Automating NGS Workflows: A Strategic Guide to Unlocking Reproducible Chemogenomic Research
Next-generation sequencing (NGS) is revolutionizing drug discovery and biomedical research, but its potential is often limited by manual workflow inconsistencies.
Automating NGS Workflows: A Strategic Guide to Unlocking Reproducible Chemogenomic Research
Abstract
Next-generation sequencing (NGS) is revolutionizing drug discovery and biomedical research, but its potential is often limited by manual workflow inconsistencies. This article provides researchers, scientists, and drug development professionals with a comprehensive guide to automating NGS workflows to achieve superior chemogenomic reproducibility. We explore the foundational drivers, including market growth and strategic partnerships, detail methodological implementations from library prep to data analysis, offer best practices for troubleshooting and optimization, and establish a framework for rigorous validation and quality control to ensure compliance with clinical standards.
The Imperative for Automation: Foundations of Reproducible NGS in Chemogenomics
Technical Support Center
Troubleshooting Guides
Guide 1: Troubleshooting Common Automated NGS Library Preparation Failures
Problem: Low Library Yield
Low library yield is a frequent and frustrating outcome that can compromise entire sequencing runs. The table below outlines the primary causes and their respective corrective actions [1].
| Cause of Failure | Mechanism of Yield Loss | Corrective Action |
|---|---|---|
| Poor Input Quality / Contaminants | Enzyme inhibition from residual salts, phenol, EDTA, or polysaccharides [1]. | Re-purify input sample; ensure wash buffers are fresh; target high purity (260/230 > 1.8, 260/280 ~1.8) [1] [2]. |
| Inaccurate Quantification / Pipetting | Suboptimal enzyme stoichiometry due to concentration errors [1]. | Use fluorometric methods (Qubit) over UV absorbance; calibrate pipettes; use master mixes [1] [2]. |
| Fragmentation/Tagmentation Inefficiency | Over- or under-fragmentation reduces adapter ligation efficiency [1]. | Optimize fragmentation parameters (time, energy); verify fragmentation profile before proceeding [1]. |
| Suboptimal Adapter Ligation | Poor ligase performance, wrong molar ratio, or reaction conditions reduce adapter incorporation [1]. | Titrate adapter-to-insert molar ratios; ensure fresh ligase and buffer; maintain optimal temperature [1]. |
Problem: High Duplicate Read Rate and Amplification Bias
Over-amplification during library preparation is a major source of bias and artifacts, leading to inaccurate data [1].
| Cause of Failure | Mechanism of Bias | Corrective Action |
|---|---|---|
| Too Many PCR Cycles | Overcycling introduces size bias, duplicates, and flattens fragment size distribution [1]. | Optimize and minimize the number of PCR cycles; repeat amplification from leftover ligation product rather than overamplifying a weak product [1]. |
| Carryover of Enzyme Inhibitors | Residual salts or phenol can inhibit polymerases mid-amplification [1]. | Re-purify input sample using clean columns or beads to remove inhibitors [1]. |
| Primer Exhaustion or Mispriming | Primers may run out prematurely or misprime under suboptimal conditions [1]. | Optimize primer design and annealing conditions; ensure adequate primer concentration [1]. |
Problem: Contamination and Batch Effects
Batch effects, where technical variables systematically influence data, can confound results and lead to false conclusions [3] [4].
| Cause of Failure | Impact on Data | Corrective Action |
|---|---|---|
| Researcher-to-Researcher Variation | Differences in manual pipetting technique can cause batch effects, masking true biological differences [4] [5]. | Implement automated liquid handling to standardize protocols and eliminate user-based variation [4] [5]. |
| Cross-Contamination | Improper sample handling leads to contamination, resulting in inaccurate results and data misinterpretation [5] [6]. | Use automated, closed systems; sterilize workstations; handle one sample at a time; include DNA-free controls [5] [6]. |
| Reagent Degradation | Ethanol wash solutions losing concentration over time can lead to suboptimal washes and failures [1]. | Enforce reagent quality control logs; track lot numbers and expiry dates [1]. |
Guide 2: Diagnosing Systemic NGS Data Biases
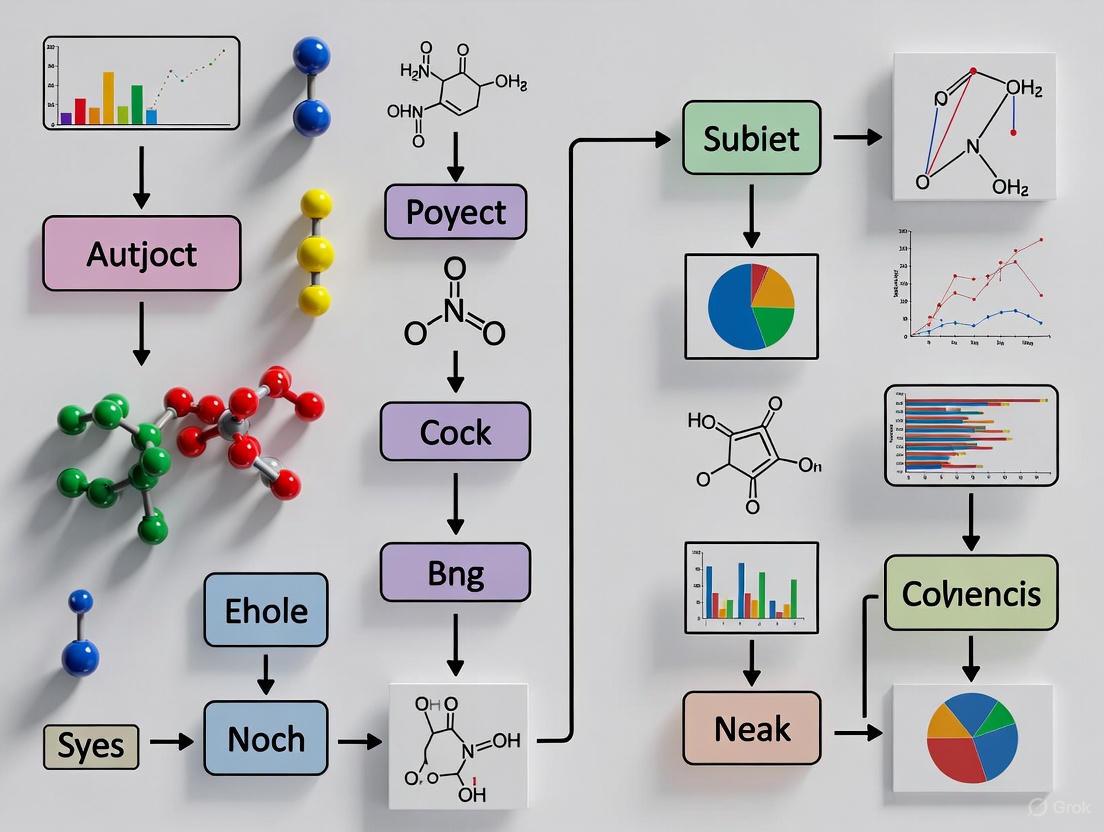
Systemic biases can be introduced at various stages of the automated NGS workflow. The following diagram illustrates the logical flow for diagnosing the root cause of common data biases.
The table below details these specific biases and their solutions.
| Bias Type | Description & Impact | Solution |
|---|---|---|
| GC Coverage Bias | Strong, reproducible effect of local GC content on sequencing read coverage. Problematic for RNA-Seq, ChIP-Seq, and copy number detection [3]. | Adjust signal for GC content in bioinformatic analysis to improve precision [3]. |
| Base-Call Error Bias | Base-call errors are not random and can cluster by cycle position on the sequencer. Impacts alignment and can cause false-positive variant calls [3]. | Employ alternative base-calling methods or post-hoc error correction algorithms [3]. |
| Batch Effects | Technical variability (e.g., processing date, technician, reagent lot) correlates with and confounds experimental outcomes [3]. | Use careful experimental design with randomization; apply batch effect correction methods (e.g., surrogate variable analysis) during data analysis [3]. |
Frequently Asked Questions (FAQs)
Q1: What are the most significant challenges when first automating an NGS workflow, and how can we overcome them?
A1: Labs new to automation often face three core challenges [7]:
- Lack of Software Knowledge: Building and modifying custom protocols can require coding expertise. Solution: Choose platforms with modular, user-friendly software (e.g., Tecan's FluentControl) that separates method development from daily operation, enabling protocol customization without programming [7].
- Difficulty Designing a Worktable: The vast array of hardware and accessories can be confusing. Solution: Invest in a flexible, universal worktable configuration and ensure the software GUI clearly displays reagent and sample loading requirements [7].
- Long Workflow Optimization Times: It can take months to optimize a new automated script. Solution: Select platforms with pre-developed, extensively tested routines for common tasks and commercial kits (e.g., the collaboration between Zymo Research and Tecan) to eliminate lengthy optimization [7].
Q2: Our automated preps are inconsistent. What are the common hidden sources of variation?
A2: Inconsistency in automated runs often stems from these hidden factors:
- Liquid Handler Calibration: Improperly calibrated pipetting axes (x, y, z) can lead to inaccurate liquid transfers. Regularly maintain and calibrate instruments [7].
- Reagent Degradation: Enzymes (e.g., ligases, polymerases) and buffers lose activity over time. Strictly monitor reagent lot numbers and expiry dates, and avoid using expired reagents [1].
- Human Procedural Errors: Even on automated systems, manual pre- and post-steps can introduce variation. Implement standardized operating procedures (SOPs), checklists, and master mixes to reduce pipetting errors and improve consistency across technicians [1].
Q3: How can we reduce the cost of our automated NGS workflows without sacrificing quality?
A3: Several strategies can lead to significant cost savings:
- Reagent Miniaturization: Automated liquid handlers can accurately dispense low-volume reactions. Miniaturizing reactions to 1/10th of the manufacturer's recommended volume can drastically reduce reagent consumption and cost [8] [5].
- Reduce Repeat Experiments: Automation enhances precision and reduces human error, which minimizes failed runs and the need for costly reagent-wasting repeats [4] [5].
- Efficient Normalization: Use library prep kits with high levels of auto-normalization to achieve consistent read depths across samples without the need for individual sample normalization, saving time and reagents [6].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for robust automated NGS workflows.
| Item | Function in Automated NGS |
|---|---|
| High-Fidelity DNA Polymerase | Enzymes with proofreading capabilities minimize errors during PCR amplification, ensuring accurate representation of the template DNA [9]. |
| Fluorometric Quantitation Kits (e.g., Qubit) | Provides highly accurate quantification of DNA/RNA concentration by specifically binding to nucleic acids, unlike UV absorbance which can be skewed by contaminants [1] [2]. |
| Magnetic Beads (SPRI) | Used for automated purification and size selection of DNA fragments, enabling efficient cleanup and removal of unwanted reagents like adapter dimers [1]. |
| Multiplexed Sequencing Adapters | Short, double-stranded DNA sequences with unique molecular barcodes ligated to fragments, allowing multiple samples to be pooled and sequenced in a single run [10]. |
| Automated NGS Library Prep Kit | Integrated kits (e.g., seqWell's ExpressPlex, Tecan/Zymo's DreamPrep) provide pre-optimized, ready-to-use reagents formatted for automated liquid handlers, streamlining the entire process [7] [6]. |
| Internal Control Spikes | Known DNA sequences added to the sample to monitor the efficiency and accuracy of the entire workflow, from library prep to sequencing [8]. |
Automated NGS Workflow Diagram
The diagram below outlines the key stages of a typical automated NGS workflow, highlighting where automation and critical quality control (QC) steps are integrated.
Strategic industry partnerships are revolutionizing next-generation sequencing (NGS) by integrating specialized expertise to overcome critical bottlenecks in automated workflows. In chemogenomic reproducibility research, where consistent, high-throughput genetic data is paramount for evaluating compound effects, these collaborations are not merely beneficial—they are essential. They combine advanced library preparation chemistries with sophisticated automation platforms, directly addressing longstanding challenges in manual NGS protocols such as pipetting variability, cross-contamination, and workflow inefficiencies that compromise data integrity. This technical support center provides targeted guidance for scientists leveraging these collaborative tools to achieve robust, reproducible results in their drug discovery pipelines.
Frequently Asked Questions (FAQs)
How do strategic partnerships specifically improve the quality of my NGS library prep? Partnerships merge distinct areas of expertise, such as a reagent company's specialized enzymes with an automation firm's precision liquid handling. This synergy creates optimized, validated, and standardized protocols. For example, a study comparing manual and automated library prep for a 22-gene solid tumour panel showed that the automated workflow, developed through a partnership, achieved on-target rates exceeding 90% and higher reproducibility, significantly improving data quality for clinical analysis [11].
My lab is new to automation. What is the biggest challenge we should anticipate? The most common initial challenge is a lack of software knowledge and the complexity of designing a functional worktable [7]. Building custom scripts for your specific protocols and selecting the correct hardware from hundreds of configurations can delay projects for months. The solution is to seek partnerships that offer platforms with pre-developed, optimized routines for common NGS tasks and intuitive software that separates complex method development from daily operation [7].
Are collaborative automation solutions compatible with the regulatory standards required for drug development? Yes, a key driver behind these partnerships is to ensure compliance with stringent regulatory frameworks like IVDR and ISO 13485 [12]. Automated systems enhance compliance by providing standardized, traceable processes, integrated quality control checks, and thorough documentation—features that are critical for gaining regulatory approval for diagnostics and therapies [12].
What is the return on investment (ROI) for implementing a partnered automation solution? The ROI is realized through significant long-term savings from reduced reagent waste (via miniaturized dispensing), decreased hands-on time, and fewer failed experiments due to human error [5] [12]. Automation can reduce hands-on time in library preparation by over 75%, from hours to just 45 minutes in some cases, freeing highly skilled personnel for data analysis and other value-added tasks [11].
Troubleshooting Guides
Problem 1: Inconsistent Library Yields and Quality
Potential Causes and Solutions:
- Cause: Manual pipetting inaccuracies during reagent dispensing. Even minor volumetric errors are amplified during PCR.
- Cause: Inefficient or variable bead-based clean-up steps in manual protocols.
- Solution: Integrate an automated clean-up device like the G.PURE into your workflow. These devices perform rapid, consistent magnetic bead-based purification in plate formats, standardizing this critical step across all samples [13].
- Cause: User-to-user and batch-to-batch variation.
Problem 2: Difficulty Scaling from Low- to High-Throughput NGS
Potential Causes and Solutions:
- Cause: Laboratory Information Management System (LIMS) integration failures create data silos and tracking issues.
- Solution: Prior to purchasing, verify the automation platform's compatibility with your existing LIMS. Choose systems designed for seamless integration to ensure smooth sample and data tracking from sample-in to result-out [12].
- Cause: Inability to efficiently process large sample batches due to hardware limitations.
- Cause: Protocol optimization for high-throughput takes too long.
- Solution: Leverage partnership-based solutions that offer pre-developed and pre-optimized scripts for common high-throughput kits, such as the DreamPrep NAP solution from Tecan and Zymo Research, which can save months of optimization time [7].
Problem 3: High Contamination Rates and False Positives
Potential Causes and Solutions:
- Cause: Sample cross-contamination from manual pipetting and handling.
- Cause: Inadequate real-time quality control, allowing low-quality samples to proceed.
- Solution: Implement automated QC tools like omnomicsQ that monitor sample quality in real-time against pre-set thresholds, flagging failing samples before they consume valuable sequencing resources [12].
Workflow Visualization
The following diagram illustrates how strategic partnerships integrate different technological components to create a seamless, automated NGS workflow, directly addressing common manual challenges.
Automated NGS Workflow Integration
Market Data and Performance Metrics
The tables below summarize key market data on the growing NGS library preparation market and quantitative performance gains from automation.
| Metric | Value | Source / Note |
|---|---|---|
| Global Market (2025) | USD 2.07 Billion | [14] |
| Projected Market (2034) | USD 6.44 Billion | [14] |
| CAGR (2025-2034) | 13.47% | [14] |
| Dominant Region (2024) | North America (44% share) | [14] |
| Fastest Growing Region | Asia Pacific (CAGR ~15%) | [14] |
| Fastest Growing Segment | Automated/High-Throughput Prep (CAGR 14%) | [14] |
Documented Benefits of Automated NGS Workflows
| Performance Metric | Manual Workflow | Automated Workflow | Improvement & Source |
|---|---|---|---|
| Hands-on Time (per run) | ~23 hours [11] | ~6 hours [11] | ~73% reduction |
| Total Runtime | 42.5 hours [11] | 24 hours [11] | ~44% faster |
| Aligned Reads | ~85% [11] | ~90% [11] | ~5 percentage point increase |
| Single-Cell Prep Hands-on Time | 4 hours [11] | 45 minutes [11] | Over 81% reduction |
| Inter-User Variation | High [5] | Eliminated [5] [12] | Essential for reproducibility |
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential components and platforms, often developed through industry partnerships, that are critical for establishing robust, automated NGS workflows.
| Item | Function in Automated NGS Workflow |
|---|---|
| Library Preparation Kits | Designed for compatibility with specific sequencers (e.g., Illumina, Oxford Nanopore) and applications (e.g., whole genome, targeted). Partnerships create kits optimized for automated liquid handlers [14] [11]. |
| Automated Liquid Handling Systems | Precisely dispense reagents and samples in nanoliter-to-microliter volumes, eliminating pipetting error and enabling high-throughput processing. Examples include Tecan Fluent and Beckman Biomek i-Series [12] [7]. |
| Magnetic Bead-Based Clean-Up Modules | Integrated automated systems for purifying and size-selecting nucleic acid fragments post-amplification, replacing manual and variable centrifugation steps. The G.PURE device is an example [13]. |
| Real-Time QC Software | Tools like omnomicsQ automatically monitor sample quality metrics (e.g., concentration, fragment size) against defined thresholds, flagging failures before sequencing [12]. |
| Integrated Workflow Software | Software (e.g., FluentControl) that allows users to build, run, and monitor automated protocols without needing advanced programming skills, streamlining operations [7]. |
In modern drug discovery, chemogenomics—the study of the interaction of chemical compounds with biological systems on a genome-wide scale—relies on generating consistent, reliable data. Reproducibility is the cornerstone that ensures scientific findings are valid, trustworthy, and translatable to clinical applications. The adoption of Automated Next-Generation Sequencing (NGS) workflows is pivotal for achieving the high-throughput and precision required for reproducible chemogenomic research. This guide addresses common challenges and provides actionable protocols to help researchers fortify the reproducibility of their chemogenomic studies.
Troubleshooting Guides for Automated NGS Workflows
FAQ 1: How can I minimize variability in automated NGS library preparation?
Issue: Inconsistent library yields and quality between automated runs.
Solution:
- Regular Calibration: Perform daily calibration of robotic liquid handlers. Use fluorescent dye-based volume verification kits to ensure pipetting accuracy [15].
- Process Lockdown: Once a method is validated, "lock down" the entire automated workflow. Document all parameters, including reagent brands, lot numbers, and incubation times [16].
- Environmental Controls: Monitor and record ambient temperature and humidity in the automation workspace, as these can affect enzymatic steps in library prep [15].
FAQ 2: What are the best practices for integrating automated sample tracking to ensure data integrity?
Issue: Sample misidentification or lost chain-of-custody in high-throughput screens.
Solution:
- Barcode Integration: Implement a system where sample plates are labeled with 2D barcodes. Configure your automated liquid handler to scan and verify each barcode at critical transfer points [17].
- LIMS Connection: Integate your automation platform with a Laboratory Information Management System (LIMS). This enables real-time data capture and traceability for every sample from receipt to sequencing [15].
- Verification Steps: Program the automation software to include verification steps, such as checking for successful tip attachment and confirming liquid presence in source wells before aspiration [18].
FAQ 3: How do I validate a new automated NGS workflow for chemogenomic applications?
Issue: Uncertainty about validation criteria and metrics when transitioning from manual to automated processes.
Solution: Adhere to a structured validation plan. The NGS Quality Initiative (NGS QI) provides frameworks specifically for this purpose [16]. Key metrics to evaluate are summarized in the table below.
Table 1: Key Performance Indicators (KPIs) for Automated NGS Workflow Validation
| Metric | Target | Measurement Method |
|---|---|---|
| Sample-to-Sample Contamination | < 0.1% | Quantification of negative controls via qPCR or bioanalyzer [16] |
| Library Prep Success Rate | > 95% | Fraction of samples passing QC thresholds (e.g., DV200 > 50%) [15] |
| Inter-Run Reproducibility | CV < 10% | Coefficient of Variation (CV) of on-target rate or unique reads across multiple runs [16] |
| Variant Calling Concordance | > 99.5% | Comparison of variant calls (SNPs, Indels) between automated and validated manual methods [18] |
| Hands-on Time Reduction | 50-65% | Comparison of active technician time pre- and post-automation [15] |
FAQ 4: How can I manage the high computational cost and data complexity of automated NGS?
Issue: Bioinformatics bottlenecks and data storage challenges.
Solution:
- AI-Enhanced Pipelines: Utilize AI-driven tools like
DeepVariantfor more accurate and efficient variant calling, which can reduce manual review time [18]. - Cloud Computing: Leverage cloud-based analysis platforms (e.g., DNAnexus, Illumina BaseSpace) that offer scalable computing power and pre-configured, validated bioinformatics pipelines [18].
- Data Management Plan: Establish a formal data lifecycle policy outlining retention periods for raw sequence data, processed files, and final reports to optimize storage costs [15].
Essential Experimental Protocols for Reproducibility
Protocol 1: Validating an Automated NGS Method for Chemogenomic Screening
This protocol outlines the core steps for ensuring your automated NGS method produces reproducible and reliable data, based on guidelines from the NGS Quality Initiative [16].
1. Define Objectives and Criteria:
- Clearly state the assay's purpose (e.g., "Identify genetic variants in a cell pool after treatment with a chemogenomic library").
- Establish acceptance criteria for all Key Performance Indicators (KPIs) prior to starting, referencing targets like those in Table 1.
2. Design the Validation Study:
- Sample Selection: Include a range of sample types (e.g., high/low quality DNA, positive/negative controls) that reflect real-world conditions.
- Replication: Perform a minimum of three independent runs on different days to assess inter-run precision.
3. Execute the Locked-Down Workflow:
- Use the automated system with standardized reagents and the "locked" protocol for all validation runs.
- Integrate with LIMS for full sample tracking.
4. Data Analysis and Performance Assessment:
- Process all sequencing data through a single, version-controlled bioinformatics pipeline.
- Calculate all pre-defined KPIs and compare them against the acceptance criteria.
5. Documentation and Reporting:
- Compile a validation report detailing the protocol, raw data, results for all KPIs, and a statement of pass/fail against each acceptance criterion.
Protocol 2: Implementing a Quality Management System (QMS) for NGS
A robust QMS is non-negotiable for reproducible science. The NGS QI provides tools to build this system [16].
1. Personnel Management:
- Standardized Training: Use SOPs like the "Bioinformatics Employee Training SOP" for consistent onboarding [16].
- Competency Assessment: Regularly assess staff proficiency using tools like the "Bioinformatician Competency Assessment SOP" [16].
2. Equipment Management:
- Preventive Maintenance: Adhere to a strict schedule for all automated equipment, including liquid handlers and sequencers.
- Documentation: Maintain logs for all maintenance, calibration, and performance verification activities.
3. Process Management:
- Standard Operating Procedures (SOPs): Develop and use detailed SOPs for every stage of the workflow, from sample accessioning to data reporting. The NGS QI's "NGS Method Validation SOP" is an excellent template [16].
- Continuous Monitoring: Use the "Identifying and Monitoring NGS Key Performance Indicators SOP" to track metrics like read quality and contamination rates over time, enabling proactive process corrections [16].
Essential Visualizations for Reproducible Workflows
NGS QMS Framework
Automated NGS Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Reproducible Chemogenomic Research
| Item | Function | Example / Key Feature |
|---|---|---|
| Chemogenomic (CG) Compound Library | Collections of small molecules with defined activity profiles used for high-throughput screening and target deconvolution [19]. | The EUbOPEN library covers one-third of the druggable proteome and is openly available [19]. |
| Validated Chemical Probes | The gold standard for modulating specific protein targets; highly characterized, potent, and selective small molecules [19]. | EUbOPEN probes are peer-reviewed and released with a structurally similar inactive control compound [19]. |
| Automated Liquid Handling Systems | Robots that perform precise and reproducible liquid transfers for NGS library preparation and assay setup [15] [18]. | Tecan Fluent systems automate PCR setup, NGS library prep, and nucleic acid extractions, integrating with AI for error detection [18]. |
| NGS Method Validation Plan Template | A structured document to guide the validation of NGS assays, ensuring they meet regulatory and quality standards [16]. | A template from the NGS Quality Initiative helps labs generate standardized validation documents, reducing development burden [16]. |
| AI-Enhanced Bioinformatics Tools | Software that uses machine learning to improve the accuracy and speed of NGS data analysis, such as variant calling [18]. | Tools like DeepVariant use deep neural networks to call genetic variants more accurately than traditional methods [18]. |
Within chemogenomic reproducibility research, the push to automate Next-Generation Sequencing (NGS) workflows is driven by two powerful, interconnected forces: the dramatic decline in sequencing costs and the escalating demand for high-throughput data. As sequencing becomes more affordable, larger and more robust experiments are possible, placing immense pressure on laboratories to maintain precision and consistency across thousands of samples. This technical support center addresses the specific challenges researchers and drug development professionals face when implementing automation to meet these demands, providing targeted troubleshooting and foundational protocols to ensure data integrity and reproducibility.
Troubleshooting Guides and FAQs
FAQ: My automated liquid handler is causing inconsistent library yields. What should I check?
- Problem: Variability in NGS library preparation yields on an automated platform.
- Solution:
- Verify Liquid Handler Calibration: Regularly calibrate the robotic pipettors to ensure volume dispensing accuracy. Improper calibration is a primary source of yield inconsistency [12].
- Inspect Reagent Quality and Storage: Ensure all reagents are fresh, thoroughly mixed, and have not expired. Pre-aliquot reagents to minimize freeze-thaw cycles [2].
- Check for Tip-Seating Issues: Confirm that disposable tips are consistently and firmly seated on the pipetting head to prevent volume loss [12].
- Audit Sample Quality: Before automation, quantify DNA input samples using a fluorometric method (e.g., Qubit) to ensure accurate starting concentrations and purity, as contaminants like salts or solvents can impair reactions [2].
FAQ: My sequencing run failed during instrument initialization with a "Chip Not Detected" error.
- Problem: The sequencer fails to recognize the flow cell or sequencing chip.
- Solution:
- Re-seat the Chip: Open the chip clamp, remove the chip, and carefully re-install it, ensuring it is properly seated [20].
- Inspect for Damage: Visually inspect the chip for any signs of physical damage or liquid where it shouldn't be. Replace if damaged [20].
- Wait for Green Checkmark: After inserting a new chip, wait for a green check mark to appear on the instrument screen indicating successful detection before proceeding [20].
- Reboot and Retry: Power cycle the instrument and its associated server. If the problem persists, contact technical support, as the chip socket may be faulty [20].
FAQ: How can I improve cross-contamination in my high-throughput automated workflow?
- Problem: Suspected sample-to-sample contamination in an automated NGS pipeline.
- Solution:
- Use Filter Tips: Always use filter tips to prevent aerosol contamination and sample carryover [12].
- Implement Wash Protocols: Utilize and optimize the liquid handler's wash routines for the robotic pipetting arms between reagent additions or sample transfers.
- Validate with Blanks: Incorporate negative control samples (e.g., water blanks) at regular intervals in your sample plates to monitor for contamination.
- Maintain Instrument Cleanliness: Adhere to a strict schedule for decontaminating and cleaning the instrument's work surface, grippers, and other components [12].
Data Presentation: NGS Platforms and Costs
The following tables summarize key quantitative data relevant to automated NGS workflows, aiding in platform selection and cost-benefit analysis.
Table 1: Comparison of Common NGS Sequencing Technologies
| Platform | Sequencing Technology | Read Length | Key Limitations |
|---|---|---|---|
| Illumina [21] | Sequencing-by-Synthesis (Bridge PCR) | Short (36-300 bp) | Overcrowding can spike error rate to ~1% [21] |
| Ion Torrent [21] | Sequencing-by-Synthesis (Semiconductor) | Short (200-400 bp) | Inefficient homopolymer sequencing causes signal loss [21] |
| PacBio SMRT [21] | Sequencing-by-Synthesis (Single Molecule) | Long (avg. 10,000-25,000 bp) | Higher cost per run [21] |
| Oxford Nanopore [21] | Electrical Impedance Detection (Single Molecule) | Long (avg. 10,000-30,000 bp) | Error rates can be high (up to 15%) [21] |
Table 2: Evolution of Whole Genome Sequencing (WGS) Cost
This cost reduction is a fundamental driver for scaling up chemogenomic studies through automation [22].
| Year | Approximate Cost per Human Genome | Key Driver |
|---|---|---|
| 2007 [22] | ~$1 Million | Early NGS commercialization |
| 2024 [22] | ~$600 | Established high-throughput platforms (e.g., Illumina) |
| Projected [22] | ~$200 | Next-generation platforms (e.g., Illumina NovaSeq X) |
Experimental Protocols
Detailed Methodology: Automated NGS Library Preparation for Reproducibility
This protocol is designed for a robotic liquid handling system integrated with a Laboratory Information Management System (LIMS) for traceability.
Sample Quality Control and Normalization:
- Quantify DNA samples using a fluorometer (e.g., Qubit) for high accuracy [2].
- Using the liquid handler, normalize all samples to a uniform concentration (e.g., 70 ng/μL) in nuclease-free water in a 96-well or 384-well plate [2].
- Barcode each sample well and register the plate in the LIMS to establish a chain of custody [15].
Automated Library Construction:
- DNA Shearing: Transfer normalized samples to a microplate designated for acoustic shearing (e.g., Covaris) to fragment DNA to the desired size.
- End Repair & A-Tailing: The robot adds master mix for end-repair and A-tailing to the sheared DNA fragments. The plate is sealed, mixed, and transferred to a thermocycler for incubation.
- Adapter Ligation: The system adds a unique dual-indexed adapter to each sample well. This step is critical for sample multiplexing and must be highly precise to avoid index swapping [12].
- Library Clean-Up: The robot performs solid-phase reversible immobilization (SPRI) using magnetic beads to purify the ligated library fragments, removing short fragments and excess adapters [2].
Library QC and Normalization:
- Quality Check: The system aliquots a sample of the purified library for QC, typically using a fragment analyzer (e.g., Agilent TapeStation) [2].
- Library Quantification: Quantify the library using a fluorometric method or qPCR.
- Pooling: Based on quantification data, the liquid handler precisely combines equimolar amounts of each indexed library into a single pooling tube for sequencing.
Workflow Visualization: Automated NGS Pipeline
The following diagram illustrates the logical workflow and integration points in an automated NGS pipeline for chemogenomic research.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and their functions in a typical automated NGS workflow.
| Item | Function | Brief Explanation |
|---|---|---|
| Fluorometer (e.g., Qubit) [2] | Nucleic Acid Quantification | Provides highly accurate concentration measurements of dsDNA or RNA, crucial for normalizing input material before automation. |
| Magnetic Beads (e.g., AMPure XP) [2] | Library Clean-up | Selectively bind to DNA fragments of desired sizes to remove enzymes, salts, and short fragments after reaction steps. |
| Fragmentation Kit [2] | DNA Shearing | Prepares genomic DNA for sequencing by breaking it into smaller, random fragments (e.g., via acoustic shearing or enzymatic digestion). |
| Library Prep Kit with Indexed Adapters [12] | Library Construction | Contains all enzymes and buffers for end-repair, A-tailing, and adapter ligation. Unique indexes allow sample multiplexing. |
| Fragment Analyzer [2] | Library Quality Control | Assesses the size distribution and integrity of the final sequencing library, ensuring it meets the specifications for the sequencer. |
Building Your Automated NGS Workflow: From Library Prep to Data Generation
Troubleshooting Guides
Troubleshooting Liquid Handling Errors
Precise liquid handling is critical for NGS library preparation. Inaccurate dispensing can lead to failed runs, inconsistent coverage, and compromised data integrity.
Problem: Inconsistent NGS Library Yields
- Symptoms: Low final library concentration, high duplicate rates in sequencing data, or uneven coverage.
- Potential Causes & Solutions:
- Cause: Pipetting inaccuracy, especially with small volumes. Manual pipetting of microliter volumes is a common source of error [1].
- Solution: Regularly maintain and calibrate automated liquid handlers. For manual steps, use master mixes to reduce pipetting steps and enforce the use of calibrated pipettes [1].
- Cause: Incorrect bead-based cleanup ratios (e.g., during library purification) leading to unintended size selection or sample loss [1].
- Solution: Strictly adhere to recommended bead-to-sample ratios. Standardize mixing and incubation times across all users [1].
Problem: Contamination in Sequencing Data
- Symptoms: High levels of adapter-dimers (sharp peak at ~70-90 bp on electropherogram) or foreign sequence reads [1].
- Potential Causes & Solutions:
- Cause: Carryover contamination from previous runs or cross-contamination between samples on the automated deck.
- Solution: Utilize liquid handlers with integrated contamination control features, such as HEPA filters, UV decontamination lights, and enclosed waste containers [23]. Implement rigorous deck cleaning protocols between runs.
Problem: Low-Quality Sequencing Libraries
- Symptoms: Broad or multi-peaked fragment size distributions in quality control checks.
- Potential Causes & Solutions:
- Cause: Inefficient fragmentation or enzymatic steps due to reagent or enzyme inhibitors [1].
- Solution: Use liquid handlers with real-time liquid-level sensing and pressure monitoring to confirm that reagents are fully aspirated and dispensed, preventing skipped steps [23]. Ensure input nucleic acid is pure and free of contaminants.
The following diagram outlines a systematic diagnostic strategy for resolving NGS library preparation failures.
Troubleshooting Robotic System Failures
Robotic components are subject to mechanical wear and require systematic maintenance to prevent downtime.
Problem: Robot Arm Movement Errors
- Symptoms: The robotic arm fails to move, is out of sync, or cannot reach its intended positions, leading to misaligned pipetting or plate handling.
- Potential Causes & Solutions:
- Cause: Mechanical misalignment or worn-out components in joints and gears [24].
- Solution: Perform regular mechanical inspections and lubrication of moving parts as per the manufacturer's schedule [24].
- Cause: Incorrect calibration of the motion and axis systems [24].
- Solution: Recalibrate the robotic arm and all deck positions. Use systems with integrated high-precision cameras to simplify and standardize the calibration process [23].
Problem: System Generates Fault Codes
- Symptoms: The automation software displays error or fault codes, halting the workflow.
- Potential Causes & Solutions:
Troubleshooting Workflow Software Integration
Seamless integration between software systems is essential for a fully automated NGS workflow.
Problem: Incompatibility with Existing Systems
- Symptoms: Inability to transfer sample data from a Laboratory Information Management System (LIMS) to the liquid handler, or failure to export run files for downstream analysis.
- Potential Causes & Solutions:
- Cause: The automated platform lacks compatibility with existing laboratory systems and data formats [12] [25].
- Solution: Prior to purchase, verify that the automation platform supports integration with your specific LIMS and NGS analysis pipelines. Look for systems that offer API access and compatibility with common file formats like CSV for sample lists [12] [26].
Problem: Failure in Sample Tracking
- Symptoms: Lost sample metadata or inability to trace results back to original samples.
- Potential Causes & Solutions:
- Cause: Poor integration between workflow software, robotics, and LIMS, breaking the chain of custody [12].
- Solution: Ensure the automated workflow software is fully integrated with LIMS for real-time tracking of samples, reagents, and process steps. This is critical for meeting regulatory compliance requirements like IVDR [12].
Frequently Asked Questions (FAQs)
1. What are the key benefits of automating NGS library preparation?
Automation significantly enhances reproducibility by standardizing protocols and eliminating human variability in pipetting [12]. It improves efficiency by increasing throughput and freeing up researcher time, and boosts accuracy by precisely dispensing small volumes, which is crucial for miniaturized reactions and cost savings [26] [25].
2. How do I choose the right automated liquid handler for my chemogenomics research?
When selecting a system, consider your required throughput (number of samples per run), the volume range (especially for low-volume dispensing), and precision needs (look for CVs <5% at microliter volumes) [26] [25]. Ensure it has features to prevent contamination and can integrate seamlessly with your existing LIMS and bioinformatics pipelines [12] [25].
3. Our automated NGS runs are showing inconsistencies between operators. How can we fix this?
This is a common issue in manual or semi-automated workflows. The solution is to standardize protocols within the automated system's software [12]. Create locked-down, validated protocols that all operators must use, and implement thorough training programs to ensure everyone is proficient in operating and basic troubleshooting of the systems [12] [24].
4. What regular maintenance do automated liquid handlers require?
Regular maintenance includes calibrating pipetting heads for volume accuracy, calibrating deck positions (a built-in camera can simplify this [23]), and performing mechanical inspections of robotic arms and moving parts [24]. Also, follow manufacturer guidelines for replacing consumables like HEPA filters and UV lamps to maintain contamination control [23].
5. How can automation help our lab meet regulatory standards like IVDR or ISO 13485?
Automated systems support compliance by providing complete traceability of samples and reagents, enforcing standardized and validated protocols, and generating the necessary documentation for audits [12]. Integrated quality control tools, which can flag samples that don't meet pre-defined quality thresholds, further ensure the reliability of results in a regulated environment [12].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential components and their functions in an automated NGS workflow for chemogenomic research.
| Item | Function in Automated NGS Workflows |
|---|---|
| Liquid Handling System | Precisely dispenses and transfers liquid reagents and samples for library prep. Key for complex, multi-step protocols and reaction miniaturization [23] [26]. |
| Magnetic Bead Station | Integrated on the deck of liquid handlers for automated purification and size selection of libraries, replacing manual centrifugation columns [23]. |
| Cooling/Heating Blocks | Maintains specific temperatures for enzymatic reactions (e.g., ligation, PCR) during automated runs, ensuring optimal reaction conditions [23]. |
| Laboratory Information Management System (LIMS) | Tracks samples, reagents, and process steps in real-time, ensuring data integrity and traceability for reproducible and compliant workflows [12]. |
| qPCR Instrument | Used for accurate quantification of sequencing libraries pre-pooling. Some systems can be seamlessly operated from the same interface as the liquid handler [23]. |
| Variant Interpretation Software | Tertiary analysis software that links identified variants to biological and clinical annotations, enabling the creation of custom reports for chemogenomic insights [27]. |
Automated NGS Workflow Integration
The diagram below illustrates the logical relationship and data flow between the core components of an automated NGS workflow.
FAQs: Addressing Common Library Preparation Challenges
Q1: What are the primary causes of low library yield and how can they be fixed? Low library yield often stems from poor input DNA/RNA quality, inaccurate quantification, inefficient fragmentation or ligation, or over-aggressive purification steps [1]. To address this:
- Re-purify Input Sample: Ensure nucleic acid purity with 260/280 ratios around ~1.8 and 260/230 > 1.8 to remove enzyme inhibitors [1].
- Use Fluorometric Quantification: Replace UV absorbance methods with Qubit or PicoGreen for accurate template quantification [1] [28].
- Optimize Ligation Conditions: Titrate adapter-to-insert molar ratios, use fresh ligase, and maintain optimal temperature [29] [1].
- Review Cleanup Parameters: Avoid over-drying magnetic beads and use correct bead-to-sample ratios to prevent sample loss [1].
Q2: How can I reduce PCR-induced bias in my library? PCR bias, which leads to uneven coverage and high duplicate rates, can be minimized by:
- Reducing PCR Cycles: Use the minimum number of cycles necessary. Optimize your kit to require fewer cycles through high-efficiency end repair, A-tailing, and adapter ligation [28].
- Choosing Robust Enzymes: Select polymerases known to minimize amplification bias [30].
- Utilizing Unique Molecular Identifiers (UMIs): Tag individual molecules with UMIs to differentiate true variants from PCR errors [28].
- Adopting Hybridization Capture: For targeted sequencing, prefer hybridization-based enrichment over amplicon approaches, as it typically requires fewer PCR cycles and yields better uniformity [28].
Q3: What are the critical steps to prevent sample contamination and cross-contamination? Contamination risk can be significantly reduced through laboratory best practices and automation:
- Dedicate Pre-PCR Areas: Perform sample extraction and PCR setup in separate, dedicated areas to prevent amplicon contamination [30].
- Use Unique Dual Indexes (UDIs): Employ UDIs for multiplexing, which allows for accurate demultiplexing and helps identify and prevent index hopping [28].
- Automate Liquid Handling: Automated systems use disposable tips and controlled workflows to minimize the chance of carryover between samples [12] [29].
- Follow Basic Lab Hygiene: Aliquot reagents to avoid freeze-thaw cycles, wipe surfaces with appropriate solutions, and prepare fresh 70% ethanol daily for wash steps [28].
Q4: How does automation specifically improve the reproducibility of NGS library prep? Automation enhances reproducibility by standardizing every aspect of the protocol:
- Eliminates Manual Variability: Automated liquid handling systems dispense reagents with precise volumes, removing inconsistencies introduced by manual pipetting [12] [29].
- Enforces Standardized Protocols: Robotic systems execute predefined, validated protocols with consistent timing and incubation conditions, eliminating batch-to-batch variations [12].
- Integrates Quality Control: Some automated platforms can integrate with quality control tools (e.g., omnomicsQ) to monitor sample quality in real-time, flagging deviations before they affect downstream steps [12].
Troubleshooting Guides
Common Library Preparation Failures and Solutions
Table: Troubleshooting Common NGS Library Preparation Issues
| Problem Category | Typical Failure Signals | Common Root Causes | Corrective Actions |
|---|---|---|---|
| Sample Input & Quality | Low yield; smeared electropherogram; low complexity [1] | Degraded DNA/RNA; sample contaminants (phenol, salts); inaccurate quantification [1] | Re-purify input; use fluorometric quantification (Qubit); check purity ratios [1] |
| Fragmentation & Ligation | Unexpected fragment size; sharp ~70-90 bp peak (adapter dimers) [1] | Over-/under-shearing; poor ligase performance; incorrect adapter:insert ratio [1] | Optimize fragmentation parameters; titrate adapter ratios; ensure fresh ligation reagents [29] [1] |
| Amplification & PCR | High duplicate rate; over-amplification artifacts; sequence bias [30] [1] | Too many PCR cycles; inefficient polymerase; primer exhaustion [1] | Reduce PCR cycles; use high-fidelity enzymes; employ UMIs [30] [28] |
| Purification & Cleanup | High adapter-dimer signal; sample loss; carryover of salts [1] | Wrong bead:sample ratio; over-dried beads; inadequate washing [1] | Precisely follow bead cleanup protocols; avoid over-drying beads; use fresh wash buffers [1] [28] |
Quantitative Performance Metrics for Automated Workflows
Automated NGS library preparation directly enhances key performance metrics essential for reproducible chemogenomic research.
Table: Key Performance Metrics from an Automated Targeted Sequencing Workflow [31]
| Performance Measure | Result (at 95% CI) | Significance for Reproducibility |
|---|---|---|
| Sensitivity | 98.23% | High likelihood of detecting true variants, including low-frequency mutations. |
| Specificity | 99.99% | Minimal false positives, ensuring reliable variant calls for downstream analysis. |
| Repeatability (Intra-run Precision) | 99.99% | Exceptional consistency within a single sequencing run. |
| Reproducibility (Inter-run Precision) | 99.98% | High consistency across different runs, operators, and days. |
| Accuracy | 99.99% | Overall reliability of the sequencing data generated by the automated workflow. |
Workflow Visualization: Automated NGS Library Preparation
The following diagram illustrates a streamlined, automated workflow for NGS library preparation, integrating key steps from nucleic acid extraction to sequencing-ready libraries.
Automated NGS Library Prep Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Table: Key Reagents and Kits for Automated NGS Library Preparation
| Item | Function | Application Notes |
|---|---|---|
| Magnetic Beads | Size selection and purification of nucleic acids; used in clean-up steps [30] [1] | Bead-to-sample ratio is critical. Over-drying can lead to inefficient elution and sample loss [1]. |
| Hybridization Capture Kits (e.g., xGen Hybrid Capture) | Target enrichment for sequencing specific genomic regions; used in automated targeted panels [32] | More robust than amplicon-based methods, providing better uniformity and fewer false positives [28]. |
| Unique Dual Indexes (UDIs) | Barcodes for multiplexing samples; allow accurate demultiplexing and prevent index hopping [28] | Essential for complex, multi-sample studies. Enables pooling of dozens of libraries in a single run [28]. |
| FFPE DNA Repair Mix | Enzyme mixture to reverse DNA damage from formalin fixation [28] | Crucial for working with degraded clinical FFPE samples to reduce sequencing artifacts and recover original sequence complexity [28]. |
| Library Quantification Kits (qPCR-based) | Accurately measure concentration of amplifiable library fragments [33] | Prefer over fluorometric methods for pooling libraries, as it only measures adapter-ligated molecules, preventing over/under-loading [28] [33]. |
| Automated Library Prep Kits (e.g., for MGI SP-100RS) | Reagents formulated for compatibility with automated liquid handling systems [31] | Designed for reduced hands-on time and improved reproducibility on platforms like the Biomek i3 or MGISP-100 [31] [32]. |
Frequently Asked Questions (FAQs)
Q1: What are the main benefits of automating NGS sample preparation? Automating NGS sample prep significantly enhances accuracy, reproducibility, and throughput while reducing costs. It eliminates human errors associated with manual pipetting, minimizes the risk of cross-contamination, and standardizes protocols to ensure consistent results across different runs and operators [5] [12]. Furthermore, automation drastically reduces hands-on time, freeing up researchers for more complex tasks [5].
Q2: How does miniaturization of reagent volumes lead to cost savings? Miniaturization involves using nanoliter-scale liquid handling to dispense reagents. This directly conserves expensive reagents and enables the use of smaller, cheaper labware (e.g., 384-well plates). One study demonstrated that a miniaturized, automated approach could process thousands of samples weekly for less than $15 per sample [13].
Q3: My automated workflow is producing inconsistent library yields. What could be the cause? Inconsistent yields often point to issues with liquid handling or reagent integration. First, verify that your liquid handler is correctly calibrated, as imprecise dispensing will directly affect reaction efficiency [7]. Second, ensure all reagents are thoroughly mixed and at the correct temperature before the run begins. Contamination from previous runs can also be a factor, so implement regular cleaning procedures [20].
Q4: What are the first steps in transitioning from a manual to an automated NGS workflow? A successful transition requires careful planning. Begin by conducting a thorough assessment of your laboratory's specific needs, including sample volume, required throughput, and existing bottlenecks [12]. Next, select an automation platform that integrates seamlessly with your Laboratory Information Management System (LIMS) and downstream analysis pipelines. Finally, invest in comprehensive, hands-on training for personnel to ensure a smooth adoption of the new system and protocols [12].
Q5: How can I ensure my automated NGS workflow is reproducible for chemogenomic research? Reproducibility is achieved through rigorous standardization. Use automated systems to enforce strict adherence to validated protocols, eliminating user-to-user variation [5] [12]. Implement real-time quality control tools to monitor sample quality and flag deviations immediately [12]. Finally, choose automation platforms that provide complete traceability for regulatory compliance, which is crucial for chemogenomic reproducibility research [13] [12].
Troubleshooting Guides
Issue 1: Low or Inconsistent Sequencing Data Output
| Possible Cause | Recommended Action | Prevention Strategy |
|---|---|---|
| Error in library quantification | Re-quantify libraries using fluorometric methods (e.g., Qubit) to ensure accuracy over spectrophotometry. | Standardize quantification and quality control steps across all automated runs [12]. |
| Pipetting inaccuracies in automation | Check liquid handler calibration; verify nozzle and tip performance for consistent nanoliter dispensing [13]. | Implement regular maintenance and calibration schedules for all automated equipment. |
| Poor template preparation | Verify the quantity and quality of the input library and template preparations before sequencing [20]. | Use integrated systems that automate the entire workflow from sample-in to library-out to minimize variability [13]. |
Issue 2: High Contamination or Background Noise in Data
| Possible Cause | Recommended Action | Prevention Strategy |
|---|---|---|
| Carryover contamination | Perform consumable-free clean-ups or use fresh tips for every sample transfer [5]. | Use closed, automated systems to minimize environmental exposure and human intervention [5]. |
| Contaminated reagents | Prepare fresh reagents and aliquot into single-use volumes. | Use automated quality control to flag samples that do not meet pre-defined quality thresholds before sequencing [12]. |
Issue 3: Automated Liquid Handling Failures
| Possible Cause | Recommended Action | Prevention Strategy |
|---|---|---|
| Clogged nozzles | Execute a line clear procedure and perform routine cleaning with recommended solutions (e.g., isopropanol) [20]. | Implement a regular cleaning and maintenance schedule as per the manufacturer's instructions. |
| Incorrect worktable design | Re-configure the worktable layout to ensure sufficient deck space and correct placement of labware [7]. | Invest in a universal worktable configuration with a user-friendly GUI that visually confirms correct deck setup [7]. |
| Software or connectivity issues | Restart the instrument and connected servers; check for and install any required software updates [20]. | Choose automation software that is modular and does not require extensive programming expertise to operate [7]. |
Quantitative Data on Automation and Miniaturization
The following table summarizes key quantitative benefits of implementing automation and miniaturization in NGS workflows, as evidenced by published studies.
Table 1: Impact of Automation and Miniaturization on NGS Workflows
| Metric | Manual Workflow | Automated & Miniaturized Workflow | Source / Protocol |
|---|---|---|---|
| Hands-on Time | ~3 hours | < 15 minutes | Sequencing-ready DNA prep platforms [13] |
| Cost per Sample | High | < $15 per sample | COVseq protocol using I.DOT Liquid Handler [13] |
| Reagent Consumption | High | Reduced via nanoliter dispensing | Non-contact, low-volume dispensing [13] |
| Data Reproducibility | Variable, user-dependent | High, minimal batch effects | Automated library prep systems [5] |
Experimental Protocols
Protocol 1: Automated, Miniaturized Library Preparation for Genomic Surveillance
This protocol, adapted from Simonetti et al. (2021), outlines a cost-effective method for large-scale sequencing, such as viral genomic surveillance [13].
- Sample Input: Use low-input samples (e.g., 5-10 ng of DNA).
- Liquid Handling: Employ a non-contact liquid handler (e.g., I.DOT Liquid Handler) to dispense library construction reagents in nanoliter volumes into a 384-well plate.
- Library Construction: Automate key steps, including enzymatic fragmentation, end-repair, adapter ligation, and PCR amplification, using an integrated workstation.
- Purification: Perform magnetic bead-based clean-up using an integrated device (e.g., G.PURE NGS Clean-Up Device).
- Quality Control: Pool the libraries and quantify using a fluorometric method. The resulting libraries are ready for sequencing.
Protocol 2: Open-Source, Automated Multiplexed Imaging (PRISMS)
This protocol, based on Zhang et al. (2025), describes an automated pipeline for spatial omics, demonstrating modularity and cost reduction [34].
- Automated Staining: Use a liquid handling robot with thermal control (e.g., Opentrons OT-2) to perform rapid, cyclic staining of RNA or protein targets on multiple tissue slides or coverslips.
- Modular Mounting: Place samples in 3D-printed or laser-cut acrylic holders compatible with various microscopes.
- Automated Imaging: Execute a custom Python (Jupyter notebook) script that:
- Writes commands for microscope software (e.g., Nikon NIS Elements) for automated acquisition.
- Computes autofocus correction for Z-drift.
- Captures individual fields of view (FOVs), tiled scans, or a combination.
- Post-Processing: The Python script generates a Fiji/ImageJ macro to stitch overlapping images and, if required, perform super-resolved reconstructions (e.g., SRRF).
Workflow Diagrams
Automated NGS Library Prep
PRISMS Multiplexed Imaging
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for Automated NGS
| Item | Function in Automated Workflows |
|---|---|
| Non-Contact Liquid Handler | Precisely dispenses nanoliter volumes of reagents for library prep, enabling miniaturization and reducing costs [13]. |
| Magnetic Bead-Based Clean-Up Kits | Used in automated systems for rapid and consistent purification of nucleic acids during library preparation steps [13]. |
| Sequencing-Ready DNA Prep Kits | Integrated reagent kits designed for fully automated, "sample-in, library-out" workflows, minimizing hands-on time [13]. |
| Open-Source Control Software | Python-based scripts (e.g., PRISMS) that customize and control laboratory instruments for tailored, automated assays [34]. |
| External Quality Assessment (EQA) Panels | Standardized samples used to validate and ensure cross-laboratory consistency and accuracy of automated NGS workflows [12]. |
Troubleshooting Guides
Guide 1: Resolving Data Transfer Failures Between Sequencer and LIMS
Q: The automated data transfer from our NextSeq 550 system to Clarity LIMS has failed. The run is complete, but the data is not appearing in the LIMS. What are the first steps I should take?
A: This is often a disruption in the automation trigger. Follow these steps to diagnose the issue [35]:
- Check the Integration Version: Confirm the version of the installed Illumina NextSeq Integration Package by running the command
rpm -qa | grep -i nextseqfrom the Clarity LIMS server console [35]. - Review Log Files: If the error involves data parsing or missing results, check the
NextSeqIntegrator.logfile, typically located at/opt/gls/clarity/extensions/Illumina_NextSeq/v2/SequencingService/[35]. - Investigate Automation Worker: Refer to the "Troubleshooting Automation Worker" section in your Clarity LIMS administration documentation for broader issues with automation triggers [35].
Q: For a NovaSeq 6000, the automated run step starts but does not complete. How can I find more details?
A: You can access detailed logging information directly from the Clarity LIMS interface [36]:
- Log in to Clarity LIMS and locate the in-progress step via the "Lab View" in the "Recent Activities" pane or by searching with the Library Tube or Flowcell barcode [36].
- On the "Record Details" screen, find the "Sequencing Log" multiline text field. This log contains specific information about the run process [36].
- If the interface does not provide enough information, review the
sequencer-api.logfile on the server for deeper technical details [36].
Guide 2: Troubleshooting Bioinformatics Pipeline Failures at the LIMS Handoff
Q: Our bioinformatics pipeline has failed with a "Foreign key constraint violation" error. What does this mean and how can it be fixed?
A: This technical error often has a simple scientific cause. It typically means that sample IDs in the sequencing file do not match any samples registered in the experiment within your LIMS [37]. This is a common sample tracking issue.
- Actionable Solution: Instead of a generic SQL error, a well-designed pipeline would display: "Sample ID ABC123 not found in experiment registry. Check [Your Sample Registry, e.g., Benchling] or contact the data team if this sample should exist." [37]. This message points you directly to the problem—a sample ID mismatch—and tells you exactly what to do next.
Q: The pipeline fails a QC step. What is the most likely cause and what are the next steps?
A: A QC failure usually indicates an issue with the raw sequencing data or sample quality.
- Actionable Solution: Look for a specific error like, "QC failed: 12% of reads below quality threshold (expected <5%). Contact the sequencing core." [37]. This tells you the metric that failed, the observed value, the expected value, and the responsible team to contact. This is preferable to a non-actionable "ValueError" which provides no guidance [37].
Guide 3: Addressing Data Quality and Sample Tracking Errors
Q: I am concerned about the "Garbage In, Garbage Out" (GIGO) principle. What are the key data quality pitfalls in automated NGS workflows?
A: Ensuring data quality is critical, as errors at the start can corrupt all downstream analysis [38]. Common pitfalls include:
- Sample Mislabeling: A survey found up to 5% of samples in clinical sequencing labs had labeling or tracking errors. This can lead to incorrect scientific conclusions or, in clinical settings, misdiagnoses [38].
- Batch Effects: Systematic technical differences between groups of samples processed at different times can mimic biological signals. This requires careful experimental design and statistical correction [38].
- Technical Artifacts: PCR duplicates, adapter contamination, and systematic sequencing errors can mimic real biological signals. Using tools like FastQC, Picard, and Trimmomatic is essential to identify these issues [38].
Proactive Methodologies for Ensuring Data Quality [38]:
- Implement Standard Operating Procedures (SOPs): Use detailed, validated protocols for every step from sample collection to data analysis.
- Automate Where Possible: Use automated sample handling and LIMS tracking to reduce human error in repetitive tasks.
- Establish QC Checkpoints: Monitor metrics like Phred scores, read length distributions, and alignment rates at every stage of the pipeline.
- Perform Data Validation: Check that data makes biological sense (e.g., gene expression profiles match known tissue types) and use cross-validation with alternative methods like qPCR.
Frequently Asked Questions (FAQs)
Q: What are the core benefits of integrating automation with a LIMS for NGS workflows?
A: Seamless integration creates a unified digital backbone for the lab, offering [39] [40]:
- Elimination of Manual Data Entry: Direct instrument integration automatically captures test results and parameters, saving time and preventing transcription errors [40].
- Complete Traceability: Track a sample and all its derivatives (extracted DNA, libraries, etc.) from submission through testing, analysis, and reporting with a full audit trail [39].
- Workflow Automation: Automate repetitive tasks like sample registration, QC checking, and report generation, allowing scientists to focus on complex analysis [40].
- Enhanced Reproducibility: Enforces standardized procedures and captures all data and metadata, which is crucial for chemogenomic reproducibility research [39].
Q: We are planning a new LIMS implementation. What are the best practices to ensure successful integration with our automated systems?
A: A successful implementation hinges on careful planning [41] [40]:
- Define Clear Goals: Start with specific, measurable objectives (e.g., "reduce data entry time by 30%") rather than vague desires to "improve efficiency" [41].
- Create a Detailed Requirements List: Have a complete understanding of your lab's processes and the data types/formats the LIMS must handle. Focus on main requirements first [40].
- Avoid Over-Customization: Stick to the must-have features and use a vendor that offers them. Excessive customizations drive up costs and complexity [41].
- Allocate Proper Resources: Implementation is a two-team effort involving both the vendor's specialists and your own lab staff to ensure the system fits daily workflows [41].
- Plan for Data Migration: Carefully plan and execute the transfer of data from legacy systems to ensure data integrity and compliance [41].
Q: How can we make our bioinformatics pipelines more user-friendly and easier for scientists to debug?
A: The key is to translate technical failures into actionable, scientific context [37]. Build these elements into your pipelines:
- Clear Error Messages: Errors should state what happened and why in scientific terms, and suggest a clear next step. For example, "Missing replicate numbers for 3 samples in plate P2024-089. Replicates required for statistical analysis." [37].
- Comprehensive Logging: Logs should tell a story with timestamps, input files, sample counts, and quality metrics so scientists can reconstruct what happened [37].
- Sensible Retry Logic: Configure the pipeline to retry after transient errors like network glitches, but not for failed QC, which requires human judgment [37].
Workflow and Data Flow Diagrams
NGS Integration Architecture
Error Resolution Workflow
Research Reagent Solutions
The following table details key materials and digital solutions essential for robust and reproducible automated NGS workflows.
| Item Name | Type | Function in Automated Workflow |
|---|---|---|
| GLUE Integration Engine [39] | Software/Data Infrastructure | Acts as a data cloud management solution; standardizes data models and enables seamless connectivity between over 200 laboratory instruments, data sources, and bioinformatics tools via API, SFTP, ASTM, and HL7 protocols [39]. |
| LabWare LIMS [42] | Enterprise Software Platform | A highly configurable LIMS designed for complex lab workflows. Provides robust sample lifecycle management, instrument integration, and compliance features (21 CFR Part 11, GLP) for large-scale, reproducible operations [42]. |
| Clarity LIMS [35] [36] | Software Platform | Illumina's web-based LIMS, commonly integrated with NGS platforms like NextSeq and NovaSeq. Manages sample tracking, sequencing runs, and automated data transfer from instrument to analysis [35] [36]. |
| FastQC [38] | Bioinformatics Tool | Provides quality control metrics for raw sequencing data (e.g., Phred scores, GC content). Used as an initial checkpoint to prevent "garbage in, garbage out" by identifying issues in sequencing runs or sample prep [38]. |
| Genome Analysis Toolkit (GATK) [38] | Bioinformatics Pipeline | A standard for variant discovery in high-throughput sequencing data. Its best practices provide detailed recommendations for variant quality assessment and filtering, which is critical for data integrity in chemogenomic research [38]. |
| Electronic Lab Notebook (ELN) [39] [42] | Software Module | Integrated within modern LIMS platforms to digitally record methods, protocols, and observations. Ensures procedural reproducibility and creates a full audit trail for regulated environments [39] [42]. |
| OncoKB / PharmGKB [39] | Knowledge Database | Curated databases of actionable genomic variants and drug-gene relationships. Integration with the bioinformatics pipeline enables automated therapeutic interpretation of variant data for clinical reporting [39]. |
Troubleshooting Guides & FAQs for Automated NGS Workflows
Oncology Research
FAQ: Our automated variant calling in oncology panels shows inconsistent results between runs. How can we improve reproducibility?
Inconsistent variant calling often stems from pre-analytical variables. Key steps to improve reproducibility include:
- Standardize Input Quality: Ensure all samples meet minimum quality thresholds (e.g., DV200 > 30% for FFPE RNA) before entering the automated workflow. Use fluorometric quantification (Qubit) instead of absorbance to accurately quantify usable nucleic acids [1].
- Automate Library Quantification: Use automated, qPCR-based library quantification instead of manual methods to ensure precise, equal molar pooling of libraries, which is critical for uniform coverage [12] [15].
- Implement Real-Time QC: Integrate a quality control solution like omnomicsQ to monitor samples in real-time and flag those that fall below pre-defined quality thresholds before downstream analysis [12].
FAQ: We are observing high duplicate read rates in our automated hybrid capture workflows for cancer genomics. What is the cause?
High duplication rates often indicate issues early in the workflow, frequently related to insufficient library complexity. Common causes and solutions are summarized below [1]:
| Cause | Mechanism | Corrective Action |
|---|---|---|
| Low Input DNA | Inadequate starting material reduces library complexity, leading to over-amplification of fewer original molecules. | Re-quantify input DNA with a fluorometric method; ensure input mass meets the protocol's minimum requirement. |
| Over-amplification | Too many PCR cycles during library amplification preferentially amplify a subset of fragments. | Optimize and reduce the number of PCR cycles in the automated protocol; use the minimum necessary for detection. |
| Inefficient Purification | Incomplete removal of primers and adapter dimers can lead to their over-representation in the final library. | Review and adjust automated bead-based cleanup parameters on your liquid handler, such as the bead-to-sample ratio [1]. |
Infectious Disease Research
FAQ: How can we improve the detection of low-abundance pathogens in metagenomic sequencing on an automated system?
Sensitivity in metagenomic sequencing is highly dependent on reducing background and maximizing the yield of microbial sequences.
- Minimize Cross-Contamination: Automated liquid handlers with disposable tips are excellent for reducing cross-contamination between samples, which is crucial for avoiding false positives [12].
- Reduce Host Nucleic Acids: Incorporate an automated host depletion step (e.g., using probes to remove human rRNA and DNA) into your workflow to enrich for microbial sequences.
- Optimize Fragmentation: Verify that the automated fragmentation settings (e.g., sonication time, enzymatic digestion) are calibrated to produce the desired insert size for your platform, as over-fragmentation can bias GC-rich microbial genomes [1].
FAQ: Our automated RNA library prep for transcriptomic studies of pathogens yields low. What should we check?
Low yield in RNA library prep can halt a project. Follow this diagnostic flowchart to identify the root cause.
Single-Cell Sequencing
FAQ: Our automated single-cell RNA-seq workflow shows high levels of ambient RNA contamination. How can we mitigate this?
Ambient RNA is a common issue in droplet-based single-cell workflows. Automation can both introduce and help solve this problem.
- Review Reagent Dispensing: Ensure the liquid handler is calibrated to dispense cell suspension and reagents smoothly and accurately. Aggressive pipetting can lyse cells, releasing RNA into the solution [12].
- Incorporate Enzymatic Cleanup: Use an automated platform to integrate enzymatic cleanup steps (e.g., using RNase inhibitors or specific nucleases) that degrade free-floating RNA without affecting encapsulated cellular material.
- Utilize Software Solutions: Employ bioinformatic tools post-sequencing to computationally identify and subtract the ambient RNA signal from your cell counts.
FAQ: Cell throughput in our automated single-cell sample loading is lower than expected.
This is often a hardware or fluidics issue.
- Check for Clogs: Inspect the fluidics lines and nozzles of the automated dispenser for partial clogs.
- Verify Cell Concentration and Viability: Ensure your input cell suspension is at the optimal concentration and has high viability. Clumps of dead cells can easily clog microfluidic chips.
- Re-calibrate Pressure/Vacuum Settings: The pressure or vacuum settings on the instrument may need re-calibration to ensure smooth and continuous flow of cells.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential reagents and their functions in automated NGS workflows for the featured application areas [32].
| Reagent Solution | Function in Automated Workflow |
|---|---|
| Archer FUSIONPlex | Targeted RNA-based assay for gene fusion detection in oncology, automated on platforms like the Biomek i3 [32]. |
| VARIANTPlex | Targeted DNA-based assay for mutation detection in oncology, optimized for automated liquid handling to ensure reproducibility [32]. |
| xGen Hybrid Capture | Solution for enriching specific genomic regions (e.g., for infectious disease pathogen detection or exome sequencing) in an automated, high-throughput format [32]. |
| Automated Library Prep Kits | Formulated for reduced hands-on time and consistent performance with robotic systems, covering applications from DNA-seq to single-cell RNA-seq [12] [15]. |
| Pooled Barcoded Primers | Enable multiplexing of hundreds of samples by adding unique molecular identifiers during automated library construction, crucial for single-cell and high-throughput projects [12]. |
Detailed Experimental Protocol: Automated Targeted NGS for Oncology
This protocol outlines the automated preparation of libraries for targeted sequencing (e.g., using VARIANTPlex) on a benchtop liquid handler like the Biomek i3 [32].
Workflow Overview: The process transforms extracted DNA into a sequenced-ready library through a series of automated steps.
Step-by-Step Methodology:
Input DNA Quality Control (Manual):
- Quantify DNA using a fluorometric method (e.g., Qubit dsDNA HS Assay). Do not rely on absorbance alone [1].
- Assess DNA integrity (e.g., via Genomic DNA ScreenTape or similar). For FFPE samples, note the degree of fragmentation.
- Dilute all samples to the required mass and volume in a 96-well plate using the liquid handler's automated dilution function.
Automated Library Construction (Hands-off):
- Transfer the normalized DNA plate to the deck of the liquid handler.
- The method automatically adds fragmentation and end-repair enzymes to each sample.
- Following incubation, the system adds ligation buffer and barcoded adapters to each reaction. The precise molar ratio of adapter to insert is critical and is handled accurately by the robot [12] [1].
- The workflow includes a bead-based cleanup step to stop the reaction and remove excess adapters.
Indexing PCR & Post-PCR Cleanup (Hands-off):
- The liquid handler adds a PCR master mix containing index primers to each sample.
- The plate is transferred by the robot to an integrated on-deck thermocycler for amplification [32].
- After cycling, the plate is retrieved, and a second bead-based cleanup is performed to remove PCR reagents and select for the desired library size.
Automated Hybrid Capture (Hands-off):
- The normalized libraries are pooled by the liquid handler into a single tube or well.
- The system adds biotinylated probes (e.g., xGen Lockdown Probes) to the pooled library and transfers the mixture to the integrated thermocycler for hybridization.
- Streptavidin-coated magnetic beads are added, and the target-library complexes are bound to the beads. The liquid handler performs a series of wash steps to remove non-specifically bound DNA.
Final Amplification & QC (Hands-off):
- A final PCR amplifies the captured library. The robot performs a last bead-based cleanup.
- The final library is quantified via an automated qPCR assay on the liquid handler to determine the concentration of amplifiable molecules [12].
- The library is normalized and pooled with other samples for sequencing.
Maximizing Performance: Best Practices for Troubleshooting and Optimizing Automated NGS
FAQs and Troubleshooting Guides
Adapter Ligation Troubleshooting
Q: My sequencing results show a high percentage of adapter-dimer contamination. What are the primary causes and solutions?
Adapter dimers, often visible as a sharp peak near 70-90 bp on an electropherogram, can dominate a library and reduce usable sequencing data [1]. The following table outlines the common causes and corrective actions.
| Cause | Mechanism | Corrective Action |
|---|---|---|
| Suboptimal Adapter-to-Insert Ratio [1] | Excess adapters in the ligation reaction promote adapter-to-adapter ligation instead of adapter-to-insert ligation. | Titrate the adapter:insert molar ratio. Use a lower ratio to minimize dimer formation while maintaining ligation efficiency [1]. |
| Inefficient Ligation [1] | Poor ligase performance or reaction conditions reduce the rate of insert ligation, allowing adapter dimerization. | Ensure fresh ligase and buffer; maintain optimal temperature (~20°C for blunt-end); avoid heated lid interference; optimize incubation time [1]. |
| Incomplete Purification [1] | Failure to remove adapter dimers after the ligation reaction allows them to be amplified in subsequent PCR steps. | Use bead-based cleanup with an optimized bead-to-sample ratio to selectively remove small fragments [1]. |
| Overly Aggressive Size Selection [1] | Excessive loss of the target insert size range during cleanup can make adapter dimers a larger proportion of the final library. | Optimize size selection parameters to maximize recovery of desired fragments without co-purifying dimers. |
Q: I am experiencing low library yield after adapter ligation. How can I improve efficiency?
Low yield post-ligation can stem from several issues related to input DNA, reaction setup, and preceding steps [1].
| Cause | Mechanism of Yield Loss | Corrective Action |
|---|---|---|
| Poor Input DNA Quality [1] | Residual contaminants (e.g., salts, phenol, EDTA) can inhibit the ligase enzyme. | Re-purify the input DNA using clean columns or beads. Check absorbance ratios (260/280 ~1.8, 260/230 >1.8) to confirm purity [1]. |
| Incorrect Ends for Ligation | DNA fragments lack the required blunt, phosphorylated ends or the 3'A-overhang for TA-ligation. | Ensure the end-repair and A-tailing steps were performed correctly with fresh reagents and appropriate incubation times [43]. |
| Suboptimal Ligation Temperature/Time [29] | The reaction conditions do not allow for maximum enzyme efficiency. | For cohesive-end ligations, use lower temperatures (12–16°C) and longer durations (e.g., overnight). For blunt-end ligations, room temperature for 15-30 minutes with high enzyme concentration is typical [29]. |
Enzyme Handling Troubleshooting
Q: My enzymatic fragmentation (or tagmentation) results are inconsistent between runs. What factors should I control?
Inconsistent fragmentation leads to skewed insert size distributions and biased sequencing coverage [1].
| Cause | Impact on Experiment | Corrective Action |
|---|---|---|
| Enzyme Degradation [29] | Reduced enzyme activity causes under-fragmentation, leading to longer than expected insert sizes. | Maintain a stable cold chain; avoid repeated freeze-thaw cycles by aliquoting enzymes; store at recommended temperatures [29]. |
| Inaccurate Quantification/Pipetting [1] | An incorrect enzyme-to-DNA ratio results in over- or under-fragmentation. | Use fluorometric methods (e.g., Qubit) for accurate DNA quantification. Calibrate pipettes and use master mixes to reduce pipetting error [1]. |
| Presence of Enzyme Inhibitors [1] | Contaminants in the DNA sample inhibit the fragmentation enzyme. | Re-purify the input DNA to remove salts, solvents, and other inhibitors prior to fragmentation [1]. |
| Lot-to-Lot Reagent Variation | Different batches of enzymes may have slightly different activities. | Validate fragmentation parameters with each new reagent lot to ensure consistency [43]. |
Q: How does improper enzyme handling specifically impact PCR amplification during library prep?
Improper handling during the amplification step can introduce bias and reduce library complexity [1].
| Problem | Observed Failure Signal | Solution |
|---|---|---|
| Overamplification [1] | High duplicate read rates, amplification artifacts, and skewed sequence representation. | Minimize the number of PCR cycles. Re-amplify from leftover ligation product rather than overcycling a weak product [1]. |
| Enzyme Inhibition [1] | Low or no yield after PCR. | Ensure carryover of salts or phenol from previous steps is eliminated through effective cleanup. Use high-fidelity polymerases that are more tolerant of reaction conditions. |
Visual Workflows: From Manual to Automated Optimization
The following diagrams illustrate the workflow for optimizing adapter ligation and enzyme handling, highlighting critical points where automation can significantly enhance reproducibility.
Manual NGS Library Prep Risk Points
Automated NGS Library Prep Benefits
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and their critical functions in ensuring successful adapter ligation and maintaining enzyme integrity.
| Reagent / Kit | Primary Function | Critical Handling & Optimization Notes |
|---|---|---|
| DNA Ligase (e.g., T4 DNA Ligase) | Catalyzes the formation of a phosphodiester bond between the adapter and the DNA insert [43]. | Use fresh buffer (ATP degrades with freeze-thaw cycles). Titrate adapter:insert ratio (1:1 to 1:10). For difficult ligations (e.g., single base overhangs), consider specialized master mixes [44]. |
| Methylated Adapters | Adapters that are methylated to protect against cleavage by certain restriction nucleases. Allows for indexing at the initial ligation step, streamlining the workflow [45]. | Universal, methylated adapter designs can reduce the number of purification and pipetting steps, improving overall workflow efficiency and robustness for multiplex sequencing [45]. |
| High-Fidelity DNA Polymerase | Amplifies the adapter-ligated library while introducing minimal errors and bias [43]. | Essential for minimizing mutations during PCR. Use polymerases with proofreading activity. Always minimize the number of amplification cycles to avoid skewing representation and increasing duplicate rates [1] [43]. |
| Magnetic Beads (AMPure-style) | Purifies reactions by removing unwanted components like adapter dimers, salts, and enzymes. Used for size selection and cleanup [1] [43]. | The bead-to-sample ratio is critical. An incorrect ratio can lead to loss of desired fragments or failure to remove small artifacts. Avoid over-drying the bead pellet, as this leads to inefficient resuspension and low elution yield [1]. |
| Nuclease-Free Water | A pure, uncontaminated solvent for resuspending oligos and diluting samples. | Using low-quality water can introduce nucleases that degrade primers, adapters, and enzymes, leading to complete workflow failure. Always use certified nuclease-free water. |
In chemogenomic reproducibility research, the integrity of Next-Generation Sequencing (NGS) data is paramount. Manual liquid handling introduces significant variability through pipetting inaccuracies and human error, directly compromising the reliability of experimental outcomes. Automated pipetting and reagent dispensing systems address these challenges by standardizing workflows, enhancing precision, and ensuring that results are both reproducible and trustworthy.
FAQs: Troubleshooting Automated Liquid Handling
1. Our automated liquid handler seems to be over-dispensing expensive reagents. What could be causing this and how can we fix it?
Inaccuracy in volume dispensing can stem from several sources. First, verify that the instrument is regularly calibrated, as drift can occur over time [46]. Second, ensure you are using manufacturer-approved tips, as poor-quality or ill-fitting tips are a common root cause of volume delivery errors [47]. Finally, review the liquid class settings and aspirate/dispense parameters in your software; these must be optimized for the specific viscosity and surface tension of the reagents you are using [47].
2. We've noticed cross-contamination between wells during a serial dilution protocol. How can we prevent this?
Cross-contamination in automated systems often arises from satellite droplets or liquid carryover. To mitigate this:
- Use Filter Tips: If your system uses disposable tips, filter tips can prevent aerosol contamination [46].
- Optimize Dispensing Parameters: Adjust dispense rates and heights to minimize droplet formation. For some reagents, adding a trailing air gap can prevent liquid from slipping out of the tip [47].
- Implement Tip Wash Protocols: If using fixed tips, ensure rigorous and validated washing protocols are in place to remove all residual reagent [47].
- System Flushing: Perform post-dispense line flushing and tip clean cycles as recommended by the manufacturer [48].
3. After switching to an automated system for NGS library prep, we are seeing increased variability in our sequencing coverage. Could the automation be at fault?
While automation generally improves reproducibility, variability can be introduced if the system is not properly validated. Key areas to check include:
- Mixing Efficiency: Ensure that the automated mixing steps in your protocol are sufficient to create homogenous solutions, particularly after reagent additions. Inefficient mixing will lead to uneven concentrations across your plate [47].
- Sequential Dispensing Inaccuracy: When a large volume is aspirated and then dispensed sequentially, the first and last dispenses can have different volumes. Validate that the same volume is dispensed across all wells [47].
- Tip Depth: Ensure the aspiration depth is consistent and compensated for decreasing liquid levels in source reservoirs to maintain accuracy [47].
4. What are the best practices for handling viscous or volatile reagents with an automated liquid handler?
Specialized techniques are required for non-aqueous reagents:
- Viscous Reagents (e.g., Glycerol, PEG): Use "reverse mode" pipetting, where more liquid is aspirated than is dispensed. Employ wider bore or low-retention tips, and use slower aspiration and dispense rates to ensure accuracy [49].
- Volatile Reagents: Use a "reverse pipette" mode or a rapid dispense feature to minimize the time between aspiration and dispensing, thus reducing evaporation. A prewetting step can also help equilibrate the air cushion in the tip [49].
- Consult Guidelines: Refer to system-specific application notes for compatible concentration ranges of additives like detergents and viscous agents [48].
Quantitative Error Analysis: Manual vs. Automated Pipetting
The following table summarizes common pipetting errors and the performance improvements offered by automation, which are critical for sensitive NGS applications.
Table 1: Comparison of Common Pipetting Errors and Automated Solutions
| Error Source | Impact in Manual Pipetting | Automated Solution & Performance |
|---|---|---|
| Inconsistent Angle | Volume inaccuracy when deviating beyond 20 degrees [49]. | Robotic systems maintain a consistent, vertical pipetting angle [49]. |
| Pre-wetting Not Performed | Variable volumes due to surface tension and evaporation [49]. | Programmable pre-wetting steps ensure equilibrium [49]. |
| Inconsistent Plunger Force | Significant intra- and inter-user variability in aspirated volumes [46]. | Automated systems apply consistent force and speed for every transfer [46]. |
| Sequential Dispensing | The first and last dispenses in a series often have different volumes [47]. | Advanced systems can be validated to dispense uniform volumes across all wells [47]. |
| Liquid Handling Accuracy | High risk of error, especially in high-throughput manual tasks [5]. | Systems like the I.DOT Non-Contact Dispenser achieve precision down to 8 nL with 5% CV for reproducible library prep [50] [51]. |
Experimental Protocols for Error Minimization
Protocol 1: Calibration and Verification of Automated Liquid Handler Volume Transfer
Purpose: To regularly verify the accuracy and precision of volume transfers by an automated liquid handler, ensuring data integrity in quantitative NGS steps.
Materials:
- Automated liquid handler (e.g., I.DOT Non-Contact Dispenser)
- Analytical balance (sensitivity to 0.0001 g)
- Weighing boat or low-retention microcentrifuge tubes
- Purified water
- Temperature probe
Method:
- Environmental Equilibration: Allow the purified water and all equipment to equilibrate to the same ambient temperature (e.g., 20–25 °C) for at least 2 hours.
- Density Calculation: Using the analytical balance and temperature probe, measure the density of the water at the ambient temperature.
- System Priming: Prime the liquid handler according to the manufacturer's instructions.
- Gravimetric Analysis:
- Tare a clean weighing boat or tube on the balance.
- Program the liquid handler to dispense a target volume (e.g., 1 µL, 10 µL) into the vessel.
- Record the weight of the dispensed water.
- Repeat this process at least 10 times for statistical significance.
- Volume Calculation: Calculate the actual dispensed volume for each trial using the formula: Volume (µL) = Mass (mg) / Density (g/mL).
- Data Analysis: Determine the average dispensed volume, accuracy (% of target value), and precision (% Coefficient of Variation).
Troubleshooting: If accuracy or precision falls outside acceptable limits (e.g., >5% deviation), proceed with instrument calibration, check for tip seal integrity, and verify liquid class parameters [47] [46].
Protocol 2: Validation of Homogeneous Mixing in NGS Library Preparation Clean-up Steps
Purpose: To confirm that automated mixing steps produce homogenous bead-resuspension mixtures, which is critical for efficient and uniform NGS library clean-ups.
Materials:
- Automated liquid handler with mixing capabilities (e.g., orbital mixing or aspirate/dispense mixing)
- 96-well or 384-well microplate containing magnetic beads
- Assay buffer
- Spectrophotometer or imaging system
Method:
- Plate Setup: Dispense a consistent volume of magnetic beads and buffer into a column of wells on a microplate using the automated system.
- Automated Mixing: Execute the automated mixing protocol (e.g., a defined number of aspirate/dispense cycles at a set rate or orbital mixing for a specified duration).
- Homogeneity Assessment:
- Immediately after mixing, use the liquid handler to rapidly transfer equal aliquots from the top, middle, and bottom of the liquid column in multiple wells to a clear-bottom assay plate.
- Measure the optical density or take a high-resolution image of the assay plate to visualize the consistency of bead distribution across the aliquots.
- Data Analysis: Quantify the signal variation between the aliquots. A low coefficient of variation (<10%) indicates successful homogenization.
Troubleshooting: If mixing is inhomogeneous, increase the number of mix cycles, adjust the mix speed, or change the mixing depth. Inefficient mixing leads to inconsistent bead binding and variable library yields [47].
Workflow Visualization
The following diagram illustrates a standardized automated NGS library preparation workflow, highlighting key stages where automation minimizes human error.
The diagram above maps the key stages of NGS library preparation where automation directly intervenes to standardize the process. At each step, automated systems mitigate specific error types: precise reagent dispensing ensures correct enzymatic reactions, accurate mix transfers prevent adapter dimer formation, and consistent bead handling during clean-ups leads to uniform library yields. This end-to-end standardization is fundamental for achieving reproducible chemogenomic data.
The Scientist's Toolkit: Key Research Reagent Solutions
The table below details common reagents used in NGS workflows and the specific considerations for their automated dispensing.
Table 2: Key Reagents for Automated NGS Workflows
| Reagent / Additive | Function in NGS | Automated Dispensing Considerations |
|---|---|---|
| PEG 8000 | Library purification and size selection [48]. | Viscous additive. For a 50 nL dispense, keep concentration between 2.5-17.5% (w/v) to minimize satellite droplets [48]. |
| Glycerol | Cryoprotectant; component of enzyme storage buffers [48]. | Highly viscous. Use reverse pipetting mode. Compatible with dispensing at 30% (v/v) for 50 nL volumes [48]. |
| Tween-20 | Surfactant to reduce surface tension and prevent non-specific binding [48]. | Non-ionic detergent. For a 50 nL dispense, concentrations of 0.1-5% (v/v) are compatible with minimal satellite droplets [48]. |
| SDS | Ionic detergent for cell lysis and protein denaturation [48]. | Anionic detergent. Dispensing is highly volume-dependent. For 100 nL, keep concentration ≤0.05% (w/v) to avoid contamination [48]. |
| Magnetic Beads | SPRI clean-up for size selection and purification [50]. | Suspensions must be kept homogenous during transfer. Automated systems must include vigorous mixing steps before and during dispensing [50]. |
The transition from manual to automated pipetting is a critical step towards achieving the high levels of accuracy and reproducibility required in modern chemogenomic research. By understanding common error sources, implementing rigorous validation protocols, and leveraging the precise control offered by automated systems, researchers can significantly enhance the reliability of their NGS data and drive more confident scientific conclusions.
FAQ: Troubleshooting Library Normalization
Why is accurate library normalization critical for my sequencing results? Inaccurate normalization leads to the over- or under-representation of individual libraries in a pooled sequence run [29]. This causes significant bias in sequencing depth, where some samples consume a disproportionately high number of reads while others are poorly sequenced, compromising data quality and the ability to compare results across samples [29].
What are the common pitfalls of manual normalization? Manual quantification and dilution are time-consuming and introduce variability due to human error during pipetting [29]. This often results in batch effects and inconsistent data, making it difficult to achieve reproducible results, especially across large sample batches or different users [29] [12].
My sequencing results show uneven coverage across samples. Could this be due to poor normalization? Yes, uneven coverage is a classic symptom of improper library normalization [29]. When libraries are not accurately quantified and pooled in equimolar amounts, the sequencing instrument's capacity is not utilized evenly, leading to some genomic regions or samples being deeply sequenced while others have very low coverage.
How can I prevent adapter dimers from affecting my library quantification? Adapter dimers are small fragments that can form during library preparation and are co-amplified with your target library [52]. To prevent them from skewing quantification results, it is crucial to include a cleanup step, such as size selection using magnetic beads or gel electrophoresis, to deplete these dimers before library quantification and pooling [52].
Quantification Techniques for Accurate Normalization
Selecting the right quantification method is the first step toward eliminating bias. The table below compares the common techniques.
| Method | Principle | Advantages | Limitations | Best for |
|---|---|---|---|---|
| qPCR | Quantifies only amplifiable library fragments using adapter-specific primers [33]. | Most accurate for NGS; reflects sequencing potential; recommended for barcode balancing [33]. | More complex and time-consuming than fluorometry [33]. | Projects requiring the highest accuracy, such as clinical assays [33]. |
| Fluorometry | Uses fluorescent dyes to bind to nucleic acids (e.g., dsDNA) [29]. | Fast and easy; suitable for checking library yield and size [29]. | Cannot distinguish between adapter-ligated fragments and primer dimers; can overestimate concentration [29]. | Initial quality control check; not recommended for final normalization before pooling. |
| Fragment Analysis | Separates library fragments by size via capillary electrophoresis. | Provides a visual profile of fragment size distribution and identifies contaminants. | Higher cost and more specialized equipment than fluorometry. | Verifying library fragment size and detecting adapter dimer contamination. |
Experimental Protocol: Bead-Based Normalization for Automated Workflows
This protocol is designed for integration with automated liquid handling systems, ensuring high reproducibility for chemogenomic research.
1. Principle: Utilizes magnetic beads to both clean up and normalize libraries. The bead-to-sample ratio can be adjusted to selectively bind to the desired library fragment size range, removing unwanted reagents and simultaneously normalizing library concentrations across samples [29].
2. Reagents and Equipment:
- Purified, adapter-ligated NGS libraries
- Magnetic beads (e.g., SPRIselect)
- Freshly prepared 80% ethanol
- Nuclease-free water or elution buffer
- Automated liquid handling workstation (e.g., incorporating a non-contact dispenser like the I.DOT [29])
- Thermonixer or compatible automated heating/shaking module
- Magnetic stand (compatible with automation)
3. Step-by-Step Procedure: 1. Quantify: Quantify all individual libraries using a qPCR-based method to determine the starting concentration [33]. 2. Dilute: Dilute each library to a low, uniform concentration (e.g., 1-2 nM) based on the qPCR results. 3. Bind: Combine a precise, calibrated volume of magnetic beads with each diluted library on the automated workstation. The bead volume determines the size cutoff and the final normalized concentration. Mix thoroughly. 4. Incubate: Incubate at room temperature for 5-10 minutes to allow DNA fragments to bind to the beads. 5. Separate: Engage the magnetic stand to separate beads from the solution. Wait until the supernatant is clear. 6. Wash: With the magnetic stand engaged, automatically remove and discard the supernatant. Perform two washes with 80% ethanol without disturbing the bead pellet. 7. Dry: Air-dry the bead pellet for a few minutes to ensure all ethanol has evaporated. Do not over-dry. 8. Elute: Resuspend the beads in a standardized volume of elution buffer or nuclease-free water to release the purified DNA. The resulting libraries are now cleaned and normalized. 9. Finalize: Combine equal volumes of each eluted, normalized library to create the final sequencing pool.
4. Quality Control:
- Re-quantify the final pooled library using fluorometry to confirm the expected concentration.
- Run the pool on a fragment analyzer to verify the correct size profile and ensure adapter dimers have been removed.
Research Reagent Solutions
| Item | Function |
|---|---|
| Automated Liquid Handler | Precisely dispenses nanoliter-scale volumes of reagents and libraries, eliminating pipetting errors and ensuring consistency across all samples [29] [12]. |
| Magnetic Beads | Provide a scalable and automatable method for library cleanup, size selection, and normalization based on sample-to-bead ratios [29]. |
| qPCR Quantification Kit | Accurately measures the concentration of amplifiable, adapter-ligated library fragments, which is critical for calculating equimolar pooling ratios [33]. |
| Library Preparation Kit | Provides optimized, ready-to-use reagents for efficient end repair, adapter ligation, and PCR amplification, reducing protocol variability [52]. |
Integration with Automated NGS Workflows
For chemogenomic reproducibility research, manual normalization is a major source of irreproducibility. Automated systems directly address this by:
- Standardizing Protocols: Automated systems enforce strict adherence to validated protocols, eliminating technician-to-technician variability in pipetting and reagent handling [12].
- Ensuring Traceability: Integration with Laboratory Information Management Systems (LIMS) enables real-time tracking of samples and process steps, which is critical for regulatory compliance and replicating studies [15] [12].
- Enabling Scalability: Automation allows laboratories to process hundreds of samples per week with minimal hands-on time, making large-scale chemogenomic screens feasible and reproducible [15].
Automated Library Normalization Workflow
Implementing Real-Time Quality Control and Automated Monitoring Systems
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What are the most common signs of a failed NGS library preparation, and what are their primary causes?
A: Common failure signals include low library yield, high duplication rates, and prominent adapter-dimer peaks (e.g., a sharp peak at ~70-90 bp on an electropherogram) [1]. The root causes are often categorized into a few key areas [1]:
- Sample Input/Quality: Degraded DNA/RNA or contaminants like phenol or salts that inhibit enzymes.
- Fragmentation/Ligation: Over- or under-shearing, or an improper adapter-to-insert molar ratio.
- Amplification/PCR: Too many PCR cycles, leading to overamplification artifacts and bias.
- Purification/Cleanup: Using an incorrect bead-to-sample ratio, leading to incomplete removal of adapter dimers or significant sample loss.
Q2: How can automation reduce human error in NGS workflows?
A: Automated sample prep addresses several sources of human error [5] [53]:
- Pipetting Precision: It removes variability and inaccuracies in manual pipetting.
- Protocol Deviation: It ensures that complex, multi-step protocols are followed precisely every time, eliminating variations between technicians.
- Cross-Contamination: Automated, closed systems minimize human handling, thereby reducing the risk of sample contamination.
Q3: Our lab is experiencing intermittent NGS failures that seem operator-dependent. What steps can we take to improve consistency?
A: Intermittent, operator-dependent failures point to procedural variations [1]. Corrective actions include:
- Reinforcing SOPs: Highlight critical steps in your Standard Operating Procedures (SOPs) and use checklists.
- Master Mixes: Switch to master mixes to reduce the number of pipetting steps and associated errors.
- Process Safeguards: Introduce "waste plates" to temporarily hold discarded material, allowing for recovery in case of a mistake.
- Automation: For highly repetitive and sensitive steps, consider implementing automated liquid handling systems [5].
Q4: What key metrics should we monitor for real-time quality control of a sequencing run?
A: Key quality metrics to monitor in real-time include [54]:
- Q Score: A measure of base-calling accuracy. A score above 30 is generally considered good.
- Error Rate: The percentage of bases incorrectly called.
- Cluster Density: The number of clusters per square millimeter. A very high density can lower the percentage of clusters passing filter (% PF).
- PhiX/Prephasing: The percentage of signal loss because clusters fall behind (phasing) or jump ahead (prephasing) during sequencing.
Troubleshooting Guides
Table 1: Troubleshooting Common NGS Library Preparation Issues
| Problem Symptom | Potential Root Cause | Corrective Action |
|---|---|---|
| Low Library Yield [1] | Poor input quality/contaminants; inaccurate quantification; suboptimal adapter ligation; aggressive size selection. | Re-purify input sample; use fluorometric quantification (e.g., Qubit) instead of UV absorbance only; titrate adapter:insert ratio; optimize bead-based cleanup ratios. |
| High Duplicate Read Rate [1] | Over-amplification due to too many PCR cycles; insufficient starting material. | Reduce the number of PCR cycles; increase input material if possible. |
| Prominent Adapter-Dimer Peak [1] | Inefficient ligation; incorrect adapter-to-insert molar ratio; incomplete cleanup. | Titrate adapter concentration; optimize ligase reaction conditions; use a higher bead-to-sample ratio in cleanup to remove short fragments. |
| Inconsistent Results Between Operators [1] | Deviations from protocol in pipetting, mixing, or timing; reagent degradation. | Implement detailed SOPs with emphasized critical steps; use master mixes; introduce operator training checklists. |
| Poor Base Quality Scores, especially at read ends [54] | Normal signal decay in sequencing-by-synthesis; instrument issues. | Perform quality trimming of read ends using tools like CutAdapt or Trimmomatic as part of the standard bioinformatic pipeline. |
Detailed Experimental Protocol: Implementing an Automated QC Workflow
This protocol outlines the methodology for integrating real-time quality control checks within an automated NGS library preparation workflow, based on innovations in microfluidic and liquid handling systems [55] [13].
1. System Setup and Integration:
- Automated Platform: Utilize an integrated automated system, such as a microfluidic lab-on-a-chip (LoC) cartridge or a liquid handling workstation. The system should be capable of performing library prep steps (multiplex PCR, end-repair, ligation, purification) and integrated quantification [55].
- Reagent Storage: Pre-store all necessary enzymes, buffers, and magnetic beads in the designated reagent reservoirs or as lyophilized beads within the cartridge to avoid manual intervention [55].
- QC Module Integration: Ensure the platform has an integrated optical readout system (e.g., for qPCR) to perform in-line quantification and assess library quality metrics before sequencing [55].
2. Automated Library Preparation with In-Process QC:
- Target Enrichment (Multiplex PCR): The automated system performs the initial multiplex PCR to enrich target regions. The reaction mix is shuttled between different temperature zones on the chip for thermal cycling [55].
- Library Construction: The workflow automatically executes end-repair, adapter ligation, and index PCR using pre-stored reagents. Each enzymatic step is followed by a magnetic bead-based purification using Solid Phase Reversible Immobilization (SPRI) to remove enzymes, salts, and short fragments [55].
- In-Line Quantification: After the final purification, the system uses an integrated quantification step (e.g., a qPCR assay or fluorescence measurement) to determine the concentration of the final, amplifiable library. This data serves as a key quality indicator and is used to normalize loading for sequencing [55].
3. Data Analysis and Validation:
- Sequencing: Pool normalized libraries and sequence on the chosen NGS platform.
- Bioinformatic QC: Process the raw sequencing data (FASTQ files) using quality control tools like FastQC to generate reports on per-base sequence quality, GC content, and adapter contamination [54].
- Variant Calling Validation: For target enrichment workflows, analyze the resulting BAM files using a variant caller. Compare the variant allelic frequencies (e.g., from a reference cfDNA sample with known mutations) between the automated on-chip preparation and the manual reference workflow. Successful validation is indicated by a high correlation (e.g., Pearson r = 0.94) [55].
Workflow Visualization
Automated NGS QC System Workflow
Integrated Quality Control Checkpoints
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Automated NGS QC Workflows
| Item | Function in the Workflow |
|---|---|
| NEBnext Ultra II Library Kit | Provides all necessary enzymes and buffers for manual or automated library construction, including end-repair, ligation, and PCR mix [55]. |
| Cell-free DNA (cfDNA) Reference Material | A biologically relevant control with known mutations at varying allelic frequencies (e.g., 0.1%, 1%, 5%) to validate the performance and sensitivity of the automated workflow [55]. |
| Magnetic Carboxylated Beads | Used in Solid Phase Reversible Immobilization (SPRI) for automated nucleic acid purification and size selection between enzymatic steps in the microfluidic cartridge [55]. |
| Qubit dsDNA HS Assay Kit | A fluorometric method for accurate quantification of double-stranded DNA library concentration, superior to UV absorbance for this purpose [1] [55]. |
| HS NGS Fragment Analysis Kit | Used with a Fragment Analyzer or TapeStation to assess library size distribution and detect contaminants like adapter dimers, providing a crucial QC checkpoint [55] [54]. |
In chemogenomic research, the ability to reproducibly identify interactions between chemical compounds and genomic targets is paramount. Next-generation sequencing (NGS) is a cornerstone of this research, but traditional manual library preparation methods can introduce variability that compromises data integrity [56] [15]. Automation is a powerful strategy to overcome these challenges, ensuring the precision, efficiency, and scalability required for robust, reproducible science [15]. This guide provides a strategic framework and technical support for selecting and implementing the right NGS library preparation automation platform for your laboratory's specific needs.
Part 1: A Strategic Framework for Automation Assessment
Selecting an automation platform is a strategic process that extends beyond merely purchasing equipment. The following phased framework ensures your investment aligns with long-term scientific and operational goals.
Phase 1: Foundational Assessment & Goal Setting
Before evaluating specific technologies, establish a clear understanding of your internal needs and constraints.
- Define Roles and Responsibilities: Ensure clarity among all stakeholders. The Product Owner (often an end-user scientist) defines scientific needs, the Project Owner manages timelines and communications, and Key Stakeholders (e.g., facilities managers, executive sponsors) align the project with business objectives and ROI [57].
- Establish Project Goals and ROI Metrics: Balance upfront implementation costs (equipment, purchasing, deployment) against long-term operational costs (maintenance, reagent consumption, personnel time) [57]. Key questions to ask include:
- What are our short-term versus long-term throughput needs?
- How will automation improve our data reproducibility and reduce error rates?
- Do we have the in-house expertise to operate and maintain the system, or will we rely on vendor support?
Phase 2: Workflow & Technical Specification
With goals defined, translate them into technical requirements.
- Conduct a Workflow Audit: Identify repetitive, error-prone, or bottleneck steps in your current NGS library prep workflow that are most suitable for automation [15]. Common candidates include liquid handling steps, adapter ligation, and library normalization.
- Define Technical Requirements: Based on the audit, specify your needs for:
- Throughput: Number of samples processed per day or week.
- Compatibility: Must work with your preferred NGS library prep kits (e.g., Illumina, IDT) and sequencers [14] [58].
- Functionality: Essential features like on-deck thermocycling, magnetic bead-based cleanups, and integrated quality control [56] [58].
Phase 3: Vendor Evaluation & Platform Selection
Evaluate potential platforms against the criteria established in Phase 2.
- Integration and Interoperability: Choose a platform with broad compatibility. Prefer systems that support open standards and robust APIs for seamless integration with existing instruments, Laboratory Information Management Systems (LIMS), and data analysis pipelines [59] [15]. Proprietary, closed systems can lead to data silos and workflow disruptions [59].
- Scalability and Flexibility: Your system should scale with your research. As one source notes, "As laboratories expand and their needs evolve, a system that meets current demands may become insufficient" [59]. Consider modular systems that can be upgraded or reconfigured.
- Vendor Support and Service: Investigate the vendor's history, local support staff, and the comprehensiveness of their training programs. Inadequate training is a common cause of system underutilization and errors [60] [59].
The diagram below summarizes this strategic assessment workflow.
Part 2: Laboratory Readiness & Implementation Planning
Successful automation requires careful planning for space, safety, and data management.
Facilities and Space Planning
A thorough site assessment is critical for a smooth installation [57]. Key considerations include:
- Space Constraints: Check ceiling height, doorway measurements, and pathway widths for safe equipment transport and accessibility [57].
- Floor Requirements: Assess floor flatness, levelness, and weight restrictions [57].
- Utilities Planning: Identify available power sources, compressed air, and networking connections. Engage your facilities team early [57].
Safety: A Non-Negotiable Priority
Safety must be integrated from the initial design phase [57]. Critical actions include:
- Conduct a Risk Assessment: Perform a structured analysis to identify and prioritize potential injury risks from the automated system [57] [61].
- Implement Safety Architecture: Apply required protective measures such as E-stops, safety interlocks, and physical enclosures [57].
- Provide Protection: Large equipment can increase exposure to noise and heat; ensure staff have appropriate protective gear and that lab temperature is controlled [61].
Data Management and Integration
Automated systems generate large volumes of data. A proactive data strategy is essential.
- Plan for Data Integration: Map your software architecture and define data inputs and outputs. Ensure the system can integrate with your LIMS or Electronic Lab Notebook (ELN) for traceability [57] [15].
- Ensure Data Security and Integrity: Implement software with robust data management features, including secure storage, real-time tracking, and comprehensive audit trails for regulatory compliance [59].
Part 3: Troubleshooting Guides and FAQs
Frequently Asked Questions
1. How can a lab automation solution help me manage my lab more efficiently? Automation addresses productivity challenges posed by complex testing and staff shortages. It improves workflow, standardizes processes, reduces manual errors, and offers faster results, which is crucial for the reproducibility of chemogenomic assays [60] [15].
2. What are the most common failure points in automated systems? Many errors occur at the human-computer interface or in specific hardware components [61]. Common issues include:
- Barcode Read Failures: Caused by poorly printed labels, dirty readers, or tubes that are not vertical [61].
- Solenoid or Sensor Errors: These sensitive components can halt the system if they become dirty, faulty, or misaligned [61].
- Gripper Failures: Often due to tube misalignment, labels sticking to grippers, or general wear and tear [61].
3. Our team is resistant to new technology. How can we encourage adoption? Foster a culture of innovation and open communication. Involve employees in the transition process, emphasize how automation will enhance their roles by reducing repetitive tasks, and provide opportunities for skill development [59]. Comprehensive training is key to overcoming reluctance [59] [61].
4. How important is the vendor's IT or middleware solution? It is critical. An integrated IT solution from your primary vendor is often preferable to a third-party system. If there is a problem with a third-party system, resolving it may involve additional vendors, leading to extra charges and longer downtime [60].
Troubleshooting Common Issues
| Issue Category | Specific Problem | Potential Cause | Solution |
|---|---|---|---|
| Hardware | System halts with sensor error | Dirty, faulty, or misaligned sensor [61] | Clean, realign, or replace the sensor as per manufacturer guidelines. |
| Hardware | Barcode read failure | Poorly printed label; smeared reader; tube not vertical [61] | Use a high-quality label printer; clean the barcode reader; ensure tube is seated correctly. |
| Hardware | Gripper fails to pick up tube | Tube misalignment in carrier; worn gripper pads [61] | Realign tube in carrier; inspect and replace gripper pads if worn. |
| Data & Software | Inability to connect to LIMS | Incompatible data formats; insufficient network permissions [59] | Work with IT and vendor to ensure software compatibility and correct security settings. |
| Process | Inconsistent library yields | Variable liquid handling; reagent degradation | Perform liquid handler calibration; ensure proper storage and handling of reagents. |
| Process | Contamination in libraries | Carry-over during liquid transfer; open well plates | Implement protocols with sufficient clean-up steps; use sealed plates where possible. |
Part 4: Experimental Protocols & The Scientist's Toolkit
Automating an Illumina DNA Prep Workflow
The following methodology outlines how to automate a common NGS library prep protocol, ensuring consistency for chemogenomic applications.
1. Pre-Run Preparation
- Equipment & Reagents: Ensure the automated liquid handler (e.g., Beckman Coulter Biomek i7, Hamilton NGS STAR) is calibrated. Thaw and mix all reagents from the Illumina DNA Prep kit. Keep reagents cool on deck chillers if available [58].
- Labware Setup: Load the deck with required tip boxes, a 96-well PCR plate for reactions, and reservoirs for beads and other reagents.
2. Automated Protocol Steps
- DNA Normalization & Tagmentation: The robot transfers a standardized volume of DNA sample to the PCR plate and adds tagmentation buffer. After a controlled incubation, a neutralizing reagent is added.
- PCR Setup: The system adds unique dual index primers and PCR mix to each well for sample multiplexing.
- Post-PCR Clean-Up: The method uses magnetic beads for purification. The robot performs multiple wash steps to remove excess primers and enzymes, and finally elutes the purified library in a resuspension buffer.
3. Post-Processing and QC
- The finished libraries are manually transferred from the plate for quality control analysis, such as fragment size distribution and quantification, using methods like fluorometry or automated electrophoresis (e.g., Fragment Analyzer) [56] [58].
Key Research Reagent Solutions for Automated NGS
The table below details essential materials and their functions in a typical automated NGS library prep workflow.
| Item | Function in Automated Workflow |
|---|---|
| Library Prep Kits (e.g., Illumina DNA Prep, IDT xGen) | Provide all necessary enzymes, buffers, and adapters in a formulation optimized for automated liquid handling, ensuring consistent reaction performance [14] [32]. |
| Magnetic Beads | Used for automated reaction clean-up and size selection. They selectively bind to nucleic acids, allowing the system to perform wash steps and elution without manual intervention [56]. |
| Indexing Primers | Unique barcode sequences added by the automation to each sample library, enabling multiplexing of hundreds of samples in a single sequencing run [58]. |
| Lyophilized Reagents | Pre-mixed, room-temperature-stable reagents that remove cold-chain shipping constraints, reduce preparation time, and enhance workflow sustainability [14]. |
| Automation-Compatible Plates & Tips | Labware designed for low dead volume and precise liquid handling by robots, minimizing reagent waste and ensuring accurate transfers [56]. |
Implementing automation for NGS library preparation is a strategic investment in the future of your chemogenomics research. By following a structured framework to assess needs, plan meticulously, and anticipate common challenges, laboratories can successfully deploy systems that significantly enhance reproducibility, throughput, and operational efficiency. This guide provides the foundational knowledge and practical tools to begin that journey, setting the stage for more reliable and impactful scientific discovery.
Ensuring Data Integrity: Validation, Compliance, and Comparative Analysis of Automated NGS
This technical support center provides troubleshooting guides and frequently asked questions (FAQs) for researchers establishing validated Next-Generation Sequencing (NGS) workflows. The content is framed within a broader thesis on automating NGS workflows for chemogenomic reproducibility research, addressing specific issues scientists might encounter during experimental validation. Based on guidelines from the Association for Molecular Pathology (AMP) and the College of American Pathologists (CAP), this resource focuses on practical implementation challenges and solutions for researchers, scientists, and drug development professionals.
Core Validation Requirements: AMP/CAP Guidelines
What are the fundamental analytical validation requirements for clinical NGS assays?
According to AMP and CAP guidelines, laboratories must establish several key performance characteristics during validation. The table below summarizes the core requirements:
Table 1: Essential Performance Characteristics for NGS Assay Validation
| Performance Characteristic | Requirement Description | Application by Variant Type |
|---|---|---|
| Analytical Sensitivity (Limit of Detection) | Must be defined and described for each variant and/or variant class [62] [63]. | Required for SNVs, indels, CNAs, and structural variants [63]. |
| Analytical Specificity | Must be established to ensure assay accurately detects target variants [62]. | Should minimize false positives across all variant classes. |
| Accuracy, PPV, and NPV | Must be determined through validation studies [62]. | Overall and variant-specific performance should be documented. |
| Precision/Reproducibility | Must demonstrate consistent results across runs and operators [63]. | Applicable to all variant types detected by the assay. |
For ctDNA assays specifically, the Association for Molecular Pathology recommends that laboratories clearly define and describe key clinical assay performance characteristics (sensitivity, specificity, positive predictive value, negative predictive value, accuracy, and concordance) appropriate for the medical indication for the test [62]. These characteristics should be evaluated on an individual variant basis but may be aggregated for each variant class, including SNVs, indels, copy number alterations, structural variants, or signatures [62].
What are the sample and validation set requirements?
AMP/CAP guidelines provide specific recommendations for validation set composition:
Table 2: Validation Set Requirements
| Parameter | Minimum Requirement | Additional Considerations |
|---|---|---|
| Number of Samples | No absolute minimum specified; sufficient to establish performance [63]. | Should reflect real-world clinical samples and include a range of variants. |
| Variant Representation | Should include SNVs, indels, CNAs, and fusions relevant to assay [63]. | For ctDNA, should cover variant classes the test is designed to detect [62]. |
| Alternative Fixatives | 10 positive and 10 negative cases for IHC on cytology specimens [64]. | Required when fixation differs from original validation [64]. |
| Tumor Purity | Should include samples with varying tumor percentages [63]. | Must establish minimum required tumor content for reliable detection. |
For immunohistochemical assays, the updated CAP guidelines state that laboratories should perform separate validations with a minimum of 10 positive and 10 negative cases for IHC performed on specimens fixed in alternative fixatives [64]. The guideline panel recognized that these new recommendations impose an added burden to laboratories but noted that literature has shown variable sensitivity of IHC assays performed on specimens collected in fixatives often used in cytology laboratories compared with formalin-fixed, paraffin-embedded tissues [64].
Troubleshooting Common Validation Challenges
How do we address low concordance rates during validation?
If your validation shows concordance below the recommended 90% threshold [64] [65], systematically investigate these potential causes:
- Sample Quality Issues: Check pre-analytical variables including sample collection, storage, and nucleic acid quality. For ctDNA assays, document pre-analytical variables such as volume and type of collected fluid, collection tube, and details of storage and processing [62].
- Variant Type-Specific Problems: Certain variant types (e.g., indels, structural variants) may have lower detection rates. Analyze concordance separately by variant class to identify specific weaknesses [63].
- Bioinformatic Pipeline Errors: Review variant calling parameters, alignment quality, and filtering thresholds. Validate the bioinformatics pipeline for specific variant types, especially fusions and copy number alterations [63].
- Reference Material Problems: Verify that reference materials are appropriate for your assay and properly characterized.
The CAP updated guideline harmonizes concordance requirements to 90% for all IHC assays, including predictive markers like ER, PR, and HER2 [64] [65]. If validation yields unexpected results, the causes should be investigated by the medical director [65].
What should we do when encountering high rates of false positives or false negatives?
False Positives Troubleshooting:
- Review sequencing data for systematic errors (e.g., specific sequence contexts, homopolymer regions)
- Adjust bioinformatic filtering parameters
- Verify sample preparation didn't introduce contamination
- Increase stringency of variant calling thresholds
False Negatives Troubleshooting:
- Check assay sensitivity and limit of detection for specific variant types
- Verify target coverage meets minimum requirements (e.g., depth of coverage)
- Review sample quality and input requirements
- Check for allelic dropout due to primer/probe binding issues
- For hybrid capture methods, ensure efficient target enrichment
According to AMP guidelines, laboratories should use an error-based approach that identifies potential sources of errors that may occur throughout the analytical process and address these potential errors through test design, method validation, or quality controls [63].
How do we validate assays with multiple scoring systems?
For predictive marker assays with distinct scoring systems (e.g., HER2, PD-L1), CAP guidelines now require separate validation for each assay-scoring system combination [64] [65]. This means:
- Clone-Specific Validation: Each antibody clone must be validated with its intended scoring system.
- Site-Specific Requirements: For markers with different scoring systems by tumor site (e.g., PD-L1), validate each application separately.
- Documentation: Clearly document which validation applies to which clinical scenario.
The updated CAP guideline includes guidance on validation of predictive markers with distinct scoring systems, like PD-L1 and HER2, and harmonizes validation requirements for all predictive markers [64].
Validation Workflow Diagram
Diagram 1: Assay Validation Workflow
Frequently Asked Questions (FAQs)
How do we establish the limit of detection for different variant types?
The limit of detection (LOD) must be established for each variant class your assay detects. For NGS panels, this includes:
- SNVs and Small Indels: Use serial dilutions of characterized reference materials to determine the minimum variant allele frequency reliably detected.
- Copy Number Alterations: Establish LOD using samples with known copy number states at various tumor percentages.
- Structural Variants/Fusions: Validate using samples with confirmed fusions at varying dilution levels.
The AMP guidelines recommend determining positive percentage agreement and positive predictive value for each variant type during validation [63]. For ctDNA assays, the LOD should be defined for each variant and/or variant class [62].
What are the requirements for bioinformatics pipeline validation?
- Variant Calling Accuracy: Establish accuracy for each variant type (SNVs, indels, CNAs, fusions).
- Reproducibility: Demonstrate consistent results across different analysis runs and operators.
- Version Control: Document all software versions and parameters used.
- Error Handling: Establish procedures for identifying and addressing computational errors.
AMP guidelines emphasize that the bioinformatics pipeline must be appropriately validated for specific variant types, with special attention to fusion detection algorithms [63].
How do we handle validation for automated NGS workflows?
Automation introduces specific validation considerations:
- Platform Integration: Verify seamless integration between automated liquid handling, library preparation, and sequencing platforms.
- Reagent Dispensing Accuracy: Confirm automated systems maintain precision in reagent dispensing.
- Cross-Contamination Checks: Validate that automated systems minimize carryover between samples.
- Process Consistency: Demonstrate that automated workflows produce consistent results across multiple runs.
Automated NGS workflows enhance reproducibility by eliminating batch-to-batch variations that often occur in manual workflows due to subtle differences in reagent handling or incubation times [12]. Integration with Laboratory Information Management Systems (LIMS) enables real-time tracking of samples, reagents, and process steps, ensuring complete traceability [12].
Research Reagent Solutions
Table 3: Essential Materials for NGS Validation
| Reagent/Material | Function in Validation | Key Considerations |
|---|---|---|
| Reference Cell Lines | Provide known variants for establishing accuracy [63]. | Should contain relevant variants at known allele frequencies. |
| Control Materials | Monitor assay performance and reproducibility [63]. | Include positive, negative, and sensitivity controls. |
| Hybrid Capture Probes | Target enrichment for specific genomic regions [63]. | Design affects coverage uniformity and variant detection. |
| Library Preparation Kits | Convert nucleic acids to sequenceable libraries [63]. | Impact library complexity and sequencing quality. |
| Automated Liquid Handlers | Standardize reagent dispensing and sample processing [12] [15]. | Reduce variability and increase throughput. |
Successful implementation of a validation framework following AMP and CAP guidelines requires careful planning, execution, and documentation. By addressing these common troubleshooting scenarios and following established best practices, laboratories can ensure their NGS workflows produce reliable, reproducible results suitable for chemogenomic research and clinical applications. Regular monitoring and continuous quality improvement are essential for maintaining assay performance over time.
Frequently Asked Questions
What are the primary benefits of automating my NGS library prep? Automation significantly enhances consistency, reduces hands-on time, and increases throughput. The most direct benefits are:
- Improved Reproducibility: Automated systems standardize protocols, eliminating batch-to-batch variations caused by human handling [12].
- Enhanced Accuracy: Automated liquid handling removes pipetting variability and reduces cross-contamination risks, leading to more uniform sequencing results [12] [66].
- Increased Efficiency: Automation reduces hands-on time dramatically. For example, a manual protocol taking over 3 hours of hands-on time can be reduced to about 30 minutes of setup time with an automated run [66].
- Scalability: Automated platforms allow labs to easily process from 4 to 384 samples per run, adapting to changing project sizes [66].
My automated NGS run failed. What are the most common first steps in troubleshooting? Begin with a systematic check of the most frequent failure points:
- Review Liquid Handler Calibration: Ensure proper calibration of aspiration and dispensing channels, a common source of error [66].
- Inspect Reagents and Consumables: Check reagent logs, kit lot numbers, and expiry dates. Incompatible consumables can leave residues that inhibit enzymatic reactions [1] [67].
- Verify Sample Quality: Use fluorometric methods (e.g., Qubit) rather than just UV absorbance to accurately quantify usable input material [1].
- Examine Purification Steps: Check bead-to-sample ratios and avoid over-drying beads during clean-up steps, as this can lead to inefficient resuspension and sample loss [1].
How does the cost of automation compare to manual workflows? While the initial investment is significant, the return on investment (ROI) can be substantial. One analysis found that businesses implementing automation strategically saw a 537% ROI over five years [68].
- Initial Investment: Automated liquid handling systems can range from approximately $45,000 for low-throughput platforms to $300,000 for high-throughput instruments [66].
- Ongoing Costs: Annual preventative maintenance contracts can cost $15,000–$30,000 [66]. However, these costs are offset by long-term savings from reduced reagent waste, repeat experiments, and increased personnel efficiency [12] [5].
Can I still use my existing library prep kits with an automated system? Many automated platforms are designed to be vendor-agnostic, allowing use of existing kits [67]. However, verification is crucial. When implementing automation, you should:
- Validate Performance: Re-validate the entire workflow using the automated system and your preferred kits to ensure data quality meets standards [16].
- Check for Pre-Programmed Protocols: Some manufacturers provide pre-optimized protocols for specific kits on their systems, which can save development time [69].
- Ensure Consumable Compatibility: Verify that your labware (e.g., 96-well plates) is compatible, as some plastics contain contaminants that can inhibit enzymatic reactions [67].
We are a small lab with limited resources. Is automation still feasible for us? Yes. The market now offers compact, benchtop systems designed for lower throughput and simpler operation, making automation accessible for smaller labs [69] [67]. Key considerations include:
- Modular Platforms: Select systems that allow you to start with core functionality and add modules (like on-deck thermocyclers) as needs evolve [67].
- Throughput Alignment: Choose a system matching your typical sample volume; not all automation requires 384-well capabilities [66].
- Training Investment: Plan for comprehensive training to ensure all personnel can operate and perform basic troubleshooting on the system efficiently [66].
Troubleshooting Guides
Problem 1: Low Library Yield After Automated Preparation
Symptoms:
- Final library concentrations are significantly lower than expected.
- Broad or faint peaks on the electropherogram.
- Adapter-dimer peaks may dominate the profile.
Diagnostic Steps:
- Verify Input Quality:
- Check Automated Liquid Handling:
- Review Reagent Parameters:
Corrective Actions:
- For Contamination Issues: Implement additional purification steps and use fresh wash buffers.
- For Pipetting Issues: Recalibrate liquid handler and verify tip attachment and liquid detection.
- For Ligation Issues: Optimize adapter concentration and extend ligation incubation time.
Problem 2: Inconsistent Results Between Automated Runs
Symptoms:
- Variable sequencing metrics (e.g., coverage, duplication rates) between identical runs.
- Batch effects apparent in data analysis.
- Some samples in a run fail while others succeed.
Diagnostic Steps:
- Review Maintenance Records:
- Analyze Operator Techniques:
- Compare results across different operators to identify technique variations.
- Review SOP adherence, particularly in manual steps that may remain in the workflow.
- Check Environmental Factors:
- Monitor laboratory temperature and humidity, which can affect reagent performance and evaporation rates.
Corrective Actions:
- Standardize Protocols: Implement master mixes to reduce pipetting steps and variations [1].
- Enhance Training: Ensure all personnel are trained on the exact same protocol with emphasis on critical steps.
- Implement QC Monitoring: Use tools like omnomicsQ for real-time quality monitoring to flag samples that fall below pre-defined quality thresholds [12].
Problem 3: High Adapter-Dimer Contamination in Final Libraries
Symptoms:
- Sharp peak at ~70-90 bp on electropherogram.
- Reduced complexity of sequencing libraries.
- Lower useful read percentage after sequencing.
Diagnostic Steps:
- Analyze Purification Steps:
- Verify bead-to-sample ratios are correct for the specific cleanup step [1].
- Check that washing steps are sufficient to remove excess adapters.
- Review Ligation Parameters:
- Confirm adapter concentration is not excessively high.
- Check ligation reaction time and temperature.
- Assess Fragment Size Distribution:
- Verify that fragmentation/tagmentation produced the expected fragment sizes before ligation.
Corrective Actions:
- Optimize Cleanup: Increase bead-to-sample ratio to better exclude small fragments [1].
- Adjust Ligation: Titrate adapter concentration to find the optimal level that minimizes dimers while maintaining efficiency.
- Implement Size Selection: Add or refine size selection steps, either with beads or other methods.
Quantitative Comparison: Automated vs. Manual NGS Workflows
Table 1: Performance and Operational Metrics Comparison
| Metric | Manual Workflow | Automated Workflow | Data Source |
|---|---|---|---|
| Hands-on Time (per 8 samples) | 3+ hours | ~30 minutes | [66] |
| Typical Sample Throughput | Limited by technician capacity | 4-384 samples per run | [66] |
| Error Rate (Liquid Handling) | Variable between technicians | Highly consistent | [12] |
| Cross-Contamination Risk | Higher | Significantly reduced | [12] [5] |
| Startup Cost | Lower | $45,000 - $300,000+ | [66] |
| Operational Consistency | Technician-dependent | Standardized across users | [12] [5] |
Table 2: Business and Workflow Impact Comparison
| Consideration | Manual Workflow | Automated Workflow | Data Source |
|---|---|---|---|
| ROI (5-year period) | Baseline | 537% (strategic implementation) | [68] |
| Training Requirements | Protocol-specific | System operation and troubleshooting | [66] |
| Scalability | Difficult, requires more staff | Easily scalable | [66] [5] |
| Regulatory Compliance | More challenging to standardize | Easier documentation and tracking | [12] |
| Batch Effect | Common between runs and operators | Greatly reduced | [5] |
Experimental Protocols for Benchmarking
Protocol 1: Direct Comparison of Manual vs. Automated Library Preparation
Objective: To quantitatively compare the performance of manual and automated NGS library preparation methods using the same input samples and reagents.
Materials:
- Identical biological samples (split for parallel processing)
- Commercial library preparation kit (compatible with both methods)
- Manual pipetting equipment
- Automated liquid handler (e.g., Beckman Coulter Biomek i3, Hamilton, or similar)
- QC instruments (e.g., BioAnalyzer, Qubit, qPCR)
Methodology:
- Sample Partitioning: Divide each sample into two equal aliquots for parallel manual and automated processing.
- Protocol Synchronization: Use the same commercial kit and protocol steps for both methods, adjusting only for the liquid handling method.
- Processing: Execute library preparation simultaneously using experienced technicians for the manual method and trained operators for the automated method.
- Quality Assessment: Evaluate all libraries using:
- Yield quantification (Qubit and qPCR)
- Fragment size distribution (BioAnalyzer)
- Adapter-dimer percentage
- Sequencing and Analysis: Sequence all libraries on the same flow cell and compare:
- Coverage uniformity
- Duplication rates
- GC bias
- Variant calling accuracy (if applicable)
Expected Outcomes: The automated workflow should show reduced variability between technical replicates, more consistent fragment size distribution, and lower adapter-dimer rates [12] [66].
Protocol 2: Inter-Operator Variability Assessment
Objective: To quantify how individual operator technique affects library preparation outcomes in both manual and automated workflows.
Materials:
- Standardized reference DNA sample
- Single lot of library preparation reagents
- Multiple trained technicians (minimum of 3)
- Automated liquid handling system
Methodology:
- Study Design: Have each technician prepare libraries from the same reference sample using both manual and automated methods.
- Blinding: Blind technicians to the identity of samples where possible to reduce bias.
- Standardization: Provide the same written protocol to all technicians but allow them to follow their usual techniques.
- Data Collection: Track:
- Preparation time
- Pipetting variations (deviations from protocol)
- Final library metrics (yield, quality, size distribution)
- Statistical Analysis: Calculate coefficient of variation for each metric across operators for both manual and automated methods.
Expected Outcomes: Automated workflows should demonstrate significantly lower inter-operator variability compared to manual methods, leading to more reproducible results across different personnel [5].
Workflow Visualization
NGS Workflow Comparison: Manual vs. Automated
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Solutions for Automated NGS Workflows
| Item | Function | Automation-Specific Considerations |
|---|---|---|
| Automation-Compatible Library Prep Kits | Provide optimized reagents for NGS library construction | Look for lyophilized formats (e.g., Meridian Bioscience) to remove cold-chain constraints [14] |
| Liquid Handling Calibration Solutions | Verify precision and accuracy of automated pipetting | Use daily for channel calibration of aspiration and dispensing [66] |
| High-Purity Consumables | Labware (plates, tubes) for automated processing | Select "DNase/RNAse Free" and "endotoxin-free" options to prevent enzymatic inhibition [67] |
| Magnetic Beads | Library purification and size selection | Optimize bead-to-sample ratios for automated platforms to minimize sample loss [1] |
| QC Assay Kits | Assess input DNA/RNA and final library quality | Implement fluorometric quantification (Qubit) rather than just UV absorbance [1] |
| Automation-Ready Enzymes | Ligases, polymerases for library construction | Test compatibility with automated dispensing and on-deck incubation [69] |
In automated next-generation sequencing (NGS) workflows for chemogenomic reproducibility research, consistent and high-quality data is paramount. Three technical metrics serve as critical indicators of experimental success: on-target rate, coverage uniformity, and variant calling accuracy. Monitoring these key performance indicators (KPIs) allows researchers and drug development professionals to troubleshoot workflows, validate automated processes, and ensure the reliability of their genomic data for downstream analysis and decision-making.
FAQs: Understanding and Troubleshooting Key NGS Metrics
FAQ 1: What do my on-target rates and coverage uniformity metrics actually mean?
On-target rate provides information about the specificity of your target enrichment experiment. It is calculated as the percentage of sequencing reads or bases that map to the intended target regions you designed your panel to capture. A high on-target rate indicates strong probe specificity and efficient hybridization, ensuring your sequencing resources are focused on the regions of interest [70].
- Percent bases on-target: The number of bases that map to the target region.
- Percent reads on-target: Includes all sequencing reads that overlap the target region by even a single base [70].
Coverage uniformity measures how evenly sequencing reads are distributed across all target regions. It is often assessed using the Fold-80 base penalty metric. This value describes how much more sequencing is required to bring 80% of the target bases to the mean coverage level. A perfect uniformity score would be 1.0, while values higher than 1 indicate uneven coverage [70] [71].
Table 1: Interpreting Key NGS Metrics
| Metric | Ideal Value/Range | Interpretation | Impact of Low Score |
|---|---|---|---|
| On-Target Rate | > 80% (varies by panel) | High experiment specificity and probe efficiency | Wasted sequencing capacity; higher cost per target variant |
| Fold-80 Penalty | As close to 1.0 as possible | Even read distribution across all targets | Inconsistent variant detection; gaps in coverage |
| Variant Calling Accuracy (F1 Score) | > 99% for high-confidence SNPs | Precision and recall of variant caller [72] | False positives/negatives; unreliable data for clinical decisions |
FAQ 2: My on-target rate is lower than expected. What are the most likely causes and solutions?
A low on-target rate is a common issue that points to inefficiencies in the library preparation or target enrichment steps. The following table outlines the primary culprits and recommended corrective actions.
Table 2: Troubleshooting Low On-Target Rates
| Root Cause | Specific Issues | Corrective Actions |
|---|---|---|
| Suboptimal Probe Design | Poorly designed or low-quality capture probes [70]. | Invest in well-designed, high-quality probes from reputable vendors [70]. |
| Library Preparation Issues | Inefficient fragmentation or ligation; low-quality input DNA/RNA [1]. | Re-optimize fragmentation protocols; use fluorometric methods for accurate input quantification [1]. |
| Hybridization Problems | Poorly optimized hybridization protocol; low-quality reagents [70]. | Validate and strictly follow hybridization protocols; use fresh, high-quality reagents [70]. |
| Contamination | Carryover of contaminants (e.g., salts, phenol) that inhibit enzymes [1]. | Re-purify input sample; ensure wash buffers are fresh and used correctly [1]. |
FAQ 3: How can I improve poor coverage uniformity in my hybrid capture data?
Poor coverage uniformity, indicated by a high Fold-80 base penalty, often stems from biases introduced during the workflow. To improve uniformity:
- Use High-Quality Probes: The Fold-80 base penalty provides information about the capture efficiency of the probes. Well-designed, high-quality probes are fundamental to achieving uniform coverage [70].
- Minimize GC Bias: Regions with high or low GC content are often unevenly represented. GC-bias can be introduced during library preparation (especially with PCR) or during hybrid capture [70].
- Solution: Prepare sequencing libraries with a robust workflow known to minimize GC-bias, optimize PCR enrichment steps, and use properly calibrated thermocyclers [70].
- Optimize Automation: Manual library prep can introduce variability. Automating the NGS workflow can enhance precision and reproducibility, leading to more uniform coverage across samples and runs [69].
FAQ 4: Which variant calling tool should I choose for the most accurate results in a reproducible automated workflow?
The choice of variant caller significantly impacts the accuracy of your final data. Recent systematic benchmarks using gold-standard datasets have evaluated the performance of popular tools.
Table 3: Variant Caller Performance Comparison
| Variant Caller | Reported Performance Characteristics | Considerations for Automated Workflows |
|---|---|---|
| DeepVariant | Consistently showed the best performance and highest robustness in benchmarks [72]. | Excellent for standardized, automated pipelines due to high consistency. |
| Strelka2 | Performed well, though its efficiency had greater dependence on data quality and type [72]. | A strong, reliable choice for most applications. |
| GATK HaplotypeCaller | A well-established tool; performance can be improved with additional filtering [73] [72]. | Widely adopted with extensive community support. |
| FreeBayes | Yielded lower numbers of SNPs and more modest error rates in one study [73]. | Can be a conservative option for SNP calling. |
| UnifiedGenotyper | With filtering, consistently produced the smallest proportion of genotype errors in a familial study [73]. |
Key Insight: The accuracy of variant discovery is also improved by using a robust read aligner. While BWA-MEM is considered a gold standard, the benchmark found that the choice of variant caller often has a larger impact on final accuracy than the choice of aligner (with the exception of Bowtie2, which performed significantly worse and is not recommended for medical variant calling) [72].
FAQ 5: How does workflow automation specifically help improve these key metrics?
Automating NGS workflows directly addresses several sources of human error and variability that degrade key metrics:
- Improved Reproducibility: Automated liquid handlers like the Biomek i3 perform liquid transfers with high precision, reducing pipetting errors and well-to-well contamination that can cause uneven coverage or low on-target rates [69].
- Reduced Hands-on Time: Automation allows for the walk-away processing of samples, which not only increases throughput but also minimizes the risk of procedural deviations or fatigue-related mistakes during critical steps like hybridization and cleanup [69].
- Standardization: By encapsulating a validated protocol into an automated method, labs ensure that every sample is processed identically. This is crucial for chemogenomic studies where reproducibility across many compounds and cell lines is essential [69].
Essential NGS Workflow
The diagram below illustrates the core steps of a typical automated NGS workflow, highlighting the stages where the key metrics are most influenced.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents for Robust NGS Workflows
| Item / Solution | Function / Purpose | Troubleshooting Application |
|---|---|---|
| Lyophilized NGS Library Prep Kits | Pre-made, stable kits that remove cold-chain shipping constraints [14]. | Improves reagent consistency and reduces risk of degradation-related failures. |
| Automation-Compatible Target Enrichment Kits | Assay solutions (e.g., Hybrid Capture, Amplicon) validated for use on liquid handlers [69]. | Essential for achieving the reproducibility benefits of automated workflows. |
| High-Quality, Biased-Reduced Polymerase | Enzyme for PCR amplification during library prep. | Minimizes the introduction of GC-bias and duplicate reads, directly improving coverage uniformity [70]. |
| Unique Dual Index (UDI) Adapters | Oligonucleotides that allow sample multiplexing and identification of index-hopped reads [74]. | Critical for accurate sample demultiplexing in pooled runs, preventing cross-contamination. |
| Fragmentation & Library Prep Kits | Reagents for shearing DNA and preparing sequencing-ready libraries [14] [75]. | The foundation of library quality; optimized kits minimize adapter dimer formation and maximize library complexity. |
Automating Next-Generation Sequencing (NGS) workflows presents significant advantages for chemogenomic reproducibility research, including enhanced precision, reduced human error, and improved throughput [5]. However, operating these automated systems within a regulated research and development environment requires adherence to a complex framework of international standards and regulations. Key among these are ISO 13485 for quality management systems, the In Vitro Diagnostic Regulation (IVDR) in the European Union, and the Health Insurance Portability and Accountability Act (HIPAA) in the United States for data security. This technical support center provides targeted guidance to help researchers, scientists, and drug development professionals navigate these requirements, ensuring that their automated NGS workflows are not only scientifically robust but also fully compliant.
Frequently Asked Questions (FAQs)
Q1: Our lab is automating NGS library preparation for chemogenomic screening. Does this fall under IVDR? It depends on the intended use of the data. If the results are used for diagnostic purposes or to inform patient treatment decisions, then the automated workflow is subject to IVDR [12]. IVDR imposes strict requirements for clinical evidence, performance evaluation, post-market surveillance, and technical documentation [76]. If the research is purely for basic discovery and not linked to clinical decision-making, IVDR may not apply, but maintaining high standards aligned with ISO 13485 is still recommended for data quality and reproducibility.
Q2: What is the most critical aspect of ISO 13485 for an automated NGS workflow? A robust and well-documented quality management system (QMS) is the cornerstone of ISO 13485 [77]. For an automated NGS workflow, this means having controlled procedures for every step: from validating the automation software and robotic methods, to ensuring the calibration of liquid handling systems, to maintaining detailed records of sample preparation and reagent lots [7] [12]. The focus is on demonstrating control over all processes that affect the quality of the final genomic data.
Q3: How does HIPAA apply to the genomic data generated by our automated systems? If your NGS workflow processes human genomic samples and you are operating in the U.S., HIPAA's rules for protecting Protected Health Information (PHI) apply. Genomic data is considered PHI. Your automated systems, including the liquid handlers, servers storing sequencing data, and analysis platforms, must have safeguards in place. This includes implementing strict access controls, encrypting data in transit and at rest, and ensuring your software partners provide solutions that support HIPAA compliance [12].
Q4: We use an AI-based tool for variant calling. How does this impact our regulatory strategy? The use of Artificial Intelligence/Machine Learning (AI/ML) introduces additional regulatory considerations. Under the EU's IVDR, you must provide extensive clinical evidence for your AI-based diagnostic tool [76]. Furthermore, the EU AI Act classifies medical device AI as high-risk, requiring stringent risk management, data quality, transparency, and human oversight [77]. You will need to document the algorithm's performance, including its training and validation datasets, and establish a protocol for ongoing monitoring post-deployment.
Q5: What are the common pitfalls when transitioning from a manual to an automated NGS protocol? Three common challenges are [7]:
- Lack of Software Expertise: Needing to build custom scripts without programming knowledge.
- Incorrect Worktable Design: Choosing hardware and deck layouts that limit throughput or efficiency.
- Insufficient Workflow Optimization: Failing to rigorously test and validate the automated script, leading to errors in DNA purification or library preparation that can compromise downstream analysis.
Troubleshooting Guides
Issue: Failure in an IVDR Audit Due to Lack of Traceability
Problem: An audit uncovered insufficient traceability between user needs, technical requirements, and validation data for your automated NGS library prep system.
Solution:
- Immediate Action: Halt any clinical use of the data generated by the system until traceability is established.
- Root Cause Analysis: Map the current documentation to identify gaps. Is the intended use of the device clearly defined? Are all engineering requirements (e.g., pipetting accuracy, temperature control) linked to specific user needs (e.g., reproducibility, accuracy)? Is there a documented risk management file per ISO 14971? [77]
- Corrective Action: Implement a dedicated requirements management tool. Re-document the entire workflow, creating a hierarchical traceability matrix that connects:
- User Requirements (e.g., "The system must process 96 samples with a cross-contamination rate of <0.1%").
- Technical/Engineering Requirements (e.g., "The liquid handler must use filtered tips and have a specified aspirate/dispense precision").
- Risk Control Measures (from your ISO 14971 risk management file) [77].
- Validation Protocols and Results (e.g., "Protocol XYZ-001 demonstrates a cross-contamination rate of 0.05% over 10 runs").
- Verification: Have an internal quality audit verify the updated traceability matrix before the next external audit.
Issue: HIPAA Breach Involving Genomic Data from an Automated Run
Problem: A laptop containing unencrypted genomic data files from an automated sequencer was stolen, constituting a potential HIPAA breach.
Solution:
- Immediate Action: Activate your incident response plan. Revoke access rights and physically secure the remaining equipment. Report the breach to your organization's Privacy Officer as mandated by policy.
- Containment: Identify the scope of the breach. Which samples and data fields were involved? Determine if the breach affected 500 or more individuals, which triggers mandatory reporting to the Department of Health and Human Services (HHS) and the media.
- Corrective Action: Encrypt all data storage devices, including those on instruments and data transfer stations. Implement strict policies against storing PHI on portable devices without encryption. Reinforce employee training on data handling protocols and physically securing equipment. Ensure your automated platform's software integrates with your secure data management systems to prevent unauthorized data exports [12].
- Prevention: Conduct a periodic security risk analysis as required by the HIPAA Security Rule. Apply system updates and patches promptly.
Issue: Poor Reproducibility in Automated NGS Library Prep
Problem: Despite automation, your NGS libraries show high variability in yield and quality, leading to inconsistent sequencing results and failed reproducibility experiments.
Solution:
- Check the Automation Script: Verify that the liquid handling protocol is optimized and validated. Small errors in scripted volumes, mixing speeds, or incubation times can compromise quality [7]. Use pre-validated, commercial protocols where possible.
- Inspect the Hardware: Calibrate the liquid handling system to ensure pipetting accuracy and precision. Check for clogged tips or worn-out components on the robotic deck [5].
- Review Reagent Handling: Ensure reagents are stored correctly and are not expired. In automated systems, reagent evaporation in open wells can be a source of error; use sealed plates or humidity chambers if available [5].
- Implement Real-Time QC: Integrate a quality control solution, such as omnomicsQ, to monitor genomic samples in real-time and flag those that do not meet pre-defined quality thresholds before they proceed to expensive sequencing [12].
Data and Compliance Tables
Table 1: Key Regulatory Requirements for Automated NGS Workflows
| Regulation / Standard | Core Focus | Key Requirements for Automated NGS | Documentation Needed |
|---|---|---|---|
| ISO 13485 | Quality Management System | - Documented procedures for design, development, and validation of automated methods.- Control of monitoring and measuring equipment (e.g., calibrated pipettors).- Management of software used in the quality system (automation software) [77] [12]. | - Quality Manual- Standard Operating Procedures (SOPs)- Validation Protocols & Reports- Calibration Records |
| IVDR (EU) | Safety & Performance of IVDs | - Performance evaluation with clinical evidence.- Strict post-market performance monitoring (PMPF).- Compliance with ISO 13485 is a key requirement for certification [76] [12]. | - Technical Documentation- Performance Evaluation Report- Post-Market Surveillance Plan & Report- Risk Management File (per ISO 14971) |
| HIPAA (US) | Data Privacy & Security | - Administrative, physical, and technical safeguards for Protected Health Information (PHI).- Encryption of electronic PHI (ePHI), including genomic data files.- Access controls and audit trails for systems handling ePHI [12]. | - Risk Analysis Documentation- Policies and Procedures- Incident Response Plan- Employee Training Records |
Table 2: Contrast Requirements for Text and Visual Elements (Per WCAG)
| Element Type | Size / Weight | Minimum Contrast Ratio (Level AA) | Enhanced Contrast Ratio (Level AAA) |
|---|---|---|---|
| Text | Small (below 18 pt / 24 px) | 4.5:1 | 7:1 [78] |
| Text | Large (18 pt / 24 px and above) | 3:1 | 4.5:1 [78] |
| Text | Bold (14 pt / 18.7 px and above) | 3:1 | 4.5:1 [78] |
| User Interface Components | (e.g., icons, graphs, buttons) | 3:1 | Not specified |
Experimental Protocols
Protocol: Validation of an Automated NGS Library Prep Workflow for Regulatory Compliance
Purpose: To establish and document that the automated NGS library preparation workflow consistently produces libraries that meet pre-defined specifications for yield, quality, and performance, in compliance with ISO 13485 and IVDR requirements for process validation.
Materials:
- Automated Liquid Handling System: (e.g., Tecan Fluent, Dispendix I.DOT)
- NGS Library Prep Kit: (Specify brand and version)
- Reference Genomic DNA: (e.g., Coriell Institute samples with known variants)
- QC Instruments: Fluorometer (e.g., Qubit), Fragment Analyzer (e.g., Agilent Bioanalyzer/TapeStation)
- Sequencing Platform: (e.g., Illumina NovaSeq)
Methodology:
- Protocol Installation & Operational Qualification (IQ/OQ):
- Install the automated library prep script on the liquid handler. Execute the script without reagents to verify all movements and functions operate as intended.
- Perform pipetting accuracy and precision verification using a dye-based gravimetric measurement.
Performance Qualification (PQ):
- Run Configuration: Process a minimum of three independent batches of reference DNA samples (n=96 per batch) on different days by different operators.
- Parameter Monitoring: For each library, measure:
- DNA Yield: Using a fluorometer.
- Library Size Distribution: Using a fragment analyzer.
- Adapter Dimer Presence: Quantified as a percentage of total material.
- Sequencing Performance: Pool and sequence all libraries. Analyze data for:
- Coverage Uniformity: >80% of target bases covered at 20x.
- Variant Calling Accuracy: >99% concordance with known variants in the reference DNA.
- Duplicate Read Rate: <10%.
Data Analysis & Acceptance Criteria:
- Compile all data. The method is considered validated if ≥95% of all libraries across all batches meet all pre-defined acceptance criteria for yield, size, and sequencing metrics. Any outliers must be investigated and root cause determined.
Protocol: Conducting a Data Security Risk Analysis for HIPAA Compliance
Purpose: To identify potential threats and vulnerabilities to the confidentiality, integrity, and availability of electronic Protected Health Information (ePHI) generated by automated NGS workflows.
Materials:
- Asset Inventory List: (Servers, sequencers, automation workstations, laptops, backup drives)
- Data Flow Diagrams
- Risk Assessment Matrix Template
Methodology:
- Scope Definition: Define the scope to include all systems that create, receive, maintain, or transmit ePHI (e.g., the automated NGS system, the sequencing instrument, the data analysis server, and any portable media).
- Data Flow Mapping: Create a visual diagram tracing the path of genomic data from the sample tube on the automated liquid handler through to final variant report storage and archiving.
- Threat & Vulnerability Identification: For each system and data flow, identify potential threats (e.g., theft of a laptop, ransomware attack on the server, unauthorized access by a former employee) and existing vulnerabilities (e.g., unencrypted storage, lack of multi-factor authentication, outdated software).
- Risk Analysis: Assess the likelihood and impact of each threat-vulnerability pair. Use a risk matrix to categorize risks as High, Medium, or Low.
- Risk Mitigation Plan: For each identified risk, especially High and Medium, define a mitigation strategy. Examples: implementing full-disk encryption (addresses stolen laptop), deploying a patch management policy (addresses ransomware), and revoking access immediately upon employee termination [12].
Workflow and Process Diagrams
Regulatory Compliance Pathway for Automated NGS
Automated NGS Wet-Lab & Data Flow
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Automated NGS
| Item | Function in Automated NGS Workflow |
|---|---|
| Nucleic Acid Extraction Kits | Designed for use with automated liquid handlers to purify DNA/RNA from raw samples. Their buffers and bead-based chemistry are optimized for robotic pipetting and magnetic module separation [7]. |
| NGS Library Prep Kits | Provide all enzymes, buffers, and adapters needed for end-repair, A-tailing, and adapter ligation in a format suitable for automation. Pre-mixed, stabilized reagents are critical for run-to-run reproducibility [12]. |
| Size Selection Beads | Magnetic beads used to selectively purify DNA fragments within a specific size range, a key step in library prep that can be fully automated on platforms with magnetic separation modules [5]. |
| Universal Blocking Reagents | Used to reduce non-specific binding in hybridization-based capture workflows, improving the on-target rate and uniformity of the sequencing library. |
| PCR Master Mixes | Optimized, ready-to-use mixes for the library amplification step. Their consistency is vital for ensuring uniform PCR efficiency across all samples in an automated run [5]. |
In the field of chemogenomic reproducibility research, the demand for high-throughput, precise genomic data has made automation a cornerstone of sustainable and scalable operations [15]. Traditional manual methods for Next-Generation Sequencing (NGS) are no longer adequate for the throughput and precision demands of modern genomics, particularly in drug development where reproducible results are critical [15]. Automation, through the integration of robotics, liquid-handling systems, and advanced data workflows, is transforming the field by reducing hands-on time, minimizing variability, and improving reproducibility [15]. This case study quantifies the significant gains in efficiency and data quality achieved through the implementation of automated NGS workflows, providing a framework for researchers and scientists seeking to optimize their genomic operations for chemogenomic applications.
Quantitative Gains from Automated NGS Workflows
Documented Efficiency and Quality Metrics
The transition from manual to automated NGS workflows yields measurable operational, scientific, and economic advantages. The following table summarizes key quantitative gains documented across multiple studies:
| Performance Metric | Manual Workflow Performance | Automated Workflow Performance | Magnitude of Improvement |
|---|---|---|---|
| Hands-on Time | High (Baseline) | Reduced by 65% [15] | High Impact |
| Sample Throughput | ~200 samples/week [15] | 600 samples/week [15] | 3x increase |
| Process Contamination | Variable/Baseline | Dropped to near zero [15] | Near elimination |
| Library Prep Hands-on Time | ~3 hours [13] | <15 minutes [13] | Over 90% reduction |
| Cost per Sample (Surveillance) | Not Specified | <$15 per sample [13] | Significant cost reduction |
Broader Impacts on Laboratory Operations
Beyond these direct metrics, automation delivers broader operational benefits that are critical for chemogenomic research. These include enhanced consistency and reproducibility by reducing human variability, improved scalability without proportional increases in headcount, and stronger regulatory compliance through built-in documentation and traceability [15] [12]. One case study noted that staff satisfaction improved as technicians transitioned from repetitive pipetting to more valuable roles in system programming and data validation [15].
FAQs: Troubleshooting Automated NGS Workflows
Q1: Our automated runs are showing low coverage uniformity. What are the primary causes?
Low coverage uniformity often stems from inconsistencies in library preparation that automation is meant to solve. Key culprits include:
- Imprecise Liquid Handling: Verify calibration of automated liquid handlers. Inconsistent reagent dispensing leads to varied fragment sizes and adapter ligation efficiency [12] [79].
- Inadequate Bead-Based Cleanup: Ensure the automated method for magnetic bead-based purification is optimized for consistent bead mixing and binding time, as this critically affects library fragment selection and normalization [13].
- Suboptimal Input DNA Quality: Automation relies on high-quality starting material. Low-input or degraded samples will result in lower coverage and increased bias, which amplification during library prep cannot fully correct [80].
Q2: How can we minimize cross-contamination in a fully automated, high-throughput system?
Minimizing contamination requires both technical and procedural controls:
- Use Disposable Tips: Always use disposable tips for liquid handling to prevent nucleic acid carryover between samples [12].
- Dedicated Workflow Areas: Run different workflows in dedicated areas or on dedicated equipment if possible. Some automated platforms are designed with contamination-free control as a key feature [80].
- Integrated Clean-up Steps: Utilize automated systems that integrate bead-based clean-up steps, which can reduce carryover compared to manual wash steps [13].
Q3: Our data shows high duplication rates post-automation. Is this a result of the automation itself?
High duplication rates are typically not a direct result of automation but point to issues upstream of sequencing:
- Low Input DNA: This is the most common cause. An automated process will faithfully amplify limited starting material, leading to a high proportion of PCR duplicates. Re-check nucleic acid quantification and quality control steps prior to library prep [81] [80].
- Over-Amplification during Library Prep: Review the number of PCR cycles in your automated library preparation protocol. Excessive cycles should be avoided [79].
- Sequencing Depth: Evaluate if you are simply sequencing too deeply for your application, which can inflate duplication metrics.
Experimental Protocols for Key Workflows
Protocol: Automated NGS Library Preparation and Quality Control
This protocol is designed for a mid-sized academic or biopharmaceutical genomics core lab implementing a fully automated NGS pipeline.
1. Sample Quality Control (Pre-Automation)
- Objective: Ensure only high-quality samples enter the automated workflow.
- Method: Use fluorometric methods (e.g., Qubit) for accurate DNA/RNA quantification and fragment analyzers (e.g., Bioanalyzer, TapeStation) to assess integrity.
- Quality Threshold: Samples must pass pre-defined quality thresholds for concentration and integrity (e.g., RIN > 8 for RNA, DIN > 7 for DNA) [80]. Tools like
omnomicsQcan be integrated for real-time quality monitoring [12].
2. Automated Library Preparation
- System: Use an integrated robotic system (e.g., Hamilton NIMBUS or Microlab STAR, or the G.STATION NGS Workstation) with a pre-validated, automation-friendly library prep kit [82] [13].
- Process: The automated method should execute the following steps in a closed, walk-away fashion:
- Fragmentation: Shearing of DNA to a target size (e.g., 200-500bp).
- End Repair & A-Tailing: Preparation of fragments for adapter ligation.
- Adapter Ligation: Attachment of platform-specific adapters containing sample barcodes (multiplexing).
- Library Amplification: Limited-cycle PCR to enrich for adapter-ligated fragments.
- Bead-Based Cleanup: Size selection and purification of the final library using integrated magnetic bead handlers [13].
3. Post-Preparation QC
- Quantification: Use an automated fluorometer or qPCR-based method for accurate library quantification.
- Quality Assessment: Run a sample on a fragment analyzer to confirm library size distribution and absence of adapter dimers.
4. Pooling and Normalization
- Method: Use the liquid handler to normalize and pool libraries based on QC data into a single sequencing pool.
- Final QC: Quantify the pooled library to ensure optimal loading concentration for the sequencer.
Workflow Visualization of Automated NGS Process
The following diagram illustrates the streamlined, automated workflow from sample to data, highlighting key quality control checkpoints.
The Scientist's Toolkit: Essential Reagents & Solutions
The successful implementation of an automated NGS workflow relies on a suite of specialized reagents and tools. The following table details key components and their functions.
| Item | Function in Automated Workflow | Key Considerations |
|---|---|---|
| Automation-Friendly Library Prep Kits | Provides all enzymes, buffers, and adapters optimized for robotic liquid handling (e.g., xGen, Archer) [82]. | Pre-validated protocols for specific platforms reduce optimization time and ensure reproducibility. |
| Liquid Handling Platforms (e.g., Hamilton STAR/NIMBUS, DISPENDIX I.DOT) | Precisely dispenses reagents and samples in nanoliter-to-microliter ranges, eliminating pipetting error [12] [13]. | Flexibility to handle various protocols and compatibility with 96-/384-well plates are critical for scalability. |
| Magnetic Bead Clean-up Reagents | Performs size selection and purification of DNA fragments during library prep in an automatable format [13]. | Bead consistency and suspension properties are vital for uniform automated performance. |
| Integrated Robotic Arms & Workstations (e.g., G.STATION) | Links individual instruments (liquid handler, thermal cycler, bead handler) into a single, walk-away "sample-to-library" system [13]. | Reduces manual intervention to an absolute minimum, maximizing throughput and consistency. |
| Laboratory Information Management System (LIMS) | Tracks samples, reagents, and process steps in real-time, ensuring traceability and regulatory compliance (e.g., for IVDR) [15] [12]. | Seamless integration with automation hardware is essential for end-to-end data capture. |
Conclusion
The strategic automation of NGS workflows is a cornerstone for achieving the high levels of reproducibility required in modern chemogenomics and drug development. By integrating the foundational principles, methodological applications, optimization strategies, and rigorous validation frameworks detailed in this guide, research laboratories can transform their operational efficiency. The resulting gains in data consistency, accuracy, and throughput are not merely incremental; they are foundational to accelerating the discovery of novel therapies and the advancement of precision medicine. The future of biomedical research will be built on these automated, reproducible, and scalable genomic platforms, ultimately translating complex genomic data into actionable health outcomes.
References
- 1. How to Troubleshoot Sequencing Preparation Errors (NGS ... [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 2. What's wrong with my NGS? [https://www.ogt.com/resources/ngs-resources-and-support/ngs-support/whats-wrong-with-my-ngs/]
- 3. Overcoming bias and systematic errors in next generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3025429/]
- 4. The Complete Guide to Automated Sample Preparation for NGS [https://dispendix.com/blog/the-complete-guide-to-automated-sample-preparation-for-ngs]
- 5. Overcoming Challenges in NGS Workflows with Automated ... [https://dispendix.com/blog/overcoming-challenges-in-ngs-workflows-with-automated-sample-prep]
- 6. Avoid Costly Errors in NGS Sample Handling and Library ... [https://seqwell.com/avoid-costly-errors-in-ngs-sample-handling-and-library-prep/]
- 7. How to tackle 3 common challenges when automating ... [https://www.tecan.com/blog/3-common-challenges-when-automating-sample-prep-in-genomics]
- 8. From Bench to Breakthrough: Streamlining NGS Assay ... [https://dispendix.com/blog/ngs-assay-development-challenges]
- 9. Mastering DNA chromatogram analysis in Sanger ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10643650/]
- 10. Next-Generation Sequencing: Principles, Applications, & Advantages [https://www.excedr.com/blog/next-generation-sequencing-101]
- 11. NGS is evolving: collaboration and tech lead the way [https://www.drugtargetreview.com/article/168383/ngs-is-evolving-collaboration-and-tech-lead-the-way/]
- 12. How NGS Automation Improves Library Preparation ... [https://www.euformatics.com/blog-post/how-ngs-automation-improves-library-preparation-efficiency-and-accuracy]
- 13. 3 Innovations in Next-Generation Sequencing Sample Prep [https://dispendix.com/blog/3-innovations-in-next-generation-sequencing-sample-prep]
- 14. Next-generation Sequencing Library Preparation Market ... [https://www.precedenceresearch.com/next-generation-sequencing-library-preparation-market]
- 15. Automation in Genomics Workflows | How Labs Improve ... [https://www.labmanager.com/automation-in-genomics-workflows-driving-precision-efficiency-and-scale-34446]
- 16. The Next-Generation Sequencing Quality Initiative and ... [https://wwwnc.cdc.gov/eid/article/31/13/24-1175_article]
- 17. Automating NGS Workflows [https://www.technologynetworks.com/genomics/infographics/automating-ngs-workflows-401578]
- 18. Integrating Artificial Intelligence in Next-Generation Sequencing [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191491/]
- 19. Toward target 2035: EUbOPEN - a public–private partnership ... [https://pubs.rsc.org/en/content/articlehtml/2025/md/d4md00735b]
- 20. NGS Sequencing Support-Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-support/ngs-support-troubleshooting.html]
- 21. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 22. 2024 Update: Whole Genome Sequencing Costs [https://3billion.io/blog/whole-genome-sequencing-costs-2024-new-prices-and-future-projections]
- 23. Liquid Handling System | Myra by Bio Molecular Systems [https://biomolecularsystems.com/myra-liquid-handling-system/]
- 24. Troubleshooting Industrial Robots: Skills Technicians Need [https://www.uti.edu/blog/robotics-and-automation/troubleshooting-industrial-robots-skills]
- 25. The Ultimate Guide to Automated Liquid Handling in Life ... [https://dispendix.com/blog/the-ultimate-guide-to-automated-liquid-handling-in-life-sciences]
- 26. Automated Liquid Handling for NGS Library Prep [https://formulatrix.com/automated-liquid-handling-for-ngs-library-prep/]
- 27. NGS Software Support – Getting Started [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-software-support/ngs-software-support-getting-started.html]
- 28. NGS: Six top tips to improve your sequencing library [https://www.ogt.com/resources/ngs-resources-and-support/ngs-resources/ngs-six-top-tips-to-improve-your-sequencing-library/]
- 29. 5 Best Practices for NGS Library Prep Success [https://dispendix.com/blog/5-best-practices-for-ngs-library-prep-success]
- 30. Sample Preparation for NGS – A Comprehensive Guide [https://frontlinegenomics.com/sample-preparation-for-ngs-a-comprehensive-guide/]
- 31. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 32. IDT & Beckman Coulter Partner to Automate NGS Workflows [https://lifesciences.danaher.com/us/en/news/automated-ngs-workflows-cancer-research]
- 33. NGS Library Preparation Support—Getting Started [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/next-generation-sequencing-support-center/ngs-library-preparation-support/ngs-library-preparation-support-getting-started.html]
- 34. Modular, open-sourced multiplexing for democratizing spatial ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00286a]
- 35. Troubleshooting [https://support-docs.illumina.com/SW/ClarityLIMS-INT/Content/SW/ClarityLIMS/Integrations/NextSeq_500_550/NextSeq500550Intv23Troubleshooting.htm]
- 36. Troubleshooting [https://support-docs.illumina.com/SW/ClarityLIMS/ClarityINT/Content/SW/ClarityLIMS/Integrations/NovaSeqIntv340ValidationTroubleshooting.htm]
- 37. Data Pipelines That Scientists Can Debug (Without Calling ... [https://boston-wib.org/blog/quicktake/data-pipelines-that-scientists-can-debug-without-calling-you-at-9-pm]
- 38. Garbage In, Garbage Out: Dealing with Data Errors ... [https://blog.omni-inc.com/blog/garbage-in-garbage-out-dealing-with-data-errors-bioinformatics]
- 39. Best LIMS for Precision Medicine in 2025 [https://www.scispot.com/blog/best-lims-for-precision-medicine]
- 40. LIMS integration: Types, benefits, and best practices [https://blackthorn-vision.com/blog/lims-integration/]
- 41. 9 Best Practices for Smooth LIMS Deployment [https://www.1lims.com/blog/9-best-practices-for-lims-implementation]
- 42. Guide to LIMS: Core Functions & 2025 System Comparison [https://intuitionlabs.ai/articles/lims-system-guide-2025]
- 43. NGS Library Preparation [https://www.cd-genomics.com/resource-library-preparation-for-ngs.html]
- 44. Troubleshooting Guide for Cloning [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/troubleshooting-guide-for-cloning?srsltid=AfmBOoqTNZVIYqn41KnUAdrofAn0cd3ADIX38_sw3UQoAZRj60TwgL0s]
- 45. Adapter Ligation technology | Flexibility for many study ... [https://www.illumina.com/techniques/sequencing/ngs-library-prep/ligation.html]
- 46. Error-Free and Optimized Liquid Handling with These ... [https://resources.govsci.com/error-free-liquid-handling/]
- 47. Automated Liquid Handlers As Sources of Error [https://www.bioprocessintl.com/assays/automated-liquid-handlers-as-sources-of-error]
- 48. Reagent formulation and dispensing with CELLSTUDIO ... [https://www.takarabio.com/learning-centers/automation-systems/icell8-introduction/technical-notes/icell8-cx-system-reagent-formulation-and-dispense-guidelines?srsltid=AfmBOop-Fart2H2sIGu3LmAjA9S5BsM1VsyEpA-QpB2MNeGWt8VRM1xA]
- 49. 8 common pipetting errors and how to avoid them | INTEGRA [https://www.integra-biosciences.com/united-states/en/stories/8-common-pipetting-errors-and-simple-solutions-address-them]
- 50. G.PREP NGS Automation [https://dispendix.com/gprep-ngs-automation]
- 51. The Complete Guide to Automated Pipetting [https://dispendix.com/blog/complete-guide-to-automated-pipetting]
- 52. NGS library preparation [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/ngs/dna-sequencing/library-preparation]
- 53. 5 Reasons To Automate Your NGS Workflow [https://opentrons.com/archives/resource/5-reasons-to-automate-your-ngs-workflow?srsltid=AfmBOopbLAegcz0DjQxdFEb-eniPFE26Ap2sTrGb6o3eK-tvwFeyHyNj]
- 54. How-to: NGS Quality Control [https://frontlinegenomics.com/how-to-ngs-quality-control/]
- 55. Automation of customizable library preparation for next- ... [https://www.nature.com/articles/s41598-024-67950-6]
- 56. How to automate NGS library preparation [https://frontlinegenomics.com/how-to-automate-ngs-library-preparation/]
- 57. How to Build the Ideal Lab Work Cell: A Practical Guide for ... [https://highresbio.com/blog/how-to-build-the-ideal-lab-work-cell-a-practical-guide-for-user-friendly-productive-laboratory-automation]
- 58. Library prep automation | Automated NGS protocols [https://www.illumina.com/techniques/sequencing/ngs-library-prep/automation.html]
- 59. Avoiding Common Pitfalls in Lab Automation Best Practices [https://www.wakoautomation.com/avoiding-common-pitfalls-in-laboratory-automation-best-practices-and-solutions]
- 60. Laboratory Automation and IT FAQs [https://www.siemens-healthineers.com/en-us/laboratory-automation/lab-automation-information-technology-faqs]
- 61. Securing Success in Your Automated Lab [https://www.labmanager.com/securing-success-in-your-automated-lab-32252]
- 62. AMP Cell-Free DNA Assay Validations Guideline Summary [https://www.guidelinecentral.com/guideline/3303808]
- 63. Guidelines for Validation of Next-Generation Sequencing– ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6941185/]
- 64. Principles of Analytic Validation of Immunohistochemical ... [https://www.cap.org/protocols-and-guidelines/cap-guidelines/current-cap-guidelines/principles-of-analytic-validation-of-immunohistochemical-assays]
- 65. CAP Updates Their 'Principles of Analytic Validation ... [https://www.bioanalysis-zone.com/cap-updates-their-guidelines-for-principles-of-analytic-validation-of-immunohistochemical-assays/]
- 66. Implementing laboratory automation for next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10373871/]
- 67. Key Strategies for Optimizing NGS Workflows [https://www.technologynetworks.com/genomics/articles/key-strategies-for-optimizing-ngs-workflows-395232]
- 68. Benchmarking Automation vs. Manual Workflows [https://imsnucleii.com/blogs/benchmarking-automation-vs-manual-workflows-this-is-what-you-need-to-know/]
- 69. Automated NGS Workflows for Cancer Research | IDT [http://eupages.idtdna.com/pages/about/news/2025/11/12/integrated-dna-technologies-and-beckman-coulter-life-sciences-partner-to-advance-cancer-research-through-automated-ngs-workflows]
- 70. Making the Most of Your NGS Data: Understanding Metrics ... [https://sequencing.roche.com/us/en/article-listing/metrics-for-target-enriched-ngs.html]
- 71. Coverage Uniformity [https://support.illumina.com/content/dam/illumina-support/help/Illumina_DRAGEN_Bio_IT_Platform_v3_7_1000000141465/Content/SW/Informatics/Dragen/CoverageUniformityCNVCalling_fDG.htm]
- 72. Systematic benchmark of state-of-the-art variant calling ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-022-08365-3]
- 73. Evaluating the accuracy of variant calling methods using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9544674/]
- 74. Next-generation Sequencing Glossary | NGS terminology [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/tutorials/glossary.html]
- 75. Next-Generation Sequencing Illumina Workflow–4 Key Steps [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/next-generation-sequencing/illumina-workflow.html]
- 76. Mastering IVDR in 2025: Challenges and Strategies Across ... [https://www.ul.com/resources/mastering-ivdr-2025-challenges-and-strategies-across-full-compliance-spectrum]
- 77. Guide to Medical Device Requirements Management [https://www.ptc.com/en/blogs/medtech/medical-device-requirements-management]
- 78. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 79. Accurate Library Preparation in NGS Workflows - Uncoded [https://uncoded.in/the-importance-of-accurate-library-preparation-in-ngs-workflows/]
- 80. 7 secrets for success when automating NGS for clinical ... [https://www.tecan.com/blog/next-generation-sequencing-for-clinical-diagnostics-automation]
- 81. Troubleshooting Your First NGS Dataset [https://genomebeans.com/blog/troubleshooting-your-first-ngs-dataset-how-genomebeans-simplifies-it]
- 82. Automated NGS Workflows for Biomarker Discovery | IDT [https://www.idtdna.com/pages/about/news/2025/10/01/integrated-dna-technologies-and-hamilton-company-partner-to-automate-customizable-ngs-workflows-and-accelerate-biomarker-discovery]