Procedure:
Reagent Preparation:
- Prepare DNA dilution buffer (10 mM Tris-HCl, pH 8.0-8.5 + 0.05% Tween 20)
- Thaw and thoroughly mix all kit components
- For first-time use: Add the entire 1 ml Library Quantification Primer Premix (10x) to the 5 ml KAPA SYBR FAST qPCR Master Mix (2x) bottle
- Vortex thoroughly and record the date of mixing
Sample and Standard Preparation:
- Prepare appropriate dilutions of libraries (typically 1:1,000 to 1:100,000) in DNA dilution buffer
- Include at least one additional 2-fold dilution for each library
- Prepare the provided DNA standard dilutions (6-point serial dilution)
qPCR Reaction Setup:
- Prepare master mix according to the following formulation for 20μL reactions:
- 10.0 μL KAPA SYBR FAST qPCR Master Mix with primer premix
- 6.0 μL PCR-grade water
- 4.0 μL template (standard, diluted library, or control)
- Distribute appropriate volumes to each well
- Add templates: water for NTCs, standards from lowest to highest concentration, then diluted libraries
- Seal the plate and centrifuge briefly
- Prepare master mix according to the following formulation for 20μL reactions:
qPCR Cycling Conditions:
- Initial denaturation: 95°C for 5 minutes
- 35 cycles of:
- 95°C for 30 seconds (denaturation)
- 60°C for 45 seconds (annealing/extension; increase to 90 seconds for libraries >700bp)
- Melt curve analysis (optional)
Data Analysis:
- Generate standard curve by plotting average Cq values against log10 concentration of standards
- Ensure standard curve meets quality criteria: efficiency 90-110%, R² ≥ 0.99
- Calculate library concentrations using absolute quantification adjusted for fragment size [64]
Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for Automated NGS Workflows
| Reagent/Kit | Function | Application Notes |
|---|---|---|
| Revelo DNA-Seq Enz [62] | Automated DNA library preparation with enzymatic fragmentation | Input: 50-500 ng; 32 reactions/kit; Compatible with Illumina platforms |
| Revelo PCR-free DNA-Seq Enz [62] | PCR-free DNA library preparation to eliminate amplification bias | Input: 100-400 ng; Ideal for sensitive applications; 32 reactions/kit |
| Revelo mRNA-Seq [62] | Automated mRNA sequencing library preparation from total RNA | Input: 10 ng-1 μg; Includes poly-A transcript selection; 32 reactions/kit |
| KAPA Library Quantification Kit [64] | qPCR-based absolute quantification of Illumina libraries | Uses P5/P7-targeting primers; Validated for libraries up to 1 kb |
| TruSeq Library Preparation Kits [66] | High-quality manual library preparation with proven coverage uniformity | Various applications (DNA, RNA, targeted); Known for uniform coverage |
| KAPA SYBR FAST qPCR Master Mix [64] | High-performance qPCR detection with engineered polymerase | Antibody-mediated hot start; Suitable for automation; 30 freeze-thaw cycles |
Optimization Recommendations for Chemogenomics
Addressing Specific Chemogenomics Bottlenecks
For High-Throughput Compound Screening:
- Implement automated library preparation systems to ensure reproducibility across thousands of compound-treated samples
- Utilize unique dual indexes (UDIs) to enable flexible multiplexing of different treatment conditions [62]
- Establish standardized QC checkpoints to maintain data quality throughout large-scale experiments
For Data Analysis Challenges:
- Deploy AI/ML-accelerated variant calling pipelines to reduce analysis time from hours to minutes [65]
- Implement cloud-hybrid architectures to manage computational resource demands during peak analysis periods
- Develop standardized data processing protocols to ensure consistency across research teams and studies
For Integration with Existing Infrastructure:
- Select systems that offer compatibility with laboratory information management systems (LIMS) and electronic health records (EHR)
- Consider platforms that provide application programming interfaces (APIs) for custom integration needs
- Establish data governance protocols that address privacy regulations and data sovereignty requirements, particularly for international collaborations [65]
Computational Resource Optimization for Large-Scale Studies
Troubleshooting Guides
FAQ: Diagnosing Resource Bottlenecks
Q: How can I identify if my NGS analysis is bottlenecked by CPU, memory, or storage I/O? A bottleneck occurs when one computational resource limits overall performance, causing delays even when other resources are underutilized.
- CPU Bottleneck: Your processing units are at 100% utilization for extended periods, while memory and disk I/O show lower usage. Analysis tasks like read alignment and variant calling are queued, and overall progress is slow [67].
- Memory (RAM) Bottleneck: The system's RAM is fully occupied, leading to heavy use of "swap" space on the disk. This causes a severe performance drop, as disk access is much slower than RAM [67].
- Storage I/O Bottleneck: The storage disk (HDD/SSD) is constantly at high read/write capacity, while CPU and RAM are not maxed out. This is common during file-intensive steps like merging large BAM files [67].
Table 1: Symptoms and Solutions for Common Computational Bottlenecks
| Bottleneck Type | Key Symptoms | Corrective Actions |
|---|---|---|
| CPU | CPU utilization consistently at or near 100%; slow task progression [67]. | Distribute workload across more CPU cores; use optimized, parallelized algorithms; consider a higher-core-count instance in the cloud [24] [67]. |
| Memory (RAM) | System uses all RAM and starts "swapping" to disk; severe performance degradation [67]. | Allocate more RAM; optimize tool settings to lower memory footprint; process data in smaller batches [67]. |
| Storage I/O | High disk read/write rates; processes are stalled waiting for disk access [67]. | Shift to faster solid-state drives (SSDs); use a parallel file system; leverage local scratch disks for temporary files [67]. |
FAQ: Strategies for Cloud and HPC Environments
Q: What is the most computationally efficient strategy for aligning large-scale NGS data? The choice between local computation and offloading to cloud or edge servers depends on your data size and latency requirements [68].
- Local Computation: Best for small to medium data sizes where communication latency to the cloud would be a bottleneck [68].
- Partial Offloading (Hybrid): For larger datasets, a hybrid approach that splits the computational load between local resources and the cloud offers the best computational energy efficiency and performance [68].
- Full Cloud Offloading: Ideal for massive, project-scale analyses, providing scalability and access to advanced tools without local infrastructure investment [24] [67].
Q: How can I optimize costs when using cloud platforms for genomic analysis? Cloud platforms like AWS, Google Cloud, and Azure offer scalable resources but require careful management to control costs [24] [67].
- Use Spot/Preemptible Instances: For fault-tolerant batch jobs like secondary analysis, these instances can offer significant cost savings [67].
- Right-Sizing Resources: Select instance types that match your workload's specific needs for CPU, memory, and storage to avoid over-provisioning [67].
- Leverage Managed Services: Use cloud-native genomics services (e.g., AWS HealthOmics, Illumina Connected Analytics) which are optimized for NGS workflows and can reduce management overhead [24] [69].
- Implement Data Lifecycle Policies: Automate the archiving of raw data to cheaper, long-term storage classes after processing to minimize storage costs [67].
Experimental Protocols
Detailed Methodology: Resource-Optimized Variant Calling Pipeline
This protocol outlines a best-practice workflow for the tertiary analysis of NGS data, specifically designed to be computationally efficient for large-scale chemogenomics studies [70].
1. Input: Aligned Sequencing Data (BAM files)
- Begin with sequencing reads that have already been aligned to a reference genome (secondary analysis is complete) [70].
2. Variant Quality Control (QC)
- Procedure: Filter variants based on quality metrics to remove artifacts and low-confidence calls. Key metrics include:
- Variant Allele Frequency (VAF)
- Quality Score (QUAL)
- Strand Bias (SB)
- Read depth and coverage for the tested genes [70].
- Computational Tip: Use software that allows setting automatic PASS/FAIL thresholds to standardize this step and save time [70].
3. Variant Annotation
- Procedure: Annotate the filtered variants with biological and clinical information from curated knowledge bases.
- Resources: Query multiple databases simultaneously for comprehensive insights. Essential databases include:
- Population Databases: gnomAD
- Cancer Databases: COSMIC, OncoKB, CIViC
- Clinical Databases: ClinVar
- Functional Predictors: CADD, REVEL, SIFT, SpliceAI [70].
- Computational Tip: Automated annotation software can query these sources in parallel, dramatically increasing efficiency compared to manual curation [70].
4. Variant Interpretation and Classification
- Procedure: Classify variants based on pathogenicity/oncogenicity and clinical actionability according to established guidelines (e.g., AMP/ASCO/CAP) [70].
- Tiering System:
- Tier 1: Variants with strong clinical significance and association with targeted therapies.
- Tier 2: Variants with potential clinical significance, often linked to clinical trials.
- Tier 3: Variants of unknown significance.
- Tier 4: Benign or likely benign variants [70].
5. Report Generation
- Procedure: Compile the classified and interpreted variants into a structured clinical or research report [70].
- Automation Benefit: Specialized software can reduce the time for this entire tertiary workflow from 7-8 hours (manual) to approximately 30 minutes, drastically accelerating the path to clinical decisions [70].
NGS Bottleneck Diagnostic Workflow
The following diagram illustrates a systematic approach to diagnosing and resolving NGS computational bottlenecks.
Computational Resource Allocation Strategy
This diagram outlines the decision process for selecting a computational strategy based on data size and requirements.
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for NGS Workflows
| Tool / Resource | Function / Explanation |
|---|---|
| Cloud Computing Platforms (AWS, Google Cloud, Azure) [24] [67] | Provide on-demand, scalable computational resources (CPUs, GPUs, memory, storage), eliminating the need for large local hardware investments. |
| High-Performance Computing (HPC) Clusters [67] | Groups of powerful, interconnected computers that provide extremely high computing performance for intensive tasks like genome assembly and population-scale analysis. |
| Containerization Solutions (Docker, Kubernetes) [67] | Create isolated, reproducible software environments that ensure analysis tools and their dependencies run consistently across different computing systems. |
| AI-Powered Variant Callers (e.g., DeepVariant) [24] [69] | Use deep learning models to identify genetic variants from NGS data with higher accuracy than traditional methods, reducing false positives and the need for manual review. |
| Managed Bioinformatics Services (e.g., Illumina Connected Analytics, AWS HealthOmics) [24] [69] | Cloud-based platforms that offer pre-configured, optimized workflows for NGS data analysis, reducing the bioinformatics burden on research teams. |
| Specialized Processors (GPUs/TPUs) [67] | Accelerate specific, parallelizable tasks within the NGS pipeline, such as AI model training and certain aspects of sequence alignment, leading to faster results. |
Standardized Pipelines to Reduce Variability in Results
In chemogenomics research, where the interaction between chemical compounds and biological systems is studied at a genome-wide scale, the reproducibility of results is paramount. Next-Generation Sequencing (NGS) has become a fundamental tool in this field, enabling researchers to understand the genomic basis of drug response, identify novel therapeutic targets, and characterize off-target effects. However, the analytical phase of NGS has become a critical bottleneck, with a lack of standardized pipelines introducing significant variability that can compromise the validity and reproducibility of research findings [18].
The shift from data generation and processing bottlenecks to an analysis bottleneck means that the sheer volume and complexity of data, combined with a vast array of potential analytical choices, can lead to inconsistent results across studies and laboratories [18] [70]. This variability is particularly problematic in chemogenomics, where precise and reliable data is essential for making informed decisions in drug development. This guide addresses these challenges by providing clear troubleshooting advice and advocating for robust, standardized analytical workflows.
FAQs: Addressing Common NGS Analysis Challenges
Q1: Why do my NGS results show high variability even when using the same samples? High variability often stems from inconsistencies in the bioinformatic processing of your data, a problem known as the "analysis bottleneck" [18]. Unlike the earlier bottlenecks of data acquisition and processing, this refers to the challenge of consistently analyzing the vast amounts of data generated. Different choices in key pipeline steps—such as the algorithms used for read alignment, variant calling, or data filtering—can produce significantly different results from the same raw sequencing data. Adopting a standardized pipeline for all analyses is the most effective way to minimize this type of variability.
Q2: What are the most common causes of a failed NGS library preparation? Library preparation failures typically manifest through specific signals and have identifiable causes [2]:
| Failure Signal | Common Root Causes |
|---|---|
| Low library yield | Degraded DNA/RNA; sample contaminants (phenol, salts); inaccurate quantification; over-aggressive purification [2]. |
| High adapter dimer peaks | Inefficient ligation; suboptimal adapter-to-insert molar ratio; incomplete cleanup [2]. |
| High duplication rates | Over-amplification (too many PCR cycles); insufficient starting material; bias during fragmentation [2]. |
| Abnormally flat coverage | Contaminants inhibiting enzymes; poor fragmentation efficiency; PCR artifacts [2]. |
Q3: How can I reduce the turnaround time for interpreting NGS data in a clinical chemogenomics context? The interpretation of variants (tertiary analysis) is a major bottleneck, with manual interpretation taking 7-8 hours per report, potentially delaying clinical decisions for weeks [70]. To reduce this time to as little as 30 minutes, implement specialized tertiary analysis software. These solutions automate key steps such as variant quality control, annotation against curated knowledge bases (e.g., OncoKB, CIViC), prioritization, and report generation, ensuring both speed and standardization [70].
Q4: My computational analysis is too slow for large-scale chemogenomics datasets. What are my options? You are likely facing a modern computational bottleneck, where the volume of data outpaces traditional computing resources [7]. To navigate this, consider the following trade-offs:
- Speed vs. Accuracy: Techniques like data sketching provide massive speed-ups by using approximations, sacrificing perfect accuracy for a vast increase in computational efficiency [7].
- Cost vs. Time: Utilizing hardware accelerators like GPUs or cloud-based solutions (e.g., Illumina's Dragen on AWS) can drastically reduce analysis times, though at a higher financial cost per sample [7].
- Infrastructure Complexity: While powerful, these new technologies often require specialized expertise to implement and manage [7].
Troubleshooting Guide: NGS Data Processing Issues
Problem 1: Low Mapping Rates
Symptoms: A low percentage of sequencing reads successfully align to the reference genome. Methodologies for Diagnosis and Resolution:
- Assess Read Quality: Use tools like
FastQCto check for pervasive low-quality bases or an overrepresentation of adapter sequences, which can interfere with mapping. - Verify Reference Genome: Ensure the reference genome build and annotation sources (e.g., Ensembl, NCBI) match those used in your pipeline and are consistent across analyses [71].
- Check for Contamination: Align reads to a host genome (e.g., human) and a target genome (e.g., pathogen or cell line) if applicable. Unexplained mappings may indicate sample contamination. Using well-curated cell line records from sources like Cellosaurus can help identify cross-species contamination [71].
- Standardize Alignment Parameters: Document and consistently use the same alignment software (e.g., BWA, STAR) and its parameters (e.g., seed length, mismatch penalty) across all experiments to ensure reproducibility.
Problem 2: Inconsistent Variant Calls Between Replicates
Symptoms: The same sample processed in technical or biological replicates yields different sets of called genetic variants. Methodologies for Diagnosis and Resolution:
- Inspect Sequencing Depth: Confirm that the coverage depth is sufficiently high and uniform across all replicates. Low coverage in certain genomic regions is a common source of false negatives.
- Standardize Variant Calling and Filtering: Use the same variant calling software (e.g., GATK, VarScan) and, crucially, the same filtering thresholds for quality score, read depth, and allele frequency for all samples [70]. Inconsistent filtering is a major source of variability.
- Utilize Integrated Knowledge Bases: Annotate variants using standardized, regularly updated knowledge bases like ClinVar, COSMIC, and the Comparative Toxicogenomics Database (CTD) to help distinguish true biological variants from technical artifacts [71] [70].
- Implement a Portable Pipeline: Use a containerized or workflow management system (e.g., Docker, Nextflow, Snakemake) to encapsulate the entire variant calling pipeline, ensuring an identical software environment is used for every analysis, regardless of the computing platform.
Problem 3: High Technical Variation in Functional Connectivity (from fMRI)
Note: While from a different field (neuroscience), this problem is a powerful analogue for high variability in gene expression or pathway analysis networks in chemogenomics. The principles of pipeline standardization are directly transferable.
Symptoms: Network topology (e.g., gene co-expression networks) differs vastly between scans of the same sample or subject, obscuring true biological signals. Methodologies for Diagnosis and Resolution:
- Systematic Pipeline Evaluation: A comprehensive study evaluated 768 different data-processing pipelines for functional connectomics and found vast variability in their reliability [72].
- Minimize Spurious Differences: The study's primary criterion was to identify pipelines that minimized motion confounds and spurious test-retest discrepancies in network topology [72].
- Adopt Optimal, Multi-Criteria Pipelines: The solution is to use a pipeline that has been validated against multiple criteria, including sensitivity to true inter-subject differences and experimental effects, not just technical reliability. A subset of pipelines was found to consistently satisfy all criteria across different datasets [72].
- Standardize Node and Edge Definitions: In a genomics context, this translates to consistently using the same gene sets/pathways (nodes) and the same statistical measures (e.g., Pearson correlation, mutual information) to define interactions (edges) between them [72].
Essential Components of a Standardized NGS Pipeline
A robust and reproducible NGS pipeline for chemogenomics integrates data from multiple sources and employs automated, standardized processes. The following diagram illustrates the key stages and data flows of such a pipeline, highlighting its cyclical nature of data integration, analysis, and knowledge extraction.
Detailed Breakdown of Pipeline Components
| Pipeline Stage | Key Actions | Role in Reducing Variability |
|---|---|---|
| Data Integration | Automatically import and harmonize data from external sources (e.g., Ensembl, ClinVar, CTD, UniProt) [71]. | Ensures all analyses are based on a consistent, up-to-date, and comprehensive set of reference data, preventing errors from using outdated or conflicting annotations. |
| Primary Analysis | Convert raw signals from the sequencer into nucleotide sequences (base calls) with quality scores. | Using standardized base-calling algorithms ensures the starting point for all downstream analysis is consistent and of high quality. |
| Secondary Analysis | Align sequences to a reference genome and identify genomic variants (SNPs, indels). | Employing the same alignment and variant-calling software with fixed parameters across all studies is critical for producing comparable variant sets [70]. |
| Tertiary Analysis | Annotate and filter variants, then interpret their biological and clinical significance. | Automating this step with software that queries curated knowledge bases standardizes interpretation and drastically reduces turnaround time and manual error [70]. |
The Scientist's Toolkit: Research Reagent & Resource Solutions
The following table lists key databases and resources that are essential for building and maintaining a standardized NGS analysis pipeline in chemogenomics.
| Resource Name | Function & Role in Standardization |
|---|---|
| Rat Genome Database (RGD) | A knowledgebase that integrates genetic, genomic, phenotypic, and disease data. It demonstrates how automated pipelines import and integrate data from multiple sources to ensure data consistency and provenance [71]. |
| ClinVar | A public archive of reports detailing the relationships between human genomic variants and phenotypes. Using it as a standard annotation source ensures variant interpretations are based on community-reviewed evidence [71] [70]. |
| Comparative Toxicogenomics Database (CTD) | A crucial resource for chemogenomics, providing curated information on chemical-gene/protein interactions, chemical-disease relationships, and gene-disease relationships. Its integration provides a standardized basis for understanding molecular mechanisms of compound action [71]. |
| OncoKB | A precision oncology knowledge base that contains information about the oncogenic effects and therapeutic implications of specific genetic variants. Using it ensures cancer-related interpretations align with a highly curated clinical standard [70]. |
| Alliance of Genome Resources | A consortium of model organism databases that provides consistent comparative biology data, including gene descriptions and ortholog assignments. This supports cross-species analysis standardization, vital for translational chemogenomics [71]. |
| UniProtKB | A comprehensive resource for protein sequence and functional information. It provides a standardized set of canonical protein sequences and functional annotations critical for interpreting the functional impact of genomic variants [71]. |
Cloud-Based Platforms for Scalable Data Analysis and Collaboration
Technical Support Center: Troubleshooting NGS Data Analysis Bottlenecks in Chemogenomics
Frequently Asked Questions (FAQs)
1. What are the most common computational bottlenecks in NGS data analysis for chemogenomics screening?
The most frequent bottlenecks occur during the secondary analysis phase, particularly in data alignment and variant calling, which are computationally intensive [51]. These steps require powerful servers and optimized workflows; without proper resources, analyses may be prohibitively slow or fail altogether [51]. Managing the massive volume of data, often terabytes per project, also demands scalable storage and processing solutions that exceed the capabilities of traditional on-premises systems [24].
2. How can cloud computing specifically address these bottlenecks for a typical academic research lab?
Cloud platforms provide on-demand, scalable infrastructure that eliminates the need for large capital investments in local hardware [24] [73]. They offer dynamic scalability, allowing researchers to access advanced computational tools for specific projects and scale down during less intensive periods, optimizing costs [74]. Furthermore, cloud environments facilitate global collaboration, enabling researchers from different institutions to work on the same datasets in real-time [24].
3. Our team lacks extensive bioinformatics expertise. What cloud solutions can help us analyze NGS data from compound-treated cell lines?
Purpose-built managed services are ideal for this scenario. AWS HealthOmics, for example, allows the execution of standardized bioinformatics pipelines (e.g., those written in Nextflow or WDL) without the need to manage the underlying infrastructure [75] [74]. Alternatively, you can leverage AI-powered platforms that provide a natural language interface, allowing you to ask complex questions (e.g., "Which samples show differential expression in target gene X after treatment?") without writing custom scripts or complex SQL queries [75].
4. What are the key cost considerations when moving NGS data analysis to the cloud?
Costs are primarily driven by data storage, computational processing, and data egress. A benchmark study on Google Cloud Platform compared two common pipelines and found costs were manageable and predictable [73]. You can control storage costs by leveraging different storage tiers (e.g., moving raw data from older projects to low-cost archive storage) and optimizing compute costs by selecting the right virtual machine for the pipeline and using spot instances where possible [73] [74].
Table 1: Benchmarking Cost and Performance for Germline Variant Calling Pipelines on Google Cloud Platform (GCP) [73]
| Pipeline Name | Virtual Machine Configuration | Baseline Cost per Hour | Use Case |
|---|---|---|---|
| Sentieon DNASeq | 64 vCPUs, 57 GB Memory | $1.79 | CPU-accelerated processing |
| Clara Parabricks Germline | 48 vCPUs, 58 GB Memory, 1 NVIDIA T4 GPU | $1.65 | GPU-accelerated processing |
5. How do we ensure the security and privacy of sensitive chemogenomics data in the cloud?
Reputable cloud providers comply with strict regulatory frameworks like HIPAA and GDPR, providing a foundation for secure data handling [24]. Security is managed through a shared responsibility model: the provider secures the underlying infrastructure, while your organization is responsible for configuring access controls, encrypting data, and managing user permissions using built-in tools like AWS Identity and Access Management (IAM) [75] [74].
Troubleshooting Guides
Problem: Slow or Failed Alignment of NGS Reads
- Symptoms: The alignment step (e.g., using BWA or Bowtie 2) takes an excessively long time, fails to complete, or produces a high rate of unmapped reads [51] [76].
- Potential Causes and Solutions:
- Insufficient Computational Resources: Alignment is computationally demanding. Solution: On the cloud, switch to a virtual machine instance with more CPUs and memory. Consider using compute-optimized instances [73].
- Poor Read Quality: Low-quality reads cannot be mapped confidently. Solution: Always perform rigorous quality control (QC) as the first step. Use tools like FastQC to check for per-base sequence quality, adapter contamination, and overrepresented sequences. Trim low-quality bases and adapters from your reads before alignment [76].
- Incorrect Reference Genome: Using an outdated or incorrect reference genome will cause alignment failures. Solution: Ensure you are using the correct, most recent version of the reference genome (e.g., GRCh38/hg38 for human data) and be consistent across all analyses [76].
Problem: High Error Rate or Artifacts in Variant Calling
- Symptoms: The final VCF file contains an implausibly high number of variants, many of which are likely false positives, or known variants are missing [51].
- Potential Causes and Solutions:
- Inadequate Removal of PCR Duplicates: PCR duplicates can artificially inflate coverage and lead to false variant calls. Solution: Ensure your pipeline includes a duplicate marking/removal step. Using Unique Molecular Identifiers (UMIs) during library preparation can help correctly identify and account for PCR duplicates [76].
- Poorly Calibrated Base Quality Scores: Systematic errors in base quality scores can mislead the variant caller. Solution: Implement a base quality score recalibration (BQSR) step in your workflow, which is a standard part of best-practice pipelines like GATK, Sentieon, and Parabricks [73] [75].
- Low Sequencing Depth: Regions with very low coverage (<20x-30x for whole genomes) lack the statistical power to call variants reliably. Solution: Check the coverage in problematic regions using your BAM file. For critical regions or samples, you may need to sequence to a higher depth [76].
Problem: Difficulty Managing and Querying Large Multi-Sample VCF Files
- Symptoms: It becomes slow and cumbersome to find specific variants (e.g., "all pathogenic variants in gene BRCA1 across all treated samples") from a large, multi-sample VCF file [75].
- Potential Causes and Solutions:
- Analysis on Flat Files: Trying to query large VCF files directly is computationally inefficient. Solution: Transform your annotated VCF files into a structured, query-optimized format. On AWS, you can use Amazon S3 Tables with PyIceberg to convert VCF data into a structured table format (like Apache Iceberg) that can be queried efficiently using SQL with Amazon Athena [75]. This enables rapid, complex queries across millions of variants.
Experimental Protocol: Implementing a Cloud-Based NGS Analysis Pipeline
This protocol outlines the steps to deploy and run an ultra-rapid germline variant calling pipeline on Google Cloud Platform, suitable for analyzing genomic data from control or compound-treated cell lines [73].
1. Prerequisites
- A GCP account with billing enabled.
- A valid software license (if using a commercial tool like Sentieon).
- Raw sequencing data in FASTQ format, stored in a Google Cloud Storage bucket.
2. Computational Resource Configuration
- Based on your chosen pipeline, create a virtual machine (VM) with an appropriate configuration.
3. Pipeline Execution Steps The following workflow details the core steps for secondary analysis, which are common across most pipelines. This process converts raw sequencing reads (FASTQ) into a list of genetic variants (VCF).
NGS Secondary Analysis Workflow
- Step 1: Quality Control (QC) and Read Cleanup. Use a tool like FastQC to assess the quality of the raw sequencing data. Following this, trim adapters and low-quality bases from the reads to produce a "cleaned" FASTQ file [76].
- Step 2: Sequence Alignment. Align the cleaned reads to a reference genome using an aligner like BWA or Bowtie 2. This step produces a BAM file containing the mapped reads [76].
- Step 3: Post-Alignment Processing. This includes:
- Marking duplicates: Identify and tag PCR duplicate reads to avoid overcounting.
- Base Quality Score Recalibration (BQSR): Correct systematic errors in the base quality scores.
- Step 4: Variant Calling. Call genomic variants (SNPs, indels) using a tool like GATK HaplotypeCaller or its equivalent in Sentieon/Parabricks. This generates a raw VCF file [73] [75].
- Step 5: Variant Filtering and Annotation. Filter the raw variants based on quality metrics and annotate them with functional predictions (using tools like VEP - Variant Effect Predictor) and clinical significance (from databases like ClinVar) [75].
4. Downstream Analysis and Cost Management
- Once the VCF is generated, proceed with tertiary analysis specific to your chemogenomics project (e.g., identifying treatment-specific variants).
- To manage costs, remember to stop or delete your cloud VM when the analysis is complete to avoid ongoing charges [73].
The Scientist's Toolkit: Essential Research Reagents & Computational Solutions
Table 2: Key Resources for NGS-based Chemogenomics Experiments
| Item | Function / Purpose |
|---|---|
| Twist Core Exome Capture | For target enrichment to focus sequencing on protein-coding regions, commonly used in chemogenomics studies [73]. |
| Illumina NextSeq 500 | A high-throughput sequencing platform frequently used for large-scale genomic screens, generating paired-end reads [73]. |
| Unique Molecular Identifiers (UMIs) | Short nucleotide barcodes added to each molecule before amplification to correct for PCR duplicates and improve quantification accuracy [76]. |
| Sentieon DNASeq Pipeline | A highly optimized, CPU-based software for rapid and accurate secondary analysis from FASTQ to VCF, reducing runtime significantly [73]. |
| NVIDIA Clara Parabricks | A GPU-accelerated software suite that provides a rapid implementation of common secondary analysis tools like GATK [73]. |
| Variant Effect Predictor (VEP) | A tool for annotating genomic variants with their functional consequences (e.g., missense, stop-gain) on genes and transcripts [75]. |
| ClinVar Database | A public archive of reports detailing the relationships between human genomic variants and phenotypes with supporting evidence [75]. |
The following diagram illustrates the event-driven serverless architecture for a scalable NGS analysis pipeline on AWS, which automates the workflow from data upload to queryable results.
Cloud NGS Analysis Architecture
Benchmarking and Clinical Translation: Ensuring Reliability in Chemogenomics Insights
Validation Frameworks for NGS-Based Biomarker Discovery
In chemogenomics research, the transition from discovering a potential biomarker to its clinical application is a critical and complex journey. A validation framework ensures that a biomarker's performance is accurately characterized, guaranteeing its reliability for downstream analysis and clinical decision-making. Within the context of NGS data analysis bottlenecks, a robust validation strategy is your primary defense against analytical false positives, irreproducible results, and the costly failure of experimental programs.
Core Principles of Analytical Validation
Analytical validation is a prerequisite for using any NGS-based application as a reliable tool. It demonstrates that the test consistently and accurately measures what it is intended to measure [77]. For an NGS-based qualitative test used in pharmacogenetic profiling or chemogenomics, a comprehensive analytical validation must, at a minimum, address the following performance criteria [77]:
- Accuracy: The closeness of agreement between a test result and an accepted reference value. This is often evaluated in terms of Positive Percent Agreement (PPA) and Negative Percent Agreement (NPA) when compared to a validated reference method [77].
- Precision: The closeness of agreement between independent results obtained under stipulated conditions. This includes assessments of both reproducibility (across days, operators, instruments) and repeatability (within a single run) [77].
- Limit of Detection (LOD): The lowest amount or concentration of an analyte in a sample that can be reliably detected with a stated probability. This is crucial for detecting low-frequency variants in tumor samples or liquid biopsies.
- Analytical Specificity: The ability of an assay to detect only the intended analyte. This includes evaluating interference from endogenous and exogenous substances, cross-reactivity, and cross-contamination [77].
The following table summarizes the key performance criteria that should be evaluated during analytical validation of an NGS-based biomarker test.
Table 1: Key Analytical Performance Criteria for NGS-Based Biomarker Tests
| Performance Criterion | Description | Common Evaluation Metrics |
|---|---|---|
| Accuracy [77] | Agreement between the test result and a reference standard. | Positive Percent Agreement (PPA), Negative Percent Agreement (NPA), Positive Predictive Value (PPV) |
| Precision [77] | Closeness of agreement between independent results. | Repeatability, Reproducibility |
| Limit of Detection (LOD) [77] | Lowest concentration of an analyte that can be reliably detected. | Variant Allele Frequency (VAF) at a defined coverage |
| Analytical Specificity [77] | Ability to assess the analyte without interference from other components. | Assessment of interference, cross-reactivity, and cross-contamination |
| Reportable Range [77] | The range of values an assay can report. | The spectrum of genetic variants the test can detect |
The Biomarker Validation Workflow: From Discovery to Clinical Application
A structured workflow is essential for successful biomarker development. This process bridges fundamental research and clinical application, ensuring that biomarkers are not only discovered but also rigorously vetted for real-world use. The following diagram illustrates the key stages of this workflow.
Diagram 1: The Biomarker Development and Validation Workflow
Phase 1: Study Design and Sample Collection
A flawed design at this initial stage can invalidate all subsequent work.
- Precisely Define Objectives: Clearly define the scientific objective and scope, including precise primary and secondary biomedical outcomes and detailed subject inclusion/exclusion criteria [78].
- Ensure Proper Powering: Perform sample size determination to ensure the study is adequately powered to detect a statistically significant effect, preventing wasted resources on underpowered studies [78].
- Plan for Confounders: Account for potential confounding factors in the sampling design. For predictive studies, select covariates based on their ability to increase predictive performance [78].
Phase 2: Quality Control and Data Preprocessing
Biomedical data is affected by multiple sources of noise and bias. Quality control and preprocessing are critical to discriminate between technical noise and biological variance [78].
- Implement Rigorous QC: Use data type-specific quality control tools, such as FastQC for NGS data, to perform statistical outlier checks and compute quality metrics [78] [79].
- Preprocess and Filter Data: Remove adapter sequences and trim low-quality bases from reads to improve downstream analysis accuracy [79]. Filter out uninformative features, such as those with zero or small variance, and consider imputation for missing values [78].
- Standardize Data: Apply standardization or transformation (e.g., variance-stabilizing transformations for omics data) to make features comparable and meet model assumptions [78].
Phase 3: Biomarker Discovery and Candidate Selection
This phase involves processing and interpreting the data to identify promising biomarker candidates.
- Variant Calling and Annotation: Select an appropriate variant caller (e.g., for germline, somatic, or RNA-seq data) and fine-tune its parameters to optimize sensitivity and specificity [79]. Annotate called variants with their genomic location, functional impact, and population frequency [79].
- Data Integration: Effectively integrate different data types (e.g., clinical and omics data) using early, intermediate, or late integration strategies to gain a comprehensive view [78].
- Assess Added Value: When traditional clinical markers are available, conduct comparative evaluations to determine if omics-based biomarkers provide a significant added value for decision-making [78].
Phase 4: Analytical and Clinical Validation
Selected biomarkers must undergo rigorous validation to confirm their accuracy, reliability, and clinical relevance [80].
- Analytical Validation: As detailed in Table 1, this step confirms the test itself is robust [77].
- Clinical Validation: This separate process establishes the biomarker's clinical utility—does it effectively diagnose, predict, or prognosticate a disease state in the intended patient population?
Phase 5: Clinical Implementation
Once validated, biomarkers can be integrated into clinical practice to support diagnostics and personalized treatment. Continuous monitoring is required to ensure ongoing efficacy and safety [80].
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ: Pre-Analytical and Experimental Setup
Q1: My NGS library yield is unexpectedly low. What are the most common causes?
Low library yield is a frequent challenge with several potential root causes. The following table outlines the primary culprits and their solutions.
Table 2: Troubleshooting Guide for Low NGS Library Yield
| Root Cause | Mechanism of Yield Loss | Corrective Action |
|---|---|---|
| Poor Input Quality / Contaminants [2] | Enzyme inhibition from residual salts, phenol, or EDTA. | Re-purify input sample; ensure 260/230 > 1.8; use fluorometric quantification (Qubit) over UV. |
| Inaccurate Quantification / Pipetting Error [2] | Suboptimal enzyme stoichiometry due to concentration errors. | Calibrate pipettes; use master mixes; rely on fluorometric methods for template quantification. |
| Fragmentation / Tagmentation Inefficiency [2] | Over- or under-fragmentation reduces adapter ligation efficiency. | Optimize fragmentation time/energy; verify fragmentation profile before proceeding. |
| Suboptimal Adapter Ligation [2] | Poor ligase performance or incorrect adapter-to-insert ratio. | Titrate adapter:insert ratio; ensure fresh ligase and buffer; maintain optimal temperature. |
| Overly Aggressive Purification [2] | Desired fragments are excluded during size selection or cleanup. | Optimize bead-to-sample ratios; avoid over-drying beads during clean-up steps. |
Q2: My sequencing data shows high duplication rates or adapter contamination. How do I fix this?
These issues typically originate from library preparation.
- High Duplication Rates: This often indicates low input material or over-amplification during PCR. To fix this, increase the amount of starting material and reduce the number of PCR cycles. Overcycling introduces size bias and duplicates [2].
- Adapter Contamination: This is signaled by a sharp peak around 70-90 bp on an electropherogram. The cause is typically inefficient ligation or an incorrect adapter-to-insert molar ratio (excess adapters). The solution is to titrate the adapter concentration and ensure optimal ligation reaction conditions [2].
FAQ: Data Analysis and Computational Bottlenecks
Q3: What are the best practices for NGS data analysis to ensure reliable biomarker identification?
Following a structured pipeline is key to avoiding pitfalls.
- Do Not Skip QC: "Insufficient QC can lead to inaccurate results and wasted effort" [79]. Always use tools like FastQC to assess raw read quality.
- Choose and Tune Tools Appropriately: Avoid over-reliance on default settings for aligners and variant callers. "Misconfigured alignment parameters can result in suboptimal alignments and missed variants" [79]. Optimize parameters for your specific data (genome size, read length).
- Filter Variants Stringently: "Failure to filter variants appropriately can lead to the inclusion of false positives and irrelevant variants" [79]. Use metrics like variant quality score, depth of coverage, and allele frequency.
- Provide Biological Context: "Interpreting variants without considering biological context can lead to misleading conclusions" [79]. Use biological databases and knowledge to interpret the significance of identified variants.
Q4: How can we manage the computational bottlenecks associated with large-scale NGS data analysis?
With sequencing costs falling, computation has become a significant part of the total cost and time investment [7]. Key strategies include:
- Evaluate Trade-offs: Consider the trade-off between accuracy and computational cost. For example, a slower algorithm may be 5% more accurate but take 10 times longer. You must decide if the accuracy gain is worth the computational expense for your specific application [7].
- Leverage Accelerated Hardware: Using hardware accelerators like GPUs (e.g., Illumina's Dragen system) can reduce a 10-hour analysis to under an hour, though it may come at a higher direct compute cost [7].
- Consider Cloud Computing: The cloud offers flexibility. You can choose to run analyses on standard hardware for lower cost or on accelerated hardware for speed, making hardware decisions a part of every experimental analysis rather than a fixed infrastructure choice [7].
- Explore Approximate Methods: For some applications, "sketching" methods that use lossy approximations can provide orders-of-magnitude speed-up by capturing only the most important features of the data, though this comes at the cost of perfect accuracy [7].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key reagents and materials used in NGS-based biomarker discovery, along with their critical functions.
Table 3: Research Reagent Solutions for NGS-Based Biomarker Discovery
| Item | Function |
|---|---|
| Nucleic Acid Extraction Kits | To isolate high-quality, intact DNA/RNA from various sample types (tissue, blood, FFPE) for library preparation. |
| Library Preparation Kits | To fragment nucleic acids, ligate platform-specific sequencing adapters, and often incorporate sample barcodes. |
| Target Enrichment Panels | To selectively capture genomic regions of interest (e.g., a cancer gene panel) from a complex whole genome library. |
| High-Fidelity DNA Polymerase | For accurate amplification of library molecules during PCR steps, minimizing the introduction of errors. |
| Size Selection Beads | To purify and select for library fragments within a specific size range, removing adapter dimers and overly long fragments. |
| QC Instruments (e.g., BioAnalyzer, Qubit) | To accurately quantify and assess the size distribution of libraries before sequencing. |
Navigating the path of NGS-based biomarker discovery requires a disciplined approach grounded in a robust validation framework. By adhering to structured workflows, implementing rigorous quality control, understanding and mitigating common experimental and computational bottlenecks, and proactively troubleshooting issues, researchers can overcome the significant bottlenecks in chemogenomics research. This disciplined process transforms raw genomic data into reliable, clinically actionable biomarkers, ultimately advancing the field of personalized medicine.
Comparative Analysis of Short-Read vs. Long-Read Sequencing Platforms
Next-generation sequencing (NGS) technologies have become fundamental tools in chemogenomics and drug development research. The choice between short-read and long-read sequencing platforms directly impacts the ability to resolve complex genomic regions, identify structural variants, and phase haplotypes—all critical for understanding drug response and toxicity. This technical support resource compares these platforms, addresses common experimental bottlenecks, and provides troubleshooting guidance to inform sequencing strategy in preclinical research.
Short-read sequencing (50-300 base pairs) and long-read sequencing (5,000-30,000+ base pairs) employ fundamentally different approaches to DNA sequencing, each with distinct performance characteristics [81] [82].
Table 1: Key Technical Specifications of Major Sequencing Platforms
| Feature | Short-Read Platforms (Illumina) | PacBio SMRT | Oxford Nanopore |
|---|---|---|---|
| Typical Read Length | 50-300 bp [83] | 10,000-25,000 bp [36] | 10,000-30,000 bp (up to 1 Mb+) [81] [36] |
| Primary Chemistry | Sequencing-by-Synthesis (SBS) [36] | Single-Molecule Real-Time (SMRT) [81] | Nanopore Electrical Sensing [81] |
| Accuracy | High (>Q30) [81] | HiFi Reads: >Q30 (99.9%) [81] [84] | Raw: ~Q20-30; Consensus: Higher [81] [85] |
| DNA Input | Low to Moderate | High Molecular Weight DNA critical [86] | High Molecular Weight DNA preferred |
| Library Prep Time | Moderate | Longer, more complex [86] | Rapid (minutes for some kits) |
| Key Applications | SNP calling, small indels, gene panels, WES, WGS [83] | SV detection, haplotype phasing, de novo assembly [81] | SV detection, real-time sequencing, direct RNA-seq [84] [82] |
Table 2: Performance Comparison for Key Genomic Applications
| Application | Short-Read Performance | Long-Read Performance |
|---|---|---|
| SNP & Small Indel Detection | Excellent (High accuracy, depth) [87] | Good (with HiFi/consensus) [81] |
| Structural Variant Detection | Limited for large SVs [83] | Excellent (spans complex events) [84] [86] |
| Repetitive Region Resolution | Poor (fragmentation issue) [81] | Excellent (spans repeats) [81] [86] |
| Haplotype Phasing | Limited (statistical phasing) | Excellent (direct phasing) [84] [86] |
| De Novo Assembly | Challenging (fragmented contigs) [84] | Excellent (continuous contigs) [87] |
| Methylation Detection | Requires bisulfite conversion | Direct detection (native DNA) [84] |
Platform Selection Guide for Chemogenomics
Choosing the right platform depends on the specific research question. The decision workflow below outlines key considerations for common scenarios in drug development.
Decision Workflow for Sequencing Platform Selection
Resolving Complex Pharmacogenes
Many genes critical for drug metabolism (e.g., CYP2D6, CYP2A7, CYP2B6) contain complex regions with pseudogenes, high homology, or structural variants that challenge short-read platforms [88]. Long-read sequencing excels here by spanning these complex architectures to provide full gene context and accurate haplotyping [88] [84].
Detecting Structural Variants and Repeat Expansions
Short-read sequencing often fails to identify large structural variants (deletions, duplications, inversions) and cannot resolve repeat expansion disorders when the expansion length exceeds the read length [83]. Long-read sequencing enables direct detection of these variants, which is crucial for understanding disease mechanisms and drug resistance [84].
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Our short-read data shows poor coverage in GC-rich regions of a key pharmacogene. What are our options?
A: GC bias during PCR amplification in short-read library prep can cause this [81]. Solutions include:
- Protocol Adjustment: Use PCR-free library preparation kits to eliminate amplification bias.
- Platform Switch: Employ long-read sequencing (PacBio or Nanopore), which uses PCR-free protocols and does not exhibit the same GC bias [84].
Q2: We suspect a complex structural variant is causing an adverse drug reaction. How can we confirm this?
A: Short-read sequencing often struggles with complex SVs [83]. A targeted long-read approach is recommended:
- Confirmatory Experiment: Design PCR primers flanking the suspected SV region.
- Long-Read Sequencing: Sequence the large amplicon on a PacBio or Nanopore platform. The long read will span the entire variant, revealing its precise structure [84].
Q3: Can we use long-read sequencing for high-throughput SNP validation in large sample cohorts?
A: While long-read accuracy has improved, short-read platforms (like Illumina NovaSeq) currently offer higher throughput, lower per-sample cost, and proven accuracy for large-scale SNP screening [81] [87]. For cost-effective SNP validation in hundreds to thousands of samples, short-read remains the preferred choice. Reserve long-read for cases requiring phasing or complex region resolution.
Common Experimental Issues and Solutions
Table 3: Troubleshooting Common Sequencing Problems
| Problem | Potential Causes | Solutions |
|---|---|---|
| Low Coverage in Repetitive Regions (Short-Read) | Short fragments cannot be uniquely mapped [81]. | Use long-read sequencing to span repetitive elements [86]. |
| Insufficient Long-Read Yield | DNA degradation; poor HMW DNA quality [86]. | Optimize DNA extraction (use fresh samples, HMW protocols), check DNA quality with pulsed-field gel electrophoresis. |
| High Error Rate in Long Reads | Raw reads have random errors (PacBio) or systematic errors (ONT) [81] [85]. | Generate HiFi reads (PacBio) or apply consensus correction (ONT) via increased coverage [81] [84]. |
| Difficulty Phasing Haplotypes | Short reads lack connecting information [83]. | Use long-read sequencing for direct phasing, or consider linked-read technology as an alternative [86]. |
Essential Research Reagent Solutions
Successful sequencing experiments, particularly in challenging genomic regions, require high-quality starting materials and appropriate library preparation kits.
Table 4: Key Reagents and Their Functions in NGS Workflows
| Reagent / Kit Type | Function | Consideration for Chemogenomics |
|---|---|---|
| High Molecular Weight (HMW) DNA Extraction Kits | Preserves long DNA fragments crucial for long-read sequencing. | Critical for analyzing large structural variants in pharmacogenes [86]. |
| PCR-Free Library Prep Kits (Short-Read) | Prevents amplification bias in GC-rich regions. | Improves coverage uniformity in genes with extreme GC content [81]. |
| Target Enrichment Panels (e.g., Hybridization Capture) | Isolates specific genes of interest from the whole genome. | Custom panels can focus sequencing on a curated set of 100+ pharmacogenes [88]. |
| SMRTbell Prep Kit (PacBio) | Prepares DNA libraries for PacBio circular consensus sequencing. | Enables high-fidelity (HiFi) sequencing of complex diploid regions [81]. |
| Ligation Sequencing Kit (Oxford Nanopore) | Prepares DNA libraries for nanopore sequencing by adding motor proteins. | Allows for direct detection of base modifications (e.g., methylation) from native DNA [84]. |
Short-read and long-read sequencing are complementary technologies in the chemogenomics toolkit. Short-read platforms offer a cost-effective solution for high-confidence variant detection across exomes and targeted panels, while long-read technologies are indispensable for resolving complex genomic landscapes, including repetitive regions, structural variants, and highly homologous pharmacogenes. The choice of platform should be driven by the specific biological question. As both technologies continue to evolve in accuracy and throughput, hybrid approaches that leverage the strengths of each will provide the most comprehensive insights for drug development and personalized medicine.
Benchmarking AI Tools Against Traditional Analysis Methods
Troubleshooting Guides and FAQs
Data Quality and Preprocessing
Q: My AI model for variant calling is underperforming, showing low accuracy compared to traditional methods. What could be wrong?
A: This common issue often stems from inadequate training data or data quality problems. Ensure your dataset has sufficient coverage depth and diversity. Traditional variant callers like GATK rely on statistical models that may be more robust with limited data, while AI tools like DeepVariant require comprehensive training sets to excel [31]. Check that your training data includes diverse genetic contexts and that sequencing quality metrics meet minimum thresholds (Q-score >30 for Illumina data). Consider using hybrid approaches where AI handles complex variants while traditional methods process straightforward regions [24] [26].
Q: How do I handle batch effects when benchmarking AI tools across multiple sequencing runs?
A:* Batch effects significantly impact both AI and traditional methods. Implement these steps:
- Use positive control samples across all batches
- Apply harmonization methods like ComBat before analysis
- For AI specifically, include batch identity as a covariate during training
- Validate with external datasets not used in training Traditional methods often incorporate batch adjustment in their statistical models, while AI approaches may require explicit training on multi-batch data to generalize properly [26] [69].
Tool Selection and Implementation
Q: When should I choose AI-based tools over traditional methods for chemogenomics applications?
A:* The decision depends on your specific application and resources. Use this comparative table to guide your selection:
| Application | Recommended AI Tools | Traditional Alternatives | Best Use Cases |
|---|---|---|---|
| Variant Calling | DeepVariant, Clair3 [31] | GATK, Samtools [24] | Complex variants, long-read data |
| Somatic Mutation Detection | NeuSomatic, SomaticSeq [31] | Mutect2, VarScan2 [24] | Low-frequency variants, heterogeneous tumors |
| Base Calling | Bonito, Dorado [31] | Albacore, Guppy [36] | Noisy long-read data |
| Methylation Analysis | DeepCpG [31] | Bismark, MethylKit [24] | Pattern recognition in epigenomics |
| Multi-omics Integration | MOFA+, MAUI [31] | PCA, mixed models [24] | High-dimensional data integration |
AI tools typically excel with complex patterns and large datasets, while traditional methods offer better interpretability and stability with smaller samples [26] [31].
Q: What computational resources are necessary for implementing AI tools in our NGS pipeline?
A:* AI tools demand significant resources, which is a key bottleneck. Cloud platforms like AWS HealthOmics and Google Cloud Genomics provide scalable solutions, connecting over 800 institutions globally [69]. Minimum requirements include:
- Storage: 1TB+ for model weights and sequencing data
- Memory: 32GB RAM minimum, 128GB+ for large models
- GPU: NVIDIA cards with 16GB+ VRAM for training
- Processing: Traditional methods often use CPU-intensive processes, while AI leverages GPU acceleration [24] [69]
Traditional tools may complete analyses in hours on standard servers, while AI training requires substantial upfront investment but faster inference times once deployed [69].
Benchmarking Methodologies
Q: How do I design a rigorous benchmarking study comparing AI and traditional NGS analysis methods?
A:* Follow this experimental protocol for comprehensive benchmarking:
Experimental Design
- Dataset Curation: Use standardized benchmarks like GUANinE, which provides large-scale, denoised genomic tasks with proper controls [89]
- Performance Metrics: Evaluate using multiple metrics - accuracy, precision, recall, F1-score, computational efficiency, and reproducibility
- Statistical Power: Ensure sufficient sample size (typically thousands of variants or sequences) to detect significant differences
- Validation: Include orthogonal validation through experimental methods like PCR or Sanger sequencing
Implementation Workflow
This methodology ensures fair comparison while accounting for the different operational characteristics of AI versus traditional approaches [90] [89] [91].
Q: What are the key benchmarking metrics for evaluating NGS analysis tools in chemogenomics?
A:* Use this comprehensive metrics table:
| Metric Category | Specific Metrics | AI Tool Considerations | Traditional Tool Considerations |
|---|---|---|---|
| Accuracy | Precision, Recall, F1-score, AUROC | Training data dependence [31] | Statistical model robustness [24] |
| Computational | CPU/GPU hours, Memory usage, Storage | High GPU demand for training [69] | CPU-intensive, consistent memory [24] |
| Scalability | Processing time vs. dataset size | Better scaling with large data [26] | Linear scaling, predictable [36] |
| Reproducibility | Result consistency across runs | Model stability issues [90] | High reproducibility [24] |
| Interpretability | Feature importance, Explainability | Requires XAI methods [92] | Built-in statistical interpretability [24] |
| Clinical Utility | Positive predictive value, Specificity | FDA validation requirements | Established clinical validity [93] |
Interpretation and Validation
Q: How can I improve interpretability of AI tool outputs for regulatory submissions?
A:* Implement Explainable AI (XAI) methods to address the "black box" problem. BenchXAI evaluations show that Integrated Gradients, DeepLift, and DeepLiftShap perform well across biomedical data types [92]. For chemogenomics applications:
- Use saliency maps to highlight influential genomic regions
- Apply perturbation tests to validate feature importance
- Compare AI decisions with known biological mechanisms
- Utilize ensemble approaches combining multiple XAI methods Traditional methods naturally provide interpretable outputs through p-values, confidence intervals, and explicit statistical models, which remains a significant advantage for regulatory acceptance [24] [92].
Q: We're seeing discrepant results between AI and traditional methods for variant calling. How should we resolve these conflicts?
A:* Discrepancies often reveal meaningful biological or technical insights. Follow this resolution workflow:
Prioritize traditional methods in well-characterized genomic regions while considering AI tools for complex variants where they demonstrate superior performance in benchmarking studies [24] [31].
Research Reagent Solutions
| Reagent/Tool | Function | Application in Benchmarking |
|---|---|---|
| GUANinE Benchmark [89] | Standardized evaluation dataset | Provides controlled comparison across tools |
| BLURB Benchmark [91] | Biomedical language understanding | NLP tasks in chemogenomics |
| BenchXAI [92] | Explainable AI evaluation | Interpreting AI tool decisions |
| Reference Materials (GIAB) | Ground truth genetic variants | Validation standard for variant calling |
| Cloud Computing Platforms (AWS, Google Cloud) [69] | Scalable computational resources | Equal resource allocation for fair comparison |
| Multi-omics Integration Tools (MOFA+) [31] | Integrated data analysis | Cross-platform performance assessment |
Leveraging Therapeutic Drug Monitoring Data for Variant Validation
The integration of Therapeutic Drug Monitoring (TDM) data with Next-Generation Sequencing (NGS) represents a powerful approach for addressing critical bottlenecks in chemogenomics research. TDM, the clinical practice of measuring specific drug concentrations in a patient's bloodstream to optimize dosage regimens, provides crucial phenotypic data on drug response [94]. When correlated with genomic variants identified through NGS, researchers can validate which genetic alterations have functional consequences on drug pharmacokinetics and pharmacodynamics [52] [95]. This integration is particularly valuable for drugs with narrow therapeutic ranges, marked pharmacokinetic variability, and those known to cause therapeutic and adverse effects [94]. However, this multidisciplinary approach faces significant technical challenges, including NGS data variability, TDM assay validation requirements, and computational bottlenecks that must be systematically addressed [95] [51] [96].
Frequently Asked Questions (FAQs)
1. How can TDM data specifically help validate genetic variants found in NGS analysis?
TDM provides direct biological evidence of a variant's functional impact by revealing how it affects drug concentration-response relationships [94]. For example, if NGS identifies a variant in a drug metabolism gene, consistently elevated or reduced drug concentrations in patients with that variant (as measured by TDM) provide functional validation that the variant alters drug processing. This moves beyond computational predictions of variant impact to empirical validation using pharmacokinetic and pharmacodynamic data [52] [94].
2. What are the most critical quality control measures when correlating TDM results with NGS data?
The essential quality control measures span both domains:
- For TDM: Demonstrate acceptable inaccuracy (bias), within-run imprecision (repeatability), and between-run imprecision (intermediate precision) using established clinical criteria [97] [98].
- For NGS: Implement robust quality control at every stage, from sequencing accuracy to variant calling, using standardized pipelines to reduce inconsistencies [51].
- Integrated QC: Ensure consistent sample pairing and temporal alignment between TDM measurements and NGS analysis [95] [97].
3. Our NGS pipeline identifies multiple potentially significant variants. How should we prioritize them for TDM correlation?
Prioritization should consider:
- Variants in genes with known roles in drug absorption, distribution, metabolism, and excretion (ADME)
- Variants predicted to have high functional impact by multiple algorithms (SIFT, PolyPhen, etc.)
- Variants with population frequency that doesn't contradict the observed drug response phenotype
- Nonsynonymous coding variants and splice-site variants over non-coding variants This prioritized approach ensures efficient use of resources by focusing on the most biologically plausible candidates [52] [95].
4. What technical challenges might cause discrepancies between TDM and NGS results?
Several technical factors can cause discrepancies:
- NGS sequencing errors or misalignment, particularly in complex genomic regions
- TDM assay variability between different analytical platforms or reagent lots
- Incorrect timing of blood sampling for TDM in relation to drug administration
- Somatic vs. germline variant considerations in oncology settings
- Population-specific differences in linkage disequilibrium that complicate variant interpretation
- Drug-drug interactions that confound the genotype-phenotype correlation [94] [51] [97].
Troubleshooting Guides
Problem 1: Inconsistent Variant Validation Across Multiple TDM Datasets
Symptoms: A genetic variant shows strong correlation with TDM data in one patient cohort but fails to replicate in subsequent studies.
Potential Causes and Solutions:
Table 1: Troubleshooting Inconsistent Variant Validation
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Population Stratification | Perform principal component analysis on genomic data to identify population substructure. | Include population structure as a covariate in association analyses or use homogeneous cohorts. |
| Differences in TDM Methodology | Compare coefficient of variation (CV) values between studies; review calibration methods. | Standardize TDM protocols across sites; use common reference materials and calibrators [99] [97]. |
| Confounding Medications | Review patient medication records for drugs known to interact with the target drug. | Exclude patients with interacting medications or statistically adjust for polypharmacy. |
| Insufficient Statistical Power | Calculate power based on effect size, minor allele frequency, and sample size. | Increase sample size through multi-center collaborations or meta-analysis. |
Problem 2: High Measurement Uncertainty in TDM Data Compromising Variant Correlation
Symptoms: Weak or non-significant correlations between genetic variants and drug concentrations despite strong biological plausibility.
Potential Causes and Solutions:
Table 2: Addressing TDM Measurement Uncertainty
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Poor Assay Precision | Calculate within-run and between-run coefficients of variation (CV) using patient samples [97]. | Implement stricter quality control protocols; consider alternative analytical methods with better precision. |
| Calibrator Inaccuracy | Compare calibrators against reference standards; participate in proficiency testing programs. | Use certified reference materials; establish traceability to reference methods [99]. |
| Platform Differences | Conduct method comparison studies between different analytical systems. | Standardize on a single platform across studies or establish reliable cross-walk formulas [97]. |
| Sample Timing Issues | Audit sample collection times relative to drug administration. | Implement strict protocols for trough-level sampling or other standardized timing. |
Problem 3: NGS Bioinformatics Bottlenecks Delaying Integrated Analysis with TDM
Symptoms: Long turnaround times from raw sequencing data to variant calls impede timely correlation with TDM results.
Potential Causes and Solutions:
Symptoms: Bioinformatics processing requires excessive computational time and resources, creating analysis bottlenecks.
Potential Causes and Solutions:
Table 3: Overcoming NGS Bioinformatics Bottlenecks
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Suboptimal Workflow Management | Document computational steps and parameters; identify slowest pipeline stages. | Implement standardized workflow languages (CWL) and container technologies (Docker) for reproducibility and efficiency [95] [96]. |
| Insufficient Computational Resources | Monitor CPU, memory, and storage utilization during analysis. | Utilize cloud-based platforms (DNAnexus, Seven Bridges) that offer scalable computational resources [95] [96]. |
| Inefficient Parameter Settings | Profile different parameter combinations on a subset of data. | Optimize tool parameters for specific applications rather than using default settings. |
| Data Transfer Delays | Measure data transfer times between sequencing instruments and analysis servers. | Implement local computational infrastructure or high-speed dedicated network connections. |
Experimental Protocols
Protocol 1: Validating Pharmacogenomic Variants Using TDM Data
Purpose: To empirically validate the functional impact of genetic variants on drug metabolism using therapeutic drug monitoring data.
Materials:
- Patient cohorts with appropriate drug exposure
- DNA samples from whole blood or saliva
- TDM samples (serum, plasma, or whole blood)
- NGS library preparation kit
- TDM analytical platform (e.g., HPLC/MS, immunoassay)
Methodology:
- Patient Selection and Stratification:
- Recruit patients undergoing treatment with the target drug
- Exclude patients with known drug interactions, renal/hepatic impairment, or poor adherence
- Obtain informed consent for genetic analysis
TDM Sample Collection and Analysis:
Genomic Analysis:
Data Integration and Analysis:
- Correlate variant genotypes with drug concentration data
- Adjust for covariates (age, weight, renal/hepatic function, concomitant medications)
- Apply statistical tests (linear regression for continuous traits, logistic regression for categorical outcomes)
- Apply multiple testing corrections as appropriate
Protocol 2: Analytical Validation of TDM Assays for Genomic Correlation Studies
Purpose: To establish and document the analytical performance of TDM assays used for pharmacogenomic variant validation.
Materials:
- TDM analytical platform (e.g., Abbott AxSYM, HPLC/MS)
- Drug-free human serum or plasma
- Certified reference standards
- Quality control materials at multiple concentrations
- Patient samples for method comparison
Methodology:
- Accuracy Assessment:
- Analyze three concentration levels of commercial control samples
- Perform three replicates at each level
- Calculate bias as (measured value - declared value)/declared value × 100%
- Compare to acceptance criteria (e.g., CLIA Proficiency Testing criteria) [97]
Precision Evaluation:
- Within-run imprecision: Analyze two patient samples ten times in a single batch
- Between-run imprecision: Analyze patient sample aliquots once daily for 10-15 days
- Calculate mean, standard deviation, and coefficient of variation (CV) for each
- Compare to established acceptance criteria [97]
Method Comparison (if implementing new assay):
- Analyze 30-40 patient samples by both old and new methods
- Perform Passing-Bablock regression analysis
- Use Cusum test to verify linearity
- Establish concordance between methods [97]
Measurement Uncertainty Calculation:
- Combine uncertainty components from calibration, imprecision, and inaccuracy
- Use formula: U = √(U²calibrator + U²imprecision + U²_bias)
- Report expanded uncertainty for clinical interpretation [97]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for TDM-Variant Validation Studies
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Certified Reference Standards | Provide traceable calibrators for TDM assays | Essential for establishing assay accuracy and cross-platform comparability [99]. |
| Multi-level Quality Controls | Monitor assay precision and accuracy over time | Should include concentrations spanning therapeutic range and critical decision points [98]. |
| NGS Library Preparation Kits | Prepare sequencing libraries from genomic DNA | Select kits based on application: whole genome, exome, or targeted panels [100]. |
| Targeted Capture Panels | Enrich pharmacogenomic regions of interest | Custom panels can focus on ADME genes and known pharmacogenetic variants [95]. |
| Bioinformatic Tools | Variant calling, annotation, and interpretation | Use validated pipelines with tools like GATK, VEP, SIFT, PolyPhen for consistent analysis [95] [51]. |
| Reference Materials | Genomic DNA with known variants | Used for validating NGS assay performance and bioinformatics pipelines [95]. |
Next-generation sequencing (NGS) has revolutionized chemogenomics research, enabling rapid identification of genetic targets and personalized therapeutic strategies [36] [101]. However, the transition from analytically valid genomic data to clinically useful applications faces significant bottlenecks that hinder drug development pipelines. The core challenge lies in the multi-step analytical process where computational limitations, interpretation variability, and technical artifacts collectively create barriers to clinical translation [7] [102] [95].
In chemogenomics, where researchers correlate genomic data with chemical compound responses, these bottlenecks manifest most acutely in variant calling reproducibility, clinical interpretation consistency, and analytical validation of results [95]. The PrecisionFDA Consistency Challenge revealed that even identical input data analyzed with different pipelines can yield divergent variant calls in up to 2.6% of cases - a critical concern when identifying drug targets or biomarkers [95]. This technical introduction establishes why dedicated troubleshooting resources are essential for overcoming these barriers and achieving reliable clinical utility in NGS-based chemogenomics research.
Troubleshooting Guides
Common Problem Identification
The first step in effective troubleshooting involves recognizing frequent issues and their manifestations in NGS data. The table below summarizes key problems, their potential impact on chemogenomics research, and immediate diagnostic steps.
Table: Common NGS Problems in Chemogenomics Research
| Problem | Symptoms | Potential Impact on Drug Research | Immediate Diagnostic Steps |
|---|---|---|---|
| Low Coverage in Target Regions | High duplicate read rates (>15-40%), uneven coverage [103] | Missed pathogenic variants affecting drug target identification; unreliable genotype-phenotype correlations | Check enrichment efficiency metrics; review duplicate read percentage; analyze coverage uniformity [103] |
| Variant Calling Inconsistencies | Different variant sets from same data; missing known variants [95] | Irreproducible biomarker discovery; flawed patient stratification for clinical trials | Run positive controls; verify algorithm parameters; check concordance with orthogonal methods [95] |
| High Error Rates in GC-Rich Regions | Coverage dropout in high GC areas; false positive/negative variants [103] | Incomplete profiling of drug target genes with extreme GC content | Analyze coverage vs. GC correlation; compare performance across enrichment methods [103] |
| Interpretation Discrepancies | Different clinical significance assigned to same variant [95] | Inconsistent therapeutic decisions based on genomic findings | Utilize multiple annotation databases; follow established guidelines; document evidence criteria [102] [95] |
Step-by-Step Resolution Protocols
Resolution Protocol: Addressing Low Coverage in Critical Genomic Regions
Problem: Inadequate sequencing depth in pharmacogenetically relevant genes, potentially missing variants that affect drug response.
Required Materials: BAM/CRAM files from sequencing, target BED file, quality control reports (FastQC, MultiQC), computing infrastructure with bioinformatics tools.
Step-by-Step Procedure:
Confirm and Localize the Problem:
Document specific genes and genomic coordinates with insufficient coverage, prioritizing regions known to be pharmacologically relevant.
Determine Root Cause:
- Check library complexity: High duplicate read percentages (>15-40%) indicate potential issues during library preparation [103].
- Evaluate enrichment efficiency: Compare on-target percentages (should be >75-85% for capture-based methods) [103].
- Assess base quality scores: Identify systematic decreases in quality that might indicate technical issues.
Implement Solution Based on Root Cause:
- For library complexity issues: Optimize input DNA quantity and quality; adjust fragmentation parameters; use PCR-free protocols when possible.
- For enrichment issues: Consider alternative capture methods; NimbleGen demonstrates better coverage uniformity compared to other methods [103].
- For persistent gaps: Design supplemental PCR primers for problematic regions and sequence with orthogonal method.
Validation:
- Resequence 10% of samples to confirm improved coverage.
- Use control samples with known variants in previously problematic regions to verify detection.
Diagram: Troubleshooting Low Target Coverage
Resolution Protocol: Managing Variant Calling Inconsistencies
Problem: The same raw sequencing data produces different variant calls when analyzed with different pipelines or parameters, creating uncertainty in chemogenomics results.
Required Materials: Raw FASTQ files, reference genome, computational resources, multiple variant calling pipelines (GATK, DeepVariant, etc.), known positive control variants.
Step-by-Step Procedure:
Quantify Inconsistency:
Calculate percentage concordance and identify variants specific to each pipeline.
Identify Sources of Discrepancy:
- Check algorithm parameters: Default settings may not be optimal for specific applications.
- Review quality filtering thresholds: Different quality score cutoffs significantly impact results.
- Examine stochastic effects: Some algorithms introduce randomness in parallel processing.
Standardize Analysis Pipeline:
- Use Common Workflow Language (CWL) or similar standards to define exact computational steps [95].
- Implement container technologies like Docker for reproducible environments.
- Establish benchmark variants for pipeline optimization and validation.
Validate Clinically Relevant Variants:
- Confirm potentially significant variants (those affecting drug targets or biomarkers) using orthogonal methods like Sanger sequencing.
- Document all parameters and software versions for regulatory compliance.
Continuous Monitoring:
- Implement routine precision checks using control samples.
- Participate in proficiency testing programs when available.
Frequently Asked Questions (FAQs)
Data Generation & Quality Control
Q1: What are the key quality metrics we should check in every NGS run for chemogenomics applications?
Focus on metrics that directly impact variant detection and drug target identification:
- Coverage uniformity: Ensure even coverage across all target regions, with <10-20% coefficient of variation [103].
- On-target efficiency: Aim for >75-85% reads mapping to target regions for capture-based methods [103].
- Duplicate read rate: Maintain <15% for capture methods; higher rates indicate library complexity issues [103].
- Base quality scores: >90% bases with Q≥30 for reliable variant calling.
- GC bias: Check coverage distribution across GC-rich and GC-poor regions, as extreme bias can miss important genomic regions [103].
Q2: How do we choose between short-read and long-read sequencing for chemogenomics studies?
The choice depends on your specific research questions:
- Short-read (Illumina): Best for detecting single nucleotide variants and small indels with high accuracy (>99.9%) [36] [7]. Ideal for targeted panels and exome sequencing in large cohorts.
- Long-read (PacBio, Nanopore): Essential for resolving complex regions, structural variants, and phasing haplotypes [36] [7]. Particularly valuable for profiling pharmacogenes with complex architectures like CYP2D6.
- Hybrid approaches: Combining both technologies provides comprehensive variant detection, though at higher cost and computational burden.
Q3: What are the specific advantages of different target enrichment methods for drug target discovery?
Table: Comparison of NGS Enrichment Methods for Clinical Applications
| Method | Preparation Time | DNA Input | Performance in GC-Rich Regions | Best Use Cases in Chemogenomics |
|---|---|---|---|---|
| NimbleGen SeqCap EZ | Standard | 100-200ng | Good coverage uniformity [103] | Comprehensive drug target panels; clinical validation studies |
| Agilent SureSelectQXT | Reduced (~1.5 days) | 10-200ng | Better performance in high GC content [103] | Rapid screening; samples with limited DNA |
| Illumina NRCCE | Rapid (~1 day) | 25-50ng | Lower performance in high GC content [103] | Quick turnaround studies; proof-of-concept work |
Data Analysis & Interpretation
Q4: How can we improve consistency in variant interpretation across different analysts in our drug discovery team?
Implement a systematic approach to variant classification:
- Standardized guidelines: Adopt ACMG-AMP guidelines for variant interpretation and develop drug-specific modifications [95].
- Multi-source annotation: Use multiple databases simultaneously (ClinVar, COSMIC, dbSNP) to assess variant evidence [104] [95].
- Computational predictions: Employ consistent tools (SIFT, PolyPhen, REVEL) for functional impact prediction, but use them as supporting evidence only [104] [95].
- Regular review meetings: Conduct multidisciplinary team reviews for variants of uncertain significance that may impact therapeutic decisions.
- Documentation standards: Maintain detailed records of evidence and reasoning for all variant classifications.
Q5: What computational infrastructure do we need for NGS analysis in a medium-sized drug discovery program?
A balanced approach combining cloud and local resources works best:
- Cloud platforms (AWS, Google Cloud, DNAnexus): Provide scalability for large analyses and access to curated pipelines, essential for fluctuating workloads [7] [24].
- Local servers: Maintain sensitive data on-premises with appropriate security controls.
- Accelerated hardware (DRAGEN, GPUs): Reduce analysis time from days to hours for rapid turnaround [7].
- Storage architecture: Plan for 1-5TB per whole genome, including raw data, processed files, and backups, with appropriate growth capacity.
Q6: How can AI and machine learning improve our NGS analysis for drug discovery?
AI/ML approaches are transforming several aspects of chemogenomics:
- Variant calling: DeepVariant uses deep learning to achieve superior accuracy compared to traditional methods [24].
- Variant prioritization: ML algorithms can integrate multiple evidence types to prioritize variants most likely to be therapeutically relevant.
- Drug response prediction: Models can correlate complex variant patterns with treatment outcomes using multi-omics integration [25] [24].
- Target discovery: Network-based ML approaches can identify novel drug targets from genomic data [24].
Clinical Translation & Validation
Q7: What are the key steps for validating NGS findings before using them for patient stratification in clinical trials?
A rigorous multi-step validation protocol is essential:
- Analytical validation: Verify technical performance of the assay for each variant type (SNVs, indels, CNVs) using samples with known genotypes.
- Orthogonal confirmation: Use different technology (Sanger sequencing, digital PCR) to confirm clinically actionable variants.
- Functional validation: For novel variants, conduct experimental studies (cell-based assays, protein modeling) to establish biological impact.
- Clinical correlation: Examine variant associations with drug response in available clinical data.
- Regulatory compliance: Follow FDA guidelines for NGS-based tests, including documentation of all steps and parameters [95].
Q8: How do we handle incidental findings in chemogenomics research, particularly when repurposing drugs?
Establish a clear institutional policy that addresses:
- Pre-defined gene list: Specify which genes and variant types will be reported based on clinical actionability.
- Informed consent: Clearly explain the possibility of incidental findings and options for receiving results.
- Clinical consultation: Provide access to genetic counselors for participants with significant findings.
- Drug repurposing considerations: Be aware that variants in genes not directly related to the primary research question may impact safety or efficacy of repurposed drugs.
Q9: What are the biggest challenges in achieving clinical utility for NGS-based biomarkers?
Key challenges include:
- Evidence generation: Proving that using the biomarker actually improves patient outcomes, not just correlates with biology.
- Standardization: Achieving consistency across laboratories in testing and interpretation [95].
- Regulatory approval: Navigating FDA requirements for companion diagnostics [95].
- Reimbursement: Demonstrating value to payers for test reimbursement.
- Implementation: Integrating genomic testing into clinical workflows with appropriate decision support.
Q10: How is the integration of multi-omics data changing chemogenomics research?
Multi-omics approaches are transforming drug discovery by:
- Providing mechanistic insights: Combining genomics with transcriptomics, epigenomics, and proteomics reveals functional consequences of genetic variants [25] [24].
- Identifying novel biomarkers: Integrated profiles often provide better predictive power than genomic data alone.
- Enabling network pharmacology: Mapping interactions across molecular layers identifies complex therapeutic targets.
- Accelerating repurposing: Multi-omics signatures can connect existing drugs to new indications more reliably [101].
The Scientist's Toolkit
Research Reagent Solutions
Table: Essential Materials for NGS-based Chemogenomics
| Reagent/Category | Specific Examples | Function in Workflow | Considerations for Selection |
|---|---|---|---|
| Target Enrichment Kits | NimbleGen SeqCap EZ, Agilent SureSelectQXT, Illumina NRCCE [103] | Isolate genomic regions of interest for sequencing | Balance preparation time, input DNA requirements, and coverage uniformity based on research priorities [103] |
| Library Preparation Kits | Illumina Nextera, TruSeq | Fragment DNA and add adapters for sequencing | Consider input DNA quality, required throughput, and need for PCR-free protocols |
| Sequencing Reagents | Illumina SBS chemistry, PacBio SMRT cells, Nanopore flow cells | Generate raw sequence data | Match to platform; consider read length, accuracy, and throughput requirements |
| Bioinformatics Tools | BWA, GATK, DeepVariant, ANNOVAR [104] [95] | Align sequences, call variants, and annotate results | Evaluate accuracy, computational requirements, and compatibility with existing pipelines |
| Variant Databases | dbSNP, COSMIC, ClinVar, PharmGKB [104] | Interpret variant clinical significance and functional impact | Consider curation quality, update frequency, and disease-specific coverage |
| Analysis Platforms | Galaxy, DNAnexus, Seven Bridges [95] | Provide integrated environments for data analysis | Assess scalability, collaboration features, and compliance with regulatory requirements |
Experimental Workflow Visualization
Diagram: NGS Data Analysis Pathway from Raw Data to Clinical Utility
Conclusion
The integration of NGS into chemogenomics has fundamentally transformed drug discovery but faces persistent analytical challenges that span data generation, processing, and interpretation. Successfully navigating these bottlenecks requires a multi-faceted approach combining robust quality control, strategic implementation of AI and machine learning, workflow automation, and rigorous validation frameworks. The future of chemogenomics lies in developing more integrated, automated, and intelligent analysis systems that can handle the growing complexity and scale of genomic data while providing clinically actionable insights. Emerging technologies such as long-read sequencing, single-cell approaches, and federated learning for privacy-preserving analysis promise to further revolutionize the field. By addressing these bottlenecks systematically, researchers can unlock the full potential of NGS in chemogenomics, accelerating the development of personalized therapies and improving patient outcomes through more precise targeting of drug responses and adverse effects.
References
- 1. Frequently Asked Questions - ChemoGenix - IRIC [https://chemogenix.iric.ca/faq]
- 2. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 3. Avoid Costly Errors in NGS Sample Handling and Library ... [https://seqwell.com/avoid-costly-errors-in-ngs-sample-handling-and-library-prep/]
- 4. Custom Bioinformatics Workflows & Pipelines [https://ardigen.com/bioinformatics-workflows/]
- 5. FAQ | Chemical Probes Portal [https://www.chemicalprobes.org/faq]
- 6. Benchmarking of computational error-correction methods for ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-020-01988-3]
- 7. Navigating bottlenecks and trade-offs in genomic data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC10204111/]
- 8. Computational pharmacogenotype extraction from clinical ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1199741/full]
- 9. The Role of Next-Generation Sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6360866/]
- 10. Standards and Guidelines for Validating Next-Generation ... [https://www.sciencedirect.com/science/article/pii/S1525157817303732]
- 11. Emerging strategies to bridge the gap between ... [https://www.nature.com/articles/s41525-020-0119-2]
- 12. Scientific Challenges and Implementation Barriers to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3603526/]
- 13. Progress in Pharmacogenomics Implementation in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439016/]
- 14. Artificial intelligence, medications, pharmacogenomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11703462/]
- 15. Translating pharmacogenomic sequencing data into drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11773106/]
- 16. Pharmacogenetic analysis of structural variation in the ... [https://www.nature.com/articles/s41598-024-73748-3]
- 17. Troubleshooting the gene-variant workflow [https://re-docs.genomicsengland.co.uk/gv_faqs/]
- 18. How Omics Data Analysis Software can solve ... [https://bigomics.ch/blog/the-current-bottleneck-in-omics-data-analysis/]
- 19. A practical guide for structural variation detection in human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7738216/]
- 20. Bioinformatics challenges of new sequencing technology [https://pmc.ncbi.nlm.nih.gov/articles/PMC2680276/]
- 21. By 2025, an estimated 40 exabytes of storage capacity will ... [https://www.facebook.com/googlecloud/posts/by-2025-an-estimated-40-exabytes-of-storage-capacity-will-be-required-for-human-/1496997334035170/]
- 22. Broad Institute and Manifold: Pulling the Future of Biomedical ... [https://www.manifold.ai/resources/broad-institute-and-manifold-pulling-the-future-of-biomedical-science-forward-together]
- 23. NGS Data Storage Market Size, Share & Trends Analysis ... [https://www.insightaceanalytic.com/report/ngs-data-storage-market/1862]
- 24. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 25. 2025 Trends: NGS [https://www.genengnews.com/topics/genome-editing/2025-trends-ngs/]
- 26. Integrating Artificial Intelligence in Next-Generation Sequencing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191491/]
- 27. The Next-Generation Sequencing Quality Initiative and ... [https://wwwnc.cdc.gov/eid/article/31/13/24-1175_article]
- 28. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 29. Top NGS Data Storage Companies & How to Compare ... [https://www.linkedin.com/pulse/top-ngs-data-storage-companies-how-compare-them-anb7e/]
- 30. Artificial intelligence in variant calling: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12055765/]
- 31. AI Tools Used for NGS Data Analysis [https://ibri.org.in/blog/ai-tools-used-for-ngs-data-analysis]
- 32. Bioinformatics: From NGS Data to Biological Complexity in Variant Detection and Oncological Clinical Practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495893/]
- 33. Transformers meets neoantigen detection: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11377031/]
- 34. A review on the applications of Transformer-based ... [https://www.sciencedirect.com/science/article/pii/S2001037025000935]
- 35. NGS for Beginners | Learn the basics of NGS [https://www.illumina.com/science/technology/next-generation-sequencing/beginners.html]
- 36. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 37. Resources and tools for rare disease variant interpretation [https://pmc.ncbi.nlm.nih.gov/articles/PMC10206239/]
- 38. Benchmarking computational variant effect predictors by their ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03314-7]
- 39. NGS Software Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-software-support/ngs-software-support-troubleshooting.html]
- 40. FAQs [https://phasegenomics.com/resources-and-support/faqs-2/]
- 41. Computational tools [https://www.pacb.com/computational-tools/]
- 42. Q&A: How does computer science advance biology? [https://www.psu.edu/news/engineering/story/qa-how-does-computer-science-advance-biology]
- 43. Multi-omics Data Integration, Interpretation, and Its Application [https://pmc.ncbi.nlm.nih.gov/articles/PMC7003173/]
- 44. Gene-centric multi-omics integration with convolutional ... [https://www.sciencedirect.com/science/article/pii/S0010482522009003]
- 45. Designing and interpreting 'multi-omic' experiments that may ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7477987/]
- 46. Integrative chemical biology approaches to examine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4382910/]
- 47. How Automation Overcomes Variability & Limitations in ... [https://dispendix.com/blog/how-automation-overcomes-variability-limitations-in-hts-troubleshooting]
- 48. Automation in Genomics Workflows | How Labs Improve ... [https://www.labmanager.com/automation-in-genomics-workflows-driving-precision-efficiency-and-scale-34446]
- 49. Do The Math: The Unrealized ROI In Lab Automation [https://www.genedata.com/resources/learn/details/blog/do-the-math-the-unrealized-roi-in-lab-automation]
- 50. Compound Screening in Drug Discovery - Automated Workflows [https://lifesciences.danaher.com/us/en/solutions/small-molecule-drug-discovery/preliminary-screening.html]
- 51. NGS Data Analysis Bottlenecks: Common Pitfalls & Proven ... [https://www.genomebeans.com/blog/ngs-data-analysis-bottlenecks-common-pitfalls-and-how-to-overcome-them]
- 52. Chemogenomic Approaches for Revealing Drug Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8844939/]
- 53. Next Generation Sequencing Market 2025-2033 Analysis [https://www.archivemarketresearch.com/reports/next-generation-sequencing-market-2866]
- 54. Pharmacogenomics, How to Deal with Different Types of ... [https://www.mdpi.com/2077-0383/10/1/34]
- 55. Genome-wide functional annotation of variants: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11911558/]
- 56. The trouble with PCR duplicates [https://www.molecularecologist.com/2016/08/25/the-trouble-with-pcr-duplicates/]
- 57. How PCR duplicates arise in next-generation sequencing [https://www.cureffi.org/2012/12/11/how-pcr-duplicates-arise-in-next-generation-sequencing/]
- 58. Identifying and Mitigating Bias in Next-Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4473780/]
- 59. – Quality Control NGS Analysis [https://learn.gencore.bio.nyu.edu/metgenomics/quality-control/]
- 60. Assessment of quality approaches for metagenomic control ... data [https://www.nature.com/articles/srep06957?error=cookies_not_supported&code=6f64802f-b884-4be0-8afc-8e53c3e3fd7f]
- 61. FAQs Next Generation Sequencing [https://eurofinsgenomics.eu/en/eurofins-genomics/product-faqs/next-generation-sequencing/]
- 62. MagicPrep™ NGS 一站式建库仪- 帝肯 [https://lifesciences.tecan.cn/magicprep-ngs]
- 63. NGS 中DNA/RNA 提取流程优化 [https://www.mybeckman.cn/resources/technologies/next-generation-sequencing/importance-of-optimizing-your-ngs-workflow]
- 64. 产品说明书:KAPA文库定量试剂盒Illumina®平台 [https://cn.bio-protocol.org/mv2/e1010508]
- 65. 次世代基因定序信息学市场规模、预测、分析与份额2030 [https://www.mordorintelligence.com/zh-CN/industry-reports/next-generation-sequencing-informatics-market]
- 66. 测序工作流程的准确性| TruSeq技术 [https://www.illumina.com.cn/science/education/sequencing-workflow-accuracy.html]
- 67. Computational Resources: Definition, operation and role [https://datascientest.com/en/computational-resources-definition-operation-and-role]
- 68. Communication and computational resource optimization ... [https://www.sciencedirect.com/science/article/pii/S131915782300424X]
- 69. The 2025 Bioinformatics Toolkit: From Sample Prep to AI- ... [https://blog.omni-inc.com/blog/the-2025-bioinformatics-toolkit-from-sample-prep-to-ai-driven-analysis]
- 70. Break NGS Bottlenecks to Improve Patient Outcomes [https://www.technologynetworks.com/genomics/ebooks/break-through-the-ngs-interpretation-bottleneck-to-improve-patient-outcomes-399722]
- 71. Standardized pipelines support and facilitate integration of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11753291/]
- 72. Systematic evaluation of fMRI data-processing pipelines for ... [https://www.nature.com/articles/s41467-024-48781-5]
- 73. Rapid NGS Analysis on Google Cloud Platform [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627752/]
- 74. AWS Genomics Data Storage & Cloud Processing ... [https://hypersense-software.com/blog/2025/04/01/genomics-data-storage-processing-aws/]
- 75. Accelerating genomics variant interpretation with ... [https://aws.amazon.com/blogs/machine-learning/accelerating-genomics-variant-interpretation-with-aws-healthomics-and-amazon-bedrock-agentcore/]
- 76. NGS Data Analysis for Illumina Platform—Overview and ... [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/next-generation-sequencing/ngs-data-analysis-illumina.html]
- 77. Current status of the analytical validation of next generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10635985/]
- 78. Ten quick tips for biomarker discovery and validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9371329/]
- 79. NGS Data Analysis: Best Practices and Common Pitfalls [https://dromicsedu.com/blog-details/ngs-data-analysis-best-practices-and-common-pitfalls]
- 80. Biomarker discovery and validation: Bridging research and ... [https://www.abcam.com/en-us/knowledge-center/immunology-and-infectious-disease/biomarker-discovery-and-validation]
- 81. Long-read sequencing vs short-read sequencing [https://frontlinegenomics.com/long-read-sequencing-vs-short-read-sequencing/]
- 82. Short read vs long read sequencing - INTEGRA Biosciences [https://www.integra-biosciences.com/united-states/en/blog/article/short-read-vs-long-read-sequencing]
- 83. Short-read sequencing — Knowledge Hub [https://www.genomicseducation.hee.nhs.uk/genotes/knowledge-hub/short-read-sequencing/]
- 84. The application of long-read sequencing in clinical settings [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-023-00522-3]
- 85. Opportunities and challenges in long-read sequencing data ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-020-1935-5]
- 86. Long-Read Sequencing Technology | For challenging ... [https://www.illumina.com/science/technology/next-generation-sequencing/long-read-sequencing.html]
- 87. Short-Read Sequencing vs. Long ... [https://seqwell.com/short-read-sequencing-vs-long-read-sequencing-which-technology-is-right-for-your-research/]
- 88. Leveraging long-read sequencing technologies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075302/]
- 89. Benchmark Datasets for Genomic AI Sequence-to-Function ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10614795/]
- 90. Benchmarking and Evaluation of AI Models in Biology [https://arxiv.org/abs/2507.10502]
- 91. LLM Benchmarks in Life Sciences: Comprehensive Overview [https://intuitionlabs.ai/articles/large-language-model-benchmarks-life-sciences-overview]
- 92. BenchXAI: Comprehensive benchmarking of post-hoc ... [https://www.sciencedirect.com/science/article/pii/S0010482525004755]
- 93. United States Next Generation Sequencing (NGS) Market ... [https://crisprmedicinenews.com/press-release-service/card/united-states-next-generation-sequencing-ngs-market-research-2025-2033-personalized-medicine-res/]
- 94. Overview of Therapeutic Drug Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2687654/]
- 95. The Use of Next-Generation Sequencing in Drug ... [https://www.ddw-online.com/the-use-of-next-generation-sequencing-in-drug-development-1506-201712/]
- 96. Challenges in the Setup of Large-scale Next-Generation ... [https://www.sciencedirect.com/science/article/pii/S2001037017300776]
- 97. Analytical validation of therapeutic drug monitoring (TDM) ... [https://www.biochemia-medica.com/en/journal/20/2/10.11613/BM.2010.032/fullArticle]
- 98. Therapeutic Drug Monitoring: The Basics - Utak [https://utak.com/blog/therapeutic-drug-monitoring-the-basics/]
- 99. Documenting assay quality in TDM [https://www.sciencedirect.com/science/article/pii/S003130251632102X]
- 100. NGS for Drug Development [https://www.illumina.com/areas-of-interest/genomics-in-drug-development/ngs-for-drug-development.html]
- 101. Applications of NGS in Drug Research [https://www.psomagen.com/blog/next-generation-sequencing-revolutionizes-drug-discovery-and-development]
- 102. Challenges in clinical interpretation of next-generation ... [https://www.sciencedirect.com/science/article/pii/S2590123023005480?dgcid=rss_sd_all&]
- 103. Assessment of the latest NGS enrichment capture methods ... [https://www.nature.com/articles/srep20948]
- 104. Next generation DNA Sequencing data analysis and its ... [https://www.sciencedirect.com/science/article/abs/pii/S034403382500473X]